User login
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM's "Best Practices in Managing a Hospital Medicine Program" course. Write to him at john.nelson@nelsonflores.com.
Concerns Grow as Top Clinicians Choose Nonclinical Roles
On a spring day a couple of years ago, I met with some internal medicine residents in a “Healthcare Systems Immersion” elective. I was to provide thoughts about the nonclinical portion of my work that I spend consulting with other hospitalist groups.
I asked for their thoughts about whether the ranks of doctors providing direct bedside care were losing too many of the most talented clinicians to nonclinical roles. The most vocal resident was confident that was not the case; these doctors would ultimately have a positive impact on the care of larger numbers of patients through administrative work than through direct patient care.
I wonder if she is right.
Numerous Hospitalists Opt for Nonnclinical Work
It seems like lots of hospitalists are transitioning to nonclinical work. My experience is that most who have administrative or other nonclinical roles continue—for part of their time—to provide direct patient care. But some leave clinical work behind altogether. Some of them are very prominent people in our field, like the top physician at CMS, the current U.S. Surgeon General, and this year’s most influential physician executive as judged by Modern Healthcare. I think it is pretty cool that these people come from our specialty.
I couldn’t find published survey data on the portion of hospitalists, or doctors in any specialty, who have entirely (or almost entirely) nonclinical roles. My impression is that this was a vanishingly small number across all specialties 30 or 40 years ago, but it seems to have increased pretty dramatically in the last 10 years. At the start of my career, few hospitals had a physician in an administrative position. Now it is common.
Physician leadership roles now include information technology (CMIO), quality (CQO), leader of the employed physician group, and hospital CEO (at least two hospitalists I know are in this role). And there are lots of nonclinical roles for doctors outside of hospitals.
Pros, Cons for Healthcare
I’ve had mixed feelings watching many people leave clinical practice. Most of them, like those mentioned above, continue to make important contributions to our healthcare system; they improve the services and care patients receive. Yet it seems like some of the best clinicians are taken from active practice and are difficult to replace.
At the start of my career, the few doctors who left clinical practice for nonclinical work tended to do so late in their careers. Now many make this choice very early in their careers. Of the six or seven residents I met with above, several planned to pursue entirely nonclinical work either immediately upon completing residency or after just a few years of clinical practice. They were at one of the top internal medicine programs in the country and will, presumably, provide direct clinical care to a really small number of patients over their careers.
It makes me wonder if there is a meaningful effect of more talented people having, and exercising, the option to leave clinical practice, resulting in a tilt toward somewhat-less-talented doctors left to treat patients. I hope there is no meaningful effect in this direction, but I’m not sure.
Reasons to Move
My experience is that most doctors who have left clinical work will wax eloquent about how they really loved it and weren’t fleeing it but did so because they wanted to “try something new” or contribute to healthcare in other ways. I’m suspicious that for many of them this isn’t entirely true. Some must have been fleeing it. They were burned out, tired of being on call, and so on, and were eager to find relief from clinical work more than they were “drawn to a new career challenge.” They just don’t want to admit it.
I sometimes think about what several nationally prominent hospitalist leaders have said to me over my career. Not long ago, one said, “Wow. You’re still seeing patients and making rounds? I can’t believe it. You need to find something better.”
This doctor seemed to equate an entire career spent in clinical practice as something done mostly by those who aren’t talented enough to have other options. What a change from 30 or 40 years ago.
Several years ago, in a very moving conversation, another nationally prominent hospitalist leader told me, “It’s all about the patient and how we care for them at the bedside. There’s no better way we can spend our time.”
The Best Career
Within a few years, he left clinical practice entirely, even though he was still mid-career.
I hold in highest esteem hospitalists and other doctors who spend a full career in direct patient care and do it well. At the top of that list is my own dad, who is up there with Osler when it comes to dedicated physicians.
Of course, those who spend most or all of their time in nonclinical work really can make important contributions that help the healthcare system better serve patients, in some cases clearly making a bigger difference for more patients than they could via direct clinical care. We need talented people in both roles, but we also need to always be looking for ways to minimize the numbers of doctors who feel the need to flee a clinical career.
Like many hospitalists, I think about these things a lot when making decisions about my own career. I hope we all have the wisdom to make the best choices for ourselves, and for the patients we set out to serve when we entered medical school. TH

On a spring day a couple of years ago, I met with some internal medicine residents in a “Healthcare Systems Immersion” elective. I was to provide thoughts about the nonclinical portion of my work that I spend consulting with other hospitalist groups.
I asked for their thoughts about whether the ranks of doctors providing direct bedside care were losing too many of the most talented clinicians to nonclinical roles. The most vocal resident was confident that was not the case; these doctors would ultimately have a positive impact on the care of larger numbers of patients through administrative work than through direct patient care.
I wonder if she is right.
Numerous Hospitalists Opt for Nonnclinical Work
It seems like lots of hospitalists are transitioning to nonclinical work. My experience is that most who have administrative or other nonclinical roles continue—for part of their time—to provide direct patient care. But some leave clinical work behind altogether. Some of them are very prominent people in our field, like the top physician at CMS, the current U.S. Surgeon General, and this year’s most influential physician executive as judged by Modern Healthcare. I think it is pretty cool that these people come from our specialty.
I couldn’t find published survey data on the portion of hospitalists, or doctors in any specialty, who have entirely (or almost entirely) nonclinical roles. My impression is that this was a vanishingly small number across all specialties 30 or 40 years ago, but it seems to have increased pretty dramatically in the last 10 years. At the start of my career, few hospitals had a physician in an administrative position. Now it is common.
Physician leadership roles now include information technology (CMIO), quality (CQO), leader of the employed physician group, and hospital CEO (at least two hospitalists I know are in this role). And there are lots of nonclinical roles for doctors outside of hospitals.
Pros, Cons for Healthcare
I’ve had mixed feelings watching many people leave clinical practice. Most of them, like those mentioned above, continue to make important contributions to our healthcare system; they improve the services and care patients receive. Yet it seems like some of the best clinicians are taken from active practice and are difficult to replace.
At the start of my career, the few doctors who left clinical practice for nonclinical work tended to do so late in their careers. Now many make this choice very early in their careers. Of the six or seven residents I met with above, several planned to pursue entirely nonclinical work either immediately upon completing residency or after just a few years of clinical practice. They were at one of the top internal medicine programs in the country and will, presumably, provide direct clinical care to a really small number of patients over their careers.
It makes me wonder if there is a meaningful effect of more talented people having, and exercising, the option to leave clinical practice, resulting in a tilt toward somewhat-less-talented doctors left to treat patients. I hope there is no meaningful effect in this direction, but I’m not sure.
Reasons to Move
My experience is that most doctors who have left clinical work will wax eloquent about how they really loved it and weren’t fleeing it but did so because they wanted to “try something new” or contribute to healthcare in other ways. I’m suspicious that for many of them this isn’t entirely true. Some must have been fleeing it. They were burned out, tired of being on call, and so on, and were eager to find relief from clinical work more than they were “drawn to a new career challenge.” They just don’t want to admit it.
I sometimes think about what several nationally prominent hospitalist leaders have said to me over my career. Not long ago, one said, “Wow. You’re still seeing patients and making rounds? I can’t believe it. You need to find something better.”
This doctor seemed to equate an entire career spent in clinical practice as something done mostly by those who aren’t talented enough to have other options. What a change from 30 or 40 years ago.
Several years ago, in a very moving conversation, another nationally prominent hospitalist leader told me, “It’s all about the patient and how we care for them at the bedside. There’s no better way we can spend our time.”
The Best Career
Within a few years, he left clinical practice entirely, even though he was still mid-career.
I hold in highest esteem hospitalists and other doctors who spend a full career in direct patient care and do it well. At the top of that list is my own dad, who is up there with Osler when it comes to dedicated physicians.
Of course, those who spend most or all of their time in nonclinical work really can make important contributions that help the healthcare system better serve patients, in some cases clearly making a bigger difference for more patients than they could via direct clinical care. We need talented people in both roles, but we also need to always be looking for ways to minimize the numbers of doctors who feel the need to flee a clinical career.
Like many hospitalists, I think about these things a lot when making decisions about my own career. I hope we all have the wisdom to make the best choices for ourselves, and for the patients we set out to serve when we entered medical school. TH

On a spring day a couple of years ago, I met with some internal medicine residents in a “Healthcare Systems Immersion” elective. I was to provide thoughts about the nonclinical portion of my work that I spend consulting with other hospitalist groups.
I asked for their thoughts about whether the ranks of doctors providing direct bedside care were losing too many of the most talented clinicians to nonclinical roles. The most vocal resident was confident that was not the case; these doctors would ultimately have a positive impact on the care of larger numbers of patients through administrative work than through direct patient care.
I wonder if she is right.
Numerous Hospitalists Opt for Nonnclinical Work
It seems like lots of hospitalists are transitioning to nonclinical work. My experience is that most who have administrative or other nonclinical roles continue—for part of their time—to provide direct patient care. But some leave clinical work behind altogether. Some of them are very prominent people in our field, like the top physician at CMS, the current U.S. Surgeon General, and this year’s most influential physician executive as judged by Modern Healthcare. I think it is pretty cool that these people come from our specialty.
I couldn’t find published survey data on the portion of hospitalists, or doctors in any specialty, who have entirely (or almost entirely) nonclinical roles. My impression is that this was a vanishingly small number across all specialties 30 or 40 years ago, but it seems to have increased pretty dramatically in the last 10 years. At the start of my career, few hospitals had a physician in an administrative position. Now it is common.
Physician leadership roles now include information technology (CMIO), quality (CQO), leader of the employed physician group, and hospital CEO (at least two hospitalists I know are in this role). And there are lots of nonclinical roles for doctors outside of hospitals.
Pros, Cons for Healthcare
I’ve had mixed feelings watching many people leave clinical practice. Most of them, like those mentioned above, continue to make important contributions to our healthcare system; they improve the services and care patients receive. Yet it seems like some of the best clinicians are taken from active practice and are difficult to replace.
At the start of my career, the few doctors who left clinical practice for nonclinical work tended to do so late in their careers. Now many make this choice very early in their careers. Of the six or seven residents I met with above, several planned to pursue entirely nonclinical work either immediately upon completing residency or after just a few years of clinical practice. They were at one of the top internal medicine programs in the country and will, presumably, provide direct clinical care to a really small number of patients over their careers.
It makes me wonder if there is a meaningful effect of more talented people having, and exercising, the option to leave clinical practice, resulting in a tilt toward somewhat-less-talented doctors left to treat patients. I hope there is no meaningful effect in this direction, but I’m not sure.
Reasons to Move
My experience is that most doctors who have left clinical work will wax eloquent about how they really loved it and weren’t fleeing it but did so because they wanted to “try something new” or contribute to healthcare in other ways. I’m suspicious that for many of them this isn’t entirely true. Some must have been fleeing it. They were burned out, tired of being on call, and so on, and were eager to find relief from clinical work more than they were “drawn to a new career challenge.” They just don’t want to admit it.
I sometimes think about what several nationally prominent hospitalist leaders have said to me over my career. Not long ago, one said, “Wow. You’re still seeing patients and making rounds? I can’t believe it. You need to find something better.”
This doctor seemed to equate an entire career spent in clinical practice as something done mostly by those who aren’t talented enough to have other options. What a change from 30 or 40 years ago.
Several years ago, in a very moving conversation, another nationally prominent hospitalist leader told me, “It’s all about the patient and how we care for them at the bedside. There’s no better way we can spend our time.”
The Best Career
Within a few years, he left clinical practice entirely, even though he was still mid-career.
I hold in highest esteem hospitalists and other doctors who spend a full career in direct patient care and do it well. At the top of that list is my own dad, who is up there with Osler when it comes to dedicated physicians.
Of course, those who spend most or all of their time in nonclinical work really can make important contributions that help the healthcare system better serve patients, in some cases clearly making a bigger difference for more patients than they could via direct clinical care. We need talented people in both roles, but we also need to always be looking for ways to minimize the numbers of doctors who feel the need to flee a clinical career.
Like many hospitalists, I think about these things a lot when making decisions about my own career. I hope we all have the wisdom to make the best choices for ourselves, and for the patients we set out to serve when we entered medical school. TH

Poor Continuity of Patient Care Increases Work for Hospitalist Groups
I think every hospitalist group should diligently try to maximize hospitalist-patient continuity, but many seem to adopt schedules and other operational practices that erode it. Let’s walk through the issue of continuity, starting with some history.
Inpatient Continuity in Old Healthcare System
Proudly carrying a pager nearly the size of a loaf of bread and wearing a white shirt and pants with Converse All Stars, I served as a hospital orderly in the 1970s. This position involved things like getting patients out of bed, placing Foley catheters, performing chest compressions during codes, and transporting the bodies of the deceased to the morgue. I really enjoyed the work, and the experience serves as one of my historical frames of reference for how hospital care has evolved since then.
The way I remember it, nearly everyone at the hospital worked a predictable schedule. RN staffing was the same each day; it didn’t vary based on census. Each full-time RN worked five shifts a week, eight hours each. Most or all would work alternate weekends and would have two compensatory days off during the following work week. This resulted in terrific continuity between nurse and patient, and the long length of stays meant patients and nurses got to know one another really well.
Continuity Takes a Hit
But things have changed. Nurse-patient continuity seems to have declined significantly as a result of two main forces: the hospital’s efforts to reduce staffing costs by varying nurse staffing to match daily patient volume, and nurses’ desire for a wide variety of work schedules. Asking a bedside nurse in today’s hospital whether the patient’s confusion, diarrhea, or appetite is meaningfully different today than yesterday typically yields the same reply. “This is my first day with the patient; I’ll have to look at the chart.”
I couldn’t find many research articles or editorials regarding hospital nurse-patient continuity from one day to the next. But several researchers seem to have begun studying this issue and have recently published a proposed framework for assessing it, and I found one study showing it wasn’t correlated with rates of pressure ulcers.1,2.
My anecdotal experience tells me continuity between the patient and caregivers of all stripes matters a lot. Research will be valuable in helping us to better understand its most significant costs and benefits, but I’m already convinced “Continuity is King” and should be one of the most important factors in the design of work schedules and patient allocation models for nurses and hospitalists alike.
While some might say we should wait for randomized trials of continuity to determine its importance, I’m inclined to see it like the authors of “Parachute use to prevent death and major trauma related to gravitational challenge: systematic review of randomised controlled trials.” As a ding against those who insist on research data when common sense may be sufficient, they concluded “…that everyone might benefit if the most radical protagonists of evidence-based medicine organised and participated in a double-blind, randomised, placebo-controlled, crossover trial of the parachute.3
Continuity and Hospitalists
On top of what I see as erosion in nurse-patient continuity, the arrival of hospitalists disrupted doctor-patient continuity across the inpatient and outpatient setting. While there was significant concern about this when our field first took off in the 1990s, it seems to be getting a great deal less attention over the last few years. In many hospitalist groups I work with, it is one of the last factors considered when creating a work schedule. Factors that are examined include the following:
- Solely for provider convenience, a group might regularly schedule a provider for only two or three consecutive daytime shifts, or sometimes only single days;
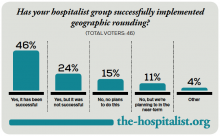
- Groups that use unit-based hospital (a.k.a. “geographic”) staffing might have a patient transfer to a different attending hospitalist solely as a result of moving to a room in a different nursing unit; and
- As part of morning load leveling, some groups reassign existing patients to a new hospitalist.
I think all groups should work hard to avoid doing these things. And while I seem to be a real outlier on this one, I think the benefits of a separate daytime hospitalist admitter shift are not worth the cost of having different doctors always do the admission and first follow-up visit. Most groups should consider moving the admitter into an additional rounder position and allocating daytime admissions across all hospitalists.
One study found that hospitalist discontinuity was not associated with adverse events, and another found it was associated with higher length of stay for selected diagnoses.4,5 But there is too little research to draw hard conclusions. I’m convinced poor continuity increases the possibility of handoff-related errors, likely results in lower patient satisfaction, and increases the overall work of the hospitalist group, because more providers have to take the time to get to know the patient.
Although there will always be some tension between terrific continuity and a sustainable hospitalist lifestyle—a person can work only so many consecutive days before wearing out—every group should thoughtfully consider whether they are doing everything reasonable to maximize continuity. After all, continuity is king.

