User login
RT + ADT linked with improved survival in mPC
The addition of radiotherapy (RT) to androgen deprivation therapy (ADT) appears to boost overall survival in men with metastatic prostate cancer. However, it is more common for men to receive ADT alone than ADT plus RT.
“In this large contemporary analysis, men receiving prostate RT plus ADT lived substantially longer than men treated with ADT alone,” noted Dr. Chad Rusthoven of the University of Colorado, Aurora, and his associates (J Clin Oncol. 2016 June doi: 10.1200/JCO.2016.67.4788).
Investigators reviewed the National Cancer Data Base and identified 6,382 men with metastatic prostate cancer who received ADT as first-line therapy. Of those men, 5,844 (91.6%) received ADT alone, and the remaining 538 (8.4%) men received ADT plus prostate RT. The median age of the study population was 69, 75% were white, the most common T stage was T2, N0 was the most common N stage, and 6% of the entire cohort received chemotherapy. The median follow-up time was 5.1 years, and the median time from diagnosis to initiation of RT was 101 days. Patients were excluded from the study if they died within a month of diagnosis or if they were receiving prostatectomy, cryotherapy, or brachytherapy.
Among men receiving ADT plus RT, 48% were on Medicare and 41% were privately insured. Among men receiving ADT alone, 56% were on Medicare and 27% were privately insured.
Univariate analysis revealed that, compared with ADT alone, RT plus ADT was associated with longer median overall survival (29 vs. 53 months) as well as improved 3-year (43% vs. 62%), 5-year (25% vs. 49%), and 8-year (13% vs. 33%) overall survival estimates.
Multivariate analysis also found an independent association between the addition of radiotherapy with improved overall survival (HR, 0.624; 95% confidence interval, 0.551-0.706; P less than .001). In addition, RT to the prostate only and RT to the prostate and pelvis were both associated with longer overall survival times compared with ADT alone.
The funding source for this study was not listed. Six investigators reported serving in advisory roles for, receiving honoraria or financial compensation from, or holding patents in accordance with multiple companies.
On Twitter @jessnicolecraig
The addition of radiotherapy (RT) to androgen deprivation therapy (ADT) appears to boost overall survival in men with metastatic prostate cancer. However, it is more common for men to receive ADT alone than ADT plus RT.
“In this large contemporary analysis, men receiving prostate RT plus ADT lived substantially longer than men treated with ADT alone,” noted Dr. Chad Rusthoven of the University of Colorado, Aurora, and his associates (J Clin Oncol. 2016 June doi: 10.1200/JCO.2016.67.4788).
Investigators reviewed the National Cancer Data Base and identified 6,382 men with metastatic prostate cancer who received ADT as first-line therapy. Of those men, 5,844 (91.6%) received ADT alone, and the remaining 538 (8.4%) men received ADT plus prostate RT. The median age of the study population was 69, 75% were white, the most common T stage was T2, N0 was the most common N stage, and 6% of the entire cohort received chemotherapy. The median follow-up time was 5.1 years, and the median time from diagnosis to initiation of RT was 101 days. Patients were excluded from the study if they died within a month of diagnosis or if they were receiving prostatectomy, cryotherapy, or brachytherapy.
Among men receiving ADT plus RT, 48% were on Medicare and 41% were privately insured. Among men receiving ADT alone, 56% were on Medicare and 27% were privately insured.
Univariate analysis revealed that, compared with ADT alone, RT plus ADT was associated with longer median overall survival (29 vs. 53 months) as well as improved 3-year (43% vs. 62%), 5-year (25% vs. 49%), and 8-year (13% vs. 33%) overall survival estimates.
Multivariate analysis also found an independent association between the addition of radiotherapy with improved overall survival (HR, 0.624; 95% confidence interval, 0.551-0.706; P less than .001). In addition, RT to the prostate only and RT to the prostate and pelvis were both associated with longer overall survival times compared with ADT alone.
The funding source for this study was not listed. Six investigators reported serving in advisory roles for, receiving honoraria or financial compensation from, or holding patents in accordance with multiple companies.
On Twitter @jessnicolecraig
The addition of radiotherapy (RT) to androgen deprivation therapy (ADT) appears to boost overall survival in men with metastatic prostate cancer. However, it is more common for men to receive ADT alone than ADT plus RT.
“In this large contemporary analysis, men receiving prostate RT plus ADT lived substantially longer than men treated with ADT alone,” noted Dr. Chad Rusthoven of the University of Colorado, Aurora, and his associates (J Clin Oncol. 2016 June doi: 10.1200/JCO.2016.67.4788).
Investigators reviewed the National Cancer Data Base and identified 6,382 men with metastatic prostate cancer who received ADT as first-line therapy. Of those men, 5,844 (91.6%) received ADT alone, and the remaining 538 (8.4%) men received ADT plus prostate RT. The median age of the study population was 69, 75% were white, the most common T stage was T2, N0 was the most common N stage, and 6% of the entire cohort received chemotherapy. The median follow-up time was 5.1 years, and the median time from diagnosis to initiation of RT was 101 days. Patients were excluded from the study if they died within a month of diagnosis or if they were receiving prostatectomy, cryotherapy, or brachytherapy.
Among men receiving ADT plus RT, 48% were on Medicare and 41% were privately insured. Among men receiving ADT alone, 56% were on Medicare and 27% were privately insured.
Univariate analysis revealed that, compared with ADT alone, RT plus ADT was associated with longer median overall survival (29 vs. 53 months) as well as improved 3-year (43% vs. 62%), 5-year (25% vs. 49%), and 8-year (13% vs. 33%) overall survival estimates.
Multivariate analysis also found an independent association between the addition of radiotherapy with improved overall survival (HR, 0.624; 95% confidence interval, 0.551-0.706; P less than .001). In addition, RT to the prostate only and RT to the prostate and pelvis were both associated with longer overall survival times compared with ADT alone.
The funding source for this study was not listed. Six investigators reported serving in advisory roles for, receiving honoraria or financial compensation from, or holding patents in accordance with multiple companies.
On Twitter @jessnicolecraig
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: The addition of radiotherapy (RT) to androgen deprivation therapy (ADT) was associated with improved survival in men with prostate cancer.
Major finding: The addition of radiotherapy to androgen deprivation therapy was independently associated with improved overall survival (HR, 0.624; 95% confidence interval, 0.551-0.706; P less than .001).
Data source: A review of the National Cancer Data Base on 6,382 men with metastatic prostate cancer.
Disclosures: The funding source for this study was not listed. Six investigators reported serving in advisory roles for, receiving honoraria or financial compensation from, or holding patents in accordance with multiple companies.
FDA reports shortage of doxorubicin for injection, initiates importation
A critical shortage of doxorubicin hydrochloride 50 mg powder for injection has been reported to the Food and Drug Administration.
Doxorubicin is approved to treat acute lymphoblastic leukemia, acute myeloid leukemia, breast cancer, gastric cancer, ovarian cancer, neuroblastoma, and other cancer types.
To increase availability, the pharmaceutical company Hospira (a Pfizer company) is coordinating with the FDA to import the drug from Ahmedabad, India, where it is manufactured by Zydus Hospira Oncology Private Ltd. at an FDA-inspected facility that is in compliance with current good manufacturing practice requirements.
“It is important to note that there are substantive differences in the format and content of the labeling between the U.S.-approved doxorubicin hydrochloride for injection, USP and the Hospira Limited’s doxorubicin hydrochloride 50 mg powder for injection,” Hospira reported in a letter to health care providers.
To place an order or to get questions answered, contact Hospira directly by calling customer care at 1-877-946-7747 (Mondays-Fridays, 7 a.m.-6 p.m. Central time).
For clinical inquiries, contact Hospira Medical Communications at 1-800-615-0187 or email medcom@hospira.com.
According to the letter, adverse events or quality problems associated with use of this product should be reported by calling Hospira Global Complaint Management by phone, 1-800-441-4100; by sending an email to ProductComplaintsPP@hospira.com; or by submitting a report online to Medwatch.
On Twitter @jessnicolecraig
A critical shortage of doxorubicin hydrochloride 50 mg powder for injection has been reported to the Food and Drug Administration.
Doxorubicin is approved to treat acute lymphoblastic leukemia, acute myeloid leukemia, breast cancer, gastric cancer, ovarian cancer, neuroblastoma, and other cancer types.
To increase availability, the pharmaceutical company Hospira (a Pfizer company) is coordinating with the FDA to import the drug from Ahmedabad, India, where it is manufactured by Zydus Hospira Oncology Private Ltd. at an FDA-inspected facility that is in compliance with current good manufacturing practice requirements.
“It is important to note that there are substantive differences in the format and content of the labeling between the U.S.-approved doxorubicin hydrochloride for injection, USP and the Hospira Limited’s doxorubicin hydrochloride 50 mg powder for injection,” Hospira reported in a letter to health care providers.
To place an order or to get questions answered, contact Hospira directly by calling customer care at 1-877-946-7747 (Mondays-Fridays, 7 a.m.-6 p.m. Central time).
For clinical inquiries, contact Hospira Medical Communications at 1-800-615-0187 or email medcom@hospira.com.
According to the letter, adverse events or quality problems associated with use of this product should be reported by calling Hospira Global Complaint Management by phone, 1-800-441-4100; by sending an email to ProductComplaintsPP@hospira.com; or by submitting a report online to Medwatch.
On Twitter @jessnicolecraig
A critical shortage of doxorubicin hydrochloride 50 mg powder for injection has been reported to the Food and Drug Administration.
Doxorubicin is approved to treat acute lymphoblastic leukemia, acute myeloid leukemia, breast cancer, gastric cancer, ovarian cancer, neuroblastoma, and other cancer types.
To increase availability, the pharmaceutical company Hospira (a Pfizer company) is coordinating with the FDA to import the drug from Ahmedabad, India, where it is manufactured by Zydus Hospira Oncology Private Ltd. at an FDA-inspected facility that is in compliance with current good manufacturing practice requirements.
“It is important to note that there are substantive differences in the format and content of the labeling between the U.S.-approved doxorubicin hydrochloride for injection, USP and the Hospira Limited’s doxorubicin hydrochloride 50 mg powder for injection,” Hospira reported in a letter to health care providers.
To place an order or to get questions answered, contact Hospira directly by calling customer care at 1-877-946-7747 (Mondays-Fridays, 7 a.m.-6 p.m. Central time).
For clinical inquiries, contact Hospira Medical Communications at 1-800-615-0187 or email medcom@hospira.com.
According to the letter, adverse events or quality problems associated with use of this product should be reported by calling Hospira Global Complaint Management by phone, 1-800-441-4100; by sending an email to ProductComplaintsPP@hospira.com; or by submitting a report online to Medwatch.
On Twitter @jessnicolecraig
In-person, telephone genetic counseling yield similar outcomes
Genetic counseling by telephone was noninferior to in-person counseling among women at increased risk of hereditary breast and/or ovarian cancer (HBOC) for all psychosocial, decision-making, and quality-of-life measures, investigators found.
In addition, genetic testing was more common among women who received in-person counseling and women who lived in rural settings.
“This trial provides important evidence that telephone genetic counseling for HBOC is noninferior to in-person counseling and can be delivered as safely as in-person counseling without an adverse effect on long-term psychological, quality-of-life, and decision-making outcomes,” according to Anita Kinney, Ph.D., of the University of New Mexico, Albuquerque, and her associates (J Clin Oncol. 2016 Jun. doi: 10.1200/JCO.2015.65.9557).
Investigators used the Utah Population Database and Utah Cancer Registry to identify breast and ovarian cancer survivors and their at-risk female relatives with deleterious BRCA 1/2 mutations. Of the 988 women who met study requirements, 495 were randomly assigned to receive in-person genetic counseling, and 493 women were assigned to receive genetic counseling via telephone. All patients received counseling by a certified cancer genetic counselor according to standardized national protocols. Importantly, there were no significant differences in age, race/ethnicity, marital status, education level, rural vs. urban residence, income, employment status or health care coverage between the two study arms.
At the 1-year follow-up, there was no significant difference between patients receiving in-person or telephone counseling for all psychosocial and informed decision-making outcomes which included anxiety (average brief symptom inventory scores, 2.37 vs. 2.74), cancer-specific distress (average impact of event scores, 10.06 vs. 11.19), quality-of-life for physical health (average short form health survey scores, 50.54 vs. 49.75), quality-of-life for mental health (50.51 vs. 50.74), decisional conflict (average decisional conflict score, 26.88 vs. 26.76), decisional regret (average decision regret score, 21.38 vs. 21.07), and perceived personal control (average questionnaire scores, 1.53 vs. 1.52).
Genetic testing was more common among women who received in-person counseling (37.3% vs. 27.9%; 95% confidence interval comparing difference in testing uptake, 2.2%-16.8%). Interestingly, testing was higher for rural, compared with urban residents, for both telephone and in-person counseling.
