User login
FDA approves first CAR T-cell therapy to treat ALL
The US Food and Drug Administration (FDA) has approved the first chimeric antigen receptor (CAR) T-cell therapy, tisagenlecleucel (KymriahTM, formerly CTL019).
The therapy is approved for use in children and young adults up to 25 years of age who have B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse.
Tisagenlecleucel consists of autologous T cells expressing a CD19-specific CAR.
The therapy was first developed by the University of Pennsylvania. In 2012, the university and Novartis entered into a global collaboration to further research, develop, and commercialize CAR T-cell therapies. Novartis holds the worldwide rights to tisagenlecleucel and other therapies developed through the collaboration.
The application for tisagenlecleucel was supported by results from 3 clinical trials:
- A pilot study presented at the 2015 ASH Annual Meeting
- The phase 2 ENSIGN trial, which was presented at the 2016 ASH Annual Meeting
- The phase 2 ELIANA study, which was recently presented at the 22nd Congress of the European Hematology Association (EHA).
Safety concerns
The prescribing information for tisagenlecleucel includes a boxed warning noting that the treatment poses a risk of cytokine release syndrome (CRS) and neurological toxicity, both of which can be life-threatening.
Because of the risk of CRS, the FDA has expanded the approved use of tocilizumab (Actemra) to include treatment of CAR T-cell-induced severe or life-threatening CRS in patients age 2 and older.
The risk of CRS and neurological toxicity also prompted the FDA to approve tisagenlecleucel with a risk evaluation and mitigation strategy (REMS), which includes elements to assure safe use.
The FDA is requiring that hospitals and their associated clinics that dispense tisagenlecleucel be specially certified. As part of that certification, staff involved in the prescribing, dispensing, or administration of tisagenlecleucel are required to be trained to recognize and manage CRS and neurological events.
Additionally, the certified healthcare settings are required to have protocols in place to ensure that tisagenlecleucel is only given to patients after verifying that tocilizumab is available for immediate administration.
The REMS program specifies that patients be informed of the signs and symptoms of CRS and neurological toxicities following infusion and of the importance of promptly returning to the treatment site if they develop fever or other adverse reactions after receiving tisagenlecleucel.
To further evaluate the long-term safety of tisagenlecleucel, Novartis is required to conduct a post-marketing observational study involving patients who received the treatment.
Access and cost
Tisagenlecleucel will be manufactured for each individual patient at Novartis’s facility in Morris Plains, New Jersey.
Novartis said it has designed a manufacturing and supply chain platform that allows for an individualized treatment approach on a global scale. This process includes cryopreservation of a patient’s harvested cells, providing the flexibility to initiate treatment with tisagenlecleucel based on the individual patient’s condition.
Tisagenlecleucel will reportedly cost $475,000 for a single course of treatment. However, Novartis said it will help patients navigate insurance coverage and provide financial assistance for those who are uninsured or underinsured.
In addition, patients will only be required to pay for tisagenlecleucel if they respond within a month of receiving the treatment. This is a result of a collaboration between Novartis and the US Centers for Medicare and Medicaid Services that is focused on delivering value-based care. The approach is intended to include indication-based pricing for medicines and supports payments for a medicine based on the clinical outcomes achieved. ![]()
The US Food and Drug Administration (FDA) has approved the first chimeric antigen receptor (CAR) T-cell therapy, tisagenlecleucel (KymriahTM, formerly CTL019).
The therapy is approved for use in children and young adults up to 25 years of age who have B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse.
Tisagenlecleucel consists of autologous T cells expressing a CD19-specific CAR.
The therapy was first developed by the University of Pennsylvania. In 2012, the university and Novartis entered into a global collaboration to further research, develop, and commercialize CAR T-cell therapies. Novartis holds the worldwide rights to tisagenlecleucel and other therapies developed through the collaboration.
The application for tisagenlecleucel was supported by results from 3 clinical trials:
- A pilot study presented at the 2015 ASH Annual Meeting
- The phase 2 ENSIGN trial, which was presented at the 2016 ASH Annual Meeting
- The phase 2 ELIANA study, which was recently presented at the 22nd Congress of the European Hematology Association (EHA).
Safety concerns
The prescribing information for tisagenlecleucel includes a boxed warning noting that the treatment poses a risk of cytokine release syndrome (CRS) and neurological toxicity, both of which can be life-threatening.
Because of the risk of CRS, the FDA has expanded the approved use of tocilizumab (Actemra) to include treatment of CAR T-cell-induced severe or life-threatening CRS in patients age 2 and older.
The risk of CRS and neurological toxicity also prompted the FDA to approve tisagenlecleucel with a risk evaluation and mitigation strategy (REMS), which includes elements to assure safe use.
The FDA is requiring that hospitals and their associated clinics that dispense tisagenlecleucel be specially certified. As part of that certification, staff involved in the prescribing, dispensing, or administration of tisagenlecleucel are required to be trained to recognize and manage CRS and neurological events.
Additionally, the certified healthcare settings are required to have protocols in place to ensure that tisagenlecleucel is only given to patients after verifying that tocilizumab is available for immediate administration.
The REMS program specifies that patients be informed of the signs and symptoms of CRS and neurological toxicities following infusion and of the importance of promptly returning to the treatment site if they develop fever or other adverse reactions after receiving tisagenlecleucel.
To further evaluate the long-term safety of tisagenlecleucel, Novartis is required to conduct a post-marketing observational study involving patients who received the treatment.
Access and cost
Tisagenlecleucel will be manufactured for each individual patient at Novartis’s facility in Morris Plains, New Jersey.
Novartis said it has designed a manufacturing and supply chain platform that allows for an individualized treatment approach on a global scale. This process includes cryopreservation of a patient’s harvested cells, providing the flexibility to initiate treatment with tisagenlecleucel based on the individual patient’s condition.
Tisagenlecleucel will reportedly cost $475,000 for a single course of treatment. However, Novartis said it will help patients navigate insurance coverage and provide financial assistance for those who are uninsured or underinsured.
In addition, patients will only be required to pay for tisagenlecleucel if they respond within a month of receiving the treatment. This is a result of a collaboration between Novartis and the US Centers for Medicare and Medicaid Services that is focused on delivering value-based care. The approach is intended to include indication-based pricing for medicines and supports payments for a medicine based on the clinical outcomes achieved. ![]()
The US Food and Drug Administration (FDA) has approved the first chimeric antigen receptor (CAR) T-cell therapy, tisagenlecleucel (KymriahTM, formerly CTL019).
The therapy is approved for use in children and young adults up to 25 years of age who have B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse.
Tisagenlecleucel consists of autologous T cells expressing a CD19-specific CAR.
The therapy was first developed by the University of Pennsylvania. In 2012, the university and Novartis entered into a global collaboration to further research, develop, and commercialize CAR T-cell therapies. Novartis holds the worldwide rights to tisagenlecleucel and other therapies developed through the collaboration.
The application for tisagenlecleucel was supported by results from 3 clinical trials:
- A pilot study presented at the 2015 ASH Annual Meeting
- The phase 2 ENSIGN trial, which was presented at the 2016 ASH Annual Meeting
- The phase 2 ELIANA study, which was recently presented at the 22nd Congress of the European Hematology Association (EHA).
Safety concerns
The prescribing information for tisagenlecleucel includes a boxed warning noting that the treatment poses a risk of cytokine release syndrome (CRS) and neurological toxicity, both of which can be life-threatening.
Because of the risk of CRS, the FDA has expanded the approved use of tocilizumab (Actemra) to include treatment of CAR T-cell-induced severe or life-threatening CRS in patients age 2 and older.
The risk of CRS and neurological toxicity also prompted the FDA to approve tisagenlecleucel with a risk evaluation and mitigation strategy (REMS), which includes elements to assure safe use.
The FDA is requiring that hospitals and their associated clinics that dispense tisagenlecleucel be specially certified. As part of that certification, staff involved in the prescribing, dispensing, or administration of tisagenlecleucel are required to be trained to recognize and manage CRS and neurological events.
Additionally, the certified healthcare settings are required to have protocols in place to ensure that tisagenlecleucel is only given to patients after verifying that tocilizumab is available for immediate administration.
The REMS program specifies that patients be informed of the signs and symptoms of CRS and neurological toxicities following infusion and of the importance of promptly returning to the treatment site if they develop fever or other adverse reactions after receiving tisagenlecleucel.
To further evaluate the long-term safety of tisagenlecleucel, Novartis is required to conduct a post-marketing observational study involving patients who received the treatment.
Access and cost
Tisagenlecleucel will be manufactured for each individual patient at Novartis’s facility in Morris Plains, New Jersey.
Novartis said it has designed a manufacturing and supply chain platform that allows for an individualized treatment approach on a global scale. This process includes cryopreservation of a patient’s harvested cells, providing the flexibility to initiate treatment with tisagenlecleucel based on the individual patient’s condition.
Tisagenlecleucel will reportedly cost $475,000 for a single course of treatment. However, Novartis said it will help patients navigate insurance coverage and provide financial assistance for those who are uninsured or underinsured.
In addition, patients will only be required to pay for tisagenlecleucel if they respond within a month of receiving the treatment. This is a result of a collaboration between Novartis and the US Centers for Medicare and Medicaid Services that is focused on delivering value-based care. The approach is intended to include indication-based pricing for medicines and supports payments for a medicine based on the clinical outcomes achieved. ![]()
FDA approves drug to treat CRS induced by CAR T-cell therapy
The US Food and Drug Administration (FDA) has approved tocilizumab (Actemra®) for the treatment of patients age 2 and older who have severe or life-threatening cytokine release syndrome (CRS) induced by chimeric antigen receptor (CAR) T-cell therapy.