References
- Stifter J, Yao Y, Lopez KC, Khokhar A, Wilkie DJ, Keenan GM. Proposing a new conceptual model and an exemplar measure using health information technology to examine the impact of relational nurse continuity on hospital-acquired pressure ulcers. ANS Adv Nurs Sci. 2015;38(3):241-251.
- Stifter J, Yao Y, Lodhi MK, et al. Nurse continuity and hospital-acquired pressure ulcers: a comparative analysis using an electronic health record “big data” set. Nurs Res. 2015;64(5):361-371.
- Smith GC, Pell JP. Parachute use to prevent death and major trauma related to gravitational challenge: systematic review of randomised controlled trials. BMJ. 2003;327(7429):1459-1461.
- O’Leary KJ, Turner J, Christensen N, et al. The effect of hospitalist discontinuity on adverse events. J Hosp Med. 2015;10(3):147-151.
- Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-338.
I think every hospitalist group should diligently try to maximize hospitalist-patient continuity, but many seem to adopt schedules and other operational practices that erode it. Let’s walk through the issue of continuity, starting with some history.
Inpatient Continuity in Old Healthcare System
Proudly carrying a pager nearly the size of a loaf of bread and wearing a white shirt and pants with Converse All Stars, I served as a hospital orderly in the 1970s. This position involved things like getting patients out of bed, placing Foley catheters, performing chest compressions during codes, and transporting the bodies of the deceased to the morgue. I really enjoyed the work, and the experience serves as one of my historical frames of reference for how hospital care has evolved since then.
The way I remember it, nearly everyone at the hospital worked a predictable schedule. RN staffing was the same each day; it didn’t vary based on census. Each full-time RN worked five shifts a week, eight hours each. Most or all would work alternate weekends and would have two compensatory days off during the following work week. This resulted in terrific continuity between nurse and patient, and the long length of stays meant patients and nurses got to know one another really well.
Continuity Takes a Hit
But things have changed. Nurse-patient continuity seems to have declined significantly as a result of two main forces: the hospital’s efforts to reduce staffing costs by varying nurse staffing to match daily patient volume, and nurses’ desire for a wide variety of work schedules. Asking a bedside nurse in today’s hospital whether the patient’s confusion, diarrhea, or appetite is meaningfully different today than yesterday typically yields the same reply. “This is my first day with the patient; I’ll have to look at the chart.”
I couldn’t find many research articles or editorials regarding hospital nurse-patient continuity from one day to the next. But several researchers seem to have begun studying this issue and have recently published a proposed framework for assessing it, and I found one study showing it wasn’t correlated with rates of pressure ulcers.1,2.
My anecdotal experience tells me continuity between the patient and caregivers of all stripes matters a lot. Research will be valuable in helping us to better understand its most significant costs and benefits, but I’m already convinced “Continuity is King” and should be one of the most important factors in the design of work schedules and patient allocation models for nurses and hospitalists alike.
While some might say we should wait for randomized trials of continuity to determine its importance, I’m inclined to see it like the authors of “Parachute use to prevent death and major trauma related to gravitational challenge: systematic review of randomised controlled trials.” As a ding against those who insist on research data when common sense may be sufficient, they concluded “…that everyone might benefit if the most radical protagonists of evidence-based medicine organised and participated in a double-blind, randomised, placebo-controlled, crossover trial of the parachute.3
Continuity and Hospitalists
On top of what I see as erosion in nurse-patient continuity, the arrival of hospitalists disrupted doctor-patient continuity across the inpatient and outpatient setting. While there was significant concern about this when our field first took off in the 1990s, it seems to be getting a great deal less attention over the last few years. In many hospitalist groups I work with, it is one of the last factors considered when creating a work schedule. Factors that are examined include the following:
- Solely for provider convenience, a group might regularly schedule a provider for only two or three consecutive daytime shifts, or sometimes only single days;
- Groups that use unit-based hospital (a.k.a. “geographic”) staffing might have a patient transfer to a different attending hospitalist solely as a result of moving to a room in a different nursing unit; and
- As part of morning load leveling, some groups reassign existing patients to a new hospitalist.
I think all groups should work hard to avoid doing these things. And while I seem to be a real outlier on this one, I think the benefits of a separate daytime hospitalist admitter shift are not worth the cost of having different doctors always do the admission and first follow-up visit. Most groups should consider moving the admitter into an additional rounder position and allocating daytime admissions across all hospitalists.
One study found that hospitalist discontinuity was not associated with adverse events, and another found it was associated with higher length of stay for selected diagnoses.4,5 But there is too little research to draw hard conclusions. I’m convinced poor continuity increases the possibility of handoff-related errors, likely results in lower patient satisfaction, and increases the overall work of the hospitalist group, because more providers have to take the time to get to know the patient.
Although there will always be some tension between terrific continuity and a sustainable hospitalist lifestyle—a person can work only so many consecutive days before wearing out—every group should thoughtfully consider whether they are doing everything reasonable to maximize continuity. After all, continuity is king.

References
- Stifter J, Yao Y, Lopez KC, Khokhar A, Wilkie DJ, Keenan GM. Proposing a new conceptual model and an exemplar measure using health information technology to examine the impact of relational nurse continuity on hospital-acquired pressure ulcers. ANS Adv Nurs Sci. 2015;38(3):241-251.
- Stifter J, Yao Y, Lodhi MK, et al. Nurse continuity and hospital-acquired pressure ulcers: a comparative analysis using an electronic health record “big data” set. Nurs Res. 2015;64(5):361-371.
- Smith GC, Pell JP. Parachute use to prevent death and major trauma related to gravitational challenge: systematic review of randomised controlled trials. BMJ. 2003;327(7429):1459-1461.
- O’Leary KJ, Turner J, Christensen N, et al. The effect of hospitalist discontinuity on adverse events. J Hosp Med. 2015;10(3):147-151.
- Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-338.
I think every hospitalist group should diligently try to maximize hospitalist-patient continuity, but many seem to adopt schedules and other operational practices that erode it. Let’s walk through the issue of continuity, starting with some history.
Inpatient Continuity in Old Healthcare System
Proudly carrying a pager nearly the size of a loaf of bread and wearing a white shirt and pants with Converse All Stars, I served as a hospital orderly in the 1970s. This position involved things like getting patients out of bed, placing Foley catheters, performing chest compressions during codes, and transporting the bodies of the deceased to the morgue. I really enjoyed the work, and the experience serves as one of my historical frames of reference for how hospital care has evolved since then.
The way I remember it, nearly everyone at the hospital worked a predictable schedule. RN staffing was the same each day; it didn’t vary based on census. Each full-time RN worked five shifts a week, eight hours each. Most or all would work alternate weekends and would have two compensatory days off during the following work week. This resulted in terrific continuity between nurse and patient, and the long length of stays meant patients and nurses got to know one another really well.
Continuity Takes a Hit
But things have changed. Nurse-patient continuity seems to have declined significantly as a result of two main forces: the hospital’s efforts to reduce staffing costs by varying nurse staffing to match daily patient volume, and nurses’ desire for a wide variety of work schedules. Asking a bedside nurse in today’s hospital whether the patient’s confusion, diarrhea, or appetite is meaningfully different today than yesterday typically yields the same reply. “This is my first day with the patient; I’ll have to look at the chart.”
I couldn’t find many research articles or editorials regarding hospital nurse-patient continuity from one day to the next. But several researchers seem to have begun studying this issue and have recently published a proposed framework for assessing it, and I found one study showing it wasn’t correlated with rates of pressure ulcers.1,2.
My anecdotal experience tells me continuity between the patient and caregivers of all stripes matters a lot. Research will be valuable in helping us to better understand its most significant costs and benefits, but I’m already convinced “Continuity is King” and should be one of the most important factors in the design of work schedules and patient allocation models for nurses and hospitalists alike.
While some might say we should wait for randomized trials of continuity to determine its importance, I’m inclined to see it like the authors of “Parachute use to prevent death and major trauma related to gravitational challenge: systematic review of randomised controlled trials.” As a ding against those who insist on research data when common sense may be sufficient, they concluded “…that everyone might benefit if the most radical protagonists of evidence-based medicine organised and participated in a double-blind, randomised, placebo-controlled, crossover trial of the parachute.3
Continuity and Hospitalists
On top of what I see as erosion in nurse-patient continuity, the arrival of hospitalists disrupted doctor-patient continuity across the inpatient and outpatient setting. While there was significant concern about this when our field first took off in the 1990s, it seems to be getting a great deal less attention over the last few years. In many hospitalist groups I work with, it is one of the last factors considered when creating a work schedule. Factors that are examined include the following:
- Solely for provider convenience, a group might regularly schedule a provider for only two or three consecutive daytime shifts, or sometimes only single days;
- Groups that use unit-based hospital (a.k.a. “geographic”) staffing might have a patient transfer to a different attending hospitalist solely as a result of moving to a room in a different nursing unit; and
- As part of morning load leveling, some groups reassign existing patients to a new hospitalist.
I think all groups should work hard to avoid doing these things. And while I seem to be a real outlier on this one, I think the benefits of a separate daytime hospitalist admitter shift are not worth the cost of having different doctors always do the admission and first follow-up visit. Most groups should consider moving the admitter into an additional rounder position and allocating daytime admissions across all hospitalists.
One study found that hospitalist discontinuity was not associated with adverse events, and another found it was associated with higher length of stay for selected diagnoses.4,5 But there is too little research to draw hard conclusions. I’m convinced poor continuity increases the possibility of handoff-related errors, likely results in lower patient satisfaction, and increases the overall work of the hospitalist group, because more providers have to take the time to get to know the patient.
Although there will always be some tension between terrific continuity and a sustainable hospitalist lifestyle—a person can work only so many consecutive days before wearing out—every group should thoughtfully consider whether they are doing everything reasonable to maximize continuity. After all, continuity is king.

References
- Stifter J, Yao Y, Lopez KC, Khokhar A, Wilkie DJ, Keenan GM. Proposing a new conceptual model and an exemplar measure using health information technology to examine the impact of relational nurse continuity on hospital-acquired pressure ulcers. ANS Adv Nurs Sci. 2015;38(3):241-251.
- Stifter J, Yao Y, Lodhi MK, et al. Nurse continuity and hospital-acquired pressure ulcers: a comparative analysis using an electronic health record “big data” set. Nurs Res. 2015;64(5):361-371.
- Smith GC, Pell JP. Parachute use to prevent death and major trauma related to gravitational challenge: systematic review of randomised controlled trials. BMJ. 2003;327(7429):1459-1461.
- O’Leary KJ, Turner J, Christensen N, et al. The effect of hospitalist discontinuity on adverse events. J Hosp Med. 2015;10(3):147-151.
- Epstein K, Juarez E, Epstein A, Loya K, Singer A. The impact of fragmentation of hospitalist care on length of stay. J Hosp Med. 2010;5(6):335-338.
Eliminations Hospitalist Groups Should Consider
Editor’s note: Second in a continuing series of articles exploring ways hospitalist groups can cut back.
In last month’s column, I made the case that most hospitalist groups should think about doing away with a morning meeting to distribute overnight admissions and changing a daytime admitter shift into another rounder and having all of the day rounders share admissions. Here I’ll describe additional things in place at some hospitalist groups that should probably be eliminated.
Obscuring Attending Hospitalist Name
Some hospitalist groups admit patients to the “blue team” or “gold team” or use a similar system. I encountered one place that had a fuchsia team. Such designations typically take the place of the attending physician’s name and can be convenient when one hospitalist goes off service and is replaced by another; the team name stays the same. Even if the attending hospitalist makes up the entire team (i.e., no residents or students), some groups use the “team” name rather than the attending hospitalist name.
But when the patient’s chart, sign on the door, and other identifying materials all refer only to the team that is caring for the patient, the patients, their families, and most hospital staff don’t have an easy way to identify the responsible physician. Say a worried daughter steps into the hall to ask the nurse, “Which doctor is taking care of my dad?” The nurse might readily see that the blue team is responsible but may not know which hospitalist is working on the blue team today and might have to walk back to the nursing station to look over a sheet of paper (a “decoder ring”) to figure out the hospitalist’s name.
This scenario has all kinds of drawbacks. To the daughter, the name of the doctor in charge is a big deal. It doesn’t inspire confidence if the nurse can’t readily say who that is. And the busy nurse might forget to investigate and provide the name to the daughter in a timely way.
I think groups using a system like this should seriously consider replacing team names with the attending hospitalist name and updating that name in the medical record, whether that is an EHR, a paper chart, or some other form, every time that doctor rotates off service and is replaced by another. Hospital staff, patients, and families should always see the name of the attending physician and not an uninformative color or nondescript team name.
It will require work for someone, the hospitalist in many cases, to go into the EHR and write an order or send a message to ensure that the hospitalist name is kept current every time one doctor replaces another. But it’s worth the effort.
Day Hospitalists Should Round on Patients Admitted after Midnight
Although not exactly common, I’ve come across this scenario often enough that it’s worth mentioning.
Hospitalists, sometimes with a hint of indignity or even chest thumping, have told me they don’t visit or round on patients admitted after midnight by their night doctor. “You can’t bill for a second visit on the same calendar day,” they explain, firmly. “So if I can’t get paid to see the patient, then I won’t.”
This is just crazy.
For one thing, these same doctors are typically employed by the hospital and are being paid to provide whatever care patients need. I think they’ve just latched onto the “can’t bill another visit” as an excuse to get out of some work.
Don’t forget that many of these patients may wait over 30 hours from their admitting visit to the first follow-up visit; this delay is at the beginning of their hospital stay, when they might be most unstable. And it delays initiation of discharge planning and other important steps in patient care.
I don’t see any room for meaningful debate on this. The rounder who picks up a patient admitted the night before should always make a full rounding visit, even if the admission was after midnight.
But if the visit isn’t billable, you are freed from the typical billing-related documentation requirements. No need to document detail in the note that doesn’t meaningfully contribute to the care of the patient. For example, you might omit a chief complaint for this encounter.
Daytime Triage Doctor
Practices larger than about 20 full-time equivalents often have one daytime doctor hold a “triage” or “hot” pager, which others call to make a new referral. This triage doctor will hear about all referrals and keep track of and contact the hospitalist responsible for the next new patient. This can be a very busy job and often comes on top of a full clinical load for that doctor.
As I mentioned in my July 2015 and December 2010 articles, in many or most groups, a clerical person could take over this function, at least during business hours.
Vacation Time
In many or most cases, hospitalists that have specified vacation time are not getting a better deal than those that have no vacation time. What really matters is how many shifts you’re responsible for in a year. For the days you aren’t on shift, in most hospitalist groups it really doesn’t matter whether you label some of them as vacation days or CME days.
I discussed this issue in greater detail in my March 2007 article.
But if you’re in the 30% of hospitalist groups that have a vacation (or PTO) provision currently and it works well, then there certainly isn’t a compelling reason to change or do away with it.

Editor’s note: Second in a continuing series of articles exploring ways hospitalist groups can cut back.
In last month’s column, I made the case that most hospitalist groups should think about doing away with a morning meeting to distribute overnight admissions and changing a daytime admitter shift into another rounder and having all of the day rounders share admissions. Here I’ll describe additional things in place at some hospitalist groups that should probably be eliminated.
Obscuring Attending Hospitalist Name
Some hospitalist groups admit patients to the “blue team” or “gold team” or use a similar system. I encountered one place that had a fuchsia team. Such designations typically take the place of the attending physician’s name and can be convenient when one hospitalist goes off service and is replaced by another; the team name stays the same. Even if the attending hospitalist makes up the entire team (i.e., no residents or students), some groups use the “team” name rather than the attending hospitalist name.
But when the patient’s chart, sign on the door, and other identifying materials all refer only to the team that is caring for the patient, the patients, their families, and most hospital staff don’t have an easy way to identify the responsible physician. Say a worried daughter steps into the hall to ask the nurse, “Which doctor is taking care of my dad?” The nurse might readily see that the blue team is responsible but may not know which hospitalist is working on the blue team today and might have to walk back to the nursing station to look over a sheet of paper (a “decoder ring”) to figure out the hospitalist’s name.
This scenario has all kinds of drawbacks. To the daughter, the name of the doctor in charge is a big deal. It doesn’t inspire confidence if the nurse can’t readily say who that is. And the busy nurse might forget to investigate and provide the name to the daughter in a timely way.
I think groups using a system like this should seriously consider replacing team names with the attending hospitalist name and updating that name in the medical record, whether that is an EHR, a paper chart, or some other form, every time that doctor rotates off service and is replaced by another. Hospital staff, patients, and families should always see the name of the attending physician and not an uninformative color or nondescript team name.
It will require work for someone, the hospitalist in many cases, to go into the EHR and write an order or send a message to ensure that the hospitalist name is kept current every time one doctor replaces another. But it’s worth the effort.
Day Hospitalists Should Round on Patients Admitted after Midnight
Although not exactly common, I’ve come across this scenario often enough that it’s worth mentioning.
Hospitalists, sometimes with a hint of indignity or even chest thumping, have told me they don’t visit or round on patients admitted after midnight by their night doctor. “You can’t bill for a second visit on the same calendar day,” they explain, firmly. “So if I can’t get paid to see the patient, then I won’t.”
This is just crazy.
For one thing, these same doctors are typically employed by the hospital and are being paid to provide whatever care patients need. I think they’ve just latched onto the “can’t bill another visit” as an excuse to get out of some work.
Don’t forget that many of these patients may wait over 30 hours from their admitting visit to the first follow-up visit; this delay is at the beginning of their hospital stay, when they might be most unstable. And it delays initiation of discharge planning and other important steps in patient care.
I don’t see any room for meaningful debate on this. The rounder who picks up a patient admitted the night before should always make a full rounding visit, even if the admission was after midnight.
But if the visit isn’t billable, you are freed from the typical billing-related documentation requirements. No need to document detail in the note that doesn’t meaningfully contribute to the care of the patient. For example, you might omit a chief complaint for this encounter.
Daytime Triage Doctor
Practices larger than about 20 full-time equivalents often have one daytime doctor hold a “triage” or “hot” pager, which others call to make a new referral. This triage doctor will hear about all referrals and keep track of and contact the hospitalist responsible for the next new patient. This can be a very busy job and often comes on top of a full clinical load for that doctor.
As I mentioned in my July 2015 and December 2010 articles, in many or most groups, a clerical person could take over this function, at least during business hours.
Vacation Time
In many or most cases, hospitalists that have specified vacation time are not getting a better deal than those that have no vacation time. What really matters is how many shifts you’re responsible for in a year. For the days you aren’t on shift, in most hospitalist groups it really doesn’t matter whether you label some of them as vacation days or CME days.
I discussed this issue in greater detail in my March 2007 article.
But if you’re in the 30% of hospitalist groups that have a vacation (or PTO) provision currently and it works well, then there certainly isn’t a compelling reason to change or do away with it.

