User login
A Talking Map for Family Meetings in the Intensive Care Unit
From the Department of Neurology, Duke University Medical Center, Durham, NC (Dr. McFarlin), the Department of Psychosocial Oncology and Palliative Care, Dana-Farber Cancer Institute, Boston, MA (Dr. Tulsky), Harborview Medical Center, University of Washington, Seattle, WA (Dr. Back), and Department of Medicine, University of Pittsburgh, Pittsburgh, PA (Dr. Arnold).
Abstract
- Objective: To describe the use of a cognitive map for navigating family meetings with surrogate decision makers of patients in an intensive care unit.
- Methods: Descriptive report and discussion using an illustrative case to outline the steps in the cognitive map.
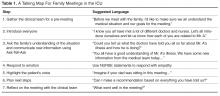
- Results: The use of cognitive maps has improved the ability of physicians to efficiently perform a specific communication skill. During a “goals of care” conversation, the cognitive map follows these steps: (1) Gather the clinical team for a pre-meeting, (2) Introduce everyone, (3) Use the “ask-tell-ask” strategy to communicate information, (4) Respond to emotion, (5) Highlight the patient’s voice, (6) Plan next steps, (7) Reflect on the meeting with the team. Providing this map of key communication skills will help faculty teach learners the core components of a family meeting.
- Conclusion: Practicing the behaviors demonstrated in the cognitive map may increase clinician skill during difficult conversations. Improving communication with surrogate decision makers will increase the support we offer to critically ill patients and their loved ones.
Key words: intensive care unit; communication; family meeting; critical illness; decision making; end of life care.
Family members of patients in the ICU value high-quality communication with the medical team. In fact, family members report that physicians’ communication skills are often more important than their medical skills [1]. Multiple professional societies, including the American Thoracic Society and the Society of Critical Care Medicine, define communication with families as a key component of high-quality critical care. Effective physician-patient communication improves measureable outcomes including decreased ICU length of stay [2] and may reduce distress amongst patients’ families [3]. The American College of Chest Physicians position statement on Palliative and End-of-Life Care for Patients with Cardiopulmonary Diseases urges physicians to develop curricula that incorporate interpersonal communication skills into training [4].
Unfortunately, such high-quality communication is not the norm. Surrogate decision makers are often displeased with the frequency of communication, the limited availability of attending physicians, and report feeling excluded from discussions [5]. When family meetings do occur, surrogate decision makers report inadequate understanding of diagnosis, prognosis, and treatment plans [6].
Physicians also find family meetings difficult. Intensivists worry that high-quality family meetings are time consuming and difficult to do in a busy ICU [7]. Critical care fellows report not feeling adequately trained to conduct family meetings [8]. It makes sense that untrained clinicians would want to avoid a conversation that is emotionally charged, particularly if one is unsure how to respond effectively.
The Case of Mr. A
Thomas A. is a 79-year-old man admitted to the medical intensive care unit 7 days earlier with a large left middle cerebral artery territory infarction. Given his decreased mental status, on admission he was intubated for airway protection. He is awake but aphasic and unable to follow any commands or move his right side. The neurology consultants do not feel this will improve. He has significant secretions and episodes of hypoxia. He has also developed acute on chronic kidney injury and may need to start dialysis. The social worker explains that his need for dialysis limits his placement options and that he will not be able to be discharged to home. Given his lack of improvement the team is concerned he will need a tracheostomy and feeding tube placed in order to safely continue this level of care. A family meeting is arranged to understand Mr. A’s goals of care.
Talking Map Basics
Before each step is discussed in detail, some definitions are needed. “Family” can be defined as anyone important enough, biologically related or not, to be present at a conversation with a clinician [10]. Second, a “family meeting” is a planned event between the family and interdisciplinary members of the ICU team as well as any other health care providers who have been involved in the patient’s care. The meeting takes place in a private space and at a time that is scheduled with the families’ needs in mind. Thus it is different from having families present on rounds or one-off meetings with particular clinicians.
Goals of care meetings are typically held when, in the clinicians’ view, the current treatments are not achieving the previously stated goals. Thus, the meeting has 2 purposes: first, to give the family the bad news that the current plan is not working and second, to develop a new plan based on the patient’s values. The family’s job, as surrogate decision maker, is to provide information about what would be most important to the patient. The clinician’s job is to suggest treatment plans that have the best probability of matching the patient’s values.
Not all of these tasks need be done at once. Some families will not be able to move from hearing bad news to making a decision without having time to first reflect and grieve. Others will need to confer with other family members privately before deciding on a plan. In many cases, a time-limited trial may be the right option with a plan for subsequent meetings. Given this, we recommend checking in with the family between each step to ensure that they feel safe moving ahead. For example, one might ask “Is it OK if we talk about what happens next?”
Talking Map Steps in Detail
1. Gather the Clinical Team for a Pre-Meeting
ICU care involves a large interdisciplinary care team. A “meeting before the meeting” with the entire clinical team is an opportunity to reach consensus on prognosis and therapeutic options, share prior interactions with family, and determine goals for the family meeting. It is also helpful to clarify team members’ roles at the meeting and to choose a primary facilitator. All of this helps to ensure that the family receives a consistent message during the meeting. The pre-meeting is also an opportunity to ask a team member to observe the communication skills of the facilitator and be prepared to give feedback after the meeting.
At this time, the team should also create the proper environment for the family meeting. This includes a quiet room free of interruptions with ample seating, available tissues, and transferred pagers and cell phones.
The intensivist and bedside nurse should always be present at the family meeting, and it is best when the same attending can be at subsequent family meetings Their consistent dual presence provides the uniform communication from the team, can reduce anxiety in family members and the collaboration reduces ICU nurse and physician burnout [11]. For illnesses that involve a specific disease or organ system, it is important to have the specialist at the meeting who can provide the appropriate expertise.
The Pre-Meeting
A family meeting was scheduled in the family meeting room for 3 pm, after morning rounds. Thirty minutes prior to the meeting the medical team, including the MICU intensivist, the bedside nurse, the neurology attending who has been involved in the care, the case manager and 2 residents sat to discuss Mr. A’s care. The neurology team confirmed that this stroke was considered very large and would result in a level of disability that could only be cared for in a nursing home and would require both a tracheostomy and feeding tube for safe care. The bedside nurse relayed that the family had asked if Mr. A. would ever recover enough to get back to his home. The neurology team shared they did not expect much improvement at all. Given the worsening renal failure and need for dialysis the case manager reminded the team that Mr. A’s nursing home placements were limited. The team decided that the intensivist would lead the meeting as she had updated various family members on rounds for the past 4 days and would be on service for another week. The team decided that their goal for the meeting was to make sure the family understands that Mr. A’s several medical illnesses portend a poor prognosis. They recognized this may be breaking bad news to the family. They also wanted to better understand what Mr. A would have thought given this situation. The residents were asked to watch for the family’s responses when the team delivered the news.
2. Introduce Everyone
Each meeting should start with formal introductions. Even if most providers know most family members it is a polite way to start the meeting. Introducing each family member present and how they know the patient provides insight into how the family is constructed and makes decisions. For example, the entire family may defer to the daughter who introduces herself as a nurse. In other situations, although there is one legal decision maker, the family may explain that they make decisions by consensus.
Each member of the treating team should also introduce themselves. Even if the clinician has been working with the family, it is polite to be formal and give your name and role. Given the number of people the family sees every day, one should not assume that the family remembers all of the clinicians.
In teaching hospitals, providers should also help the family understand their level of training. Surrogates do not always understand the different roles or level of training between students, residents and fellows, advanced practice providers, consultants and their attending physicians. Uncertainty about the roles can lead to family members feeling as though they are receiving contradictory information. Family satisfaction decreases when multiple attending physicians are involved in a patient’s care [12]. When possible, a consistent presence among providers at family meetings is always best.
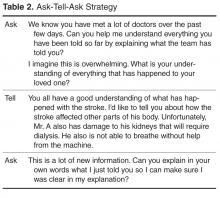
3. Ask the Family's Understanding of the Situation (Ask-Tell-Ask)
Asking the family to explain the situation in their own language reveals how well they understand the medical facts and helps the medical team determine what information will be most helpful to the family. An opening statement might be “We have all seen your dad and talked to many of his providers. It would help us all be on the same page if you can you tell me what the doctors are telling you?” Starting with the family’s understanding builds trust with the medical team as it creates an opportunity for the family to lead the meeting and indicates that the team is available to listen to their concerns. Asking surrogates for their understanding allows them to tell their story and not hear a reiteration of things they already know. Providing time for the family to share their perspective of the care elicits family’s concerns.
In a large meeting, ensure that all members of the family have an opportunity to communicate their concerns. Does a particular person do all of the talking? Are there individuals that do not speak at all? One way to further understand unspoken concerns during the meeting is to ask “I notice you have been quiet, what questions do you have that I can answer?” There may be several rounds of “asking” in order to ensure all the family members’ concerns are heard. Letting the family tell what they have heard helps the clinicians get a better idea of their health literacy. Do they explain information using technical data or jargon? Finally, as the family talks the clinicians can determine how surprising the “serious news” will be to them. For example, if the family says they know their dad is doing much worse and may die, the information to be delivered can be truncated. However if family incorrectly thinks their dad is doing better or is uncertain they will be much more surprised by the serious news.
After providing time for the family to express their understanding, tell them the information the team needs to communicate. When delivering serious news it is important to focus on the key 1 to 2 points you want the family to take away from the meeting. Typically when health care professionals talk to each other, they talk about every medical detail. Families find this amount of information overwhelming and are not sure what is most important, asking “So what does that mean?” Focusing on the “headline” helps the family focus on what you think the most important piece of information is. Studies suggest that what families most want to know is what the information means for the patient’s future and what treatments are possible. After delivering the new information, stop to allow the family space to think about what you said. If you are giving serious news, you will know they have heard what you said as they will get emotional (see next step).
Checking for understanding is the final “ask” in Ask-Tell-Ask. Begin by asking “What questions do you have?” Data in primary care has shown that patients are more likely to ask questions if you ask “what questions do you have” rather than “do you have any questions?” It is important to continue to ask this question until the family has asked all their questions. Often the family’s tough questions do not come until they get more comfortable and confident in the health care team. In cases where one family member is dominant it might also help to say “What questions do others have?” Next, using techniques like the “teach back” model the physician should check in to see what the family is taking away from the conversation. If a family understands, they can “teach back” the information accurately. This “ask” can be done in a way that does not make the family feel they are being tested: “I am not always clear when I communicate. Do you mind telling me back in your own words what you thought I said so I know we are on the same page?” This also provides an opportunity to answer any new questions that arise. Hearing the information directly from the family can allow the team to clarify any misconceptions and give insight into any emotional responses that the family might have.
4. Respond to Emotion
Discussing serious news in the ICU setting naturally leads to an emotional reaction. The clinician’s ability to notice emotional cues and respond with empathy is a key communication skill in family meetings [13]. Emotional reactions impede individual’s ability to process cognitive information and make it hard to think cognitively about what should be done next.
Physicians miss opportunities to respond to emotion in family meetings [14]. Missed opportunities lead to decreased family satisfaction and may lead to treatment decisions not consistent with the wishes of their loved ones. Empathic responses improve the family-clinician relationship and helps build trust and rapport [15]. Well- placed empathic statements may help surrogates disclose concerns that help the physician better understand the goals and values of the family and patient. Families also can more fully process cognitive information when their emotional responses have been attended to.
Physicians can develop the capacity to recognize and respond to the emotional cues family members are delivering. Intensivists should actively look for the emotions, the empathic opportunity, that are displayed by the family. This emotion is the “data” that will help lead to an empathic response. A family that just received bad news typically responds by showing emotion. Clues that emotions are present include: the family asking the same questions multiple times; using emotional words such as “sad” or “frustrated;” existential questions that do not have a cognitive answer such as “Why did God let this happen?;” or non-verbal cues like tears and hand wringing.
Sometimes the emotional responses are more difficult to recognize. Families may continue to ask for more cognitive information after hearing bad news. Someone keeps asking “Why did his kidney function worsen?” or “I thought the team said the chest x-ray looked better.” It is tempting to start answering these questions with more medical facts. However, if the question comes after bad news, it is usually an expression of frustration or sadness rather than a request for more information. Rather than giving information, it might help to acknowledge this by saying “I imagine this new is overwhelming.”
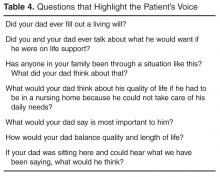
5. Highlight the Patient’s Voice
Family meetings are often used to develop new treatment plans (given that the old plans are not working). In these situations, it is essential to understand what the incapacitated patient would say if they were part of the family meeting. The surrogate’s primary role is to represent the patient’s voice. To do this, surrogates need assistance in applying their critically ill loved one’s thoughts and values to complex, possibly life limiting, situations. Surrogate decision makers struggle with the decisions’ emotional impact, as well as how to reconcile their desires with their loved one’s wishes [18]. This can lead them to make decisions that conflict with the loved one’s values [19] as well as emotional sequelae such as PTSD and depression [20].
As families reflect on their loved one’s values, conflicting desires will arise. For example, someone may have wanted to live as long as possible and also values independence. Or someone may value their ability to think clearly more than being physically well but would not want to be physically dependent on artificial life support. Exploring which values would be more important can help resolve these conflicts.
Clinicians should check for understanding while family members are identifying the values of their loved ones. Providing the family with a summary of what you have heard will help ensure a more accurate understanding of these crucial issues. A summary statement might be, “It sounds like you are saying your dad really valued his independence. He enjoyed being able to take care of his loved ones and himself. Is that right?”
6. Plan Next Steps
The family meeting serves to attend to family emotion and allow space to elicit patients’ values. Following a family meeting surrogate decision makers may be able to begin to consider the next steps in their loved one’s care. If bad news was delivered they may need space to adjust to a different future than they expected. Using an empathic statement of support “We will continue to make sure we communicate with you as we work together to plan next steps” will reassure a family that they have time and space to plan for the future.
Families vary regarding how much physician input they desire in planning next steps [21]. You can explicitly ask how the team can best help the family with decisions: “Some families like to hear the options for next steps from the team and make a decision, other families like to hear a recommendation from the team. What would be the most helpful for you?” Throughout the course of an illness a surrogate’s preference for decision making may change and clinicians should be responsive to those changing needs.
