User login
Paraphilic disorders: A better understanding
In my role as the Director of The Johns Hopkins Sex and Gender Clinic, I have had the opportunity to provide care to 3 broad categories of patients: patients with sexual dysfunctions, patients experiencing gender dysphoria, and patients manifesting a paraphilic disorder. This article will not address sexual dysfunctions or gender dysphoria, but these terms are defined in the Box1-3 to clearly distinguish them from paraphilic disorders.
Box
Individuals with a sexual dysfunction (eg, erectile dysfunction or anorgasmia) generally experience conventional sexual feelings, but they may have difficulty performing sexually.1 Although ordinarily capable of adequate sexual performance, persons with a paraphilic disorder experience atypical erotic cravings.2 Such cravings can either be for an atypical or unacceptable category of potential partner (eg, animals or children), or for an atypical or unacceptable type of behavior (eg, crossdressing or public exhibitionism). Individuals with gender dysphoria frequently experience distress because their internal sense of feeling either male or female is not congruent with their external physical anatomy.3 The primary concerns of individuals experiencing gender dysphoria relate to feelings of gender identity, as opposed to problems involving erotic arousal.
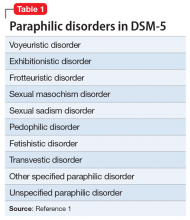
Persons with paraphilic disorders (predominantly males) experience recurrent atypical sexual fantasies and urges that cause clinically significant impairment or distress.1 Those atypical fantasies and urges may be directed towards unacceptable partners such as animals or children, or towards unacceptable behaviors such as public exhibitionism. Table 11 lists the paraphilic disorders identified in DSM-5. This article focuses primarily, though not exclusively, upon pedophilic disorder, and its pharmacologic treatment. However, the rationale underlying such treatment is applicable across the paraphilic spectrum. Before providing such treatment, it is important for clinicians to have a clear conceptual understanding of paraphilic disorders.
When is a difference a disorder?
Cancer and respiration are 2 different biologic phenomenon. Cancer causes suffering and impairment, and as a consequence, we label it a disorder. We do so in the hope of learning more about it, and being able to successfully treat it. We do not classify respiration as a disorder because we do not consider it to be harmful.
The spectrum of human sexuality is quite broad, and psychiatry is generally not concerned with private sexual thoughts and behaviors involving consenting adults that do not cause suffering or impairment. When adults choose to engage in “kinky sex” that causes neither harm nor distress, so be it.
Some individuals may be privately aware of experiencing either an exclusive or nonexclusive sexual attraction to children. Some of these individuals may not be distressed by experiencing such attractions, and may be fully capable of resisting the temptation to enact them. In such an instance, even though an individual may be experiencing sexual attractions that are different from the norm, there may not be a sufficient basis for diagnosing pedophilic disorder. However, that difference in sexual phenomenology (ie, mental experience) could rise to the level of a diagnosable disorder if the individual in question expresses distress about experiencing such attractions, and/or if his capacity to resist acting upon them is impaired.4 Under such circumstances, treatment would be warranted.
Patients with paraphilic disorders deserve treatment
Prior to establishment of the Betty Ford Clinic in 1982, individuals who were drug- or alcohol-dependent were often portrayed in a negative light and referred to by derogatory pejoratives such as “bum” or “pothead.”5 Over time, society came to appreciate that good people, deserving of treatment, can become dependent upon substances, and in recent years there has been considerable support for related research initiatives and humane care. However, there has not been analogous support for individuals who manifest paraphilic disorders, especially those with pedophilic disorder. Instead, such individuals are often perceived as undeserving of mental health care and resources. This has been the case, even though successful treatment of a pedophilic disorder could help prevent the serious consequences of child molestation from occurring.
In contemporary society, the term pedophilia, which is a psychiatric specifier intended to guide research and treatment, has been hijacked by the nonmedical community and turned into a demeaning pejorative. In the collective consciousness of the public, the term pedophilia is routinely and mistakenly equated with the behavior of child molestation. Just as all alcoholics are not drunk drivers, all individuals with pedophilic disorder are not “child molesters.” Conversely, not all “child molesters” have pedophilic disorder.
Continue to: Individuals with other types...
Individuals with other types of paraphilic disorders are frequently similarly maligned and referred to as “perverts” or “deviants.” Public service announcements are frequently aired to reach out to individuals who are depressed, or drug- or alcohol-dependent, or suffering with other forms of mental disorders. When does one hear a public service announcement that encourages young people who may be experiencing disturbing or unacceptable sexual feelings to seek psychiatric treatment? There is a support group on the internet called Virtuous Pedophiles.6 That organization is unequivocally opposed to child molestation, while supporting efforts to improve the mental well-being of individuals who, through no fault of their own, experience unwanted pedophilic feelings.
Causes and noncauses
In attempting to elucidate etiology, researchers typically investigate nature (biology) and/or nurture (life experiences). In terms of the development of pedophilic disorder, there is evidence that both nature and nurture can play a role. Researchers have found that boys who are sexually abused are at increased risk for developing pedophilic disorder, and evidence of temporal lobe disturbances has also been documented in some instances.7,8
From clinical, societal, and forensic perspectives, it may be equally important to identify noncausal factors. Paraphilic disorders, including pedophilic disorder, do not develop as a consequence of volitional choice.9 For example, none of us decide which category, or categories, of potential partners are going to attract us sexually. Rather, in maturing we discover the nature of our own sexuality. Children do not ponder their options, somehow deciding while growing up to be attracted to the opposite sex (heterosexuality), the same sex (homosexuality), or both sexes (bisexuality). Similarly, in maturing into adulthood, individuals do not decide to become sexually attracted to prepubescent children. Who would decide to do that? Instead, unlike most of us, some individuals discover this about themselves; this often is a deeply disturbing insight.
It is not an individual’s fault that he or she has a paraphilic disorder. It is, however, his or her responsibility to do something about it. This may require accessing appropriate psychiatric care.
Why treatment may be needed
Sex is a powerful, biologically based appetite that recurrently craves satiation. God or nature has put that drive into all of us to ensure the survival of humanity. Even when that powerful biologic drive becomes misdirected (for example, towards children, or towards a desire to engage in public exhibitionism), it still recurrently craves satisfaction. It does not require mental health expertise to appreciate what a problematic situation this could become.
Continue to: Some individuals need help...
Some individuals need help in overcoming cravings related to nonsexual appetites. For example, Americans spend millions of dollars each year trying to diet; they often require some form of assistance in order to succeed. Individuals who crave drugs or alcohol often require mental health interventions to abstain because they are unable to consistently resist through willpower alone the powerful biologic urges that drive their actions.
