User login
Providers endorse medical marijuana for kids with cancer
A survey of nearly 300 US medical providers revealed that many were open to helping children with cancer access medical marijuana (MM).
However, most of the providers surveyed did not know state-specific regulations pertaining to MM.
Providers who were legally eligible to certify (ETC) for MM were less open to endorsing its use.
The lack of standards on formulations, dosing, and potency of MM was identified as the greatest barrier to recommending MM for children with cancer.
Kelly Michelson, MD, of Ann & Robert H. Lurie Children’s Hospital of Chicago in Illinois, and her colleagues reported these findings in Pediatrics.
The researchers used a 32-item survey to assess MM practices, knowledge, attitudes, and barriers for pediatric oncology providers in Illinois, Massachusetts, and Washington.
The survey was sent to providers at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, Seattle Children’s Cancer and Blood Disorders Center, and Lurie Children’s Center for Cancer and Blood Disorders.
There were 288 respondents, and 33% were legally ETC for MM. Eighty-six percent of ETC providers were physicians, and 14% were nurse practitioners or physician assistants.
Of the non-ETC providers, 89% were nurses, 8% were nurse practitioners or physician assistants, 2% were psychosocial providers, and 2% were “other” providers.
Thirty percent of all providers said they had received at least 1 request for MM in the previous month. And 14% of these providers facilitated patient access to MM.
Ninety-two percent of providers said they were willing to help pediatric cancer patients access MM. Fifty-seven percent of providers approved of patients smoking MM, 89% approved of oral formulations, 67% approved of using MM as cancer-directed therapy, and 92% approved of using MM to manage symptoms.
Fifty-nine percent of providers knew that MM is against federal laws, and 86% knew that their state had legalized MM, but only 5% knew state-specific regulations.
ETC providers were less likely to report willingness to help patients access MM. These providers were also less likely to approve of MM use by smoking, oral formulations, as cancer-directed therapy, or to manage symptoms.
“It is not surprising that providers who are eligible to certify for medical marijuana were more cautious about recommending it, given that their licensure could be jeopardized due to federal prohibition,” Dr Michelson said.
“Institutional policies also may have influenced their attitudes. Lurie Children’s, for example, prohibits pediatric providers from facilitating medical marijuana access in accordance with the federal law, even though it is legal in Illinois.”
Most providers considered MM more permissible for use in children with advanced cancer or near the end of life than in earlier stages of cancer treatment. This is consistent with the current American Academy of Pediatrics position that sanctions MM use for “children with life-limiting or seriously debilitating conditions.”
Only 2% of providers reported that MM was never appropriate for a child with cancer.
Most providers (63%) were not concerned about substance abuse in children who receive MM or about being prosecuted for helping patients access MM (80%).
The greatest concern (listed by 46% of providers) was the absence of standards around prescribing MM to children with cancer.
“In addition to unclear dosage guidelines, the lack of high quality scientific data that medical marijuana benefits outweigh possible harm is a huge concern for providers accustomed to evidence-based practice,” Dr Michelson said. “We need rigorously designed clinical trials on the use of medical marijuana in children with cancer.” ![]()
A survey of nearly 300 US medical providers revealed that many were open to helping children with cancer access medical marijuana (MM).
However, most of the providers surveyed did not know state-specific regulations pertaining to MM.
Providers who were legally eligible to certify (ETC) for MM were less open to endorsing its use.
The lack of standards on formulations, dosing, and potency of MM was identified as the greatest barrier to recommending MM for children with cancer.
Kelly Michelson, MD, of Ann & Robert H. Lurie Children’s Hospital of Chicago in Illinois, and her colleagues reported these findings in Pediatrics.
The researchers used a 32-item survey to assess MM practices, knowledge, attitudes, and barriers for pediatric oncology providers in Illinois, Massachusetts, and Washington.
The survey was sent to providers at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, Seattle Children’s Cancer and Blood Disorders Center, and Lurie Children’s Center for Cancer and Blood Disorders.
There were 288 respondents, and 33% were legally ETC for MM. Eighty-six percent of ETC providers were physicians, and 14% were nurse practitioners or physician assistants.
Of the non-ETC providers, 89% were nurses, 8% were nurse practitioners or physician assistants, 2% were psychosocial providers, and 2% were “other” providers.
Thirty percent of all providers said they had received at least 1 request for MM in the previous month. And 14% of these providers facilitated patient access to MM.
Ninety-two percent of providers said they were willing to help pediatric cancer patients access MM. Fifty-seven percent of providers approved of patients smoking MM, 89% approved of oral formulations, 67% approved of using MM as cancer-directed therapy, and 92% approved of using MM to manage symptoms.
Fifty-nine percent of providers knew that MM is against federal laws, and 86% knew that their state had legalized MM, but only 5% knew state-specific regulations.
ETC providers were less likely to report willingness to help patients access MM. These providers were also less likely to approve of MM use by smoking, oral formulations, as cancer-directed therapy, or to manage symptoms.
“It is not surprising that providers who are eligible to certify for medical marijuana were more cautious about recommending it, given that their licensure could be jeopardized due to federal prohibition,” Dr Michelson said.
“Institutional policies also may have influenced their attitudes. Lurie Children’s, for example, prohibits pediatric providers from facilitating medical marijuana access in accordance with the federal law, even though it is legal in Illinois.”
Most providers considered MM more permissible for use in children with advanced cancer or near the end of life than in earlier stages of cancer treatment. This is consistent with the current American Academy of Pediatrics position that sanctions MM use for “children with life-limiting or seriously debilitating conditions.”
Only 2% of providers reported that MM was never appropriate for a child with cancer.
Most providers (63%) were not concerned about substance abuse in children who receive MM or about being prosecuted for helping patients access MM (80%).
The greatest concern (listed by 46% of providers) was the absence of standards around prescribing MM to children with cancer.
“In addition to unclear dosage guidelines, the lack of high quality scientific data that medical marijuana benefits outweigh possible harm is a huge concern for providers accustomed to evidence-based practice,” Dr Michelson said. “We need rigorously designed clinical trials on the use of medical marijuana in children with cancer.” ![]()
A survey of nearly 300 US medical providers revealed that many were open to helping children with cancer access medical marijuana (MM).
However, most of the providers surveyed did not know state-specific regulations pertaining to MM.
Providers who were legally eligible to certify (ETC) for MM were less open to endorsing its use.
The lack of standards on formulations, dosing, and potency of MM was identified as the greatest barrier to recommending MM for children with cancer.
Kelly Michelson, MD, of Ann & Robert H. Lurie Children’s Hospital of Chicago in Illinois, and her colleagues reported these findings in Pediatrics.
The researchers used a 32-item survey to assess MM practices, knowledge, attitudes, and barriers for pediatric oncology providers in Illinois, Massachusetts, and Washington.
The survey was sent to providers at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, Seattle Children’s Cancer and Blood Disorders Center, and Lurie Children’s Center for Cancer and Blood Disorders.
There were 288 respondents, and 33% were legally ETC for MM. Eighty-six percent of ETC providers were physicians, and 14% were nurse practitioners or physician assistants.
Of the non-ETC providers, 89% were nurses, 8% were nurse practitioners or physician assistants, 2% were psychosocial providers, and 2% were “other” providers.
Thirty percent of all providers said they had received at least 1 request for MM in the previous month. And 14% of these providers facilitated patient access to MM.
Ninety-two percent of providers said they were willing to help pediatric cancer patients access MM. Fifty-seven percent of providers approved of patients smoking MM, 89% approved of oral formulations, 67% approved of using MM as cancer-directed therapy, and 92% approved of using MM to manage symptoms.
Fifty-nine percent of providers knew that MM is against federal laws, and 86% knew that their state had legalized MM, but only 5% knew state-specific regulations.
ETC providers were less likely to report willingness to help patients access MM. These providers were also less likely to approve of MM use by smoking, oral formulations, as cancer-directed therapy, or to manage symptoms.
“It is not surprising that providers who are eligible to certify for medical marijuana were more cautious about recommending it, given that their licensure could be jeopardized due to federal prohibition,” Dr Michelson said.
“Institutional policies also may have influenced their attitudes. Lurie Children’s, for example, prohibits pediatric providers from facilitating medical marijuana access in accordance with the federal law, even though it is legal in Illinois.”
Most providers considered MM more permissible for use in children with advanced cancer or near the end of life than in earlier stages of cancer treatment. This is consistent with the current American Academy of Pediatrics position that sanctions MM use for “children with life-limiting or seriously debilitating conditions.”
Only 2% of providers reported that MM was never appropriate for a child with cancer.
Most providers (63%) were not concerned about substance abuse in children who receive MM or about being prosecuted for helping patients access MM (80%).
The greatest concern (listed by 46% of providers) was the absence of standards around prescribing MM to children with cancer.
“In addition to unclear dosage guidelines, the lack of high quality scientific data that medical marijuana benefits outweigh possible harm is a huge concern for providers accustomed to evidence-based practice,” Dr Michelson said. “We need rigorously designed clinical trials on the use of medical marijuana in children with cancer.” ![]()
A+AVD improves modified PFS in advanced HL
ATLANTA—Phase 3 trial results suggest one 4-drug combination may be more effective than another as frontline treatment for advanced Hodgkin lymphoma (HL).
In the ECHELON-1 trial, treatment with brentuximab vedotin, doxorubicin, vinblastine, and dacarbazine (A+AVD) staved off progression, death, and the need for subsequent therapy more effectively than treatment with doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD).
However, there was no significant difference between the treatment arms when it came to response rates or overall survival.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with A+AVD, while pulmonary toxicity was more common with ABVD.
These data were presented at the 2017 ASH Annual Meeting (abstract 6) and simultaneously published in The New England Journal of Medicine. The trial was funded by Millennium Pharmaceuticals and Seattle Genetics, Inc.
“The standard of care in the treatment of Hodgkin lymphoma has not changed over the last several decades, and there remains an unmet need for additional regimens in frontline treatment,” said Joseph M. Connors, MD, of BC Cancer in Vancouver, British Columbia, Canada.
With this in mind, he and his colleagues conducted ECHELON-1. The study enrolled 1334 patients who had stage III or IV HL and had not previously received systemic chemotherapy or radiotherapy.
Fifty-eight percent of patients were male, and the median age was 36 (range, 18-83). Sixty-four percent of patients had stage IV disease, 62% had extranodal involvement at diagnosis, and 58% had B symptoms.
The patients were randomized to receive A+AVD (n=664) or ABVD (n=670) on days 1 and 15 of each 28-day cycle for up to 6 cycles. Baseline characteristics were well-balanced between the treatment arms.
