User login
FDA aims to improve review of generic drugs
The US Food and Drug Administration (FDA) has announced that it is taking new steps to facilitate efficient review of generic drugs.
The agency has released 2 documents intended to help streamline and improve the submission and review of generic drug applications, or Abbreviated New Drug Applications (ANDAs).
The first document is a draft guidance for industry, “Good ANDA Submission Practices,” which highlights common, recurring deficiencies the FDA sees in generic drug applications that may lead to a delay in their approval.
The FDA’s goal in releasing this document is to reduce the number of review cycles for ANDAs by helping applicants avoid these deficiencies.
The second document is a Manual of Policies and Procedures (MAPP), “Good ANDA Assessment Practices,” which outlines ANDA assessment practices for FDA staff.
This document formalizes a more streamlined generic review process, including the introduction of new templates designed to make each cycle of the review process more efficient and complete.
Releasing these new documents is part of the FDA’s Drug Competition Action Plan, which has 3 main goals:
- To reduce actions by branded pharmaceutical companies that can delay generic drug entry into the marketplace
- To resolve scientific and regulatory obstacles that can make it difficult to win approval of generic versions of certain complex drugs
- To improve the efficiency and predictability of the FDA’s generic review process to reduce the time it takes to get a generic drug approved and lessen the number of review cycles needed for generic applications.
The new MAPP and draft guidance documents for ANDAs are intended to help the FDA meet the third goal of the Drug Competition Action Plan.
The FDA is hoping to address the second goal of the plan later this year, building upon its initiatives to accelerate review and approval of complex generics.
The agency is also planning to develop guidance documents during the first quarter of 2018 that will address 3 issues related to the first goal of the plan—potential abuses of the citizen petition process, companies that restrict access to testing samples of branded drugs, and abuses of the single, shared system REMS (risk evaluation and mitigation strategy) negotiation process. ![]()
The US Food and Drug Administration (FDA) has announced that it is taking new steps to facilitate efficient review of generic drugs.
The agency has released 2 documents intended to help streamline and improve the submission and review of generic drug applications, or Abbreviated New Drug Applications (ANDAs).
The first document is a draft guidance for industry, “Good ANDA Submission Practices,” which highlights common, recurring deficiencies the FDA sees in generic drug applications that may lead to a delay in their approval.
The FDA’s goal in releasing this document is to reduce the number of review cycles for ANDAs by helping applicants avoid these deficiencies.
The second document is a Manual of Policies and Procedures (MAPP), “Good ANDA Assessment Practices,” which outlines ANDA assessment practices for FDA staff.
This document formalizes a more streamlined generic review process, including the introduction of new templates designed to make each cycle of the review process more efficient and complete.
Releasing these new documents is part of the FDA’s Drug Competition Action Plan, which has 3 main goals:
- To reduce actions by branded pharmaceutical companies that can delay generic drug entry into the marketplace
- To resolve scientific and regulatory obstacles that can make it difficult to win approval of generic versions of certain complex drugs
- To improve the efficiency and predictability of the FDA’s generic review process to reduce the time it takes to get a generic drug approved and lessen the number of review cycles needed for generic applications.
The new MAPP and draft guidance documents for ANDAs are intended to help the FDA meet the third goal of the Drug Competition Action Plan.
The FDA is hoping to address the second goal of the plan later this year, building upon its initiatives to accelerate review and approval of complex generics.
The agency is also planning to develop guidance documents during the first quarter of 2018 that will address 3 issues related to the first goal of the plan—potential abuses of the citizen petition process, companies that restrict access to testing samples of branded drugs, and abuses of the single, shared system REMS (risk evaluation and mitigation strategy) negotiation process. ![]()
The US Food and Drug Administration (FDA) has announced that it is taking new steps to facilitate efficient review of generic drugs.
The agency has released 2 documents intended to help streamline and improve the submission and review of generic drug applications, or Abbreviated New Drug Applications (ANDAs).
The first document is a draft guidance for industry, “Good ANDA Submission Practices,” which highlights common, recurring deficiencies the FDA sees in generic drug applications that may lead to a delay in their approval.
The FDA’s goal in releasing this document is to reduce the number of review cycles for ANDAs by helping applicants avoid these deficiencies.
The second document is a Manual of Policies and Procedures (MAPP), “Good ANDA Assessment Practices,” which outlines ANDA assessment practices for FDA staff.
This document formalizes a more streamlined generic review process, including the introduction of new templates designed to make each cycle of the review process more efficient and complete.
Releasing these new documents is part of the FDA’s Drug Competition Action Plan, which has 3 main goals:
- To reduce actions by branded pharmaceutical companies that can delay generic drug entry into the marketplace
- To resolve scientific and regulatory obstacles that can make it difficult to win approval of generic versions of certain complex drugs
- To improve the efficiency and predictability of the FDA’s generic review process to reduce the time it takes to get a generic drug approved and lessen the number of review cycles needed for generic applications.
The new MAPP and draft guidance documents for ANDAs are intended to help the FDA meet the third goal of the Drug Competition Action Plan.
The FDA is hoping to address the second goal of the plan later this year, building upon its initiatives to accelerate review and approval of complex generics.
The agency is also planning to develop guidance documents during the first quarter of 2018 that will address 3 issues related to the first goal of the plan—potential abuses of the citizen petition process, companies that restrict access to testing samples of branded drugs, and abuses of the single, shared system REMS (risk evaluation and mitigation strategy) negotiation process. ![]()
Obesity has negative impact on HSC compartment
Obesity can affect the long-term health of hematopoietic stem cells (HSCs), according to research published in the Journal of Experimental Medicine.
Conducted largely in models of obese mice, the research showed that obesity causes durable and harmful changes to the HSC compartment.
“Keeping this compartment healthy is essential to human health,” said study author Damien Reynaud, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This includes maintaining the diverse pool of [HSCs] needed to produce blood cells the body needs to function properly.”
Although still poorly understood, research is showing that age and environmental stresses can lessen the healthy diversity of cells in the hematopoietic system.
This can include skewing blood cell formation toward myeloid cells and possibly promoting pre-leukemic fates, according to Dr Reynaud and his colleagues.
With the current study, the team found that obesity-related stresses alter the cellular architecture of the HSC compartment and reduce its long-term functional fitness.
Tests in obese mice showed these effects were progressive. And some of the harmful manifestations persisted even after the researchers normalized the animals’ weight through dietary controls.
These alterations of the hematopoietic system appear to be linked to overexpression of the transcription factor Gfi1.
The researchers found that oxidative stresses in the body caused by obesity drive overexpression of Gfi1. When this happens, it produces a lasting alteration of the HSC compartment.
The researchers said their study provides groundwork to investigate how lifestyle choices, such as diet, can durably impact blood formation and may contribute to the development of blood cancers.
The study also raises questions about the use of HSCs isolated from obese transplant donors.
“Little is known about how obesity in marrow donors could affect the quality of the hematopoietic stem cell compartment,” Dr Reynaud explained.
“We want to better understand the molecular alterations in obesity to predict potential risks associated with the therapeutic use of stem cells isolated from obese donors.” ![]()
Obesity can affect the long-term health of hematopoietic stem cells (HSCs), according to research published in the Journal of Experimental Medicine.
Conducted largely in models of obese mice, the research showed that obesity causes durable and harmful changes to the HSC compartment.
“Keeping this compartment healthy is essential to human health,” said study author Damien Reynaud, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This includes maintaining the diverse pool of [HSCs] needed to produce blood cells the body needs to function properly.”
Although still poorly understood, research is showing that age and environmental stresses can lessen the healthy diversity of cells in the hematopoietic system.
This can include skewing blood cell formation toward myeloid cells and possibly promoting pre-leukemic fates, according to Dr Reynaud and his colleagues.
With the current study, the team found that obesity-related stresses alter the cellular architecture of the HSC compartment and reduce its long-term functional fitness.
Tests in obese mice showed these effects were progressive. And some of the harmful manifestations persisted even after the researchers normalized the animals’ weight through dietary controls.
These alterations of the hematopoietic system appear to be linked to overexpression of the transcription factor Gfi1.