The fundamental mental characteristic of any paraphilic disorder is the presence of intense, recurrent, sexual urges of an atypical nature. In the case of a pedophilic disorder, those urges involve sexual feelings about children.2 In the case of an exhibitionistic disorder, the afflicted individual experiences intense, recurrent sexual fantasies/urges related to exposing his genitals in public.1 Clearly, most men do not have to recurrently fight off the urge to act in such a fashion. Given the driven nature of intense erotic cravings, individuals who experience such cravings will frequently require access to competent mental health care.
Pharmacologic treatment of paraphilic disorders
In the future, we may develop a scientifically based understanding of the biologic factors that underlie qualitative differences in sexuality. At that point, it may become possible to intervene pharmacologically, changing the qualitative nature of a sexual urge with pharmacologic interventions. This cannot yet be done. H
In 1939, a Nobel Prize in Chemistry was awarded for the identification and isolation of the hormone testosterone, which energizes sexual drive.10 If an individual is hungering sexually to expose himself, to view child pornography, or to engage in sexual acts with children, the intensity of such hungers can be significantly reduced by lowering testosterone, thereby enhancing the capacity for successful sexual self-control.
A large body of scientific data has documented a marked decrease in sexually motivated behaviors when testosterone levels are significantly diminished.11 There is also evidence that recidivism rates of sexually motivated crimes can be significantly reduced when testosterone-lowering interventions are used.12
Continue to: Historically, removal of the testes...
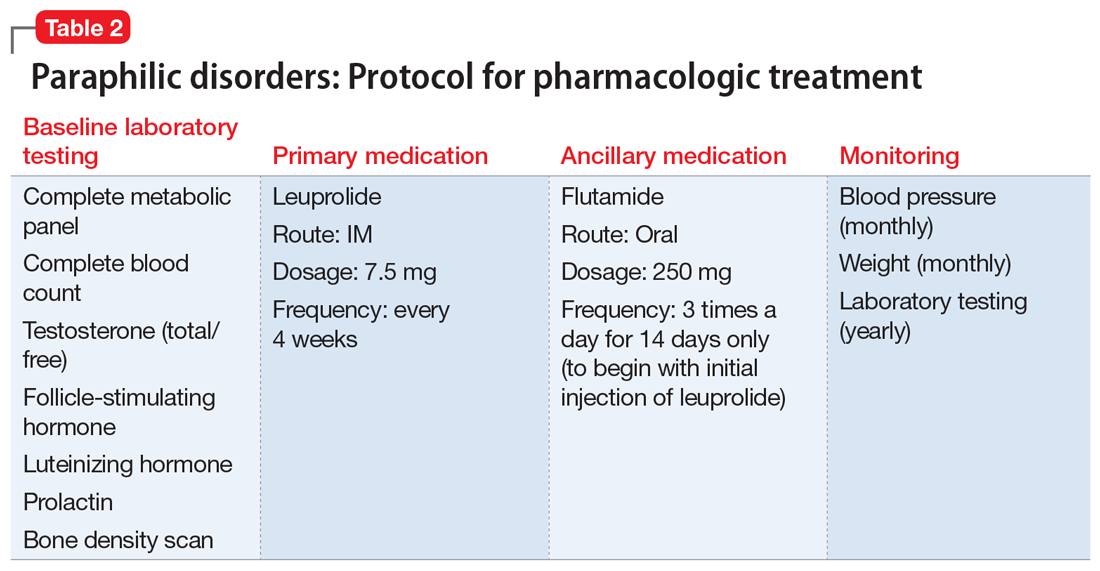
Historically, removal of the testes (surgical castration) had been the only effective way to reliably lower testosterone. Today, this can be achieved pharmacologically. Use of a sex drive–lowering medication should be considered when either the clinician or the patient is concerned that a nonpharmacologic approach may be inadequate. In all instances, a patient with a paraphilic disorder should be informed that pharmacologic treatment is an option. A protocol for the pharmacologic treatment of paraphilic disorders that is based on my clinical experience is summarized in Table 2.
Leuprolide. A depot form of leuprolide is the most commonly employed agent to pharmacologically lower testosterone to treat a paraphilic disorder.13 When injected into muscle, leuprolide binds to it before gradually being released into the bloodstream. Previously, a depot medroxyprogesterone (a form of progesterone) had been used to treat paraphilic disorders.14 However, that had required weekly rather than monthly injections, and carried an increased risk of thrombotic emboli.
Prescribing leuprolide to treat a paraphilic disorder falls under FDA guidelines regarding the use of an approved drug for an “off-label” indication, and therefore is not considered investigational. For treating a paraphilic disorder, an effective dosage of leuprolide is 7.5 mg IM every 4 weeks. Long-term treatment is generally required, analogous to the management of diabetes. Because the initial injection of the series can cause a transient increase in testosterone (prior to its sustained decline), flutamide, a testosterone receptor blocking agent, is ordinarily prescribed for the first 14 days only, following initiation of treatment with depot leuprolide.15 Using flutamide in this fashion prevents the transient increase in testosterone from transiently increasing sexual drive. Flutamide should be discontinued after 14 days because long-term use can result in liver toxicity.
Some clinicians have been hesitant to prescribe leuprolide because of negative connotations associated with the term “chemical castration.” Unlike surgical castration, use of leuprolide is not a physically irreversible intervention, and does not result in sterility (although there may be an increase of atypical sperm and a decrease in total sperm production). The dosage can sometimes be titrated without a loss of efficacy.
In general, leuprolide’s safety protocol is well within the range associated with psychotropic medications.13 Low-risk adverse effects, such as hot flashes or cold sweats, may occur, especially during the period when hormone levels are in transition. There are no absolute contraindications to the use of leuprolide.
Continue to: Other medications
Other medications. Some researchers have suggested treating paraphilic disorders with psychotropic medications known to lower libido, such as selective serotonin reuptake inhibitors (SSRIs).16 However, leuprolide is far more reliable in consistently lowering testosterone and lowering the frequency and intensity of sexual urges. Although psychiatrists unfamiliar with treating paraphilic disorders may feel more comfortable initiating treatment with an SSRI, in my clinical experience, SSRIs have often proven inadequate for this purpose. When it comes to those paraphilic disorders in which treatment failure can result in significant harm (eg, pedophilic disorder), in my judgment, leuprolide should be the pharmacologic treatment of choice.
The opioid antagonist naltrexone has been used clinically to reduce cravings, primarily cravings for alcohol or drugs.17 However, I have not seen convincing evidence that it can be reliably beneficial in treating paraphilic disorders.
