User login
The Veterans Affairs Patient Safety Center of Inquiry—Suicide Prevention Collaborative: Creating Novel Approaches to Suicide Prevention Among Veterans Receiving Community Services
Since 2008, suicide has ranked as the tenth leading cause of death for all ages in the US, with rates of suicide continuing to rise.1-3 Suicide is even more urgent to address in veteran populations. The age- and sex-adjusted suicide rate in 2017 was more than 1.5 times greater for veterans than it was for nonveteran adults.2 Of importance, rates of suicide are increasing at a faster rate in veterans who are not connected to Veterans Health Administration (VHA) care.4,5 These at-risk veterans include individuals who are eligible for VHA care yet have not had a VHA appointment within the year before death; veterans who may be ineligible to receive VHA care due to complex rules set by legislation; and veterans who are eligible but not enrolled in VHA care. Notably, between 2005 and 2016, the number of veterans not enrolled in VHA care rose more quickly than did the number of veterans enrolled in VHA care.5,6 Thus, to impact the high veteran suicide rates, an emergent challenge for VHA is to prevent suicide among unenrolled veterans and veterans receiving community care, while continuing to increase access to mental health services for veterans enrolled in VHA health care.
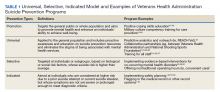
In response to the high rates of veteran suicide deaths, the US Department of Veterans Affairs (VA) has developed a broad, multicomponent suicide prevention program that is unparalleled in private US health care systems.4,7 Suicide prevention efforts are led and implemented by both the VHA National Center for Patient Safety and the VHA Office of Mental Health and Suicide Prevention. Program components are numerous and multifaceted, falling within the broad promotion and prevention strategies outlined by the National Academy of Medicine (NAM).1,8-11 The NAM continuum of prevention model encompassing multiple strategies is also referred to as the Universal, Selective, Indicated (USI) Model.7,8,10 The VHA suicide prevention program contains a wide spread of program components, making it both comprehensive and innovative (Table 1).
Although significant momentum and progress has been made within the VHA, policy set by legislation has historically limited access to VHA health care services to VHA-eligible veterans. This is particularly concerning given the rising suicide rates among veterans not engaged in VHA care.2 Adding to this complexity, recent legislation has increased veterans’ access to non-VHA health care, in addition to their existing access through Medicare, Medicaid, and other health care programs.12-14 Best practices for suicide prevention are not often implemented in the private sector; thus, these systems are ill prepared to adequately meet the suicide prevention care needs of veterans.4,15-18 Furthermore, VHA and non-VHA services generally are not well coordinated, and private sector health care providers (HCPs) are not required to complete a commensurate level of suicide prevention training as are VHA HCPs.16-18 Most non-VHA HCPs do not receive military cultural competence training.19 These issues create a significant gap in suicide prevention services and may contribute to the increases in suicide rates in veterans who do not receive VHA care. Thus, changes in policy to increase access through private sector care may have paradoxical effects on veteran suicide deaths. To impact the veteran suicide rate, VHA must develop and disseminate best practices for veterans who use non-VHA services.
A Roadmap to Suicide Prevention
There is significant momentum at the federal level regarding this issue. The President’s Roadmap to Empower Veterans and End the National Tragedy of Suicide (Executive Order 13,861) directs the VHA to work closely with community organizations to improve veteran suicide prevention.20 The VHA and partners, such as the Substance Abuse and Mental Health Services Administration (SAMHSA), are bridging this gap with collaborative efforts that increase suicide prevention resources for veterans living in the community through programs such as the Governor’s Challenges to Prevent Suicide Among Service Members, Veterans, and their Families. These programs intend to empower communities to develop statewide, strategic action plans to prevent veteran suicide.7,21-24
In addition to partnerships, VHA has built other aspects of outreach and intervention into its programming. A key VHA initiative is to “know all veterans” by committing to identifying and reaching out to all veterans who may be at risk for suicide.22 The VHA has committed to offering “emergency stabilization care for former service members who present at the facility with an emergent mental health need” regardless of eligibility.25 The intent is to provide temporary emergent mental health care to veterans who are otherwise ineligible for care, such as those who were discharged under other-than-honorable conditions while the VHA determines eligibility status.26 However, veterans must meet certain criteria, and there is a limit on services.
Although services are being expanded to reach veterans who do not access VHA health care, how to best implement these new directives with regard to suicide prevention is unclear. Strategic development and innovations to expand suicide prevention care to veterans outside the current reach of VHA are desperately needed.
Program Overview
VHA Patient Safety Center of Inquiry-Suicide Prevention Collaborative (PSCI-SPC), funded by the VHA National Center for Patient Safety, aims to help fill the gap in community-based suicide prevention for veterans. PSCI-SPC is located within the VHA Rocky Mountain Mental Illness Research, Education, and Clinical Center in Aurora, Colorado. The overarching mission of PSCI-SPC is to develop, implement, and evaluate practical solutions to reduce suicide among veterans not receiving VHA care. PSCI-SPC serves as a national clinical innovation and dissemination center for best practices in suicide prevention for organizations that serve veterans who receive care in the community. PSCI-SPC creates products to support dissemination of these practices to other VAMCs and works to ensure these programs are sustainable. PSCI-SPC focuses on 3 primary objectives. All PSCI-SPC projects are currently underway.
Objective 1: Growing a Community Learning Collaborative
Acknowledging that nearly two-thirds of veterans who die by suicide do not use VHA services, PSCI-SPC aims to reduce suicide among all veterans by expanding the reach of best practices for suicide prevention to veterans who receive myriad services in the community.27 Community organizations are defined here as organizations that may in some way serve, interact with, or work with veterans, and/or employ veterans. Examples include non-VHA health care systems, public services such as police and fire departments, nonprofit organizations, mental health clinics, and veterans’ courts. As veterans increasingly seek health care and other services within their communities, the success of suicide prevention will be influenced by the capability of non-VHA public and private organizations. Objective 1, therefore, seeks to develop a VHA-community collaborative that can be leveraged to improve systems of suicide prevention.
Current programs in the VHA have focused on implementation of suicide prevention awareness and prevention education campaigns instead of grassroots partnerships that are intended to be sustainable. Additionally, these programs typically lack the capacity and systems to sustain numerous meaningful community partnerships. Traditionally, community organizations have been hesitant to partner with government agencies, such as the VHA, due to histories of institutional mistrust and bureaucracy.28
The PSCI-SPC model for developing a VHA-community collaborative partnership draws from the tradition of community-based participatory research. The best community-based participatory research practices are to build on strengths and resources within the local community; develop collaborative, equitable partnerships that involve an empowering and power-sharing process; foster colearning, heuristics, and capacity building among partners; and focus on systems development using an iterative process. These practices also are consistent with the literature on learning collaboratives.29-31
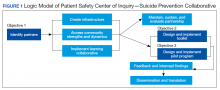
The premise for a learning collaborative is to bridge the gap between knowledge and practice in health care.31 Figure 1 depicts how this collaborative was developed, and how it supports Objectives 2 and 3. To achieve Objective 1, we developed a VHA-learning collaborative of 13 influential community partners in the Denver and Colorado Springs region of Colorado. The VHA team consists of a learning collaborative leader, a program manager, and a program support assistant. The principal investigator attends and contributes to all meetings. Learning collaborative partners include a university psychology clinic that focuses on veterans’ care, 3 veterans service organizations, a mental health private practice, a university school of nursing, a community mental health center, veterans’ courts, and 5 city departments.
These partners participated in qualitative interviews to identify where gaps and breakdowns were occurring. With this information, the PSCI-SPC team and VHA-learning collaborative held a kickoff event. At this meeting the team discussed the qualitative findings, provided veteran suicide prevention information, and basic information regarding suicide prevention program building and implementation science.
Throughout quarterly learning collaborative meetings and monthly facilitation calls, we have worked to develop a blueprint and an action plan for each partner to develop best practices for dissemination to aid in providing consistency in the standard of care. A postimplementation event will be held to identify successes and challenges encountered while operationalizing project action plans.
Currently, activities of the learning collaborative are making a large impact on the community. Not all collaborative members track information regarding their populations served, nor specific metrics on veterans encountered. Even so, of those who do capture metrics, suicide prevention program components implemented by the collaborative will impact more than 21,000 individuals and at least 2,500 known veterans. In addition, 52 new connections have been made between community organizations or between community organizations and the VHA, and > 300 individuals have been trained.The learning collaborative support team has assisted in the dissemination of a large resource list for veterans. As the learning collaborative is ongoing and we are working with organizations to improve their data collection and analytics, we expect these numbers to increase. We anticipate that the learning collaborative will develop a stronger suicide prevention safety net within the community. In addition, we expect increased referrals of at-risk veterans to the VHA and enhance the long-term continuity of care between community and VHA services.
Objective 2: Implementation Toolkit
The second PSCI-SPC objective is to develop a toolkit for the implementation of best practices within a VHA-community suicide prevention learning collaborative. Lessons from the development of a successful suicide prevention learning collaborative will be shared through an online guide that other VHA facilities can use to support similar collaborative efforts within their communities. The toolkit will be disseminated across the VHA to assist suicide prevention coordinators and other staff in developing a suicide prevention learning collaborative at their facilities.
PSCI-SPC uses the Zero Suicide framework and the VA/US Department of Defense (DoD) Clinical Practice Guideline for the Assessment and Management of Patients at Risk for Suicide as models for preventing suicide in veterans not enrolled in VHA care.11,32 This implementation toolkit focuses on how to implement suicide prevention best practices into organizations that serve veterans. This toolkit differs from clinical practice guidelines in that it focuses on implementation strategies to promote success and effectively address challenges.
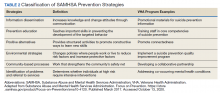
In order to provide a menu of available options for the learning collaborative and resulting toolkit, PSCI-SPC uses a logic model to compare the components of the VHA suicide prevention program, as well as other similar veteran and military suicide prevention programs.7,12,14,21,33,34 These programs are categorized into 2 types of prevention frameworks, the USI model as described above, and the SAMHSA Strategic Prevention Framework (Table 2).35 The SAMHSA framework was designed to promote mental health and prevent substance abuse, yet the derived classification is also applicable to suicide prevention programs.35 The results of the logic model comparison form the basis of the best practice interventions for the learning collaborative and initial toolkit. In addition to the best practice interventions, the toolkit consists of documents describing how to develop a veteran suicide prevention learning collaborative, as well as tools for learning collaborative members. Current tool development includes workbooks to guide collaborative members through the implementation process, guides for community organizations in implementing suicide prevention screening and risk assessment, a standard operating procedure for suicide prevention in a veterans court, and peer support training for veteran suicide prevention.
The methods to achieve Objective 2 include regular discussions with the VHA-learning collaborative on current best practices, identifying gaps and overlap of community programs. Successes and challenges of implementing suicide prevention best practices into learning collaborative organizations will be documented and incorporated into the toolkit. The learning collaborative will work iteratively as a team to improve the toolkit. Once complete, the toolkit will be disseminated to other VHA health care systems nationally, as well as to other state or regional partners that the learning collaborative identifies. A plan is under development for national suicide prevention entities to also disseminate the toolkit to lessen the burden of veteran suicide through their stakeholder base.
Objective 3: High-Risk Veterans Not Receiving VHA Care
Although veterans not receiving VHA care account for a number of veteran deaths by suicide, we are not aware of any current VHA programs that provide temporary psychotherapy and intensive case management to at-risk veterans ineligible for VHA care who are in need of immediate care while an appropriate permanent community placement is identified. In the current system, veterans in the community can present to VHA suicide prevention services through several different systems, including referrals to VHA and the Veterans Crisis Line (VCL). However, a portion of VCL calls are from veterans whose VHA eligibility is unknown or who are ineligible for services. If veterans are at imminent risk for suicide, emergency care is coordinated for them. However, if veterans are not at imminent suicide risk they are referred to the local suicide prevention coordinator and instructed to independently work toward determining their VHA eligibility.
It is currently unknown how many veterans follow through with these instructions. Nonetheless, if veterans are deemed eligible, they may present to VHA to obtain a same-day appointment. If not eligible, a suicide prevention coordinator may give them the phone number of a community referral. However, this practice is not standardized across VA medical centers, and the provided resources are up to the suicide prevention coordinator to research. Additionally, when a VHA suicide prevention coordinator leaves the position, knowledge of these community resources and rapport with community HCPs are often lost, leaving the next coordinator to develop these again, which reduces the efficiency and effectiveness of limited resources. It is also unknown how many veterans complete this contact and receive evidence-based treatment following referral. This is a complex system to navigate, particularly when at risk for suicide and in need of immediate but not emergency services.
Suicide prevention in such circumstances may be improved by adapting current suicide prevention practices, including evidence-based interventions, and the new VHA intensive case management program,11,36 within a Zero Suicide framework. PSCI-SPC has developed a brief intervention to transition ineligible veterans to permanent community treatment and provide them with additional resources to meet their varied needs. The brief 1 to 3 session intervention combines practices from brief cognitive behavioral therapy (BCBT) for suicide prevention, crisis response planning (CRP), and intensive case management within a Zero Suicide framework. Both the 2019 VA/DoD suicide prevention clinical practice guidelines and Zero Suicide recommend using cognitive behavioral therapy (CBT)-based interventions for suicide prevention.11,32 These interventions are packaged into a single intervention delivered by a PSCI-SPC therapist, typically a licensed clinical social worker, a licensed clinical psychologist, or an unlicensed psychologist under the supervision of a licensed clinical psychologist.
BCBT is one type of CBT that has shown initial efficacy in reducing suicide attempts.37 BCBT reduces the risk for suicide attempts both at the conclusion of treatment and at 24-month follow-up.37 BCBT is boiled down to its most essential components so it can be delivered in a distilled format. An essential element of BCBT that will remain is the CRP. A CRP11,37,38 entails collaboratively identifying effective, appropriate coping strategies and specific individuals to contact during a crisis. CRPs demonstrated efficacy as a stand-alone intervention to existing suicide prevention methods in a randomized clinical trial, such that individuals who received CRP had faster reductions in suicidal ideation and were 76% less likely to make a suicide attempt during the 6-month follow-up period.39 These results demonstrate that use of a CRP is connected to a decrease in suicidal behavior among suicidal patients.
The VHA has developed and is piloting a new initiative focused on restructuring its intensive case management services. RACETIME to Integrated Care (eg, Risk stratification, Assessment of complexity, Coordinator of lead assignment, Evaluate whole health needs, Trusting partnerships, Integrate care, Monitor progress, Experience of the veteran and employee) is a framework that assists VHA case managers in transitioning from a traditional case management mind-set to a more integrated and holistic method of care.36 RACETIME intensive case management practices will be incorporated into the intervention. However, RACETIME focuses on case management internally to the VHA. A modification for this treatment will be to focus on intensive case management from a mental health perspective and connecting to external community resources. Community referrals are mapped within a structured process and stored on a shared drive. This improves continuity between suicide prevention coordinators when they leave for a new position.
This intervention is conducted within a Zero Suicide framework. Pertinent to PSCI-SPC innovation to enhance care for non-VHA veterans is the care transitions element within the Zero Suicide framework, which has developed comprehensive suicide prevention guidance, including a pathway to care.32 This pathway refers a process to conduct follow-up supportive contacts that are tracked and recorded.
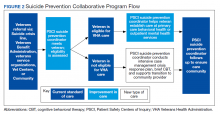
The PSCI-SPC pilot program incorporates the elements of CRP and brief CBT within a Zero Suicide framework. The PSCI-SPC team is developing and testing a protocol for providing brief treatment and community referrals to ineligible veterans that integrates these programming elements (Figure 2). A PSCI-SPC social worker will coordinate with the eligibility office to determine VHA eligibility. Ineligible veterans are referred to community partners and nonenrolled, eligible veterans are linked to VHA HCPs if they desire. These transitions will be coordinated, closely monitored, and verified.
Once the eligibility is determined, and the veteran’s preference is assessed, the team will perform a warm handoff to a VHA representative for enrollment into VHA care or to a community placement. We have sourced multiple community placements at varied payor levels. All veterans who are ineligible for care or who do not desire to be enrolled in VHA care will be provided the intervention package described above. After the veteran is placed in community care, PSCI-SPC team will follow up regularly with the veteran for 3 months to ensure continuity of care. If additional sessions are needed while the veteran needs a community placement, the PSCI team can accommodate this and will track the number of participants who needed additional sessions. If the veteran is deemed to be at imminent risk for suicide at any time during the pilot, he/she is transferred to emergency care. The veteran is allowed to participate once stabilized.
Findings from the pilot program will inform a manual intended for dissemination to patient safety and suicide prevention coordinators nationally across the VHA. The products from this objective will be integrated with the other objectives in training that will be provided on how to develop a local collaborative (Objective 1), disseminate the toolkit (Objective 2), and receive referrals into VHA or refer veterans to community clinical partners through the pilot program (Objective 3). Products developed and disseminated throughout PSCI-SPC aim to create momentum to reduce rates of suicide in veterans who are not connected to the VHA at the local community level.
Discussion
Improving suicide prevention for veterans who receive non-VHA health care is essential to significantly reduce veteran suicide rates. For the past decade, VHA suicide prevention initiatives have largely focused on veterans eligible for care, although the fastest increase in veteran suicide rates has occurred among veterans not connected to VHA services. Currently, if a veteran is deemed ineligible for care, it is up to the veteran to find other health care services in his or her community. There is not always a clear next step for the veteran to take, nor clear guidance provided to the VHA registration staff to assist with this care transition. This is particularly concerning for veterans at high risk for suicide as this could further thwart the veteran’s sense of belongingness and increase perceived burdensomeness, both suicide risk factors, and discourage them from attaining help.40 Overall, while the VHA has successfully implemented diverse suicide prevention initiatives and services, the need for continued system improvement focused on non-VHA veterans remains. PSCI-SPC was developed for this purpose.
By creating a collaborative that will connect VHA and community organizations, there will be better utilization of resources and more appropriate referrals throughout systems that interact with veterans. Sharing suicide prevention best practices between VHA and community partners is expected to increase access to mental health treatment to all veterans. Finally, by allowing best practices for suicide prevention in the VHA to serve as a guide in the development of best practices for suicide prevention between the VHA and the local health and behavioral health care community, PSCI-SPC will create a new suicide prevention intervention for veterans with mental health needs. Through these initiatives, PSCI-SPC will support providers’ and concerned citizens’ efforts to ensure that fewer veterans fall through the cracks of disjointed systems and will promote healthier communities where, regardless of VHA enrollment status, veterans receive suicide prevention care.
Conclusions
PSCI-SPC is a novel center for the innovation and dissemination of the nation’s best practices in suicide prevention for veterans who are ineligible for or otherwise not engaged in VHA services and who turn to their community for health care. PSCI-SPC not only seeks to create, develop, and measure various solutions to reduce suicide among veterans who receive non-VHA care, but also seeks to facilitate the overall quality of existing practices for suicide prevention and care coordination for enrolled veterans who use community resources. By bridging the gap between the VHA, civilian health care systems, and other community partners striving to prevent veteran suicides, we can create better access to care and a more seamless path of communication among these important entities that impact the lives of our veterans daily
1. US Department of Veterans Affairs. National strategy for preventing veteran suicide 2018-2028. https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf. Published September 2018. Accessed October 14, 2020.
2. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention. National veteran suicide prevention annual report. https://www.mentalhealth.va.gov/suicide_prevention/data.asp. Accessed October 14, 2020.
3. Centers for Disease Control and Prevention. Web-based injury statistics query and reporting system (WISQARS). 2014. https://www.cdc.gov/injury/wisqars/index.html. Updated July 1, 2020. Accessed October 14, 2020.
4. Lemle RB. Choice program expansion jeopardizes high-quality VHA mental health services. Fed Pract. 2018;35(3):18-24.
5. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention. VA national suicide data report 2005-2016. https://www.mentalhealth.va.gov/docs/data-sheets/OMHSP_National_Suicide_Data_Report_2005-2016_508.pdf. Published September 2018. Accessed October 14, 2020.
6. US Department of Veterans Affairs, Office of Suicide Prevention. VA national suicide data report 2005-2015. https://www.mentalhealth.va.gov/docs/data-sheets/2015/OMHSP_National_Suicide_Data_Report_2005-2015_06-14-18_508.pdf. Published June 2018. Accessed October 14, 2020.
7. US Department of Veterans Affairs. National strategy for preventing veteran suicide 2018-2028. https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf. Published 2018. Accessed October 30, 2020.