If the surrogate wants a clinician’s recommendation, 3 points are worth stressing. First, the recommendation should be personalized to this patient and his values. The goal is to reveal how the understanding of the patient’s values led to the treatment plan offered. Second, the recommendation should focus primarily on what will be done to achieve the patient’s values. Focusing on what the clinicians will do may help the family feel that the clinicians are still “trying” and not abandoning their loved one. In this case, the team will continue medical care that will help the patient regain/maintain independence. Only after talking about what will be done should the clinician point out that certain interventions will not achieve the patient’s goals and thus will not be done:
“It sounds like your father really valued his independence and that this illness has really taken that away. Knowing this, would it be helpful for me to make a recommendation for next steps?” “I think we should continue providing excellent medical care for your father in hopes he can get better and go home. One the other hand, if he gets worse, we should not use therapies such as CPR or dialysis that are unlikely to help him regain his independence.”
Finally, be concrete when planning next steps. If a time-limited trial of a therapy is proposed, make sure the family understands what a successful and unsuccessful trial will look like. Make plans to meet again on a specific date in order to ensure the family understands the progress being made. If a transition to comfort care is agreed upon, ensure support of the entire family during the next hours to days and offer services such as chaplaincy or child life specialists.
A family may not agree with the recommendation and back and forth discussion can help create a plan that is in line with their understanding of the illness. Rather than convincing, a clinician should keep an open mind about why they and the surrogate disagree. Do they have different views about the patient’s future? Did the medical team misunderstand the patient’s values? Are there emotional factors that inhibit the surrogate’s ability to attend to the discussion? It is only by learning where the disagreement is that a clinician can move the conversation forward.
A surrogate may ask about a therapy that is not beneficial or may increase distress to the patient. The use of “I wish” or “I worry” statements can be helpful at these points. These specific phrases recognize the surrogate’s desire to do more but also imply that the therapies are not helpful.
“I wish that his ability to communicate and tell you what he wants would get better with a little more time as well.”
“I worry that waiting 2 more weeks for improvement will actually cause complications to occur.”
7. Reflect
Family meetings have an impact on both the family and the medical team. Following the meeting, a short debriefing with the clinical team can be helpful. Summarizing the events of the meeting ensures clarity about the treatment plan going forward. It provides team members a chance to discuss conflicts that may have arisen. It allows the participants in the meeting to reflect on what communication skills they used and how they can improve their skills going forward.
Conclusion
Family meetings with surrogate decision makers must navigate multiple agendas of the family and providers. The goal of excellent communication with surrogates in an ICU should be to understand the patient’s goals and values and seek to make treatment plans that align with their perspective. This talking map provides a conceptual framework for physicians to guide a family through these conversations. The framework creates an opportunity to focus on the patient’s values and preferences for care while allowing space to attend to emotional responses to reduce the distress inherent in surrogate decision-making. Practicing the behaviors demonstrated in the talking map may increase clinician skill during difficult conversations. Improving communication with surrogate decision makers will increase the support we offer to critically ill patients and their loved ones.
Corresponding author: Jessica McFarlin, MD, jessmcfarlin@gmail.com.
Funding/support: Dr. Arnold receives support though the Leo H. Criep Chair in Patient Care.
Financial disclosures: None.
1. Hickey M. What are the needs of families of critically ill patients? A review of the literature since 1976. Heart Lung 1990;19:401–15.
2. Mosenthal AC, Murphy PA, Barker LK, et al. Changing culture around end-of-life care in the trauma intensive care unit. J Trauma 2008;64:1587–93.
3. Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 2007;356:469–78.
4. Selecky PA, Eliasson AH, Hall RI, et al. Palliative and end-of-life care for patients with cardiopulmonary diseases. Chest 2005;128:3599–610.
5. Henrich NJ, Dodek P, Heyland D, et al. Qualitative analysis of an intensive care unit family satisfaction survey. Crit Care Med 2011;39:1000–5.
6. Azoulet E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med 2000;28:3044–9.
7. Curtis JR. Communicating about end-of-life care with patients and families in the intensive care unit. Crit Care Clin 2004;20:363–80.
8. Hope AA, Hsieh SJ, Howes JM, et al. Let’s talk critical. Development and evaluation of a communication skills training program for critical care fellows. Ann Am Thorac Soc 2015;12:505–11.
9. Back AL, Arnold RM, Baile WF, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 2007;167:453–60.
10. Vital Talk. Conduct a family conference. Accessed 27 June 2016 at www.vitaltalk.org/clinicians/family.
11. Kramer M, Schmalenberg C. Securing “good” nurse/physician relationships. Nurs Manage 2003;34:34–8.
12. Johnson D, Wilson M, Cavanaugh B, et al. Measuring the ability to meet family needs in an intensive care unit. Crit Care Med 1998;26:266–71.
13. Back AL, Arnold RM. “Isn’t there anything more you can do?’’: when empathic statements work, and when they don’t. J Palliat Med 2013;16:1429–32.
14. Curtis JR, Engelberg RA, Wenrich MD. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med 2005;171:844–9.
15. Pollak KI, Arnold RM, Jeffreys AS, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol 2007;36:5748–52.
16. Back AL, Arnold RM, Tulsky JA. Mastering communication with seriously ill patients: balancing honesty with empathy and hope. Cambridge: Cambridge University Press; 2009.
17. Back AL, Arnold RM, Baile WF, et al. Approaching difficult communication tasks in oncology. CA Cancer J Clin 2005;55:164–77.
18. Schenker Y, White D, Crowley-Matoka M, et al. “It hurts to know…and it helps”: exploring how surrogates in the ICU cope with prognostic information. J Palliat Med 2013;16:243–9.
19. Scheunemann LP, Arnold RM, White DB. The facilitated values history: helping surrogates make authentic decisions for incapacitated patients with advanced illness. Am J Respir Crit Care Med 2012;186:480–6.
20. Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 2005;171:987–94.
21. White DB, Braddock CH, Bereknyei et al. Toward shared decision making at the end of life in intensive care units: opportunities for improvement. Arch Intern Med 2007;167:461–7.
From the Department of Neurology, Duke University Medical Center, Durham, NC (Dr. McFarlin), the Department of Psychosocial Oncology and Palliative Care, Dana-Farber Cancer Institute, Boston, MA (Dr. Tulsky), Harborview Medical Center, University of Washington, Seattle, WA (Dr. Back), and Department of Medicine, University of Pittsburgh, Pittsburgh, PA (Dr. Arnold).
Abstract
- Objective: To describe the use of a cognitive map for navigating family meetings with surrogate decision makers of patients in an intensive care unit.
- Methods: Descriptive report and discussion using an illustrative case to outline the steps in the cognitive map.
- Results: The use of cognitive maps has improved the ability of physicians to efficiently perform a specific communication skill. During a “goals of care” conversation, the cognitive map follows these steps: (1) Gather the clinical team for a pre-meeting, (2) Introduce everyone, (3) Use the “ask-tell-ask” strategy to communicate information, (4) Respond to emotion, (5) Highlight the patient’s voice, (6) Plan next steps, (7) Reflect on the meeting with the team. Providing this map of key communication skills will help faculty teach learners the core components of a family meeting.
- Conclusion: Practicing the behaviors demonstrated in the cognitive map may increase clinician skill during difficult conversations. Improving communication with surrogate decision makers will increase the support we offer to critically ill patients and their loved ones.
Key words: intensive care unit; communication; family meeting; critical illness; decision making; end of life care.
Family members of patients in the ICU value high-quality communication with the medical team. In fact, family members report that physicians’ communication skills are often more important than their medical skills [1]. Multiple professional societies, including the American Thoracic Society and the Society of Critical Care Medicine, define communication with families as a key component of high-quality critical care. Effective physician-patient communication improves measureable outcomes including decreased ICU length of stay [2] and may reduce distress amongst patients’ families [3]. The American College of Chest Physicians position statement on Palliative and End-of-Life Care for Patients with Cardiopulmonary Diseases urges physicians to develop curricula that incorporate interpersonal communication skills into training [4].
Unfortunately, such high-quality communication is not the norm. Surrogate decision makers are often displeased with the frequency of communication, the limited availability of attending physicians, and report feeling excluded from discussions [5]. When family meetings do occur, surrogate decision makers report inadequate understanding of diagnosis, prognosis, and treatment plans [6].
Physicians also find family meetings difficult. Intensivists worry that high-quality family meetings are time consuming and difficult to do in a busy ICU [7]. Critical care fellows report not feeling adequately trained to conduct family meetings [8]. It makes sense that untrained clinicians would want to avoid a conversation that is emotionally charged, particularly if one is unsure how to respond effectively.
The Case of Mr. A
Thomas A. is a 79-year-old man admitted to the medical intensive care unit 7 days earlier with a large left middle cerebral artery territory infarction. Given his decreased mental status, on admission he was intubated for airway protection. He is awake but aphasic and unable to follow any commands or move his right side. The neurology consultants do not feel this will improve. He has significant secretions and episodes of hypoxia. He has also developed acute on chronic kidney injury and may need to start dialysis. The social worker explains that his need for dialysis limits his placement options and that he will not be able to be discharged to home. Given his lack of improvement the team is concerned he will need a tracheostomy and feeding tube placed in order to safely continue this level of care. A family meeting is arranged to understand Mr. A’s goals of care.
Talking Map Basics
Before each step is discussed in detail, some definitions are needed. “Family” can be defined as anyone important enough, biologically related or not, to be present at a conversation with a clinician [10]. Second, a “family meeting” is a planned event between the family and interdisciplinary members of the ICU team as well as any other health care providers who have been involved in the patient’s care. The meeting takes place in a private space and at a time that is scheduled with the families’ needs in mind. Thus it is different from having families present on rounds or one-off meetings with particular clinicians.
Goals of care meetings are typically held when, in the clinicians’ view, the current treatments are not achieving the previously stated goals. Thus, the meeting has 2 purposes: first, to give the family the bad news that the current plan is not working and second, to develop a new plan based on the patient’s values. The family’s job, as surrogate decision maker, is to provide information about what would be most important to the patient. The clinician’s job is to suggest treatment plans that have the best probability of matching the patient’s values.
Not all of these tasks need be done at once. Some families will not be able to move from hearing bad news to making a decision without having time to first reflect and grieve. Others will need to confer with other family members privately before deciding on a plan. In many cases, a time-limited trial may be the right option with a plan for subsequent meetings. Given this, we recommend checking in with the family between each step to ensure that they feel safe moving ahead. For example, one might ask “Is it OK if we talk about what happens next?”
Talking Map Steps in Detail
1. Gather the Clinical Team for a Pre-Meeting
ICU care involves a large interdisciplinary care team. A “meeting before the meeting” with the entire clinical team is an opportunity to reach consensus on prognosis and therapeutic options, share prior interactions with family, and determine goals for the family meeting. It is also helpful to clarify team members’ roles at the meeting and to choose a primary facilitator. All of this helps to ensure that the family receives a consistent message during the meeting. The pre-meeting is also an opportunity to ask a team member to observe the communication skills of the facilitator and be prepared to give feedback after the meeting.
At this time, the team should also create the proper environment for the family meeting. This includes a quiet room free of interruptions with ample seating, available tissues, and transferred pagers and cell phones.
The intensivist and bedside nurse should always be present at the family meeting, and it is best when the same attending can be at subsequent family meetings Their consistent dual presence provides the uniform communication from the team, can reduce anxiety in family members and the collaboration reduces ICU nurse and physician burnout [11]. For illnesses that involve a specific disease or organ system, it is important to have the specialist at the meeting who can provide the appropriate expertise.
The Pre-Meeting
A family meeting was scheduled in the family meeting room for 3 pm, after morning rounds. Thirty minutes prior to the meeting the medical team, including the MICU intensivist, the bedside nurse, the neurology attending who has been involved in the care, the case manager and 2 residents sat to discuss Mr. A’s care. The neurology team confirmed that this stroke was considered very large and would result in a level of disability that could only be cared for in a nursing home and would require both a tracheostomy and feeding tube for safe care. The bedside nurse relayed that the family had asked if Mr. A. would ever recover enough to get back to his home. The neurology team shared they did not expect much improvement at all. Given the worsening renal failure and need for dialysis the case manager reminded the team that Mr. A’s nursing home placements were limited. The team decided that the intensivist would lead the meeting as she had updated various family members on rounds for the past 4 days and would be on service for another week. The team decided that their goal for the meeting was to make sure the family understands that Mr. A’s several medical illnesses portend a poor prognosis. They recognized this may be breaking bad news to the family. They also wanted to better understand what Mr. A would have thought given this situation. The residents were asked to watch for the family’s responses when the team delivered the news.
2. Introduce Everyone
Each meeting should start with formal introductions. Even if most providers know most family members it is a polite way to start the meeting. Introducing each family member present and how they know the patient provides insight into how the family is constructed and makes decisions. For example, the entire family may defer to the daughter who introduces herself as a nurse. In other situations, although there is one legal decision maker, the family may explain that they make decisions by consensus.
Each member of the treating team should also introduce themselves. Even if the clinician has been working with the family, it is polite to be formal and give your name and role. Given the number of people the family sees every day, one should not assume that the family remembers all of the clinicians.
In teaching hospitals, providers should also help the family understand their level of training. Surrogates do not always understand the different roles or level of training between students, residents and fellows, advanced practice providers, consultants and their attending physicians. Uncertainty about the roles can lead to family members feeling as though they are receiving contradictory information. Family satisfaction decreases when multiple attending physicians are involved in a patient’s care [12]. When possible, a consistent presence among providers at family meetings is always best.
3. Ask the Family's Understanding of the Situation (Ask-Tell-Ask)
Asking the family to explain the situation in their own language reveals how well they understand the medical facts and helps the medical team determine what information will be most helpful to the family. An opening statement might be “We have all seen your dad and talked to many of his providers. It would help us all be on the same page if you can you tell me what the doctors are telling you?” Starting with the family’s understanding builds trust with the medical team as it creates an opportunity for the family to lead the meeting and indicates that the team is available to listen to their concerns. Asking surrogates for their understanding allows them to tell their story and not hear a reiteration of things they already know. Providing time for the family to share their perspective of the care elicits family’s concerns.
In a large meeting, ensure that all members of the family have an opportunity to communicate their concerns. Does a particular person do all of the talking? Are there individuals that do not speak at all? One way to further understand unspoken concerns during the meeting is to ask “I notice you have been quiet, what questions do you have that I can answer?” There may be several rounds of “asking” in order to ensure all the family members’ concerns are heard. Letting the family tell what they have heard helps the clinicians get a better idea of their health literacy. Do they explain information using technical data or jargon? Finally, as the family talks the clinicians can determine how surprising the “serious news” will be to them. For example, if the family says they know their dad is doing much worse and may die, the information to be delivered can be truncated. However if family incorrectly thinks their dad is doing better or is uncertain they will be much more surprised by the serious news.