Editor’s note: Second in a continuing series of articles exploring ways hospitalist groups can cut back.
In last month’s column, I made the case that most hospitalist groups should think about doing away with a morning meeting to distribute overnight admissions and changing a daytime admitter shift into another rounder and having all of the day rounders share admissions. Here I’ll describe additional things in place at some hospitalist groups that should probably be eliminated.
Obscuring Attending Hospitalist Name
Some hospitalist groups admit patients to the “blue team” or “gold team” or use a similar system. I encountered one place that had a fuchsia team. Such designations typically take the place of the attending physician’s name and can be convenient when one hospitalist goes off service and is replaced by another; the team name stays the same. Even if the attending hospitalist makes up the entire team (i.e., no residents or students), some groups use the “team” name rather than the attending hospitalist name.
But when the patient’s chart, sign on the door, and other identifying materials all refer only to the team that is caring for the patient, the patients, their families, and most hospital staff don’t have an easy way to identify the responsible physician. Say a worried daughter steps into the hall to ask the nurse, “Which doctor is taking care of my dad?” The nurse might readily see that the blue team is responsible but may not know which hospitalist is working on the blue team today and might have to walk back to the nursing station to look over a sheet of paper (a “decoder ring”) to figure out the hospitalist’s name.
This scenario has all kinds of drawbacks. To the daughter, the name of the doctor in charge is a big deal. It doesn’t inspire confidence if the nurse can’t readily say who that is. And the busy nurse might forget to investigate and provide the name to the daughter in a timely way.
I think groups using a system like this should seriously consider replacing team names with the attending hospitalist name and updating that name in the medical record, whether that is an EHR, a paper chart, or some other form, every time that doctor rotates off service and is replaced by another. Hospital staff, patients, and families should always see the name of the attending physician and not an uninformative color or nondescript team name.
It will require work for someone, the hospitalist in many cases, to go into the EHR and write an order or send a message to ensure that the hospitalist name is kept current every time one doctor replaces another. But it’s worth the effort.
Day Hospitalists Should Round on Patients Admitted after Midnight
Although not exactly common, I’ve come across this scenario often enough that it’s worth mentioning.
Hospitalists, sometimes with a hint of indignity or even chest thumping, have told me they don’t visit or round on patients admitted after midnight by their night doctor. “You can’t bill for a second visit on the same calendar day,” they explain, firmly. “So if I can’t get paid to see the patient, then I won’t.”
This is just crazy.
For one thing, these same doctors are typically employed by the hospital and are being paid to provide whatever care patients need. I think they’ve just latched onto the “can’t bill another visit” as an excuse to get out of some work.
Don’t forget that many of these patients may wait over 30 hours from their admitting visit to the first follow-up visit; this delay is at the beginning of their hospital stay, when they might be most unstable. And it delays initiation of discharge planning and other important steps in patient care.
I don’t see any room for meaningful debate on this. The rounder who picks up a patient admitted the night before should always make a full rounding visit, even if the admission was after midnight.
But if the visit isn’t billable, you are freed from the typical billing-related documentation requirements. No need to document detail in the note that doesn’t meaningfully contribute to the care of the patient. For example, you might omit a chief complaint for this encounter.
Daytime Triage Doctor
Practices larger than about 20 full-time equivalents often have one daytime doctor hold a “triage” or “hot” pager, which others call to make a new referral. This triage doctor will hear about all referrals and keep track of and contact the hospitalist responsible for the next new patient. This can be a very busy job and often comes on top of a full clinical load for that doctor.
As I mentioned in my July 2015 and December 2010 articles, in many or most groups, a clerical person could take over this function, at least during business hours.
Vacation Time
In many or most cases, hospitalists that have specified vacation time are not getting a better deal than those that have no vacation time. What really matters is how many shifts you’re responsible for in a year. For the days you aren’t on shift, in most hospitalist groups it really doesn’t matter whether you label some of them as vacation days or CME days.
I discussed this issue in greater detail in my March 2007 article.
But if you’re in the 30% of hospitalist groups that have a vacation (or PTO) provision currently and it works well, then there certainly isn’t a compelling reason to change or do away with it.

Hospital Groups Might Do Better Without Daytime Admission Shifts, Morning Meetings
You shouldn’t maintain things that do not deliver the value you anticipated when you first put them in place. For example, I thought Netflix streaming would be terrific, but I have used it so infrequently that it probably costs me $50 per movie or show watched. I should probably dump it.
Your hospitalist group might have some operational practices that are not as valuable as they seem and could be replaced with something better. For many groups, this might include doing away with a separate daytime admitter shift and a morning meeting to distribute the overnight admissions.
Daytime Admission Shift
My experience is that hospitalist groups with more than about five daytime doctors almost always have a day-shift person dedicated to seeing new admissions. In most cases, this procedure is implemented with the idea of reducing the stress of other day-shift doctors, who don’t have to interrupt rounds to admit a new patient. Some see a dedicated admitter as a tool to improve ED throughput, because this doctor isn’t tied up with rounds and can immediately start seeing a new admission.
I think an admitter shift does deliver both of these benefits, but its costs make it suboptimal in most settings. For example, a single admitter will impede ED throughput any time more than one new admission is waiting to be seen, and for most groups that will be much of the day. In fact, improved ED throughput is best achieved by having many hospitalists available for admissions, not just a single admitter. (There are many other factors influencing ED throughput, such as whether ED doctors simply send patients to their “floor” bed prior to being seen by a hospitalist. But for this article, I’m just considering the influence of a dedicated admitter.)
I think “silo-ing” work into different roles, such as separating rounding and admitting, makes it more difficult to ensure that each is always working productively. There are likely to be times when the admitter has little or nothing to do, even though the rounders are very busy. Or perhaps the rounders aren’t very busy, but the admitter has just been asked to admit four ED patients at the same time.
While protecting rounders from the stress of admissions is valuable, it comes at the cost of a net increase in hospitalist work, because a new doctor must get to know the patient on the day following admission. And this admitter-to-rounder handoff serves as another opportunity for errors—and probably lowers patient satisfaction.
I think most groups should consider moving the admitter shift into an additional rounder position, dividing admissions across all of the doctors working during the daytime. For example, a group that has six rounders and a separate admitter would change to seven rounders, each available to admit every seventh daytime admission. Each would bear the meaningful stress of having rounds interrupted to admit a new patient, but accepting every seventh daytime admission shouldn’t be too difficult on most days.
Don’t forget that eliminating the admitter means that the list of new patients you take on each morning will be shorter. Mornings may be a little less stressful.
A.M. Distribution
The daytime doctors at many hospitalist groups meet each morning to discuss how the new admissions from the prior night (or even the last 24 hours) will be distributed. Or perhaps one person, sometimes a nurse or clerical staff, arrives very early each day to do this.
Although it might take some careful planning, I think most groups that use this sort of morning distribution should abandon it for a better system. Consider a group in which all six daytime doctors spend an average of 20 minutes distributing patients each morning. Twenty minutes (0.33 hours) times six doctors times 365 days comes to 730 hours annually.
Assuming these doctors are compensated at typical rates, the practice is spending more than $100,000 annually just so the doctors can distribute patients each morning. On top of this, nurses and others at the hospital are usually delayed in learning which daytime hospitalist is caring for each patient. These costs seem unreasonably high.
An alternative is to develop a system by which any admitter, such as a night doctor, who will not be providing subsequent care to a patient can identify by name the doctor who will be providing that care. During the admission encounter, the admitter can tell patient/family, “Dr. Boswell will be taking over your care starting tomorrow. He’s a great guy and has been named one of Portland’s best doctors.” This seems so much better than saying, “One of my partners will be taking over tomorrow. I don’t know which of my partners it will be, but they’re all good doctors.” And Dr. Boswell’s name can be entered into the attending physician field of the EHR so that all hospital staff will know without delay.
MedAptus has recently launched software they call “Assign” that may be able to replace the morning meeting and automate assigning new admissions to each hospitalist. I haven’t seen it in operation, so I can’t speak for its effectiveness, but it might be worthwhile for some groups.
Practical Considerations
The changes I’ve described above might not be optimal for every group, and they may take meaningful work to implement. But I don’t think the difficulty of these things is the biggest barrier. The biggest barrier is probably just inertia in most cases, the same reason I’m still a Netflix streaming subscriber even though I almost never watch it. I did, however, really enjoy the Nexflix original series Lilyhammer.

You shouldn’t maintain things that do not deliver the value you anticipated when you first put them in place. For example, I thought Netflix streaming would be terrific, but I have used it so infrequently that it probably costs me $50 per movie or show watched. I should probably dump it.
Your hospitalist group might have some operational practices that are not as valuable as they seem and could be replaced with something better. For many groups, this might include doing away with a separate daytime admitter shift and a morning meeting to distribute the overnight admissions.
Daytime Admission Shift
My experience is that hospitalist groups with more than about five daytime doctors almost always have a day-shift person dedicated to seeing new admissions. In most cases, this procedure is implemented with the idea of reducing the stress of other day-shift doctors, who don’t have to interrupt rounds to admit a new patient. Some see a dedicated admitter as a tool to improve ED throughput, because this doctor isn’t tied up with rounds and can immediately start seeing a new admission.
I think an admitter shift does deliver both of these benefits, but its costs make it suboptimal in most settings. For example, a single admitter will impede ED throughput any time more than one new admission is waiting to be seen, and for most groups that will be much of the day. In fact, improved ED throughput is best achieved by having many hospitalists available for admissions, not just a single admitter. (There are many other factors influencing ED throughput, such as whether ED doctors simply send patients to their “floor” bed prior to being seen by a hospitalist. But for this article, I’m just considering the influence of a dedicated admitter.)
I think “silo-ing” work into different roles, such as separating rounding and admitting, makes it more difficult to ensure that each is always working productively. There are likely to be times when the admitter has little or nothing to do, even though the rounders are very busy. Or perhaps the rounders aren’t very busy, but the admitter has just been asked to admit four ED patients at the same time.
While protecting rounders from the stress of admissions is valuable, it comes at the cost of a net increase in hospitalist work, because a new doctor must get to know the patient on the day following admission. And this admitter-to-rounder handoff serves as another opportunity for errors—and probably lowers patient satisfaction.
I think most groups should consider moving the admitter shift into an additional rounder position, dividing admissions across all of the doctors working during the daytime. For example, a group that has six rounders and a separate admitter would change to seven rounders, each available to admit every seventh daytime admission. Each would bear the meaningful stress of having rounds interrupted to admit a new patient, but accepting every seventh daytime admission shouldn’t be too difficult on most days.
Don’t forget that eliminating the admitter means that the list of new patients you take on each morning will be shorter. Mornings may be a little less stressful.
A.M. Distribution
The daytime doctors at many hospitalist groups meet each morning to discuss how the new admissions from the prior night (or even the last 24 hours) will be distributed. Or perhaps one person, sometimes a nurse or clerical staff, arrives very early each day to do this.
Although it might take some careful planning, I think most groups that use this sort of morning distribution should abandon it for a better system. Consider a group in which all six daytime doctors spend an average of 20 minutes distributing patients each morning. Twenty minutes (0.33 hours) times six doctors times 365 days comes to 730 hours annually.
Assuming these doctors are compensated at typical rates, the practice is spending more than $100,000 annually just so the doctors can distribute patients each morning. On top of this, nurses and others at the hospital are usually delayed in learning which daytime hospitalist is caring for each patient. These costs seem unreasonably high.
An alternative is to develop a system by which any admitter, such as a night doctor, who will not be providing subsequent care to a patient can identify by name the doctor who will be providing that care. During the admission encounter, the admitter can tell patient/family, “Dr. Boswell will be taking over your care starting tomorrow. He’s a great guy and has been named one of Portland’s best doctors.” This seems so much better than saying, “One of my partners will be taking over tomorrow. I don’t know which of my partners it will be, but they’re all good doctors.” And Dr. Boswell’s name can be entered into the attending physician field of the EHR so that all hospital staff will know without delay.
MedAptus has recently launched software they call “Assign” that may be able to replace the morning meeting and automate assigning new admissions to each hospitalist. I haven’t seen it in operation, so I can’t speak for its effectiveness, but it might be worthwhile for some groups.
Practical Considerations
The changes I’ve described above might not be optimal for every group, and they may take meaningful work to implement. But I don’t think the difficulty of these things is the biggest barrier. The biggest barrier is probably just inertia in most cases, the same reason I’m still a Netflix streaming subscriber even though I almost never watch it. I did, however, really enjoy the Nexflix original series Lilyhammer.

You shouldn’t maintain things that do not deliver the value you anticipated when you first put them in place. For example, I thought Netflix streaming would be terrific, but I have used it so infrequently that it probably costs me $50 per movie or show watched. I should probably dump it.
Your hospitalist group might have some operational practices that are not as valuable as they seem and could be replaced with something better. For many groups, this might include doing away with a separate daytime admitter shift and a morning meeting to distribute the overnight admissions.
Daytime Admission Shift
My experience is that hospitalist groups with more than about five daytime doctors almost always have a day-shift person dedicated to seeing new admissions. In most cases, this procedure is implemented with the idea of reducing the stress of other day-shift doctors, who don’t have to interrupt rounds to admit a new patient. Some see a dedicated admitter as a tool to improve ED throughput, because this doctor isn’t tied up with rounds and can immediately start seeing a new admission.
I think an admitter shift does deliver both of these benefits, but its costs make it suboptimal in most settings. For example, a single admitter will impede ED throughput any time more than one new admission is waiting to be seen, and for most groups that will be much of the day. In fact, improved ED throughput is best achieved by having many hospitalists available for admissions, not just a single admitter. (There are many other factors influencing ED throughput, such as whether ED doctors simply send patients to their “floor” bed prior to being seen by a hospitalist. But for this article, I’m just considering the influence of a dedicated admitter.)
I think “silo-ing” work into different roles, such as separating rounding and admitting, makes it more difficult to ensure that each is always working productively. There are likely to be times when the admitter has little or nothing to do, even though the rounders are very busy. Or perhaps the rounders aren’t very busy, but the admitter has just been asked to admit four ED patients at the same time.
While protecting rounders from the stress of admissions is valuable, it comes at the cost of a net increase in hospitalist work, because a new doctor must get to know the patient on the day following admission. And this admitter-to-rounder handoff serves as another opportunity for errors—and probably lowers patient satisfaction.
I think most groups should consider moving the admitter shift into an additional rounder position, dividing admissions across all of the doctors working during the daytime. For example, a group that has six rounders and a separate admitter would change to seven rounders, each available to admit every seventh daytime admission. Each would bear the meaningful stress of having rounds interrupted to admit a new patient, but accepting every seventh daytime admission shouldn’t be too difficult on most days.
Don’t forget that eliminating the admitter means that the list of new patients you take on each morning will be shorter. Mornings may be a little less stressful.
A.M. Distribution
The daytime doctors at many hospitalist groups meet each morning to discuss how the new admissions from the prior night (or even the last 24 hours) will be distributed. Or perhaps one person, sometimes a nurse or clerical staff, arrives very early each day to do this.
Although it might take some careful planning, I think most groups that use this sort of morning distribution should abandon it for a better system. Consider a group in which all six daytime doctors spend an average of 20 minutes distributing patients each morning. Twenty minutes (0.33 hours) times six doctors times 365 days comes to 730 hours annually.
Assuming these doctors are compensated at typical rates, the practice is spending more than $100,000 annually just so the doctors can distribute patients each morning. On top of this, nurses and others at the hospital are usually delayed in learning which daytime hospitalist is caring for each patient. These costs seem unreasonably high.
An alternative is to develop a system by which any admitter, such as a night doctor, who will not be providing subsequent care to a patient can identify by name the doctor who will be providing that care. During the admission encounter, the admitter can tell patient/family, “Dr. Boswell will be taking over your care starting tomorrow. He’s a great guy and has been named one of Portland’s best doctors.” This seems so much better than saying, “One of my partners will be taking over tomorrow. I don’t know which of my partners it will be, but they’re all good doctors.” And Dr. Boswell’s name can be entered into the attending physician field of the EHR so that all hospital staff will know without delay.
MedAptus has recently launched software they call “Assign” that may be able to replace the morning meeting and automate assigning new admissions to each hospitalist. I haven’t seen it in operation, so I can’t speak for its effectiveness, but it might be worthwhile for some groups.
Practical Considerations
The changes I’ve described above might not be optimal for every group, and they may take meaningful work to implement. But I don’t think the difficulty of these things is the biggest barrier. The biggest barrier is probably just inertia in most cases, the same reason I’m still a Netflix streaming subscriber even though I almost never watch it. I did, however, really enjoy the Nexflix original series Lilyhammer.