8. Gordon RS. An operational classification of disease prevention. Public Health Rep. 1983;98(2):107-109.
9. National Research Council and Institute of Medicine. O’Connell ME, Boat T, Warner KE, eds. Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. Washington, DC: National Academies Press; 2009.
10. US Department of Health and Human Services, National Institute on Drug Abuse, Office of Science Policy and Communications. Drug Abuse Prevention: What Works. Rockville, MD: National Institutes of Health; 1997.
11. US Department of Veterans Affairs, US Department of Defense. VA/DoD clinical practice guideline for the assessment and management of patients at risk for suicide. https://www.healthquality.va.gov/guidelines/MH/srb. Published 2019. Updated July 30, 2020. Accessed October 14, 2020.
12. US Department of Veterans Affairs. Veterans Access, Choice and Accountability Act of 2014. https://www.govinfo.gov/content/pkg/PLAW-113publ146/pdf/PLAW-113publ146.pdf. Accessed October 14, 2020.
13. US Department of Veterans Affairs. Strategic Health Care. VA MISSION Act: Extension of the VA choice program. https://strategichealthcare.net/wp-content/uploads/2018/05/052718-VA-MISSION-Act-Summary.pdf. Accessed October 14, 2020.
14. US Congress. H.R.5674—VA MISSION Act of 2018. https://www.congress.gov/bill/115th-congress/house-bill/5674. Accessed October 15, 2020.
15. Grumet JG, Hogan MF, Chu A, Covington DW, Johnson KE. Compliance standards pave the way for reducing suicide in health care systems. J Health Care Compliance. 2019;17-26.
16. Hillestad R, Bigelow J, Bower A, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff (Millwood). 2005;24(5):1103-1117. doi:10.1377/hlthaff.24.5.110
17. Porter ME, Pabo EA, Lee TH. Redesigning primary care: a strategic vision to improve value by organizing around patients’ needs. Health Aff (Millwood). 2013;32(3):516-525. doi:10.1377/hlthaff.2012.0961
18. Nevedal AL, Wagner TH, Ellerbe LS, Asch SM, Koenig CJ. A qualitative study of primary care providers’ experiences with the Veterans Choice Program. J Gen Intern Med. 2019;34:598-603. doi:10.1007/s11606-018-4810-2
19. Tanielian T, Farris C, Epley C, et al. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf. Published 2014. Accessed October 15, 2020.
20. White House. Executive Order 13861: President’s roadmap to empower veterans and end the national tragedy of suicide (PREVENTS). https://www.va.gov/PREVENTS/docs/PRE-007-The-PREVENTS-Roadmap-1-2_508.pdf. Published June 17, 2020. Accessed October 15, 2020.
21. US Department of Veterans Affairs, Office of the Under Secretary for Health. Memorandum. VA continues community suicide prevention challenge at another mayor’s challenge policy academy. https://www.blogs.va.gov/VAntage/58468/va-continues-community-suicide-prevention-challenge-another-mayors-challenge-policy-academy. Published April 4, 2019. Accessed October 15, 2020.
22. US Department of Veterans Affairs, Veterans Health Administration (VHA) Veterans Health Administration (VHA) Fiscal Year (FY) 2018-2019 Operational Plan. www.navao.org/wp-content/uploads/2018/06/USH-Memo-10-2018-03-VHA_FY_2018-2019_Operational_Plan-4-19-18.pdf. Published April 19, 2018. Accessed October 15, 2020.
23. US Department of Veterans Affairs. VA, Health and Human Services announce governor’s challenge to prevent suicide. https://www.blogs.va.gov/VAntage/55707/va-health-human-services-announce-governors-challenge-prevent-suicide. Published January 17, 2019. Accessed October 15, 2020.
24. VA’s suicide prevention campaign “Be There’’ kicks off in Times Square. https://www.blogs.va.gov/VAntage/57272/vas-suicide-prevention-campaign-kicks-off-times-square. Published March 6, 2019. Accessed October 15, 2020.
25. US Department of Veterans Affairs, Office of Public Affairs Media Relations. Emergent mental health care for former service members. https://www.mentalhealth.va.gov/docs/Fact_Sheet-Emergent_Mental_Health_Care_Former_Service_Members.pdf. Published 2017. Accessed October 15, 2020.
26. US Department of Veterans Affairs. VA secretary formalizes expansion of emergency mental health care to former service members with other-than-honorable discharges. https://www.blogs.va.gov/VAntage/39092/va-secretary-formalizes-expansion-emergency-mental-health-care-former-service-members-honorable-discharges. Published June 27, 2017. Accessed October 15, 2020.
27. Shane L. New veteran suicide numbers raise concerns among experts hoping for positive news. Military Times. https://www.militarytimes.com/news/pentagon-congress/2019/10/09/new-veteran-suicide-numbers-raise-concerns-among-experts-hoping-for-positive-news. Published October 9, 2019. Accessed October 15, 2020.
28. US Department of Veterans Affairs. Department of Veterans Affairs FY 2018-2024 Strategic Plan. https://www.va.gov/oei/docs/VA2018-2024strategicPlan.pdf. Updated May 31, 2019. Accessed October 15, 2020.
29. Komaie G, Goodman M, McCall A, et al. Training community members in public health research: development and implementation of a community participatory research pilot project. Health Equity. 2018;2(1):282-287. doi:10.1089/heq.2018.0043
30. Wang KH, Ray NJ, Berg DN, et al. Using community-based participatory research and organizational diagnosis to characterize relationships between community leaders and academic researchers. Prev Med Reports. 2017;7:180-186. doi:10.1016/j.pmedr.2017.06.007
31. Institute for Healthcare Improvement. The breakthrough series: IHI’s collaborative model for achieving breakthrough improvement. http://www.ihi.org/resources/Pages/IHIWhitePapers/TheBreakthroughSeriesIHIsCollaborativeModelforAchievingBreakthroughImprovement.aspx. Published 2003. Accessed October 15, 2020.
32. Zero Suicide in Health and Behavioral Health Care Institute. Zero suicide toolkit. https://zerosuicide.sprc.org/toolkit. Accessed October 15, 2020.

33. Preventing suicide: a technical package of policy, programs, and practices. https://www.cdc.gov/violenceprevention/pdf/suicideTechnicalPackage.pdf. Published 2017. Accessed October 30, 2020.
34. US Department of Veterans Affairs. VA Office of Mental Health and Suicide Prevention guidebook. https://www.mentalhealth.va.gov/docs/VA-Office-of-Mental-Health-and-Suicide-Prevention-Guidebook-June-2018-FINAL-508.pdf. Published June 2018. Accessed October 15, 2020.
35. US Department of Health and Human Services, Substance Abuse and Mental Health Services, Administration Center for Substance Abuse Prevention. Focus on prevention: strategies and programs to prevent substance abuse. HHS Publication No. (SMA) 10-4120. https://helpandhopewv.org/docs/Focus%20on%20Prevention.pdf. Revised 2017. Accessed October 15, 2020.
36. Misiti R, Risinger A. RACETIME: an organizational care coordination approach to improving patient outcomes in a complex healthcare setting. Presentation at the Military Social Work & Behavioral Health Conference Austin, Texas. July 23, 2020. https://sites.utexas.edu/military-social-work-conference/misiti-risinger. Accessed October 23, 2020.
37. Rudd MD, Bryan CJ, Wertenberger EG, et al. Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: results of a randomized clinical trial with 2-year follow-up. Am J Psychiatry. 2015;172(5):441-449. doi:10.1176/appi.ajp.2014.14070843
38. Rudd MD, Mandrusiak M, Joiner TE Jr. The case against no-suicide contracts: The commitment to treatment statement as a practice alternative. Clin Psychol. 2006;62(2):243-251.
39. Bryan CJ, Mintz J, Clemans TA, et al. Effect of crisis response planning vs. contracts for safety on suicide risk in US Army soldiers: a randomized clinical trial. J Affect Disord. 2017;212:64-72. doi:10.1016/j.jad.2017.01.028
40. Joiner TE. Why People Die by Suicide. Cambridge, MA: First Harvard University Press; 2005:27.
41. Office of the Under Secretary of Defense for Personnel and Readiness. DoD Instruction 6490.16: Defense suicide prevention program. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/649016p.pdf?ver=2020-09-11-122632-850. Published November 6, 2017. Updated September 11, 2020. Accessed October 14, 2020.
42. Zero Suicide in Health and Behavioral Health Care Institute. Engage: engaging patients. http://zerosuicide.edc.org/toolkit/engage#quicktabs-engage=0. Accessed October 14, 2020.
43. Stone D, Holland K, Bartholow B, Crosby A, Davis S, Wilkins N. Preventing Suicide: A technical package of policy, programs, and practices. https://www.cdc.gov/violenceprevention/pdf/suicidetechnicalpackage.pdf. Published 2017. Accessed October 14, 2020.
44. Mills PD, Watts BV, Miller S, et al. A checklist to identify inpatient suicide hazards in veterans affairs hospitals. Jt Comm J Qual Patient Saf. 2010;36(2):87-93. doi:10.1016/s1553-7250(10)36015-6
45. US Department of Veterans Affairs, Office of Research and Development. Crisis prevention: study evaluates VA program that identifies vets at highest risk for suicide. https://www.research.va.gov/currents/0918-Study-evaluates-VA-program-that-identifies-Vets-at-highest-risk-for-suicide.cfm. Updated September, 20, 2018. Accessed October 14, 2020.
46. Zero Suicide in Health and Behavioral Health Care Institute. Engage: active engagement for safer suicide care--reducing access to lethal means. http://zerosuicide.edc.org/toolkit/engage#quicktabs-engage=1. Published 2017. Accessed October 14, 2020.
47. Zero Suicide in Health and Behavioral Health Care Institute. Train: training for all. http://zerosuicide.sprc.org/toolkit/train. Accessed October 14, 2020.
48. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention (OMHSP). Facts about veteran suicide. https://www.mentalhealth.va.gov/docs/FINAL_VA_OMHSP_Suicide_Prevention_Fact_Sheet_508.pdf. Published June 2018. Accessed October 14, 2020.
49. Zero Suicide in Health and Behavioral Health Care Institute. Treat: direct treatment. http://zerosuicide.edc.org/toolkit/treat. Accessed October 14, 2020.
50. Office of the Under Secretary of Defense for Personnel and Readiness. DoD Instruction 6490.04: Mental health evaluations of members of the military services. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/649004p.pdf. Published March 4, 2013. Updated April 22, 2020. Accessed October 14, 2020.
51. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention Frequently asked questions: VA National Suicide Data Report. https://www.mentalhealth.va.gov/docs/data-sheets/2015_Data_Release_FAQs_508.pdf. Published September 2018. Updated June 22, 2018. Accessed October 14, 2020.
52. Zero Suicide in Health and Behavioral Health Care Institute. ZERO Suicide engage: active engagement for safer suicide care safety planning. http://zerosuicide.edc.org/toolkit/engage#quicktabs-engage=1. Accessed October 14, 2020.
Since 2008, suicide has ranked as the tenth leading cause of death for all ages in the US, with rates of suicide continuing to rise.1-3 Suicide is even more urgent to address in veteran populations. The age- and sex-adjusted suicide rate in 2017 was more than 1.5 times greater for veterans than it was for nonveteran adults.2 Of importance, rates of suicide are increasing at a faster rate in veterans who are not connected to Veterans Health Administration (VHA) care.4,5 These at-risk veterans include individuals who are eligible for VHA care yet have not had a VHA appointment within the year before death; veterans who may be ineligible to receive VHA care due to complex rules set by legislation; and veterans who are eligible but not enrolled in VHA care. Notably, between 2005 and 2016, the number of veterans not enrolled in VHA care rose more quickly than did the number of veterans enrolled in VHA care.5,6 Thus, to impact the high veteran suicide rates, an emergent challenge for VHA is to prevent suicide among unenrolled veterans and veterans receiving community care, while continuing to increase access to mental health services for veterans enrolled in VHA health care.
In response to the high rates of veteran suicide deaths, the US Department of Veterans Affairs (VA) has developed a broad, multicomponent suicide prevention program that is unparalleled in private US health care systems.4,7 Suicide prevention efforts are led and implemented by both the VHA National Center for Patient Safety and the VHA Office of Mental Health and Suicide Prevention. Program components are numerous and multifaceted, falling within the broad promotion and prevention strategies outlined by the National Academy of Medicine (NAM).1,8-11 The NAM continuum of prevention model encompassing multiple strategies is also referred to as the Universal, Selective, Indicated (USI) Model.7,8,10 The VHA suicide prevention program contains a wide spread of program components, making it both comprehensive and innovative (Table 1).
Although significant momentum and progress has been made within the VHA, policy set by legislation has historically limited access to VHA health care services to VHA-eligible veterans. This is particularly concerning given the rising suicide rates among veterans not engaged in VHA care.2 Adding to this complexity, recent legislation has increased veterans’ access to non-VHA health care, in addition to their existing access through Medicare, Medicaid, and other health care programs.12-14 Best practices for suicide prevention are not often implemented in the private sector; thus, these systems are ill prepared to adequately meet the suicide prevention care needs of veterans.4,15-18 Furthermore, VHA and non-VHA services generally are not well coordinated, and private sector health care providers (HCPs) are not required to complete a commensurate level of suicide prevention training as are VHA HCPs.16-18 Most non-VHA HCPs do not receive military cultural competence training.19 These issues create a significant gap in suicide prevention services and may contribute to the increases in suicide rates in veterans who do not receive VHA care. Thus, changes in policy to increase access through private sector care may have paradoxical effects on veteran suicide deaths. To impact the veteran suicide rate, VHA must develop and disseminate best practices for veterans who use non-VHA services.
A Roadmap to Suicide Prevention
There is significant momentum at the federal level regarding this issue. The President’s Roadmap to Empower Veterans and End the National Tragedy of Suicide (Executive Order 13,861) directs the VHA to work closely with community organizations to improve veteran suicide prevention.20 The VHA and partners, such as the Substance Abuse and Mental Health Services Administration (SAMHSA), are bridging this gap with collaborative efforts that increase suicide prevention resources for veterans living in the community through programs such as the Governor’s Challenges to Prevent Suicide Among Service Members, Veterans, and their Families. These programs intend to empower communities to develop statewide, strategic action plans to prevent veteran suicide.7,21-24
In addition to partnerships, VHA has built other aspects of outreach and intervention into its programming. A key VHA initiative is to “know all veterans” by committing to identifying and reaching out to all veterans who may be at risk for suicide.22 The VHA has committed to offering “emergency stabilization care for former service members who present at the facility with an emergent mental health need” regardless of eligibility.25 The intent is to provide temporary emergent mental health care to veterans who are otherwise ineligible for care, such as those who were discharged under other-than-honorable conditions while the VHA determines eligibility status.26 However, veterans must meet certain criteria, and there is a limit on services.
Although services are being expanded to reach veterans who do not access VHA health care, how to best implement these new directives with regard to suicide prevention is unclear. Strategic development and innovations to expand suicide prevention care to veterans outside the current reach of VHA are desperately needed.
Program Overview
VHA Patient Safety Center of Inquiry-Suicide Prevention Collaborative (PSCI-SPC), funded by the VHA National Center for Patient Safety, aims to help fill the gap in community-based suicide prevention for veterans. PSCI-SPC is located within the VHA Rocky Mountain Mental Illness Research, Education, and Clinical Center in Aurora, Colorado. The overarching mission of PSCI-SPC is to develop, implement, and evaluate practical solutions to reduce suicide among veterans not receiving VHA care. PSCI-SPC serves as a national clinical innovation and dissemination center for best practices in suicide prevention for organizations that serve veterans who receive care in the community. PSCI-SPC creates products to support dissemination of these practices to other VAMCs and works to ensure these programs are sustainable. PSCI-SPC focuses on 3 primary objectives. All PSCI-SPC projects are currently underway.
Objective 1: Growing a Community Learning Collaborative
Acknowledging that nearly two-thirds of veterans who die by suicide do not use VHA services, PSCI-SPC aims to reduce suicide among all veterans by expanding the reach of best practices for suicide prevention to veterans who receive myriad services in the community.27 Community organizations are defined here as organizations that may in some way serve, interact with, or work with veterans, and/or employ veterans. Examples include non-VHA health care systems, public services such as police and fire departments, nonprofit organizations, mental health clinics, and veterans’ courts. As veterans increasingly seek health care and other services within their communities, the success of suicide prevention will be influenced by the capability of non-VHA public and private organizations. Objective 1, therefore, seeks to develop a VHA-community collaborative that can be leveraged to improve systems of suicide prevention.
Current programs in the VHA have focused on implementation of suicide prevention awareness and prevention education campaigns instead of grassroots partnerships that are intended to be sustainable. Additionally, these programs typically lack the capacity and systems to sustain numerous meaningful community partnerships. Traditionally, community organizations have been hesitant to partner with government agencies, such as the VHA, due to histories of institutional mistrust and bureaucracy.28
The PSCI-SPC model for developing a VHA-community collaborative partnership draws from the tradition of community-based participatory research. The best community-based participatory research practices are to build on strengths and resources within the local community; develop collaborative, equitable partnerships that involve an empowering and power-sharing process; foster colearning, heuristics, and capacity building among partners; and focus on systems development using an iterative process. These practices also are consistent with the literature on learning collaboratives.29-31
The premise for a learning collaborative is to bridge the gap between knowledge and practice in health care.31 Figure 1 depicts how this collaborative was developed, and how it supports Objectives 2 and 3. To achieve Objective 1, we developed a VHA-learning collaborative of 13 influential community partners in the Denver and Colorado Springs region of Colorado. The VHA team consists of a learning collaborative leader, a program manager, and a program support assistant. The principal investigator attends and contributes to all meetings. Learning collaborative partners include a university psychology clinic that focuses on veterans’ care, 3 veterans service organizations, a mental health private practice, a university school of nursing, a community mental health center, veterans’ courts, and 5 city departments.
These partners participated in qualitative interviews to identify where gaps and breakdowns were occurring. With this information, the PSCI-SPC team and VHA-learning collaborative held a kickoff event. At this meeting the team discussed the qualitative findings, provided veteran suicide prevention information, and basic information regarding suicide prevention program building and implementation science.
Throughout quarterly learning collaborative meetings and monthly facilitation calls, we have worked to develop a blueprint and an action plan for each partner to develop best practices for dissemination to aid in providing consistency in the standard of care. A postimplementation event will be held to identify successes and challenges encountered while operationalizing project action plans.
Currently, activities of the learning collaborative are making a large impact on the community. Not all collaborative members track information regarding their populations served, nor specific metrics on veterans encountered. Even so, of those who do capture metrics, suicide prevention program components implemented by the collaborative will impact more than 21,000 individuals and at least 2,500 known veterans. In addition, 52 new connections have been made between community organizations or between community organizations and the VHA, and > 300 individuals have been trained.The learning collaborative support team has assisted in the dissemination of a large resource list for veterans. As the learning collaborative is ongoing and we are working with organizations to improve their data collection and analytics, we expect these numbers to increase. We anticipate that the learning collaborative will develop a stronger suicide prevention safety net within the community. In addition, we expect increased referrals of at-risk veterans to the VHA and enhance the long-term continuity of care between community and VHA services.
Objective 2: Implementation Toolkit
The second PSCI-SPC objective is to develop a toolkit for the implementation of best practices within a VHA-community suicide prevention learning collaborative. Lessons from the development of a successful suicide prevention learning collaborative will be shared through an online guide that other VHA facilities can use to support similar collaborative efforts within their communities. The toolkit will be disseminated across the VHA to assist suicide prevention coordinators and other staff in developing a suicide prevention learning collaborative at their facilities.
PSCI-SPC uses the Zero Suicide framework and the VA/US Department of Defense (DoD) Clinical Practice Guideline for the Assessment and Management of Patients at Risk for Suicide as models for preventing suicide in veterans not enrolled in VHA care.11,32 This implementation toolkit focuses on how to implement suicide prevention best practices into organizations that serve veterans. This toolkit differs from clinical practice guidelines in that it focuses on implementation strategies to promote success and effectively address challenges.
In order to provide a menu of available options for the learning collaborative and resulting toolkit, PSCI-SPC uses a logic model to compare the components of the VHA suicide prevention program, as well as other similar veteran and military suicide prevention programs.7,12,14,21,33,34 These programs are categorized into 2 types of prevention frameworks, the USI model as described above, and the SAMHSA Strategic Prevention Framework (Table 2).35 The SAMHSA framework was designed to promote mental health and prevent substance abuse, yet the derived classification is also applicable to suicide prevention programs.35 The results of the logic model comparison form the basis of the best practice interventions for the learning collaborative and initial toolkit. In addition to the best practice interventions, the toolkit consists of documents describing how to develop a veteran suicide prevention learning collaborative, as well as tools for learning collaborative members. Current tool development includes workbooks to guide collaborative members through the implementation process, guides for community organizations in implementing suicide prevention screening and risk assessment, a standard operating procedure for suicide prevention in a veterans court, and peer support training for veteran suicide prevention.
