User login
Tests reveal risk of passing on SCD, other diseases
Quest Diagnostics has announced the US launch of QHerit™, a genetic screening service that helps people of multiple ethnicities identify their risk of passing on heritable disorders to their offspring.
The QHerit Pan-Ethnic Expanded Carrier Screen is a panel of tests for the 22 heritable diseases cited in new screening guidelines from the American College of Gynecology (ACOG).
Among the diseases are alpha-thalassemia, Fanconi anemia, and beta-hemoglobinopathies, including sickle cell disease (SCD).
Traditionally, genetic carrier screening has been used for at-risk populations based on specific ancestry assumptions and focused on only a few likely disorders with higher prevalence associated with that ethnicity.
In its new guidelines, ACOG recommends offering pan-ethnic, expanded carrier, and ethnic-specific screening for all women considering pregnancy. The guidelines also state that the partner of a woman who tests positive may be a candidate for screening.
QHerit screens women and men for clinically relevant variants of genes for disorders that could have potentially devastating consequences, result in early death, or create a need for significant early intervention.
The disorders covered by QHerit include:
| Disease | Race/ethnicity | |||
| Alpha-thalassemia | Mediterranean, Middle East, Southeast Asian, African, Chinese, Asian Indian | |||
| Beta-
hemoglobinopathies (including SCD) |
Mediterranean, Middle East, Southeast Asian, African, Chinese, Asian Indian | |||
| Bloom syndrome | Ashkenazi Jewish descent (AJ) | |||
| Canavan disease | AJ and non-AJ | |||
| Cystic fibrosis | African American, AJ, Asian American, Hispanic American, non-Hispanic Caucasian | |||
| Dihydrolipoamide
dehydrogenase deficiency |
AJ | |||
| Familial dysautonomia | AJ | |||
| Familial hyperinsulinism | AJ | |||
| Fanconi anemia Type C | AJ | |||
| Fragile X syndrome | Females | |||
| Gaucher disease | AJ | |||
| Glycogen storage
disease Type Ia |
AJ, Caucasian | |||
| Joubert syndrome 2 | AJ | |||
| Maple syrup urine
disease |
AJ | |||
| Mucolipidosis Type IV | AJ | |||
| Nemaline myopathy | AJ | |||
| Niemann-Pick
disease Types A & B |
AJ | |||
| Spinal muscular
atrophy |
African American, AJ, Asian, Caucasian, Hispanic | |||
| Tay-Sachs disease | AJ, French Canadian, general population | |||
| Usher syndrome,
Type IF |
AJ | |||
| Usher syndrome,
Type IIIA |
AJ | |||
| Walker-Warburg
syndrome |
AJ | |||
QHerit is now available for order by US physicians. For more information, visit www.QHerit.com. ![]()
Quest Diagnostics has announced the US launch of QHerit™, a genetic screening service that helps people of multiple ethnicities identify their risk of passing on heritable disorders to their offspring.
The QHerit Pan-Ethnic Expanded Carrier Screen is a panel of tests for the 22 heritable diseases cited in new screening guidelines from the American College of Gynecology (ACOG).
Among the diseases are alpha-thalassemia, Fanconi anemia, and beta-hemoglobinopathies, including sickle cell disease (SCD).
Traditionally, genetic carrier screening has been used for at-risk populations based on specific ancestry assumptions and focused on only a few likely disorders with higher prevalence associated with that ethnicity.
In its new guidelines, ACOG recommends offering pan-ethnic, expanded carrier, and ethnic-specific screening for all women considering pregnancy. The guidelines also state that the partner of a woman who tests positive may be a candidate for screening.
QHerit screens women and men for clinically relevant variants of genes for disorders that could have potentially devastating consequences, result in early death, or create a need for significant early intervention.
The disorders covered by QHerit include:
| Disease | Race/ethnicity | |||
| Alpha-thalassemia | Mediterranean, Middle East, Southeast Asian, African, Chinese, Asian Indian | |||
| Beta-
hemoglobinopathies (including SCD) |
Mediterranean, Middle East, Southeast Asian, African, Chinese, Asian Indian | |||
| Bloom syndrome | Ashkenazi Jewish descent (AJ) | |||
| Canavan disease | AJ and non-AJ | |||
| Cystic fibrosis | African American, AJ, Asian American, Hispanic American, non-Hispanic Caucasian | |||
| Dihydrolipoamide
dehydrogenase deficiency |
AJ | |||
| Familial dysautonomia | AJ | |||
| Familial hyperinsulinism | AJ | |||
| Fanconi anemia Type C | AJ | |||
| Fragile X syndrome | Females | |||
| Gaucher disease | AJ | |||
| Glycogen storage
disease Type Ia |
AJ, Caucasian | |||
| Joubert syndrome 2 | AJ | |||
| Maple syrup urine
disease |
AJ | |||
| Mucolipidosis Type IV | AJ | |||
| Nemaline myopathy | AJ | |||
| Niemann-Pick
disease Types A & B |
AJ | |||
| Spinal muscular
atrophy |
African American, AJ, Asian, Caucasian, Hispanic | |||
| Tay-Sachs disease | AJ, French Canadian, general population | |||
| Usher syndrome,
Type IF |
AJ | |||
| Usher syndrome,
Type IIIA |
AJ | |||
| Walker-Warburg
syndrome |
AJ | |||
QHerit is now available for order by US physicians. For more information, visit www.QHerit.com. ![]()
Quest Diagnostics has announced the US launch of QHerit™, a genetic screening service that helps people of multiple ethnicities identify their risk of passing on heritable disorders to their offspring.
The QHerit Pan-Ethnic Expanded Carrier Screen is a panel of tests for the 22 heritable diseases cited in new screening guidelines from the American College of Gynecology (ACOG).
Among the diseases are alpha-thalassemia, Fanconi anemia, and beta-hemoglobinopathies, including sickle cell disease (SCD).
Traditionally, genetic carrier screening has been used for at-risk populations based on specific ancestry assumptions and focused on only a few likely disorders with higher prevalence associated with that ethnicity.
In its new guidelines, ACOG recommends offering pan-ethnic, expanded carrier, and ethnic-specific screening for all women considering pregnancy. The guidelines also state that the partner of a woman who tests positive may be a candidate for screening.
QHerit screens women and men for clinically relevant variants of genes for disorders that could have potentially devastating consequences, result in early death, or create a need for significant early intervention.
The disorders covered by QHerit include:
| Disease | Race/ethnicity | |||
| Alpha-thalassemia | Mediterranean, Middle East, Southeast Asian, African, Chinese, Asian Indian | |||
| Beta-
hemoglobinopathies (including SCD) |
Mediterranean, Middle East, Southeast Asian, African, Chinese, Asian Indian | |||
| Bloom syndrome | Ashkenazi Jewish descent (AJ) | |||
| Canavan disease | AJ and non-AJ | |||
| Cystic fibrosis | African American, AJ, Asian American, Hispanic American, non-Hispanic Caucasian | |||
| Dihydrolipoamide
dehydrogenase deficiency |
AJ | |||
| Familial dysautonomia | AJ | |||
| Familial hyperinsulinism | AJ | |||
| Fanconi anemia Type C | AJ | |||
| Fragile X syndrome | Females | |||
| Gaucher disease | AJ | |||
| Glycogen storage
disease Type Ia |
AJ, Caucasian | |||
| Joubert syndrome 2 | AJ | |||
| Maple syrup urine
disease |
AJ | |||
| Mucolipidosis Type IV | AJ | |||
| Nemaline myopathy | AJ | |||
| Niemann-Pick
disease Types A & B |
AJ | |||
| Spinal muscular
atrophy |
African American, AJ, Asian, Caucasian, Hispanic | |||
| Tay-Sachs disease | AJ, French Canadian, general population | |||
| Usher syndrome,
Type IF |
AJ | |||
| Usher syndrome,
Type IIIA |
AJ | |||
| Walker-Warburg
syndrome |
AJ | |||
QHerit is now available for order by US physicians. For more information, visit www.QHerit.com. ![]()
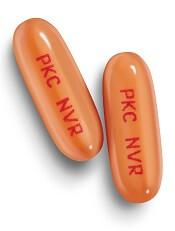
CHMP recommends midostaurin for FLT3+ AML, SM
The European Medicines Agency's Committee for Medicinal Products for Human Use (CHMP) is recommending approval for midostaurin (Rydapt®) as a treatment for acute myeloid leukemia (AML) and systemic mastocytosis (SM).
If approved by the European Commission, midostaurin would be used in combination with standard daunorubicin and cytarabine induction and high-dose cytarabine consolidation—followed by midostaurin maintenance for patients in complete response—in adults with newly diagnosed acute myeloid leukemia (AML) who are FLT3-mutation-positive.
Midostaurin would also be approved to treat adults with aggressive SM, SM with associated hematological neoplasm (SM-AHN), and mast cell leukemia (MCL).
If approved, midostaurin would be the first targeted treatment available in the European Union for newly diagnosed FLT3+ AML patients and advanced SM patients.
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 2 to 3 months’ of the CHMP’s recommendation. The decision will be applicable to all member states of the European Union, plus Iceland, Liechtenstein, and Norway.
Midostaurin in AML
The CHMP’s recommendation for midostaurin in AML is based on results from the phase 3 RATIFY trial, which were recently published in NEJM.
