User login
FDA approves first treatment for ECD
The US Food and Drug Administration (FDA) has expanded the approved use of vemurafenib (Zelboraf) to include the treatment of adults who have Erdheim-Chester disease (ECD) with BRAF V600 mutation.
Vemurafenib is a kinase inhibitor designed to inhibit some mutated forms of BRAF.
The drug was already approved by the FDA to treat patients with unresectable or metastatic melanoma with BRAF V600E mutation, as detected by an FDA-approved test.
Now, vemurafenib is the first FDA-approved treatment for ECD.
The FDA previously granted vemurafenib orphan drug and breakthrough therapy designations for this indication, and the supplemental new drug application for vemurafenib in ECD received priority review.
“Today’s approval of Zelboraf for patients with ECD demonstrates how we can apply knowledge of the underlying genetic characteristics of certain malignancies to other cancers,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
“This product was first approved in 2011 to treat certain patients with melanoma that harbor the BRAF V600E mutation, and we are now bringing the therapy to patients with a rare cancer with no approved therapies.”
The application for vemurafenib in ECD was supported by data from the phase 2 VE-BASKET study. Initial results from this study were published in NEJM in August 2015.
VE-BASKET was designed to investigate the use of vemurafenib in patients with BRAF V600 mutation-positive diseases, including ECD.
In the 22 patients with ECD, the best overall response rate was 54.5%. Eleven patients experienced a partial response, and 1 patient achieved a complete response.
The median duration of response, progression-free survival, and overall survival were not reached at a median follow-up of 26.6 months.
The most common adverse events (>50%) were joint pain, rash, hair loss, fatigue, change in heart rhythm, and skin tags. The most common grade 3 or higher adverse events (≥10%) were new skin cancers, high blood pressure, rash, and joint pain. ![]()
The US Food and Drug Administration (FDA) has expanded the approved use of vemurafenib (Zelboraf) to include the treatment of adults who have Erdheim-Chester disease (ECD) with BRAF V600 mutation.
Vemurafenib is a kinase inhibitor designed to inhibit some mutated forms of BRAF.
The drug was already approved by the FDA to treat patients with unresectable or metastatic melanoma with BRAF V600E mutation, as detected by an FDA-approved test.
Now, vemurafenib is the first FDA-approved treatment for ECD.
The FDA previously granted vemurafenib orphan drug and breakthrough therapy designations for this indication, and the supplemental new drug application for vemurafenib in ECD received priority review.
“Today’s approval of Zelboraf for patients with ECD demonstrates how we can apply knowledge of the underlying genetic characteristics of certain malignancies to other cancers,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
“This product was first approved in 2011 to treat certain patients with melanoma that harbor the BRAF V600E mutation, and we are now bringing the therapy to patients with a rare cancer with no approved therapies.”
The application for vemurafenib in ECD was supported by data from the phase 2 VE-BASKET study. Initial results from this study were published in NEJM in August 2015.
VE-BASKET was designed to investigate the use of vemurafenib in patients with BRAF V600 mutation-positive diseases, including ECD.
In the 22 patients with ECD, the best overall response rate was 54.5%. Eleven patients experienced a partial response, and 1 patient achieved a complete response.
The median duration of response, progression-free survival, and overall survival were not reached at a median follow-up of 26.6 months.
The most common adverse events (>50%) were joint pain, rash, hair loss, fatigue, change in heart rhythm, and skin tags. The most common grade 3 or higher adverse events (≥10%) were new skin cancers, high blood pressure, rash, and joint pain. ![]()
The US Food and Drug Administration (FDA) has expanded the approved use of vemurafenib (Zelboraf) to include the treatment of adults who have Erdheim-Chester disease (ECD) with BRAF V600 mutation.
Vemurafenib is a kinase inhibitor designed to inhibit some mutated forms of BRAF.
The drug was already approved by the FDA to treat patients with unresectable or metastatic melanoma with BRAF V600E mutation, as detected by an FDA-approved test.
Now, vemurafenib is the first FDA-approved treatment for ECD.
The FDA previously granted vemurafenib orphan drug and breakthrough therapy designations for this indication, and the supplemental new drug application for vemurafenib in ECD received priority review.
“Today’s approval of Zelboraf for patients with ECD demonstrates how we can apply knowledge of the underlying genetic characteristics of certain malignancies to other cancers,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
“This product was first approved in 2011 to treat certain patients with melanoma that harbor the BRAF V600E mutation, and we are now bringing the therapy to patients with a rare cancer with no approved therapies.”
The application for vemurafenib in ECD was supported by data from the phase 2 VE-BASKET study. Initial results from this study were published in NEJM in August 2015.
VE-BASKET was designed to investigate the use of vemurafenib in patients with BRAF V600 mutation-positive diseases, including ECD.
In the 22 patients with ECD, the best overall response rate was 54.5%. Eleven patients experienced a partial response, and 1 patient achieved a complete response.
The median duration of response, progression-free survival, and overall survival were not reached at a median follow-up of 26.6 months.
The most common adverse events (>50%) were joint pain, rash, hair loss, fatigue, change in heart rhythm, and skin tags. The most common grade 3 or higher adverse events (≥10%) were new skin cancers, high blood pressure, rash, and joint pain. ![]()
FDA approves wider use of hematology analyzer
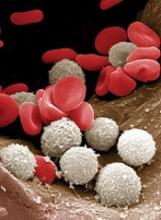
The US Food and Drug Administration (FDA) has expanded the approved use of the XW-100 Automated Hematology Analyzer.
The analyzer can now be used at non-traditional laboratory sites by non-medical personnel.
The XW-100 Automated Hematology Analyzer is intended for use in patients age 2 and older who require a whole blood cell count and white blood cell differential.
Test results can be used with other clinical and laboratory findings to provide early alerts of patients with serious conditions, such as severe anemia and agranulocytosis, who require additional testing.
The XW-100 Automated Hematology Analyzer is not intended to diagnose or monitor patients with primary and/or secondary hematologic diseases.
The device works by using a blood sample to classify and quantify 12 hematology parameters, which provides patients with a blood component profile as part of their overall health assessment.
Expanded clearance
The FDA granted the XW-100 Automated Hematology Analyzer a waiver under the Clinical Laboratory Improvement Amendments of 1988 (CLIA). The waiver allows the device to be used by a variety of non-traditional laboratory sites, including physicians’ offices, clinics, or other types of healthcare facilities with a CLIA Certificate of Waiver.
The XW-100 Automated Hematology Analyzer was reviewed through the dual submission pathway, a streamlined regulatory pathway for 510(k) marketing clearance and CLIA Waiver by Application.
A 510(k) notification is a premarket submission made by device manufacturers to the FDA to demonstrate that the new device is substantially equivalent to a legally marketed predicate device.
The XW-100 Automated Hematology Analyzer was originally cleared through the 510(k) pathway in 2015 for use at the patient’s point-of-care.
To support the use of this device in CLIA-waived settings with non-medical personnel, the analyzer is now accompanied by simple instructions for operator actions when results are flagged or outside of a specified range.
To further ensure accurate testing in this setting and to eliminate results that are most susceptible to inaccuracy or require additional testing, the number of hematology parameters has been reduced to 12.
The FDA found this modified version of the XW-100 Automated Hematology Analyzer to be substantially equivalent to the 2015 model.
In addition, data submitted by Sysmex America, Inc. (the company marketing the analyzer) demonstrated ease of use and a low risk of false results when the modified XW-100 Automated Hematology Analyzer was used by untrained operators.
The FDA reviewed data from a study conducted on 582 samples collected from patients ages 2 to 92.
In this study, researchers compared XW-100 Automated Hematology Analyzer results collected by non-medical personnel in CLIA-waived settings to results from a hematology analyzer in an accredited clinical laboratory.
Results showed that, by following the manufacturer’s instructions for use, accurate testing can be effectively conducted by untrained personnel. ![]()
The US Food and Drug Administration (FDA) has expanded the approved use of the XW-100 Automated Hematology Analyzer.
The analyzer can now be used at non-traditional laboratory sites by non-medical personnel.
The XW-100 Automated Hematology Analyzer is intended for use in patients age 2 and older who require a whole blood cell count and white blood cell differential.
Test results can be used with other clinical and laboratory findings to provide early alerts of patients with serious conditions, such as severe anemia and agranulocytosis, who require additional testing.
The XW-100 Automated Hematology Analyzer is not intended to diagnose or monitor patients with primary and/or secondary hematologic diseases.
The device works by using a blood sample to classify and quantify 12 hematology parameters, which provides patients with a blood component profile as part of their overall health assessment.
Expanded clearance
The FDA granted the XW-100 Automated Hematology Analyzer a waiver under the Clinical Laboratory Improvement Amendments of 1988 (CLIA). The waiver allows the device to be used by a variety of non-traditional laboratory sites, including physicians’ offices, clinics, or other types of healthcare facilities with a CLIA Certificate of Waiver.
The XW-100 Automated Hematology Analyzer was reviewed through the dual submission pathway, a streamlined regulatory pathway for 510(k) marketing clearance and CLIA Waiver by Application.
A 510(k) notification is a premarket submission made by device manufacturers to the FDA to demonstrate that the new device is substantially equivalent to a legally marketed predicate device.
The XW-100 Automated Hematology Analyzer was originally cleared through the 510(k) pathway in 2015 for use at the patient’s point-of-care.
To support the use of this device in CLIA-waived settings with non-medical personnel, the analyzer is now accompanied by simple instructions for operator actions when results are flagged or outside of a specified range.
To further ensure accurate testing in this setting and to eliminate results that are most susceptible to inaccuracy or require additional testing, the number of hematology parameters has been reduced to 12.
The FDA found this modified version of the XW-100 Automated Hematology Analyzer to be substantially equivalent to the 2015 model.
In addition, data submitted by Sysmex America, Inc. (the company marketing the analyzer) demonstrated ease of use and a low risk of false results when the modified XW-100 Automated Hematology Analyzer was used by untrained operators.
The FDA reviewed data from a study conducted on 582 samples collected from patients ages 2 to 92.
In this study, researchers compared XW-100 Automated Hematology Analyzer results collected by non-medical personnel in CLIA-waived settings to results from a hematology analyzer in an accredited clinical laboratory.