This study received funding from the National Institutes of Health, the Huntsman Cancer Foundation, the University of New Mexico Comprehensive Cancer Center, and the University of Utah. Twelve of the investigators had no disclosures to report. Two investigators reported serving in advisory roles or receiving honoraria from Myriad Genetics or In Vitae.
On Twitter @jessnicolecraig
Genetic counseling by telephone was noninferior to in-person counseling among women at increased risk of hereditary breast and/or ovarian cancer (HBOC) for all psychosocial, decision-making, and quality-of-life measures, investigators found.
In addition, genetic testing was more common among women who received in-person counseling and women who lived in rural settings.
“This trial provides important evidence that telephone genetic counseling for HBOC is noninferior to in-person counseling and can be delivered as safely as in-person counseling without an adverse effect on long-term psychological, quality-of-life, and decision-making outcomes,” according to Anita Kinney, Ph.D., of the University of New Mexico, Albuquerque, and her associates (J Clin Oncol. 2016 Jun. doi: 10.1200/JCO.2015.65.9557).
Investigators used the Utah Population Database and Utah Cancer Registry to identify breast and ovarian cancer survivors and their at-risk female relatives with deleterious BRCA 1/2 mutations. Of the 988 women who met study requirements, 495 were randomly assigned to receive in-person genetic counseling, and 493 women were assigned to receive genetic counseling via telephone. All patients received counseling by a certified cancer genetic counselor according to standardized national protocols. Importantly, there were no significant differences in age, race/ethnicity, marital status, education level, rural vs. urban residence, income, employment status or health care coverage between the two study arms.
At the 1-year follow-up, there was no significant difference between patients receiving in-person or telephone counseling for all psychosocial and informed decision-making outcomes which included anxiety (average brief symptom inventory scores, 2.37 vs. 2.74), cancer-specific distress (average impact of event scores, 10.06 vs. 11.19), quality-of-life for physical health (average short form health survey scores, 50.54 vs. 49.75), quality-of-life for mental health (50.51 vs. 50.74), decisional conflict (average decisional conflict score, 26.88 vs. 26.76), decisional regret (average decision regret score, 21.38 vs. 21.07), and perceived personal control (average questionnaire scores, 1.53 vs. 1.52).
Genetic testing was more common among women who received in-person counseling (37.3% vs. 27.9%; 95% confidence interval comparing difference in testing uptake, 2.2%-16.8%). Interestingly, testing was higher for rural, compared with urban residents, for both telephone and in-person counseling.
This study received funding from the National Institutes of Health, the Huntsman Cancer Foundation, the University of New Mexico Comprehensive Cancer Center, and the University of Utah. Twelve of the investigators had no disclosures to report. Two investigators reported serving in advisory roles or receiving honoraria from Myriad Genetics or In Vitae.
On Twitter @jessnicolecraig
Genetic counseling by telephone was noninferior to in-person counseling among women at increased risk of hereditary breast and/or ovarian cancer (HBOC) for all psychosocial, decision-making, and quality-of-life measures, investigators found.
In addition, genetic testing was more common among women who received in-person counseling and women who lived in rural settings.
“This trial provides important evidence that telephone genetic counseling for HBOC is noninferior to in-person counseling and can be delivered as safely as in-person counseling without an adverse effect on long-term psychological, quality-of-life, and decision-making outcomes,” according to Anita Kinney, Ph.D., of the University of New Mexico, Albuquerque, and her associates (J Clin Oncol. 2016 Jun. doi: 10.1200/JCO.2015.65.9557).
Investigators used the Utah Population Database and Utah Cancer Registry to identify breast and ovarian cancer survivors and their at-risk female relatives with deleterious BRCA 1/2 mutations. Of the 988 women who met study requirements, 495 were randomly assigned to receive in-person genetic counseling, and 493 women were assigned to receive genetic counseling via telephone. All patients received counseling by a certified cancer genetic counselor according to standardized national protocols. Importantly, there were no significant differences in age, race/ethnicity, marital status, education level, rural vs. urban residence, income, employment status or health care coverage between the two study arms.
At the 1-year follow-up, there was no significant difference between patients receiving in-person or telephone counseling for all psychosocial and informed decision-making outcomes which included anxiety (average brief symptom inventory scores, 2.37 vs. 2.74), cancer-specific distress (average impact of event scores, 10.06 vs. 11.19), quality-of-life for physical health (average short form health survey scores, 50.54 vs. 49.75), quality-of-life for mental health (50.51 vs. 50.74), decisional conflict (average decisional conflict score, 26.88 vs. 26.76), decisional regret (average decision regret score, 21.38 vs. 21.07), and perceived personal control (average questionnaire scores, 1.53 vs. 1.52).
Genetic testing was more common among women who received in-person counseling (37.3% vs. 27.9%; 95% confidence interval comparing difference in testing uptake, 2.2%-16.8%). Interestingly, testing was higher for rural, compared with urban residents, for both telephone and in-person counseling.
This study received funding from the National Institutes of Health, the Huntsman Cancer Foundation, the University of New Mexico Comprehensive Cancer Center, and the University of Utah. Twelve of the investigators had no disclosures to report. Two investigators reported serving in advisory roles or receiving honoraria from Myriad Genetics or In Vitae.
On Twitter @jessnicolecraig
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Telephone genetic counseling was noninferior to in-person counseling for women at increased risk of hereditary breast and/or ovarian cancer.
Major finding: Anxiety, cancer-specific distress, quality-of-life for physical and mental health, decisional conflict, decisional regret, and perceived personal control measures were not significantly different between the two study arms.
Data source: A randomized noninferiority trial of 988 women at increased risk of hereditary breast and/or ovarian cancer.
Disclosures: This study received funding from the National Institutes of Health, the Huntsman Cancer Foundation, the University of New Mexico Comprehensive Cancer Center, and the University of Utah. Twelve of the investigators had no disclosures to report. Two investigators reported serving in advisory roles or receiving honoraria from Myriad Genetics or In Vitae.
Early results promising for pembrolizumab in combination regimens for NSCLC
CHICAGO – Overall response rates ranged from 48% to 71% when pembrolizumab was added to chemotherapy combinations in patients with advanced non–small cell lung cancer (NSCLC), and close to 30% when added to an R2 inhibitor in patients with advanced NSCLC and other tumor types, according to two early phase clinical trials presented at the annual meeting of the American Society of Clinical Oncology.
Safety and efficacy of pembrolizumab in combination with either carboplatin and paclitaxel; carboplatin, paclitaxel, and bevacizumab; or carboplatin and pemetrexed were evaluated in the KEYNOTE-021 trial. Patients were split between two doses of pembrolizumab: 2 or 10 mg/kg every 3 weeks. The overall response rate for the entire cohort of 74 patients with advanced NSCLC was 57% (95% confidence interval, 45-68), reported Dr. Shirish Gadgeel of Karmanos Cancer Institute, Detroit.
For the 25 patients who received pembrolizumab, carboplatin, and paclitaxel (cohort A) the overall response was 52% (95% CI, 31-72). For the 25 patients who also received bevacizumab in addition to pembrolizumab, carboplatin, and paclitaxel (cohort B), the overall response rate was 48% (95% CI, 28-69).
Among 24 patients who received pemetrexed with pembrolizumab and carboplatin (cohort C), the overall response was the highest at 71% (95% CI, 49-87).
Grade 3 or 4 adverse events occurred in 36%, 46%, and 42% of patients in cohort A, B, and C, respectively. The most common adverse events were anemia and neutropenia including febrile neutropenia.
“Pembro in combination with standard chemotherapy regimens is feasible and yields substantial clinical efficacy regardless of pembro dose or PD-L1 status in treatment-naïve advanced NSCLC,” Dr Gadgeel said.
A randomized phase III study evaluating pemetrexed/platinum with or without pembrolizumab is currently recruiting, he said.
These combinations, while perhaps better than chemotherapy alone, may be no better than just immunotherapy alone, session moderator Dr. Scott Antonia of the Moffitt Cancer Center, Tampa, Fla., commented. “And the truth is that concurrent therapy is clearly more toxic.”
In another study presented at the meeting, led by Dr. Roy Herbst of Yale Cancer Center, New Haven, Conn., pembrolizumab was combined with ramucirumab, a recently approved vascular endothelial growth factor receptor–2 inhibitor. “Hallmarks of tumor growth include angiogenesis and immunosuppression,” Dr. Herbst and his coauthors wrote in their abstract, noting that this was the first study to combine these agents to target both processes simultaneously.
“The idea is the R2 inhibitor might have an effect on the microimmune environment and drive T cells into the tumor,” Dr. Herbst said.
The study cohort included patients with advanced gastric or gastroesophageal junction adenocarcinoma, NSCLC, and urothelial carcinoma.
Overall, the response rate was close to 30% in the first 10 patients, Dr. Herbst reported. Furthermore, the preliminary data did not reveal any unexpected safety signals.
Although the data was from a small, ongoing phase I trial, Dr. Herbst noted the data is promising. Researchers are continuing to collect data on the safety profile of this drug combination, and are planning to enroll patients with additional tumor types.
The KEYNOTE-021 trial was funded by Merck Sharp and Dohme. Dr. Gadgeel reported having a consulting or advisory role and receiving research funding from multiple companies. The trial headed by Dr. Herbst was funded by Eli Lilly. Dr. Herbst reported having a consulting or advisory role and receiving honoraria and research funding from multiple companies including Eli Lilly.
On Twitter @jessnicolecraig
CHICAGO – Overall response rates ranged from 48% to 71% when pembrolizumab was added to chemotherapy combinations in patients with advanced non–small cell lung cancer (NSCLC), and close to 30% when added to an R2 inhibitor in patients with advanced NSCLC and other tumor types, according to two early phase clinical trials presented at the annual meeting of the American Society of Clinical Oncology.
Safety and efficacy of pembrolizumab in combination with either carboplatin and paclitaxel; carboplatin, paclitaxel, and bevacizumab; or carboplatin and pemetrexed were evaluated in the KEYNOTE-021 trial. Patients were split between two doses of pembrolizumab: 2 or 10 mg/kg every 3 weeks. The overall response rate for the entire cohort of 74 patients with advanced NSCLC was 57% (95% confidence interval, 45-68), reported Dr. Shirish Gadgeel of Karmanos Cancer Institute, Detroit.
For the 25 patients who received pembrolizumab, carboplatin, and paclitaxel (cohort A) the overall response was 52% (95% CI, 31-72). For the 25 patients who also received bevacizumab in addition to pembrolizumab, carboplatin, and paclitaxel (cohort B), the overall response rate was 48% (95% CI, 28-69).
Among 24 patients who received pemetrexed with pembrolizumab and carboplatin (cohort C), the overall response was the highest at 71% (95% CI, 49-87).
Grade 3 or 4 adverse events occurred in 36%, 46%, and 42% of patients in cohort A, B, and C, respectively. The most common adverse events were anemia and neutropenia including febrile neutropenia.
“Pembro in combination with standard chemotherapy regimens is feasible and yields substantial clinical efficacy regardless of pembro dose or PD-L1 status in treatment-naïve advanced NSCLC,” Dr Gadgeel said.
A randomized phase III study evaluating pemetrexed/platinum with or without pembrolizumab is currently recruiting, he said.
These combinations, while perhaps better than chemotherapy alone, may be no better than just immunotherapy alone, session moderator Dr. Scott Antonia of the Moffitt Cancer Center, Tampa, Fla., commented. “And the truth is that concurrent therapy is clearly more toxic.”
In another study presented at the meeting, led by Dr. Roy Herbst of Yale Cancer Center, New Haven, Conn., pembrolizumab was combined with ramucirumab, a recently approved vascular endothelial growth factor receptor–2 inhibitor. “Hallmarks of tumor growth include angiogenesis and immunosuppression,” Dr. Herbst and his coauthors wrote in their abstract, noting that this was the first study to combine these agents to target both processes simultaneously.
“The idea is the R2 inhibitor might have an effect on the microimmune environment and drive T cells into the tumor,” Dr. Herbst said.
The study cohort included patients with advanced gastric or gastroesophageal junction adenocarcinoma, NSCLC, and urothelial carcinoma.
Overall, the response rate was close to 30% in the first 10 patients, Dr. Herbst reported. Furthermore, the preliminary data did not reveal any unexpected safety signals.
Although the data was from a small, ongoing phase I trial, Dr. Herbst noted the data is promising. Researchers are continuing to collect data on the safety profile of this drug combination, and are planning to enroll patients with additional tumor types.
The KEYNOTE-021 trial was funded by Merck Sharp and Dohme. Dr. Gadgeel reported having a consulting or advisory role and receiving research funding from multiple companies. The trial headed by Dr. Herbst was funded by Eli Lilly. Dr. Herbst reported having a consulting or advisory role and receiving honoraria and research funding from multiple companies including Eli Lilly.