The median follow-up was 24.9 months (range, 0-49.3).
Primary endpoint
The study’s primary endpoint is modified progression-free survival (PFS), which is defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review facility, A+AVD provided a significant improvement in modified PFS compared to ABVD. The hazard ratio was 0.77 (P=0.035), which corresponds to a 23% reduction in the risk of progression, death, or the need for additional anticancer therapy.
“Reducing the risk of relapse is an important concern for patients and their physicians,” Dr Connors noted. “In the trial, 33% fewer patients [in the A+AVD arm] required subsequent salvage chemotherapy or high-dose chemotherapy and transplant compared to the patients treated with ABVD.”
According to the independent review facility, the 2-year modified PFS rate was 82.1% in the A+AVD arm and 77.2% in the ABVD arm.
Certain pre-specified subgroups of patients appeared to benefit more with A+AVD than with ABVD, including:
- Males
- Patients treated in North America
- Patients with involvement of more than 1 extranodal site
- Patients with International Prognostic Scores of 4 to 7
- Patients with stage IV disease
- Patients younger than 60.
Secondary endpoints
Secondary endpoints trended in favor of the A+AVD arm, although there were no significant differences between the treatment arms.
The objective response rate at the end of the randomized regimen was 86% in the A+AVD arm and 83% in the ABVD arm (P=0.12). The complete response rate was 73% and 70%, respectively (P=0.22).
The proportion of patients with a Deauville score ≤2 after the completion of frontline therapy was 85% in the A+AVD arm and 80% in the ABVD arm (P=0.03).
The interim 2-year overall survival rate was 97% in the A+AVD arm and 95% in the ABVD arm (hazard ratio=0.72; P=0.19).
Safety
“[T]he safety profile [of A+AVD] was generally consistent with that known for the single-agent components of the regimen,” Dr Connors said.
The overall incidence of adverse events (AEs) was 99% in the A+AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively, and the incidence of serious AEs was 43% and 27%, respectively.
Common AEs (in the A+AVD and ABVD arms, respectively) included neutropenia (58% and 45%), constipation (42% and 37%), vomiting (33% and 28%), fatigue (both 32%), diarrhea (27% and 18%), pyrexia (27% and 22%), abdominal pain (21% and 10%), and stomatitis (21% and 16%).
Peripheral neuropathy events were observed in 67% of patients in the A+AVD arm and 43% in the ABVD arm. Grade 3 or higher peripheral neuropathy was reported in 11% and 2%, respectively.
Febrile neutropenia occurred in 19% of patients in the A+AVD arm and 8% of those in the ABVD arm. However, prophylaxis with granulocyte colony-stimulating factor (G-CSF) was able to reduce the incidence of febrile neutropenia. In the A+AVD arm, the rate of febrile neutropenia was 11% among patients who received G-CSF and 21% among patients who did not.
Pulmonary toxicity occurred in 2% of patients in the A+AVD arm and 7% of those in the ABVD arm. Grade 3 or higher pulmonary toxicity was reported in 0.76% and 3%, respectively.
There were 9 deaths during treatment in the A+AVD arm. Seven were due to neutropenia or associated complications, and 2 were due to myocardial infarction. One of the patients who died of neutropenia had the condition prior to trial enrollment. The remaining 6 patients did not receive G-CSF prophylaxis.
In the ABVD arm, there were 13 deaths during treatment. Eleven were due to or associated with pulmonary-related toxicity, 1 was due to cardiopulmonary failure, and 1 death had an unknown cause. ![]()
ATLANTA—Phase 3 trial results suggest one 4-drug combination may be more effective than another as frontline treatment for advanced Hodgkin lymphoma (HL).
In the ECHELON-1 trial, treatment with brentuximab vedotin, doxorubicin, vinblastine, and dacarbazine (A+AVD) staved off progression, death, and the need for subsequent therapy more effectively than treatment with doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD).
However, there was no significant difference between the treatment arms when it came to response rates or overall survival.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with A+AVD, while pulmonary toxicity was more common with ABVD.
These data were presented at the 2017 ASH Annual Meeting (abstract 6) and simultaneously published in The New England Journal of Medicine. The trial was funded by Millennium Pharmaceuticals and Seattle Genetics, Inc.
“The standard of care in the treatment of Hodgkin lymphoma has not changed over the last several decades, and there remains an unmet need for additional regimens in frontline treatment,” said Joseph M. Connors, MD, of BC Cancer in Vancouver, British Columbia, Canada.
With this in mind, he and his colleagues conducted ECHELON-1. The study enrolled 1334 patients who had stage III or IV HL and had not previously received systemic chemotherapy or radiotherapy.
Fifty-eight percent of patients were male, and the median age was 36 (range, 18-83). Sixty-four percent of patients had stage IV disease, 62% had extranodal involvement at diagnosis, and 58% had B symptoms.
The patients were randomized to receive A+AVD (n=664) or ABVD (n=670) on days 1 and 15 of each 28-day cycle for up to 6 cycles. Baseline characteristics were well-balanced between the treatment arms.
The median follow-up was 24.9 months (range, 0-49.3).
Primary endpoint
The study’s primary endpoint is modified progression-free survival (PFS), which is defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review facility, A+AVD provided a significant improvement in modified PFS compared to ABVD. The hazard ratio was 0.77 (P=0.035), which corresponds to a 23% reduction in the risk of progression, death, or the need for additional anticancer therapy.
“Reducing the risk of relapse is an important concern for patients and their physicians,” Dr Connors noted. “In the trial, 33% fewer patients [in the A+AVD arm] required subsequent salvage chemotherapy or high-dose chemotherapy and transplant compared to the patients treated with ABVD.”
According to the independent review facility, the 2-year modified PFS rate was 82.1% in the A+AVD arm and 77.2% in the ABVD arm.
Certain pre-specified subgroups of patients appeared to benefit more with A+AVD than with ABVD, including:
- Males
- Patients treated in North America
- Patients with involvement of more than 1 extranodal site
- Patients with International Prognostic Scores of 4 to 7
- Patients with stage IV disease
- Patients younger than 60.
Secondary endpoints
Secondary endpoints trended in favor of the A+AVD arm, although there were no significant differences between the treatment arms.
The objective response rate at the end of the randomized regimen was 86% in the A+AVD arm and 83% in the ABVD arm (P=0.12). The complete response rate was 73% and 70%, respectively (P=0.22).
The proportion of patients with a Deauville score ≤2 after the completion of frontline therapy was 85% in the A+AVD arm and 80% in the ABVD arm (P=0.03).
The interim 2-year overall survival rate was 97% in the A+AVD arm and 95% in the ABVD arm (hazard ratio=0.72; P=0.19).
Safety
“[T]he safety profile [of A+AVD] was generally consistent with that known for the single-agent components of the regimen,” Dr Connors said.
The overall incidence of adverse events (AEs) was 99% in the A+AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively, and the incidence of serious AEs was 43% and 27%, respectively.
Common AEs (in the A+AVD and ABVD arms, respectively) included neutropenia (58% and 45%), constipation (42% and 37%), vomiting (33% and 28%), fatigue (both 32%), diarrhea (27% and 18%), pyrexia (27% and 22%), abdominal pain (21% and 10%), and stomatitis (21% and 16%).
Peripheral neuropathy events were observed in 67% of patients in the A+AVD arm and 43% in the ABVD arm. Grade 3 or higher peripheral neuropathy was reported in 11% and 2%, respectively.
Febrile neutropenia occurred in 19% of patients in the A+AVD arm and 8% of those in the ABVD arm. However, prophylaxis with granulocyte colony-stimulating factor (G-CSF) was able to reduce the incidence of febrile neutropenia. In the A+AVD arm, the rate of febrile neutropenia was 11% among patients who received G-CSF and 21% among patients who did not.
Pulmonary toxicity occurred in 2% of patients in the A+AVD arm and 7% of those in the ABVD arm. Grade 3 or higher pulmonary toxicity was reported in 0.76% and 3%, respectively.
There were 9 deaths during treatment in the A+AVD arm. Seven were due to neutropenia or associated complications, and 2 were due to myocardial infarction. One of the patients who died of neutropenia had the condition prior to trial enrollment. The remaining 6 patients did not receive G-CSF prophylaxis.
In the ABVD arm, there were 13 deaths during treatment. Eleven were due to or associated with pulmonary-related toxicity, 1 was due to cardiopulmonary failure, and 1 death had an unknown cause. ![]()
ATLANTA—Phase 3 trial results suggest one 4-drug combination may be more effective than another as frontline treatment for advanced Hodgkin lymphoma (HL).
In the ECHELON-1 trial, treatment with brentuximab vedotin, doxorubicin, vinblastine, and dacarbazine (A+AVD) staved off progression, death, and the need for subsequent therapy more effectively than treatment with doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD).
However, there was no significant difference between the treatment arms when it came to response rates or overall survival.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with A+AVD, while pulmonary toxicity was more common with ABVD.
These data were presented at the 2017 ASH Annual Meeting (abstract 6) and simultaneously published in The New England Journal of Medicine. The trial was funded by Millennium Pharmaceuticals and Seattle Genetics, Inc.
“The standard of care in the treatment of Hodgkin lymphoma has not changed over the last several decades, and there remains an unmet need for additional regimens in frontline treatment,” said Joseph M. Connors, MD, of BC Cancer in Vancouver, British Columbia, Canada.
With this in mind, he and his colleagues conducted ECHELON-1. The study enrolled 1334 patients who had stage III or IV HL and had not previously received systemic chemotherapy or radiotherapy.
Fifty-eight percent of patients were male, and the median age was 36 (range, 18-83). Sixty-four percent of patients had stage IV disease, 62% had extranodal involvement at diagnosis, and 58% had B symptoms.
The patients were randomized to receive A+AVD (n=664) or ABVD (n=670) on days 1 and 15 of each 28-day cycle for up to 6 cycles. Baseline characteristics were well-balanced between the treatment arms.
The median follow-up was 24.9 months (range, 0-49.3).
Primary endpoint
The study’s primary endpoint is modified progression-free survival (PFS), which is defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review facility, A+AVD provided a significant improvement in modified PFS compared to ABVD. The hazard ratio was 0.77 (P=0.035), which corresponds to a 23% reduction in the risk of progression, death, or the need for additional anticancer therapy.
“Reducing the risk of relapse is an important concern for patients and their physicians,” Dr Connors noted. “In the trial, 33% fewer patients [in the A+AVD arm] required subsequent salvage chemotherapy or high-dose chemotherapy and transplant compared to the patients treated with ABVD.”