Tests to order before starting leuprolide
Long-term use of leuprolide can increase the risk of osteoporosis. Therefore, a baseline bone density scan should be performed before starting a patient on leuprolide. Baseline levels of testosterone, follicle-stimulating hormone, and luteinizing hormone also should be obtained. Patients should have yearly physical examinations, with accompanying laboratory testing. Hematocrit levels are often marginally low after beginning treatment, but not in a clinically significant way. Patients should also undergo routine monitoring for possible weight gain and the potential for associated hypertension. Treatment is predicated upon the known testosterone-suppressing effects of leuprolide, not upon routine monitoring of blood androgen levels.
Pharmacologic treatment of a paraphilic disorder should ordinarily occur in conjunction with nonpharmacologic modalities. One such modality would be group therapy, similar to the type frequently used to treat other craving disorders, such as drug or alcohol dependency.
In recent years, I have seen increasing numbers of patients presenting with a history of accessing and viewing child pornography. Once they have become more aware of the serious consequences of this behavior, most patients have been able to discontinue doing so without pharmacologic treatment. However, for patients in whom that behavior has seemed more driven (suggestive of a variant of voyeuristic disorder), prescription of leuprolide has been beneficial. Under such circumstances, I have diagnosed the patient’s condition as “other specified paraphilic disorder” with elements of pedophilia and voyeurism—the associated behaviors restricted to the voyeuristic viewing of child pornography.18
Continue to: Can treated patients still be sexual?
Can treated patients still be sexual?
If pharmacologic treatment of a paraphilic disorder results in erectile dysfunction, prescription of a medication such as sildenafil can be considered for patients who are in a consenting adult relationship, generally with the knowledge of their partner. Sildenafil can facilitate erectile capacity without increasing sexual drive. It can be helpful to explain to a patient that the purpose of pharmacologic treatment is not to prevent the enjoyment of sexual feelings within the context of a healthy, consenting, adult relationship, but instead to lower the intensity of problematic sexual urges, thereby facilitating sexual self-control. Just as lowering the appetite for food can make it easier to diet but not impossible to eat, lowering sexual appetite can facilitate successful self-control without necessarily interfering with erotic feelings experienced during sexual intimacy.
Bottom Line
Paraphilic disorders are not manifestations of a character flaw, but manifestations of unchosen qualitative differences in the nature of one’s sexual cravings. Not enough is yet known about the biology of sex to be able to pharmacologically alter its qualitative nature. However, pharmacologically lowering the intensity of a patient’s sexual drive can facilitate successful sexual self-regulation.
Related Resources
- LeVay S. Gay, straight and the reason why: the science of sexual orientation. London, UK: Oxford University Press; 2011.
- Rosler A, Witztum E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 1998;338(7):416-422.
- Brown GR. Overview of paraphilic disorders (paraphilias). https://www.merckmanuals.com/professional/psychiatricdisorders/sexuality,-gender-dysphoria,-and-paraphilias/overview-of-paraphilic-disorders.
Drug Brand Names
Flutamide • Eulexin
Leuprolide injection •
Eligard, Lupron Depot
Medroxyprogesterone •
Provera
Naltrexone • Revia, Vivitrol
Progesterone • Prometrium
Sildenafil • Viagra
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:423-450.
2. Berlin FS. Pedophilia: criminal mind-set or mental disorder? A conceptual review. American Journal of Forensic Psychiatry. 2001;32(2):3-25.
3. Berlin FS. A conceptual overview and commentary on gender dysphoria. J Am Acad Psychiatry Law. 2016;44(2):246-252
4. Berlin FS. Pedophilia: when is a difference a disorder: Peer commentaries on Green (2002) and Schmidt (2002). Arch Sex Behav. 2002;31:1-2.
5. Ford B, Chase C. Betty: a glad awakening. New York, NY: Doubleday; 1987.
6. Virtuous Pedophiles. https://www.virped.org/. Accessed September 28, 2018.
7. Freund K, Kuban M. The basis of the abused abuser theory of pedophilia: A further elaboration of an earlier study. Arch Sex Behav. 1994;23(5):553-563.
8. Mendes MF, Chow T, Ringman T, et al. Pedophilia and temporal lobe disturbances. J Neuropsychiatry Clin Neurosci. 2000;12(1):71-76.
9. Money J. Love and love sickness: The science of sex, gender differences, and pair bonding. Baltimore, MD: Johns Hopkins University Press; 1980.
10. The Nobel Prize in Chemistry 1939. https://www.nobelprize.org/prizes/chemistry/1939/summary/. Accessed September 29, 2018.
11. Berlin FS. Commentary: The impact of surgical castration on sexual recidivism risk among civilly committed sex offenders. J Am Acad Psychiatry Law. 2005;33(1):37-41.
12. Hansen H. Treatment of dangerous sexual offenders. In: Seminar on Prison Health Services in Tampere, Finland. Helsinki, Finland: Ministry of Justice, Government Printing Centre; 1991:33-38.
13. Berlin FS. Risk/benefit ratio of androgen deprivation treatment for sex offenders. J Am Acad Psychiatry Law. 2009;37(1):59-62.
14. Berlin FS, Meinecke CF. Treatment of sex offenders with antiandrogenic medication: conceptualization, review of treatment modalities, and preliminary findings. Am J Psychiatry. 1981;138(5):601-607.
15. Neri R. Pharmacology and pharmacokinetics of flutamide. Urology. 1989;34(suppl 4):19-21; discussion 46-56.
16. Adi Y, Ashcroft D, Browne K, et al. Clinical effectiveness and cost consequences of selective serotonin receptor reuptake inhibitors in the treatment of sex offenders. Health Technol Assess. 2002;6(28):1-66.
17. Anton RF. Naltrexone for the management of alcohol dependence. N Engl J Med. 2008;359(7):715-721.
18. Berlin FS. Commentary on pedophilia diagnostic criteria in DSM-5. J Am Acad Psychiatry Law. 2011;39(2):242-244.
In my role as the Director of The Johns Hopkins Sex and Gender Clinic, I have had the opportunity to provide care to 3 broad categories of patients: patients with sexual dysfunctions, patients experiencing gender dysphoria, and patients manifesting a paraphilic disorder. This article will not address sexual dysfunctions or gender dysphoria, but these terms are defined in the Box1-3 to clearly distinguish them from paraphilic disorders.
