User login
CHMP backs approval of caplacizumab
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval of caplacizumab (Cablivi) for the treatment of adults with acquired thrombotic thrombocytopenic purpura (aTTP).
Caplacizumab is a humanized bivalent nanobody that inhibits the interaction between von Willebrand factor and platelets.
The CHMP’s recommendation regarding caplacizumab will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The CHMP’s opinion of caplacizumab is supported by data from the phase 2 TITAN study and the phase 3 HERCULES study.
TITAN trial
Results from TITAN were published in NEJM in 2016. TITAN included 75 aTTP patients who were randomized to caplacizumab (n=36) or placebo (n=39), with all patients receiving the current standard of care (daily plasma exchange and immunosuppressive therapy).
The study’s primary endpoint was time to response (platelet count normalization). Patients in the caplacizumab arm had a 39% reduction in the median time to response compared to patients in the placebo arm (P=0.005).
Among the 69 patients who had not undergone a plasma-exchange session before enrollment, the median time to response was 3.0 days in the caplacizumab arm and 4.9 days in the placebo arm.
Among the 6 patients who did undergo a plasma-exchange session before enrollment, the median time to a response was 2.4 days in the caplacizumab arm and 4.3 days in the placebo arm.
The rate of confirmed response was 86.1% (n=31) in the caplacizumab arm and 71.8% (n=28) in the placebo arm.
There were 541 adverse events (AEs) in 34 of the 35 evaluable patients receiving caplacizumab (97%) and 522 AEs in all 37 evaluable patients receiving placebo (100%). TTP exacerbations and relapses were not included as AEs.
The rate of AEs thought to be related to the study drug was 17% in the caplacizumab arm and 11% in the placebo arm. The rate of AEs that were possibly related was 54% and 8%, respectively. And the rate of serious AEs was 37% and 32%, respectively.
There were no deaths in the caplacizumab arm and 2 in the placebo arm. One death was due to severe, refractory TTP, and the other was due to cerebral hemorrhage.
HERCULES trial
Results from HERCULES were presented at the 2017 ASH Annual Meeting.
The study enrolled patients with an acute episode of aTTP. They were randomized to receive either caplacizumab (n=72) or placebo (n=73) in addition to standard care, which consisted of plasma exchange and immunosuppression.
The study’s primary endpoint was the time to normalization of platelet count response, which was defined as an initial platelet count of at least 150 x 109/L with subsequent stop of daily plasma exchange within 5 days.
There was a significant reduction in time to platelet count response in the caplacizumab arm compared to the placebo arm. The platelet normalization rate ratio was 1.55 (P<0.01).
A secondary endpoint was the combination of aTTP-related death, aTTP recurrence, and at least 1 major thromboembolic event during study treatment. The incidence of this combined endpoint was 12.7% (n=9) in the caplacizumab arm and 49.3% (n=36) in the placebo arm (P<0.0001).
The incidence of aTTP-related death was 0% (n=0) in the caplacizumab arm and 4.1% (n=3) in the placebo arm. The incidence of aTTP recurrence was 4.2% (n=3) and 38.4% (n=28), respectively. And the incidence of at least 1 major thromboembolic event was 8.5% (n=6) and 8.2% (n=6), respectively.
The proportion of patients with at least 1 study-drug-related AE was 57.7% in the caplacizumab arm and 43.8% in the placebo arm. The proportion of patients with at least 1 study-drug-related serious AE was 14.1% (n=10) and 5.5% (n=4), respectively. The rate of discontinuation due to at least 1 AE was 7.0% and 12.3%, respectively.
During the treatment period, there were no deaths in the caplacizumab arm and 3 deaths in the placebo arm. There was 1 death in the caplacizumab arm during the follow-up period, but it was considered unrelated to caplacizumab.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval of caplacizumab (Cablivi) for the treatment of adults with acquired thrombotic thrombocytopenic purpura (aTTP).
Caplacizumab is a humanized bivalent nanobody that inhibits the interaction between von Willebrand factor and platelets.
The CHMP’s recommendation regarding caplacizumab will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The CHMP’s opinion of caplacizumab is supported by data from the phase 2 TITAN study and the phase 3 HERCULES study.
TITAN trial
Results from TITAN were published in NEJM in 2016. TITAN included 75 aTTP patients who were randomized to caplacizumab (n=36) or placebo (n=39), with all patients receiving the current standard of care (daily plasma exchange and immunosuppressive therapy).
The study’s primary endpoint was time to response (platelet count normalization). Patients in the caplacizumab arm had a 39% reduction in the median time to response compared to patients in the placebo arm (P=0.005).
Among the 69 patients who had not undergone a plasma-exchange session before enrollment, the median time to response was 3.0 days in the caplacizumab arm and 4.9 days in the placebo arm.
Among the 6 patients who did undergo a plasma-exchange session before enrollment, the median time to a response was 2.4 days in the caplacizumab arm and 4.3 days in the placebo arm.
The rate of confirmed response was 86.1% (n=31) in the caplacizumab arm and 71.8% (n=28) in the placebo arm.
There were 541 adverse events (AEs) in 34 of the 35 evaluable patients receiving caplacizumab (97%) and 522 AEs in all 37 evaluable patients receiving placebo (100%). TTP exacerbations and relapses were not included as AEs.
The rate of AEs thought to be related to the study drug was 17% in the caplacizumab arm and 11% in the placebo arm. The rate of AEs that were possibly related was 54% and 8%, respectively. And the rate of serious AEs was 37% and 32%, respectively.
There were no deaths in the caplacizumab arm and 2 in the placebo arm. One death was due to severe, refractory TTP, and the other was due to cerebral hemorrhage.
HERCULES trial
Results from HERCULES were presented at the 2017 ASH Annual Meeting.
The study enrolled patients with an acute episode of aTTP. They were randomized to receive either caplacizumab (n=72) or placebo (n=73) in addition to standard care, which consisted of plasma exchange and immunosuppression.
The study’s primary endpoint was the time to normalization of platelet count response, which was defined as an initial platelet count of at least 150 x 109/L with subsequent stop of daily plasma exchange within 5 days.
There was a significant reduction in time to platelet count response in the caplacizumab arm compared to the placebo arm. The platelet normalization rate ratio was 1.55 (P<0.01).
A secondary endpoint was the combination of aTTP-related death, aTTP recurrence, and at least 1 major thromboembolic event during study treatment. The incidence of this combined endpoint was 12.7% (n=9) in the caplacizumab arm and 49.3% (n=36) in the placebo arm (P<0.0001).
The incidence of aTTP-related death was 0% (n=0) in the caplacizumab arm and 4.1% (n=3) in the placebo arm. The incidence of aTTP recurrence was 4.2% (n=3) and 38.4% (n=28), respectively. And the incidence of at least 1 major thromboembolic event was 8.5% (n=6) and 8.2% (n=6), respectively.
The proportion of patients with at least 1 study-drug-related AE was 57.7% in the caplacizumab arm and 43.8% in the placebo arm. The proportion of patients with at least 1 study-drug-related serious AE was 14.1% (n=10) and 5.5% (n=4), respectively. The rate of discontinuation due to at least 1 AE was 7.0% and 12.3%, respectively.
During the treatment period, there were no deaths in the caplacizumab arm and 3 deaths in the placebo arm. There was 1 death in the caplacizumab arm during the follow-up period, but it was considered unrelated to caplacizumab.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval of caplacizumab (Cablivi) for the treatment of adults with acquired thrombotic thrombocytopenic purpura (aTTP).
Caplacizumab is a humanized bivalent nanobody that inhibits the interaction between von Willebrand factor and platelets.
The CHMP’s recommendation regarding caplacizumab will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The CHMP’s opinion of caplacizumab is supported by data from the phase 2 TITAN study and the phase 3 HERCULES study.
TITAN trial
Results from TITAN were published in NEJM in 2016. TITAN included 75 aTTP patients who were randomized to caplacizumab (n=36) or placebo (n=39), with all patients receiving the current standard of care (daily plasma exchange and immunosuppressive therapy).
The study’s primary endpoint was time to response (platelet count normalization). Patients in the caplacizumab arm had a 39% reduction in the median time to response compared to patients in the placebo arm (P=0.005).
Among the 69 patients who had not undergone a plasma-exchange session before enrollment, the median time to response was 3.0 days in the caplacizumab arm and 4.9 days in the placebo arm.
Among the 6 patients who did undergo a plasma-exchange session before enrollment, the median time to a response was 2.4 days in the caplacizumab arm and 4.3 days in the placebo arm.
The rate of confirmed response was 86.1% (n=31) in the caplacizumab arm and 71.8% (n=28) in the placebo arm.
There were 541 adverse events (AEs) in 34 of the 35 evaluable patients receiving caplacizumab (97%) and 522 AEs in all 37 evaluable patients receiving placebo (100%). TTP exacerbations and relapses were not included as AEs.
The rate of AEs thought to be related to the study drug was 17% in the caplacizumab arm and 11% in the placebo arm. The rate of AEs that were possibly related was 54% and 8%, respectively. And the rate of serious AEs was 37% and 32%, respectively.
There were no deaths in the caplacizumab arm and 2 in the placebo arm. One death was due to severe, refractory TTP, and the other was due to cerebral hemorrhage.
HERCULES trial
Results from HERCULES were presented at the 2017 ASH Annual Meeting.