After providing time for the family to express their understanding, tell them the information the team needs to communicate. When delivering serious news it is important to focus on the key 1 to 2 points you want the family to take away from the meeting. Typically when health care professionals talk to each other, they talk about every medical detail. Families find this amount of information overwhelming and are not sure what is most important, asking “So what does that mean?” Focusing on the “headline” helps the family focus on what you think the most important piece of information is. Studies suggest that what families most want to know is what the information means for the patient’s future and what treatments are possible. After delivering the new information, stop to allow the family space to think about what you said. If you are giving serious news, you will know they have heard what you said as they will get emotional (see next step).
Checking for understanding is the final “ask” in Ask-Tell-Ask. Begin by asking “What questions do you have?” Data in primary care has shown that patients are more likely to ask questions if you ask “what questions do you have” rather than “do you have any questions?” It is important to continue to ask this question until the family has asked all their questions. Often the family’s tough questions do not come until they get more comfortable and confident in the health care team. In cases where one family member is dominant it might also help to say “What questions do others have?” Next, using techniques like the “teach back” model the physician should check in to see what the family is taking away from the conversation. If a family understands, they can “teach back” the information accurately. This “ask” can be done in a way that does not make the family feel they are being tested: “I am not always clear when I communicate. Do you mind telling me back in your own words what you thought I said so I know we are on the same page?” This also provides an opportunity to answer any new questions that arise. Hearing the information directly from the family can allow the team to clarify any misconceptions and give insight into any emotional responses that the family might have.
4. Respond to Emotion
Discussing serious news in the ICU setting naturally leads to an emotional reaction. The clinician’s ability to notice emotional cues and respond with empathy is a key communication skill in family meetings [13]. Emotional reactions impede individual’s ability to process cognitive information and make it hard to think cognitively about what should be done next.
Physicians miss opportunities to respond to emotion in family meetings [14]. Missed opportunities lead to decreased family satisfaction and may lead to treatment decisions not consistent with the wishes of their loved ones. Empathic responses improve the family-clinician relationship and helps build trust and rapport [15]. Well- placed empathic statements may help surrogates disclose concerns that help the physician better understand the goals and values of the family and patient. Families also can more fully process cognitive information when their emotional responses have been attended to.
Physicians can develop the capacity to recognize and respond to the emotional cues family members are delivering. Intensivists should actively look for the emotions, the empathic opportunity, that are displayed by the family. This emotion is the “data” that will help lead to an empathic response. A family that just received bad news typically responds by showing emotion. Clues that emotions are present include: the family asking the same questions multiple times; using emotional words such as “sad” or “frustrated;” existential questions that do not have a cognitive answer such as “Why did God let this happen?;” or non-verbal cues like tears and hand wringing.
Sometimes the emotional responses are more difficult to recognize. Families may continue to ask for more cognitive information after hearing bad news. Someone keeps asking “Why did his kidney function worsen?” or “I thought the team said the chest x-ray looked better.” It is tempting to start answering these questions with more medical facts. However, if the question comes after bad news, it is usually an expression of frustration or sadness rather than a request for more information. Rather than giving information, it might help to acknowledge this by saying “I imagine this new is overwhelming.”
5. Highlight the Patient’s Voice
Family meetings are often used to develop new treatment plans (given that the old plans are not working). In these situations, it is essential to understand what the incapacitated patient would say if they were part of the family meeting. The surrogate’s primary role is to represent the patient’s voice. To do this, surrogates need assistance in applying their critically ill loved one’s thoughts and values to complex, possibly life limiting, situations. Surrogate decision makers struggle with the decisions’ emotional impact, as well as how to reconcile their desires with their loved one’s wishes [18]. This can lead them to make decisions that conflict with the loved one’s values [19] as well as emotional sequelae such as PTSD and depression [20].
As families reflect on their loved one’s values, conflicting desires will arise. For example, someone may have wanted to live as long as possible and also values independence. Or someone may value their ability to think clearly more than being physically well but would not want to be physically dependent on artificial life support. Exploring which values would be more important can help resolve these conflicts.
Clinicians should check for understanding while family members are identifying the values of their loved ones. Providing the family with a summary of what you have heard will help ensure a more accurate understanding of these crucial issues. A summary statement might be, “It sounds like you are saying your dad really valued his independence. He enjoyed being able to take care of his loved ones and himself. Is that right?”
6. Plan Next Steps
The family meeting serves to attend to family emotion and allow space to elicit patients’ values. Following a family meeting surrogate decision makers may be able to begin to consider the next steps in their loved one’s care. If bad news was delivered they may need space to adjust to a different future than they expected. Using an empathic statement of support “We will continue to make sure we communicate with you as we work together to plan next steps” will reassure a family that they have time and space to plan for the future.
Families vary regarding how much physician input they desire in planning next steps [21]. You can explicitly ask how the team can best help the family with decisions: “Some families like to hear the options for next steps from the team and make a decision, other families like to hear a recommendation from the team. What would be the most helpful for you?” Throughout the course of an illness a surrogate’s preference for decision making may change and clinicians should be responsive to those changing needs.
If the surrogate wants a clinician’s recommendation, 3 points are worth stressing. First, the recommendation should be personalized to this patient and his values. The goal is to reveal how the understanding of the patient’s values led to the treatment plan offered. Second, the recommendation should focus primarily on what will be done to achieve the patient’s values. Focusing on what the clinicians will do may help the family feel that the clinicians are still “trying” and not abandoning their loved one. In this case, the team will continue medical care that will help the patient regain/maintain independence. Only after talking about what will be done should the clinician point out that certain interventions will not achieve the patient’s goals and thus will not be done:
“It sounds like your father really valued his independence and that this illness has really taken that away. Knowing this, would it be helpful for me to make a recommendation for next steps?” “I think we should continue providing excellent medical care for your father in hopes he can get better and go home. One the other hand, if he gets worse, we should not use therapies such as CPR or dialysis that are unlikely to help him regain his independence.”
Finally, be concrete when planning next steps. If a time-limited trial of a therapy is proposed, make sure the family understands what a successful and unsuccessful trial will look like. Make plans to meet again on a specific date in order to ensure the family understands the progress being made. If a transition to comfort care is agreed upon, ensure support of the entire family during the next hours to days and offer services such as chaplaincy or child life specialists.
A family may not agree with the recommendation and back and forth discussion can help create a plan that is in line with their understanding of the illness. Rather than convincing, a clinician should keep an open mind about why they and the surrogate disagree. Do they have different views about the patient’s future? Did the medical team misunderstand the patient’s values? Are there emotional factors that inhibit the surrogate’s ability to attend to the discussion? It is only by learning where the disagreement is that a clinician can move the conversation forward.
A surrogate may ask about a therapy that is not beneficial or may increase distress to the patient. The use of “I wish” or “I worry” statements can be helpful at these points. These specific phrases recognize the surrogate’s desire to do more but also imply that the therapies are not helpful.
“I wish that his ability to communicate and tell you what he wants would get better with a little more time as well.”
“I worry that waiting 2 more weeks for improvement will actually cause complications to occur.”
7. Reflect
Family meetings have an impact on both the family and the medical team. Following the meeting, a short debriefing with the clinical team can be helpful. Summarizing the events of the meeting ensures clarity about the treatment plan going forward. It provides team members a chance to discuss conflicts that may have arisen. It allows the participants in the meeting to reflect on what communication skills they used and how they can improve their skills going forward.
Conclusion
Family meetings with surrogate decision makers must navigate multiple agendas of the family and providers. The goal of excellent communication with surrogates in an ICU should be to understand the patient’s goals and values and seek to make treatment plans that align with their perspective. This talking map provides a conceptual framework for physicians to guide a family through these conversations. The framework creates an opportunity to focus on the patient’s values and preferences for care while allowing space to attend to emotional responses to reduce the distress inherent in surrogate decision-making. Practicing the behaviors demonstrated in the talking map may increase clinician skill during difficult conversations. Improving communication with surrogate decision makers will increase the support we offer to critically ill patients and their loved ones.
Corresponding author: Jessica McFarlin, MD, jessmcfarlin@gmail.com.
Funding/support: Dr. Arnold receives support though the Leo H. Criep Chair in Patient Care.
Financial disclosures: None.
From the Department of Neurology, Duke University Medical Center, Durham, NC (Dr. McFarlin), the Department of Psychosocial Oncology and Palliative Care, Dana-Farber Cancer Institute, Boston, MA (Dr. Tulsky), Harborview Medical Center, University of Washington, Seattle, WA (Dr. Back), and Department of Medicine, University of Pittsburgh, Pittsburgh, PA (Dr. Arnold).
Abstract
- Objective: To describe the use of a cognitive map for navigating family meetings with surrogate decision makers of patients in an intensive care unit.
- Methods: Descriptive report and discussion using an illustrative case to outline the steps in the cognitive map.
- Results: The use of cognitive maps has improved the ability of physicians to efficiently perform a specific communication skill. During a “goals of care” conversation, the cognitive map follows these steps: (1) Gather the clinical team for a pre-meeting, (2) Introduce everyone, (3) Use the “ask-tell-ask” strategy to communicate information, (4) Respond to emotion, (5) Highlight the patient’s voice, (6) Plan next steps, (7) Reflect on the meeting with the team. Providing this map of key communication skills will help faculty teach learners the core components of a family meeting.
- Conclusion: Practicing the behaviors demonstrated in the cognitive map may increase clinician skill during difficult conversations. Improving communication with surrogate decision makers will increase the support we offer to critically ill patients and their loved ones.
Key words: intensive care unit; communication; family meeting; critical illness; decision making; end of life care.
Family members of patients in the ICU value high-quality communication with the medical team. In fact, family members report that physicians’ communication skills are often more important than their medical skills [1]. Multiple professional societies, including the American Thoracic Society and the Society of Critical Care Medicine, define communication with families as a key component of high-quality critical care. Effective physician-patient communication improves measureable outcomes including decreased ICU length of stay [2] and may reduce distress amongst patients’ families [3]. The American College of Chest Physicians position statement on Palliative and End-of-Life Care for Patients with Cardiopulmonary Diseases urges physicians to develop curricula that incorporate interpersonal communication skills into training [4].
Unfortunately, such high-quality communication is not the norm. Surrogate decision makers are often displeased with the frequency of communication, the limited availability of attending physicians, and report feeling excluded from discussions [5]. When family meetings do occur, surrogate decision makers report inadequate understanding of diagnosis, prognosis, and treatment plans [6].
Physicians also find family meetings difficult. Intensivists worry that high-quality family meetings are time consuming and difficult to do in a busy ICU [7]. Critical care fellows report not feeling adequately trained to conduct family meetings [8]. It makes sense that untrained clinicians would want to avoid a conversation that is emotionally charged, particularly if one is unsure how to respond effectively.
The Case of Mr. A
Thomas A. is a 79-year-old man admitted to the medical intensive care unit 7 days earlier with a large left middle cerebral artery territory infarction. Given his decreased mental status, on admission he was intubated for airway protection. He is awake but aphasic and unable to follow any commands or move his right side. The neurology consultants do not feel this will improve. He has significant secretions and episodes of hypoxia. He has also developed acute on chronic kidney injury and may need to start dialysis. The social worker explains that his need for dialysis limits his placement options and that he will not be able to be discharged to home. Given his lack of improvement the team is concerned he will need a tracheostomy and feeding tube placed in order to safely continue this level of care. A family meeting is arranged to understand Mr. A’s goals of care.
Talking Map Basics
Before each step is discussed in detail, some definitions are needed. “Family” can be defined as anyone important enough, biologically related or not, to be present at a conversation with a clinician [10]. Second, a “family meeting” is a planned event between the family and interdisciplinary members of the ICU team as well as any other health care providers who have been involved in the patient’s care. The meeting takes place in a private space and at a time that is scheduled with the families’ needs in mind. Thus it is different from having families present on rounds or one-off meetings with particular clinicians.
Goals of care meetings are typically held when, in the clinicians’ view, the current treatments are not achieving the previously stated goals. Thus, the meeting has 2 purposes: first, to give the family the bad news that the current plan is not working and second, to develop a new plan based on the patient’s values. The family’s job, as surrogate decision maker, is to provide information about what would be most important to the patient. The clinician’s job is to suggest treatment plans that have the best probability of matching the patient’s values.
Not all of these tasks need be done at once. Some families will not be able to move from hearing bad news to making a decision without having time to first reflect and grieve. Others will need to confer with other family members privately before deciding on a plan. In many cases, a time-limited trial may be the right option with a plan for subsequent meetings. Given this, we recommend checking in with the family between each step to ensure that they feel safe moving ahead. For example, one might ask “Is it OK if we talk about what happens next?”
Talking Map Steps in Detail
1. Gather the Clinical Team for a Pre-Meeting
ICU care involves a large interdisciplinary care team. A “meeting before the meeting” with the entire clinical team is an opportunity to reach consensus on prognosis and therapeutic options, share prior interactions with family, and determine goals for the family meeting. It is also helpful to clarify team members’ roles at the meeting and to choose a primary facilitator. All of this helps to ensure that the family receives a consistent message during the meeting. The pre-meeting is also an opportunity to ask a team member to observe the communication skills of the facilitator and be prepared to give feedback after the meeting.
At this time, the team should also create the proper environment for the family meeting. This includes a quiet room free of interruptions with ample seating, available tissues, and transferred pagers and cell phones.
The intensivist and bedside nurse should always be present at the family meeting, and it is best when the same attending can be at subsequent family meetings Their consistent dual presence provides the uniform communication from the team, can reduce anxiety in family members and the collaboration reduces ICU nurse and physician burnout [11]. For illnesses that involve a specific disease or organ system, it is important to have the specialist at the meeting who can provide the appropriate expertise.
The Pre-Meeting
A family meeting was scheduled in the family meeting room for 3 pm, after morning rounds. Thirty minutes prior to the meeting the medical team, including the MICU intensivist, the bedside nurse, the neurology attending who has been involved in the care, the case manager and 2 residents sat to discuss Mr. A’s care. The neurology team confirmed that this stroke was considered very large and would result in a level of disability that could only be cared for in a nursing home and would require both a tracheostomy and feeding tube for safe care. The bedside nurse relayed that the family had asked if Mr. A. would ever recover enough to get back to his home. The neurology team shared they did not expect much improvement at all. Given the worsening renal failure and need for dialysis the case manager reminded the team that Mr. A’s nursing home placements were limited. The team decided that the intensivist would lead the meeting as she had updated various family members on rounds for the past 4 days and would be on service for another week. The team decided that their goal for the meeting was to make sure the family understands that Mr. A’s several medical illnesses portend a poor prognosis. They recognized this may be breaking bad news to the family. They also wanted to better understand what Mr. A would have thought given this situation. The residents were asked to watch for the family’s responses when the team delivered the news.