Results showed that, by following the manufacturer’s instructions for use, accurate testing can be effectively conducted by untrained personnel. ![]()
The US Food and Drug Administration (FDA) has expanded the approved use of the XW-100 Automated Hematology Analyzer.
The analyzer can now be used at non-traditional laboratory sites by non-medical personnel.
The XW-100 Automated Hematology Analyzer is intended for use in patients age 2 and older who require a whole blood cell count and white blood cell differential.
Test results can be used with other clinical and laboratory findings to provide early alerts of patients with serious conditions, such as severe anemia and agranulocytosis, who require additional testing.
The XW-100 Automated Hematology Analyzer is not intended to diagnose or monitor patients with primary and/or secondary hematologic diseases.
The device works by using a blood sample to classify and quantify 12 hematology parameters, which provides patients with a blood component profile as part of their overall health assessment.
Expanded clearance
The FDA granted the XW-100 Automated Hematology Analyzer a waiver under the Clinical Laboratory Improvement Amendments of 1988 (CLIA). The waiver allows the device to be used by a variety of non-traditional laboratory sites, including physicians’ offices, clinics, or other types of healthcare facilities with a CLIA Certificate of Waiver.
The XW-100 Automated Hematology Analyzer was reviewed through the dual submission pathway, a streamlined regulatory pathway for 510(k) marketing clearance and CLIA Waiver by Application.
A 510(k) notification is a premarket submission made by device manufacturers to the FDA to demonstrate that the new device is substantially equivalent to a legally marketed predicate device.
The XW-100 Automated Hematology Analyzer was originally cleared through the 510(k) pathway in 2015 for use at the patient’s point-of-care.
To support the use of this device in CLIA-waived settings with non-medical personnel, the analyzer is now accompanied by simple instructions for operator actions when results are flagged or outside of a specified range.
To further ensure accurate testing in this setting and to eliminate results that are most susceptible to inaccuracy or require additional testing, the number of hematology parameters has been reduced to 12.
The FDA found this modified version of the XW-100 Automated Hematology Analyzer to be substantially equivalent to the 2015 model.
In addition, data submitted by Sysmex America, Inc. (the company marketing the analyzer) demonstrated ease of use and a low risk of false results when the modified XW-100 Automated Hematology Analyzer was used by untrained operators.
The FDA reviewed data from a study conducted on 582 samples collected from patients ages 2 to 92.
In this study, researchers compared XW-100 Automated Hematology Analyzer results collected by non-medical personnel in CLIA-waived settings to results from a hematology analyzer in an accredited clinical laboratory.
Results showed that, by following the manufacturer’s instructions for use, accurate testing can be effectively conducted by untrained personnel. ![]()
Intervention improves well-being in AYAs with cancer
SAN DIEGO—New research suggests an intervention can improve psychosocial health in adolescents and young adults (AYAs) living with cancer.
The intervention, Promoting Resilience in Stress Management (PRISM), is designed to help patients manage stress, set goals, and change their perspective.
Overall, PRISM improved resilience, enhanced quality of life, increased hope, and lowered distress and depression in the patients studied.
Abby R. Rosenberg, MD, of Seattle Children’s Research Institute in Seattle, Washington, presented these results at the 2017 Palliative and Supportive Care in Oncology Symposium (abstract 176*).
“The experience of cancer is stressful in all realms, but we tend to focus more on physical symptoms than the equally important social and emotional challenges,” Dr Rosenberg said.
“This is particularly true for adolescents and young adults who already struggle with normal developmental changes. When you throw cancer into the mix, it can become much harder.”
With this in mind, Dr Rosenberg and her colleagues tested PRISM in AYAs with cancer. The trial included 99 English-speaking patients, ages 12 to 25, who were diagnosed with new or newly recurrent cancer.
The patients were randomized to receive PRISM (n=49) plus standard psychosocial supportive care or standard care alone (n=50). Standard care at Seattle Children’s Research Institute includes a dedicated social worker and access to psychologists, child-life specialists, and other experts in AYA oncology care, as needed.
PRISM targets 4 topics:
- Managing stress with skills based on mindfulness and relaxation
- Setting goals that are specific and realistic, as well as planning for roadblocks
- Positive reframing, or recognizing and replacing negative self-talk
- Making meaning, or identifying benefits, gratitude, purpose, and legacy.
Each of the 4 topics were discussed with patients in separate, one-on-one sessions with a trained research associate. The sessions lasted 30 minutes to an hour. Patients also received boosters and worksheets for practicing the skills discussed in the meetings.
After all 4 sessions had been completed, patients could participate in an optional family meeting. During this meeting, patients could discuss with their family members which aspects of PRISM worked.
Results
Patients completed surveys at study enrollment, 2 months, 4 months, and 6 months. There were 74 participants who were still alive and well enough to complete the 6-month survey—36 in the PRISM group and 38 in the control group.
At the 6-month mark, PRISM was associated with (sometimes significant) improvements in resilience (P=0.02), generic quality of life (P=0.08), cancer-specific quality of life (P=0.01), hope (P=0.34), and distress (P=0.03). (P values are for absolute difference from baseline to 6 months.)
In addition, the incidence of depression at 6 months was lower in the PRISM group than the control group—6% and 21%, respectively (odds ratio=0.09, 95% CI 0.01, 1.09).
All but 4 of the PRISM recipients chose to participate in the family meeting following their one-on-one sessions.
“We included the family meeting because teens told us they wanted to share with their parents, and parents told us they wanted to know what their children had learned,” Dr Rosenberg said. “While the specific impact of this meeting is yet to be determined, we hope it will guide families so that there is continued support of teen or young adult patients.”
Now, Dr Rosenberg and her colleagues would like to test PRISM in other patient populations.
“We need to include a much larger cultural demographic in future studies,” Dr Rosenberg noted. “Beyond that, we also need to determine if this type of intervention could translate to other centers where usual care may not be as comprehensive as what we have here.” ![]()
*Some data in the abstract differ from the presentation.
SAN DIEGO—New research suggests an intervention can improve psychosocial health in adolescents and young adults (AYAs) living with cancer.
The intervention, Promoting Resilience in Stress Management (PRISM), is designed to help patients manage stress, set goals, and change their perspective.
Overall, PRISM improved resilience, enhanced quality of life, increased hope, and lowered distress and depression in the patients studied.
Abby R. Rosenberg, MD, of Seattle Children’s Research Institute in Seattle, Washington, presented these results at the 2017 Palliative and Supportive Care in Oncology Symposium (abstract 176*).
“The experience of cancer is stressful in all realms, but we tend to focus more on physical symptoms than the equally important social and emotional challenges,” Dr Rosenberg said.
“This is particularly true for adolescents and young adults who already struggle with normal developmental changes. When you throw cancer into the mix, it can become much harder.”
With this in mind, Dr Rosenberg and her colleagues tested PRISM in AYAs with cancer. The trial included 99 English-speaking patients, ages 12 to 25, who were diagnosed with new or newly recurrent cancer.
The patients were randomized to receive PRISM (n=49) plus standard psychosocial supportive care or standard care alone (n=50). Standard care at Seattle Children’s Research Institute includes a dedicated social worker and access to psychologists, child-life specialists, and other experts in AYA oncology care, as needed.
PRISM targets 4 topics:
- Managing stress with skills based on mindfulness and relaxation
- Setting goals that are specific and realistic, as well as planning for roadblocks
- Positive reframing, or recognizing and replacing negative self-talk
- Making meaning, or identifying benefits, gratitude, purpose, and legacy.
Each of the 4 topics were discussed with patients in separate, one-on-one sessions with a trained research associate. The sessions lasted 30 minutes to an hour. Patients also received boosters and worksheets for practicing the skills discussed in the meetings.
After all 4 sessions had been completed, patients could participate in an optional family meeting. During this meeting, patients could discuss with their family members which aspects of PRISM worked.
Results
Patients completed surveys at study enrollment, 2 months, 4 months, and 6 months. There were 74 participants who were still alive and well enough to complete the 6-month survey—36 in the PRISM group and 38 in the control group.
At the 6-month mark, PRISM was associated with (sometimes significant) improvements in resilience (P=0.02), generic quality of life (P=0.08), cancer-specific quality of life (P=0.01), hope (P=0.34), and distress (P=0.03). (P values are for absolute difference from baseline to 6 months.)
In addition, the incidence of depression at 6 months was lower in the PRISM group than the control group—6% and 21%, respectively (odds ratio=0.09, 95% CI 0.01, 1.09).
All but 4 of the PRISM recipients chose to participate in the family meeting following their one-on-one sessions.
“We included the family meeting because teens told us they wanted to share with their parents, and parents told us they wanted to know what their children had learned,” Dr Rosenberg said. “While the specific impact of this meeting is yet to be determined, we hope it will guide families so that there is continued support of teen or young adult patients.”
Now, Dr Rosenberg and her colleagues would like to test PRISM in other patient populations.
“We need to include a much larger cultural demographic in future studies,” Dr Rosenberg noted. “Beyond that, we also need to determine if this type of intervention could translate to other centers where usual care may not be as comprehensive as what we have here.” ![]()
*Some data in the abstract differ from the presentation.
SAN DIEGO—New research suggests an intervention can improve psychosocial health in adolescents and young adults (AYAs) living with cancer.
The intervention, Promoting Resilience in Stress Management (PRISM), is designed to help patients manage stress, set goals, and change their perspective.
Overall, PRISM improved resilience, enhanced quality of life, increased hope, and lowered distress and depression in the patients studied.
Abby R. Rosenberg, MD, of Seattle Children’s Research Institute in Seattle, Washington, presented these results at the 2017 Palliative and Supportive Care in Oncology Symposium (abstract 176*).
“The experience of cancer is stressful in all realms, but we tend to focus more on physical symptoms than the equally important social and emotional challenges,” Dr Rosenberg said.
“This is particularly true for adolescents and young adults who already struggle with normal developmental changes. When you throw cancer into the mix, it can become much harder.”
With this in mind, Dr Rosenberg and her colleagues tested PRISM in AYAs with cancer. The trial included 99 English-speaking patients, ages 12 to 25, who were diagnosed with new or newly recurrent cancer.