The study enrolled patients with an acute episode of aTTP. They were randomized to receive either caplacizumab (n=72) or placebo (n=73) in addition to standard care, which consisted of plasma exchange and immunosuppression.
The study’s primary endpoint was the time to normalization of platelet count response, which was defined as an initial platelet count of at least 150 x 109/L with subsequent stop of daily plasma exchange within 5 days.
There was a significant reduction in time to platelet count response in the caplacizumab arm compared to the placebo arm. The platelet normalization rate ratio was 1.55 (P<0.01).
A secondary endpoint was the combination of aTTP-related death, aTTP recurrence, and at least 1 major thromboembolic event during study treatment. The incidence of this combined endpoint was 12.7% (n=9) in the caplacizumab arm and 49.3% (n=36) in the placebo arm (P<0.0001).
The incidence of aTTP-related death was 0% (n=0) in the caplacizumab arm and 4.1% (n=3) in the placebo arm. The incidence of aTTP recurrence was 4.2% (n=3) and 38.4% (n=28), respectively. And the incidence of at least 1 major thromboembolic event was 8.5% (n=6) and 8.2% (n=6), respectively.
The proportion of patients with at least 1 study-drug-related AE was 57.7% in the caplacizumab arm and 43.8% in the placebo arm. The proportion of patients with at least 1 study-drug-related serious AE was 14.1% (n=10) and 5.5% (n=4), respectively. The rate of discontinuation due to at least 1 AE was 7.0% and 12.3%, respectively.
During the treatment period, there were no deaths in the caplacizumab arm and 3 deaths in the placebo arm. There was 1 death in the caplacizumab arm during the follow-up period, but it was considered unrelated to caplacizumab.
CHMP recommends CAR T for ALL, DLBCL
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended the approval of tisagenlecleucel (Kymriah®, formerly CTL019) for 2 indications.
According to the CHMP, the chimeric antigen receptor (CAR) T-cell therapy should be approved to treat adults with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) who have received 2 or more lines of systemic therapy and patients up to 25 years of age who have B-cell acute lymphoblastic leukemia (ALL) that is refractory, in relapse post-transplant, or in second or later relapse.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The CHMP’s recommendation is based on results from a pair of phase 2 trials—ELIANA and JULIET.
JULIET trial
Updated results from JULIET were presented at the recent 23rd Annual Congress of the European Hematology Association (EHA) as abstract S799.
The trial enrolled 165 adults with relapsed/refractory DLBCL, and 111 of them received a single infusion of tisagenlecleucel. Most of the patients who discontinued before dosing did so due to disease progression or clinical deterioration. The patients’ median age at baseline was 56 (range, 22-76).
Ninety-two percent of patients received bridging therapy, and 93% received lymphodepleting chemotherapy prior to tisagenlecleucel.
The median time from infusion to data cutoff was 13.9 months.
The overall response rate was 52%, and the complete response (CR) rate was 40%. Of the patients in CR at month 3, 83% remained in CR at month 12. The median duration of response was not reached.
At the time of data cutoff, none of the responders had proceeded to stem cell transplant.
For all infused patients (n=111), the 12-month overall survival (OS) rate was 49%, and the median OS was 11.7 months. The median OS was not reached for patients in CR.
Within 8 weeks of tisagenlecleucel infusion, 22% of patients had developed grade 3/4 cytokine release syndrome (CRS). Fifteen percent of patients received tocilizumab for CRS, including 3% of patients with grade 2 CRS and 50% of patients with grade 3 CRS.
Other adverse events (AEs) of interest included grade 3/4 neurologic events (12%), grade 3/4 cytopenias lasting more than 28 days (32%), grade 3/4 infections (20%), and grade 3/4 febrile neutropenia (15%).
ELIANA trial
Updated results from ELIANA were published in NEJM in February.
The trial included 75 children and young adults with relapsed/refractory ALL. The patients’ median age was 11 (range, 3 to 23).
All 75 patients received a single infusion of tisagenlecleucel, and 72 received lymphodepleting chemotherapy.
The median duration of follow-up was 13.1 months. The study’s primary endpoint was overall remission rate, which was defined as the rate of a best overall response of either CR or CR with incomplete hematologic recovery (CRi) within 3 months.
The overall remission rate was 81% (61/75), with 60% of patients (n=45) achieving a CR and 21% (n=16) achieving a CRi.
All patients whose best response was CR/CRi were negative for minimal residual disease. The median duration of response was not met.
Eight patients proceeded to transplant while in remission. At last follow-up, 4 were still in remission, and 4 had unknown disease status.
At 6 months, the event-free survival rate was 73%, and the OS rate was 90%. At 12 months, the rates were 50% and 76%, respectively.
All patients experienced at least 1 AE, and 95% had AEs thought to be related to tisagenlecleucel. The rate of grade 3/4 AEs was 88%, and the rate of related grade 3/4 AEs was 73%.
AEs of special interest included CRS (77%), neurologic events (40%), infections (43%), febrile neutropenia (35%), cytopenias not resolved by day 28 (37%), and tumor lysis syndrome (4%).
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended the approval of tisagenlecleucel (Kymriah®, formerly CTL019) for 2 indications.
According to the CHMP, the chimeric antigen receptor (CAR) T-cell therapy should be approved to treat adults with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) who have received 2 or more lines of systemic therapy and patients up to 25 years of age who have B-cell acute lymphoblastic leukemia (ALL) that is refractory, in relapse post-transplant, or in second or later relapse.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The CHMP’s recommendation is based on results from a pair of phase 2 trials—ELIANA and JULIET.
JULIET trial
Updated results from JULIET were presented at the recent 23rd Annual Congress of the European Hematology Association (EHA) as abstract S799.
The trial enrolled 165 adults with relapsed/refractory DLBCL, and 111 of them received a single infusion of tisagenlecleucel. Most of the patients who discontinued before dosing did so due to disease progression or clinical deterioration. The patients’ median age at baseline was 56 (range, 22-76).
Ninety-two percent of patients received bridging therapy, and 93% received lymphodepleting chemotherapy prior to tisagenlecleucel.
The median time from infusion to data cutoff was 13.9 months.
The overall response rate was 52%, and the complete response (CR) rate was 40%. Of the patients in CR at month 3, 83% remained in CR at month 12. The median duration of response was not reached.
At the time of data cutoff, none of the responders had proceeded to stem cell transplant.
For all infused patients (n=111), the 12-month overall survival (OS) rate was 49%, and the median OS was 11.7 months. The median OS was not reached for patients in CR.
Within 8 weeks of tisagenlecleucel infusion, 22% of patients had developed grade 3/4 cytokine release syndrome (CRS). Fifteen percent of patients received tocilizumab for CRS, including 3% of patients with grade 2 CRS and 50% of patients with grade 3 CRS.
Other adverse events (AEs) of interest included grade 3/4 neurologic events (12%), grade 3/4 cytopenias lasting more than 28 days (32%), grade 3/4 infections (20%), and grade 3/4 febrile neutropenia (15%).
ELIANA trial
Updated results from ELIANA were published in NEJM in February.
The trial included 75 children and young adults with relapsed/refractory ALL. The patients’ median age was 11 (range, 3 to 23).
All 75 patients received a single infusion of tisagenlecleucel, and 72 received lymphodepleting chemotherapy.
The median duration of follow-up was 13.1 months. The study’s primary endpoint was overall remission rate, which was defined as the rate of a best overall response of either CR or CR with incomplete hematologic recovery (CRi) within 3 months.
The overall remission rate was 81% (61/75), with 60% of patients (n=45) achieving a CR and 21% (n=16) achieving a CRi.
All patients whose best response was CR/CRi were negative for minimal residual disease. The median duration of response was not met.
Eight patients proceeded to transplant while in remission. At last follow-up, 4 were still in remission, and 4 had unknown disease status.
At 6 months, the event-free survival rate was 73%, and the OS rate was 90%. At 12 months, the rates were 50% and 76%, respectively.
All patients experienced at least 1 AE, and 95% had AEs thought to be related to tisagenlecleucel. The rate of grade 3/4 AEs was 88%, and the rate of related grade 3/4 AEs was 73%.
AEs of special interest included CRS (77%), neurologic events (40%), infections (43%), febrile neutropenia (35%), cytopenias not resolved by day 28 (37%), and tumor lysis syndrome (4%).
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended the approval of tisagenlecleucel (Kymriah®, formerly CTL019) for 2 indications.
According to the CHMP, the chimeric antigen receptor (CAR) T-cell therapy should be approved to treat adults with relapsed/refractory diffuse large B-cell lymphoma (DLBCL) who have received 2 or more lines of systemic therapy and patients up to 25 years of age who have B-cell acute lymphoblastic leukemia (ALL) that is refractory, in relapse post-transplant, or in second or later relapse.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The CHMP’s recommendation is based on results from a pair of phase 2 trials—ELIANA and JULIET.
JULIET trial
Updated results from JULIET were presented at the recent 23rd Annual Congress of the European Hematology Association (EHA) as abstract S799.
The trial enrolled 165 adults with relapsed/refractory DLBCL, and 111 of them received a single infusion of tisagenlecleucel. Most of the patients who discontinued before dosing did so due to disease progression or clinical deterioration. The patients’ median age at baseline was 56 (range, 22-76).