In RATIFY, researchers compared midostaurin plus standard chemotherapy to placebo plus standard chemotherapy in 717 adults younger than age 60 who had FLT3-mutated AML.
The median overall survival was significantly longer in the midostaurin arm than the placebo arm—74.7 months and 25.6 months, respectively (hazard ratio=0.77, P=0.016).
And the median event-free survival was significantly longer in the midostaurin arm than the placebo arm—8.2 months and 3.0 months, respectively (hazard ratio=0.78, P=0.004).
The most frequent adverse events (AEs) in the midostaurin arm (occurring in at least 20% of patients) were febrile neutropenia, nausea, vomiting, mucositis, headache, musculoskeletal pain, petechiae, device-related infection, epistaxis, hyperglycemia, and upper respiratory tract infections.
The most frequent grade 3/4 AEs (occurring in at least 10% of patients) were febrile neutropenia, device-related infection, and mucositis. Nine percent of patients in the midostaurin arm stopped treatment due to AEs, as did 6% in the placebo arm.
Midostaurin in advanced SM
The CHMP’s recommendation for midostaurin in advanced SM was based on results from a pair of phase 2, single-arm studies, hereafter referred to as Study 2 and Study 3.
Data from Study 2 were published in NEJM in June 2016, and data from Study 3 were presented at the 2010 ASH Annual Meeting.
Study 2 included 116 patients, 115 of whom were evaluable for response.
The overall response rate (ORR) was 17% in the entire cohort, 31% among patients with ASM, 11% among patients with SM-AHN, and 19% among patients with MCL. The complete response rates were 2%, 6%, 0%, and 5%, respectively.
Study 3 included 26 patients with advanced SM. In 3 of the patients, the subtype of SM was unconfirmed.
Among the 17 patients with SM-AHN, there were 10 responses (ORR=59%), including 1 partial response and 9 major responses. In the 6 patients with MCL, there were 2 responses (ORR=33%), which included 1 partial response and 1 major response.
In both studies combined, there were 142 adults with ASM, SM-AHN, or MCL.
The most frequent AEs (excluding laboratory abnormalities) that occurred in at least 20% of these patients were nausea, vomiting, diarrhea, edema, musculoskeletal pain, abdominal pain, fatigue, upper respiratory tract infection, constipation, pyrexia, headache, and dyspnea.
The most frequent grade 3 or higher AEs (excluding laboratory abnormalities) that occurred in at least 5% of patients were fatigue, sepsis, gastrointestinal hemorrhage, pneumonia, diarrhea, febrile neutropenia, edema, dyspnea, nausea, vomiting, abdominal pain, and renal insufficiency.
Serious AEs occurred in 68% of patients, most commonly infections and gastrointestinal disorders. Twenty-one percent of patients discontinued treatment due to AEs, the most frequent of which were infection, nausea or vomiting, QT prolongation, and gastrointestinal hemorrhage. ![]()
The European Medicines Agency's Committee for Medicinal Products for Human Use (CHMP) is recommending approval for midostaurin (Rydapt®) as a treatment for acute myeloid leukemia (AML) and systemic mastocytosis (SM).
If approved by the European Commission, midostaurin would be used in combination with standard daunorubicin and cytarabine induction and high-dose cytarabine consolidation—followed by midostaurin maintenance for patients in complete response—in adults with newly diagnosed acute myeloid leukemia (AML) who are FLT3-mutation-positive.
Midostaurin would also be approved to treat adults with aggressive SM, SM with associated hematological neoplasm (SM-AHN), and mast cell leukemia (MCL).
If approved, midostaurin would be the first targeted treatment available in the European Union for newly diagnosed FLT3+ AML patients and advanced SM patients.
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 2 to 3 months’ of the CHMP’s recommendation. The decision will be applicable to all member states of the European Union, plus Iceland, Liechtenstein, and Norway.
Midostaurin in AML
The CHMP’s recommendation for midostaurin in AML is based on results from the phase 3 RATIFY trial, which were recently published in NEJM.
In RATIFY, researchers compared midostaurin plus standard chemotherapy to placebo plus standard chemotherapy in 717 adults younger than age 60 who had FLT3-mutated AML.
The median overall survival was significantly longer in the midostaurin arm than the placebo arm—74.7 months and 25.6 months, respectively (hazard ratio=0.77, P=0.016).
And the median event-free survival was significantly longer in the midostaurin arm than the placebo arm—8.2 months and 3.0 months, respectively (hazard ratio=0.78, P=0.004).
The most frequent adverse events (AEs) in the midostaurin arm (occurring in at least 20% of patients) were febrile neutropenia, nausea, vomiting, mucositis, headache, musculoskeletal pain, petechiae, device-related infection, epistaxis, hyperglycemia, and upper respiratory tract infections.
The most frequent grade 3/4 AEs (occurring in at least 10% of patients) were febrile neutropenia, device-related infection, and mucositis. Nine percent of patients in the midostaurin arm stopped treatment due to AEs, as did 6% in the placebo arm.
Midostaurin in advanced SM
The CHMP’s recommendation for midostaurin in advanced SM was based on results from a pair of phase 2, single-arm studies, hereafter referred to as Study 2 and Study 3.
Data from Study 2 were published in NEJM in June 2016, and data from Study 3 were presented at the 2010 ASH Annual Meeting.
Study 2 included 116 patients, 115 of whom were evaluable for response.
The overall response rate (ORR) was 17% in the entire cohort, 31% among patients with ASM, 11% among patients with SM-AHN, and 19% among patients with MCL. The complete response rates were 2%, 6%, 0%, and 5%, respectively.
Study 3 included 26 patients with advanced SM. In 3 of the patients, the subtype of SM was unconfirmed.
Among the 17 patients with SM-AHN, there were 10 responses (ORR=59%), including 1 partial response and 9 major responses. In the 6 patients with MCL, there were 2 responses (ORR=33%), which included 1 partial response and 1 major response.
In both studies combined, there were 142 adults with ASM, SM-AHN, or MCL.
The most frequent AEs (excluding laboratory abnormalities) that occurred in at least 20% of these patients were nausea, vomiting, diarrhea, edema, musculoskeletal pain, abdominal pain, fatigue, upper respiratory tract infection, constipation, pyrexia, headache, and dyspnea.
The most frequent grade 3 or higher AEs (excluding laboratory abnormalities) that occurred in at least 5% of patients were fatigue, sepsis, gastrointestinal hemorrhage, pneumonia, diarrhea, febrile neutropenia, edema, dyspnea, nausea, vomiting, abdominal pain, and renal insufficiency.
Serious AEs occurred in 68% of patients, most commonly infections and gastrointestinal disorders. Twenty-one percent of patients discontinued treatment due to AEs, the most frequent of which were infection, nausea or vomiting, QT prolongation, and gastrointestinal hemorrhage. ![]()
The European Medicines Agency's Committee for Medicinal Products for Human Use (CHMP) is recommending approval for midostaurin (Rydapt®) as a treatment for acute myeloid leukemia (AML) and systemic mastocytosis (SM).
If approved by the European Commission, midostaurin would be used in combination with standard daunorubicin and cytarabine induction and high-dose cytarabine consolidation—followed by midostaurin maintenance for patients in complete response—in adults with newly diagnosed acute myeloid leukemia (AML) who are FLT3-mutation-positive.
Midostaurin would also be approved to treat adults with aggressive SM, SM with associated hematological neoplasm (SM-AHN), and mast cell leukemia (MCL).
If approved, midostaurin would be the first targeted treatment available in the European Union for newly diagnosed FLT3+ AML patients and advanced SM patients.
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 2 to 3 months’ of the CHMP’s recommendation. The decision will be applicable to all member states of the European Union, plus Iceland, Liechtenstein, and Norway.
Midostaurin in AML
The CHMP’s recommendation for midostaurin in AML is based on results from the phase 3 RATIFY trial, which were recently published in NEJM.
In RATIFY, researchers compared midostaurin plus standard chemotherapy to placebo plus standard chemotherapy in 717 adults younger than age 60 who had FLT3-mutated AML.
The median overall survival was significantly longer in the midostaurin arm than the placebo arm—74.7 months and 25.6 months, respectively (hazard ratio=0.77, P=0.016).
And the median event-free survival was significantly longer in the midostaurin arm than the placebo arm—8.2 months and 3.0 months, respectively (hazard ratio=0.78, P=0.004).
The most frequent adverse events (AEs) in the midostaurin arm (occurring in at least 20% of patients) were febrile neutropenia, nausea, vomiting, mucositis, headache, musculoskeletal pain, petechiae, device-related infection, epistaxis, hyperglycemia, and upper respiratory tract infections.
The most frequent grade 3/4 AEs (occurring in at least 10% of patients) were febrile neutropenia, device-related infection, and mucositis. Nine percent of patients in the midostaurin arm stopped treatment due to AEs, as did 6% in the placebo arm.
Midostaurin in advanced SM
The CHMP’s recommendation for midostaurin in advanced SM was based on results from a pair of phase 2, single-arm studies, hereafter referred to as Study 2 and Study 3.
Data from Study 2 were published in NEJM in June 2016, and data from Study 3 were presented at the 2010 ASH Annual Meeting.
Study 2 included 116 patients, 115 of whom were evaluable for response.