The methods to achieve Objective 2 include regular discussions with the VHA-learning collaborative on current best practices, identifying gaps and overlap of community programs. Successes and challenges of implementing suicide prevention best practices into learning collaborative organizations will be documented and incorporated into the toolkit. The learning collaborative will work iteratively as a team to improve the toolkit. Once complete, the toolkit will be disseminated to other VHA health care systems nationally, as well as to other state or regional partners that the learning collaborative identifies. A plan is under development for national suicide prevention entities to also disseminate the toolkit to lessen the burden of veteran suicide through their stakeholder base.
Objective 3: High-Risk Veterans Not Receiving VHA Care
Although veterans not receiving VHA care account for a number of veteran deaths by suicide, we are not aware of any current VHA programs that provide temporary psychotherapy and intensive case management to at-risk veterans ineligible for VHA care who are in need of immediate care while an appropriate permanent community placement is identified. In the current system, veterans in the community can present to VHA suicide prevention services through several different systems, including referrals to VHA and the Veterans Crisis Line (VCL). However, a portion of VCL calls are from veterans whose VHA eligibility is unknown or who are ineligible for services. If veterans are at imminent risk for suicide, emergency care is coordinated for them. However, if veterans are not at imminent suicide risk they are referred to the local suicide prevention coordinator and instructed to independently work toward determining their VHA eligibility.
It is currently unknown how many veterans follow through with these instructions. Nonetheless, if veterans are deemed eligible, they may present to VHA to obtain a same-day appointment. If not eligible, a suicide prevention coordinator may give them the phone number of a community referral. However, this practice is not standardized across VA medical centers, and the provided resources are up to the suicide prevention coordinator to research. Additionally, when a VHA suicide prevention coordinator leaves the position, knowledge of these community resources and rapport with community HCPs are often lost, leaving the next coordinator to develop these again, which reduces the efficiency and effectiveness of limited resources. It is also unknown how many veterans complete this contact and receive evidence-based treatment following referral. This is a complex system to navigate, particularly when at risk for suicide and in need of immediate but not emergency services.
Suicide prevention in such circumstances may be improved by adapting current suicide prevention practices, including evidence-based interventions, and the new VHA intensive case management program,11,36 within a Zero Suicide framework. PSCI-SPC has developed a brief intervention to transition ineligible veterans to permanent community treatment and provide them with additional resources to meet their varied needs. The brief 1 to 3 session intervention combines practices from brief cognitive behavioral therapy (BCBT) for suicide prevention, crisis response planning (CRP), and intensive case management within a Zero Suicide framework. Both the 2019 VA/DoD suicide prevention clinical practice guidelines and Zero Suicide recommend using cognitive behavioral therapy (CBT)-based interventions for suicide prevention.11,32 These interventions are packaged into a single intervention delivered by a PSCI-SPC therapist, typically a licensed clinical social worker, a licensed clinical psychologist, or an unlicensed psychologist under the supervision of a licensed clinical psychologist.
BCBT is one type of CBT that has shown initial efficacy in reducing suicide attempts.37 BCBT reduces the risk for suicide attempts both at the conclusion of treatment and at 24-month follow-up.37 BCBT is boiled down to its most essential components so it can be delivered in a distilled format. An essential element of BCBT that will remain is the CRP. A CRP11,37,38 entails collaboratively identifying effective, appropriate coping strategies and specific individuals to contact during a crisis. CRPs demonstrated efficacy as a stand-alone intervention to existing suicide prevention methods in a randomized clinical trial, such that individuals who received CRP had faster reductions in suicidal ideation and were 76% less likely to make a suicide attempt during the 6-month follow-up period.39 These results demonstrate that use of a CRP is connected to a decrease in suicidal behavior among suicidal patients.
The VHA has developed and is piloting a new initiative focused on restructuring its intensive case management services. RACETIME to Integrated Care (eg, Risk stratification, Assessment of complexity, Coordinator of lead assignment, Evaluate whole health needs, Trusting partnerships, Integrate care, Monitor progress, Experience of the veteran and employee) is a framework that assists VHA case managers in transitioning from a traditional case management mind-set to a more integrated and holistic method of care.36 RACETIME intensive case management practices will be incorporated into the intervention. However, RACETIME focuses on case management internally to the VHA. A modification for this treatment will be to focus on intensive case management from a mental health perspective and connecting to external community resources. Community referrals are mapped within a structured process and stored on a shared drive. This improves continuity between suicide prevention coordinators when they leave for a new position.
This intervention is conducted within a Zero Suicide framework. Pertinent to PSCI-SPC innovation to enhance care for non-VHA veterans is the care transitions element within the Zero Suicide framework, which has developed comprehensive suicide prevention guidance, including a pathway to care.32 This pathway refers a process to conduct follow-up supportive contacts that are tracked and recorded.
The PSCI-SPC pilot program incorporates the elements of CRP and brief CBT within a Zero Suicide framework. The PSCI-SPC team is developing and testing a protocol for providing brief treatment and community referrals to ineligible veterans that integrates these programming elements (Figure 2). A PSCI-SPC social worker will coordinate with the eligibility office to determine VHA eligibility. Ineligible veterans are referred to community partners and nonenrolled, eligible veterans are linked to VHA HCPs if they desire. These transitions will be coordinated, closely monitored, and verified.
Once the eligibility is determined, and the veteran’s preference is assessed, the team will perform a warm handoff to a VHA representative for enrollment into VHA care or to a community placement. We have sourced multiple community placements at varied payor levels. All veterans who are ineligible for care or who do not desire to be enrolled in VHA care will be provided the intervention package described above. After the veteran is placed in community care, PSCI-SPC team will follow up regularly with the veteran for 3 months to ensure continuity of care. If additional sessions are needed while the veteran needs a community placement, the PSCI team can accommodate this and will track the number of participants who needed additional sessions. If the veteran is deemed to be at imminent risk for suicide at any time during the pilot, he/she is transferred to emergency care. The veteran is allowed to participate once stabilized.
Findings from the pilot program will inform a manual intended for dissemination to patient safety and suicide prevention coordinators nationally across the VHA. The products from this objective will be integrated with the other objectives in training that will be provided on how to develop a local collaborative (Objective 1), disseminate the toolkit (Objective 2), and receive referrals into VHA or refer veterans to community clinical partners through the pilot program (Objective 3). Products developed and disseminated throughout PSCI-SPC aim to create momentum to reduce rates of suicide in veterans who are not connected to the VHA at the local community level.
Discussion
Improving suicide prevention for veterans who receive non-VHA health care is essential to significantly reduce veteran suicide rates. For the past decade, VHA suicide prevention initiatives have largely focused on veterans eligible for care, although the fastest increase in veteran suicide rates has occurred among veterans not connected to VHA services. Currently, if a veteran is deemed ineligible for care, it is up to the veteran to find other health care services in his or her community. There is not always a clear next step for the veteran to take, nor clear guidance provided to the VHA registration staff to assist with this care transition. This is particularly concerning for veterans at high risk for suicide as this could further thwart the veteran’s sense of belongingness and increase perceived burdensomeness, both suicide risk factors, and discourage them from attaining help.40 Overall, while the VHA has successfully implemented diverse suicide prevention initiatives and services, the need for continued system improvement focused on non-VHA veterans remains. PSCI-SPC was developed for this purpose.
By creating a collaborative that will connect VHA and community organizations, there will be better utilization of resources and more appropriate referrals throughout systems that interact with veterans. Sharing suicide prevention best practices between VHA and community partners is expected to increase access to mental health treatment to all veterans. Finally, by allowing best practices for suicide prevention in the VHA to serve as a guide in the development of best practices for suicide prevention between the VHA and the local health and behavioral health care community, PSCI-SPC will create a new suicide prevention intervention for veterans with mental health needs. Through these initiatives, PSCI-SPC will support providers’ and concerned citizens’ efforts to ensure that fewer veterans fall through the cracks of disjointed systems and will promote healthier communities where, regardless of VHA enrollment status, veterans receive suicide prevention care.
Conclusions
PSCI-SPC is a novel center for the innovation and dissemination of the nation’s best practices in suicide prevention for veterans who are ineligible for or otherwise not engaged in VHA services and who turn to their community for health care. PSCI-SPC not only seeks to create, develop, and measure various solutions to reduce suicide among veterans who receive non-VHA care, but also seeks to facilitate the overall quality of existing practices for suicide prevention and care coordination for enrolled veterans who use community resources. By bridging the gap between the VHA, civilian health care systems, and other community partners striving to prevent veteran suicides, we can create better access to care and a more seamless path of communication among these important entities that impact the lives of our veterans daily
Since 2008, suicide has ranked as the tenth leading cause of death for all ages in the US, with rates of suicide continuing to rise.1-3 Suicide is even more urgent to address in veteran populations. The age- and sex-adjusted suicide rate in 2017 was more than 1.5 times greater for veterans than it was for nonveteran adults.2 Of importance, rates of suicide are increasing at a faster rate in veterans who are not connected to Veterans Health Administration (VHA) care.4,5 These at-risk veterans include individuals who are eligible for VHA care yet have not had a VHA appointment within the year before death; veterans who may be ineligible to receive VHA care due to complex rules set by legislation; and veterans who are eligible but not enrolled in VHA care. Notably, between 2005 and 2016, the number of veterans not enrolled in VHA care rose more quickly than did the number of veterans enrolled in VHA care.5,6 Thus, to impact the high veteran suicide rates, an emergent challenge for VHA is to prevent suicide among unenrolled veterans and veterans receiving community care, while continuing to increase access to mental health services for veterans enrolled in VHA health care.
In response to the high rates of veteran suicide deaths, the US Department of Veterans Affairs (VA) has developed a broad, multicomponent suicide prevention program that is unparalleled in private US health care systems.4,7 Suicide prevention efforts are led and implemented by both the VHA National Center for Patient Safety and the VHA Office of Mental Health and Suicide Prevention. Program components are numerous and multifaceted, falling within the broad promotion and prevention strategies outlined by the National Academy of Medicine (NAM).1,8-11 The NAM continuum of prevention model encompassing multiple strategies is also referred to as the Universal, Selective, Indicated (USI) Model.7,8,10 The VHA suicide prevention program contains a wide spread of program components, making it both comprehensive and innovative (Table 1).
Although significant momentum and progress has been made within the VHA, policy set by legislation has historically limited access to VHA health care services to VHA-eligible veterans. This is particularly concerning given the rising suicide rates among veterans not engaged in VHA care.2 Adding to this complexity, recent legislation has increased veterans’ access to non-VHA health care, in addition to their existing access through Medicare, Medicaid, and other health care programs.12-14 Best practices for suicide prevention are not often implemented in the private sector; thus, these systems are ill prepared to adequately meet the suicide prevention care needs of veterans.4,15-18 Furthermore, VHA and non-VHA services generally are not well coordinated, and private sector health care providers (HCPs) are not required to complete a commensurate level of suicide prevention training as are VHA HCPs.16-18 Most non-VHA HCPs do not receive military cultural competence training.19 These issues create a significant gap in suicide prevention services and may contribute to the increases in suicide rates in veterans who do not receive VHA care. Thus, changes in policy to increase access through private sector care may have paradoxical effects on veteran suicide deaths. To impact the veteran suicide rate, VHA must develop and disseminate best practices for veterans who use non-VHA services.
A Roadmap to Suicide Prevention
There is significant momentum at the federal level regarding this issue. The President’s Roadmap to Empower Veterans and End the National Tragedy of Suicide (Executive Order 13,861) directs the VHA to work closely with community organizations to improve veteran suicide prevention.20 The VHA and partners, such as the Substance Abuse and Mental Health Services Administration (SAMHSA), are bridging this gap with collaborative efforts that increase suicide prevention resources for veterans living in the community through programs such as the Governor’s Challenges to Prevent Suicide Among Service Members, Veterans, and their Families. These programs intend to empower communities to develop statewide, strategic action plans to prevent veteran suicide.7,21-24
In addition to partnerships, VHA has built other aspects of outreach and intervention into its programming. A key VHA initiative is to “know all veterans” by committing to identifying and reaching out to all veterans who may be at risk for suicide.22 The VHA has committed to offering “emergency stabilization care for former service members who present at the facility with an emergent mental health need” regardless of eligibility.25 The intent is to provide temporary emergent mental health care to veterans who are otherwise ineligible for care, such as those who were discharged under other-than-honorable conditions while the VHA determines eligibility status.26 However, veterans must meet certain criteria, and there is a limit on services.
Although services are being expanded to reach veterans who do not access VHA health care, how to best implement these new directives with regard to suicide prevention is unclear. Strategic development and innovations to expand suicide prevention care to veterans outside the current reach of VHA are desperately needed.
Program Overview
VHA Patient Safety Center of Inquiry-Suicide Prevention Collaborative (PSCI-SPC), funded by the VHA National Center for Patient Safety, aims to help fill the gap in community-based suicide prevention for veterans. PSCI-SPC is located within the VHA Rocky Mountain Mental Illness Research, Education, and Clinical Center in Aurora, Colorado. The overarching mission of PSCI-SPC is to develop, implement, and evaluate practical solutions to reduce suicide among veterans not receiving VHA care. PSCI-SPC serves as a national clinical innovation and dissemination center for best practices in suicide prevention for organizations that serve veterans who receive care in the community. PSCI-SPC creates products to support dissemination of these practices to other VAMCs and works to ensure these programs are sustainable. PSCI-SPC focuses on 3 primary objectives. All PSCI-SPC projects are currently underway.
Objective 1: Growing a Community Learning Collaborative
Acknowledging that nearly two-thirds of veterans who die by suicide do not use VHA services, PSCI-SPC aims to reduce suicide among all veterans by expanding the reach of best practices for suicide prevention to veterans who receive myriad services in the community.27 Community organizations are defined here as organizations that may in some way serve, interact with, or work with veterans, and/or employ veterans. Examples include non-VHA health care systems, public services such as police and fire departments, nonprofit organizations, mental health clinics, and veterans’ courts. As veterans increasingly seek health care and other services within their communities, the success of suicide prevention will be influenced by the capability of non-VHA public and private organizations. Objective 1, therefore, seeks to develop a VHA-community collaborative that can be leveraged to improve systems of suicide prevention.
Current programs in the VHA have focused on implementation of suicide prevention awareness and prevention education campaigns instead of grassroots partnerships that are intended to be sustainable. Additionally, these programs typically lack the capacity and systems to sustain numerous meaningful community partnerships. Traditionally, community organizations have been hesitant to partner with government agencies, such as the VHA, due to histories of institutional mistrust and bureaucracy.28
The PSCI-SPC model for developing a VHA-community collaborative partnership draws from the tradition of community-based participatory research. The best community-based participatory research practices are to build on strengths and resources within the local community; develop collaborative, equitable partnerships that involve an empowering and power-sharing process; foster colearning, heuristics, and capacity building among partners; and focus on systems development using an iterative process. These practices also are consistent with the literature on learning collaboratives.29-31
The premise for a learning collaborative is to bridge the gap between knowledge and practice in health care.31 Figure 1 depicts how this collaborative was developed, and how it supports Objectives 2 and 3. To achieve Objective 1, we developed a VHA-learning collaborative of 13 influential community partners in the Denver and Colorado Springs region of Colorado. The VHA team consists of a learning collaborative leader, a program manager, and a program support assistant. The principal investigator attends and contributes to all meetings. Learning collaborative partners include a university psychology clinic that focuses on veterans’ care, 3 veterans service organizations, a mental health private practice, a university school of nursing, a community mental health center, veterans’ courts, and 5 city departments.
These partners participated in qualitative interviews to identify where gaps and breakdowns were occurring. With this information, the PSCI-SPC team and VHA-learning collaborative held a kickoff event. At this meeting the team discussed the qualitative findings, provided veteran suicide prevention information, and basic information regarding suicide prevention program building and implementation science.
Throughout quarterly learning collaborative meetings and monthly facilitation calls, we have worked to develop a blueprint and an action plan for each partner to develop best practices for dissemination to aid in providing consistency in the standard of care. A postimplementation event will be held to identify successes and challenges encountered while operationalizing project action plans.
Currently, activities of the learning collaborative are making a large impact on the community. Not all collaborative members track information regarding their populations served, nor specific metrics on veterans encountered. Even so, of those who do capture metrics, suicide prevention program components implemented by the collaborative will impact more than 21,000 individuals and at least 2,500 known veterans. In addition, 52 new connections have been made between community organizations or between community organizations and the VHA, and > 300 individuals have been trained.The learning collaborative support team has assisted in the dissemination of a large resource list for veterans. As the learning collaborative is ongoing and we are working with organizations to improve their data collection and analytics, we expect these numbers to increase. We anticipate that the learning collaborative will develop a stronger suicide prevention safety net within the community. In addition, we expect increased referrals of at-risk veterans to the VHA and enhance the long-term continuity of care between community and VHA services.
Objective 2: Implementation Toolkit
The second PSCI-SPC objective is to develop a toolkit for the implementation of best practices within a VHA-community suicide prevention learning collaborative. Lessons from the development of a successful suicide prevention learning collaborative will be shared through an online guide that other VHA facilities can use to support similar collaborative efforts within their communities. The toolkit will be disseminated across the VHA to assist suicide prevention coordinators and other staff in developing a suicide prevention learning collaborative at their facilities.
PSCI-SPC uses the Zero Suicide framework and the VA/US Department of Defense (DoD) Clinical Practice Guideline for the Assessment and Management of Patients at Risk for Suicide as models for preventing suicide in veterans not enrolled in VHA care.11,32 This implementation toolkit focuses on how to implement suicide prevention best practices into organizations that serve veterans. This toolkit differs from clinical practice guidelines in that it focuses on implementation strategies to promote success and effectively address challenges.
In order to provide a menu of available options for the learning collaborative and resulting toolkit, PSCI-SPC uses a logic model to compare the components of the VHA suicide prevention program, as well as other similar veteran and military suicide prevention programs.7,12,14,21,33,34 These programs are categorized into 2 types of prevention frameworks, the USI model as described above, and the SAMHSA Strategic Prevention Framework (Table 2).35 The SAMHSA framework was designed to promote mental health and prevent substance abuse, yet the derived classification is also applicable to suicide prevention programs.35 The results of the logic model comparison form the basis of the best practice interventions for the learning collaborative and initial toolkit. In addition to the best practice interventions, the toolkit consists of documents describing how to develop a veteran suicide prevention learning collaborative, as well as tools for learning collaborative members. Current tool development includes workbooks to guide collaborative members through the implementation process, guides for community organizations in implementing suicide prevention screening and risk assessment, a standard operating procedure for suicide prevention in a veterans court, and peer support training for veteran suicide prevention.
The methods to achieve Objective 2 include regular discussions with the VHA-learning collaborative on current best practices, identifying gaps and overlap of community programs. Successes and challenges of implementing suicide prevention best practices into learning collaborative organizations will be documented and incorporated into the toolkit. The learning collaborative will work iteratively as a team to improve the toolkit. Once complete, the toolkit will be disseminated to other VHA health care systems nationally, as well as to other state or regional partners that the learning collaborative identifies. A plan is under development for national suicide prevention entities to also disseminate the toolkit to lessen the burden of veteran suicide through their stakeholder base.
Objective 3: High-Risk Veterans Not Receiving VHA Care
Although veterans not receiving VHA care account for a number of veteran deaths by suicide, we are not aware of any current VHA programs that provide temporary psychotherapy and intensive case management to at-risk veterans ineligible for VHA care who are in need of immediate care while an appropriate permanent community placement is identified. In the current system, veterans in the community can present to VHA suicide prevention services through several different systems, including referrals to VHA and the Veterans Crisis Line (VCL). However, a portion of VCL calls are from veterans whose VHA eligibility is unknown or who are ineligible for services. If veterans are at imminent risk for suicide, emergency care is coordinated for them. However, if veterans are not at imminent suicide risk they are referred to the local suicide prevention coordinator and instructed to independently work toward determining their VHA eligibility.