The patients were randomized to receive PRISM (n=49) plus standard psychosocial supportive care or standard care alone (n=50). Standard care at Seattle Children’s Research Institute includes a dedicated social worker and access to psychologists, child-life specialists, and other experts in AYA oncology care, as needed.
PRISM targets 4 topics:
- Managing stress with skills based on mindfulness and relaxation
- Setting goals that are specific and realistic, as well as planning for roadblocks
- Positive reframing, or recognizing and replacing negative self-talk
- Making meaning, or identifying benefits, gratitude, purpose, and legacy.
Each of the 4 topics were discussed with patients in separate, one-on-one sessions with a trained research associate. The sessions lasted 30 minutes to an hour. Patients also received boosters and worksheets for practicing the skills discussed in the meetings.
After all 4 sessions had been completed, patients could participate in an optional family meeting. During this meeting, patients could discuss with their family members which aspects of PRISM worked.
Results
Patients completed surveys at study enrollment, 2 months, 4 months, and 6 months. There were 74 participants who were still alive and well enough to complete the 6-month survey—36 in the PRISM group and 38 in the control group.
At the 6-month mark, PRISM was associated with (sometimes significant) improvements in resilience (P=0.02), generic quality of life (P=0.08), cancer-specific quality of life (P=0.01), hope (P=0.34), and distress (P=0.03). (P values are for absolute difference from baseline to 6 months.)
In addition, the incidence of depression at 6 months was lower in the PRISM group than the control group—6% and 21%, respectively (odds ratio=0.09, 95% CI 0.01, 1.09).
All but 4 of the PRISM recipients chose to participate in the family meeting following their one-on-one sessions.
“We included the family meeting because teens told us they wanted to share with their parents, and parents told us they wanted to know what their children had learned,” Dr Rosenberg said. “While the specific impact of this meeting is yet to be determined, we hope it will guide families so that there is continued support of teen or young adult patients.”
Now, Dr Rosenberg and her colleagues would like to test PRISM in other patient populations.
“We need to include a much larger cultural demographic in future studies,” Dr Rosenberg noted. “Beyond that, we also need to determine if this type of intervention could translate to other centers where usual care may not be as comprehensive as what we have here.” ![]()
*Some data in the abstract differ from the presentation.
Cancer drug costs increasing despite competition
Cancer drug costs in the US increase substantially after launch, regardless of competition, according to a study published in the Journal of Clinical Oncology.*
Researchers studied 24 cancer drugs approved over the last 20 years and found a mean cumulative cost increase of about 37%, or 19% when adjusted for inflation.
Among drugs approved to treat hematologic malignancies, the greatest inflation-adjusted price increases were for arsenic trioxide (57%), nelarabine (55%), and rituximab (49%).
The lowest inflation-adjusted price increases were for ofatumumab (8%), clofarabine (8%), and liposomal vincristine (18%).
For this study, Daniel A. Goldstein, MD, of Emory University in Atlanta, Georgia, and his colleagues measured the monthly price trajectories of 24 cancer drugs approved by the US Food and Drug Administration. This included 10 drugs approved to treat hematologic malignancies between 1997 and 2011.
To account for discounts and rebates, the researchers used the average sales prices published by the Centers for Medicare and Medicaid Services and adjusted to general and health-related inflation rates. For each drug, the researchers calculated the cumulative and annual drug cost changes.
Results
The mean follow-up was 8 years. The mean cumulative cost increase for all 24 drugs was +36.5% (95% CI, 24.7% to 48.3%).
The general inflation-adjusted increase was +19.1% (95% CI, 11.0% to 27.2%), and the health-related inflation-adjusted increase was +8.4% (95% CI, 1.4% to 15.4%).
Only 1 of the 24 drugs studied had a price decrease over time. That drug is ziv-aflibercept, which was approved to treat metastatic colorectal cancer in 2012.
Ziv-aflibercept was launched with an annual price exceeding $110,000. After public outcry, the drug’s manufacturer, Sanofi, cut the price in half. By the end of the study’s follow-up period in 2017, the cost of ziv-aflibercept had decreased 13% (inflation-adjusted decrease of 15%, health-related inflation-adjusted decrease of 20%).
Cost changes for the drugs approved to treat hematologic malignancies are listed in the following table.
| Drug (indication, approval date, years of follow-up) | Mean monthly cost at launch | Mean annual cost change (SD) | Cumulative cost change | General and health-related inflation-adjusted change, respectively |
| Arsenic trioxide (APL, 2000, 12) | $11,455 | +6% (4) | +95% | +57%, +39% |
| Bendamustine (CLL, NHL, 2008, 8) | $6924 | +5% (5) | +50% | +32%, +21% |
| Bortezomib (MM, MCL, 2003, 12) | $5490 | +4% (3) | +63% | +31%, +16% |
| Brentuximab (lymphoma, 2011, 4) | $19,482 | +8% (0.1) | +35% | +29%, +22% |
| Clofarabine (ALL, 2004, 11) | $56,486 | +3% (3) | +31% | +8%, -4% |
| Liposomal vincristine (ALL, 2012, 3) | $34,602 | +8% (0.5) | +21% | +18%, +14% |
| Nelarabine (ALL, lymphoma, 2005, 10) | $18,513 | +6% (2) | +83% | +55%, +39% |
| Ofatumumab (CLL, 2009, 6) | $4538 | +3% (2) | +17% | +8%, -0.5% |
| Pralatrexate (lymphoma, 2009, 6) | $31,684 | +6% (4) | +43% | +31%, +21% |
| Rituximab (NHL, CLL, 1997, 12) | $4111 | +5% (0.5) | +85% | +49%, +32% |
Abbreviations: ALL, acute lymphoblastic leukemia; APL, acute promyelocytic leukemia; CLL, chronic lymphocytic leukemia; MCL, mantle cell lymphoma; MM, multiple myeloma; NHL, non-Hodgkin lymphoma; SD, standard deviation.
The researchers noted that there was a steady increase in drug costs over the study period, regardless of whether a drug was granted a new supplemental indication, the drug had a new off-label indication, or a competitor drug was approved.
The only variable that was significantly associated with price change was the amount of time that had elapsed from a drug’s launch.
This association was significant in models in which the researchers used prices adjusted to inflation (P=0.002) and health-related inflation (P=0.023). However, it was not significant when the researchers used the actual drug price (P=0.085). ![]()
*Data in the abstract differ from data in the body of the JCO paper. This article includes data from the body of the JCO paper.
Cancer drug costs in the US increase substantially after launch, regardless of competition, according to a study published in the Journal of Clinical Oncology.*
Researchers studied 24 cancer drugs approved over the last 20 years and found a mean cumulative cost increase of about 37%, or 19% when adjusted for inflation.
Among drugs approved to treat hematologic malignancies, the greatest inflation-adjusted price increases were for arsenic trioxide (57%), nelarabine (55%), and rituximab (49%).
The lowest inflation-adjusted price increases were for ofatumumab (8%), clofarabine (8%), and liposomal vincristine (18%).
For this study, Daniel A. Goldstein, MD, of Emory University in Atlanta, Georgia, and his colleagues measured the monthly price trajectories of 24 cancer drugs approved by the US Food and Drug Administration. This included 10 drugs approved to treat hematologic malignancies between 1997 and 2011.
To account for discounts and rebates, the researchers used the average sales prices published by the Centers for Medicare and Medicaid Services and adjusted to general and health-related inflation rates. For each drug, the researchers calculated the cumulative and annual drug cost changes.
Results
The mean follow-up was 8 years. The mean cumulative cost increase for all 24 drugs was +36.5% (95% CI, 24.7% to 48.3%).
The general inflation-adjusted increase was +19.1% (95% CI, 11.0% to 27.2%), and the health-related inflation-adjusted increase was +8.4% (95% CI, 1.4% to 15.4%).
Only 1 of the 24 drugs studied had a price decrease over time. That drug is ziv-aflibercept, which was approved to treat metastatic colorectal cancer in 2012.
Ziv-aflibercept was launched with an annual price exceeding $110,000. After public outcry, the drug’s manufacturer, Sanofi, cut the price in half. By the end of the study’s follow-up period in 2017, the cost of ziv-aflibercept had decreased 13% (inflation-adjusted decrease of 15%, health-related inflation-adjusted decrease of 20%).
Cost changes for the drugs approved to treat hematologic malignancies are listed in the following table.
| Drug (indication, approval date, years of follow-up) | Mean monthly cost at launch | Mean annual cost change (SD) | Cumulative cost change | General and health-related inflation-adjusted change, respectively |
| Arsenic trioxide (APL, 2000, 12) | $11,455 | +6% (4) | +95% | +57%, +39% |
| Bendamustine (CLL, NHL, 2008, 8) | $6924 | +5% (5) | +50% | +32%, +21% |
| Bortezomib (MM, MCL, 2003, 12) | $5490 | +4% (3) | +63% | +31%, +16% |
| Brentuximab (lymphoma, 2011, 4) | $19,482 | +8% (0.1) | +35% | +29%, +22% |
| Clofarabine (ALL, 2004, 11) | $56,486 | +3% (3) | +31% | +8%, -4% |
| Liposomal vincristine (ALL, 2012, 3) | $34,602 | +8% (0.5) | +21% | +18%, +14% |
| Nelarabine (ALL, lymphoma, 2005, 10) | $18,513 | +6% (2) | +83% | +55%, +39% |
| Ofatumumab (CLL, 2009, 6) | $4538 | +3% (2) | +17% | +8%, -0.5% |
| Pralatrexate (lymphoma, 2009, 6) | $31,684 | +6% (4) | +43% | +31%, +21% |
| Rituximab (NHL, CLL, 1997, 12) | $4111 | +5% (0.5) | +85% | +49%, +32% |
Abbreviations: ALL, acute lymphoblastic leukemia; APL, acute promyelocytic leukemia; CLL, chronic lymphocytic leukemia; MCL, mantle cell lymphoma; MM, multiple myeloma; NHL, non-Hodgkin lymphoma; SD, standard deviation.
