User login
Two skin problems related or not?
HISTORY
A 36-year-old man self-refers to dermatology with two complaints. The more serious is the very itchy rash present on his back for several weeks. He has tried treating it with several OTC creams, including 1% hydrocortisone, triple-antibiotic, and diphenhydramine. The hydrocortisone cream provided some short-term relief from the itching, but over time, the rash has grown and become more symptomatic.
The condition affecting his feet has caused little in the way of symptoms. However, it has caused quite a stir in the family; every night, on returning from work, the patient removes his shoes, releasing a pervasive, highly objectionable odor. It didn’t take long for his family to insist that he remove his shoes in the backyard, where he is to remain until the odor clears a bit. The patient is also concerned about a “spongy” feeling the soles of his feet have acquired along with the odor. Neither symptom has responded to topical OTC products, such as athlete’s foot cream (tonaftate) and spray or calamine lotion; lengthy soaks in bleach-containing water have not helped, either.
The patient claims to be in reasonably good health. He is working in a new job, repairing air conditioners on the roofs of commercial buildings.
EXAMINATION
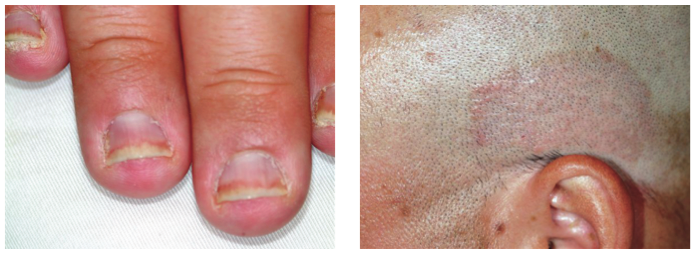
An impressive rash is seen on the patient’s upper back, extending from the hairline to mid-back, with a long, curved papulosquamous border on its inferior aspect. Aside from the soles of his feet, the only other skin abnormality is a faintly erythematous rash around the rims of both feet. KOH examination reveals these patches to be loaded with fungal elements.
Both soles have a spongy, whitish look, with focal areas of punctuate crateriform and arciform superficial loss of the outer keratin layer of skin. But there is no erythema or no tenderness on palpation.
DISCUSSION
Daily exposure to constant sweat and heat is responsible for all of this man’s skin problems, although there are two different conditions involved. Tinea corporis is the explanation for the extensive rash on his upper back. However, the repeated application of topical steroids is the likely explanation for the astonishing size and scope of the rash, since steroids (even 1% hydrocortisone!) blunt the body’s immune response to this superficial dermatophytosis. As is often the case, this outbreak was so large it was hard to see. Heat and sweat might be the immediate cause, but what about the source?
The fungal organisms on the rims of his feet, probably present asymptomatically (and unrecognized) for years, provide a clue to the patient’s susceptibility to this class of organisms. Trichophyton rubrum is by far the most common cause; given enough heat, sweat, and steroids, it can easily spread to other areas of the body.
Now to the feet, where antifungal cream (tolnaftate) and bleach had no good effect: The name given to this common condition is pitted keratolysis (PK). PK is caused by several bacterial organisms that thrive in this hot, humid environment, feeding on the keratin layer and producing the pattern seen. The most common bacteria involved is Kytococcus sedentarius, but all are part of normal gram-positive flora and are also responsible for the powerful odor noted in many—though not all—cases. Since the organism feeds on lifeless keratin and causes no inflammatory response or symptoms, PK is not really an “infection” in the sense that we normally use this word.
TREATMENT AND PROGNOSIS
PK is successfully treated with a combination of topically applied antiperspirant (such as prescription-strength aluminum chloride, or OTC antiperspirant with aluminum chorhydroxide) and topical clindamycin 2% solution. Though an endpoint is unlikely with these treatments, control is possible.
The same could be said for the steroid-exacerbated tinea corporis on the patient’s back, since the conditions that lead to its appearance will still be present. Given the severity and symptomatic nature of this eruption, I gave the patient oral terbinafine (250 mg bid for 10 days) plus topical econazole cream (bid until the rash is clear). For maintenance, he’ll use OTC ketoconazole shampoo as a body wash, to reduce the numbers of these organisms.
During the winter, both of these conditions will abate sharply, only to reappear when the weather heats up in the spring. Patient education is necessary as to this aspect of both conditions, including their prognoses.
For the provider, this case highlights, once again, the difficulty that dermatologic complaints present. PK, for example, looks very much as though it should “have a name,” but neither its name nor its origins nor remedies will be clear if the requisite time has not been spent learning about it in advance of its inevitable sighting.
HISTORY
A 36-year-old man self-refers to dermatology with two complaints. The more serious is the very itchy rash present on his back for several weeks. He has tried treating it with several OTC creams, including 1% hydrocortisone, triple-antibiotic, and diphenhydramine. The hydrocortisone cream provided some short-term relief from the itching, but over time, the rash has grown and become more symptomatic.
The condition affecting his feet has caused little in the way of symptoms. However, it has caused quite a stir in the family; every night, on returning from work, the patient removes his shoes, releasing a pervasive, highly objectionable odor. It didn’t take long for his family to insist that he remove his shoes in the backyard, where he is to remain until the odor clears a bit. The patient is also concerned about a “spongy” feeling the soles of his feet have acquired along with the odor. Neither symptom has responded to topical OTC products, such as athlete’s foot cream (tonaftate) and spray or calamine lotion; lengthy soaks in bleach-containing water have not helped, either.
The patient claims to be in reasonably good health. He is working in a new job, repairing air conditioners on the roofs of commercial buildings.
EXAMINATION
An impressive rash is seen on the patient’s upper back, extending from the hairline to mid-back, with a long, curved papulosquamous border on its inferior aspect. Aside from the soles of his feet, the only other skin abnormality is a faintly erythematous rash around the rims of both feet. KOH examination reveals these patches to be loaded with fungal elements.
Both soles have a spongy, whitish look, with focal areas of punctuate crateriform and arciform superficial loss of the outer keratin layer of skin. But there is no erythema or no tenderness on palpation.
DISCUSSION
Daily exposure to constant sweat and heat is responsible for all of this man’s skin problems, although there are two different conditions involved. Tinea corporis is the explanation for the extensive rash on his upper back. However, the repeated application of topical steroids is the likely explanation for the astonishing size and scope of the rash, since steroids (even 1% hydrocortisone!) blunt the body’s immune response to this superficial dermatophytosis. As is often the case, this outbreak was so large it was hard to see. Heat and sweat might be the immediate cause, but what about the source?
The fungal organisms on the rims of his feet, probably present asymptomatically (and unrecognized) for years, provide a clue to the patient’s susceptibility to this class of organisms. Trichophyton rubrum is by far the most common cause; given enough heat, sweat, and steroids, it can easily spread to other areas of the body.
Now to the feet, where antifungal cream (tolnaftate) and bleach had no good effect: The name given to this common condition is pitted keratolysis (PK). PK is caused by several bacterial organisms that thrive in this hot, humid environment, feeding on the keratin layer and producing the pattern seen. The most common bacteria involved is Kytococcus sedentarius, but all are part of normal gram-positive flora and are also responsible for the powerful odor noted in many—though not all—cases. Since the organism feeds on lifeless keratin and causes no inflammatory response or symptoms, PK is not really an “infection” in the sense that we normally use this word.
TREATMENT AND PROGNOSIS
PK is successfully treated with a combination of topically applied antiperspirant (such as prescription-strength aluminum chloride, or OTC antiperspirant with aluminum chorhydroxide) and topical clindamycin 2% solution. Though an endpoint is unlikely with these treatments, control is possible.
The same could be said for the steroid-exacerbated tinea corporis on the patient’s back, since the conditions that lead to its appearance will still be present. Given the severity and symptomatic nature of this eruption, I gave the patient oral terbinafine (250 mg bid for 10 days) plus topical econazole cream (bid until the rash is clear). For maintenance, he’ll use OTC ketoconazole shampoo as a body wash, to reduce the numbers of these organisms.
During the winter, both of these conditions will abate sharply, only to reappear when the weather heats up in the spring. Patient education is necessary as to this aspect of both conditions, including their prognoses.
For the provider, this case highlights, once again, the difficulty that dermatologic complaints present. PK, for example, looks very much as though it should “have a name,” but neither its name nor its origins nor remedies will be clear if the requisite time has not been spent learning about it in advance of its inevitable sighting.
HISTORY
A 36-year-old man self-refers to dermatology with two complaints. The more serious is the very itchy rash present on his back for several weeks. He has tried treating it with several OTC creams, including 1% hydrocortisone, triple-antibiotic, and diphenhydramine. The hydrocortisone cream provided some short-term relief from the itching, but over time, the rash has grown and become more symptomatic.
The condition affecting his feet has caused little in the way of symptoms. However, it has caused quite a stir in the family; every night, on returning from work, the patient removes his shoes, releasing a pervasive, highly objectionable odor. It didn’t take long for his family to insist that he remove his shoes in the backyard, where he is to remain until the odor clears a bit. The patient is also concerned about a “spongy” feeling the soles of his feet have acquired along with the odor. Neither symptom has responded to topical OTC products, such as athlete’s foot cream (tonaftate) and spray or calamine lotion; lengthy soaks in bleach-containing water have not helped, either.
The patient claims to be in reasonably good health. He is working in a new job, repairing air conditioners on the roofs of commercial buildings.
EXAMINATION
An impressive rash is seen on the patient’s upper back, extending from the hairline to mid-back, with a long, curved papulosquamous border on its inferior aspect. Aside from the soles of his feet, the only other skin abnormality is a faintly erythematous rash around the rims of both feet. KOH examination reveals these patches to be loaded with fungal elements.
Both soles have a spongy, whitish look, with focal areas of punctuate crateriform and arciform superficial loss of the outer keratin layer of skin. But there is no erythema or no tenderness on palpation.
DISCUSSION
Daily exposure to constant sweat and heat is responsible for all of this man’s skin problems, although there are two different conditions involved. Tinea corporis is the explanation for the extensive rash on his upper back. However, the repeated application of topical steroids is the likely explanation for the astonishing size and scope of the rash, since steroids (even 1% hydrocortisone!) blunt the body’s immune response to this superficial dermatophytosis. As is often the case, this outbreak was so large it was hard to see. Heat and sweat might be the immediate cause, but what about the source?
The fungal organisms on the rims of his feet, probably present asymptomatically (and unrecognized) for years, provide a clue to the patient’s susceptibility to this class of organisms. Trichophyton rubrum is by far the most common cause; given enough heat, sweat, and steroids, it can easily spread to other areas of the body.
Now to the feet, where antifungal cream (tolnaftate) and bleach had no good effect: The name given to this common condition is pitted keratolysis (PK). PK is caused by several bacterial organisms that thrive in this hot, humid environment, feeding on the keratin layer and producing the pattern seen. The most common bacteria involved is Kytococcus sedentarius, but all are part of normal gram-positive flora and are also responsible for the powerful odor noted in many—though not all—cases. Since the organism feeds on lifeless keratin and causes no inflammatory response or symptoms, PK is not really an “infection” in the sense that we normally use this word.
TREATMENT AND PROGNOSIS
PK is successfully treated with a combination of topically applied antiperspirant (such as prescription-strength aluminum chloride, or OTC antiperspirant with aluminum chorhydroxide) and topical clindamycin 2% solution. Though an endpoint is unlikely with these treatments, control is possible.
The same could be said for the steroid-exacerbated tinea corporis on the patient’s back, since the conditions that lead to its appearance will still be present. Given the severity and symptomatic nature of this eruption, I gave the patient oral terbinafine (250 mg bid for 10 days) plus topical econazole cream (bid until the rash is clear). For maintenance, he’ll use OTC ketoconazole shampoo as a body wash, to reduce the numbers of these organisms.
During the winter, both of these conditions will abate sharply, only to reappear when the weather heats up in the spring. Patient education is necessary as to this aspect of both conditions, including their prognoses.
For the provider, this case highlights, once again, the difficulty that dermatologic complaints present. PK, for example, looks very much as though it should “have a name,” but neither its name nor its origins nor remedies will be clear if the requisite time has not been spent learning about it in advance of its inevitable sighting.
Ear lesion suspicious for melanoma?
Family members bring in an 80-year-old man for urgent evaluation of a number of skin lesions. Most alarming to them is the lesion on his right ear, although many others, including numerous dark lesions on his back, have also raised their concern. The patient and his wife are “positive” all the lesions have been present, unchanged, for years.
EXAMINATION
Your attention is quickly drawn to the superior helical area of the patient’s right ear, where a large, irregularly pigmented and bordered black patch covers most of the superior helix. The surrounding skin is quite fair and sun-damaged, with extensive solar elastosis seen all across the patient’s face—especially on the forehead, where multiple actinic keratoses are also seen and felt.