The researchers found that oxidative stresses in the body caused by obesity drive overexpression of Gfi1. When this happens, it produces a lasting alteration of the HSC compartment.
The researchers said their study provides groundwork to investigate how lifestyle choices, such as diet, can durably impact blood formation and may contribute to the development of blood cancers.
The study also raises questions about the use of HSCs isolated from obese transplant donors.
“Little is known about how obesity in marrow donors could affect the quality of the hematopoietic stem cell compartment,” Dr Reynaud explained.
“We want to better understand the molecular alterations in obesity to predict potential risks associated with the therapeutic use of stem cells isolated from obese donors.” ![]()
Obesity can affect the long-term health of hematopoietic stem cells (HSCs), according to research published in the Journal of Experimental Medicine.
Conducted largely in models of obese mice, the research showed that obesity causes durable and harmful changes to the HSC compartment.
“Keeping this compartment healthy is essential to human health,” said study author Damien Reynaud, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
“This includes maintaining the diverse pool of [HSCs] needed to produce blood cells the body needs to function properly.”
Although still poorly understood, research is showing that age and environmental stresses can lessen the healthy diversity of cells in the hematopoietic system.
This can include skewing blood cell formation toward myeloid cells and possibly promoting pre-leukemic fates, according to Dr Reynaud and his colleagues.
With the current study, the team found that obesity-related stresses alter the cellular architecture of the HSC compartment and reduce its long-term functional fitness.
Tests in obese mice showed these effects were progressive. And some of the harmful manifestations persisted even after the researchers normalized the animals’ weight through dietary controls.
These alterations of the hematopoietic system appear to be linked to overexpression of the transcription factor Gfi1.
The researchers found that oxidative stresses in the body caused by obesity drive overexpression of Gfi1. When this happens, it produces a lasting alteration of the HSC compartment.
The researchers said their study provides groundwork to investigate how lifestyle choices, such as diet, can durably impact blood formation and may contribute to the development of blood cancers.
The study also raises questions about the use of HSCs isolated from obese transplant donors.
“Little is known about how obesity in marrow donors could affect the quality of the hematopoietic stem cell compartment,” Dr Reynaud explained.
“We want to better understand the molecular alterations in obesity to predict potential risks associated with the therapeutic use of stem cells isolated from obese donors.” ![]()
CX-01 receives orphan designation for AML
The US Food and Drug Administration (FDA) has granted orphan drug designation to CX-01 for the treatment of acute myeloid leukemia (AML).
CX-01 is a polysaccharide derived from heparin that is thought to enhance chemotherapy by disrupting the adhesion of leukemia cells in the bone marrow.
CX-01 inhibits the activity of HMGB1, disrupts the CXCL12/CXCR4 axis, and neutralizes the activity of platelet factor 4.
HMGB1 has been implicated in autophagy, a mechanism by which cells withstand the effects of chemotherapy. The CXCL12/CXCR4 axis is thought to be involved in protecting leukemia cells from chemotherapy. And platelet factor 4 inhibits bone marrow recovery after chemotherapy.
Cantex Pharmaceuticals, Inc., is conducting a randomized, phase 2b study to determine whether CX-01 can improve the efficacy of frontline chemotherapy in patients with AML.
This study builds upon results of a pilot study, which were presented at the 2015 ASCO Annual Meeting (abstract 7053).
The study enrolled 12 adults with newly diagnosed AML. They received CX-01 as a 7-day continuous infusion, along with standard induction chemotherapy (cytarabine and idarubicin, 7+3).
Eleven patients (92%), all of whom had de novo AML, had a complete response (CR) with a single induction cycle.
The median time to neutrophil recovery was 23 days, and the median time to platelet recovery was 22 days.
With a median follow-up of 14.2 months, the median event-free survival exceeded 11.6 months, and the median overall survival exceeded 13.6 months.
No adverse events related to CX-01 were reported.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to CX-01 for the treatment of acute myeloid leukemia (AML).
CX-01 is a polysaccharide derived from heparin that is thought to enhance chemotherapy by disrupting the adhesion of leukemia cells in the bone marrow.
CX-01 inhibits the activity of HMGB1, disrupts the CXCL12/CXCR4 axis, and neutralizes the activity of platelet factor 4.
HMGB1 has been implicated in autophagy, a mechanism by which cells withstand the effects of chemotherapy. The CXCL12/CXCR4 axis is thought to be involved in protecting leukemia cells from chemotherapy. And platelet factor 4 inhibits bone marrow recovery after chemotherapy.
Cantex Pharmaceuticals, Inc., is conducting a randomized, phase 2b study to determine whether CX-01 can improve the efficacy of frontline chemotherapy in patients with AML.
This study builds upon results of a pilot study, which were presented at the 2015 ASCO Annual Meeting (abstract 7053).
The study enrolled 12 adults with newly diagnosed AML. They received CX-01 as a 7-day continuous infusion, along with standard induction chemotherapy (cytarabine and idarubicin, 7+3).
Eleven patients (92%), all of whom had de novo AML, had a complete response (CR) with a single induction cycle.
The median time to neutrophil recovery was 23 days, and the median time to platelet recovery was 22 days.
With a median follow-up of 14.2 months, the median event-free survival exceeded 11.6 months, and the median overall survival exceeded 13.6 months.
No adverse events related to CX-01 were reported.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to CX-01 for the treatment of acute myeloid leukemia (AML).
CX-01 is a polysaccharide derived from heparin that is thought to enhance chemotherapy by disrupting the adhesion of leukemia cells in the bone marrow.
CX-01 inhibits the activity of HMGB1, disrupts the CXCL12/CXCR4 axis, and neutralizes the activity of platelet factor 4.
HMGB1 has been implicated in autophagy, a mechanism by which cells withstand the effects of chemotherapy. The CXCL12/CXCR4 axis is thought to be involved in protecting leukemia cells from chemotherapy. And platelet factor 4 inhibits bone marrow recovery after chemotherapy.
Cantex Pharmaceuticals, Inc., is conducting a randomized, phase 2b study to determine whether CX-01 can improve the efficacy of frontline chemotherapy in patients with AML.
This study builds upon results of a pilot study, which were presented at the 2015 ASCO Annual Meeting (abstract 7053).
The study enrolled 12 adults with newly diagnosed AML. They received CX-01 as a 7-day continuous infusion, along with standard induction chemotherapy (cytarabine and idarubicin, 7+3).
Eleven patients (92%), all of whom had de novo AML, had a complete response (CR) with a single induction cycle.
The median time to neutrophil recovery was 23 days, and the median time to platelet recovery was 22 days.
With a median follow-up of 14.2 months, the median event-free survival exceeded 11.6 months, and the median overall survival exceeded 13.6 months.
No adverse events related to CX-01 were reported.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
Brentuximab vedotin sBLA receives priority review
The US Food and Drug Administration (FDA) has accepted for priority review a supplemental biologics license application (sBLA) for brentuximab vedotin (ADCETRIS).
With this sBLA, Seattle Genetics, Inc., is seeking approval for brentuximab vedotin in combination with chemotherapy for frontline treatment of patients with advanced classical Hodgkin lymphoma (HL).
The FDA expects to make a decision on the sBLA by May 1, 2018.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The priority review for this sBLA is based on positive results from the phase 3 ECHELON-1 trial.
The FDA previously granted brentuximab vedotin breakthrough therapy designation based on ECHELON-1 results.
Breakthrough therapy designation is intended to expedite the development and review of promising drug candidates for serious or life-threatening conditions. It is based upon clinical evidence of substantial improvement over existing therapies in one or more clinically significant endpoints.
ECHELON-1
Result from ECHELON-1 were presented at the 2017 ASH Annual Meeting and simultaneously published in NEJM.
In this trial, researchers compared brentuximab vedotin, doxorubicin, vinblastine, and dacarbazine (A+AVD) to doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline treatment for 1334 patients with advanced HL.
The study’s primary endpoint was modified progression-free survival (PFS), which was defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review facility, A+AVD provided a significant improvement in modified PFS compared to ABVD. The hazard ratio was 0.77 (P=0.035), which corresponds to a 23% reduction in the risk of progression, death, or the need for additional anticancer therapy.
The 2-year modified PFS rate was 82.1% in the A+AVD arm and 77.2% in the ABVD arm.
There was no significant difference between the treatment arms when it came to response rates or overall survival.
The objective response rate was 86% in the A+AVD arm and 83% in the ABVD arm (P=0.12). The complete response rate was 73% and 70%, respectively (P=0.22).
The interim 2-year overall survival rate was 97% in the A+AVD arm and 95% in the ABVD arm (hazard ratio=0.72; P=0.19).
The overall incidence of adverse events (AEs) was 99% in the A+AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively, and the incidence of serious AEs was 43% and 27%, respectively.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with A+AVD, while pulmonary toxicity was more common with ABVD.
About brentuximab vedotin
Brentuximab vedotin is already FDA-approved to treat adults with:
- Classical HL who have failed autologous hematopoietic stem cell transplant (auto-HSCT) or, in those who are not auto-HSCT candidates, have failed at least 2 prior multi-agent chemotherapy regimens.
- Classical HL at high risk of relapse or progression as post-auto-HSCT consolidation.
- Primary cutaneous anaplastic large-cell lymphoma (ALCL) or CD30-expressing mycosis fungoides who have received prior systemic therapy.
- Systemic ALCL who have failed at least 1 prior multi-agent chemotherapy regimen. (The drug has accelerated approval for this indication, based on overall response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.)

The US Food and Drug Administration (FDA) has accepted for priority review a supplemental biologics license application (sBLA) for brentuximab vedotin (ADCETRIS).
With this sBLA, Seattle Genetics, Inc., is seeking approval for brentuximab vedotin in combination with chemotherapy for frontline treatment of patients with advanced classical Hodgkin lymphoma (HL).
The FDA expects to make a decision on the sBLA by May 1, 2018.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The priority review for this sBLA is based on positive results from the phase 3 ECHELON-1 trial.
The FDA previously granted brentuximab vedotin breakthrough therapy designation based on ECHELON-1 results.
Breakthrough therapy designation is intended to expedite the development and review of promising drug candidates for serious or life-threatening conditions. It is based upon clinical evidence of substantial improvement over existing therapies in one or more clinically significant endpoints.
ECHELON-1
Result from ECHELON-1 were presented at the 2017 ASH Annual Meeting and simultaneously published in NEJM.
In this trial, researchers compared brentuximab vedotin, doxorubicin, vinblastine, and dacarbazine (A+AVD) to doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline treatment for 1334 patients with advanced HL.
The study’s primary endpoint was modified progression-free survival (PFS), which was defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review facility, A+AVD provided a significant improvement in modified PFS compared to ABVD. The hazard ratio was 0.77 (P=0.035), which corresponds to a 23% reduction in the risk of progression, death, or the need for additional anticancer therapy.
The 2-year modified PFS rate was 82.1% in the A+AVD arm and 77.2% in the ABVD arm.
There was no significant difference between the treatment arms when it came to response rates or overall survival.
The objective response rate was 86% in the A+AVD arm and 83% in the ABVD arm (P=0.12). The complete response rate was 73% and 70%, respectively (P=0.22).
The interim 2-year overall survival rate was 97% in the A+AVD arm and 95% in the ABVD arm (hazard ratio=0.72; P=0.19).
The overall incidence of adverse events (AEs) was 99% in the A+AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively, and the incidence of serious AEs was 43% and 27%, respectively.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with A+AVD, while pulmonary toxicity was more common with ABVD.
About brentuximab vedotin
Brentuximab vedotin is already FDA-approved to treat adults with:
- Classical HL who have failed autologous hematopoietic stem cell transplant (auto-HSCT) or, in those who are not auto-HSCT candidates, have failed at least 2 prior multi-agent chemotherapy regimens.
- Classical HL at high risk of relapse or progression as post-auto-HSCT consolidation.
- Primary cutaneous anaplastic large-cell lymphoma (ALCL) or CD30-expressing mycosis fungoides who have received prior systemic therapy.
- Systemic ALCL who have failed at least 1 prior multi-agent chemotherapy regimen. (The drug has accelerated approval for this indication, based on overall response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.)

The US Food and Drug Administration (FDA) has accepted for priority review a supplemental biologics license application (sBLA) for brentuximab vedotin (ADCETRIS).
With this sBLA, Seattle Genetics, Inc., is seeking approval for brentuximab vedotin in combination with chemotherapy for frontline treatment of patients with advanced classical Hodgkin lymphoma (HL).
The FDA expects to make a decision on the sBLA by May 1, 2018.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The priority review for this sBLA is based on positive results from the phase 3 ECHELON-1 trial.
The FDA previously granted brentuximab vedotin breakthrough therapy designation based on ECHELON-1 results.
Breakthrough therapy designation is intended to expedite the development and review of promising drug candidates for serious or life-threatening conditions. It is based upon clinical evidence of substantial improvement over existing therapies in one or more clinically significant endpoints.
ECHELON-1
Result from ECHELON-1 were presented at the 2017 ASH Annual Meeting and simultaneously published in NEJM.
In this trial, researchers compared brentuximab vedotin, doxorubicin, vinblastine, and dacarbazine (A+AVD) to doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline treatment for 1334 patients with advanced HL.
The study’s primary endpoint was modified progression-free survival (PFS), which was defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review facility, A+AVD provided a significant improvement in modified PFS compared to ABVD. The hazard ratio was 0.77 (P=0.035), which corresponds to a 23% reduction in the risk of progression, death, or the need for additional anticancer therapy.
The 2-year modified PFS rate was 82.1% in the A+AVD arm and 77.2% in the ABVD arm.
There was no significant difference between the treatment arms when it came to response rates or overall survival.
The objective response rate was 86% in the A+AVD arm and 83% in the ABVD arm (P=0.12). The complete response rate was 73% and 70%, respectively (P=0.22).
The interim 2-year overall survival rate was 97% in the A+AVD arm and 95% in the ABVD arm (hazard ratio=0.72; P=0.19).
The overall incidence of adverse events (AEs) was 99% in the A+AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively, and the incidence of serious AEs was 43% and 27%, respectively.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with A+AVD, while pulmonary toxicity was more common with ABVD.
About brentuximab vedotin
Brentuximab vedotin is already FDA-approved to treat adults with:
- Classical HL who have failed autologous hematopoietic stem cell transplant (auto-HSCT) or, in those who are not auto-HSCT candidates, have failed at least 2 prior multi-agent chemotherapy regimens.
- Classical HL at high risk of relapse or progression as post-auto-HSCT consolidation.
- Primary cutaneous anaplastic large-cell lymphoma (ALCL) or CD30-expressing mycosis fungoides who have received prior systemic therapy.
- Systemic ALCL who have failed at least 1 prior multi-agent chemotherapy regimen. (The drug has accelerated approval for this indication, based on overall response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.)

FDA lifts hold on trial of SEL24 in AML
The US Food and Drug Administration (FDA) has lifted the clinical hold placed on a phase 1/2 trial of SEL24, a dual PIM/FLT3 kinase inhibitor, in patients with relapsed/refractory acute myeloid leukemia (AML).
Selvita and Menarini Group, the companies developing SEL24, agreed to continue the trial with additional provisions to its protocol.
The companies will be working with trial investigators and clinical sites to obtain institutional review board approval on the revised protocol and resume enrollment in the trial, according to Krzysztof Brzozka, PhD, chief scientific officer of Selvita.
The trial is a dose-escalation study of SEL24 in patients with relapsed and refractory AML. The study was designed to determine the maximum tolerated dose and recommended dose of SEL24.
The first patient was dosed in March 2017. The study began with a 25 mg daily dose, which was then escalated following cohort reviews.
In October, the trial was placed on full clinical hold, which meant no new patients could be enrolled on the trial, and enrolled patients could not receive SEL24 until the hold was lifted.
The hold was the result of a fatal cerebral adverse event that was considered possibly related to SEL24.
The event occurred in a patient who started treatment with a 150 mg dose of SEL24 as the third patient in this dose cohort.
The patient received 4 doses of the drug and developed a life-threatening, grade 4 venous thrombus in the brain with subsequent intracerebral hemorrhage, which required hospitalization.
The patient died in hospice 4 days later. The patient’s death was deemed possibly related to SEL24.
In response to the death, a safety report was submitted to the FDA, along with a review by the trial’s data monitoring committee.
The FDA then placed a hold on the trial and requested more safety data on patients who have received SEL24, as well as specific protocol changes and additional guidance to the study staff.
Selvita and Menarini Group complied with the FDA’s requests and agreed to revise the dose-finding scheme to a standard 3+3 design under an amended protocol. ![]()
The US Food and Drug Administration (FDA) has lifted the clinical hold placed on a phase 1/2 trial of SEL24, a dual PIM/FLT3 kinase inhibitor, in patients with relapsed/refractory acute myeloid leukemia (AML).
Selvita and Menarini Group, the companies developing SEL24, agreed to continue the trial with additional provisions to its protocol.
The companies will be working with trial investigators and clinical sites to obtain institutional review board approval on the revised protocol and resume enrollment in the trial, according to Krzysztof Brzozka, PhD, chief scientific officer of Selvita.
The trial is a dose-escalation study of SEL24 in patients with relapsed and refractory AML. The study was designed to determine the maximum tolerated dose and recommended dose of SEL24.
The first patient was dosed in March 2017. The study began with a 25 mg daily dose, which was then escalated following cohort reviews.
In October, the trial was placed on full clinical hold, which meant no new patients could be enrolled on the trial, and enrolled patients could not receive SEL24 until the hold was lifted.
The hold was the result of a fatal cerebral adverse event that was considered possibly related to SEL24.
The event occurred in a patient who started treatment with a 150 mg dose of SEL24 as the third patient in this dose cohort.
The patient received 4 doses of the drug and developed a life-threatening, grade 4 venous thrombus in the brain with subsequent intracerebral hemorrhage, which required hospitalization.
The patient died in hospice 4 days later. The patient’s death was deemed possibly related to SEL24.
In response to the death, a safety report was submitted to the FDA, along with a review by the trial’s data monitoring committee.
The FDA then placed a hold on the trial and requested more safety data on patients who have received SEL24, as well as specific protocol changes and additional guidance to the study staff.
Selvita and Menarini Group complied with the FDA’s requests and agreed to revise the dose-finding scheme to a standard 3+3 design under an amended protocol. ![]()
The US Food and Drug Administration (FDA) has lifted the clinical hold placed on a phase 1/2 trial of SEL24, a dual PIM/FLT3 kinase inhibitor, in patients with relapsed/refractory acute myeloid leukemia (AML).
Selvita and Menarini Group, the companies developing SEL24, agreed to continue the trial with additional provisions to its protocol.
The companies will be working with trial investigators and clinical sites to obtain institutional review board approval on the revised protocol and resume enrollment in the trial, according to Krzysztof Brzozka, PhD, chief scientific officer of Selvita.
The trial is a dose-escalation study of SEL24 in patients with relapsed and refractory AML. The study was designed to determine the maximum tolerated dose and recommended dose of SEL24.
The first patient was dosed in March 2017. The study began with a 25 mg daily dose, which was then escalated following cohort reviews.
In October, the trial was placed on full clinical hold, which meant no new patients could be enrolled on the trial, and enrolled patients could not receive SEL24 until the hold was lifted.
The hold was the result of a fatal cerebral adverse event that was considered possibly related to SEL24.
The event occurred in a patient who started treatment with a 150 mg dose of SEL24 as the third patient in this dose cohort.
The patient received 4 doses of the drug and developed a life-threatening, grade 4 venous thrombus in the brain with subsequent intracerebral hemorrhage, which required hospitalization.
The patient died in hospice 4 days later. The patient’s death was deemed possibly related to SEL24.
In response to the death, a safety report was submitted to the FDA, along with a review by the trial’s data monitoring committee.
The FDA then placed a hold on the trial and requested more safety data on patients who have received SEL24, as well as specific protocol changes and additional guidance to the study staff.
Selvita and Menarini Group complied with the FDA’s requests and agreed to revise the dose-finding scheme to a standard 3+3 design under an amended protocol. ![]()
Repurposed drug could improve HSCT
A medication used to treat joint and skin conditions might also improve allogeneic hematopoietic stem cell transplant (HSCT), according to research published in Science Translational Medicine.
Researchers discovered that, once transplanted, some differentiated cells produce tumor necrosis factor-alpha (TNFα), which impairs cell division and survival of hematopoietic stem and progenitor cells (HSPCs).
This led the researchers to explore whether a drug that blocks TNFα would allow HSPCs to thrive in a new host.
The team administered etanercept, an antibody that binds to and disables TNFα, to mice receiving umbilical cord blood (UCB) transplants.
Mice that received the drug had better bone marrow reconstitution than control mice.
“If this strategy boosts the survival rate of blood stem cells in humans, then we can get away with using smaller grafts,” said study author Peter Zandstra, PhD, of the University of British Columbia in Vancouver, British Columbia, Canada.
“That would vastly increase the pool of usable umbilical cord blood donations, making stem cell transplants more feasible, not only for blood cancers, which we are already doing, but also for auto-immune diseases, like Crohn’s disease, even HIV.”
Dr Zandstra and his colleagues began this research by performing UCB transplants in immunodeficient mice.
The team was surprised to find that mice receiving the highest numbers of UCB cells had the worst outcomes in terms of bone marrow reconstitution. The researchers also found elevated levels of cytokines in the animals’ sera.
The team speculated that mature immune cells within UCB might be producing inflammatory cytokines, thus preventing HSPCs from successfully repopulating the bone marrow.
One molecule in particular, TNFα, inhibited HSPC survival and division.
Treating recipient mice with the TNFα blocker etanercept enhanced short-term HSPC engraftment and accelerated hematopoietic recovery after UCB transplants.
According to the researchers, these results implicate TNFα as a central player in setting off the cytokine storm that can impair donor HSPC survival.
The team also believes their results provide a strong basis for conducting a clinical trial to see whether etanercept or another TNFα blocker would improve outcomes for people receiving HSCTs.
“Failure of the graft after stem cell transplantation is always a potentially life-threatening complication,” said Kirk Schultz, MD, a professor at the University of British Columbia who was not involved in this study.
“This is especially the case when we must use mismatched stem cells derived from umbilical cord blood. This advance may offer a significant advance in making these transplants more successful.” ![]()
A medication used to treat joint and skin conditions might also improve allogeneic hematopoietic stem cell transplant (HSCT), according to research published in Science Translational Medicine.
Researchers discovered that, once transplanted, some differentiated cells produce tumor necrosis factor-alpha (TNFα), which impairs cell division and survival of hematopoietic stem and progenitor cells (HSPCs).
This led the researchers to explore whether a drug that blocks TNFα would allow HSPCs to thrive in a new host.
The team administered etanercept, an antibody that binds to and disables TNFα, to mice receiving umbilical cord blood (UCB) transplants.
Mice that received the drug had better bone marrow reconstitution than control mice.
“If this strategy boosts the survival rate of blood stem cells in humans, then we can get away with using smaller grafts,” said study author Peter Zandstra, PhD, of the University of British Columbia in Vancouver, British Columbia, Canada.
“That would vastly increase the pool of usable umbilical cord blood donations, making stem cell transplants more feasible, not only for blood cancers, which we are already doing, but also for auto-immune diseases, like Crohn’s disease, even HIV.”
Dr Zandstra and his colleagues began this research by performing UCB transplants in immunodeficient mice.
The team was surprised to find that mice receiving the highest numbers of UCB cells had the worst outcomes in terms of bone marrow reconstitution. The researchers also found elevated levels of cytokines in the animals’ sera.
The team speculated that mature immune cells within UCB might be producing inflammatory cytokines, thus preventing HSPCs from successfully repopulating the bone marrow.
One molecule in particular, TNFα, inhibited HSPC survival and division.
Treating recipient mice with the TNFα blocker etanercept enhanced short-term HSPC engraftment and accelerated hematopoietic recovery after UCB transplants.
According to the researchers, these results implicate TNFα as a central player in setting off the cytokine storm that can impair donor HSPC survival.
The team also believes their results provide a strong basis for conducting a clinical trial to see whether etanercept or another TNFα blocker would improve outcomes for people receiving HSCTs.
“Failure of the graft after stem cell transplantation is always a potentially life-threatening complication,” said Kirk Schultz, MD, a professor at the University of British Columbia who was not involved in this study.
“This is especially the case when we must use mismatched stem cells derived from umbilical cord blood. This advance may offer a significant advance in making these transplants more successful.” ![]()
A medication used to treat joint and skin conditions might also improve allogeneic hematopoietic stem cell transplant (HSCT), according to research published in Science Translational Medicine.
Researchers discovered that, once transplanted, some differentiated cells produce tumor necrosis factor-alpha (TNFα), which impairs cell division and survival of hematopoietic stem and progenitor cells (HSPCs).
This led the researchers to explore whether a drug that blocks TNFα would allow HSPCs to thrive in a new host.
The team administered etanercept, an antibody that binds to and disables TNFα, to mice receiving umbilical cord blood (UCB) transplants.
Mice that received the drug had better bone marrow reconstitution than control mice.
“If this strategy boosts the survival rate of blood stem cells in humans, then we can get away with using smaller grafts,” said study author Peter Zandstra, PhD, of the University of British Columbia in Vancouver, British Columbia, Canada.
“That would vastly increase the pool of usable umbilical cord blood donations, making stem cell transplants more feasible, not only for blood cancers, which we are already doing, but also for auto-immune diseases, like Crohn’s disease, even HIV.”
Dr Zandstra and his colleagues began this research by performing UCB transplants in immunodeficient mice.
The team was surprised to find that mice receiving the highest numbers of UCB cells had the worst outcomes in terms of bone marrow reconstitution. The researchers also found elevated levels of cytokines in the animals’ sera.
The team speculated that mature immune cells within UCB might be producing inflammatory cytokines, thus preventing HSPCs from successfully repopulating the bone marrow.
One molecule in particular, TNFα, inhibited HSPC survival and division.
Treating recipient mice with the TNFα blocker etanercept enhanced short-term HSPC engraftment and accelerated hematopoietic recovery after UCB transplants.
According to the researchers, these results implicate TNFα as a central player in setting off the cytokine storm that can impair donor HSPC survival.
The team also believes their results provide a strong basis for conducting a clinical trial to see whether etanercept or another TNFα blocker would improve outcomes for people receiving HSCTs.
“Failure of the graft after stem cell transplantation is always a potentially life-threatening complication,” said Kirk Schultz, MD, a professor at the University of British Columbia who was not involved in this study.
“This is especially the case when we must use mismatched stem cells derived from umbilical cord blood. This advance may offer a significant advance in making these transplants more successful.” ![]()
Carfilzomib poses higher risk of CVAEs, review suggests
Treatment with the proteasome inhibitor carfilzomib is associated with a “significant incidence” of cardiovascular adverse events (CVAEs) in patients with multiple myeloma (MM), according to researchers.
An analysis of 24 studies showed that 18% of MM patients receiving carfilzomib had CVAEs, and 8% had grade 3 or higher CVAEs.
The relative risk of CVAEs (all-grade or high-grade) was higher among patients who received carfilzomib than among those who did not.
These findings were published in JAMA Oncology.
The researchers gathered data from 24 studies reported from 2007 through 2017. The studies included 2594 MM patients.
The team looked at the incidence of CVAEs, which included heart failure, hypertension, ischemia, and arrhythmia.
The data showed that 18.1% of patients who took carfilzomib experienced CVAEs, and 8.2% of the patients had grade 3 or higher CVAEs.
For comparison, a similar review of bortezomib showed that 3.8% of patients experienced CVAEs, and 2.3% of patients had high-grade CVAEs.
Among the carfilzomib-treated patients, the most common CVAE was hypertension (12.2%), followed by heart failure (4.1%), arrhythmias (2.4%), and ischemic events (1.8%).
Higher doses of carfilzomib were associated with higher rates of high-grade CVAEs. The incidence of high-grade CVAEs was 6.4% in patients who received carfilzomib doses below 45 mg/m2 and 11.9% in patients who received the drug at doses of 45 mg/m2 or higher (P=0.02).
The researchers also compared CVAE rates in carfilzomib-treated patients and non-carfilzomib-treated patients enrolled in a trio of phase 3, randomized trials:
- ASPIRE (carfilzomib, lenalidomide, and dexamethasone vs lenalidomide and dexamethasone)
- ENDEAVOR (carfilzomib and dexamethasone vs bortezomib and dexamethasone)
- FOCUS (carfilzomib and dexamethasone vs dexamethasone with or without cyclophosphamide).
The relative risk of all-grade CVAEs was 1.8 for carfilzomib-treated patients vs controls (P<0.001), and the relative risk of grade 3 or higher CVAEs was 2.2 (P<0.001).
“Taken together, these findings argue that carfilzomib is responsible for an elevated risk, and anyone who is treating patients with this drug needs to be aware that this is a common event,” said study author Adam J. Waxman, MD, of the Perelman School of Medicine at the University of Pennsylvania in Philadelphia.
“Clinicians should be paying attention to who may be at highest risk for these events so they can tailor their therapy accordingly.”
Dr Waxman and his colleagues also called for further clinical trials to evaluate the association between carfilzomib and CVAEs, arguing that it may be underrepresented by current data.
“If you’re not specifically looking for this, you might report it differently,” Dr Waxman said.
This research was supported by the National Institutes of Health (T32-GM075766). ![]()
Treatment with the proteasome inhibitor carfilzomib is associated with a “significant incidence” of cardiovascular adverse events (CVAEs) in patients with multiple myeloma (MM), according to researchers.
An analysis of 24 studies showed that 18% of MM patients receiving carfilzomib had CVAEs, and 8% had grade 3 or higher CVAEs.
The relative risk of CVAEs (all-grade or high-grade) was higher among patients who received carfilzomib than among those who did not.
These findings were published in JAMA Oncology.
The researchers gathered data from 24 studies reported from 2007 through 2017. The studies included 2594 MM patients.
The team looked at the incidence of CVAEs, which included heart failure, hypertension, ischemia, and arrhythmia.
The data showed that 18.1% of patients who took carfilzomib experienced CVAEs, and 8.2% of the patients had grade 3 or higher CVAEs.
For comparison, a similar review of bortezomib showed that 3.8% of patients experienced CVAEs, and 2.3% of patients had high-grade CVAEs.
Among the carfilzomib-treated patients, the most common CVAE was hypertension (12.2%), followed by heart failure (4.1%), arrhythmias (2.4%), and ischemic events (1.8%).
Higher doses of carfilzomib were associated with higher rates of high-grade CVAEs. The incidence of high-grade CVAEs was 6.4% in patients who received carfilzomib doses below 45 mg/m2 and 11.9% in patients who received the drug at doses of 45 mg/m2 or higher (P=0.02).
The researchers also compared CVAE rates in carfilzomib-treated patients and non-carfilzomib-treated patients enrolled in a trio of phase 3, randomized trials:
- ASPIRE (carfilzomib, lenalidomide, and dexamethasone vs lenalidomide and dexamethasone)
- ENDEAVOR (carfilzomib and dexamethasone vs bortezomib and dexamethasone)
- FOCUS (carfilzomib and dexamethasone vs dexamethasone with or without cyclophosphamide).
The relative risk of all-grade CVAEs was 1.8 for carfilzomib-treated patients vs controls (P<0.001), and the relative risk of grade 3 or higher CVAEs was 2.2 (P<0.001).
“Taken together, these findings argue that carfilzomib is responsible for an elevated risk, and anyone who is treating patients with this drug needs to be aware that this is a common event,” said study author Adam J. Waxman, MD, of the Perelman School of Medicine at the University of Pennsylvania in Philadelphia.
“Clinicians should be paying attention to who may be at highest risk for these events so they can tailor their therapy accordingly.”
Dr Waxman and his colleagues also called for further clinical trials to evaluate the association between carfilzomib and CVAEs, arguing that it may be underrepresented by current data.
“If you’re not specifically looking for this, you might report it differently,” Dr Waxman said.
This research was supported by the National Institutes of Health (T32-GM075766). ![]()
Treatment with the proteasome inhibitor carfilzomib is associated with a “significant incidence” of cardiovascular adverse events (CVAEs) in patients with multiple myeloma (MM), according to researchers.
An analysis of 24 studies showed that 18% of MM patients receiving carfilzomib had CVAEs, and 8% had grade 3 or higher CVAEs.
The relative risk of CVAEs (all-grade or high-grade) was higher among patients who received carfilzomib than among those who did not.
These findings were published in JAMA Oncology.
The researchers gathered data from 24 studies reported from 2007 through 2017. The studies included 2594 MM patients.
The team looked at the incidence of CVAEs, which included heart failure, hypertension, ischemia, and arrhythmia.
The data showed that 18.1% of patients who took carfilzomib experienced CVAEs, and 8.2% of the patients had grade 3 or higher CVAEs.
For comparison, a similar review of bortezomib showed that 3.8% of patients experienced CVAEs, and 2.3% of patients had high-grade CVAEs.
Among the carfilzomib-treated patients, the most common CVAE was hypertension (12.2%), followed by heart failure (4.1%), arrhythmias (2.4%), and ischemic events (1.8%).
Higher doses of carfilzomib were associated with higher rates of high-grade CVAEs. The incidence of high-grade CVAEs was 6.4% in patients who received carfilzomib doses below 45 mg/m2 and 11.9% in patients who received the drug at doses of 45 mg/m2 or higher (P=0.02).
The researchers also compared CVAE rates in carfilzomib-treated patients and non-carfilzomib-treated patients enrolled in a trio of phase 3, randomized trials:
- ASPIRE (carfilzomib, lenalidomide, and dexamethasone vs lenalidomide and dexamethasone)
- ENDEAVOR (carfilzomib and dexamethasone vs bortezomib and dexamethasone)
- FOCUS (carfilzomib and dexamethasone vs dexamethasone with or without cyclophosphamide).
The relative risk of all-grade CVAEs was 1.8 for carfilzomib-treated patients vs controls (P<0.001), and the relative risk of grade 3 or higher CVAEs was 2.2 (P<0.001).
“Taken together, these findings argue that carfilzomib is responsible for an elevated risk, and anyone who is treating patients with this drug needs to be aware that this is a common event,” said study author Adam J. Waxman, MD, of the Perelman School of Medicine at the University of Pennsylvania in Philadelphia.
“Clinicians should be paying attention to who may be at highest risk for these events so they can tailor their therapy accordingly.”
Dr Waxman and his colleagues also called for further clinical trials to evaluate the association between carfilzomib and CVAEs, arguing that it may be underrepresented by current data.
“If you’re not specifically looking for this, you might report it differently,” Dr Waxman said.
This research was supported by the National Institutes of Health (T32-GM075766).
Iron chelating agent could enhance chemo in AML
Chemotherapy for acute myeloid leukemia (AML) might be improved by the addition of deferoxamine, according to preclinical research published in Cell Stem Cell.
Researchers found that, when certain areas of the bone marrow are overtaken by AML cells, hematopoietic stem cells (HSCs) are lost, and the delivery of chemotherapy may be compromised.
However, the team also discovered that deferoxamine, a drug already approved to treat iron overload, can protect these areas of the bone marrow, allowing HSCs to survive and improving the efficacy of chemotherapy.
“Since the drug is already approved for human use for a different condition, we already know that it is safe,” said study author Cristina Lo Celso, PhD, of Imperial College London in the UK.
“We still need to test it in the context of leukemia and chemotherapy, but, because it is already in use, we can progress to clinical trials much quicker than we could with a brand-new drug.”
For the current study, Dr Lo Celso and her colleagues used intravital microscopy to study AML cells, healthy hematopoietic cells, and the bone marrow microenvironment in mice.
The researchers found the endosteal microenvironment was hit particularly hard by AML. Specifically, AML progression led to endosteal remodeling, with AML cells degrading endosteal endothelium, stromal cells, and osteoblastic cells.
This remodeling resulted in the loss of nonleukemic HSCs, which hindered hematopoiesis. However, preserving endosteal vessels prevented the loss of HSCs.
Previous research had shown that deferoxamine could induce endosteal vessel expansion through enhancement of hypoxia-inducible factor 1a stability and activity. So the researchers administered deferoxamine to mice with AML.
The drug had a protective effect on endosteal vessels, which were able to support healthy HSCs and improve HSC homing.
The researchers also found that enhanced endosteal vessels improved the efficacy of chemotherapy (cytarabine and doxorubicin) in mice with AML.
The team compared Fbxw7iΔEC-mutant mice, in which the administration of tamoxifen increases the number of endosteal vessels and arterioles, to control mice. Both sets of mice had AML.
After confirming the mutant mice had increased numbers of endosteal vessels, the researchers treated the mutant mice and controls with cytarabine and doxorubicin.
Both sets of mice had significant chemotherapy-induced damage to the bone marrow vasculature, including endosteal vessels.
However, after treatment, the Fbxw7iΔEC-mutant mice had lower numbers of surviving AML cells in the bone marrow, delayed relapse, and longer survival than control mice.
The researchers therefore concluded that rescuing endosteal vessels before starting chemotherapy can improve the efficacy of treatment in AML.
“Our work suggests that therapies targeting these blood vessels may improve existing therapeutic regimens for AML and perhaps other leukemias too,” said study author Delfim Duarte, MD, of Imperial College London.
Based on this work, the researchers are hoping to start trials of deferoxamine in patients with AML.
Chemotherapy for acute myeloid leukemia (AML) might be improved by the addition of deferoxamine, according to preclinical research published in Cell Stem Cell.
Researchers found that, when certain areas of the bone marrow are overtaken by AML cells, hematopoietic stem cells (HSCs) are lost, and the delivery of chemotherapy may be compromised.
However, the team also discovered that deferoxamine, a drug already approved to treat iron overload, can protect these areas of the bone marrow, allowing HSCs to survive and improving the efficacy of chemotherapy.
“Since the drug is already approved for human use for a different condition, we already know that it is safe,” said study author Cristina Lo Celso, PhD, of Imperial College London in the UK.
“We still need to test it in the context of leukemia and chemotherapy, but, because it is already in use, we can progress to clinical trials much quicker than we could with a brand-new drug.”
For the current study, Dr Lo Celso and her colleagues used intravital microscopy to study AML cells, healthy hematopoietic cells, and the bone marrow microenvironment in mice.
The researchers found the endosteal microenvironment was hit particularly hard by AML. Specifically, AML progression led to endosteal remodeling, with AML cells degrading endosteal endothelium, stromal cells, and osteoblastic cells.
This remodeling resulted in the loss of nonleukemic HSCs, which hindered hematopoiesis. However, preserving endosteal vessels prevented the loss of HSCs.
Previous research had shown that deferoxamine could induce endosteal vessel expansion through enhancement of hypoxia-inducible factor 1a stability and activity. So the researchers administered deferoxamine to mice with AML.
The drug had a protective effect on endosteal vessels, which were able to support healthy HSCs and improve HSC homing.
The researchers also found that enhanced endosteal vessels improved the efficacy of chemotherapy (cytarabine and doxorubicin) in mice with AML.
The team compared Fbxw7iΔEC-mutant mice, in which the administration of tamoxifen increases the number of endosteal vessels and arterioles, to control mice. Both sets of mice had AML.
After confirming the mutant mice had increased numbers of endosteal vessels, the researchers treated the mutant mice and controls with cytarabine and doxorubicin.
Both sets of mice had significant chemotherapy-induced damage to the bone marrow vasculature, including endosteal vessels.
However, after treatment, the Fbxw7iΔEC-mutant mice had lower numbers of surviving AML cells in the bone marrow, delayed relapse, and longer survival than control mice.
The researchers therefore concluded that rescuing endosteal vessels before starting chemotherapy can improve the efficacy of treatment in AML.
“Our work suggests that therapies targeting these blood vessels may improve existing therapeutic regimens for AML and perhaps other leukemias too,” said study author Delfim Duarte, MD, of Imperial College London.
Based on this work, the researchers are hoping to start trials of deferoxamine in patients with AML.
Chemotherapy for acute myeloid leukemia (AML) might be improved by the addition of deferoxamine, according to preclinical research published in Cell Stem Cell.
Researchers found that, when certain areas of the bone marrow are overtaken by AML cells, hematopoietic stem cells (HSCs) are lost, and the delivery of chemotherapy may be compromised.
However, the team also discovered that deferoxamine, a drug already approved to treat iron overload, can protect these areas of the bone marrow, allowing HSCs to survive and improving the efficacy of chemotherapy.
“Since the drug is already approved for human use for a different condition, we already know that it is safe,” said study author Cristina Lo Celso, PhD, of Imperial College London in the UK.
“We still need to test it in the context of leukemia and chemotherapy, but, because it is already in use, we can progress to clinical trials much quicker than we could with a brand-new drug.”
For the current study, Dr Lo Celso and her colleagues used intravital microscopy to study AML cells, healthy hematopoietic cells, and the bone marrow microenvironment in mice.
The researchers found the endosteal microenvironment was hit particularly hard by AML. Specifically, AML progression led to endosteal remodeling, with AML cells degrading endosteal endothelium, stromal cells, and osteoblastic cells.
This remodeling resulted in the loss of nonleukemic HSCs, which hindered hematopoiesis. However, preserving endosteal vessels prevented the loss of HSCs.
Previous research had shown that deferoxamine could induce endosteal vessel expansion through enhancement of hypoxia-inducible factor 1a stability and activity. So the researchers administered deferoxamine to mice with AML.
The drug had a protective effect on endosteal vessels, which were able to support healthy HSCs and improve HSC homing.
The researchers also found that enhanced endosteal vessels improved the efficacy of chemotherapy (cytarabine and doxorubicin) in mice with AML.
The team compared Fbxw7iΔEC-mutant mice, in which the administration of tamoxifen increases the number of endosteal vessels and arterioles, to control mice. Both sets of mice had AML.
After confirming the mutant mice had increased numbers of endosteal vessels, the researchers treated the mutant mice and controls with cytarabine and doxorubicin.
Both sets of mice had significant chemotherapy-induced damage to the bone marrow vasculature, including endosteal vessels.
However, after treatment, the Fbxw7iΔEC-mutant mice had lower numbers of surviving AML cells in the bone marrow, delayed relapse, and longer survival than control mice.
The researchers therefore concluded that rescuing endosteal vessels before starting chemotherapy can improve the efficacy of treatment in AML.
“Our work suggests that therapies targeting these blood vessels may improve existing therapeutic regimens for AML and perhaps other leukemias too,” said study author Delfim Duarte, MD, of Imperial College London.
Based on this work, the researchers are hoping to start trials of deferoxamine in patients with AML.
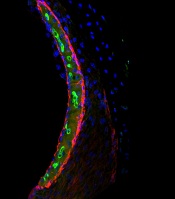
Research explains why cisplatin causes hearing loss
Researchers have gained new insight into hearing loss caused by cisplatin.
By measuring and mapping cisplatin retention in mouse and human inner ear tissues, the researchers found that cisplatin builds up in the inner ear and can remain there for years.
The team also found that a region in the inner ear called the stria vascularis could be targeted to prevent hearing loss resulting from cisplatin.
Lisa L. Cunningham, PhD, of the National Institute on Deafness and other Communications Disorders (NIDCD) in Bethesda, Maryland, and her colleagues reported these findings in Nature Communications.
The researchers noted that cisplatin can cause permanent hearing loss in 40% to 80% of treated patients. The team’s new findings help explain why.
The researchers found that, in most areas of the body, cisplatin is eliminated within days or weeks of treatment, but, in the inner ear, the drug remains much longer.
The team developed a mouse model that represents cisplatin-induced hearing loss seen in human patients.
By looking at inner ear tissue of mice after the first, second, and third cisplatin treatment, the researchers saw that cisplatin remained in the mouse inner ear much longer than in most other body tissues, and the drug builds up with each successive treatment.
The team also studied inner ear tissue donated by deceased adults who had been treated with cisplatin and found the drug is retained in the inner ear months or years after treatment.
When the researchers examined inner ear tissue from a child, they found cisplatin buildup that was even higher than that seen in adults.
Taken together, these results suggest the inner ear readily takes up cisplatin but has limited ability to remove the drug.
In mice and human tissues, the researchers saw the highest buildup of cisplatin in a part of the inner ear called the stria vascularis, which helps maintain the positive electrical charge in inner ear fluid that certain cells need to detect sound.
The team found the accumulation of cisplatin in the stria vascularis contributed to cisplatin-related hearing loss.
“Our findings suggest that if we can prevent cisplatin from entering the stria vascularis in the inner ear during treatment, we may be able to protect cancer patients from developing cisplatin-induced hearing loss,” Dr Cunningham said.
Researchers have gained new insight into hearing loss caused by cisplatin.
By measuring and mapping cisplatin retention in mouse and human inner ear tissues, the researchers found that cisplatin builds up in the inner ear and can remain there for years.
The team also found that a region in the inner ear called the stria vascularis could be targeted to prevent hearing loss resulting from cisplatin.
Lisa L. Cunningham, PhD, of the National Institute on Deafness and other Communications Disorders (NIDCD) in Bethesda, Maryland, and her colleagues reported these findings in Nature Communications.
The researchers noted that cisplatin can cause permanent hearing loss in 40% to 80% of treated patients. The team’s new findings help explain why.
The researchers found that, in most areas of the body, cisplatin is eliminated within days or weeks of treatment, but, in the inner ear, the drug remains much longer.
The team developed a mouse model that represents cisplatin-induced hearing loss seen in human patients.
By looking at inner ear tissue of mice after the first, second, and third cisplatin treatment, the researchers saw that cisplatin remained in the mouse inner ear much longer than in most other body tissues, and the drug builds up with each successive treatment.
The team also studied inner ear tissue donated by deceased adults who had been treated with cisplatin and found the drug is retained in the inner ear months or years after treatment.
When the researchers examined inner ear tissue from a child, they found cisplatin buildup that was even higher than that seen in adults.
Taken together, these results suggest the inner ear readily takes up cisplatin but has limited ability to remove the drug.
In mice and human tissues, the researchers saw the highest buildup of cisplatin in a part of the inner ear called the stria vascularis, which helps maintain the positive electrical charge in inner ear fluid that certain cells need to detect sound.
The team found the accumulation of cisplatin in the stria vascularis contributed to cisplatin-related hearing loss.
“Our findings suggest that if we can prevent cisplatin from entering the stria vascularis in the inner ear during treatment, we may be able to protect cancer patients from developing cisplatin-induced hearing loss,” Dr Cunningham said.
Researchers have gained new insight into hearing loss caused by cisplatin.
By measuring and mapping cisplatin retention in mouse and human inner ear tissues, the researchers found that cisplatin builds up in the inner ear and can remain there for years.
The team also found that a region in the inner ear called the stria vascularis could be targeted to prevent hearing loss resulting from cisplatin.
Lisa L. Cunningham, PhD, of the National Institute on Deafness and other Communications Disorders (NIDCD) in Bethesda, Maryland, and her colleagues reported these findings in Nature Communications.
The researchers noted that cisplatin can cause permanent hearing loss in 40% to 80% of treated patients. The team’s new findings help explain why.
The researchers found that, in most areas of the body, cisplatin is eliminated within days or weeks of treatment, but, in the inner ear, the drug remains much longer.
The team developed a mouse model that represents cisplatin-induced hearing loss seen in human patients.
By looking at inner ear tissue of mice after the first, second, and third cisplatin treatment, the researchers saw that cisplatin remained in the mouse inner ear much longer than in most other body tissues, and the drug builds up with each successive treatment.
The team also studied inner ear tissue donated by deceased adults who had been treated with cisplatin and found the drug is retained in the inner ear months or years after treatment.
When the researchers examined inner ear tissue from a child, they found cisplatin buildup that was even higher than that seen in adults.
Taken together, these results suggest the inner ear readily takes up cisplatin but has limited ability to remove the drug.
In mice and human tissues, the researchers saw the highest buildup of cisplatin in a part of the inner ear called the stria vascularis, which helps maintain the positive electrical charge in inner ear fluid that certain cells need to detect sound.
The team found the accumulation of cisplatin in the stria vascularis contributed to cisplatin-related hearing loss.
“Our findings suggest that if we can prevent cisplatin from entering the stria vascularis in the inner ear during treatment, we may be able to protect cancer patients from developing cisplatin-induced hearing loss,” Dr Cunningham said.
Drug receives fast track, orphan designations for PTCL
The US Food and Drug Administration (FDA) has granted orphan drug and fast track designations to tenalisib (RP6530) for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib is a dual PI3K delta/gamma inhibitor being developed by Rhizen Pharmaceuticals.
Research has shown that tenalisib inhibits the growth of immortalized cancerous cell lines and primary leukemia/lymphoma cells.
In preclinical studies, tenalisib reprogrammed macrophages from an immunosuppressive M2-like phenotype (pro-tumor) to an inflammatory M1-like state (anti-tumor).
Researchers are currently conducting a phase 1 study of tenalisib in patients with relapsed/refractory PTCL. Results from this study were presented at the 2017 ASH Annual Meeting (abstract 2791*).
The presentation included data on 50 patients—24 with PTCL and 26 with cutaneous T-cell lymphoma (CTCL).
For the PTCL patients, the median age was 63 (range, 40-89), and 67% were male. The median number of prior therapies was 3 (range, 1-7). All patients had an ECOG status of 0 (n=14) or 1 (n=10). More patients had relapsed disease (n=17, 58%) than refractory disease (n=10, 42%).
For the CTCL patients, the median age was 67 (range, 37-84), and 46% were male. The median number of prior therapies was 5.5 (range, 2-15). All patients had an ECOG status of 0 (n=23) or 1 (n=3). More patients had refractory disease (n=15, 58%) than relapsed disease (n=11, 42%).
In the dose-escalation portion of the study, patients received tenalisib at 200 mg twice daily (BID), 400 mg BID, 800 mg BID fasting, or 800 mg BID fed. The maximum tolerated dose was 800 mg BID fasting, so this dose is being used in the expansion cohort.
Twelve PTCL patients were evaluable for efficacy. The overall response rate in these patients was 58% (7/12), with a 25% complete response rate (3/12).
Sixteen CTCL patients were evaluable for efficacy. The overall response rate was 56% (9/16). All responders had partial responses.
In both PTCL and CTCL patients, treatment-related grade 3 or higher adverse events (AEs) included transaminitis (22%), rash (6%), neutropenia (6%), hypophosphatemia (2%), increased international normalized ratio (2%), diplopia secondary to neuropathy (2%), and sepsis (2%).
Treatment-related serious AEs included sepsis, increased international normalized ratio, diplopia secondary to neuropathy, and pyrexia. Five patients discontinued treatment due to AEs.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available.
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted orphan drug and fast track designations to tenalisib (RP6530) for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib is a dual PI3K delta/gamma inhibitor being developed by Rhizen Pharmaceuticals.
Research has shown that tenalisib inhibits the growth of immortalized cancerous cell lines and primary leukemia/lymphoma cells.
In preclinical studies, tenalisib reprogrammed macrophages from an immunosuppressive M2-like phenotype (pro-tumor) to an inflammatory M1-like state (anti-tumor).
Researchers are currently conducting a phase 1 study of tenalisib in patients with relapsed/refractory PTCL. Results from this study were presented at the 2017 ASH Annual Meeting (abstract 2791*).
The presentation included data on 50 patients—24 with PTCL and 26 with cutaneous T-cell lymphoma (CTCL).
For the PTCL patients, the median age was 63 (range, 40-89), and 67% were male. The median number of prior therapies was 3 (range, 1-7). All patients had an ECOG status of 0 (n=14) or 1 (n=10). More patients had relapsed disease (n=17, 58%) than refractory disease (n=10, 42%).
For the CTCL patients, the median age was 67 (range, 37-84), and 46% were male. The median number of prior therapies was 5.5 (range, 2-15). All patients had an ECOG status of 0 (n=23) or 1 (n=3). More patients had refractory disease (n=15, 58%) than relapsed disease (n=11, 42%).
In the dose-escalation portion of the study, patients received tenalisib at 200 mg twice daily (BID), 400 mg BID, 800 mg BID fasting, or 800 mg BID fed. The maximum tolerated dose was 800 mg BID fasting, so this dose is being used in the expansion cohort.
Twelve PTCL patients were evaluable for efficacy. The overall response rate in these patients was 58% (7/12), with a 25% complete response rate (3/12).
Sixteen CTCL patients were evaluable for efficacy. The overall response rate was 56% (9/16). All responders had partial responses.
In both PTCL and CTCL patients, treatment-related grade 3 or higher adverse events (AEs) included transaminitis (22%), rash (6%), neutropenia (6%), hypophosphatemia (2%), increased international normalized ratio (2%), diplopia secondary to neuropathy (2%), and sepsis (2%).
Treatment-related serious AEs included sepsis, increased international normalized ratio, diplopia secondary to neuropathy, and pyrexia. Five patients discontinued treatment due to AEs.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available.
*Data in the abstract differ from the presentation.
The US Food and Drug Administration (FDA) has granted orphan drug and fast track designations to tenalisib (RP6530) for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib is a dual PI3K delta/gamma inhibitor being developed by Rhizen Pharmaceuticals.
Research has shown that tenalisib inhibits the growth of immortalized cancerous cell lines and primary leukemia/lymphoma cells.
In preclinical studies, tenalisib reprogrammed macrophages from an immunosuppressive M2-like phenotype (pro-tumor) to an inflammatory M1-like state (anti-tumor).
Researchers are currently conducting a phase 1 study of tenalisib in patients with relapsed/refractory PTCL. Results from this study were presented at the 2017 ASH Annual Meeting (abstract 2791*).
The presentation included data on 50 patients—24 with PTCL and 26 with cutaneous T-cell lymphoma (CTCL).
For the PTCL patients, the median age was 63 (range, 40-89), and 67% were male. The median number of prior therapies was 3 (range, 1-7). All patients had an ECOG status of 0 (n=14) or 1 (n=10). More patients had relapsed disease (n=17, 58%) than refractory disease (n=10, 42%).
For the CTCL patients, the median age was 67 (range, 37-84), and 46% were male. The median number of prior therapies was 5.5 (range, 2-15). All patients had an ECOG status of 0 (n=23) or 1 (n=3). More patients had refractory disease (n=15, 58%) than relapsed disease (n=11, 42%).
In the dose-escalation portion of the study, patients received tenalisib at 200 mg twice daily (BID), 400 mg BID, 800 mg BID fasting, or 800 mg BID fed. The maximum tolerated dose was 800 mg BID fasting, so this dose is being used in the expansion cohort.
Twelve PTCL patients were evaluable for efficacy. The overall response rate in these patients was 58% (7/12), with a 25% complete response rate (3/12).
Sixteen CTCL patients were evaluable for efficacy. The overall response rate was 56% (9/16). All responders had partial responses.
In both PTCL and CTCL patients, treatment-related grade 3 or higher adverse events (AEs) included transaminitis (22%), rash (6%), neutropenia (6%), hypophosphatemia (2%), increased international normalized ratio (2%), diplopia secondary to neuropathy (2%), and sepsis (2%).
Treatment-related serious AEs included sepsis, increased international normalized ratio, diplopia secondary to neuropathy, and pyrexia. Five patients discontinued treatment due to AEs.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available.
*Data in the abstract differ from the presentation.