2. Introduce Everyone
Each meeting should start with formal introductions. Even if most providers know most family members it is a polite way to start the meeting. Introducing each family member present and how they know the patient provides insight into how the family is constructed and makes decisions. For example, the entire family may defer to the daughter who introduces herself as a nurse. In other situations, although there is one legal decision maker, the family may explain that they make decisions by consensus.
Each member of the treating team should also introduce themselves. Even if the clinician has been working with the family, it is polite to be formal and give your name and role. Given the number of people the family sees every day, one should not assume that the family remembers all of the clinicians.
In teaching hospitals, providers should also help the family understand their level of training. Surrogates do not always understand the different roles or level of training between students, residents and fellows, advanced practice providers, consultants and their attending physicians. Uncertainty about the roles can lead to family members feeling as though they are receiving contradictory information. Family satisfaction decreases when multiple attending physicians are involved in a patient’s care [12]. When possible, a consistent presence among providers at family meetings is always best.
3. Ask the Family's Understanding of the Situation (Ask-Tell-Ask)
Asking the family to explain the situation in their own language reveals how well they understand the medical facts and helps the medical team determine what information will be most helpful to the family. An opening statement might be “We have all seen your dad and talked to many of his providers. It would help us all be on the same page if you can you tell me what the doctors are telling you?” Starting with the family’s understanding builds trust with the medical team as it creates an opportunity for the family to lead the meeting and indicates that the team is available to listen to their concerns. Asking surrogates for their understanding allows them to tell their story and not hear a reiteration of things they already know. Providing time for the family to share their perspective of the care elicits family’s concerns.
In a large meeting, ensure that all members of the family have an opportunity to communicate their concerns. Does a particular person do all of the talking? Are there individuals that do not speak at all? One way to further understand unspoken concerns during the meeting is to ask “I notice you have been quiet, what questions do you have that I can answer?” There may be several rounds of “asking” in order to ensure all the family members’ concerns are heard. Letting the family tell what they have heard helps the clinicians get a better idea of their health literacy. Do they explain information using technical data or jargon? Finally, as the family talks the clinicians can determine how surprising the “serious news” will be to them. For example, if the family says they know their dad is doing much worse and may die, the information to be delivered can be truncated. However if family incorrectly thinks their dad is doing better or is uncertain they will be much more surprised by the serious news.
After providing time for the family to express their understanding, tell them the information the team needs to communicate. When delivering serious news it is important to focus on the key 1 to 2 points you want the family to take away from the meeting. Typically when health care professionals talk to each other, they talk about every medical detail. Families find this amount of information overwhelming and are not sure what is most important, asking “So what does that mean?” Focusing on the “headline” helps the family focus on what you think the most important piece of information is. Studies suggest that what families most want to know is what the information means for the patient’s future and what treatments are possible. After delivering the new information, stop to allow the family space to think about what you said. If you are giving serious news, you will know they have heard what you said as they will get emotional (see next step).
Checking for understanding is the final “ask” in Ask-Tell-Ask. Begin by asking “What questions do you have?” Data in primary care has shown that patients are more likely to ask questions if you ask “what questions do you have” rather than “do you have any questions?” It is important to continue to ask this question until the family has asked all their questions. Often the family’s tough questions do not come until they get more comfortable and confident in the health care team. In cases where one family member is dominant it might also help to say “What questions do others have?” Next, using techniques like the “teach back” model the physician should check in to see what the family is taking away from the conversation. If a family understands, they can “teach back” the information accurately. This “ask” can be done in a way that does not make the family feel they are being tested: “I am not always clear when I communicate. Do you mind telling me back in your own words what you thought I said so I know we are on the same page?” This also provides an opportunity to answer any new questions that arise. Hearing the information directly from the family can allow the team to clarify any misconceptions and give insight into any emotional responses that the family might have.
4. Respond to Emotion
Discussing serious news in the ICU setting naturally leads to an emotional reaction. The clinician’s ability to notice emotional cues and respond with empathy is a key communication skill in family meetings [13]. Emotional reactions impede individual’s ability to process cognitive information and make it hard to think cognitively about what should be done next.
Physicians miss opportunities to respond to emotion in family meetings [14]. Missed opportunities lead to decreased family satisfaction and may lead to treatment decisions not consistent with the wishes of their loved ones. Empathic responses improve the family-clinician relationship and helps build trust and rapport [15]. Well- placed empathic statements may help surrogates disclose concerns that help the physician better understand the goals and values of the family and patient. Families also can more fully process cognitive information when their emotional responses have been attended to.
Physicians can develop the capacity to recognize and respond to the emotional cues family members are delivering. Intensivists should actively look for the emotions, the empathic opportunity, that are displayed by the family. This emotion is the “data” that will help lead to an empathic response. A family that just received bad news typically responds by showing emotion. Clues that emotions are present include: the family asking the same questions multiple times; using emotional words such as “sad” or “frustrated;” existential questions that do not have a cognitive answer such as “Why did God let this happen?;” or non-verbal cues like tears and hand wringing.
Sometimes the emotional responses are more difficult to recognize. Families may continue to ask for more cognitive information after hearing bad news. Someone keeps asking “Why did his kidney function worsen?” or “I thought the team said the chest x-ray looked better.” It is tempting to start answering these questions with more medical facts. However, if the question comes after bad news, it is usually an expression of frustration or sadness rather than a request for more information. Rather than giving information, it might help to acknowledge this by saying “I imagine this new is overwhelming.”
5. Highlight the Patient’s Voice
Family meetings are often used to develop new treatment plans (given that the old plans are not working). In these situations, it is essential to understand what the incapacitated patient would say if they were part of the family meeting. The surrogate’s primary role is to represent the patient’s voice. To do this, surrogates need assistance in applying their critically ill loved one’s thoughts and values to complex, possibly life limiting, situations. Surrogate decision makers struggle with the decisions’ emotional impact, as well as how to reconcile their desires with their loved one’s wishes [18]. This can lead them to make decisions that conflict with the loved one’s values [19] as well as emotional sequelae such as PTSD and depression [20].
As families reflect on their loved one’s values, conflicting desires will arise. For example, someone may have wanted to live as long as possible and also values independence. Or someone may value their ability to think clearly more than being physically well but would not want to be physically dependent on artificial life support. Exploring which values would be more important can help resolve these conflicts.
Clinicians should check for understanding while family members are identifying the values of their loved ones. Providing the family with a summary of what you have heard will help ensure a more accurate understanding of these crucial issues. A summary statement might be, “It sounds like you are saying your dad really valued his independence. He enjoyed being able to take care of his loved ones and himself. Is that right?”
6. Plan Next Steps
The family meeting serves to attend to family emotion and allow space to elicit patients’ values. Following a family meeting surrogate decision makers may be able to begin to consider the next steps in their loved one’s care. If bad news was delivered they may need space to adjust to a different future than they expected. Using an empathic statement of support “We will continue to make sure we communicate with you as we work together to plan next steps” will reassure a family that they have time and space to plan for the future.
Families vary regarding how much physician input they desire in planning next steps [21]. You can explicitly ask how the team can best help the family with decisions: “Some families like to hear the options for next steps from the team and make a decision, other families like to hear a recommendation from the team. What would be the most helpful for you?” Throughout the course of an illness a surrogate’s preference for decision making may change and clinicians should be responsive to those changing needs.
If the surrogate wants a clinician’s recommendation, 3 points are worth stressing. First, the recommendation should be personalized to this patient and his values. The goal is to reveal how the understanding of the patient’s values led to the treatment plan offered. Second, the recommendation should focus primarily on what will be done to achieve the patient’s values. Focusing on what the clinicians will do may help the family feel that the clinicians are still “trying” and not abandoning their loved one. In this case, the team will continue medical care that will help the patient regain/maintain independence. Only after talking about what will be done should the clinician point out that certain interventions will not achieve the patient’s goals and thus will not be done:
“It sounds like your father really valued his independence and that this illness has really taken that away. Knowing this, would it be helpful for me to make a recommendation for next steps?” “I think we should continue providing excellent medical care for your father in hopes he can get better and go home. One the other hand, if he gets worse, we should not use therapies such as CPR or dialysis that are unlikely to help him regain his independence.”
Finally, be concrete when planning next steps. If a time-limited trial of a therapy is proposed, make sure the family understands what a successful and unsuccessful trial will look like. Make plans to meet again on a specific date in order to ensure the family understands the progress being made. If a transition to comfort care is agreed upon, ensure support of the entire family during the next hours to days and offer services such as chaplaincy or child life specialists.
A family may not agree with the recommendation and back and forth discussion can help create a plan that is in line with their understanding of the illness. Rather than convincing, a clinician should keep an open mind about why they and the surrogate disagree. Do they have different views about the patient’s future? Did the medical team misunderstand the patient’s values? Are there emotional factors that inhibit the surrogate’s ability to attend to the discussion? It is only by learning where the disagreement is that a clinician can move the conversation forward.
A surrogate may ask about a therapy that is not beneficial or may increase distress to the patient. The use of “I wish” or “I worry” statements can be helpful at these points. These specific phrases recognize the surrogate’s desire to do more but also imply that the therapies are not helpful.
“I wish that his ability to communicate and tell you what he wants would get better with a little more time as well.”
“I worry that waiting 2 more weeks for improvement will actually cause complications to occur.”
7. Reflect
Family meetings have an impact on both the family and the medical team. Following the meeting, a short debriefing with the clinical team can be helpful. Summarizing the events of the meeting ensures clarity about the treatment plan going forward. It provides team members a chance to discuss conflicts that may have arisen. It allows the participants in the meeting to reflect on what communication skills they used and how they can improve their skills going forward.
Conclusion
Family meetings with surrogate decision makers must navigate multiple agendas of the family and providers. The goal of excellent communication with surrogates in an ICU should be to understand the patient’s goals and values and seek to make treatment plans that align with their perspective. This talking map provides a conceptual framework for physicians to guide a family through these conversations. The framework creates an opportunity to focus on the patient’s values and preferences for care while allowing space to attend to emotional responses to reduce the distress inherent in surrogate decision-making. Practicing the behaviors demonstrated in the talking map may increase clinician skill during difficult conversations. Improving communication with surrogate decision makers will increase the support we offer to critically ill patients and their loved ones.
Corresponding author: Jessica McFarlin, MD, jessmcfarlin@gmail.com.
Funding/support: Dr. Arnold receives support though the Leo H. Criep Chair in Patient Care.
Financial disclosures: None.
1. Hickey M. What are the needs of families of critically ill patients? A review of the literature since 1976. Heart Lung 1990;19:401–15.
2. Mosenthal AC, Murphy PA, Barker LK, et al. Changing culture around end-of-life care in the trauma intensive care unit. J Trauma 2008;64:1587–93.
3. Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 2007;356:469–78.
4. Selecky PA, Eliasson AH, Hall RI, et al. Palliative and end-of-life care for patients with cardiopulmonary diseases. Chest 2005;128:3599–610.
5. Henrich NJ, Dodek P, Heyland D, et al. Qualitative analysis of an intensive care unit family satisfaction survey. Crit Care Med 2011;39:1000–5.
6. Azoulet E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med 2000;28:3044–9.
7. Curtis JR. Communicating about end-of-life care with patients and families in the intensive care unit. Crit Care Clin 2004;20:363–80.
8. Hope AA, Hsieh SJ, Howes JM, et al. Let’s talk critical. Development and evaluation of a communication skills training program for critical care fellows. Ann Am Thorac Soc 2015;12:505–11.
9. Back AL, Arnold RM, Baile WF, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 2007;167:453–60.
10. Vital Talk. Conduct a family conference. Accessed 27 June 2016 at www.vitaltalk.org/clinicians/family.
11. Kramer M, Schmalenberg C. Securing “good” nurse/physician relationships. Nurs Manage 2003;34:34–8.
12. Johnson D, Wilson M, Cavanaugh B, et al. Measuring the ability to meet family needs in an intensive care unit. Crit Care Med 1998;26:266–71.
13. Back AL, Arnold RM. “Isn’t there anything more you can do?’’: when empathic statements work, and when they don’t. J Palliat Med 2013;16:1429–32.
14. Curtis JR, Engelberg RA, Wenrich MD. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med 2005;171:844–9.
15. Pollak KI, Arnold RM, Jeffreys AS, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol 2007;36:5748–52.
16. Back AL, Arnold RM, Tulsky JA. Mastering communication with seriously ill patients: balancing honesty with empathy and hope. Cambridge: Cambridge University Press; 2009.
17. Back AL, Arnold RM, Baile WF, et al. Approaching difficult communication tasks in oncology. CA Cancer J Clin 2005;55:164–77.
18. Schenker Y, White D, Crowley-Matoka M, et al. “It hurts to know…and it helps”: exploring how surrogates in the ICU cope with prognostic information. J Palliat Med 2013;16:243–9.
19. Scheunemann LP, Arnold RM, White DB. The facilitated values history: helping surrogates make authentic decisions for incapacitated patients with advanced illness. Am J Respir Crit Care Med 2012;186:480–6.
20. Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 2005;171:987–94.
21. White DB, Braddock CH, Bereknyei et al. Toward shared decision making at the end of life in intensive care units: opportunities for improvement. Arch Intern Med 2007;167:461–7.
1. Hickey M. What are the needs of families of critically ill patients? A review of the literature since 1976. Heart Lung 1990;19:401–15.
2. Mosenthal AC, Murphy PA, Barker LK, et al. Changing culture around end-of-life care in the trauma intensive care unit. J Trauma 2008;64:1587–93.
3. Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 2007;356:469–78.
4. Selecky PA, Eliasson AH, Hall RI, et al. Palliative and end-of-life care for patients with cardiopulmonary diseases. Chest 2005;128:3599–610.
5. Henrich NJ, Dodek P, Heyland D, et al. Qualitative analysis of an intensive care unit family satisfaction survey. Crit Care Med 2011;39:1000–5.
6. Azoulet E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med 2000;28:3044–9.
7. Curtis JR. Communicating about end-of-life care with patients and families in the intensive care unit. Crit Care Clin 2004;20:363–80.