Hundreds of dark brown–to-black warty epidermal papules, nodules, and plaques are observed on the patient’s trunk; some are as large as 6 cm, while most average 2 to 3 cm. Fortunately, no other worrisome lesions are seen, except for the right superior helical lesion, which appears exceptionally suspicious for melanoma.
A tray is set up for the performance of a 3-mm punch biopsy of the ear lesion. Prior to that procedure, direct examination of the lesion is carried out with a dermatoscope, a magnifying (10x power) handheld viewing device that illuminates the site with flat, polarized light. It can be used to look for specific features of benign versus malignant lesions. After the entire lesion’s surface has been examined, the biopsy is cancelled and the family reassured regarding the benignancy of the ear lesion.
DISCUSSION
One reason for the dermatoscopic examination was the size of the ear lesion; it was so large that the chance of sampling error became a definite concern. A single 3-mm punch biopsy taken from a 4-cm lesion, if negative for cancer, could simply have missed the malignancy. However, removal of the entire lesion was not at all practical. Multiple punch biopsies from several areas within the lesion would have been an acceptable, but clumsy, alternative.
Thankfully, the dermatoscopic examination results obviated the need for invasive alternatives. Here’s why: Seen with the dermatoscope, over the entire surface of the lesion, were white pinpoint spots at regular intervals, called pseudocysts. These indentations are filled with keratin and are pathognomic for the diagnosis of seborrheic keratosis (SK). Moreover, no organized collections of pigment (streaks, globules, or networks) were seen; these might have suggested melanoma. The presence of so many other SKs elsewhere lent credence to that same diagnosis on the ear.
Even though SKs are often seen in non–sun-exposed areas, there is evidence to suggest that ultraviolet exposure can play a part in their genesis. Heredity and age are arguably more significant factors; SKs are seldom seen before the fourth decade of life.
SKs have little if any malignant potential, but they have been known to coincide with sun-caused skin cancers, such as basal or squamous cell carcinoma and melanoma, with one adjacent to or even overlying the other. And while the lesions of SK are typically raised and warty (epidermal or “stuck on”), they can appear quite flat and smooth at times, in addition to occasionally being darker than SKs are “supposed to be,” increasing their resemblance to a melanoma.
Biopsy of an SK shows diagnostic features of variable papillomatosis, as well as comedone-like openings, fissures, and keratin-filled pseudocysts. The differential for SKs includes wart, melanoma, and solar lentigo.
No treatment was attempted for this helical SK. However, the patient will be monitored during twice-yearly follow-up visits to dermatology, not only for changes to his ear lesion but also for changes anywhere else on his skin.
LEARNING POINTS
• Seborrheic keratosis (SK) is the most common example of a benign epidermal (“stuck-on”) lesion.
• That “stuck-on” nature is what usually distinguishes SK from melanoma.
• However, some SKs are almost completely flat and occasionally totally black—and therefore difficult to distinguish from melanoma, especially in sebum-rich skin.
• Biopsy is often necessary, but dermatoscopic examination (in trained hands) is a useful noninvasive procedure that can obviate the need for biopsy.
Family members bring in an 80-year-old man for urgent evaluation of a number of skin lesions. Most alarming to them is the lesion on his right ear, although many others, including numerous dark lesions on his back, have also raised their concern. The patient and his wife are “positive” all the lesions have been present, unchanged, for years.
EXAMINATION
Your attention is quickly drawn to the superior helical area of the patient’s right ear, where a large, irregularly pigmented and bordered black patch covers most of the superior helix. The surrounding skin is quite fair and sun-damaged, with extensive solar elastosis seen all across the patient’s face—especially on the forehead, where multiple actinic keratoses are also seen and felt.
Hundreds of dark brown–to-black warty epidermal papules, nodules, and plaques are observed on the patient’s trunk; some are as large as 6 cm, while most average 2 to 3 cm. Fortunately, no other worrisome lesions are seen, except for the right superior helical lesion, which appears exceptionally suspicious for melanoma.
A tray is set up for the performance of a 3-mm punch biopsy of the ear lesion. Prior to that procedure, direct examination of the lesion is carried out with a dermatoscope, a magnifying (10x power) handheld viewing device that illuminates the site with flat, polarized light. It can be used to look for specific features of benign versus malignant lesions. After the entire lesion’s surface has been examined, the biopsy is cancelled and the family reassured regarding the benignancy of the ear lesion.
DISCUSSION
One reason for the dermatoscopic examination was the size of the ear lesion; it was so large that the chance of sampling error became a definite concern. A single 3-mm punch biopsy taken from a 4-cm lesion, if negative for cancer, could simply have missed the malignancy. However, removal of the entire lesion was not at all practical. Multiple punch biopsies from several areas within the lesion would have been an acceptable, but clumsy, alternative.
Thankfully, the dermatoscopic examination results obviated the need for invasive alternatives. Here’s why: Seen with the dermatoscope, over the entire surface of the lesion, were white pinpoint spots at regular intervals, called pseudocysts. These indentations are filled with keratin and are pathognomic for the diagnosis of seborrheic keratosis (SK). Moreover, no organized collections of pigment (streaks, globules, or networks) were seen; these might have suggested melanoma. The presence of so many other SKs elsewhere lent credence to that same diagnosis on the ear.
Even though SKs are often seen in non–sun-exposed areas, there is evidence to suggest that ultraviolet exposure can play a part in their genesis. Heredity and age are arguably more significant factors; SKs are seldom seen before the fourth decade of life.
SKs have little if any malignant potential, but they have been known to coincide with sun-caused skin cancers, such as basal or squamous cell carcinoma and melanoma, with one adjacent to or even overlying the other. And while the lesions of SK are typically raised and warty (epidermal or “stuck on”), they can appear quite flat and smooth at times, in addition to occasionally being darker than SKs are “supposed to be,” increasing their resemblance to a melanoma.
Biopsy of an SK shows diagnostic features of variable papillomatosis, as well as comedone-like openings, fissures, and keratin-filled pseudocysts. The differential for SKs includes wart, melanoma, and solar lentigo.
No treatment was attempted for this helical SK. However, the patient will be monitored during twice-yearly follow-up visits to dermatology, not only for changes to his ear lesion but also for changes anywhere else on his skin.
LEARNING POINTS
• Seborrheic keratosis (SK) is the most common example of a benign epidermal (“stuck-on”) lesion.
• That “stuck-on” nature is what usually distinguishes SK from melanoma.
• However, some SKs are almost completely flat and occasionally totally black—and therefore difficult to distinguish from melanoma, especially in sebum-rich skin.
• Biopsy is often necessary, but dermatoscopic examination (in trained hands) is a useful noninvasive procedure that can obviate the need for biopsy.
Family members bring in an 80-year-old man for urgent evaluation of a number of skin lesions. Most alarming to them is the lesion on his right ear, although many others, including numerous dark lesions on his back, have also raised their concern. The patient and his wife are “positive” all the lesions have been present, unchanged, for years.
EXAMINATION
Your attention is quickly drawn to the superior helical area of the patient’s right ear, where a large, irregularly pigmented and bordered black patch covers most of the superior helix. The surrounding skin is quite fair and sun-damaged, with extensive solar elastosis seen all across the patient’s face—especially on the forehead, where multiple actinic keratoses are also seen and felt.
Hundreds of dark brown–to-black warty epidermal papules, nodules, and plaques are observed on the patient’s trunk; some are as large as 6 cm, while most average 2 to 3 cm. Fortunately, no other worrisome lesions are seen, except for the right superior helical lesion, which appears exceptionally suspicious for melanoma.
A tray is set up for the performance of a 3-mm punch biopsy of the ear lesion. Prior to that procedure, direct examination of the lesion is carried out with a dermatoscope, a magnifying (10x power) handheld viewing device that illuminates the site with flat, polarized light. It can be used to look for specific features of benign versus malignant lesions. After the entire lesion’s surface has been examined, the biopsy is cancelled and the family reassured regarding the benignancy of the ear lesion.
DISCUSSION
One reason for the dermatoscopic examination was the size of the ear lesion; it was so large that the chance of sampling error became a definite concern. A single 3-mm punch biopsy taken from a 4-cm lesion, if negative for cancer, could simply have missed the malignancy. However, removal of the entire lesion was not at all practical. Multiple punch biopsies from several areas within the lesion would have been an acceptable, but clumsy, alternative.
Thankfully, the dermatoscopic examination results obviated the need for invasive alternatives. Here’s why: Seen with the dermatoscope, over the entire surface of the lesion, were white pinpoint spots at regular intervals, called pseudocysts. These indentations are filled with keratin and are pathognomic for the diagnosis of seborrheic keratosis (SK). Moreover, no organized collections of pigment (streaks, globules, or networks) were seen; these might have suggested melanoma. The presence of so many other SKs elsewhere lent credence to that same diagnosis on the ear.
Even though SKs are often seen in non–sun-exposed areas, there is evidence to suggest that ultraviolet exposure can play a part in their genesis. Heredity and age are arguably more significant factors; SKs are seldom seen before the fourth decade of life.
SKs have little if any malignant potential, but they have been known to coincide with sun-caused skin cancers, such as basal or squamous cell carcinoma and melanoma, with one adjacent to or even overlying the other. And while the lesions of SK are typically raised and warty (epidermal or “stuck on”), they can appear quite flat and smooth at times, in addition to occasionally being darker than SKs are “supposed to be,” increasing their resemblance to a melanoma.
Biopsy of an SK shows diagnostic features of variable papillomatosis, as well as comedone-like openings, fissures, and keratin-filled pseudocysts. The differential for SKs includes wart, melanoma, and solar lentigo.
No treatment was attempted for this helical SK. However, the patient will be monitored during twice-yearly follow-up visits to dermatology, not only for changes to his ear lesion but also for changes anywhere else on his skin.
LEARNING POINTS
• Seborrheic keratosis (SK) is the most common example of a benign epidermal (“stuck-on”) lesion.
• That “stuck-on” nature is what usually distinguishes SK from melanoma.
• However, some SKs are almost completely flat and occasionally totally black—and therefore difficult to distinguish from melanoma, especially in sebum-rich skin.
• Biopsy is often necessary, but dermatoscopic examination (in trained hands) is a useful noninvasive procedure that can obviate the need for biopsy.
Recurrent "rash" on eyelid cause for concern?
With her family’s encouragement, this 17-year-old girl self-refers to dermatology for a recurrent facial lesion. It has reappeared in the same location and in the same manner over the past 18 months; they suspect it is a staph infection.
First, the patient experiences localized itching and tingling in the same location on her left upper eyelid. Within a day or two, clusters of tiny blisters appear and the surrounding skin becomes erythematous. Ten days or so into the episode, the blisters begin to scab over and the redness subsides. Within two weeks, the condition totally resolves, only to reappear later.
Each time, she has been seen in an urgent care clinic, given a diagnosis of staph infection, and prescribed a 10-day course of trimethoprim/sulfa, which appears to clear the infection.
DIAGNOSIS/DISCUSSION
This case nicely illustrates the curious nature of extragenital/extralabial herpes simplex virus (HSV), which can manifest in virtually any location on the body. We can all agree that HSV far more commonly affects the lip, where a lesion such as this one would be readily recognized. But the diagnosis becomes problematic when the same blisters appear in an unfamiliar location.
Assumptions are made, often fueled by family fears, themselves fed by opinions from other well-meaning friends and acquaintances. And in such cases, treatment with antibiotics certainly appears to corroborate the diagnosis because it “works.” But the family’s nagging question of “Why?” is reasonable, and the answer telling.
The truth is, it would be quite out of the ordinary for a staph infection to present with grouped vesicles on an erythematous base, over and over again in the same location. It would also be unlike staph to merely tingle and itch, since pain and tenderness are far more typical.
If we really wanted to rule out staph infection, we would have to obtain a culture, which would not only provide an organism but also solid information about which antibiotics are likely to be effective against that particular organism. Had that been done in this case, the culture would have shown “no growth,” leaving us where we started, since a routine culture only identifies bacteria. A viral culture, taken from the vesicular fluid, would probably have proven the culprit to be herpes—but that possibility would first have to be entertained.
Had herpes been considered as a diagnosis, other corroboratory historical facts might have included the patient’s history of severe atopy, plus the fact that most of the episodes occurred during periods of increased stress. Both of these factors are well known to predispose patients to a number of skin infections—most notably, HSV. The premonitory symptoms of tingle and itch (and sometimes a bit of pain) were also instructive.