The overall response rate (ORR) was 17% in the entire cohort, 31% among patients with ASM, 11% among patients with SM-AHN, and 19% among patients with MCL. The complete response rates were 2%, 6%, 0%, and 5%, respectively.
Study 3 included 26 patients with advanced SM. In 3 of the patients, the subtype of SM was unconfirmed.
Among the 17 patients with SM-AHN, there were 10 responses (ORR=59%), including 1 partial response and 9 major responses. In the 6 patients with MCL, there were 2 responses (ORR=33%), which included 1 partial response and 1 major response.
In both studies combined, there were 142 adults with ASM, SM-AHN, or MCL.
The most frequent AEs (excluding laboratory abnormalities) that occurred in at least 20% of these patients were nausea, vomiting, diarrhea, edema, musculoskeletal pain, abdominal pain, fatigue, upper respiratory tract infection, constipation, pyrexia, headache, and dyspnea.
The most frequent grade 3 or higher AEs (excluding laboratory abnormalities) that occurred in at least 5% of patients were fatigue, sepsis, gastrointestinal hemorrhage, pneumonia, diarrhea, febrile neutropenia, edema, dyspnea, nausea, vomiting, abdominal pain, and renal insufficiency.
Serious AEs occurred in 68% of patients, most commonly infections and gastrointestinal disorders. Twenty-one percent of patients discontinued treatment due to AEs, the most frequent of which were infection, nausea or vomiting, QT prolongation, and gastrointestinal hemorrhage. ![]()
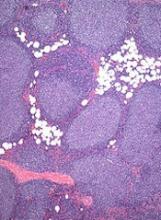
CHMP recommends new indication for obinutuzumab
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the marketing authorization for obinutuzumab (Gazyvaro).
The new proposed indication is for obinutuzumab in combination with chemotherapy for patients with previously untreated, advanced follicular lymphoma (FL). This would be followed by obinutuzumab maintenance in patients who achieved a response.
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 2 to 3 months’ of the CHMP’s recommendation.
The decision will be applicable to all member states of the European Union, plus Iceland, Liechtenstein, and Norway.
If approved for this new indication, obinutuzumab will be authorized for use in the European Economic Area as follows:
- In combination with chlorambucil for the treatment of adults with previously untreated chronic lymphocytic leukemia and comorbidities making them unsuitable for full-dose fludarabine-based therapy.
- In combination with bendamustine, followed by obinutuzumab maintenance, for the treatment of patients with FL who did not respond to, or who progressed during or up to 6 months after, treatment with rituximab or a rituximab-containing regimen.
- In combination with chemotherapy, followed by obinutuzumab maintenance in responders, for the treatment of patients with previously untreated, advanced FL.
GALLIUM trial
The CHMP’s recommendation is based on results of the phase 3 GALLIUM trial, which were presented at the 2016 ASH Annual Meeting.
The study enrolled 1401 patients with previously untreated, indolent non-Hodgkin lymphoma, including 1202 with FL.
Half of the FL patients (n=601) were randomized to receive obinutuzumab plus chemotherapy (followed by obinutuzumab maintenance for up to 2 years), and half were randomized to rituximab plus chemotherapy (followed by rituximab maintenance for up to 2 years).
The different chemotherapies used were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), CVP (cyclophosphamide, vincristine, and prednisolone), and bendamustine.
Patients who received obinutuzumab had significantly better progression-free survival than patients who received rituximab. The 3-year progression-free survival rate was 73.3% in the rituximab arm and 80% in the obinutuzumab arm (hazard ratio [HR]=0.66, P=0.0012).
There was no significant difference between the treatment arms with regard to overall survival. The 3-year overall survival was 92.1% in the rituximab arm and 94% in the obinutuzumab arm (HR=0.75, P=0.21).
The overall incidence of adverse events (AEs) was 98.3% in the rituximab arm and 99.5% in the obinutuzumab arm. The incidence of serious AEs was 39.9% and 46.1%, respectively.
The incidence of grade 3 or higher AEs was higher among patients who received obinutuzumab.
Grade 3 or higher AEs occurring in at least 5% of patients in either arm (rituximab and obinutuzumab, respectively) included neutropenia (67.8% and 74.6%), leukopenia (37.9% and 43.9%), febrile neutropenia (4.9% and 6.9%), infections and infestations (3.7% and 6.7%), and thrombocytopenia (2.7% and 6.1%). ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the marketing authorization for obinutuzumab (Gazyvaro).
The new proposed indication is for obinutuzumab in combination with chemotherapy for patients with previously untreated, advanced follicular lymphoma (FL). This would be followed by obinutuzumab maintenance in patients who achieved a response.
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 2 to 3 months’ of the CHMP’s recommendation.
The decision will be applicable to all member states of the European Union, plus Iceland, Liechtenstein, and Norway.
If approved for this new indication, obinutuzumab will be authorized for use in the European Economic Area as follows:
- In combination with chlorambucil for the treatment of adults with previously untreated chronic lymphocytic leukemia and comorbidities making them unsuitable for full-dose fludarabine-based therapy.
- In combination with bendamustine, followed by obinutuzumab maintenance, for the treatment of patients with FL who did not respond to, or who progressed during or up to 6 months after, treatment with rituximab or a rituximab-containing regimen.
- In combination with chemotherapy, followed by obinutuzumab maintenance in responders, for the treatment of patients with previously untreated, advanced FL.
GALLIUM trial
The CHMP’s recommendation is based on results of the phase 3 GALLIUM trial, which were presented at the 2016 ASH Annual Meeting.
The study enrolled 1401 patients with previously untreated, indolent non-Hodgkin lymphoma, including 1202 with FL.
Half of the FL patients (n=601) were randomized to receive obinutuzumab plus chemotherapy (followed by obinutuzumab maintenance for up to 2 years), and half were randomized to rituximab plus chemotherapy (followed by rituximab maintenance for up to 2 years).
The different chemotherapies used were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), CVP (cyclophosphamide, vincristine, and prednisolone), and bendamustine.
Patients who received obinutuzumab had significantly better progression-free survival than patients who received rituximab. The 3-year progression-free survival rate was 73.3% in the rituximab arm and 80% in the obinutuzumab arm (hazard ratio [HR]=0.66, P=0.0012).
There was no significant difference between the treatment arms with regard to overall survival. The 3-year overall survival was 92.1% in the rituximab arm and 94% in the obinutuzumab arm (HR=0.75, P=0.21).
The overall incidence of adverse events (AEs) was 98.3% in the rituximab arm and 99.5% in the obinutuzumab arm. The incidence of serious AEs was 39.9% and 46.1%, respectively.
The incidence of grade 3 or higher AEs was higher among patients who received obinutuzumab.
Grade 3 or higher AEs occurring in at least 5% of patients in either arm (rituximab and obinutuzumab, respectively) included neutropenia (67.8% and 74.6%), leukopenia (37.9% and 43.9%), febrile neutropenia (4.9% and 6.9%), infections and infestations (3.7% and 6.7%), and thrombocytopenia (2.7% and 6.1%). ![]()
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the marketing authorization for obinutuzumab (Gazyvaro).
The new proposed indication is for obinutuzumab in combination with chemotherapy for patients with previously untreated, advanced follicular lymphoma (FL). This would be followed by obinutuzumab maintenance in patients who achieved a response.
The European Commission typically adheres to the CHMP’s recommendations and delivers its final decision within 2 to 3 months’ of the CHMP’s recommendation.
The decision will be applicable to all member states of the European Union, plus Iceland, Liechtenstein, and Norway.
If approved for this new indication, obinutuzumab will be authorized for use in the European Economic Area as follows:
- In combination with chlorambucil for the treatment of adults with previously untreated chronic lymphocytic leukemia and comorbidities making them unsuitable for full-dose fludarabine-based therapy.
- In combination with bendamustine, followed by obinutuzumab maintenance, for the treatment of patients with FL who did not respond to, or who progressed during or up to 6 months after, treatment with rituximab or a rituximab-containing regimen.
- In combination with chemotherapy, followed by obinutuzumab maintenance in responders, for the treatment of patients with previously untreated, advanced FL.
GALLIUM trial
The CHMP’s recommendation is based on results of the phase 3 GALLIUM trial, which were presented at the 2016 ASH Annual Meeting.
The study enrolled 1401 patients with previously untreated, indolent non-Hodgkin lymphoma, including 1202 with FL.
Half of the FL patients (n=601) were randomized to receive obinutuzumab plus chemotherapy (followed by obinutuzumab maintenance for up to 2 years), and half were randomized to rituximab plus chemotherapy (followed by rituximab maintenance for up to 2 years).
The different chemotherapies used were CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), CVP (cyclophosphamide, vincristine, and prednisolone), and bendamustine.
Patients who received obinutuzumab had significantly better progression-free survival than patients who received rituximab. The 3-year progression-free survival rate was 73.3% in the rituximab arm and 80% in the obinutuzumab arm (hazard ratio [HR]=0.66, P=0.0012).
There was no significant difference between the treatment arms with regard to overall survival. The 3-year overall survival was 92.1% in the rituximab arm and 94% in the obinutuzumab arm (HR=0.75, P=0.21).
The overall incidence of adverse events (AEs) was 98.3% in the rituximab arm and 99.5% in the obinutuzumab arm. The incidence of serious AEs was 39.9% and 46.1%, respectively.
The incidence of grade 3 or higher AEs was higher among patients who received obinutuzumab.