Why Hospitalist Morale is Declining and Ways to Improve It
Using quotes to ensure that the results were only those that include the two words adjacent to one another, rather than separated, I entered the following phrases into my Google search engine:
- “hospitalist burnout” = 1,580 results
- “hospitalist morale” = 208 results
- “hospitalist well-being” = 0 results
I think the number of results suggests the level of interest in each topic and, if that is the case, clearly thinking about how hospitalists are doing in their careers is more commonly done through the paradigm of burnout than the other two terms. (Of course, there may be other terms that I didn’t consider.) In fact, there have been a handful of published studies of hospitalist burnout and job satisfaction.1,2
Those studies generally have shown both reasonably high levels of job satisfaction and troubling levels of burnout.
But I’ve been thinking about hospitalist morale for a while. I think morale is reasonably distinct from both burnout and job satisfaction.
Causes of a National Decline in Hospitalist Morale
I think hospitalist morale has declined some over the past two or three years across the country. This observation is meaningful because it comes from my experience working with a lot of hospitalist groups coast to coast. But I’m the first to admit it is just anecdotal and is subject to my own biases.
I can think of several things contributing to a decline in morale.
EHR adoption. Near the top of the list is the adoption of EHRs in many hospitals, which typically leads doctors in other specialties to seek hospitalist assistance with EHR-related tasks (e.g. medicine reconciliation and order writing) even in cases where there is little or no clinical reason for hospitalist involvement. Lots of hospitalists complain about this. To be clear, in many hospitals the hospitalists are reasonably content with using the EHR, but they experience ongoing frustration and low morale resulting from nonclinical work other doctors pressure them to take over.
Observation status. Many hospitals began classifying a larger portion of patients as observation status over the last few years; at the same time, patients and families have become more aware of how much of a disadvantage this is. In many cases, it is the hospitalist who takes the brunt of patient and family frustration. This can get awfully stressful and frustrating, and I think it is a contributor to allegations of malpractice.
Budgetary stress. Ever since SHM began collecting survey data in the late 1990s, the financial support hospitals have been providing to hospitalists has increased dramatically. The most recent State of Hospital Medicine report, published in 2104, showed median support provided by hospitals of $156,063 per FTE hospitalist, per year. Some hospitals have begun to resist providing more support, and this translates into stress and lower morale for hospitalists. This is far from a universal issue, but it does lead to lower morale for hospitalists who face it.
Many other factors may be contributing to a national decline in morale, but I think these are some of the most important.
What Can Be Done?
Some hospitalist groups have great morale now and don’t need to do much of anything right now, but some groups should think about a deliberate strategy to improve it.
Sadly, there isn’t a prescription that is sure to work. But there are some things you can try.
Self-care. The field of palliative care has thought a lot about caring for caregivers, and hospitalist groups might want to adopt some of their practices. Search the Internet on “self-care” + “palliative care,” and you’ll find a lot of interesting things. The group I’m part of launched a deliberate program of professionally led and facilitated hospitalist self-care, with high hopes that included mindful meditation, among other things. As soon as we had designed our program, the Mayo Clinic published their favorable experience with a program that was very similar to what we had planned, and I thought we would see similar benefits.3
But, while all who attended the sessions thought they were valuable, attendance was so poor that we ended up cancelling the program. The hospitalists were interested in attending but were either on service and busy seeing patients, or were off and didn’t want to drive in to work solely for the purpose of reducing work stress.
I’m convinced a self-care program is valuable but very tricky to schedule effectively. Maybe others have come up with effective ways of overcoming this problem.
Social connections. Some hospitalist groups seem to have little social and personal connection to other physicians and hospital leaders. I think this results in lower hospitalist morale and tends to be self-reinforcing. If you’re in such a group, you and your hospitalist colleagues should deliberately seek better relationships with other doctors and hospital administrative leaders. Ensure that you visit with others at lunch, talk with them at committee meetings, ask about their vacation and personal activities, and pursue activities with them outside of work.
When these sorts of social connections are strong, work is far more satisfying and you’re much more likely to be treated as a peer by other doctors. I think this is really important and shouldn’t be overlooked if your group is suffering from low morale.
Adaptive work. Lastly, you might want to approach changes to your work and morale as “adaptive work,” rather than “technical work.” Space doesn’t permit a description of these, but it is worth reading about how they differ. Many groups will find value in reframing their approach to aspects of work they don’t like as adaptive work.

References
- Hinami K, Whelan CT, Wolosin RJ, Miller JA, Wetterneck TB. Worklife and satisfaction of hospitalists: toward flourishing careers. J Gen Intern Med. 2012;27(1):28-36.
- Hoff TH, Whitcomb WF, Williams K, Nelson JR, Cheesman RA. Characteristics and work experiences of hospitalists in the United States. Arch Intern Med. 2001;161(6):851-858.
- West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527-533.
Using quotes to ensure that the results were only those that include the two words adjacent to one another, rather than separated, I entered the following phrases into my Google search engine:
- “hospitalist burnout” = 1,580 results
- “hospitalist morale” = 208 results
- “hospitalist well-being” = 0 results
I think the number of results suggests the level of interest in each topic and, if that is the case, clearly thinking about how hospitalists are doing in their careers is more commonly done through the paradigm of burnout than the other two terms. (Of course, there may be other terms that I didn’t consider.) In fact, there have been a handful of published studies of hospitalist burnout and job satisfaction.1,2
Those studies generally have shown both reasonably high levels of job satisfaction and troubling levels of burnout.
But I’ve been thinking about hospitalist morale for a while. I think morale is reasonably distinct from both burnout and job satisfaction.
Causes of a National Decline in Hospitalist Morale
I think hospitalist morale has declined some over the past two or three years across the country. This observation is meaningful because it comes from my experience working with a lot of hospitalist groups coast to coast. But I’m the first to admit it is just anecdotal and is subject to my own biases.
I can think of several things contributing to a decline in morale.
EHR adoption. Near the top of the list is the adoption of EHRs in many hospitals, which typically leads doctors in other specialties to seek hospitalist assistance with EHR-related tasks (e.g. medicine reconciliation and order writing) even in cases where there is little or no clinical reason for hospitalist involvement. Lots of hospitalists complain about this. To be clear, in many hospitals the hospitalists are reasonably content with using the EHR, but they experience ongoing frustration and low morale resulting from nonclinical work other doctors pressure them to take over.
Observation status. Many hospitals began classifying a larger portion of patients as observation status over the last few years; at the same time, patients and families have become more aware of how much of a disadvantage this is. In many cases, it is the hospitalist who takes the brunt of patient and family frustration. This can get awfully stressful and frustrating, and I think it is a contributor to allegations of malpractice.
Budgetary stress. Ever since SHM began collecting survey data in the late 1990s, the financial support hospitals have been providing to hospitalists has increased dramatically. The most recent State of Hospital Medicine report, published in 2104, showed median support provided by hospitals of $156,063 per FTE hospitalist, per year. Some hospitals have begun to resist providing more support, and this translates into stress and lower morale for hospitalists. This is far from a universal issue, but it does lead to lower morale for hospitalists who face it.
Many other factors may be contributing to a national decline in morale, but I think these are some of the most important.
What Can Be Done?
Some hospitalist groups have great morale now and don’t need to do much of anything right now, but some groups should think about a deliberate strategy to improve it.
Sadly, there isn’t a prescription that is sure to work. But there are some things you can try.
Self-care. The field of palliative care has thought a lot about caring for caregivers, and hospitalist groups might want to adopt some of their practices. Search the Internet on “self-care” + “palliative care,” and you’ll find a lot of interesting things. The group I’m part of launched a deliberate program of professionally led and facilitated hospitalist self-care, with high hopes that included mindful meditation, among other things. As soon as we had designed our program, the Mayo Clinic published their favorable experience with a program that was very similar to what we had planned, and I thought we would see similar benefits.3
But, while all who attended the sessions thought they were valuable, attendance was so poor that we ended up cancelling the program. The hospitalists were interested in attending but were either on service and busy seeing patients, or were off and didn’t want to drive in to work solely for the purpose of reducing work stress.
I’m convinced a self-care program is valuable but very tricky to schedule effectively. Maybe others have come up with effective ways of overcoming this problem.
Social connections. Some hospitalist groups seem to have little social and personal connection to other physicians and hospital leaders. I think this results in lower hospitalist morale and tends to be self-reinforcing. If you’re in such a group, you and your hospitalist colleagues should deliberately seek better relationships with other doctors and hospital administrative leaders. Ensure that you visit with others at lunch, talk with them at committee meetings, ask about their vacation and personal activities, and pursue activities with them outside of work.
When these sorts of social connections are strong, work is far more satisfying and you’re much more likely to be treated as a peer by other doctors. I think this is really important and shouldn’t be overlooked if your group is suffering from low morale.
Adaptive work. Lastly, you might want to approach changes to your work and morale as “adaptive work,” rather than “technical work.” Space doesn’t permit a description of these, but it is worth reading about how they differ. Many groups will find value in reframing their approach to aspects of work they don’t like as adaptive work.

References
- Hinami K, Whelan CT, Wolosin RJ, Miller JA, Wetterneck TB. Worklife and satisfaction of hospitalists: toward flourishing careers. J Gen Intern Med. 2012;27(1):28-36.
- Hoff TH, Whitcomb WF, Williams K, Nelson JR, Cheesman RA. Characteristics and work experiences of hospitalists in the United States. Arch Intern Med. 2001;161(6):851-858.
- West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527-533.
Using quotes to ensure that the results were only those that include the two words adjacent to one another, rather than separated, I entered the following phrases into my Google search engine:
- “hospitalist burnout” = 1,580 results
- “hospitalist morale” = 208 results
- “hospitalist well-being” = 0 results
I think the number of results suggests the level of interest in each topic and, if that is the case, clearly thinking about how hospitalists are doing in their careers is more commonly done through the paradigm of burnout than the other two terms. (Of course, there may be other terms that I didn’t consider.) In fact, there have been a handful of published studies of hospitalist burnout and job satisfaction.1,2
Those studies generally have shown both reasonably high levels of job satisfaction and troubling levels of burnout.
But I’ve been thinking about hospitalist morale for a while. I think morale is reasonably distinct from both burnout and job satisfaction.
Causes of a National Decline in Hospitalist Morale
I think hospitalist morale has declined some over the past two or three years across the country. This observation is meaningful because it comes from my experience working with a lot of hospitalist groups coast to coast. But I’m the first to admit it is just anecdotal and is subject to my own biases.
I can think of several things contributing to a decline in morale.
EHR adoption. Near the top of the list is the adoption of EHRs in many hospitals, which typically leads doctors in other specialties to seek hospitalist assistance with EHR-related tasks (e.g. medicine reconciliation and order writing) even in cases where there is little or no clinical reason for hospitalist involvement. Lots of hospitalists complain about this. To be clear, in many hospitals the hospitalists are reasonably content with using the EHR, but they experience ongoing frustration and low morale resulting from nonclinical work other doctors pressure them to take over.
Observation status. Many hospitals began classifying a larger portion of patients as observation status over the last few years; at the same time, patients and families have become more aware of how much of a disadvantage this is. In many cases, it is the hospitalist who takes the brunt of patient and family frustration. This can get awfully stressful and frustrating, and I think it is a contributor to allegations of malpractice.
Budgetary stress. Ever since SHM began collecting survey data in the late 1990s, the financial support hospitals have been providing to hospitalists has increased dramatically. The most recent State of Hospital Medicine report, published in 2104, showed median support provided by hospitals of $156,063 per FTE hospitalist, per year. Some hospitals have begun to resist providing more support, and this translates into stress and lower morale for hospitalists. This is far from a universal issue, but it does lead to lower morale for hospitalists who face it.
Many other factors may be contributing to a national decline in morale, but I think these are some of the most important.
What Can Be Done?
Some hospitalist groups have great morale now and don’t need to do much of anything right now, but some groups should think about a deliberate strategy to improve it.
Sadly, there isn’t a prescription that is sure to work. But there are some things you can try.
Self-care. The field of palliative care has thought a lot about caring for caregivers, and hospitalist groups might want to adopt some of their practices. Search the Internet on “self-care” + “palliative care,” and you’ll find a lot of interesting things. The group I’m part of launched a deliberate program of professionally led and facilitated hospitalist self-care, with high hopes that included mindful meditation, among other things. As soon as we had designed our program, the Mayo Clinic published their favorable experience with a program that was very similar to what we had planned, and I thought we would see similar benefits.3
But, while all who attended the sessions thought they were valuable, attendance was so poor that we ended up cancelling the program. The hospitalists were interested in attending but were either on service and busy seeing patients, or were off and didn’t want to drive in to work solely for the purpose of reducing work stress.
I’m convinced a self-care program is valuable but very tricky to schedule effectively. Maybe others have come up with effective ways of overcoming this problem.
Social connections. Some hospitalist groups seem to have little social and personal connection to other physicians and hospital leaders. I think this results in lower hospitalist morale and tends to be self-reinforcing. If you’re in such a group, you and your hospitalist colleagues should deliberately seek better relationships with other doctors and hospital administrative leaders. Ensure that you visit with others at lunch, talk with them at committee meetings, ask about their vacation and personal activities, and pursue activities with them outside of work.
When these sorts of social connections are strong, work is far more satisfying and you’re much more likely to be treated as a peer by other doctors. I think this is really important and shouldn’t be overlooked if your group is suffering from low morale.
Adaptive work. Lastly, you might want to approach changes to your work and morale as “adaptive work,” rather than “technical work.” Space doesn’t permit a description of these, but it is worth reading about how they differ. Many groups will find value in reframing their approach to aspects of work they don’t like as adaptive work.

References
- Hinami K, Whelan CT, Wolosin RJ, Miller JA, Wetterneck TB. Worklife and satisfaction of hospitalists: toward flourishing careers. J Gen Intern Med. 2012;27(1):28-36.
- Hoff TH, Whitcomb WF, Williams K, Nelson JR, Cheesman RA. Characteristics and work experiences of hospitalists in the United States. Arch Intern Med. 2001;161(6):851-858.
- West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527-533.
Tips for Hospitalists on Spending More of Their Time at the Top of Their License
Hospitalists spend too little time working at the top of their license. Put differently, I think a hospitalist often spends only about 1.5 to two hours in a 10- or 12-hour workday making use of the knowledge base and skills developed in training. (I wrote about this and referenced some hospitalist time-motion studies in my December 2010 column.)
The remaining hours are typically spent in activities such as figuring out which surgeon is on call and tracking her down, managing patient lists, filling out paper or electronic forms, explaining observation status to patients, and so on.
When I first became a hospitalist in the 1980s, there was already a lot of talk about the paperwork burden faced by doctors across all specialties. I recall the gnashing of teeth that ensued—lots of articles and seminars, and it seems to me even a few legislative proposals, focused on the topic. It appears that nearly every recruitment ad at the time mentioned something like “Let us take care of running the business, so you can focus solely on patient care.” Clearly, doctors were seeking relief from the burden of nonclinical work even back then.
I can’t recall reading or hearing anyone talk about the “paperwork” burden of physician practice in the past few years. This isn’t because things have gotten better; in fact, I think the burden of “non-doctoring activities” has steadily increased. We hear less about the problem of excessive paperwork simply because, more recently, it has been framed differently—it is now typically referred to as the problem of too little time spent practicing at the top of license.
Search the Internet for “top of license” and a number of interesting things turn up. Most are healthcare related—maybe other professions don’t use the term—and there are just as many links referring to nurses as physicians. Much is written about the need for primary care physicians to spend more time working at the top of their license, but I couldn’t find anything addressing this issue specifically for hospitalists.
What Can Be Done?
Moving your work as a hospitalist more to the top of your license isn’t a simple thing, and our whole field will need to work on this over time. The most effective interventions will vary some from place to place, but here are some ideas that may be relevant for many hospitalist groups.
Medication reconciliation. I fully support the idea of careful medication reconciliation, but, given that such a large portion of hospitalist patients are on so many medications, this is a time-consuming task. And, in many or most hospitals, the task suffers from diffusion of responsibility; for example, the ED nurse makes only a half-hearted attempt to get an accurate list, and the hospitalist believes that whatever the ED nurse entered into the record regarding patient medications is probably the best obtainable list.
A pharmacy technician stationed in the ED and charged with recording the best obtainable list of medicines on patient arrival can address both of these problems (for more information, the American Society of Health-System Pharmacists offers webinars and other resources on this topic). This would include calling family members, pharmacies, and physician offices for clarification in some cases. Hospitalists working in such an environment nearly always say it is extremely valuable in reducing inaccuracies in the pre-hospital medication list, as well as saving hospitalists time when they are admitting patients.
Unfortunately, hospitals may resist adding pharmacy technicians because of the expense or, in some cases, because of concerns that such work may exceed the legal scope of work for technicians.
Post-hospital appointments. I think arranging post-hospital appointments should be no more difficult for the hospitalist than ordering a complete blood count (CBC). It shouldn’t matter whether I want the patient to follow up with the PCP he has been seeing for years, or see a neurologist or diabetes educator as a new patient consult. Any treating doctor in the hospital should be able to arrange such post-hospital visits with just a click or two in the EHR, or a stroke of the pen. And the patient should leave the hospital with a written date and time of the appointment that has been made for them.
Few hospitals can reliably provide this, however, so, all too often, hospitalists spend their time calling clerical staff at outpatient clinics to arrange appointments, writing them down, and delivering them to patients. This is far from what anyone would consider top of license work. (I wrote a little more about this in last month’s column.)
Medicare benefits specialist. Many hospitalists end up spending significant time explaining to patients and families the reason a patient is on observation status and trying to defuse the resulting frustration and anger. As I stated in my November 2014 column, I think observation status is so frustrating to patients that it is often the root cause of complaints about care and, potentially, the source of malpractice suits.
Physicians have an unavoidable role in determining observation versus inpatient status, but I think hospitals should work hard to ensure that someone other than the doctor is available to explain to patients and families the reason for observation status, along with its implications, and to provide sympathy for their frustrations. This allows the doctor to stay focused on clinical care.
Limit reliance on a “triage hospitalist.” Hospitalist groups larger than about 20 providers often have one provider devoted through much of a daytime shift to triaging and assigning new referrals across all providers working that day. For larger practices, this triage work may consume all of the provider’s shift, so that person has no time left for clinical care. It is hard for me to see this as top of license work that only a physician or advanced practice clinician can do. In my December 2010 column, I provided some potential alternatives to dedicating a physician or other provider to a triage role.
Your list of important changes that are needed to move hospitalists toward more time spent working at the top of their license will likely differ a lot from the issues above. But every group could benefit from deliberately thinking about what would be most valuable for them and trying to make that a reality.