On Twitter @jessnicolecraig
CHICAGO – Overall response rates ranged from 48% to 71% when pembrolizumab was added to chemotherapy combinations in patients with advanced non–small cell lung cancer (NSCLC), and close to 30% when added to an R2 inhibitor in patients with advanced NSCLC and other tumor types, according to two early phase clinical trials presented at the annual meeting of the American Society of Clinical Oncology.
Safety and efficacy of pembrolizumab in combination with either carboplatin and paclitaxel; carboplatin, paclitaxel, and bevacizumab; or carboplatin and pemetrexed were evaluated in the KEYNOTE-021 trial. Patients were split between two doses of pembrolizumab: 2 or 10 mg/kg every 3 weeks. The overall response rate for the entire cohort of 74 patients with advanced NSCLC was 57% (95% confidence interval, 45-68), reported Dr. Shirish Gadgeel of Karmanos Cancer Institute, Detroit.
For the 25 patients who received pembrolizumab, carboplatin, and paclitaxel (cohort A) the overall response was 52% (95% CI, 31-72). For the 25 patients who also received bevacizumab in addition to pembrolizumab, carboplatin, and paclitaxel (cohort B), the overall response rate was 48% (95% CI, 28-69).
Among 24 patients who received pemetrexed with pembrolizumab and carboplatin (cohort C), the overall response was the highest at 71% (95% CI, 49-87).
Grade 3 or 4 adverse events occurred in 36%, 46%, and 42% of patients in cohort A, B, and C, respectively. The most common adverse events were anemia and neutropenia including febrile neutropenia.
“Pembro in combination with standard chemotherapy regimens is feasible and yields substantial clinical efficacy regardless of pembro dose or PD-L1 status in treatment-naïve advanced NSCLC,” Dr Gadgeel said.
A randomized phase III study evaluating pemetrexed/platinum with or without pembrolizumab is currently recruiting, he said.
These combinations, while perhaps better than chemotherapy alone, may be no better than just immunotherapy alone, session moderator Dr. Scott Antonia of the Moffitt Cancer Center, Tampa, Fla., commented. “And the truth is that concurrent therapy is clearly more toxic.”
In another study presented at the meeting, led by Dr. Roy Herbst of Yale Cancer Center, New Haven, Conn., pembrolizumab was combined with ramucirumab, a recently approved vascular endothelial growth factor receptor–2 inhibitor. “Hallmarks of tumor growth include angiogenesis and immunosuppression,” Dr. Herbst and his coauthors wrote in their abstract, noting that this was the first study to combine these agents to target both processes simultaneously.
“The idea is the R2 inhibitor might have an effect on the microimmune environment and drive T cells into the tumor,” Dr. Herbst said.
The study cohort included patients with advanced gastric or gastroesophageal junction adenocarcinoma, NSCLC, and urothelial carcinoma.
Overall, the response rate was close to 30% in the first 10 patients, Dr. Herbst reported. Furthermore, the preliminary data did not reveal any unexpected safety signals.
Although the data was from a small, ongoing phase I trial, Dr. Herbst noted the data is promising. Researchers are continuing to collect data on the safety profile of this drug combination, and are planning to enroll patients with additional tumor types.
The KEYNOTE-021 trial was funded by Merck Sharp and Dohme. Dr. Gadgeel reported having a consulting or advisory role and receiving research funding from multiple companies. The trial headed by Dr. Herbst was funded by Eli Lilly. Dr. Herbst reported having a consulting or advisory role and receiving honoraria and research funding from multiple companies including Eli Lilly.
On Twitter @jessnicolecraig
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Overall response rates ranged from 30% to 71% when pembrolizumab was added to chemotherapy combinations or paired with an R2 inhibitor in patients with advanced NSCLC and other tumor types.
Major finding: Overall response rates ranged from 48% to 71% for NSCLC patients receiving pembrolizumab in combination with standard chemotherapy regimens, one with bevacizumab. In combinations with an R2-inhibitor, the overall response rate was nearly 30% for patients with advanced NSCLC or gastric or urothelial tumors.
Data source: The phase I/II KEYNOTE-021 trial of 74 patients with advanced NSCLC, and the phase I trial that included patients with advanced gastric or gastroesophageal junction adenocarcinoma, NSCLC, and urothelial carcinoma.
Disclosures: The KEYNOTE-021 trial was funded by Merck Sharp and Dohme. Dr. Gadgeel reported having a consulting or advisory role and receiving research funding from multiple companies. The trial headed by Dr. Herbst was funded by Eli Lilly. Dr. Herbst reported having a consulting or advisory role and receiving honoraria and research funding from multiple companies including Eli Lilly.
Better pembrolizumab outcomes with increasing PD-L1 in NSCLC
CHICAGO – The PD-1 inhibitor, pembrolizumab, is superior to docetaxel in prolonging overall and progression-free survival in patients with non–small cell lung cancer (NSCLC), according to the results of the phase III KEYNOTE-010 trial.
Furthermore, increasing PD-L1 expression was associated with more favorable outcomes with pembrolizumab while level of PD-L1 expression had no effect on outcomes in docetaxel.
Results of the KEYNOTE-010 study were published earlier this year in the Lancet, but the results reported at the annual meeting of the American Society of Clinical Oncology further categorized study participants by tumor proportion score, a measure of viable tumor cells showing partial or complete membrane staining for PD-L1.
This finding verifies PD-L1 as a “predictive biomarker for ‘pembro’ in NSCLC,” lead study author Dr. Paul Baas of the Netherlands Cancer Institute, Amsterdam, said.
Out of 690 patients receiving pembrolizumab, 184 had a tumor proportion score (TPS) of 75% or more. For those 184 patients, median overall survival was 16.6 months and median progression-free survival was 6.2 months. The overall response rate was 33.7% for patients receiving pembrolizumab with TPS greater than 75%.
These survival and response rates were significantly higher, compared with the 8.2 month median overall survival, 4.0 month progression-free survival, and 7% overall response rate observed in 100 patients with the same TPS score who instead received docetaxel (overall survival: hazard ratio, 0.51; 95% confidence interval, 0.36-0.73; P less than .0001; progression-free survival: HR, 0.52; 95% CI, 0.38-0.69; P less than .0001; overall response rate: P less than .0001).
For the 106 patients receiving pembrolizumab who had a TPS between 50% and 74%, median OS was 15.8 months, PFS was 4.3 months, and the ORR was 22.6%. Median overall survival was significantly higher for pembrolizumab than docetaxel which was 8.2 months (HR, 0.58; 95% CI, 0.36-0.95; P = .01). ORR was also significantly higher for pembrolizumab than for docetaxel, which was 9.6% (P = .01).
The KEYNOTE-010 study was funded by Merck Sharp & Dohme. Dr. Baas reported having a consulting or advisory role and receiving honoraria and financial compensation from multiple companies including Merck Sharp & Dohme.
CHICAGO – The PD-1 inhibitor, pembrolizumab, is superior to docetaxel in prolonging overall and progression-free survival in patients with non–small cell lung cancer (NSCLC), according to the results of the phase III KEYNOTE-010 trial.
Furthermore, increasing PD-L1 expression was associated with more favorable outcomes with pembrolizumab while level of PD-L1 expression had no effect on outcomes in docetaxel.
Results of the KEYNOTE-010 study were published earlier this year in the Lancet, but the results reported at the annual meeting of the American Society of Clinical Oncology further categorized study participants by tumor proportion score, a measure of viable tumor cells showing partial or complete membrane staining for PD-L1.
This finding verifies PD-L1 as a “predictive biomarker for ‘pembro’ in NSCLC,” lead study author Dr. Paul Baas of the Netherlands Cancer Institute, Amsterdam, said.
Out of 690 patients receiving pembrolizumab, 184 had a tumor proportion score (TPS) of 75% or more. For those 184 patients, median overall survival was 16.6 months and median progression-free survival was 6.2 months. The overall response rate was 33.7% for patients receiving pembrolizumab with TPS greater than 75%.
These survival and response rates were significantly higher, compared with the 8.2 month median overall survival, 4.0 month progression-free survival, and 7% overall response rate observed in 100 patients with the same TPS score who instead received docetaxel (overall survival: hazard ratio, 0.51; 95% confidence interval, 0.36-0.73; P less than .0001; progression-free survival: HR, 0.52; 95% CI, 0.38-0.69; P less than .0001; overall response rate: P less than .0001).
For the 106 patients receiving pembrolizumab who had a TPS between 50% and 74%, median OS was 15.8 months, PFS was 4.3 months, and the ORR was 22.6%. Median overall survival was significantly higher for pembrolizumab than docetaxel which was 8.2 months (HR, 0.58; 95% CI, 0.36-0.95; P = .01). ORR was also significantly higher for pembrolizumab than for docetaxel, which was 9.6% (P = .01).
The KEYNOTE-010 study was funded by Merck Sharp & Dohme. Dr. Baas reported having a consulting or advisory role and receiving honoraria and financial compensation from multiple companies including Merck Sharp & Dohme.
CHICAGO – The PD-1 inhibitor, pembrolizumab, is superior to docetaxel in prolonging overall and progression-free survival in patients with non–small cell lung cancer (NSCLC), according to the results of the phase III KEYNOTE-010 trial.
Furthermore, increasing PD-L1 expression was associated with more favorable outcomes with pembrolizumab while level of PD-L1 expression had no effect on outcomes in docetaxel.
Results of the KEYNOTE-010 study were published earlier this year in the Lancet, but the results reported at the annual meeting of the American Society of Clinical Oncology further categorized study participants by tumor proportion score, a measure of viable tumor cells showing partial or complete membrane staining for PD-L1.
This finding verifies PD-L1 as a “predictive biomarker for ‘pembro’ in NSCLC,” lead study author Dr. Paul Baas of the Netherlands Cancer Institute, Amsterdam, said.
Out of 690 patients receiving pembrolizumab, 184 had a tumor proportion score (TPS) of 75% or more. For those 184 patients, median overall survival was 16.6 months and median progression-free survival was 6.2 months. The overall response rate was 33.7% for patients receiving pembrolizumab with TPS greater than 75%.
These survival and response rates were significantly higher, compared with the 8.2 month median overall survival, 4.0 month progression-free survival, and 7% overall response rate observed in 100 patients with the same TPS score who instead received docetaxel (overall survival: hazard ratio, 0.51; 95% confidence interval, 0.36-0.73; P less than .0001; progression-free survival: HR, 0.52; 95% CI, 0.38-0.69; P less than .0001; overall response rate: P less than .0001).
For the 106 patients receiving pembrolizumab who had a TPS between 50% and 74%, median OS was 15.8 months, PFS was 4.3 months, and the ORR was 22.6%. Median overall survival was significantly higher for pembrolizumab than docetaxel which was 8.2 months (HR, 0.58; 95% CI, 0.36-0.95; P = .01). ORR was also significantly higher for pembrolizumab than for docetaxel, which was 9.6% (P = .01).
The KEYNOTE-010 study was funded by Merck Sharp & Dohme. Dr. Baas reported having a consulting or advisory role and receiving honoraria and financial compensation from multiple companies including Merck Sharp & Dohme.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Pembrolizumab is superior to docetaxel in patients with non–small cell lung cancer especially at higher TPS. PD-L1 may be a predictive biomarker for pembrolizumab.
Major finding: For patients with tumor proportion scores of 75% or higher, median overall survival for pembrolizumab as single agent therapy was 16.6 months and only 8.2 months for single agent docetaxel (hazard ratio, .51; 95% confidence interval, .36-.73; P less than .0001).
Data source: The phase III KEYNOTE-010 trial of 1,034 patients with NSCLC.
Disclosures: The KEYNOTE-010 study was funded by Merck Sharp & Dohme. Dr. Baas reported having a consulting or advisory role and having received honoraria and financial compensation from multiple companies, including Merck Sharp & Dohme.
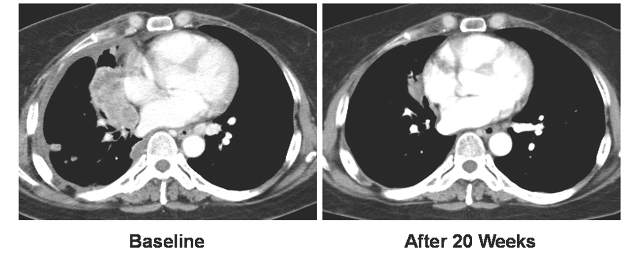
Study results differ on benefits of proton radiotherapy in NSCLC
CHICAGO – Whether proton radiotherapy is an option superior to photon radiotherapy for patients with non–small-cell lung cancer is still unclear, in light of results from a small randomized clinical trial and a review of the National Cancer Data Base.
The randomized trial of 149 patients showed there was no significant difference in radiation pneumonitis incidence rate nor overall survival by treatment received, while a retrospective analysis of 140,383 patients revealed that receipt of proton radiotherapy was associated with higher 5-year survival rates. The findings were presented at the annual meeting of the American Society of Clinical Oncology.