Grade 3 or higher AEs occurring in at least 5% of patients in either arm (rituximab and obinutuzumab, respectively) included neutropenia (67.8% and 74.6%), leukopenia (37.9% and 43.9%), febrile neutropenia (4.9% and 6.9%), infections and infestations (3.7% and 6.7%), and thrombocytopenia (2.7% and 6.1%). ![]()
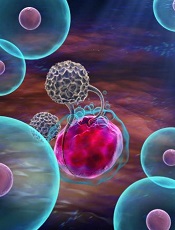
Modified, CB-derived NK cells target CLL and BL
Natural killer (NK) cells derived from cord blood (CB) can be modified to fight chronic lymphocytic leukemia (CLL) and Burkitt lymphoma (BL), according to research published in Leukemia.
Using a viral vector, researchers transduced CB-derived NK cells with a chimeric antigen receptor (CAR), interleukin-15 (IL-15), and an inducible caspase-9-based suicide gene.
The CAR directed the NK cells to kill CD19-expressing cells, IL-15 prolonged the NK cells’ survival and enhanced their antitumor activity, and the suicide gene allowed researchers to kill off the NK cells in the event of a severe inflammatory response.
“Natural killer cells are the immune system’s most potent killers, but they are short-lived, and cancers manage to evade a patient’s own NK cells to progress,” said study author Katy Rezvani, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston.
“Our cord-blood derived NK cells, genetically equipped with a receptor that focuses them on B-cell malignancies and with interleukin-15 to help them persist longer—potentially for months instead of 2 or 3 weeks—are designed to address these challenges.”
Dr Rezvani and her colleagues tested their CB-derived CAR NK cells in primary CLL cells and a mouse model of BL. Compared to unmodified NK cells, the CAR NK cells killed malignant cells more efficiently and extended the survival of mice.
Another experiment showed the CB-derived CAR NK cells killed CLL cells more efficiently than NK cells that were taken from CLL patients and modified in the same way. The researchers said this highlights the need to transplant CAR-engineered NK cells derived from healthy CB rather than using a patient’s own cells.
Additional experiments in the mouse model of BL showed that a single infusion of low-dose CAR NK cells resulted in prolonged survival.
When CAR NK cells were given at a higher dose, none of the mice died of BL. Half of them survived 100 days and beyond. However, all mice treated with other types of NK cells died by day 41.
Some mice treated with the higher dose of CAR NK cells died of cytokine release syndrome (CRS).
To counteract this toxicity, the researchers activated the suicide gene (iC9) via treatment with a small-molecule dimerizer, AP1903.
The team found that adding as little as 10 nM of AP1903 to cell cultures induced apoptosis/necrosis of the CAR NK cells within 4 hours but had no effect on non-CAR CB-derived NK cells. Similar results were observed in the mouse model.
Next steps
A phase 1/2 trial of these CB-derived CAR NK cells opened at MD Anderson in June for patients with relapsed or refractory CLL, acute lymphocytic leukemia, or non-Hodgkin lymphoma.
Dr Rezvani, the principal investigator of the trial, said the protocol calls for vigilance for signs of CRS, treatment with steroids and tocilizumab for low-grade CRS, and AP1903 added to activate the suicide gene for grade 3 or 4 CRS.
She and her colleagues noted that CB-derived NK cells do not cause graft-vs-host disease. Therefore, they can be an off-the-shelf product, prepared in advance with the necessary receptor and given to patients promptly.
The researchers are developing CB-derived CAR NK cells for other targets in hematologic and solid tumor malignancies.
MD Anderson and the researchers have intellectual property related to the engineered NK cells, which is being managed in accordance with the institution’s conflict-of-interest rules.
Funding for this research was provided by MD Anderson’s Moon Shots Program, the National Cancer Institute of the National Institutes of Health Cancer Center Support Grant (CA016672) to MD Anderson, and grants from the Leukemia and Lymphoma Society and the American Cancer Society. ![]()
Natural killer (NK) cells derived from cord blood (CB) can be modified to fight chronic lymphocytic leukemia (CLL) and Burkitt lymphoma (BL), according to research published in Leukemia.
Using a viral vector, researchers transduced CB-derived NK cells with a chimeric antigen receptor (CAR), interleukin-15 (IL-15), and an inducible caspase-9-based suicide gene.
The CAR directed the NK cells to kill CD19-expressing cells, IL-15 prolonged the NK cells’ survival and enhanced their antitumor activity, and the suicide gene allowed researchers to kill off the NK cells in the event of a severe inflammatory response.
“Natural killer cells are the immune system’s most potent killers, but they are short-lived, and cancers manage to evade a patient’s own NK cells to progress,” said study author Katy Rezvani, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston.
“Our cord-blood derived NK cells, genetically equipped with a receptor that focuses them on B-cell malignancies and with interleukin-15 to help them persist longer—potentially for months instead of 2 or 3 weeks—are designed to address these challenges.”
Dr Rezvani and her colleagues tested their CB-derived CAR NK cells in primary CLL cells and a mouse model of BL. Compared to unmodified NK cells, the CAR NK cells killed malignant cells more efficiently and extended the survival of mice.
Another experiment showed the CB-derived CAR NK cells killed CLL cells more efficiently than NK cells that were taken from CLL patients and modified in the same way. The researchers said this highlights the need to transplant CAR-engineered NK cells derived from healthy CB rather than using a patient’s own cells.
Additional experiments in the mouse model of BL showed that a single infusion of low-dose CAR NK cells resulted in prolonged survival.
When CAR NK cells were given at a higher dose, none of the mice died of BL. Half of them survived 100 days and beyond. However, all mice treated with other types of NK cells died by day 41.
Some mice treated with the higher dose of CAR NK cells died of cytokine release syndrome (CRS).
To counteract this toxicity, the researchers activated the suicide gene (iC9) via treatment with a small-molecule dimerizer, AP1903.
The team found that adding as little as 10 nM of AP1903 to cell cultures induced apoptosis/necrosis of the CAR NK cells within 4 hours but had no effect on non-CAR CB-derived NK cells. Similar results were observed in the mouse model.
Next steps
A phase 1/2 trial of these CB-derived CAR NK cells opened at MD Anderson in June for patients with relapsed or refractory CLL, acute lymphocytic leukemia, or non-Hodgkin lymphoma.
Dr Rezvani, the principal investigator of the trial, said the protocol calls for vigilance for signs of CRS, treatment with steroids and tocilizumab for low-grade CRS, and AP1903 added to activate the suicide gene for grade 3 or 4 CRS.
She and her colleagues noted that CB-derived NK cells do not cause graft-vs-host disease. Therefore, they can be an off-the-shelf product, prepared in advance with the necessary receptor and given to patients promptly.
The researchers are developing CB-derived CAR NK cells for other targets in hematologic and solid tumor malignancies.
MD Anderson and the researchers have intellectual property related to the engineered NK cells, which is being managed in accordance with the institution’s conflict-of-interest rules.
Funding for this research was provided by MD Anderson’s Moon Shots Program, the National Cancer Institute of the National Institutes of Health Cancer Center Support Grant (CA016672) to MD Anderson, and grants from the Leukemia and Lymphoma Society and the American Cancer Society. ![]()
Natural killer (NK) cells derived from cord blood (CB) can be modified to fight chronic lymphocytic leukemia (CLL) and Burkitt lymphoma (BL), according to research published in Leukemia.
Using a viral vector, researchers transduced CB-derived NK cells with a chimeric antigen receptor (CAR), interleukin-15 (IL-15), and an inducible caspase-9-based suicide gene.
The CAR directed the NK cells to kill CD19-expressing cells, IL-15 prolonged the NK cells’ survival and enhanced their antitumor activity, and the suicide gene allowed researchers to kill off the NK cells in the event of a severe inflammatory response.
“Natural killer cells are the immune system’s most potent killers, but they are short-lived, and cancers manage to evade a patient’s own NK cells to progress,” said study author Katy Rezvani, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston.
“Our cord-blood derived NK cells, genetically equipped with a receptor that focuses them on B-cell malignancies and with interleukin-15 to help them persist longer—potentially for months instead of 2 or 3 weeks—are designed to address these challenges.”
Dr Rezvani and her colleagues tested their CB-derived CAR NK cells in primary CLL cells and a mouse model of BL. Compared to unmodified NK cells, the CAR NK cells killed malignant cells more efficiently and extended the survival of mice.
Another experiment showed the CB-derived CAR NK cells killed CLL cells more efficiently than NK cells that were taken from CLL patients and modified in the same way. The researchers said this highlights the need to transplant CAR-engineered NK cells derived from healthy CB rather than using a patient’s own cells.
Additional experiments in the mouse model of BL showed that a single infusion of low-dose CAR NK cells resulted in prolonged survival.
When CAR NK cells were given at a higher dose, none of the mice died of BL. Half of them survived 100 days and beyond. However, all mice treated with other types of NK cells died by day 41.
Some mice treated with the higher dose of CAR NK cells died of cytokine release syndrome (CRS).
To counteract this toxicity, the researchers activated the suicide gene (iC9) via treatment with a small-molecule dimerizer, AP1903.
The team found that adding as little as 10 nM of AP1903 to cell cultures induced apoptosis/necrosis of the CAR NK cells within 4 hours but had no effect on non-CAR CB-derived NK cells. Similar results were observed in the mouse model.