The researchers noted that there was a steady increase in drug costs over the study period, regardless of whether a drug was granted a new supplemental indication, the drug had a new off-label indication, or a competitor drug was approved.
The only variable that was significantly associated with price change was the amount of time that had elapsed from a drug’s launch.
This association was significant in models in which the researchers used prices adjusted to inflation (P=0.002) and health-related inflation (P=0.023). However, it was not significant when the researchers used the actual drug price (P=0.085). ![]()
*Data in the abstract differ from data in the body of the JCO paper. This article includes data from the body of the JCO paper.
Cancer drug costs in the US increase substantially after launch, regardless of competition, according to a study published in the Journal of Clinical Oncology.*
Researchers studied 24 cancer drugs approved over the last 20 years and found a mean cumulative cost increase of about 37%, or 19% when adjusted for inflation.
Among drugs approved to treat hematologic malignancies, the greatest inflation-adjusted price increases were for arsenic trioxide (57%), nelarabine (55%), and rituximab (49%).
The lowest inflation-adjusted price increases were for ofatumumab (8%), clofarabine (8%), and liposomal vincristine (18%).
For this study, Daniel A. Goldstein, MD, of Emory University in Atlanta, Georgia, and his colleagues measured the monthly price trajectories of 24 cancer drugs approved by the US Food and Drug Administration. This included 10 drugs approved to treat hematologic malignancies between 1997 and 2011.
To account for discounts and rebates, the researchers used the average sales prices published by the Centers for Medicare and Medicaid Services and adjusted to general and health-related inflation rates. For each drug, the researchers calculated the cumulative and annual drug cost changes.
Results
The mean follow-up was 8 years. The mean cumulative cost increase for all 24 drugs was +36.5% (95% CI, 24.7% to 48.3%).
The general inflation-adjusted increase was +19.1% (95% CI, 11.0% to 27.2%), and the health-related inflation-adjusted increase was +8.4% (95% CI, 1.4% to 15.4%).
Only 1 of the 24 drugs studied had a price decrease over time. That drug is ziv-aflibercept, which was approved to treat metastatic colorectal cancer in 2012.
Ziv-aflibercept was launched with an annual price exceeding $110,000. After public outcry, the drug’s manufacturer, Sanofi, cut the price in half. By the end of the study’s follow-up period in 2017, the cost of ziv-aflibercept had decreased 13% (inflation-adjusted decrease of 15%, health-related inflation-adjusted decrease of 20%).
Cost changes for the drugs approved to treat hematologic malignancies are listed in the following table.
| Drug (indication, approval date, years of follow-up) | Mean monthly cost at launch | Mean annual cost change (SD) | Cumulative cost change | General and health-related inflation-adjusted change, respectively |
| Arsenic trioxide (APL, 2000, 12) | $11,455 | +6% (4) | +95% | +57%, +39% |
| Bendamustine (CLL, NHL, 2008, 8) | $6924 | +5% (5) | +50% | +32%, +21% |
| Bortezomib (MM, MCL, 2003, 12) | $5490 | +4% (3) | +63% | +31%, +16% |
| Brentuximab (lymphoma, 2011, 4) | $19,482 | +8% (0.1) | +35% | +29%, +22% |
| Clofarabine (ALL, 2004, 11) | $56,486 | +3% (3) | +31% | +8%, -4% |
| Liposomal vincristine (ALL, 2012, 3) | $34,602 | +8% (0.5) | +21% | +18%, +14% |
| Nelarabine (ALL, lymphoma, 2005, 10) | $18,513 | +6% (2) | +83% | +55%, +39% |
| Ofatumumab (CLL, 2009, 6) | $4538 | +3% (2) | +17% | +8%, -0.5% |
| Pralatrexate (lymphoma, 2009, 6) | $31,684 | +6% (4) | +43% | +31%, +21% |
| Rituximab (NHL, CLL, 1997, 12) | $4111 | +5% (0.5) | +85% | +49%, +32% |
Abbreviations: ALL, acute lymphoblastic leukemia; APL, acute promyelocytic leukemia; CLL, chronic lymphocytic leukemia; MCL, mantle cell lymphoma; MM, multiple myeloma; NHL, non-Hodgkin lymphoma; SD, standard deviation.
The researchers noted that there was a steady increase in drug costs over the study period, regardless of whether a drug was granted a new supplemental indication, the drug had a new off-label indication, or a competitor drug was approved.
The only variable that was significantly associated with price change was the amount of time that had elapsed from a drug’s launch.
This association was significant in models in which the researchers used prices adjusted to inflation (P=0.002) and health-related inflation (P=0.023). However, it was not significant when the researchers used the actual drug price (P=0.085). ![]()
*Data in the abstract differ from data in the body of the JCO paper. This article includes data from the body of the JCO paper.
Protein may be target for enhancing HSC transplants
Targeting the protein Del-1 could potentially improve hematopoietic stem cell (HSC) transplants, according to researchers.
The team found that Del-1 promoted engraftment in murine transplant recipients, but the protein also promoted the retention of hematopoietic progenitors in the bone marrow of mice that received granulocyte colony-stimulating factor (G-CSF).
The researchers therefore believe that enhancing Del-1 in HSC transplant recipients might improve engraftment.
And inhibiting Del-1 could increase progenitor mobilization in transplant donors.
The researchers detailed these findings and theories in The Journal of Clinical Investigation.
“Because the hematopoietic stem cell niche is so important for the creation of bone marrow and blood cells and because Del-1 is a soluble protein and easily manipulated, one can see that it could be a target in many potential applications,” said study author George Hajishengallis, DDS, PhD, of Penn Dental Medicine in Philadelphia, Pennsylvania.
For Dr Hajishengallis, the route to studying Del-1 in the bone marrow began in his field of dental medicine.
Dr Hajishengallis and Triantafyllos Chavakis, Dr med, of Technische Universität Dresden in Germany, identified Del-1 as a potential drug target for gum disease. (Del-1 prevents inflammatory cells from moving into the gums.)
Both of the researchers’ labs also discovered that Del-1 is expressed in bone marrow, so the groups began following up to examine the protein’s function there.
Their work revealed that Del-1 is a key regulator of the HSC niche.
Del-1 is expressed by cells that promote HSC maintenance under steady-state conditions. This includes arteriolar endothelial cells, CXCL12-abundant reticular cells, and cells of the osteoblastic lineage.
The researchers also found that Del-1 regulates long-term HSC proliferation and differentiation toward the myeloid lineage.
In mice that received HSC transplants, Del-1 promoted progenitor engraftment and the generation of both progenitors and mature myeloid cells. The researchers noted that this was dependent upon β3 integrin expression in hematopoietic cells.
The team also found that Del-1 promotes hematopoietic progenitors’ response to systemic inflammation (induced by lipopolysaccharide). And the protein promotes the retention of hematopoietic progenitors in the bone marrow after G-CSF administration.
Taken together, these findings suggest that manipulating Del-1 might enhance HSC transplants.
“It’s easy to think of practical applications,” Dr Hajishengallis said. “Now, we need to find out whether it works in practice, so our studies continue.” ![]()
Targeting the protein Del-1 could potentially improve hematopoietic stem cell (HSC) transplants, according to researchers.
The team found that Del-1 promoted engraftment in murine transplant recipients, but the protein also promoted the retention of hematopoietic progenitors in the bone marrow of mice that received granulocyte colony-stimulating factor (G-CSF).
The researchers therefore believe that enhancing Del-1 in HSC transplant recipients might improve engraftment.
And inhibiting Del-1 could increase progenitor mobilization in transplant donors.
The researchers detailed these findings and theories in The Journal of Clinical Investigation.
“Because the hematopoietic stem cell niche is so important for the creation of bone marrow and blood cells and because Del-1 is a soluble protein and easily manipulated, one can see that it could be a target in many potential applications,” said study author George Hajishengallis, DDS, PhD, of Penn Dental Medicine in Philadelphia, Pennsylvania.
For Dr Hajishengallis, the route to studying Del-1 in the bone marrow began in his field of dental medicine.
Dr Hajishengallis and Triantafyllos Chavakis, Dr med, of Technische Universität Dresden in Germany, identified Del-1 as a potential drug target for gum disease. (Del-1 prevents inflammatory cells from moving into the gums.)
Both of the researchers’ labs also discovered that Del-1 is expressed in bone marrow, so the groups began following up to examine the protein’s function there.
Their work revealed that Del-1 is a key regulator of the HSC niche.
Del-1 is expressed by cells that promote HSC maintenance under steady-state conditions. This includes arteriolar endothelial cells, CXCL12-abundant reticular cells, and cells of the osteoblastic lineage.
The researchers also found that Del-1 regulates long-term HSC proliferation and differentiation toward the myeloid lineage.
In mice that received HSC transplants, Del-1 promoted progenitor engraftment and the generation of both progenitors and mature myeloid cells. The researchers noted that this was dependent upon β3 integrin expression in hematopoietic cells.
The team also found that Del-1 promotes hematopoietic progenitors’ response to systemic inflammation (induced by lipopolysaccharide). And the protein promotes the retention of hematopoietic progenitors in the bone marrow after G-CSF administration.
Taken together, these findings suggest that manipulating Del-1 might enhance HSC transplants.
“It’s easy to think of practical applications,” Dr Hajishengallis said. “Now, we need to find out whether it works in practice, so our studies continue.” ![]()
Targeting the protein Del-1 could potentially improve hematopoietic stem cell (HSC) transplants, according to researchers.
The team found that Del-1 promoted engraftment in murine transplant recipients, but the protein also promoted the retention of hematopoietic progenitors in the bone marrow of mice that received granulocyte colony-stimulating factor (G-CSF).
The researchers therefore believe that enhancing Del-1 in HSC transplant recipients might improve engraftment.
And inhibiting Del-1 could increase progenitor mobilization in transplant donors.
The researchers detailed these findings and theories in The Journal of Clinical Investigation.
“Because the hematopoietic stem cell niche is so important for the creation of bone marrow and blood cells and because Del-1 is a soluble protein and easily manipulated, one can see that it could be a target in many potential applications,” said study author George Hajishengallis, DDS, PhD, of Penn Dental Medicine in Philadelphia, Pennsylvania.