The Bayesian randomized trial compared rates of treatment failure and adverse events in patients receiving either intensity-modulated radiotherapy (IMRT) or 3D passively scattered proton therapy (3DPT). Of the 149 patients who met randomization requirements, 92 received IMRT and 57 received 3DPT. All patients received concurrent chemotherapy, and the patient characteristics were well balanced, although in the 3DPT group target volumes were larger.
Treatment failure rates at 12 months were 15.6% in the IMRT group and 24.6% in the 3DPT group. The median time to treatment failure was 10.5 months for both groups, reported Dr. Zhongxing Liao of the University of Texas MD Anderson Cancer Center, Houston.
The incident rates of radiation pneumonitis were 7.2% among patients receiving IMRT and 11% among patients receiving 3DPT; the median time to radiation pneumonitis was 4.5 and 4.0 months, respectively.
Dr. Liao pointed out that, historically, incidence rates of radiation pneumonitis were 15% in IMRT and 5% in 3DPT, and that rates observed in this study represented a deviation from those rates.
Local recurrence occurred in 22.8% of the IMRT patients and 24.6% of the 3DPT patients; time to local occurrence was 12.7 and 13.4 months, respectively. Finally, statistical analysis revealed no significant difference in overall survival by treatment received, Dr. Liao reported.
“Considerably fewer [adverse] events occurred in the current trial actually suggesting that both IMRT and the proton [therapy] are excellent treatments for non–small-cell lung cancer,” Dr. Liao said. “No differences were found between IMRT versus 3DPT in treatment failure in this randomized trial.”
Dr. Liao pointed out that as the trial went on, patients experienced fewer adverse events and went longer periods of time before experiencing treatment failure. This was an indication that the administration of both proton therapy and radiation therapy improved over time, he said.
In another study presented at the meeting, investigators used the National Cancer Data Base to collect demographic and clinical data on 140,383 patients with non–small-cell lung cancer who were treated with thoracic radiation from 2004 to 2012.
Across the entire cohort, median age was 68 years, 57% were male, 59% had stage II or III cancer, and 85% of patients were white. Only 348 patients received proton radiotherapy while the remaining 140,035 patients received photon radiotherapy, reported Madhusmita Behera, Ph.D., of Winship Cancer Institute at Emory University in Acworth, Georgia.
Multivariate analysis revealed that receipt of photon radiotherapy was associated with an increased risk of mortality, compared to proton radiotherapy (hazard ratio, 1.46; P less than .001).
For patients with stage II or III disease, 5-year overall survival rates were 15% for those who received photon radiotherapy and 22.3% for those who received proton radiotherapy (P = .01).
Patients were less likely to receive proton radiotherapy in community (odds ratio, .2; P less than .001) or comprehensive community (OR, .32; P less than .001) centers compared to academic centers, Dr. Behera reported.
Among the patients who received proton radiotherapy, 45.12% reported residing in a geographical location (defined by ZIP codes) with a median income quartile of $46,000 or more, the “highest median income quartile according to the U.S. census.” In addition, “only 14% of patients were from ZIP codes where more than 29% did not have a high school degree,” Dr. Behera said.
Both Dr. Behera and Dr. Liao noted that insurance denial continues to be a barrier to proton therapy. Following enrollment, 26 patients were denied insurance coverage for proton radiotherapy, Dr. Liao reported.
“This is only the beginning of the story of randomized trials [studying] proton and photon therapy in lung cancer in my opinion,” Dr. Liao said. “We only randomized patients with equivalent plans which may have excluded patients who could have benefited from protons the most.”
The study headed by Dr. Liao was funded by the MD Anderson Cancer Center and the National Cancer Institute. Dr. Liao had no relevant disclosures. One coinvestigator reported having stock or other ownership interest in Liquid Biotech, USA. The study headed by Dr. Behera was funded by the Biostatistics and Bioinformatics Shared Resource of Winship Cancer Institute of Emory University and the National Cancer Institute. Dr. Behera had no relevant disclosures; four of her coinvestigators disclosed having consulting or advisory roles or receiving financial compensation or honoraria from multiple companies.
On Twitter @jessnicolecraig
CHICAGO – Whether proton radiotherapy is an option superior to photon radiotherapy for patients with non–small-cell lung cancer is still unclear, in light of results from a small randomized clinical trial and a review of the National Cancer Data Base.
The randomized trial of 149 patients showed there was no significant difference in radiation pneumonitis incidence rate nor overall survival by treatment received, while a retrospective analysis of 140,383 patients revealed that receipt of proton radiotherapy was associated with higher 5-year survival rates. The findings were presented at the annual meeting of the American Society of Clinical Oncology.
The Bayesian randomized trial compared rates of treatment failure and adverse events in patients receiving either intensity-modulated radiotherapy (IMRT) or 3D passively scattered proton therapy (3DPT). Of the 149 patients who met randomization requirements, 92 received IMRT and 57 received 3DPT. All patients received concurrent chemotherapy, and the patient characteristics were well balanced, although in the 3DPT group target volumes were larger.
Treatment failure rates at 12 months were 15.6% in the IMRT group and 24.6% in the 3DPT group. The median time to treatment failure was 10.5 months for both groups, reported Dr. Zhongxing Liao of the University of Texas MD Anderson Cancer Center, Houston.
The incident rates of radiation pneumonitis were 7.2% among patients receiving IMRT and 11% among patients receiving 3DPT; the median time to radiation pneumonitis was 4.5 and 4.0 months, respectively.
Dr. Liao pointed out that, historically, incidence rates of radiation pneumonitis were 15% in IMRT and 5% in 3DPT, and that rates observed in this study represented a deviation from those rates.
Local recurrence occurred in 22.8% of the IMRT patients and 24.6% of the 3DPT patients; time to local occurrence was 12.7 and 13.4 months, respectively. Finally, statistical analysis revealed no significant difference in overall survival by treatment received, Dr. Liao reported.
“Considerably fewer [adverse] events occurred in the current trial actually suggesting that both IMRT and the proton [therapy] are excellent treatments for non–small-cell lung cancer,” Dr. Liao said. “No differences were found between IMRT versus 3DPT in treatment failure in this randomized trial.”
Dr. Liao pointed out that as the trial went on, patients experienced fewer adverse events and went longer periods of time before experiencing treatment failure. This was an indication that the administration of both proton therapy and radiation therapy improved over time, he said.
In another study presented at the meeting, investigators used the National Cancer Data Base to collect demographic and clinical data on 140,383 patients with non–small-cell lung cancer who were treated with thoracic radiation from 2004 to 2012.
Across the entire cohort, median age was 68 years, 57% were male, 59% had stage II or III cancer, and 85% of patients were white. Only 348 patients received proton radiotherapy while the remaining 140,035 patients received photon radiotherapy, reported Madhusmita Behera, Ph.D., of Winship Cancer Institute at Emory University in Acworth, Georgia.
Multivariate analysis revealed that receipt of photon radiotherapy was associated with an increased risk of mortality, compared to proton radiotherapy (hazard ratio, 1.46; P less than .001).
For patients with stage II or III disease, 5-year overall survival rates were 15% for those who received photon radiotherapy and 22.3% for those who received proton radiotherapy (P = .01).
Patients were less likely to receive proton radiotherapy in community (odds ratio, .2; P less than .001) or comprehensive community (OR, .32; P less than .001) centers compared to academic centers, Dr. Behera reported.
Among the patients who received proton radiotherapy, 45.12% reported residing in a geographical location (defined by ZIP codes) with a median income quartile of $46,000 or more, the “highest median income quartile according to the U.S. census.” In addition, “only 14% of patients were from ZIP codes where more than 29% did not have a high school degree,” Dr. Behera said.
Both Dr. Behera and Dr. Liao noted that insurance denial continues to be a barrier to proton therapy. Following enrollment, 26 patients were denied insurance coverage for proton radiotherapy, Dr. Liao reported.
“This is only the beginning of the story of randomized trials [studying] proton and photon therapy in lung cancer in my opinion,” Dr. Liao said. “We only randomized patients with equivalent plans which may have excluded patients who could have benefited from protons the most.”
The study headed by Dr. Liao was funded by the MD Anderson Cancer Center and the National Cancer Institute. Dr. Liao had no relevant disclosures. One coinvestigator reported having stock or other ownership interest in Liquid Biotech, USA. The study headed by Dr. Behera was funded by the Biostatistics and Bioinformatics Shared Resource of Winship Cancer Institute of Emory University and the National Cancer Institute. Dr. Behera had no relevant disclosures; four of her coinvestigators disclosed having consulting or advisory roles or receiving financial compensation or honoraria from multiple companies.
On Twitter @jessnicolecraig
CHICAGO – Whether proton radiotherapy is an option superior to photon radiotherapy for patients with non–small-cell lung cancer is still unclear, in light of results from a small randomized clinical trial and a review of the National Cancer Data Base.
The randomized trial of 149 patients showed there was no significant difference in radiation pneumonitis incidence rate nor overall survival by treatment received, while a retrospective analysis of 140,383 patients revealed that receipt of proton radiotherapy was associated with higher 5-year survival rates. The findings were presented at the annual meeting of the American Society of Clinical Oncology.
The Bayesian randomized trial compared rates of treatment failure and adverse events in patients receiving either intensity-modulated radiotherapy (IMRT) or 3D passively scattered proton therapy (3DPT). Of the 149 patients who met randomization requirements, 92 received IMRT and 57 received 3DPT. All patients received concurrent chemotherapy, and the patient characteristics were well balanced, although in the 3DPT group target volumes were larger.
Treatment failure rates at 12 months were 15.6% in the IMRT group and 24.6% in the 3DPT group. The median time to treatment failure was 10.5 months for both groups, reported Dr. Zhongxing Liao of the University of Texas MD Anderson Cancer Center, Houston.
The incident rates of radiation pneumonitis were 7.2% among patients receiving IMRT and 11% among patients receiving 3DPT; the median time to radiation pneumonitis was 4.5 and 4.0 months, respectively.
Dr. Liao pointed out that, historically, incidence rates of radiation pneumonitis were 15% in IMRT and 5% in 3DPT, and that rates observed in this study represented a deviation from those rates.
Local recurrence occurred in 22.8% of the IMRT patients and 24.6% of the 3DPT patients; time to local occurrence was 12.7 and 13.4 months, respectively. Finally, statistical analysis revealed no significant difference in overall survival by treatment received, Dr. Liao reported.
“Considerably fewer [adverse] events occurred in the current trial actually suggesting that both IMRT and the proton [therapy] are excellent treatments for non–small-cell lung cancer,” Dr. Liao said. “No differences were found between IMRT versus 3DPT in treatment failure in this randomized trial.”
Dr. Liao pointed out that as the trial went on, patients experienced fewer adverse events and went longer periods of time before experiencing treatment failure. This was an indication that the administration of both proton therapy and radiation therapy improved over time, he said.
In another study presented at the meeting, investigators used the National Cancer Data Base to collect demographic and clinical data on 140,383 patients with non–small-cell lung cancer who were treated with thoracic radiation from 2004 to 2012.
Across the entire cohort, median age was 68 years, 57% were male, 59% had stage II or III cancer, and 85% of patients were white. Only 348 patients received proton radiotherapy while the remaining 140,035 patients received photon radiotherapy, reported Madhusmita Behera, Ph.D., of Winship Cancer Institute at Emory University in Acworth, Georgia.
Multivariate analysis revealed that receipt of photon radiotherapy was associated with an increased risk of mortality, compared to proton radiotherapy (hazard ratio, 1.46; P less than .001).
For patients with stage II or III disease, 5-year overall survival rates were 15% for those who received photon radiotherapy and 22.3% for those who received proton radiotherapy (P = .01).
Patients were less likely to receive proton radiotherapy in community (odds ratio, .2; P less than .001) or comprehensive community (OR, .32; P less than .001) centers compared to academic centers, Dr. Behera reported.
Among the patients who received proton radiotherapy, 45.12% reported residing in a geographical location (defined by ZIP codes) with a median income quartile of $46,000 or more, the “highest median income quartile according to the U.S. census.” In addition, “only 14% of patients were from ZIP codes where more than 29% did not have a high school degree,” Dr. Behera said.
Both Dr. Behera and Dr. Liao noted that insurance denial continues to be a barrier to proton therapy. Following enrollment, 26 patients were denied insurance coverage for proton radiotherapy, Dr. Liao reported.
“This is only the beginning of the story of randomized trials [studying] proton and photon therapy in lung cancer in my opinion,” Dr. Liao said. “We only randomized patients with equivalent plans which may have excluded patients who could have benefited from protons the most.”