8. Hope AA, Hsieh SJ, Howes JM, et al. Let’s talk critical. Development and evaluation of a communication skills training program for critical care fellows. Ann Am Thorac Soc 2015;12:505–11.
9. Back AL, Arnold RM, Baile WF, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 2007;167:453–60.
10. Vital Talk. Conduct a family conference. Accessed 27 June 2016 at www.vitaltalk.org/clinicians/family.
11. Kramer M, Schmalenberg C. Securing “good” nurse/physician relationships. Nurs Manage 2003;34:34–8.
12. Johnson D, Wilson M, Cavanaugh B, et al. Measuring the ability to meet family needs in an intensive care unit. Crit Care Med 1998;26:266–71.
13. Back AL, Arnold RM. “Isn’t there anything more you can do?’’: when empathic statements work, and when they don’t. J Palliat Med 2013;16:1429–32.
14. Curtis JR, Engelberg RA, Wenrich MD. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med 2005;171:844–9.
15. Pollak KI, Arnold RM, Jeffreys AS, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol 2007;36:5748–52.
16. Back AL, Arnold RM, Tulsky JA. Mastering communication with seriously ill patients: balancing honesty with empathy and hope. Cambridge: Cambridge University Press; 2009.
17. Back AL, Arnold RM, Baile WF, et al. Approaching difficult communication tasks in oncology. CA Cancer J Clin 2005;55:164–77.
18. Schenker Y, White D, Crowley-Matoka M, et al. “It hurts to know…and it helps”: exploring how surrogates in the ICU cope with prognostic information. J Palliat Med 2013;16:243–9.
19. Scheunemann LP, Arnold RM, White DB. The facilitated values history: helping surrogates make authentic decisions for incapacitated patients with advanced illness. Am J Respir Crit Care Med 2012;186:480–6.
20. Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 2005;171:987–94.
21. White DB, Braddock CH, Bereknyei et al. Toward shared decision making at the end of life in intensive care units: opportunities for improvement. Arch Intern Med 2007;167:461–7.
Weight-loss talks: What works (and what doesn’t)
Background In primary care encounters, it is unknown whether physician advice on weight-related matters leads to patient weight loss. To examine this issue, we analyzed physician weight loss advice and measured corresponding changes in patients’ dietary intake, physical activity, and weight.
Methods Using audio-recorded primary care encounters between 40 physicians and 461 of their overweight or obese patients, we coded weight-related advice as nonspecific, specific nutritional, specific exercise, or specific weight. Physicians and patients were told the study was about preventive health, not weight. We used mixed models (SAS Proc Mixed), controlled for physician clustering and baseline covariates, to assess changes in diet, exercise, and measured weight, both pre-encounter and 3 months post-encounter.
Results When discussing weight, physicians typically provided a combination of specific weight, nutrition, and physical activity advice to their patients (34%). Combined advice resulted in patients reducing their dietary fat intake (P=.02). However, when physicians provided physical activity advice only, patients were significantly (P=.02) more likely to gain weight (+1.41 kg) compared with those who received no advice.
Conclusion When giving weight-related advice, most physicians provided a combination of lifestyle recommendations. Combining advice may help patients reduce their fat in-take. Physical activity advice alone may not be particularly helpful.
The US Preventive Services Task Force (USPSTF) recommends that physicians screen patients for obesity and offer intensive counseling and behavioral interventions to promote sustained weight loss.1 Evidence suggests that physician counseling, including advice, can help patients to lose weight, increase physical activity, and improve diet.2-9 However, little is known about what specific types of weight loss advice physicians give to patients, and whether some types are more effective than others at influencing behavior change.
We analyzed physician weight loss advice delivered in primary care visits and measured changes in patients’ dietary intake, physical activity, and body weight. We examined both the type of weight loss advice delivered and the impact of type of advice on weight and behavior change.
Methods
This study analyzed audio recordings from Project CHAT – Communicating Health: Analyzing Talk. The project was approved by the Duke University Medical Center Institutional Review Board.
Recruitment Physicians. We obtained consent from 40 primary care physicians in community-based practices and told them the study would examine communication around preventive health topics, not weight specifically.
Patients. We identified potential participants by reviewing scheduled appointments 3 weeks in advance. Eligible participants were at least 18 years of age, English-speaking, overweight or obese (body mass index [BMI] ≥25 kg/m2), cognitively competent, and not pregnant. After we obtained consent, a remotely located research assistant started a digital audio recorder as the patient entered the exam room. Immediately after the encounter, the research assistant administered a post-encounter survey to the patient and recorded the patient’s vital signs (N=461). Three months later, the research assistant met with the participant to record vital signs and administer a survey assessing changes in dietary fat intake and exercise (N=426).
Data coding
We coded advice into 4 broad categories: (1) nutrition advice, (2) physical activity advice, (3) specific weight loss advice, and (4) nonspecific weight loss/weight-related advice. We transcribed each piece of advice verbatim.
Nutrition advice consisted of 9 sub-categories: calorie/portion control, meal timing/planning, commercial diet plans, negative diet plans, increase fruits/vegetables, reduce sugar/carbohydrates, reduce fat/cholesterol, other micronutrient recommendations, and specific food items from multiple categories.
Physical activity advice consisted of 6 subcategories: walking, aerobic exercise, anaerobic exercise, exercise intensity, exercise duration, and exercise for comorbid conditions.
Specific weight loss advice consisted of 3 categories: weight loss behavior, weight loss for comorbid conditions, and referrals.
Nonspecific weight loss advice also consisted of 3 subcategories in which physicians provided no details about the general topics of nutrition, physical activity, or weight loss.
Two independent coders (CBT and MEC) assessed each piece of advice and double coded 20% of conversations for reliability. Cohen’s kappa was used to calculate inter-rater reliability for each code using Landis and Koch’s classification (0.21-0.40=fair agreement; 0.41-0.60=moderate agreement; 0.61-0.80=substantial agreement; 0.81-1.0=near-perfect agreement).10 Three advice categories achieved near perfect agreement: nutrition (kappa= 0.94; 95% confidence interval [CI] 0.82-1.0; 99.2% agreement), physical activity (kappa=0.91; 95% CI, 0.84-0.99; 98.6% agreement), and weight loss (kappa=0.95; 95% CI, 0.82-1.0; 99.7% agreement). The nonspecific weight loss advice category had slightly lower agreement but still achieved near-perfect agreement (kappa=0.82; 95% CI, 0.62-1.0; 99.2% agreement).
After all advice was coded, we placed conversations into 1 of 6 categories: (1) no advice given; (2) nonspecific advice only; (3) nutrition only; (4) physical activity only; (5) weight loss only; or (6) combination of nutrition, physical activity, and/or weight loss.
Measures
Dietary fat and fiber intake. We assessed dietary fat intake at baseline and at 3 months using the 22-item Fat- and Fiber-Related Diet Behavior Questionnaire.11,12 Questions about frequency of food selections included, “When you ate dessert, how often did you eat only fruit?” and “When you ate chicken, how often did you take off the skin?” We averaged responses into a total score wherein 1 reflected higher fiber, lower fat food choices; a score of 4 reflected lower fiber, higher fat choices (α=0.74 at baseline and α=0.77 at 3-month follow-up).
Physical activity. We measured physical activity (baseline, 3 months) using the Framingham Physical Activity Index.13 Participants recalled the average number of hours spent engaged in various daily activities (sleeping, working, leisure) and the level of activity for each (sedentary, slight, moderate, or heavy). The composite score accounts for activity duration and intensity.
Anthropometrics. We measured patient weight (baseline, 3 months) and height (baseline only) using a calibrated scale and portable stadiometer. Patients removed shoes, outerwear, and belongings from their pockets before being weighed.
Analysis
We analyzed data using SAS (SAS Institute, Inc., Cary, NC). We assessed the association between type of advice and weight loss, improvement in dietary fat intake behaviors, and increase in physical activity between baseline and the 3-month follow-up visit. We used PROC MIXED to fit general linear models; we incorporated responses into these models from all participants who provided measurements for at least one time point. This modeling framework yields unbiased estimates when missing data are unrelated to the observed variable.14
Primary predictors: (1) type of advice (none, nonspecific, nutrition, physical activity, weight loss, and combination), (2) time since baseline visit, and (3) time by type of advice interaction. All models included a priori defined patient, physician, and visit-related covariates that were theoretically or empirically related to changes in the outcomes (weight, physical activity, or dietary fat in-take). The 14 patient covariates were sex; age; race; high school education; economic security (enough money to pay monthly bills); over-weight (BMI, 25-29.9 kg/m2) or obese (BMI ≥30 kg/m2); actively trying to lose weight (yes/ no); motivated to lose weight (Likert scale 1-7); comfortable discussing weight (Likert scale 1-5); confident about losing weight (Likert scale 1-5); and patient-reported comorbid conditions of diabetes, hypertension, arthritis, and hyperlipidemia.
The 9 physician covariates were sex; race; years since medical school graduation; specialty (family vs internal medicine); self-efficacy (Likert scale 1-5); barriers for weight counseling (Likert scale 1-5); comfort discussing weight (Likert scale 1-5); insurance reimbursement concerns (Likert scale 1-5); and prior training in behavioral counseling (yes/no). Finally, 2 visit-level covariates were included: minutes spent addressing weight issues and visit type (preventive vs chronic).
Results
Sample characteristics
Of the 40 physicians, 19 were family physicians and 21 were internists. More than half of the physicians were female (60%), and 85% were white. Mean age was 47.2 years and mean BMI was 24.9 kg/m2. Of the 461 patients, 66% were female, 65% were white, 35% were African American, and two-thirds had post-high school education (TABLE 1). Mean patient age was 59.8 years; only 4% of the patients were new to their physicians.
TABLE 1
Patient characteristics (N=461)
| % or mean (SD) | |
|---|---|
| Race | |
| White/Asian/Pacific Islander | 65% |
| African American | 35% |
| Female | 66% |
| Age, y (missing=1)* | 59.8 (13.9) |
| BMI, kg/m2 (missing=1)* | 33.1 (7.1) |
| Education (missing=1)* | |
| Post-high school | 67% |
| Income (missing=37)* | |
| $45,000 or less | 48% |
| High financial burden (missing=13)* | |
| Pay bills with trouble | 14% |
| Diagnosed with: | |
| Diabetes | 31% |
| Hypertension (missing=1)* | 69% |
| Hyperlipidemia (missing=1)* | 56% |
| Arthritis | 47% |
| New patient | 4% |
| BMI, body mass index; SD, standard deviation. * Missing data at baseline. | |
Frequency of advice
Physicians gave some type of weight-related advice in 63% of the encounters. They combined types of advice in 34% of all conversations, provided physical activity advice only in 13%, nutrition advice only in 8%, nonspecific advice in 5%, and weight loss advice only in 3%. Many times when physicians gave advice, it was centered on self (eg, “I need you to do X” or “What will it take for me to get you to do Y?”).
Nutrition advice most commonly pertained to specific food items from multiple categories (27% of conversations). Physicians also advised patients to reduce sugar/carbohydrates, control calories and portions, add other micronutrients, eat more fruits/vegetables, and eat meals more frequently.
Walking was the physical activity topic discussed most frequently, followed by exercise duration, exercise for comorbidities, aerobic activities, exercise intensity, and anaerobic exercise. The most common specific weight loss topic was weight loss behavioral advice, followed by weight loss for comorbid conditions. Physicians rarely provided referrals to weight-loss programs.
Effect of type of advice on fat and fiber diet behavior score
Receipt of nutrition advice only was not associated with reduction in fat intake (P=.43, TABLE 2). However, those who received combined types of advice exhibited a significantly greater reduction of fat intake compared with those who received no advice (Fat- and Fiber-Related Diet Behavior Questionnaire score reduction of 0.15 vs 0.05; P=.02).
TABLE 2
How types of physician advice affected dietary fat intake, physical activity, and weight
| Type of advice | ||||||
|---|---|---|---|---|---|---|
| None | Nutrition only | Physical activity only | Weight loss only | Combined advice | Nonspecific | |
| Dietary fat change in Fat- and Fiber-Related Diet Behavior Questionnaire score differences | ||||||
| At 3 months from baseline (95% CI) | -0.05 (-0.11 to 0.004) | -0.10 (-0.22 to 0.01) | -0.07 (-0.16 to 0.02) | -0.08 (-0.26 to 0.09) | -0.15 (-0.20 to -0.09) | 0.03 (0.11 to 0.18) |
| P value* | .43 | .75 | .73 | .02 | .31 | |
| Physical activity score (change in MET hours) | ||||||
| At 3 months from baseline (95% CI) | 0.48 (-0.17 to 1.11) | 0.83 (-0.51 to 2.14) | 0.69 (-0.33 to 1.69) | -0.72 (-2.66 to 1.21) | 0.24 (-0.40 to 0.86) | -0.07 (-1.74 to 1.59) |
| P value* | .64 | .73 | .25 | .60 | .55 | |
| Weight change (kg) | ||||||
| At 3 months from baseline (95% CI) | -0.18 (-0.39 to 0.75) | -0.18 (-1.38 to 1.02) | 1.41 (0.51 to 2.31) | -0.26 (-1.99 to 1.47) | -0.55 (-1.12 to 0.02) | -0.62 (-2.11 to 0.87) |
| P value* | .59 | .02 | .63 | .08 | .32 | |
| CI, confidence interval; MET, metabolic equivalent tasks. *Test of difference between advice given and no advice given. | ||||||
Effect of type of advice on Framingham Physical Activity score
No type of advice, including physical activity advice, led to a change in Framingham Physical Activity scores at the 3-month visit (overall P=.76; TABLE 2).
Effect of type of advice on weight loss
Patients who received physical activity advice gained significantly more weight than patients who received no advice (1.41 kg gained vs 0.18 kg lost; P=.02). Patients who received combined advice lost more weight than patients who received no advice, but the difference did not reach statistical significance (0.55 kg lost vs 0.18 kg lost; P=.08).
Discussion
Physicians typically took an “all or nothing” approach to weight-related issues, giving no advice (37%) or a combination of nutrition, physical activity, and weight loss advice (34%). It seems when physicians do give advice, most of them follow the USPSTF guidelines by addressing nutrition and physical activity together.15
Providing advice alone did not predict a change in patient behavior. For instance, we found no significant association between dietary fat reduction and having received only nutrition advice. Possible explanations include the following:
- Although physicians advised patients to reduce fat/cholesterol intake in 28% of conversations, they did so mostly in combination with other types of advice. Nutrition-only advice occurred in only 8% of conversations. Thus, there may have been insufficient power to detect the impact of this specific type of advice.
