User login
FDA grants orphan designation to drug for AML
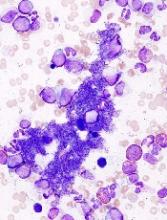
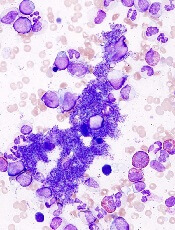
The US Food and Drug Administration (FDA) has granted orphan drug designation to CG’806 for the treatment of patients with acute myeloid leukemia (AML).
CG’806 is an oral, first-in-class pan-FLT3/pan-BTK inhibitor being developed by Aptose Biosciences Inc.
In preclinical studies, CG’806 inhibited all wild-type and mutant forms of FLT3 tested, suppressed multiple oncogenic pathways operative in AML, and eliminated AML tumors (without toxicity) in murine xenograft models.
In addition, CG’806 demonstrated non-covalent inhibition of the wild-type and Cys481Ser mutant forms of the BTK enzyme, as well as other oncogenic kinases operative in B-cell malignancies.
Preclinical results with CG’806 were presented as posters at the AACR conference “Hematologic Malignancies: Translating Discoveries to Novel Therapies,” which took place last May.
“Results from non-clinical studies that we and our research collaborators have generated are promising and give reason for our eagerness to begin clinical trials in both AML and B-cell malignancies in 2018,” said William G. Rice, PhD, chairman, president, and chief executive officer at Aptose.
“We are pleased that the FDA has recognized the unique potential of CG’806 to address AML and has assigned CG’806 the status of orphan drug designation.”
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to CG’806 for the treatment of patients with acute myeloid leukemia (AML).
CG’806 is an oral, first-in-class pan-FLT3/pan-BTK inhibitor being developed by Aptose Biosciences Inc.
In preclinical studies, CG’806 inhibited all wild-type and mutant forms of FLT3 tested, suppressed multiple oncogenic pathways operative in AML, and eliminated AML tumors (without toxicity) in murine xenograft models.
In addition, CG’806 demonstrated non-covalent inhibition of the wild-type and Cys481Ser mutant forms of the BTK enzyme, as well as other oncogenic kinases operative in B-cell malignancies.
Preclinical results with CG’806 were presented as posters at the AACR conference “Hematologic Malignancies: Translating Discoveries to Novel Therapies,” which took place last May.
“Results from non-clinical studies that we and our research collaborators have generated are promising and give reason for our eagerness to begin clinical trials in both AML and B-cell malignancies in 2018,” said William G. Rice, PhD, chairman, president, and chief executive officer at Aptose.
“We are pleased that the FDA has recognized the unique potential of CG’806 to address AML and has assigned CG’806 the status of orphan drug designation.”
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to CG’806 for the treatment of patients with acute myeloid leukemia (AML).
CG’806 is an oral, first-in-class pan-FLT3/pan-BTK inhibitor being developed by Aptose Biosciences Inc.
In preclinical studies, CG’806 inhibited all wild-type and mutant forms of FLT3 tested, suppressed multiple oncogenic pathways operative in AML, and eliminated AML tumors (without toxicity) in murine xenograft models.
In addition, CG’806 demonstrated non-covalent inhibition of the wild-type and Cys481Ser mutant forms of the BTK enzyme, as well as other oncogenic kinases operative in B-cell malignancies.
Preclinical results with CG’806 were presented as posters at the AACR conference “Hematologic Malignancies: Translating Discoveries to Novel Therapies,” which took place last May.
“Results from non-clinical studies that we and our research collaborators have generated are promising and give reason for our eagerness to begin clinical trials in both AML and B-cell malignancies in 2018,” said William G. Rice, PhD, chairman, president, and chief executive officer at Aptose.
“We are pleased that the FDA has recognized the unique potential of CG’806 to address AML and has assigned CG’806 the status of orphan drug designation.”
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
Drug approved for kids with sickle cell anemia
The US Food and Drug Administration (FDA) has approved a hydroxyurea product (Addmedica’s Siklos) for use in pediatric patients with sickle cell anemia.
Siklos is intended to reduce the frequency of painful crises and the need for blood transfusions in pediatric patients age 2 and older who have sickle cell anemia and recurrent moderate to severe painful crises.
The recommended dose of Siklos is 20 mg/kg once daily.
The FDA granted priority review and orphan drug designation to the application for Siklos.
The agency’s approval of Siklos was based on data from the ESCORT HU study (NCT02516579). The trial was an evaluation of Siklos in 405 patients, ages 2 to 18, with sickle cell disease (SCD).
Thirty-five percent of these patients (n=141) had not received hydroxyurea prior to study enrollment and were therefore evaluable for efficacy. The median follow-up was 23 months (range, 12 to 80 months).
The researchers found that Siklos prompted an increase in fetal hemoglobin. Median fetal hemoglobin percentages were 5.6% (range, 1.3 to 15.0) at baseline and 12.8% (range, 2.1 to 37.2) at around 6 months after Siklos initiation (the value closest to 6 months collected between 5 and 14 months).
In addition, the percentage of patients with at least 1 vaso-occlusive episode, 1 episode of acute chest syndrome, 1 hospitalization due to SCD, or 1 blood transfusion decreased after 12 months of Siklos treatment.
The proportion of patients with at least 1 vaso-occlusive episode was 69.2% at baseline and 42.5% at 12 months. The proportion with at least 1 episode of acute chest syndrome was 23.6% and 5.7%, respectively.
The proportion with at least 1 hospitalization due to SCD was 75.5% and 41.8%, respectively. And the proportion with at least 1 blood transfusion was 45.9% and 23.0%, respectively.
The most common adverse events (occurring in at least 10% of patients) were infections (39.8%), gastrointestinal disorders (13.1%), neutropenia (12.6%), nervous system disorders (11.1%), and metabolic and nutrition disorders (10.9%).
Full prescribing information for Siklos is available on the FDA website. ![]()
The US Food and Drug Administration (FDA) has approved a hydroxyurea product (Addmedica’s Siklos) for use in pediatric patients with sickle cell anemia.
Siklos is intended to reduce the frequency of painful crises and the need for blood transfusions in pediatric patients age 2 and older who have sickle cell anemia and recurrent moderate to severe painful crises.
The recommended dose of Siklos is 20 mg/kg once daily.
The FDA granted priority review and orphan drug designation to the application for Siklos.
The agency’s approval of Siklos was based on data from the ESCORT HU study (NCT02516579). The trial was an evaluation of Siklos in 405 patients, ages 2 to 18, with sickle cell disease (SCD).
Thirty-five percent of these patients (n=141) had not received hydroxyurea prior to study enrollment and were therefore evaluable for efficacy. The median follow-up was 23 months (range, 12 to 80 months).
The researchers found that Siklos prompted an increase in fetal hemoglobin. Median fetal hemoglobin percentages were 5.6% (range, 1.3 to 15.0) at baseline and 12.8% (range, 2.1 to 37.2) at around 6 months after Siklos initiation (the value closest to 6 months collected between 5 and 14 months).
In addition, the percentage of patients with at least 1 vaso-occlusive episode, 1 episode of acute chest syndrome, 1 hospitalization due to SCD, or 1 blood transfusion decreased after 12 months of Siklos treatment.
The proportion of patients with at least 1 vaso-occlusive episode was 69.2% at baseline and 42.5% at 12 months. The proportion with at least 1 episode of acute chest syndrome was 23.6% and 5.7%, respectively.
The proportion with at least 1 hospitalization due to SCD was 75.5% and 41.8%, respectively. And the proportion with at least 1 blood transfusion was 45.9% and 23.0%, respectively.
The most common adverse events (occurring in at least 10% of patients) were infections (39.8%), gastrointestinal disorders (13.1%), neutropenia (12.6%), nervous system disorders (11.1%), and metabolic and nutrition disorders (10.9%).
Full prescribing information for Siklos is available on the FDA website. ![]()
The US Food and Drug Administration (FDA) has approved a hydroxyurea product (Addmedica’s Siklos) for use in pediatric patients with sickle cell anemia.
Siklos is intended to reduce the frequency of painful crises and the need for blood transfusions in pediatric patients age 2 and older who have sickle cell anemia and recurrent moderate to severe painful crises.
The recommended dose of Siklos is 20 mg/kg once daily.
The FDA granted priority review and orphan drug designation to the application for Siklos.
The agency’s approval of Siklos was based on data from the ESCORT HU study (NCT02516579). The trial was an evaluation of Siklos in 405 patients, ages 2 to 18, with sickle cell disease (SCD).
Thirty-five percent of these patients (n=141) had not received hydroxyurea prior to study enrollment and were therefore evaluable for efficacy. The median follow-up was 23 months (range, 12 to 80 months).
The researchers found that Siklos prompted an increase in fetal hemoglobin. Median fetal hemoglobin percentages were 5.6% (range, 1.3 to 15.0) at baseline and 12.8% (range, 2.1 to 37.2) at around 6 months after Siklos initiation (the value closest to 6 months collected between 5 and 14 months).
In addition, the percentage of patients with at least 1 vaso-occlusive episode, 1 episode of acute chest syndrome, 1 hospitalization due to SCD, or 1 blood transfusion decreased after 12 months of Siklos treatment.
The proportion of patients with at least 1 vaso-occlusive episode was 69.2% at baseline and 42.5% at 12 months. The proportion with at least 1 episode of acute chest syndrome was 23.6% and 5.7%, respectively.
The proportion with at least 1 hospitalization due to SCD was 75.5% and 41.8%, respectively. And the proportion with at least 1 blood transfusion was 45.9% and 23.0%, respectively.
The most common adverse events (occurring in at least 10% of patients) were infections (39.8%), gastrointestinal disorders (13.1%), neutropenia (12.6%), nervous system disorders (11.1%), and metabolic and nutrition disorders (10.9%).
Full prescribing information for Siklos is available on the FDA website. ![]()
Nilotinib label updated with info on discontinuation
The US Food and Drug Administration (FDA) has approved an update to the product label for nilotinib (Tasigna) that includes information about how to discontinue the drug in certain patients.
Nilotinib, which was first approved by the FDA in 2007, is indicated for the treatment of patients with Philadelphia chromosome positive (Ph+) chronic myeloid leukemia (CML).
The updated prescribing information for the drug now outlines which of these patients may be eligible to stop receiving nilotinib.
Patients with chronic phase, Ph+ CML who have been taking nilotinib for 3 years or more (as first-line treatment or after failure with imatinib) and have achieved a sustained deep molecular response may be eligible to stop treatment.
Patients must have maintained a molecular response of at least MR4.0 for 1 year prior to discontinuation and achieved an MR4.5 at their last assessment.
Patients must have typical BCR-ABL transcripts (e13a2/b2a2 or e14a2/b3a2), no history of accelerated phase or blast crisis, and no past attempts at treatment discontinuation that resulted in relapse.
After discontinuation, patients must be monitored for possible loss of major molecular response (MMR). BCR-ABL transcript levels must be assessed and a complete blood count with differential performed monthly for 1 year, then every 6 weeks for the second year, and every 12 weeks thereafter.
BCR-ABL transcript levels should be measured using the MolecularMD MRDxTM BCR-ABL test, an FDA-authorized companion diagnostic validated to measure down to MR4.5.
If patients lose MMR, they must restart nilotinib within 4 weeks and receive the dose level they were receiving prior to discontinuation.
BCR-ABL transcript levels should be monitored every 2 weeks until they are lower than MMR for 4 consecutive measurements. Patients can then return to the original monitoring schedule.
The update of nilotinib’s label to include this information was based on results from 2 single-arm trials—ENESTfreedom and ENESTop.
ENESTfreedom
This phase 2 trial included 215 patients with Ph+, chronic phase CML. Researchers evaluated stopping treatment in 190 patients who had achieved a response of MR4.5 with nilotinib as first-line treatment. The patients had sustained deep molecular response for 1 year prior to treatment discontinuation.
Ninety-six weeks after stopping treatment, 48.9% of patients were still in MMR, also known as treatment-free remission (TFR).
Of the 88 patients who restarted nilotinib due to loss of MMR by the cut-off date, 98.9% were able to regain MMR (n=87). One patient discontinued the study at 7.1 weeks without regaining MMR after reinitiating treatment with nilotinib. Eighty-one patients (92.0%) regained MR4.5 by the cut-off date.
Common adverse events (AEs) in patients who discontinued nilotinib included musculoskeletal symptoms such as body aches, bone pain, and pain in extremities. However, these AEs decreased over time.
The incidence of musculoskeletal pain-related AEs decreased from 34.0% to 9.0% during the first and second 48 weeks of the TFR phase, respectively. In comparison, the incidence of such AEs was 17.0% during the treatment consolidation phase.
ENESTop
This phase 2 trial included 163 patients with Ph+, chronic phase CML. Researchers evaluated stopping treatment in 126 patients who had previously received imatinib, then switched to nilotinib and sustained a molecular response for 1 year prior to stopping nilotinib.
At 96 weeks, 53.2% of patients were still in TFR.
Fifty-six patients with confirmed loss of MR4.0 or loss of MMR restarted nilotinib by the cut-off date. Of these patients, 92.9% (n=52) regained both MR4.0 and MR4.5.
As in ENESTfreedom, patients who discontinued nilotinib had musculoskeletal symptoms that decreased over time.
The incidence of musculoskeletal pain-related AEs decreased from 47.9% to 15.1% during the first and second 48 weeks of the TFR phase, respectively. In comparison, the incidence of such AEs was 13.7% during the treatment consolidation phase.
Additional data from ENESTop and ENESTfreedom, as well as the recommendations for stopping nilotinib, are included in the updated prescribing information, which is available at https://www.us.tasigna.com/. ![]()
The US Food and Drug Administration (FDA) has approved an update to the product label for nilotinib (Tasigna) that includes information about how to discontinue the drug in certain patients.
Nilotinib, which was first approved by the FDA in 2007, is indicated for the treatment of patients with Philadelphia chromosome positive (Ph+) chronic myeloid leukemia (CML).
The updated prescribing information for the drug now outlines which of these patients may be eligible to stop receiving nilotinib.
Patients with chronic phase, Ph+ CML who have been taking nilotinib for 3 years or more (as first-line treatment or after failure with imatinib) and have achieved a sustained deep molecular response may be eligible to stop treatment.
Patients must have maintained a molecular response of at least MR4.0 for 1 year prior to discontinuation and achieved an MR4.5 at their last assessment.
Patients must have typical BCR-ABL transcripts (e13a2/b2a2 or e14a2/b3a2), no history of accelerated phase or blast crisis, and no past attempts at treatment discontinuation that resulted in relapse.
After discontinuation, patients must be monitored for possible loss of major molecular response (MMR). BCR-ABL transcript levels must be assessed and a complete blood count with differential performed monthly for 1 year, then every 6 weeks for the second year, and every 12 weeks thereafter.
BCR-ABL transcript levels should be measured using the MolecularMD MRDxTM BCR-ABL test, an FDA-authorized companion diagnostic validated to measure down to MR4.5.
If patients lose MMR, they must restart nilotinib within 4 weeks and receive the dose level they were receiving prior to discontinuation.
BCR-ABL transcript levels should be monitored every 2 weeks until they are lower than MMR for 4 consecutive measurements. Patients can then return to the original monitoring schedule.
The update of nilotinib’s label to include this information was based on results from 2 single-arm trials—ENESTfreedom and ENESTop.
ENESTfreedom
This phase 2 trial included 215 patients with Ph+, chronic phase CML. Researchers evaluated stopping treatment in 190 patients who had achieved a response of MR4.5 with nilotinib as first-line treatment. The patients had sustained deep molecular response for 1 year prior to treatment discontinuation.
Ninety-six weeks after stopping treatment, 48.9% of patients were still in MMR, also known as treatment-free remission (TFR).
Of the 88 patients who restarted nilotinib due to loss of MMR by the cut-off date, 98.9% were able to regain MMR (n=87). One patient discontinued the study at 7.1 weeks without regaining MMR after reinitiating treatment with nilotinib. Eighty-one patients (92.0%) regained MR4.5 by the cut-off date.
Common adverse events (AEs) in patients who discontinued nilotinib included musculoskeletal symptoms such as body aches, bone pain, and pain in extremities. However, these AEs decreased over time.
The incidence of musculoskeletal pain-related AEs decreased from 34.0% to 9.0% during the first and second 48 weeks of the TFR phase, respectively. In comparison, the incidence of such AEs was 17.0% during the treatment consolidation phase.
ENESTop
This phase 2 trial included 163 patients with Ph+, chronic phase CML. Researchers evaluated stopping treatment in 126 patients who had previously received imatinib, then switched to nilotinib and sustained a molecular response for 1 year prior to stopping nilotinib.
At 96 weeks, 53.2% of patients were still in TFR.
Fifty-six patients with confirmed loss of MR4.0 or loss of MMR restarted nilotinib by the cut-off date. Of these patients, 92.9% (n=52) regained both MR4.0 and MR4.5.
As in ENESTfreedom, patients who discontinued nilotinib had musculoskeletal symptoms that decreased over time.
The incidence of musculoskeletal pain-related AEs decreased from 47.9% to 15.1% during the first and second 48 weeks of the TFR phase, respectively. In comparison, the incidence of such AEs was 13.7% during the treatment consolidation phase.
Additional data from ENESTop and ENESTfreedom, as well as the recommendations for stopping nilotinib, are included in the updated prescribing information, which is available at https://www.us.tasigna.com/. ![]()
The US Food and Drug Administration (FDA) has approved an update to the product label for nilotinib (Tasigna) that includes information about how to discontinue the drug in certain patients.
Nilotinib, which was first approved by the FDA in 2007, is indicated for the treatment of patients with Philadelphia chromosome positive (Ph+) chronic myeloid leukemia (CML).
The updated prescribing information for the drug now outlines which of these patients may be eligible to stop receiving nilotinib.
Patients with chronic phase, Ph+ CML who have been taking nilotinib for 3 years or more (as first-line treatment or after failure with imatinib) and have achieved a sustained deep molecular response may be eligible to stop treatment.
Patients must have maintained a molecular response of at least MR4.0 for 1 year prior to discontinuation and achieved an MR4.5 at their last assessment.
Patients must have typical BCR-ABL transcripts (e13a2/b2a2 or e14a2/b3a2), no history of accelerated phase or blast crisis, and no past attempts at treatment discontinuation that resulted in relapse.
After discontinuation, patients must be monitored for possible loss of major molecular response (MMR). BCR-ABL transcript levels must be assessed and a complete blood count with differential performed monthly for 1 year, then every 6 weeks for the second year, and every 12 weeks thereafter.
BCR-ABL transcript levels should be measured using the MolecularMD MRDxTM BCR-ABL test, an FDA-authorized companion diagnostic validated to measure down to MR4.5.
If patients lose MMR, they must restart nilotinib within 4 weeks and receive the dose level they were receiving prior to discontinuation.
BCR-ABL transcript levels should be monitored every 2 weeks until they are lower than MMR for 4 consecutive measurements. Patients can then return to the original monitoring schedule.
The update of nilotinib’s label to include this information was based on results from 2 single-arm trials—ENESTfreedom and ENESTop.
ENESTfreedom
This phase 2 trial included 215 patients with Ph+, chronic phase CML. Researchers evaluated stopping treatment in 190 patients who had achieved a response of MR4.5 with nilotinib as first-line treatment. The patients had sustained deep molecular response for 1 year prior to treatment discontinuation.
Ninety-six weeks after stopping treatment, 48.9% of patients were still in MMR, also known as treatment-free remission (TFR).
Of the 88 patients who restarted nilotinib due to loss of MMR by the cut-off date, 98.9% were able to regain MMR (n=87). One patient discontinued the study at 7.1 weeks without regaining MMR after reinitiating treatment with nilotinib. Eighty-one patients (92.0%) regained MR4.5 by the cut-off date.
Common adverse events (AEs) in patients who discontinued nilotinib included musculoskeletal symptoms such as body aches, bone pain, and pain in extremities. However, these AEs decreased over time.
The incidence of musculoskeletal pain-related AEs decreased from 34.0% to 9.0% during the first and second 48 weeks of the TFR phase, respectively. In comparison, the incidence of such AEs was 17.0% during the treatment consolidation phase.
ENESTop
This phase 2 trial included 163 patients with Ph+, chronic phase CML. Researchers evaluated stopping treatment in 126 patients who had previously received imatinib, then switched to nilotinib and sustained a molecular response for 1 year prior to stopping nilotinib.
At 96 weeks, 53.2% of patients were still in TFR.
Fifty-six patients with confirmed loss of MR4.0 or loss of MMR restarted nilotinib by the cut-off date. Of these patients, 92.9% (n=52) regained both MR4.0 and MR4.5.
As in ENESTfreedom, patients who discontinued nilotinib had musculoskeletal symptoms that decreased over time.
The incidence of musculoskeletal pain-related AEs decreased from 47.9% to 15.1% during the first and second 48 weeks of the TFR phase, respectively. In comparison, the incidence of such AEs was 13.7% during the treatment consolidation phase.
Additional data from ENESTop and ENESTfreedom, as well as the recommendations for stopping nilotinib, are included in the updated prescribing information, which is available at https://www.us.tasigna.com/. ![]()
FDA expands approved use of bosutinib in CML
The US Food and Drug Administration (FDA) has expanded the approved indication for bosutinib (BOSULIF®).
The tyrosine kinase inhibitor (TKI) is now approved to treat adults with newly diagnosed, chronic phase, Philadelphia chromosome-positive (Ph+) chronic myelogenous leukemia (CML).
Bosutinib has accelerated approval for this indication. The approval was based on molecular and cytogenetic response rates.
Continued approval may be contingent upon verification and confirmation of clinical benefit in an ongoing, long-term follow-up trial.
Bosutinib was first approved by the FDA in September 2012. At that time, the TKI was approved to treat adults with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
A 400 mg tablet of bosutinib was recently approved by the FDA, adding to the previously approved 100 mg and 500 mg strengths.
The recommended dose of bosutinib for newly diagnosed patients is 400 mg orally once daily with food.
For patients who are resistant or intolerant to prior TKI therapy, the recommended dose is 500 mg orally once daily with food.
BFORE trial
The approval of bosutinib in adults with newly diagnosed, chronic phase, Ph+ CML was based on the phase 3 BFORE trial. Results from the trial were presented at the 2017 ASCO Annual Meeting.
In this ongoing study, researchers are comparing bosutinib and imatinib as first-line treatment of chronic phase CML.
As of the ASCO presentation, the trial had enrolled 536 patients who were randomized 1:1 to receive bosutinib (n=268) or imatinib (n=268).
The presentation included results in a modified intent-to-treat population of Ph+ patients with e13a2/e14a2 transcripts who had at least 12 months of follow-up. In this group, there were 246 patients in the bosutinib arm and 241 in the imatinib arm.
Most of the patients were still on therapy at the 12-month mark or beyond—78% in the bosutinib arm and 73.2% in the imatinib arm. The median treatment duration was 14.1 months and 13.8 months, respectively.
At 12 months, the rate of major molecular response was 47.2% in the bosutinib arm and 36.9% in the imatinib arm (P=0.02). The rate of complete cytogenetic response was 77.2% and 66.4%, respectively (P<0.008).
One patient in the bosutinib arm and 4 in the imatinib arm discontinued treatment due to disease progression, while 12.7% and 8.7%, respectively, discontinued treatment due to drug-related toxicity.
Adverse events that were more common in the bosutinib arm than the imatinib arm included grade 3 or higher diarrhea (7.8% vs 0.8%), increased alanine levels (19% vs 1.5%), increased aspartate levels (9.7% vs 1.9%), cardiovascular events (3% vs 0.4%), and peripheral vascular events (1.5% vs 1.1%).
Cerebrovascular events were more common with imatinib than bosutinib (0.4% and 0%, respectively).
Pfizer and Avillion entered into an exclusive collaborative development agreement in 2014 to conduct the BFORE trial.
Under the terms of the agreement, Avillion provided funding and conducted the trial to generate the clinical data used to support regulatory filings for marketing authorization for bosutinib as first-line treatment for patients with chronic phase, Ph+ CML.
With this approval, Avillion is eligible to receive milestone payments from Pfizer. Pfizer retains all rights to commercialize bosutinib globally. ![]()
The US Food and Drug Administration (FDA) has expanded the approved indication for bosutinib (BOSULIF®).
The tyrosine kinase inhibitor (TKI) is now approved to treat adults with newly diagnosed, chronic phase, Philadelphia chromosome-positive (Ph+) chronic myelogenous leukemia (CML).
Bosutinib has accelerated approval for this indication. The approval was based on molecular and cytogenetic response rates.
Continued approval may be contingent upon verification and confirmation of clinical benefit in an ongoing, long-term follow-up trial.
Bosutinib was first approved by the FDA in September 2012. At that time, the TKI was approved to treat adults with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
A 400 mg tablet of bosutinib was recently approved by the FDA, adding to the previously approved 100 mg and 500 mg strengths.
The recommended dose of bosutinib for newly diagnosed patients is 400 mg orally once daily with food.
For patients who are resistant or intolerant to prior TKI therapy, the recommended dose is 500 mg orally once daily with food.
BFORE trial
The approval of bosutinib in adults with newly diagnosed, chronic phase, Ph+ CML was based on the phase 3 BFORE trial. Results from the trial were presented at the 2017 ASCO Annual Meeting.
In this ongoing study, researchers are comparing bosutinib and imatinib as first-line treatment of chronic phase CML.
As of the ASCO presentation, the trial had enrolled 536 patients who were randomized 1:1 to receive bosutinib (n=268) or imatinib (n=268).
The presentation included results in a modified intent-to-treat population of Ph+ patients with e13a2/e14a2 transcripts who had at least 12 months of follow-up. In this group, there were 246 patients in the bosutinib arm and 241 in the imatinib arm.
Most of the patients were still on therapy at the 12-month mark or beyond—78% in the bosutinib arm and 73.2% in the imatinib arm. The median treatment duration was 14.1 months and 13.8 months, respectively.
At 12 months, the rate of major molecular response was 47.2% in the bosutinib arm and 36.9% in the imatinib arm (P=0.02). The rate of complete cytogenetic response was 77.2% and 66.4%, respectively (P<0.008).
One patient in the bosutinib arm and 4 in the imatinib arm discontinued treatment due to disease progression, while 12.7% and 8.7%, respectively, discontinued treatment due to drug-related toxicity.
Adverse events that were more common in the bosutinib arm than the imatinib arm included grade 3 or higher diarrhea (7.8% vs 0.8%), increased alanine levels (19% vs 1.5%), increased aspartate levels (9.7% vs 1.9%), cardiovascular events (3% vs 0.4%), and peripheral vascular events (1.5% vs 1.1%).
Cerebrovascular events were more common with imatinib than bosutinib (0.4% and 0%, respectively).
Pfizer and Avillion entered into an exclusive collaborative development agreement in 2014 to conduct the BFORE trial.
Under the terms of the agreement, Avillion provided funding and conducted the trial to generate the clinical data used to support regulatory filings for marketing authorization for bosutinib as first-line treatment for patients with chronic phase, Ph+ CML.
With this approval, Avillion is eligible to receive milestone payments from Pfizer. Pfizer retains all rights to commercialize bosutinib globally. ![]()
The US Food and Drug Administration (FDA) has expanded the approved indication for bosutinib (BOSULIF®).
The tyrosine kinase inhibitor (TKI) is now approved to treat adults with newly diagnosed, chronic phase, Philadelphia chromosome-positive (Ph+) chronic myelogenous leukemia (CML).
Bosutinib has accelerated approval for this indication. The approval was based on molecular and cytogenetic response rates.
Continued approval may be contingent upon verification and confirmation of clinical benefit in an ongoing, long-term follow-up trial.
Bosutinib was first approved by the FDA in September 2012. At that time, the TKI was approved to treat adults with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
A 400 mg tablet of bosutinib was recently approved by the FDA, adding to the previously approved 100 mg and 500 mg strengths.
The recommended dose of bosutinib for newly diagnosed patients is 400 mg orally once daily with food.
For patients who are resistant or intolerant to prior TKI therapy, the recommended dose is 500 mg orally once daily with food.
BFORE trial
The approval of bosutinib in adults with newly diagnosed, chronic phase, Ph+ CML was based on the phase 3 BFORE trial. Results from the trial were presented at the 2017 ASCO Annual Meeting.
In this ongoing study, researchers are comparing bosutinib and imatinib as first-line treatment of chronic phase CML.
As of the ASCO presentation, the trial had enrolled 536 patients who were randomized 1:1 to receive bosutinib (n=268) or imatinib (n=268).
The presentation included results in a modified intent-to-treat population of Ph+ patients with e13a2/e14a2 transcripts who had at least 12 months of follow-up. In this group, there were 246 patients in the bosutinib arm and 241 in the imatinib arm.
Most of the patients were still on therapy at the 12-month mark or beyond—78% in the bosutinib arm and 73.2% in the imatinib arm. The median treatment duration was 14.1 months and 13.8 months, respectively.
At 12 months, the rate of major molecular response was 47.2% in the bosutinib arm and 36.9% in the imatinib arm (P=0.02). The rate of complete cytogenetic response was 77.2% and 66.4%, respectively (P<0.008).
One patient in the bosutinib arm and 4 in the imatinib arm discontinued treatment due to disease progression, while 12.7% and 8.7%, respectively, discontinued treatment due to drug-related toxicity.
Adverse events that were more common in the bosutinib arm than the imatinib arm included grade 3 or higher diarrhea (7.8% vs 0.8%), increased alanine levels (19% vs 1.5%), increased aspartate levels (9.7% vs 1.9%), cardiovascular events (3% vs 0.4%), and peripheral vascular events (1.5% vs 1.1%).
Cerebrovascular events were more common with imatinib than bosutinib (0.4% and 0%, respectively).
Pfizer and Avillion entered into an exclusive collaborative development agreement in 2014 to conduct the BFORE trial.
Under the terms of the agreement, Avillion provided funding and conducted the trial to generate the clinical data used to support regulatory filings for marketing authorization for bosutinib as first-line treatment for patients with chronic phase, Ph+ CML.
With this approval, Avillion is eligible to receive milestone payments from Pfizer. Pfizer retains all rights to commercialize bosutinib globally. ![]()
FDA issues requirements, recommendations for GBCA use
The US Food and Drug Administration (FDA) has issued new safety-related requirements pertaining to gadolinium-based contrast agents (GBCAs) used for magnetic resonance imaging (MRI).
The agency’s action is due to the fact that gadolinium can be retained in patients’ brains and other body tissues for months to years after they receive GBCAs.
The only known adverse event related to gadolinium retention is nephrogenic systemic fibrosis, which occurs in a small subgroup of patients with pre-existing kidney failure.
Patients with normal kidney function and gadolinium retention have experienced adverse events involving multiple organ systems. However, the FDA has found no evidence confirming that gadolinium retention is causing these events.
Therefore, the agency concluded that the benefit of all approved GBCAs continues to outweigh any potential risks.
Still, the FDA has issued the following safety requirements related to GBCAs:
- Patients receiving GBCAs must read a new medication guide explaining about gadolinium retention
- Manufacturers of GBCAs must conduct human and animal studies to assess the safety of GBCAs
- Labels of GBCAs must be updated with a “Warning and Precaution” about gadolinium retention
- Labels must be changed to include mention of gadolinium retention in the Adverse Reactions, Pregnancy, Clinical Pharmacology, and Patient Instructions sections.
The FDA is also recommending that healthcare professionals consider the retention characteristics of each agent when choosing a GBCA for patients who may be at higher risk for gadolinium retention. This includes patients requiring multiple lifetime doses, pregnant women, children, and patients with inflammatory conditions.
In its latest safety communication on gadolinium retention, the FDA noted that linear GBCAs result in more and longer retention than macrocyclic GBCAs.
Specifically, gadolinium retention is higher with Omniscan (gadodiamide) or OptiMARK (gadoversetamide) than with Eovist (gadoxetate disodium), Magnevist (gadopentetate dimeglumine), or MultiHance (gadobenate dimeglumine).
Gadolinium retention is lowest with Dotarem (gadoterate meglumine), Gadavist (gadobutrol), and ProHance (gadoteridol), which all have similar levels of gadolinium retention.
Finally, the FDA is recommending that healthcare professionals minimize repeated GBCA imaging studies when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be deferred or avoided.
The FDA said it is still assessing the health effects of gadolinium retention and will update the public when new information becomes available. In the meantime, patients and healthcare professionals can report adverse events involving GBCAs to the agency’s MedWatch program. ![]()
The US Food and Drug Administration (FDA) has issued new safety-related requirements pertaining to gadolinium-based contrast agents (GBCAs) used for magnetic resonance imaging (MRI).
The agency’s action is due to the fact that gadolinium can be retained in patients’ brains and other body tissues for months to years after they receive GBCAs.
The only known adverse event related to gadolinium retention is nephrogenic systemic fibrosis, which occurs in a small subgroup of patients with pre-existing kidney failure.
Patients with normal kidney function and gadolinium retention have experienced adverse events involving multiple organ systems. However, the FDA has found no evidence confirming that gadolinium retention is causing these events.
Therefore, the agency concluded that the benefit of all approved GBCAs continues to outweigh any potential risks.
Still, the FDA has issued the following safety requirements related to GBCAs:
- Patients receiving GBCAs must read a new medication guide explaining about gadolinium retention
- Manufacturers of GBCAs must conduct human and animal studies to assess the safety of GBCAs
- Labels of GBCAs must be updated with a “Warning and Precaution” about gadolinium retention
- Labels must be changed to include mention of gadolinium retention in the Adverse Reactions, Pregnancy, Clinical Pharmacology, and Patient Instructions sections.
The FDA is also recommending that healthcare professionals consider the retention characteristics of each agent when choosing a GBCA for patients who may be at higher risk for gadolinium retention. This includes patients requiring multiple lifetime doses, pregnant women, children, and patients with inflammatory conditions.
In its latest safety communication on gadolinium retention, the FDA noted that linear GBCAs result in more and longer retention than macrocyclic GBCAs.
Specifically, gadolinium retention is higher with Omniscan (gadodiamide) or OptiMARK (gadoversetamide) than with Eovist (gadoxetate disodium), Magnevist (gadopentetate dimeglumine), or MultiHance (gadobenate dimeglumine).
Gadolinium retention is lowest with Dotarem (gadoterate meglumine), Gadavist (gadobutrol), and ProHance (gadoteridol), which all have similar levels of gadolinium retention.
Finally, the FDA is recommending that healthcare professionals minimize repeated GBCA imaging studies when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be deferred or avoided.
The FDA said it is still assessing the health effects of gadolinium retention and will update the public when new information becomes available. In the meantime, patients and healthcare professionals can report adverse events involving GBCAs to the agency’s MedWatch program. ![]()
The US Food and Drug Administration (FDA) has issued new safety-related requirements pertaining to gadolinium-based contrast agents (GBCAs) used for magnetic resonance imaging (MRI).
The agency’s action is due to the fact that gadolinium can be retained in patients’ brains and other body tissues for months to years after they receive GBCAs.
The only known adverse event related to gadolinium retention is nephrogenic systemic fibrosis, which occurs in a small subgroup of patients with pre-existing kidney failure.
Patients with normal kidney function and gadolinium retention have experienced adverse events involving multiple organ systems. However, the FDA has found no evidence confirming that gadolinium retention is causing these events.
Therefore, the agency concluded that the benefit of all approved GBCAs continues to outweigh any potential risks.
Still, the FDA has issued the following safety requirements related to GBCAs:
- Patients receiving GBCAs must read a new medication guide explaining about gadolinium retention
- Manufacturers of GBCAs must conduct human and animal studies to assess the safety of GBCAs
- Labels of GBCAs must be updated with a “Warning and Precaution” about gadolinium retention
- Labels must be changed to include mention of gadolinium retention in the Adverse Reactions, Pregnancy, Clinical Pharmacology, and Patient Instructions sections.
The FDA is also recommending that healthcare professionals consider the retention characteristics of each agent when choosing a GBCA for patients who may be at higher risk for gadolinium retention. This includes patients requiring multiple lifetime doses, pregnant women, children, and patients with inflammatory conditions.
In its latest safety communication on gadolinium retention, the FDA noted that linear GBCAs result in more and longer retention than macrocyclic GBCAs.
Specifically, gadolinium retention is higher with Omniscan (gadodiamide) or OptiMARK (gadoversetamide) than with Eovist (gadoxetate disodium), Magnevist (gadopentetate dimeglumine), or MultiHance (gadobenate dimeglumine).
Gadolinium retention is lowest with Dotarem (gadoterate meglumine), Gadavist (gadobutrol), and ProHance (gadoteridol), which all have similar levels of gadolinium retention.
Finally, the FDA is recommending that healthcare professionals minimize repeated GBCA imaging studies when possible, particularly closely spaced MRI studies. However, necessary GBCA MRI scans should not be deferred or avoided.
The FDA said it is still assessing the health effects of gadolinium retention and will update the public when new information becomes available. In the meantime, patients and healthcare professionals can report adverse events involving GBCAs to the agency’s MedWatch program. ![]()
FDA lifts clinical hold on fitusiran trials
The US Food and Drug Administration (FDA) has lifted the hold on clinical trials of fitusiran, an RNAi therapeutic being developed to treat patients with hemophilia A and B, with and without inhibitors.
The hold encompassed a phase 2 open-label extension study and the ATLAS phase 3 program, which includes 3 separate trials.
Dosing was suspended in these trials after a fatal thrombotic event was reported in a patient enrolled on the phase 2 trial.
The patient had hemophilia A without inhibitors. He developed exercise-induced right hip pain that was treated with 3 doses of factor VIII concentrate (31-46 IU/kg) on 3 separate days.
The patient then developed a cerebral venous sinus thrombosis that was considered possibly related to treatment. He ultimately died of cerebral edema.
As a result of this death, Alnylam Pharmaceuticals, Inc., (the company developing fitusiran with Sanofi Genzyme) announced the hold on fitusiran trials in September.
Since then, Alnylam has reached an agreement with the FDA on new clinical risk mitigation measures for fitusiran trials. This includes protocol-specified guidelines and additional investigator and patient education concerning reduced doses of replacement factor or bypassing agent to treat any breakthrough bleeds in fitusiran studies.
With these protocol amendments in place and clinical materials updated, the FDA has lifted the hold on fitusiran trials.
“We are pleased with the FDA’s decision to lift the clinical hold, as fitusiran holds the potential to help improve the lives of people living with hemophilia,” said Akin Akinc, PhD, vice-president and general manager of fitusiran at Alnylam.
“With the additional risk mitigation measures in place, we look forward to the continued late-stage development of fitusiran and expect to resume dosing around year-end.”
About fitusiran
Fitusiran is an investigational, once-monthly, subcutaneously administered RNAi therapeutic targeting antithrombin. It is in development for the treatment of hemophilia A and B, with and without inhibitors.
Fitusiran is designed to lower levels of antithrombin with the goal of promoting sufficient thrombin generation to restore hemostasis and prevent bleeding.
Fitusiran is under investigation in a phase 2 open-label extension study of patients with moderate or severe hemophilia A or B who have participated in a previous clinical study of fitusiran.
The therapy is also being tested in the phase 3 ATLAS program, which includes 3 trials.
The ATLAS-INH trial is a 9-month, randomized, active controlled study designed to enroll approximately 50 patients with hemophilia A or B with inhibitors who received prior on-demand therapy.
The ATLAS-A/B trial is a 9-month, randomized, active controlled study designed to enroll approximately 100 patients with hemophilia A or B without inhibitors who received prior on-demand therapy.
The ATLAS-PPX trial is a one-way crossover study designed to enroll approximately 100 patients with hemophilia A or B, with or without inhibitors, receiving prophylaxis therapy as prior standard of care.
In ATLAS-PPX, patients receive standard of care prophylaxis for 6 months and then transition to fitusiran treatment for 7 months. The study’s primary endpoint is the annualized bleeding rate in the fitusiran period and in the factor/bypassing agent prophylaxis period. ![]()
The US Food and Drug Administration (FDA) has lifted the hold on clinical trials of fitusiran, an RNAi therapeutic being developed to treat patients with hemophilia A and B, with and without inhibitors.
The hold encompassed a phase 2 open-label extension study and the ATLAS phase 3 program, which includes 3 separate trials.
Dosing was suspended in these trials after a fatal thrombotic event was reported in a patient enrolled on the phase 2 trial.
The patient had hemophilia A without inhibitors. He developed exercise-induced right hip pain that was treated with 3 doses of factor VIII concentrate (31-46 IU/kg) on 3 separate days.
The patient then developed a cerebral venous sinus thrombosis that was considered possibly related to treatment. He ultimately died of cerebral edema.
As a result of this death, Alnylam Pharmaceuticals, Inc., (the company developing fitusiran with Sanofi Genzyme) announced the hold on fitusiran trials in September.
Since then, Alnylam has reached an agreement with the FDA on new clinical risk mitigation measures for fitusiran trials. This includes protocol-specified guidelines and additional investigator and patient education concerning reduced doses of replacement factor or bypassing agent to treat any breakthrough bleeds in fitusiran studies.
With these protocol amendments in place and clinical materials updated, the FDA has lifted the hold on fitusiran trials.
“We are pleased with the FDA’s decision to lift the clinical hold, as fitusiran holds the potential to help improve the lives of people living with hemophilia,” said Akin Akinc, PhD, vice-president and general manager of fitusiran at Alnylam.
“With the additional risk mitigation measures in place, we look forward to the continued late-stage development of fitusiran and expect to resume dosing around year-end.”
About fitusiran
Fitusiran is an investigational, once-monthly, subcutaneously administered RNAi therapeutic targeting antithrombin. It is in development for the treatment of hemophilia A and B, with and without inhibitors.
Fitusiran is designed to lower levels of antithrombin with the goal of promoting sufficient thrombin generation to restore hemostasis and prevent bleeding.
Fitusiran is under investigation in a phase 2 open-label extension study of patients with moderate or severe hemophilia A or B who have participated in a previous clinical study of fitusiran.
The therapy is also being tested in the phase 3 ATLAS program, which includes 3 trials.
The ATLAS-INH trial is a 9-month, randomized, active controlled study designed to enroll approximately 50 patients with hemophilia A or B with inhibitors who received prior on-demand therapy.
The ATLAS-A/B trial is a 9-month, randomized, active controlled study designed to enroll approximately 100 patients with hemophilia A or B without inhibitors who received prior on-demand therapy.
The ATLAS-PPX trial is a one-way crossover study designed to enroll approximately 100 patients with hemophilia A or B, with or without inhibitors, receiving prophylaxis therapy as prior standard of care.
In ATLAS-PPX, patients receive standard of care prophylaxis for 6 months and then transition to fitusiran treatment for 7 months. The study’s primary endpoint is the annualized bleeding rate in the fitusiran period and in the factor/bypassing agent prophylaxis period. ![]()
The US Food and Drug Administration (FDA) has lifted the hold on clinical trials of fitusiran, an RNAi therapeutic being developed to treat patients with hemophilia A and B, with and without inhibitors.
The hold encompassed a phase 2 open-label extension study and the ATLAS phase 3 program, which includes 3 separate trials.
Dosing was suspended in these trials after a fatal thrombotic event was reported in a patient enrolled on the phase 2 trial.
The patient had hemophilia A without inhibitors. He developed exercise-induced right hip pain that was treated with 3 doses of factor VIII concentrate (31-46 IU/kg) on 3 separate days.
The patient then developed a cerebral venous sinus thrombosis that was considered possibly related to treatment. He ultimately died of cerebral edema.
As a result of this death, Alnylam Pharmaceuticals, Inc., (the company developing fitusiran with Sanofi Genzyme) announced the hold on fitusiran trials in September.
Since then, Alnylam has reached an agreement with the FDA on new clinical risk mitigation measures for fitusiran trials. This includes protocol-specified guidelines and additional investigator and patient education concerning reduced doses of replacement factor or bypassing agent to treat any breakthrough bleeds in fitusiran studies.
With these protocol amendments in place and clinical materials updated, the FDA has lifted the hold on fitusiran trials.
“We are pleased with the FDA’s decision to lift the clinical hold, as fitusiran holds the potential to help improve the lives of people living with hemophilia,” said Akin Akinc, PhD, vice-president and general manager of fitusiran at Alnylam.
“With the additional risk mitigation measures in place, we look forward to the continued late-stage development of fitusiran and expect to resume dosing around year-end.”
About fitusiran
Fitusiran is an investigational, once-monthly, subcutaneously administered RNAi therapeutic targeting antithrombin. It is in development for the treatment of hemophilia A and B, with and without inhibitors.
Fitusiran is designed to lower levels of antithrombin with the goal of promoting sufficient thrombin generation to restore hemostasis and prevent bleeding.
Fitusiran is under investigation in a phase 2 open-label extension study of patients with moderate or severe hemophilia A or B who have participated in a previous clinical study of fitusiran.
The therapy is also being tested in the phase 3 ATLAS program, which includes 3 trials.
The ATLAS-INH trial is a 9-month, randomized, active controlled study designed to enroll approximately 50 patients with hemophilia A or B with inhibitors who received prior on-demand therapy.
The ATLAS-A/B trial is a 9-month, randomized, active controlled study designed to enroll approximately 100 patients with hemophilia A or B without inhibitors who received prior on-demand therapy.
The ATLAS-PPX trial is a one-way crossover study designed to enroll approximately 100 patients with hemophilia A or B, with or without inhibitors, receiving prophylaxis therapy as prior standard of care.
In ATLAS-PPX, patients receive standard of care prophylaxis for 6 months and then transition to fitusiran treatment for 7 months. The study’s primary endpoint is the annualized bleeding rate in the fitusiran period and in the factor/bypassing agent prophylaxis period. ![]()
NK cell product receives orphan designation
The European Commission has granted orphan designation to a natural killer (NK) cell product for the treatment of multiple myeloma.
The product, called CellProtect, is manufactured from a patient’s own blood.
It consists of NK cells that have been activated and expanded so they can recognize and attack cancer cells.
CellProtect has been studied in a phase 1/2 trial of patients with multiple myeloma.
In this trial, the NK cell product was used as a supplement to autologous stem cell transplant.
CellProtect exhibited a good safety profile and signals of effect in the trial, according to CellProtect Nordic Pharmaceuticals AB, the company developing CellProtect.
Results from the trial are expected to be published in 2018.
“The decision from the commission is based on a recommendation from the European Medicines Agency’s Committee for Orphan Medicinal Products and confirms that a future product is considered to be of significant benefit to those suffering from multiple myeloma,” said Karin Mellström, chief executive officer of CellProtect Nordic Pharmaceuticals AB.
“We can now proceed and plan for additional clinical trials in order to receive approval to market CellProtect.”
Orphan designation from the European Commission provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if a therapy receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. ![]()
The European Commission has granted orphan designation to a natural killer (NK) cell product for the treatment of multiple myeloma.
The product, called CellProtect, is manufactured from a patient’s own blood.
It consists of NK cells that have been activated and expanded so they can recognize and attack cancer cells.
CellProtect has been studied in a phase 1/2 trial of patients with multiple myeloma.
In this trial, the NK cell product was used as a supplement to autologous stem cell transplant.
CellProtect exhibited a good safety profile and signals of effect in the trial, according to CellProtect Nordic Pharmaceuticals AB, the company developing CellProtect.
Results from the trial are expected to be published in 2018.
“The decision from the commission is based on a recommendation from the European Medicines Agency’s Committee for Orphan Medicinal Products and confirms that a future product is considered to be of significant benefit to those suffering from multiple myeloma,” said Karin Mellström, chief executive officer of CellProtect Nordic Pharmaceuticals AB.
“We can now proceed and plan for additional clinical trials in order to receive approval to market CellProtect.”
Orphan designation from the European Commission provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if a therapy receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision. ![]()
The European Commission has granted orphan designation to a natural killer (NK) cell product for the treatment of multiple myeloma.
The product, called CellProtect, is manufactured from a patient’s own blood.
It consists of NK cells that have been activated and expanded so they can recognize and attack cancer cells.
CellProtect has been studied in a phase 1/2 trial of patients with multiple myeloma.
In this trial, the NK cell product was used as a supplement to autologous stem cell transplant.
CellProtect exhibited a good safety profile and signals of effect in the trial, according to CellProtect Nordic Pharmaceuticals AB, the company developing CellProtect.
Results from the trial are expected to be published in 2018.
“The decision from the commission is based on a recommendation from the European Medicines Agency’s Committee for Orphan Medicinal Products and confirms that a future product is considered to be of significant benefit to those suffering from multiple myeloma,” said Karin Mellström, chief executive officer of CellProtect Nordic Pharmaceuticals AB.
“We can now proceed and plan for additional clinical trials in order to receive approval to market CellProtect.”
Orphan designation from the European Commission provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides a 10-year period of marketing exclusivity if a therapy receives regulatory approval.
The designation also provides incentives for companies seeking protocol assistance from the European Medicines Agency during the product development phase and direct access to the centralized authorization procedure.
The European Medicines Agency’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision.
CHMP recommends generic drug for ET
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion recommending marketing authorization for Anagrelide Mylan.
The product is intended to reduce elevated platelet counts in at-risk patients with essential thrombocythemia (ET).
Anagrelide Mylan is a generic of Xagrid (0.5 mg hard capsules), which has been authorized in the European Union since November 2004.
The active substance of Anagrelide Mylan is the antineoplastic agent anagrelide.
The precise mechanism by which anagrelide reduces platelet counts is unknown. Anagrelide is an inhibitor of cyclic AMP phosphodiesterase III.
If authorized, Anagrelide Mylan will be available as 0.5 mg and 1 mg hard capsules.
The full indication for the drug will be to reduce elevated platelet counts in at-risk ET patients who are intolerant to their current therapy or whose elevated platelet counts are not reduced to an acceptable level by their current therapy.
An at-risk ET patient is defined by 1 or more of the following features:
- Age older than 60
- Platelet count greater than 1000 x 109/L
- A history of thrombo-hemorrhagic events.
The CHMP’s opinion on Anagrelide Mylan will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion recommending marketing authorization for Anagrelide Mylan.
The product is intended to reduce elevated platelet counts in at-risk patients with essential thrombocythemia (ET).
Anagrelide Mylan is a generic of Xagrid (0.5 mg hard capsules), which has been authorized in the European Union since November 2004.
The active substance of Anagrelide Mylan is the antineoplastic agent anagrelide.
The precise mechanism by which anagrelide reduces platelet counts is unknown. Anagrelide is an inhibitor of cyclic AMP phosphodiesterase III.
If authorized, Anagrelide Mylan will be available as 0.5 mg and 1 mg hard capsules.
The full indication for the drug will be to reduce elevated platelet counts in at-risk ET patients who are intolerant to their current therapy or whose elevated platelet counts are not reduced to an acceptable level by their current therapy.
An at-risk ET patient is defined by 1 or more of the following features:
- Age older than 60
- Platelet count greater than 1000 x 109/L
- A history of thrombo-hemorrhagic events.
The CHMP’s opinion on Anagrelide Mylan will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive opinion recommending marketing authorization for Anagrelide Mylan.
The product is intended to reduce elevated platelet counts in at-risk patients with essential thrombocythemia (ET).
Anagrelide Mylan is a generic of Xagrid (0.5 mg hard capsules), which has been authorized in the European Union since November 2004.
The active substance of Anagrelide Mylan is the antineoplastic agent anagrelide.
The precise mechanism by which anagrelide reduces platelet counts is unknown. Anagrelide is an inhibitor of cyclic AMP phosphodiesterase III.
If authorized, Anagrelide Mylan will be available as 0.5 mg and 1 mg hard capsules.
The full indication for the drug will be to reduce elevated platelet counts in at-risk ET patients who are intolerant to their current therapy or whose elevated platelet counts are not reduced to an acceptable level by their current therapy.
An at-risk ET patient is defined by 1 or more of the following features:
- Age older than 60
- Platelet count greater than 1000 x 109/L
- A history of thrombo-hemorrhagic events.
The CHMP’s opinion on Anagrelide Mylan will be reviewed by the European Commission (EC).
If the EC agrees with the CHMP, the commission will grant a centralized marketing authorization that will be valid in the European Union. Norway, Iceland, and Liechtenstein will make corresponding decisions on the basis of the EC’s decision.
The EC typically makes a decision within 67 days of the CHMP’s recommendation.
Pembrolizumab sBLA receives priority review
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) for the anti-PD-1 therapy pembrolizumab (KEYTRUDA).
With this sBLA, Merck is seeking approval for pembrolizumab to treat adult and pediatric patients with refractory primary mediastinal B-cell lymphoma (PMBCL) or patients with PMBCL who have relapsed after 2 or more prior lines of therapy.
The FDA expects to make a decision on the sBLA by April 3, 2018.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, microsatellite instability-high cancer, and gastric cancer.
The sBLA for pembrolizumab as a treatment for PMBCL is supported by the phase 2 KEYNOTE-170 trial. Results from this trial were presented at the 2017 ASH Annual Meeting (abstract 2833).
KEYNOTE-170 is an ongoing study in which researchers are evaluating pembrolizumab (given at a 200 mg fixed dose every 3 weeks) in patients with relapsed/refractory PMBCL or relapsed/refractory Richter syndrome.
The PMBCL cohort enrolled patients who relapsed after autologous stem cell transplant (ASCT), were refractory to ASCT, or were ineligible for ASCT. Patients ineligible for ASCT had to have received 2 or more lines of prior therapy.
The median duration of follow-up was 10.5 months (range, 0.1-17.7).
In the efficacy population (n=29), the overall response rate was 41% (n=12), and the complete response rate was 24% (n=7).
The median time to response was 2.8 months (range, 2.4-5.5), and the median duration of response was not reached (range, 1.1+ to 13.6+ months).
Of the 53 patients evaluated for safety, 57% (n=30) experienced treatment-related adverse events (TRAEs), including 21% (n=11) who experienced grade 3-4 TRAEs.
The most common TRAEs (occurring in at least 5% of patients) were neutropenia (n=11), hypothyroidism (n=4), asthenia (n=3), and pyrexia (n=3).
Immune-mediated adverse events of all grades occurred in 11% (n=6) of patients. These include hypothyroidism (n=4), hyperthyroidism (n=2), pneumonitis (n=1), and thyroiditis (n=1). There were no treatment-related deaths.
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) for the anti-PD-1 therapy pembrolizumab (KEYTRUDA).
With this sBLA, Merck is seeking approval for pembrolizumab to treat adult and pediatric patients with refractory primary mediastinal B-cell lymphoma (PMBCL) or patients with PMBCL who have relapsed after 2 or more prior lines of therapy.
The FDA expects to make a decision on the sBLA by April 3, 2018.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, microsatellite instability-high cancer, and gastric cancer.
The sBLA for pembrolizumab as a treatment for PMBCL is supported by the phase 2 KEYNOTE-170 trial. Results from this trial were presented at the 2017 ASH Annual Meeting (abstract 2833).
KEYNOTE-170 is an ongoing study in which researchers are evaluating pembrolizumab (given at a 200 mg fixed dose every 3 weeks) in patients with relapsed/refractory PMBCL or relapsed/refractory Richter syndrome.
The PMBCL cohort enrolled patients who relapsed after autologous stem cell transplant (ASCT), were refractory to ASCT, or were ineligible for ASCT. Patients ineligible for ASCT had to have received 2 or more lines of prior therapy.
The median duration of follow-up was 10.5 months (range, 0.1-17.7).
In the efficacy population (n=29), the overall response rate was 41% (n=12), and the complete response rate was 24% (n=7).
The median time to response was 2.8 months (range, 2.4-5.5), and the median duration of response was not reached (range, 1.1+ to 13.6+ months).
Of the 53 patients evaluated for safety, 57% (n=30) experienced treatment-related adverse events (TRAEs), including 21% (n=11) who experienced grade 3-4 TRAEs.
The most common TRAEs (occurring in at least 5% of patients) were neutropenia (n=11), hypothyroidism (n=4), asthenia (n=3), and pyrexia (n=3).
Immune-mediated adverse events of all grades occurred in 11% (n=6) of patients. These include hypothyroidism (n=4), hyperthyroidism (n=2), pneumonitis (n=1), and thyroiditis (n=1). There were no treatment-related deaths.
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) for the anti-PD-1 therapy pembrolizumab (KEYTRUDA).
With this sBLA, Merck is seeking approval for pembrolizumab to treat adult and pediatric patients with refractory primary mediastinal B-cell lymphoma (PMBCL) or patients with PMBCL who have relapsed after 2 or more prior lines of therapy.
The FDA expects to make a decision on the sBLA by April 3, 2018.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Pembrolizumab is currently FDA-approved to treat classical Hodgkin lymphoma, melanoma, lung cancer, head and neck cancer, urothelial carcinoma, microsatellite instability-high cancer, and gastric cancer.
The sBLA for pembrolizumab as a treatment for PMBCL is supported by the phase 2 KEYNOTE-170 trial. Results from this trial were presented at the 2017 ASH Annual Meeting (abstract 2833).
KEYNOTE-170 is an ongoing study in which researchers are evaluating pembrolizumab (given at a 200 mg fixed dose every 3 weeks) in patients with relapsed/refractory PMBCL or relapsed/refractory Richter syndrome.
The PMBCL cohort enrolled patients who relapsed after autologous stem cell transplant (ASCT), were refractory to ASCT, or were ineligible for ASCT. Patients ineligible for ASCT had to have received 2 or more lines of prior therapy.
The median duration of follow-up was 10.5 months (range, 0.1-17.7).
In the efficacy population (n=29), the overall response rate was 41% (n=12), and the complete response rate was 24% (n=7).
The median time to response was 2.8 months (range, 2.4-5.5), and the median duration of response was not reached (range, 1.1+ to 13.6+ months).
Of the 53 patients evaluated for safety, 57% (n=30) experienced treatment-related adverse events (TRAEs), including 21% (n=11) who experienced grade 3-4 TRAEs.
The most common TRAEs (occurring in at least 5% of patients) were neutropenia (n=11), hypothyroidism (n=4), asthenia (n=3), and pyrexia (n=3).
Immune-mediated adverse events of all grades occurred in 11% (n=6) of patients. These include hypothyroidism (n=4), hyperthyroidism (n=2), pneumonitis (n=1), and thyroiditis (n=1). There were no treatment-related deaths.
*Data in the abstract differ from the presentation.
CRP drives bone destruction in myeloma, team says
New research suggests that C-reactive protein (CRP) drives multiple myeloma (MM) to destroy bone.
Researchers found that CRP accelerated the onset of bone destruction and made bone damage more severe in mouse models of MM.
The team also observed an association between elevated serum CRP levels and greater degree of bone damage in newly diagnosed MM patients.
The researchers therefore believe that CRP might be targeted to prevent or treat MM-associated bone disease.
Qing Yi, MD, PhD, of the Lerner Research Institute at the Cleveland Clinic in Ohio, and his colleagues conducted this research and reported the results in Science Translational Medicine.
The researchers noted that high levels of circulating CRP have been associated with poor prognosis in many cancers, including MM.
In a previous study, the team found that CRP enhanced MM cell proliferation under stressed conditions and protected MM cells from chemotherapy-induced apoptosis.
Now, the researchers have found that CRP activates MM cells to promote osteoclastogenesis and bone destruction.
In experiments with mouse models, the team found that CRP promoted MM-cell-mediated lytic bone disease. The researchers said CRP enhanced osteoclast differentiation and bone resorption activity.
In vitro experiments showed that CRP stimulates MM cells to produce osteoclast activators such as RANKL, MCP-1, and MIP-1a.
Further investigation revealed that CRP binds to CD32 on MM cells. This activates a pathway mediated by the kinase p38 MAPK and the transcription factor Twist, which increases MM cells’ production of osteolytic cytokines.
Finally, the researchers analyzed samples from newly diagnosed MM patients.
The team found that serum CRP levels “significantly and positively” correlated with the number of bone lesions patients had. And CRP was abundant in lesion biopsies from individuals with severe skeletal disease.
New research suggests that C-reactive protein (CRP) drives multiple myeloma (MM) to destroy bone.
Researchers found that CRP accelerated the onset of bone destruction and made bone damage more severe in mouse models of MM.
The team also observed an association between elevated serum CRP levels and greater degree of bone damage in newly diagnosed MM patients.
The researchers therefore believe that CRP might be targeted to prevent or treat MM-associated bone disease.
Qing Yi, MD, PhD, of the Lerner Research Institute at the Cleveland Clinic in Ohio, and his colleagues conducted this research and reported the results in Science Translational Medicine.
The researchers noted that high levels of circulating CRP have been associated with poor prognosis in many cancers, including MM.
In a previous study, the team found that CRP enhanced MM cell proliferation under stressed conditions and protected MM cells from chemotherapy-induced apoptosis.
Now, the researchers have found that CRP activates MM cells to promote osteoclastogenesis and bone destruction.
In experiments with mouse models, the team found that CRP promoted MM-cell-mediated lytic bone disease. The researchers said CRP enhanced osteoclast differentiation and bone resorption activity.
In vitro experiments showed that CRP stimulates MM cells to produce osteoclast activators such as RANKL, MCP-1, and MIP-1a.
Further investigation revealed that CRP binds to CD32 on MM cells. This activates a pathway mediated by the kinase p38 MAPK and the transcription factor Twist, which increases MM cells’ production of osteolytic cytokines.
Finally, the researchers analyzed samples from newly diagnosed MM patients.
The team found that serum CRP levels “significantly and positively” correlated with the number of bone lesions patients had. And CRP was abundant in lesion biopsies from individuals with severe skeletal disease.
New research suggests that C-reactive protein (CRP) drives multiple myeloma (MM) to destroy bone.
Researchers found that CRP accelerated the onset of bone destruction and made bone damage more severe in mouse models of MM.
The team also observed an association between elevated serum CRP levels and greater degree of bone damage in newly diagnosed MM patients.
The researchers therefore believe that CRP might be targeted to prevent or treat MM-associated bone disease.
Qing Yi, MD, PhD, of the Lerner Research Institute at the Cleveland Clinic in Ohio, and his colleagues conducted this research and reported the results in Science Translational Medicine.
The researchers noted that high levels of circulating CRP have been associated with poor prognosis in many cancers, including MM.
In a previous study, the team found that CRP enhanced MM cell proliferation under stressed conditions and protected MM cells from chemotherapy-induced apoptosis.
Now, the researchers have found that CRP activates MM cells to promote osteoclastogenesis and bone destruction.
In experiments with mouse models, the team found that CRP promoted MM-cell-mediated lytic bone disease. The researchers said CRP enhanced osteoclast differentiation and bone resorption activity.
In vitro experiments showed that CRP stimulates MM cells to produce osteoclast activators such as RANKL, MCP-1, and MIP-1a.
Further investigation revealed that CRP binds to CD32 on MM cells. This activates a pathway mediated by the kinase p38 MAPK and the transcription factor Twist, which increases MM cells’ production of osteolytic cytokines.
Finally, the researchers analyzed samples from newly diagnosed MM patients.
The team found that serum CRP levels “significantly and positively” correlated with the number of bone lesions patients had. And CRP was abundant in lesion biopsies from individuals with severe skeletal disease.