The study headed by Dr. Liao was funded by the MD Anderson Cancer Center and the National Cancer Institute. Dr. Liao had no relevant disclosures. One coinvestigator reported having stock or other ownership interest in Liquid Biotech, USA. The study headed by Dr. Behera was funded by the Biostatistics and Bioinformatics Shared Resource of Winship Cancer Institute of Emory University and the National Cancer Institute. Dr. Behera had no relevant disclosures; four of her coinvestigators disclosed having consulting or advisory roles or receiving financial compensation or honoraria from multiple companies.
On Twitter @jessnicolecraig
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Results of a small randomized trial and an analysis of the National Cancer Data Base show conflicting results about the benefits of proton therapy in NSCLC patients.
Major finding: In the small randomized trial, there was no significant difference in overall survival between photon and proton radiotherapy. The analysis of patient records from the NCDB revealed that receipt of photon radiotherapy was associated with an increased risk of mortality compared to proton radiotherapy (hazard ratio, 1.46; P less than .001).
Data source: A randomized trial of 149 patients and an analysis of 140,383 patients with NSCLC who received either proton radiotherapy or photon radiotherapy.
Disclosures: The study headed by Dr. Liao was funded by the MD Anderson Cancer Center and the National Cancer Institute. Dr. Liao had no relevant disclosures. One coinvestigator reported having stock or other ownership interest in Liquid Biotech, USA. The study headed by Dr. Behera was funded by the Biostatistics and Bioinformatics Shared Resource of Winship Cancer Institute of Emory University and the National Cancer Institute. Dr. Behera had no relevant disclosures, and four of her coinvestigators disclosed having consulting or advisory roles or receiving financial compensation or honoraria from multiple companies.
Heat shock protein peptide vaccine appears safe, effective for glioblastoma patients
Chicago – A newly developed heat shock protein peptide vaccination appears to be safe and effective in treating patients with newly diagnosed glioblastoma (GBM), according to the results of a phase II single arm study.
In adding the vaccine to standard therapy for 46 patients with newly diagnosed GBM, median overall survival was 23.8 months, and there were no grade 3 or 4 adverse events associated with the vaccine, lead author Dr. Orin Bloch of Northwestern University, Chicago, reported at the annual meeting of the American Society of Clinical Oncology.
Standard therapy typically results in a median survival of 16 months, he said.
“There is a lot of information out there right now regarding CNS and other solid organ tumors particularly in the area of checkpoint modulation and its ability to stimulate an innate immune response against a tumor. I think in GBM we are facing a bit of a different scenario, however, because the tumor exists in a very privileged area behind the blood brain barrier and doesn’t regularly metastasize beyond the CNS,” Dr. Bloch said.
Therefore, only modulating checkpoints without stimulating and educating the immune system may not be the most effective approach. Adaptive immunity through vaccination or some other form of stimulation might be more successful, Dr. Bloch said.
“As a way of inducing immune stimulation and education using tumor-autologous peptides, one can capitalize on the native system of heat shock stimulation. Heat shock proteins are chaperone proteins that are ubiquitously expressed in cells and they’re bound to any number of intracellular peptides at any one time including, in tumor cells, neoantigens. If you extract these heat shock proteins with their bound antigens and deliver them in a naked form into the systemic circulation, their uptake into antigen-presenting cells through the CD91 receptor [will result in] the peptide [being] cleaved and presented on MHC class one and two for stimulation of CD8- and CD4-positive T cell response,” he said.
Heat shock proteins also interact with toll-like receptors and stimulate the secretion of pro-inflammatory cytokines, “acting as their own adjuvant,” Dr. Bloch further explained. Utilizing heat shock proteins activates both the innate and adaptive immune responses.
“This is an ideal platform for developing an immunotherapy for glioblastoma,” Dr. Bloch said.
In this phase II study, 46 adult patients with GBM underwent surgical resection of their tumors followed by chemoradiotherapy. At least four 25-microgram doses of vaccine were generated from tissue obtained during surgery. Within 5 weeks of completing radiotherapy, patients began receiving weekly vaccinations in combination with adjuvant temozolomide. Patients continued receiving vaccines until depletion or until tumor progression.
Median progression-free survival was 17.8 months (95% confidence interval, 11.3-21.6) and median overall survival was 23.8 months (95% CI, 19.8-30.2).
PD-L1 expression on circulating monocytes was also measured from peripheral blood samples obtained during surgery. Patients were classified as having either high PD-L1 expression (54.5% or more of monocytes) or low PD-L1 expression. Among patients classified as having high PD-L1 expression, the median overall survival was 18.0 months (95% CI, 10.0-23.3). Patients who had low PD-L1 expression had a significantly longer median overall survival time of 44.7 months with a confidence interval not calculable (hazard ratio, 3.35; 95% CI, 1.36-8.23; P = .003).
Finally, a multivariate proportional hazards model showed the MGMT methylation status and PD-L1 expression were the two greatest independent predictors of survival.
“Survival among patients who received the HSPPV-96 was greater than expected compared to historical controls... These results certainly, we feel, provide rationale for a phase III trial of vaccine plus standard of care versus standard of care alone,” Dr. Bloch said.
“PD-L1 expression on circulating myeloid cells is independently predictive of clinical response to vaccination, and it suggests that the low PD-L1 expressing population will most benefit from this anti-tumor vaccination scheme, but it also suggests that high PD-L1 expressing patients may benefit from combined checkpoint inhibition. Systemic immunosuppression driven by peripheral monocyte expression of PD-L1 is a previously unidentified factor that may mitigate vaccine efficacy,” Dr. Bloch further commented.
This study was funded by the National Cancer Institute, the National Institute of Neurological Disorders and Stroke, the National Brain Tumor Society, the American Brain Tumor Association, and Accelerated Brain Cancer Cure. Dr. Bloch reporting having no relevant disclosures.
On Twitter @jessnicolecraig
Chicago – A newly developed heat shock protein peptide vaccination appears to be safe and effective in treating patients with newly diagnosed glioblastoma (GBM), according to the results of a phase II single arm study.
In adding the vaccine to standard therapy for 46 patients with newly diagnosed GBM, median overall survival was 23.8 months, and there were no grade 3 or 4 adverse events associated with the vaccine, lead author Dr. Orin Bloch of Northwestern University, Chicago, reported at the annual meeting of the American Society of Clinical Oncology.
Standard therapy typically results in a median survival of 16 months, he said.
“There is a lot of information out there right now regarding CNS and other solid organ tumors particularly in the area of checkpoint modulation and its ability to stimulate an innate immune response against a tumor. I think in GBM we are facing a bit of a different scenario, however, because the tumor exists in a very privileged area behind the blood brain barrier and doesn’t regularly metastasize beyond the CNS,” Dr. Bloch said.
Therefore, only modulating checkpoints without stimulating and educating the immune system may not be the most effective approach. Adaptive immunity through vaccination or some other form of stimulation might be more successful, Dr. Bloch said.
“As a way of inducing immune stimulation and education using tumor-autologous peptides, one can capitalize on the native system of heat shock stimulation. Heat shock proteins are chaperone proteins that are ubiquitously expressed in cells and they’re bound to any number of intracellular peptides at any one time including, in tumor cells, neoantigens. If you extract these heat shock proteins with their bound antigens and deliver them in a naked form into the systemic circulation, their uptake into antigen-presenting cells through the CD91 receptor [will result in] the peptide [being] cleaved and presented on MHC class one and two for stimulation of CD8- and CD4-positive T cell response,” he said.
Heat shock proteins also interact with toll-like receptors and stimulate the secretion of pro-inflammatory cytokines, “acting as their own adjuvant,” Dr. Bloch further explained. Utilizing heat shock proteins activates both the innate and adaptive immune responses.
“This is an ideal platform for developing an immunotherapy for glioblastoma,” Dr. Bloch said.
In this phase II study, 46 adult patients with GBM underwent surgical resection of their tumors followed by chemoradiotherapy. At least four 25-microgram doses of vaccine were generated from tissue obtained during surgery. Within 5 weeks of completing radiotherapy, patients began receiving weekly vaccinations in combination with adjuvant temozolomide. Patients continued receiving vaccines until depletion or until tumor progression.
Median progression-free survival was 17.8 months (95% confidence interval, 11.3-21.6) and median overall survival was 23.8 months (95% CI, 19.8-30.2).
PD-L1 expression on circulating monocytes was also measured from peripheral blood samples obtained during surgery. Patients were classified as having either high PD-L1 expression (54.5% or more of monocytes) or low PD-L1 expression. Among patients classified as having high PD-L1 expression, the median overall survival was 18.0 months (95% CI, 10.0-23.3). Patients who had low PD-L1 expression had a significantly longer median overall survival time of 44.7 months with a confidence interval not calculable (hazard ratio, 3.35; 95% CI, 1.36-8.23; P = .003).
Finally, a multivariate proportional hazards model showed the MGMT methylation status and PD-L1 expression were the two greatest independent predictors of survival.
“Survival among patients who received the HSPPV-96 was greater than expected compared to historical controls... These results certainly, we feel, provide rationale for a phase III trial of vaccine plus standard of care versus standard of care alone,” Dr. Bloch said.
“PD-L1 expression on circulating myeloid cells is independently predictive of clinical response to vaccination, and it suggests that the low PD-L1 expressing population will most benefit from this anti-tumor vaccination scheme, but it also suggests that high PD-L1 expressing patients may benefit from combined checkpoint inhibition. Systemic immunosuppression driven by peripheral monocyte expression of PD-L1 is a previously unidentified factor that may mitigate vaccine efficacy,” Dr. Bloch further commented.
This study was funded by the National Cancer Institute, the National Institute of Neurological Disorders and Stroke, the National Brain Tumor Society, the American Brain Tumor Association, and Accelerated Brain Cancer Cure. Dr. Bloch reporting having no relevant disclosures.
On Twitter @jessnicolecraig
Chicago – A newly developed heat shock protein peptide vaccination appears to be safe and effective in treating patients with newly diagnosed glioblastoma (GBM), according to the results of a phase II single arm study.
In adding the vaccine to standard therapy for 46 patients with newly diagnosed GBM, median overall survival was 23.8 months, and there were no grade 3 or 4 adverse events associated with the vaccine, lead author Dr. Orin Bloch of Northwestern University, Chicago, reported at the annual meeting of the American Society of Clinical Oncology.
Standard therapy typically results in a median survival of 16 months, he said.
“There is a lot of information out there right now regarding CNS and other solid organ tumors particularly in the area of checkpoint modulation and its ability to stimulate an innate immune response against a tumor. I think in GBM we are facing a bit of a different scenario, however, because the tumor exists in a very privileged area behind the blood brain barrier and doesn’t regularly metastasize beyond the CNS,” Dr. Bloch said.
Therefore, only modulating checkpoints without stimulating and educating the immune system may not be the most effective approach. Adaptive immunity through vaccination or some other form of stimulation might be more successful, Dr. Bloch said.
“As a way of inducing immune stimulation and education using tumor-autologous peptides, one can capitalize on the native system of heat shock stimulation. Heat shock proteins are chaperone proteins that are ubiquitously expressed in cells and they’re bound to any number of intracellular peptides at any one time including, in tumor cells, neoantigens. If you extract these heat shock proteins with their bound antigens and deliver them in a naked form into the systemic circulation, their uptake into antigen-presenting cells through the CD91 receptor [will result in] the peptide [being] cleaved and presented on MHC class one and two for stimulation of CD8- and CD4-positive T cell response,” he said.
Heat shock proteins also interact with toll-like receptors and stimulate the secretion of pro-inflammatory cytokines, “acting as their own adjuvant,” Dr. Bloch further explained. Utilizing heat shock proteins activates both the innate and adaptive immune responses.
“This is an ideal platform for developing an immunotherapy for glioblastoma,” Dr. Bloch said.
In this phase II study, 46 adult patients with GBM underwent surgical resection of their tumors followed by chemoradiotherapy. At least four 25-microgram doses of vaccine were generated from tissue obtained during surgery. Within 5 weeks of completing radiotherapy, patients began receiving weekly vaccinations in combination with adjuvant temozolomide. Patients continued receiving vaccines until depletion or until tumor progression.
Median progression-free survival was 17.8 months (95% confidence interval, 11.3-21.6) and median overall survival was 23.8 months (95% CI, 19.8-30.2).
PD-L1 expression on circulating monocytes was also measured from peripheral blood samples obtained during surgery. Patients were classified as having either high PD-L1 expression (54.5% or more of monocytes) or low PD-L1 expression. Among patients classified as having high PD-L1 expression, the median overall survival was 18.0 months (95% CI, 10.0-23.3). Patients who had low PD-L1 expression had a significantly longer median overall survival time of 44.7 months with a confidence interval not calculable (hazard ratio, 3.35; 95% CI, 1.36-8.23; P = .003).
Finally, a multivariate proportional hazards model showed the MGMT methylation status and PD-L1 expression were the two greatest independent predictors of survival.
“Survival among patients who received the HSPPV-96 was greater than expected compared to historical controls... These results certainly, we feel, provide rationale for a phase III trial of vaccine plus standard of care versus standard of care alone,” Dr. Bloch said.