For Dr Hajishengallis, the route to studying Del-1 in the bone marrow began in his field of dental medicine.
Dr Hajishengallis and Triantafyllos Chavakis, Dr med, of Technische Universität Dresden in Germany, identified Del-1 as a potential drug target for gum disease. (Del-1 prevents inflammatory cells from moving into the gums.)
Both of the researchers’ labs also discovered that Del-1 is expressed in bone marrow, so the groups began following up to examine the protein’s function there.
Their work revealed that Del-1 is a key regulator of the HSC niche.
Del-1 is expressed by cells that promote HSC maintenance under steady-state conditions. This includes arteriolar endothelial cells, CXCL12-abundant reticular cells, and cells of the osteoblastic lineage.
The researchers also found that Del-1 regulates long-term HSC proliferation and differentiation toward the myeloid lineage.
In mice that received HSC transplants, Del-1 promoted progenitor engraftment and the generation of both progenitors and mature myeloid cells. The researchers noted that this was dependent upon β3 integrin expression in hematopoietic cells.
The team also found that Del-1 promotes hematopoietic progenitors’ response to systemic inflammation (induced by lipopolysaccharide). And the protein promotes the retention of hematopoietic progenitors in the bone marrow after G-CSF administration.
Taken together, these findings suggest that manipulating Del-1 might enhance HSC transplants.
“It’s easy to think of practical applications,” Dr Hajishengallis said. “Now, we need to find out whether it works in practice, so our studies continue.” ![]()
Product can improve joint health in hemophilia A
New research suggests prophylaxis with a recombinant factor VIII Fc fusion protein (rFVIIIFc) can improve joint health over time in patients with hemophilia A.
Patients saw continuous improvement in joint health over a nearly 3-year period, regardless of prior treatment regimen, severity of joint damage, or target joints.
“Gradual joint destruction, which is the leading cause of morbidity for people with hemophilia, remains a significant challenge in the treatment of hemophilia A,” said Johannes Oldenburg, MD, of University Clinic Bonn in Germany.
“This is the first study to show that functional joint health can continue to improve using prophylactic treatment with an extended half-life factor therapy, even for those who have severe joint disease at the start of treatment.”
Dr Oldenburg and his colleagues reported these findings in Haemophilia. The research was sponsored by Biogen/Bioverativ and Sobi, the companies marketing rFVIIIFc (or efmoroctocog alfa) as Eloctate or Elocta.
This interim post hoc analysis was an evaluation of joint health in adults and adolescents who received rFVIIIFc prophylaxis in the A-LONG and ASPIRE studies.
In A-LONG, patients age 12 and older who had severe hemophilia A received rFVIIIFc at 25-65 IU/kg every 3 to 5 days (arm 1), at 65 IU/kg weekly (arm 2), or as episodic treatment (arm 3). Patients who completed A-LONG could then enroll in the ASPIRE extension study.
For the current analysis, Dr Oldenburg and his colleagues assessed joint health in ASPIRE enrollees using a modified version of the Hemophilia Joint Health Score (mHJHS). This tool grades joints by specific domains, including swelling, muscle atrophy, alignment, range of motion, joint pain, strength, and global gait.
The researchers examined mHJHS measurements (a decrease in score reflecting improvement) taken at A-LONG baseline, ASPIRE baseline, and annually thereafter for roughly 2.8 years of treatment.
There were 47 patients who had mHJHS data at both study baselines, ASPIRE year 1, and ASPIRE year 2.
These patients had a mean improvement in joint health score of -4.1 at ASPIRE year 2, compared with A-LONG baseline (P=0.001).
The mean improvement was -2.4 (P=0.09) for patients who received pre-study prophylaxis and -7.2 (P=0.003) for those who received pre-study episodic treatment.
The mean improvement was -5.6 (P=0.005) in patients with target joints and -8.8 (P=0.02) in those with severe joint destruction.
The mHJHS components with the greatest improvement at ASPIRE year 2 were swelling (-1.4, P=0.008), range of motion (-1.1, P=0.03), and strength (-0.8, P=0.04). ![]()
New research suggests prophylaxis with a recombinant factor VIII Fc fusion protein (rFVIIIFc) can improve joint health over time in patients with hemophilia A.
Patients saw continuous improvement in joint health over a nearly 3-year period, regardless of prior treatment regimen, severity of joint damage, or target joints.
“Gradual joint destruction, which is the leading cause of morbidity for people with hemophilia, remains a significant challenge in the treatment of hemophilia A,” said Johannes Oldenburg, MD, of University Clinic Bonn in Germany.
“This is the first study to show that functional joint health can continue to improve using prophylactic treatment with an extended half-life factor therapy, even for those who have severe joint disease at the start of treatment.”
Dr Oldenburg and his colleagues reported these findings in Haemophilia. The research was sponsored by Biogen/Bioverativ and Sobi, the companies marketing rFVIIIFc (or efmoroctocog alfa) as Eloctate or Elocta.
This interim post hoc analysis was an evaluation of joint health in adults and adolescents who received rFVIIIFc prophylaxis in the A-LONG and ASPIRE studies.
In A-LONG, patients age 12 and older who had severe hemophilia A received rFVIIIFc at 25-65 IU/kg every 3 to 5 days (arm 1), at 65 IU/kg weekly (arm 2), or as episodic treatment (arm 3). Patients who completed A-LONG could then enroll in the ASPIRE extension study.
For the current analysis, Dr Oldenburg and his colleagues assessed joint health in ASPIRE enrollees using a modified version of the Hemophilia Joint Health Score (mHJHS). This tool grades joints by specific domains, including swelling, muscle atrophy, alignment, range of motion, joint pain, strength, and global gait.
The researchers examined mHJHS measurements (a decrease in score reflecting improvement) taken at A-LONG baseline, ASPIRE baseline, and annually thereafter for roughly 2.8 years of treatment.
There were 47 patients who had mHJHS data at both study baselines, ASPIRE year 1, and ASPIRE year 2.
These patients had a mean improvement in joint health score of -4.1 at ASPIRE year 2, compared with A-LONG baseline (P=0.001).
The mean improvement was -2.4 (P=0.09) for patients who received pre-study prophylaxis and -7.2 (P=0.003) for those who received pre-study episodic treatment.
The mean improvement was -5.6 (P=0.005) in patients with target joints and -8.8 (P=0.02) in those with severe joint destruction.
The mHJHS components with the greatest improvement at ASPIRE year 2 were swelling (-1.4, P=0.008), range of motion (-1.1, P=0.03), and strength (-0.8, P=0.04). ![]()
New research suggests prophylaxis with a recombinant factor VIII Fc fusion protein (rFVIIIFc) can improve joint health over time in patients with hemophilia A.
Patients saw continuous improvement in joint health over a nearly 3-year period, regardless of prior treatment regimen, severity of joint damage, or target joints.
“Gradual joint destruction, which is the leading cause of morbidity for people with hemophilia, remains a significant challenge in the treatment of hemophilia A,” said Johannes Oldenburg, MD, of University Clinic Bonn in Germany.
“This is the first study to show that functional joint health can continue to improve using prophylactic treatment with an extended half-life factor therapy, even for those who have severe joint disease at the start of treatment.”
Dr Oldenburg and his colleagues reported these findings in Haemophilia. The research was sponsored by Biogen/Bioverativ and Sobi, the companies marketing rFVIIIFc (or efmoroctocog alfa) as Eloctate or Elocta.
This interim post hoc analysis was an evaluation of joint health in adults and adolescents who received rFVIIIFc prophylaxis in the A-LONG and ASPIRE studies.
In A-LONG, patients age 12 and older who had severe hemophilia A received rFVIIIFc at 25-65 IU/kg every 3 to 5 days (arm 1), at 65 IU/kg weekly (arm 2), or as episodic treatment (arm 3). Patients who completed A-LONG could then enroll in the ASPIRE extension study.
For the current analysis, Dr Oldenburg and his colleagues assessed joint health in ASPIRE enrollees using a modified version of the Hemophilia Joint Health Score (mHJHS). This tool grades joints by specific domains, including swelling, muscle atrophy, alignment, range of motion, joint pain, strength, and global gait.
The researchers examined mHJHS measurements (a decrease in score reflecting improvement) taken at A-LONG baseline, ASPIRE baseline, and annually thereafter for roughly 2.8 years of treatment.
There were 47 patients who had mHJHS data at both study baselines, ASPIRE year 1, and ASPIRE year 2.
These patients had a mean improvement in joint health score of -4.1 at ASPIRE year 2, compared with A-LONG baseline (P=0.001).
The mean improvement was -2.4 (P=0.09) for patients who received pre-study prophylaxis and -7.2 (P=0.003) for those who received pre-study episodic treatment.
The mean improvement was -5.6 (P=0.005) in patients with target joints and -8.8 (P=0.02) in those with severe joint destruction.
The mHJHS components with the greatest improvement at ASPIRE year 2 were swelling (-1.4, P=0.008), range of motion (-1.1, P=0.03), and strength (-0.8, P=0.04). ![]()
Team identifies HSCs that rapidly reconstitute hematopoiesis
Researchers say they have identified a subpopulation of hematopoietic stem cells (HSCs) that immediately contributes to long-term, multilineage hematopoietic reconstitution after transplant.
These HSCs were discovered in macaques, but the cells are similar to a subset of HSCs found in humans.
The researchers found the 2 sets of cells behaved identically when tested in vitro.
The team believes their findings will increase the efficiency of future efforts for HSC transplants, gene therapies, and gene editing.
Hans-Peter Kiem, MD, PhD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington, and his colleagues reported these findings in Science Translational Medicine.
The researchers performed HSC transplants in pig-tailed macaques, following hundreds of thousands of cells immediately after transplant and over the course of 7.5 years.
Previous reports had suggested that successive waves of progenitor cells expand and contract to establish the new bone marrow after transplant.
However, Dr Kiem and his colleagues homed in on a distinct group of HSCs that took hold early after transplant and went on to produce all cell lineages that constitute a complete blood system.
“These findings came as a surprise,” Dr Kiem said. “We had thought that there were multiple types of blood stem cells that take on different roles in rebuilding a blood and immune system. This population does it all.”