Box
Individuals with a sexual dysfunction (eg, erectile dysfunction or anorgasmia) generally experience conventional sexual feelings, but they may have difficulty performing sexually.1 Although ordinarily capable of adequate sexual performance, persons with a paraphilic disorder experience atypical erotic cravings.2 Such cravings can either be for an atypical or unacceptable category of potential partner (eg, animals or children), or for an atypical or unacceptable type of behavior (eg, crossdressing or public exhibitionism). Individuals with gender dysphoria frequently experience distress because their internal sense of feeling either male or female is not congruent with their external physical anatomy.3 The primary concerns of individuals experiencing gender dysphoria relate to feelings of gender identity, as opposed to problems involving erotic arousal.
Persons with paraphilic disorders (predominantly males) experience recurrent atypical sexual fantasies and urges that cause clinically significant impairment or distress.1 Those atypical fantasies and urges may be directed towards unacceptable partners such as animals or children, or towards unacceptable behaviors such as public exhibitionism. Table 11 lists the paraphilic disorders identified in DSM-5. This article focuses primarily, though not exclusively, upon pedophilic disorder, and its pharmacologic treatment. However, the rationale underlying such treatment is applicable across the paraphilic spectrum. Before providing such treatment, it is important for clinicians to have a clear conceptual understanding of paraphilic disorders.
When is a difference a disorder?
Cancer and respiration are 2 different biologic phenomenon. Cancer causes suffering and impairment, and as a consequence, we label it a disorder. We do so in the hope of learning more about it, and being able to successfully treat it. We do not classify respiration as a disorder because we do not consider it to be harmful.
The spectrum of human sexuality is quite broad, and psychiatry is generally not concerned with private sexual thoughts and behaviors involving consenting adults that do not cause suffering or impairment. When adults choose to engage in “kinky sex” that causes neither harm nor distress, so be it.
Some individuals may be privately aware of experiencing either an exclusive or nonexclusive sexual attraction to children. Some of these individuals may not be distressed by experiencing such attractions, and may be fully capable of resisting the temptation to enact them. In such an instance, even though an individual may be experiencing sexual attractions that are different from the norm, there may not be a sufficient basis for diagnosing pedophilic disorder. However, that difference in sexual phenomenology (ie, mental experience) could rise to the level of a diagnosable disorder if the individual in question expresses distress about experiencing such attractions, and/or if his capacity to resist acting upon them is impaired.4 Under such circumstances, treatment would be warranted.
Patients with paraphilic disorders deserve treatment
Prior to establishment of the Betty Ford Clinic in 1982, individuals who were drug- or alcohol-dependent were often portrayed in a negative light and referred to by derogatory pejoratives such as “bum” or “pothead.”5 Over time, society came to appreciate that good people, deserving of treatment, can become dependent upon substances, and in recent years there has been considerable support for related research initiatives and humane care. However, there has not been analogous support for individuals who manifest paraphilic disorders, especially those with pedophilic disorder. Instead, such individuals are often perceived as undeserving of mental health care and resources. This has been the case, even though successful treatment of a pedophilic disorder could help prevent the serious consequences of child molestation from occurring.
In contemporary society, the term pedophilia, which is a psychiatric specifier intended to guide research and treatment, has been hijacked by the nonmedical community and turned into a demeaning pejorative. In the collective consciousness of the public, the term pedophilia is routinely and mistakenly equated with the behavior of child molestation. Just as all alcoholics are not drunk drivers, all individuals with pedophilic disorder are not “child molesters.” Conversely, not all “child molesters” have pedophilic disorder.
Continue to: Individuals with other types...
Individuals with other types of paraphilic disorders are frequently similarly maligned and referred to as “perverts” or “deviants.” Public service announcements are frequently aired to reach out to individuals who are depressed, or drug- or alcohol-dependent, or suffering with other forms of mental disorders. When does one hear a public service announcement that encourages young people who may be experiencing disturbing or unacceptable sexual feelings to seek psychiatric treatment? There is a support group on the internet called Virtuous Pedophiles.6 That organization is unequivocally opposed to child molestation, while supporting efforts to improve the mental well-being of individuals who, through no fault of their own, experience unwanted pedophilic feelings.
Causes and noncauses
In attempting to elucidate etiology, researchers typically investigate nature (biology) and/or nurture (life experiences). In terms of the development of pedophilic disorder, there is evidence that both nature and nurture can play a role. Researchers have found that boys who are sexually abused are at increased risk for developing pedophilic disorder, and evidence of temporal lobe disturbances has also been documented in some instances.7,8
From clinical, societal, and forensic perspectives, it may be equally important to identify noncausal factors. Paraphilic disorders, including pedophilic disorder, do not develop as a consequence of volitional choice.9 For example, none of us decide which category, or categories, of potential partners are going to attract us sexually. Rather, in maturing we discover the nature of our own sexuality. Children do not ponder their options, somehow deciding while growing up to be attracted to the opposite sex (heterosexuality), the same sex (homosexuality), or both sexes (bisexuality). Similarly, in maturing into adulthood, individuals do not decide to become sexually attracted to prepubescent children. Who would decide to do that? Instead, unlike most of us, some individuals discover this about themselves; this often is a deeply disturbing insight.
It is not an individual’s fault that he or she has a paraphilic disorder. It is, however, his or her responsibility to do something about it. This may require accessing appropriate psychiatric care.
Why treatment may be needed
Sex is a powerful, biologically based appetite that recurrently craves satiation. God or nature has put that drive into all of us to ensure the survival of humanity. Even when that powerful biologic drive becomes misdirected (for example, towards children, or towards a desire to engage in public exhibitionism), it still recurrently craves satisfaction. It does not require mental health expertise to appreciate what a problematic situation this could become.
Continue to: Some individuals need help...
Some individuals need help in overcoming cravings related to nonsexual appetites. For example, Americans spend millions of dollars each year trying to diet; they often require some form of assistance in order to succeed. Individuals who crave drugs or alcohol often require mental health interventions to abstain because they are unable to consistently resist through willpower alone the powerful biologic urges that drive their actions.
The fundamental mental characteristic of any paraphilic disorder is the presence of intense, recurrent, sexual urges of an atypical nature. In the case of a pedophilic disorder, those urges involve sexual feelings about children.2 In the case of an exhibitionistic disorder, the afflicted individual experiences intense, recurrent sexual fantasies/urges related to exposing his genitals in public.1 Clearly, most men do not have to recurrently fight off the urge to act in such a fashion. Given the driven nature of intense erotic cravings, individuals who experience such cravings will frequently require access to competent mental health care.
Pharmacologic treatment of paraphilic disorders
In the future, we may develop a scientifically based understanding of the biologic factors that underlie qualitative differences in sexuality. At that point, it may become possible to intervene pharmacologically, changing the qualitative nature of a sexual urge with pharmacologic interventions. This cannot yet be done. H
In 1939, a Nobel Prize in Chemistry was awarded for the identification and isolation of the hormone testosterone, which energizes sexual drive.10 If an individual is hungering sexually to expose himself, to view child pornography, or to engage in sexual acts with children, the intensity of such hungers can be significantly reduced by lowering testosterone, thereby enhancing the capacity for successful sexual self-control.