It is currently unknown how many veterans follow through with these instructions. Nonetheless, if veterans are deemed eligible, they may present to VHA to obtain a same-day appointment. If not eligible, a suicide prevention coordinator may give them the phone number of a community referral. However, this practice is not standardized across VA medical centers, and the provided resources are up to the suicide prevention coordinator to research. Additionally, when a VHA suicide prevention coordinator leaves the position, knowledge of these community resources and rapport with community HCPs are often lost, leaving the next coordinator to develop these again, which reduces the efficiency and effectiveness of limited resources. It is also unknown how many veterans complete this contact and receive evidence-based treatment following referral. This is a complex system to navigate, particularly when at risk for suicide and in need of immediate but not emergency services.
Suicide prevention in such circumstances may be improved by adapting current suicide prevention practices, including evidence-based interventions, and the new VHA intensive case management program,11,36 within a Zero Suicide framework. PSCI-SPC has developed a brief intervention to transition ineligible veterans to permanent community treatment and provide them with additional resources to meet their varied needs. The brief 1 to 3 session intervention combines practices from brief cognitive behavioral therapy (BCBT) for suicide prevention, crisis response planning (CRP), and intensive case management within a Zero Suicide framework. Both the 2019 VA/DoD suicide prevention clinical practice guidelines and Zero Suicide recommend using cognitive behavioral therapy (CBT)-based interventions for suicide prevention.11,32 These interventions are packaged into a single intervention delivered by a PSCI-SPC therapist, typically a licensed clinical social worker, a licensed clinical psychologist, or an unlicensed psychologist under the supervision of a licensed clinical psychologist.
BCBT is one type of CBT that has shown initial efficacy in reducing suicide attempts.37 BCBT reduces the risk for suicide attempts both at the conclusion of treatment and at 24-month follow-up.37 BCBT is boiled down to its most essential components so it can be delivered in a distilled format. An essential element of BCBT that will remain is the CRP. A CRP11,37,38 entails collaboratively identifying effective, appropriate coping strategies and specific individuals to contact during a crisis. CRPs demonstrated efficacy as a stand-alone intervention to existing suicide prevention methods in a randomized clinical trial, such that individuals who received CRP had faster reductions in suicidal ideation and were 76% less likely to make a suicide attempt during the 6-month follow-up period.39 These results demonstrate that use of a CRP is connected to a decrease in suicidal behavior among suicidal patients.
The VHA has developed and is piloting a new initiative focused on restructuring its intensive case management services. RACETIME to Integrated Care (eg, Risk stratification, Assessment of complexity, Coordinator of lead assignment, Evaluate whole health needs, Trusting partnerships, Integrate care, Monitor progress, Experience of the veteran and employee) is a framework that assists VHA case managers in transitioning from a traditional case management mind-set to a more integrated and holistic method of care.36 RACETIME intensive case management practices will be incorporated into the intervention. However, RACETIME focuses on case management internally to the VHA. A modification for this treatment will be to focus on intensive case management from a mental health perspective and connecting to external community resources. Community referrals are mapped within a structured process and stored on a shared drive. This improves continuity between suicide prevention coordinators when they leave for a new position.
This intervention is conducted within a Zero Suicide framework. Pertinent to PSCI-SPC innovation to enhance care for non-VHA veterans is the care transitions element within the Zero Suicide framework, which has developed comprehensive suicide prevention guidance, including a pathway to care.32 This pathway refers a process to conduct follow-up supportive contacts that are tracked and recorded.
The PSCI-SPC pilot program incorporates the elements of CRP and brief CBT within a Zero Suicide framework. The PSCI-SPC team is developing and testing a protocol for providing brief treatment and community referrals to ineligible veterans that integrates these programming elements (Figure 2). A PSCI-SPC social worker will coordinate with the eligibility office to determine VHA eligibility. Ineligible veterans are referred to community partners and nonenrolled, eligible veterans are linked to VHA HCPs if they desire. These transitions will be coordinated, closely monitored, and verified.
Once the eligibility is determined, and the veteran’s preference is assessed, the team will perform a warm handoff to a VHA representative for enrollment into VHA care or to a community placement. We have sourced multiple community placements at varied payor levels. All veterans who are ineligible for care or who do not desire to be enrolled in VHA care will be provided the intervention package described above. After the veteran is placed in community care, PSCI-SPC team will follow up regularly with the veteran for 3 months to ensure continuity of care. If additional sessions are needed while the veteran needs a community placement, the PSCI team can accommodate this and will track the number of participants who needed additional sessions. If the veteran is deemed to be at imminent risk for suicide at any time during the pilot, he/she is transferred to emergency care. The veteran is allowed to participate once stabilized.
Findings from the pilot program will inform a manual intended for dissemination to patient safety and suicide prevention coordinators nationally across the VHA. The products from this objective will be integrated with the other objectives in training that will be provided on how to develop a local collaborative (Objective 1), disseminate the toolkit (Objective 2), and receive referrals into VHA or refer veterans to community clinical partners through the pilot program (Objective 3). Products developed and disseminated throughout PSCI-SPC aim to create momentum to reduce rates of suicide in veterans who are not connected to the VHA at the local community level.
Discussion
Improving suicide prevention for veterans who receive non-VHA health care is essential to significantly reduce veteran suicide rates. For the past decade, VHA suicide prevention initiatives have largely focused on veterans eligible for care, although the fastest increase in veteran suicide rates has occurred among veterans not connected to VHA services. Currently, if a veteran is deemed ineligible for care, it is up to the veteran to find other health care services in his or her community. There is not always a clear next step for the veteran to take, nor clear guidance provided to the VHA registration staff to assist with this care transition. This is particularly concerning for veterans at high risk for suicide as this could further thwart the veteran’s sense of belongingness and increase perceived burdensomeness, both suicide risk factors, and discourage them from attaining help.40 Overall, while the VHA has successfully implemented diverse suicide prevention initiatives and services, the need for continued system improvement focused on non-VHA veterans remains. PSCI-SPC was developed for this purpose.
By creating a collaborative that will connect VHA and community organizations, there will be better utilization of resources and more appropriate referrals throughout systems that interact with veterans. Sharing suicide prevention best practices between VHA and community partners is expected to increase access to mental health treatment to all veterans. Finally, by allowing best practices for suicide prevention in the VHA to serve as a guide in the development of best practices for suicide prevention between the VHA and the local health and behavioral health care community, PSCI-SPC will create a new suicide prevention intervention for veterans with mental health needs. Through these initiatives, PSCI-SPC will support providers’ and concerned citizens’ efforts to ensure that fewer veterans fall through the cracks of disjointed systems and will promote healthier communities where, regardless of VHA enrollment status, veterans receive suicide prevention care.
Conclusions
PSCI-SPC is a novel center for the innovation and dissemination of the nation’s best practices in suicide prevention for veterans who are ineligible for or otherwise not engaged in VHA services and who turn to their community for health care. PSCI-SPC not only seeks to create, develop, and measure various solutions to reduce suicide among veterans who receive non-VHA care, but also seeks to facilitate the overall quality of existing practices for suicide prevention and care coordination for enrolled veterans who use community resources. By bridging the gap between the VHA, civilian health care systems, and other community partners striving to prevent veteran suicides, we can create better access to care and a more seamless path of communication among these important entities that impact the lives of our veterans daily
1. US Department of Veterans Affairs. National strategy for preventing veteran suicide 2018-2028. https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf. Published September 2018. Accessed October 14, 2020.
2. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention. National veteran suicide prevention annual report. https://www.mentalhealth.va.gov/suicide_prevention/data.asp. Accessed October 14, 2020.
3. Centers for Disease Control and Prevention. Web-based injury statistics query and reporting system (WISQARS). 2014. https://www.cdc.gov/injury/wisqars/index.html. Updated July 1, 2020. Accessed October 14, 2020.
4. Lemle RB. Choice program expansion jeopardizes high-quality VHA mental health services. Fed Pract. 2018;35(3):18-24.
5. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention. VA national suicide data report 2005-2016. https://www.mentalhealth.va.gov/docs/data-sheets/OMHSP_National_Suicide_Data_Report_2005-2016_508.pdf. Published September 2018. Accessed October 14, 2020.
6. US Department of Veterans Affairs, Office of Suicide Prevention. VA national suicide data report 2005-2015. https://www.mentalhealth.va.gov/docs/data-sheets/2015/OMHSP_National_Suicide_Data_Report_2005-2015_06-14-18_508.pdf. Published June 2018. Accessed October 14, 2020.
7. US Department of Veterans Affairs. National strategy for preventing veteran suicide 2018-2028. https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf. Published 2018. Accessed October 30, 2020.
8. Gordon RS. An operational classification of disease prevention. Public Health Rep. 1983;98(2):107-109.
9. National Research Council and Institute of Medicine. O’Connell ME, Boat T, Warner KE, eds. Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. Washington, DC: National Academies Press; 2009.
10. US Department of Health and Human Services, National Institute on Drug Abuse, Office of Science Policy and Communications. Drug Abuse Prevention: What Works. Rockville, MD: National Institutes of Health; 1997.
11. US Department of Veterans Affairs, US Department of Defense. VA/DoD clinical practice guideline for the assessment and management of patients at risk for suicide. https://www.healthquality.va.gov/guidelines/MH/srb. Published 2019. Updated July 30, 2020. Accessed October 14, 2020.
12. US Department of Veterans Affairs. Veterans Access, Choice and Accountability Act of 2014. https://www.govinfo.gov/content/pkg/PLAW-113publ146/pdf/PLAW-113publ146.pdf. Accessed October 14, 2020.
13. US Department of Veterans Affairs. Strategic Health Care. VA MISSION Act: Extension of the VA choice program. https://strategichealthcare.net/wp-content/uploads/2018/05/052718-VA-MISSION-Act-Summary.pdf. Accessed October 14, 2020.
14. US Congress. H.R.5674—VA MISSION Act of 2018. https://www.congress.gov/bill/115th-congress/house-bill/5674. Accessed October 15, 2020.
15. Grumet JG, Hogan MF, Chu A, Covington DW, Johnson KE. Compliance standards pave the way for reducing suicide in health care systems. J Health Care Compliance. 2019;17-26.
16. Hillestad R, Bigelow J, Bower A, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff (Millwood). 2005;24(5):1103-1117. doi:10.1377/hlthaff.24.5.110
17. Porter ME, Pabo EA, Lee TH. Redesigning primary care: a strategic vision to improve value by organizing around patients’ needs. Health Aff (Millwood). 2013;32(3):516-525. doi:10.1377/hlthaff.2012.0961
18. Nevedal AL, Wagner TH, Ellerbe LS, Asch SM, Koenig CJ. A qualitative study of primary care providers’ experiences with the Veterans Choice Program. J Gen Intern Med. 2019;34:598-603. doi:10.1007/s11606-018-4810-2
19. Tanielian T, Farris C, Epley C, et al. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf. Published 2014. Accessed October 15, 2020.
20. White House. Executive Order 13861: President’s roadmap to empower veterans and end the national tragedy of suicide (PREVENTS). https://www.va.gov/PREVENTS/docs/PRE-007-The-PREVENTS-Roadmap-1-2_508.pdf. Published June 17, 2020. Accessed October 15, 2020.
21. US Department of Veterans Affairs, Office of the Under Secretary for Health. Memorandum. VA continues community suicide prevention challenge at another mayor’s challenge policy academy. https://www.blogs.va.gov/VAntage/58468/va-continues-community-suicide-prevention-challenge-another-mayors-challenge-policy-academy. Published April 4, 2019. Accessed October 15, 2020.
22. US Department of Veterans Affairs, Veterans Health Administration (VHA) Veterans Health Administration (VHA) Fiscal Year (FY) 2018-2019 Operational Plan. www.navao.org/wp-content/uploads/2018/06/USH-Memo-10-2018-03-VHA_FY_2018-2019_Operational_Plan-4-19-18.pdf. Published April 19, 2018. Accessed October 15, 2020.
23. US Department of Veterans Affairs. VA, Health and Human Services announce governor’s challenge to prevent suicide. https://www.blogs.va.gov/VAntage/55707/va-health-human-services-announce-governors-challenge-prevent-suicide. Published January 17, 2019. Accessed October 15, 2020.
24. VA’s suicide prevention campaign “Be There’’ kicks off in Times Square. https://www.blogs.va.gov/VAntage/57272/vas-suicide-prevention-campaign-kicks-off-times-square. Published March 6, 2019. Accessed October 15, 2020.
25. US Department of Veterans Affairs, Office of Public Affairs Media Relations. Emergent mental health care for former service members. https://www.mentalhealth.va.gov/docs/Fact_Sheet-Emergent_Mental_Health_Care_Former_Service_Members.pdf. Published 2017. Accessed October 15, 2020.
26. US Department of Veterans Affairs. VA secretary formalizes expansion of emergency mental health care to former service members with other-than-honorable discharges. https://www.blogs.va.gov/VAntage/39092/va-secretary-formalizes-expansion-emergency-mental-health-care-former-service-members-honorable-discharges. Published June 27, 2017. Accessed October 15, 2020.
27. Shane L. New veteran suicide numbers raise concerns among experts hoping for positive news. Military Times. https://www.militarytimes.com/news/pentagon-congress/2019/10/09/new-veteran-suicide-numbers-raise-concerns-among-experts-hoping-for-positive-news. Published October 9, 2019. Accessed October 15, 2020.
28. US Department of Veterans Affairs. Department of Veterans Affairs FY 2018-2024 Strategic Plan. https://www.va.gov/oei/docs/VA2018-2024strategicPlan.pdf. Updated May 31, 2019. Accessed October 15, 2020.
29. Komaie G, Goodman M, McCall A, et al. Training community members in public health research: development and implementation of a community participatory research pilot project. Health Equity. 2018;2(1):282-287. doi:10.1089/heq.2018.0043
30. Wang KH, Ray NJ, Berg DN, et al. Using community-based participatory research and organizational diagnosis to characterize relationships between community leaders and academic researchers. Prev Med Reports. 2017;7:180-186. doi:10.1016/j.pmedr.2017.06.007
31. Institute for Healthcare Improvement. The breakthrough series: IHI’s collaborative model for achieving breakthrough improvement. http://www.ihi.org/resources/Pages/IHIWhitePapers/TheBreakthroughSeriesIHIsCollaborativeModelforAchievingBreakthroughImprovement.aspx. Published 2003. Accessed October 15, 2020.
32. Zero Suicide in Health and Behavioral Health Care Institute. Zero suicide toolkit. https://zerosuicide.sprc.org/toolkit. Accessed October 15, 2020.

33. Preventing suicide: a technical package of policy, programs, and practices. https://www.cdc.gov/violenceprevention/pdf/suicideTechnicalPackage.pdf. Published 2017. Accessed October 30, 2020.
34. US Department of Veterans Affairs. VA Office of Mental Health and Suicide Prevention guidebook. https://www.mentalhealth.va.gov/docs/VA-Office-of-Mental-Health-and-Suicide-Prevention-Guidebook-June-2018-FINAL-508.pdf. Published June 2018. Accessed October 15, 2020.
35. US Department of Health and Human Services, Substance Abuse and Mental Health Services, Administration Center for Substance Abuse Prevention. Focus on prevention: strategies and programs to prevent substance abuse. HHS Publication No. (SMA) 10-4120. https://helpandhopewv.org/docs/Focus%20on%20Prevention.pdf. Revised 2017. Accessed October 15, 2020.
36. Misiti R, Risinger A. RACETIME: an organizational care coordination approach to improving patient outcomes in a complex healthcare setting. Presentation at the Military Social Work & Behavioral Health Conference Austin, Texas. July 23, 2020. https://sites.utexas.edu/military-social-work-conference/misiti-risinger. Accessed October 23, 2020.
37. Rudd MD, Bryan CJ, Wertenberger EG, et al. Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: results of a randomized clinical trial with 2-year follow-up. Am J Psychiatry. 2015;172(5):441-449. doi:10.1176/appi.ajp.2014.14070843
38. Rudd MD, Mandrusiak M, Joiner TE Jr. The case against no-suicide contracts: The commitment to treatment statement as a practice alternative. Clin Psychol. 2006;62(2):243-251.
39. Bryan CJ, Mintz J, Clemans TA, et al. Effect of crisis response planning vs. contracts for safety on suicide risk in US Army soldiers: a randomized clinical trial. J Affect Disord. 2017;212:64-72. doi:10.1016/j.jad.2017.01.028
40. Joiner TE. Why People Die by Suicide. Cambridge, MA: First Harvard University Press; 2005:27.
41. Office of the Under Secretary of Defense for Personnel and Readiness. DoD Instruction 6490.16: Defense suicide prevention program. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/649016p.pdf?ver=2020-09-11-122632-850. Published November 6, 2017. Updated September 11, 2020. Accessed October 14, 2020.
42. Zero Suicide in Health and Behavioral Health Care Institute. Engage: engaging patients. http://zerosuicide.edc.org/toolkit/engage#quicktabs-engage=0. Accessed October 14, 2020.
43. Stone D, Holland K, Bartholow B, Crosby A, Davis S, Wilkins N. Preventing Suicide: A technical package of policy, programs, and practices. https://www.cdc.gov/violenceprevention/pdf/suicidetechnicalpackage.pdf. Published 2017. Accessed October 14, 2020.
44. Mills PD, Watts BV, Miller S, et al. A checklist to identify inpatient suicide hazards in veterans affairs hospitals. Jt Comm J Qual Patient Saf. 2010;36(2):87-93. doi:10.1016/s1553-7250(10)36015-6
45. US Department of Veterans Affairs, Office of Research and Development. Crisis prevention: study evaluates VA program that identifies vets at highest risk for suicide. https://www.research.va.gov/currents/0918-Study-evaluates-VA-program-that-identifies-Vets-at-highest-risk-for-suicide.cfm. Updated September, 20, 2018. Accessed October 14, 2020.
46. Zero Suicide in Health and Behavioral Health Care Institute. Engage: active engagement for safer suicide care--reducing access to lethal means. http://zerosuicide.edc.org/toolkit/engage#quicktabs-engage=1. Published 2017. Accessed October 14, 2020.
47. Zero Suicide in Health and Behavioral Health Care Institute. Train: training for all. http://zerosuicide.sprc.org/toolkit/train. Accessed October 14, 2020.
48. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention (OMHSP). Facts about veteran suicide. https://www.mentalhealth.va.gov/docs/FINAL_VA_OMHSP_Suicide_Prevention_Fact_Sheet_508.pdf. Published June 2018. Accessed October 14, 2020.
49. Zero Suicide in Health and Behavioral Health Care Institute. Treat: direct treatment. http://zerosuicide.edc.org/toolkit/treat. Accessed October 14, 2020.
50. Office of the Under Secretary of Defense for Personnel and Readiness. DoD Instruction 6490.04: Mental health evaluations of members of the military services. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/649004p.pdf. Published March 4, 2013. Updated April 22, 2020. Accessed October 14, 2020.
51. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention Frequently asked questions: VA National Suicide Data Report. https://www.mentalhealth.va.gov/docs/data-sheets/2015_Data_Release_FAQs_508.pdf. Published September 2018. Updated June 22, 2018. Accessed October 14, 2020.
52. Zero Suicide in Health and Behavioral Health Care Institute. ZERO Suicide engage: active engagement for safer suicide care safety planning. http://zerosuicide.edc.org/toolkit/engage#quicktabs-engage=1. Accessed October 14, 2020.
1. US Department of Veterans Affairs. National strategy for preventing veteran suicide 2018-2028. https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf. Published September 2018. Accessed October 14, 2020.
2. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention. National veteran suicide prevention annual report. https://www.mentalhealth.va.gov/suicide_prevention/data.asp. Accessed October 14, 2020.
3. Centers for Disease Control and Prevention. Web-based injury statistics query and reporting system (WISQARS). 2014. https://www.cdc.gov/injury/wisqars/index.html. Updated July 1, 2020. Accessed October 14, 2020.
4. Lemle RB. Choice program expansion jeopardizes high-quality VHA mental health services. Fed Pract. 2018;35(3):18-24.
5. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention. VA national suicide data report 2005-2016. https://www.mentalhealth.va.gov/docs/data-sheets/OMHSP_National_Suicide_Data_Report_2005-2016_508.pdf. Published September 2018. Accessed October 14, 2020.
6. US Department of Veterans Affairs, Office of Suicide Prevention. VA national suicide data report 2005-2015. https://www.mentalhealth.va.gov/docs/data-sheets/2015/OMHSP_National_Suicide_Data_Report_2005-2015_06-14-18_508.pdf. Published June 2018. Accessed October 14, 2020.
7. US Department of Veterans Affairs. National strategy for preventing veteran suicide 2018-2028. https://www.mentalhealth.va.gov/suicide_prevention/docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf. Published 2018. Accessed October 30, 2020.