Tocilizumab is a humanized interleukin-6 receptor antagonist.
The drug is also FDA-approved to treat adults with rheumatoid arthritis or giant cell arteritis and patients age 2 and older with polyarticular juvenile idiopathic arthritis or systemic juvenile idiopathic arthritis.
The full prescribing information for tocilizumab, which includes a boxed warning about the risk of serious infections, is available at http://www.actemra.com. The drug is jointly developed by Genentech (a member of the Roche Group) and Chugai Pharmaceutical Co.
The FDA’s latest approval of tocilizumab coincided with the FDA’s approval of the CAR T-cell therapy tisagenlecleucel (Kymriah, formerly CTL019) to treat pediatric and young adult patients with relapsed or refractory B-cell precursor acute lymphoblastic leukemia.
According to Genentech, the FDA’s decision to expand the approval of tocilizumab is based on a retrospective analysis of pooled outcome data from clinical trials of CAR T-cell therapies in patients with hematologic malignancies.
For this analysis, researchers assessed 45 pediatric and adult patients treated with tocilizumab, with or without additional high-dose corticosteroids, for severe or life-threatening CRS.
Thirty-one patients (69%) achieved a response, defined as resolution of CRS within 14 days of the first dose of tocilizumab.
No more than 2 doses of tocilizumab were needed, and no drugs other than tocilizumab and corticosteroids were used for treatment.
No adverse reactions related to tocilizumab were reported. ![]()
The US Food and Drug Administration (FDA) has approved tocilizumab (Actemra®) for the treatment of patients age 2 and older who have severe or life-threatening cytokine release syndrome (CRS) induced by chimeric antigen receptor (CAR) T-cell therapy.
Tocilizumab is a humanized interleukin-6 receptor antagonist.
The drug is also FDA-approved to treat adults with rheumatoid arthritis or giant cell arteritis and patients age 2 and older with polyarticular juvenile idiopathic arthritis or systemic juvenile idiopathic arthritis.
The full prescribing information for tocilizumab, which includes a boxed warning about the risk of serious infections, is available at http://www.actemra.com. The drug is jointly developed by Genentech (a member of the Roche Group) and Chugai Pharmaceutical Co.
The FDA’s latest approval of tocilizumab coincided with the FDA’s approval of the CAR T-cell therapy tisagenlecleucel (Kymriah, formerly CTL019) to treat pediatric and young adult patients with relapsed or refractory B-cell precursor acute lymphoblastic leukemia.
According to Genentech, the FDA’s decision to expand the approval of tocilizumab is based on a retrospective analysis of pooled outcome data from clinical trials of CAR T-cell therapies in patients with hematologic malignancies.
For this analysis, researchers assessed 45 pediatric and adult patients treated with tocilizumab, with or without additional high-dose corticosteroids, for severe or life-threatening CRS.
Thirty-one patients (69%) achieved a response, defined as resolution of CRS within 14 days of the first dose of tocilizumab.
No more than 2 doses of tocilizumab were needed, and no drugs other than tocilizumab and corticosteroids were used for treatment.
No adverse reactions related to tocilizumab were reported. ![]()
The US Food and Drug Administration (FDA) has approved tocilizumab (Actemra®) for the treatment of patients age 2 and older who have severe or life-threatening cytokine release syndrome (CRS) induced by chimeric antigen receptor (CAR) T-cell therapy.
Tocilizumab is a humanized interleukin-6 receptor antagonist.
The drug is also FDA-approved to treat adults with rheumatoid arthritis or giant cell arteritis and patients age 2 and older with polyarticular juvenile idiopathic arthritis or systemic juvenile idiopathic arthritis.
The full prescribing information for tocilizumab, which includes a boxed warning about the risk of serious infections, is available at http://www.actemra.com. The drug is jointly developed by Genentech (a member of the Roche Group) and Chugai Pharmaceutical Co.
The FDA’s latest approval of tocilizumab coincided with the FDA’s approval of the CAR T-cell therapy tisagenlecleucel (Kymriah, formerly CTL019) to treat pediatric and young adult patients with relapsed or refractory B-cell precursor acute lymphoblastic leukemia.
According to Genentech, the FDA’s decision to expand the approval of tocilizumab is based on a retrospective analysis of pooled outcome data from clinical trials of CAR T-cell therapies in patients with hematologic malignancies.
For this analysis, researchers assessed 45 pediatric and adult patients treated with tocilizumab, with or without additional high-dose corticosteroids, for severe or life-threatening CRS.
Thirty-one patients (69%) achieved a response, defined as resolution of CRS within 14 days of the first dose of tocilizumab.
No more than 2 doses of tocilizumab were needed, and no drugs other than tocilizumab and corticosteroids were used for treatment.
No adverse reactions related to tocilizumab were reported. ![]()
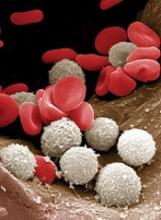
Protein may be target for improving HSCT
New research published in The Journal of Clinical Investigation suggests the protein Del-1 regulates the hematopoietic stem cell (HSC) niche.
Researchers therefore believe that targeting Del-1 could be an effective way to improve HSC transplants (HSCTs) for donors and recipients.
There may also be ways to modulate levels of Del-1 to enhance immune cell production in patients with certain hematologic malignancies.
“Because the hematopoietic stem cell niche is so important for the creation of bone marrow and blood cells and because Del-1 is a soluble protein and is easily manipulated, one can see that it could be a target in many potential applications,” said study author George Hajishengallis, DDS, PhD, of the University of Pennsylvania School of Dental Medicine in Philadelphia.
“I think that Del-1 represents a major regulator of the hematopoietic stem cell niche,” added study author Triantafyllos Chavakis, MD, PhD, of the Technical University of Dresden in Germany. “It will be worthwhile to study its expression in the context of hematopoietic malignancy.”
This research began when Drs Hajishengallis and Chavakis identified Del-1 as a potential drug target for gum disease. They found the protein prevents inflammatory cells from moving into the gums.
Both researchers and their labs also discovered that Del-1 was expressed in the bone marrow as well. So the researchers began following up to determine the protein’s function there.
“In the beginning, I thought it would have a simple function, like regulating the exit of mature leukocytes from the marrow into the periphery, something analogous to what it was doing in the gingiva,” Dr Hajishengallis said. “But it turned out it had a much more important and global role than what I had imagined.”
The researchers’ investigations revealed that Del-1 was expressed by at least 3 cell types that support HSCs: arteriolar endothelial cells, CXCL12-abundant reticular cells, and cells of the osteoblastic lineage.
Using mice deficient in Del-1, the researchers found the protein promotes proliferation and differentiation of HSCs, sending more progenitor cells down a path toward becoming myeloid cells rather than lymphocytes.
In HSCT experiments, the team discovered the presence of Del-1 in recipient bone marrow is required for the transplanted HSCs to engraft in the recipient and to facilitate the process of myelopoiesis.
When the researchers mimicked a systemic infection in mice, animals deficient in Del-1 were slower to begin making myeloid cells again compared to mice with normal Del-1 levels.
“We saw roles for Del-1 in both steady-state and emergency conditions,” Dr Hajishengallis said.
He and his colleagues also identified the protein with which Del-1 interacts, the ß3 integrin, perhaps pointing to a target for therapeutic interventions down the line.
The researchers see potential applications in HSCTs, for both donors and recipients.
In donors, blocking the interaction between Del-1 and HSCs could enhance the mobilization of those progenitors into the bloodstream. This could be helpful for increasing donor cell numbers for transplantation.
HSCT recipients, on the other hand, may need enhanced Del-1 interaction to ensure the transplanted cells engraft and begin making new blood cells more rapidly.
In addition, people undergoing chemotherapy who develop febrile neutropenia might benefit from the role of Del-1 in supporting the production of immune-related blood cells such as neutrophils.
“It’s easy to think of practical applications for these findings,” Dr Hajishengallis said. “Now, we need to find out whether it works in practice, so our studies continue.” ![]()
New research published in The Journal of Clinical Investigation suggests the protein Del-1 regulates the hematopoietic stem cell (HSC) niche.
Researchers therefore believe that targeting Del-1 could be an effective way to improve HSC transplants (HSCTs) for donors and recipients.
There may also be ways to modulate levels of Del-1 to enhance immune cell production in patients with certain hematologic malignancies.
“Because the hematopoietic stem cell niche is so important for the creation of bone marrow and blood cells and because Del-1 is a soluble protein and is easily manipulated, one can see that it could be a target in many potential applications,” said study author George Hajishengallis, DDS, PhD, of the University of Pennsylvania School of Dental Medicine in Philadelphia.
“I think that Del-1 represents a major regulator of the hematopoietic stem cell niche,” added study author Triantafyllos Chavakis, MD, PhD, of the Technical University of Dresden in Germany. “It will be worthwhile to study its expression in the context of hematopoietic malignancy.”
This research began when Drs Hajishengallis and Chavakis identified Del-1 as a potential drug target for gum disease. They found the protein prevents inflammatory cells from moving into the gums.
Both researchers and their labs also discovered that Del-1 was expressed in the bone marrow as well. So the researchers began following up to determine the protein’s function there.
“In the beginning, I thought it would have a simple function, like regulating the exit of mature leukocytes from the marrow into the periphery, something analogous to what it was doing in the gingiva,” Dr Hajishengallis said. “But it turned out it had a much more important and global role than what I had imagined.”
The researchers’ investigations revealed that Del-1 was expressed by at least 3 cell types that support HSCs: arteriolar endothelial cells, CXCL12-abundant reticular cells, and cells of the osteoblastic lineage.
Using mice deficient in Del-1, the researchers found the protein promotes proliferation and differentiation of HSCs, sending more progenitor cells down a path toward becoming myeloid cells rather than lymphocytes.