Hospitalists spend too little time working at the top of their license. Put differently, I think a hospitalist often spends only about 1.5 to two hours in a 10- or 12-hour workday making use of the knowledge base and skills developed in training. (I wrote about this and referenced some hospitalist time-motion studies in my December 2010 column.)
The remaining hours are typically spent in activities such as figuring out which surgeon is on call and tracking her down, managing patient lists, filling out paper or electronic forms, explaining observation status to patients, and so on.
When I first became a hospitalist in the 1980s, there was already a lot of talk about the paperwork burden faced by doctors across all specialties. I recall the gnashing of teeth that ensued—lots of articles and seminars, and it seems to me even a few legislative proposals, focused on the topic. It appears that nearly every recruitment ad at the time mentioned something like “Let us take care of running the business, so you can focus solely on patient care.” Clearly, doctors were seeking relief from the burden of nonclinical work even back then.
I can’t recall reading or hearing anyone talk about the “paperwork” burden of physician practice in the past few years. This isn’t because things have gotten better; in fact, I think the burden of “non-doctoring activities” has steadily increased. We hear less about the problem of excessive paperwork simply because, more recently, it has been framed differently—it is now typically referred to as the problem of too little time spent practicing at the top of license.
Search the Internet for “top of license” and a number of interesting things turn up. Most are healthcare related—maybe other professions don’t use the term—and there are just as many links referring to nurses as physicians. Much is written about the need for primary care physicians to spend more time working at the top of their license, but I couldn’t find anything addressing this issue specifically for hospitalists.
What Can Be Done?
Moving your work as a hospitalist more to the top of your license isn’t a simple thing, and our whole field will need to work on this over time. The most effective interventions will vary some from place to place, but here are some ideas that may be relevant for many hospitalist groups.
Medication reconciliation. I fully support the idea of careful medication reconciliation, but, given that such a large portion of hospitalist patients are on so many medications, this is a time-consuming task. And, in many or most hospitals, the task suffers from diffusion of responsibility; for example, the ED nurse makes only a half-hearted attempt to get an accurate list, and the hospitalist believes that whatever the ED nurse entered into the record regarding patient medications is probably the best obtainable list.
A pharmacy technician stationed in the ED and charged with recording the best obtainable list of medicines on patient arrival can address both of these problems (for more information, the American Society of Health-System Pharmacists offers webinars and other resources on this topic). This would include calling family members, pharmacies, and physician offices for clarification in some cases. Hospitalists working in such an environment nearly always say it is extremely valuable in reducing inaccuracies in the pre-hospital medication list, as well as saving hospitalists time when they are admitting patients.
Unfortunately, hospitals may resist adding pharmacy technicians because of the expense or, in some cases, because of concerns that such work may exceed the legal scope of work for technicians.
Post-hospital appointments. I think arranging post-hospital appointments should be no more difficult for the hospitalist than ordering a complete blood count (CBC). It shouldn’t matter whether I want the patient to follow up with the PCP he has been seeing for years, or see a neurologist or diabetes educator as a new patient consult. Any treating doctor in the hospital should be able to arrange such post-hospital visits with just a click or two in the EHR, or a stroke of the pen. And the patient should leave the hospital with a written date and time of the appointment that has been made for them.
Few hospitals can reliably provide this, however, so, all too often, hospitalists spend their time calling clerical staff at outpatient clinics to arrange appointments, writing them down, and delivering them to patients. This is far from what anyone would consider top of license work. (I wrote a little more about this in last month’s column.)
Medicare benefits specialist. Many hospitalists end up spending significant time explaining to patients and families the reason a patient is on observation status and trying to defuse the resulting frustration and anger. As I stated in my November 2014 column, I think observation status is so frustrating to patients that it is often the root cause of complaints about care and, potentially, the source of malpractice suits.
Physicians have an unavoidable role in determining observation versus inpatient status, but I think hospitals should work hard to ensure that someone other than the doctor is available to explain to patients and families the reason for observation status, along with its implications, and to provide sympathy for their frustrations. This allows the doctor to stay focused on clinical care.
Limit reliance on a “triage hospitalist.” Hospitalist groups larger than about 20 providers often have one provider devoted through much of a daytime shift to triaging and assigning new referrals across all providers working that day. For larger practices, this triage work may consume all of the provider’s shift, so that person has no time left for clinical care. It is hard for me to see this as top of license work that only a physician or advanced practice clinician can do. In my December 2010 column, I provided some potential alternatives to dedicating a physician or other provider to a triage role.
Your list of important changes that are needed to move hospitalists toward more time spent working at the top of their license will likely differ a lot from the issues above. But every group could benefit from deliberately thinking about what would be most valuable for them and trying to make that a reality.

Hospitalists spend too little time working at the top of their license. Put differently, I think a hospitalist often spends only about 1.5 to two hours in a 10- or 12-hour workday making use of the knowledge base and skills developed in training. (I wrote about this and referenced some hospitalist time-motion studies in my December 2010 column.)
The remaining hours are typically spent in activities such as figuring out which surgeon is on call and tracking her down, managing patient lists, filling out paper or electronic forms, explaining observation status to patients, and so on.
When I first became a hospitalist in the 1980s, there was already a lot of talk about the paperwork burden faced by doctors across all specialties. I recall the gnashing of teeth that ensued—lots of articles and seminars, and it seems to me even a few legislative proposals, focused on the topic. It appears that nearly every recruitment ad at the time mentioned something like “Let us take care of running the business, so you can focus solely on patient care.” Clearly, doctors were seeking relief from the burden of nonclinical work even back then.
I can’t recall reading or hearing anyone talk about the “paperwork” burden of physician practice in the past few years. This isn’t because things have gotten better; in fact, I think the burden of “non-doctoring activities” has steadily increased. We hear less about the problem of excessive paperwork simply because, more recently, it has been framed differently—it is now typically referred to as the problem of too little time spent practicing at the top of license.
Search the Internet for “top of license” and a number of interesting things turn up. Most are healthcare related—maybe other professions don’t use the term—and there are just as many links referring to nurses as physicians. Much is written about the need for primary care physicians to spend more time working at the top of their license, but I couldn’t find anything addressing this issue specifically for hospitalists.
What Can Be Done?
Moving your work as a hospitalist more to the top of your license isn’t a simple thing, and our whole field will need to work on this over time. The most effective interventions will vary some from place to place, but here are some ideas that may be relevant for many hospitalist groups.
Medication reconciliation. I fully support the idea of careful medication reconciliation, but, given that such a large portion of hospitalist patients are on so many medications, this is a time-consuming task. And, in many or most hospitals, the task suffers from diffusion of responsibility; for example, the ED nurse makes only a half-hearted attempt to get an accurate list, and the hospitalist believes that whatever the ED nurse entered into the record regarding patient medications is probably the best obtainable list.
A pharmacy technician stationed in the ED and charged with recording the best obtainable list of medicines on patient arrival can address both of these problems (for more information, the American Society of Health-System Pharmacists offers webinars and other resources on this topic). This would include calling family members, pharmacies, and physician offices for clarification in some cases. Hospitalists working in such an environment nearly always say it is extremely valuable in reducing inaccuracies in the pre-hospital medication list, as well as saving hospitalists time when they are admitting patients.
Unfortunately, hospitals may resist adding pharmacy technicians because of the expense or, in some cases, because of concerns that such work may exceed the legal scope of work for technicians.
Post-hospital appointments. I think arranging post-hospital appointments should be no more difficult for the hospitalist than ordering a complete blood count (CBC). It shouldn’t matter whether I want the patient to follow up with the PCP he has been seeing for years, or see a neurologist or diabetes educator as a new patient consult. Any treating doctor in the hospital should be able to arrange such post-hospital visits with just a click or two in the EHR, or a stroke of the pen. And the patient should leave the hospital with a written date and time of the appointment that has been made for them.
Few hospitals can reliably provide this, however, so, all too often, hospitalists spend their time calling clerical staff at outpatient clinics to arrange appointments, writing them down, and delivering them to patients. This is far from what anyone would consider top of license work. (I wrote a little more about this in last month’s column.)
Medicare benefits specialist. Many hospitalists end up spending significant time explaining to patients and families the reason a patient is on observation status and trying to defuse the resulting frustration and anger. As I stated in my November 2014 column, I think observation status is so frustrating to patients that it is often the root cause of complaints about care and, potentially, the source of malpractice suits.
Physicians have an unavoidable role in determining observation versus inpatient status, but I think hospitals should work hard to ensure that someone other than the doctor is available to explain to patients and families the reason for observation status, along with its implications, and to provide sympathy for their frustrations. This allows the doctor to stay focused on clinical care.
Limit reliance on a “triage hospitalist.” Hospitalist groups larger than about 20 providers often have one provider devoted through much of a daytime shift to triaging and assigning new referrals across all providers working that day. For larger practices, this triage work may consume all of the provider’s shift, so that person has no time left for clinical care. It is hard for me to see this as top of license work that only a physician or advanced practice clinician can do. In my December 2010 column, I provided some potential alternatives to dedicating a physician or other provider to a triage role.
Your list of important changes that are needed to move hospitalists toward more time spent working at the top of their license will likely differ a lot from the issues above. But every group could benefit from deliberately thinking about what would be most valuable for them and trying to make that a reality.

Hospital Medicine's Old Practices Become New Again
The musty collections of National Geographic magazines once found in so many basements are largely gone. Replacing them are dusty sets of the Advisory Board binders and booklets found in hospital administration offices around the country. I think the same principle drives the impulse to collect both publications—the idea that they contain worthwhile information that one day will be reviewed. But I think it’s more likely they will be ignored until it is time to move and someone has to decide what to do with the painfully heavy pile of paper.
Lots of old and largely forgotten things are making a comeback in healthcare. I suppose this is always happening, but I sense we’re now experiencing more of this than usual. It’s a renaissance of sorts.
I first heard about fecal transplant for Clostridium difficile infection (instilling a “better” microbiome in the hope of realizing many benefits) about six or eight years ago. Although I was sure this was a new idea, my retired internist father told me this had been around when he was in training. Wikipedia says that four Colorado surgeons published a paper about it in 1958 and that the Chinese were doing this 1,600 years ago.
PCPs Visit Hospitalized Patients
Writing in the NEJM earlier this year, Goroll and Hunt proposed that primary care physicians visit their hospitalized patients in the role of consultant while the hospitalist remains attending. As they note, this idea surfaced as soon as the hospitalist model began taking hold. Back then, we usually referred to it as a “social visit” by the PCP. Anecdotal experience from my work with hundreds of hospitalist groups tells me that such visits have all but disappeared. But nearly every such PCP visit on a patient I’ve cared for has seemed worthwhile; in many cases, these hospital calls simply reassure a nervous patient or family member, and occasionally they ensure that the PCP and I arrive at a more effective plan of care than we might otherwise.
Perhaps new forms of healthcare reimbursement, accountable care, and population health may make “continuity visits” economically viable for PCPs. Wouldn’t it be interesting if PCP visits to hospitalized patients and hospitalist visits to outpatients, such as those occurring in a pre-op clinic or a skilled nursing facility, become commonplace? The trick in all of this will be to ensure the right amount of overlap, or shared visits, between PCP and hospitalist without expensive duplication of effort or errors stemming from too many cooks in the kitchen.
Post-Hospital Follow-Up Schedules
When I began practicing as a hospitalist in the 1980s, doctors routinely wrote orders similar to this one: “Have patient follow up with Dr. Smith (PCP or specialist) in 1-2 weeks.” The unit secretary or other hospital clerical staff would contact the physician’s office to schedule the appointment, and the patient would leave the hospital with a written reminder in hand. My sense is that nearly all hospitals had been doing this for decades; somehow this practice has nearly disappeared over the last 10-20 years, however, and I sometimes hear this old practice discussed as a new idea.
I think making sure the patient has a follow-up appointment in hand when leaving the hospital is likely good for clinical outcomes, readmissions, and patient satisfaction. In my view, it is hardly worth lots of research to prove the benefit of what should be a relatively low-cost intervention. Why not just have providers write orders detailing follow-up with a specific doctor or clinic and a timeframe, and have unit secretaries communicate with outpatient clinics to schedule the appointments and ensure that the details are provided to the patient, maybe via an EHR-generated after visit summary? Seems pretty easy, right?
Turns out it isn’t easy at all for most hospitals. Lots of energetic hospitalists have taken on a project like this, only to run into so many brick walls. One hospitalist told me recently that the unit secretary’s labor union at her hospital refused to allow it. So some hospitals have turned to a single person, or a small group of people, who make appointments for all hospital patients. Some hospitalist groups have one of their own staff make appointments for hospitalist patients. This relieves the unit secretaries of the task but requires additional funding for the salaries of these people.
Maybe, at some time not so far off, EHRs will be so user-friendly and patients/families so accustomed to using them that it will be common for patients/families to arrange the appointments on their own. It could even be a required step—a hard stop—in the discharge process.
Whatever emerges as the most common method of making these appointments, I think it is safe to say this old practice will become “new” and common within the next few years.
Multidisciplinary Rounds
While working as an orderly in the 1970s, I would often visit with the nurses in their break room. When a doctor arrived to make rounds on the floor, the RN would jump up, stub out her cigarette, and round with the doctor. I sometimes tagged along as an observer. The nurse let the doctor know just how the patient had been doing and provided test results and any other relevant information the doctor might need. The doctor would provide orders, and sometimes the nurse wrote them into the chart (think of today’s medical scribes). Although their interaction was much less collaborative than is typical today, they did ask lots of questions of one another to clarify ambiguities.
I think these 1970s caregivers were doing effective multidisciplinary rounds. But by the late 1980s or so, as both doctor and nurse became busier, they stopped rounding together.
I smile when I hear descriptions of this “new” idea of doctor and nurse (and often other caregivers) rounding together. Today’s hospital culture is less hierarchical than the 1970s, though some would say it still has a ways to go, so teamwork and multidisciplinary rounds may yield more benefit than decades ago. But the idea of rounding together certainly isn’t new.
As we try to figure out the best way to thrive in a rapidly changing healthcare environment, we may find value in returning to the old ways of doing some things.

The musty collections of National Geographic magazines once found in so many basements are largely gone. Replacing them are dusty sets of the Advisory Board binders and booklets found in hospital administration offices around the country. I think the same principle drives the impulse to collect both publications—the idea that they contain worthwhile information that one day will be reviewed. But I think it’s more likely they will be ignored until it is time to move and someone has to decide what to do with the painfully heavy pile of paper.
Lots of old and largely forgotten things are making a comeback in healthcare. I suppose this is always happening, but I sense we’re now experiencing more of this than usual. It’s a renaissance of sorts.
I first heard about fecal transplant for Clostridium difficile infection (instilling a “better” microbiome in the hope of realizing many benefits) about six or eight years ago. Although I was sure this was a new idea, my retired internist father told me this had been around when he was in training. Wikipedia says that four Colorado surgeons published a paper about it in 1958 and that the Chinese were doing this 1,600 years ago.
PCPs Visit Hospitalized Patients
Writing in the NEJM earlier this year, Goroll and Hunt proposed that primary care physicians visit their hospitalized patients in the role of consultant while the hospitalist remains attending. As they note, this idea surfaced as soon as the hospitalist model began taking hold. Back then, we usually referred to it as a “social visit” by the PCP. Anecdotal experience from my work with hundreds of hospitalist groups tells me that such visits have all but disappeared. But nearly every such PCP visit on a patient I’ve cared for has seemed worthwhile; in many cases, these hospital calls simply reassure a nervous patient or family member, and occasionally they ensure that the PCP and I arrive at a more effective plan of care than we might otherwise.
Perhaps new forms of healthcare reimbursement, accountable care, and population health may make “continuity visits” economically viable for PCPs. Wouldn’t it be interesting if PCP visits to hospitalized patients and hospitalist visits to outpatients, such as those occurring in a pre-op clinic or a skilled nursing facility, become commonplace? The trick in all of this will be to ensure the right amount of overlap, or shared visits, between PCP and hospitalist without expensive duplication of effort or errors stemming from too many cooks in the kitchen.
Post-Hospital Follow-Up Schedules
When I began practicing as a hospitalist in the 1980s, doctors routinely wrote orders similar to this one: “Have patient follow up with Dr. Smith (PCP or specialist) in 1-2 weeks.” The unit secretary or other hospital clerical staff would contact the physician’s office to schedule the appointment, and the patient would leave the hospital with a written reminder in hand. My sense is that nearly all hospitals had been doing this for decades; somehow this practice has nearly disappeared over the last 10-20 years, however, and I sometimes hear this old practice discussed as a new idea.
I think making sure the patient has a follow-up appointment in hand when leaving the hospital is likely good for clinical outcomes, readmissions, and patient satisfaction. In my view, it is hardly worth lots of research to prove the benefit of what should be a relatively low-cost intervention. Why not just have providers write orders detailing follow-up with a specific doctor or clinic and a timeframe, and have unit secretaries communicate with outpatient clinics to schedule the appointments and ensure that the details are provided to the patient, maybe via an EHR-generated after visit summary? Seems pretty easy, right?
Turns out it isn’t easy at all for most hospitals. Lots of energetic hospitalists have taken on a project like this, only to run into so many brick walls. One hospitalist told me recently that the unit secretary’s labor union at her hospital refused to allow it. So some hospitals have turned to a single person, or a small group of people, who make appointments for all hospital patients. Some hospitalist groups have one of their own staff make appointments for hospitalist patients. This relieves the unit secretaries of the task but requires additional funding for the salaries of these people.
Maybe, at some time not so far off, EHRs will be so user-friendly and patients/families so accustomed to using them that it will be common for patients/families to arrange the appointments on their own. It could even be a required step—a hard stop—in the discharge process.
Whatever emerges as the most common method of making these appointments, I think it is safe to say this old practice will become “new” and common within the next few years.
Multidisciplinary Rounds
While working as an orderly in the 1970s, I would often visit with the nurses in their break room. When a doctor arrived to make rounds on the floor, the RN would jump up, stub out her cigarette, and round with the doctor. I sometimes tagged along as an observer. The nurse let the doctor know just how the patient had been doing and provided test results and any other relevant information the doctor might need. The doctor would provide orders, and sometimes the nurse wrote them into the chart (think of today’s medical scribes). Although their interaction was much less collaborative than is typical today, they did ask lots of questions of one another to clarify ambiguities.
I think these 1970s caregivers were doing effective multidisciplinary rounds. But by the late 1980s or so, as both doctor and nurse became busier, they stopped rounding together.
I smile when I hear descriptions of this “new” idea of doctor and nurse (and often other caregivers) rounding together. Today’s hospital culture is less hierarchical than the 1970s, though some would say it still has a ways to go, so teamwork and multidisciplinary rounds may yield more benefit than decades ago. But the idea of rounding together certainly isn’t new.
As we try to figure out the best way to thrive in a rapidly changing healthcare environment, we may find value in returning to the old ways of doing some things.