8. Gordon RS. An operational classification of disease prevention. Public Health Rep. 1983;98(2):107-109.
9. National Research Council and Institute of Medicine. O’Connell ME, Boat T, Warner KE, eds. Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. Washington, DC: National Academies Press; 2009.
10. US Department of Health and Human Services, National Institute on Drug Abuse, Office of Science Policy and Communications. Drug Abuse Prevention: What Works. Rockville, MD: National Institutes of Health; 1997.
11. US Department of Veterans Affairs, US Department of Defense. VA/DoD clinical practice guideline for the assessment and management of patients at risk for suicide. https://www.healthquality.va.gov/guidelines/MH/srb. Published 2019. Updated July 30, 2020. Accessed October 14, 2020.
12. US Department of Veterans Affairs. Veterans Access, Choice and Accountability Act of 2014. https://www.govinfo.gov/content/pkg/PLAW-113publ146/pdf/PLAW-113publ146.pdf. Accessed October 14, 2020.
13. US Department of Veterans Affairs. Strategic Health Care. VA MISSION Act: Extension of the VA choice program. https://strategichealthcare.net/wp-content/uploads/2018/05/052718-VA-MISSION-Act-Summary.pdf. Accessed October 14, 2020.
14. US Congress. H.R.5674—VA MISSION Act of 2018. https://www.congress.gov/bill/115th-congress/house-bill/5674. Accessed October 15, 2020.
15. Grumet JG, Hogan MF, Chu A, Covington DW, Johnson KE. Compliance standards pave the way for reducing suicide in health care systems. J Health Care Compliance. 2019;17-26.
16. Hillestad R, Bigelow J, Bower A, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff (Millwood). 2005;24(5):1103-1117. doi:10.1377/hlthaff.24.5.110
17. Porter ME, Pabo EA, Lee TH. Redesigning primary care: a strategic vision to improve value by organizing around patients’ needs. Health Aff (Millwood). 2013;32(3):516-525. doi:10.1377/hlthaff.2012.0961
18. Nevedal AL, Wagner TH, Ellerbe LS, Asch SM, Koenig CJ. A qualitative study of primary care providers’ experiences with the Veterans Choice Program. J Gen Intern Med. 2019;34:598-603. doi:10.1007/s11606-018-4810-2
19. Tanielian T, Farris C, Epley C, et al. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf. Published 2014. Accessed October 15, 2020.
20. White House. Executive Order 13861: President’s roadmap to empower veterans and end the national tragedy of suicide (PREVENTS). https://www.va.gov/PREVENTS/docs/PRE-007-The-PREVENTS-Roadmap-1-2_508.pdf. Published June 17, 2020. Accessed October 15, 2020.
21. US Department of Veterans Affairs, Office of the Under Secretary for Health. Memorandum. VA continues community suicide prevention challenge at another mayor’s challenge policy academy. https://www.blogs.va.gov/VAntage/58468/va-continues-community-suicide-prevention-challenge-another-mayors-challenge-policy-academy. Published April 4, 2019. Accessed October 15, 2020.
22. US Department of Veterans Affairs, Veterans Health Administration (VHA) Veterans Health Administration (VHA) Fiscal Year (FY) 2018-2019 Operational Plan. www.navao.org/wp-content/uploads/2018/06/USH-Memo-10-2018-03-VHA_FY_2018-2019_Operational_Plan-4-19-18.pdf. Published April 19, 2018. Accessed October 15, 2020.
23. US Department of Veterans Affairs. VA, Health and Human Services announce governor’s challenge to prevent suicide. https://www.blogs.va.gov/VAntage/55707/va-health-human-services-announce-governors-challenge-prevent-suicide. Published January 17, 2019. Accessed October 15, 2020.
24. VA’s suicide prevention campaign “Be There’’ kicks off in Times Square. https://www.blogs.va.gov/VAntage/57272/vas-suicide-prevention-campaign-kicks-off-times-square. Published March 6, 2019. Accessed October 15, 2020.
25. US Department of Veterans Affairs, Office of Public Affairs Media Relations. Emergent mental health care for former service members. https://www.mentalhealth.va.gov/docs/Fact_Sheet-Emergent_Mental_Health_Care_Former_Service_Members.pdf. Published 2017. Accessed October 15, 2020.
26. US Department of Veterans Affairs. VA secretary formalizes expansion of emergency mental health care to former service members with other-than-honorable discharges. https://www.blogs.va.gov/VAntage/39092/va-secretary-formalizes-expansion-emergency-mental-health-care-former-service-members-honorable-discharges. Published June 27, 2017. Accessed October 15, 2020.
27. Shane L. New veteran suicide numbers raise concerns among experts hoping for positive news. Military Times. https://www.militarytimes.com/news/pentagon-congress/2019/10/09/new-veteran-suicide-numbers-raise-concerns-among-experts-hoping-for-positive-news. Published October 9, 2019. Accessed October 15, 2020.
28. US Department of Veterans Affairs. Department of Veterans Affairs FY 2018-2024 Strategic Plan. https://www.va.gov/oei/docs/VA2018-2024strategicPlan.pdf. Updated May 31, 2019. Accessed October 15, 2020.
29. Komaie G, Goodman M, McCall A, et al. Training community members in public health research: development and implementation of a community participatory research pilot project. Health Equity. 2018;2(1):282-287. doi:10.1089/heq.2018.0043
30. Wang KH, Ray NJ, Berg DN, et al. Using community-based participatory research and organizational diagnosis to characterize relationships between community leaders and academic researchers. Prev Med Reports. 2017;7:180-186. doi:10.1016/j.pmedr.2017.06.007
31. Institute for Healthcare Improvement. The breakthrough series: IHI’s collaborative model for achieving breakthrough improvement. http://www.ihi.org/resources/Pages/IHIWhitePapers/TheBreakthroughSeriesIHIsCollaborativeModelforAchievingBreakthroughImprovement.aspx. Published 2003. Accessed October 15, 2020.
32. Zero Suicide in Health and Behavioral Health Care Institute. Zero suicide toolkit. https://zerosuicide.sprc.org/toolkit. Accessed October 15, 2020.

33. Preventing suicide: a technical package of policy, programs, and practices. https://www.cdc.gov/violenceprevention/pdf/suicideTechnicalPackage.pdf. Published 2017. Accessed October 30, 2020.
34. US Department of Veterans Affairs. VA Office of Mental Health and Suicide Prevention guidebook. https://www.mentalhealth.va.gov/docs/VA-Office-of-Mental-Health-and-Suicide-Prevention-Guidebook-June-2018-FINAL-508.pdf. Published June 2018. Accessed October 15, 2020.
35. US Department of Health and Human Services, Substance Abuse and Mental Health Services, Administration Center for Substance Abuse Prevention. Focus on prevention: strategies and programs to prevent substance abuse. HHS Publication No. (SMA) 10-4120. https://helpandhopewv.org/docs/Focus%20on%20Prevention.pdf. Revised 2017. Accessed October 15, 2020.
36. Misiti R, Risinger A. RACETIME: an organizational care coordination approach to improving patient outcomes in a complex healthcare setting. Presentation at the Military Social Work & Behavioral Health Conference Austin, Texas. July 23, 2020. https://sites.utexas.edu/military-social-work-conference/misiti-risinger. Accessed October 23, 2020.
37. Rudd MD, Bryan CJ, Wertenberger EG, et al. Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: results of a randomized clinical trial with 2-year follow-up. Am J Psychiatry. 2015;172(5):441-449. doi:10.1176/appi.ajp.2014.14070843
38. Rudd MD, Mandrusiak M, Joiner TE Jr. The case against no-suicide contracts: The commitment to treatment statement as a practice alternative. Clin Psychol. 2006;62(2):243-251.
39. Bryan CJ, Mintz J, Clemans TA, et al. Effect of crisis response planning vs. contracts for safety on suicide risk in US Army soldiers: a randomized clinical trial. J Affect Disord. 2017;212:64-72. doi:10.1016/j.jad.2017.01.028
40. Joiner TE. Why People Die by Suicide. Cambridge, MA: First Harvard University Press; 2005:27.
41. Office of the Under Secretary of Defense for Personnel and Readiness. DoD Instruction 6490.16: Defense suicide prevention program. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/649016p.pdf?ver=2020-09-11-122632-850. Published November 6, 2017. Updated September 11, 2020. Accessed October 14, 2020.
42. Zero Suicide in Health and Behavioral Health Care Institute. Engage: engaging patients. http://zerosuicide.edc.org/toolkit/engage#quicktabs-engage=0. Accessed October 14, 2020.
43. Stone D, Holland K, Bartholow B, Crosby A, Davis S, Wilkins N. Preventing Suicide: A technical package of policy, programs, and practices. https://www.cdc.gov/violenceprevention/pdf/suicidetechnicalpackage.pdf. Published 2017. Accessed October 14, 2020.
44. Mills PD, Watts BV, Miller S, et al. A checklist to identify inpatient suicide hazards in veterans affairs hospitals. Jt Comm J Qual Patient Saf. 2010;36(2):87-93. doi:10.1016/s1553-7250(10)36015-6
45. US Department of Veterans Affairs, Office of Research and Development. Crisis prevention: study evaluates VA program that identifies vets at highest risk for suicide. https://www.research.va.gov/currents/0918-Study-evaluates-VA-program-that-identifies-Vets-at-highest-risk-for-suicide.cfm. Updated September, 20, 2018. Accessed October 14, 2020.
46. Zero Suicide in Health and Behavioral Health Care Institute. Engage: active engagement for safer suicide care--reducing access to lethal means. http://zerosuicide.edc.org/toolkit/engage#quicktabs-engage=1. Published 2017. Accessed October 14, 2020.
47. Zero Suicide in Health and Behavioral Health Care Institute. Train: training for all. http://zerosuicide.sprc.org/toolkit/train. Accessed October 14, 2020.
48. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention (OMHSP). Facts about veteran suicide. https://www.mentalhealth.va.gov/docs/FINAL_VA_OMHSP_Suicide_Prevention_Fact_Sheet_508.pdf. Published June 2018. Accessed October 14, 2020.
49. Zero Suicide in Health and Behavioral Health Care Institute. Treat: direct treatment. http://zerosuicide.edc.org/toolkit/treat. Accessed October 14, 2020.
50. Office of the Under Secretary of Defense for Personnel and Readiness. DoD Instruction 6490.04: Mental health evaluations of members of the military services. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/649004p.pdf. Published March 4, 2013. Updated April 22, 2020. Accessed October 14, 2020.
51. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention Frequently asked questions: VA National Suicide Data Report. https://www.mentalhealth.va.gov/docs/data-sheets/2015_Data_Release_FAQs_508.pdf. Published September 2018. Updated June 22, 2018. Accessed October 14, 2020.
52. Zero Suicide in Health and Behavioral Health Care Institute. ZERO Suicide engage: active engagement for safer suicide care safety planning. http://zerosuicide.edc.org/toolkit/engage#quicktabs-engage=1. Accessed October 14, 2020.
NP and PA Scope of Practice
Nurse practitioners (NPs) and physician assistants (PAs) provide healthcare in numerous environments internationally and in the United States.[1, 2] However, their role in the inpatient medicine setting is not well described.[2] In the United States, there are more than 157,000 NPs and 85,000 PAs with projected increases.[3, 4] Although both professions provide direct medical care, there are key differences.[1, 3, 4, 5] NPs typically complete a master's or doctoral degree with advanced clinical training beyond nursing. PAs complete at least 2 years of college courses similar to premedical school requirements. PA programs use a medical school‐based curriculum and train for about 2 years before awarding a master's degree. NPs are regulated through state nursing boards, whereas PAs are regulated through state licensing or medical boards. NPs and PAs have different, yet overlapping scopes of practice. A key difference is that PAs can only practice collaborating with a physician.[5, 6] Overall, both have been shown to provide healthcare that is similar in quality to physicians in specific primary care and surgical settings.[2]
NPs and PAs, often referred to as advanced practice providers (APPs), are employed primarily in outpatient clinic settings providing direct patient care. Most APP studies have focused on the outpatient setting, despite nearly a third of US healthcare expenditure for hospital care.[2, 7] Little is known about APP involvement, specific roles, or impact on outcomes in inpatient medicine settings where they are often referred to as NP or PA hospitalists.[2, 8, 9, 10]
The Veterans Health Administration (VHA) is 1 of the largest employers of APPs, with 3.6% of all NPs and 2.1% of all PAs reported to practice in the VHA.[11, 12, 13] As the largest fully integrated healthcare system in the US, the VHA had 8.8 million veterans enrolled and 703,500 inpatient admissions in 2012.[14] Although this makes the VHA an ideal environment to study the role of APPs, few studies have done so.[13, 15, 16, 17, 18, 19] Although studies have compared NPs and PAs to physicians, very little is known about how NPs differ from PAs when practicing in the same environment.
Our objective was to describe the scope of practice, defined as activities that an individual healthcare practitioner is licensed to perform, of NPs and PAs in the inpatient medicine setting and in the VHA. A secondary objective was to explore important outcomes that could potentially be affected by the presence of NPs and PAs on inpatient medicine.
METHODS
The Organizational Factors and Inpatient Medical Care Quality and Efficiency (OFIM) study provides a basis for this study with detail published elsewhere.[20] The OFIM study was conducted between 2010 and 2011 to evaluate quality of care in VHA inpatient medicine surveying chiefs of medicine (COM), inpatient medicine nurse managers (NM), attending physicians, and extant VHA survey data. The COM is the senior attending physician in charge of departments of medicine that include most medical subspecialties within the VHA medical centers. We used the subset of questions specific to NPs and PAs from the COM and NM surveys. Both COMs and NMs answered identical questions for NPs and PAs in 2 separate sections to avoid overlap of responses. NM survey responses were only used for the coordination of care regression model. Surveys were conducted by e‐mail with up to 4 reminders and a subsequent paper mailing. The inpatient medicine service included adult general internal medicine, medical subspecialties, and critical care. The study was approved by the institutional review boards of the VA Boston Healthcare System, the University of Iowa, and the Iowa City VA Healthcare System.
Measurements
To create our primary variable of interestNP and PA employmentwe used the COM survey. Respondents indicated the number and full‐time employee equivalent (FTEE) values for APPs on inpatient medicine. Based on responses, we created a categorical variable with 4 options: (1) facilities with NPs only, (2) facilities with PAs only, (3) facilities with both NPs and PAs, and (4) facilities with neither NPs nor PAs. We selected 3 outcomes that could potentially be affected by the presence of NPs and PAs on inpatient medicine: patient satisfaction, registered nurse (RN) satisfaction, and coordination of care. Patient satisfaction has been shown to improve with NPs and PAs in prior studies, and improving coordination of care has been a stated goal of medical centers in hiring NPs and PAs.[2, 9] Based on our personal experience and previous studies that have shown that nurses report better communication with NPs than physicians,[21] and that NPs retain a visible nursing component in their NP role,[22] we hypothesized that nurse satisfaction on inpatient medicine would improve with the presence of NPs and PAs.
Patient satisfaction was obtained from the 2010 VHA Survey of Healthcare Experiences of Patients (SHEP).[23] The average response rate was 45%. Approximately half the questions on the SHEP are identical to the Hospital Consumer Assessment of Healthcare Providers and Systems survey (HCAHPS).[24] We examined 2 items: an overall rating and willingness to recommend the facility. For the overall rating, patients rated their hospitalization on a scale from 0 (worst hospital possible) to 10 (best hospital possible). Following HCAHPS guidelines, responses of either 9 or 10 were coded as positive and all other nonmissing responses were coded 0. For willingness to recommend, patients were asked Would you recommend this hospital to your friends and family? using a 4‐point response scale. Responses of definitely and probably no were coded as 0, and probably and definitely yes were coded as 1.
Nurse satisfaction was obtained from the 2011 Veterans Administration Nursing Outcomes Database, an annual survey of VHA nurses that includes demographic, work environment and satisfaction data.[25] The survey, a modified version of the Practice Environment Scale,[26] had a response rate of 52.9% (out of 51,870). For this analysis, we selected only inpatient medicine RNs. We used 2 measures: overall job satisfaction and collegial RN/MD (physician) relations. The former was assessed using the item Compared to what you think it should be, what is your current overall level of satisfaction with your job? The RN/MD relations scale had 3 items, including Physicians and nurses have good working relationships. Both items were evaluated on a similar 5‐point response scale.
Coordination of care was assessed from COM and NM surveys. Overall coordination was evaluated from the COM survey using 1 of 8 items in a question about care coordination, In the past month, how would you rate the following aspects of coordination of patient care inpatient coordination overall. Overall coordination was also evaluated from the NM survey using a similar item. Discharge coordination was evaluated only from the NM survey using 1 of 8 items, Thinking about your experiences during the past month, how would you rate the following aspects of the coordination of patient care related to the discharge process on your inpatient medicine unit discharge coordination overall. When a service had more than 1 response from the NM survey, we took an average of responses to represent the mean score. Responses for all questions ranged from 1 for poor to 5 for excellent (for all of the questions see Supporting Information, Appendix 1, in the online version of this article).
Last, we modeled for several contextual features that could influence outcomes: geographic region as a 4‐item categorical variable; teaching affiliation as a dichotomous variable based on whether the hospital was a member of the Council of Teaching Hospitals, urban or rural status, and facility size as a continuous variable using the number of inpatient medicine service beds.
Statistical Analysis
Descriptive bivariate analyses used t tests, 2, or 2‐tailed Fisher tests when appropriate to compare NP and PA autonomy, tasks, location of care, work schedule, clinical workload, organizational characteristics (ie, academic, urban, facility complexity, inpatient medicine team structure), and performance evaluations.
Next, we examined whether any of the contextual characteristics were associated with use of NPs or PAs using inferential statistics. For patient satisfaction, we developed a hierarchical linear model (HLM) that nested patients within facilities. We controlled for patient age, sex, health status, and length of stay. For nurse satisfaction, individual responses of RNs also were analyzed using the HLM. We controlled for whether the nurse had a leadership position, worked during the daily shift, and job tenure. Ordinary least squares regression was used to examine the 3 measures of coordination from the COM and NM surveys. All analyses were performed using Stata version 12 (StataCorp, College Station, TX) and SAS version 9.2 (SAS Institute Inc., Cary, NC).
RESULTS
Of 123 inpatient medicine services that we surveyed, we included responses from the COMs of 118 services (response rate 95.2%); 5 responses were incomplete. Across 123 inpatient medicine services, we surveyed 264 nurse managers and received 198 responses (75.0%) from 114 inpatient medicine services. In the only model using NM responsesthe care coordination model104 inpatient medicine services had responses from both COM and NM surveys.
Of 118 VHA inpatient medicine services, 56 (47.5%) had APPs, of which 27 (48.2%) had NPs only, 15 (26.8%) had PAs only, and 14 (25.0%) had both NPs and PAs. FTEEs for NPs ranged from 0.5 to 7 (mean=2.22) and for PAs from 1 to 9 (mean=2.23) on the inpatient medicine service per hospital.
There were no significant differences on use of NPs and PAs by teaching affiliation, urban or rural setting, and geography. A significant difference was observed based on bed size (F[3,109]=5.13, P<0.001); facilities with both NPs and PAs had, on average, a larger number of inpatient beds (mean=79.0, standard deviation [SD]=32.3) compared to those without NPs or PAs (mean=50.1, SD=29.4) or with PAs only (mean=44.2, SD=20.5) using Tukey post hoc analysis.
The most common staffing model used staff (attending) physicians only working directly with APPs (N=29, 24.6%). Next most common was an academic model with staff physicians, housestaff, and APPs working together in teams (N=16, 13.4%). For performance evaluations, COMs contributed for both NPs (60.2%) and PAs (56.4%); in fewer cases, COMs completed evaluations of NPs (12.9%) and of PAs (29.0%) without input from other service managers (P=0.02).