The population is a subset of CD34+ cells expressing CD90 and lacking CD45RA markers.
“The gold standard target cell population for stem cell gene therapy are cells with the marker CD34,” said study author Stefan Radtke, PhD, of the Fred Hutchinson Cancer Research Center.
“But we used 2 additional markers to further distinguish the population from the other blood stem cells.”
The researchers noted that the CD34+ CD45RA- CD90+ HSCs started repopulating the hematopoietic system within 10 days of being infused in macaques undergoing transplant.
A year later, the researchers found strong molecular traces of the cells, suggesting they were responsible for the ongoing maintenance of the newly transplanted system.
The team also determined the minimum numbers of CD34+ CD45RA- CD90+ HSCs that were necessary for successful transplant (defined as sustained neutrophil and platelet recovery).
And the researchers found similar gene expression profiles between macaque and human CD34+ CD45RA- CD90+ HSCs.
The team therefore believes these findings could have implications for HSC transplants in humans.
The researchers are now working to move their findings into the clinic with the hopes of integrating them in ongoing clinical trials. The team is currently looking for commercial partners. ![]()
Researchers say they have identified a subpopulation of hematopoietic stem cells (HSCs) that immediately contributes to long-term, multilineage hematopoietic reconstitution after transplant.
These HSCs were discovered in macaques, but the cells are similar to a subset of HSCs found in humans.
The researchers found the 2 sets of cells behaved identically when tested in vitro.
The team believes their findings will increase the efficiency of future efforts for HSC transplants, gene therapies, and gene editing.
Hans-Peter Kiem, MD, PhD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington, and his colleagues reported these findings in Science Translational Medicine.
The researchers performed HSC transplants in pig-tailed macaques, following hundreds of thousands of cells immediately after transplant and over the course of 7.5 years.
Previous reports had suggested that successive waves of progenitor cells expand and contract to establish the new bone marrow after transplant.
However, Dr Kiem and his colleagues homed in on a distinct group of HSCs that took hold early after transplant and went on to produce all cell lineages that constitute a complete blood system.
“These findings came as a surprise,” Dr Kiem said. “We had thought that there were multiple types of blood stem cells that take on different roles in rebuilding a blood and immune system. This population does it all.”
The population is a subset of CD34+ cells expressing CD90 and lacking CD45RA markers.
“The gold standard target cell population for stem cell gene therapy are cells with the marker CD34,” said study author Stefan Radtke, PhD, of the Fred Hutchinson Cancer Research Center.
“But we used 2 additional markers to further distinguish the population from the other blood stem cells.”
The researchers noted that the CD34+ CD45RA- CD90+ HSCs started repopulating the hematopoietic system within 10 days of being infused in macaques undergoing transplant.
A year later, the researchers found strong molecular traces of the cells, suggesting they were responsible for the ongoing maintenance of the newly transplanted system.
The team also determined the minimum numbers of CD34+ CD45RA- CD90+ HSCs that were necessary for successful transplant (defined as sustained neutrophil and platelet recovery).
And the researchers found similar gene expression profiles between macaque and human CD34+ CD45RA- CD90+ HSCs.
The team therefore believes these findings could have implications for HSC transplants in humans.
The researchers are now working to move their findings into the clinic with the hopes of integrating them in ongoing clinical trials. The team is currently looking for commercial partners. ![]()
Researchers say they have identified a subpopulation of hematopoietic stem cells (HSCs) that immediately contributes to long-term, multilineage hematopoietic reconstitution after transplant.
These HSCs were discovered in macaques, but the cells are similar to a subset of HSCs found in humans.
The researchers found the 2 sets of cells behaved identically when tested in vitro.
The team believes their findings will increase the efficiency of future efforts for HSC transplants, gene therapies, and gene editing.
Hans-Peter Kiem, MD, PhD, of the Fred Hutchinson Cancer Research Center in Seattle, Washington, and his colleagues reported these findings in Science Translational Medicine.
The researchers performed HSC transplants in pig-tailed macaques, following hundreds of thousands of cells immediately after transplant and over the course of 7.5 years.
Previous reports had suggested that successive waves of progenitor cells expand and contract to establish the new bone marrow after transplant.
However, Dr Kiem and his colleagues homed in on a distinct group of HSCs that took hold early after transplant and went on to produce all cell lineages that constitute a complete blood system.
“These findings came as a surprise,” Dr Kiem said. “We had thought that there were multiple types of blood stem cells that take on different roles in rebuilding a blood and immune system. This population does it all.”
The population is a subset of CD34+ cells expressing CD90 and lacking CD45RA markers.
“The gold standard target cell population for stem cell gene therapy are cells with the marker CD34,” said study author Stefan Radtke, PhD, of the Fred Hutchinson Cancer Research Center.
“But we used 2 additional markers to further distinguish the population from the other blood stem cells.”
The researchers noted that the CD34+ CD45RA- CD90+ HSCs started repopulating the hematopoietic system within 10 days of being infused in macaques undergoing transplant.
A year later, the researchers found strong molecular traces of the cells, suggesting they were responsible for the ongoing maintenance of the newly transplanted system.
The team also determined the minimum numbers of CD34+ CD45RA- CD90+ HSCs that were necessary for successful transplant (defined as sustained neutrophil and platelet recovery).
And the researchers found similar gene expression profiles between macaque and human CD34+ CD45RA- CD90+ HSCs.
The team therefore believes these findings could have implications for HSC transplants in humans.
The researchers are now working to move their findings into the clinic with the hopes of integrating them in ongoing clinical trials. The team is currently looking for commercial partners.
FDA grants product breakthrough designation for MM
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to GSK2857916, an anti-B-cell maturation antigen (BCMA) monoclonal antibody conjugated to the cytotoxic agent monomethyl auristatin-F via a non-cleavable linker.
The designation is for GSK2857916 as monotherapy for patients with multiple myeloma (MM) who have failed at least 3 prior lines of therapy, including an anti-CD38 antibody, and who are refractory to a proteasome inhibitor and an immunomodulatory agent.
The designation is based on results from a phase 1, dose-escalation and expansion study in patients with relapsed/refractory MM, irrespective of BCMA expression (NCT02064387).
Data from this ongoing trial are scheduled to be presented December 11 in an oral presentation at the 59th Annual Meeting of the American Society of Hematology (ASH) in Atlanta, Georgia.
GSK2857916 has also received orphan drug designation from the FDA and the European Medicines Agency (EMA) as well as PRIME designation from the EMA.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions. The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
Orphan and PRIME designations
The FDA grants orphan designation to therapies intended to treat conditions that affect fewer than 200,000 people in the US. The designation qualifies a drug’s sponsor for various development incentives of the Orphan Drug Act, including tax credits for qualified clinical testing and 7 years of market exclusivity.
In Europe, sponsors who obtain orphan designation for a potential new medicine benefit from a range of incentives, including protocol assistance, access to the centralized procedure, 10 years of market exclusivity, and fee reductions.
The EMA grants PRIME designation to enhance support for the development of medicines that target an unmet medical need. The designation is based on enhanced interaction between sponsor companies and the EMA to optimize development plans and speed up evaluation so these medicines can reach patients earlier.
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to GSK2857916, an anti-B-cell maturation antigen (BCMA) monoclonal antibody conjugated to the cytotoxic agent monomethyl auristatin-F via a non-cleavable linker.
The designation is for GSK2857916 as monotherapy for patients with multiple myeloma (MM) who have failed at least 3 prior lines of therapy, including an anti-CD38 antibody, and who are refractory to a proteasome inhibitor and an immunomodulatory agent.
The designation is based on results from a phase 1, dose-escalation and expansion study in patients with relapsed/refractory MM, irrespective of BCMA expression (NCT02064387).
Data from this ongoing trial are scheduled to be presented December 11 in an oral presentation at the 59th Annual Meeting of the American Society of Hematology (ASH) in Atlanta, Georgia.
GSK2857916 has also received orphan drug designation from the FDA and the European Medicines Agency (EMA) as well as PRIME designation from the EMA.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions. The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
Orphan and PRIME designations
The FDA grants orphan designation to therapies intended to treat conditions that affect fewer than 200,000 people in the US. The designation qualifies a drug’s sponsor for various development incentives of the Orphan Drug Act, including tax credits for qualified clinical testing and 7 years of market exclusivity.
In Europe, sponsors who obtain orphan designation for a potential new medicine benefit from a range of incentives, including protocol assistance, access to the centralized procedure, 10 years of market exclusivity, and fee reductions.
The EMA grants PRIME designation to enhance support for the development of medicines that target an unmet medical need. The designation is based on enhanced interaction between sponsor companies and the EMA to optimize development plans and speed up evaluation so these medicines can reach patients earlier.
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to GSK2857916, an anti-B-cell maturation antigen (BCMA) monoclonal antibody conjugated to the cytotoxic agent monomethyl auristatin-F via a non-cleavable linker.
The designation is for GSK2857916 as monotherapy for patients with multiple myeloma (MM) who have failed at least 3 prior lines of therapy, including an anti-CD38 antibody, and who are refractory to a proteasome inhibitor and an immunomodulatory agent.
The designation is based on results from a phase 1, dose-escalation and expansion study in patients with relapsed/refractory MM, irrespective of BCMA expression (NCT02064387).
Data from this ongoing trial are scheduled to be presented December 11 in an oral presentation at the 59th Annual Meeting of the American Society of Hematology (ASH) in Atlanta, Georgia.
GSK2857916 has also received orphan drug designation from the FDA and the European Medicines Agency (EMA) as well as PRIME designation from the EMA.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions. The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
Orphan and PRIME designations
The FDA grants orphan designation to therapies intended to treat conditions that affect fewer than 200,000 people in the US. The designation qualifies a drug’s sponsor for various development incentives of the Orphan Drug Act, including tax credits for qualified clinical testing and 7 years of market exclusivity.
In Europe, sponsors who obtain orphan designation for a potential new medicine benefit from a range of incentives, including protocol assistance, access to the centralized procedure, 10 years of market exclusivity, and fee reductions.