A large body of scientific data has documented a marked decrease in sexually motivated behaviors when testosterone levels are significantly diminished.11 There is also evidence that recidivism rates of sexually motivated crimes can be significantly reduced when testosterone-lowering interventions are used.12
Continue to: Historically, removal of the testes...
Historically, removal of the testes (surgical castration) had been the only effective way to reliably lower testosterone. Today, this can be achieved pharmacologically. Use of a sex drive–lowering medication should be considered when either the clinician or the patient is concerned that a nonpharmacologic approach may be inadequate. In all instances, a patient with a paraphilic disorder should be informed that pharmacologic treatment is an option. A protocol for the pharmacologic treatment of paraphilic disorders that is based on my clinical experience is summarized in Table 2.
Leuprolide. A depot form of leuprolide is the most commonly employed agent to pharmacologically lower testosterone to treat a paraphilic disorder.13 When injected into muscle, leuprolide binds to it before gradually being released into the bloodstream. Previously, a depot medroxyprogesterone (a form of progesterone) had been used to treat paraphilic disorders.14 However, that had required weekly rather than monthly injections, and carried an increased risk of thrombotic emboli.
Prescribing leuprolide to treat a paraphilic disorder falls under FDA guidelines regarding the use of an approved drug for an “off-label” indication, and therefore is not considered investigational. For treating a paraphilic disorder, an effective dosage of leuprolide is 7.5 mg IM every 4 weeks. Long-term treatment is generally required, analogous to the management of diabetes. Because the initial injection of the series can cause a transient increase in testosterone (prior to its sustained decline), flutamide, a testosterone receptor blocking agent, is ordinarily prescribed for the first 14 days only, following initiation of treatment with depot leuprolide.15 Using flutamide in this fashion prevents the transient increase in testosterone from transiently increasing sexual drive. Flutamide should be discontinued after 14 days because long-term use can result in liver toxicity.
Some clinicians have been hesitant to prescribe leuprolide because of negative connotations associated with the term “chemical castration.” Unlike surgical castration, use of leuprolide is not a physically irreversible intervention, and does not result in sterility (although there may be an increase of atypical sperm and a decrease in total sperm production). The dosage can sometimes be titrated without a loss of efficacy.
In general, leuprolide’s safety protocol is well within the range associated with psychotropic medications.13 Low-risk adverse effects, such as hot flashes or cold sweats, may occur, especially during the period when hormone levels are in transition. There are no absolute contraindications to the use of leuprolide.
Continue to: Other medications
Other medications. Some researchers have suggested treating paraphilic disorders with psychotropic medications known to lower libido, such as selective serotonin reuptake inhibitors (SSRIs).16 However, leuprolide is far more reliable in consistently lowering testosterone and lowering the frequency and intensity of sexual urges. Although psychiatrists unfamiliar with treating paraphilic disorders may feel more comfortable initiating treatment with an SSRI, in my clinical experience, SSRIs have often proven inadequate for this purpose. When it comes to those paraphilic disorders in which treatment failure can result in significant harm (eg, pedophilic disorder), in my judgment, leuprolide should be the pharmacologic treatment of choice.
The opioid antagonist naltrexone has been used clinically to reduce cravings, primarily cravings for alcohol or drugs.17 However, I have not seen convincing evidence that it can be reliably beneficial in treating paraphilic disorders.
Tests to order before starting leuprolide
Long-term use of leuprolide can increase the risk of osteoporosis. Therefore, a baseline bone density scan should be performed before starting a patient on leuprolide. Baseline levels of testosterone, follicle-stimulating hormone, and luteinizing hormone also should be obtained. Patients should have yearly physical examinations, with accompanying laboratory testing. Hematocrit levels are often marginally low after beginning treatment, but not in a clinically significant way. Patients should also undergo routine monitoring for possible weight gain and the potential for associated hypertension. Treatment is predicated upon the known testosterone-suppressing effects of leuprolide, not upon routine monitoring of blood androgen levels.
Pharmacologic treatment of a paraphilic disorder should ordinarily occur in conjunction with nonpharmacologic modalities. One such modality would be group therapy, similar to the type frequently used to treat other craving disorders, such as drug or alcohol dependency.
In recent years, I have seen increasing numbers of patients presenting with a history of accessing and viewing child pornography. Once they have become more aware of the serious consequences of this behavior, most patients have been able to discontinue doing so without pharmacologic treatment. However, for patients in whom that behavior has seemed more driven (suggestive of a variant of voyeuristic disorder), prescription of leuprolide has been beneficial. Under such circumstances, I have diagnosed the patient’s condition as “other specified paraphilic disorder” with elements of pedophilia and voyeurism—the associated behaviors restricted to the voyeuristic viewing of child pornography.18
Continue to: Can treated patients still be sexual?
Can treated patients still be sexual?
If pharmacologic treatment of a paraphilic disorder results in erectile dysfunction, prescription of a medication such as sildenafil can be considered for patients who are in a consenting adult relationship, generally with the knowledge of their partner. Sildenafil can facilitate erectile capacity without increasing sexual drive. It can be helpful to explain to a patient that the purpose of pharmacologic treatment is not to prevent the enjoyment of sexual feelings within the context of a healthy, consenting, adult relationship, but instead to lower the intensity of problematic sexual urges, thereby facilitating sexual self-control. Just as lowering the appetite for food can make it easier to diet but not impossible to eat, lowering sexual appetite can facilitate successful self-control without necessarily interfering with erotic feelings experienced during sexual intimacy.
Bottom Line
Paraphilic disorders are not manifestations of a character flaw, but manifestations of unchosen qualitative differences in the nature of one’s sexual cravings. Not enough is yet known about the biology of sex to be able to pharmacologically alter its qualitative nature. However, pharmacologically lowering the intensity of a patient’s sexual drive can facilitate successful sexual self-regulation.
Related Resources
- LeVay S. Gay, straight and the reason why: the science of sexual orientation. London, UK: Oxford University Press; 2011.
- Rosler A, Witztum E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 1998;338(7):416-422.
- Brown GR. Overview of paraphilic disorders (paraphilias). https://www.merckmanuals.com/professional/psychiatricdisorders/sexuality,-gender-dysphoria,-and-paraphilias/overview-of-paraphilic-disorders.