In HSCT experiments, the team discovered the presence of Del-1 in recipient bone marrow is required for the transplanted HSCs to engraft in the recipient and to facilitate the process of myelopoiesis.
When the researchers mimicked a systemic infection in mice, animals deficient in Del-1 were slower to begin making myeloid cells again compared to mice with normal Del-1 levels.
“We saw roles for Del-1 in both steady-state and emergency conditions,” Dr Hajishengallis said.
He and his colleagues also identified the protein with which Del-1 interacts, the ß3 integrin, perhaps pointing to a target for therapeutic interventions down the line.
The researchers see potential applications in HSCTs, for both donors and recipients.
In donors, blocking the interaction between Del-1 and HSCs could enhance the mobilization of those progenitors into the bloodstream. This could be helpful for increasing donor cell numbers for transplantation.
HSCT recipients, on the other hand, may need enhanced Del-1 interaction to ensure the transplanted cells engraft and begin making new blood cells more rapidly.
In addition, people undergoing chemotherapy who develop febrile neutropenia might benefit from the role of Del-1 in supporting the production of immune-related blood cells such as neutrophils.
“It’s easy to think of practical applications for these findings,” Dr Hajishengallis said. “Now, we need to find out whether it works in practice, so our studies continue.” ![]()
New research published in The Journal of Clinical Investigation suggests the protein Del-1 regulates the hematopoietic stem cell (HSC) niche.
Researchers therefore believe that targeting Del-1 could be an effective way to improve HSC transplants (HSCTs) for donors and recipients.
There may also be ways to modulate levels of Del-1 to enhance immune cell production in patients with certain hematologic malignancies.
“Because the hematopoietic stem cell niche is so important for the creation of bone marrow and blood cells and because Del-1 is a soluble protein and is easily manipulated, one can see that it could be a target in many potential applications,” said study author George Hajishengallis, DDS, PhD, of the University of Pennsylvania School of Dental Medicine in Philadelphia.
“I think that Del-1 represents a major regulator of the hematopoietic stem cell niche,” added study author Triantafyllos Chavakis, MD, PhD, of the Technical University of Dresden in Germany. “It will be worthwhile to study its expression in the context of hematopoietic malignancy.”
This research began when Drs Hajishengallis and Chavakis identified Del-1 as a potential drug target for gum disease. They found the protein prevents inflammatory cells from moving into the gums.
Both researchers and their labs also discovered that Del-1 was expressed in the bone marrow as well. So the researchers began following up to determine the protein’s function there.
“In the beginning, I thought it would have a simple function, like regulating the exit of mature leukocytes from the marrow into the periphery, something analogous to what it was doing in the gingiva,” Dr Hajishengallis said. “But it turned out it had a much more important and global role than what I had imagined.”
The researchers’ investigations revealed that Del-1 was expressed by at least 3 cell types that support HSCs: arteriolar endothelial cells, CXCL12-abundant reticular cells, and cells of the osteoblastic lineage.
Using mice deficient in Del-1, the researchers found the protein promotes proliferation and differentiation of HSCs, sending more progenitor cells down a path toward becoming myeloid cells rather than lymphocytes.
In HSCT experiments, the team discovered the presence of Del-1 in recipient bone marrow is required for the transplanted HSCs to engraft in the recipient and to facilitate the process of myelopoiesis.
When the researchers mimicked a systemic infection in mice, animals deficient in Del-1 were slower to begin making myeloid cells again compared to mice with normal Del-1 levels.
“We saw roles for Del-1 in both steady-state and emergency conditions,” Dr Hajishengallis said.
He and his colleagues also identified the protein with which Del-1 interacts, the ß3 integrin, perhaps pointing to a target for therapeutic interventions down the line.
The researchers see potential applications in HSCTs, for both donors and recipients.
In donors, blocking the interaction between Del-1 and HSCs could enhance the mobilization of those progenitors into the bloodstream. This could be helpful for increasing donor cell numbers for transplantation.
HSCT recipients, on the other hand, may need enhanced Del-1 interaction to ensure the transplanted cells engraft and begin making new blood cells more rapidly.
In addition, people undergoing chemotherapy who develop febrile neutropenia might benefit from the role of Del-1 in supporting the production of immune-related blood cells such as neutrophils.
“It’s easy to think of practical applications for these findings,” Dr Hajishengallis said. “Now, we need to find out whether it works in practice, so our studies continue.” ![]()
Study: Two antithrombotic drugs better than 3
BARCELONA—A new study suggests a combination of 2 antithrombotic drugs is as effective as, but safer than, a 3-drug combination for patients with atrial fibrillation who have undergone percutaneous coronary intervention (PCI).
The combinations were similarly effective in preventing thromboembolic events, unplanned revascularization, or death.
But the 2-drug combination—dabigatran plus clopidogrel/ticagrelor—reduced the risk of major or clinically relevant non-major bleeding when compared to the 3-drug combination—warfarin plus aspirin and clopidogrel/ticagrelor.
These results were presented at ESC Congress 2017 (abstract 1920) and published in NEJM. The trial, known as RE-DUAL PCI, was sponsored by Boehringer Ingelheim, makers of dabigatran.
“When we treat patients who have atrial fibrillation and need a stent, we need to strike a difficult balance between risk of clotting and risk of bleeding,” said study author Christopher Cannon, MD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“Our study finds that patients who received 2 anticlotting medications—including one of a newer class of drug—had fewer bleeding events without being more at risk for a stroke or other cardiac events.”
Patients and treatment
The RE-DUAL PCI trial included 2725 patients with atrial fibrillation who had undergone PCI. Patients were randomized to receive the 3-drug combination or the 2-drug combination. The 2-drug combination included 2 different doses of dabigatran—110 mg or 150 mg twice daily.
The researchers compared the 100-mg dual-therapy group (n=981) to the entire triple-therapy group (n=981), and they compared the 150-mg dual-therapy group (n=763) to a corresponding triple-therapy group (n=764).
The corresponding triple-therapy group only included patients who had been eligible for the 150-mg dual-therapy group, meaning this group did not include elderly patients outside the US.
Results
The primary endpoint was the first major or clinically relevant non-major bleeding event.
The incidence of this endpoint was 15.4% in the 110-mg dual-therapy group and 26.9% in the triple-therapy group (hazard ratio [HR]=0.52, P<0.001 for non-inferiority, P<0.001 for superiority).
The incidence was 20.2% in the 150-mg dual-therapy group and 25.7% in the corresponding triple-therapy group (HR=0.72, P<0.001 for non-inferiority).
A main secondary endpoint was a composite efficacy endpoint of thromboembolic events (myocardial infarction, stroke, or systemic embolism), unplanned revascularization (PCI or coronary-artery bypass grafting), or death.
The incidence of this endpoint was 15.2% in the 110-mg dual-therapy group and 13.4% in the triple-therapy group (HR=1.13, P=0.30). And it was 11.8% in the 150-mg dual-therapy group and 12.8% in the corresponding triple-therapy group (HR=0.89, P=0.44).
The incidence was 13.7% in the 2 dual-therapy groups combined and 13.4% in the triple-therapy group (HR=1.04. P=0.005 for non-inferiority).
Serious adverse events during treatment occurred in 42.7% of the patients in the 110-mg dual-therapy group, 39.6% in the 150-mg dual-therapy group, and 41.8% in the triple-therapy group.
Fatal serious adverse events occurred during treatment in 3.9%, 3.2%, and 4.3%, respectively.
“These data are very reassuring,” Dr Cannon said. “We now have new information to help select the right treatment for individual patients, which has been hard to date, and this study can help.” ![]()
BARCELONA—A new study suggests a combination of 2 antithrombotic drugs is as effective as, but safer than, a 3-drug combination for patients with atrial fibrillation who have undergone percutaneous coronary intervention (PCI).
The combinations were similarly effective in preventing thromboembolic events, unplanned revascularization, or death.
But the 2-drug combination—dabigatran plus clopidogrel/ticagrelor—reduced the risk of major or clinically relevant non-major bleeding when compared to the 3-drug combination—warfarin plus aspirin and clopidogrel/ticagrelor.
These results were presented at ESC Congress 2017 (abstract 1920) and published in NEJM. The trial, known as RE-DUAL PCI, was sponsored by Boehringer Ingelheim, makers of dabigatran.
“When we treat patients who have atrial fibrillation and need a stent, we need to strike a difficult balance between risk of clotting and risk of bleeding,” said study author Christopher Cannon, MD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“Our study finds that patients who received 2 anticlotting medications—including one of a newer class of drug—had fewer bleeding events without being more at risk for a stroke or other cardiac events.”
Patients and treatment
The RE-DUAL PCI trial included 2725 patients with atrial fibrillation who had undergone PCI. Patients were randomized to receive the 3-drug combination or the 2-drug combination. The 2-drug combination included 2 different doses of dabigatran—110 mg or 150 mg twice daily.
The researchers compared the 100-mg dual-therapy group (n=981) to the entire triple-therapy group (n=981), and they compared the 150-mg dual-therapy group (n=763) to a corresponding triple-therapy group (n=764).
The corresponding triple-therapy group only included patients who had been eligible for the 150-mg dual-therapy group, meaning this group did not include elderly patients outside the US.
Results
The primary endpoint was the first major or clinically relevant non-major bleeding event.
The incidence of this endpoint was 15.4% in the 110-mg dual-therapy group and 26.9% in the triple-therapy group (hazard ratio [HR]=0.52, P<0.001 for non-inferiority, P<0.001 for superiority).
The incidence was 20.2% in the 150-mg dual-therapy group and 25.7% in the corresponding triple-therapy group (HR=0.72, P<0.001 for non-inferiority).