It also helps simply to know that such HSV infections are quite common (though often, as in this case, misdiagnosed). I’ve seen HSV in the scalp, on the ear, on the chest, on fingers, toes, thighs, and on the bottom of the foot. I’ve also seen it affect the eye itself, where it can cause scarring of the cornea. Fortunately, our patient had no symptoms referable to the eye. Had that been the case, referral to ophthalmology on an urgent basis would have been necessary.
Had this condition occurred only once, other items in the differential might have been considered: contact dermatitis and the blistering diseases (pemphigus, bullous pemphigoid, and others). But the recurrent nature was all but pathognomic.
TREATMENT
For this patient, there was no effective treatment for the current episode, since the acyclovir family of antivirals can only slow viral replication, which had already taken place. But I did provide a prescription for valcyclovir 500-mg capsules, dispensing 10. The patient was advised to take them twice a day for five days, starting at the earliest signs of her next episode, which should halt the progression. If the patient has more than six or eight eruptions a year, a case could be made for prophylactic medication to be taken daily.
Ultimately, the most valuable thing provided to this patient was the answer to the questions: What is this, and why does it affect me? Two good questions remain unanswered: How did she get HSV in that exact location? And how can we cure her? With a little luck, in the reader’s career, we’ll come up with a cure, just as science came up with the acyclovir family of medicines early in my career.
LEARNING POINTS
• Grouped vesicles on an erythematous base, recurring in the same location, are HSV until proven otherwise.
• HSV episodes typically last 10 to 14 days.
• Staph infections are typically painful, and rarely recur in the same locations.
• Atopy predisposes to extralabial HSV.
• There are many causes of inflammation, only one of which is infection.
• There are many types of infection that are not bacterial (eg, viral, fungal, protozoan).
With her family’s encouragement, this 17-year-old girl self-refers to dermatology for a recurrent facial lesion. It has reappeared in the same location and in the same manner over the past 18 months; they suspect it is a staph infection.
First, the patient experiences localized itching and tingling in the same location on her left upper eyelid. Within a day or two, clusters of tiny blisters appear and the surrounding skin becomes erythematous. Ten days or so into the episode, the blisters begin to scab over and the redness subsides. Within two weeks, the condition totally resolves, only to reappear later.
Each time, she has been seen in an urgent care clinic, given a diagnosis of staph infection, and prescribed a 10-day course of trimethoprim/sulfa, which appears to clear the infection.
DIAGNOSIS/DISCUSSION
This case nicely illustrates the curious nature of extragenital/extralabial herpes simplex virus (HSV), which can manifest in virtually any location on the body. We can all agree that HSV far more commonly affects the lip, where a lesion such as this one would be readily recognized. But the diagnosis becomes problematic when the same blisters appear in an unfamiliar location.
Assumptions are made, often fueled by family fears, themselves fed by opinions from other well-meaning friends and acquaintances. And in such cases, treatment with antibiotics certainly appears to corroborate the diagnosis because it “works.” But the family’s nagging question of “Why?” is reasonable, and the answer telling.
The truth is, it would be quite out of the ordinary for a staph infection to present with grouped vesicles on an erythematous base, over and over again in the same location. It would also be unlike staph to merely tingle and itch, since pain and tenderness are far more typical.
If we really wanted to rule out staph infection, we would have to obtain a culture, which would not only provide an organism but also solid information about which antibiotics are likely to be effective against that particular organism. Had that been done in this case, the culture would have shown “no growth,” leaving us where we started, since a routine culture only identifies bacteria. A viral culture, taken from the vesicular fluid, would probably have proven the culprit to be herpes—but that possibility would first have to be entertained.
Had herpes been considered as a diagnosis, other corroboratory historical facts might have included the patient’s history of severe atopy, plus the fact that most of the episodes occurred during periods of increased stress. Both of these factors are well known to predispose patients to a number of skin infections—most notably, HSV. The premonitory symptoms of tingle and itch (and sometimes a bit of pain) were also instructive.
It also helps simply to know that such HSV infections are quite common (though often, as in this case, misdiagnosed). I’ve seen HSV in the scalp, on the ear, on the chest, on fingers, toes, thighs, and on the bottom of the foot. I’ve also seen it affect the eye itself, where it can cause scarring of the cornea. Fortunately, our patient had no symptoms referable to the eye. Had that been the case, referral to ophthalmology on an urgent basis would have been necessary.
Had this condition occurred only once, other items in the differential might have been considered: contact dermatitis and the blistering diseases (pemphigus, bullous pemphigoid, and others). But the recurrent nature was all but pathognomic.
TREATMENT
For this patient, there was no effective treatment for the current episode, since the acyclovir family of antivirals can only slow viral replication, which had already taken place. But I did provide a prescription for valcyclovir 500-mg capsules, dispensing 10. The patient was advised to take them twice a day for five days, starting at the earliest signs of her next episode, which should halt the progression. If the patient has more than six or eight eruptions a year, a case could be made for prophylactic medication to be taken daily.
Ultimately, the most valuable thing provided to this patient was the answer to the questions: What is this, and why does it affect me? Two good questions remain unanswered: How did she get HSV in that exact location? And how can we cure her? With a little luck, in the reader’s career, we’ll come up with a cure, just as science came up with the acyclovir family of medicines early in my career.
LEARNING POINTS
• Grouped vesicles on an erythematous base, recurring in the same location, are HSV until proven otherwise.
• HSV episodes typically last 10 to 14 days.
• Staph infections are typically painful, and rarely recur in the same locations.
• Atopy predisposes to extralabial HSV.
• There are many causes of inflammation, only one of which is infection.
• There are many types of infection that are not bacterial (eg, viral, fungal, protozoan).
With her family’s encouragement, this 17-year-old girl self-refers to dermatology for a recurrent facial lesion. It has reappeared in the same location and in the same manner over the past 18 months; they suspect it is a staph infection.
First, the patient experiences localized itching and tingling in the same location on her left upper eyelid. Within a day or two, clusters of tiny blisters appear and the surrounding skin becomes erythematous. Ten days or so into the episode, the blisters begin to scab over and the redness subsides. Within two weeks, the condition totally resolves, only to reappear later.
Each time, she has been seen in an urgent care clinic, given a diagnosis of staph infection, and prescribed a 10-day course of trimethoprim/sulfa, which appears to clear the infection.
DIAGNOSIS/DISCUSSION
This case nicely illustrates the curious nature of extragenital/extralabial herpes simplex virus (HSV), which can manifest in virtually any location on the body. We can all agree that HSV far more commonly affects the lip, where a lesion such as this one would be readily recognized. But the diagnosis becomes problematic when the same blisters appear in an unfamiliar location.
Assumptions are made, often fueled by family fears, themselves fed by opinions from other well-meaning friends and acquaintances. And in such cases, treatment with antibiotics certainly appears to corroborate the diagnosis because it “works.” But the family’s nagging question of “Why?” is reasonable, and the answer telling.
The truth is, it would be quite out of the ordinary for a staph infection to present with grouped vesicles on an erythematous base, over and over again in the same location. It would also be unlike staph to merely tingle and itch, since pain and tenderness are far more typical.
If we really wanted to rule out staph infection, we would have to obtain a culture, which would not only provide an organism but also solid information about which antibiotics are likely to be effective against that particular organism. Had that been done in this case, the culture would have shown “no growth,” leaving us where we started, since a routine culture only identifies bacteria. A viral culture, taken from the vesicular fluid, would probably have proven the culprit to be herpes—but that possibility would first have to be entertained.
Had herpes been considered as a diagnosis, other corroboratory historical facts might have included the patient’s history of severe atopy, plus the fact that most of the episodes occurred during periods of increased stress. Both of these factors are well known to predispose patients to a number of skin infections—most notably, HSV. The premonitory symptoms of tingle and itch (and sometimes a bit of pain) were also instructive.
It also helps simply to know that such HSV infections are quite common (though often, as in this case, misdiagnosed). I’ve seen HSV in the scalp, on the ear, on the chest, on fingers, toes, thighs, and on the bottom of the foot. I’ve also seen it affect the eye itself, where it can cause scarring of the cornea. Fortunately, our patient had no symptoms referable to the eye. Had that been the case, referral to ophthalmology on an urgent basis would have been necessary.
Had this condition occurred only once, other items in the differential might have been considered: contact dermatitis and the blistering diseases (pemphigus, bullous pemphigoid, and others). But the recurrent nature was all but pathognomic.
TREATMENT
For this patient, there was no effective treatment for the current episode, since the acyclovir family of antivirals can only slow viral replication, which had already taken place. But I did provide a prescription for valcyclovir 500-mg capsules, dispensing 10. The patient was advised to take them twice a day for five days, starting at the earliest signs of her next episode, which should halt the progression. If the patient has more than six or eight eruptions a year, a case could be made for prophylactic medication to be taken daily.
Ultimately, the most valuable thing provided to this patient was the answer to the questions: What is this, and why does it affect me? Two good questions remain unanswered: How did she get HSV in that exact location? And how can we cure her? With a little luck, in the reader’s career, we’ll come up with a cure, just as science came up with the acyclovir family of medicines early in my career.
LEARNING POINTS
• Grouped vesicles on an erythematous base, recurring in the same location, are HSV until proven otherwise.
• HSV episodes typically last 10 to 14 days.
• Staph infections are typically painful, and rarely recur in the same locations.
• Atopy predisposes to extralabial HSV.
• There are many causes of inflammation, only one of which is infection.
• There are many types of infection that are not bacterial (eg, viral, fungal, protozoan).
Recurrent pigment loss worries patient
HISTORY
Pigment loss is no joke, especially when it appears annually in the same locations. Although it eventually clears up, this 30-year-old-woman has been worried about her condition ever since her (no doubt, well-meaning) sister-in-law suggested it might be vitiligo.
The patient had no idea what vitiligo was but soon found out when she looked it up. To add to that angst, she has been seen by any number of providers over the years and has been given about as many different diagnoses, including the ever-popular “ringworm,” psoriasis, and mere dry skin.
The patient knows she has always had exceptionally dry skin, as well as seasonal allergies. These are problems almost everyone on her mother’s side of the family has had (as well as the patient’s two siblings).
The patient’s pigment loss seems to peak in the summer, resolving almost completely by Christmas.
DISCUSSION
In general, change in pigment is called dyschromia, but when one adds or loses the normal color of the skin, it’s called either hyperchromia or hypochromia. The distinction is not merely academic, since dyschromic patients can turn a variety of colors: blue (with ingestion of silver salts or minocycline, for example), bronze (seen with Wilson’s and Addison’s diseases and hemochromatosis), brown (as in melasma), or gray (seen with administration of gold salts).
One unusual form of hypochromia is vitiligo, an autoimmune disease eventuating in sharply demarcated areas of complete pigment loss, leaving perfectly white skin in its wake. Vitiligo seldom, if ever, waxes and wanes and never involves associated scaling. But it can certainly be a cosmetic problem, often affecting the face, hands, arms, and legs.
Vitilgo can be treated with varying degrees of success, depending on how early the treatment is instituted and how aggressive the disease is. Quite often, it progresses unnoticed until it has become permanent.
Fortunately, our patient did not have vitiligo and instead had the extremely common pityriasis alba (PA). Osler, the most famous physician of his time (1900), once quipped that he could ”forgive dermatology its complexity, but never its terminology.” Pityriasis alba (PA) sounds imposing. But in fact, it represents a simple but important concept: As cutaneous inflammation subsides, the epidermis can add pigment (called postinflammatory hyperpigmentation) or lose it (postinflammatory hypopigmentation).
PA manifests with patchy partial pigment loss as a postinflammatory consequence of antecedent eczema. The latter, originating most commonly in winter, is almost always part of an overarching diagnosis of atopic dermatitis, minor diagnostic criteria for which also include dry, sensitive skin, seasonal allergies, and asthma (all inherited traits).
The usual progression is thus: Patients with xerosis (dry skin), which is worsened by the low humidity of winter and the appeal of long, hot showers, begin to develop faintly defined, round, slightly scaly patches of eczema on the sides of the face and on the arms. These are so faint that they are often missed by the patient and family until later, in the spring, when the postinflammatory loss of pigment is made more obvious by tanning of the surrounding skin. As one might expect, this is especially obvious in darker-skinned patients whose eczema has long since faded, leaving an exceedingly fine scale (if any).
When the eczema is especially active and inflamed, the annular shape and scaly surface put the inexperienced provider in mind of “ringworm” (tinea corporis). This can be ruled out with a KOH prep and brief history-taking to identify whether a potential source for fungal organisms (new pet, playmates, siblings) exists. Keep in mind that pityriasis alba is far more common than tinea corporis.