The musty collections of National Geographic magazines once found in so many basements are largely gone. Replacing them are dusty sets of the Advisory Board binders and booklets found in hospital administration offices around the country. I think the same principle drives the impulse to collect both publications—the idea that they contain worthwhile information that one day will be reviewed. But I think it’s more likely they will be ignored until it is time to move and someone has to decide what to do with the painfully heavy pile of paper.
Lots of old and largely forgotten things are making a comeback in healthcare. I suppose this is always happening, but I sense we’re now experiencing more of this than usual. It’s a renaissance of sorts.
I first heard about fecal transplant for Clostridium difficile infection (instilling a “better” microbiome in the hope of realizing many benefits) about six or eight years ago. Although I was sure this was a new idea, my retired internist father told me this had been around when he was in training. Wikipedia says that four Colorado surgeons published a paper about it in 1958 and that the Chinese were doing this 1,600 years ago.
PCPs Visit Hospitalized Patients
Writing in the NEJM earlier this year, Goroll and Hunt proposed that primary care physicians visit their hospitalized patients in the role of consultant while the hospitalist remains attending. As they note, this idea surfaced as soon as the hospitalist model began taking hold. Back then, we usually referred to it as a “social visit” by the PCP. Anecdotal experience from my work with hundreds of hospitalist groups tells me that such visits have all but disappeared. But nearly every such PCP visit on a patient I’ve cared for has seemed worthwhile; in many cases, these hospital calls simply reassure a nervous patient or family member, and occasionally they ensure that the PCP and I arrive at a more effective plan of care than we might otherwise.
Perhaps new forms of healthcare reimbursement, accountable care, and population health may make “continuity visits” economically viable for PCPs. Wouldn’t it be interesting if PCP visits to hospitalized patients and hospitalist visits to outpatients, such as those occurring in a pre-op clinic or a skilled nursing facility, become commonplace? The trick in all of this will be to ensure the right amount of overlap, or shared visits, between PCP and hospitalist without expensive duplication of effort or errors stemming from too many cooks in the kitchen.
Post-Hospital Follow-Up Schedules
When I began practicing as a hospitalist in the 1980s, doctors routinely wrote orders similar to this one: “Have patient follow up with Dr. Smith (PCP or specialist) in 1-2 weeks.” The unit secretary or other hospital clerical staff would contact the physician’s office to schedule the appointment, and the patient would leave the hospital with a written reminder in hand. My sense is that nearly all hospitals had been doing this for decades; somehow this practice has nearly disappeared over the last 10-20 years, however, and I sometimes hear this old practice discussed as a new idea.
I think making sure the patient has a follow-up appointment in hand when leaving the hospital is likely good for clinical outcomes, readmissions, and patient satisfaction. In my view, it is hardly worth lots of research to prove the benefit of what should be a relatively low-cost intervention. Why not just have providers write orders detailing follow-up with a specific doctor or clinic and a timeframe, and have unit secretaries communicate with outpatient clinics to schedule the appointments and ensure that the details are provided to the patient, maybe via an EHR-generated after visit summary? Seems pretty easy, right?
Turns out it isn’t easy at all for most hospitals. Lots of energetic hospitalists have taken on a project like this, only to run into so many brick walls. One hospitalist told me recently that the unit secretary’s labor union at her hospital refused to allow it. So some hospitals have turned to a single person, or a small group of people, who make appointments for all hospital patients. Some hospitalist groups have one of their own staff make appointments for hospitalist patients. This relieves the unit secretaries of the task but requires additional funding for the salaries of these people.
Maybe, at some time not so far off, EHRs will be so user-friendly and patients/families so accustomed to using them that it will be common for patients/families to arrange the appointments on their own. It could even be a required step—a hard stop—in the discharge process.
Whatever emerges as the most common method of making these appointments, I think it is safe to say this old practice will become “new” and common within the next few years.
Multidisciplinary Rounds
While working as an orderly in the 1970s, I would often visit with the nurses in their break room. When a doctor arrived to make rounds on the floor, the RN would jump up, stub out her cigarette, and round with the doctor. I sometimes tagged along as an observer. The nurse let the doctor know just how the patient had been doing and provided test results and any other relevant information the doctor might need. The doctor would provide orders, and sometimes the nurse wrote them into the chart (think of today’s medical scribes). Although their interaction was much less collaborative than is typical today, they did ask lots of questions of one another to clarify ambiguities.
I think these 1970s caregivers were doing effective multidisciplinary rounds. But by the late 1980s or so, as both doctor and nurse became busier, they stopped rounding together.
I smile when I hear descriptions of this “new” idea of doctor and nurse (and often other caregivers) rounding together. Today’s hospital culture is less hierarchical than the 1970s, though some would say it still has a ways to go, so teamwork and multidisciplinary rounds may yield more benefit than decades ago. But the idea of rounding together certainly isn’t new.
As we try to figure out the best way to thrive in a rapidly changing healthcare environment, we may find value in returning to the old ways of doing some things.

Standard Text Messaging for Smartphones Not HIPAA Compliant
Doctors were the first to begin using pagers and, along with drug dealers, appear to be the last to give them up. But we really need to get rid of them.
Sadly, for the foreseeable future, we will need a pager replacement, but, in the longer term, I’m hopeful that we can:
- Reduce the frequency of electronic interruptions—all forms of interruptions—and the adverse effects that reliably accompany them, and
- Ensure that each interruption has value—that is, reduce or eliminate the many low value and non-urgent messages we all get (e.g. the ones informing you of a lab result you’ve already seen).
Death to the Pager
I can’t imagine anyone who will be more pleased than I will if pagers go the way of now rare hospital-wide PA announcements. Some hospitals have eliminated these announcements entirely, and even critical messages like “code blue” announcements are sent directly to each responder via a pager or other personal device.
Around the time the first iPhone was born, hospital signs banning cell phones began coming down. It seems the fear that they would disrupt hospital electronics, such as telemetry and other monitoring devices, has proven largely unfounded (though, along with things like computer keyboards and stethoscopes, pagers and cell phones can serve as dangerous repositories of bacteria).
Now nearly everyone, from staff to patients, keeps a cell phone with them while in the hospital. I think that is the most important step toward getting rid of pagers. Many doctors already are using the standard text messaging apps that come with the phone to communicate with one another efficiently.
“Regular” Texting Won’t Cut It
Unfortunately, the standard text messaging that comes with every smartphone is not HIPAA compliant. Though I certainly don’t know how anyone would do it, it is apparently too easy for another person to intercept the message. So, if you’re texting information related to your clinical work, you need to make sure it doesn’t include anything that could be considered protected health information. It isn’t enough just to leave the patient’s name off the message. If you’re in the habit of regularly texting doctors, nurses, and other healthcare personnel about patient care, you are at high risk of violating HIPAA, even if you try hard to avoid it.
Another big drawback is that there isn’t a good way to turn off work-related texting when you’re off duty, while leaving your texting app open for communication with your friends and family. Hospital staff will sometimes fail to check whether you’re on duty before texting, and that will lead to your personal time being interrupted by work reminders.
I think these shortcomings mean that none of us should rely on the standard text messaging apps that come with our phones.
But in order for a different app or service to be of any value, we will need to ensure that most providers associated with our hospital are on the same messaging system. That is a tall order, but fortunately there are a lot of companies trying to produce an attractive product that makes it as easy as possible to attract a critical mass of users at your institution.
HIPAA-Compliant Texting Vendors
Many healthcare tech companies provide secure messaging, usually at no additional cost, as an add-on to their main products, such as charge capture software (e.g. IngeniousMed), or physician social networking (e.g. Doximity). Something like 30 companies now offer a dedicated HIPAA-compliant texting option, including IM Your Doc, Voalte, Telmediq, PerfectServe, Vocera, and TigerText. There are so many that it is awfully tough to understand all of their strengths and shortcomings in detail, but I’m having fun trying to do just that. And I anticipate there will be significant consolidation in vendors within the next two to three years.
The dedicated HIPAA-compliant texting services range in price from free for basic features to a monthly fee per user that varies depending on the features you choose to enable. Some offer integration with the hospital’s EHR, which can let a message sender who only knows the patient’s name to see which doctor, nurse, or other caregiver is currently responsible for the patient. Some offer integration with a call schedule and answering service, or even replace an answering service.
No pager replacement will be viable if there are sites in the hospital or elsewhere where it is out of contact; a solution that works on both cellular networks and Wi-Fi is essential. Some vendors offer the ability for messages not delivered to or acknowledged by the recipient to escalate to other forms of delivery after a specified period of time.
I would love to see a feature that I don’t think any vendor offers yet. It would be great if all messages the sender hasn’t marked “stat” or “urgent” first went to a queue in the EHR rather than immediately interrupting the recipient. That way a doctor or other caregiver could see messages while already working in the EHR, rather than glancing at each new message as it arrives, something that all too often needlessly interrupts another important task such as talking with a patient.
And, since most work in EHRs is done in front of a larger device with a full keyboard, it would be easier to type a quick reply message than it would be to rely on a smartphone keyboard for return messaging. Protocols could be established such that messages waiting in the EHR without a reply or dismissal after a specified time would then be sent to the recipient’s personal device.
A Texting Ecosystem
In nearly every case, the hospital will select the text messaging vendor, though hospitalists and nurses, who will typically be among the highest-volume users, should participate in the decision. But the real value of the system hinges on ensuring its wide adoption by most, or nearly all, hospital caregivers and affiliated ambulatory providers.
I would enjoy hearing from those who are already using a HIPAA-secure texting and pager replacement service now, as well as those still researching their options. This has the potential to meaningfully change the way hospitalists and others do their work.

Doctors were the first to begin using pagers and, along with drug dealers, appear to be the last to give them up. But we really need to get rid of them.
Sadly, for the foreseeable future, we will need a pager replacement, but, in the longer term, I’m hopeful that we can:
- Reduce the frequency of electronic interruptions—all forms of interruptions—and the adverse effects that reliably accompany them, and
- Ensure that each interruption has value—that is, reduce or eliminate the many low value and non-urgent messages we all get (e.g. the ones informing you of a lab result you’ve already seen).
Death to the Pager
I can’t imagine anyone who will be more pleased than I will if pagers go the way of now rare hospital-wide PA announcements. Some hospitals have eliminated these announcements entirely, and even critical messages like “code blue” announcements are sent directly to each responder via a pager or other personal device.
Around the time the first iPhone was born, hospital signs banning cell phones began coming down. It seems the fear that they would disrupt hospital electronics, such as telemetry and other monitoring devices, has proven largely unfounded (though, along with things like computer keyboards and stethoscopes, pagers and cell phones can serve as dangerous repositories of bacteria).
Now nearly everyone, from staff to patients, keeps a cell phone with them while in the hospital. I think that is the most important step toward getting rid of pagers. Many doctors already are using the standard text messaging apps that come with the phone to communicate with one another efficiently.
“Regular” Texting Won’t Cut It
Unfortunately, the standard text messaging that comes with every smartphone is not HIPAA compliant. Though I certainly don’t know how anyone would do it, it is apparently too easy for another person to intercept the message. So, if you’re texting information related to your clinical work, you need to make sure it doesn’t include anything that could be considered protected health information. It isn’t enough just to leave the patient’s name off the message. If you’re in the habit of regularly texting doctors, nurses, and other healthcare personnel about patient care, you are at high risk of violating HIPAA, even if you try hard to avoid it.
Another big drawback is that there isn’t a good way to turn off work-related texting when you’re off duty, while leaving your texting app open for communication with your friends and family. Hospital staff will sometimes fail to check whether you’re on duty before texting, and that will lead to your personal time being interrupted by work reminders.
I think these shortcomings mean that none of us should rely on the standard text messaging apps that come with our phones.
But in order for a different app or service to be of any value, we will need to ensure that most providers associated with our hospital are on the same messaging system. That is a tall order, but fortunately there are a lot of companies trying to produce an attractive product that makes it as easy as possible to attract a critical mass of users at your institution.
HIPAA-Compliant Texting Vendors
Many healthcare tech companies provide secure messaging, usually at no additional cost, as an add-on to their main products, such as charge capture software (e.g. IngeniousMed), or physician social networking (e.g. Doximity). Something like 30 companies now offer a dedicated HIPAA-compliant texting option, including IM Your Doc, Voalte, Telmediq, PerfectServe, Vocera, and TigerText. There are so many that it is awfully tough to understand all of their strengths and shortcomings in detail, but I’m having fun trying to do just that. And I anticipate there will be significant consolidation in vendors within the next two to three years.
The dedicated HIPAA-compliant texting services range in price from free for basic features to a monthly fee per user that varies depending on the features you choose to enable. Some offer integration with the hospital’s EHR, which can let a message sender who only knows the patient’s name to see which doctor, nurse, or other caregiver is currently responsible for the patient. Some offer integration with a call schedule and answering service, or even replace an answering service.
No pager replacement will be viable if there are sites in the hospital or elsewhere where it is out of contact; a solution that works on both cellular networks and Wi-Fi is essential. Some vendors offer the ability for messages not delivered to or acknowledged by the recipient to escalate to other forms of delivery after a specified period of time.
I would love to see a feature that I don’t think any vendor offers yet. It would be great if all messages the sender hasn’t marked “stat” or “urgent” first went to a queue in the EHR rather than immediately interrupting the recipient. That way a doctor or other caregiver could see messages while already working in the EHR, rather than glancing at each new message as it arrives, something that all too often needlessly interrupts another important task such as talking with a patient.
And, since most work in EHRs is done in front of a larger device with a full keyboard, it would be easier to type a quick reply message than it would be to rely on a smartphone keyboard for return messaging. Protocols could be established such that messages waiting in the EHR without a reply or dismissal after a specified time would then be sent to the recipient’s personal device.
A Texting Ecosystem
In nearly every case, the hospital will select the text messaging vendor, though hospitalists and nurses, who will typically be among the highest-volume users, should participate in the decision. But the real value of the system hinges on ensuring its wide adoption by most, or nearly all, hospital caregivers and affiliated ambulatory providers.
I would enjoy hearing from those who are already using a HIPAA-secure texting and pager replacement service now, as well as those still researching their options. This has the potential to meaningfully change the way hospitalists and others do their work.