A main secondary endpoint was a composite efficacy endpoint of thromboembolic events (myocardial infarction, stroke, or systemic embolism), unplanned revascularization (PCI or coronary-artery bypass grafting), or death.
The incidence of this endpoint was 15.2% in the 110-mg dual-therapy group and 13.4% in the triple-therapy group (HR=1.13, P=0.30). And it was 11.8% in the 150-mg dual-therapy group and 12.8% in the corresponding triple-therapy group (HR=0.89, P=0.44).
The incidence was 13.7% in the 2 dual-therapy groups combined and 13.4% in the triple-therapy group (HR=1.04. P=0.005 for non-inferiority).
Serious adverse events during treatment occurred in 42.7% of the patients in the 110-mg dual-therapy group, 39.6% in the 150-mg dual-therapy group, and 41.8% in the triple-therapy group.
Fatal serious adverse events occurred during treatment in 3.9%, 3.2%, and 4.3%, respectively.
“These data are very reassuring,” Dr Cannon said. “We now have new information to help select the right treatment for individual patients, which has been hard to date, and this study can help.” ![]()
BARCELONA—A new study suggests a combination of 2 antithrombotic drugs is as effective as, but safer than, a 3-drug combination for patients with atrial fibrillation who have undergone percutaneous coronary intervention (PCI).
The combinations were similarly effective in preventing thromboembolic events, unplanned revascularization, or death.
But the 2-drug combination—dabigatran plus clopidogrel/ticagrelor—reduced the risk of major or clinically relevant non-major bleeding when compared to the 3-drug combination—warfarin plus aspirin and clopidogrel/ticagrelor.
These results were presented at ESC Congress 2017 (abstract 1920) and published in NEJM. The trial, known as RE-DUAL PCI, was sponsored by Boehringer Ingelheim, makers of dabigatran.
“When we treat patients who have atrial fibrillation and need a stent, we need to strike a difficult balance between risk of clotting and risk of bleeding,” said study author Christopher Cannon, MD, of Brigham and Women’s Hospital in Boston, Massachusetts.
“Our study finds that patients who received 2 anticlotting medications—including one of a newer class of drug—had fewer bleeding events without being more at risk for a stroke or other cardiac events.”
Patients and treatment
The RE-DUAL PCI trial included 2725 patients with atrial fibrillation who had undergone PCI. Patients were randomized to receive the 3-drug combination or the 2-drug combination. The 2-drug combination included 2 different doses of dabigatran—110 mg or 150 mg twice daily.
The researchers compared the 100-mg dual-therapy group (n=981) to the entire triple-therapy group (n=981), and they compared the 150-mg dual-therapy group (n=763) to a corresponding triple-therapy group (n=764).
The corresponding triple-therapy group only included patients who had been eligible for the 150-mg dual-therapy group, meaning this group did not include elderly patients outside the US.
Results
The primary endpoint was the first major or clinically relevant non-major bleeding event.
The incidence of this endpoint was 15.4% in the 110-mg dual-therapy group and 26.9% in the triple-therapy group (hazard ratio [HR]=0.52, P<0.001 for non-inferiority, P<0.001 for superiority).
The incidence was 20.2% in the 150-mg dual-therapy group and 25.7% in the corresponding triple-therapy group (HR=0.72, P<0.001 for non-inferiority).
A main secondary endpoint was a composite efficacy endpoint of thromboembolic events (myocardial infarction, stroke, or systemic embolism), unplanned revascularization (PCI or coronary-artery bypass grafting), or death.
The incidence of this endpoint was 15.2% in the 110-mg dual-therapy group and 13.4% in the triple-therapy group (HR=1.13, P=0.30). And it was 11.8% in the 150-mg dual-therapy group and 12.8% in the corresponding triple-therapy group (HR=0.89, P=0.44).
The incidence was 13.7% in the 2 dual-therapy groups combined and 13.4% in the triple-therapy group (HR=1.04. P=0.005 for non-inferiority).
Serious adverse events during treatment occurred in 42.7% of the patients in the 110-mg dual-therapy group, 39.6% in the 150-mg dual-therapy group, and 41.8% in the triple-therapy group.
Fatal serious adverse events occurred during treatment in 3.9%, 3.2%, and 4.3%, respectively.
“These data are very reassuring,” Dr Cannon said. “We now have new information to help select the right treatment for individual patients, which has been hard to date, and this study can help.” ![]()
CNS lymphoma responds to CAR T-cell therapy
Researchers have reported the first known case of central nervous system (CNS) lymphoma responding to chimeric antigen receptor (CAR) T-cell therapy.
The investigational CAR T-cell therapy JCAR017 induced complete remission of brain metastasis in a patient with refractory diffuse large B-cell lymphoma (DLBCL).
When a subcutaneous tumor began to recur 2 months after the patient received JCAR017 and a surgical biopsy was performed, the CAR T cells spontaneously re-expanded and the tumor again went into remission.
While the patient eventually relapsed and died more than a year after receiving JCAR017, the brain tumor never recurred.
“Brain involvement in DLBCL carries a grave prognosis, and the ability to induce a complete and durable response with conventional therapies is rare,” said Jeremy Abramson, MD, of Massachusetts General Hospital in Boston.
“In addition, all available CAR T-cell trials have excluded patients with central nervous system involvement. This result has implications not only for secondary DLBCL like this case but also for primary central nervous system lymphoma, for which treatment options are similarly limited after relapse and few patents are cured.”
Dr Abramson and his colleagues described this case in a letter to NEJM. The patient was involved in a trial of JCAR017, which was sponsored by Juno Therapeutics.
The patient was a 68-year-old woman with germinal center B-cell-like DLBCL with a BCL2 rearrangement and multiple copies of MYC and BCL6.
The patients’ disease was refractory to conventional chemotherapy and an 8/8 HLA-matched stem cell transplant. After she enrolled in a phase 1 trial of JCAR017, the patient was found to have a new lesion in the right temporal lobe of her brain.
One month after the patient received JCAR017—given after lymphodepletion with fludarabine and cyclophosphamide—imaging showed complete remission of the brain lesion.
The subcutaneous lesion that recurred 2 months later disappeared after the biopsy with no further treatment. Blood testing showed an expansion of CAR T cells that coincided with the tumor’s regression.
While re-expansion of CAR T cells has been reported in response to other immunotherapy drugs, this is the first report of such a response to a biopsy.
“Typically, the drugs we use to fight cancer and other diseases wear off over time,” Dr Abramson said. “This spontaneous re-expansion after biopsy highlights this therapy as something entirely different, a ‘living drug’ that can re-expand and proliferate in response to biologic stimuli.” ![]()
Researchers have reported the first known case of central nervous system (CNS) lymphoma responding to chimeric antigen receptor (CAR) T-cell therapy.
The investigational CAR T-cell therapy JCAR017 induced complete remission of brain metastasis in a patient with refractory diffuse large B-cell lymphoma (DLBCL).
When a subcutaneous tumor began to recur 2 months after the patient received JCAR017 and a surgical biopsy was performed, the CAR T cells spontaneously re-expanded and the tumor again went into remission.
While the patient eventually relapsed and died more than a year after receiving JCAR017, the brain tumor never recurred.
“Brain involvement in DLBCL carries a grave prognosis, and the ability to induce a complete and durable response with conventional therapies is rare,” said Jeremy Abramson, MD, of Massachusetts General Hospital in Boston.
“In addition, all available CAR T-cell trials have excluded patients with central nervous system involvement. This result has implications not only for secondary DLBCL like this case but also for primary central nervous system lymphoma, for which treatment options are similarly limited after relapse and few patents are cured.”
Dr Abramson and his colleagues described this case in a letter to NEJM. The patient was involved in a trial of JCAR017, which was sponsored by Juno Therapeutics.
The patient was a 68-year-old woman with germinal center B-cell-like DLBCL with a BCL2 rearrangement and multiple copies of MYC and BCL6.
The patients’ disease was refractory to conventional chemotherapy and an 8/8 HLA-matched stem cell transplant. After she enrolled in a phase 1 trial of JCAR017, the patient was found to have a new lesion in the right temporal lobe of her brain.
One month after the patient received JCAR017—given after lymphodepletion with fludarabine and cyclophosphamide—imaging showed complete remission of the brain lesion.
The subcutaneous lesion that recurred 2 months later disappeared after the biopsy with no further treatment. Blood testing showed an expansion of CAR T cells that coincided with the tumor’s regression.
While re-expansion of CAR T cells has been reported in response to other immunotherapy drugs, this is the first report of such a response to a biopsy.
“Typically, the drugs we use to fight cancer and other diseases wear off over time,” Dr Abramson said. “This spontaneous re-expansion after biopsy highlights this therapy as something entirely different, a ‘living drug’ that can re-expand and proliferate in response to biologic stimuli.” ![]()
Researchers have reported the first known case of central nervous system (CNS) lymphoma responding to chimeric antigen receptor (CAR) T-cell therapy.
The investigational CAR T-cell therapy JCAR017 induced complete remission of brain metastasis in a patient with refractory diffuse large B-cell lymphoma (DLBCL).
When a subcutaneous tumor began to recur 2 months after the patient received JCAR017 and a surgical biopsy was performed, the CAR T cells spontaneously re-expanded and the tumor again went into remission.
While the patient eventually relapsed and died more than a year after receiving JCAR017, the brain tumor never recurred.
“Brain involvement in DLBCL carries a grave prognosis, and the ability to induce a complete and durable response with conventional therapies is rare,” said Jeremy Abramson, MD, of Massachusetts General Hospital in Boston.
“In addition, all available CAR T-cell trials have excluded patients with central nervous system involvement. This result has implications not only for secondary DLBCL like this case but also for primary central nervous system lymphoma, for which treatment options are similarly limited after relapse and few patents are cured.”