Drug Brand Names
Flutamide • Eulexin
Leuprolide injection •
Eligard, Lupron Depot
Medroxyprogesterone •
Provera
Naltrexone • Revia, Vivitrol
Progesterone • Prometrium
Sildenafil • Viagra
In my role as the Director of The Johns Hopkins Sex and Gender Clinic, I have had the opportunity to provide care to 3 broad categories of patients: patients with sexual dysfunctions, patients experiencing gender dysphoria, and patients manifesting a paraphilic disorder. This article will not address sexual dysfunctions or gender dysphoria, but these terms are defined in the Box1-3 to clearly distinguish them from paraphilic disorders.
Box
Individuals with a sexual dysfunction (eg, erectile dysfunction or anorgasmia) generally experience conventional sexual feelings, but they may have difficulty performing sexually.1 Although ordinarily capable of adequate sexual performance, persons with a paraphilic disorder experience atypical erotic cravings.2 Such cravings can either be for an atypical or unacceptable category of potential partner (eg, animals or children), or for an atypical or unacceptable type of behavior (eg, crossdressing or public exhibitionism). Individuals with gender dysphoria frequently experience distress because their internal sense of feeling either male or female is not congruent with their external physical anatomy.3 The primary concerns of individuals experiencing gender dysphoria relate to feelings of gender identity, as opposed to problems involving erotic arousal.
Persons with paraphilic disorders (predominantly males) experience recurrent atypical sexual fantasies and urges that cause clinically significant impairment or distress.1 Those atypical fantasies and urges may be directed towards unacceptable partners such as animals or children, or towards unacceptable behaviors such as public exhibitionism. Table 11 lists the paraphilic disorders identified in DSM-5. This article focuses primarily, though not exclusively, upon pedophilic disorder, and its pharmacologic treatment. However, the rationale underlying such treatment is applicable across the paraphilic spectrum. Before providing such treatment, it is important for clinicians to have a clear conceptual understanding of paraphilic disorders.
When is a difference a disorder?
Cancer and respiration are 2 different biologic phenomenon. Cancer causes suffering and impairment, and as a consequence, we label it a disorder. We do so in the hope of learning more about it, and being able to successfully treat it. We do not classify respiration as a disorder because we do not consider it to be harmful.
The spectrum of human sexuality is quite broad, and psychiatry is generally not concerned with private sexual thoughts and behaviors involving consenting adults that do not cause suffering or impairment. When adults choose to engage in “kinky sex” that causes neither harm nor distress, so be it.
Some individuals may be privately aware of experiencing either an exclusive or nonexclusive sexual attraction to children. Some of these individuals may not be distressed by experiencing such attractions, and may be fully capable of resisting the temptation to enact them. In such an instance, even though an individual may be experiencing sexual attractions that are different from the norm, there may not be a sufficient basis for diagnosing pedophilic disorder. However, that difference in sexual phenomenology (ie, mental experience) could rise to the level of a diagnosable disorder if the individual in question expresses distress about experiencing such attractions, and/or if his capacity to resist acting upon them is impaired.4 Under such circumstances, treatment would be warranted.
Patients with paraphilic disorders deserve treatment
Prior to establishment of the Betty Ford Clinic in 1982, individuals who were drug- or alcohol-dependent were often portrayed in a negative light and referred to by derogatory pejoratives such as “bum” or “pothead.”5 Over time, society came to appreciate that good people, deserving of treatment, can become dependent upon substances, and in recent years there has been considerable support for related research initiatives and humane care. However, there has not been analogous support for individuals who manifest paraphilic disorders, especially those with pedophilic disorder. Instead, such individuals are often perceived as undeserving of mental health care and resources. This has been the case, even though successful treatment of a pedophilic disorder could help prevent the serious consequences of child molestation from occurring.
In contemporary society, the term pedophilia, which is a psychiatric specifier intended to guide research and treatment, has been hijacked by the nonmedical community and turned into a demeaning pejorative. In the collective consciousness of the public, the term pedophilia is routinely and mistakenly equated with the behavior of child molestation. Just as all alcoholics are not drunk drivers, all individuals with pedophilic disorder are not “child molesters.” Conversely, not all “child molesters” have pedophilic disorder.
Continue to: Individuals with other types...
Individuals with other types of paraphilic disorders are frequently similarly maligned and referred to as “perverts” or “deviants.” Public service announcements are frequently aired to reach out to individuals who are depressed, or drug- or alcohol-dependent, or suffering with other forms of mental disorders. When does one hear a public service announcement that encourages young people who may be experiencing disturbing or unacceptable sexual feelings to seek psychiatric treatment? There is a support group on the internet called Virtuous Pedophiles.6 That organization is unequivocally opposed to child molestation, while supporting efforts to improve the mental well-being of individuals who, through no fault of their own, experience unwanted pedophilic feelings.
Causes and noncauses
In attempting to elucidate etiology, researchers typically investigate nature (biology) and/or nurture (life experiences). In terms of the development of pedophilic disorder, there is evidence that both nature and nurture can play a role. Researchers have found that boys who are sexually abused are at increased risk for developing pedophilic disorder, and evidence of temporal lobe disturbances has also been documented in some instances.7,8
From clinical, societal, and forensic perspectives, it may be equally important to identify noncausal factors. Paraphilic disorders, including pedophilic disorder, do not develop as a consequence of volitional choice.9 For example, none of us decide which category, or categories, of potential partners are going to attract us sexually. Rather, in maturing we discover the nature of our own sexuality. Children do not ponder their options, somehow deciding while growing up to be attracted to the opposite sex (heterosexuality), the same sex (homosexuality), or both sexes (bisexuality). Similarly, in maturing into adulthood, individuals do not decide to become sexually attracted to prepubescent children. Who would decide to do that? Instead, unlike most of us, some individuals discover this about themselves; this often is a deeply disturbing insight.
It is not an individual’s fault that he or she has a paraphilic disorder. It is, however, his or her responsibility to do something about it. This may require accessing appropriate psychiatric care.
Why treatment may be needed
Sex is a powerful, biologically based appetite that recurrently craves satiation. God or nature has put that drive into all of us to ensure the survival of humanity. Even when that powerful biologic drive becomes misdirected (for example, towards children, or towards a desire to engage in public exhibitionism), it still recurrently craves satisfaction. It does not require mental health expertise to appreciate what a problematic situation this could become.
Continue to: Some individuals need help...
Some individuals need help in overcoming cravings related to nonsexual appetites. For example, Americans spend millions of dollars each year trying to diet; they often require some form of assistance in order to succeed. Individuals who crave drugs or alcohol often require mental health interventions to abstain because they are unable to consistently resist through willpower alone the powerful biologic urges that drive their actions.