The EMA grants PRIME designation to enhance support for the development of medicines that target an unmet medical need. The designation is based on enhanced interaction between sponsor companies and the EMA to optimize development plans and speed up evaluation so these medicines can reach patients earlier.
Cancer patients prefer computer-free interactions
SAN DIEGO—A new study suggests patients with advanced cancer may prefer doctors who do not use a computer while communicating with them.
Most of the 120 patients studied said they preferred face-to-face consultations in which a doctor used a notepad rather than a computer.
Doctors who did not use a computer were perceived as more compassionate, communicative, and professional.
These findings were presented at the 2017 Palliative and Supportive Care in Oncology Symposium (abstract 26*).
“To our knowledge, this is the only study that compares exam room interactions between people with advanced cancer and their physicians, with or without a computer present,” said study investigator Ali Haider, MD, of the University of Texas MD Anderson Cancer Center in Houston.
For this study, Dr Haider and his colleagues enrolled 120 patients with localized, recurrent, or metastatic disease. The patients’ median ECOG performance status was 2.
All patients were English speakers, they had a median age of 58 (range, 44-66), and 55% were female. Sixty-seven percent of patients were white, 18% were Hispanic, 13% were African American, and 2% were “other.” Forty-one percent of patients had completed college.
According to the Edmonton Symptom Assessment System, patients’ median pain score was 5 (range, 2-7), and their median fatigue score was 4 (range, 3-7). According to the Hospital Anxiety and Depression Scale, patients’ median anxiety score was 6 (range, 4-8), and their median depression score was 6 (range, 4-9).
The intervention
The investigators randomly assigned patients to watch different videos showing doctor-patient interactions with and without computer use. The team had filmed 4 short videos that featured actors playing the parts of doctor and patient.
All study participants were blinded to the hypothesis of the study. The actors were carefully scripted and used the same gestures, expressions, and other nonverbal communication in each video to minimize bias.
Video 1 involved Doctor A in a face-to-face consultation with just a notepad in hand, and Video 2 involved Doctor A in a consultation using a computer.
Video 3 involved Doctor B in a face-to-face consultation with just a notepad in hand, and Video 4 involved Doctor B in a consultation using a computer.
Doctors A and B looked similar, which was intended to minimize bias.
After viewing their first video, patients completed a validated questionnaire rating the doctor’s communication skills, professionalism, and compassion.
Subsequently, each group was assigned to a video topic (face-to-face or computer) they had not viewed previously featuring the doctor they had not viewed in the first video.
A follow-up questionnaire was given after this round of viewing, and the patients were also asked to rate their overall physician preference.
Results
After the first round of viewing, the patients gave better ratings to doctors (A or B) in the face-to-face videos than in the computer videos. Face-to-face doctors were rated significantly higher for compassion (P=0.0003), communication skills (P=0.0012), and professionalism (P=0.0001).
After patients had watched both videos, doctors in the face-to-face videos still had better scores for compassion, communication, and professionalism (P<0.001 for all).
Most patients (72%) said they preferred the face-to-face consultation, while 8% said they preferred the computer consultation, and 20% said they had no preference.
Dr Haider said a possible explanation for these findings is that patients with serious chronic illnesses might value undivided attention from their physicians, and patients might perceive providers using computers as more distracted or multitasking during visits.
“We know that having a good rapport with patients can be extremely beneficial for their health,” Dr Haider said. “Patients with advanced disease need the cues that come with direct interaction to help them along with their care.”
However, Dr Haider also noted that additional research is needed to confirm these results. And he said perceptions might be different in a younger population with higher computer literacy.
*Data in the abstract differ from the presentation.
SAN DIEGO—A new study suggests patients with advanced cancer may prefer doctors who do not use a computer while communicating with them.
Most of the 120 patients studied said they preferred face-to-face consultations in which a doctor used a notepad rather than a computer.
Doctors who did not use a computer were perceived as more compassionate, communicative, and professional.
These findings were presented at the 2017 Palliative and Supportive Care in Oncology Symposium (abstract 26*).
“To our knowledge, this is the only study that compares exam room interactions between people with advanced cancer and their physicians, with or without a computer present,” said study investigator Ali Haider, MD, of the University of Texas MD Anderson Cancer Center in Houston.
For this study, Dr Haider and his colleagues enrolled 120 patients with localized, recurrent, or metastatic disease. The patients’ median ECOG performance status was 2.
All patients were English speakers, they had a median age of 58 (range, 44-66), and 55% were female. Sixty-seven percent of patients were white, 18% were Hispanic, 13% were African American, and 2% were “other.” Forty-one percent of patients had completed college.
According to the Edmonton Symptom Assessment System, patients’ median pain score was 5 (range, 2-7), and their median fatigue score was 4 (range, 3-7). According to the Hospital Anxiety and Depression Scale, patients’ median anxiety score was 6 (range, 4-8), and their median depression score was 6 (range, 4-9).
The intervention
The investigators randomly assigned patients to watch different videos showing doctor-patient interactions with and without computer use. The team had filmed 4 short videos that featured actors playing the parts of doctor and patient.
All study participants were blinded to the hypothesis of the study. The actors were carefully scripted and used the same gestures, expressions, and other nonverbal communication in each video to minimize bias.
Video 1 involved Doctor A in a face-to-face consultation with just a notepad in hand, and Video 2 involved Doctor A in a consultation using a computer.
Video 3 involved Doctor B in a face-to-face consultation with just a notepad in hand, and Video 4 involved Doctor B in a consultation using a computer.
Doctors A and B looked similar, which was intended to minimize bias.
After viewing their first video, patients completed a validated questionnaire rating the doctor’s communication skills, professionalism, and compassion.
Subsequently, each group was assigned to a video topic (face-to-face or computer) they had not viewed previously featuring the doctor they had not viewed in the first video.
A follow-up questionnaire was given after this round of viewing, and the patients were also asked to rate their overall physician preference.
Results
After the first round of viewing, the patients gave better ratings to doctors (A or B) in the face-to-face videos than in the computer videos. Face-to-face doctors were rated significantly higher for compassion (P=0.0003), communication skills (P=0.0012), and professionalism (P=0.0001).
After patients had watched both videos, doctors in the face-to-face videos still had better scores for compassion, communication, and professionalism (P<0.001 for all).
Most patients (72%) said they preferred the face-to-face consultation, while 8% said they preferred the computer consultation, and 20% said they had no preference.
Dr Haider said a possible explanation for these findings is that patients with serious chronic illnesses might value undivided attention from their physicians, and patients might perceive providers using computers as more distracted or multitasking during visits.
“We know that having a good rapport with patients can be extremely beneficial for their health,” Dr Haider said. “Patients with advanced disease need the cues that come with direct interaction to help them along with their care.”
However, Dr Haider also noted that additional research is needed to confirm these results. And he said perceptions might be different in a younger population with higher computer literacy.
*Data in the abstract differ from the presentation.
SAN DIEGO—A new study suggests patients with advanced cancer may prefer doctors who do not use a computer while communicating with them.
Most of the 120 patients studied said they preferred face-to-face consultations in which a doctor used a notepad rather than a computer.
Doctors who did not use a computer were perceived as more compassionate, communicative, and professional.
These findings were presented at the 2017 Palliative and Supportive Care in Oncology Symposium (abstract 26*).
“To our knowledge, this is the only study that compares exam room interactions between people with advanced cancer and their physicians, with or without a computer present,” said study investigator Ali Haider, MD, of the University of Texas MD Anderson Cancer Center in Houston.
For this study, Dr Haider and his colleagues enrolled 120 patients with localized, recurrent, or metastatic disease. The patients’ median ECOG performance status was 2.
All patients were English speakers, they had a median age of 58 (range, 44-66), and 55% were female. Sixty-seven percent of patients were white, 18% were Hispanic, 13% were African American, and 2% were “other.” Forty-one percent of patients had completed college.
According to the Edmonton Symptom Assessment System, patients’ median pain score was 5 (range, 2-7), and their median fatigue score was 4 (range, 3-7). According to the Hospital Anxiety and Depression Scale, patients’ median anxiety score was 6 (range, 4-8), and their median depression score was 6 (range, 4-9).
The intervention
The investigators randomly assigned patients to watch different videos showing doctor-patient interactions with and without computer use. The team had filmed 4 short videos that featured actors playing the parts of doctor and patient.
All study participants were blinded to the hypothesis of the study. The actors were carefully scripted and used the same gestures, expressions, and other nonverbal communication in each video to minimize bias.
Video 1 involved Doctor A in a face-to-face consultation with just a notepad in hand, and Video 2 involved Doctor A in a consultation using a computer.
Video 3 involved Doctor B in a face-to-face consultation with just a notepad in hand, and Video 4 involved Doctor B in a consultation using a computer.
Doctors A and B looked similar, which was intended to minimize bias.
After viewing their first video, patients completed a validated questionnaire rating the doctor’s communication skills, professionalism, and compassion.
Subsequently, each group was assigned to a video topic (face-to-face or computer) they had not viewed previously featuring the doctor they had not viewed in the first video.
A follow-up questionnaire was given after this round of viewing, and the patients were also asked to rate their overall physician preference.
Results
After the first round of viewing, the patients gave better ratings to doctors (A or B) in the face-to-face videos than in the computer videos. Face-to-face doctors were rated significantly higher for compassion (P=0.0003), communication skills (P=0.0012), and professionalism (P=0.0001).
After patients had watched both videos, doctors in the face-to-face videos still had better scores for compassion, communication, and professionalism (P<0.001 for all).
Most patients (72%) said they preferred the face-to-face consultation, while 8% said they preferred the computer consultation, and 20% said they had no preference.
Dr Haider said a possible explanation for these findings is that patients with serious chronic illnesses might value undivided attention from their physicians, and patients might perceive providers using computers as more distracted or multitasking during visits.
“We know that having a good rapport with patients can be extremely beneficial for their health,” Dr Haider said. “Patients with advanced disease need the cues that come with direct interaction to help them along with their care.”
However, Dr Haider also noted that additional research is needed to confirm these results. And he said perceptions might be different in a younger population with higher computer literacy.
*Data in the abstract differ from the presentation.
Study reveals misperceptions among AML patients
SAN DIEGO—A study of acute myeloid leukemia (AML) patients has revealed misperceptions about treatment risks and the likelihood of cure.