Doctors were the first to begin using pagers and, along with drug dealers, appear to be the last to give them up. But we really need to get rid of them.
Sadly, for the foreseeable future, we will need a pager replacement, but, in the longer term, I’m hopeful that we can:
- Reduce the frequency of electronic interruptions—all forms of interruptions—and the adverse effects that reliably accompany them, and
- Ensure that each interruption has value—that is, reduce or eliminate the many low value and non-urgent messages we all get (e.g. the ones informing you of a lab result you’ve already seen).
Death to the Pager
I can’t imagine anyone who will be more pleased than I will if pagers go the way of now rare hospital-wide PA announcements. Some hospitals have eliminated these announcements entirely, and even critical messages like “code blue” announcements are sent directly to each responder via a pager or other personal device.
Around the time the first iPhone was born, hospital signs banning cell phones began coming down. It seems the fear that they would disrupt hospital electronics, such as telemetry and other monitoring devices, has proven largely unfounded (though, along with things like computer keyboards and stethoscopes, pagers and cell phones can serve as dangerous repositories of bacteria).
Now nearly everyone, from staff to patients, keeps a cell phone with them while in the hospital. I think that is the most important step toward getting rid of pagers. Many doctors already are using the standard text messaging apps that come with the phone to communicate with one another efficiently.
“Regular” Texting Won’t Cut It
Unfortunately, the standard text messaging that comes with every smartphone is not HIPAA compliant. Though I certainly don’t know how anyone would do it, it is apparently too easy for another person to intercept the message. So, if you’re texting information related to your clinical work, you need to make sure it doesn’t include anything that could be considered protected health information. It isn’t enough just to leave the patient’s name off the message. If you’re in the habit of regularly texting doctors, nurses, and other healthcare personnel about patient care, you are at high risk of violating HIPAA, even if you try hard to avoid it.
Another big drawback is that there isn’t a good way to turn off work-related texting when you’re off duty, while leaving your texting app open for communication with your friends and family. Hospital staff will sometimes fail to check whether you’re on duty before texting, and that will lead to your personal time being interrupted by work reminders.
I think these shortcomings mean that none of us should rely on the standard text messaging apps that come with our phones.
But in order for a different app or service to be of any value, we will need to ensure that most providers associated with our hospital are on the same messaging system. That is a tall order, but fortunately there are a lot of companies trying to produce an attractive product that makes it as easy as possible to attract a critical mass of users at your institution.
HIPAA-Compliant Texting Vendors
Many healthcare tech companies provide secure messaging, usually at no additional cost, as an add-on to their main products, such as charge capture software (e.g. IngeniousMed), or physician social networking (e.g. Doximity). Something like 30 companies now offer a dedicated HIPAA-compliant texting option, including IM Your Doc, Voalte, Telmediq, PerfectServe, Vocera, and TigerText. There are so many that it is awfully tough to understand all of their strengths and shortcomings in detail, but I’m having fun trying to do just that. And I anticipate there will be significant consolidation in vendors within the next two to three years.
The dedicated HIPAA-compliant texting services range in price from free for basic features to a monthly fee per user that varies depending on the features you choose to enable. Some offer integration with the hospital’s EHR, which can let a message sender who only knows the patient’s name to see which doctor, nurse, or other caregiver is currently responsible for the patient. Some offer integration with a call schedule and answering service, or even replace an answering service.
No pager replacement will be viable if there are sites in the hospital or elsewhere where it is out of contact; a solution that works on both cellular networks and Wi-Fi is essential. Some vendors offer the ability for messages not delivered to or acknowledged by the recipient to escalate to other forms of delivery after a specified period of time.
I would love to see a feature that I don’t think any vendor offers yet. It would be great if all messages the sender hasn’t marked “stat” or “urgent” first went to a queue in the EHR rather than immediately interrupting the recipient. That way a doctor or other caregiver could see messages while already working in the EHR, rather than glancing at each new message as it arrives, something that all too often needlessly interrupts another important task such as talking with a patient.
And, since most work in EHRs is done in front of a larger device with a full keyboard, it would be easier to type a quick reply message than it would be to rely on a smartphone keyboard for return messaging. Protocols could be established such that messages waiting in the EHR without a reply or dismissal after a specified time would then be sent to the recipient’s personal device.
A Texting Ecosystem
In nearly every case, the hospital will select the text messaging vendor, though hospitalists and nurses, who will typically be among the highest-volume users, should participate in the decision. But the real value of the system hinges on ensuring its wide adoption by most, or nearly all, hospital caregivers and affiliated ambulatory providers.
I would enjoy hearing from those who are already using a HIPAA-secure texting and pager replacement service now, as well as those still researching their options. This has the potential to meaningfully change the way hospitalists and others do their work.

Rapid-Response Teams Help Hospitalists Manage Non-Medical Distress
A team that could respond quickly to social and behavioral concerns—and not medical issues per se—would have tremendous benefits for patients and caregivers.
I think there has been a steady increase, over the last 20 years or so, in the number of very unhappy, angry, or misbehaving patients (e.g. abusive/threatening to staff). In some cases, the hospital and caregivers have failed the patient. In other cases, their frustration arises out of things outside the hospital’s direct control, such as Medicare observation status, or perhaps the patient or family is just unreasonable or suffering from a psychiatric or substance abuse disorder.
I’m not talking about the common occurrence of a disappointed patient or family who might calmly complain about something. Instead, I want to focus on those patients who, whether we perceive them as justifiably unhappy or not, are so angry that they become very time consuming and distressing to deal with. Maybe they shout about how their lawyer will be suing us and the newspaper will be writing a story about how awful we are. Or they shout and throw things, and staff become afraid of them.
In my May 2013 column, I discussed care plans for patients like this who are admitted frequently, but such plans are not sufficient in every case.
A Haphazard Approach
Most hospitals have an informal process of dealing with these patients; it starts with the bedside nurse and/or doctor trying to apologize or make adjustments to satisfy and calm the patient. If that fails, then perhaps the manager of the nursing unit gets involved. Others may be recruited, such as someone from the hospital’s risk management or “patient advocate” departments and hospital executives such as the CNO, CMO, or CEO. Sometimes several of these people may meet as a group in an effort to come up with a plan to address the situation. But, most institutions do not have a clear and consistent approach to this important work, so the hospital personnel involved end up “reinventing the wheel” each time.
The growing awareness that hospital personnel don’t seem to have a robust and confident approach to addressing this type of situation can increase a patient’s distress, and it may embolden some to become even more demanding or threatening.
And all of this takes a significant toll on bedside caregivers, who often spend so much time dealing with the angry patient that they have less time to devote to other patients, who are in turn at least a little more likely to become unhappy or suffer as a result of a distressed and busy caregiver.
A Consistent Approach: RRT for Non-Medical Distress
I think the potential benefit for patients and caregivers is significant enough that hospitals should develop a standardized approach to managing such patients, and rapid response teams (RRTs) could serve as a model. To be clear, I’m not advocating that RRTs add management of very angry or distressed patients to their current role. Let’s call it an “RRT for non-medical distress.” And, while I think it is a worthwhile idea, and I am in the early steps of trying to develop it at “my” hospital, I’m not aware of any such team in place anywhere now.
To make it practical, I think this team should be available only during weekday business hours and would comprise something like six to 10 people with clinical backgrounds who do mostly administrative work. For example, the team members could include two nursing unit directors, a risk manager, a patient advocate (or patient satisfaction “czar”), a psychiatrist, the hospitalist medical director, the chief medical officer, and a few other individuals selected for their communication skills.
One of the team members would be on call for a day or week at a time and would carry the team’s pager during business hours. Any hospital caregiver could send a page requesting the team’s assistance, and the on-call team member would respond immediately by phone or, if possible, in person. After the on-call team member’s initial assessment, the whole team would meet later the same day or early the next day. On most days, a few members of the team would be off and unable to attend the meeting. So, if the team has eight members, each meeting of the team might average about five participants.
Non-Medical Distress RRT Processes
When meeting to establish a plan for addressing an extraordinarily distressed patient/family, the team should follow a standardized written approach. A designated person should lead the conversation—perhaps the on-call team member who responded first—and another should take notes. Using a form developed for this purpose, the note-taker would capture a standardized data set that is likely to be useful in determining a course of action, as well as valuable in helping the team fine-tune its approach by reviewing trends in aggregate data. The form might include things like patient demographics; the patient’s complaints and demands; potential complicating patient issues such as substance abuse, psychoactive drugs, or psychiatric history; location in the hospital; and names of bedside caregivers. Every effort should be made to keep the meetings efficient and as brief as practical—typically 30-60 minutes.
I’m convinced that when deciding how to respond to the situation, the team should try to limit itself to choosing one or more of eight to 10 standard interventions, rather than aiming for an entirely customized response in every case. Among the standardized interventions:
- Service recovery tools, such as a handwritten apology letter;
- A meeting between the patient/family and the hospital CEO or CMO;
- Security guard(s) at the door, on “high alert” to help if called; or
- A behavioral contract specifying the expectations for both patient and hospital staff behavior.
You might think of additional “tools” this team could have in their standardized response set.
Why limit the team as much as possible to a small set of standardized interventions? Developing customized responses in each situation is time consuming and, arguably, has a higher risk of failure, since it will be difficult to ensure that all staff caring for the patient can understand and execute them effectively. And the small set of interventions will make it easier to track their effectiveness over multiple patients so that the whole process can be improved over time.
Set a High Bar
The team should not be activated for every unhappy or difficult patient; that would be overkill and would result in many activations requiring dedicated staff with no other duties to serve on the team each day. Instead, I think the team should be activated only for the most difficult and distressing cases, at least for the first few years. In a 300-bed hospital, this would be approximately one to 1.5 activations per week.
Bedside caregivers would likely feel some reassurance knowing that they can reliably get help managing the most difficult patients, and, if the plan is executed well, these patients may get care that is safer for both themselves and staff. Who knows, medical outcomes might be improved for these patients also.

A team that could respond quickly to social and behavioral concerns—and not medical issues per se—would have tremendous benefits for patients and caregivers.
I think there has been a steady increase, over the last 20 years or so, in the number of very unhappy, angry, or misbehaving patients (e.g. abusive/threatening to staff). In some cases, the hospital and caregivers have failed the patient. In other cases, their frustration arises out of things outside the hospital’s direct control, such as Medicare observation status, or perhaps the patient or family is just unreasonable or suffering from a psychiatric or substance abuse disorder.
I’m not talking about the common occurrence of a disappointed patient or family who might calmly complain about something. Instead, I want to focus on those patients who, whether we perceive them as justifiably unhappy or not, are so angry that they become very time consuming and distressing to deal with. Maybe they shout about how their lawyer will be suing us and the newspaper will be writing a story about how awful we are. Or they shout and throw things, and staff become afraid of them.
In my May 2013 column, I discussed care plans for patients like this who are admitted frequently, but such plans are not sufficient in every case.
A Haphazard Approach
Most hospitals have an informal process of dealing with these patients; it starts with the bedside nurse and/or doctor trying to apologize or make adjustments to satisfy and calm the patient. If that fails, then perhaps the manager of the nursing unit gets involved. Others may be recruited, such as someone from the hospital’s risk management or “patient advocate” departments and hospital executives such as the CNO, CMO, or CEO. Sometimes several of these people may meet as a group in an effort to come up with a plan to address the situation. But, most institutions do not have a clear and consistent approach to this important work, so the hospital personnel involved end up “reinventing the wheel” each time.
The growing awareness that hospital personnel don’t seem to have a robust and confident approach to addressing this type of situation can increase a patient’s distress, and it may embolden some to become even more demanding or threatening.
And all of this takes a significant toll on bedside caregivers, who often spend so much time dealing with the angry patient that they have less time to devote to other patients, who are in turn at least a little more likely to become unhappy or suffer as a result of a distressed and busy caregiver.
A Consistent Approach: RRT for Non-Medical Distress
I think the potential benefit for patients and caregivers is significant enough that hospitals should develop a standardized approach to managing such patients, and rapid response teams (RRTs) could serve as a model. To be clear, I’m not advocating that RRTs add management of very angry or distressed patients to their current role. Let’s call it an “RRT for non-medical distress.” And, while I think it is a worthwhile idea, and I am in the early steps of trying to develop it at “my” hospital, I’m not aware of any such team in place anywhere now.
To make it practical, I think this team should be available only during weekday business hours and would comprise something like six to 10 people with clinical backgrounds who do mostly administrative work. For example, the team members could include two nursing unit directors, a risk manager, a patient advocate (or patient satisfaction “czar”), a psychiatrist, the hospitalist medical director, the chief medical officer, and a few other individuals selected for their communication skills.
One of the team members would be on call for a day or week at a time and would carry the team’s pager during business hours. Any hospital caregiver could send a page requesting the team’s assistance, and the on-call team member would respond immediately by phone or, if possible, in person. After the on-call team member’s initial assessment, the whole team would meet later the same day or early the next day. On most days, a few members of the team would be off and unable to attend the meeting. So, if the team has eight members, each meeting of the team might average about five participants.
Non-Medical Distress RRT Processes
When meeting to establish a plan for addressing an extraordinarily distressed patient/family, the team should follow a standardized written approach. A designated person should lead the conversation—perhaps the on-call team member who responded first—and another should take notes. Using a form developed for this purpose, the note-taker would capture a standardized data set that is likely to be useful in determining a course of action, as well as valuable in helping the team fine-tune its approach by reviewing trends in aggregate data. The form might include things like patient demographics; the patient’s complaints and demands; potential complicating patient issues such as substance abuse, psychoactive drugs, or psychiatric history; location in the hospital; and names of bedside caregivers. Every effort should be made to keep the meetings efficient and as brief as practical—typically 30-60 minutes.
I’m convinced that when deciding how to respond to the situation, the team should try to limit itself to choosing one or more of eight to 10 standard interventions, rather than aiming for an entirely customized response in every case. Among the standardized interventions:
- Service recovery tools, such as a handwritten apology letter;
- A meeting between the patient/family and the hospital CEO or CMO;
- Security guard(s) at the door, on “high alert” to help if called; or
- A behavioral contract specifying the expectations for both patient and hospital staff behavior.
You might think of additional “tools” this team could have in their standardized response set.
Why limit the team as much as possible to a small set of standardized interventions? Developing customized responses in each situation is time consuming and, arguably, has a higher risk of failure, since it will be difficult to ensure that all staff caring for the patient can understand and execute them effectively. And the small set of interventions will make it easier to track their effectiveness over multiple patients so that the whole process can be improved over time.
Set a High Bar
The team should not be activated for every unhappy or difficult patient; that would be overkill and would result in many activations requiring dedicated staff with no other duties to serve on the team each day. Instead, I think the team should be activated only for the most difficult and distressing cases, at least for the first few years. In a 300-bed hospital, this would be approximately one to 1.5 activations per week.
Bedside caregivers would likely feel some reassurance knowing that they can reliably get help managing the most difficult patients, and, if the plan is executed well, these patients may get care that is safer for both themselves and staff. Who knows, medical outcomes might be improved for these patients also.

A team that could respond quickly to social and behavioral concerns—and not medical issues per se—would have tremendous benefits for patients and caregivers.
I think there has been a steady increase, over the last 20 years or so, in the number of very unhappy, angry, or misbehaving patients (e.g. abusive/threatening to staff). In some cases, the hospital and caregivers have failed the patient. In other cases, their frustration arises out of things outside the hospital’s direct control, such as Medicare observation status, or perhaps the patient or family is just unreasonable or suffering from a psychiatric or substance abuse disorder.
I’m not talking about the common occurrence of a disappointed patient or family who might calmly complain about something. Instead, I want to focus on those patients who, whether we perceive them as justifiably unhappy or not, are so angry that they become very time consuming and distressing to deal with. Maybe they shout about how their lawyer will be suing us and the newspaper will be writing a story about how awful we are. Or they shout and throw things, and staff become afraid of them.
In my May 2013 column, I discussed care plans for patients like this who are admitted frequently, but such plans are not sufficient in every case.
A Haphazard Approach
Most hospitals have an informal process of dealing with these patients; it starts with the bedside nurse and/or doctor trying to apologize or make adjustments to satisfy and calm the patient. If that fails, then perhaps the manager of the nursing unit gets involved. Others may be recruited, such as someone from the hospital’s risk management or “patient advocate” departments and hospital executives such as the CNO, CMO, or CEO. Sometimes several of these people may meet as a group in an effort to come up with a plan to address the situation. But, most institutions do not have a clear and consistent approach to this important work, so the hospital personnel involved end up “reinventing the wheel” each time.
The growing awareness that hospital personnel don’t seem to have a robust and confident approach to addressing this type of situation can increase a patient’s distress, and it may embolden some to become even more demanding or threatening.
And all of this takes a significant toll on bedside caregivers, who often spend so much time dealing with the angry patient that they have less time to devote to other patients, who are in turn at least a little more likely to become unhappy or suffer as a result of a distressed and busy caregiver.
A Consistent Approach: RRT for Non-Medical Distress
I think the potential benefit for patients and caregivers is significant enough that hospitals should develop a standardized approach to managing such patients, and rapid response teams (RRTs) could serve as a model. To be clear, I’m not advocating that RRTs add management of very angry or distressed patients to their current role. Let’s call it an “RRT for non-medical distress.” And, while I think it is a worthwhile idea, and I am in the early steps of trying to develop it at “my” hospital, I’m not aware of any such team in place anywhere now.
To make it practical, I think this team should be available only during weekday business hours and would comprise something like six to 10 people with clinical backgrounds who do mostly administrative work. For example, the team members could include two nursing unit directors, a risk manager, a patient advocate (or patient satisfaction “czar”), a psychiatrist, the hospitalist medical director, the chief medical officer, and a few other individuals selected for their communication skills.
One of the team members would be on call for a day or week at a time and would carry the team’s pager during business hours. Any hospital caregiver could send a page requesting the team’s assistance, and the on-call team member would respond immediately by phone or, if possible, in person. After the on-call team member’s initial assessment, the whole team would meet later the same day or early the next day. On most days, a few members of the team would be off and unable to attend the meeting. So, if the team has eight members, each meeting of the team might average about five participants.
Non-Medical Distress RRT Processes
When meeting to establish a plan for addressing an extraordinarily distressed patient/family, the team should follow a standardized written approach. A designated person should lead the conversation—perhaps the on-call team member who responded first—and another should take notes. Using a form developed for this purpose, the note-taker would capture a standardized data set that is likely to be useful in determining a course of action, as well as valuable in helping the team fine-tune its approach by reviewing trends in aggregate data. The form might include things like patient demographics; the patient’s complaints and demands; potential complicating patient issues such as substance abuse, psychoactive drugs, or psychiatric history; location in the hospital; and names of bedside caregivers. Every effort should be made to keep the meetings efficient and as brief as practical—typically 30-60 minutes.
I’m convinced that when deciding how to respond to the situation, the team should try to limit itself to choosing one or more of eight to 10 standard interventions, rather than aiming for an entirely customized response in every case. Among the standardized interventions:
- Service recovery tools, such as a handwritten apology letter;
- A meeting between the patient/family and the hospital CEO or CMO;
- Security guard(s) at the door, on “high alert” to help if called; or
- A behavioral contract specifying the expectations for both patient and hospital staff behavior.
You might think of additional “tools” this team could have in their standardized response set.
Why limit the team as much as possible to a small set of standardized interventions? Developing customized responses in each situation is time consuming and, arguably, has a higher risk of failure, since it will be difficult to ensure that all staff caring for the patient can understand and execute them effectively. And the small set of interventions will make it easier to track their effectiveness over multiple patients so that the whole process can be improved over time.
Set a High Bar
The team should not be activated for every unhappy or difficult patient; that would be overkill and would result in many activations requiring dedicated staff with no other duties to serve on the team each day. Instead, I think the team should be activated only for the most difficult and distressing cases, at least for the first few years. In a 300-bed hospital, this would be approximately one to 1.5 activations per week.
Bedside caregivers would likely feel some reassurance knowing that they can reliably get help managing the most difficult patients, and, if the plan is executed well, these patients may get care that is safer for both themselves and staff. Who knows, medical outcomes might be improved for these patients also.