According to the independent review facility, the 2-year modified PFS rate was 82.1% in the A+AVD arm and 77.2% in the ABVD arm.
Certain pre-specified subgroups of patients appeared to benefit more with A+AVD than with ABVD, including:
- Males
- Patients treated in North America
- Patients with involvement of more than 1 extranodal site
- Patients with International Prognostic Scores of 4 to 7
- Patients with stage IV disease
- Patients younger than 60.
Secondary endpoints
Secondary endpoints trended in favor of the A+AVD arm, although there were no significant differences between the treatment arms.
The objective response rate at the end of the randomized regimen was 86% in the A+AVD arm and 83% in the ABVD arm (P=0.12). The complete response rate was 73% and 70%, respectively (P=0.22).
The proportion of patients with a Deauville score ≤2 after the completion of frontline therapy was 85% in the A+AVD arm and 80% in the ABVD arm (P=0.03).
The interim 2-year overall survival rate was 97% in the A+AVD arm and 95% in the ABVD arm (hazard ratio=0.72; P=0.19).
Safety
“[T]he safety profile [of A+AVD] was generally consistent with that known for the single-agent components of the regimen,” Dr Connors said.
The overall incidence of adverse events (AEs) was 99% in the A+AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively, and the incidence of serious AEs was 43% and 27%, respectively.
Common AEs (in the A+AVD and ABVD arms, respectively) included neutropenia (58% and 45%), constipation (42% and 37%), vomiting (33% and 28%), fatigue (both 32%), diarrhea (27% and 18%), pyrexia (27% and 22%), abdominal pain (21% and 10%), and stomatitis (21% and 16%).
Peripheral neuropathy events were observed in 67% of patients in the A+AVD arm and 43% in the ABVD arm. Grade 3 or higher peripheral neuropathy was reported in 11% and 2%, respectively.
Febrile neutropenia occurred in 19% of patients in the A+AVD arm and 8% of those in the ABVD arm. However, prophylaxis with granulocyte colony-stimulating factor (G-CSF) was able to reduce the incidence of febrile neutropenia. In the A+AVD arm, the rate of febrile neutropenia was 11% among patients who received G-CSF and 21% among patients who did not.
Pulmonary toxicity occurred in 2% of patients in the A+AVD arm and 7% of those in the ABVD arm. Grade 3 or higher pulmonary toxicity was reported in 0.76% and 3%, respectively.
There were 9 deaths during treatment in the A+AVD arm. Seven were due to neutropenia or associated complications, and 2 were due to myocardial infarction. One of the patients who died of neutropenia had the condition prior to trial enrollment. The remaining 6 patients did not receive G-CSF prophylaxis.
In the ABVD arm, there were 13 deaths during treatment. Eleven were due to or associated with pulmonary-related toxicity, 1 was due to cardiopulmonary failure, and 1 death had an unknown cause. ![]()
EC approves new formulation of pegaspargase
The European Commission (EC) has granted marketing authorization for a lyophilized formulation of pegaspargase (ONCASPAR).
The product is intended for use as a component of antineoplastic combination therapy in acute lymphoblastic leukemia patients of all ages.
The EC’s approval authorizes Shire to market lyophilized pegaspargase in the 28 member states of the European Union as well as Iceland, Liechtenstein, and Norway.
Lyophilized pegaspargase works the same way as the liquid formulation. By depleting serum L-asparagine levels and thereby interfering with protein synthesis, pegaspargase deprives lymphoblasts of L-asparagine, resulting in cell death.
The lyophilized formulation offers the same dosing regimen as liquid pegaspargase but also provides a shelf life of up to 24 months—3 times longer than that of the liquid formulation.
Shire expects lyophilized pegaspargase to be available in European markets beginning in the first half of 2018.
“With this lyophilized formulation, we aim to make pegylated asparaginase, part of the pediatric standard therapy in acute lymphoblastic leukemia, available to patients in countries where liquid ONCASPAR is not currently offered,” said Howard B. Mayer, MD, senior vice-president and ad-interim head of global research and development at Shire.
“Additionally, with extended shelf life up to 24 months, treatment centers will have flexibility in inventory management to help ensure continuous treatment supply for patients.” ![]()
The European Commission (EC) has granted marketing authorization for a lyophilized formulation of pegaspargase (ONCASPAR).
The product is intended for use as a component of antineoplastic combination therapy in acute lymphoblastic leukemia patients of all ages.
The EC’s approval authorizes Shire to market lyophilized pegaspargase in the 28 member states of the European Union as well as Iceland, Liechtenstein, and Norway.
Lyophilized pegaspargase works the same way as the liquid formulation. By depleting serum L-asparagine levels and thereby interfering with protein synthesis, pegaspargase deprives lymphoblasts of L-asparagine, resulting in cell death.
The lyophilized formulation offers the same dosing regimen as liquid pegaspargase but also provides a shelf life of up to 24 months—3 times longer than that of the liquid formulation.
Shire expects lyophilized pegaspargase to be available in European markets beginning in the first half of 2018.
“With this lyophilized formulation, we aim to make pegylated asparaginase, part of the pediatric standard therapy in acute lymphoblastic leukemia, available to patients in countries where liquid ONCASPAR is not currently offered,” said Howard B. Mayer, MD, senior vice-president and ad-interim head of global research and development at Shire.
“Additionally, with extended shelf life up to 24 months, treatment centers will have flexibility in inventory management to help ensure continuous treatment supply for patients.” ![]()
The European Commission (EC) has granted marketing authorization for a lyophilized formulation of pegaspargase (ONCASPAR).
The product is intended for use as a component of antineoplastic combination therapy in acute lymphoblastic leukemia patients of all ages.
The EC’s approval authorizes Shire to market lyophilized pegaspargase in the 28 member states of the European Union as well as Iceland, Liechtenstein, and Norway.
Lyophilized pegaspargase works the same way as the liquid formulation. By depleting serum L-asparagine levels and thereby interfering with protein synthesis, pegaspargase deprives lymphoblasts of L-asparagine, resulting in cell death.
The lyophilized formulation offers the same dosing regimen as liquid pegaspargase but also provides a shelf life of up to 24 months—3 times longer than that of the liquid formulation.
Shire expects lyophilized pegaspargase to be available in European markets beginning in the first half of 2018.
“With this lyophilized formulation, we aim to make pegylated asparaginase, part of the pediatric standard therapy in acute lymphoblastic leukemia, available to patients in countries where liquid ONCASPAR is not currently offered,” said Howard B. Mayer, MD, senior vice-president and ad-interim head of global research and development at Shire.
“Additionally, with extended shelf life up to 24 months, treatment centers will have flexibility in inventory management to help ensure continuous treatment supply for patients.” ![]()
Technique may be effective for diagnosing NHL
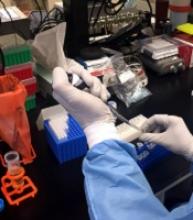
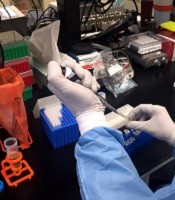
Preclinical research suggests infrared spectroscopy could be used to diagnose non-Hodgkin lymphoma (NHL).
Researchers used mid-infrared spectroscopy to analyze blood serum derived from mice and differentiate mice with NHL and subcutaneous melanoma from each other and from healthy control mice.
The findings suggest infrared spectroscopy can detect biochemical changes induced by NHL and melanoma and therefore has diagnostic potential as a screening technique for these cancers.
A.G. Unil Perera, PhD, of Georgia State University in Atlanta, and his colleagues detailed these findings in Scientific Reports.
The researchers said that Fourier Transform Infrared (FTIR) spectroscopy in Attenuated Total Reflection (ATR) sampling mode provides high-quality results with better reproducibility compared to other vibrational spectroscopy.
With previous work, Dr Perera and his colleagues discovered that a blood test for ulcerative colitis using ATR-FTIR spectroscopy could provide a cheaper, less invasive alternative for screening compared to colonoscopy.
In the current study, the researchers tested ATR-FTIR spectroscopy in mouse models of malignancy—EL4 NHL and B16 subcutaneous melanoma.
The team extracted blood serum from these mice and control mice. Droplets of serum were placed on an ATR crystal of the FTIR instrument.
Incident infrared beams were absorbed and reflected by the serum, creating a wave that was recorded and used to produce an absorbance curve with peaks that identified the presence of certain biomarkers in the sample.
The researchers compared the absorbance curves from the control and cancer mice and assessed biochemical changes induced by NHL and melanoma.
The team found “remarkable” differences between the ATR-FTIR spectra of serum samples from tumor-bearing mice and control mice.
Dr Perera said these findings are applicable to humans because mice and humans have some biomarkers and chemicals in common.
Using the data collected on the biomarkers for NHL and melanoma, the researchers could develop detectors for these particular absorbance peaks, which doctors could use to test patients’ blood samples for these cancers.
“Our final goal is to say we can use this infrared technique to identify various diseases,” Dr Perera said. “This study shows infrared spectroscopy can identify cancer. Right now, when you go to the doctor, they do blood tests for sugar and several other things but not for serious diseases like cancer and colitis.”
“One day, we hope that even these serious diseases can be rapidly screened. Your primary doctor could keep a record of your number and check that every time you come back. Then, if there is some indication of cancer or colitis, they can do biopsies, colonoscopies, etc.” ![]()
Preclinical research suggests infrared spectroscopy could be used to diagnose non-Hodgkin lymphoma (NHL).
Researchers used mid-infrared spectroscopy to analyze blood serum derived from mice and differentiate mice with NHL and subcutaneous melanoma from each other and from healthy control mice.
The findings suggest infrared spectroscopy can detect biochemical changes induced by NHL and melanoma and therefore has diagnostic potential as a screening technique for these cancers.
A.G. Unil Perera, PhD, of Georgia State University in Atlanta, and his colleagues detailed these findings in Scientific Reports.
The researchers said that Fourier Transform Infrared (FTIR) spectroscopy in Attenuated Total Reflection (ATR) sampling mode provides high-quality results with better reproducibility compared to other vibrational spectroscopy.
With previous work, Dr Perera and his colleagues discovered that a blood test for ulcerative colitis using ATR-FTIR spectroscopy could provide a cheaper, less invasive alternative for screening compared to colonoscopy.
In the current study, the researchers tested ATR-FTIR spectroscopy in mouse models of malignancy—EL4 NHL and B16 subcutaneous melanoma.