Investigators surveyed 100 AML patients receiving intensive and non-intensive chemotherapy, as well as the patients’ oncologists.
The results showed that patients tended to overestimate both the risk of dying due to treatment and the likelihood of cure.
These findings were presented at the 2017 Palliative and Supportive Care in Oncology Symposium (abstract 43).
“Patients with AML face very challenging treatment decisions that are often placed upon them within days after being diagnosed,” said study investigator Areej El-Jawahri, MD, of Massachusetts General Hospital in Boston.
“Because they face a grave decision, they need to understand what the risks of treatment are versus the possibility of a cure.”
For this study, Dr El-Jawahri and her colleagues enrolled 50 patients who were receiving intensive care for AML (which usually meant hospitalization for 4 to 6 weeks) and 50 patients who were receiving non-intensive care (often given as outpatient treatment).
The patients’ median age was 71 (range, 60-100), and 92% were white. Six percent of patients had low-risk disease, 48% had intermediate-risk, and 46% had high-risk disease.
Within 3 days of starting treatment, both the patients and their physicians were given a questionnaire to assess how they perceived the likelihood of the patient dying from treatment.
One month later, patients and physicians completed a follow-up questionnaire to assess perceptions of patient prognosis. Within that time frame, most patients received laboratory results that more definitively established the type and stage of cancer.
At 24 weeks, the investigators asked patients if they had discussed their end-of-life wishes with their oncologists.
Results
Initially, most of the patient population (91.3%) thought it was “somewhat” or “extremely” likely they would die from their treatment. However, only 22% of treating oncologists said the same.
One month later, a majority of patients in both treatment groups thought it was “somewhat” or “extremely” likely they would be cured of their AML.
Specifically, 82.1% of patients receiving non-intensive chemotherapy said it was “somewhat” or “extremely” likely they would be cured, while 10% of their oncologists said the same.
Meanwhile, 97.6% of patients receiving intensive chemotherapy said it was “somewhat” or “extremely” likely they would be cured, and 42% of their oncologists said the same.
Overall, 77.8% of patients said they had not discussed their end-of-life wishes with their oncologists at 24 weeks.
“There were several very important factors we were not able to capture in our study, including what was actually discussed between patients and their oncologists and whether patients simply misunderstood or misheard the information conveyed to them,” Dr El-Jawahri said.
“Perhaps most importantly, we did not audio-record the discussions between the patients and their physicians, which could provide additional details regarding barriers to accurate prognostic understanding in these conversations.”
Related research and next steps
Prior to this study, Dr El-Jawahri and her colleagues had looked at similar perceptions in patients with solid tumor malignancies as well as in patients with hematologic malignancies who were receiving hematopoietic stem cell transplants.
The gaps in perception of treatment risk and cure for patients compared to their physicians were not as large in those cases as in the AML patients in this study. The investigators attribute this to higher levels of distress seen in AML patients due to the urgency of their treatment decisions.
Dr El-Jawahri and her colleagues have found that early consideration of palliative care in a treatment plan for patients with solid tumors improves patients’ understanding of the prognosis. The team hopes to implement a similar study in patients with AML.
“Clearly, there are important communication gaps between oncologists and their patients,” Dr El-Jawahri said. “We need to find ways to help physicians do a better job of communicating with their patients, especially in diseases like AML where stress levels are remarkably high.”
SAN DIEGO—A study of acute myeloid leukemia (AML) patients has revealed misperceptions about treatment risks and the likelihood of cure.
Investigators surveyed 100 AML patients receiving intensive and non-intensive chemotherapy, as well as the patients’ oncologists.
The results showed that patients tended to overestimate both the risk of dying due to treatment and the likelihood of cure.
These findings were presented at the 2017 Palliative and Supportive Care in Oncology Symposium (abstract 43).
“Patients with AML face very challenging treatment decisions that are often placed upon them within days after being diagnosed,” said study investigator Areej El-Jawahri, MD, of Massachusetts General Hospital in Boston.
“Because they face a grave decision, they need to understand what the risks of treatment are versus the possibility of a cure.”
For this study, Dr El-Jawahri and her colleagues enrolled 50 patients who were receiving intensive care for AML (which usually meant hospitalization for 4 to 6 weeks) and 50 patients who were receiving non-intensive care (often given as outpatient treatment).
The patients’ median age was 71 (range, 60-100), and 92% were white. Six percent of patients had low-risk disease, 48% had intermediate-risk, and 46% had high-risk disease.
Within 3 days of starting treatment, both the patients and their physicians were given a questionnaire to assess how they perceived the likelihood of the patient dying from treatment.
One month later, patients and physicians completed a follow-up questionnaire to assess perceptions of patient prognosis. Within that time frame, most patients received laboratory results that more definitively established the type and stage of cancer.
At 24 weeks, the investigators asked patients if they had discussed their end-of-life wishes with their oncologists.
Results
Initially, most of the patient population (91.3%) thought it was “somewhat” or “extremely” likely they would die from their treatment. However, only 22% of treating oncologists said the same.
One month later, a majority of patients in both treatment groups thought it was “somewhat” or “extremely” likely they would be cured of their AML.
Specifically, 82.1% of patients receiving non-intensive chemotherapy said it was “somewhat” or “extremely” likely they would be cured, while 10% of their oncologists said the same.
Meanwhile, 97.6% of patients receiving intensive chemotherapy said it was “somewhat” or “extremely” likely they would be cured, and 42% of their oncologists said the same.
Overall, 77.8% of patients said they had not discussed their end-of-life wishes with their oncologists at 24 weeks.
“There were several very important factors we were not able to capture in our study, including what was actually discussed between patients and their oncologists and whether patients simply misunderstood or misheard the information conveyed to them,” Dr El-Jawahri said.
“Perhaps most importantly, we did not audio-record the discussions between the patients and their physicians, which could provide additional details regarding barriers to accurate prognostic understanding in these conversations.”
Related research and next steps
Prior to this study, Dr El-Jawahri and her colleagues had looked at similar perceptions in patients with solid tumor malignancies as well as in patients with hematologic malignancies who were receiving hematopoietic stem cell transplants.
The gaps in perception of treatment risk and cure for patients compared to their physicians were not as large in those cases as in the AML patients in this study. The investigators attribute this to higher levels of distress seen in AML patients due to the urgency of their treatment decisions.
Dr El-Jawahri and her colleagues have found that early consideration of palliative care in a treatment plan for patients with solid tumors improves patients’ understanding of the prognosis. The team hopes to implement a similar study in patients with AML.
“Clearly, there are important communication gaps between oncologists and their patients,” Dr El-Jawahri said. “We need to find ways to help physicians do a better job of communicating with their patients, especially in diseases like AML where stress levels are remarkably high.”
SAN DIEGO—A study of acute myeloid leukemia (AML) patients has revealed misperceptions about treatment risks and the likelihood of cure.
Investigators surveyed 100 AML patients receiving intensive and non-intensive chemotherapy, as well as the patients’ oncologists.
The results showed that patients tended to overestimate both the risk of dying due to treatment and the likelihood of cure.
These findings were presented at the 2017 Palliative and Supportive Care in Oncology Symposium (abstract 43).
“Patients with AML face very challenging treatment decisions that are often placed upon them within days after being diagnosed,” said study investigator Areej El-Jawahri, MD, of Massachusetts General Hospital in Boston.
“Because they face a grave decision, they need to understand what the risks of treatment are versus the possibility of a cure.”
For this study, Dr El-Jawahri and her colleagues enrolled 50 patients who were receiving intensive care for AML (which usually meant hospitalization for 4 to 6 weeks) and 50 patients who were receiving non-intensive care (often given as outpatient treatment).
The patients’ median age was 71 (range, 60-100), and 92% were white. Six percent of patients had low-risk disease, 48% had intermediate-risk, and 46% had high-risk disease.
Within 3 days of starting treatment, both the patients and their physicians were given a questionnaire to assess how they perceived the likelihood of the patient dying from treatment.
One month later, patients and physicians completed a follow-up questionnaire to assess perceptions of patient prognosis. Within that time frame, most patients received laboratory results that more definitively established the type and stage of cancer.
At 24 weeks, the investigators asked patients if they had discussed their end-of-life wishes with their oncologists.
Results
Initially, most of the patient population (91.3%) thought it was “somewhat” or “extremely” likely they would die from their treatment. However, only 22% of treating oncologists said the same.
One month later, a majority of patients in both treatment groups thought it was “somewhat” or “extremely” likely they would be cured of their AML.
Specifically, 82.1% of patients receiving non-intensive chemotherapy said it was “somewhat” or “extremely” likely they would be cured, while 10% of their oncologists said the same.
Meanwhile, 97.6% of patients receiving intensive chemotherapy said it was “somewhat” or “extremely” likely they would be cured, and 42% of their oncologists said the same.
Overall, 77.8% of patients said they had not discussed their end-of-life wishes with their oncologists at 24 weeks.
“There were several very important factors we were not able to capture in our study, including what was actually discussed between patients and their oncologists and whether patients simply misunderstood or misheard the information conveyed to them,” Dr El-Jawahri said.
“Perhaps most importantly, we did not audio-record the discussions between the patients and their physicians, which could provide additional details regarding barriers to accurate prognostic understanding in these conversations.”
Related research and next steps
Prior to this study, Dr El-Jawahri and her colleagues had looked at similar perceptions in patients with solid tumor malignancies as well as in patients with hematologic malignancies who were receiving hematopoietic stem cell transplants.
The gaps in perception of treatment risk and cure for patients compared to their physicians were not as large in those cases as in the AML patients in this study. The investigators attribute this to higher levels of distress seen in AML patients due to the urgency of their treatment decisions.
Dr El-Jawahri and her colleagues have found that early consideration of palliative care in a treatment plan for patients with solid tumors improves patients’ understanding of the prognosis. The team hopes to implement a similar study in patients with AML.
“Clearly, there are important communication gaps between oncologists and their patients,” Dr El-Jawahri said. “We need to find ways to help physicians do a better job of communicating with their patients, especially in diseases like AML where stress levels are remarkably high.”