The differential diagnosis for patchy hypopigmentation also includes tinea versicolor and (in older patients) cutaneous T-cell lymphoma, which would be progressive (albeit slowly) and not seasonal. The organism responsible for tinea versicolor (the commensal yeast Malassezia furfur) needs, among other things, much sebum in order to thrive. As this is an ingredient missing in prepubescent children, it is an important point in ruling out tinea versicolor, which is almost always seasonal as well, in young patients.
On a practical level, the “treatment” of PA predominantly involves easing patients’ (and parents’) minds by giving them a firm diagnosis that does not involve “ringworm,” and a clear idea of the self-limiting nature of the problem. See below for other treatment ideas.
LEARNING POINTS
Pityriasis alba (PA) favors the sides of the face and triceps areas of both arms; it is especially common in darker-skinned children.
PA is nearly always part of atopic dermatitis, the presence of which can help to corroborate the diagnosis.
The use of sunscreen helps to prevent the darkening of surrounding skin, making PA less obvious.
Preventing the eczema in the first place, by taking short showers, using emollients soaps, and moisturizing daily, may be beneficial.
Treating the antecedent eczema early on with group IV or V steroid creams (such as desonide) is useful in decreasing hypopigmentation later on.
HISTORY
Pigment loss is no joke, especially when it appears annually in the same locations. Although it eventually clears up, this 30-year-old-woman has been worried about her condition ever since her (no doubt, well-meaning) sister-in-law suggested it might be vitiligo.
The patient had no idea what vitiligo was but soon found out when she looked it up. To add to that angst, she has been seen by any number of providers over the years and has been given about as many different diagnoses, including the ever-popular “ringworm,” psoriasis, and mere dry skin.
The patient knows she has always had exceptionally dry skin, as well as seasonal allergies. These are problems almost everyone on her mother’s side of the family has had (as well as the patient’s two siblings).
The patient’s pigment loss seems to peak in the summer, resolving almost completely by Christmas.
DISCUSSION
In general, change in pigment is called dyschromia, but when one adds or loses the normal color of the skin, it’s called either hyperchromia or hypochromia. The distinction is not merely academic, since dyschromic patients can turn a variety of colors: blue (with ingestion of silver salts or minocycline, for example), bronze (seen with Wilson’s and Addison’s diseases and hemochromatosis), brown (as in melasma), or gray (seen with administration of gold salts).
One unusual form of hypochromia is vitiligo, an autoimmune disease eventuating in sharply demarcated areas of complete pigment loss, leaving perfectly white skin in its wake. Vitiligo seldom, if ever, waxes and wanes and never involves associated scaling. But it can certainly be a cosmetic problem, often affecting the face, hands, arms, and legs.
Vitilgo can be treated with varying degrees of success, depending on how early the treatment is instituted and how aggressive the disease is. Quite often, it progresses unnoticed until it has become permanent.
Fortunately, our patient did not have vitiligo and instead had the extremely common pityriasis alba (PA). Osler, the most famous physician of his time (1900), once quipped that he could ”forgive dermatology its complexity, but never its terminology.” Pityriasis alba (PA) sounds imposing. But in fact, it represents a simple but important concept: As cutaneous inflammation subsides, the epidermis can add pigment (called postinflammatory hyperpigmentation) or lose it (postinflammatory hypopigmentation).
PA manifests with patchy partial pigment loss as a postinflammatory consequence of antecedent eczema. The latter, originating most commonly in winter, is almost always part of an overarching diagnosis of atopic dermatitis, minor diagnostic criteria for which also include dry, sensitive skin, seasonal allergies, and asthma (all inherited traits).
The usual progression is thus: Patients with xerosis (dry skin), which is worsened by the low humidity of winter and the appeal of long, hot showers, begin to develop faintly defined, round, slightly scaly patches of eczema on the sides of the face and on the arms. These are so faint that they are often missed by the patient and family until later, in the spring, when the postinflammatory loss of pigment is made more obvious by tanning of the surrounding skin. As one might expect, this is especially obvious in darker-skinned patients whose eczema has long since faded, leaving an exceedingly fine scale (if any).
When the eczema is especially active and inflamed, the annular shape and scaly surface put the inexperienced provider in mind of “ringworm” (tinea corporis). This can be ruled out with a KOH prep and brief history-taking to identify whether a potential source for fungal organisms (new pet, playmates, siblings) exists. Keep in mind that pityriasis alba is far more common than tinea corporis.
The differential diagnosis for patchy hypopigmentation also includes tinea versicolor and (in older patients) cutaneous T-cell lymphoma, which would be progressive (albeit slowly) and not seasonal. The organism responsible for tinea versicolor (the commensal yeast Malassezia furfur) needs, among other things, much sebum in order to thrive. As this is an ingredient missing in prepubescent children, it is an important point in ruling out tinea versicolor, which is almost always seasonal as well, in young patients.
On a practical level, the “treatment” of PA predominantly involves easing patients’ (and parents’) minds by giving them a firm diagnosis that does not involve “ringworm,” and a clear idea of the self-limiting nature of the problem. See below for other treatment ideas.
LEARNING POINTS
Pityriasis alba (PA) favors the sides of the face and triceps areas of both arms; it is especially common in darker-skinned children.
PA is nearly always part of atopic dermatitis, the presence of which can help to corroborate the diagnosis.
The use of sunscreen helps to prevent the darkening of surrounding skin, making PA less obvious.
Preventing the eczema in the first place, by taking short showers, using emollients soaps, and moisturizing daily, may be beneficial.
Treating the antecedent eczema early on with group IV or V steroid creams (such as desonide) is useful in decreasing hypopigmentation later on.
HISTORY
Pigment loss is no joke, especially when it appears annually in the same locations. Although it eventually clears up, this 30-year-old-woman has been worried about her condition ever since her (no doubt, well-meaning) sister-in-law suggested it might be vitiligo.
The patient had no idea what vitiligo was but soon found out when she looked it up. To add to that angst, she has been seen by any number of providers over the years and has been given about as many different diagnoses, including the ever-popular “ringworm,” psoriasis, and mere dry skin.
The patient knows she has always had exceptionally dry skin, as well as seasonal allergies. These are problems almost everyone on her mother’s side of the family has had (as well as the patient’s two siblings).
The patient’s pigment loss seems to peak in the summer, resolving almost completely by Christmas.
DISCUSSION
In general, change in pigment is called dyschromia, but when one adds or loses the normal color of the skin, it’s called either hyperchromia or hypochromia. The distinction is not merely academic, since dyschromic patients can turn a variety of colors: blue (with ingestion of silver salts or minocycline, for example), bronze (seen with Wilson’s and Addison’s diseases and hemochromatosis), brown (as in melasma), or gray (seen with administration of gold salts).
One unusual form of hypochromia is vitiligo, an autoimmune disease eventuating in sharply demarcated areas of complete pigment loss, leaving perfectly white skin in its wake. Vitiligo seldom, if ever, waxes and wanes and never involves associated scaling. But it can certainly be a cosmetic problem, often affecting the face, hands, arms, and legs.
Vitilgo can be treated with varying degrees of success, depending on how early the treatment is instituted and how aggressive the disease is. Quite often, it progresses unnoticed until it has become permanent.
Fortunately, our patient did not have vitiligo and instead had the extremely common pityriasis alba (PA). Osler, the most famous physician of his time (1900), once quipped that he could ”forgive dermatology its complexity, but never its terminology.” Pityriasis alba (PA) sounds imposing. But in fact, it represents a simple but important concept: As cutaneous inflammation subsides, the epidermis can add pigment (called postinflammatory hyperpigmentation) or lose it (postinflammatory hypopigmentation).
PA manifests with patchy partial pigment loss as a postinflammatory consequence of antecedent eczema. The latter, originating most commonly in winter, is almost always part of an overarching diagnosis of atopic dermatitis, minor diagnostic criteria for which also include dry, sensitive skin, seasonal allergies, and asthma (all inherited traits).
The usual progression is thus: Patients with xerosis (dry skin), which is worsened by the low humidity of winter and the appeal of long, hot showers, begin to develop faintly defined, round, slightly scaly patches of eczema on the sides of the face and on the arms. These are so faint that they are often missed by the patient and family until later, in the spring, when the postinflammatory loss of pigment is made more obvious by tanning of the surrounding skin. As one might expect, this is especially obvious in darker-skinned patients whose eczema has long since faded, leaving an exceedingly fine scale (if any).
When the eczema is especially active and inflamed, the annular shape and scaly surface put the inexperienced provider in mind of “ringworm” (tinea corporis). This can be ruled out with a KOH prep and brief history-taking to identify whether a potential source for fungal organisms (new pet, playmates, siblings) exists. Keep in mind that pityriasis alba is far more common than tinea corporis.
The differential diagnosis for patchy hypopigmentation also includes tinea versicolor and (in older patients) cutaneous T-cell lymphoma, which would be progressive (albeit slowly) and not seasonal. The organism responsible for tinea versicolor (the commensal yeast Malassezia furfur) needs, among other things, much sebum in order to thrive. As this is an ingredient missing in prepubescent children, it is an important point in ruling out tinea versicolor, which is almost always seasonal as well, in young patients.
On a practical level, the “treatment” of PA predominantly involves easing patients’ (and parents’) minds by giving them a firm diagnosis that does not involve “ringworm,” and a clear idea of the self-limiting nature of the problem. See below for other treatment ideas.
LEARNING POINTS
Pityriasis alba (PA) favors the sides of the face and triceps areas of both arms; it is especially common in darker-skinned children.
PA is nearly always part of atopic dermatitis, the presence of which can help to corroborate the diagnosis.
The use of sunscreen helps to prevent the darkening of surrounding skin, making PA less obvious.
Preventing the eczema in the first place, by taking short showers, using emollients soaps, and moisturizing daily, may be beneficial.
Treating the antecedent eczema early on with group IV or V steroid creams (such as desonide) is useful in decreasing hypopigmentation later on.
Patient caught in "vicious cycle" with perioral rash
PATIENT HISTORY
A 38-year-old woman presents with a perioral rash composed of fine papules and pustules, slight erythema, and focal fine scale, which spares the vermillion border by several millimeters. The rash, which burns slightly and feels “tight,” has been present for several months.
During this time, the patient has been applying her sister’s psoriasis cream (clobetasol 0.05%) to the area several times a week. After each application, the rash feels and looks better—but only for a few hours. When she tries to stop using the cream, however, the burning and tightness worsen until she relents and re-applies the cream.
She has already tried changing her makeup and other facial care products, without success. A visit to her primary care provider yielded the diagnosis of “yeast infection,” but the clotrimazole cream he prescribed only made the situation worse.
The patient feels trapped in a vicious cycle, knowing the clobetasol is not really helping but unable to endure the symptoms if she doesn’t use it. A friend finally suggests she see a dermatology provider, an option she hadn’t considered.
DIAGNOSIS/DISCUSSION
This is a typical case of perioral dermatitis (POD), a very common condition that nonetheless seems to baffle non-derm providers. As with so many conditions, POD’s etiology is unknown.
The literature says that at least 90% of POD patients are women, but in my experience, it’s closer to 98%. There are rare cases seen in young children of both genders, and every five years or so, in an adult male.
But just because it occurs mostly in women ages 20 to 50 doesn’t mean it is hormonal in origin, or related to makeup or facial care. As this case illustrates, virtually every woman I’ve seen with POD has long since eliminated those items by trial and error, prior to being seen in dermatology.
The use of steroid medications, as in this case, is common; however, at least half the cases I see do not involve them. By the same token, we often see patients who were treating facial seborrhea or psoriasis with potent topical steroid creams and developed a POD-like eruption in the treated areas (eg, periocular or pernasilar skin).
This case also illustrates the phenomenon of “steroid addiction,” in which the symptoms worsen with attempted withdrawal from the steroid preparation. This locks the patient into a vicious cycle that not only irreparably thins the treated skin, but also makes the POD more difficult to treat.
Histologically, POD closely resembles rosacea, and it responds to some of the same medications. But POD in no way resembles rosacea clinically, and it does not afflict the same population (“flushers and blushers”).
The fine papulopustular, slightly scaly perioral rash seen in this case is typical, as is the sharp sparing of the vermillion border. Various microorganisms have been cultured from POD lesions, but none appear to be causative.
TREATMENT/PROGNOSIS
Topical medications, such as clindamycin and metronidazole, have been used for POD with modest success, but many POD patients complain of already sensitive skin that is further irritated by topical antibiotics. More effective and better tolerated are the oral antibiotics, such as tetracycline (250 to 500 mg bid) or minocycline (50 to 100 mg bid), typically given for at least a month, occasionally longer. This usually results in a cure, though relapses months later are not uncommon.