“PD-L1 expression on circulating myeloid cells is independently predictive of clinical response to vaccination, and it suggests that the low PD-L1 expressing population will most benefit from this anti-tumor vaccination scheme, but it also suggests that high PD-L1 expressing patients may benefit from combined checkpoint inhibition. Systemic immunosuppression driven by peripheral monocyte expression of PD-L1 is a previously unidentified factor that may mitigate vaccine efficacy,” Dr. Bloch further commented.
This study was funded by the National Cancer Institute, the National Institute of Neurological Disorders and Stroke, the National Brain Tumor Society, the American Brain Tumor Association, and Accelerated Brain Cancer Cure. Dr. Bloch reporting having no relevant disclosures.
On Twitter @jessnicolecraig
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: A heat shock protein peptide vaccine appears safe and effective for patients with glioblastoma in an early stage trial.
Major finding: Median progression-free survival was 17.8 months (95% CI, 11.3-21.6). Median overall survival was 23.8 months (95% CI, 19.8-30.2).
Data source: A phase II single arm study of 46 adult patients with glioblastoma.
Disclosures: This study was funded by the National Cancer Institute, the National Institute of Neurological Disorders and Stroke, the National Brain Tumor Society, the American Brain Tumor Association, and Accelerated Brain Cancer Cure. Dr. Bloch reporting having no relevant disclosures.
Neoadjuvant chemo for advanced ovarian cancer opens ‘window of opportunity’ for immunotherapies
Presurgical neoadjuvant chemotherapy (NACT) altered the immune microenvironment in patients with stage IIIC/IV tubo-ovarian high-grade serous carcinoma (HGSC), perhaps enhancing the potential response to immunotherapy, investigators report.
“The results suggest that the effects of immunotherapy might be enhanced if given after chemotherapy, potentially improving disease control in patients with advanced HGSC and other cancer types,” wrote Dr. Steffen Bohm of Barts Cancer Institute in London and his associates (CCR. 2016. doi: 10.1158/1078-0432.CCR-15-2657).
Dr. Bohm and associates collected pre- and postchemotherapy biopsies and blood samples from 60 patients with stage IIIC or IV HGSC; 54 patients underwent platinum-based neoadjuvant chemotherapy and 6 received chemotherapy after debulking surgery. The investigators used immunohistochemistry and RNA sequencing to evaluate the changes before and after chemotherapy. The patients were grouped by their response to chemotherapy.
Results indicated that NACT induced T cell activation, with results most pronounced among those who had a good response to chemotherapy. Among a subset of 25 patients, omental metastases biopsies indicated CD8+ T cells and memory cells were present in the tumors after NACT. Proinflammatory cytokines decreased in all patients following NACT.
Immunohistochemical staining for PD-1 ligands showed that PD-L1 levels were significantly increased in post-NACT samples regardless of a patient’s response to chemotherapy.
“Our results suggest that NACT opens a window of opportunity for immunotherapies such as immune checkpoint blockade for patients with different levels of response to chemotherapy,” Dr. Bohm and associates said.
The study was funded by the Swiss Cancer League, the European Research Council, Cancer Research UK, and Barts and The London Charity. The authors had no relevant disclosures to report.
On Twitter @jessnicolecraig
Presurgical neoadjuvant chemotherapy (NACT) altered the immune microenvironment in patients with stage IIIC/IV tubo-ovarian high-grade serous carcinoma (HGSC), perhaps enhancing the potential response to immunotherapy, investigators report.
“The results suggest that the effects of immunotherapy might be enhanced if given after chemotherapy, potentially improving disease control in patients with advanced HGSC and other cancer types,” wrote Dr. Steffen Bohm of Barts Cancer Institute in London and his associates (CCR. 2016. doi: 10.1158/1078-0432.CCR-15-2657).
Dr. Bohm and associates collected pre- and postchemotherapy biopsies and blood samples from 60 patients with stage IIIC or IV HGSC; 54 patients underwent platinum-based neoadjuvant chemotherapy and 6 received chemotherapy after debulking surgery. The investigators used immunohistochemistry and RNA sequencing to evaluate the changes before and after chemotherapy. The patients were grouped by their response to chemotherapy.
Results indicated that NACT induced T cell activation, with results most pronounced among those who had a good response to chemotherapy. Among a subset of 25 patients, omental metastases biopsies indicated CD8+ T cells and memory cells were present in the tumors after NACT. Proinflammatory cytokines decreased in all patients following NACT.
Immunohistochemical staining for PD-1 ligands showed that PD-L1 levels were significantly increased in post-NACT samples regardless of a patient’s response to chemotherapy.
“Our results suggest that NACT opens a window of opportunity for immunotherapies such as immune checkpoint blockade for patients with different levels of response to chemotherapy,” Dr. Bohm and associates said.
The study was funded by the Swiss Cancer League, the European Research Council, Cancer Research UK, and Barts and The London Charity. The authors had no relevant disclosures to report.
On Twitter @jessnicolecraig
Presurgical neoadjuvant chemotherapy (NACT) altered the immune microenvironment in patients with stage IIIC/IV tubo-ovarian high-grade serous carcinoma (HGSC), perhaps enhancing the potential response to immunotherapy, investigators report.
“The results suggest that the effects of immunotherapy might be enhanced if given after chemotherapy, potentially improving disease control in patients with advanced HGSC and other cancer types,” wrote Dr. Steffen Bohm of Barts Cancer Institute in London and his associates (CCR. 2016. doi: 10.1158/1078-0432.CCR-15-2657).
Dr. Bohm and associates collected pre- and postchemotherapy biopsies and blood samples from 60 patients with stage IIIC or IV HGSC; 54 patients underwent platinum-based neoadjuvant chemotherapy and 6 received chemotherapy after debulking surgery. The investigators used immunohistochemistry and RNA sequencing to evaluate the changes before and after chemotherapy. The patients were grouped by their response to chemotherapy.
Results indicated that NACT induced T cell activation, with results most pronounced among those who had a good response to chemotherapy. Among a subset of 25 patients, omental metastases biopsies indicated CD8+ T cells and memory cells were present in the tumors after NACT. Proinflammatory cytokines decreased in all patients following NACT.
Immunohistochemical staining for PD-1 ligands showed that PD-L1 levels were significantly increased in post-NACT samples regardless of a patient’s response to chemotherapy.
“Our results suggest that NACT opens a window of opportunity for immunotherapies such as immune checkpoint blockade for patients with different levels of response to chemotherapy,” Dr. Bohm and associates said.
The study was funded by the Swiss Cancer League, the European Research Council, Cancer Research UK, and Barts and The London Charity. The authors had no relevant disclosures to report.
On Twitter @jessnicolecraig
FROM CLINICAL CANCER RESEARCH
Key clinical point: Neoadjuvant chemotherapy alters the immune microenvironment in patients with advanced ovarian cancer.
Major finding: Neoadjuvant chemotherapy induced T cell activity in patients with stage IIIC/IV tubo-ovarian high-grade serous carcinoma. Proinflammatory cytokines decreased in all patients following neoadjuvant chemotherapy.
Data source: A longitudinal cohort study of 60 patients with stage IIIC/IV tubo-ovarian high-grade serous carcinoma.
Disclosures: The research was funded by the Swiss Cancer League, the European Research Council, Cancer Research UK, and Barts and The London Charity. The authors had no relevant disclosures to report.
Vandetanib shows variable response, toxicity in RET-positive NSCLC
CHICAGO – The RET tyrosine kinase inhibitor vandetanib shows marked yet variable antitumor activity and toxicity in patients whose RET-positive non–small cell lung cancer (NSCLC) was unsuccessfully treated with chemotherapy, according to results of two small phase II trials presented at the annual meeting of the American Society of Clinical Oncology.
The overall response rates were 53% and 61% in two independent trials conducted by Dr. Takashi Seto of the National Kyushu Cancer Center, Japan, and by Dr. Se-Hoon Lee of Sungkyunkwan University, South Korea, respectively.
Compared to previous studies with other RET inhibitors, though all had small cohorts, there were many similarities in response rates. Progression-free survival was the most variable, but was much higher in the cabozantinib data reported at the 2015 ASCO annual meeting, according to moderator Dr. Karen Reckamp of the City of Hope Comprehensive Cancer Center, Duarte, Calif. “Vandetanib may have lower response rates than some of the others,” she said.
RET is a tyrosine kinase domain that fuses to and undergoes rearrangements with KIF5B and CCDC6 genes. This fusion and subsequent rearrangement results in ligand-dependent dimerization, which causes tumor growth. RET rearrangements were first identified in thyroid cancers.
“RET fusions were identified as new driver oncogenes of NSCLC in 2012 and observed in 1%-2% of all NSCLC,” Dr. Seto said. “Non–small cell lung cancer with RET rearrangement is regarded as a unique entity in terms of pathogenesis,” said Dr. Lee. There are currently multiple RET inhibitors in various stages of development.
In the trial headed by Dr. Seto, the Japanese genetic screening network was utilized to identify 34 NSCLC patients with RET rearrangements. Among the 34 patients, 17 met the eligibility requirements of having failed at least one prior chemotherapy treatment. Of those 17 patients, the median age was 59 years, 74% were female, all had adenocarcinomas, and 68% were nonsmokers.
All 17 patients received vandetanib at a dose of 300 mg once daily. The overall response rate was 53% (90% confidence interval, 31-74), and the disease control rate was 88%. The median progression-free survival was 4.7 months (90% CI, 2.8-8.3).
There was a marked difference in overall response rate and progression-free survival among RET fusion subtypes. For CCDC6-RET, the overall response was 83% and the progression-free survival was 8.3 months. For KIF5B-RET, the overall response was 20% with a median progression-free survival of 2.9 months.
Dr. Seto noted that there was no known biological explanation for the observed discrepancy in response rate or survival.
Dr. Seto reported that the safety profile was similar to previous reports. Four patients ended treatment due to adverse events while 16 experienced dose interruptions due to treatment-related toxicities. The most common grade three and four toxicities were hypertension (58%), rash (16%), and diarrhea (11%).
In the trial headed by Dr. Lee, 18 patients with RET rearrangements (confirmed by fluorescent in situ hybridization) met the eligibility requirement of having failed platinum-based chemotherapy. The median age of the cohort was 55 years, and 33% were female.
Similar to Dr. Seto’s study, all 18 patients received vandetanib at 300 mg once daily. Of the 18 patient cohort, 17% achieved partial remission and 44% achieved stable disease. Seven patients had no remission or stabilization. There were no treatment-related mortalities or grade 4 adverse events. Two grade 3 adverse events were reported.
“Looking at these two studies together, I think the important thing about the characteristics you see [is] that the age range is very similar [with a] median in the 50’s,” commented Dr. Reckamp. “The male to female ratio is actually opposite in both so [this] can occur in both men and women. The smoking status, interestingly is similar in both, where about a third of patients were former smokers. Most of the patients had adenocarcinoma. Many of these patients were highly previously treated. Only the Seto group looked at RET fusion partner, which may be important in looking at efficacy for these agents.” Vandetanib is a “challenging drug to tolerate,” Dr. Reckamp also noted.
“Is there a preferred RET inhibitor in small cell lung cancer?” Dr. Reckamp asked. “There are many RET inhibitors approved for other cancer types at this point, and they are multitargeted tyrosine kinases. In small studies they have similar efficacy. Toxicities vary because of the off-target effects, and most of the [treatment] decisions were made based on potential toxicities rather than differing efficacy. So none is really differentiated as the best choice, and it is unlikely that we are going to have the trials to evaluate them head to head.”
Dr. Reckamp suggested that “most patients with adenocarcinoma” should be tested for RET rearrangements. “Both men and women, both smokers and nonsmokers. And if you don’t test, you won’t find it. And if you don’t find it, you won’t be able to treat.” Dr. Reckamp also noted that next generation sequencing (NGS) should be the preferred method of identifying RET status because NGS uses less tissue, provides genetic sequencing, and allows for the identification of binding partners.
“Does targeting RET improve patient outcomes?” she continued. “Because that is really the question we need to answer if we need to move forward with RET inhibition for lung cancer. So there are variable response rates, less than other inhibitors of other oncogenic-driven tumors, that’s for sure... But if you look at the data, and these are [for] heavily pretreated patients for the most part, the response rates are better than second-line cytotoxic chemotherapy that we have had in the past and similar to unselected checkpoint inhibition. So there is potential for improving outcomes, and again if we don’t know someone is RET, we potentially are not going to offer a treatment that could help them live longer or better.”
When asked how she would treat a newly-diagnosed patient with RET-positive NSCLC, Dr. Reckamp said she would treat with first-line chemotherapy rather than a tyrosine kinase inhibitor (TKI) but would enroll the patient in whatever TKI trial was ongoing at that point in time.