Table 1 shows the differences reported by COMs between NPs and PAs scope of practice. Overall, 58.9% of NPs and 65.4% of PAs functioned somewhat or completely autonomously; 23.1% of NPs and 30.8% of PAs worked in a role closer to a ward assistant (eg, work directly with a physician, cowriting orders, and making care decisions with physician oversight). Tasks frequently performed by the majority of NPs and PAs included writing orders (87.9%), coordinating discharge plans (86.7%), communicating with consultants (83.1%), performing history and physicals (82.5%), writing daily progress notes (80.7%), communicating with primary care providers (73.5%), and working directly with hospitalists (72.8%). Less common tasks included serving on committees (46.4%), championing quality improvement activities (40.6%), and research (2.9%). There were no statistically significant differences between tasks, except for a higher proportion of services reporting PAs rather than NPs performing procedures (50.0% vs 22.0%, P=0.02) and teaching nonphysicians (50.0% vs 24.4%, P=0.04).
| Services With NPs, | Services With PAs, | P Value | |
|---|---|---|---|
| |||
| How do NPs and PAs function in conjunction with inpatient medicine staff (attending) physicians in the day‐to‐day care of patients (ie, scope of practice)? | N=39 (%)* | N=26 (%)* | |
| Autonomously, in a manner similar to physicians | 10 (25.6%) | 5 (19.2%) | 0.77 |
| Somewhat autonomously, but with limitations | 13 (33.3%) | 12 (46.2%) | 0.31 |
| In a role closer to a ward assistant | 9 (23.1%) | 8 (30.8%) | 0.57 |
| Administrative | 2 (5.1%) | 0 (0.0%) | 0.51 |
| Other | 6 (15.4%) | 1 (3.8%) | 0.23 |
| What types of tasks do NPs and PAs perform? | N=41 (%)* | N=28 (%)* | |
| Write orders | 34 (82.9%) | 26 (92.9%) | 0.29 |
| Coordinate discharge plans | 33 (80.5%) | 26 (92.9%) | 0.18 |
| Communicate with consultants | 33 (80.5%) | 24 (85.7%) | 0.75 |
| History and physicals | 31 (75.6%) | 25 (89.3%) | 0.22 |
| Daily progress notes | 31 (75.6%) | 24 (85.7%) | 0.37 |
| Communicate with primary care providers | 31 (75.6%) | 20 (71.4% | 0.78 |
| Work directly with hospitalists | 26 (63.4%) | 23 (82.1%) | 0.18 |
| Committees | 16 (39.0%) | 16 (57.1%) | 0.15 |
| Champion quality improvement activities | 14 (34.1%) | 14 (50.0%) | 0.22 |
| Teach nonphysician students | 10 (24.4%) | 14 (50.0%) | 0.04 |
| Perform procedures | 9 (22.0%) | 14 (50.0%) | 0.02 |
| Research | 1 (2.4%) | 1 (3.6%) | 1.00 |
| Other | 6 (14.6%) | 0 (0.0%) | 0.04 |
Table 2 reports location of practice in the hospital and workload. There were no significant differences in locations where NPs and PAs provided care. Overall, 81.9% of APPs worked in inpatient wards, 23.1% in step‐down units, 18.6% in intensive care units, 13.8% in skilled care units, and 4.9% in other locations. In addition, 97.4% of NPs and 89.3% of PAs worked weekdays, whereas only 7.9% of NPs and 17.9% of PAs worked nights. More PAs than NPs worked federal holidays (32.1% vs 7.9%, P=0.02) and weekends (32.1% vs 13.2%, P=0.08). Most NPs and PAs handled a caseload of 4 to 10 patients with a mean of 6.5, with no difference between the 2. The minority, 27.0% of NPs and 23.1% of PAs, were not assigned specific patients.
| Services With NPs | Services With PAs | P Value | |
|---|---|---|---|
| |||
| Where do NPs and PAs provide care? | N=38 (%)* | N=28 (%)* | |
| Wards | 31 (81.6%) | 23 (82.1%) | 1.00 |
| Step‐down unit | 8 (21.1%) | 7 (25.0%) | 0.77 |
| Intensive care unit | 6 (15.8%) | 6 (21.4%) | 0.75 |
| Skilled care units | 5 (13.2%) | 4 (14.3%) | 1.00 |
| Other | 1 (2.6%) | 2 (7.1%) | 0.57 |
| What are NPs and PAs tours of duty? | N=38 (%)* | N=28 (%)* | |
| Weekdays | 37 (97.4%) | 25 (89.3%) | 0.30 |
| Weekends | 5 (13.2%) | 9 (32.1%) | 0.08 |
| Nights | 3 (7.9%) | 5 (17.9%) | 0.27 |
| Federal holidays | 3 (7.9%) | 9 (32.1%) | 0.02 |
| Other | 2 (5.3%) | 1 (3.6%) | 1.00 |
| What is the average clinical workload for NPs and PAs? | N=37 (%)* | N=26 (%)* | |
| Mean no. of patients | 6.81 | 6.18 | 0.45 |
| N/A | 10 (27.0%) | 6 (23.1%) | 0.56 |
| Other | 1 (2.7%) | 0 (0.0%) | |
In multivariable adjusted analyses evaluating the association between patient satisfaction and use of APPs (Table 3), no significant differences were observed for patients' rating of the hospital (F[3,95]=0.19; P=0.90) or willingness to recommend the hospital (F[3,95]=0.54; P=0.65). Similarly, no significant differences were observed based on use of APPs for nurse overall job satisfaction (F[3,101]=1.85; P=0.14) or collegial relations with physicians (F[3,101]=0.96; P=0.41).
| Patient Satisfaction | Nurse Satisfaction | Coordination of Care | |||||
|---|---|---|---|---|---|---|---|
| Overall Rating | Willingness to Recommend | RN Overall Job Satisfaction | RN/MD Relations | Chief of Medicine: Inpatient Coordination | Nurse Manager: Inpatient Coordination | Nurse Manager: Discharge Coordination | |
| |||||||
| Intercept | 0.67 (0.14) | 10.20 (0.15) | 30.41 (0.13) | 20.89 (0.07) | 30.78 (0.26) | 30.67 (0.24) | 30.23 (0.26) |
| Facilities with NPs only | 0.06 (0.10) | 0.12 (0.09) | 0.14 (0.09) | 0.02 (0.05) | 10.63 (0.91) | 0.00 (0.19) | 0.42 (0.20)* |
| Facilities with PAs only | 0.06 (0.09) | 0.10 (0.11) | 0.10 (0.10) | 0.06 (0.05) | 10.08 (0.87) | 0.41 (0.22) | 0.36 (0.25) |
| Facilities with both NPs and PAs | 0.02 (0.12) | 0.11 (0.130 | 0.17 (0.11) | 0.00 (0.00) | 0.31 (0.92) | 0.03 (0.27) | 0.21 (0.30) |
| Facilities with neither NPs nor PAs | |||||||
COM ratings of overall inpatient coordination were also nonsignificant (F[3, 100]=2.01; P=0.12), but their ratings of coordination were higher in facilities with NPs only than in those without either NPs or PAs (=1.63, P=0.08). Nurse manager ratings of overall inpatient coordination were not associated with APP use (F[3,91]=1.24; P=0.30), but were marginally lower with facilities using only PAs (=1.48; P=0.06). Nurse manager ratings of discharge coordination showed a significant effect for APP use (F[3,90]=3.30; P=0.02) with facilities having NPs only significantly higher than places without either NPs or PAs (=1.84, P=0.04).
DISCUSSION
Little evidence exists regarding the role of APPs in the inpatient medicine setting,[2] and important deficit concerns in medical knowledge, technical skills, and clinical experience have been raised.[27, 28] These concerns have called into question the appropriateness of involving APPs in the care of medical inpatients with extensive differential diagnoses and complex care requirements.[27, 28] In spite of these concerns, we found widespread use of APPs with almost half of the VHA inpatient medicine services reporting use, which stands in contrast to prior research.[9, 10, 22, 29, 30, 31, 32, 33, 34, 35] APPs practice in a variety of acute and subacute inpatient medicine settings including academic, community, rural, and urban settings without many discernable differences. The spectrum of activities performed by APPs in the VHA is similar to those reported in these inpatient medicine studies, although their scope of practice appears to be much broader than in these few small single academic center studies.[10, 22, 29, 30, 31, 32, 33, 34, 35, 36] For example, only 11% of hospitalist PAs did procedures in a 2006 Society of Hospital Medicine survey, whereas 50% did in our study.[36]
Interestingly, we found that VHA NPs and PAs perform very similar tasks with similar caseloads despite differences in their background, training, regulation, reimbursement, and the longstanding observation that nurse practitioners are not physician assistants.[1, 3, 4, 5] These findings may reflect that APP scope can be more extensive in the VHA. For example, PAs in the VHA practice under federal jurisdiction and can bypass state legislation of scope of practice.[13] It also may reflect ongoing expansion of the role of APPs in the healthcare system since prior studies.[33, 36]
We did, however, note a few significant differences in NP and PA scope. PAs are twice as likely to perform procedures as NPs in inpatient medicine. It is unclear why PAs may do more procedures, as acute care NPs also are commonly taught and perform similar procedures.[33] We also found that PAs teach nonphysician students twice as often as NPs. This may reflect the deep commitment shown by the VHA to PA education dating back to the 1960s.[13] Finally, we found that PAs were significantly more likely to work weekends and federal holidays, a finding that may have implications for inpatient medicine services hiring APPs. Although not statistically significant, PAs, in general, performed more clinically oriented tasks like history and physicals and more often worked directly with hospitalists.
We found no difference in patient satisfaction or nurse satisfaction related to the presence of APPs, consistent with prior studies, where higher levels of satisfaction with APPs are observed in primary care but not hospital settings.[2, 10] However, it is surprising that no differences were observed for nurse satisfaction. NPs traditionally have a nursing focus, which might foster better relationships with nurses.[22] Expecting changes in either patient or nurse satisfaction with just the addition of APPs in the inpatient medicine setting without addressing other factors may be unrealistic. Patient satisfaction is a complex amalgam of various factors including patient expectations, sociodemographics, emotional and physical state, quality of care, and physician communication.[24] Similarly, nurse satisfaction depends on many factors including job stress, nursephysician collaboration, autonomy, staffing, and support.[37]
Finally, we found higher perception of both overall coordination of inpatient care and discharge coordination on services with NPs. A primary reason stated by medical centers to hire APPs is to improve continuity of care.[9] Prior research has shown better communication and collaboration between nurses, physicians, and NPs on inpatient medicine services.[21] NPs may feel that coordination of care is a major focus for their profession and may spend more time than physicians on care coordination activities.[38] Moreover, their background in both nursing and medicine may better lend itself to coordinating care between disciplines.[39] However, we were surprised to find that services with PAs had lower ratings of overall coordination by nurse managers given that care coordination also is a core competency of PA practice and a primary reason for medical centers to employ them.[9] The lack of a nursing background for PAs and potentially less overall medical experience than NPs possibly may contribute to this finding. However, our study does not suggest a direct explanation for this finding, and we had no measure of prior clinical experience, and thus it should be an area for further research.
There are a number of limitations to our study. First, findings from the VHA may not be generalizable to other healthcare systems.[39] However, VHA inpatient medicine services are, in general, structured similarly to non‐VHA settings and are often affiliated with academic medical centers. Further, this is the largest study to our knowledge to look at the specific roles and perceptions of care provided by both NPs and PAs in inpatient medicine. Second, we did not measure other outcomes of care that may be affected by the use of APPs, such as clinical outcomes, process of care measures, or cost‐effectiveness, some of which have been shown in small studies to be impacted by APPs in inpatient medicine.[10, 22, 29, 30, 31, 32, 33, 34, 35] Third, we are unable to attribute causality to our findings and may not have accounted for all the differences between services. Ideally, a randomized controlled trial of APPs in inpatient medicine would be helpful to address these concerns, but no such trials have been conducted. Finally, we did not survey APPs directly, but surveyed the chiefs of their service instead. The chiefs, however, are directly responsible for the scope of practice of all providers on their service and were directly involved in performance evaluations of most of these practitioners.
In conclusion, we found that NPs and PAs, functioning as APP hospitalists are more widely used and have a broader scope of practice on inpatient medicine than previously known or appreciated, at least in the VHA. In spite of their different backgrounds, training, regulations, and reimbursements, they appear to have a similar scope of practice with few differences in roles or perceived impact. Their impact on inpatient healthcare should be a subject of future research. In the meantime, inpatient medicine services should factor these findings into their decision making as they rapidly expand the use of APPs to provide better care to their patients and to address challenges in healthcare reform.[3, 27, 28, 40]
Acknowledgments
Disclosures: The work reported here was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (IIR 08067) and the Comprehensive Access & Delivery Research and Evaluation (CADRE) Center at the Iowa City VAMC (CIN 13412), and the Center for Healthcare Organization and Implementation Research (CHOIR) at the Boston VA Healthcare System (HFP 04145). The funders did not play any role in the design and conduct of the study; in the collection, analysis, and interpretation of data; and in preparation, review, and approval of the manuscript. The authors do not have any conflicts of interest or financial relationships related to the content of this manuscript. The authors had full access to and take full responsibility for the integrity of the data and the accuracy of the data analysis. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
- . Advanced nurse practitioners and physician assistants: what is the difference? Comparing the USA and UK. Hosp Med. 2001;62:169–171.
- , , , , , . The impact of nonphysician clinicians: do they improve the quality and cost‐effectiveness of health care services? Med Care Res Rev. 2009;66(6 suppl):36S–89S.
- . Will the NP workforce grow in the future? New forecasts and implications for healthcare delivery. Med Care. 2012;50(7):606–610.
- , , . The certified physician assistant iin the United States: a 2011 snapshot. JAAPA. 2012;25(4):58.
- , , . The use of nonphysician providers in adult intensive care units. Am J Respir Crit Care Med. 2012;185(6):600–605.
- American Academy of Physician Assistants. State law issues: supervision of PAs: access and excellence in patient care. October 2011. Available at: http://www.aapa.org/WorkArea/DownloadAsset.aspx?id=632. Accessed on June 22, 2014.
- Centers for Medicare 5(2):99–102.
- , , , . Physician assistant and nurse practitioner utilization in academic medical centers. Am J Med Qual. 2011;26(6):452–460.
- , , , et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361–368.
- American Academy of Physician Assistants. 2010 AAPA Physician Assistant Census. Alexandria, VA, 2011. Available at: http://www.aapa.org/WorkArea/DownloadAsset.aspx?id=838. Accessed on June 22, 2014.
- . 2009–2010 AANP national nurse practitioner sample survey: an overview. J Am Acad Nurse Pract. 2011;23(5):266–268.
- , . Physician assistants working in the Department of Veterans Affairs. JAAPA 2010;23(11):41–44.
- National Center for Veterans Analysis and Statistics. Selected Veterans Health Administration Characteristics: FY2002 to FY2012. 2013; http://www.va.gov/vetdata/docs/Utilization/VHAStats.xls. Accessed January 7, 2014.
- , , , . The physician assistant profession and military veterans. Mil Med. 2011;176(2):197–203.
- , , , . Veterans' perceptions of care by nurse practitioners, physician assistants, and physicians: a comparison from satisfaction surveys. J Am Acad Nurse Pract. 2010;22(3):170–176.
- , , , . Nurse practitioners as primary care providers within the VA. Mil Med. 2011;176(7):791–797.
- . Federally employed physician assistants. Mil Med. 2008;173(9):895–899.
- , , , , . Variations in nurse practitioner use in Veterans Affairs primary care practices. Health Serv Res. 2004;39(4 pt 1):887–904.
- , , , , . The association of hospital characteristics and quality improvement activities in inpatient medical services. J Gen Intern Med. 2014;29(5):715–722.
- , , , . Effect of a multidisciplinary intervention on communication and collaboration among physicians and nurses. Am J Crit Care. 2005;14(1):71–77.
- , , , , . Utilization‐focused evaluation of acute care nurse practitioner role. Outcomes Manag Nurs Pract. 1998;2(4):152–160; quiz 160–151.
- , , , , . Factors affecting the use of patient survey data for quality improvement in the Veterans Health Administration. BMC Health Serv Res. 2011;11:334.
- , , , . Patients' perception of hospital care in the United States. N Engl J Med. 2008;359(18):1921–1931.
- , , , et al. Nurse staffing and patient outcomes in Veterans Affairs hospitals. J Nurs Adm. 2005;35(10):459–466.
- . Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002;25(3):176–188.
- , , , . Broadening the scope of nursing practice. N Engl J Med. 2011;364(3):193–196.
- . Expanding the role of advanced nurse practitioners—risks and rewards. N Engl J Med. 2013;368(20):1935–1941.
- , , , et al. The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs. J Nurs Adm. 2006;36(2):79–85.
- , , , . Description of a nurse practitioner inpatient service in a public teaching hospital. J Gen Intern Med. 1993;8(1):29–30.
- , . Acute care nurse practitioners: creating and implementing a model of care for an inpatient general medical service. Am J Crit Care. 2002;11(5):448–458.
- , , , , . Improving resource utilization in a teaching hospital: development of a nonteaching service for chest pain admissions. Acad Med. 2006;81(5):432–435.
- , , , et al. Care activities and outcomes of patients cared for by acute care nurse practitioners, physician assistants, and resident physicians: a comparison. Am J Crit Care. 1998;7(4):267–281.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- , , . Resource use by physician assistant services versus teaching services. JAAPA 2002;15(1):33–38, 40, 42.
- . Physician assistants in hospital medicine. In: Ballweg R, Sullivan EM, Brown D, Vetrosky D, eds. Physician Assistant: A Guide to Clinical Practice. 5th ed. Philadelphia, PA: W.B. Saunders; 2013:450–455.
- , , . Factors contributing to nurse job satisfaction in the acute hospital setting: a review of recent literature. J Nurs Manage. 2010;18(7):804–814.
- , , , , . Outcomes of care managed by an acute care nurse practitioner/attending physician team in a subacute medical intensive care unit. Am J Crit Care. 2005;14(2):121–130; quiz 131–132.
- , . The organizational and performance effects of nurse practitioner roles. J Adv Nurs. 2004;47(6):672–681.
- , , . Gaps in the supply of physicians, advance practice nurses, and physician assistants. J Am Coll Surg. 2011;212(6):991–999.
Nurse practitioners (NPs) and physician assistants (PAs) provide healthcare in numerous environments internationally and in the United States.[1, 2] However, their role in the inpatient medicine setting is not well described.[2] In the United States, there are more than 157,000 NPs and 85,000 PAs with projected increases.[3, 4] Although both professions provide direct medical care, there are key differences.[1, 3, 4, 5] NPs typically complete a master's or doctoral degree with advanced clinical training beyond nursing. PAs complete at least 2 years of college courses similar to premedical school requirements. PA programs use a medical school‐based curriculum and train for about 2 years before awarding a master's degree. NPs are regulated through state nursing boards, whereas PAs are regulated through state licensing or medical boards. NPs and PAs have different, yet overlapping scopes of practice. A key difference is that PAs can only practice collaborating with a physician.[5, 6] Overall, both have been shown to provide healthcare that is similar in quality to physicians in specific primary care and surgical settings.[2]
NPs and PAs, often referred to as advanced practice providers (APPs), are employed primarily in outpatient clinic settings providing direct patient care. Most APP studies have focused on the outpatient setting, despite nearly a third of US healthcare expenditure for hospital care.[2, 7] Little is known about APP involvement, specific roles, or impact on outcomes in inpatient medicine settings where they are often referred to as NP or PA hospitalists.[2, 8, 9, 10]
The Veterans Health Administration (VHA) is 1 of the largest employers of APPs, with 3.6% of all NPs and 2.1% of all PAs reported to practice in the VHA.[11, 12, 13] As the largest fully integrated healthcare system in the US, the VHA had 8.8 million veterans enrolled and 703,500 inpatient admissions in 2012.[14] Although this makes the VHA an ideal environment to study the role of APPs, few studies have done so.[13, 15, 16, 17, 18, 19] Although studies have compared NPs and PAs to physicians, very little is known about how NPs differ from PAs when practicing in the same environment.
Our objective was to describe the scope of practice, defined as activities that an individual healthcare practitioner is licensed to perform, of NPs and PAs in the inpatient medicine setting and in the VHA. A secondary objective was to explore important outcomes that could potentially be affected by the presence of NPs and PAs on inpatient medicine.
METHODS
The Organizational Factors and Inpatient Medical Care Quality and Efficiency (OFIM) study provides a basis for this study with detail published elsewhere.[20] The OFIM study was conducted between 2010 and 2011 to evaluate quality of care in VHA inpatient medicine surveying chiefs of medicine (COM), inpatient medicine nurse managers (NM), attending physicians, and extant VHA survey data. The COM is the senior attending physician in charge of departments of medicine that include most medical subspecialties within the VHA medical centers. We used the subset of questions specific to NPs and PAs from the COM and NM surveys. Both COMs and NMs answered identical questions for NPs and PAs in 2 separate sections to avoid overlap of responses. NM survey responses were only used for the coordination of care regression model. Surveys were conducted by e‐mail with up to 4 reminders and a subsequent paper mailing. The inpatient medicine service included adult general internal medicine, medical subspecialties, and critical care. The study was approved by the institutional review boards of the VA Boston Healthcare System, the University of Iowa, and the Iowa City VA Healthcare System.