- With nutrition-only advice, the most common recommendation was to reduce carbohydrates/sweets, which should not affect fat intake.
Advising patients solely on physical activity led to unintended weight gain overall. Other data have shown that exercise without dietary changes, though beneficial in many ways, is not substantially effective for weight loss.15 People may eat more when they exercise, either to reward themselves or to satiate increased appetite from increased energy expenditure. Or, if physicians recommend the standard goal of 150 minutes of intensive physical activity per week, normally sedentary patients may see that as unattainable and become too discouraged to try.1,16,17
Combining types of advice seemed to help patients reduce their fat intake. Overall, however, simple, brief advice from a physician may not be enough to promote healthy lifestyle changes.
Also notable was that physicians rarely provided referrals, even though this is a strong recommendation from the National Institutes of Health, the American Diabetes Association, and the USPSTF.1,16,17 It could be that many physicians believe referrals are not covered by insurance. Yet, the low frequency of referrals may suggest an important missing component of weight loss therapy, especially given that physician advice alone seems an inadequate intervention.
Avoid physician-centered appeals. Advice was often given in a physician-centered way. There are 3 possible explanations for such phrasing:
- In the absence of clear evidence about how to deliver weight loss advice, physicians may be formulating advice based on their personal or clinical experiences.
- Physicians either assume or sense that patients lack internal motivation to make lifestyle changes for themselves and instead request that patients make changes for the doctor-patient relationship.
- Physicians might be trying to invoke authority in the hope that patients will respond accordingly.
Whatever the reason, the literature on self-centered physician talk indicates that patients are less satisfied when physicians make the visit more about themselves than about patients.18 A better strategy might be to use Motivational Interviewing19 that supports patient autonomy and attempts to elicit and build on internal motivation.
The take-away message is that behavior change is complex and that knowledge is a necessary but insufficient agent for change. Following the tenets of Social Cognitive Theory,20 physicians might also need to address patient motivation, confidence, outcome expectations, and skills to help promote behavior change.
Strengths and limitations of this study
We recorded conversations rather than relying on physician or patient recall. Additionally, these primary care patients were not enrolled in a weight-loss trial and, therefore, were not self-selected to be highly motivated to lose weight. Because of this, and the large and ethnically diverse sample, our results should be generalizable to many clinical settings.
One limitation is that few younger, lower-income patients were included in the sample, which limits generalizability to those populations. Also, the study was observational. Although we adjusted for a broad set of patient, physician, and visit covariates, unmeasured confounding variables may still account for at least part of the observed associations. The analysis is limited by the use of self-reported dietary fat intake and physical activity measures. A food diary and accelerometer would have been more accurate; however, such involved measures could invoke changes in behavior, which would have confounded our ability to assess the effect of physician advice on weight loss.
Acknowledgements
The authors thank all of the physicians and patients who participated in this study, the study project managers Gretchen Yonish and Iguehi Esoimeme, and research assistant Justin Manusov.
CORRESPONDENCE
Stewart C. Alexander, PhD, Department of Medicine, Duke University School of Medicine, P.O. Box 3140 Medical Center, Durham, NC 27710; alexa045@mc.duke.edu
1. US Preventive Services Task Force. Screening for obesity in adults: recommendations and rationale. Ann Intern Med. 2003;139:930-932.
2. Nawaz H, Adams ML, Katz DL. Physician-patient interactions regarding diet, exercise, and smoking. Prev Med. 2000;31:652-657.
3. Sciamanna CN, Tate DF, Lang W, et al. Who reports receiving advice to lose weight? Results from a multistate survey. Arch Intern Med. 2000;160:2334-2339.
4. Galuska DA, Will JC, Serdula MK, et al. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282:1576-1578.
5. Evans E. Why should obesity be managed? The obese individual’s perspective. Int J Obes Relat Metab Disord. 1999;23(suppl 4):S3-S6.
6. Mehrotra C, Naimi TS, Serdula M, et al. Arthritis, body mass index, and professional advice to lose weight: implications for clinical medicine and public health. Am J Prev Med. 2004;27:16-21.
7. Loureiro ML, Nayga RM Jr. Obesity, weight loss, and physician’s advice. Soc Sci Med. 2006;62:2458-2468.
8. Flocke SA, Clark A, Schlessman K, et al. Exercise, diet, and weight loss advice in the family medicine outpatient setting. Fam Med. 2005;37:415-421.
9. Alexander SC, Cox ME, Østbye T, et al. Do the 5 A’s work for weight-loss counseling? Presented at: International Conference on Communication in Healthcare; October 4–7, 2009; Miami, Fla.
10. McGinn T, Wyer PC, Newman TB, et al. Tips for learners of evidence-based medicine: 3. Measures of observer variability (kappa statistic). CMAJ. 2004;171:1369-1373.
11. Shannon J, Kristal AR, Curry SJ, et al. Application of a behavioral approach to measuring dietary change: the fat- and fiber-related diet behavior questionnaire. Cancer Epidemiol Biomarkers Prev. 1997;6:355-361.
12. Kristal AR, Shattuck AL, Henry HJ. Patterns of dietary behavior associated with selecting diets low in fat: reliability and validity of a behavioral approach to dietary assessment. J Am Diet Assoc. 1990;90:214-220.
13. Kannel WB, Sorlie P. Some health benefits of physical activity: the Framingham study. Arch Intern Med. 1979;139:857-861.
14. Little RJA, Rubin DB. Statistical Analysis With Missing Data. New York, NY: John Wiley & Sons; 2002.
15. Franz MJ, VanWormer JJ, Crain AL, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755-1767.
16. National Institutes of Health. The practical guide: identification, evaluation, and treatment of overweight and obesity in adults. NIH publication 00-4084. 2000. Available at: http://www.nhlbi.nih.gov/guidelines/obesity/prctgd_c.pdf. Accessed August 17, 2009.
17. American Diabetes Association. Standards of medical care in diabetes–2010. Diabetes Care. 2010;33(suppl 1):S11-S61.
18. Beach MC, Roter DL. Interpersonal expectations in the patient-physician relationship. J Gen Intern Med. 2000;15:825-827.
19. Miller WR, Rollnick SP, Miller WR. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford Press; 2002.
20. Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.
Background In primary care encounters, it is unknown whether physician advice on weight-related matters leads to patient weight loss. To examine this issue, we analyzed physician weight loss advice and measured corresponding changes in patients’ dietary intake, physical activity, and weight.
Methods Using audio-recorded primary care encounters between 40 physicians and 461 of their overweight or obese patients, we coded weight-related advice as nonspecific, specific nutritional, specific exercise, or specific weight. Physicians and patients were told the study was about preventive health, not weight. We used mixed models (SAS Proc Mixed), controlled for physician clustering and baseline covariates, to assess changes in diet, exercise, and measured weight, both pre-encounter and 3 months post-encounter.
Results When discussing weight, physicians typically provided a combination of specific weight, nutrition, and physical activity advice to their patients (34%). Combined advice resulted in patients reducing their dietary fat intake (P=.02). However, when physicians provided physical activity advice only, patients were significantly (P=.02) more likely to gain weight (+1.41 kg) compared with those who received no advice.
Conclusion When giving weight-related advice, most physicians provided a combination of lifestyle recommendations. Combining advice may help patients reduce their fat in-take. Physical activity advice alone may not be particularly helpful.
The US Preventive Services Task Force (USPSTF) recommends that physicians screen patients for obesity and offer intensive counseling and behavioral interventions to promote sustained weight loss.1 Evidence suggests that physician counseling, including advice, can help patients to lose weight, increase physical activity, and improve diet.2-9 However, little is known about what specific types of weight loss advice physicians give to patients, and whether some types are more effective than others at influencing behavior change.
We analyzed physician weight loss advice delivered in primary care visits and measured changes in patients’ dietary intake, physical activity, and body weight. We examined both the type of weight loss advice delivered and the impact of type of advice on weight and behavior change.
Methods
This study analyzed audio recordings from Project CHAT – Communicating Health: Analyzing Talk. The project was approved by the Duke University Medical Center Institutional Review Board.
Recruitment Physicians. We obtained consent from 40 primary care physicians in community-based practices and told them the study would examine communication around preventive health topics, not weight specifically.
Patients. We identified potential participants by reviewing scheduled appointments 3 weeks in advance. Eligible participants were at least 18 years of age, English-speaking, overweight or obese (body mass index [BMI] ≥25 kg/m2), cognitively competent, and not pregnant. After we obtained consent, a remotely located research assistant started a digital audio recorder as the patient entered the exam room. Immediately after the encounter, the research assistant administered a post-encounter survey to the patient and recorded the patient’s vital signs (N=461). Three months later, the research assistant met with the participant to record vital signs and administer a survey assessing changes in dietary fat intake and exercise (N=426).
Data coding
We coded advice into 4 broad categories: (1) nutrition advice, (2) physical activity advice, (3) specific weight loss advice, and (4) nonspecific weight loss/weight-related advice. We transcribed each piece of advice verbatim.
Nutrition advice consisted of 9 sub-categories: calorie/portion control, meal timing/planning, commercial diet plans, negative diet plans, increase fruits/vegetables, reduce sugar/carbohydrates, reduce fat/cholesterol, other micronutrient recommendations, and specific food items from multiple categories.
Physical activity advice consisted of 6 subcategories: walking, aerobic exercise, anaerobic exercise, exercise intensity, exercise duration, and exercise for comorbid conditions.
Specific weight loss advice consisted of 3 categories: weight loss behavior, weight loss for comorbid conditions, and referrals.
Nonspecific weight loss advice also consisted of 3 subcategories in which physicians provided no details about the general topics of nutrition, physical activity, or weight loss.
Two independent coders (CBT and MEC) assessed each piece of advice and double coded 20% of conversations for reliability. Cohen’s kappa was used to calculate inter-rater reliability for each code using Landis and Koch’s classification (0.21-0.40=fair agreement; 0.41-0.60=moderate agreement; 0.61-0.80=substantial agreement; 0.81-1.0=near-perfect agreement).10 Three advice categories achieved near perfect agreement: nutrition (kappa= 0.94; 95% confidence interval [CI] 0.82-1.0; 99.2% agreement), physical activity (kappa=0.91; 95% CI, 0.84-0.99; 98.6% agreement), and weight loss (kappa=0.95; 95% CI, 0.82-1.0; 99.7% agreement). The nonspecific weight loss advice category had slightly lower agreement but still achieved near-perfect agreement (kappa=0.82; 95% CI, 0.62-1.0; 99.2% agreement).
After all advice was coded, we placed conversations into 1 of 6 categories: (1) no advice given; (2) nonspecific advice only; (3) nutrition only; (4) physical activity only; (5) weight loss only; or (6) combination of nutrition, physical activity, and/or weight loss.
Measures
Dietary fat and fiber intake. We assessed dietary fat intake at baseline and at 3 months using the 22-item Fat- and Fiber-Related Diet Behavior Questionnaire.11,12 Questions about frequency of food selections included, “When you ate dessert, how often did you eat only fruit?” and “When you ate chicken, how often did you take off the skin?” We averaged responses into a total score wherein 1 reflected higher fiber, lower fat food choices; a score of 4 reflected lower fiber, higher fat choices (α=0.74 at baseline and α=0.77 at 3-month follow-up).
Physical activity. We measured physical activity (baseline, 3 months) using the Framingham Physical Activity Index.13 Participants recalled the average number of hours spent engaged in various daily activities (sleeping, working, leisure) and the level of activity for each (sedentary, slight, moderate, or heavy). The composite score accounts for activity duration and intensity.
Anthropometrics. We measured patient weight (baseline, 3 months) and height (baseline only) using a calibrated scale and portable stadiometer. Patients removed shoes, outerwear, and belongings from their pockets before being weighed.
Analysis
We analyzed data using SAS (SAS Institute, Inc., Cary, NC). We assessed the association between type of advice and weight loss, improvement in dietary fat intake behaviors, and increase in physical activity between baseline and the 3-month follow-up visit. We used PROC MIXED to fit general linear models; we incorporated responses into these models from all participants who provided measurements for at least one time point. This modeling framework yields unbiased estimates when missing data are unrelated to the observed variable.14
Primary predictors: (1) type of advice (none, nonspecific, nutrition, physical activity, weight loss, and combination), (2) time since baseline visit, and (3) time by type of advice interaction. All models included a priori defined patient, physician, and visit-related covariates that were theoretically or empirically related to changes in the outcomes (weight, physical activity, or dietary fat in-take). The 14 patient covariates were sex; age; race; high school education; economic security (enough money to pay monthly bills); over-weight (BMI, 25-29.9 kg/m2) or obese (BMI ≥30 kg/m2); actively trying to lose weight (yes/ no); motivated to lose weight (Likert scale 1-7); comfortable discussing weight (Likert scale 1-5); confident about losing weight (Likert scale 1-5); and patient-reported comorbid conditions of diabetes, hypertension, arthritis, and hyperlipidemia.
The 9 physician covariates were sex; race; years since medical school graduation; specialty (family vs internal medicine); self-efficacy (Likert scale 1-5); barriers for weight counseling (Likert scale 1-5); comfort discussing weight (Likert scale 1-5); insurance reimbursement concerns (Likert scale 1-5); and prior training in behavioral counseling (yes/no). Finally, 2 visit-level covariates were included: minutes spent addressing weight issues and visit type (preventive vs chronic).
Results
Sample characteristics
Of the 40 physicians, 19 were family physicians and 21 were internists. More than half of the physicians were female (60%), and 85% were white. Mean age was 47.2 years and mean BMI was 24.9 kg/m2. Of the 461 patients, 66% were female, 65% were white, 35% were African American, and two-thirds had post-high school education (TABLE 1). Mean patient age was 59.8 years; only 4% of the patients were new to their physicians.
TABLE 1
Patient characteristics (N=461)
| % or mean (SD) | |
|---|---|
| Race | |
| White/Asian/Pacific Islander | 65% |
| African American | 35% |
| Female | 66% |
| Age, y (missing=1)* | 59.8 (13.9) |
| BMI, kg/m2 (missing=1)* | 33.1 (7.1) |
| Education (missing=1)* | |
| Post-high school | 67% |
| Income (missing=37)* | |
| $45,000 or less | 48% |
| High financial burden (missing=13)* | |
| Pay bills with trouble | 14% |
| Diagnosed with: | |
| Diabetes | 31% |
| Hypertension (missing=1)* | 69% |
| Hyperlipidemia (missing=1)* | 56% |
| Arthritis | 47% |
| New patient | 4% |
| BMI, body mass index; SD, standard deviation. * Missing data at baseline. | |
Frequency of advice
Physicians gave some type of weight-related advice in 63% of the encounters. They combined types of advice in 34% of all conversations, provided physical activity advice only in 13%, nutrition advice only in 8%, nonspecific advice in 5%, and weight loss advice only in 3%. Many times when physicians gave advice, it was centered on self (eg, “I need you to do X” or “What will it take for me to get you to do Y?”).