Dr Abramson and his colleagues described this case in a letter to NEJM. The patient was involved in a trial of JCAR017, which was sponsored by Juno Therapeutics.
The patient was a 68-year-old woman with germinal center B-cell-like DLBCL with a BCL2 rearrangement and multiple copies of MYC and BCL6.
The patients’ disease was refractory to conventional chemotherapy and an 8/8 HLA-matched stem cell transplant. After she enrolled in a phase 1 trial of JCAR017, the patient was found to have a new lesion in the right temporal lobe of her brain.
One month after the patient received JCAR017—given after lymphodepletion with fludarabine and cyclophosphamide—imaging showed complete remission of the brain lesion.
The subcutaneous lesion that recurred 2 months later disappeared after the biopsy with no further treatment. Blood testing showed an expansion of CAR T cells that coincided with the tumor’s regression.
While re-expansion of CAR T cells has been reported in response to other immunotherapy drugs, this is the first report of such a response to a biopsy.
“Typically, the drugs we use to fight cancer and other diseases wear off over time,” Dr Abramson said. “This spontaneous re-expansion after biopsy highlights this therapy as something entirely different, a ‘living drug’ that can re-expand and proliferate in response to biologic stimuli.” ![]()
TKI granted priority review for newly diagnosed CML
The US Food and Drug Administration (FDA) has granted priority review to a supplemental new drug application (sNDA) for the tyrosine kinase inhibitor (TKI) bosutinib (Bosulif®).
If approved, the sNDA would expand the use of bosutinib to include patients with newly diagnosed, chronic phase, Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML).
Bosutinib is currently FDA-approved to treat adults with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the sNDA for bosutinib by the end of this year.
Meanwhile, the European Medicines Agency (EMA) has validated for review a type II variation application for bosutinib in patients with newly diagnosed, chronic phase Ph+ CML.
Bosutinib already has conditional marketing authorization in the European Economic Area for the treatment of adults with Ph+ CML who previously received at least 1 TKI and adults with Ph+ CML for whom imatinib, nilotinib, and dasatinib are not considered appropriate.
Phase 3 trial
The applications submitted to the EMA and FDA are both supported by early results from the phase 3 BFORE trial. Results from this trial were presented at the ASCO Annual Meeting in May.
In this ongoing study, researchers are comparing bosutinib and imatinib as first-line treatment of chronic phase CML.
As of the ASCO presentation, the trial had enrolled 536 patients who were randomized 1:1 to receive bosutinib (n=268) or imatinib (n=268).
The presentation included results in a modified intent-to-treat population of Ph+ patients with e13a2/e14a2 transcripts who had at least 12 months of follow-up. In this group, there were 246 patients in the bosutinib arm and 241 in the imatinib arm.
Most of the patients were still on therapy at the 12-month mark or beyond—78% in the bosutinib arm and 73.2% in the imatinib arm. The median treatment duration was 14.1 months and 13.8 months, respectively.
At 12 months, the rate of major molecular response was 47.2% in the bosutinib arm and 36.9% in the imatinib arm (P= 0.02). The rate of complete cytogenetic response was 77.2% and 66.4%, respectively (P<0.008).
One patient in the bosutinib arm and 4 in the imatinib arm discontinued treatment due to disease progression, while 12.7% and 8.7%, respectively, discontinued treatment due to drug-related toxicity.
Adverse events that were more common in the bosutinib arm than the imatinib arm included grade 3 or higher diarrhea (7.8% vs 0.8%), increased alanine levels (19% vs 1.5%), increased aspartate levels (9.7% vs 1.9%), cardiovascular events (3% vs 0.4%), and peripheral vascular events (1.5% vs 1.1%). Cerebrovascular events were more common with imatinib than bosutinib (0.4% and 0%, respectively). ![]()
The US Food and Drug Administration (FDA) has granted priority review to a supplemental new drug application (sNDA) for the tyrosine kinase inhibitor (TKI) bosutinib (Bosulif®).
If approved, the sNDA would expand the use of bosutinib to include patients with newly diagnosed, chronic phase, Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML).
Bosutinib is currently FDA-approved to treat adults with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the sNDA for bosutinib by the end of this year.
Meanwhile, the European Medicines Agency (EMA) has validated for review a type II variation application for bosutinib in patients with newly diagnosed, chronic phase Ph+ CML.
Bosutinib already has conditional marketing authorization in the European Economic Area for the treatment of adults with Ph+ CML who previously received at least 1 TKI and adults with Ph+ CML for whom imatinib, nilotinib, and dasatinib are not considered appropriate.
Phase 3 trial
The applications submitted to the EMA and FDA are both supported by early results from the phase 3 BFORE trial. Results from this trial were presented at the ASCO Annual Meeting in May.
In this ongoing study, researchers are comparing bosutinib and imatinib as first-line treatment of chronic phase CML.
As of the ASCO presentation, the trial had enrolled 536 patients who were randomized 1:1 to receive bosutinib (n=268) or imatinib (n=268).
The presentation included results in a modified intent-to-treat population of Ph+ patients with e13a2/e14a2 transcripts who had at least 12 months of follow-up. In this group, there were 246 patients in the bosutinib arm and 241 in the imatinib arm.
Most of the patients were still on therapy at the 12-month mark or beyond—78% in the bosutinib arm and 73.2% in the imatinib arm. The median treatment duration was 14.1 months and 13.8 months, respectively.
At 12 months, the rate of major molecular response was 47.2% in the bosutinib arm and 36.9% in the imatinib arm (P= 0.02). The rate of complete cytogenetic response was 77.2% and 66.4%, respectively (P<0.008).
One patient in the bosutinib arm and 4 in the imatinib arm discontinued treatment due to disease progression, while 12.7% and 8.7%, respectively, discontinued treatment due to drug-related toxicity.
Adverse events that were more common in the bosutinib arm than the imatinib arm included grade 3 or higher diarrhea (7.8% vs 0.8%), increased alanine levels (19% vs 1.5%), increased aspartate levels (9.7% vs 1.9%), cardiovascular events (3% vs 0.4%), and peripheral vascular events (1.5% vs 1.1%). Cerebrovascular events were more common with imatinib than bosutinib (0.4% and 0%, respectively). ![]()
The US Food and Drug Administration (FDA) has granted priority review to a supplemental new drug application (sNDA) for the tyrosine kinase inhibitor (TKI) bosutinib (Bosulif®).
If approved, the sNDA would expand the use of bosutinib to include patients with newly diagnosed, chronic phase, Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML).
Bosutinib is currently FDA-approved to treat adults with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the sNDA for bosutinib by the end of this year.
Meanwhile, the European Medicines Agency (EMA) has validated for review a type II variation application for bosutinib in patients with newly diagnosed, chronic phase Ph+ CML.
Bosutinib already has conditional marketing authorization in the European Economic Area for the treatment of adults with Ph+ CML who previously received at least 1 TKI and adults with Ph+ CML for whom imatinib, nilotinib, and dasatinib are not considered appropriate.
Phase 3 trial
The applications submitted to the EMA and FDA are both supported by early results from the phase 3 BFORE trial. Results from this trial were presented at the ASCO Annual Meeting in May.
In this ongoing study, researchers are comparing bosutinib and imatinib as first-line treatment of chronic phase CML.
As of the ASCO presentation, the trial had enrolled 536 patients who were randomized 1:1 to receive bosutinib (n=268) or imatinib (n=268).
The presentation included results in a modified intent-to-treat population of Ph+ patients with e13a2/e14a2 transcripts who had at least 12 months of follow-up. In this group, there were 246 patients in the bosutinib arm and 241 in the imatinib arm.
Most of the patients were still on therapy at the 12-month mark or beyond—78% in the bosutinib arm and 73.2% in the imatinib arm. The median treatment duration was 14.1 months and 13.8 months, respectively.
At 12 months, the rate of major molecular response was 47.2% in the bosutinib arm and 36.9% in the imatinib arm (P= 0.02). The rate of complete cytogenetic response was 77.2% and 66.4%, respectively (P<0.008).
One patient in the bosutinib arm and 4 in the imatinib arm discontinued treatment due to disease progression, while 12.7% and 8.7%, respectively, discontinued treatment due to drug-related toxicity.
Adverse events that were more common in the bosutinib arm than the imatinib arm included grade 3 or higher diarrhea (7.8% vs 0.8%), increased alanine levels (19% vs 1.5%), increased aspartate levels (9.7% vs 1.9%), cardiovascular events (3% vs 0.4%), and peripheral vascular events (1.5% vs 1.1%). Cerebrovascular events were more common with imatinib than bosutinib (0.4% and 0%, respectively). ![]()
Shorter DAPT appears safe, effective long-term
BARCELONA—Three-year follow-up of the NIPPON study showed no significant difference in net clinical benefit with short-term or long-term dual antiplatelet therapy (DAPT).
Overall, there was no significant difference in safety or efficacy outcomes between patients who received 6 months of DAPT or 18 months of DAPT after placement of a drug-eluting stent (DES).
However, the data did suggest certain patients may benefit from long-term DAPT.
Details of this study were presented at ESC Congress 2017 (abstract 3831).
“These findings support and strengthen the evidence for short-term DAPT after DES deployment and may help confirm that clinical benefits of extended DAPT are reduced in patients with newer-generation DES,” said study investigator Masato Nakamura MD, PhD, of Toho University Ohashi Medical Center in Tokyo, Japan.
“The findings are important because shorter duration of therapy is less expensive and could theoretically reduce the risk of side effects.”
NIPPON enrolled 3775 patients with coronary artery disease or acute myocardial infarction who had undergone percutaneous coronary intervention and DES placement at 130 Japanese institutions.
All patients had received the Nobori bioabsorbable abluminal-coated stent. They then received DAPT—consisting of aspirin (81–162 mg/day) and clopidogrel (75 mg/day) or ticlopidine (200 mg/day)—for 6 months or 18 months.
Initial results from this trial were presented last year at ESC Congress.
The 3-year follow-up included 3307 patients—1887 who received long-term DAPT and 1886 who received short-term DAPT.
Dr Nakamura first reported the net adverse clinical and cerebrovascular events (NACCEs)—which included all-cause mortality, myocardial infarction, stroke, and major bleeding—in each arm.
Three years from the start of the study, the cumulative incidence of NACCE was 7.03% in the short-term DAPT arm and 4.85% in the long-term DAPT arm (hazard ratio [HR]=1.20, P=0.27).
In the landmark analysis, which only included data from 6 months to 3 years, the incidence of NACCE was 5.60% in the short-term DAPT arm and 3.48% in the long-term DAPT arm (HR=1.49, P=0.06).
The investigators also looked at efficacy and safety endpoints separately.
The efficacy endpoint included cardiovascular death, myocardial infarction, stroke, and definite or probable stent thrombosis. The safety endpoint included BARC 2, 3, or 5 bleeding.
In the landmark analysis, the incidence of the efficacy endpoint was 2.58% in the short-term DAPT arm and 1.70% in the long-term DAPT arm (HR=1.53, P=0.17). The incidence of the safety endpoint was 2.22% and 2.01%, respectively (HR=1.02, P=0.94).
Although there were no significant differences between the arms in the overall cohort, the investigators did identify patients with a high risk of ischemic events who might benefit from long-term DAPT.
In patients older than 70 who had a SYNTAX score above 23.3, the rate of efficacy events was 0% in those on long-term DAPT and 18.8% in those on short-term DAPT (HR=13.24, P=0.01).
In patients age 70 to 76 who had diabetes, the rate of efficacy events was 2.0% in those on long-term DAPT and 6.0% in those on short-term DAPT (HR=2.89, P=0.04)
“In real-world practice, it is not easy to find the balance between risks and benefits of DAPT duration, and consensus criteria for individualization therapy have not been established,” Dr Nakamura said.
“The present findings may provide some assistance, although it is essential to obtain confirmation by further investigation.”
This study was sponsored by the Association for Establishment of Evidence in Interventions. Dr Nakamura disclosed research expert witness payment from Terumo Corporation, grant support from Daiichi Sankyo and Sanofi, and honoraria from Terumo Corporation, Daiichi Sankyo, and Sanofi. ![]()
BARCELONA—Three-year follow-up of the NIPPON study showed no significant difference in net clinical benefit with short-term or long-term dual antiplatelet therapy (DAPT).
Overall, there was no significant difference in safety or efficacy outcomes between patients who received 6 months of DAPT or 18 months of DAPT after placement of a drug-eluting stent (DES).
However, the data did suggest certain patients may benefit from long-term DAPT.
Details of this study were presented at ESC Congress 2017 (abstract 3831).
“These findings support and strengthen the evidence for short-term DAPT after DES deployment and may help confirm that clinical benefits of extended DAPT are reduced in patients with newer-generation DES,” said study investigator Masato Nakamura MD, PhD, of Toho University Ohashi Medical Center in Tokyo, Japan.
“The findings are important because shorter duration of therapy is less expensive and could theoretically reduce the risk of side effects.”
NIPPON enrolled 3775 patients with coronary artery disease or acute myocardial infarction who had undergone percutaneous coronary intervention and DES placement at 130 Japanese institutions.
All patients had received the Nobori bioabsorbable abluminal-coated stent. They then received DAPT—consisting of aspirin (81–162 mg/day) and clopidogrel (75 mg/day) or ticlopidine (200 mg/day)—for 6 months or 18 months.
Initial results from this trial were presented last year at ESC Congress.
The 3-year follow-up included 3307 patients—1887 who received long-term DAPT and 1886 who received short-term DAPT.
Dr Nakamura first reported the net adverse clinical and cerebrovascular events (NACCEs)—which included all-cause mortality, myocardial infarction, stroke, and major bleeding—in each arm.
Three years from the start of the study, the cumulative incidence of NACCE was 7.03% in the short-term DAPT arm and 4.85% in the long-term DAPT arm (hazard ratio [HR]=1.20, P=0.27).
In the landmark analysis, which only included data from 6 months to 3 years, the incidence of NACCE was 5.60% in the short-term DAPT arm and 3.48% in the long-term DAPT arm (HR=1.49, P=0.06).
The investigators also looked at efficacy and safety endpoints separately.
The efficacy endpoint included cardiovascular death, myocardial infarction, stroke, and definite or probable stent thrombosis. The safety endpoint included BARC 2, 3, or 5 bleeding.
In the landmark analysis, the incidence of the efficacy endpoint was 2.58% in the short-term DAPT arm and 1.70% in the long-term DAPT arm (HR=1.53, P=0.17). The incidence of the safety endpoint was 2.22% and 2.01%, respectively (HR=1.02, P=0.94).
Although there were no significant differences between the arms in the overall cohort, the investigators did identify patients with a high risk of ischemic events who might benefit from long-term DAPT.
In patients older than 70 who had a SYNTAX score above 23.3, the rate of efficacy events was 0% in those on long-term DAPT and 18.8% in those on short-term DAPT (HR=13.24, P=0.01).
In patients age 70 to 76 who had diabetes, the rate of efficacy events was 2.0% in those on long-term DAPT and 6.0% in those on short-term DAPT (HR=2.89, P=0.04)
“In real-world practice, it is not easy to find the balance between risks and benefits of DAPT duration, and consensus criteria for individualization therapy have not been established,” Dr Nakamura said.
“The present findings may provide some assistance, although it is essential to obtain confirmation by further investigation.”
This study was sponsored by the Association for Establishment of Evidence in Interventions. Dr Nakamura disclosed research expert witness payment from Terumo Corporation, grant support from Daiichi Sankyo and Sanofi, and honoraria from Terumo Corporation, Daiichi Sankyo, and Sanofi. ![]()
BARCELONA—Three-year follow-up of the NIPPON study showed no significant difference in net clinical benefit with short-term or long-term dual antiplatelet therapy (DAPT).
Overall, there was no significant difference in safety or efficacy outcomes between patients who received 6 months of DAPT or 18 months of DAPT after placement of a drug-eluting stent (DES).
However, the data did suggest certain patients may benefit from long-term DAPT.
Details of this study were presented at ESC Congress 2017 (abstract 3831).
“These findings support and strengthen the evidence for short-term DAPT after DES deployment and may help confirm that clinical benefits of extended DAPT are reduced in patients with newer-generation DES,” said study investigator Masato Nakamura MD, PhD, of Toho University Ohashi Medical Center in Tokyo, Japan.
“The findings are important because shorter duration of therapy is less expensive and could theoretically reduce the risk of side effects.”
NIPPON enrolled 3775 patients with coronary artery disease or acute myocardial infarction who had undergone percutaneous coronary intervention and DES placement at 130 Japanese institutions.
All patients had received the Nobori bioabsorbable abluminal-coated stent. They then received DAPT—consisting of aspirin (81–162 mg/day) and clopidogrel (75 mg/day) or ticlopidine (200 mg/day)—for 6 months or 18 months.
Initial results from this trial were presented last year at ESC Congress.
The 3-year follow-up included 3307 patients—1887 who received long-term DAPT and 1886 who received short-term DAPT.
Dr Nakamura first reported the net adverse clinical and cerebrovascular events (NACCEs)—which included all-cause mortality, myocardial infarction, stroke, and major bleeding—in each arm.
Three years from the start of the study, the cumulative incidence of NACCE was 7.03% in the short-term DAPT arm and 4.85% in the long-term DAPT arm (hazard ratio [HR]=1.20, P=0.27).
In the landmark analysis, which only included data from 6 months to 3 years, the incidence of NACCE was 5.60% in the short-term DAPT arm and 3.48% in the long-term DAPT arm (HR=1.49, P=0.06).
The investigators also looked at efficacy and safety endpoints separately.
The efficacy endpoint included cardiovascular death, myocardial infarction, stroke, and definite or probable stent thrombosis. The safety endpoint included BARC 2, 3, or 5 bleeding.
In the landmark analysis, the incidence of the efficacy endpoint was 2.58% in the short-term DAPT arm and 1.70% in the long-term DAPT arm (HR=1.53, P=0.17). The incidence of the safety endpoint was 2.22% and 2.01%, respectively (HR=1.02, P=0.94).
Although there were no significant differences between the arms in the overall cohort, the investigators did identify patients with a high risk of ischemic events who might benefit from long-term DAPT.
In patients older than 70 who had a SYNTAX score above 23.3, the rate of efficacy events was 0% in those on long-term DAPT and 18.8% in those on short-term DAPT (HR=13.24, P=0.01).
In patients age 70 to 76 who had diabetes, the rate of efficacy events was 2.0% in those on long-term DAPT and 6.0% in those on short-term DAPT (HR=2.89, P=0.04)
“In real-world practice, it is not easy to find the balance between risks and benefits of DAPT duration, and consensus criteria for individualization therapy have not been established,” Dr Nakamura said.
“The present findings may provide some assistance, although it is essential to obtain confirmation by further investigation.”
This study was sponsored by the Association for Establishment of Evidence in Interventions. Dr Nakamura disclosed research expert witness payment from Terumo Corporation, grant support from Daiichi Sankyo and Sanofi, and honoraria from Terumo Corporation, Daiichi Sankyo, and Sanofi.
Drug receives priority review for FL
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) for obinutuzumab (Gazyva®).
With this sBLA, Genentech is seeking approval for obinutuzumab to be used, first in combination with chemotherapy and then alone as maintenance, in patients with previously untreated follicular lymphoma (FL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the sBLA for obinutuzumab by December 23, 2017.
The sBLA is supported by results of the GALLIUM study, which were presented at the 2016 ASH Annual Meeting.
About obinutuzumab
Obinutuzumab is a glycoengineered, humanized, monoclonal antibody that selectively binds to the extracellular domain of the CD20 antigen on B cells.
The drug is FDA-approved for use in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia.
Obinutuzumab is also approved to treat FL patients who relapse after, or are refractory to, a rituximab-containing regimen. In these patients, obinutuzumab is given first in combination with bendamustine and then alone as maintenance.
The full prescribing information for obinutuzumab is available at http://www.Gazyva.com.
About the GALLIUM study
GALLIUM enrolled 1401 patients with previously untreated, indolent non-Hodgkin lymphoma, including 1202 with FL.
Half of the FL patients (n=601) were randomized to receive obinutuzumab plus chemotherapy (followed by obinutuzumab maintenance for up to 2 years), and half were randomized to rituximab plus chemotherapy (followed by rituximab maintenance for up to 2 years).
The different chemotherapies used were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), CVP (cyclophosphamide, vincristine, and prednisolone), and bendamustine.
Patients who received obinutuzumab had significantly better progression-free survival than patients who received rituximab. The 3-year progression-free survival rate was 73.3% in the rituximab arm and 80% in the obinutuzumab arm (hazard ratio [HR]=0.66, P=0.0012).
There was no significant difference between the treatment arms with regard to overall survival. The 3-year overall survival was 92.1% in the rituximab arm and 94% in the obinutuzumab arm (HR=0.75, P=0.21).
The overall incidence of adverse events (AEs) was 98.3% in the rituximab arm and 99.5% in the obinutuzumab arm. The incidence of serious AEs was 39.9% and 46.1%, respectively.
The incidence of grade 3 or higher AEs was higher among patients who received obinutuzumab.
Grade 3 or higher AEs occurring in at least 5% of patients in either arm (rituximab and obinutuzumab, respectively) included neutropenia (67.8% and 74.6%), leukopenia (37.9% and 43.9%), febrile neutropenia (4.9% and 6.9%), infections and infestations (3.7% and 6.7%), and thrombocytopenia (2.7% and 6.1%).
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) for obinutuzumab (Gazyva®).
With this sBLA, Genentech is seeking approval for obinutuzumab to be used, first in combination with chemotherapy and then alone as maintenance, in patients with previously untreated follicular lymphoma (FL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the sBLA for obinutuzumab by December 23, 2017.
The sBLA is supported by results of the GALLIUM study, which were presented at the 2016 ASH Annual Meeting.
About obinutuzumab
Obinutuzumab is a glycoengineered, humanized, monoclonal antibody that selectively binds to the extracellular domain of the CD20 antigen on B cells.
The drug is FDA-approved for use in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia.
Obinutuzumab is also approved to treat FL patients who relapse after, or are refractory to, a rituximab-containing regimen. In these patients, obinutuzumab is given first in combination with bendamustine and then alone as maintenance.
The full prescribing information for obinutuzumab is available at http://www.Gazyva.com.
About the GALLIUM study
GALLIUM enrolled 1401 patients with previously untreated, indolent non-Hodgkin lymphoma, including 1202 with FL.
Half of the FL patients (n=601) were randomized to receive obinutuzumab plus chemotherapy (followed by obinutuzumab maintenance for up to 2 years), and half were randomized to rituximab plus chemotherapy (followed by rituximab maintenance for up to 2 years).
The different chemotherapies used were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), CVP (cyclophosphamide, vincristine, and prednisolone), and bendamustine.
Patients who received obinutuzumab had significantly better progression-free survival than patients who received rituximab. The 3-year progression-free survival rate was 73.3% in the rituximab arm and 80% in the obinutuzumab arm (hazard ratio [HR]=0.66, P=0.0012).
There was no significant difference between the treatment arms with regard to overall survival. The 3-year overall survival was 92.1% in the rituximab arm and 94% in the obinutuzumab arm (HR=0.75, P=0.21).
The overall incidence of adverse events (AEs) was 98.3% in the rituximab arm and 99.5% in the obinutuzumab arm. The incidence of serious AEs was 39.9% and 46.1%, respectively.
The incidence of grade 3 or higher AEs was higher among patients who received obinutuzumab.
Grade 3 or higher AEs occurring in at least 5% of patients in either arm (rituximab and obinutuzumab, respectively) included neutropenia (67.8% and 74.6%), leukopenia (37.9% and 43.9%), febrile neutropenia (4.9% and 6.9%), infections and infestations (3.7% and 6.7%), and thrombocytopenia (2.7% and 6.1%).
The US Food and Drug Administration (FDA) has granted priority review to a supplemental biologics license application (sBLA) for obinutuzumab (Gazyva®).
With this sBLA, Genentech is seeking approval for obinutuzumab to be used, first in combination with chemotherapy and then alone as maintenance, in patients with previously untreated follicular lymphoma (FL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the sBLA for obinutuzumab by December 23, 2017.
The sBLA is supported by results of the GALLIUM study, which were presented at the 2016 ASH Annual Meeting.
About obinutuzumab
Obinutuzumab is a glycoengineered, humanized, monoclonal antibody that selectively binds to the extracellular domain of the CD20 antigen on B cells.
The drug is FDA-approved for use in combination with chlorambucil to treat patients with previously untreated chronic lymphocytic leukemia.
Obinutuzumab is also approved to treat FL patients who relapse after, or are refractory to, a rituximab-containing regimen. In these patients, obinutuzumab is given first in combination with bendamustine and then alone as maintenance.
The full prescribing information for obinutuzumab is available at http://www.Gazyva.com.
About the GALLIUM study
GALLIUM enrolled 1401 patients with previously untreated, indolent non-Hodgkin lymphoma, including 1202 with FL.
Half of the FL patients (n=601) were randomized to receive obinutuzumab plus chemotherapy (followed by obinutuzumab maintenance for up to 2 years), and half were randomized to rituximab plus chemotherapy (followed by rituximab maintenance for up to 2 years).
The different chemotherapies used were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), CVP (cyclophosphamide, vincristine, and prednisolone), and bendamustine.
Patients who received obinutuzumab had significantly better progression-free survival than patients who received rituximab. The 3-year progression-free survival rate was 73.3% in the rituximab arm and 80% in the obinutuzumab arm (hazard ratio [HR]=0.66, P=0.0012).
There was no significant difference between the treatment arms with regard to overall survival. The 3-year overall survival was 92.1% in the rituximab arm and 94% in the obinutuzumab arm (HR=0.75, P=0.21).
The overall incidence of adverse events (AEs) was 98.3% in the rituximab arm and 99.5% in the obinutuzumab arm. The incidence of serious AEs was 39.9% and 46.1%, respectively.
The incidence of grade 3 or higher AEs was higher among patients who received obinutuzumab.
Grade 3 or higher AEs occurring in at least 5% of patients in either arm (rituximab and obinutuzumab, respectively) included neutropenia (67.8% and 74.6%), leukopenia (37.9% and 43.9%), febrile neutropenia (4.9% and 6.9%), infections and infestations (3.7% and 6.7%), and thrombocytopenia (2.7% and 6.1%).
Bacterial infection inhibits hematopoiesis
New research suggests that bacterial infection activates hematopoietic stem cells (HSCs) and significantly reduces their ability to produce blood by forcibly inducing proliferation.
These findings indicate that bacterial infections might cause dysregulated hematopoiesis like that which occurs in patients with anemias and leukemias.
Hitoshi Takizawa, PhD, of Kumamoto University’s International Research Center for Medical Sciences in Kumamoto, Japan, and his colleagues reported these findings in Cell Stem Cell.
The researchers gave lipopolysaccharide to mice to generate a bacterial infection model and analyzed the role of Toll-like receptors (TLRs) in HSCs.
The team found that lipopolysaccharides spread throughout the body, with some eventually reaching the bone marrow. This stimulated TLR4 and induced HSCs to proliferate.
However, the stimulus also induced stress on the HSCs.
So although HSCs proliferate temporarily upon TLR4 stimulation, their ability to successfully self-replicate decreases, resulting in diminished blood production.
The researchers observed similar results after infecting mice with Salmonella Typhimurium.
“Fortunately, we were able to confirm that this molecular reaction can be inhibited by drugs,” Dr Takizawa said.
Specifically, the researchers found that activation of reactive oxygen species and p38 through TLR4 ligation is key to HSC dysfunction.
And small-molecule inhibitors of reactive oxygen species and p38 were able to prevent HSC dysfunction.
“The medication maintains the production of blood and immune cells without weakening the immune reaction against pathogenic bacteria,” Dr Takizawa said. “It might be possible to simultaneously prevent blood diseases and many bacterial infections in the future.”
New research suggests that bacterial infection activates hematopoietic stem cells (HSCs) and significantly reduces their ability to produce blood by forcibly inducing proliferation.
These findings indicate that bacterial infections might cause dysregulated hematopoiesis like that which occurs in patients with anemias and leukemias.
Hitoshi Takizawa, PhD, of Kumamoto University’s International Research Center for Medical Sciences in Kumamoto, Japan, and his colleagues reported these findings in Cell Stem Cell.
The researchers gave lipopolysaccharide to mice to generate a bacterial infection model and analyzed the role of Toll-like receptors (TLRs) in HSCs.
The team found that lipopolysaccharides spread throughout the body, with some eventually reaching the bone marrow. This stimulated TLR4 and induced HSCs to proliferate.
However, the stimulus also induced stress on the HSCs.
So although HSCs proliferate temporarily upon TLR4 stimulation, their ability to successfully self-replicate decreases, resulting in diminished blood production.
The researchers observed similar results after infecting mice with Salmonella Typhimurium.
“Fortunately, we were able to confirm that this molecular reaction can be inhibited by drugs,” Dr Takizawa said.
Specifically, the researchers found that activation of reactive oxygen species and p38 through TLR4 ligation is key to HSC dysfunction.
And small-molecule inhibitors of reactive oxygen species and p38 were able to prevent HSC dysfunction.
“The medication maintains the production of blood and immune cells without weakening the immune reaction against pathogenic bacteria,” Dr Takizawa said. “It might be possible to simultaneously prevent blood diseases and many bacterial infections in the future.”
New research suggests that bacterial infection activates hematopoietic stem cells (HSCs) and significantly reduces their ability to produce blood by forcibly inducing proliferation.
These findings indicate that bacterial infections might cause dysregulated hematopoiesis like that which occurs in patients with anemias and leukemias.
Hitoshi Takizawa, PhD, of Kumamoto University’s International Research Center for Medical Sciences in Kumamoto, Japan, and his colleagues reported these findings in Cell Stem Cell.
The researchers gave lipopolysaccharide to mice to generate a bacterial infection model and analyzed the role of Toll-like receptors (TLRs) in HSCs.
The team found that lipopolysaccharides spread throughout the body, with some eventually reaching the bone marrow. This stimulated TLR4 and induced HSCs to proliferate.
However, the stimulus also induced stress on the HSCs.
So although HSCs proliferate temporarily upon TLR4 stimulation, their ability to successfully self-replicate decreases, resulting in diminished blood production.
The researchers observed similar results after infecting mice with Salmonella Typhimurium.
“Fortunately, we were able to confirm that this molecular reaction can be inhibited by drugs,” Dr Takizawa said.
Specifically, the researchers found that activation of reactive oxygen species and p38 through TLR4 ligation is key to HSC dysfunction.
And small-molecule inhibitors of reactive oxygen species and p38 were able to prevent HSC dysfunction.
“The medication maintains the production of blood and immune cells without weakening the immune reaction against pathogenic bacteria,” Dr Takizawa said. “It might be possible to simultaneously prevent blood diseases and many bacterial infections in the future.”
Therapy shows promise for PUPs with severe hemophilia A
A fourth-generation recombinant factor VIII (FVIII) therapy has demonstrated “convincing” efficacy and tolerability as well as low immunogenicity in previously untreated patients (PUPs) with severe hemophilia A, according to researchers.
The therapy, simoctocog alfa, is a B-domain-deleted recombinant FVIII product derived from a human cell line.
In the NuProtect study (also known as GENA-05), researchers are evaluating simoctocog alfa in PUPs with severe hemophilia A.
Interim results from this study were recently published in Haemophilia. The research is sponsored by Octapharma, makers of simoctocog alfa.
Thus far, NuProtect has enrolled 110 PUPs who will receive simoctocog alfa for up to 100 exposure days (EDs).
The Haemophilia article describes interim results for 66 PUPs treated for at least 20 EDs, the time by which most inhibitors arise. The patients’ median age at first treatment was 13 months (range, 3 months to 135 months).
The patients received simoctocog alfa for standard prophylaxis, surgical prophylaxis, or on-demand treatment.
Forty-five (68.2%) patients received standard prophylaxis, 13 (19.7%) received only on-demand treatment, 8 (12.1%) were initially treated on-demand but later received prophylaxis, and 13 (19.7%) patients received surgical prophylaxis (for 14 procedures).
The median number of EDs was 43.0 (range, 4-120).
Results
The primary objective of this study is to assess the immunogenicity of simoctocog alfa by determining inhibitor activity using the Nijmegen-modified Bethesda assay at a central laboratory.
After a median of 11.5 EDs (range, 6-24), 8 patients had developed high-titer anti-FVIII inhibitors, and 5 patients had developed low-titer inhibitors, 4 of them transient.
The cumulative incidence of all inhibitors was 20.8%—12.8% for high-titer and 8.4% for low-titer inhibitors.
For patients who received prophylaxis, the median annual bleeding rate, during inhibitor-free periods, was 2.40 for all bleeds and 0 for spontaneous bleeds.
When simoctocog alfa was used on-demand, 92.4% of bleeds were controlled with 1 or 2 infusions. In addition, simoctocog alfa was said to demonstrate “excellent” or “good” efficacy in 89% of surgical procedures.
Three patients experienced adverse events (other than inhibitor development) that were considered related to simoctocog alfa.
One patient developed a mild fever. Another had a mild allergic reaction after 3 consecutive infusions of simoctocog alfa (but not after subsequent infusions).
The third patient developed a rash that was described as mild but considered serious due to hospitalization. This patient continued treatment and completed the study.
A fourth-generation recombinant factor VIII (FVIII) therapy has demonstrated “convincing” efficacy and tolerability as well as low immunogenicity in previously untreated patients (PUPs) with severe hemophilia A, according to researchers.
The therapy, simoctocog alfa, is a B-domain-deleted recombinant FVIII product derived from a human cell line.
In the NuProtect study (also known as GENA-05), researchers are evaluating simoctocog alfa in PUPs with severe hemophilia A.
Interim results from this study were recently published in Haemophilia. The research is sponsored by Octapharma, makers of simoctocog alfa.
Thus far, NuProtect has enrolled 110 PUPs who will receive simoctocog alfa for up to 100 exposure days (EDs).
The Haemophilia article describes interim results for 66 PUPs treated for at least 20 EDs, the time by which most inhibitors arise. The patients’ median age at first treatment was 13 months (range, 3 months to 135 months).
The patients received simoctocog alfa for standard prophylaxis, surgical prophylaxis, or on-demand treatment.
Forty-five (68.2%) patients received standard prophylaxis, 13 (19.7%) received only on-demand treatment, 8 (12.1%) were initially treated on-demand but later received prophylaxis, and 13 (19.7%) patients received surgical prophylaxis (for 14 procedures).
The median number of EDs was 43.0 (range, 4-120).
Results
The primary objective of this study is to assess the immunogenicity of simoctocog alfa by determining inhibitor activity using the Nijmegen-modified Bethesda assay at a central laboratory.
After a median of 11.5 EDs (range, 6-24), 8 patients had developed high-titer anti-FVIII inhibitors, and 5 patients had developed low-titer inhibitors, 4 of them transient.
The cumulative incidence of all inhibitors was 20.8%—12.8% for high-titer and 8.4% for low-titer inhibitors.
For patients who received prophylaxis, the median annual bleeding rate, during inhibitor-free periods, was 2.40 for all bleeds and 0 for spontaneous bleeds.
When simoctocog alfa was used on-demand, 92.4% of bleeds were controlled with 1 or 2 infusions. In addition, simoctocog alfa was said to demonstrate “excellent” or “good” efficacy in 89% of surgical procedures.
Three patients experienced adverse events (other than inhibitor development) that were considered related to simoctocog alfa.
One patient developed a mild fever. Another had a mild allergic reaction after 3 consecutive infusions of simoctocog alfa (but not after subsequent infusions).
The third patient developed a rash that was described as mild but considered serious due to hospitalization. This patient continued treatment and completed the study.
A fourth-generation recombinant factor VIII (FVIII) therapy has demonstrated “convincing” efficacy and tolerability as well as low immunogenicity in previously untreated patients (PUPs) with severe hemophilia A, according to researchers.
The therapy, simoctocog alfa, is a B-domain-deleted recombinant FVIII product derived from a human cell line.
In the NuProtect study (also known as GENA-05), researchers are evaluating simoctocog alfa in PUPs with severe hemophilia A.
Interim results from this study were recently published in Haemophilia. The research is sponsored by Octapharma, makers of simoctocog alfa.
Thus far, NuProtect has enrolled 110 PUPs who will receive simoctocog alfa for up to 100 exposure days (EDs).
The Haemophilia article describes interim results for 66 PUPs treated for at least 20 EDs, the time by which most inhibitors arise. The patients’ median age at first treatment was 13 months (range, 3 months to 135 months).
The patients received simoctocog alfa for standard prophylaxis, surgical prophylaxis, or on-demand treatment.
Forty-five (68.2%) patients received standard prophylaxis, 13 (19.7%) received only on-demand treatment, 8 (12.1%) were initially treated on-demand but later received prophylaxis, and 13 (19.7%) patients received surgical prophylaxis (for 14 procedures).
The median number of EDs was 43.0 (range, 4-120).
Results
The primary objective of this study is to assess the immunogenicity of simoctocog alfa by determining inhibitor activity using the Nijmegen-modified Bethesda assay at a central laboratory.
After a median of 11.5 EDs (range, 6-24), 8 patients had developed high-titer anti-FVIII inhibitors, and 5 patients had developed low-titer inhibitors, 4 of them transient.
The cumulative incidence of all inhibitors was 20.8%—12.8% for high-titer and 8.4% for low-titer inhibitors.
For patients who received prophylaxis, the median annual bleeding rate, during inhibitor-free periods, was 2.40 for all bleeds and 0 for spontaneous bleeds.
When simoctocog alfa was used on-demand, 92.4% of bleeds were controlled with 1 or 2 infusions. In addition, simoctocog alfa was said to demonstrate “excellent” or “good” efficacy in 89% of surgical procedures.
Three patients experienced adverse events (other than inhibitor development) that were considered related to simoctocog alfa.
One patient developed a mild fever. Another had a mild allergic reaction after 3 consecutive infusions of simoctocog alfa (but not after subsequent infusions).
The third patient developed a rash that was described as mild but considered serious due to hospitalization. This patient continued treatment and completed the study.