Geographic Rounding of Hospital Nurses Challenges Unit-Based Theory
Nurses, of course, have always been assigned by unit—that is, geographically. So it should come as no surprise that searching “unit-based” at the-hospitalist.org returns many articles about assigning hospitalists geographically, but not nurses, partly because few would consider it a new idea. But this article is about a new wrinkle in assigning nurses.
Although there likely are a number of hospitals doing something similar, I’ll describe a place I was lucky enough to see up close.
Bassett Medical Center
On a cold day last December, I was part of a team that spent a few days in Cooperstown, N.Y. This is a place that is so pretty that I didn’t immediately recognize we had arrived at the Bassett Medical Center Campus, since the entrance we used looked more like a library topped by a pretty cupola and warmly decorated for the holidays. We met so many nice people, including Kai Mebust, MD, FHM, who I’m convinced works full-time for the local Chamber of Commerce and tourism industry. If he doesn’t, then they should put him on their payroll.
Not long after our arrival, Dr. Mebust led us outside in the winter air without our coats to see the very beautiful view from the patio adjacent to the hospital cafeteria. And before we left for home he climbed in our car to direct us on a tour of the town. I’m sold. What a beautiful place. So much more than the Baseball Hall of Fame for which Cooperstown is known.
When not promoting his town’s tourism or enthusiastically describing his eighth-grade son playing with the Preservation Hall Jazz Band in New Orleans, he seems to find time to serve as the chief of this academic hospital’s hospital medicine practice. He was the principal engineer of the geographic assignment of nurses and describes it with an enthusiasm that matches his service as tour guide.
Geographic Care: Single RN Caring for Five Adjacent Patients
The idea is simple and best described using an illustration. A single nurse cares for five patients in adjacent rooms referred to as a “pod.” A second nurse is responsible for the next pod of five consecutive patients, and a single hospitalist cares for all 10 in both pods. There are currently four pods on a single floor of 36 beds; however, they hope to expand this system to most of the medical-surgical beds in the hospital.
The nurses eligible to care for patients in these pods are all trained to be able to provide “step down” level of care, meaning patients don’t need to transfer to a different location for more frequent monitoring and such therapies as vasopressors, mask ventilation, and the like.
Each hospitalist caring for two pods of 10 adjacent patients will typically have additional patients in other locations. This is the hospital’s way of finding the sweet spot between the competing interests of “load leveling” patient volume across hospitalists and rigidly assigning each doctor to a single location, though if they succeed in expanding the model through most of the hospital, the hospitalists will likely need to figure out how to assign themselves more rigidly to three or four pods.
Additional Components
Each morning, the hospitalist meets with the two pod nurses. They briefly discuss overnight events and plans for the day.
Much later in the morning, they also conduct daily multidisciplinary rounds involving nurse, case manager, pharmacist, dietician, social worker, respiratory therapist, and hospitalist. These follow a standard format, which is posted on the wall, and are done in a workroom that allows most participants to be in front of a computer, so they can enter notes and orders into the electronic health record (EHR) as they discuss patients.
What Is the Big Deal Here?
A lot of smart people have developed and written about systems that assign hospitalists geographically, but in most cases this has not been accompanied by adjustments in the way nurses are assigned. On nursing units at most hospitals, this means that even if a hospitalist has all of her patients on the same floor, she is still interacting with five to seven nurses caring for her patients. That usually means the hospitalist and nurse have less awareness of each other’s thinking and doing than if the ratio is reduced to no more than three or four nurses for a single hospitalist.
Dr. Mebust provided a document enumerating the goals for the program:
- Improve communication;
- Reduce patient bed moves;
- Improve patient and staff satisfaction; and
- Provide more efficient care as measured in time-of-discharge, decreased physician time-per-patient, and possibly length of stay.
Because of a number of problems teasing out the effects of this program and its limited duration to this point, Dr. Mebust and staff can’t provide robust statistics to document success in these goals. But anecdotal information is very encouraging, and clearly the nurses love it.
A major barrier to assigning nurses based rigidly on patients in adjacent rooms is the inability to ensure that each nurse has a workload of roughly equivalent complexity, but they’ve found this is a much less significant problem than feared. The nurse I spoke with said any risk of ending up with unusually complex and time-consuming patients is essentially offset by the efficiency gained by having the same attending hospitalist for all of her patients.
In fact, the nurses love it so much that they much prefer being assigned to a pod rather than a traditional assortment of patients with different attending physicians, even if the latter offers a chance to address uneven acuity.
The Big Picture
I’ve often wished that I could incorporate into hospitalist work some of the efficient ways a doctor and nurse can work together seeing scheduled patients in an outpatient setting. Surely assigning hospitalists geographically does this to some degree and has a number of advantages that others have written about. But it comes at the cost of difficult tradeoffs for hospitalists, and I know of many groups that have abandoned it after concluding that the challenges of the system exceeded its benefits.
But when it is coupled with assigning nurses geographically, I think the benefits are even greater, not only for the hospitalists, but also for patients, nurses, and other hospital staff.
Next time you’re in Cooperstown, be sure you don’t just visit the Baseball Hall of Fame. Look up Dr. Mebust, Komron Ostovar, MD, and their colleagues at Bassett Medical Center. I betcha you’ll be persuaded to see the value of their geographic model.
And maybe you’ll even fall so far under the spell of how they all talk about where they work and live that you’ll be ready to move there and join them.

Nurses, of course, have always been assigned by unit—that is, geographically. So it should come as no surprise that searching “unit-based” at the-hospitalist.org returns many articles about assigning hospitalists geographically, but not nurses, partly because few would consider it a new idea. But this article is about a new wrinkle in assigning nurses.
Although there likely are a number of hospitals doing something similar, I’ll describe a place I was lucky enough to see up close.
Bassett Medical Center
On a cold day last December, I was part of a team that spent a few days in Cooperstown, N.Y. This is a place that is so pretty that I didn’t immediately recognize we had arrived at the Bassett Medical Center Campus, since the entrance we used looked more like a library topped by a pretty cupola and warmly decorated for the holidays. We met so many nice people, including Kai Mebust, MD, FHM, who I’m convinced works full-time for the local Chamber of Commerce and tourism industry. If he doesn’t, then they should put him on their payroll.
Not long after our arrival, Dr. Mebust led us outside in the winter air without our coats to see the very beautiful view from the patio adjacent to the hospital cafeteria. And before we left for home he climbed in our car to direct us on a tour of the town. I’m sold. What a beautiful place. So much more than the Baseball Hall of Fame for which Cooperstown is known.
When not promoting his town’s tourism or enthusiastically describing his eighth-grade son playing with the Preservation Hall Jazz Band in New Orleans, he seems to find time to serve as the chief of this academic hospital’s hospital medicine practice. He was the principal engineer of the geographic assignment of nurses and describes it with an enthusiasm that matches his service as tour guide.
Geographic Care: Single RN Caring for Five Adjacent Patients
The idea is simple and best described using an illustration. A single nurse cares for five patients in adjacent rooms referred to as a “pod.” A second nurse is responsible for the next pod of five consecutive patients, and a single hospitalist cares for all 10 in both pods. There are currently four pods on a single floor of 36 beds; however, they hope to expand this system to most of the medical-surgical beds in the hospital.
The nurses eligible to care for patients in these pods are all trained to be able to provide “step down” level of care, meaning patients don’t need to transfer to a different location for more frequent monitoring and such therapies as vasopressors, mask ventilation, and the like.
Each hospitalist caring for two pods of 10 adjacent patients will typically have additional patients in other locations. This is the hospital’s way of finding the sweet spot between the competing interests of “load leveling” patient volume across hospitalists and rigidly assigning each doctor to a single location, though if they succeed in expanding the model through most of the hospital, the hospitalists will likely need to figure out how to assign themselves more rigidly to three or four pods.
Additional Components
Each morning, the hospitalist meets with the two pod nurses. They briefly discuss overnight events and plans for the day.
Much later in the morning, they also conduct daily multidisciplinary rounds involving nurse, case manager, pharmacist, dietician, social worker, respiratory therapist, and hospitalist. These follow a standard format, which is posted on the wall, and are done in a workroom that allows most participants to be in front of a computer, so they can enter notes and orders into the electronic health record (EHR) as they discuss patients.
What Is the Big Deal Here?
A lot of smart people have developed and written about systems that assign hospitalists geographically, but in most cases this has not been accompanied by adjustments in the way nurses are assigned. On nursing units at most hospitals, this means that even if a hospitalist has all of her patients on the same floor, she is still interacting with five to seven nurses caring for her patients. That usually means the hospitalist and nurse have less awareness of each other’s thinking and doing than if the ratio is reduced to no more than three or four nurses for a single hospitalist.
Dr. Mebust provided a document enumerating the goals for the program:
- Improve communication;
- Reduce patient bed moves;
- Improve patient and staff satisfaction; and
- Provide more efficient care as measured in time-of-discharge, decreased physician time-per-patient, and possibly length of stay.
Because of a number of problems teasing out the effects of this program and its limited duration to this point, Dr. Mebust and staff can’t provide robust statistics to document success in these goals. But anecdotal information is very encouraging, and clearly the nurses love it.
A major barrier to assigning nurses based rigidly on patients in adjacent rooms is the inability to ensure that each nurse has a workload of roughly equivalent complexity, but they’ve found this is a much less significant problem than feared. The nurse I spoke with said any risk of ending up with unusually complex and time-consuming patients is essentially offset by the efficiency gained by having the same attending hospitalist for all of her patients.
In fact, the nurses love it so much that they much prefer being assigned to a pod rather than a traditional assortment of patients with different attending physicians, even if the latter offers a chance to address uneven acuity.
The Big Picture
I’ve often wished that I could incorporate into hospitalist work some of the efficient ways a doctor and nurse can work together seeing scheduled patients in an outpatient setting. Surely assigning hospitalists geographically does this to some degree and has a number of advantages that others have written about. But it comes at the cost of difficult tradeoffs for hospitalists, and I know of many groups that have abandoned it after concluding that the challenges of the system exceeded its benefits.
But when it is coupled with assigning nurses geographically, I think the benefits are even greater, not only for the hospitalists, but also for patients, nurses, and other hospital staff.
Next time you’re in Cooperstown, be sure you don’t just visit the Baseball Hall of Fame. Look up Dr. Mebust, Komron Ostovar, MD, and their colleagues at Bassett Medical Center. I betcha you’ll be persuaded to see the value of their geographic model.
And maybe you’ll even fall so far under the spell of how they all talk about where they work and live that you’ll be ready to move there and join them.

Nurses, of course, have always been assigned by unit—that is, geographically. So it should come as no surprise that searching “unit-based” at the-hospitalist.org returns many articles about assigning hospitalists geographically, but not nurses, partly because few would consider it a new idea. But this article is about a new wrinkle in assigning nurses.
Although there likely are a number of hospitals doing something similar, I’ll describe a place I was lucky enough to see up close.
Bassett Medical Center
On a cold day last December, I was part of a team that spent a few days in Cooperstown, N.Y. This is a place that is so pretty that I didn’t immediately recognize we had arrived at the Bassett Medical Center Campus, since the entrance we used looked more like a library topped by a pretty cupola and warmly decorated for the holidays. We met so many nice people, including Kai Mebust, MD, FHM, who I’m convinced works full-time for the local Chamber of Commerce and tourism industry. If he doesn’t, then they should put him on their payroll.
Not long after our arrival, Dr. Mebust led us outside in the winter air without our coats to see the very beautiful view from the patio adjacent to the hospital cafeteria. And before we left for home he climbed in our car to direct us on a tour of the town. I’m sold. What a beautiful place. So much more than the Baseball Hall of Fame for which Cooperstown is known.
When not promoting his town’s tourism or enthusiastically describing his eighth-grade son playing with the Preservation Hall Jazz Band in New Orleans, he seems to find time to serve as the chief of this academic hospital’s hospital medicine practice. He was the principal engineer of the geographic assignment of nurses and describes it with an enthusiasm that matches his service as tour guide.
Geographic Care: Single RN Caring for Five Adjacent Patients
The idea is simple and best described using an illustration. A single nurse cares for five patients in adjacent rooms referred to as a “pod.” A second nurse is responsible for the next pod of five consecutive patients, and a single hospitalist cares for all 10 in both pods. There are currently four pods on a single floor of 36 beds; however, they hope to expand this system to most of the medical-surgical beds in the hospital.
The nurses eligible to care for patients in these pods are all trained to be able to provide “step down” level of care, meaning patients don’t need to transfer to a different location for more frequent monitoring and such therapies as vasopressors, mask ventilation, and the like.
Each hospitalist caring for two pods of 10 adjacent patients will typically have additional patients in other locations. This is the hospital’s way of finding the sweet spot between the competing interests of “load leveling” patient volume across hospitalists and rigidly assigning each doctor to a single location, though if they succeed in expanding the model through most of the hospital, the hospitalists will likely need to figure out how to assign themselves more rigidly to three or four pods.
Additional Components
Each morning, the hospitalist meets with the two pod nurses. They briefly discuss overnight events and plans for the day.
Much later in the morning, they also conduct daily multidisciplinary rounds involving nurse, case manager, pharmacist, dietician, social worker, respiratory therapist, and hospitalist. These follow a standard format, which is posted on the wall, and are done in a workroom that allows most participants to be in front of a computer, so they can enter notes and orders into the electronic health record (EHR) as they discuss patients.
What Is the Big Deal Here?
A lot of smart people have developed and written about systems that assign hospitalists geographically, but in most cases this has not been accompanied by adjustments in the way nurses are assigned. On nursing units at most hospitals, this means that even if a hospitalist has all of her patients on the same floor, she is still interacting with five to seven nurses caring for her patients. That usually means the hospitalist and nurse have less awareness of each other’s thinking and doing than if the ratio is reduced to no more than three or four nurses for a single hospitalist.
Dr. Mebust provided a document enumerating the goals for the program:
- Improve communication;
- Reduce patient bed moves;
- Improve patient and staff satisfaction; and
- Provide more efficient care as measured in time-of-discharge, decreased physician time-per-patient, and possibly length of stay.
Because of a number of problems teasing out the effects of this program and its limited duration to this point, Dr. Mebust and staff can’t provide robust statistics to document success in these goals. But anecdotal information is very encouraging, and clearly the nurses love it.
A major barrier to assigning nurses based rigidly on patients in adjacent rooms is the inability to ensure that each nurse has a workload of roughly equivalent complexity, but they’ve found this is a much less significant problem than feared. The nurse I spoke with said any risk of ending up with unusually complex and time-consuming patients is essentially offset by the efficiency gained by having the same attending hospitalist for all of her patients.
In fact, the nurses love it so much that they much prefer being assigned to a pod rather than a traditional assortment of patients with different attending physicians, even if the latter offers a chance to address uneven acuity.
The Big Picture
I’ve often wished that I could incorporate into hospitalist work some of the efficient ways a doctor and nurse can work together seeing scheduled patients in an outpatient setting. Surely assigning hospitalists geographically does this to some degree and has a number of advantages that others have written about. But it comes at the cost of difficult tradeoffs for hospitalists, and I know of many groups that have abandoned it after concluding that the challenges of the system exceeded its benefits.
But when it is coupled with assigning nurses geographically, I think the benefits are even greater, not only for the hospitalists, but also for patients, nurses, and other hospital staff.
Next time you’re in Cooperstown, be sure you don’t just visit the Baseball Hall of Fame. Look up Dr. Mebust, Komron Ostovar, MD, and their colleagues at Bassett Medical Center. I betcha you’ll be persuaded to see the value of their geographic model.
And maybe you’ll even fall so far under the spell of how they all talk about where they work and live that you’ll be ready to move there and join them.