Ninety-two percent of patients received bridging therapy, and 93% received lymphodepleting chemotherapy prior to tisagenlecleucel.
The median time from infusion to data cutoff was 13.9 months.
The overall response rate was 52%, and the complete response (CR) rate was 40%. Of the patients in CR at month 3, 83% remained in CR at month 12. The median duration of response was not reached.
At the time of data cutoff, none of the responders had proceeded to stem cell transplant.
For all infused patients (n=111), the 12-month overall survival (OS) rate was 49%, and the median OS was 11.7 months. The median OS was not reached for patients in CR.
Within 8 weeks of tisagenlecleucel infusion, 22% of patients had developed grade 3/4 cytokine release syndrome (CRS). Fifteen percent of patients received tocilizumab for CRS, including 3% of patients with grade 2 CRS and 50% of patients with grade 3 CRS.
Other adverse events (AEs) of interest included grade 3/4 neurologic events (12%), grade 3/4 cytopenias lasting more than 28 days (32%), grade 3/4 infections (20%), and grade 3/4 febrile neutropenia (15%).
ELIANA trial
Updated results from ELIANA were published in NEJM in February.
The trial included 75 children and young adults with relapsed/refractory ALL. The patients’ median age was 11 (range, 3 to 23).
All 75 patients received a single infusion of tisagenlecleucel, and 72 received lymphodepleting chemotherapy.
The median duration of follow-up was 13.1 months. The study’s primary endpoint was overall remission rate, which was defined as the rate of a best overall response of either CR or CR with incomplete hematologic recovery (CRi) within 3 months.
The overall remission rate was 81% (61/75), with 60% of patients (n=45) achieving a CR and 21% (n=16) achieving a CRi.
All patients whose best response was CR/CRi were negative for minimal residual disease. The median duration of response was not met.
Eight patients proceeded to transplant while in remission. At last follow-up, 4 were still in remission, and 4 had unknown disease status.
At 6 months, the event-free survival rate was 73%, and the OS rate was 90%. At 12 months, the rates were 50% and 76%, respectively.
All patients experienced at least 1 AE, and 95% had AEs thought to be related to tisagenlecleucel. The rate of grade 3/4 AEs was 88%, and the rate of related grade 3/4 AEs was 73%.
AEs of special interest included CRS (77%), neurologic events (40%), infections (43%), febrile neutropenia (35%), cytopenias not resolved by day 28 (37%), and tumor lysis syndrome (4%).
CHMP recommends CAR T for DLBCL, PMBCL
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for the chimeric antigen receptor (CAR) T-cell therapy axicabtagene ciloleucel (Yescarta®, formerly KTE-C19).
The recommendation pertains to axicabtagene ciloleucel as a treatment for adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) or primary mediastinal large B-cell lymphoma (PMBCL) who have received 2 or more lines of systemic therapy.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The marketing authorization application for axicabtagene ciloleucel is supported by data from the ZUMA-1 trial.
Results from this phase 2 trial were presented at the 2017 ASH Annual Meeting and published simultaneously in NEJM.
The trial enrolled 111 patients with relapsed/refractory B-cell lymphomas. There were 101 patients who received axicabtagene ciloleucel—77 with DLBCL, 8 with PMBCL, and 16 with transformed follicular lymphoma (TFL).
Patients received conditioning with low-dose cyclophosphamide and fludarabine, followed by axicabtagene ciloleucel.
The objective response rate (ORR) was 82% (n=83), and the complete response (CR) rate was 54% (n=55).
Among the DLBCL patients, the ORR was 82% (63/77), and the CR rate was 49% (38/77). In the patients with PMBCL or TFL, the ORR was 83% (20/24), and the CR rate was 71% (17/24).
With a median follow-up of 15.4 months, 42% of patients retained their response, and 40% retained a CR.
At 18 months, the overall survival was 52%. Most deaths were due to disease progression.
However, 2 patients died of adverse events related to axicabtagene ciloleucel, both cytokine release syndrome (CRS).
The most common grade 3 or higher adverse events were neutropenia (78%), anemia (43%), thrombocytopenia (38%), and febrile neutropenia (31%).
Grade 3 or higher CRS occurred in 13% of patients, and grade 3 or higher neurologic events occurred in 28%.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for the chimeric antigen receptor (CAR) T-cell therapy axicabtagene ciloleucel (Yescarta®, formerly KTE-C19).
The recommendation pertains to axicabtagene ciloleucel as a treatment for adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) or primary mediastinal large B-cell lymphoma (PMBCL) who have received 2 or more lines of systemic therapy.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The marketing authorization application for axicabtagene ciloleucel is supported by data from the ZUMA-1 trial.
Results from this phase 2 trial were presented at the 2017 ASH Annual Meeting and published simultaneously in NEJM.
The trial enrolled 111 patients with relapsed/refractory B-cell lymphomas. There were 101 patients who received axicabtagene ciloleucel—77 with DLBCL, 8 with PMBCL, and 16 with transformed follicular lymphoma (TFL).
Patients received conditioning with low-dose cyclophosphamide and fludarabine, followed by axicabtagene ciloleucel.
The objective response rate (ORR) was 82% (n=83), and the complete response (CR) rate was 54% (n=55).
Among the DLBCL patients, the ORR was 82% (63/77), and the CR rate was 49% (38/77). In the patients with PMBCL or TFL, the ORR was 83% (20/24), and the CR rate was 71% (17/24).
With a median follow-up of 15.4 months, 42% of patients retained their response, and 40% retained a CR.
At 18 months, the overall survival was 52%. Most deaths were due to disease progression.
However, 2 patients died of adverse events related to axicabtagene ciloleucel, both cytokine release syndrome (CRS).
The most common grade 3 or higher adverse events were neutropenia (78%), anemia (43%), thrombocytopenia (38%), and febrile neutropenia (31%).
Grade 3 or higher CRS occurred in 13% of patients, and grade 3 or higher neurologic events occurred in 28%.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for the chimeric antigen receptor (CAR) T-cell therapy axicabtagene ciloleucel (Yescarta®, formerly KTE-C19).
The recommendation pertains to axicabtagene ciloleucel as a treatment for adults with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) or primary mediastinal large B-cell lymphoma (PMBCL) who have received 2 or more lines of systemic therapy.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
The marketing authorization application for axicabtagene ciloleucel is supported by data from the ZUMA-1 trial.
Results from this phase 2 trial were presented at the 2017 ASH Annual Meeting and published simultaneously in NEJM.
The trial enrolled 111 patients with relapsed/refractory B-cell lymphomas. There were 101 patients who received axicabtagene ciloleucel—77 with DLBCL, 8 with PMBCL, and 16 with transformed follicular lymphoma (TFL).
Patients received conditioning with low-dose cyclophosphamide and fludarabine, followed by axicabtagene ciloleucel.
The objective response rate (ORR) was 82% (n=83), and the complete response (CR) rate was 54% (n=55).
Among the DLBCL patients, the ORR was 82% (63/77), and the CR rate was 49% (38/77). In the patients with PMBCL or TFL, the ORR was 83% (20/24), and the CR rate was 71% (17/24).
With a median follow-up of 15.4 months, 42% of patients retained their response, and 40% retained a CR.
At 18 months, the overall survival was 52%. Most deaths were due to disease progression.
However, 2 patients died of adverse events related to axicabtagene ciloleucel, both cytokine release syndrome (CRS).
The most common grade 3 or higher adverse events were neutropenia (78%), anemia (43%), thrombocytopenia (38%), and febrile neutropenia (31%).
Grade 3 or higher CRS occurred in 13% of patients, and grade 3 or higher neurologic events occurred in 28%.
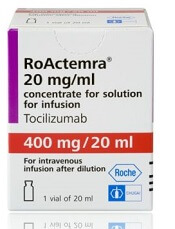
CHMP backs expanded approval of tocilizumab
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the approved use of tocilizumab (RoActemra).
The recommendation is for tocilizumab to treat adults and pediatric patients age 2 and older who have severe or life-threatening cytokine release syndrome (CRS) induced by chimeric antigen receptor (CAR) T-cell therapy.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
Tocilizumab is a humanized interleukin-6 receptor antagonist marketed by Roche Registration GmbH.
The drug is already approved by the European Commission to treat rheumatoid arthritis, active systemic juvenile idiopathic arthritis, and juvenile idiopathic polyarthritis.
The CHMP’s recommendation to expand the approved use of tocilizumab is supported by results from a retrospective analysis of data from clinical trials of CAR T-cell therapies in patients with hematologic malignancies.
For this analysis, researchers assessed 45 pediatric and adult patients treated with tocilizumab, with or without additional high-dose corticosteroids, for severe or life-threatening CRS.
Thirty-one patients (69%) achieved a response, defined as resolution of CRS within 14 days of the first dose of tocilizumab.
No more than 2 doses of tocilizumab were needed, and no drugs other than tocilizumab and corticosteroids were used for treatment.
No adverse reactions related to tocilizumab were reported.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the approved use of tocilizumab (RoActemra).
The recommendation is for tocilizumab to treat adults and pediatric patients age 2 and older who have severe or life-threatening cytokine release syndrome (CRS) induced by chimeric antigen receptor (CAR) T-cell therapy.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
Tocilizumab is a humanized interleukin-6 receptor antagonist marketed by Roche Registration GmbH.