The team extracted blood serum from these mice and control mice. Droplets of serum were placed on an ATR crystal of the FTIR instrument.
Incident infrared beams were absorbed and reflected by the serum, creating a wave that was recorded and used to produce an absorbance curve with peaks that identified the presence of certain biomarkers in the sample.
The researchers compared the absorbance curves from the control and cancer mice and assessed biochemical changes induced by NHL and melanoma.
The team found “remarkable” differences between the ATR-FTIR spectra of serum samples from tumor-bearing mice and control mice.
Dr Perera said these findings are applicable to humans because mice and humans have some biomarkers and chemicals in common.
Using the data collected on the biomarkers for NHL and melanoma, the researchers could develop detectors for these particular absorbance peaks, which doctors could use to test patients’ blood samples for these cancers.
“Our final goal is to say we can use this infrared technique to identify various diseases,” Dr Perera said. “This study shows infrared spectroscopy can identify cancer. Right now, when you go to the doctor, they do blood tests for sugar and several other things but not for serious diseases like cancer and colitis.”
“One day, we hope that even these serious diseases can be rapidly screened. Your primary doctor could keep a record of your number and check that every time you come back. Then, if there is some indication of cancer or colitis, they can do biopsies, colonoscopies, etc.” ![]()
Preclinical research suggests infrared spectroscopy could be used to diagnose non-Hodgkin lymphoma (NHL).
Researchers used mid-infrared spectroscopy to analyze blood serum derived from mice and differentiate mice with NHL and subcutaneous melanoma from each other and from healthy control mice.
The findings suggest infrared spectroscopy can detect biochemical changes induced by NHL and melanoma and therefore has diagnostic potential as a screening technique for these cancers.
A.G. Unil Perera, PhD, of Georgia State University in Atlanta, and his colleagues detailed these findings in Scientific Reports.
The researchers said that Fourier Transform Infrared (FTIR) spectroscopy in Attenuated Total Reflection (ATR) sampling mode provides high-quality results with better reproducibility compared to other vibrational spectroscopy.
With previous work, Dr Perera and his colleagues discovered that a blood test for ulcerative colitis using ATR-FTIR spectroscopy could provide a cheaper, less invasive alternative for screening compared to colonoscopy.
In the current study, the researchers tested ATR-FTIR spectroscopy in mouse models of malignancy—EL4 NHL and B16 subcutaneous melanoma.
The team extracted blood serum from these mice and control mice. Droplets of serum were placed on an ATR crystal of the FTIR instrument.
Incident infrared beams were absorbed and reflected by the serum, creating a wave that was recorded and used to produce an absorbance curve with peaks that identified the presence of certain biomarkers in the sample.
The researchers compared the absorbance curves from the control and cancer mice and assessed biochemical changes induced by NHL and melanoma.
The team found “remarkable” differences between the ATR-FTIR spectra of serum samples from tumor-bearing mice and control mice.
Dr Perera said these findings are applicable to humans because mice and humans have some biomarkers and chemicals in common.
Using the data collected on the biomarkers for NHL and melanoma, the researchers could develop detectors for these particular absorbance peaks, which doctors could use to test patients’ blood samples for these cancers.
“Our final goal is to say we can use this infrared technique to identify various diseases,” Dr Perera said. “This study shows infrared spectroscopy can identify cancer. Right now, when you go to the doctor, they do blood tests for sugar and several other things but not for serious diseases like cancer and colitis.”
“One day, we hope that even these serious diseases can be rapidly screened. Your primary doctor could keep a record of your number and check that every time you come back. Then, if there is some indication of cancer or colitis, they can do biopsies, colonoscopies, etc.” ![]()
Method may improve HSC mobilization, engraftment
New research suggests a 2-drug combination might improve hematopoietic stem cell transplant (HSCT) for donors and recipients.
Researchers found that a single dose of the drugs provides HSC mobilization that rivals 5-day treatment with granulocyte colony-stimulating factor (G-CSF).
And the combination mobilizes HSCs that have higher engraftment efficiency than HSCs mobilized by G-CSF.
Jonathan Hoggatt, PhD, of Massachusetts General Hospital in Boston, and his colleagues reported these findings in Cell.
“Our new method of harvesting stem cells requires only a single injection and mobilizes the cells needed in 15 minutes,” Dr Hoggatt said. “So in the time it takes to boil an egg, we are able to acquire the number of stem cells produced by the current standard 5-day protocol. This means less pain, time off work, and lifestyle disruption for the donor, more convenience for the clinical staff, and more predictability for the harvesting procedure.”
Dr Hoggatt and his colleagues have investigated ways to enhance HSC donation for several years. In a previous study, the researchers found that a CXCR2 agonist called GRO-beta induced rapid movement of HSCs from the marrow into the blood in animal models.
Initial experiments in the current study revealed that GRO-beta injections were safe and well tolerated in human volunteers but had only a modest effect in mobilizing HSCs. Therefore, the team tried combining GRO-beta with the CXCR4 antagonist AMD3100 (plerixafor).
The researchers found that simultaneous administration of both drugs rapidly (within 15 minutes) produced a quantity of HSCs equal to that provided by the 5-day G-CSF protocol.
When transplanted in mice, the HSCs mobilized by AMD3100 and GRO-beta prompted faster reconstitution of bone marrow and recovery of immune cell populations than HSCs mobilized by G-CSF.
The HSCs mobilized by AMD3100 and GRO-beta showed patterns of gene expression similar to those of fetal HSCs.
“These highly engraftable hematopoietic stem cells produced by our new strategy are essentially the A+ students of bone marrow stem cells,” Dr Hoggatt said. “Finding that they express genes similar to those of fetal liver HSCs . . . suggests that they will be very good at moving into an empty bone marrow space and rapidly dividing to fill the marrow and produce blood. Now, we need to test the combination in a clinical trial to confirm its safety and effectiveness in humans.” ![]()
New research suggests a 2-drug combination might improve hematopoietic stem cell transplant (HSCT) for donors and recipients.
Researchers found that a single dose of the drugs provides HSC mobilization that rivals 5-day treatment with granulocyte colony-stimulating factor (G-CSF).
And the combination mobilizes HSCs that have higher engraftment efficiency than HSCs mobilized by G-CSF.
Jonathan Hoggatt, PhD, of Massachusetts General Hospital in Boston, and his colleagues reported these findings in Cell.
“Our new method of harvesting stem cells requires only a single injection and mobilizes the cells needed in 15 minutes,” Dr Hoggatt said. “So in the time it takes to boil an egg, we are able to acquire the number of stem cells produced by the current standard 5-day protocol. This means less pain, time off work, and lifestyle disruption for the donor, more convenience for the clinical staff, and more predictability for the harvesting procedure.”
Dr Hoggatt and his colleagues have investigated ways to enhance HSC donation for several years. In a previous study, the researchers found that a CXCR2 agonist called GRO-beta induced rapid movement of HSCs from the marrow into the blood in animal models.
Initial experiments in the current study revealed that GRO-beta injections were safe and well tolerated in human volunteers but had only a modest effect in mobilizing HSCs. Therefore, the team tried combining GRO-beta with the CXCR4 antagonist AMD3100 (plerixafor).
The researchers found that simultaneous administration of both drugs rapidly (within 15 minutes) produced a quantity of HSCs equal to that provided by the 5-day G-CSF protocol.
When transplanted in mice, the HSCs mobilized by AMD3100 and GRO-beta prompted faster reconstitution of bone marrow and recovery of immune cell populations than HSCs mobilized by G-CSF.
The HSCs mobilized by AMD3100 and GRO-beta showed patterns of gene expression similar to those of fetal HSCs.
“These highly engraftable hematopoietic stem cells produced by our new strategy are essentially the A+ students of bone marrow stem cells,” Dr Hoggatt said. “Finding that they express genes similar to those of fetal liver HSCs . . . suggests that they will be very good at moving into an empty bone marrow space and rapidly dividing to fill the marrow and produce blood. Now, we need to test the combination in a clinical trial to confirm its safety and effectiveness in humans.” ![]()
New research suggests a 2-drug combination might improve hematopoietic stem cell transplant (HSCT) for donors and recipients.
Researchers found that a single dose of the drugs provides HSC mobilization that rivals 5-day treatment with granulocyte colony-stimulating factor (G-CSF).
And the combination mobilizes HSCs that have higher engraftment efficiency than HSCs mobilized by G-CSF.
Jonathan Hoggatt, PhD, of Massachusetts General Hospital in Boston, and his colleagues reported these findings in Cell.
“Our new method of harvesting stem cells requires only a single injection and mobilizes the cells needed in 15 minutes,” Dr Hoggatt said. “So in the time it takes to boil an egg, we are able to acquire the number of stem cells produced by the current standard 5-day protocol. This means less pain, time off work, and lifestyle disruption for the donor, more convenience for the clinical staff, and more predictability for the harvesting procedure.”
Dr Hoggatt and his colleagues have investigated ways to enhance HSC donation for several years. In a previous study, the researchers found that a CXCR2 agonist called GRO-beta induced rapid movement of HSCs from the marrow into the blood in animal models.
Initial experiments in the current study revealed that GRO-beta injections were safe and well tolerated in human volunteers but had only a modest effect in mobilizing HSCs. Therefore, the team tried combining GRO-beta with the CXCR4 antagonist AMD3100 (plerixafor).
The researchers found that simultaneous administration of both drugs rapidly (within 15 minutes) produced a quantity of HSCs equal to that provided by the 5-day G-CSF protocol.
When transplanted in mice, the HSCs mobilized by AMD3100 and GRO-beta prompted faster reconstitution of bone marrow and recovery of immune cell populations than HSCs mobilized by G-CSF.
The HSCs mobilized by AMD3100 and GRO-beta showed patterns of gene expression similar to those of fetal HSCs.
“These highly engraftable hematopoietic stem cells produced by our new strategy are essentially the A+ students of bone marrow stem cells,” Dr Hoggatt said. “Finding that they express genes similar to those of fetal liver HSCs . . . suggests that they will be very good at moving into an empty bone marrow space and rapidly dividing to fill the marrow and produce blood. Now, we need to test the combination in a clinical trial to confirm its safety and effectiveness in humans.” ![]()
Procedure deemed unnecessary in most DVT patients
Researchers have found evidence to suggest that pharmacomechanical catheter-directed thrombolysis is largely inappropriate as first-line treatment for patients with acute proximal deep vein thrombosis (DVT).
The team found that anticoagulation plus pharmacomechanical thrombolysis was no more effective than anticoagulation alone for preventing post-thrombotic syndrome (PTS).
Additionally, patients who received pharmacomechanical thrombolysis had a higher risk of major bleeding.
The researchers reported these findings in NEJM.
The trial, known as the ATTRACT study, was designed to determine whether performing pharmacomechanical thrombolysis as part of initial treatment for patients with DVT would reduce the number of patients who later develop PTS.
“The clinical research in deep vein thrombosis and post-thrombotic syndrome is very important to the clinical community and of interest to the National Heart, Lung, and Blood Institute [NHLBI],” said Andrei Kindzelski, MD, PhD, the NHLBI program officer for the ATTRACT trial.
“This landmark study, conducted at 56 clinical sites, demonstrated, in an unbiased manner, no benefits of catheter-directed thrombolysis as a first-line deep vein thrombosis treatment, enabling patients to avoid an unnecessary medical procedure. At the same time, ATTRACT identified a potential future research need in more targeted use of catheter-directed thrombolysis in specific patient groups.”
The study included 692 patients who were randomized to receive anticoagulation alone or anticoagulation plus pharmacomechanical thrombolysis.
Anticoagulation consisted of unfractionated heparin, enoxaparin, dalteparin, or tinzaparin for at least 5 days, overlapped with long-term warfarin, as well as the prescription of elastic compression stockings.
Pharmacomechanical thrombolysis consisted of catheter-mediated or device-mediated intrathrombus delivery of recombinant tissue plasminogen activator and thrombus aspiration or maceration, with or without stenting.
Results
The study’s primary outcome was the development of PTS between 6 and 24 months of follow-up.
There was no significant difference in PTS incidence between the treatment arms. PTS occurred in 47% (157/336) of patients in the pharmacomechanical-thrombolysis group and 48% (171/355) of patients in the control group (risk ratio=0.96, P=0.56).
Pharmacomechanical thrombolysis did reduce the severity of PTS, however. The incidence of moderate-to-severe PTS was 24% in the control group and 18% in the pharmacomechanical-thrombolysis group (risk ratio=0.73; P=0.04).
Severity scores for PTS were significantly lower in the pharmacomechanical-thrombolysis group than the control group at 6, 12, 18, and 24 months of follow-up (P<0.01 for each time point).
There was no significant difference between the treatment arms in the incidence of recurrent venous thromboembolism (VTE) over the 24-month follow-up period. Recurrent VTE was observed in 12% of patients in the pharmacomechanical-thrombolysis group and 8% of controls (P=0.09).
On the other hand, there was a significant increase in the incidence of major bleeding within 10 days in the pharmacomechanical-thrombolysis group. The incidence was 1.7% (n=6) in the pharmacomechanical thrombolysis group and 0.3% (n=1) in the control group (P=0.049).
“None of us was surprised to find that this treatment [pharmacomechanical thrombolysis] is riskier than blood-thinning drugs alone,” said study author Suresh Vedantham, MD, of Washington University School of Medicine in St. Louis, Missouri.
“To justify that extra risk, we would have had to show a dramatic improvement in long-term outcomes, and the study didn’t show that. We saw some improvement in disease severity but not enough to justify the risks for most patients.”
While the results indicate that most patients should not undergo pharmacomechanical thrombolysis, the data also hint that the benefits may outweigh the risks in some patients, such as those with exceptionally large clots.
“This is the first large, rigorous study to examine the ability of imaging-guided treatment to address post-thrombotic syndrome,” Dr Vedantham said. “This study will advance patient care by helping many people avoid an unnecessary procedure.”
“The findings are also interesting because there is the suggestion that at least some patients may have benefited. Sorting that out is going to be very important.”
For now, pharmacomechanical thrombolysis should be reserved for use as a second-line treatment for some carefully selected patients who are experiencing particularly severe limitations of leg function from DVT and who are not responding to anticoagulation alone, Dr Vedantham added.
This research was sponsored by NHLBI. Additional funding was provided by Boston Scientific, Covidien (now Medtronic), and Genentech, which provided recombinant tissue plasminogen activator for the study. Compression stockings were donated by BSN Medical. ![]()
Researchers have found evidence to suggest that pharmacomechanical catheter-directed thrombolysis is largely inappropriate as first-line treatment for patients with acute proximal deep vein thrombosis (DVT).
The team found that anticoagulation plus pharmacomechanical thrombolysis was no more effective than anticoagulation alone for preventing post-thrombotic syndrome (PTS).
Additionally, patients who received pharmacomechanical thrombolysis had a higher risk of major bleeding.
The researchers reported these findings in NEJM.
The trial, known as the ATTRACT study, was designed to determine whether performing pharmacomechanical thrombolysis as part of initial treatment for patients with DVT would reduce the number of patients who later develop PTS.
“The clinical research in deep vein thrombosis and post-thrombotic syndrome is very important to the clinical community and of interest to the National Heart, Lung, and Blood Institute [NHLBI],” said Andrei Kindzelski, MD, PhD, the NHLBI program officer for the ATTRACT trial.
“This landmark study, conducted at 56 clinical sites, demonstrated, in an unbiased manner, no benefits of catheter-directed thrombolysis as a first-line deep vein thrombosis treatment, enabling patients to avoid an unnecessary medical procedure. At the same time, ATTRACT identified a potential future research need in more targeted use of catheter-directed thrombolysis in specific patient groups.”
The study included 692 patients who were randomized to receive anticoagulation alone or anticoagulation plus pharmacomechanical thrombolysis.
Anticoagulation consisted of unfractionated heparin, enoxaparin, dalteparin, or tinzaparin for at least 5 days, overlapped with long-term warfarin, as well as the prescription of elastic compression stockings.
Pharmacomechanical thrombolysis consisted of catheter-mediated or device-mediated intrathrombus delivery of recombinant tissue plasminogen activator and thrombus aspiration or maceration, with or without stenting.
Results
The study’s primary outcome was the development of PTS between 6 and 24 months of follow-up.
There was no significant difference in PTS incidence between the treatment arms. PTS occurred in 47% (157/336) of patients in the pharmacomechanical-thrombolysis group and 48% (171/355) of patients in the control group (risk ratio=0.96, P=0.56).
Pharmacomechanical thrombolysis did reduce the severity of PTS, however. The incidence of moderate-to-severe PTS was 24% in the control group and 18% in the pharmacomechanical-thrombolysis group (risk ratio=0.73; P=0.04).
Severity scores for PTS were significantly lower in the pharmacomechanical-thrombolysis group than the control group at 6, 12, 18, and 24 months of follow-up (P<0.01 for each time point).
There was no significant difference between the treatment arms in the incidence of recurrent venous thromboembolism (VTE) over the 24-month follow-up period. Recurrent VTE was observed in 12% of patients in the pharmacomechanical-thrombolysis group and 8% of controls (P=0.09).
On the other hand, there was a significant increase in the incidence of major bleeding within 10 days in the pharmacomechanical-thrombolysis group. The incidence was 1.7% (n=6) in the pharmacomechanical thrombolysis group and 0.3% (n=1) in the control group (P=0.049).
“None of us was surprised to find that this treatment [pharmacomechanical thrombolysis] is riskier than blood-thinning drugs alone,” said study author Suresh Vedantham, MD, of Washington University School of Medicine in St. Louis, Missouri.
“To justify that extra risk, we would have had to show a dramatic improvement in long-term outcomes, and the study didn’t show that. We saw some improvement in disease severity but not enough to justify the risks for most patients.”
While the results indicate that most patients should not undergo pharmacomechanical thrombolysis, the data also hint that the benefits may outweigh the risks in some patients, such as those with exceptionally large clots.
“This is the first large, rigorous study to examine the ability of imaging-guided treatment to address post-thrombotic syndrome,” Dr Vedantham said. “This study will advance patient care by helping many people avoid an unnecessary procedure.”
“The findings are also interesting because there is the suggestion that at least some patients may have benefited. Sorting that out is going to be very important.”
For now, pharmacomechanical thrombolysis should be reserved for use as a second-line treatment for some carefully selected patients who are experiencing particularly severe limitations of leg function from DVT and who are not responding to anticoagulation alone, Dr Vedantham added.
This research was sponsored by NHLBI. Additional funding was provided by Boston Scientific, Covidien (now Medtronic), and Genentech, which provided recombinant tissue plasminogen activator for the study. Compression stockings were donated by BSN Medical. ![]()
Researchers have found evidence to suggest that pharmacomechanical catheter-directed thrombolysis is largely inappropriate as first-line treatment for patients with acute proximal deep vein thrombosis (DVT).
The team found that anticoagulation plus pharmacomechanical thrombolysis was no more effective than anticoagulation alone for preventing post-thrombotic syndrome (PTS).
Additionally, patients who received pharmacomechanical thrombolysis had a higher risk of major bleeding.
The researchers reported these findings in NEJM.
The trial, known as the ATTRACT study, was designed to determine whether performing pharmacomechanical thrombolysis as part of initial treatment for patients with DVT would reduce the number of patients who later develop PTS.
“The clinical research in deep vein thrombosis and post-thrombotic syndrome is very important to the clinical community and of interest to the National Heart, Lung, and Blood Institute [NHLBI],” said Andrei Kindzelski, MD, PhD, the NHLBI program officer for the ATTRACT trial.
“This landmark study, conducted at 56 clinical sites, demonstrated, in an unbiased manner, no benefits of catheter-directed thrombolysis as a first-line deep vein thrombosis treatment, enabling patients to avoid an unnecessary medical procedure. At the same time, ATTRACT identified a potential future research need in more targeted use of catheter-directed thrombolysis in specific patient groups.”
The study included 692 patients who were randomized to receive anticoagulation alone or anticoagulation plus pharmacomechanical thrombolysis.
Anticoagulation consisted of unfractionated heparin, enoxaparin, dalteparin, or tinzaparin for at least 5 days, overlapped with long-term warfarin, as well as the prescription of elastic compression stockings.
Pharmacomechanical thrombolysis consisted of catheter-mediated or device-mediated intrathrombus delivery of recombinant tissue plasminogen activator and thrombus aspiration or maceration, with or without stenting.
Results
The study’s primary outcome was the development of PTS between 6 and 24 months of follow-up.
There was no significant difference in PTS incidence between the treatment arms. PTS occurred in 47% (157/336) of patients in the pharmacomechanical-thrombolysis group and 48% (171/355) of patients in the control group (risk ratio=0.96, P=0.56).
Pharmacomechanical thrombolysis did reduce the severity of PTS, however. The incidence of moderate-to-severe PTS was 24% in the control group and 18% in the pharmacomechanical-thrombolysis group (risk ratio=0.73; P=0.04).
Severity scores for PTS were significantly lower in the pharmacomechanical-thrombolysis group than the control group at 6, 12, 18, and 24 months of follow-up (P<0.01 for each time point).
There was no significant difference between the treatment arms in the incidence of recurrent venous thromboembolism (VTE) over the 24-month follow-up period. Recurrent VTE was observed in 12% of patients in the pharmacomechanical-thrombolysis group and 8% of controls (P=0.09).
On the other hand, there was a significant increase in the incidence of major bleeding within 10 days in the pharmacomechanical-thrombolysis group. The incidence was 1.7% (n=6) in the pharmacomechanical thrombolysis group and 0.3% (n=1) in the control group (P=0.049).
“None of us was surprised to find that this treatment [pharmacomechanical thrombolysis] is riskier than blood-thinning drugs alone,” said study author Suresh Vedantham, MD, of Washington University School of Medicine in St. Louis, Missouri.
“To justify that extra risk, we would have had to show a dramatic improvement in long-term outcomes, and the study didn’t show that. We saw some improvement in disease severity but not enough to justify the risks for most patients.”
While the results indicate that most patients should not undergo pharmacomechanical thrombolysis, the data also hint that the benefits may outweigh the risks in some patients, such as those with exceptionally large clots.
“This is the first large, rigorous study to examine the ability of imaging-guided treatment to address post-thrombotic syndrome,” Dr Vedantham said. “This study will advance patient care by helping many people avoid an unnecessary procedure.”
“The findings are also interesting because there is the suggestion that at least some patients may have benefited. Sorting that out is going to be very important.”
For now, pharmacomechanical thrombolysis should be reserved for use as a second-line treatment for some carefully selected patients who are experiencing particularly severe limitations of leg function from DVT and who are not responding to anticoagulation alone, Dr Vedantham added.
This research was sponsored by NHLBI. Additional funding was provided by Boston Scientific, Covidien (now Medtronic), and Genentech, which provided recombinant tissue plasminogen activator for the study. Compression stockings were donated by BSN Medical. ![]()
Gene-based Zika vaccine proves immunogenic in healthy adults
An experimental Zika vaccine is safe and induces an immune response in healthy adults, according to research published in The Lancet.
Investigators tested 2 potential Zika vaccines, VRC5288 and VRC5283, in a pair of phase 1 trials.
Both vaccines were considered well-tolerated, but one of them, VRC5283, induced a greater immune response than the other.
Both vaccines were developed by investigators at the National Institute of Allergy and Infectious Diseases (NIAID).
Now, NIAID is leading an international effort to evaluate VRC5283 in a phase 2/2b trial.
“Following early reports that Zika infection during pregnancy can lead to birth defects, NIAID scientists rapidly created one of the first investigational Zika vaccines using a DNA-based platform and began initial studies in healthy adults less than 1 year later,” said NIAID Director Anthony S. Fauci, MD.
To create their vaccines, the investigators inserted into plasmids genes that encode proteins found on the surface of the Zika virus.
The team developed 2 different plasmids for clinical testing: VRC5288 (Zika virus and Japanese encephalitis virus chimera) and VRC5283 (wild-type Zika virus).
In August 2016, NIAID initiated a phase 1 trial of the VRC5288 plasmid in 80 healthy volunteers ages 18 to 35. Subjects received a 4 mg dose via a needle and syringe injection in the arm muscle.
They received doses of VRC5288 at 0 and 8 weeks; 0 and 12 weeks; 0, 4, and 8 weeks; or 0, 4, and 20 weeks.
In December 2016, NIAID initiated a separate trial testing the VRC5283 plasmid. This study enrolled 45 healthy volunteers ages 18 to 50.
Subjects in this trial received 4 mg doses of VRC5283 at 0, 4, and 8 weeks. They were vaccinated in 3 different ways—via single-dose needle and syringe injection in 1 arm, via split-dose needle and syringe injection in each arm, or via needle-free injection in each arm.
Safety
The vaccinations were considered safe and well-tolerated in both trials, although some participants experienced mild to moderate reactions.
Local reactions (with VRC5288 and VRC5283, respectively) included pain/tenderness (mild—46% and 73%, moderate—0% and 7%), mild swelling (1% and 7%), and mild redness (6% and 2%).
Systemic reactions (with VRC5288 and VRC5283, respectively) included malaise (mild—25% and 33%, moderate—3% and 4%), myalgia (mild—18% and 13%, moderate—4% and 7%), headache (mild—19% and 29%, moderate—4% and 4%), chills (mild—6% and 2%, moderate—1% and 2%), nausea (mild—8% and 4%, moderate—1% and 0%), and joint pain (mild—5% and 16%, moderate—0% and 2%).
Immunogenicity
The investigators analyzed blood samples from all subjects 4 weeks after their final vaccinations.
The team found that 60% to 89% of subjects generated a neutralizing antibody response to VRC5288, and 77% to 100% of subjects generated a neutralizing antibody response to VRC5283.
Subjects who received VRC5283 via the needle-free injector all generated a neutralizing antibody response and had the highest levels of neutralizing antibodies.
Subjects who received VRC5283 in a split-dose administered to both arms had more robust immune responses than those receiving the full dose in 1 arm.
“NIAID has begun phase 2 testing of this candidate to determine if it can prevent Zika virus infection, and the promising phase 1 data . . . support its continued development,” Dr Fauci said. ![]()
An experimental Zika vaccine is safe and induces an immune response in healthy adults, according to research published in The Lancet.
Investigators tested 2 potential Zika vaccines, VRC5288 and VRC5283, in a pair of phase 1 trials.
Both vaccines were considered well-tolerated, but one of them, VRC5283, induced a greater immune response than the other.
Both vaccines were developed by investigators at the National Institute of Allergy and Infectious Diseases (NIAID).
Now, NIAID is leading an international effort to evaluate VRC5283 in a phase 2/2b trial.
“Following early reports that Zika infection during pregnancy can lead to birth defects, NIAID scientists rapidly created one of the first investigational Zika vaccines using a DNA-based platform and began initial studies in healthy adults less than 1 year later,” said NIAID Director Anthony S. Fauci, MD.
To create their vaccines, the investigators inserted into plasmids genes that encode proteins found on the surface of the Zika virus.
The team developed 2 different plasmids for clinical testing: VRC5288 (Zika virus and Japanese encephalitis virus chimera) and VRC5283 (wild-type Zika virus).
In August 2016, NIAID initiated a phase 1 trial of the VRC5288 plasmid in 80 healthy volunteers ages 18 to 35. Subjects received a 4 mg dose via a needle and syringe injection in the arm muscle.
They received doses of VRC5288 at 0 and 8 weeks; 0 and 12 weeks; 0, 4, and 8 weeks; or 0, 4, and 20 weeks.
In December 2016, NIAID initiated a separate trial testing the VRC5283 plasmid. This study enrolled 45 healthy volunteers ages 18 to 50.
Subjects in this trial received 4 mg doses of VRC5283 at 0, 4, and 8 weeks. They were vaccinated in 3 different ways—via single-dose needle and syringe injection in 1 arm, via split-dose needle and syringe injection in each arm, or via needle-free injection in each arm.
Safety
The vaccinations were considered safe and well-tolerated in both trials, although some participants experienced mild to moderate reactions.
Local reactions (with VRC5288 and VRC5283, respectively) included pain/tenderness (mild—46% and 73%, moderate—0% and 7%), mild swelling (1% and 7%), and mild redness (6% and 2%).
Systemic reactions (with VRC5288 and VRC5283, respectively) included malaise (mild—25% and 33%, moderate—3% and 4%), myalgia (mild—18% and 13%, moderate—4% and 7%), headache (mild—19% and 29%, moderate—4% and 4%), chills (mild—6% and 2%, moderate—1% and 2%), nausea (mild—8% and 4%, moderate—1% and 0%), and joint pain (mild—5% and 16%, moderate—0% and 2%).
Immunogenicity
The investigators analyzed blood samples from all subjects 4 weeks after their final vaccinations.
The team found that 60% to 89% of subjects generated a neutralizing antibody response to VRC5288, and 77% to 100% of subjects generated a neutralizing antibody response to VRC5283.
Subjects who received VRC5283 via the needle-free injector all generated a neutralizing antibody response and had the highest levels of neutralizing antibodies.
Subjects who received VRC5283 in a split-dose administered to both arms had more robust immune responses than those receiving the full dose in 1 arm.
“NIAID has begun phase 2 testing of this candidate to determine if it can prevent Zika virus infection, and the promising phase 1 data . . . support its continued development,” Dr Fauci said. ![]()
An experimental Zika vaccine is safe and induces an immune response in healthy adults, according to research published in The Lancet.
Investigators tested 2 potential Zika vaccines, VRC5288 and VRC5283, in a pair of phase 1 trials.
Both vaccines were considered well-tolerated, but one of them, VRC5283, induced a greater immune response than the other.
Both vaccines were developed by investigators at the National Institute of Allergy and Infectious Diseases (NIAID).
Now, NIAID is leading an international effort to evaluate VRC5283 in a phase 2/2b trial.
“Following early reports that Zika infection during pregnancy can lead to birth defects, NIAID scientists rapidly created one of the first investigational Zika vaccines using a DNA-based platform and began initial studies in healthy adults less than 1 year later,” said NIAID Director Anthony S. Fauci, MD.
To create their vaccines, the investigators inserted into plasmids genes that encode proteins found on the surface of the Zika virus.
The team developed 2 different plasmids for clinical testing: VRC5288 (Zika virus and Japanese encephalitis virus chimera) and VRC5283 (wild-type Zika virus).
In August 2016, NIAID initiated a phase 1 trial of the VRC5288 plasmid in 80 healthy volunteers ages 18 to 35. Subjects received a 4 mg dose via a needle and syringe injection in the arm muscle.
They received doses of VRC5288 at 0 and 8 weeks; 0 and 12 weeks; 0, 4, and 8 weeks; or 0, 4, and 20 weeks.
In December 2016, NIAID initiated a separate trial testing the VRC5283 plasmid. This study enrolled 45 healthy volunteers ages 18 to 50.
Subjects in this trial received 4 mg doses of VRC5283 at 0, 4, and 8 weeks. They were vaccinated in 3 different ways—via single-dose needle and syringe injection in 1 arm, via split-dose needle and syringe injection in each arm, or via needle-free injection in each arm.
Safety
The vaccinations were considered safe and well-tolerated in both trials, although some participants experienced mild to moderate reactions.
Local reactions (with VRC5288 and VRC5283, respectively) included pain/tenderness (mild—46% and 73%, moderate—0% and 7%), mild swelling (1% and 7%), and mild redness (6% and 2%).
Systemic reactions (with VRC5288 and VRC5283, respectively) included malaise (mild—25% and 33%, moderate—3% and 4%), myalgia (mild—18% and 13%, moderate—4% and 7%), headache (mild—19% and 29%, moderate—4% and 4%), chills (mild—6% and 2%, moderate—1% and 2%), nausea (mild—8% and 4%, moderate—1% and 0%), and joint pain (mild—5% and 16%, moderate—0% and 2%).
Immunogenicity
The investigators analyzed blood samples from all subjects 4 weeks after their final vaccinations.
The team found that 60% to 89% of subjects generated a neutralizing antibody response to VRC5288, and 77% to 100% of subjects generated a neutralizing antibody response to VRC5283.
Subjects who received VRC5283 via the needle-free injector all generated a neutralizing antibody response and had the highest levels of neutralizing antibodies.
Subjects who received VRC5283 in a split-dose administered to both arms had more robust immune responses than those receiving the full dose in 1 arm.
“NIAID has begun phase 2 testing of this candidate to determine if it can prevent Zika virus infection, and the promising phase 1 data . . . support its continued development,” Dr Fauci said.
Gene therapy seems safe, effective in hemophilia B
The gene therapy SPK-9001 has produced positive results in a phase 1/2 trial of adults with hemophilia B, according to researchers.
SPK-9001 produced sustained factor IX (FIX) activity and allowed all 10 patients in this study to stop FIX prophylaxis.
Eight patients had no further FIX treatment after SPK-9001, and 9 patients had 0 bleeds.
There were no serious adverse events, and none of the patients had thrombotic events or developed FIX inhibitors.
“A one-time therapy sufficient to prevent bleeding without further medical intervention is the ideal treatment goal for patients with hemophilia,” said Lindsey A. George, MD, a hematologist at Children’s Hospital of Philadelphia in Pennsylvania.
“This cohort of 10 patients all safely experienced sustained clinical benefit after one infusion.”
Dr George and her colleagues reported these results in NEJM. The trial was sponsored by Spark Therapeutics and Pfizer.
SPK-9001 is an investigational vector that contains a bio-engineered adeno-associated virus capsid and a codon-optimized, high-activity human FIX gene enabling endogenous production of FIX.
The researchers tested SPK-9001 in 10 males with hemophilia B.
With a cumulative follow-up of 492 weeks, the mean steady-state FIX activity was 34% of normal (range, 14% to 81%) after a single administration of SPK-9001.
The annualized bleeding rate was reduced 97%, from a mean rate of 11.1 events per year before SPK-9001 administration to 0.4 events per year after (P=0.02).
Nine patients had 0 bleeds after SPK-9001, and 1 patient had 4 bleeds.
Use of FIX treatment was reduced 99% during this study, from a mean dose of 2908 IU/kg (range, 0 to 8090) before SPK-9001 to a mean dose of 49.3 IU/kg (range, 0 to 376) after SPK-9001 (P=0.004).
Two patients did receive FIX treatment after SPK-9001, but none of the patients received FIX prophylaxis.
The researchers noted that the patient who required FIX treatment for bleeding (4 events) had significant baseline joint damage. However, this patient still used 91% less FIX than before he received SPK-9001.
There were a total of 40 adverse events in this study, but none were serious. There were no deaths, no thrombotic events, and no cases of inhibitor development.
The only adverse events thought to be related to SPK-9001 were asymptomatic and transient increases in liver enzymes in 2 patients. These events resolved with a tapering dose of oral corticosteroids.
“People who live with hemophilia face a life-long need for vigilant monitoring and recurrent factor concentrate infusions to prevent spontaneous, potentially life-threatening bleeds and to protect their joints,” said study author Katherine High, MD, president and head of Research and Development at Spark Therapeutics.
“The data suggest a one-time infusion of SPK-9001 has the potential to safely sustain factor IX coagulant activity level that may result in the termination of baseline prophylaxis factor infusions, significantly reduce bleeding, and nearly eliminate the need for exogenous factor IX concentrate infusions.”
The gene therapy SPK-9001 has produced positive results in a phase 1/2 trial of adults with hemophilia B, according to researchers.
SPK-9001 produced sustained factor IX (FIX) activity and allowed all 10 patients in this study to stop FIX prophylaxis.
Eight patients had no further FIX treatment after SPK-9001, and 9 patients had 0 bleeds.
There were no serious adverse events, and none of the patients had thrombotic events or developed FIX inhibitors.
“A one-time therapy sufficient to prevent bleeding without further medical intervention is the ideal treatment goal for patients with hemophilia,” said Lindsey A. George, MD, a hematologist at Children’s Hospital of Philadelphia in Pennsylvania.
“This cohort of 10 patients all safely experienced sustained clinical benefit after one infusion.”
Dr George and her colleagues reported these results in NEJM. The trial was sponsored by Spark Therapeutics and Pfizer.
SPK-9001 is an investigational vector that contains a bio-engineered adeno-associated virus capsid and a codon-optimized, high-activity human FIX gene enabling endogenous production of FIX.
The researchers tested SPK-9001 in 10 males with hemophilia B.
With a cumulative follow-up of 492 weeks, the mean steady-state FIX activity was 34% of normal (range, 14% to 81%) after a single administration of SPK-9001.
The annualized bleeding rate was reduced 97%, from a mean rate of 11.1 events per year before SPK-9001 administration to 0.4 events per year after (P=0.02).
Nine patients had 0 bleeds after SPK-9001, and 1 patient had 4 bleeds.
Use of FIX treatment was reduced 99% during this study, from a mean dose of 2908 IU/kg (range, 0 to 8090) before SPK-9001 to a mean dose of 49.3 IU/kg (range, 0 to 376) after SPK-9001 (P=0.004).
Two patients did receive FIX treatment after SPK-9001, but none of the patients received FIX prophylaxis.
The researchers noted that the patient who required FIX treatment for bleeding (4 events) had significant baseline joint damage. However, this patient still used 91% less FIX than before he received SPK-9001.
There were a total of 40 adverse events in this study, but none were serious. There were no deaths, no thrombotic events, and no cases of inhibitor development.
The only adverse events thought to be related to SPK-9001 were asymptomatic and transient increases in liver enzymes in 2 patients. These events resolved with a tapering dose of oral corticosteroids.
“People who live with hemophilia face a life-long need for vigilant monitoring and recurrent factor concentrate infusions to prevent spontaneous, potentially life-threatening bleeds and to protect their joints,” said study author Katherine High, MD, president and head of Research and Development at Spark Therapeutics.
“The data suggest a one-time infusion of SPK-9001 has the potential to safely sustain factor IX coagulant activity level that may result in the termination of baseline prophylaxis factor infusions, significantly reduce bleeding, and nearly eliminate the need for exogenous factor IX concentrate infusions.”
The gene therapy SPK-9001 has produced positive results in a phase 1/2 trial of adults with hemophilia B, according to researchers.
SPK-9001 produced sustained factor IX (FIX) activity and allowed all 10 patients in this study to stop FIX prophylaxis.
Eight patients had no further FIX treatment after SPK-9001, and 9 patients had 0 bleeds.
There were no serious adverse events, and none of the patients had thrombotic events or developed FIX inhibitors.
“A one-time therapy sufficient to prevent bleeding without further medical intervention is the ideal treatment goal for patients with hemophilia,” said Lindsey A. George, MD, a hematologist at Children’s Hospital of Philadelphia in Pennsylvania.
“This cohort of 10 patients all safely experienced sustained clinical benefit after one infusion.”
Dr George and her colleagues reported these results in NEJM. The trial was sponsored by Spark Therapeutics and Pfizer.
SPK-9001 is an investigational vector that contains a bio-engineered adeno-associated virus capsid and a codon-optimized, high-activity human FIX gene enabling endogenous production of FIX.
The researchers tested SPK-9001 in 10 males with hemophilia B.
With a cumulative follow-up of 492 weeks, the mean steady-state FIX activity was 34% of normal (range, 14% to 81%) after a single administration of SPK-9001.
The annualized bleeding rate was reduced 97%, from a mean rate of 11.1 events per year before SPK-9001 administration to 0.4 events per year after (P=0.02).
Nine patients had 0 bleeds after SPK-9001, and 1 patient had 4 bleeds.
Use of FIX treatment was reduced 99% during this study, from a mean dose of 2908 IU/kg (range, 0 to 8090) before SPK-9001 to a mean dose of 49.3 IU/kg (range, 0 to 376) after SPK-9001 (P=0.004).
Two patients did receive FIX treatment after SPK-9001, but none of the patients received FIX prophylaxis.
The researchers noted that the patient who required FIX treatment for bleeding (4 events) had significant baseline joint damage. However, this patient still used 91% less FIX than before he received SPK-9001.
There were a total of 40 adverse events in this study, but none were serious. There were no deaths, no thrombotic events, and no cases of inhibitor development.
The only adverse events thought to be related to SPK-9001 were asymptomatic and transient increases in liver enzymes in 2 patients. These events resolved with a tapering dose of oral corticosteroids.
“People who live with hemophilia face a life-long need for vigilant monitoring and recurrent factor concentrate infusions to prevent spontaneous, potentially life-threatening bleeds and to protect their joints,” said study author Katherine High, MD, president and head of Research and Development at Spark Therapeutics.
“The data suggest a one-time infusion of SPK-9001 has the potential to safely sustain factor IX coagulant activity level that may result in the termination of baseline prophylaxis factor infusions, significantly reduce bleeding, and nearly eliminate the need for exogenous factor IX concentrate infusions.”
FDA lifts partial hold on nivolumab trials
The US Food and Drug Administration (FDA) has lifted the partial clinical hold placed on 2 trials of the PD-1 immune checkpoint inhibitor nivolumab (Opdivo).
In these trials, CheckMate-039 (CA209 -039) and CA204142, researchers are investigating nivolumab-based combinations in patients with relapsed or refractory multiple myeloma (MM).
The partial clinical hold on these trials was a result of risks identified in studies involving another anti-PD-1 agent, pembrolizumab.
Data from the pembrolizumab trials suggested that risks outweigh benefits when PD-1/PD-L1 treatment is given to MM patients in combination with dexamethasone and pomalidomide or lenalidomide.
In addition, there could be an unfavorable risk-benefit ratio for MM patients receiving PD-1/PD-L1 treatments alone or in other combinations.
Therefore, the FDA placed a partial hold on the following nivolumab trials:
- CheckMate-602: A randomized, phase 3 trial of combinations of nivolumab, elotuzumab, pomalidomide, and dexamethasone in relapsed and refractory MM
- CheckMate-039: A phase 1 study intended to establish the tolerability of nivolumab and the combination of nivolumab and daratumumab, with or without pomalidomide and dexamethasone, in patients with relapsed or refractory MM
- CA204142: A phase 2 study of elotuzumab in combination with pomalidomide and low-dose dexamethasone, and in combination with nivolumab, in patients with MM who relapsed after or were refractory to prior treatment with lenalidomide.
After consulting with Bristol-Myers Squibb, the FDA decided to lift the hold on CheckMate-039 (CA209 -039) and CA204142. These trials will continue with amended protocols.
The third trial, CheckMate-602, remains on partial clinical hold. Bristol-Myers Squibb said it is continuing to work with the FDA to determine next steps for this trial.
CheckMate-602 is not enrolling new patients. However, patients who are experiencing clinical benefit are continuing to receive treatment.
The US Food and Drug Administration (FDA) has lifted the partial clinical hold placed on 2 trials of the PD-1 immune checkpoint inhibitor nivolumab (Opdivo).
In these trials, CheckMate-039 (CA209 -039) and CA204142, researchers are investigating nivolumab-based combinations in patients with relapsed or refractory multiple myeloma (MM).
The partial clinical hold on these trials was a result of risks identified in studies involving another anti-PD-1 agent, pembrolizumab.
Data from the pembrolizumab trials suggested that risks outweigh benefits when PD-1/PD-L1 treatment is given to MM patients in combination with dexamethasone and pomalidomide or lenalidomide.
In addition, there could be an unfavorable risk-benefit ratio for MM patients receiving PD-1/PD-L1 treatments alone or in other combinations.
Therefore, the FDA placed a partial hold on the following nivolumab trials:
- CheckMate-602: A randomized, phase 3 trial of combinations of nivolumab, elotuzumab, pomalidomide, and dexamethasone in relapsed and refractory MM
- CheckMate-039: A phase 1 study intended to establish the tolerability of nivolumab and the combination of nivolumab and daratumumab, with or without pomalidomide and dexamethasone, in patients with relapsed or refractory MM
- CA204142: A phase 2 study of elotuzumab in combination with pomalidomide and low-dose dexamethasone, and in combination with nivolumab, in patients with MM who relapsed after or were refractory to prior treatment with lenalidomide.
After consulting with Bristol-Myers Squibb, the FDA decided to lift the hold on CheckMate-039 (CA209 -039) and CA204142. These trials will continue with amended protocols.
The third trial, CheckMate-602, remains on partial clinical hold. Bristol-Myers Squibb said it is continuing to work with the FDA to determine next steps for this trial.
CheckMate-602 is not enrolling new patients. However, patients who are experiencing clinical benefit are continuing to receive treatment.
The US Food and Drug Administration (FDA) has lifted the partial clinical hold placed on 2 trials of the PD-1 immune checkpoint inhibitor nivolumab (Opdivo).
In these trials, CheckMate-039 (CA209 -039) and CA204142, researchers are investigating nivolumab-based combinations in patients with relapsed or refractory multiple myeloma (MM).
The partial clinical hold on these trials was a result of risks identified in studies involving another anti-PD-1 agent, pembrolizumab.
Data from the pembrolizumab trials suggested that risks outweigh benefits when PD-1/PD-L1 treatment is given to MM patients in combination with dexamethasone and pomalidomide or lenalidomide.
In addition, there could be an unfavorable risk-benefit ratio for MM patients receiving PD-1/PD-L1 treatments alone or in other combinations.
Therefore, the FDA placed a partial hold on the following nivolumab trials:
- CheckMate-602: A randomized, phase 3 trial of combinations of nivolumab, elotuzumab, pomalidomide, and dexamethasone in relapsed and refractory MM
- CheckMate-039: A phase 1 study intended to establish the tolerability of nivolumab and the combination of nivolumab and daratumumab, with or without pomalidomide and dexamethasone, in patients with relapsed or refractory MM
- CA204142: A phase 2 study of elotuzumab in combination with pomalidomide and low-dose dexamethasone, and in combination with nivolumab, in patients with MM who relapsed after or were refractory to prior treatment with lenalidomide.
After consulting with Bristol-Myers Squibb, the FDA decided to lift the hold on CheckMate-039 (CA209 -039) and CA204142. These trials will continue with amended protocols.
The third trial, CheckMate-602, remains on partial clinical hold. Bristol-Myers Squibb said it is continuing to work with the FDA to determine next steps for this trial.
CheckMate-602 is not enrolling new patients. However, patients who are experiencing clinical benefit are continuing to receive treatment.
Company launches digital PCR test for monitoring CML
Bio-Rad Laboratories, Inc., has launched the QXDx BCR-ABL %IS Kit, a digital polymerase chain reaction (PCR) test that can monitor molecular response to therapy in patients with chronic myeloid leukemia (CML).
The kit has a CE-IVD mark and is available for in vitro diagnostic use in Europe, Hong Kong, and New Zealand.
The QXDx BCR-ABL %IS Kit uses Bio-Rad’s Droplet Digital PCR (ddPCR) technology to provide an absolute measure of BCR-ABL transcripts.
The kit measures BCR-ABL1 and ABL1 chromosomal transcripts in total RNA from whole blood of t(9;22)-positive CML patients expressing BCR-ABL1 fusion transcripts type e13a2 and/or e14a2.
The QXDx BCR-ABL %IS Kit measures the e13a2 and/or e14a2 transcripts of BCR-ABL1, normalized to the ABL1 endogenous control. The kit does not differentiate between e13a2 and e14a2 transcripts and does not monitor other rare fusion transcripts resulting from t(9;22).
The kit’s results are reported as percent reduction from a baseline of 100% on the International Scale (%IS) and on a log molecular reduction (MR) scale.
The kit is able to detect deep molecular response values of MR 4.7 (%IS 0.002) or MR 5.0 (%IS 0.001) in 2- or 4-well formats. This exceeds the typical limitations of reverse transcription quantitative PCR-based tests that are reliable down to MR 4.5 (%IS 0.0032).
Bio-Rad says the QXDx BCR-ABL %IS Kit delivers absolute quantitation, which eliminates the need for standard curves and minimizes variation between samples. The kit also provides scalable throughput, allowing for testing of 8 to 48 samples per run.
The QXDx BCR-ABL %IS Kit can be used with Bio-Rad’s QX200 AutoDG ddPCR Dx System or with the QX200 ddPCR Dx System. The QXDx BCR-ABL %IS Kit uses QuantaSoft Software v1.7 for data acquisition and output.
Bio-Rad Laboratories, Inc., has launched the QXDx BCR-ABL %IS Kit, a digital polymerase chain reaction (PCR) test that can monitor molecular response to therapy in patients with chronic myeloid leukemia (CML).
The kit has a CE-IVD mark and is available for in vitro diagnostic use in Europe, Hong Kong, and New Zealand.
The QXDx BCR-ABL %IS Kit uses Bio-Rad’s Droplet Digital PCR (ddPCR) technology to provide an absolute measure of BCR-ABL transcripts.
The kit measures BCR-ABL1 and ABL1 chromosomal transcripts in total RNA from whole blood of t(9;22)-positive CML patients expressing BCR-ABL1 fusion transcripts type e13a2 and/or e14a2.
The QXDx BCR-ABL %IS Kit measures the e13a2 and/or e14a2 transcripts of BCR-ABL1, normalized to the ABL1 endogenous control. The kit does not differentiate between e13a2 and e14a2 transcripts and does not monitor other rare fusion transcripts resulting from t(9;22).
The kit’s results are reported as percent reduction from a baseline of 100% on the International Scale (%IS) and on a log molecular reduction (MR) scale.
The kit is able to detect deep molecular response values of MR 4.7 (%IS 0.002) or MR 5.0 (%IS 0.001) in 2- or 4-well formats. This exceeds the typical limitations of reverse transcription quantitative PCR-based tests that are reliable down to MR 4.5 (%IS 0.0032).
Bio-Rad says the QXDx BCR-ABL %IS Kit delivers absolute quantitation, which eliminates the need for standard curves and minimizes variation between samples. The kit also provides scalable throughput, allowing for testing of 8 to 48 samples per run.
The QXDx BCR-ABL %IS Kit can be used with Bio-Rad’s QX200 AutoDG ddPCR Dx System or with the QX200 ddPCR Dx System. The QXDx BCR-ABL %IS Kit uses QuantaSoft Software v1.7 for data acquisition and output.
Bio-Rad Laboratories, Inc., has launched the QXDx BCR-ABL %IS Kit, a digital polymerase chain reaction (PCR) test that can monitor molecular response to therapy in patients with chronic myeloid leukemia (CML).
The kit has a CE-IVD mark and is available for in vitro diagnostic use in Europe, Hong Kong, and New Zealand.
The QXDx BCR-ABL %IS Kit uses Bio-Rad’s Droplet Digital PCR (ddPCR) technology to provide an absolute measure of BCR-ABL transcripts.
The kit measures BCR-ABL1 and ABL1 chromosomal transcripts in total RNA from whole blood of t(9;22)-positive CML patients expressing BCR-ABL1 fusion transcripts type e13a2 and/or e14a2.
The QXDx BCR-ABL %IS Kit measures the e13a2 and/or e14a2 transcripts of BCR-ABL1, normalized to the ABL1 endogenous control. The kit does not differentiate between e13a2 and e14a2 transcripts and does not monitor other rare fusion transcripts resulting from t(9;22).
The kit’s results are reported as percent reduction from a baseline of 100% on the International Scale (%IS) and on a log molecular reduction (MR) scale.
The kit is able to detect deep molecular response values of MR 4.7 (%IS 0.002) or MR 5.0 (%IS 0.001) in 2- or 4-well formats. This exceeds the typical limitations of reverse transcription quantitative PCR-based tests that are reliable down to MR 4.5 (%IS 0.0032).
Bio-Rad says the QXDx BCR-ABL %IS Kit delivers absolute quantitation, which eliminates the need for standard curves and minimizes variation between samples. The kit also provides scalable throughput, allowing for testing of 8 to 48 samples per run.
The QXDx BCR-ABL %IS Kit can be used with Bio-Rad’s QX200 AutoDG ddPCR Dx System or with the QX200 ddPCR Dx System. The QXDx BCR-ABL %IS Kit uses QuantaSoft Software v1.7 for data acquisition and output.