The fundamental mental characteristic of any paraphilic disorder is the presence of intense, recurrent, sexual urges of an atypical nature. In the case of a pedophilic disorder, those urges involve sexual feelings about children.2 In the case of an exhibitionistic disorder, the afflicted individual experiences intense, recurrent sexual fantasies/urges related to exposing his genitals in public.1 Clearly, most men do not have to recurrently fight off the urge to act in such a fashion. Given the driven nature of intense erotic cravings, individuals who experience such cravings will frequently require access to competent mental health care.
Pharmacologic treatment of paraphilic disorders
In the future, we may develop a scientifically based understanding of the biologic factors that underlie qualitative differences in sexuality. At that point, it may become possible to intervene pharmacologically, changing the qualitative nature of a sexual urge with pharmacologic interventions. This cannot yet be done. H
In 1939, a Nobel Prize in Chemistry was awarded for the identification and isolation of the hormone testosterone, which energizes sexual drive.10 If an individual is hungering sexually to expose himself, to view child pornography, or to engage in sexual acts with children, the intensity of such hungers can be significantly reduced by lowering testosterone, thereby enhancing the capacity for successful sexual self-control.
A large body of scientific data has documented a marked decrease in sexually motivated behaviors when testosterone levels are significantly diminished.11 There is also evidence that recidivism rates of sexually motivated crimes can be significantly reduced when testosterone-lowering interventions are used.12
Continue to: Historically, removal of the testes...
Historically, removal of the testes (surgical castration) had been the only effective way to reliably lower testosterone. Today, this can be achieved pharmacologically. Use of a sex drive–lowering medication should be considered when either the clinician or the patient is concerned that a nonpharmacologic approach may be inadequate. In all instances, a patient with a paraphilic disorder should be informed that pharmacologic treatment is an option. A protocol for the pharmacologic treatment of paraphilic disorders that is based on my clinical experience is summarized in Table 2.
Leuprolide. A depot form of leuprolide is the most commonly employed agent to pharmacologically lower testosterone to treat a paraphilic disorder.13 When injected into muscle, leuprolide binds to it before gradually being released into the bloodstream. Previously, a depot medroxyprogesterone (a form of progesterone) had been used to treat paraphilic disorders.14 However, that had required weekly rather than monthly injections, and carried an increased risk of thrombotic emboli.
Prescribing leuprolide to treat a paraphilic disorder falls under FDA guidelines regarding the use of an approved drug for an “off-label” indication, and therefore is not considered investigational. For treating a paraphilic disorder, an effective dosage of leuprolide is 7.5 mg IM every 4 weeks. Long-term treatment is generally required, analogous to the management of diabetes. Because the initial injection of the series can cause a transient increase in testosterone (prior to its sustained decline), flutamide, a testosterone receptor blocking agent, is ordinarily prescribed for the first 14 days only, following initiation of treatment with depot leuprolide.15 Using flutamide in this fashion prevents the transient increase in testosterone from transiently increasing sexual drive. Flutamide should be discontinued after 14 days because long-term use can result in liver toxicity.
Some clinicians have been hesitant to prescribe leuprolide because of negative connotations associated with the term “chemical castration.” Unlike surgical castration, use of leuprolide is not a physically irreversible intervention, and does not result in sterility (although there may be an increase of atypical sperm and a decrease in total sperm production). The dosage can sometimes be titrated without a loss of efficacy.
In general, leuprolide’s safety protocol is well within the range associated with psychotropic medications.13 Low-risk adverse effects, such as hot flashes or cold sweats, may occur, especially during the period when hormone levels are in transition. There are no absolute contraindications to the use of leuprolide.
Continue to: Other medications
Other medications. Some researchers have suggested treating paraphilic disorders with psychotropic medications known to lower libido, such as selective serotonin reuptake inhibitors (SSRIs).16 However, leuprolide is far more reliable in consistently lowering testosterone and lowering the frequency and intensity of sexual urges. Although psychiatrists unfamiliar with treating paraphilic disorders may feel more comfortable initiating treatment with an SSRI, in my clinical experience, SSRIs have often proven inadequate for this purpose. When it comes to those paraphilic disorders in which treatment failure can result in significant harm (eg, pedophilic disorder), in my judgment, leuprolide should be the pharmacologic treatment of choice.
The opioid antagonist naltrexone has been used clinically to reduce cravings, primarily cravings for alcohol or drugs.17 However, I have not seen convincing evidence that it can be reliably beneficial in treating paraphilic disorders.
Tests to order before starting leuprolide
Long-term use of leuprolide can increase the risk of osteoporosis. Therefore, a baseline bone density scan should be performed before starting a patient on leuprolide. Baseline levels of testosterone, follicle-stimulating hormone, and luteinizing hormone also should be obtained. Patients should have yearly physical examinations, with accompanying laboratory testing. Hematocrit levels are often marginally low after beginning treatment, but not in a clinically significant way. Patients should also undergo routine monitoring for possible weight gain and the potential for associated hypertension. Treatment is predicated upon the known testosterone-suppressing effects of leuprolide, not upon routine monitoring of blood androgen levels.
Pharmacologic treatment of a paraphilic disorder should ordinarily occur in conjunction with nonpharmacologic modalities. One such modality would be group therapy, similar to the type frequently used to treat other craving disorders, such as drug or alcohol dependency.
In recent years, I have seen increasing numbers of patients presenting with a history of accessing and viewing child pornography. Once they have become more aware of the serious consequences of this behavior, most patients have been able to discontinue doing so without pharmacologic treatment. However, for patients in whom that behavior has seemed more driven (suggestive of a variant of voyeuristic disorder), prescription of leuprolide has been beneficial. Under such circumstances, I have diagnosed the patient’s condition as “other specified paraphilic disorder” with elements of pedophilia and voyeurism—the associated behaviors restricted to the voyeuristic viewing of child pornography.18
Continue to: Can treated patients still be sexual?
Can treated patients still be sexual?
If pharmacologic treatment of a paraphilic disorder results in erectile dysfunction, prescription of a medication such as sildenafil can be considered for patients who are in a consenting adult relationship, generally with the knowledge of their partner. Sildenafil can facilitate erectile capacity without increasing sexual drive. It can be helpful to explain to a patient that the purpose of pharmacologic treatment is not to prevent the enjoyment of sexual feelings within the context of a healthy, consenting, adult relationship, but instead to lower the intensity of problematic sexual urges, thereby facilitating sexual self-control. Just as lowering the appetite for food can make it easier to diet but not impossible to eat, lowering sexual appetite can facilitate successful self-control without necessarily interfering with erotic feelings experienced during sexual intimacy.