Nutrition advice most commonly pertained to specific food items from multiple categories (27% of conversations). Physicians also advised patients to reduce sugar/carbohydrates, control calories and portions, add other micronutrients, eat more fruits/vegetables, and eat meals more frequently.
Walking was the physical activity topic discussed most frequently, followed by exercise duration, exercise for comorbidities, aerobic activities, exercise intensity, and anaerobic exercise. The most common specific weight loss topic was weight loss behavioral advice, followed by weight loss for comorbid conditions. Physicians rarely provided referrals to weight-loss programs.
Effect of type of advice on fat and fiber diet behavior score
Receipt of nutrition advice only was not associated with reduction in fat intake (P=.43, TABLE 2). However, those who received combined types of advice exhibited a significantly greater reduction of fat intake compared with those who received no advice (Fat- and Fiber-Related Diet Behavior Questionnaire score reduction of 0.15 vs 0.05; P=.02).
TABLE 2
How types of physician advice affected dietary fat intake, physical activity, and weight
| Type of advice | ||||||
|---|---|---|---|---|---|---|
| None | Nutrition only | Physical activity only | Weight loss only | Combined advice | Nonspecific | |
| Dietary fat change in Fat- and Fiber-Related Diet Behavior Questionnaire score differences | ||||||
| At 3 months from baseline (95% CI) | -0.05 (-0.11 to 0.004) | -0.10 (-0.22 to 0.01) | -0.07 (-0.16 to 0.02) | -0.08 (-0.26 to 0.09) | -0.15 (-0.20 to -0.09) | 0.03 (0.11 to 0.18) |
| P value* | .43 | .75 | .73 | .02 | .31 | |
| Physical activity score (change in MET hours) | ||||||
| At 3 months from baseline (95% CI) | 0.48 (-0.17 to 1.11) | 0.83 (-0.51 to 2.14) | 0.69 (-0.33 to 1.69) | -0.72 (-2.66 to 1.21) | 0.24 (-0.40 to 0.86) | -0.07 (-1.74 to 1.59) |
| P value* | .64 | .73 | .25 | .60 | .55 | |
| Weight change (kg) | ||||||
| At 3 months from baseline (95% CI) | -0.18 (-0.39 to 0.75) | -0.18 (-1.38 to 1.02) | 1.41 (0.51 to 2.31) | -0.26 (-1.99 to 1.47) | -0.55 (-1.12 to 0.02) | -0.62 (-2.11 to 0.87) |
| P value* | .59 | .02 | .63 | .08 | .32 | |
| CI, confidence interval; MET, metabolic equivalent tasks. *Test of difference between advice given and no advice given. | ||||||
Effect of type of advice on Framingham Physical Activity score
No type of advice, including physical activity advice, led to a change in Framingham Physical Activity scores at the 3-month visit (overall P=.76; TABLE 2).
Effect of type of advice on weight loss
Patients who received physical activity advice gained significantly more weight than patients who received no advice (1.41 kg gained vs 0.18 kg lost; P=.02). Patients who received combined advice lost more weight than patients who received no advice, but the difference did not reach statistical significance (0.55 kg lost vs 0.18 kg lost; P=.08).
Discussion
Physicians typically took an “all or nothing” approach to weight-related issues, giving no advice (37%) or a combination of nutrition, physical activity, and weight loss advice (34%). It seems when physicians do give advice, most of them follow the USPSTF guidelines by addressing nutrition and physical activity together.15
Providing advice alone did not predict a change in patient behavior. For instance, we found no significant association between dietary fat reduction and having received only nutrition advice. Possible explanations include the following:
- Although physicians advised patients to reduce fat/cholesterol intake in 28% of conversations, they did so mostly in combination with other types of advice. Nutrition-only advice occurred in only 8% of conversations. Thus, there may have been insufficient power to detect the impact of this specific type of advice.
- With nutrition-only advice, the most common recommendation was to reduce carbohydrates/sweets, which should not affect fat intake.
Advising patients solely on physical activity led to unintended weight gain overall. Other data have shown that exercise without dietary changes, though beneficial in many ways, is not substantially effective for weight loss.15 People may eat more when they exercise, either to reward themselves or to satiate increased appetite from increased energy expenditure. Or, if physicians recommend the standard goal of 150 minutes of intensive physical activity per week, normally sedentary patients may see that as unattainable and become too discouraged to try.1,16,17
Combining types of advice seemed to help patients reduce their fat intake. Overall, however, simple, brief advice from a physician may not be enough to promote healthy lifestyle changes.
Also notable was that physicians rarely provided referrals, even though this is a strong recommendation from the National Institutes of Health, the American Diabetes Association, and the USPSTF.1,16,17 It could be that many physicians believe referrals are not covered by insurance. Yet, the low frequency of referrals may suggest an important missing component of weight loss therapy, especially given that physician advice alone seems an inadequate intervention.
Avoid physician-centered appeals. Advice was often given in a physician-centered way. There are 3 possible explanations for such phrasing:
- In the absence of clear evidence about how to deliver weight loss advice, physicians may be formulating advice based on their personal or clinical experiences.
- Physicians either assume or sense that patients lack internal motivation to make lifestyle changes for themselves and instead request that patients make changes for the doctor-patient relationship.
- Physicians might be trying to invoke authority in the hope that patients will respond accordingly.
Whatever the reason, the literature on self-centered physician talk indicates that patients are less satisfied when physicians make the visit more about themselves than about patients.18 A better strategy might be to use Motivational Interviewing19 that supports patient autonomy and attempts to elicit and build on internal motivation.
The take-away message is that behavior change is complex and that knowledge is a necessary but insufficient agent for change. Following the tenets of Social Cognitive Theory,20 physicians might also need to address patient motivation, confidence, outcome expectations, and skills to help promote behavior change.
Strengths and limitations of this study
We recorded conversations rather than relying on physician or patient recall. Additionally, these primary care patients were not enrolled in a weight-loss trial and, therefore, were not self-selected to be highly motivated to lose weight. Because of this, and the large and ethnically diverse sample, our results should be generalizable to many clinical settings.
One limitation is that few younger, lower-income patients were included in the sample, which limits generalizability to those populations. Also, the study was observational. Although we adjusted for a broad set of patient, physician, and visit covariates, unmeasured confounding variables may still account for at least part of the observed associations. The analysis is limited by the use of self-reported dietary fat intake and physical activity measures. A food diary and accelerometer would have been more accurate; however, such involved measures could invoke changes in behavior, which would have confounded our ability to assess the effect of physician advice on weight loss.
Acknowledgements
The authors thank all of the physicians and patients who participated in this study, the study project managers Gretchen Yonish and Iguehi Esoimeme, and research assistant Justin Manusov.
CORRESPONDENCE
Stewart C. Alexander, PhD, Department of Medicine, Duke University School of Medicine, P.O. Box 3140 Medical Center, Durham, NC 27710; alexa045@mc.duke.edu
Background In primary care encounters, it is unknown whether physician advice on weight-related matters leads to patient weight loss. To examine this issue, we analyzed physician weight loss advice and measured corresponding changes in patients’ dietary intake, physical activity, and weight.
Methods Using audio-recorded primary care encounters between 40 physicians and 461 of their overweight or obese patients, we coded weight-related advice as nonspecific, specific nutritional, specific exercise, or specific weight. Physicians and patients were told the study was about preventive health, not weight. We used mixed models (SAS Proc Mixed), controlled for physician clustering and baseline covariates, to assess changes in diet, exercise, and measured weight, both pre-encounter and 3 months post-encounter.
Results When discussing weight, physicians typically provided a combination of specific weight, nutrition, and physical activity advice to their patients (34%). Combined advice resulted in patients reducing their dietary fat intake (P=.02). However, when physicians provided physical activity advice only, patients were significantly (P=.02) more likely to gain weight (+1.41 kg) compared with those who received no advice.
Conclusion When giving weight-related advice, most physicians provided a combination of lifestyle recommendations. Combining advice may help patients reduce their fat in-take. Physical activity advice alone may not be particularly helpful.
The US Preventive Services Task Force (USPSTF) recommends that physicians screen patients for obesity and offer intensive counseling and behavioral interventions to promote sustained weight loss.1 Evidence suggests that physician counseling, including advice, can help patients to lose weight, increase physical activity, and improve diet.2-9 However, little is known about what specific types of weight loss advice physicians give to patients, and whether some types are more effective than others at influencing behavior change.
We analyzed physician weight loss advice delivered in primary care visits and measured changes in patients’ dietary intake, physical activity, and body weight. We examined both the type of weight loss advice delivered and the impact of type of advice on weight and behavior change.
Methods
This study analyzed audio recordings from Project CHAT – Communicating Health: Analyzing Talk. The project was approved by the Duke University Medical Center Institutional Review Board.
Recruitment Physicians. We obtained consent from 40 primary care physicians in community-based practices and told them the study would examine communication around preventive health topics, not weight specifically.
Patients. We identified potential participants by reviewing scheduled appointments 3 weeks in advance. Eligible participants were at least 18 years of age, English-speaking, overweight or obese (body mass index [BMI] ≥25 kg/m2), cognitively competent, and not pregnant. After we obtained consent, a remotely located research assistant started a digital audio recorder as the patient entered the exam room. Immediately after the encounter, the research assistant administered a post-encounter survey to the patient and recorded the patient’s vital signs (N=461). Three months later, the research assistant met with the participant to record vital signs and administer a survey assessing changes in dietary fat intake and exercise (N=426).
Data coding
We coded advice into 4 broad categories: (1) nutrition advice, (2) physical activity advice, (3) specific weight loss advice, and (4) nonspecific weight loss/weight-related advice. We transcribed each piece of advice verbatim.
Nutrition advice consisted of 9 sub-categories: calorie/portion control, meal timing/planning, commercial diet plans, negative diet plans, increase fruits/vegetables, reduce sugar/carbohydrates, reduce fat/cholesterol, other micronutrient recommendations, and specific food items from multiple categories.
Physical activity advice consisted of 6 subcategories: walking, aerobic exercise, anaerobic exercise, exercise intensity, exercise duration, and exercise for comorbid conditions.
Specific weight loss advice consisted of 3 categories: weight loss behavior, weight loss for comorbid conditions, and referrals.
Nonspecific weight loss advice also consisted of 3 subcategories in which physicians provided no details about the general topics of nutrition, physical activity, or weight loss.
Two independent coders (CBT and MEC) assessed each piece of advice and double coded 20% of conversations for reliability. Cohen’s kappa was used to calculate inter-rater reliability for each code using Landis and Koch’s classification (0.21-0.40=fair agreement; 0.41-0.60=moderate agreement; 0.61-0.80=substantial agreement; 0.81-1.0=near-perfect agreement).10 Three advice categories achieved near perfect agreement: nutrition (kappa= 0.94; 95% confidence interval [CI] 0.82-1.0; 99.2% agreement), physical activity (kappa=0.91; 95% CI, 0.84-0.99; 98.6% agreement), and weight loss (kappa=0.95; 95% CI, 0.82-1.0; 99.7% agreement). The nonspecific weight loss advice category had slightly lower agreement but still achieved near-perfect agreement (kappa=0.82; 95% CI, 0.62-1.0; 99.2% agreement).
After all advice was coded, we placed conversations into 1 of 6 categories: (1) no advice given; (2) nonspecific advice only; (3) nutrition only; (4) physical activity only; (5) weight loss only; or (6) combination of nutrition, physical activity, and/or weight loss.
Measures
Dietary fat and fiber intake. We assessed dietary fat intake at baseline and at 3 months using the 22-item Fat- and Fiber-Related Diet Behavior Questionnaire.11,12 Questions about frequency of food selections included, “When you ate dessert, how often did you eat only fruit?” and “When you ate chicken, how often did you take off the skin?” We averaged responses into a total score wherein 1 reflected higher fiber, lower fat food choices; a score of 4 reflected lower fiber, higher fat choices (α=0.74 at baseline and α=0.77 at 3-month follow-up).
Physical activity. We measured physical activity (baseline, 3 months) using the Framingham Physical Activity Index.13 Participants recalled the average number of hours spent engaged in various daily activities (sleeping, working, leisure) and the level of activity for each (sedentary, slight, moderate, or heavy). The composite score accounts for activity duration and intensity.
Anthropometrics. We measured patient weight (baseline, 3 months) and height (baseline only) using a calibrated scale and portable stadiometer. Patients removed shoes, outerwear, and belongings from their pockets before being weighed.
Analysis
We analyzed data using SAS (SAS Institute, Inc., Cary, NC). We assessed the association between type of advice and weight loss, improvement in dietary fat intake behaviors, and increase in physical activity between baseline and the 3-month follow-up visit. We used PROC MIXED to fit general linear models; we incorporated responses into these models from all participants who provided measurements for at least one time point. This modeling framework yields unbiased estimates when missing data are unrelated to the observed variable.14
Primary predictors: (1) type of advice (none, nonspecific, nutrition, physical activity, weight loss, and combination), (2) time since baseline visit, and (3) time by type of advice interaction. All models included a priori defined patient, physician, and visit-related covariates that were theoretically or empirically related to changes in the outcomes (weight, physical activity, or dietary fat in-take). The 14 patient covariates were sex; age; race; high school education; economic security (enough money to pay monthly bills); over-weight (BMI, 25-29.9 kg/m2) or obese (BMI ≥30 kg/m2); actively trying to lose weight (yes/ no); motivated to lose weight (Likert scale 1-7); comfortable discussing weight (Likert scale 1-5); confident about losing weight (Likert scale 1-5); and patient-reported comorbid conditions of diabetes, hypertension, arthritis, and hyperlipidemia.
The 9 physician covariates were sex; race; years since medical school graduation; specialty (family vs internal medicine); self-efficacy (Likert scale 1-5); barriers for weight counseling (Likert scale 1-5); comfort discussing weight (Likert scale 1-5); insurance reimbursement concerns (Likert scale 1-5); and prior training in behavioral counseling (yes/no). Finally, 2 visit-level covariates were included: minutes spent addressing weight issues and visit type (preventive vs chronic).