Measurements
To create our primary variable of interestNP and PA employmentwe used the COM survey. Respondents indicated the number and full‐time employee equivalent (FTEE) values for APPs on inpatient medicine. Based on responses, we created a categorical variable with 4 options: (1) facilities with NPs only, (2) facilities with PAs only, (3) facilities with both NPs and PAs, and (4) facilities with neither NPs nor PAs. We selected 3 outcomes that could potentially be affected by the presence of NPs and PAs on inpatient medicine: patient satisfaction, registered nurse (RN) satisfaction, and coordination of care. Patient satisfaction has been shown to improve with NPs and PAs in prior studies, and improving coordination of care has been a stated goal of medical centers in hiring NPs and PAs.[2, 9] Based on our personal experience and previous studies that have shown that nurses report better communication with NPs than physicians,[21] and that NPs retain a visible nursing component in their NP role,[22] we hypothesized that nurse satisfaction on inpatient medicine would improve with the presence of NPs and PAs.
Patient satisfaction was obtained from the 2010 VHA Survey of Healthcare Experiences of Patients (SHEP).[23] The average response rate was 45%. Approximately half the questions on the SHEP are identical to the Hospital Consumer Assessment of Healthcare Providers and Systems survey (HCAHPS).[24] We examined 2 items: an overall rating and willingness to recommend the facility. For the overall rating, patients rated their hospitalization on a scale from 0 (worst hospital possible) to 10 (best hospital possible). Following HCAHPS guidelines, responses of either 9 or 10 were coded as positive and all other nonmissing responses were coded 0. For willingness to recommend, patients were asked Would you recommend this hospital to your friends and family? using a 4‐point response scale. Responses of definitely and probably no were coded as 0, and probably and definitely yes were coded as 1.
Nurse satisfaction was obtained from the 2011 Veterans Administration Nursing Outcomes Database, an annual survey of VHA nurses that includes demographic, work environment and satisfaction data.[25] The survey, a modified version of the Practice Environment Scale,[26] had a response rate of 52.9% (out of 51,870). For this analysis, we selected only inpatient medicine RNs. We used 2 measures: overall job satisfaction and collegial RN/MD (physician) relations. The former was assessed using the item Compared to what you think it should be, what is your current overall level of satisfaction with your job? The RN/MD relations scale had 3 items, including Physicians and nurses have good working relationships. Both items were evaluated on a similar 5‐point response scale.
Coordination of care was assessed from COM and NM surveys. Overall coordination was evaluated from the COM survey using 1 of 8 items in a question about care coordination, In the past month, how would you rate the following aspects of coordination of patient care inpatient coordination overall. Overall coordination was also evaluated from the NM survey using a similar item. Discharge coordination was evaluated only from the NM survey using 1 of 8 items, Thinking about your experiences during the past month, how would you rate the following aspects of the coordination of patient care related to the discharge process on your inpatient medicine unit discharge coordination overall. When a service had more than 1 response from the NM survey, we took an average of responses to represent the mean score. Responses for all questions ranged from 1 for poor to 5 for excellent (for all of the questions see Supporting Information, Appendix 1, in the online version of this article).
Last, we modeled for several contextual features that could influence outcomes: geographic region as a 4‐item categorical variable; teaching affiliation as a dichotomous variable based on whether the hospital was a member of the Council of Teaching Hospitals, urban or rural status, and facility size as a continuous variable using the number of inpatient medicine service beds.
Statistical Analysis
Descriptive bivariate analyses used t tests, 2, or 2‐tailed Fisher tests when appropriate to compare NP and PA autonomy, tasks, location of care, work schedule, clinical workload, organizational characteristics (ie, academic, urban, facility complexity, inpatient medicine team structure), and performance evaluations.
Next, we examined whether any of the contextual characteristics were associated with use of NPs or PAs using inferential statistics. For patient satisfaction, we developed a hierarchical linear model (HLM) that nested patients within facilities. We controlled for patient age, sex, health status, and length of stay. For nurse satisfaction, individual responses of RNs also were analyzed using the HLM. We controlled for whether the nurse had a leadership position, worked during the daily shift, and job tenure. Ordinary least squares regression was used to examine the 3 measures of coordination from the COM and NM surveys. All analyses were performed using Stata version 12 (StataCorp, College Station, TX) and SAS version 9.2 (SAS Institute Inc., Cary, NC).
RESULTS
Of 123 inpatient medicine services that we surveyed, we included responses from the COMs of 118 services (response rate 95.2%); 5 responses were incomplete. Across 123 inpatient medicine services, we surveyed 264 nurse managers and received 198 responses (75.0%) from 114 inpatient medicine services. In the only model using NM responsesthe care coordination model104 inpatient medicine services had responses from both COM and NM surveys.
Of 118 VHA inpatient medicine services, 56 (47.5%) had APPs, of which 27 (48.2%) had NPs only, 15 (26.8%) had PAs only, and 14 (25.0%) had both NPs and PAs. FTEEs for NPs ranged from 0.5 to 7 (mean=2.22) and for PAs from 1 to 9 (mean=2.23) on the inpatient medicine service per hospital.
There were no significant differences on use of NPs and PAs by teaching affiliation, urban or rural setting, and geography. A significant difference was observed based on bed size (F[3,109]=5.13, P<0.001); facilities with both NPs and PAs had, on average, a larger number of inpatient beds (mean=79.0, standard deviation [SD]=32.3) compared to those without NPs or PAs (mean=50.1, SD=29.4) or with PAs only (mean=44.2, SD=20.5) using Tukey post hoc analysis.
The most common staffing model used staff (attending) physicians only working directly with APPs (N=29, 24.6%). Next most common was an academic model with staff physicians, housestaff, and APPs working together in teams (N=16, 13.4%). For performance evaluations, COMs contributed for both NPs (60.2%) and PAs (56.4%); in fewer cases, COMs completed evaluations of NPs (12.9%) and of PAs (29.0%) without input from other service managers (P=0.02).
Table 1 shows the differences reported by COMs between NPs and PAs scope of practice. Overall, 58.9% of NPs and 65.4% of PAs functioned somewhat or completely autonomously; 23.1% of NPs and 30.8% of PAs worked in a role closer to a ward assistant (eg, work directly with a physician, cowriting orders, and making care decisions with physician oversight). Tasks frequently performed by the majority of NPs and PAs included writing orders (87.9%), coordinating discharge plans (86.7%), communicating with consultants (83.1%), performing history and physicals (82.5%), writing daily progress notes (80.7%), communicating with primary care providers (73.5%), and working directly with hospitalists (72.8%). Less common tasks included serving on committees (46.4%), championing quality improvement activities (40.6%), and research (2.9%). There were no statistically significant differences between tasks, except for a higher proportion of services reporting PAs rather than NPs performing procedures (50.0% vs 22.0%, P=0.02) and teaching nonphysicians (50.0% vs 24.4%, P=0.04).
| Services With NPs, | Services With PAs, | P Value | |
|---|---|---|---|
| |||
| How do NPs and PAs function in conjunction with inpatient medicine staff (attending) physicians in the day‐to‐day care of patients (ie, scope of practice)? | N=39 (%)* | N=26 (%)* | |
| Autonomously, in a manner similar to physicians | 10 (25.6%) | 5 (19.2%) | 0.77 |
| Somewhat autonomously, but with limitations | 13 (33.3%) | 12 (46.2%) | 0.31 |
| In a role closer to a ward assistant | 9 (23.1%) | 8 (30.8%) | 0.57 |
| Administrative | 2 (5.1%) | 0 (0.0%) | 0.51 |
| Other | 6 (15.4%) | 1 (3.8%) | 0.23 |
| What types of tasks do NPs and PAs perform? | N=41 (%)* | N=28 (%)* | |
| Write orders | 34 (82.9%) | 26 (92.9%) | 0.29 |
| Coordinate discharge plans | 33 (80.5%) | 26 (92.9%) | 0.18 |
| Communicate with consultants | 33 (80.5%) | 24 (85.7%) | 0.75 |
| History and physicals | 31 (75.6%) | 25 (89.3%) | 0.22 |
| Daily progress notes | 31 (75.6%) | 24 (85.7%) | 0.37 |
| Communicate with primary care providers | 31 (75.6%) | 20 (71.4% | 0.78 |
| Work directly with hospitalists | 26 (63.4%) | 23 (82.1%) | 0.18 |
| Committees | 16 (39.0%) | 16 (57.1%) | 0.15 |
| Champion quality improvement activities | 14 (34.1%) | 14 (50.0%) | 0.22 |
| Teach nonphysician students | 10 (24.4%) | 14 (50.0%) | 0.04 |
| Perform procedures | 9 (22.0%) | 14 (50.0%) | 0.02 |
| Research | 1 (2.4%) | 1 (3.6%) | 1.00 |
| Other | 6 (14.6%) | 0 (0.0%) | 0.04 |
Table 2 reports location of practice in the hospital and workload. There were no significant differences in locations where NPs and PAs provided care. Overall, 81.9% of APPs worked in inpatient wards, 23.1% in step‐down units, 18.6% in intensive care units, 13.8% in skilled care units, and 4.9% in other locations. In addition, 97.4% of NPs and 89.3% of PAs worked weekdays, whereas only 7.9% of NPs and 17.9% of PAs worked nights. More PAs than NPs worked federal holidays (32.1% vs 7.9%, P=0.02) and weekends (32.1% vs 13.2%, P=0.08). Most NPs and PAs handled a caseload of 4 to 10 patients with a mean of 6.5, with no difference between the 2. The minority, 27.0% of NPs and 23.1% of PAs, were not assigned specific patients.
| Services With NPs | Services With PAs | P Value | |
|---|---|---|---|
| |||
| Where do NPs and PAs provide care? | N=38 (%)* | N=28 (%)* | |
| Wards | 31 (81.6%) | 23 (82.1%) | 1.00 |
| Step‐down unit | 8 (21.1%) | 7 (25.0%) | 0.77 |
| Intensive care unit | 6 (15.8%) | 6 (21.4%) | 0.75 |
| Skilled care units | 5 (13.2%) | 4 (14.3%) | 1.00 |
| Other | 1 (2.6%) | 2 (7.1%) | 0.57 |
| What are NPs and PAs tours of duty? | N=38 (%)* | N=28 (%)* | |
| Weekdays | 37 (97.4%) | 25 (89.3%) | 0.30 |
| Weekends | 5 (13.2%) | 9 (32.1%) | 0.08 |
| Nights | 3 (7.9%) | 5 (17.9%) | 0.27 |
| Federal holidays | 3 (7.9%) | 9 (32.1%) | 0.02 |
| Other | 2 (5.3%) | 1 (3.6%) | 1.00 |
| What is the average clinical workload for NPs and PAs? | N=37 (%)* | N=26 (%)* | |
| Mean no. of patients | 6.81 | 6.18 | 0.45 |
| N/A | 10 (27.0%) | 6 (23.1%) | 0.56 |
| Other | 1 (2.7%) | 0 (0.0%) | |
In multivariable adjusted analyses evaluating the association between patient satisfaction and use of APPs (Table 3), no significant differences were observed for patients' rating of the hospital (F[3,95]=0.19; P=0.90) or willingness to recommend the hospital (F[3,95]=0.54; P=0.65). Similarly, no significant differences were observed based on use of APPs for nurse overall job satisfaction (F[3,101]=1.85; P=0.14) or collegial relations with physicians (F[3,101]=0.96; P=0.41).
| Patient Satisfaction | Nurse Satisfaction | Coordination of Care | |||||
|---|---|---|---|---|---|---|---|
| Overall Rating | Willingness to Recommend | RN Overall Job Satisfaction | RN/MD Relations | Chief of Medicine: Inpatient Coordination | Nurse Manager: Inpatient Coordination | Nurse Manager: Discharge Coordination | |
| |||||||
| Intercept | 0.67 (0.14) | 10.20 (0.15) | 30.41 (0.13) | 20.89 (0.07) | 30.78 (0.26) | 30.67 (0.24) | 30.23 (0.26) |
| Facilities with NPs only | 0.06 (0.10) | 0.12 (0.09) | 0.14 (0.09) | 0.02 (0.05) | 10.63 (0.91) | 0.00 (0.19) | 0.42 (0.20)* |
| Facilities with PAs only | 0.06 (0.09) | 0.10 (0.11) | 0.10 (0.10) | 0.06 (0.05) | 10.08 (0.87) | 0.41 (0.22) | 0.36 (0.25) |
| Facilities with both NPs and PAs | 0.02 (0.12) | 0.11 (0.130 | 0.17 (0.11) | 0.00 (0.00) | 0.31 (0.92) | 0.03 (0.27) | 0.21 (0.30) |
| Facilities with neither NPs nor PAs | |||||||
COM ratings of overall inpatient coordination were also nonsignificant (F[3, 100]=2.01; P=0.12), but their ratings of coordination were higher in facilities with NPs only than in those without either NPs or PAs (=1.63, P=0.08). Nurse manager ratings of overall inpatient coordination were not associated with APP use (F[3,91]=1.24; P=0.30), but were marginally lower with facilities using only PAs (=1.48; P=0.06). Nurse manager ratings of discharge coordination showed a significant effect for APP use (F[3,90]=3.30; P=0.02) with facilities having NPs only significantly higher than places without either NPs or PAs (=1.84, P=0.04).
DISCUSSION
Little evidence exists regarding the role of APPs in the inpatient medicine setting,[2] and important deficit concerns in medical knowledge, technical skills, and clinical experience have been raised.[27, 28] These concerns have called into question the appropriateness of involving APPs in the care of medical inpatients with extensive differential diagnoses and complex care requirements.[27, 28] In spite of these concerns, we found widespread use of APPs with almost half of the VHA inpatient medicine services reporting use, which stands in contrast to prior research.[9, 10, 22, 29, 30, 31, 32, 33, 34, 35] APPs practice in a variety of acute and subacute inpatient medicine settings including academic, community, rural, and urban settings without many discernable differences. The spectrum of activities performed by APPs in the VHA is similar to those reported in these inpatient medicine studies, although their scope of practice appears to be much broader than in these few small single academic center studies.[10, 22, 29, 30, 31, 32, 33, 34, 35, 36] For example, only 11% of hospitalist PAs did procedures in a 2006 Society of Hospital Medicine survey, whereas 50% did in our study.[36]
Interestingly, we found that VHA NPs and PAs perform very similar tasks with similar caseloads despite differences in their background, training, regulation, reimbursement, and the longstanding observation that nurse practitioners are not physician assistants.[1, 3, 4, 5] These findings may reflect that APP scope can be more extensive in the VHA. For example, PAs in the VHA practice under federal jurisdiction and can bypass state legislation of scope of practice.[13] It also may reflect ongoing expansion of the role of APPs in the healthcare system since prior studies.[33, 36]
We did, however, note a few significant differences in NP and PA scope. PAs are twice as likely to perform procedures as NPs in inpatient medicine. It is unclear why PAs may do more procedures, as acute care NPs also are commonly taught and perform similar procedures.[33] We also found that PAs teach nonphysician students twice as often as NPs. This may reflect the deep commitment shown by the VHA to PA education dating back to the 1960s.[13] Finally, we found that PAs were significantly more likely to work weekends and federal holidays, a finding that may have implications for inpatient medicine services hiring APPs. Although not statistically significant, PAs, in general, performed more clinically oriented tasks like history and physicals and more often worked directly with hospitalists.
We found no difference in patient satisfaction or nurse satisfaction related to the presence of APPs, consistent with prior studies, where higher levels of satisfaction with APPs are observed in primary care but not hospital settings.[2, 10] However, it is surprising that no differences were observed for nurse satisfaction. NPs traditionally have a nursing focus, which might foster better relationships with nurses.[22] Expecting changes in either patient or nurse satisfaction with just the addition of APPs in the inpatient medicine setting without addressing other factors may be unrealistic. Patient satisfaction is a complex amalgam of various factors including patient expectations, sociodemographics, emotional and physical state, quality of care, and physician communication.[24] Similarly, nurse satisfaction depends on many factors including job stress, nursephysician collaboration, autonomy, staffing, and support.[37]
Finally, we found higher perception of both overall coordination of inpatient care and discharge coordination on services with NPs. A primary reason stated by medical centers to hire APPs is to improve continuity of care.[9] Prior research has shown better communication and collaboration between nurses, physicians, and NPs on inpatient medicine services.[21] NPs may feel that coordination of care is a major focus for their profession and may spend more time than physicians on care coordination activities.[38] Moreover, their background in both nursing and medicine may better lend itself to coordinating care between disciplines.[39] However, we were surprised to find that services with PAs had lower ratings of overall coordination by nurse managers given that care coordination also is a core competency of PA practice and a primary reason for medical centers to employ them.[9] The lack of a nursing background for PAs and potentially less overall medical experience than NPs possibly may contribute to this finding. However, our study does not suggest a direct explanation for this finding, and we had no measure of prior clinical experience, and thus it should be an area for further research.
There are a number of limitations to our study. First, findings from the VHA may not be generalizable to other healthcare systems.[39] However, VHA inpatient medicine services are, in general, structured similarly to non‐VHA settings and are often affiliated with academic medical centers. Further, this is the largest study to our knowledge to look at the specific roles and perceptions of care provided by both NPs and PAs in inpatient medicine. Second, we did not measure other outcomes of care that may be affected by the use of APPs, such as clinical outcomes, process of care measures, or cost‐effectiveness, some of which have been shown in small studies to be impacted by APPs in inpatient medicine.[10, 22, 29, 30, 31, 32, 33, 34, 35] Third, we are unable to attribute causality to our findings and may not have accounted for all the differences between services. Ideally, a randomized controlled trial of APPs in inpatient medicine would be helpful to address these concerns, but no such trials have been conducted. Finally, we did not survey APPs directly, but surveyed the chiefs of their service instead. The chiefs, however, are directly responsible for the scope of practice of all providers on their service and were directly involved in performance evaluations of most of these practitioners.
In conclusion, we found that NPs and PAs, functioning as APP hospitalists are more widely used and have a broader scope of practice on inpatient medicine than previously known or appreciated, at least in the VHA. In spite of their different backgrounds, training, regulations, and reimbursements, they appear to have a similar scope of practice with few differences in roles or perceived impact. Their impact on inpatient healthcare should be a subject of future research. In the meantime, inpatient medicine services should factor these findings into their decision making as they rapidly expand the use of APPs to provide better care to their patients and to address challenges in healthcare reform.[3, 27, 28, 40]
Acknowledgments
Disclosures: The work reported here was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (IIR 08067) and the Comprehensive Access & Delivery Research and Evaluation (CADRE) Center at the Iowa City VAMC (CIN 13412), and the Center for Healthcare Organization and Implementation Research (CHOIR) at the Boston VA Healthcare System (HFP 04145). The funders did not play any role in the design and conduct of the study; in the collection, analysis, and interpretation of data; and in preparation, review, and approval of the manuscript. The authors do not have any conflicts of interest or financial relationships related to the content of this manuscript. The authors had full access to and take full responsibility for the integrity of the data and the accuracy of the data analysis. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Nurse practitioners (NPs) and physician assistants (PAs) provide healthcare in numerous environments internationally and in the United States.[1, 2] However, their role in the inpatient medicine setting is not well described.[2] In the United States, there are more than 157,000 NPs and 85,000 PAs with projected increases.[3, 4] Although both professions provide direct medical care, there are key differences.[1, 3, 4, 5] NPs typically complete a master's or doctoral degree with advanced clinical training beyond nursing. PAs complete at least 2 years of college courses similar to premedical school requirements. PA programs use a medical school‐based curriculum and train for about 2 years before awarding a master's degree. NPs are regulated through state nursing boards, whereas PAs are regulated through state licensing or medical boards. NPs and PAs have different, yet overlapping scopes of practice. A key difference is that PAs can only practice collaborating with a physician.[5, 6] Overall, both have been shown to provide healthcare that is similar in quality to physicians in specific primary care and surgical settings.[2]
NPs and PAs, often referred to as advanced practice providers (APPs), are employed primarily in outpatient clinic settings providing direct patient care. Most APP studies have focused on the outpatient setting, despite nearly a third of US healthcare expenditure for hospital care.[2, 7] Little is known about APP involvement, specific roles, or impact on outcomes in inpatient medicine settings where they are often referred to as NP or PA hospitalists.[2, 8, 9, 10]
The Veterans Health Administration (VHA) is 1 of the largest employers of APPs, with 3.6% of all NPs and 2.1% of all PAs reported to practice in the VHA.[11, 12, 13] As the largest fully integrated healthcare system in the US, the VHA had 8.8 million veterans enrolled and 703,500 inpatient admissions in 2012.[14] Although this makes the VHA an ideal environment to study the role of APPs, few studies have done so.[13, 15, 16, 17, 18, 19] Although studies have compared NPs and PAs to physicians, very little is known about how NPs differ from PAs when practicing in the same environment.