Next steps
A phase 1/2 trial of these CB-derived CAR NK cells opened at MD Anderson in June for patients with relapsed or refractory CLL, acute lymphocytic leukemia, or non-Hodgkin lymphoma.
Dr Rezvani, the principal investigator of the trial, said the protocol calls for vigilance for signs of CRS, treatment with steroids and tocilizumab for low-grade CRS, and AP1903 added to activate the suicide gene for grade 3 or 4 CRS.
She and her colleagues noted that CB-derived NK cells do not cause graft-vs-host disease. Therefore, they can be an off-the-shelf product, prepared in advance with the necessary receptor and given to patients promptly.
The researchers are developing CB-derived CAR NK cells for other targets in hematologic and solid tumor malignancies.
MD Anderson and the researchers have intellectual property related to the engineered NK cells, which is being managed in accordance with the institution’s conflict-of-interest rules.
Funding for this research was provided by MD Anderson’s Moon Shots Program, the National Cancer Institute of the National Institutes of Health Cancer Center Support Grant (CA016672) to MD Anderson, and grants from the Leukemia and Lymphoma Society and the American Cancer Society. ![]()
AYA cancer survivors struggle with social functioning
New research suggests young cancer survivors struggle to get their social lives “back to normal” within the first 2 years of their diagnosis.
The study showed that adolescents and young adults (AYAs) with cancer had significantly worse social functioning than the general population around the time of cancer diagnosis as well as 1 year and 2 years later.
These findings were published in Cancer.
“The research is important to help these young survivors better reintegrate into society,” said study author Brad Zebrack, PhD, of the University of Michigan in Ann Arbor.
He and his colleagues collected data from 141 AYA cancer patients (ages 14 to 39) who visited 1 of 5 US medical facilities between March 2008 and April 2010.
The patients completed a self-report measure of social functioning within the first 4 months of diagnosis, then again at 12 months and 24 months.
Compared to the general population, the AYA cancer patients had significantly worse social functioning scores at all time points:
- Around the time of diagnosis—52.0 vs 85.1 (P<0.001)
- At 12 months—73.1 vs 85.1 (P<0.001)
- At 24 months—69.2 vs 85.1 (P<0.001).
Overall, the patients did experience improvements in social functioning from baseline to the 12-month time point, but their scores remained stable after that.
The researchers noted that 9% of patients had consistently high/normal social functioning, 47% had improvements in social functioning over time, 13% had worsening social functioning over time, and 32% had consistently low social functioning.
“This finding highlights the need to screen, identify, and respond to the needs of high-risk young adult-adolescent patients at the time of diagnosis and then monitor them over time,” Dr Zebrack said.
“They are likely the ones most in need of help in managing work, school, and potentially problematic relationships with family members and friends.”![]()
New research suggests young cancer survivors struggle to get their social lives “back to normal” within the first 2 years of their diagnosis.
The study showed that adolescents and young adults (AYAs) with cancer had significantly worse social functioning than the general population around the time of cancer diagnosis as well as 1 year and 2 years later.
These findings were published in Cancer.
“The research is important to help these young survivors better reintegrate into society,” said study author Brad Zebrack, PhD, of the University of Michigan in Ann Arbor.
He and his colleagues collected data from 141 AYA cancer patients (ages 14 to 39) who visited 1 of 5 US medical facilities between March 2008 and April 2010.
The patients completed a self-report measure of social functioning within the first 4 months of diagnosis, then again at 12 months and 24 months.
Compared to the general population, the AYA cancer patients had significantly worse social functioning scores at all time points:
- Around the time of diagnosis—52.0 vs 85.1 (P<0.001)
- At 12 months—73.1 vs 85.1 (P<0.001)
- At 24 months—69.2 vs 85.1 (P<0.001).
Overall, the patients did experience improvements in social functioning from baseline to the 12-month time point, but their scores remained stable after that.
The researchers noted that 9% of patients had consistently high/normal social functioning, 47% had improvements in social functioning over time, 13% had worsening social functioning over time, and 32% had consistently low social functioning.
“This finding highlights the need to screen, identify, and respond to the needs of high-risk young adult-adolescent patients at the time of diagnosis and then monitor them over time,” Dr Zebrack said.
“They are likely the ones most in need of help in managing work, school, and potentially problematic relationships with family members and friends.”![]()
New research suggests young cancer survivors struggle to get their social lives “back to normal” within the first 2 years of their diagnosis.
The study showed that adolescents and young adults (AYAs) with cancer had significantly worse social functioning than the general population around the time of cancer diagnosis as well as 1 year and 2 years later.
These findings were published in Cancer.
“The research is important to help these young survivors better reintegrate into society,” said study author Brad Zebrack, PhD, of the University of Michigan in Ann Arbor.
He and his colleagues collected data from 141 AYA cancer patients (ages 14 to 39) who visited 1 of 5 US medical facilities between March 2008 and April 2010.
The patients completed a self-report measure of social functioning within the first 4 months of diagnosis, then again at 12 months and 24 months.
Compared to the general population, the AYA cancer patients had significantly worse social functioning scores at all time points:
- Around the time of diagnosis—52.0 vs 85.1 (P<0.001)
- At 12 months—73.1 vs 85.1 (P<0.001)
- At 24 months—69.2 vs 85.1 (P<0.001).
Overall, the patients did experience improvements in social functioning from baseline to the 12-month time point, but their scores remained stable after that.
The researchers noted that 9% of patients had consistently high/normal social functioning, 47% had improvements in social functioning over time, 13% had worsening social functioning over time, and 32% had consistently low social functioning.
“This finding highlights the need to screen, identify, and respond to the needs of high-risk young adult-adolescent patients at the time of diagnosis and then monitor them over time,” Dr Zebrack said.
“They are likely the ones most in need of help in managing work, school, and potentially problematic relationships with family members and friends.”![]()
FDA grants orphan designation to gilteritinib in AML
The US Food and Drug Administration (FDA) has granted orphan drug designation to gilteritinib for the treatment of patients with acute myeloid leukemia (AML).
Gilteritinib, an inhibitor of FLT3 and AXL, has demonstrated activity against FLT3 internal tandem duplication (ITD) as well as tyrosine kinase domain, 2 mutations that are seen in up to a third of patients with AML.
Astellas Pharma Inc. is currently investigating gilteritinib in phase 3 trials of AML patients.
Results from a phase 1/2 study of gilteritinib in AML were presented at the 2017 ASCO Annual Meeting.
The goal of the study was to determine the tolerability and antileukemic activity of once-daily gilteritinib in a FLT3-ITD-enriched, relapsed/refractory AML population.
The drug exhibited “potent” FLT3 inhibition at doses greater than 80 mg/day. In patients who received such doses, the greatest overall response rate was 52%, and the longest median overall survival was 31 weeks.
The maximum tolerated dose of gilteritinib was 300 mg/day. Dose-limiting toxicities included diarrhea and liver function abnormalities.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to gilteritinib for the treatment of patients with acute myeloid leukemia (AML).
Gilteritinib, an inhibitor of FLT3 and AXL, has demonstrated activity against FLT3 internal tandem duplication (ITD) as well as tyrosine kinase domain, 2 mutations that are seen in up to a third of patients with AML.
Astellas Pharma Inc. is currently investigating gilteritinib in phase 3 trials of AML patients.
Results from a phase 1/2 study of gilteritinib in AML were presented at the 2017 ASCO Annual Meeting.
The goal of the study was to determine the tolerability and antileukemic activity of once-daily gilteritinib in a FLT3-ITD-enriched, relapsed/refractory AML population.
The drug exhibited “potent” FLT3 inhibition at doses greater than 80 mg/day. In patients who received such doses, the greatest overall response rate was 52%, and the longest median overall survival was 31 weeks.
The maximum tolerated dose of gilteritinib was 300 mg/day. Dose-limiting toxicities included diarrhea and liver function abnormalities.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to gilteritinib for the treatment of patients with acute myeloid leukemia (AML).
Gilteritinib, an inhibitor of FLT3 and AXL, has demonstrated activity against FLT3 internal tandem duplication (ITD) as well as tyrosine kinase domain, 2 mutations that are seen in up to a third of patients with AML.
Astellas Pharma Inc. is currently investigating gilteritinib in phase 3 trials of AML patients.
Results from a phase 1/2 study of gilteritinib in AML were presented at the 2017 ASCO Annual Meeting.
The goal of the study was to determine the tolerability and antileukemic activity of once-daily gilteritinib in a FLT3-ITD-enriched, relapsed/refractory AML population.
The drug exhibited “potent” FLT3 inhibition at doses greater than 80 mg/day. In patients who received such doses, the greatest overall response rate was 52%, and the longest median overall survival was 31 weeks.
The maximum tolerated dose of gilteritinib was 300 mg/day. Dose-limiting toxicities included diarrhea and liver function abnormalities.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
FDA approves generic tranexamic acid
Zydus Cadila has received approval from the US Food and Drug Administration (FDA) to market a tranexamic acid product for use in patients with hemophilia.
The company’s product—Tranexamic Acid Injection, 1000 mg/10 mL (100 mg/mL) Single Dose Vial—can be used to prevent or reduce bleeding in hemophilia patients undergoing tooth extraction.