The drug is already approved by the European Commission to treat rheumatoid arthritis, active systemic juvenile idiopathic arthritis, and juvenile idiopathic polyarthritis.
The CHMP’s recommendation to expand the approved use of tocilizumab is supported by results from a retrospective analysis of data from clinical trials of CAR T-cell therapies in patients with hematologic malignancies.
For this analysis, researchers assessed 45 pediatric and adult patients treated with tocilizumab, with or without additional high-dose corticosteroids, for severe or life-threatening CRS.
Thirty-one patients (69%) achieved a response, defined as resolution of CRS within 14 days of the first dose of tocilizumab.
No more than 2 doses of tocilizumab were needed, and no drugs other than tocilizumab and corticosteroids were used for treatment.
No adverse reactions related to tocilizumab were reported.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the approved use of tocilizumab (RoActemra).
The recommendation is for tocilizumab to treat adults and pediatric patients age 2 and older who have severe or life-threatening cytokine release syndrome (CRS) induced by chimeric antigen receptor (CAR) T-cell therapy.
The CHMP’s recommendation will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of the CHMP’s recommendation.
Tocilizumab is a humanized interleukin-6 receptor antagonist marketed by Roche Registration GmbH.
The drug is already approved by the European Commission to treat rheumatoid arthritis, active systemic juvenile idiopathic arthritis, and juvenile idiopathic polyarthritis.
The CHMP’s recommendation to expand the approved use of tocilizumab is supported by results from a retrospective analysis of data from clinical trials of CAR T-cell therapies in patients with hematologic malignancies.
For this analysis, researchers assessed 45 pediatric and adult patients treated with tocilizumab, with or without additional high-dose corticosteroids, for severe or life-threatening CRS.
Thirty-one patients (69%) achieved a response, defined as resolution of CRS within 14 days of the first dose of tocilizumab.
No more than 2 doses of tocilizumab were needed, and no drugs other than tocilizumab and corticosteroids were used for treatment.
No adverse reactions related to tocilizumab were reported.
FDA lifts hold on trial of MYC inhibitor
The US Food and Drug Administration (FDA) has lifted the clinical hold on a phase 1b trial of APTO-253.
APTO-253 is a small molecule that inhibits expression of the c-Myc oncogene without causing general myelosuppression of the bone marrow, according to Aptose Biosciences Inc., the company developing the drug.
Aptose was testing APTO-253 in a phase 1b trial of patients with relapsed or refractory acute myeloid leukemia (AML) or high-risk myelodysplastic syndromes (MDS) before the FDA put the trial on hold in November 2015.
The hold was placed after an event that occurred during dosing at a clinical site. The event was stoppage of an intravenous infusion pump that was caused by back pressure resulting from clogging of the in-line filter.
Aptose said no drug-related serious adverse events were reported, and the observed pharmacokinetic levels in patients treated with APTO-253 were within the expected range.
However, a review revealed concerns about the documentation records of the manufacturing procedures associated with APTO-253. So Aptose voluntarily stopped dosing in the phase 1b trial, and the FDA placed the trial on hold.
A root cause investigation revealed that the event with the infusion pump resulted from chemistry and manufacturing-based issues.
Therefore, Aptose developed a new formulation of APTO-253 that did not cause filter clogging or pump stoppage during simulated infusion studies.
Now that the FDA has lifted the hold on the phase 1b trial, Aptose said screening and dosing will resume “as soon as practicable.”
“We are eager to return APTO-253 back into the clinic,” said William G. Rice, PhD, chairman, president and chief executive officer of Aptose.
“Our understanding of this molecule has evolved dramatically, and we are excited to deliver a MYC gene expression inhibitor to patients with debilitating hematologic malignancies.”
The phase 1b trial is designed to assess the safety, tolerability, pharmacokinetics, pharmacodynamics, and efficacy of APTO-253 as a single agent and determine the recommended phase 2 dose of the drug.
APTO-253 will be administered once weekly, over a 28-day cycle. The dose-escalation cohort of the study could potentially enroll up to 20 patients with relapsed or refractory AML or high-risk MDS. The study is designed to then transition, as appropriate, to single-agent expansion cohorts in AML and MDS.
The US Food and Drug Administration (FDA) has lifted the clinical hold on a phase 1b trial of APTO-253.
APTO-253 is a small molecule that inhibits expression of the c-Myc oncogene without causing general myelosuppression of the bone marrow, according to Aptose Biosciences Inc., the company developing the drug.
Aptose was testing APTO-253 in a phase 1b trial of patients with relapsed or refractory acute myeloid leukemia (AML) or high-risk myelodysplastic syndromes (MDS) before the FDA put the trial on hold in November 2015.
The hold was placed after an event that occurred during dosing at a clinical site. The event was stoppage of an intravenous infusion pump that was caused by back pressure resulting from clogging of the in-line filter.
Aptose said no drug-related serious adverse events were reported, and the observed pharmacokinetic levels in patients treated with APTO-253 were within the expected range.
However, a review revealed concerns about the documentation records of the manufacturing procedures associated with APTO-253. So Aptose voluntarily stopped dosing in the phase 1b trial, and the FDA placed the trial on hold.
A root cause investigation revealed that the event with the infusion pump resulted from chemistry and manufacturing-based issues.
Therefore, Aptose developed a new formulation of APTO-253 that did not cause filter clogging or pump stoppage during simulated infusion studies.
Now that the FDA has lifted the hold on the phase 1b trial, Aptose said screening and dosing will resume “as soon as practicable.”
“We are eager to return APTO-253 back into the clinic,” said William G. Rice, PhD, chairman, president and chief executive officer of Aptose.
“Our understanding of this molecule has evolved dramatically, and we are excited to deliver a MYC gene expression inhibitor to patients with debilitating hematologic malignancies.”
The phase 1b trial is designed to assess the safety, tolerability, pharmacokinetics, pharmacodynamics, and efficacy of APTO-253 as a single agent and determine the recommended phase 2 dose of the drug.
APTO-253 will be administered once weekly, over a 28-day cycle. The dose-escalation cohort of the study could potentially enroll up to 20 patients with relapsed or refractory AML or high-risk MDS. The study is designed to then transition, as appropriate, to single-agent expansion cohorts in AML and MDS.
The US Food and Drug Administration (FDA) has lifted the clinical hold on a phase 1b trial of APTO-253.
APTO-253 is a small molecule that inhibits expression of the c-Myc oncogene without causing general myelosuppression of the bone marrow, according to Aptose Biosciences Inc., the company developing the drug.
Aptose was testing APTO-253 in a phase 1b trial of patients with relapsed or refractory acute myeloid leukemia (AML) or high-risk myelodysplastic syndromes (MDS) before the FDA put the trial on hold in November 2015.
The hold was placed after an event that occurred during dosing at a clinical site. The event was stoppage of an intravenous infusion pump that was caused by back pressure resulting from clogging of the in-line filter.
Aptose said no drug-related serious adverse events were reported, and the observed pharmacokinetic levels in patients treated with APTO-253 were within the expected range.
However, a review revealed concerns about the documentation records of the manufacturing procedures associated with APTO-253. So Aptose voluntarily stopped dosing in the phase 1b trial, and the FDA placed the trial on hold.
A root cause investigation revealed that the event with the infusion pump resulted from chemistry and manufacturing-based issues.
Therefore, Aptose developed a new formulation of APTO-253 that did not cause filter clogging or pump stoppage during simulated infusion studies.
Now that the FDA has lifted the hold on the phase 1b trial, Aptose said screening and dosing will resume “as soon as practicable.”
“We are eager to return APTO-253 back into the clinic,” said William G. Rice, PhD, chairman, president and chief executive officer of Aptose.
“Our understanding of this molecule has evolved dramatically, and we are excited to deliver a MYC gene expression inhibitor to patients with debilitating hematologic malignancies.”
The phase 1b trial is designed to assess the safety, tolerability, pharmacokinetics, pharmacodynamics, and efficacy of APTO-253 as a single agent and determine the recommended phase 2 dose of the drug.
APTO-253 will be administered once weekly, over a 28-day cycle. The dose-escalation cohort of the study could potentially enroll up to 20 patients with relapsed or refractory AML or high-risk MDS. The study is designed to then transition, as appropriate, to single-agent expansion cohorts in AML and MDS.
Doc reports favorable results from trial on hold
STOCKHOLM—Interim trial results suggest the EZH2 inhibitor tazemetostat can produce durable responses in patients with relapsed or refractory follicular lymphoma (FL).
In patients with EZH2 mutations, the overall response rate (ORR) was 71%, and the median duration of response (DOR) was 32 weeks.
For patients with wild-type (WT) EZH2, the ORR was 33%, and the median DOR was 76 weeks.
Tazemetostat was considered generally well tolerated in this phase 2 trial, which is currently on partial clinical hold.
Gilles Salles, MD, PhD, of the University Hospital of Lyon France, presented results from the trial at the 23rd Congress of the European Hematology Association (EHA) as abstract S100.
The trial is sponsored by Epizyme, Inc.
In April, Epizyme announced that all US-based trials of tazemetostat had been placed on partial hold after a pediatric patient on a phase 1 trial developed secondary T-cell lymphoma.
Enrollment was stopped in all the trials, but patients could continue receiving tazemetostat if they had not progressed on the drug.