Results
Sample characteristics
Of the 40 physicians, 19 were family physicians and 21 were internists. More than half of the physicians were female (60%), and 85% were white. Mean age was 47.2 years and mean BMI was 24.9 kg/m2. Of the 461 patients, 66% were female, 65% were white, 35% were African American, and two-thirds had post-high school education (TABLE 1). Mean patient age was 59.8 years; only 4% of the patients were new to their physicians.
TABLE 1
Patient characteristics (N=461)
| % or mean (SD) | |
|---|---|
| Race | |
| White/Asian/Pacific Islander | 65% |
| African American | 35% |
| Female | 66% |
| Age, y (missing=1)* | 59.8 (13.9) |
| BMI, kg/m2 (missing=1)* | 33.1 (7.1) |
| Education (missing=1)* | |
| Post-high school | 67% |
| Income (missing=37)* | |
| $45,000 or less | 48% |
| High financial burden (missing=13)* | |
| Pay bills with trouble | 14% |
| Diagnosed with: | |
| Diabetes | 31% |
| Hypertension (missing=1)* | 69% |
| Hyperlipidemia (missing=1)* | 56% |
| Arthritis | 47% |
| New patient | 4% |
| BMI, body mass index; SD, standard deviation. * Missing data at baseline. | |
Frequency of advice
Physicians gave some type of weight-related advice in 63% of the encounters. They combined types of advice in 34% of all conversations, provided physical activity advice only in 13%, nutrition advice only in 8%, nonspecific advice in 5%, and weight loss advice only in 3%. Many times when physicians gave advice, it was centered on self (eg, “I need you to do X” or “What will it take for me to get you to do Y?”).
Nutrition advice most commonly pertained to specific food items from multiple categories (27% of conversations). Physicians also advised patients to reduce sugar/carbohydrates, control calories and portions, add other micronutrients, eat more fruits/vegetables, and eat meals more frequently.
Walking was the physical activity topic discussed most frequently, followed by exercise duration, exercise for comorbidities, aerobic activities, exercise intensity, and anaerobic exercise. The most common specific weight loss topic was weight loss behavioral advice, followed by weight loss for comorbid conditions. Physicians rarely provided referrals to weight-loss programs.
Effect of type of advice on fat and fiber diet behavior score
Receipt of nutrition advice only was not associated with reduction in fat intake (P=.43, TABLE 2). However, those who received combined types of advice exhibited a significantly greater reduction of fat intake compared with those who received no advice (Fat- and Fiber-Related Diet Behavior Questionnaire score reduction of 0.15 vs 0.05; P=.02).
TABLE 2
How types of physician advice affected dietary fat intake, physical activity, and weight
| Type of advice | ||||||
|---|---|---|---|---|---|---|
| None | Nutrition only | Physical activity only | Weight loss only | Combined advice | Nonspecific | |
| Dietary fat change in Fat- and Fiber-Related Diet Behavior Questionnaire score differences | ||||||
| At 3 months from baseline (95% CI) | -0.05 (-0.11 to 0.004) | -0.10 (-0.22 to 0.01) | -0.07 (-0.16 to 0.02) | -0.08 (-0.26 to 0.09) | -0.15 (-0.20 to -0.09) | 0.03 (0.11 to 0.18) |
| P value* | .43 | .75 | .73 | .02 | .31 | |
| Physical activity score (change in MET hours) | ||||||
| At 3 months from baseline (95% CI) | 0.48 (-0.17 to 1.11) | 0.83 (-0.51 to 2.14) | 0.69 (-0.33 to 1.69) | -0.72 (-2.66 to 1.21) | 0.24 (-0.40 to 0.86) | -0.07 (-1.74 to 1.59) |
| P value* | .64 | .73 | .25 | .60 | .55 | |
| Weight change (kg) | ||||||
| At 3 months from baseline (95% CI) | -0.18 (-0.39 to 0.75) | -0.18 (-1.38 to 1.02) | 1.41 (0.51 to 2.31) | -0.26 (-1.99 to 1.47) | -0.55 (-1.12 to 0.02) | -0.62 (-2.11 to 0.87) |
| P value* | .59 | .02 | .63 | .08 | .32 | |
| CI, confidence interval; MET, metabolic equivalent tasks. *Test of difference between advice given and no advice given. | ||||||
Effect of type of advice on Framingham Physical Activity score
No type of advice, including physical activity advice, led to a change in Framingham Physical Activity scores at the 3-month visit (overall P=.76; TABLE 2).
Effect of type of advice on weight loss
Patients who received physical activity advice gained significantly more weight than patients who received no advice (1.41 kg gained vs 0.18 kg lost; P=.02). Patients who received combined advice lost more weight than patients who received no advice, but the difference did not reach statistical significance (0.55 kg lost vs 0.18 kg lost; P=.08).
Discussion
Physicians typically took an “all or nothing” approach to weight-related issues, giving no advice (37%) or a combination of nutrition, physical activity, and weight loss advice (34%). It seems when physicians do give advice, most of them follow the USPSTF guidelines by addressing nutrition and physical activity together.15
Providing advice alone did not predict a change in patient behavior. For instance, we found no significant association between dietary fat reduction and having received only nutrition advice. Possible explanations include the following:
- Although physicians advised patients to reduce fat/cholesterol intake in 28% of conversations, they did so mostly in combination with other types of advice. Nutrition-only advice occurred in only 8% of conversations. Thus, there may have been insufficient power to detect the impact of this specific type of advice.
- With nutrition-only advice, the most common recommendation was to reduce carbohydrates/sweets, which should not affect fat intake.
Advising patients solely on physical activity led to unintended weight gain overall. Other data have shown that exercise without dietary changes, though beneficial in many ways, is not substantially effective for weight loss.15 People may eat more when they exercise, either to reward themselves or to satiate increased appetite from increased energy expenditure. Or, if physicians recommend the standard goal of 150 minutes of intensive physical activity per week, normally sedentary patients may see that as unattainable and become too discouraged to try.1,16,17
Combining types of advice seemed to help patients reduce their fat intake. Overall, however, simple, brief advice from a physician may not be enough to promote healthy lifestyle changes.
Also notable was that physicians rarely provided referrals, even though this is a strong recommendation from the National Institutes of Health, the American Diabetes Association, and the USPSTF.1,16,17 It could be that many physicians believe referrals are not covered by insurance. Yet, the low frequency of referrals may suggest an important missing component of weight loss therapy, especially given that physician advice alone seems an inadequate intervention.
Avoid physician-centered appeals. Advice was often given in a physician-centered way. There are 3 possible explanations for such phrasing:
- In the absence of clear evidence about how to deliver weight loss advice, physicians may be formulating advice based on their personal or clinical experiences.
- Physicians either assume or sense that patients lack internal motivation to make lifestyle changes for themselves and instead request that patients make changes for the doctor-patient relationship.
- Physicians might be trying to invoke authority in the hope that patients will respond accordingly.
Whatever the reason, the literature on self-centered physician talk indicates that patients are less satisfied when physicians make the visit more about themselves than about patients.18 A better strategy might be to use Motivational Interviewing19 that supports patient autonomy and attempts to elicit and build on internal motivation.
The take-away message is that behavior change is complex and that knowledge is a necessary but insufficient agent for change. Following the tenets of Social Cognitive Theory,20 physicians might also need to address patient motivation, confidence, outcome expectations, and skills to help promote behavior change.
Strengths and limitations of this study
We recorded conversations rather than relying on physician or patient recall. Additionally, these primary care patients were not enrolled in a weight-loss trial and, therefore, were not self-selected to be highly motivated to lose weight. Because of this, and the large and ethnically diverse sample, our results should be generalizable to many clinical settings.
One limitation is that few younger, lower-income patients were included in the sample, which limits generalizability to those populations. Also, the study was observational. Although we adjusted for a broad set of patient, physician, and visit covariates, unmeasured confounding variables may still account for at least part of the observed associations. The analysis is limited by the use of self-reported dietary fat intake and physical activity measures. A food diary and accelerometer would have been more accurate; however, such involved measures could invoke changes in behavior, which would have confounded our ability to assess the effect of physician advice on weight loss.
Acknowledgements
The authors thank all of the physicians and patients who participated in this study, the study project managers Gretchen Yonish and Iguehi Esoimeme, and research assistant Justin Manusov.
CORRESPONDENCE
Stewart C. Alexander, PhD, Department of Medicine, Duke University School of Medicine, P.O. Box 3140 Medical Center, Durham, NC 27710; alexa045@mc.duke.edu
1. US Preventive Services Task Force. Screening for obesity in adults: recommendations and rationale. Ann Intern Med. 2003;139:930-932.
2. Nawaz H, Adams ML, Katz DL. Physician-patient interactions regarding diet, exercise, and smoking. Prev Med. 2000;31:652-657.
3. Sciamanna CN, Tate DF, Lang W, et al. Who reports receiving advice to lose weight? Results from a multistate survey. Arch Intern Med. 2000;160:2334-2339.
4. Galuska DA, Will JC, Serdula MK, et al. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282:1576-1578.
5. Evans E. Why should obesity be managed? The obese individual’s perspective. Int J Obes Relat Metab Disord. 1999;23(suppl 4):S3-S6.
6. Mehrotra C, Naimi TS, Serdula M, et al. Arthritis, body mass index, and professional advice to lose weight: implications for clinical medicine and public health. Am J Prev Med. 2004;27:16-21.
7. Loureiro ML, Nayga RM Jr. Obesity, weight loss, and physician’s advice. Soc Sci Med. 2006;62:2458-2468.
8. Flocke SA, Clark A, Schlessman K, et al. Exercise, diet, and weight loss advice in the family medicine outpatient setting. Fam Med. 2005;37:415-421.
9. Alexander SC, Cox ME, Østbye T, et al. Do the 5 A’s work for weight-loss counseling? Presented at: International Conference on Communication in Healthcare; October 4–7, 2009; Miami, Fla.
10. McGinn T, Wyer PC, Newman TB, et al. Tips for learners of evidence-based medicine: 3. Measures of observer variability (kappa statistic). CMAJ. 2004;171:1369-1373.
11. Shannon J, Kristal AR, Curry SJ, et al. Application of a behavioral approach to measuring dietary change: the fat- and fiber-related diet behavior questionnaire. Cancer Epidemiol Biomarkers Prev. 1997;6:355-361.
12. Kristal AR, Shattuck AL, Henry HJ. Patterns of dietary behavior associated with selecting diets low in fat: reliability and validity of a behavioral approach to dietary assessment. J Am Diet Assoc. 1990;90:214-220.
13. Kannel WB, Sorlie P. Some health benefits of physical activity: the Framingham study. Arch Intern Med. 1979;139:857-861.
14. Little RJA, Rubin DB. Statistical Analysis With Missing Data. New York, NY: John Wiley & Sons; 2002.
15. Franz MJ, VanWormer JJ, Crain AL, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755-1767.
16. National Institutes of Health. The practical guide: identification, evaluation, and treatment of overweight and obesity in adults. NIH publication 00-4084. 2000. Available at: http://www.nhlbi.nih.gov/guidelines/obesity/prctgd_c.pdf. Accessed August 17, 2009.
17. American Diabetes Association. Standards of medical care in diabetes–2010. Diabetes Care. 2010;33(suppl 1):S11-S61.
18. Beach MC, Roter DL. Interpersonal expectations in the patient-physician relationship. J Gen Intern Med. 2000;15:825-827.
19. Miller WR, Rollnick SP, Miller WR. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford Press; 2002.
20. Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.
1. US Preventive Services Task Force. Screening for obesity in adults: recommendations and rationale. Ann Intern Med. 2003;139:930-932.
2. Nawaz H, Adams ML, Katz DL. Physician-patient interactions regarding diet, exercise, and smoking. Prev Med. 2000;31:652-657.
3. Sciamanna CN, Tate DF, Lang W, et al. Who reports receiving advice to lose weight? Results from a multistate survey. Arch Intern Med. 2000;160:2334-2339.
4. Galuska DA, Will JC, Serdula MK, et al. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282:1576-1578.
5. Evans E. Why should obesity be managed? The obese individual’s perspective. Int J Obes Relat Metab Disord. 1999;23(suppl 4):S3-S6.
6. Mehrotra C, Naimi TS, Serdula M, et al. Arthritis, body mass index, and professional advice to lose weight: implications for clinical medicine and public health. Am J Prev Med. 2004;27:16-21.
7. Loureiro ML, Nayga RM Jr. Obesity, weight loss, and physician’s advice. Soc Sci Med. 2006;62:2458-2468.
8. Flocke SA, Clark A, Schlessman K, et al. Exercise, diet, and weight loss advice in the family medicine outpatient setting. Fam Med. 2005;37:415-421.
9. Alexander SC, Cox ME, Østbye T, et al. Do the 5 A’s work for weight-loss counseling? Presented at: International Conference on Communication in Healthcare; October 4–7, 2009; Miami, Fla.
10. McGinn T, Wyer PC, Newman TB, et al. Tips for learners of evidence-based medicine: 3. Measures of observer variability (kappa statistic). CMAJ. 2004;171:1369-1373.
11. Shannon J, Kristal AR, Curry SJ, et al. Application of a behavioral approach to measuring dietary change: the fat- and fiber-related diet behavior questionnaire. Cancer Epidemiol Biomarkers Prev. 1997;6:355-361.
12. Kristal AR, Shattuck AL, Henry HJ. Patterns of dietary behavior associated with selecting diets low in fat: reliability and validity of a behavioral approach to dietary assessment. J Am Diet Assoc. 1990;90:214-220.
13. Kannel WB, Sorlie P. Some health benefits of physical activity: the Framingham study. Arch Intern Med. 1979;139:857-861.
14. Little RJA, Rubin DB. Statistical Analysis With Missing Data. New York, NY: John Wiley & Sons; 2002.
15. Franz MJ, VanWormer JJ, Crain AL, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755-1767.
16. National Institutes of Health. The practical guide: identification, evaluation, and treatment of overweight and obesity in adults. NIH publication 00-4084. 2000. Available at: http://www.nhlbi.nih.gov/guidelines/obesity/prctgd_c.pdf. Accessed August 17, 2009.
17. American Diabetes Association. Standards of medical care in diabetes–2010. Diabetes Care. 2010;33(suppl 1):S11-S61.
18. Beach MC, Roter DL. Interpersonal expectations in the patient-physician relationship. J Gen Intern Med. 2000;15:825-827.
19. Miller WR, Rollnick SP, Miller WR. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford Press; 2002.
20. Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.