Our objective was to describe the scope of practice, defined as activities that an individual healthcare practitioner is licensed to perform, of NPs and PAs in the inpatient medicine setting and in the VHA. A secondary objective was to explore important outcomes that could potentially be affected by the presence of NPs and PAs on inpatient medicine.
METHODS
The Organizational Factors and Inpatient Medical Care Quality and Efficiency (OFIM) study provides a basis for this study with detail published elsewhere.[20] The OFIM study was conducted between 2010 and 2011 to evaluate quality of care in VHA inpatient medicine surveying chiefs of medicine (COM), inpatient medicine nurse managers (NM), attending physicians, and extant VHA survey data. The COM is the senior attending physician in charge of departments of medicine that include most medical subspecialties within the VHA medical centers. We used the subset of questions specific to NPs and PAs from the COM and NM surveys. Both COMs and NMs answered identical questions for NPs and PAs in 2 separate sections to avoid overlap of responses. NM survey responses were only used for the coordination of care regression model. Surveys were conducted by e‐mail with up to 4 reminders and a subsequent paper mailing. The inpatient medicine service included adult general internal medicine, medical subspecialties, and critical care. The study was approved by the institutional review boards of the VA Boston Healthcare System, the University of Iowa, and the Iowa City VA Healthcare System.
Measurements
To create our primary variable of interestNP and PA employmentwe used the COM survey. Respondents indicated the number and full‐time employee equivalent (FTEE) values for APPs on inpatient medicine. Based on responses, we created a categorical variable with 4 options: (1) facilities with NPs only, (2) facilities with PAs only, (3) facilities with both NPs and PAs, and (4) facilities with neither NPs nor PAs. We selected 3 outcomes that could potentially be affected by the presence of NPs and PAs on inpatient medicine: patient satisfaction, registered nurse (RN) satisfaction, and coordination of care. Patient satisfaction has been shown to improve with NPs and PAs in prior studies, and improving coordination of care has been a stated goal of medical centers in hiring NPs and PAs.[2, 9] Based on our personal experience and previous studies that have shown that nurses report better communication with NPs than physicians,[21] and that NPs retain a visible nursing component in their NP role,[22] we hypothesized that nurse satisfaction on inpatient medicine would improve with the presence of NPs and PAs.
Patient satisfaction was obtained from the 2010 VHA Survey of Healthcare Experiences of Patients (SHEP).[23] The average response rate was 45%. Approximately half the questions on the SHEP are identical to the Hospital Consumer Assessment of Healthcare Providers and Systems survey (HCAHPS).[24] We examined 2 items: an overall rating and willingness to recommend the facility. For the overall rating, patients rated their hospitalization on a scale from 0 (worst hospital possible) to 10 (best hospital possible). Following HCAHPS guidelines, responses of either 9 or 10 were coded as positive and all other nonmissing responses were coded 0. For willingness to recommend, patients were asked Would you recommend this hospital to your friends and family? using a 4‐point response scale. Responses of definitely and probably no were coded as 0, and probably and definitely yes were coded as 1.
Nurse satisfaction was obtained from the 2011 Veterans Administration Nursing Outcomes Database, an annual survey of VHA nurses that includes demographic, work environment and satisfaction data.[25] The survey, a modified version of the Practice Environment Scale,[26] had a response rate of 52.9% (out of 51,870). For this analysis, we selected only inpatient medicine RNs. We used 2 measures: overall job satisfaction and collegial RN/MD (physician) relations. The former was assessed using the item Compared to what you think it should be, what is your current overall level of satisfaction with your job? The RN/MD relations scale had 3 items, including Physicians and nurses have good working relationships. Both items were evaluated on a similar 5‐point response scale.
Coordination of care was assessed from COM and NM surveys. Overall coordination was evaluated from the COM survey using 1 of 8 items in a question about care coordination, In the past month, how would you rate the following aspects of coordination of patient care inpatient coordination overall. Overall coordination was also evaluated from the NM survey using a similar item. Discharge coordination was evaluated only from the NM survey using 1 of 8 items, Thinking about your experiences during the past month, how would you rate the following aspects of the coordination of patient care related to the discharge process on your inpatient medicine unit discharge coordination overall. When a service had more than 1 response from the NM survey, we took an average of responses to represent the mean score. Responses for all questions ranged from 1 for poor to 5 for excellent (for all of the questions see Supporting Information, Appendix 1, in the online version of this article).
Last, we modeled for several contextual features that could influence outcomes: geographic region as a 4‐item categorical variable; teaching affiliation as a dichotomous variable based on whether the hospital was a member of the Council of Teaching Hospitals, urban or rural status, and facility size as a continuous variable using the number of inpatient medicine service beds.
Statistical Analysis
Descriptive bivariate analyses used t tests, 2, or 2‐tailed Fisher tests when appropriate to compare NP and PA autonomy, tasks, location of care, work schedule, clinical workload, organizational characteristics (ie, academic, urban, facility complexity, inpatient medicine team structure), and performance evaluations.
Next, we examined whether any of the contextual characteristics were associated with use of NPs or PAs using inferential statistics. For patient satisfaction, we developed a hierarchical linear model (HLM) that nested patients within facilities. We controlled for patient age, sex, health status, and length of stay. For nurse satisfaction, individual responses of RNs also were analyzed using the HLM. We controlled for whether the nurse had a leadership position, worked during the daily shift, and job tenure. Ordinary least squares regression was used to examine the 3 measures of coordination from the COM and NM surveys. All analyses were performed using Stata version 12 (StataCorp, College Station, TX) and SAS version 9.2 (SAS Institute Inc., Cary, NC).
RESULTS
Of 123 inpatient medicine services that we surveyed, we included responses from the COMs of 118 services (response rate 95.2%); 5 responses were incomplete. Across 123 inpatient medicine services, we surveyed 264 nurse managers and received 198 responses (75.0%) from 114 inpatient medicine services. In the only model using NM responsesthe care coordination model104 inpatient medicine services had responses from both COM and NM surveys.
Of 118 VHA inpatient medicine services, 56 (47.5%) had APPs, of which 27 (48.2%) had NPs only, 15 (26.8%) had PAs only, and 14 (25.0%) had both NPs and PAs. FTEEs for NPs ranged from 0.5 to 7 (mean=2.22) and for PAs from 1 to 9 (mean=2.23) on the inpatient medicine service per hospital.
There were no significant differences on use of NPs and PAs by teaching affiliation, urban or rural setting, and geography. A significant difference was observed based on bed size (F[3,109]=5.13, P<0.001); facilities with both NPs and PAs had, on average, a larger number of inpatient beds (mean=79.0, standard deviation [SD]=32.3) compared to those without NPs or PAs (mean=50.1, SD=29.4) or with PAs only (mean=44.2, SD=20.5) using Tukey post hoc analysis.
The most common staffing model used staff (attending) physicians only working directly with APPs (N=29, 24.6%). Next most common was an academic model with staff physicians, housestaff, and APPs working together in teams (N=16, 13.4%). For performance evaluations, COMs contributed for both NPs (60.2%) and PAs (56.4%); in fewer cases, COMs completed evaluations of NPs (12.9%) and of PAs (29.0%) without input from other service managers (P=0.02).
Table 1 shows the differences reported by COMs between NPs and PAs scope of practice. Overall, 58.9% of NPs and 65.4% of PAs functioned somewhat or completely autonomously; 23.1% of NPs and 30.8% of PAs worked in a role closer to a ward assistant (eg, work directly with a physician, cowriting orders, and making care decisions with physician oversight). Tasks frequently performed by the majority of NPs and PAs included writing orders (87.9%), coordinating discharge plans (86.7%), communicating with consultants (83.1%), performing history and physicals (82.5%), writing daily progress notes (80.7%), communicating with primary care providers (73.5%), and working directly with hospitalists (72.8%). Less common tasks included serving on committees (46.4%), championing quality improvement activities (40.6%), and research (2.9%). There were no statistically significant differences between tasks, except for a higher proportion of services reporting PAs rather than NPs performing procedures (50.0% vs 22.0%, P=0.02) and teaching nonphysicians (50.0% vs 24.4%, P=0.04).
| Services With NPs, | Services With PAs, | P Value | |
|---|---|---|---|
| |||
| How do NPs and PAs function in conjunction with inpatient medicine staff (attending) physicians in the day‐to‐day care of patients (ie, scope of practice)? | N=39 (%)* | N=26 (%)* | |
| Autonomously, in a manner similar to physicians | 10 (25.6%) | 5 (19.2%) | 0.77 |
| Somewhat autonomously, but with limitations | 13 (33.3%) | 12 (46.2%) | 0.31 |
| In a role closer to a ward assistant | 9 (23.1%) | 8 (30.8%) | 0.57 |
| Administrative | 2 (5.1%) | 0 (0.0%) | 0.51 |
| Other | 6 (15.4%) | 1 (3.8%) | 0.23 |
| What types of tasks do NPs and PAs perform? | N=41 (%)* | N=28 (%)* | |
| Write orders | 34 (82.9%) | 26 (92.9%) | 0.29 |
| Coordinate discharge plans | 33 (80.5%) | 26 (92.9%) | 0.18 |
| Communicate with consultants | 33 (80.5%) | 24 (85.7%) | 0.75 |
| History and physicals | 31 (75.6%) | 25 (89.3%) | 0.22 |
| Daily progress notes | 31 (75.6%) | 24 (85.7%) | 0.37 |
| Communicate with primary care providers | 31 (75.6%) | 20 (71.4% | 0.78 |
| Work directly with hospitalists | 26 (63.4%) | 23 (82.1%) | 0.18 |
| Committees | 16 (39.0%) | 16 (57.1%) | 0.15 |
| Champion quality improvement activities | 14 (34.1%) | 14 (50.0%) | 0.22 |
| Teach nonphysician students | 10 (24.4%) | 14 (50.0%) | 0.04 |
| Perform procedures | 9 (22.0%) | 14 (50.0%) | 0.02 |
| Research | 1 (2.4%) | 1 (3.6%) | 1.00 |
| Other | 6 (14.6%) | 0 (0.0%) | 0.04 |
Table 2 reports location of practice in the hospital and workload. There were no significant differences in locations where NPs and PAs provided care. Overall, 81.9% of APPs worked in inpatient wards, 23.1% in step‐down units, 18.6% in intensive care units, 13.8% in skilled care units, and 4.9% in other locations. In addition, 97.4% of NPs and 89.3% of PAs worked weekdays, whereas only 7.9% of NPs and 17.9% of PAs worked nights. More PAs than NPs worked federal holidays (32.1% vs 7.9%, P=0.02) and weekends (32.1% vs 13.2%, P=0.08). Most NPs and PAs handled a caseload of 4 to 10 patients with a mean of 6.5, with no difference between the 2. The minority, 27.0% of NPs and 23.1% of PAs, were not assigned specific patients.
| Services With NPs | Services With PAs | P Value | |
|---|---|---|---|
| |||
| Where do NPs and PAs provide care? | N=38 (%)* | N=28 (%)* | |
| Wards | 31 (81.6%) | 23 (82.1%) | 1.00 |
| Step‐down unit | 8 (21.1%) | 7 (25.0%) | 0.77 |
| Intensive care unit | 6 (15.8%) | 6 (21.4%) | 0.75 |
| Skilled care units | 5 (13.2%) | 4 (14.3%) | 1.00 |
| Other | 1 (2.6%) | 2 (7.1%) | 0.57 |
| What are NPs and PAs tours of duty? | N=38 (%)* | N=28 (%)* | |
| Weekdays | 37 (97.4%) | 25 (89.3%) | 0.30 |
| Weekends | 5 (13.2%) | 9 (32.1%) | 0.08 |
| Nights | 3 (7.9%) | 5 (17.9%) | 0.27 |
| Federal holidays | 3 (7.9%) | 9 (32.1%) | 0.02 |
| Other | 2 (5.3%) | 1 (3.6%) | 1.00 |
| What is the average clinical workload for NPs and PAs? | N=37 (%)* | N=26 (%)* | |
| Mean no. of patients | 6.81 | 6.18 | 0.45 |
| N/A | 10 (27.0%) | 6 (23.1%) | 0.56 |
| Other | 1 (2.7%) | 0 (0.0%) | |
In multivariable adjusted analyses evaluating the association between patient satisfaction and use of APPs (Table 3), no significant differences were observed for patients' rating of the hospital (F[3,95]=0.19; P=0.90) or willingness to recommend the hospital (F[3,95]=0.54; P=0.65). Similarly, no significant differences were observed based on use of APPs for nurse overall job satisfaction (F[3,101]=1.85; P=0.14) or collegial relations with physicians (F[3,101]=0.96; P=0.41).
| Patient Satisfaction | Nurse Satisfaction | Coordination of Care | |||||
|---|---|---|---|---|---|---|---|
| Overall Rating | Willingness to Recommend | RN Overall Job Satisfaction | RN/MD Relations | Chief of Medicine: Inpatient Coordination | Nurse Manager: Inpatient Coordination | Nurse Manager: Discharge Coordination | |
| |||||||
| Intercept | 0.67 (0.14) | 10.20 (0.15) | 30.41 (0.13) | 20.89 (0.07) | 30.78 (0.26) | 30.67 (0.24) | 30.23 (0.26) |
| Facilities with NPs only | 0.06 (0.10) | 0.12 (0.09) | 0.14 (0.09) | 0.02 (0.05) | 10.63 (0.91) | 0.00 (0.19) | 0.42 (0.20)* |
| Facilities with PAs only | 0.06 (0.09) | 0.10 (0.11) | 0.10 (0.10) | 0.06 (0.05) | 10.08 (0.87) | 0.41 (0.22) | 0.36 (0.25) |
| Facilities with both NPs and PAs | 0.02 (0.12) | 0.11 (0.130 | 0.17 (0.11) | 0.00 (0.00) | 0.31 (0.92) | 0.03 (0.27) | 0.21 (0.30) |
| Facilities with neither NPs nor PAs | |||||||
COM ratings of overall inpatient coordination were also nonsignificant (F[3, 100]=2.01; P=0.12), but their ratings of coordination were higher in facilities with NPs only than in those without either NPs or PAs (=1.63, P=0.08). Nurse manager ratings of overall inpatient coordination were not associated with APP use (F[3,91]=1.24; P=0.30), but were marginally lower with facilities using only PAs (=1.48; P=0.06). Nurse manager ratings of discharge coordination showed a significant effect for APP use (F[3,90]=3.30; P=0.02) with facilities having NPs only significantly higher than places without either NPs or PAs (=1.84, P=0.04).
DISCUSSION
Little evidence exists regarding the role of APPs in the inpatient medicine setting,[2] and important deficit concerns in medical knowledge, technical skills, and clinical experience have been raised.[27, 28] These concerns have called into question the appropriateness of involving APPs in the care of medical inpatients with extensive differential diagnoses and complex care requirements.[27, 28] In spite of these concerns, we found widespread use of APPs with almost half of the VHA inpatient medicine services reporting use, which stands in contrast to prior research.[9, 10, 22, 29, 30, 31, 32, 33, 34, 35] APPs practice in a variety of acute and subacute inpatient medicine settings including academic, community, rural, and urban settings without many discernable differences. The spectrum of activities performed by APPs in the VHA is similar to those reported in these inpatient medicine studies, although their scope of practice appears to be much broader than in these few small single academic center studies.[10, 22, 29, 30, 31, 32, 33, 34, 35, 36] For example, only 11% of hospitalist PAs did procedures in a 2006 Society of Hospital Medicine survey, whereas 50% did in our study.[36]
Interestingly, we found that VHA NPs and PAs perform very similar tasks with similar caseloads despite differences in their background, training, regulation, reimbursement, and the longstanding observation that nurse practitioners are not physician assistants.[1, 3, 4, 5] These findings may reflect that APP scope can be more extensive in the VHA. For example, PAs in the VHA practice under federal jurisdiction and can bypass state legislation of scope of practice.[13] It also may reflect ongoing expansion of the role of APPs in the healthcare system since prior studies.[33, 36]
We did, however, note a few significant differences in NP and PA scope. PAs are twice as likely to perform procedures as NPs in inpatient medicine. It is unclear why PAs may do more procedures, as acute care NPs also are commonly taught and perform similar procedures.[33] We also found that PAs teach nonphysician students twice as often as NPs. This may reflect the deep commitment shown by the VHA to PA education dating back to the 1960s.[13] Finally, we found that PAs were significantly more likely to work weekends and federal holidays, a finding that may have implications for inpatient medicine services hiring APPs. Although not statistically significant, PAs, in general, performed more clinically oriented tasks like history and physicals and more often worked directly with hospitalists.
We found no difference in patient satisfaction or nurse satisfaction related to the presence of APPs, consistent with prior studies, where higher levels of satisfaction with APPs are observed in primary care but not hospital settings.[2, 10] However, it is surprising that no differences were observed for nurse satisfaction. NPs traditionally have a nursing focus, which might foster better relationships with nurses.[22] Expecting changes in either patient or nurse satisfaction with just the addition of APPs in the inpatient medicine setting without addressing other factors may be unrealistic. Patient satisfaction is a complex amalgam of various factors including patient expectations, sociodemographics, emotional and physical state, quality of care, and physician communication.[24] Similarly, nurse satisfaction depends on many factors including job stress, nursephysician collaboration, autonomy, staffing, and support.[37]
Finally, we found higher perception of both overall coordination of inpatient care and discharge coordination on services with NPs. A primary reason stated by medical centers to hire APPs is to improve continuity of care.[9] Prior research has shown better communication and collaboration between nurses, physicians, and NPs on inpatient medicine services.[21] NPs may feel that coordination of care is a major focus for their profession and may spend more time than physicians on care coordination activities.[38] Moreover, their background in both nursing and medicine may better lend itself to coordinating care between disciplines.[39] However, we were surprised to find that services with PAs had lower ratings of overall coordination by nurse managers given that care coordination also is a core competency of PA practice and a primary reason for medical centers to employ them.[9] The lack of a nursing background for PAs and potentially less overall medical experience than NPs possibly may contribute to this finding. However, our study does not suggest a direct explanation for this finding, and we had no measure of prior clinical experience, and thus it should be an area for further research.
There are a number of limitations to our study. First, findings from the VHA may not be generalizable to other healthcare systems.[39] However, VHA inpatient medicine services are, in general, structured similarly to non‐VHA settings and are often affiliated with academic medical centers. Further, this is the largest study to our knowledge to look at the specific roles and perceptions of care provided by both NPs and PAs in inpatient medicine. Second, we did not measure other outcomes of care that may be affected by the use of APPs, such as clinical outcomes, process of care measures, or cost‐effectiveness, some of which have been shown in small studies to be impacted by APPs in inpatient medicine.[10, 22, 29, 30, 31, 32, 33, 34, 35] Third, we are unable to attribute causality to our findings and may not have accounted for all the differences between services. Ideally, a randomized controlled trial of APPs in inpatient medicine would be helpful to address these concerns, but no such trials have been conducted. Finally, we did not survey APPs directly, but surveyed the chiefs of their service instead. The chiefs, however, are directly responsible for the scope of practice of all providers on their service and were directly involved in performance evaluations of most of these practitioners.
In conclusion, we found that NPs and PAs, functioning as APP hospitalists are more widely used and have a broader scope of practice on inpatient medicine than previously known or appreciated, at least in the VHA. In spite of their different backgrounds, training, regulations, and reimbursements, they appear to have a similar scope of practice with few differences in roles or perceived impact. Their impact on inpatient healthcare should be a subject of future research. In the meantime, inpatient medicine services should factor these findings into their decision making as they rapidly expand the use of APPs to provide better care to their patients and to address challenges in healthcare reform.[3, 27, 28, 40]
Acknowledgments
Disclosures: The work reported here was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (IIR 08067) and the Comprehensive Access & Delivery Research and Evaluation (CADRE) Center at the Iowa City VAMC (CIN 13412), and the Center for Healthcare Organization and Implementation Research (CHOIR) at the Boston VA Healthcare System (HFP 04145). The funders did not play any role in the design and conduct of the study; in the collection, analysis, and interpretation of data; and in preparation, review, and approval of the manuscript. The authors do not have any conflicts of interest or financial relationships related to the content of this manuscript. The authors had full access to and take full responsibility for the integrity of the data and the accuracy of the data analysis. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
- . Advanced nurse practitioners and physician assistants: what is the difference? Comparing the USA and UK. