User login
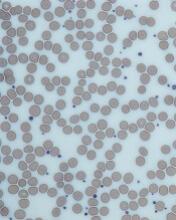
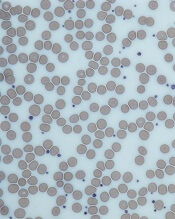
AVP stimulates red blood cell production
Researchers say they have uncovered a new function of arginine vasopressin (AVP).
It seems this hormone does more than maintain fluid balance for the kidneys.
AVP also stimulates the proliferation and differentiation of red blood cell precursors and improves recovery from anemia, according to the researchers.
The group speculates that drugs targeting an AVP receptor could be used to replenish red blood cells lost due to bleeding or treatment toxicity.
Eva Mezey, MD, PhD, of the National Institutes of Health in Bethesda, Maryland, and her colleagues conducted this research and reported the results in Science Translational Medicine.
The team uncovered the unexpected role for AVP by examining clinical data from 92 patients with central diabetes insipidus, a condition that causes AVP deficiency.
Of those individuals, 87% of males and 51% of females had anemia. In comparison, anemia rates in the US general population range from 1.5% to 6% for men and 4.4% to 12% for women.
The researchers also found that all 3 AVP receptors are present on human and murine hematopoietic stem and progenitor cells.
One of these receptors, AVPR1B, plays a predominant role in red blood cell production.
Further experiments revealed that AVP-deficient rats had delayed recovery from anemia, but treatment with AVP or the AVPR1B agonist d(Leu4Lys8)VP was able to speed up anemia recovery in mice.
The researchers tested AVP and the AVPR1B agonist in mouse models of hemorrhage. Compared to vehicle-treated mice, AVP-treated mice had an increase in hematocrit and reticulocyte numbers by day 2. Mice that received d(Leu4Lys8)VP only had an increase in reticulocytes.
The team also tested mice exposed to sublethal irradiation. When the mice received AVP for 2 days, they saw increases in hematocrit and corrected reticulocyte numbers.
The researchers then tested splenectomized mice subjected to hemorrhage. AVP-treated mice had an increase in hematocrit that was similar to that observed in non-splenectomized mice.
Finally, the researchers found that AVP’s effect on hematocrit is independent of erythropoietin. The team said AVP “appears to jump-start peripheral blood cell replenishment,” but later, erythropoietin seems to take over. ![]()
Researchers say they have uncovered a new function of arginine vasopressin (AVP).
It seems this hormone does more than maintain fluid balance for the kidneys.
AVP also stimulates the proliferation and differentiation of red blood cell precursors and improves recovery from anemia, according to the researchers.
The group speculates that drugs targeting an AVP receptor could be used to replenish red blood cells lost due to bleeding or treatment toxicity.
Eva Mezey, MD, PhD, of the National Institutes of Health in Bethesda, Maryland, and her colleagues conducted this research and reported the results in Science Translational Medicine.
The team uncovered the unexpected role for AVP by examining clinical data from 92 patients with central diabetes insipidus, a condition that causes AVP deficiency.
Of those individuals, 87% of males and 51% of females had anemia. In comparison, anemia rates in the US general population range from 1.5% to 6% for men and 4.4% to 12% for women.
The researchers also found that all 3 AVP receptors are present on human and murine hematopoietic stem and progenitor cells.
One of these receptors, AVPR1B, plays a predominant role in red blood cell production.
Further experiments revealed that AVP-deficient rats had delayed recovery from anemia, but treatment with AVP or the AVPR1B agonist d(Leu4Lys8)VP was able to speed up anemia recovery in mice.
The researchers tested AVP and the AVPR1B agonist in mouse models of hemorrhage. Compared to vehicle-treated mice, AVP-treated mice had an increase in hematocrit and reticulocyte numbers by day 2. Mice that received d(Leu4Lys8)VP only had an increase in reticulocytes.
The team also tested mice exposed to sublethal irradiation. When the mice received AVP for 2 days, they saw increases in hematocrit and corrected reticulocyte numbers.
The researchers then tested splenectomized mice subjected to hemorrhage. AVP-treated mice had an increase in hematocrit that was similar to that observed in non-splenectomized mice.
Finally, the researchers found that AVP’s effect on hematocrit is independent of erythropoietin. The team said AVP “appears to jump-start peripheral blood cell replenishment,” but later, erythropoietin seems to take over. ![]()
Researchers say they have uncovered a new function of arginine vasopressin (AVP).
It seems this hormone does more than maintain fluid balance for the kidneys.
AVP also stimulates the proliferation and differentiation of red blood cell precursors and improves recovery from anemia, according to the researchers.
The group speculates that drugs targeting an AVP receptor could be used to replenish red blood cells lost due to bleeding or treatment toxicity.
Eva Mezey, MD, PhD, of the National Institutes of Health in Bethesda, Maryland, and her colleagues conducted this research and reported the results in Science Translational Medicine.
The team uncovered the unexpected role for AVP by examining clinical data from 92 patients with central diabetes insipidus, a condition that causes AVP deficiency.
Of those individuals, 87% of males and 51% of females had anemia. In comparison, anemia rates in the US general population range from 1.5% to 6% for men and 4.4% to 12% for women.
The researchers also found that all 3 AVP receptors are present on human and murine hematopoietic stem and progenitor cells.
One of these receptors, AVPR1B, plays a predominant role in red blood cell production.
Further experiments revealed that AVP-deficient rats had delayed recovery from anemia, but treatment with AVP or the AVPR1B agonist d(Leu4Lys8)VP was able to speed up anemia recovery in mice.
The researchers tested AVP and the AVPR1B agonist in mouse models of hemorrhage. Compared to vehicle-treated mice, AVP-treated mice had an increase in hematocrit and reticulocyte numbers by day 2. Mice that received d(Leu4Lys8)VP only had an increase in reticulocytes.
The team also tested mice exposed to sublethal irradiation. When the mice received AVP for 2 days, they saw increases in hematocrit and corrected reticulocyte numbers.
The researchers then tested splenectomized mice subjected to hemorrhage. AVP-treated mice had an increase in hematocrit that was similar to that observed in non-splenectomized mice.
Finally, the researchers found that AVP’s effect on hematocrit is independent of erythropoietin. The team said AVP “appears to jump-start peripheral blood cell replenishment,” but later, erythropoietin seems to take over. ![]()
Team finds no evidence that gadolinium causes neurologic harm
CHICAGO—There is no evidence to suggest that accumulation of gadolinium in the brain speeds cognitive decline, according to research presented at RSNA 2017, the annual meeting of the Radiological Society of North America.*
Recent studies have revealed that traces of the contrast agent gadolinium can be retained in the brain for years after magnetic resonance imaging (MRI).
Earlier this year, the US Food and Drug Administration recommended cautious use of gadolinium-based contrast agents due to the risk of gadolinium retention in various organs, including the brain.
The European Medicines Agency went a step further, recommending restricting the use of some linear gadolinium agents and suspending the authorization of other agents.
Still, very little is known about the health effects of gadolinium that is retained in the brain.
Robert J. McDonald, MD, PhD, of the Mayo Clinic in Rochester, Minnesota, and his colleagues conducted a study to gain some insight.
The team used the Mayo Clinic Study of Aging (MCSA), the world’s largest prospective population-based cohort on aging, to study the effects of gadolinium exposure on neurologic and neurocognitive function.
All MCSA participants underwent extensive neurologic evaluation and neuropsychological testing at baseline and 15-month follow-up intervals.
The researchers compared neurologic and neurocognitive scores of patients with no history of prior gadolinium exposure and patients who underwent prior MRI with gadolinium-based contrast agents.
The team adjusted their analysis for age, sex, education level, baseline neurocognitive performance, and other factors.
The study included 4261 cognitively normal men and women with a mean age of 72 (range, 50-90). The mean duration of study participation was 3.7 years.
Roughly a quarter of the patients (25.6%, n=1092) had received gadolinium-based contrast agents. These patients received a median of 2 doses (range, 1-28), and the median time since first gadolinium exposure was 5.6 years.
The researchers found that gadolinium exposure was not a significant predictor of cognitive decline, as assessed by changes in clinical dementia rating (P=0.48), Blessed dementia scale (P=0.68), and mental status exam score (P=0.55).
Likewise, gadolinium exposure was not a significant predictor of diminished neuropsychological performance (P=0.13) or diminished motor performance (P=0.43), as assessed by the Unified Parkinson’s Disease Rating Scale.
Finally, gadolinium exposure was not an independent risk factor in the rate of cognitive decline from normal cognitive status to dementia (P=0.91).
“Right now, there is concern over the safety of gadolinium-based contrast agents, particularly relating to gadolinium retention in the brain and other tissues,” Dr McDonald said.
“This study provides useful data that, at the reasonable doses 95% of the population is likely to receive in their lifetime, there is no evidence, at this point, that gadolinium retention in the brain is associated with adverse clinical outcomes.” ![]()
*Abstract SSM16-01: Assessment of the Neurologic Effects of Intracranial Gadolinium Deposition Using a Large Population Based Cohort.
CHICAGO—There is no evidence to suggest that accumulation of gadolinium in the brain speeds cognitive decline, according to research presented at RSNA 2017, the annual meeting of the Radiological Society of North America.*
Recent studies have revealed that traces of the contrast agent gadolinium can be retained in the brain for years after magnetic resonance imaging (MRI).
Earlier this year, the US Food and Drug Administration recommended cautious use of gadolinium-based contrast agents due to the risk of gadolinium retention in various organs, including the brain.
The European Medicines Agency went a step further, recommending restricting the use of some linear gadolinium agents and suspending the authorization of other agents.
Still, very little is known about the health effects of gadolinium that is retained in the brain.
Robert J. McDonald, MD, PhD, of the Mayo Clinic in Rochester, Minnesota, and his colleagues conducted a study to gain some insight.
The team used the Mayo Clinic Study of Aging (MCSA), the world’s largest prospective population-based cohort on aging, to study the effects of gadolinium exposure on neurologic and neurocognitive function.
All MCSA participants underwent extensive neurologic evaluation and neuropsychological testing at baseline and 15-month follow-up intervals.
The researchers compared neurologic and neurocognitive scores of patients with no history of prior gadolinium exposure and patients who underwent prior MRI with gadolinium-based contrast agents.
The team adjusted their analysis for age, sex, education level, baseline neurocognitive performance, and other factors.
The study included 4261 cognitively normal men and women with a mean age of 72 (range, 50-90). The mean duration of study participation was 3.7 years.
Roughly a quarter of the patients (25.6%, n=1092) had received gadolinium-based contrast agents. These patients received a median of 2 doses (range, 1-28), and the median time since first gadolinium exposure was 5.6 years.
The researchers found that gadolinium exposure was not a significant predictor of cognitive decline, as assessed by changes in clinical dementia rating (P=0.48), Blessed dementia scale (P=0.68), and mental status exam score (P=0.55).
Likewise, gadolinium exposure was not a significant predictor of diminished neuropsychological performance (P=0.13) or diminished motor performance (P=0.43), as assessed by the Unified Parkinson’s Disease Rating Scale.
Finally, gadolinium exposure was not an independent risk factor in the rate of cognitive decline from normal cognitive status to dementia (P=0.91).
“Right now, there is concern over the safety of gadolinium-based contrast agents, particularly relating to gadolinium retention in the brain and other tissues,” Dr McDonald said.
“This study provides useful data that, at the reasonable doses 95% of the population is likely to receive in their lifetime, there is no evidence, at this point, that gadolinium retention in the brain is associated with adverse clinical outcomes.” ![]()
*Abstract SSM16-01: Assessment of the Neurologic Effects of Intracranial Gadolinium Deposition Using a Large Population Based Cohort.
CHICAGO—There is no evidence to suggest that accumulation of gadolinium in the brain speeds cognitive decline, according to research presented at RSNA 2017, the annual meeting of the Radiological Society of North America.*
Recent studies have revealed that traces of the contrast agent gadolinium can be retained in the brain for years after magnetic resonance imaging (MRI).
Earlier this year, the US Food and Drug Administration recommended cautious use of gadolinium-based contrast agents due to the risk of gadolinium retention in various organs, including the brain.
The European Medicines Agency went a step further, recommending restricting the use of some linear gadolinium agents and suspending the authorization of other agents.
Still, very little is known about the health effects of gadolinium that is retained in the brain.
Robert J. McDonald, MD, PhD, of the Mayo Clinic in Rochester, Minnesota, and his colleagues conducted a study to gain some insight.
The team used the Mayo Clinic Study of Aging (MCSA), the world’s largest prospective population-based cohort on aging, to study the effects of gadolinium exposure on neurologic and neurocognitive function.
All MCSA participants underwent extensive neurologic evaluation and neuropsychological testing at baseline and 15-month follow-up intervals.
The researchers compared neurologic and neurocognitive scores of patients with no history of prior gadolinium exposure and patients who underwent prior MRI with gadolinium-based contrast agents.
The team adjusted their analysis for age, sex, education level, baseline neurocognitive performance, and other factors.
The study included 4261 cognitively normal men and women with a mean age of 72 (range, 50-90). The mean duration of study participation was 3.7 years.
Roughly a quarter of the patients (25.6%, n=1092) had received gadolinium-based contrast agents. These patients received a median of 2 doses (range, 1-28), and the median time since first gadolinium exposure was 5.6 years.
The researchers found that gadolinium exposure was not a significant predictor of cognitive decline, as assessed by changes in clinical dementia rating (P=0.48), Blessed dementia scale (P=0.68), and mental status exam score (P=0.55).
Likewise, gadolinium exposure was not a significant predictor of diminished neuropsychological performance (P=0.13) or diminished motor performance (P=0.43), as assessed by the Unified Parkinson’s Disease Rating Scale.
Finally, gadolinium exposure was not an independent risk factor in the rate of cognitive decline from normal cognitive status to dementia (P=0.91).
“Right now, there is concern over the safety of gadolinium-based contrast agents, particularly relating to gadolinium retention in the brain and other tissues,” Dr McDonald said.
“This study provides useful data that, at the reasonable doses 95% of the population is likely to receive in their lifetime, there is no evidence, at this point, that gadolinium retention in the brain is associated with adverse clinical outcomes.” ![]()
*Abstract SSM16-01: Assessment of the Neurologic Effects of Intracranial Gadolinium Deposition Using a Large Population Based Cohort.
Study reveals potential target for AML treatment
New research has revealed a potential therapeutic target for acute myeloid leukemia (AML)—the methyl transferase enzyme METTL3.
Researchers found that inhibiting METTL3 destroys human and mouse AML cells without harming non-leukemic blood cells.
The team also discovered why METTL3 is required for AML cell survival by deciphering the mechanism it uses to regulate several other leukemia genes.
The researchers described this work in Nature.
“New treatments for AML are desperately needed, and we have been looking for genes that would be good drug targets,” said study author Tony Kouzarides, PhD, of University of Cambridge in the UK.
“We identified the methyl transferase enzyme METTL3 as a highly viable target against AML. Our study will inspire pharmaceutical efforts to find drugs that specifically inhibit METTL3 to treat AML.”
In their attempt to find therapeutic targets for AML, Dr Kouzarides and his colleagues used CRISPR-Cas9 to screen AML cells for vulnerable points.
The researchers created mouse leukemia cells with mutations in genes that may be targeted in human AML cells and systematically tested each gene, finding which were essential for AML survival.
The team ended up with 46 likely candidate genes, many of which produce proteins that could modify RNA. Among these, METTL3 was one of the genes with the strongest effect.
Experiments revealed that METTL3 was essential for the survival of AML cells, but it was not required for healthy blood cells.
Having found a potential target in METTL3, the researchers investigated how it worked.
They discovered that the protein produced by METTL3 bound to the beginning of 126 different genes, including several required for AML cell survival.
As RNAs were produced, the METTL3 protein added methyl groups to their middle section, something which had not been previously observed. These middle methyl groups increased the ability of the RNAs to be translated into proteins.
The researchers then found that when METTL3 was inhibited, no methyl groups were added to the RNA. This prevented the production of their essential proteins, so the AML cells started dying.
“This study uncovered an entirely new mechanism of gene regulation in AML that operates through modifications of RNA,” said study author Konstantinos Tzelepis, PhD, of Wellcome Trust Sanger Institute in Cambridge, UK.
“We discovered that inhibiting the methyl transferase activity of METTL3 would stop the translation of a whole set of proteins that the leukemia needs. This mechanism shows that a drug to inhibit methylation could be effective against AML without affecting normal cells.” ![]()
New research has revealed a potential therapeutic target for acute myeloid leukemia (AML)—the methyl transferase enzyme METTL3.
Researchers found that inhibiting METTL3 destroys human and mouse AML cells without harming non-leukemic blood cells.
The team also discovered why METTL3 is required for AML cell survival by deciphering the mechanism it uses to regulate several other leukemia genes.
The researchers described this work in Nature.
“New treatments for AML are desperately needed, and we have been looking for genes that would be good drug targets,” said study author Tony Kouzarides, PhD, of University of Cambridge in the UK.
“We identified the methyl transferase enzyme METTL3 as a highly viable target against AML. Our study will inspire pharmaceutical efforts to find drugs that specifically inhibit METTL3 to treat AML.”
In their attempt to find therapeutic targets for AML, Dr Kouzarides and his colleagues used CRISPR-Cas9 to screen AML cells for vulnerable points.
The researchers created mouse leukemia cells with mutations in genes that may be targeted in human AML cells and systematically tested each gene, finding which were essential for AML survival.
The team ended up with 46 likely candidate genes, many of which produce proteins that could modify RNA. Among these, METTL3 was one of the genes with the strongest effect.
Experiments revealed that METTL3 was essential for the survival of AML cells, but it was not required for healthy blood cells.
Having found a potential target in METTL3, the researchers investigated how it worked.
They discovered that the protein produced by METTL3 bound to the beginning of 126 different genes, including several required for AML cell survival.
As RNAs were produced, the METTL3 protein added methyl groups to their middle section, something which had not been previously observed. These middle methyl groups increased the ability of the RNAs to be translated into proteins.
The researchers then found that when METTL3 was inhibited, no methyl groups were added to the RNA. This prevented the production of their essential proteins, so the AML cells started dying.
“This study uncovered an entirely new mechanism of gene regulation in AML that operates through modifications of RNA,” said study author Konstantinos Tzelepis, PhD, of Wellcome Trust Sanger Institute in Cambridge, UK.
“We discovered that inhibiting the methyl transferase activity of METTL3 would stop the translation of a whole set of proteins that the leukemia needs. This mechanism shows that a drug to inhibit methylation could be effective against AML without affecting normal cells.” ![]()
New research has revealed a potential therapeutic target for acute myeloid leukemia (AML)—the methyl transferase enzyme METTL3.
Researchers found that inhibiting METTL3 destroys human and mouse AML cells without harming non-leukemic blood cells.
The team also discovered why METTL3 is required for AML cell survival by deciphering the mechanism it uses to regulate several other leukemia genes.
The researchers described this work in Nature.
“New treatments for AML are desperately needed, and we have been looking for genes that would be good drug targets,” said study author Tony Kouzarides, PhD, of University of Cambridge in the UK.
“We identified the methyl transferase enzyme METTL3 as a highly viable target against AML. Our study will inspire pharmaceutical efforts to find drugs that specifically inhibit METTL3 to treat AML.”
In their attempt to find therapeutic targets for AML, Dr Kouzarides and his colleagues used CRISPR-Cas9 to screen AML cells for vulnerable points.
The researchers created mouse leukemia cells with mutations in genes that may be targeted in human AML cells and systematically tested each gene, finding which were essential for AML survival.
The team ended up with 46 likely candidate genes, many of which produce proteins that could modify RNA. Among these, METTL3 was one of the genes with the strongest effect.
Experiments revealed that METTL3 was essential for the survival of AML cells, but it was not required for healthy blood cells.
Having found a potential target in METTL3, the researchers investigated how it worked.
They discovered that the protein produced by METTL3 bound to the beginning of 126 different genes, including several required for AML cell survival.
As RNAs were produced, the METTL3 protein added methyl groups to their middle section, something which had not been previously observed. These middle methyl groups increased the ability of the RNAs to be translated into proteins.
The researchers then found that when METTL3 was inhibited, no methyl groups were added to the RNA. This prevented the production of their essential proteins, so the AML cells started dying.
“This study uncovered an entirely new mechanism of gene regulation in AML that operates through modifications of RNA,” said study author Konstantinos Tzelepis, PhD, of Wellcome Trust Sanger Institute in Cambridge, UK.
“We discovered that inhibiting the methyl transferase activity of METTL3 would stop the translation of a whole set of proteins that the leukemia needs. This mechanism shows that a drug to inhibit methylation could be effective against AML without affecting normal cells.” ![]()
Inhibitor exhibits activity against range of lymphomas
Preclinical research suggests the dual PI3K/mTOR inhibitor PQR309 has activity against several types of lymphoma and works well in combination with other agents.
PQR309 exhibited anti-lymphoma activity as a single agent and in combination with venetoclax, panobinostat, ibrutinib, lenalidomide, ARV-825, marizomib, and rituximab.
PQR309 demonstrated greater activity against B-cell lymphoma than T-cell lymphoma, and the inhibitor was able to overcome both primary and acquired resistance to idelalisib.
Francesco Bertoni, MD, of the Institute of Oncology Research in Bellinzona, Switzerland, and his colleagues conducted this research and reported the results in Clinical Cancer Research.
The work was funded by PIQUR Therapeutics AG, the company developing PQR309, and some study authors are PIQUR employees.
The researchers tested PQR309 in 49 human lymphoma cell lines—7 activated B-cell-like (ABC) diffuse large B-cell lymphoma (DLBCL), 18 germinal center B-cell (GCB) DLBCL, 10 mantle cell lymphoma (MCL), 3 splenic marginal zone lymphoma (SMZL), 2 chronic lymphocytic leukemia (CLL), 4 Hodgkin lymphoma, and 5 anaplastic large-cell lymphoma (ALCL).
In most cell lines, PQR309 halted proliferation, mainly due to cell-cycle arrest with a block in G1. However, PQR309 induced apoptosis in 2 cell lines tested—SU-DHL-4 and TMD8.
The researchers noted that PQR309 was significantly more active in the B-cell lymphoma cell lines (DLBCL, MCL, CLL, and SMZL) than in the T-cell lymphoma cell line ALCL (P=0.028).
PQR309 exhibited similar activity in ABC and GCB DLBCL cell lines, de novo DLBCL, and DLBCL derived from transformed follicular lymphoma. TP53, MYC, and BCL2 status also had no significant effect on PQR309 activity.
The researchers compared cell lines that were very sensitive to PQR309 to those with low sensitivity to the drug and identified differences.
The team said that transcripts preferentially expressed in PQR309-sensitive cell lines were significantly enriched of genes involved in BCR pathway/signaling and BLIMP1 targets. Transcripts associated with less sensitive cell lines were enriched of members of proteasome pathway, response to unfolded proteins, MYC targets, XBP1 targets, genes downregulated by mTOR inhibitors, and genes involved in oxidative phosphorylation.
PQR309 demonstrated synergistic effects when combined with the BTK inhibitor ibrutinib, the immunomodulatory drug lenalidomide, the anti-CD20 monoclonal antibody rituximab, and the proteasome inhibitor marizomib.
PQR309 demonstrated synergistic or additive effects when combined with the BCL2 inhibitor venetoclax, the HDAC inhibitor panobinostat, and the PROTAC BET inhibitor ARV-825.
In addition, PQR309 was active in lymphoma cell lines with primary and secondary resistance to the PI3K inhibitor idelalisib.
The researchers believe the results of this study, together with ongoing clinical studies of PQR309, can lead to better treatments for lymphoma patients and better understanding of the mechanisms of anti-lymphoma agents. ![]()
Preclinical research suggests the dual PI3K/mTOR inhibitor PQR309 has activity against several types of lymphoma and works well in combination with other agents.
PQR309 exhibited anti-lymphoma activity as a single agent and in combination with venetoclax, panobinostat, ibrutinib, lenalidomide, ARV-825, marizomib, and rituximab.
PQR309 demonstrated greater activity against B-cell lymphoma than T-cell lymphoma, and the inhibitor was able to overcome both primary and acquired resistance to idelalisib.
Francesco Bertoni, MD, of the Institute of Oncology Research in Bellinzona, Switzerland, and his colleagues conducted this research and reported the results in Clinical Cancer Research.
The work was funded by PIQUR Therapeutics AG, the company developing PQR309, and some study authors are PIQUR employees.
The researchers tested PQR309 in 49 human lymphoma cell lines—7 activated B-cell-like (ABC) diffuse large B-cell lymphoma (DLBCL), 18 germinal center B-cell (GCB) DLBCL, 10 mantle cell lymphoma (MCL), 3 splenic marginal zone lymphoma (SMZL), 2 chronic lymphocytic leukemia (CLL), 4 Hodgkin lymphoma, and 5 anaplastic large-cell lymphoma (ALCL).
In most cell lines, PQR309 halted proliferation, mainly due to cell-cycle arrest with a block in G1. However, PQR309 induced apoptosis in 2 cell lines tested—SU-DHL-4 and TMD8.
The researchers noted that PQR309 was significantly more active in the B-cell lymphoma cell lines (DLBCL, MCL, CLL, and SMZL) than in the T-cell lymphoma cell line ALCL (P=0.028).
PQR309 exhibited similar activity in ABC and GCB DLBCL cell lines, de novo DLBCL, and DLBCL derived from transformed follicular lymphoma. TP53, MYC, and BCL2 status also had no significant effect on PQR309 activity.
The researchers compared cell lines that were very sensitive to PQR309 to those with low sensitivity to the drug and identified differences.
The team said that transcripts preferentially expressed in PQR309-sensitive cell lines were significantly enriched of genes involved in BCR pathway/signaling and BLIMP1 targets. Transcripts associated with less sensitive cell lines were enriched of members of proteasome pathway, response to unfolded proteins, MYC targets, XBP1 targets, genes downregulated by mTOR inhibitors, and genes involved in oxidative phosphorylation.
PQR309 demonstrated synergistic effects when combined with the BTK inhibitor ibrutinib, the immunomodulatory drug lenalidomide, the anti-CD20 monoclonal antibody rituximab, and the proteasome inhibitor marizomib.
PQR309 demonstrated synergistic or additive effects when combined with the BCL2 inhibitor venetoclax, the HDAC inhibitor panobinostat, and the PROTAC BET inhibitor ARV-825.
In addition, PQR309 was active in lymphoma cell lines with primary and secondary resistance to the PI3K inhibitor idelalisib.
The researchers believe the results of this study, together with ongoing clinical studies of PQR309, can lead to better treatments for lymphoma patients and better understanding of the mechanisms of anti-lymphoma agents. ![]()
Preclinical research suggests the dual PI3K/mTOR inhibitor PQR309 has activity against several types of lymphoma and works well in combination with other agents.
PQR309 exhibited anti-lymphoma activity as a single agent and in combination with venetoclax, panobinostat, ibrutinib, lenalidomide, ARV-825, marizomib, and rituximab.
PQR309 demonstrated greater activity against B-cell lymphoma than T-cell lymphoma, and the inhibitor was able to overcome both primary and acquired resistance to idelalisib.
Francesco Bertoni, MD, of the Institute of Oncology Research in Bellinzona, Switzerland, and his colleagues conducted this research and reported the results in Clinical Cancer Research.
The work was funded by PIQUR Therapeutics AG, the company developing PQR309, and some study authors are PIQUR employees.
The researchers tested PQR309 in 49 human lymphoma cell lines—7 activated B-cell-like (ABC) diffuse large B-cell lymphoma (DLBCL), 18 germinal center B-cell (GCB) DLBCL, 10 mantle cell lymphoma (MCL), 3 splenic marginal zone lymphoma (SMZL), 2 chronic lymphocytic leukemia (CLL), 4 Hodgkin lymphoma, and 5 anaplastic large-cell lymphoma (ALCL).
In most cell lines, PQR309 halted proliferation, mainly due to cell-cycle arrest with a block in G1. However, PQR309 induced apoptosis in 2 cell lines tested—SU-DHL-4 and TMD8.
The researchers noted that PQR309 was significantly more active in the B-cell lymphoma cell lines (DLBCL, MCL, CLL, and SMZL) than in the T-cell lymphoma cell line ALCL (P=0.028).
PQR309 exhibited similar activity in ABC and GCB DLBCL cell lines, de novo DLBCL, and DLBCL derived from transformed follicular lymphoma. TP53, MYC, and BCL2 status also had no significant effect on PQR309 activity.
The researchers compared cell lines that were very sensitive to PQR309 to those with low sensitivity to the drug and identified differences.
The team said that transcripts preferentially expressed in PQR309-sensitive cell lines were significantly enriched of genes involved in BCR pathway/signaling and BLIMP1 targets. Transcripts associated with less sensitive cell lines were enriched of members of proteasome pathway, response to unfolded proteins, MYC targets, XBP1 targets, genes downregulated by mTOR inhibitors, and genes involved in oxidative phosphorylation.
PQR309 demonstrated synergistic effects when combined with the BTK inhibitor ibrutinib, the immunomodulatory drug lenalidomide, the anti-CD20 monoclonal antibody rituximab, and the proteasome inhibitor marizomib.
PQR309 demonstrated synergistic or additive effects when combined with the BCL2 inhibitor venetoclax, the HDAC inhibitor panobinostat, and the PROTAC BET inhibitor ARV-825.
In addition, PQR309 was active in lymphoma cell lines with primary and secondary resistance to the PI3K inhibitor idelalisib.
The researchers believe the results of this study, together with ongoing clinical studies of PQR309, can lead to better treatments for lymphoma patients and better understanding of the mechanisms of anti-lymphoma agents. ![]()
FDA grants drug orphan designation for AML, MDS
The US Food and Drug Administration (FDA) has granted orphan drug designation to AMV564, a CD33/CD3 bispecific antibody, for the treatment of acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
AMV564 is a T-cell engager, derived from human protein sequences, that binds both CD33 and CD3 to mediate T-cell directed lysis of CD33-positive cancer cells.
Amphivena Therapeutics Inc., is currently conducting a phase 1 trial of AMV564 in relapsed or refractory AML. The company plans to launch a phase 1 trial in patients with MDS in early 2018.
According to Amphivena, AMV564 has demonstrated “potent activity” in AML patient samples, and that activity was independent of CD33 expression level, disease stage, and cytogenetic risk.
AMV564 also eliminated nearly all blasts from the bone marrow and spleen in a stringent AML patient-derived xenograft murine model.
In addition, Amphivena established a therapeutic window for AMV564 in cynomolgus monkeys, with rapid and sustained elimination of CD33-expressing cells during AMV564 dosing and rapid hematopoietic recovery following dosing.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to AMV564, a CD33/CD3 bispecific antibody, for the treatment of acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
AMV564 is a T-cell engager, derived from human protein sequences, that binds both CD33 and CD3 to mediate T-cell directed lysis of CD33-positive cancer cells.
Amphivena Therapeutics Inc., is currently conducting a phase 1 trial of AMV564 in relapsed or refractory AML. The company plans to launch a phase 1 trial in patients with MDS in early 2018.
According to Amphivena, AMV564 has demonstrated “potent activity” in AML patient samples, and that activity was independent of CD33 expression level, disease stage, and cytogenetic risk.
AMV564 also eliminated nearly all blasts from the bone marrow and spleen in a stringent AML patient-derived xenograft murine model.
In addition, Amphivena established a therapeutic window for AMV564 in cynomolgus monkeys, with rapid and sustained elimination of CD33-expressing cells during AMV564 dosing and rapid hematopoietic recovery following dosing.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to AMV564, a CD33/CD3 bispecific antibody, for the treatment of acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
AMV564 is a T-cell engager, derived from human protein sequences, that binds both CD33 and CD3 to mediate T-cell directed lysis of CD33-positive cancer cells.
Amphivena Therapeutics Inc., is currently conducting a phase 1 trial of AMV564 in relapsed or refractory AML. The company plans to launch a phase 1 trial in patients with MDS in early 2018.
According to Amphivena, AMV564 has demonstrated “potent activity” in AML patient samples, and that activity was independent of CD33 expression level, disease stage, and cytogenetic risk.
AMV564 also eliminated nearly all blasts from the bone marrow and spleen in a stringent AML patient-derived xenograft murine model.
In addition, Amphivena established a therapeutic window for AMV564 in cynomolgus monkeys, with rapid and sustained elimination of CD33-expressing cells during AMV564 dosing and rapid hematopoietic recovery following dosing.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
Group develops MM-specific CAR T-cell therapy
Researchers say they have identified a multiple myeloma (MM)-specific target for chimeric antigen receptor (CAR) T-cell therapy.
The team unearthed an MM-specific monoclonal antibody (mAb) and designed a CAR that incorporates a fragment derived from that mAb.
The resulting CAR T-cell therapy exhibited anti-MM activity in vitro and in vivo but did not have a negative effect on normal hematopoietic cells.
The researchers described this work in Nature Medicine.
The team believed that new antigen epitopes could be discovered by thoroughly searching for cancer-specific mAbs and characterizing the antigens they recognize.
“We applied this strategy to identify novel therapeutic targets for multiple myeloma . . . ,” explained study author Naoki Hosen, MD, PhD, of Osaka University in Osaka, Japan.
The researchers screened more than 10,000 anti-MM mAb clones and identified MMG49 as an MM-specific mAb that recognizes a subset of integrin β7 molecules.
The team found that MMG49 reacted to MM cells—but not to normal hematopoietic cells—in MM patient samples.
This prompted the researchers to design a CAR that incorporates a fragment derived from MMG49.
When tested in vitro, MMG49 CAR T cells exhibited cytotoxic activity against cell lines expressing the MMG49 epitope and primary MM cell from patients’ bone marrow. However, MMG49 CAR T cells did not have cytotoxic effects on MMG49-negative cells or normal hematopoietic cells.
The researchers said MM cells were completely eradicated by MMG49 CAR T cells. But the therapy did not kill T cells, even when integrin β7 was activated by MAdCAM-1 and CXCL12.
In mouse models of MM, MMG49 CAR T cells significantly prolonged survival when compared to a CD19 CAR T-cell therapy. MMG49 CAR T cells eradicated MM cells and significantly decreased tumor burden in some mice, but some mice relapsed.
MMG49 CAR T cells did not affect normal hematopoietic cells in the mice, and the researchers said there were no unexpected side effects with the treatment.
“Our results also demonstrate that the active conformer of integrin β7 can serve as an immunotherapeutic target against MM, even though the expression of the protein itself is not specific to MM,” said study author Yukiko Matsunaga, PhD, of Princess Margaret Cancer Centre, University Health Network, in Toronto, Canada.
“Therefore, it’s highly plausible that there are other cancer immunotherapeutic targets that have yet to be identified in many cell-surface proteins that undergo conformational changes, even if the expression of the proteins themselves is not cancer-specific.” ![]()
Researchers say they have identified a multiple myeloma (MM)-specific target for chimeric antigen receptor (CAR) T-cell therapy.
The team unearthed an MM-specific monoclonal antibody (mAb) and designed a CAR that incorporates a fragment derived from that mAb.
The resulting CAR T-cell therapy exhibited anti-MM activity in vitro and in vivo but did not have a negative effect on normal hematopoietic cells.
The researchers described this work in Nature Medicine.
The team believed that new antigen epitopes could be discovered by thoroughly searching for cancer-specific mAbs and characterizing the antigens they recognize.
“We applied this strategy to identify novel therapeutic targets for multiple myeloma . . . ,” explained study author Naoki Hosen, MD, PhD, of Osaka University in Osaka, Japan.
The researchers screened more than 10,000 anti-MM mAb clones and identified MMG49 as an MM-specific mAb that recognizes a subset of integrin β7 molecules.
The team found that MMG49 reacted to MM cells—but not to normal hematopoietic cells—in MM patient samples.
This prompted the researchers to design a CAR that incorporates a fragment derived from MMG49.
When tested in vitro, MMG49 CAR T cells exhibited cytotoxic activity against cell lines expressing the MMG49 epitope and primary MM cell from patients’ bone marrow. However, MMG49 CAR T cells did not have cytotoxic effects on MMG49-negative cells or normal hematopoietic cells.
The researchers said MM cells were completely eradicated by MMG49 CAR T cells. But the therapy did not kill T cells, even when integrin β7 was activated by MAdCAM-1 and CXCL12.
In mouse models of MM, MMG49 CAR T cells significantly prolonged survival when compared to a CD19 CAR T-cell therapy. MMG49 CAR T cells eradicated MM cells and significantly decreased tumor burden in some mice, but some mice relapsed.
MMG49 CAR T cells did not affect normal hematopoietic cells in the mice, and the researchers said there were no unexpected side effects with the treatment.
“Our results also demonstrate that the active conformer of integrin β7 can serve as an immunotherapeutic target against MM, even though the expression of the protein itself is not specific to MM,” said study author Yukiko Matsunaga, PhD, of Princess Margaret Cancer Centre, University Health Network, in Toronto, Canada.
“Therefore, it’s highly plausible that there are other cancer immunotherapeutic targets that have yet to be identified in many cell-surface proteins that undergo conformational changes, even if the expression of the proteins themselves is not cancer-specific.” ![]()
Researchers say they have identified a multiple myeloma (MM)-specific target for chimeric antigen receptor (CAR) T-cell therapy.
The team unearthed an MM-specific monoclonal antibody (mAb) and designed a CAR that incorporates a fragment derived from that mAb.
The resulting CAR T-cell therapy exhibited anti-MM activity in vitro and in vivo but did not have a negative effect on normal hematopoietic cells.
The researchers described this work in Nature Medicine.
The team believed that new antigen epitopes could be discovered by thoroughly searching for cancer-specific mAbs and characterizing the antigens they recognize.
“We applied this strategy to identify novel therapeutic targets for multiple myeloma . . . ,” explained study author Naoki Hosen, MD, PhD, of Osaka University in Osaka, Japan.
The researchers screened more than 10,000 anti-MM mAb clones and identified MMG49 as an MM-specific mAb that recognizes a subset of integrin β7 molecules.
The team found that MMG49 reacted to MM cells—but not to normal hematopoietic cells—in MM patient samples.
This prompted the researchers to design a CAR that incorporates a fragment derived from MMG49.
When tested in vitro, MMG49 CAR T cells exhibited cytotoxic activity against cell lines expressing the MMG49 epitope and primary MM cell from patients’ bone marrow. However, MMG49 CAR T cells did not have cytotoxic effects on MMG49-negative cells or normal hematopoietic cells.
The researchers said MM cells were completely eradicated by MMG49 CAR T cells. But the therapy did not kill T cells, even when integrin β7 was activated by MAdCAM-1 and CXCL12.
In mouse models of MM, MMG49 CAR T cells significantly prolonged survival when compared to a CD19 CAR T-cell therapy. MMG49 CAR T cells eradicated MM cells and significantly decreased tumor burden in some mice, but some mice relapsed.
MMG49 CAR T cells did not affect normal hematopoietic cells in the mice, and the researchers said there were no unexpected side effects with the treatment.
“Our results also demonstrate that the active conformer of integrin β7 can serve as an immunotherapeutic target against MM, even though the expression of the protein itself is not specific to MM,” said study author Yukiko Matsunaga, PhD, of Princess Margaret Cancer Centre, University Health Network, in Toronto, Canada.
“Therefore, it’s highly plausible that there are other cancer immunotherapeutic targets that have yet to be identified in many cell-surface proteins that undergo conformational changes, even if the expression of the proteins themselves is not cancer-specific.” ![]()
Mogamulizumab BLA receives priority review
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for mogamulizumab.
Mogamulizumab is a humanized monoclonal antibody directed against CCR4 that is being developed by Kyowa Hakko Kirin Co., Ltd.
The company is seeking FDA approval for mogamulizumab as a treatment for patients with cutaneous T-cell lymphoma (CTCL) who have received at least 1 prior systemic therapy.
The FDA expects to make a decision on the BLA by June 4, 2018.
The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The BLA for mogamulizumab is supported by data from the MAVORIC study, the largest global randomized clinical trial of systemic therapy in CTCL.
MAVORIC is a phase 3 trial in which researchers evaluated mogamulizumab and an active comparator in 372 patients with CTCL who had failed at least 1 prior systemic treatment. The study was conducted in the US, Europe, Japan, and Australia.
Results from this trial are scheduled to be presented at the 2017 ASH Annual Meeting (abstract 817).
The FDA previously granted mogamulizumab breakthrough therapy designation as a treatment for CTCL patients who have received at least 1 prior systemic therapy.
Breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions. The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for mogamulizumab.
Mogamulizumab is a humanized monoclonal antibody directed against CCR4 that is being developed by Kyowa Hakko Kirin Co., Ltd.
The company is seeking FDA approval for mogamulizumab as a treatment for patients with cutaneous T-cell lymphoma (CTCL) who have received at least 1 prior systemic therapy.
The FDA expects to make a decision on the BLA by June 4, 2018.
The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The BLA for mogamulizumab is supported by data from the MAVORIC study, the largest global randomized clinical trial of systemic therapy in CTCL.
MAVORIC is a phase 3 trial in which researchers evaluated mogamulizumab and an active comparator in 372 patients with CTCL who had failed at least 1 prior systemic treatment. The study was conducted in the US, Europe, Japan, and Australia.
Results from this trial are scheduled to be presented at the 2017 ASH Annual Meeting (abstract 817).
The FDA previously granted mogamulizumab breakthrough therapy designation as a treatment for CTCL patients who have received at least 1 prior systemic therapy.
Breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions. The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for mogamulizumab.
Mogamulizumab is a humanized monoclonal antibody directed against CCR4 that is being developed by Kyowa Hakko Kirin Co., Ltd.
The company is seeking FDA approval for mogamulizumab as a treatment for patients with cutaneous T-cell lymphoma (CTCL) who have received at least 1 prior systemic therapy.
The FDA expects to make a decision on the BLA by June 4, 2018.
The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The BLA for mogamulizumab is supported by data from the MAVORIC study, the largest global randomized clinical trial of systemic therapy in CTCL.
MAVORIC is a phase 3 trial in which researchers evaluated mogamulizumab and an active comparator in 372 patients with CTCL who had failed at least 1 prior systemic treatment. The study was conducted in the US, Europe, Japan, and Australia.
Results from this trial are scheduled to be presented at the 2017 ASH Annual Meeting (abstract 817).
The FDA previously granted mogamulizumab breakthrough therapy designation as a treatment for CTCL patients who have received at least 1 prior systemic therapy.
Breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions. The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
FDA grants priority review to NDA for avatrombopag
The US Food and Drug Administration (FDA) has granted priority review to the new drug application (NDA) for avatrombopag.
Avatrombopag is a second-generation thrombopoietin receptor agonist that is intended to address the limitations of existing treatments for thrombocytopenia.
With this NDA, Dova Pharmaceuticals, Inc., is seeking approval of avatrombopag for the treatment of thrombocytopenia in patients with chronic liver disease who are scheduled to undergo a procedure.
The FDA expects to make a decision on the NDA by May 21, 2018.
The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Phase 3 trials
The NDA submission for avatrombopag is supported by 2 identically designed phase 3 trials, ADAPT 1 and ADAPT 2. Results from these trials were presented at the 2017 American Association for the Study of Liver Disease (AASLD) Meeting last month (abstract 217).
The studies randomized 435 patients with thrombocytopenia and chronic liver disease who were scheduled to undergo a procedure.
Patients with low baseline platelet counts (<40x 109/L) were randomized to receive 60 mg of avatrombopag or placebo daily for 5 days.
Patients with higher baseline platelet counts (40 to <50 x 109/L) were randomized to receive 40 mg of avatrombopag or placebo daily for 5 days.
Patients underwent their procedures 5 to 8 days after their last dose of avatrombopag.
In ADAPT-1, 85 patients completed treatment with avatrombopag at 60 mg, 55 completed treatment with avatrombopag at 40 mg, and 78 controls completed the study.
In ADAPT-2, 68 patients completed treatment with avatrombopag at 60 mg, 55 completed treatment with avatrombopag at 40 mg, and 68 controls completed the study.
Efficacy
The primary efficacy endpoint of these trials was the proportion of patients who did not require any bleeding rescue up to 7 days post-procedure. Bleeding rescue included platelet transfusion, fresh frozen plasma, cryoprecipitate, vitamin K (phytonadione), desmopressin, recombinant activated factor VII, aminocaproicacid, tranexamic acid, whole blood transfusion, packed red cell transfusion, surgical intervention, or interventional radiology.
In ADAPT-1, the primary endpoint was achieved by 66% of patients who received avatrombopag at 60 mg and 23% of those who received placebo in the low-platelet-count cohort (P<0.0001). The endpoint was also achieved by 88% of patients who received avatrombopag at 40 mg and 38% of controls in the higher-platelet-count cohort (P<0.0001).
In ADAPT-2, the primary endpoint was achieved by 69% of patients who received avatrombopag at 60 mg and 35% of those who received placebo in the low-platelet-count cohort (P<0.0006). The endpoint was also achieved by 88% of patients who received avatrombopag at 40 mg and 33% of controls in the higher- platelet-count cohort (P<0.0001).
A secondary efficacy endpoint was the proportion of patients achieving the target platelet count (≥50 x 109/L).
In ADAPT-1, this endpoint was met by 69% of patients who received avatrombopag at 60 mg and 4% of controls in the low-platelet-count cohort (P<0.0001). It was also met by 88% of patients who received avatrombopag at 40 mg and 21% of controls in the higher-platelet-count cohort (P<0.0001)
In ADAPT-2, this endpoint was met by 67% of patients who received avatrombopag at 60 mg and 7% of controls in the low-platelet-count cohort (P<0.0001). It was also met by 93% of patients who received avatrombopag at 40 mg and 39% of controls in the higher-platelet-count cohort (P<0.0001).
Safety
The researchers pooled safety data from the 2 trials.
Treatment-emergent adverse events (AEs) occurred in 58.2% of controls and 56% of avatrombopag-treated patients in the low-platelet-count cohort (60 mg). Treatment-emergent AEs also occurred in 50.8% of controls and 51.3% of avatrombopag-treated patients in the higher-platelet-count cohort (40 mg).
The most frequently reported treatment-emergent AEs were pyrexia, abdominal pain, nausea, headache, diarrhea, and fatigue.
One patient experienced partial portal vein thrombosis that was considered non-serious and potentially related to avatrombopag.
Treatment-related AEs occurred in 17.6% of controls and 11.3% of avatrombopag-treated patients in the low-platelet-count cohort. Treatment-related AEs also occurred in 6.2% of controls and 7% of avatrombopag-treated patients in the higher-platelet-count cohort.
Serious AEs occurred in 13.2%, 6.9%, 3.1%, and 7.8%, respectively.
There were 3 deaths—2 in the 40 mg avatrombopag arm in ADAPT-1 and 1 in the control group in ADAPT-2. None of the deaths was considered treatment-related.
Future directions
Dova Pharmaceuticals, Inc., is planning to explore the potential use of avatrombopag in a broader population of patients with thrombocytopenia. This includes patients undergoing surgical procedures associated with a high risk of bleeding and patients who develop thrombocytopenia after receiving chemotherapy.
In addition, the company is exploring a potential regulatory approval pathway for avatrombopag for the treatment of adults with chronic immune thrombocytopenic purpura based on results from a completed phase 3 trial in this patient population.
The US Food and Drug Administration (FDA) has granted priority review to the new drug application (NDA) for avatrombopag.
Avatrombopag is a second-generation thrombopoietin receptor agonist that is intended to address the limitations of existing treatments for thrombocytopenia.
With this NDA, Dova Pharmaceuticals, Inc., is seeking approval of avatrombopag for the treatment of thrombocytopenia in patients with chronic liver disease who are scheduled to undergo a procedure.
The FDA expects to make a decision on the NDA by May 21, 2018.
The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Phase 3 trials
The NDA submission for avatrombopag is supported by 2 identically designed phase 3 trials, ADAPT 1 and ADAPT 2. Results from these trials were presented at the 2017 American Association for the Study of Liver Disease (AASLD) Meeting last month (abstract 217).
The studies randomized 435 patients with thrombocytopenia and chronic liver disease who were scheduled to undergo a procedure.
Patients with low baseline platelet counts (<40x 109/L) were randomized to receive 60 mg of avatrombopag or placebo daily for 5 days.
Patients with higher baseline platelet counts (40 to <50 x 109/L) were randomized to receive 40 mg of avatrombopag or placebo daily for 5 days.
Patients underwent their procedures 5 to 8 days after their last dose of avatrombopag.
In ADAPT-1, 85 patients completed treatment with avatrombopag at 60 mg, 55 completed treatment with avatrombopag at 40 mg, and 78 controls completed the study.
In ADAPT-2, 68 patients completed treatment with avatrombopag at 60 mg, 55 completed treatment with avatrombopag at 40 mg, and 68 controls completed the study.
Efficacy
The primary efficacy endpoint of these trials was the proportion of patients who did not require any bleeding rescue up to 7 days post-procedure. Bleeding rescue included platelet transfusion, fresh frozen plasma, cryoprecipitate, vitamin K (phytonadione), desmopressin, recombinant activated factor VII, aminocaproicacid, tranexamic acid, whole blood transfusion, packed red cell transfusion, surgical intervention, or interventional radiology.
In ADAPT-1, the primary endpoint was achieved by 66% of patients who received avatrombopag at 60 mg and 23% of those who received placebo in the low-platelet-count cohort (P<0.0001). The endpoint was also achieved by 88% of patients who received avatrombopag at 40 mg and 38% of controls in the higher-platelet-count cohort (P<0.0001).
In ADAPT-2, the primary endpoint was achieved by 69% of patients who received avatrombopag at 60 mg and 35% of those who received placebo in the low-platelet-count cohort (P<0.0006). The endpoint was also achieved by 88% of patients who received avatrombopag at 40 mg and 33% of controls in the higher- platelet-count cohort (P<0.0001).
A secondary efficacy endpoint was the proportion of patients achieving the target platelet count (≥50 x 109/L).
In ADAPT-1, this endpoint was met by 69% of patients who received avatrombopag at 60 mg and 4% of controls in the low-platelet-count cohort (P<0.0001). It was also met by 88% of patients who received avatrombopag at 40 mg and 21% of controls in the higher-platelet-count cohort (P<0.0001)
In ADAPT-2, this endpoint was met by 67% of patients who received avatrombopag at 60 mg and 7% of controls in the low-platelet-count cohort (P<0.0001). It was also met by 93% of patients who received avatrombopag at 40 mg and 39% of controls in the higher-platelet-count cohort (P<0.0001).
Safety
The researchers pooled safety data from the 2 trials.
Treatment-emergent adverse events (AEs) occurred in 58.2% of controls and 56% of avatrombopag-treated patients in the low-platelet-count cohort (60 mg). Treatment-emergent AEs also occurred in 50.8% of controls and 51.3% of avatrombopag-treated patients in the higher-platelet-count cohort (40 mg).
The most frequently reported treatment-emergent AEs were pyrexia, abdominal pain, nausea, headache, diarrhea, and fatigue.
One patient experienced partial portal vein thrombosis that was considered non-serious and potentially related to avatrombopag.
Treatment-related AEs occurred in 17.6% of controls and 11.3% of avatrombopag-treated patients in the low-platelet-count cohort. Treatment-related AEs also occurred in 6.2% of controls and 7% of avatrombopag-treated patients in the higher-platelet-count cohort.
Serious AEs occurred in 13.2%, 6.9%, 3.1%, and 7.8%, respectively.
There were 3 deaths—2 in the 40 mg avatrombopag arm in ADAPT-1 and 1 in the control group in ADAPT-2. None of the deaths was considered treatment-related.
Future directions
Dova Pharmaceuticals, Inc., is planning to explore the potential use of avatrombopag in a broader population of patients with thrombocytopenia. This includes patients undergoing surgical procedures associated with a high risk of bleeding and patients who develop thrombocytopenia after receiving chemotherapy.
In addition, the company is exploring a potential regulatory approval pathway for avatrombopag for the treatment of adults with chronic immune thrombocytopenic purpura based on results from a completed phase 3 trial in this patient population.
The US Food and Drug Administration (FDA) has granted priority review to the new drug application (NDA) for avatrombopag.
Avatrombopag is a second-generation thrombopoietin receptor agonist that is intended to address the limitations of existing treatments for thrombocytopenia.
With this NDA, Dova Pharmaceuticals, Inc., is seeking approval of avatrombopag for the treatment of thrombocytopenia in patients with chronic liver disease who are scheduled to undergo a procedure.
The FDA expects to make a decision on the NDA by May 21, 2018.
The FDA’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Phase 3 trials
The NDA submission for avatrombopag is supported by 2 identically designed phase 3 trials, ADAPT 1 and ADAPT 2. Results from these trials were presented at the 2017 American Association for the Study of Liver Disease (AASLD) Meeting last month (abstract 217).
The studies randomized 435 patients with thrombocytopenia and chronic liver disease who were scheduled to undergo a procedure.
Patients with low baseline platelet counts (<40x 109/L) were randomized to receive 60 mg of avatrombopag or placebo daily for 5 days.
Patients with higher baseline platelet counts (40 to <50 x 109/L) were randomized to receive 40 mg of avatrombopag or placebo daily for 5 days.
Patients underwent their procedures 5 to 8 days after their last dose of avatrombopag.
In ADAPT-1, 85 patients completed treatment with avatrombopag at 60 mg, 55 completed treatment with avatrombopag at 40 mg, and 78 controls completed the study.
In ADAPT-2, 68 patients completed treatment with avatrombopag at 60 mg, 55 completed treatment with avatrombopag at 40 mg, and 68 controls completed the study.
Efficacy
The primary efficacy endpoint of these trials was the proportion of patients who did not require any bleeding rescue up to 7 days post-procedure. Bleeding rescue included platelet transfusion, fresh frozen plasma, cryoprecipitate, vitamin K (phytonadione), desmopressin, recombinant activated factor VII, aminocaproicacid, tranexamic acid, whole blood transfusion, packed red cell transfusion, surgical intervention, or interventional radiology.
In ADAPT-1, the primary endpoint was achieved by 66% of patients who received avatrombopag at 60 mg and 23% of those who received placebo in the low-platelet-count cohort (P<0.0001). The endpoint was also achieved by 88% of patients who received avatrombopag at 40 mg and 38% of controls in the higher-platelet-count cohort (P<0.0001).
In ADAPT-2, the primary endpoint was achieved by 69% of patients who received avatrombopag at 60 mg and 35% of those who received placebo in the low-platelet-count cohort (P<0.0006). The endpoint was also achieved by 88% of patients who received avatrombopag at 40 mg and 33% of controls in the higher- platelet-count cohort (P<0.0001).
A secondary efficacy endpoint was the proportion of patients achieving the target platelet count (≥50 x 109/L).
In ADAPT-1, this endpoint was met by 69% of patients who received avatrombopag at 60 mg and 4% of controls in the low-platelet-count cohort (P<0.0001). It was also met by 88% of patients who received avatrombopag at 40 mg and 21% of controls in the higher-platelet-count cohort (P<0.0001)
In ADAPT-2, this endpoint was met by 67% of patients who received avatrombopag at 60 mg and 7% of controls in the low-platelet-count cohort (P<0.0001). It was also met by 93% of patients who received avatrombopag at 40 mg and 39% of controls in the higher-platelet-count cohort (P<0.0001).
Safety
The researchers pooled safety data from the 2 trials.
Treatment-emergent adverse events (AEs) occurred in 58.2% of controls and 56% of avatrombopag-treated patients in the low-platelet-count cohort (60 mg). Treatment-emergent AEs also occurred in 50.8% of controls and 51.3% of avatrombopag-treated patients in the higher-platelet-count cohort (40 mg).
The most frequently reported treatment-emergent AEs were pyrexia, abdominal pain, nausea, headache, diarrhea, and fatigue.
One patient experienced partial portal vein thrombosis that was considered non-serious and potentially related to avatrombopag.
Treatment-related AEs occurred in 17.6% of controls and 11.3% of avatrombopag-treated patients in the low-platelet-count cohort. Treatment-related AEs also occurred in 6.2% of controls and 7% of avatrombopag-treated patients in the higher-platelet-count cohort.
Serious AEs occurred in 13.2%, 6.9%, 3.1%, and 7.8%, respectively.
There were 3 deaths—2 in the 40 mg avatrombopag arm in ADAPT-1 and 1 in the control group in ADAPT-2. None of the deaths was considered treatment-related.
Future directions
Dova Pharmaceuticals, Inc., is planning to explore the potential use of avatrombopag in a broader population of patients with thrombocytopenia. This includes patients undergoing surgical procedures associated with a high risk of bleeding and patients who develop thrombocytopenia after receiving chemotherapy.
In addition, the company is exploring a potential regulatory approval pathway for avatrombopag for the treatment of adults with chronic immune thrombocytopenic purpura based on results from a completed phase 3 trial in this patient population.
Study reveals predictor of early mortality in AML
New research has shown an increased risk of early death in patients with acute myeloid leukemia (AML) who have high levels of indoleamine 2,3 dioxygenase-1 (IDO-1), an enzyme known to suppress the immune system.
Researchers quantified IDO-1 expression in diagnostic samples from patients with AML and discovered that high levels of IDO-1 were significantly associated with induction failure and poor overall survival (OS).
Ravindra Kolhe, MD, PhD, of the Medical College of Georgia at Augusta University, and his colleagues recounted these findings in Scientific Reports.
The researchers reviewed data from 40 AML patients. They had a median age at diagnosis of 60 (range, 27–89), 60% were female, and 55% were self-reported as Caucasian.
Most patients (72.5%) received standard anthracycline and cytarabine as induction, 10% received hypomethylating agents, and 17.5% were untreated or had unknown treatment status.
Fifteen percent of patients underwent allogeneic hematopoietic stem cell transplant (allo-HSCT) at the time of first complete remission.
Half of all patients achieved remission, and half of those patients (n=10, 25%) had a subsequent relapse. The median OS was 283 days (range, 32–1941). Twenty percent of patients (n=8) were still alive at the time of data analysis.
IDO-1 analysis
“We wanted to look at what makes this leukemia so aggressive that initial induction chemotherapy is not working,” Dr Kolhe said. “Early relapse tends to predict early mortality in these patients, and one of the things we looked at was IDO.”
The researchers extracted IDO-1 mRNA from diagnostic bone marrow samples from 29 of the patients but assessed IDO-1 protein expression in all 40 patients via immunohistochemistry.
The team quantified IDO-1 expression using a “composite IDO-1 score.” They used a cut-off point of 0.45 and divided patients’ samples into 2 groups: high (≥0.45) and low (<0.45) IDO-1 score.
The researchers compared IDO-1 results across 4 survival groups, which included patients surviving:
- Less than 6 months
- More than 6 months to 1 year
- More than 1 year to less than 5 years
- Beyond 5 years.
The team found a direct correlation between poor OS and higher composite IDO-1 score (P=0.0005).
“The patients who died at 6 months had a high expression of IDO, while the blasts produced relatively little IDO in the patients who lived 5 years or more,” Dr Kolhe said.
Independent predictor
The researchers conducted a univariate analysis and identified several factors that were significantly associated with poor OS, including:
- Higher IDO-1 mRNA (P=0.005)
- Higher composite IDO-1 score (P<0.0001)
- Higher age (P=0.0018)
- Male gender (P=0.019)
- High-risk cytogenetics (P=0.002)
- Not undergoing allo-HSCT (P=0.0005).
In a multivariate analysis including the above variables, the researchers found that a higher composite IDO-1 score (P=0.007) and not undergoing allo-HSCT (P=0.007) were significantly associated with poor OS.
The team also found that patients who failed induction had a higher composite IDO-1 score (P=0.01).
“Most of the time, we don’t know why patients are not responding to chemotherapy,” Dr Kolhe noted. “But when the researchers adjusted for other risk factors for AML, like increased age and severe anemia, IDO levels were a standout. Right now, we know it’s high in patients who die at 6 months, and we show that it’s an independent indicator if you adjust for other known variables.”
Dr Kolhe said these results suggest IDO-1 expression should be measured when the diagnostic bone marrow biopsy is performed. This may help identify AML patients who could benefit from receiving an IDO inhibitor along with standard therapy.
Researchers are currently conducting a phase 1/2 trial of the IDO inhibitor indoximod in combination with idarubicin and cytarabine in patients with newly diagnosed AML (NCT02835729).
New research has shown an increased risk of early death in patients with acute myeloid leukemia (AML) who have high levels of indoleamine 2,3 dioxygenase-1 (IDO-1), an enzyme known to suppress the immune system.
Researchers quantified IDO-1 expression in diagnostic samples from patients with AML and discovered that high levels of IDO-1 were significantly associated with induction failure and poor overall survival (OS).
Ravindra Kolhe, MD, PhD, of the Medical College of Georgia at Augusta University, and his colleagues recounted these findings in Scientific Reports.
The researchers reviewed data from 40 AML patients. They had a median age at diagnosis of 60 (range, 27–89), 60% were female, and 55% were self-reported as Caucasian.
Most patients (72.5%) received standard anthracycline and cytarabine as induction, 10% received hypomethylating agents, and 17.5% were untreated or had unknown treatment status.
Fifteen percent of patients underwent allogeneic hematopoietic stem cell transplant (allo-HSCT) at the time of first complete remission.
Half of all patients achieved remission, and half of those patients (n=10, 25%) had a subsequent relapse. The median OS was 283 days (range, 32–1941). Twenty percent of patients (n=8) were still alive at the time of data analysis.
IDO-1 analysis
“We wanted to look at what makes this leukemia so aggressive that initial induction chemotherapy is not working,” Dr Kolhe said. “Early relapse tends to predict early mortality in these patients, and one of the things we looked at was IDO.”
The researchers extracted IDO-1 mRNA from diagnostic bone marrow samples from 29 of the patients but assessed IDO-1 protein expression in all 40 patients via immunohistochemistry.
The team quantified IDO-1 expression using a “composite IDO-1 score.” They used a cut-off point of 0.45 and divided patients’ samples into 2 groups: high (≥0.45) and low (<0.45) IDO-1 score.
The researchers compared IDO-1 results across 4 survival groups, which included patients surviving:
- Less than 6 months
- More than 6 months to 1 year
- More than 1 year to less than 5 years
- Beyond 5 years.
The team found a direct correlation between poor OS and higher composite IDO-1 score (P=0.0005).
“The patients who died at 6 months had a high expression of IDO, while the blasts produced relatively little IDO in the patients who lived 5 years or more,” Dr Kolhe said.
Independent predictor
The researchers conducted a univariate analysis and identified several factors that were significantly associated with poor OS, including:
- Higher IDO-1 mRNA (P=0.005)
- Higher composite IDO-1 score (P<0.0001)
- Higher age (P=0.0018)
- Male gender (P=0.019)
- High-risk cytogenetics (P=0.002)
- Not undergoing allo-HSCT (P=0.0005).
In a multivariate analysis including the above variables, the researchers found that a higher composite IDO-1 score (P=0.007) and not undergoing allo-HSCT (P=0.007) were significantly associated with poor OS.
The team also found that patients who failed induction had a higher composite IDO-1 score (P=0.01).
“Most of the time, we don’t know why patients are not responding to chemotherapy,” Dr Kolhe noted. “But when the researchers adjusted for other risk factors for AML, like increased age and severe anemia, IDO levels were a standout. Right now, we know it’s high in patients who die at 6 months, and we show that it’s an independent indicator if you adjust for other known variables.”
Dr Kolhe said these results suggest IDO-1 expression should be measured when the diagnostic bone marrow biopsy is performed. This may help identify AML patients who could benefit from receiving an IDO inhibitor along with standard therapy.
Researchers are currently conducting a phase 1/2 trial of the IDO inhibitor indoximod in combination with idarubicin and cytarabine in patients with newly diagnosed AML (NCT02835729).
New research has shown an increased risk of early death in patients with acute myeloid leukemia (AML) who have high levels of indoleamine 2,3 dioxygenase-1 (IDO-1), an enzyme known to suppress the immune system.
Researchers quantified IDO-1 expression in diagnostic samples from patients with AML and discovered that high levels of IDO-1 were significantly associated with induction failure and poor overall survival (OS).
Ravindra Kolhe, MD, PhD, of the Medical College of Georgia at Augusta University, and his colleagues recounted these findings in Scientific Reports.
The researchers reviewed data from 40 AML patients. They had a median age at diagnosis of 60 (range, 27–89), 60% were female, and 55% were self-reported as Caucasian.
Most patients (72.5%) received standard anthracycline and cytarabine as induction, 10% received hypomethylating agents, and 17.5% were untreated or had unknown treatment status.
Fifteen percent of patients underwent allogeneic hematopoietic stem cell transplant (allo-HSCT) at the time of first complete remission.
Half of all patients achieved remission, and half of those patients (n=10, 25%) had a subsequent relapse. The median OS was 283 days (range, 32–1941). Twenty percent of patients (n=8) were still alive at the time of data analysis.
IDO-1 analysis
“We wanted to look at what makes this leukemia so aggressive that initial induction chemotherapy is not working,” Dr Kolhe said. “Early relapse tends to predict early mortality in these patients, and one of the things we looked at was IDO.”
The researchers extracted IDO-1 mRNA from diagnostic bone marrow samples from 29 of the patients but assessed IDO-1 protein expression in all 40 patients via immunohistochemistry.
The team quantified IDO-1 expression using a “composite IDO-1 score.” They used a cut-off point of 0.45 and divided patients’ samples into 2 groups: high (≥0.45) and low (<0.45) IDO-1 score.
The researchers compared IDO-1 results across 4 survival groups, which included patients surviving:
- Less than 6 months
- More than 6 months to 1 year
- More than 1 year to less than 5 years
- Beyond 5 years.
The team found a direct correlation between poor OS and higher composite IDO-1 score (P=0.0005).
“The patients who died at 6 months had a high expression of IDO, while the blasts produced relatively little IDO in the patients who lived 5 years or more,” Dr Kolhe said.
Independent predictor
The researchers conducted a univariate analysis and identified several factors that were significantly associated with poor OS, including:
- Higher IDO-1 mRNA (P=0.005)
- Higher composite IDO-1 score (P<0.0001)
- Higher age (P=0.0018)
- Male gender (P=0.019)
- High-risk cytogenetics (P=0.002)
- Not undergoing allo-HSCT (P=0.0005).
In a multivariate analysis including the above variables, the researchers found that a higher composite IDO-1 score (P=0.007) and not undergoing allo-HSCT (P=0.007) were significantly associated with poor OS.
The team also found that patients who failed induction had a higher composite IDO-1 score (P=0.01).
“Most of the time, we don’t know why patients are not responding to chemotherapy,” Dr Kolhe noted. “But when the researchers adjusted for other risk factors for AML, like increased age and severe anemia, IDO levels were a standout. Right now, we know it’s high in patients who die at 6 months, and we show that it’s an independent indicator if you adjust for other known variables.”
Dr Kolhe said these results suggest IDO-1 expression should be measured when the diagnostic bone marrow biopsy is performed. This may help identify AML patients who could benefit from receiving an IDO inhibitor along with standard therapy.
Researchers are currently conducting a phase 1/2 trial of the IDO inhibitor indoximod in combination with idarubicin and cytarabine in patients with newly diagnosed AML (NCT02835729).
Thoughts, emotions linked to opioid use in SCD
Results of a small study suggest that negative thoughts and emotions may increase opioid use in patients with sickle cell disease (SCD).
Researchers analyzed data from daily electronic patient diaries and found that patients were more likely to use short-acting opioids both when they experienced increased pain and “catastrophic” thoughts about that pain.
In fact, pain catastrophizing led to an increased use of short-acting opioids even when patients reported low levels of pain.
In addition, patients were more likely to use long-acting opioids when they experienced negative emotions.
The researchers noted that this study wasn’t designed to show that negative emotions or thinking cause an increase in opioid use. It was only designed to determine if there was an association.
Patrick Finan, PhD, of Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues described this study in The Journal of Pain.
The researchers enrolled 85 adults with SCD in this study. Patients were asked to fill out electronic diaries on a handheld personal computer every evening for 90 days.
The final analysis included only 45 patients, as these were the subjects who filled out the diary more than 25% of the time and had taken opioid pills at least once during the study period.
The patients had an average age of 37, and 71% were female. Most (93%) were African American, and 7% were classified as “other” or did not report their race.
At the start of the study, the patients reported on the dosage and type of opioid pill they were prescribed for long-acting and short-acting use. The daily diary collected data on the number of long-acting and short-acting opioid pills taken per day.
Patients rated their daily pain level on a scale of 0 to 10, with 0 being no pain and 10 being the worst pain imaginable.
Patients also rated positive emotions—including happy, calm, and cheerful—and negative emotions—including lonely, sad, anxious, and tired—on a scale of 0 to 10, with 0 being no emotion and 10 being the most intense emotion. The scores were converted to a 0-to-100 scale for the data analysis.
Separately, the researchers measured negative thinking using a Pain Catastrophizing Scale to rate “rumination,” or focus on pain, helplessness, and magnification of a current pain situation.
Results
Negative emotions were significantly associated with increased levels of long-acting opioids (P=0.001). The opioid dosage increased by 3.4 morphine milligram equivalents for every 10-point increase in negative emotions.
On the other hand, patients’ daily pain level, positive emotions, and negative thinking through catastrophizing did not significantly affect the amount of long-acting opioids taken.
“When someone is prescribed a daily, long-acting opioid, it is typically supposed to be at a fixed dose, and their pain level or emotions shouldn’t dictate whether they take more of this prescription or not,” Dr Finan said.
“Although we can’t prove misuse of the medication in our study, these data suggest that physicians and patients should clearly communicate about how patients should be taking their daily, long-acting opioids in order to minimize the potential for misuse.”
The researchers also found a significant association with short-acting opioid use and daily pain levels (P=0.006) as well as negative thinking by catastrophizing (P<0.001).
For every 10-point increase on the pain scale, the amount of short-acting opioids increased by 1.8 morphine milligram equivalents, and for every 10-point increase on the catastrophizing scale, pain medicine dosage increased by 2.5 morphine milligram equivalents.
Positive and negative emotions had no significant effect on the use of short-acting opioids.
“When pain was reported as low, sickle cell disease patients reported higher opioid use if they catastrophized, or focused their thinking on their pain, than if they didn’t,” Dr Finan said. “When pain levels were higher, negative thinking played less of a role in influencing opioid use.”
Dr Finan cautioned that studies such as this have some weaknesses, including the fact that self-reports are always uncertain, and the study only included 1 time point per day, although a person’s mood may fluctuate throughout the day based on life events and experiences.
For future studies, Dr Finan wants to use smartphone technology that can assess moods randomly throughout the day.
“Once we have a more intensive study to track mood variations throughout the day,” Dr Finan said, “then we can determine when it will be appropriate to send messages through text to intervene and affect patient behavior.”
Results of a small study suggest that negative thoughts and emotions may increase opioid use in patients with sickle cell disease (SCD).
Researchers analyzed data from daily electronic patient diaries and found that patients were more likely to use short-acting opioids both when they experienced increased pain and “catastrophic” thoughts about that pain.
In fact, pain catastrophizing led to an increased use of short-acting opioids even when patients reported low levels of pain.
In addition, patients were more likely to use long-acting opioids when they experienced negative emotions.
The researchers noted that this study wasn’t designed to show that negative emotions or thinking cause an increase in opioid use. It was only designed to determine if there was an association.
Patrick Finan, PhD, of Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues described this study in The Journal of Pain.
The researchers enrolled 85 adults with SCD in this study. Patients were asked to fill out electronic diaries on a handheld personal computer every evening for 90 days.
The final analysis included only 45 patients, as these were the subjects who filled out the diary more than 25% of the time and had taken opioid pills at least once during the study period.
The patients had an average age of 37, and 71% were female. Most (93%) were African American, and 7% were classified as “other” or did not report their race.
At the start of the study, the patients reported on the dosage and type of opioid pill they were prescribed for long-acting and short-acting use. The daily diary collected data on the number of long-acting and short-acting opioid pills taken per day.
Patients rated their daily pain level on a scale of 0 to 10, with 0 being no pain and 10 being the worst pain imaginable.
Patients also rated positive emotions—including happy, calm, and cheerful—and negative emotions—including lonely, sad, anxious, and tired—on a scale of 0 to 10, with 0 being no emotion and 10 being the most intense emotion. The scores were converted to a 0-to-100 scale for the data analysis.
Separately, the researchers measured negative thinking using a Pain Catastrophizing Scale to rate “rumination,” or focus on pain, helplessness, and magnification of a current pain situation.
Results
Negative emotions were significantly associated with increased levels of long-acting opioids (P=0.001). The opioid dosage increased by 3.4 morphine milligram equivalents for every 10-point increase in negative emotions.
On the other hand, patients’ daily pain level, positive emotions, and negative thinking through catastrophizing did not significantly affect the amount of long-acting opioids taken.
“When someone is prescribed a daily, long-acting opioid, it is typically supposed to be at a fixed dose, and their pain level or emotions shouldn’t dictate whether they take more of this prescription or not,” Dr Finan said.
“Although we can’t prove misuse of the medication in our study, these data suggest that physicians and patients should clearly communicate about how patients should be taking their daily, long-acting opioids in order to minimize the potential for misuse.”
The researchers also found a significant association with short-acting opioid use and daily pain levels (P=0.006) as well as negative thinking by catastrophizing (P<0.001).
For every 10-point increase on the pain scale, the amount of short-acting opioids increased by 1.8 morphine milligram equivalents, and for every 10-point increase on the catastrophizing scale, pain medicine dosage increased by 2.5 morphine milligram equivalents.
Positive and negative emotions had no significant effect on the use of short-acting opioids.
“When pain was reported as low, sickle cell disease patients reported higher opioid use if they catastrophized, or focused their thinking on their pain, than if they didn’t,” Dr Finan said. “When pain levels were higher, negative thinking played less of a role in influencing opioid use.”
Dr Finan cautioned that studies such as this have some weaknesses, including the fact that self-reports are always uncertain, and the study only included 1 time point per day, although a person’s mood may fluctuate throughout the day based on life events and experiences.
For future studies, Dr Finan wants to use smartphone technology that can assess moods randomly throughout the day.
“Once we have a more intensive study to track mood variations throughout the day,” Dr Finan said, “then we can determine when it will be appropriate to send messages through text to intervene and affect patient behavior.”
Results of a small study suggest that negative thoughts and emotions may increase opioid use in patients with sickle cell disease (SCD).
Researchers analyzed data from daily electronic patient diaries and found that patients were more likely to use short-acting opioids both when they experienced increased pain and “catastrophic” thoughts about that pain.
In fact, pain catastrophizing led to an increased use of short-acting opioids even when patients reported low levels of pain.
In addition, patients were more likely to use long-acting opioids when they experienced negative emotions.
The researchers noted that this study wasn’t designed to show that negative emotions or thinking cause an increase in opioid use. It was only designed to determine if there was an association.
Patrick Finan, PhD, of Johns Hopkins University School of Medicine in Baltimore, Maryland, and his colleagues described this study in The Journal of Pain.
The researchers enrolled 85 adults with SCD in this study. Patients were asked to fill out electronic diaries on a handheld personal computer every evening for 90 days.
The final analysis included only 45 patients, as these were the subjects who filled out the diary more than 25% of the time and had taken opioid pills at least once during the study period.
The patients had an average age of 37, and 71% were female. Most (93%) were African American, and 7% were classified as “other” or did not report their race.
At the start of the study, the patients reported on the dosage and type of opioid pill they were prescribed for long-acting and short-acting use. The daily diary collected data on the number of long-acting and short-acting opioid pills taken per day.
Patients rated their daily pain level on a scale of 0 to 10, with 0 being no pain and 10 being the worst pain imaginable.
Patients also rated positive emotions—including happy, calm, and cheerful—and negative emotions—including lonely, sad, anxious, and tired—on a scale of 0 to 10, with 0 being no emotion and 10 being the most intense emotion. The scores were converted to a 0-to-100 scale for the data analysis.
Separately, the researchers measured negative thinking using a Pain Catastrophizing Scale to rate “rumination,” or focus on pain, helplessness, and magnification of a current pain situation.
Results
Negative emotions were significantly associated with increased levels of long-acting opioids (P=0.001). The opioid dosage increased by 3.4 morphine milligram equivalents for every 10-point increase in negative emotions.
On the other hand, patients’ daily pain level, positive emotions, and negative thinking through catastrophizing did not significantly affect the amount of long-acting opioids taken.
“When someone is prescribed a daily, long-acting opioid, it is typically supposed to be at a fixed dose, and their pain level or emotions shouldn’t dictate whether they take more of this prescription or not,” Dr Finan said.
“Although we can’t prove misuse of the medication in our study, these data suggest that physicians and patients should clearly communicate about how patients should be taking their daily, long-acting opioids in order to minimize the potential for misuse.”
The researchers also found a significant association with short-acting opioid use and daily pain levels (P=0.006) as well as negative thinking by catastrophizing (P<0.001).
For every 10-point increase on the pain scale, the amount of short-acting opioids increased by 1.8 morphine milligram equivalents, and for every 10-point increase on the catastrophizing scale, pain medicine dosage increased by 2.5 morphine milligram equivalents.
Positive and negative emotions had no significant effect on the use of short-acting opioids.
“When pain was reported as low, sickle cell disease patients reported higher opioid use if they catastrophized, or focused their thinking on their pain, than if they didn’t,” Dr Finan said. “When pain levels were higher, negative thinking played less of a role in influencing opioid use.”
Dr Finan cautioned that studies such as this have some weaknesses, including the fact that self-reports are always uncertain, and the study only included 1 time point per day, although a person’s mood may fluctuate throughout the day based on life events and experiences.
For future studies, Dr Finan wants to use smartphone technology that can assess moods randomly throughout the day.
“Once we have a more intensive study to track mood variations throughout the day,” Dr Finan said, “then we can determine when it will be appropriate to send messages through text to intervene and affect patient behavior.”