In this and similar cases, the clobetasol must be discontinued by changing to a much weaker steroid preparation, such as hydrocortisone 2.5 % or topical pimecrolimus 0.1% ointment, eliminating the steroids within two to three weeks. Because withdrawal symptoms in such cases can be severe, considerable patient education and frequent follow-up are necessary. This particular patient was treated with oral minocycline (100 mg bid for two weeks, dropping to 100 QD for three weeks), and will be reevaluated at the end of the treatment cycle.
There is a school of thought that asserts that the best treatment for POD is to withdraw the patient from virtually every contactant, since many POD patients are applying multiple products to their face out of desperation. None work, and some possibly irritate and thus perpetuate the problem.
The rapid response of POD to oral medication is so typical that it is, in effect, diagnostic. With treatment failure, other items in the differential diagnosis would include: contact dermatitis, impetigo, psoriasis, seborrhea, and neurodermatitis (lichen simplex chronicus).
TAKE-HOME TEACHING POINTS
1. POD involves a fine sparse perioral papulopustular rash that spares the upper vermillion border sharply.
2. At least 90% of POD patients are women.
3. Injudicious and prolonged application of steroid creams (especially fluorinated) are implicated in a significant percentage of cases.
4. When steroid “addiction” is found, the medication must be withdrawn slowly and replaced by a weaker steroid cream or pimecrolimus ointment for up to a month.
5. POD can also be seen in the periorbital, perinasilar, and nasolabial areas.
6. In mild cases, consider “treating” POD by simply ceasing all contactants.
7. Consider early referral to dermatology.
PATIENT HISTORY
A 38-year-old woman presents with a perioral rash composed of fine papules and pustules, slight erythema, and focal fine scale, which spares the vermillion border by several millimeters. The rash, which burns slightly and feels “tight,” has been present for several months.
During this time, the patient has been applying her sister’s psoriasis cream (clobetasol 0.05%) to the area several times a week. After each application, the rash feels and looks better—but only for a few hours. When she tries to stop using the cream, however, the burning and tightness worsen until she relents and re-applies the cream.
She has already tried changing her makeup and other facial care products, without success. A visit to her primary care provider yielded the diagnosis of “yeast infection,” but the clotrimazole cream he prescribed only made the situation worse.
The patient feels trapped in a vicious cycle, knowing the clobetasol is not really helping but unable to endure the symptoms if she doesn’t use it. A friend finally suggests she see a dermatology provider, an option she hadn’t considered.
DIAGNOSIS/DISCUSSION
This is a typical case of perioral dermatitis (POD), a very common condition that nonetheless seems to baffle non-derm providers. As with so many conditions, POD’s etiology is unknown.
The literature says that at least 90% of POD patients are women, but in my experience, it’s closer to 98%. There are rare cases seen in young children of both genders, and every five years or so, in an adult male.
But just because it occurs mostly in women ages 20 to 50 doesn’t mean it is hormonal in origin, or related to makeup or facial care. As this case illustrates, virtually every woman I’ve seen with POD has long since eliminated those items by trial and error, prior to being seen in dermatology.
The use of steroid medications, as in this case, is common; however, at least half the cases I see do not involve them. By the same token, we often see patients who were treating facial seborrhea or psoriasis with potent topical steroid creams and developed a POD-like eruption in the treated areas (eg, periocular or pernasilar skin).
This case also illustrates the phenomenon of “steroid addiction,” in which the symptoms worsen with attempted withdrawal from the steroid preparation. This locks the patient into a vicious cycle that not only irreparably thins the treated skin, but also makes the POD more difficult to treat.
Histologically, POD closely resembles rosacea, and it responds to some of the same medications. But POD in no way resembles rosacea clinically, and it does not afflict the same population (“flushers and blushers”).
The fine papulopustular, slightly scaly perioral rash seen in this case is typical, as is the sharp sparing of the vermillion border. Various microorganisms have been cultured from POD lesions, but none appear to be causative.
TREATMENT/PROGNOSIS
Topical medications, such as clindamycin and metronidazole, have been used for POD with modest success, but many POD patients complain of already sensitive skin that is further irritated by topical antibiotics. More effective and better tolerated are the oral antibiotics, such as tetracycline (250 to 500 mg bid) or minocycline (50 to 100 mg bid), typically given for at least a month, occasionally longer. This usually results in a cure, though relapses months later are not uncommon.
In this and similar cases, the clobetasol must be discontinued by changing to a much weaker steroid preparation, such as hydrocortisone 2.5 % or topical pimecrolimus 0.1% ointment, eliminating the steroids within two to three weeks. Because withdrawal symptoms in such cases can be severe, considerable patient education and frequent follow-up are necessary. This particular patient was treated with oral minocycline (100 mg bid for two weeks, dropping to 100 QD for three weeks), and will be reevaluated at the end of the treatment cycle.
There is a school of thought that asserts that the best treatment for POD is to withdraw the patient from virtually every contactant, since many POD patients are applying multiple products to their face out of desperation. None work, and some possibly irritate and thus perpetuate the problem.
The rapid response of POD to oral medication is so typical that it is, in effect, diagnostic. With treatment failure, other items in the differential diagnosis would include: contact dermatitis, impetigo, psoriasis, seborrhea, and neurodermatitis (lichen simplex chronicus).
TAKE-HOME TEACHING POINTS
1. POD involves a fine sparse perioral papulopustular rash that spares the upper vermillion border sharply.
2. At least 90% of POD patients are women.
3. Injudicious and prolonged application of steroid creams (especially fluorinated) are implicated in a significant percentage of cases.
4. When steroid “addiction” is found, the medication must be withdrawn slowly and replaced by a weaker steroid cream or pimecrolimus ointment for up to a month.
5. POD can also be seen in the periorbital, perinasilar, and nasolabial areas.
6. In mild cases, consider “treating” POD by simply ceasing all contactants.
7. Consider early referral to dermatology.
PATIENT HISTORY
A 38-year-old woman presents with a perioral rash composed of fine papules and pustules, slight erythema, and focal fine scale, which spares the vermillion border by several millimeters. The rash, which burns slightly and feels “tight,” has been present for several months.
During this time, the patient has been applying her sister’s psoriasis cream (clobetasol 0.05%) to the area several times a week. After each application, the rash feels and looks better—but only for a few hours. When she tries to stop using the cream, however, the burning and tightness worsen until she relents and re-applies the cream.
She has already tried changing her makeup and other facial care products, without success. A visit to her primary care provider yielded the diagnosis of “yeast infection,” but the clotrimazole cream he prescribed only made the situation worse.
The patient feels trapped in a vicious cycle, knowing the clobetasol is not really helping but unable to endure the symptoms if she doesn’t use it. A friend finally suggests she see a dermatology provider, an option she hadn’t considered.
DIAGNOSIS/DISCUSSION
This is a typical case of perioral dermatitis (POD), a very common condition that nonetheless seems to baffle non-derm providers. As with so many conditions, POD’s etiology is unknown.
The literature says that at least 90% of POD patients are women, but in my experience, it’s closer to 98%. There are rare cases seen in young children of both genders, and every five years or so, in an adult male.
But just because it occurs mostly in women ages 20 to 50 doesn’t mean it is hormonal in origin, or related to makeup or facial care. As this case illustrates, virtually every woman I’ve seen with POD has long since eliminated those items by trial and error, prior to being seen in dermatology.
The use of steroid medications, as in this case, is common; however, at least half the cases I see do not involve them. By the same token, we often see patients who were treating facial seborrhea or psoriasis with potent topical steroid creams and developed a POD-like eruption in the treated areas (eg, periocular or pernasilar skin).
This case also illustrates the phenomenon of “steroid addiction,” in which the symptoms worsen with attempted withdrawal from the steroid preparation. This locks the patient into a vicious cycle that not only irreparably thins the treated skin, but also makes the POD more difficult to treat.
Histologically, POD closely resembles rosacea, and it responds to some of the same medications. But POD in no way resembles rosacea clinically, and it does not afflict the same population (“flushers and blushers”).
The fine papulopustular, slightly scaly perioral rash seen in this case is typical, as is the sharp sparing of the vermillion border. Various microorganisms have been cultured from POD lesions, but none appear to be causative.
TREATMENT/PROGNOSIS
Topical medications, such as clindamycin and metronidazole, have been used for POD with modest success, but many POD patients complain of already sensitive skin that is further irritated by topical antibiotics. More effective and better tolerated are the oral antibiotics, such as tetracycline (250 to 500 mg bid) or minocycline (50 to 100 mg bid), typically given for at least a month, occasionally longer. This usually results in a cure, though relapses months later are not uncommon.
In this and similar cases, the clobetasol must be discontinued by changing to a much weaker steroid preparation, such as hydrocortisone 2.5 % or topical pimecrolimus 0.1% ointment, eliminating the steroids within two to three weeks. Because withdrawal symptoms in such cases can be severe, considerable patient education and frequent follow-up are necessary. This particular patient was treated with oral minocycline (100 mg bid for two weeks, dropping to 100 QD for three weeks), and will be reevaluated at the end of the treatment cycle.
There is a school of thought that asserts that the best treatment for POD is to withdraw the patient from virtually every contactant, since many POD patients are applying multiple products to their face out of desperation. None work, and some possibly irritate and thus perpetuate the problem.
The rapid response of POD to oral medication is so typical that it is, in effect, diagnostic. With treatment failure, other items in the differential diagnosis would include: contact dermatitis, impetigo, psoriasis, seborrhea, and neurodermatitis (lichen simplex chronicus).
TAKE-HOME TEACHING POINTS
1. POD involves a fine sparse perioral papulopustular rash that spares the upper vermillion border sharply.
2. At least 90% of POD patients are women.
3. Injudicious and prolonged application of steroid creams (especially fluorinated) are implicated in a significant percentage of cases.
4. When steroid “addiction” is found, the medication must be withdrawn slowly and replaced by a weaker steroid cream or pimecrolimus ointment for up to a month.
5. POD can also be seen in the periorbital, perinasilar, and nasolabial areas.
6. In mild cases, consider “treating” POD by simply ceasing all contactants.
7. Consider early referral to dermatology.
A persistent rash eludes treatment
HISTORY OF PRESENT ILLNESS
A 25-year-old man is urgently referred to dermatology by a local emergency department, where he was seen this morning for the highly symptomatic rash present on his abdomen for more than a year. The presumptive diagnosis is cellulitis; however, the patient has been seen in a number of other medical venues, including urgent care clinics and his primary care provider’s office, where he has received several diagnoses and treatments for yeast infection, impetigo, and fungal infection.
The rash started a few centimeters below his umbilicus but has grown in size. Recently, it became so wet that he started applying a large adhesive bandage to the spot (sometimes twice a day). During this time, he has applied a number of topical products (antifungal creams, antihistamine creams, calamine lotion, and, most consistently, triple-antibiotic cream) and taken several courses of oral antibiotics, including cephalexin and trimethoprim/sulfa. His condition has only worsened.
The patient claims to be in good health otherwise, although he admits to a history of atopy, marked by seasonal allergies and asthma in childhood.
EXAMINATION
This striking rash is sharply confined within square-shaped linear borders (8.5 cm per side), between the umbilicus and the suprapubic area. The surface is quite red and scaly, with focal vesiculation and lichenification. The large bandage (shown reflected inferiorly) has adhesive borders; its surface is visibly damp, but with no discoloration.
The site is slightly edematous but neither tender to touch nor especially warm. There are no palpable nodes in either groin. The patient’s skin elsewhere is free of notable changes or lesions.
DIAGNOSIS/DISCUSSION
It has been pointed out that at least 50% of all cases of allergic contact dermatitis are caused by one of 25 common allergens. Among these, the #1 offender worldwide is nickel–a ubiquitous metal found in inexpensive jewelry and other accessories, such as belt buckles. Chronic exposure to the latter is probably what triggered this patient’s original rash. However, as is often the case, what the patient treats the rash with becomes the problem.
In this case, the topical medication the patient applied most consistently was triple-antibiotic ointment. Triple-antibiotic ointment contains three antimicrobials: neomycin, bacitracin, and polymyxin. The first two are common topical sensitizers. More than likely, this was part of our patient’s problem—as was the unfortunate fact that the belt he is seen wearing was the only belt he owned. In his job as a computer programmer, he was seated at his desk all day, a position that brought the buckle into constant contact with the affected area.
The red linear outline of the area likely represented an irritant dermatitis, an extremely common problem caused by the bandage’s application and removal, as well as the maceration and tearing of the skin, which was already “excited” from the adjacent process. The occlusion provided by the bandage also served to potentiate the effects of the triple-antibiotic ointment.
To summarize, it appears likely that this patient’s rash was initially caused by an allergy to the nickel in his belt buckle, was worsened by the regular application of triple-antibiotic ointment, and was further exacerbated by the application of the large adhesive bandage.
The differential diagnosis included: asteatotic eczema, seborrheic dermatitis, psoriasis, intertrigo, tinea, and impetigo.
TREATMENT/PROGNOSIS
Successful treatment is quite simple: (1) Provide patient education regarding the nature of the problem. (2) Recommend the patient discontinue use of triple-antibiotic ointment (now and forever). (3) Advise the patient to buy and use a new, nonmetallic belt to the exclusion of his old metal belt (now and forever). (4) Prescribe twice-daily application of clobetasol ointment for at least two weeks (with follow-up). (5) Consider the option of prescribing a two-week course of prednisone (tapering from 40 mg/d) or the alternative of intramuscular injection of triamcinolone acetonide (40 to 60 mg), either of which might have been necessary in a more severe case.
TAKE-HOME TEACHING POINTS
1. Consider a broad differential for inflammation of the skin, which includes noninfectious causes.
2. Nickel is the most common topical sensitizer worldwide and affects a significant percentage of the population.
3. What the patient applies to a rash often becomes the problem.
4. Neomycin and bacitracin are common topical sensitizers that are present in triple-antibiotic ointment/cream.
5. Linearity in a rash is strongly suggestive of contact dermatitis.
6. Clear serous drainage is suggestive of inflammation, not infection.
HISTORY OF PRESENT ILLNESS
A 25-year-old man is urgently referred to dermatology by a local emergency department, where he was seen this morning for the highly symptomatic rash present on his abdomen for more than a year. The presumptive diagnosis is cellulitis; however, the patient has been seen in a number of other medical venues, including urgent care clinics and his primary care provider’s office, where he has received several diagnoses and treatments for yeast infection, impetigo, and fungal infection.
The rash started a few centimeters below his umbilicus but has grown in size. Recently, it became so wet that he started applying a large adhesive bandage to the spot (sometimes twice a day). During this time, he has applied a number of topical products (antifungal creams, antihistamine creams, calamine lotion, and, most consistently, triple-antibiotic cream) and taken several courses of oral antibiotics, including cephalexin and trimethoprim/sulfa. His condition has only worsened.
The patient claims to be in good health otherwise, although he admits to a history of atopy, marked by seasonal allergies and asthma in childhood.
EXAMINATION
This striking rash is sharply confined within square-shaped linear borders (8.5 cm per side), between the umbilicus and the suprapubic area. The surface is quite red and scaly, with focal vesiculation and lichenification. The large bandage (shown reflected inferiorly) has adhesive borders; its surface is visibly damp, but with no discoloration.
The site is slightly edematous but neither tender to touch nor especially warm. There are no palpable nodes in either groin. The patient’s skin elsewhere is free of notable changes or lesions.
DIAGNOSIS/DISCUSSION
It has been pointed out that at least 50% of all cases of allergic contact dermatitis are caused by one of 25 common allergens. Among these, the #1 offender worldwide is nickel–a ubiquitous metal found in inexpensive jewelry and other accessories, such as belt buckles. Chronic exposure to the latter is probably what triggered this patient’s original rash. However, as is often the case, what the patient treats the rash with becomes the problem.
In this case, the topical medication the patient applied most consistently was triple-antibiotic ointment. Triple-antibiotic ointment contains three antimicrobials: neomycin, bacitracin, and polymyxin. The first two are common topical sensitizers. More than likely, this was part of our patient’s problem—as was the unfortunate fact that the belt he is seen wearing was the only belt he owned. In his job as a computer programmer, he was seated at his desk all day, a position that brought the buckle into constant contact with the affected area.
The red linear outline of the area likely represented an irritant dermatitis, an extremely common problem caused by the bandage’s application and removal, as well as the maceration and tearing of the skin, which was already “excited” from the adjacent process. The occlusion provided by the bandage also served to potentiate the effects of the triple-antibiotic ointment.
To summarize, it appears likely that this patient’s rash was initially caused by an allergy to the nickel in his belt buckle, was worsened by the regular application of triple-antibiotic ointment, and was further exacerbated by the application of the large adhesive bandage.
The differential diagnosis included: asteatotic eczema, seborrheic dermatitis, psoriasis, intertrigo, tinea, and impetigo.
TREATMENT/PROGNOSIS
Successful treatment is quite simple: (1) Provide patient education regarding the nature of the problem. (2) Recommend the patient discontinue use of triple-antibiotic ointment (now and forever). (3) Advise the patient to buy and use a new, nonmetallic belt to the exclusion of his old metal belt (now and forever). (4) Prescribe twice-daily application of clobetasol ointment for at least two weeks (with follow-up). (5) Consider the option of prescribing a two-week course of prednisone (tapering from 40 mg/d) or the alternative of intramuscular injection of triamcinolone acetonide (40 to 60 mg), either of which might have been necessary in a more severe case.
TAKE-HOME TEACHING POINTS
1. Consider a broad differential for inflammation of the skin, which includes noninfectious causes.
2. Nickel is the most common topical sensitizer worldwide and affects a significant percentage of the population.
3. What the patient applies to a rash often becomes the problem.
4. Neomycin and bacitracin are common topical sensitizers that are present in triple-antibiotic ointment/cream.
5. Linearity in a rash is strongly suggestive of contact dermatitis.
6. Clear serous drainage is suggestive of inflammation, not infection.
HISTORY OF PRESENT ILLNESS
A 25-year-old man is urgently referred to dermatology by a local emergency department, where he was seen this morning for the highly symptomatic rash present on his abdomen for more than a year. The presumptive diagnosis is cellulitis; however, the patient has been seen in a number of other medical venues, including urgent care clinics and his primary care provider’s office, where he has received several diagnoses and treatments for yeast infection, impetigo, and fungal infection.
The rash started a few centimeters below his umbilicus but has grown in size. Recently, it became so wet that he started applying a large adhesive bandage to the spot (sometimes twice a day). During this time, he has applied a number of topical products (antifungal creams, antihistamine creams, calamine lotion, and, most consistently, triple-antibiotic cream) and taken several courses of oral antibiotics, including cephalexin and trimethoprim/sulfa. His condition has only worsened.
The patient claims to be in good health otherwise, although he admits to a history of atopy, marked by seasonal allergies and asthma in childhood.
EXAMINATION
This striking rash is sharply confined within square-shaped linear borders (8.5 cm per side), between the umbilicus and the suprapubic area. The surface is quite red and scaly, with focal vesiculation and lichenification. The large bandage (shown reflected inferiorly) has adhesive borders; its surface is visibly damp, but with no discoloration.
The site is slightly edematous but neither tender to touch nor especially warm. There are no palpable nodes in either groin. The patient’s skin elsewhere is free of notable changes or lesions.
DIAGNOSIS/DISCUSSION
It has been pointed out that at least 50% of all cases of allergic contact dermatitis are caused by one of 25 common allergens. Among these, the #1 offender worldwide is nickel–a ubiquitous metal found in inexpensive jewelry and other accessories, such as belt buckles. Chronic exposure to the latter is probably what triggered this patient’s original rash. However, as is often the case, what the patient treats the rash with becomes the problem.
In this case, the topical medication the patient applied most consistently was triple-antibiotic ointment. Triple-antibiotic ointment contains three antimicrobials: neomycin, bacitracin, and polymyxin. The first two are common topical sensitizers. More than likely, this was part of our patient’s problem—as was the unfortunate fact that the belt he is seen wearing was the only belt he owned. In his job as a computer programmer, he was seated at his desk all day, a position that brought the buckle into constant contact with the affected area.
The red linear outline of the area likely represented an irritant dermatitis, an extremely common problem caused by the bandage’s application and removal, as well as the maceration and tearing of the skin, which was already “excited” from the adjacent process. The occlusion provided by the bandage also served to potentiate the effects of the triple-antibiotic ointment.
To summarize, it appears likely that this patient’s rash was initially caused by an allergy to the nickel in his belt buckle, was worsened by the regular application of triple-antibiotic ointment, and was further exacerbated by the application of the large adhesive bandage.
The differential diagnosis included: asteatotic eczema, seborrheic dermatitis, psoriasis, intertrigo, tinea, and impetigo.
TREATMENT/PROGNOSIS
Successful treatment is quite simple: (1) Provide patient education regarding the nature of the problem. (2) Recommend the patient discontinue use of triple-antibiotic ointment (now and forever). (3) Advise the patient to buy and use a new, nonmetallic belt to the exclusion of his old metal belt (now and forever). (4) Prescribe twice-daily application of clobetasol ointment for at least two weeks (with follow-up). (5) Consider the option of prescribing a two-week course of prednisone (tapering from 40 mg/d) or the alternative of intramuscular injection of triamcinolone acetonide (40 to 60 mg), either of which might have been necessary in a more severe case.
TAKE-HOME TEACHING POINTS
1. Consider a broad differential for inflammation of the skin, which includes noninfectious causes.
2. Nickel is the most common topical sensitizer worldwide and affects a significant percentage of the population.
3. What the patient applies to a rash often becomes the problem.
4. Neomycin and bacitracin are common topical sensitizers that are present in triple-antibiotic ointment/cream.
5. Linearity in a rash is strongly suggestive of contact dermatitis.
6. Clear serous drainage is suggestive of inflammation, not infection.
Spreading Lesions on Sun-damaged Skin
ANSWER
The correct answer is idiopathic guttate hypomelanosis (choice “d”), a common condition primarily seen on sun-damaged patients, but often mistaken for tinea versicolor (choice “b”).
Vitiligo (choice “a”) can present with “confetti” lesions, but would more likely lead to complete loss of pigment in most of the lesions, not the partial loss seen in this patient. Biopsy is indicated in questionable cases.
Tinea versicolor, equally common, is caused by a commensal yeast called Malassezia furfur that feeds on sebum, which is why it favors the oily parts of the body (back and chest, primarily). It is almost never seen on the legs, which have the fewest oil glands on the body. In addition, tinea versicolor is, by its nature, an epidermal process, leading to the formation of a fine KOH-positive scale.
Since lupus (choice “c”) is a form of vasculitis, the associated inflammation can lead to pigment loss, especially in darker-skinned patients. Without a more likely explanation for these lesions, a biopsy might well have been indicated.
DISCUSSION
Biopsy might have suggested any number of other diseases that can also present with hypomelanosis, such as cutaneous T-cell lymphoma or sarcoid. But idiopathic guttate hypomelanosis is far more common, and the patient’s age, gender, and history of chronic UV damage all lend themselves perfectly to this diagnosis.
Idiopathic guttate hypomelanosis, for unknown reasons, tends to appear in women at earlier ages than in men (usually about a decade younger). For either gender, treatment is problematic once the lesions have fully developed. Early in the process, the obvious remedy is better sun protection. Lasers, retinoids, liquid nitrogen, and anti-inflammatory creams have all been tried with little success.
ANSWER
The correct answer is idiopathic guttate hypomelanosis (choice “d”), a common condition primarily seen on sun-damaged patients, but often mistaken for tinea versicolor (choice “b”).
Vitiligo (choice “a”) can present with “confetti” lesions, but would more likely lead to complete loss of pigment in most of the lesions, not the partial loss seen in this patient. Biopsy is indicated in questionable cases.
Tinea versicolor, equally common, is caused by a commensal yeast called Malassezia furfur that feeds on sebum, which is why it favors the oily parts of the body (back and chest, primarily). It is almost never seen on the legs, which have the fewest oil glands on the body. In addition, tinea versicolor is, by its nature, an epidermal process, leading to the formation of a fine KOH-positive scale.
Since lupus (choice “c”) is a form of vasculitis, the associated inflammation can lead to pigment loss, especially in darker-skinned patients. Without a more likely explanation for these lesions, a biopsy might well have been indicated.
DISCUSSION
Biopsy might have suggested any number of other diseases that can also present with hypomelanosis, such as cutaneous T-cell lymphoma or sarcoid. But idiopathic guttate hypomelanosis is far more common, and the patient’s age, gender, and history of chronic UV damage all lend themselves perfectly to this diagnosis.
Idiopathic guttate hypomelanosis, for unknown reasons, tends to appear in women at earlier ages than in men (usually about a decade younger). For either gender, treatment is problematic once the lesions have fully developed. Early in the process, the obvious remedy is better sun protection. Lasers, retinoids, liquid nitrogen, and anti-inflammatory creams have all been tried with little success.
ANSWER
The correct answer is idiopathic guttate hypomelanosis (choice “d”), a common condition primarily seen on sun-damaged patients, but often mistaken for tinea versicolor (choice “b”).
Vitiligo (choice “a”) can present with “confetti” lesions, but would more likely lead to complete loss of pigment in most of the lesions, not the partial loss seen in this patient. Biopsy is indicated in questionable cases.
Tinea versicolor, equally common, is caused by a commensal yeast called Malassezia furfur that feeds on sebum, which is why it favors the oily parts of the body (back and chest, primarily). It is almost never seen on the legs, which have the fewest oil glands on the body. In addition, tinea versicolor is, by its nature, an epidermal process, leading to the formation of a fine KOH-positive scale.
Since lupus (choice “c”) is a form of vasculitis, the associated inflammation can lead to pigment loss, especially in darker-skinned patients. Without a more likely explanation for these lesions, a biopsy might well have been indicated.
DISCUSSION
Biopsy might have suggested any number of other diseases that can also present with hypomelanosis, such as cutaneous T-cell lymphoma or sarcoid. But idiopathic guttate hypomelanosis is far more common, and the patient’s age, gender, and history of chronic UV damage all lend themselves perfectly to this diagnosis.
Idiopathic guttate hypomelanosis, for unknown reasons, tends to appear in women at earlier ages than in men (usually about a decade younger). For either gender, treatment is problematic once the lesions have fully developed. Early in the process, the obvious remedy is better sun protection. Lasers, retinoids, liquid nitrogen, and anti-inflammatory creams have all been tried with little success.

A few years ago, a woman first noticed lesions developing on her legs. The patient sought care from her primary care provider; however, despite a number of treatment regimens, including topical clotrimazole and terbinafine creams, the lesions have not only failed to resolve but have also grown in number and spread to other areas of her body. The woman, now 48, is referred to dermatology for evaluation of her persistent but asymptomatic condition. The patient claims that her health is otherwise excellent, although she has seasonal allergies, was a long-time smoker until two months ago, and has just begun estrogen replacement therapy. She is especially concerned that the lesions have started to appear on the skin of her abdomen. She specifically denies shortness of breath, joint pain, fever, unexplained weight loss, or cough. An examination of her skin reveals a multitude of 2- to 6-mm partially depigmented, roughly round macules uniformly distributed on her legs, arms, and trunk. The lesions, which average about 3 mm, have no palpable component and no observable scale or underlying induration. There is a concentration of them on the anterior tibial areas, as well as on the dorsal forearms; however, none are seen on her face, and the volar surfaces of her forearms are almost completely spared. Significantly, the patient’s exposed skin is tremendously sun-damaged, evidenced by a deep brown color and a weathered, wrinkled look, with many telangiectasias and brown to tan–orange macules on her face.
Family Thinks Man has Worms
ANSWER
The correct answer is nummular eczema (choice “a”), an extremely common condition, especially in older men. Had this been psoriasis (choice “b”), the lesions would not have been so pruritic and would have displayed the characteristic thick, whitish scaling on a salmon pink base—and that diagnosis would, in all likelihood, have been corroborated by signs of psoriasis elsewhere on the patient’s body.
A fungal infection (choice “c”) can be difficult to treat but probably would have responded at least in part to one of the many medications the man tried. Other factors that spoke against this diagnosis were the negative KOH preparations and the apparent lack of specific sources (eg, pets or other animals) for such an infection.
Bowen’s disease (choice “d”) represents superficial epidermal squamous cell carcinoma—the round, scaly lesions of which are often mistaken for the other choices in this differential. But Bowen’s lesions will be fixed (permanent) instead of waxing and waning as this patient’s lesions did, will not itch to any appreciable extent, and will be found almost exclusively on chronically sun-damaged skin (which was not evident in this patient).
DISCUSSION
Nummular eczema (NE) is an extremely common condition with unclear origins. We often see it in the context of older patients with dry skin made drier by bathing habits, swimming, or use of hot tubs. But many cases appear without these conditions, causing much conjecture about potential triggers, such as contact versus irritant dermatitis. Indeed, the multiplicity of topical medications applied by this patient was probably making things worse, as is often the case.
NE typically manifests acutely, but can persist for months, worrying some patients a great deal. If need be, a 4-mm punch biopsy will rule out the other suspects in the differential diagnosis. Then the lesions can be treated, as in this case, with a class 1 or 2 topical steroid ointment or emollient cream, as well as advice about the need to limit the length of time spent in, and the temperature of, showers or hot tubs.
As with so many dermatologic conditions, patients with NE are greatly reassured just knowing about all the conditions they don’t have. And as is often the case for providers, just knowing a given condition such as NE exists and is common is a priceless asset.
ANSWER
The correct answer is nummular eczema (choice “a”), an extremely common condition, especially in older men. Had this been psoriasis (choice “b”), the lesions would not have been so pruritic and would have displayed the characteristic thick, whitish scaling on a salmon pink base—and that diagnosis would, in all likelihood, have been corroborated by signs of psoriasis elsewhere on the patient’s body.
A fungal infection (choice “c”) can be difficult to treat but probably would have responded at least in part to one of the many medications the man tried. Other factors that spoke against this diagnosis were the negative KOH preparations and the apparent lack of specific sources (eg, pets or other animals) for such an infection.
Bowen’s disease (choice “d”) represents superficial epidermal squamous cell carcinoma—the round, scaly lesions of which are often mistaken for the other choices in this differential. But Bowen’s lesions will be fixed (permanent) instead of waxing and waning as this patient’s lesions did, will not itch to any appreciable extent, and will be found almost exclusively on chronically sun-damaged skin (which was not evident in this patient).
DISCUSSION
Nummular eczema (NE) is an extremely common condition with unclear origins. We often see it in the context of older patients with dry skin made drier by bathing habits, swimming, or use of hot tubs. But many cases appear without these conditions, causing much conjecture about potential triggers, such as contact versus irritant dermatitis. Indeed, the multiplicity of topical medications applied by this patient was probably making things worse, as is often the case.
NE typically manifests acutely, but can persist for months, worrying some patients a great deal. If need be, a 4-mm punch biopsy will rule out the other suspects in the differential diagnosis. Then the lesions can be treated, as in this case, with a class 1 or 2 topical steroid ointment or emollient cream, as well as advice about the need to limit the length of time spent in, and the temperature of, showers or hot tubs.
As with so many dermatologic conditions, patients with NE are greatly reassured just knowing about all the conditions they don’t have. And as is often the case for providers, just knowing a given condition such as NE exists and is common is a priceless asset.
ANSWER
The correct answer is nummular eczema (choice “a”), an extremely common condition, especially in older men. Had this been psoriasis (choice “b”), the lesions would not have been so pruritic and would have displayed the characteristic thick, whitish scaling on a salmon pink base—and that diagnosis would, in all likelihood, have been corroborated by signs of psoriasis elsewhere on the patient’s body.
A fungal infection (choice “c”) can be difficult to treat but probably would have responded at least in part to one of the many medications the man tried. Other factors that spoke against this diagnosis were the negative KOH preparations and the apparent lack of specific sources (eg, pets or other animals) for such an infection.
Bowen’s disease (choice “d”) represents superficial epidermal squamous cell carcinoma—the round, scaly lesions of which are often mistaken for the other choices in this differential. But Bowen’s lesions will be fixed (permanent) instead of waxing and waning as this patient’s lesions did, will not itch to any appreciable extent, and will be found almost exclusively on chronically sun-damaged skin (which was not evident in this patient).
DISCUSSION
Nummular eczema (NE) is an extremely common condition with unclear origins. We often see it in the context of older patients with dry skin made drier by bathing habits, swimming, or use of hot tubs. But many cases appear without these conditions, causing much conjecture about potential triggers, such as contact versus irritant dermatitis. Indeed, the multiplicity of topical medications applied by this patient was probably making things worse, as is often the case.
NE typically manifests acutely, but can persist for months, worrying some patients a great deal. If need be, a 4-mm punch biopsy will rule out the other suspects in the differential diagnosis. Then the lesions can be treated, as in this case, with a class 1 or 2 topical steroid ointment or emollient cream, as well as advice about the need to limit the length of time spent in, and the temperature of, showers or hot tubs.
As with so many dermatologic conditions, patients with NE are greatly reassured just knowing about all the conditions they don’t have. And as is often the case for providers, just knowing a given condition such as NE exists and is common is a priceless asset.

A 70-year-old man self-refers to dermatology for evaluation of very itchy lesions that have been present for at least three months. The patient reports that the lesions have persisted despite the use of “everything but the kitchen sink”—meaning several OTC topical preparations, including those containing benzocaine, neomycin/polymyxin/bacitracin, and diphenhydramine, as well as “every antifungal cream I could buy.” The man has also tried pouring alcohol and peroxide over the lesions, again to no good effect. The lesions appeared in the midst of a long, cold winter with very low humidity; they itch terribly, causing the patient to scratch them vigorously. The lesions, which come and go, concern him not only because of the pruritus, but because his family is convinced he has some sort of “worms.” Further history taking reveals that the patient is not taking any new medications in addition to his simvastatin and metoprolol. He is not atopic and has no new pets, but he does admit to being “addicted” to sitting in his new hot tub. There is no history of gastric ulcers or dyspepsia, no joint pain, and no family history of psoriasis. Examination of the patient’s legs, particularly his calves, shows discrete and confluent round, scaly plaques of a striking reddish orange hue. They range from 1 to 5 cm in diameter. KOH prep of samples taken from two different lesions is negative for fungal elements. Elsewhere, the knees, elbows, nails, and scalp are free of any significant skin changes. There are no signs of chronic sun damage.
Is Patient With Fingernail Changes a "Contagious Threat"?
ANSWER
The correct answer is psoriasis (choice “d”), which often involves nail and skin changes such as those seen in this case. There was no particular reason to think this patient had an infection of any kind, but, as is often the case, the original provider considered only one diagnostic possibility.
DISCUSSION
Nail disease can be problematic for both patient and provider. Arguably the biggest issue with it, initially, is “the one-item differential”—the idea that all nail disease can be classified as “fungal infection” simply because neither the patient nor the provider considers any other explanation for the changes seen. This case illustrates that dilemma nicely.
Psoriasis affects more than 2% of the US population, making it a common skin disorder. As this case illustrates, it may affect several areas with diverse but predictable morphologic presentations, all appearing at the same time.
The key diagnostic points from this case include:
• Stress is a known trigger for psoriasis vulgaris.
• The patient’s nails failed to respond to terbinafine treatment.
• There was no obvious source of fungal infection (eg, contact with animals) or reason for him to have a yeast infection (eg, diabetes) or develop mold “infection” in the nails (eg, trauma from digging in soil).
• Fungal infections are about 18 times less likely to occur in the fingernails than in the toenails.
• A unifying explanation for simultaneous nail and skin changes was needed.
• The nail and skin changes seen here are quite typical for psoriasis.
Most important, though, is the need to overcome the urge to hop on the “fungal bandwagon” by first considering other diagnostic possibilities.
Continue for the treatment of this condition >>
TREATMENT
Unfortunately, there is no good treatment for this patient’s nails. However, there is an excellent chance that his scalp psoriasis will respond to short-term use of fluocinolone 0.05% cream.
This patient was also counseled about the role of stress in his condition and the benefits of modest increases in UV exposure. During follow-up, it will be important to ask about joint pain, since up to 30% of psoriasis patients will eventually develop psoriatic arthritis.
If the patient’s current treatment does not produce sufficient results, other options include calcipotriene ointment, oral methotrexate, or even one of the biologics (etanercept or adalimumab).
ANSWER
The correct answer is psoriasis (choice “d”), which often involves nail and skin changes such as those seen in this case. There was no particular reason to think this patient had an infection of any kind, but, as is often the case, the original provider considered only one diagnostic possibility.
DISCUSSION
Nail disease can be problematic for both patient and provider. Arguably the biggest issue with it, initially, is “the one-item differential”—the idea that all nail disease can be classified as “fungal infection” simply because neither the patient nor the provider considers any other explanation for the changes seen. This case illustrates that dilemma nicely.
Psoriasis affects more than 2% of the US population, making it a common skin disorder. As this case illustrates, it may affect several areas with diverse but predictable morphologic presentations, all appearing at the same time.
The key diagnostic points from this case include:
• Stress is a known trigger for psoriasis vulgaris.
• The patient’s nails failed to respond to terbinafine treatment.
• There was no obvious source of fungal infection (eg, contact with animals) or reason for him to have a yeast infection (eg, diabetes) or develop mold “infection” in the nails (eg, trauma from digging in soil).
• Fungal infections are about 18 times less likely to occur in the fingernails than in the toenails.
• A unifying explanation for simultaneous nail and skin changes was needed.
• The nail and skin changes seen here are quite typical for psoriasis.
Most important, though, is the need to overcome the urge to hop on the “fungal bandwagon” by first considering other diagnostic possibilities.