“There are multiple trials that are ongoing,” Dr. Reckamp said. “It is unlikely that a comparison trial will be completed and so we are going to have to look at these trials next to each other and differentiate based on toxicity [and] perceived efficacy.”
Specifically, Dr. Reckamp believes the medical community needs to move toward “universal testing” for RET status in lung cancer patients. Resistance and combination therapies will also need to be assessed in future studies.
“RET is important in lung cancer, and should be targeted. We now need to find the best way to do that,” Dr. Reckamp concluded.
The trial headed by Dr. Seto was funded by the Japan Agency for Medical Research and Development, AMED, and AstraZeneca. Dr. Seto reported receiving honoraria and research funding from multiple companies including AstraZeneca. The trial headed by Dr. Lee was funded by AstraZeneca Korea. Dr. Lee reported having a consulting or advisory role and receiving honoraria and research funding from AstraZeneca, Pfizer, and Roche/Genentech.
CHICAGO – The RET tyrosine kinase inhibitor vandetanib shows marked yet variable antitumor activity and toxicity in patients whose RET-positive non–small cell lung cancer (NSCLC) was unsuccessfully treated with chemotherapy, according to results of two small phase II trials presented at the annual meeting of the American Society of Clinical Oncology.
The overall response rates were 53% and 61% in two independent trials conducted by Dr. Takashi Seto of the National Kyushu Cancer Center, Japan, and by Dr. Se-Hoon Lee of Sungkyunkwan University, South Korea, respectively.
Compared to previous studies with other RET inhibitors, though all had small cohorts, there were many similarities in response rates. Progression-free survival was the most variable, but was much higher in the cabozantinib data reported at the 2015 ASCO annual meeting, according to moderator Dr. Karen Reckamp of the City of Hope Comprehensive Cancer Center, Duarte, Calif. “Vandetanib may have lower response rates than some of the others,” she said.
RET is a tyrosine kinase domain that fuses to and undergoes rearrangements with KIF5B and CCDC6 genes. This fusion and subsequent rearrangement results in ligand-dependent dimerization, which causes tumor growth. RET rearrangements were first identified in thyroid cancers.
“RET fusions were identified as new driver oncogenes of NSCLC in 2012 and observed in 1%-2% of all NSCLC,” Dr. Seto said. “Non–small cell lung cancer with RET rearrangement is regarded as a unique entity in terms of pathogenesis,” said Dr. Lee. There are currently multiple RET inhibitors in various stages of development.
In the trial headed by Dr. Seto, the Japanese genetic screening network was utilized to identify 34 NSCLC patients with RET rearrangements. Among the 34 patients, 17 met the eligibility requirements of having failed at least one prior chemotherapy treatment. Of those 17 patients, the median age was 59 years, 74% were female, all had adenocarcinomas, and 68% were nonsmokers.
All 17 patients received vandetanib at a dose of 300 mg once daily. The overall response rate was 53% (90% confidence interval, 31-74), and the disease control rate was 88%. The median progression-free survival was 4.7 months (90% CI, 2.8-8.3).
There was a marked difference in overall response rate and progression-free survival among RET fusion subtypes. For CCDC6-RET, the overall response was 83% and the progression-free survival was 8.3 months. For KIF5B-RET, the overall response was 20% with a median progression-free survival of 2.9 months.
Dr. Seto noted that there was no known biological explanation for the observed discrepancy in response rate or survival.
Dr. Seto reported that the safety profile was similar to previous reports. Four patients ended treatment due to adverse events while 16 experienced dose interruptions due to treatment-related toxicities. The most common grade three and four toxicities were hypertension (58%), rash (16%), and diarrhea (11%).
In the trial headed by Dr. Lee, 18 patients with RET rearrangements (confirmed by fluorescent in situ hybridization) met the eligibility requirement of having failed platinum-based chemotherapy. The median age of the cohort was 55 years, and 33% were female.
Similar to Dr. Seto’s study, all 18 patients received vandetanib at 300 mg once daily. Of the 18 patient cohort, 17% achieved partial remission and 44% achieved stable disease. Seven patients had no remission or stabilization. There were no treatment-related mortalities or grade 4 adverse events. Two grade 3 adverse events were reported.
“Looking at these two studies together, I think the important thing about the characteristics you see [is] that the age range is very similar [with a] median in the 50’s,” commented Dr. Reckamp. “The male to female ratio is actually opposite in both so [this] can occur in both men and women. The smoking status, interestingly is similar in both, where about a third of patients were former smokers. Most of the patients had adenocarcinoma. Many of these patients were highly previously treated. Only the Seto group looked at RET fusion partner, which may be important in looking at efficacy for these agents.” Vandetanib is a “challenging drug to tolerate,” Dr. Reckamp also noted.
“Is there a preferred RET inhibitor in small cell lung cancer?” Dr. Reckamp asked. “There are many RET inhibitors approved for other cancer types at this point, and they are multitargeted tyrosine kinases. In small studies they have similar efficacy. Toxicities vary because of the off-target effects, and most of the [treatment] decisions were made based on potential toxicities rather than differing efficacy. So none is really differentiated as the best choice, and it is unlikely that we are going to have the trials to evaluate them head to head.”
Dr. Reckamp suggested that “most patients with adenocarcinoma” should be tested for RET rearrangements. “Both men and women, both smokers and nonsmokers. And if you don’t test, you won’t find it. And if you don’t find it, you won’t be able to treat.” Dr. Reckamp also noted that next generation sequencing (NGS) should be the preferred method of identifying RET status because NGS uses less tissue, provides genetic sequencing, and allows for the identification of binding partners.
“Does targeting RET improve patient outcomes?” she continued. “Because that is really the question we need to answer if we need to move forward with RET inhibition for lung cancer. So there are variable response rates, less than other inhibitors of other oncogenic-driven tumors, that’s for sure... But if you look at the data, and these are [for] heavily pretreated patients for the most part, the response rates are better than second-line cytotoxic chemotherapy that we have had in the past and similar to unselected checkpoint inhibition. So there is potential for improving outcomes, and again if we don’t know someone is RET, we potentially are not going to offer a treatment that could help them live longer or better.”
When asked how she would treat a newly-diagnosed patient with RET-positive NSCLC, Dr. Reckamp said she would treat with first-line chemotherapy rather than a tyrosine kinase inhibitor (TKI) but would enroll the patient in whatever TKI trial was ongoing at that point in time.
“There are multiple trials that are ongoing,” Dr. Reckamp said. “It is unlikely that a comparison trial will be completed and so we are going to have to look at these trials next to each other and differentiate based on toxicity [and] perceived efficacy.”
Specifically, Dr. Reckamp believes the medical community needs to move toward “universal testing” for RET status in lung cancer patients. Resistance and combination therapies will also need to be assessed in future studies.
“RET is important in lung cancer, and should be targeted. We now need to find the best way to do that,” Dr. Reckamp concluded.
The trial headed by Dr. Seto was funded by the Japan Agency for Medical Research and Development, AMED, and AstraZeneca. Dr. Seto reported receiving honoraria and research funding from multiple companies including AstraZeneca. The trial headed by Dr. Lee was funded by AstraZeneca Korea. Dr. Lee reported having a consulting or advisory role and receiving honoraria and research funding from AstraZeneca, Pfizer, and Roche/Genentech.
CHICAGO – The RET tyrosine kinase inhibitor vandetanib shows marked yet variable antitumor activity and toxicity in patients whose RET-positive non–small cell lung cancer (NSCLC) was unsuccessfully treated with chemotherapy, according to results of two small phase II trials presented at the annual meeting of the American Society of Clinical Oncology.
The overall response rates were 53% and 61% in two independent trials conducted by Dr. Takashi Seto of the National Kyushu Cancer Center, Japan, and by Dr. Se-Hoon Lee of Sungkyunkwan University, South Korea, respectively.
Compared to previous studies with other RET inhibitors, though all had small cohorts, there were many similarities in response rates. Progression-free survival was the most variable, but was much higher in the cabozantinib data reported at the 2015 ASCO annual meeting, according to moderator Dr. Karen Reckamp of the City of Hope Comprehensive Cancer Center, Duarte, Calif. “Vandetanib may have lower response rates than some of the others,” she said.
RET is a tyrosine kinase domain that fuses to and undergoes rearrangements with KIF5B and CCDC6 genes. This fusion and subsequent rearrangement results in ligand-dependent dimerization, which causes tumor growth. RET rearrangements were first identified in thyroid cancers.
“RET fusions were identified as new driver oncogenes of NSCLC in 2012 and observed in 1%-2% of all NSCLC,” Dr. Seto said. “Non–small cell lung cancer with RET rearrangement is regarded as a unique entity in terms of pathogenesis,” said Dr. Lee. There are currently multiple RET inhibitors in various stages of development.
In the trial headed by Dr. Seto, the Japanese genetic screening network was utilized to identify 34 NSCLC patients with RET rearrangements. Among the 34 patients, 17 met the eligibility requirements of having failed at least one prior chemotherapy treatment. Of those 17 patients, the median age was 59 years, 74% were female, all had adenocarcinomas, and 68% were nonsmokers.
All 17 patients received vandetanib at a dose of 300 mg once daily. The overall response rate was 53% (90% confidence interval, 31-74), and the disease control rate was 88%. The median progression-free survival was 4.7 months (90% CI, 2.8-8.3).
There was a marked difference in overall response rate and progression-free survival among RET fusion subtypes. For CCDC6-RET, the overall response was 83% and the progression-free survival was 8.3 months. For KIF5B-RET, the overall response was 20% with a median progression-free survival of 2.9 months.
Dr. Seto noted that there was no known biological explanation for the observed discrepancy in response rate or survival.
Dr. Seto reported that the safety profile was similar to previous reports. Four patients ended treatment due to adverse events while 16 experienced dose interruptions due to treatment-related toxicities. The most common grade three and four toxicities were hypertension (58%), rash (16%), and diarrhea (11%).
In the trial headed by Dr. Lee, 18 patients with RET rearrangements (confirmed by fluorescent in situ hybridization) met the eligibility requirement of having failed platinum-based chemotherapy. The median age of the cohort was 55 years, and 33% were female.
Similar to Dr. Seto’s study, all 18 patients received vandetanib at 300 mg once daily. Of the 18 patient cohort, 17% achieved partial remission and 44% achieved stable disease. Seven patients had no remission or stabilization. There were no treatment-related mortalities or grade 4 adverse events. Two grade 3 adverse events were reported.
“Looking at these two studies together, I think the important thing about the characteristics you see [is] that the age range is very similar [with a] median in the 50’s,” commented Dr. Reckamp. “The male to female ratio is actually opposite in both so [this] can occur in both men and women. The smoking status, interestingly is similar in both, where about a third of patients were former smokers. Most of the patients had adenocarcinoma. Many of these patients were highly previously treated. Only the Seto group looked at RET fusion partner, which may be important in looking at efficacy for these agents.” Vandetanib is a “challenging drug to tolerate,” Dr. Reckamp also noted.
“Is there a preferred RET inhibitor in small cell lung cancer?” Dr. Reckamp asked. “There are many RET inhibitors approved for other cancer types at this point, and they are multitargeted tyrosine kinases. In small studies they have similar efficacy. Toxicities vary because of the off-target effects, and most of the [treatment] decisions were made based on potential toxicities rather than differing efficacy. So none is really differentiated as the best choice, and it is unlikely that we are going to have the trials to evaluate them head to head.”
Dr. Reckamp suggested that “most patients with adenocarcinoma” should be tested for RET rearrangements. “Both men and women, both smokers and nonsmokers. And if you don’t test, you won’t find it. And if you don’t find it, you won’t be able to treat.” Dr. Reckamp also noted that next generation sequencing (NGS) should be the preferred method of identifying RET status because NGS uses less tissue, provides genetic sequencing, and allows for the identification of binding partners.
“Does targeting RET improve patient outcomes?” she continued. “Because that is really the question we need to answer if we need to move forward with RET inhibition for lung cancer. So there are variable response rates, less than other inhibitors of other oncogenic-driven tumors, that’s for sure... But if you look at the data, and these are [for] heavily pretreated patients for the most part, the response rates are better than second-line cytotoxic chemotherapy that we have had in the past and similar to unselected checkpoint inhibition. So there is potential for improving outcomes, and again if we don’t know someone is RET, we potentially are not going to offer a treatment that could help them live longer or better.”
When asked how she would treat a newly-diagnosed patient with RET-positive NSCLC, Dr. Reckamp said she would treat with first-line chemotherapy rather than a tyrosine kinase inhibitor (TKI) but would enroll the patient in whatever TKI trial was ongoing at that point in time.
“There are multiple trials that are ongoing,” Dr. Reckamp said. “It is unlikely that a comparison trial will be completed and so we are going to have to look at these trials next to each other and differentiate based on toxicity [and] perceived efficacy.”
Specifically, Dr. Reckamp believes the medical community needs to move toward “universal testing” for RET status in lung cancer patients. Resistance and combination therapies will also need to be assessed in future studies.