Zydus Cadila’s tranexamic acid will be produced at a manufacturing facility in Moraiya, Gujarat, India. ![]()
Zydus Cadila has received approval from the US Food and Drug Administration (FDA) to market a tranexamic acid product for use in patients with hemophilia.
The company’s product—Tranexamic Acid Injection, 1000 mg/10 mL (100 mg/mL) Single Dose Vial—can be used to prevent or reduce bleeding in hemophilia patients undergoing tooth extraction.
Zydus Cadila’s tranexamic acid will be produced at a manufacturing facility in Moraiya, Gujarat, India. ![]()
Zydus Cadila has received approval from the US Food and Drug Administration (FDA) to market a tranexamic acid product for use in patients with hemophilia.
The company’s product—Tranexamic Acid Injection, 1000 mg/10 mL (100 mg/mL) Single Dose Vial—can be used to prevent or reduce bleeding in hemophilia patients undergoing tooth extraction.
Zydus Cadila’s tranexamic acid will be produced at a manufacturing facility in Moraiya, Gujarat, India.
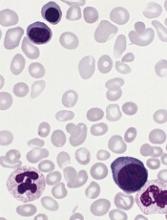
Predicting response to azacitidine in MDS
Research published in Cell Reports helps explain why some patients with myelodysplastic syndrome (MDS) do not respond to treatment with azacitidine.
The study showed that patients who were resistant to the drug had relatively quiescent hematopoietic progenitor cells (HPCs).
A smaller proportion of their HPCs were undergoing active cell-cycle progression when compared to the HPCs of patients who responded to azacitidine.
This discovery could provide the first method to identify non-responders to azacitidine early, according to study author Ashwin Unnikrishnan, PhD, of the University of New South Wales in Sydney, Australia.
“These are early days, but this could avoid what has really been a ‘wait and see’ approach with patients that sometimes results in them receiving futile treatment for 6 months,” Dr Unnikrishnan said.
“By that stage, the patient’s disease has progressed, and there’s no alternative for them.”
Dr Unnikrishnan and his colleagues also found the HPC quiescence in non-responders was mediated by integrin α5 (ITGA5) signaling, and the cells’ hematopoietic potential improved when the team combined azacitidine treatment with an ITGA5 inhibitor.
This suggests a potential avenue for future combination therapies that would improve azacitidine responsiveness.
Lastly, the researchers made discoveries that could explain why some patients who initially respond to azacitidine eventually relapse.
“All of the pernicious mutations that we associate with MDS never disappear in these patients, even after years of treatment,” Dr Unnikrishnan said. “From a clinical perspective, blood cell production is restored in patients, but they are a ticking time bomb, waiting to relapse.”
“[Azacitidine] is not a cure, and we are starting to understand why it does what it does. We need to find better treatments than azacitidine if we want a more durable therapy for MDS, and that’s the basis for our future work.”
Research published in Cell Reports helps explain why some patients with myelodysplastic syndrome (MDS) do not respond to treatment with azacitidine.
The study showed that patients who were resistant to the drug had relatively quiescent hematopoietic progenitor cells (HPCs).
A smaller proportion of their HPCs were undergoing active cell-cycle progression when compared to the HPCs of patients who responded to azacitidine.
This discovery could provide the first method to identify non-responders to azacitidine early, according to study author Ashwin Unnikrishnan, PhD, of the University of New South Wales in Sydney, Australia.
“These are early days, but this could avoid what has really been a ‘wait and see’ approach with patients that sometimes results in them receiving futile treatment for 6 months,” Dr Unnikrishnan said.
“By that stage, the patient’s disease has progressed, and there’s no alternative for them.”
Dr Unnikrishnan and his colleagues also found the HPC quiescence in non-responders was mediated by integrin α5 (ITGA5) signaling, and the cells’ hematopoietic potential improved when the team combined azacitidine treatment with an ITGA5 inhibitor.
This suggests a potential avenue for future combination therapies that would improve azacitidine responsiveness.
Lastly, the researchers made discoveries that could explain why some patients who initially respond to azacitidine eventually relapse.
“All of the pernicious mutations that we associate with MDS never disappear in these patients, even after years of treatment,” Dr Unnikrishnan said. “From a clinical perspective, blood cell production is restored in patients, but they are a ticking time bomb, waiting to relapse.”
“[Azacitidine] is not a cure, and we are starting to understand why it does what it does. We need to find better treatments than azacitidine if we want a more durable therapy for MDS, and that’s the basis for our future work.”
Research published in Cell Reports helps explain why some patients with myelodysplastic syndrome (MDS) do not respond to treatment with azacitidine.
The study showed that patients who were resistant to the drug had relatively quiescent hematopoietic progenitor cells (HPCs).
A smaller proportion of their HPCs were undergoing active cell-cycle progression when compared to the HPCs of patients who responded to azacitidine.
This discovery could provide the first method to identify non-responders to azacitidine early, according to study author Ashwin Unnikrishnan, PhD, of the University of New South Wales in Sydney, Australia.
“These are early days, but this could avoid what has really been a ‘wait and see’ approach with patients that sometimes results in them receiving futile treatment for 6 months,” Dr Unnikrishnan said.
“By that stage, the patient’s disease has progressed, and there’s no alternative for them.”
Dr Unnikrishnan and his colleagues also found the HPC quiescence in non-responders was mediated by integrin α5 (ITGA5) signaling, and the cells’ hematopoietic potential improved when the team combined azacitidine treatment with an ITGA5 inhibitor.
This suggests a potential avenue for future combination therapies that would improve azacitidine responsiveness.
Lastly, the researchers made discoveries that could explain why some patients who initially respond to azacitidine eventually relapse.
“All of the pernicious mutations that we associate with MDS never disappear in these patients, even after years of treatment,” Dr Unnikrishnan said. “From a clinical perspective, blood cell production is restored in patients, but they are a ticking time bomb, waiting to relapse.”
“[Azacitidine] is not a cure, and we are starting to understand why it does what it does. We need to find better treatments than azacitidine if we want a more durable therapy for MDS, and that’s the basis for our future work.”
Product can reduce, prevent bleeding in kids with FXD
BERLIN—Results of a phase 3 study suggest prophylaxis with plasma-derived factor X (pdFX, Coagadex®) prevents or reduces bleeding episodes in children with moderate to severe hereditary factor X deficiency (FXD).
pdFX was well tolerated in this study as well, with no treatment-related adverse events (AEs) reported.
“For the first time, we have data providing physicians with important evidence of the efficacy and safety of Coagadex as a prophylactic regimen for the reduction and prevention of bleeding episodes, as well as potential guidance on dosing for children with hereditary factor X deficiency,” said Michael Gattens, MBChB, a consultant pediatric hematologist at Cambridge University Hospitals in the UK and an investigator involved in this trial.
Data from the trial, known as TEN02, were presented in a poster (PB 818) at the International Society on Thrombosis and Haemostasis (ISTH) 2017 Congress. The trial was sponsored by Bio Products Laboratory Limited.
TEN02 was a prospective study conducted in children younger than 12 years with moderate or severe congenital FXD (basal plasma factor X activity <5 IU/dL at diagnosis) and either a history of severe bleeding or an F10 gene mutation causing a documented severe bleeding type.
The study enrolled 9 patients. Eight had severe FXD (FX:C <1 IU/dL), and 1 had moderate FXD (FX:C 1–5 IU/dL).
The patients’ mean age was 7.3 (range, 2.6 years to 11.9 years). Four patients were in the 0-5 age group, and 5 were in the 6-11 age group. Fifty-six percent of patients were female, 78% were Asian, and 22% were white.
The patients had a total of 21 prior bleeds, including overt (n=10), covert (n=9), and menorrhagic (n=2). The past bleeds were spontaneous (n=16) or caused by injury (n=2), menorrhagia (n=2), or surgery (n=2).
Treatment
Patients received 50 IU/kg of pdFX at visit 1 (baseline), followed 72 hours later by a second dose (visit 2). At the investigator’s discretion, visit 2 may have been conducted 48 hours after the first dose for subjects ages 0 to 5.
Following visit 2, patients used pdFX at 40-50 IU/kg as routine prophylaxis every 72 ± 2 hours or every 48 ± 2 hours for those age 0 to 5, at the investigator’s discretion. Dose and frequency were adjusted over the initial 6 weeks to maintain FX:C levels ≥5 IU/dL (with peak levels ≤120 IU/dL).
Treatment was continued for at least 26 weeks, with a minimum of 50 treatment days.
Following visit 2, patients returned to the study site for 3 additional visits (after 9-28, 29-42, and 50 treatment days/26 weeks; visits 3-5), during which time blood samples were collected to assess FX:C trough levels and vital signs and AEs were checked.
A final bolus dose of 50 IU/kg was administered during visit 5 to assess post-dose incremental recovery.
A dose of 25 IU/kg was recommended to treat minor bleeds, and 50 IU/kg was recommended for major bleeds. Treatment was to be repeated as often as necessary based on FX:C recovery levels and clinical need.
Nine patients completed 11 treatment cycles, including 2 patients who had 50 exposure days but less than 26 study weeks. These patients were re-screened and completed a second, per-protocol treatment cycle.
Results
A total of 537 prophylactic infusions were administered, with a mean dose of 38.6 IU/kg per patient.
Investigators rated the prophylactic efficacy of pdFX as “excellent.”
There were 10 bleeds in 3 patients. Four bleeds in 2 patients (both in the 6-11 age group) required treatment with a single infusion of pdFX (mean dose, 31.7±10.1 IU/kg).
The overall mean 30-minute incremental recovery was 1.66 IU/dL per IU/kg for patients’ baseline visit, 1.82 IU/dL per IU/kg for the end-of-study visit, and 1.74 IU/dL per IU/kg for both visits combined.
Incremental recovery was significantly lower in the 0-5 age group than the 6-11 age group:
- 1.45 vs 1.83 at baseline (P=0.027)
- 1.62 vs 1.99 at end of study (P=0.025)
- 1.53 vs 1.91 combined (P=0.001).
All patients had FX:C trough levels greater than 5% after visit 4 (days 29-42).
There were 28 AEs reported in 8 patients, but none of these events were considered related to treatment.
One patient did have 2 serious treatment-emergent AEs—lower respiratory tract infection and influenza.
There were no other serious AEs, no evidence of factor X inhibitor development, and no deaths.
BERLIN—Results of a phase 3 study suggest prophylaxis with plasma-derived factor X (pdFX, Coagadex®) prevents or reduces bleeding episodes in children with moderate to severe hereditary factor X deficiency (FXD).
pdFX was well tolerated in this study as well, with no treatment-related adverse events (AEs) reported.
“For the first time, we have data providing physicians with important evidence of the efficacy and safety of Coagadex as a prophylactic regimen for the reduction and prevention of bleeding episodes, as well as potential guidance on dosing for children with hereditary factor X deficiency,” said Michael Gattens, MBChB, a consultant pediatric hematologist at Cambridge University Hospitals in the UK and an investigator involved in this trial.
Data from the trial, known as TEN02, were presented in a poster (PB 818) at the International Society on Thrombosis and Haemostasis (ISTH) 2017 Congress. The trial was sponsored by Bio Products Laboratory Limited.
TEN02 was a prospective study conducted in children younger than 12 years with moderate or severe congenital FXD (basal plasma factor X activity <5 IU/dL at diagnosis) and either a history of severe bleeding or an F10 gene mutation causing a documented severe bleeding type.
The study enrolled 9 patients. Eight had severe FXD (FX:C <1 IU/dL), and 1 had moderate FXD (FX:C 1–5 IU/dL).
The patients’ mean age was 7.3 (range, 2.6 years to 11.9 years). Four patients were in the 0-5 age group, and 5 were in the 6-11 age group. Fifty-six percent of patients were female, 78% were Asian, and 22% were white.
The patients had a total of 21 prior bleeds, including overt (n=10), covert (n=9), and menorrhagic (n=2). The past bleeds were spontaneous (n=16) or caused by injury (n=2), menorrhagia (n=2), or surgery (n=2).
Treatment
Patients received 50 IU/kg of pdFX at visit 1 (baseline), followed 72 hours later by a second dose (visit 2). At the investigator’s discretion, visit 2 may have been conducted 48 hours after the first dose for subjects ages 0 to 5.
Following visit 2, patients used pdFX at 40-50 IU/kg as routine prophylaxis every 72 ± 2 hours or every 48 ± 2 hours for those age 0 to 5, at the investigator’s discretion. Dose and frequency were adjusted over the initial 6 weeks to maintain FX:C levels ≥5 IU/dL (with peak levels ≤120 IU/dL).
Treatment was continued for at least 26 weeks, with a minimum of 50 treatment days.
Following visit 2, patients returned to the study site for 3 additional visits (after 9-28, 29-42, and 50 treatment days/26 weeks; visits 3-5), during which time blood samples were collected to assess FX:C trough levels and vital signs and AEs were checked.
A final bolus dose of 50 IU/kg was administered during visit 5 to assess post-dose incremental recovery.
A dose of 25 IU/kg was recommended to treat minor bleeds, and 50 IU/kg was recommended for major bleeds. Treatment was to be repeated as often as necessary based on FX:C recovery levels and clinical need.
Nine patients completed 11 treatment cycles, including 2 patients who had 50 exposure days but less than 26 study weeks. These patients were re-screened and completed a second, per-protocol treatment cycle.
Results
A total of 537 prophylactic infusions were administered, with a mean dose of 38.6 IU/kg per patient.
Investigators rated the prophylactic efficacy of pdFX as “excellent.”
There were 10 bleeds in 3 patients. Four bleeds in 2 patients (both in the 6-11 age group) required treatment with a single infusion of pdFX (mean dose, 31.7±10.1 IU/kg).
The overall mean 30-minute incremental recovery was 1.66 IU/dL per IU/kg for patients’ baseline visit, 1.82 IU/dL per IU/kg for the end-of-study visit, and 1.74 IU/dL per IU/kg for both visits combined.
Incremental recovery was significantly lower in the 0-5 age group than the 6-11 age group:
- 1.45 vs 1.83 at baseline (P=0.027)
- 1.62 vs 1.99 at end of study (P=0.025)
- 1.53 vs 1.91 combined (P=0.001).
All patients had FX:C trough levels greater than 5% after visit 4 (days 29-42).
There were 28 AEs reported in 8 patients, but none of these events were considered related to treatment.
One patient did have 2 serious treatment-emergent AEs—lower respiratory tract infection and influenza.
There were no other serious AEs, no evidence of factor X inhibitor development, and no deaths.
BERLIN—Results of a phase 3 study suggest prophylaxis with plasma-derived factor X (pdFX, Coagadex®) prevents or reduces bleeding episodes in children with moderate to severe hereditary factor X deficiency (FXD).
pdFX was well tolerated in this study as well, with no treatment-related adverse events (AEs) reported.
“For the first time, we have data providing physicians with important evidence of the efficacy and safety of Coagadex as a prophylactic regimen for the reduction and prevention of bleeding episodes, as well as potential guidance on dosing for children with hereditary factor X deficiency,” said Michael Gattens, MBChB, a consultant pediatric hematologist at Cambridge University Hospitals in the UK and an investigator involved in this trial.
Data from the trial, known as TEN02, were presented in a poster (PB 818) at the International Society on Thrombosis and Haemostasis (ISTH) 2017 Congress. The trial was sponsored by Bio Products Laboratory Limited.
TEN02 was a prospective study conducted in children younger than 12 years with moderate or severe congenital FXD (basal plasma factor X activity <5 IU/dL at diagnosis) and either a history of severe bleeding or an F10 gene mutation causing a documented severe bleeding type.
The study enrolled 9 patients. Eight had severe FXD (FX:C <1 IU/dL), and 1 had moderate FXD (FX:C 1–5 IU/dL).
The patients’ mean age was 7.3 (range, 2.6 years to 11.9 years). Four patients were in the 0-5 age group, and 5 were in the 6-11 age group. Fifty-six percent of patients were female, 78% were Asian, and 22% were white.
The patients had a total of 21 prior bleeds, including overt (n=10), covert (n=9), and menorrhagic (n=2). The past bleeds were spontaneous (n=16) or caused by injury (n=2), menorrhagia (n=2), or surgery (n=2).
Treatment
Patients received 50 IU/kg of pdFX at visit 1 (baseline), followed 72 hours later by a second dose (visit 2). At the investigator’s discretion, visit 2 may have been conducted 48 hours after the first dose for subjects ages 0 to 5.
Following visit 2, patients used pdFX at 40-50 IU/kg as routine prophylaxis every 72 ± 2 hours or every 48 ± 2 hours for those age 0 to 5, at the investigator’s discretion. Dose and frequency were adjusted over the initial 6 weeks to maintain FX:C levels ≥5 IU/dL (with peak levels ≤120 IU/dL).
Treatment was continued for at least 26 weeks, with a minimum of 50 treatment days.
Following visit 2, patients returned to the study site for 3 additional visits (after 9-28, 29-42, and 50 treatment days/26 weeks; visits 3-5), during which time blood samples were collected to assess FX:C trough levels and vital signs and AEs were checked.
A final bolus dose of 50 IU/kg was administered during visit 5 to assess post-dose incremental recovery.
A dose of 25 IU/kg was recommended to treat minor bleeds, and 50 IU/kg was recommended for major bleeds. Treatment was to be repeated as often as necessary based on FX:C recovery levels and clinical need.
Nine patients completed 11 treatment cycles, including 2 patients who had 50 exposure days but less than 26 study weeks. These patients were re-screened and completed a second, per-protocol treatment cycle.
Results
A total of 537 prophylactic infusions were administered, with a mean dose of 38.6 IU/kg per patient.
Investigators rated the prophylactic efficacy of pdFX as “excellent.”
There were 10 bleeds in 3 patients. Four bleeds in 2 patients (both in the 6-11 age group) required treatment with a single infusion of pdFX (mean dose, 31.7±10.1 IU/kg).
The overall mean 30-minute incremental recovery was 1.66 IU/dL per IU/kg for patients’ baseline visit, 1.82 IU/dL per IU/kg for the end-of-study visit, and 1.74 IU/dL per IU/kg for both visits combined.
Incremental recovery was significantly lower in the 0-5 age group than the 6-11 age group:
- 1.45 vs 1.83 at baseline (P=0.027)
- 1.62 vs 1.99 at end of study (P=0.025)
- 1.53 vs 1.91 combined (P=0.001).
All patients had FX:C trough levels greater than 5% after visit 4 (days 29-42).
There were 28 AEs reported in 8 patients, but none of these events were considered related to treatment.
One patient did have 2 serious treatment-emergent AEs—lower respiratory tract infection and influenza.
There were no other serious AEs, no evidence of factor X inhibitor development, and no deaths.
Long-term maintenance deemed feasible in PV
MADRID—Long-term maintenance with ropeginterferon alfa-2b is feasible, effective, and well-tolerated in patients with polycythemia vera (PV), according to researchers.
In the ongoing phase 1/2 PEGINVERA study, patients have received ropeginterferon alfa-2b for a median of 4 years.
After the first 2 years, patients switched from bi-weekly dosing to receiving ropeginterferon alfa-2b once every 4 weeks.
None of the patients discontinued treatment after the switch, and many were able to maintain their best response.
Most adverse events (AEs) were mild, although there were several severe treatment-related AEs.
These results were presented in a poster (abstract P707) at the 22nd Congress of the European Hematology Association (EHA). The research was funded by AOP Orphan Pharmaceuticals AG.
The trial enrolled 51 patients, but the researchers reported results in the 29 patients who had completed 2 years of treatment and switched from bi-weekly dosing to receiving treatment once every 4 weeks.
All 29 patients remained on the 4-week schedule with a median observation period of roughly 2 years. The median monthly dose was 308 μg before the switch and 165 μg after.
At study entry, the patients’ median age was 58 (range, 40-80), and 76% were male. Their median spleen length was 12.8 cm (range, 8.0-22.0), and 34% of patients had prior treatment with hydroxyurea.
Patients’ median hematocrit was 45.40% (range, 36.9-53.8), their median platelet count was 431 G/L (range, 225-1016), their median leukocyte count was 11.1 G/L (range, 4.7-30.9), and their median JAKV617F allelic burden was 78% (range, 2-91.5).
Results
More than 80% of patients achieved a hematologic response, with more than 50% achieving a complete hematologic response. The same percentage of patients maintained their best hematologic response before and 6 months after switching to the 4-week schedule—51.7%.
More than 80% of patients achieved a molecular response, with nearly 20% achieving a complete molecular response. The percentage of patients maintaining their best molecular response was 62.1% before switching to the 4-week schedule and 58.6% 6 months after the switch.
The researchers said changes in hematocrit, platelet count, leukocyte count, and spleen size after the switch were “minimal and without clinical relevance.”
The median hematocrit changed from 42.3% to 42.6%, the median platelet count changed from 201.0 x 109/L to 211.9 x 109/L, the median leukocyte count changed from 5.0 x 109/L to 5.6 x 109/L, and the median spleen size changed from 12.8 cm to 12.4 cm.
The need for phlebotomy did not change, with 24.1% of patients requiring phlebotomy both before and 6 months after the switch.
The researchers also noted that ropeginterferon alfa-2b decreased mutant JAK2 allele burden in all of the patients over time, with the strongest effect observed in the second year of treatment.
After 2 years, most patients had a burden below 10%, and this was not affected by the change in dosing.
There were no cases of progression to myelofibrosis or leukemic transformation.
Seventy-one percent of AEs were mild, and 40.4% were considered likely related to ropeginterferon alfa-2b. The most frequent treatment-related AEs were arthralgia (29.4%) and fatigue (21.6%).
There were 34 severe AEs, 11 of which were related to ropeginterferon alfa-2b.
MADRID—Long-term maintenance with ropeginterferon alfa-2b is feasible, effective, and well-tolerated in patients with polycythemia vera (PV), according to researchers.
In the ongoing phase 1/2 PEGINVERA study, patients have received ropeginterferon alfa-2b for a median of 4 years.
After the first 2 years, patients switched from bi-weekly dosing to receiving ropeginterferon alfa-2b once every 4 weeks.
None of the patients discontinued treatment after the switch, and many were able to maintain their best response.
Most adverse events (AEs) were mild, although there were several severe treatment-related AEs.
These results were presented in a poster (abstract P707) at the 22nd Congress of the European Hematology Association (EHA). The research was funded by AOP Orphan Pharmaceuticals AG.
The trial enrolled 51 patients, but the researchers reported results in the 29 patients who had completed 2 years of treatment and switched from bi-weekly dosing to receiving treatment once every 4 weeks.
All 29 patients remained on the 4-week schedule with a median observation period of roughly 2 years. The median monthly dose was 308 μg before the switch and 165 μg after.
At study entry, the patients’ median age was 58 (range, 40-80), and 76% were male. Their median spleen length was 12.8 cm (range, 8.0-22.0), and 34% of patients had prior treatment with hydroxyurea.
Patients’ median hematocrit was 45.40% (range, 36.9-53.8), their median platelet count was 431 G/L (range, 225-1016), their median leukocyte count was 11.1 G/L (range, 4.7-30.9), and their median JAKV617F allelic burden was 78% (range, 2-91.5).
Results
More than 80% of patients achieved a hematologic response, with more than 50% achieving a complete hematologic response. The same percentage of patients maintained their best hematologic response before and 6 months after switching to the 4-week schedule—51.7%.
More than 80% of patients achieved a molecular response, with nearly 20% achieving a complete molecular response. The percentage of patients maintaining their best molecular response was 62.1% before switching to the 4-week schedule and 58.6% 6 months after the switch.
The researchers said changes in hematocrit, platelet count, leukocyte count, and spleen size after the switch were “minimal and without clinical relevance.”
The median hematocrit changed from 42.3% to 42.6%, the median platelet count changed from 201.0 x 109/L to 211.9 x 109/L, the median leukocyte count changed from 5.0 x 109/L to 5.6 x 109/L, and the median spleen size changed from 12.8 cm to 12.4 cm.
The need for phlebotomy did not change, with 24.1% of patients requiring phlebotomy both before and 6 months after the switch.
The researchers also noted that ropeginterferon alfa-2b decreased mutant JAK2 allele burden in all of the patients over time, with the strongest effect observed in the second year of treatment.
After 2 years, most patients had a burden below 10%, and this was not affected by the change in dosing.
There were no cases of progression to myelofibrosis or leukemic transformation.
Seventy-one percent of AEs were mild, and 40.4% were considered likely related to ropeginterferon alfa-2b. The most frequent treatment-related AEs were arthralgia (29.4%) and fatigue (21.6%).
There were 34 severe AEs, 11 of which were related to ropeginterferon alfa-2b.
MADRID—Long-term maintenance with ropeginterferon alfa-2b is feasible, effective, and well-tolerated in patients with polycythemia vera (PV), according to researchers.
In the ongoing phase 1/2 PEGINVERA study, patients have received ropeginterferon alfa-2b for a median of 4 years.
After the first 2 years, patients switched from bi-weekly dosing to receiving ropeginterferon alfa-2b once every 4 weeks.
None of the patients discontinued treatment after the switch, and many were able to maintain their best response.
Most adverse events (AEs) were mild, although there were several severe treatment-related AEs.
These results were presented in a poster (abstract P707) at the 22nd Congress of the European Hematology Association (EHA). The research was funded by AOP Orphan Pharmaceuticals AG.
The trial enrolled 51 patients, but the researchers reported results in the 29 patients who had completed 2 years of treatment and switched from bi-weekly dosing to receiving treatment once every 4 weeks.
All 29 patients remained on the 4-week schedule with a median observation period of roughly 2 years. The median monthly dose was 308 μg before the switch and 165 μg after.
At study entry, the patients’ median age was 58 (range, 40-80), and 76% were male. Their median spleen length was 12.8 cm (range, 8.0-22.0), and 34% of patients had prior treatment with hydroxyurea.
Patients’ median hematocrit was 45.40% (range, 36.9-53.8), their median platelet count was 431 G/L (range, 225-1016), their median leukocyte count was 11.1 G/L (range, 4.7-30.9), and their median JAKV617F allelic burden was 78% (range, 2-91.5).
Results
More than 80% of patients achieved a hematologic response, with more than 50% achieving a complete hematologic response. The same percentage of patients maintained their best hematologic response before and 6 months after switching to the 4-week schedule—51.7%.
More than 80% of patients achieved a molecular response, with nearly 20% achieving a complete molecular response. The percentage of patients maintaining their best molecular response was 62.1% before switching to the 4-week schedule and 58.6% 6 months after the switch.
The researchers said changes in hematocrit, platelet count, leukocyte count, and spleen size after the switch were “minimal and without clinical relevance.”
The median hematocrit changed from 42.3% to 42.6%, the median platelet count changed from 201.0 x 109/L to 211.9 x 109/L, the median leukocyte count changed from 5.0 x 109/L to 5.6 x 109/L, and the median spleen size changed from 12.8 cm to 12.4 cm.
The need for phlebotomy did not change, with 24.1% of patients requiring phlebotomy both before and 6 months after the switch.
The researchers also noted that ropeginterferon alfa-2b decreased mutant JAK2 allele burden in all of the patients over time, with the strongest effect observed in the second year of treatment.
After 2 years, most patients had a burden below 10%, and this was not affected by the change in dosing.
There were no cases of progression to myelofibrosis or leukemic transformation.
Seventy-one percent of AEs were mild, and 40.4% were considered likely related to ropeginterferon alfa-2b. The most frequent treatment-related AEs were arthralgia (29.4%) and fatigue (21.6%).
There were 34 severe AEs, 11 of which were related to ropeginterferon alfa-2b.