Continue for the treatment of this condition >>
TREATMENT
Unfortunately, there is no good treatment for this patient’s nails. However, there is an excellent chance that his scalp psoriasis will respond to short-term use of fluocinolone 0.05% cream.
This patient was also counseled about the role of stress in his condition and the benefits of modest increases in UV exposure. During follow-up, it will be important to ask about joint pain, since up to 30% of psoriasis patients will eventually develop psoriatic arthritis.
If the patient’s current treatment does not produce sufficient results, other options include calcipotriene ointment, oral methotrexate, or even one of the biologics (etanercept or adalimumab).
ANSWER
The correct answer is psoriasis (choice “d”), which often involves nail and skin changes such as those seen in this case. There was no particular reason to think this patient had an infection of any kind, but, as is often the case, the original provider considered only one diagnostic possibility.
DISCUSSION
Nail disease can be problematic for both patient and provider. Arguably the biggest issue with it, initially, is “the one-item differential”—the idea that all nail disease can be classified as “fungal infection” simply because neither the patient nor the provider considers any other explanation for the changes seen. This case illustrates that dilemma nicely.
Psoriasis affects more than 2% of the US population, making it a common skin disorder. As this case illustrates, it may affect several areas with diverse but predictable morphologic presentations, all appearing at the same time.
The key diagnostic points from this case include:
• Stress is a known trigger for psoriasis vulgaris.
• The patient’s nails failed to respond to terbinafine treatment.
• There was no obvious source of fungal infection (eg, contact with animals) or reason for him to have a yeast infection (eg, diabetes) or develop mold “infection” in the nails (eg, trauma from digging in soil).
• Fungal infections are about 18 times less likely to occur in the fingernails than in the toenails.
• A unifying explanation for simultaneous nail and skin changes was needed.
• The nail and skin changes seen here are quite typical for psoriasis.
Most important, though, is the need to overcome the urge to hop on the “fungal bandwagon” by first considering other diagnostic possibilities.
Continue for the treatment of this condition >>
TREATMENT
Unfortunately, there is no good treatment for this patient’s nails. However, there is an excellent chance that his scalp psoriasis will respond to short-term use of fluocinolone 0.05% cream.
This patient was also counseled about the role of stress in his condition and the benefits of modest increases in UV exposure. During follow-up, it will be important to ask about joint pain, since up to 30% of psoriasis patients will eventually develop psoriatic arthritis.
If the patient’s current treatment does not produce sufficient results, other options include calcipotriene ointment, oral methotrexate, or even one of the biologics (etanercept or adalimumab).

After finishing a month-long course of terbinafine (250 mg), a 27-year-old man is dismayed to see that the fingernail changes he first noted a year ago have not improved. He had been told in no uncertain terms by his primary care provider that his fingernail condition—and accompanying scalp rash—represented fungal infection. When topical antifungal creams failed to help his scalp condition, the oral medication was prescribed. Now it, too, appears to have been unhelpful. At this point, the patient requests referral to dermatology. His primary concern is that he represents a “contagious threat” to his wife and children, although none of them has shown any signs of this condition. The patient denies any skin problems prior to the nail changes and the scalp rash that manifested shortly afterward, which occurred more than a year ago. Shortly before the onset of these problems, he lost his job and had to replace it with two lower-paying part-time jobs. He denies any family history of skin disease or joint pain. There are no new pets in the house, and the patient does not work with animals. Examination reveals that the distal portions of all 10 fingernails are uniformly dystrophic and mildly onycholytic and have numerous longitudinal dark streaks. Several fingernails also have tiny scattered pits in them. The toenails are unaffected. Elsewhere, the man is observed to have salmon-pink scaly patches on the scalp and over both ears, and smaller, round plaques on the forehead, with prominent white tenacious scale. KOH prep of these latter lesions is negative for fungal elements.
A "Spider Bite" That Wasn't
ANSWER
The one unreasonable choice is a 10-day course of rifampin (choice “a”). One potential explanation for the lack of response to two different antibiotics would be the probability that there was no infection to begin with. See below for further explanation.
DISCUSSION
Erythema nodosum (EN; choice “c”) is the presumptive diagnosis in cases such as this one. The “erythemas” (multiforme, annulare centrifigum, etc) are all secondary reactions to antigenic triggers—such as herpes simplex virus, strep, or other organisms—and not primary conditions.
EN is a type of panniculitis that can be triggered by a number of conditions (eg, sarcoidosis), medicines (eg, penicillin), or organisms (eg, group A β streptococcus). It can also, as in this case, accompany inflammatory bowel disease, paralleling the flares and remissions of Crohn’s or ulcerative colitis and responding to treatment for those diseases. This is why part of the workup for EN includes evaluation for bowel disease.
The absence of breaks in the skin in such cases also speaks loudly for EN, since it involves only the adipose tissues and spares the skin. In this case, given the dearth of other suspicious items in the differential, a presumptive diagnosis of EN was quite reasonable.
Deep punch biopsy (choice “b”), which must include significant adipose tissue (5 mm or surgical wedge), can be crucial in questionable cases. It can show septal panniculitis (as opposed to lobular, which is more consistent with erythema induratum), as well as characteristic Miescher’s granulomas.
A chest radiograph (choice “d”), while not especially indicated in this case, is likewise an intelligent choice. Both tuberculosis and sarcoidosis can lead to radiographic changes and trigger EN.
If local infection were truly suspected as the direct cause of this patient’s lesions, an additional punch biopsy or two might serve to provide sufficient material for aerobic bacterial culture, acid-fast culture, and deep fungal culture—all of which are possible, though unlikely, explanations. Literally, the last thing we’d do is throw yet another antibiotic at this patient, who was in need of one simple thing: a correct diagnosis that would dictate proper treatment.
TREATMENT
A letter was dictated and sent to the gastroenterologist the patient was scheduled to see, to alert him as to our findings. If his workup
(H&P, stool cultures for salmonella, yersinia, and campylobacter, colonoscopy with biopsy) fails to pinpoint a particular trigger for her EN, additional labs will be needed. These would include antistreptolysin-O titer and tuberculosis and coccidioidomycosis skin testing, as well as actual biopsy of the lesions.
As of this writing, the patient’s GI appointment was pending, but the likely outcome will be the diagnosis of Crohn’s disease or ulcerative colitis. Treatment for either of these conditions will quiet down her EN. Often, however, EN is idiopathic and must be treated as a stand-alone diagnosis, with NSAIDs, antimalarials, or potassium iodide.
ANSWER
The one unreasonable choice is a 10-day course of rifampin (choice “a”). One potential explanation for the lack of response to two different antibiotics would be the probability that there was no infection to begin with. See below for further explanation.
DISCUSSION
Erythema nodosum (EN; choice “c”) is the presumptive diagnosis in cases such as this one. The “erythemas” (multiforme, annulare centrifigum, etc) are all secondary reactions to antigenic triggers—such as herpes simplex virus, strep, or other organisms—and not primary conditions.
EN is a type of panniculitis that can be triggered by a number of conditions (eg, sarcoidosis), medicines (eg, penicillin), or organisms (eg, group A β streptococcus). It can also, as in this case, accompany inflammatory bowel disease, paralleling the flares and remissions of Crohn’s or ulcerative colitis and responding to treatment for those diseases. This is why part of the workup for EN includes evaluation for bowel disease.
The absence of breaks in the skin in such cases also speaks loudly for EN, since it involves only the adipose tissues and spares the skin. In this case, given the dearth of other suspicious items in the differential, a presumptive diagnosis of EN was quite reasonable.
Deep punch biopsy (choice “b”), which must include significant adipose tissue (5 mm or surgical wedge), can be crucial in questionable cases. It can show septal panniculitis (as opposed to lobular, which is more consistent with erythema induratum), as well as characteristic Miescher’s granulomas.
A chest radiograph (choice “d”), while not especially indicated in this case, is likewise an intelligent choice. Both tuberculosis and sarcoidosis can lead to radiographic changes and trigger EN.
If local infection were truly suspected as the direct cause of this patient’s lesions, an additional punch biopsy or two might serve to provide sufficient material for aerobic bacterial culture, acid-fast culture, and deep fungal culture—all of which are possible, though unlikely, explanations. Literally, the last thing we’d do is throw yet another antibiotic at this patient, who was in need of one simple thing: a correct diagnosis that would dictate proper treatment.
TREATMENT
A letter was dictated and sent to the gastroenterologist the patient was scheduled to see, to alert him as to our findings. If his workup
(H&P, stool cultures for salmonella, yersinia, and campylobacter, colonoscopy with biopsy) fails to pinpoint a particular trigger for her EN, additional labs will be needed. These would include antistreptolysin-O titer and tuberculosis and coccidioidomycosis skin testing, as well as actual biopsy of the lesions.
As of this writing, the patient’s GI appointment was pending, but the likely outcome will be the diagnosis of Crohn’s disease or ulcerative colitis. Treatment for either of these conditions will quiet down her EN. Often, however, EN is idiopathic and must be treated as a stand-alone diagnosis, with NSAIDs, antimalarials, or potassium iodide.
ANSWER
The one unreasonable choice is a 10-day course of rifampin (choice “a”). One potential explanation for the lack of response to two different antibiotics would be the probability that there was no infection to begin with. See below for further explanation.
DISCUSSION
Erythema nodosum (EN; choice “c”) is the presumptive diagnosis in cases such as this one. The “erythemas” (multiforme, annulare centrifigum, etc) are all secondary reactions to antigenic triggers—such as herpes simplex virus, strep, or other organisms—and not primary conditions.
EN is a type of panniculitis that can be triggered by a number of conditions (eg, sarcoidosis), medicines (eg, penicillin), or organisms (eg, group A β streptococcus). It can also, as in this case, accompany inflammatory bowel disease, paralleling the flares and remissions of Crohn’s or ulcerative colitis and responding to treatment for those diseases. This is why part of the workup for EN includes evaluation for bowel disease.
The absence of breaks in the skin in such cases also speaks loudly for EN, since it involves only the adipose tissues and spares the skin. In this case, given the dearth of other suspicious items in the differential, a presumptive diagnosis of EN was quite reasonable.
Deep punch biopsy (choice “b”), which must include significant adipose tissue (5 mm or surgical wedge), can be crucial in questionable cases. It can show septal panniculitis (as opposed to lobular, which is more consistent with erythema induratum), as well as characteristic Miescher’s granulomas.
A chest radiograph (choice “d”), while not especially indicated in this case, is likewise an intelligent choice. Both tuberculosis and sarcoidosis can lead to radiographic changes and trigger EN.
If local infection were truly suspected as the direct cause of this patient’s lesions, an additional punch biopsy or two might serve to provide sufficient material for aerobic bacterial culture, acid-fast culture, and deep fungal culture—all of which are possible, though unlikely, explanations. Literally, the last thing we’d do is throw yet another antibiotic at this patient, who was in need of one simple thing: a correct diagnosis that would dictate proper treatment.
TREATMENT
A letter was dictated and sent to the gastroenterologist the patient was scheduled to see, to alert him as to our findings. If his workup
(H&P, stool cultures for salmonella, yersinia, and campylobacter, colonoscopy with biopsy) fails to pinpoint a particular trigger for her EN, additional labs will be needed. These would include antistreptolysin-O titer and tuberculosis and coccidioidomycosis skin testing, as well as actual biopsy of the lesions.
As of this writing, the patient’s GI appointment was pending, but the likely outcome will be the diagnosis of Crohn’s disease or ulcerative colitis. Treatment for either of these conditions will quiet down her EN. Often, however, EN is idiopathic and must be treated as a stand-alone diagnosis, with NSAIDs, antimalarials, or potassium iodide.

Sore “red bumps” began to appear on this 31-year-old woman’s posterior calves six months ago. They persisted despite a course of cephalexin (500 mg qid for 10 days), prescribed by her primary care provider for “spider bites,” and a few weeks later, a course of double-strength sulfamethoxazole/trimethoprim (bid for 10 days), for “staph infection.” When the patient is seen by dermatology, her health history is good, although she mentions a pending appointment with a gastroenterologist to investigate lower abdominal cramping and diarrhea, both of which started several months ago. There has been no weight loss, nausea, or vomiting. The patient is unaware of any bites that could explain the red patches on her legs and denies any breaks in the affected skin. No lesions are evident elsewhere on her body. There is no personal or family history of skin disease, and the patient used no OTC or prescription medication prior to the appearance of the lesions. Examination reveals several deep subcutaneous nodules palpable in the calf, ranging in size from 1.5 to 2.5 cm. There is no broken skin, nor are there other skin changes overlying the lesions, except erythema and induration. There is modest tenderness on palpation, as well as a modest increase in warmth. No nodes are palpable in the groin on that side. Examination of the patient’s skin elsewhere shows no notable changes.