“RET is important in lung cancer, and should be targeted. We now need to find the best way to do that,” Dr. Reckamp concluded.
The trial headed by Dr. Seto was funded by the Japan Agency for Medical Research and Development, AMED, and AstraZeneca. Dr. Seto reported receiving honoraria and research funding from multiple companies including AstraZeneca. The trial headed by Dr. Lee was funded by AstraZeneca Korea. Dr. Lee reported having a consulting or advisory role and receiving honoraria and research funding from AstraZeneca, Pfizer, and Roche/Genentech.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Vandetanib shows marked yet variable anti-tumor activity and toxicity in patients with RET-rearranged NSCLC.
Major finding: The overall response rates were 53% and 61% in two independent trials.
Data source: Two independently-conducted multicenter phase II trials of patients with RET-rearranged non-small cell lung cancer.
Disclosures: The trial headed by Dr. Seto was funded by the Japan Agency for Medical Research and Development, AMED, and AstraZeneca. Dr. Seto reported receiving honoraria and research funding from multiple companies including AstraZeneca. The trial headed by Dr. Lee was funded by AstraZeneca Korea Ltd. Dr. Lee reported having a consulting or advisory role and receiving honoraria and research funding from AstraZeneca, Pfizer, and Roche/Genentech.
Cancer drugs most affordable in Australia, least in India and China
CHICAGO – Cancer drugs are most expensive in the United States and least expensive in India and South Africa, but when taking into account a nation’s wealth and cost of living, the treatments are most affordable in Australia, and least affordable in India and China. The United States is somewhat in between, according to an analysis presented at the annual meeting of the American Society of Clinical Oncology.
“Value has become a major buzzword in cancer care. In addition to existing methods of cost effectiveness, new frameworks have been developed by ASCO, [the National Comprehensive Cancer Network], [the European Society for Medical Oncology], and [the American Board of Internal Medicine]. However, ultimately value boils down to a simple equation,” said Dr. Daniel A. Goldstein of Rabin Medical Center, Petah Tikva, Israel.
“Value is benefit divided by cost. In this study, we interrogated the denominator in this equation. Cost. And we did this on a global perspective.”
Dr. Goldstein and his associates collected drug prices of 15 generic and 8 patented drugs and calculated retail prices in seven countries (Australia, India, China, South Africa, Israel, the United Kingdom, and the United States) for 1 month of therapy using a standardized body surface area to determine dosage. The United States had the highest median monthly retail prices at just under $9,000 for patented drugs. China, Israel, the U.K., and Australia had similar median monthly retail prices that were just under $3,000. India and South Africa had the lowest median monthly retail prices for patented drugs.
Median monthly generic retail prices were fairly similar across the seven countries.
“It is currently unclear how the difference in prices relates to ability to pay for payers in different countries,” Dr. Goldstein said. To assess affordability, the investigators calculated the monthly drug price as a percentage of gross domestic product per capita at purchasing power parity (GDPcap), a measurement that takes into account a nation’s wealth and cost of living.
Cancer drugs were the most affordable in Australia. Monthly drug prices were 3% of GDPcap for generics and 71% for patented drugs. In the United States, the cost of generics was 14% of GDPcap while patented drugs were 192% of GDPcap. Cancer drugs were least affordable in India and China. Monthly drug prices were 48% of GDPcap for generic drugs in China, 288% for patented drugs, 33% for generic drugs in India, and 313% for patented drugs.
“Despite lower drug prices in India and China, these drugs appear to be less affordable than in other countries. In the USA despite having the highest GDP per capita, given the higher drug prices, the drugs appear to be less affordable than in other developed countries. And we see a similar pattern for generic drugs but with a lower magnitude. And this is mostly driven by differences in GDP per capita rather than differences in drug prices,” Dr. Rabin said.
“This is a very interesting international comparative study, and I think the concept of affordability is a novel one because we tend to just look at the cost and say it is so much less expensive in other parts of the world but looking at affordability adds another dimension to the many nuanced issues [of cost],” commented moderator Dr. Patricia Ganz of the University of California, Los Angeles.
A major limitation of this study was the inability to implicate the role of health insurance, drug discounts, rebates, and medical assistance programs into affordability. In response to a question from a reporter, Dr. Goldstein said that wealth disparities within countries would also be an important factor to more thoroughly understand the ability of patients to pay for cancer treatments.
Dr. Goldstein added that a better understanding of a drug’s benefit (improvements on life expectancy, toxicity, duration of therapy, and so on) is also important to truly understand the value of drugs on a global level.
“There are several questions this study does not answer,” Dr. Goldstein said. “Should drugs be priced the same globally? Is there an ethical duty to price drugs relative to an individual or population’s level of wealth? And is there a difference between drugs used in curative and metastatic setting[s]? Should governments or insurance companies provide all drugs with proven efficacy?”
This study was unfunded. Dr. Goldstein had no relevant disclosures to report. One coauthor disclosed a consulting or advisory role with Novartis, and travel, accommodations, or expenses from Genomic Health.
CHICAGO – Cancer drugs are most expensive in the United States and least expensive in India and South Africa, but when taking into account a nation’s wealth and cost of living, the treatments are most affordable in Australia, and least affordable in India and China. The United States is somewhat in between, according to an analysis presented at the annual meeting of the American Society of Clinical Oncology.
“Value has become a major buzzword in cancer care. In addition to existing methods of cost effectiveness, new frameworks have been developed by ASCO, [the National Comprehensive Cancer Network], [the European Society for Medical Oncology], and [the American Board of Internal Medicine]. However, ultimately value boils down to a simple equation,” said Dr. Daniel A. Goldstein of Rabin Medical Center, Petah Tikva, Israel.
“Value is benefit divided by cost. In this study, we interrogated the denominator in this equation. Cost. And we did this on a global perspective.”
Dr. Goldstein and his associates collected drug prices of 15 generic and 8 patented drugs and calculated retail prices in seven countries (Australia, India, China, South Africa, Israel, the United Kingdom, and the United States) for 1 month of therapy using a standardized body surface area to determine dosage. The United States had the highest median monthly retail prices at just under $9,000 for patented drugs. China, Israel, the U.K., and Australia had similar median monthly retail prices that were just under $3,000. India and South Africa had the lowest median monthly retail prices for patented drugs.
Median monthly generic retail prices were fairly similar across the seven countries.
“It is currently unclear how the difference in prices relates to ability to pay for payers in different countries,” Dr. Goldstein said. To assess affordability, the investigators calculated the monthly drug price as a percentage of gross domestic product per capita at purchasing power parity (GDPcap), a measurement that takes into account a nation’s wealth and cost of living.
Cancer drugs were the most affordable in Australia. Monthly drug prices were 3% of GDPcap for generics and 71% for patented drugs. In the United States, the cost of generics was 14% of GDPcap while patented drugs were 192% of GDPcap. Cancer drugs were least affordable in India and China. Monthly drug prices were 48% of GDPcap for generic drugs in China, 288% for patented drugs, 33% for generic drugs in India, and 313% for patented drugs.
“Despite lower drug prices in India and China, these drugs appear to be less affordable than in other countries. In the USA despite having the highest GDP per capita, given the higher drug prices, the drugs appear to be less affordable than in other developed countries. And we see a similar pattern for generic drugs but with a lower magnitude. And this is mostly driven by differences in GDP per capita rather than differences in drug prices,” Dr. Rabin said.
“This is a very interesting international comparative study, and I think the concept of affordability is a novel one because we tend to just look at the cost and say it is so much less expensive in other parts of the world but looking at affordability adds another dimension to the many nuanced issues [of cost],” commented moderator Dr. Patricia Ganz of the University of California, Los Angeles.
A major limitation of this study was the inability to implicate the role of health insurance, drug discounts, rebates, and medical assistance programs into affordability. In response to a question from a reporter, Dr. Goldstein said that wealth disparities within countries would also be an important factor to more thoroughly understand the ability of patients to pay for cancer treatments.
Dr. Goldstein added that a better understanding of a drug’s benefit (improvements on life expectancy, toxicity, duration of therapy, and so on) is also important to truly understand the value of drugs on a global level.
“There are several questions this study does not answer,” Dr. Goldstein said. “Should drugs be priced the same globally? Is there an ethical duty to price drugs relative to an individual or population’s level of wealth? And is there a difference between drugs used in curative and metastatic setting[s]? Should governments or insurance companies provide all drugs with proven efficacy?”
This study was unfunded. Dr. Goldstein had no relevant disclosures to report. One coauthor disclosed a consulting or advisory role with Novartis, and travel, accommodations, or expenses from Genomic Health.
CHICAGO – Cancer drugs are most expensive in the United States and least expensive in India and South Africa, but when taking into account a nation’s wealth and cost of living, the treatments are most affordable in Australia, and least affordable in India and China. The United States is somewhat in between, according to an analysis presented at the annual meeting of the American Society of Clinical Oncology.
“Value has become a major buzzword in cancer care. In addition to existing methods of cost effectiveness, new frameworks have been developed by ASCO, [the National Comprehensive Cancer Network], [the European Society for Medical Oncology], and [the American Board of Internal Medicine]. However, ultimately value boils down to a simple equation,” said Dr. Daniel A. Goldstein of Rabin Medical Center, Petah Tikva, Israel.
“Value is benefit divided by cost. In this study, we interrogated the denominator in this equation. Cost. And we did this on a global perspective.”
Dr. Goldstein and his associates collected drug prices of 15 generic and 8 patented drugs and calculated retail prices in seven countries (Australia, India, China, South Africa, Israel, the United Kingdom, and the United States) for 1 month of therapy using a standardized body surface area to determine dosage. The United States had the highest median monthly retail prices at just under $9,000 for patented drugs. China, Israel, the U.K., and Australia had similar median monthly retail prices that were just under $3,000. India and South Africa had the lowest median monthly retail prices for patented drugs.
Median monthly generic retail prices were fairly similar across the seven countries.
“It is currently unclear how the difference in prices relates to ability to pay for payers in different countries,” Dr. Goldstein said. To assess affordability, the investigators calculated the monthly drug price as a percentage of gross domestic product per capita at purchasing power parity (GDPcap), a measurement that takes into account a nation’s wealth and cost of living.
Cancer drugs were the most affordable in Australia. Monthly drug prices were 3% of GDPcap for generics and 71% for patented drugs. In the United States, the cost of generics was 14% of GDPcap while patented drugs were 192% of GDPcap. Cancer drugs were least affordable in India and China. Monthly drug prices were 48% of GDPcap for generic drugs in China, 288% for patented drugs, 33% for generic drugs in India, and 313% for patented drugs.
“Despite lower drug prices in India and China, these drugs appear to be less affordable than in other countries. In the USA despite having the highest GDP per capita, given the higher drug prices, the drugs appear to be less affordable than in other developed countries. And we see a similar pattern for generic drugs but with a lower magnitude. And this is mostly driven by differences in GDP per capita rather than differences in drug prices,” Dr. Rabin said.
“This is a very interesting international comparative study, and I think the concept of affordability is a novel one because we tend to just look at the cost and say it is so much less expensive in other parts of the world but looking at affordability adds another dimension to the many nuanced issues [of cost],” commented moderator Dr. Patricia Ganz of the University of California, Los Angeles.
A major limitation of this study was the inability to implicate the role of health insurance, drug discounts, rebates, and medical assistance programs into affordability. In response to a question from a reporter, Dr. Goldstein said that wealth disparities within countries would also be an important factor to more thoroughly understand the ability of patients to pay for cancer treatments.
Dr. Goldstein added that a better understanding of a drug’s benefit (improvements on life expectancy, toxicity, duration of therapy, and so on) is also important to truly understand the value of drugs on a global level.
“There are several questions this study does not answer,” Dr. Goldstein said. “Should drugs be priced the same globally? Is there an ethical duty to price drugs relative to an individual or population’s level of wealth? And is there a difference between drugs used in curative and metastatic setting[s]? Should governments or insurance companies provide all drugs with proven efficacy?”
This study was unfunded. Dr. Goldstein had no relevant disclosures to report. One coauthor disclosed a consulting or advisory role with Novartis, and travel, accommodations, or expenses from Genomic Health.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Taking into account a country’s wealth and cost of living, cancer drugs are most affordable in Australia, least affordable in India and China.
Major finding: In Australia, monthly drug prices were 3% of gross domestic product per capita at purchasing power parity (GDPcap) for generics and 71% for patented drugs. Monthly drug prices in China were 48% of GDPcap for generic drugs and 288% for patented drugs, while in India prices were 33% of GDPcap for generic drugs and 313% for patented drugs.
Data source: A multinational study of cancer drug prices, wealth, and cost of living.
Disclosures: This study was unfunded. Dr. Goldstein had no relevant disclosures to report. One coauthor disclosed a consulting or advisory role with Novartis, and travel, accommodations, or expenses from Genomic Health.