The phase 2 trial of tazemetostat in non-Hodgkin lymphoma has enrolled 89 adults with relapsed/refractory FL.
At EHA, Dr Salles presented results in 82 of these patients. There were 28 patients with EZH2-mutated FL and 54 with EZH2-WT FL.
The median age was 61 in both cohorts. Forty-three percent of EZH2-mutated and 63% of WT patients were male.
EZH2-mutated patients had a median of 3 prior therapies, and WT patients had a median of 4. Thirty-eight percent and 42%, respectively, were refractory to their last therapy. Eleven percent and 39%, respectively, had received prior transplant.
The median time from diagnosis was 5.1 years for EZH2-mutated patients and 6.4 years for WT patients. The median time from last prior therapy was 18.4 weeks and 28.1 weeks, respectively.
The patients received tazemetostat at 800 mg twice daily until disease progression or withdrawal.
Safety
In all 82 patients, the rate of treatment-emergent adverse events (AEs) was 95%, and the rate of treatment-related AEs was 78%. The rate of grade 3 or higher treatment-related AEs was 17%, and the rate of serious treatment-related AEs was 4%.
Six percent of patients discontinued treatment due to a related AE, 18% had a dose interruption, and 5% had a dose reduction due to a related AE.
Treatment-related AEs included nausea (20%), fatigue (13%), anemia (13%), diarrhea (11%), alopecia (11%), asthenia (10%), thrombocytopenia (10%), muscle spasms (6%), bronchitis (5%), vomiting (5%), headache (5%), abdominal pain (2%), pyrexia (1%), and cough (1%).
Grade 3 or higher treatment-related AEs included thrombocytopenia (4%), anemia (4%), fatigue (1%), and asthenia (1%).
Efficacy
In the EZH2-mutated cohort, the ORR was 71% (n=20). Eleven percent of patients (n=3) achieved a complete response, and 61% (n=17) had a partial response.
Twenty-nine percent (n=8) had stable disease as their best response. And 21% (n=6) of patients are still on study with stable disease.
All patients in this cohort experienced a reduction in tumor burden. None of the patients had progressive disease as their best response.
At the time of analysis (May 1, 2018), the median DOR was 32.3 weeks, and 55% of responders (n=11) had an ongoing response.
The median progression-free survival was 48.6 weeks.
In patients with WT EZH2 (n=54), the ORR was 33% (n=18). Six percent of patients (n=3) achieved a complete response, and 28% (n=15) had a partial response.
Thirty-one percent of patients (n=17) had stable disease as their best response, including 1 patient who is still receiving treatment.
Thirty-one percent of patients (n=17) progressed. For 4% (n=2), their response status was unknown.
At the time of analysis, the median DOR was 76 weeks, and 56% of responders (n=10) had an ongoing response.
The median progression-free survival was 29.9 weeks.
“I am impressed by the sustained clinical activity and the good tolerability of tazemetostat in this heavily pretreated patient population,” Dr Salles said. “This is important for patients with relapsed or refractory follicular lymphoma, as both the response rates and durations of response usually tend to decrease with each successive line of treatment.”
“I believe tazemetostat has the potential to fill a significant unmet need for these patients, and continued investigation of tazemetostat as a single agent or in combination with other agents is warranted.”
Epizyme’s president and chief executive officer, Robert Bazemore, said the company is still working to resolve the partial clinical hold on tazemetostat trials and is “making good progress.”
STOCKHOLM—Interim trial results suggest the EZH2 inhibitor tazemetostat can produce durable responses in patients with relapsed or refractory follicular lymphoma (FL).
In patients with EZH2 mutations, the overall response rate (ORR) was 71%, and the median duration of response (DOR) was 32 weeks.
For patients with wild-type (WT) EZH2, the ORR was 33%, and the median DOR was 76 weeks.
Tazemetostat was considered generally well tolerated in this phase 2 trial, which is currently on partial clinical hold.
Gilles Salles, MD, PhD, of the University Hospital of Lyon France, presented results from the trial at the 23rd Congress of the European Hematology Association (EHA) as abstract S100.
The trial is sponsored by Epizyme, Inc.
In April, Epizyme announced that all US-based trials of tazemetostat had been placed on partial hold after a pediatric patient on a phase 1 trial developed secondary T-cell lymphoma.
Enrollment was stopped in all the trials, but patients could continue receiving tazemetostat if they had not progressed on the drug.
The phase 2 trial of tazemetostat in non-Hodgkin lymphoma has enrolled 89 adults with relapsed/refractory FL.
At EHA, Dr Salles presented results in 82 of these patients. There were 28 patients with EZH2-mutated FL and 54 with EZH2-WT FL.
The median age was 61 in both cohorts. Forty-three percent of EZH2-mutated and 63% of WT patients were male.
EZH2-mutated patients had a median of 3 prior therapies, and WT patients had a median of 4. Thirty-eight percent and 42%, respectively, were refractory to their last therapy. Eleven percent and 39%, respectively, had received prior transplant.
The median time from diagnosis was 5.1 years for EZH2-mutated patients and 6.4 years for WT patients. The median time from last prior therapy was 18.4 weeks and 28.1 weeks, respectively.
The patients received tazemetostat at 800 mg twice daily until disease progression or withdrawal.
Safety
In all 82 patients, the rate of treatment-emergent adverse events (AEs) was 95%, and the rate of treatment-related AEs was 78%. The rate of grade 3 or higher treatment-related AEs was 17%, and the rate of serious treatment-related AEs was 4%.
Six percent of patients discontinued treatment due to a related AE, 18% had a dose interruption, and 5% had a dose reduction due to a related AE.
Treatment-related AEs included nausea (20%), fatigue (13%), anemia (13%), diarrhea (11%), alopecia (11%), asthenia (10%), thrombocytopenia (10%), muscle spasms (6%), bronchitis (5%), vomiting (5%), headache (5%), abdominal pain (2%), pyrexia (1%), and cough (1%).
Grade 3 or higher treatment-related AEs included thrombocytopenia (4%), anemia (4%), fatigue (1%), and asthenia (1%).
Efficacy
In the EZH2-mutated cohort, the ORR was 71% (n=20). Eleven percent of patients (n=3) achieved a complete response, and 61% (n=17) had a partial response.
Twenty-nine percent (n=8) had stable disease as their best response. And 21% (n=6) of patients are still on study with stable disease.
All patients in this cohort experienced a reduction in tumor burden. None of the patients had progressive disease as their best response.
At the time of analysis (May 1, 2018), the median DOR was 32.3 weeks, and 55% of responders (n=11) had an ongoing response.
The median progression-free survival was 48.6 weeks.
In patients with WT EZH2 (n=54), the ORR was 33% (n=18). Six percent of patients (n=3) achieved a complete response, and 28% (n=15) had a partial response.
Thirty-one percent of patients (n=17) had stable disease as their best response, including 1 patient who is still receiving treatment.
Thirty-one percent of patients (n=17) progressed. For 4% (n=2), their response status was unknown.
At the time of analysis, the median DOR was 76 weeks, and 56% of responders (n=10) had an ongoing response.
The median progression-free survival was 29.9 weeks.
“I am impressed by the sustained clinical activity and the good tolerability of tazemetostat in this heavily pretreated patient population,” Dr Salles said. “This is important for patients with relapsed or refractory follicular lymphoma, as both the response rates and durations of response usually tend to decrease with each successive line of treatment.”
“I believe tazemetostat has the potential to fill a significant unmet need for these patients, and continued investigation of tazemetostat as a single agent or in combination with other agents is warranted.”
Epizyme’s president and chief executive officer, Robert Bazemore, said the company is still working to resolve the partial clinical hold on tazemetostat trials and is “making good progress.”
STOCKHOLM—Interim trial results suggest the EZH2 inhibitor tazemetostat can produce durable responses in patients with relapsed or refractory follicular lymphoma (FL).
In patients with EZH2 mutations, the overall response rate (ORR) was 71%, and the median duration of response (DOR) was 32 weeks.
For patients with wild-type (WT) EZH2, the ORR was 33%, and the median DOR was 76 weeks.
Tazemetostat was considered generally well tolerated in this phase 2 trial, which is currently on partial clinical hold.
Gilles Salles, MD, PhD, of the University Hospital of Lyon France, presented results from the trial at the 23rd Congress of the European Hematology Association (EHA) as abstract S100.
The trial is sponsored by Epizyme, Inc.
In April, Epizyme announced that all US-based trials of tazemetostat had been placed on partial hold after a pediatric patient on a phase 1 trial developed secondary T-cell lymphoma.
Enrollment was stopped in all the trials, but patients could continue receiving tazemetostat if they had not progressed on the drug.
The phase 2 trial of tazemetostat in non-Hodgkin lymphoma has enrolled 89 adults with relapsed/refractory FL.
At EHA, Dr Salles presented results in 82 of these patients. There were 28 patients with EZH2-mutated FL and 54 with EZH2-WT FL.
The median age was 61 in both cohorts. Forty-three percent of EZH2-mutated and 63% of WT patients were male.
EZH2-mutated patients had a median of 3 prior therapies, and WT patients had a median of 4. Thirty-eight percent and 42%, respectively, were refractory to their last therapy. Eleven percent and 39%, respectively, had received prior transplant.
The median time from diagnosis was 5.1 years for EZH2-mutated patients and 6.4 years for WT patients. The median time from last prior therapy was 18.4 weeks and 28.1 weeks, respectively.
The patients received tazemetostat at 800 mg twice daily until disease progression or withdrawal.
Safety
In all 82 patients, the rate of treatment-emergent adverse events (AEs) was 95%, and the rate of treatment-related AEs was 78%. The rate of grade 3 or higher treatment-related AEs was 17%, and the rate of serious treatment-related AEs was 4%.
Six percent of patients discontinued treatment due to a related AE, 18% had a dose interruption, and 5% had a dose reduction due to a related AE.
Treatment-related AEs included nausea (20%), fatigue (13%), anemia (13%), diarrhea (11%), alopecia (11%), asthenia (10%), thrombocytopenia (10%), muscle spasms (6%), bronchitis (5%), vomiting (5%), headache (5%), abdominal pain (2%), pyrexia (1%), and cough (1%).
Grade 3 or higher treatment-related AEs included thrombocytopenia (4%), anemia (4%), fatigue (1%), and asthenia (1%).
Efficacy
In the EZH2-mutated cohort, the ORR was 71% (n=20). Eleven percent of patients (n=3) achieved a complete response, and 61% (n=17) had a partial response.
Twenty-nine percent (n=8) had stable disease as their best response. And 21% (n=6) of patients are still on study with stable disease.
All patients in this cohort experienced a reduction in tumor burden. None of the patients had progressive disease as their best response.
At the time of analysis (May 1, 2018), the median DOR was 32.3 weeks, and 55% of responders (n=11) had an ongoing response.
The median progression-free survival was 48.6 weeks.
In patients with WT EZH2 (n=54), the ORR was 33% (n=18). Six percent of patients (n=3) achieved a complete response, and 28% (n=15) had a partial response.
Thirty-one percent of patients (n=17) had stable disease as their best response, including 1 patient who is still receiving treatment.
Thirty-one percent of patients (n=17) progressed. For 4% (n=2), their response status was unknown.
At the time of analysis, the median DOR was 76 weeks, and 56% of responders (n=10) had an ongoing response.
The median progression-free survival was 29.9 weeks.
“I am impressed by the sustained clinical activity and the good tolerability of tazemetostat in this heavily pretreated patient population,” Dr Salles said. “This is important for patients with relapsed or refractory follicular lymphoma, as both the response rates and durations of response usually tend to decrease with each successive line of treatment.”
“I believe tazemetostat has the potential to fill a significant unmet need for these patients, and continued investigation of tazemetostat as a single agent or in combination with other agents is warranted.”
Epizyme’s president and chief executive officer, Robert Bazemore, said the company is still working to resolve the partial clinical hold on tazemetostat trials and is “making good progress.”
CPI-613 receives orphan designation for BL
The US Food and Drug Administration (FDA) has granted orphan drug designation to CPI-613 for the treatment of Burkitt lymphoma (BL).
CPI-613 is a novel lipoic acid analogue that inhibits multiple enzyme targets within the tricarboxylic acid cycle.
The drug is in development as a treatment for hematologic malignancies and solid tumors.
In a phase 1 trial of patients with advanced hematologic malignancies, CPI-613 produced a response in a patient with relapsed BL.
Now, Rafael Pharmaceuticals, Inc., the company developing CPI-613, is launching a phase 2 trial of the drug in patients with relapsed or refractory BL and high-grade B-cell lymphoma with rearrangements of MYC and BCL2 and/or BCL6.
In the phase 1 trial, the patient with relapsed BL achieved a partial response to CPI-613 monotherapy and was ultimately cleared of disease after surgery.
The patient, a 19-year-old female, began taking CPI-613 (2940 mg/m2) after her second relapse. She achieved a radiographic partial response after the third cycle of CPI-613.
The patient completed 17 cycles of CPI-613 over 51 weeks. She decided to stop treatment after the 17th cycle to pursue a surgical resection of residual tumor. The pathology of the surgical specimen revealed BL with extensive necrosis.
Clinical follow-up on the patient showed no evidence of disease more than 36 months later. And CPI-613 was considered well tolerated in this patient.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to CPI-613 for the treatment of Burkitt lymphoma (BL).
CPI-613 is a novel lipoic acid analogue that inhibits multiple enzyme targets within the tricarboxylic acid cycle.
The drug is in development as a treatment for hematologic malignancies and solid tumors.
In a phase 1 trial of patients with advanced hematologic malignancies, CPI-613 produced a response in a patient with relapsed BL.
Now, Rafael Pharmaceuticals, Inc., the company developing CPI-613, is launching a phase 2 trial of the drug in patients with relapsed or refractory BL and high-grade B-cell lymphoma with rearrangements of MYC and BCL2 and/or BCL6.
In the phase 1 trial, the patient with relapsed BL achieved a partial response to CPI-613 monotherapy and was ultimately cleared of disease after surgery.
The patient, a 19-year-old female, began taking CPI-613 (2940 mg/m2) after her second relapse. She achieved a radiographic partial response after the third cycle of CPI-613.
The patient completed 17 cycles of CPI-613 over 51 weeks. She decided to stop treatment after the 17th cycle to pursue a surgical resection of residual tumor. The pathology of the surgical specimen revealed BL with extensive necrosis.
Clinical follow-up on the patient showed no evidence of disease more than 36 months later. And CPI-613 was considered well tolerated in this patient.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The US Food and Drug Administration (FDA) has granted orphan drug designation to CPI-613 for the treatment of Burkitt lymphoma (BL).
CPI-613 is a novel lipoic acid analogue that inhibits multiple enzyme targets within the tricarboxylic acid cycle.
The drug is in development as a treatment for hematologic malignancies and solid tumors.
In a phase 1 trial of patients with advanced hematologic malignancies, CPI-613 produced a response in a patient with relapsed BL.
Now, Rafael Pharmaceuticals, Inc., the company developing CPI-613, is launching a phase 2 trial of the drug in patients with relapsed or refractory BL and high-grade B-cell lymphoma with rearrangements of MYC and BCL2 and/or BCL6.
In the phase 1 trial, the patient with relapsed BL achieved a partial response to CPI-613 monotherapy and was ultimately cleared of disease after surgery.
The patient, a 19-year-old female, began taking CPI-613 (2940 mg/m2) after her second relapse. She achieved a radiographic partial response after the third cycle of CPI-613.
The patient completed 17 cycles of CPI-613 over 51 weeks. She decided to stop treatment after the 17th cycle to pursue a surgical resection of residual tumor. The pathology of the surgical specimen revealed BL with extensive necrosis.
Clinical follow-up on the patient showed no evidence of disease more than 36 months later. And CPI-613 was considered well tolerated in this patient.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
Many CCSs not concerned about future health
A survey of more than 15,000 childhood cancer survivors (CCSs) revealed that many were unconcerned about their risk of health problems.
Thirty-one percent of CCSs said they were “not at all” or “not very” concerned about their future health, and 40% said they were “not at all” or “not very” concerned about developing new cancers.
Researchers say it isn’t clear what’s driving this lack of concern, but it is possible that some CCSs don’t know they have an increased risk of new malignancies and other health problems.
“Other possibilities include that some survivors may actually be aware of their increased risks and choose not to be concerned, or it may even be that some survivors are, indeed, following health guidelines and working with healthcare providers, leading to their lack of concern,” said Todd Gibson, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Gibson and his colleagues conducted this research and reported the results in Cancer.
The researchers analyzed data on 15,620 CCSs and 3991 of their siblings who did not have a history of cancer. The data came from questionnaires administered to participants in the Childhood Cancer Survivor Study.
At baseline, the median time from CCSs’ cancer diagnosis was 17 years (interquartile range [IQR], 14-21). Their median age at baseline was 26 (IQR, 22-31 years), and the siblings’ median age was 29 (IQR, 24-35).
When respondents were asked about their level of concern regarding their future health, the answers were as follows:
- 12% of both CCSs and siblings were “not at all concerned”
- 18.7% of CCSs and 21.6% of siblings were “not very concerned”
- 23.2% of CCSs and 24.1% of siblings were “concerned”
- 21.4% of CCSs and 22.2% of siblings were “somewhat concerned”
- 24.8% of CCSs and 20.1% of siblings were “very concerned.”
When respondents were asked to rate their level of concern about developing a new cancer, the answers were as follows:
- 17.2% of CCSs and 16.3% of siblings were “not at all concerned”
- 22.8% of CCSs and 22.2% of siblings were “not very concerned”
- 21.1% of CCSs and 25.1% of siblings were “concerned”
- 18.3% of CCSs and 18.4% of siblings were “somewhat concerned”
- 20.6% of CCSs and 18.1% of siblings were “very concerned.”
When the researchers adjusted for age, sex, race/ethnicity, education, and decade of diagnosis, CCSs were only slightly more likely than siblings to report concern about future health (relative risk, 1.12) or subsequent cancer (relative risk, 1.02).
“That similarity [between CCS and sibling answers] was really the major surprise in our findings,” Dr Gibson said. “Despite the fact that survivors have such a greatly increased risk of both second cancers and other health problems, their perception of risk was not always commensurate with their actual risk.”
The researchers did find that CCSs were more likely to report concern about future health or developing cancer if they were female, non-Hispanic black or Hispanic, older, identified as having clinical anxiety, or had already experienced a grade 3/4 chronic condition or subsequent cancer.
However, it isn’t clear why some CCSs are concerned about their future health and others are not.
“At this point, we can only speculate, but the most obvious reason [for lack of concern] would be that survivors may not fully understand their risks,” Dr Gibson said. “We do know from prior studies that not all survivors are fully aware of the specific treatments they received and how those might increase their risks of late effects.”
“If, however, survivors are aware but not motivated or sufficiently aroused to be concerned, then more motivational education will have to be developed. In any case, these findings offer a teaching point that we can use to emphasize to all survivors that they need to understand their risks.”
A survey of more than 15,000 childhood cancer survivors (CCSs) revealed that many were unconcerned about their risk of health problems.
Thirty-one percent of CCSs said they were “not at all” or “not very” concerned about their future health, and 40% said they were “not at all” or “not very” concerned about developing new cancers.
Researchers say it isn’t clear what’s driving this lack of concern, but it is possible that some CCSs don’t know they have an increased risk of new malignancies and other health problems.
“Other possibilities include that some survivors may actually be aware of their increased risks and choose not to be concerned, or it may even be that some survivors are, indeed, following health guidelines and working with healthcare providers, leading to their lack of concern,” said Todd Gibson, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Gibson and his colleagues conducted this research and reported the results in Cancer.
The researchers analyzed data on 15,620 CCSs and 3991 of their siblings who did not have a history of cancer. The data came from questionnaires administered to participants in the Childhood Cancer Survivor Study.
At baseline, the median time from CCSs’ cancer diagnosis was 17 years (interquartile range [IQR], 14-21). Their median age at baseline was 26 (IQR, 22-31 years), and the siblings’ median age was 29 (IQR, 24-35).
When respondents were asked about their level of concern regarding their future health, the answers were as follows:
- 12% of both CCSs and siblings were “not at all concerned”
- 18.7% of CCSs and 21.6% of siblings were “not very concerned”
- 23.2% of CCSs and 24.1% of siblings were “concerned”
- 21.4% of CCSs and 22.2% of siblings were “somewhat concerned”
- 24.8% of CCSs and 20.1% of siblings were “very concerned.”
When respondents were asked to rate their level of concern about developing a new cancer, the answers were as follows:
- 17.2% of CCSs and 16.3% of siblings were “not at all concerned”
- 22.8% of CCSs and 22.2% of siblings were “not very concerned”
- 21.1% of CCSs and 25.1% of siblings were “concerned”
- 18.3% of CCSs and 18.4% of siblings were “somewhat concerned”
- 20.6% of CCSs and 18.1% of siblings were “very concerned.”
When the researchers adjusted for age, sex, race/ethnicity, education, and decade of diagnosis, CCSs were only slightly more likely than siblings to report concern about future health (relative risk, 1.12) or subsequent cancer (relative risk, 1.02).
“That similarity [between CCS and sibling answers] was really the major surprise in our findings,” Dr Gibson said. “Despite the fact that survivors have such a greatly increased risk of both second cancers and other health problems, their perception of risk was not always commensurate with their actual risk.”
The researchers did find that CCSs were more likely to report concern about future health or developing cancer if they were female, non-Hispanic black or Hispanic, older, identified as having clinical anxiety, or had already experienced a grade 3/4 chronic condition or subsequent cancer.
However, it isn’t clear why some CCSs are concerned about their future health and others are not.
“At this point, we can only speculate, but the most obvious reason [for lack of concern] would be that survivors may not fully understand their risks,” Dr Gibson said. “We do know from prior studies that not all survivors are fully aware of the specific treatments they received and how those might increase their risks of late effects.”
“If, however, survivors are aware but not motivated or sufficiently aroused to be concerned, then more motivational education will have to be developed. In any case, these findings offer a teaching point that we can use to emphasize to all survivors that they need to understand their risks.”
A survey of more than 15,000 childhood cancer survivors (CCSs) revealed that many were unconcerned about their risk of health problems.
Thirty-one percent of CCSs said they were “not at all” or “not very” concerned about their future health, and 40% said they were “not at all” or “not very” concerned about developing new cancers.
Researchers say it isn’t clear what’s driving this lack of concern, but it is possible that some CCSs don’t know they have an increased risk of new malignancies and other health problems.
“Other possibilities include that some survivors may actually be aware of their increased risks and choose not to be concerned, or it may even be that some survivors are, indeed, following health guidelines and working with healthcare providers, leading to their lack of concern,” said Todd Gibson, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
Dr Gibson and his colleagues conducted this research and reported the results in Cancer.
The researchers analyzed data on 15,620 CCSs and 3991 of their siblings who did not have a history of cancer. The data came from questionnaires administered to participants in the Childhood Cancer Survivor Study.
At baseline, the median time from CCSs’ cancer diagnosis was 17 years (interquartile range [IQR], 14-21). Their median age at baseline was 26 (IQR, 22-31 years), and the siblings’ median age was 29 (IQR, 24-35).
When respondents were asked about their level of concern regarding their future health, the answers were as follows:
- 12% of both CCSs and siblings were “not at all concerned”
- 18.7% of CCSs and 21.6% of siblings were “not very concerned”
- 23.2% of CCSs and 24.1% of siblings were “concerned”
- 21.4% of CCSs and 22.2% of siblings were “somewhat concerned”
- 24.8% of CCSs and 20.1% of siblings were “very concerned.”
When respondents were asked to rate their level of concern about developing a new cancer, the answers were as follows:
- 17.2% of CCSs and 16.3% of siblings were “not at all concerned”
- 22.8% of CCSs and 22.2% of siblings were “not very concerned”
- 21.1% of CCSs and 25.1% of siblings were “concerned”
- 18.3% of CCSs and 18.4% of siblings were “somewhat concerned”
- 20.6% of CCSs and 18.1% of siblings were “very concerned.”
When the researchers adjusted for age, sex, race/ethnicity, education, and decade of diagnosis, CCSs were only slightly more likely than siblings to report concern about future health (relative risk, 1.12) or subsequent cancer (relative risk, 1.02).
“That similarity [between CCS and sibling answers] was really the major surprise in our findings,” Dr Gibson said. “Despite the fact that survivors have such a greatly increased risk of both second cancers and other health problems, their perception of risk was not always commensurate with their actual risk.”
The researchers did find that CCSs were more likely to report concern about future health or developing cancer if they were female, non-Hispanic black or Hispanic, older, identified as having clinical anxiety, or had already experienced a grade 3/4 chronic condition or subsequent cancer.
However, it isn’t clear why some CCSs are concerned about their future health and others are not.
“At this point, we can only speculate, but the most obvious reason [for lack of concern] would be that survivors may not fully understand their risks,” Dr Gibson said. “We do know from prior studies that not all survivors are fully aware of the specific treatments they received and how those might increase their risks of late effects.”
“If, however, survivors are aware but not motivated or sufficiently aroused to be concerned, then more motivational education will have to be developed. In any case, these findings offer a teaching point that we can use to emphasize to all survivors that they need to understand their risks.”
FDA grants priority review to drug for AML
The US Food and Drug Administration (FDA) has accepted for priority review a new drug application (NDA) for glasdegib, an oral SMO inhibitor.
With this NDA, Pfizer is seeking approval for glasdegib in combination with low-dose cytarabine (LDAC) as a treatment for adults with previously untreated acute myeloid leukemia (AML).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
The FDA expects to make a decision on the NDA for glasdegib by December 2018.
The NDA is supported by results from the phase 2 BRIGHT 1003 study. Results from this trial were presented at the 2016 ASH Annual Meeting.
The trial was a comparison of glasdegib plus LDAC (n=88) to LDAC alone (n=44) in patients with previously untreated AML or high-risk myelodysplastic syndromes who were not eligible for intensive chemotherapy.
Results demonstrated a significant improvement in overall survival with glasdegib. The median overall survival was 8.8 months in the glasdegib arm and 4.9 months in the LDAC-alone arm.
This difference represented a 49.9% reduction in the risk of death for patients treated with glasdegib plus LDAC (hazard ratio=0.501; 95% CI: 0.334, 0.752; one-sided P-value=0.0003).
The most frequent adverse events—occurring in at least 30% of patients in the glasdegib arm and LDAC-alone arm, respectively—were anemia (45% vs 42%), febrile neutropenia (36% vs 27%), nausea (36% vs 12%), decreased appetite (32% vs 12%), fatigue (31% vs 20%), and thrombocytopenia (30% vs 27%).
The most frequently reported serious adverse events—occurring in at least 15% of patients in the glasdegib and LDAC-alone arms, respectively—were febrile neutropenia (29% vs 20%) and pneumonia (21% vs 17%).
A phase 3 trial of glasdegib in AML began enrolling earlier this year. In this trial (BRIGHT AML 1019; NCT03416179), researchers are evaluating glasdegib plus intensive or non-intensive chemotherapy in patients with newly diagnosed AML.
The US Food and Drug Administration (FDA) has accepted for priority review a new drug application (NDA) for glasdegib, an oral SMO inhibitor.
With this NDA, Pfizer is seeking approval for glasdegib in combination with low-dose cytarabine (LDAC) as a treatment for adults with previously untreated acute myeloid leukemia (AML).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
The FDA expects to make a decision on the NDA for glasdegib by December 2018.
The NDA is supported by results from the phase 2 BRIGHT 1003 study. Results from this trial were presented at the 2016 ASH Annual Meeting.
The trial was a comparison of glasdegib plus LDAC (n=88) to LDAC alone (n=44) in patients with previously untreated AML or high-risk myelodysplastic syndromes who were not eligible for intensive chemotherapy.
Results demonstrated a significant improvement in overall survival with glasdegib. The median overall survival was 8.8 months in the glasdegib arm and 4.9 months in the LDAC-alone arm.
This difference represented a 49.9% reduction in the risk of death for patients treated with glasdegib plus LDAC (hazard ratio=0.501; 95% CI: 0.334, 0.752; one-sided P-value=0.0003).
The most frequent adverse events—occurring in at least 30% of patients in the glasdegib arm and LDAC-alone arm, respectively—were anemia (45% vs 42%), febrile neutropenia (36% vs 27%), nausea (36% vs 12%), decreased appetite (32% vs 12%), fatigue (31% vs 20%), and thrombocytopenia (30% vs 27%).
The most frequently reported serious adverse events—occurring in at least 15% of patients in the glasdegib and LDAC-alone arms, respectively—were febrile neutropenia (29% vs 20%) and pneumonia (21% vs 17%).
A phase 3 trial of glasdegib in AML began enrolling earlier this year. In this trial (BRIGHT AML 1019; NCT03416179), researchers are evaluating glasdegib plus intensive or non-intensive chemotherapy in patients with newly diagnosed AML.
The US Food and Drug Administration (FDA) has accepted for priority review a new drug application (NDA) for glasdegib, an oral SMO inhibitor.
With this NDA, Pfizer is seeking approval for glasdegib in combination with low-dose cytarabine (LDAC) as a treatment for adults with previously untreated acute myeloid leukemia (AML).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
The FDA expects to make a decision on the NDA for glasdegib by December 2018.
The NDA is supported by results from the phase 2 BRIGHT 1003 study. Results from this trial were presented at the 2016 ASH Annual Meeting.
The trial was a comparison of glasdegib plus LDAC (n=88) to LDAC alone (n=44) in patients with previously untreated AML or high-risk myelodysplastic syndromes who were not eligible for intensive chemotherapy.
Results demonstrated a significant improvement in overall survival with glasdegib. The median overall survival was 8.8 months in the glasdegib arm and 4.9 months in the LDAC-alone arm.
This difference represented a 49.9% reduction in the risk of death for patients treated with glasdegib plus LDAC (hazard ratio=0.501; 95% CI: 0.334, 0.752; one-sided P-value=0.0003).
The most frequent adverse events—occurring in at least 30% of patients in the glasdegib arm and LDAC-alone arm, respectively—were anemia (45% vs 42%), febrile neutropenia (36% vs 27%), nausea (36% vs 12%), decreased appetite (32% vs 12%), fatigue (31% vs 20%), and thrombocytopenia (30% vs 27%).
The most frequently reported serious adverse events—occurring in at least 15% of patients in the glasdegib and LDAC-alone arms, respectively—were febrile neutropenia (29% vs 20%) and pneumonia (21% vs 17%).
A phase 3 trial of glasdegib in AML began enrolling earlier this year. In this trial (BRIGHT AML 1019; NCT03416179), researchers are evaluating glasdegib plus intensive or non-intensive chemotherapy in patients with newly diagnosed AML.
Perioperative RBC transfusions linked to VTE
Patients who receive red blood cell (RBC) transfusions before, during, or immediately after surgery may have an increased risk of venous thromboembolism (VTE), a new study suggests.
In this retrospective study, transfusion recipients had twice the risk of VTE as patients who did not receive RBC transfusions during the perioperative period.
Investigators say these findings require validation, but they suggest a need for physicians to consider non-transfusion alternatives to treat anemia in patients undergoing surgery.
“These findings reinforce the importance of following rigorous perioperative patient blood management practices for transfusions,” said Ruchika Goel, MD, of Weill Cornell Medicine in New York, New York.
Dr Goel and her colleagues reported their findings in JAMA Surgery.
The investigators analyzed data on 750,937 patients who underwent surgery in 2014. In all, 6.3% (n=47,410) of patients received at least one RBC transfusion.
Within 30 days of surgery, 0.8% (n=6309) of all patients had a VTE. This included 0.6% (n=4336) with deep vein thrombosis (DVT), 0.3% (n=2514) with pulmonary embolism (PE), and 0.1% (n=541) with DVT and PE.
Analyses showed that patients who received RBC transfusions were twice as likely to develop VTE as those who did not receive transfusions (adjusted odds ratio [aOR]=2.1). This was true for both DVT (aOR=2.2) and PE (aOR=1.9).
“We also saw this risk across different surgical disciplines, ranging from neurosurgery to cardiac surgery,” said study author Aaron Tobian, MD, PhD, of Johns Hopkins University School of Medicine in Baltimore, Maryland.
Furthermore, VTE risk increased with the number of RBC transfusions a patient received. The aORs were 2.1 for 1 transfusion, 3.1 for 2 transfusions, and 4.5 for 3 or more transfusions (compared to patients who did not receive any transfusions).
“This retrospective study demonstrates that there may be additional risks to blood transfusion that are not generally recognized in the community,” Dr Tobian said. “While additional research is needed to confirm these results, the findings reinforce the need to limit blood transfusions to only when necessary.”
Patients who receive red blood cell (RBC) transfusions before, during, or immediately after surgery may have an increased risk of venous thromboembolism (VTE), a new study suggests.
In this retrospective study, transfusion recipients had twice the risk of VTE as patients who did not receive RBC transfusions during the perioperative period.
Investigators say these findings require validation, but they suggest a need for physicians to consider non-transfusion alternatives to treat anemia in patients undergoing surgery.
“These findings reinforce the importance of following rigorous perioperative patient blood management practices for transfusions,” said Ruchika Goel, MD, of Weill Cornell Medicine in New York, New York.
Dr Goel and her colleagues reported their findings in JAMA Surgery.
The investigators analyzed data on 750,937 patients who underwent surgery in 2014. In all, 6.3% (n=47,410) of patients received at least one RBC transfusion.
Within 30 days of surgery, 0.8% (n=6309) of all patients had a VTE. This included 0.6% (n=4336) with deep vein thrombosis (DVT), 0.3% (n=2514) with pulmonary embolism (PE), and 0.1% (n=541) with DVT and PE.
Analyses showed that patients who received RBC transfusions were twice as likely to develop VTE as those who did not receive transfusions (adjusted odds ratio [aOR]=2.1). This was true for both DVT (aOR=2.2) and PE (aOR=1.9).
“We also saw this risk across different surgical disciplines, ranging from neurosurgery to cardiac surgery,” said study author Aaron Tobian, MD, PhD, of Johns Hopkins University School of Medicine in Baltimore, Maryland.
Furthermore, VTE risk increased with the number of RBC transfusions a patient received. The aORs were 2.1 for 1 transfusion, 3.1 for 2 transfusions, and 4.5 for 3 or more transfusions (compared to patients who did not receive any transfusions).
“This retrospective study demonstrates that there may be additional risks to blood transfusion that are not generally recognized in the community,” Dr Tobian said. “While additional research is needed to confirm these results, the findings reinforce the need to limit blood transfusions to only when necessary.”
Patients who receive red blood cell (RBC) transfusions before, during, or immediately after surgery may have an increased risk of venous thromboembolism (VTE), a new study suggests.
In this retrospective study, transfusion recipients had twice the risk of VTE as patients who did not receive RBC transfusions during the perioperative period.
Investigators say these findings require validation, but they suggest a need for physicians to consider non-transfusion alternatives to treat anemia in patients undergoing surgery.
“These findings reinforce the importance of following rigorous perioperative patient blood management practices for transfusions,” said Ruchika Goel, MD, of Weill Cornell Medicine in New York, New York.
Dr Goel and her colleagues reported their findings in JAMA Surgery.
The investigators analyzed data on 750,937 patients who underwent surgery in 2014. In all, 6.3% (n=47,410) of patients received at least one RBC transfusion.
Within 30 days of surgery, 0.8% (n=6309) of all patients had a VTE. This included 0.6% (n=4336) with deep vein thrombosis (DVT), 0.3% (n=2514) with pulmonary embolism (PE), and 0.1% (n=541) with DVT and PE.
Analyses showed that patients who received RBC transfusions were twice as likely to develop VTE as those who did not receive transfusions (adjusted odds ratio [aOR]=2.1). This was true for both DVT (aOR=2.2) and PE (aOR=1.9).
“We also saw this risk across different surgical disciplines, ranging from neurosurgery to cardiac surgery,” said study author Aaron Tobian, MD, PhD, of Johns Hopkins University School of Medicine in Baltimore, Maryland.
Furthermore, VTE risk increased with the number of RBC transfusions a patient received. The aORs were 2.1 for 1 transfusion, 3.1 for 2 transfusions, and 4.5 for 3 or more transfusions (compared to patients who did not receive any transfusions).
“This retrospective study demonstrates that there may be additional risks to blood transfusion that are not generally recognized in the community,” Dr Tobian said. “While additional research is needed to confirm these results, the findings reinforce the need to limit blood transfusions to only when necessary.”