Bottom Line
Paraphilic disorders are not manifestations of a character flaw, but manifestations of unchosen qualitative differences in the nature of one’s sexual cravings. Not enough is yet known about the biology of sex to be able to pharmacologically alter its qualitative nature. However, pharmacologically lowering the intensity of a patient’s sexual drive can facilitate successful sexual self-regulation.
Related Resources
- LeVay S. Gay, straight and the reason why: the science of sexual orientation. London, UK: Oxford University Press; 2011.
- Rosler A, Witztum E. Treatment of men with paraphilia with a long-acting analogue of gonadotropin-releasing hormone. N Engl J Med. 1998;338(7):416-422.
- Brown GR. Overview of paraphilic disorders (paraphilias). https://www.merckmanuals.com/professional/psychiatricdisorders/sexuality,-gender-dysphoria,-and-paraphilias/overview-of-paraphilic-disorders.
Drug Brand Names
Flutamide • Eulexin
Leuprolide injection •
Eligard, Lupron Depot
Medroxyprogesterone •
Provera
Naltrexone • Revia, Vivitrol
Progesterone • Prometrium
Sildenafil • Viagra
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:423-450.
2. Berlin FS. Pedophilia: criminal mind-set or mental disorder? A conceptual review. American Journal of Forensic Psychiatry. 2001;32(2):3-25.
3. Berlin FS. A conceptual overview and commentary on gender dysphoria. J Am Acad Psychiatry Law. 2016;44(2):246-252
4. Berlin FS. Pedophilia: when is a difference a disorder: Peer commentaries on Green (2002) and Schmidt (2002). Arch Sex Behav. 2002;31:1-2.
5. Ford B, Chase C. Betty: a glad awakening. New York, NY: Doubleday; 1987.
6. Virtuous Pedophiles. https://www.virped.org/. Accessed September 28, 2018.
7. Freund K, Kuban M. The basis of the abused abuser theory of pedophilia: A further elaboration of an earlier study. Arch Sex Behav. 1994;23(5):553-563.
8. Mendes MF, Chow T, Ringman T, et al. Pedophilia and temporal lobe disturbances. J Neuropsychiatry Clin Neurosci. 2000;12(1):71-76.
9. Money J. Love and love sickness: The science of sex, gender differences, and pair bonding. Baltimore, MD: Johns Hopkins University Press; 1980.
10. The Nobel Prize in Chemistry 1939. https://www.nobelprize.org/prizes/chemistry/1939/summary/. Accessed September 29, 2018.
11. Berlin FS. Commentary: The impact of surgical castration on sexual recidivism risk among civilly committed sex offenders. J Am Acad Psychiatry Law. 2005;33(1):37-41.
12. Hansen H. Treatment of dangerous sexual offenders. In: Seminar on Prison Health Services in Tampere, Finland. Helsinki, Finland: Ministry of Justice, Government Printing Centre; 1991:33-38.
13. Berlin FS. Risk/benefit ratio of androgen deprivation treatment for sex offenders. J Am Acad Psychiatry Law. 2009;37(1):59-62.
14. Berlin FS, Meinecke CF. Treatment of sex offenders with antiandrogenic medication: conceptualization, review of treatment modalities, and preliminary findings. Am J Psychiatry. 1981;138(5):601-607.
15. Neri R. Pharmacology and pharmacokinetics of flutamide. Urology. 1989;34(suppl 4):19-21; discussion 46-56.
16. Adi Y, Ashcroft D, Browne K, et al. Clinical effectiveness and cost consequences of selective serotonin receptor reuptake inhibitors in the treatment of sex offenders. Health Technol Assess. 2002;6(28):1-66.
17. Anton RF. Naltrexone for the management of alcohol dependence. N Engl J Med. 2008;359(7):715-721.
18. Berlin FS. Commentary on pedophilia diagnostic criteria in DSM-5. J Am Acad Psychiatry Law. 2011;39(2):242-244.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013:423-450.
2. Berlin FS. Pedophilia: criminal mind-set or mental disorder? A conceptual review. American Journal of Forensic Psychiatry. 2001;32(2):3-25.
3. Berlin FS. A conceptual overview and commentary on gender dysphoria. J Am Acad Psychiatry Law. 2016;44(2):246-252
4. Berlin FS. Pedophilia: when is a difference a disorder: Peer commentaries on Green (2002) and Schmidt (2002). Arch Sex Behav. 2002;31:1-2.
5. Ford B, Chase C. Betty: a glad awakening. New York, NY: Doubleday; 1987.
6. Virtuous Pedophiles. https://www.virped.org/. Accessed September 28, 2018.
7. Freund K, Kuban M. The basis of the abused abuser theory of pedophilia: A further elaboration of an earlier study. Arch Sex Behav. 1994;23(5):553-563.
8. Mendes MF, Chow T, Ringman T, et al. Pedophilia and temporal lobe disturbances. J Neuropsychiatry Clin Neurosci. 2000;12(1):71-76.
9. Money J. Love and love sickness: The science of sex, gender differences, and pair bonding. Baltimore, MD: Johns Hopkins University Press; 1980.
10. The Nobel Prize in Chemistry 1939. https://www.nobelprize.org/prizes/chemistry/1939/summary/. Accessed September 29, 2018.
11. Berlin FS. Commentary: The impact of surgical castration on sexual recidivism risk among civilly committed sex offenders. J Am Acad Psychiatry Law. 2005;33(1):37-41.
12. Hansen H. Treatment of dangerous sexual offenders. In: Seminar on Prison Health Services in Tampere, Finland. Helsinki, Finland: Ministry of Justice, Government Printing Centre; 1991:33-38.
13. Berlin FS. Risk/benefit ratio of androgen deprivation treatment for sex offenders. J Am Acad Psychiatry Law. 2009;37(1):59-62.
14. Berlin FS, Meinecke CF. Treatment of sex offenders with antiandrogenic medication: conceptualization, review of treatment modalities, and preliminary findings. Am J Psychiatry. 1981;138(5):601-607.
15. Neri R. Pharmacology and pharmacokinetics of flutamide. Urology. 1989;34(suppl 4):19-21; discussion 46-56.
16. Adi Y, Ashcroft D, Browne K, et al. Clinical effectiveness and cost consequences of selective serotonin receptor reuptake inhibitors in the treatment of sex offenders. Health Technol Assess. 2002;6(28):1-66.
17. Anton RF. Naltrexone for the management of alcohol dependence. N Engl J Med. 2008;359(7):715-721.
18. Berlin FS. Commentary on pedophilia diagnostic criteria in DSM-5. J Am Acad Psychiatry Law. 2011;39(2):242-244.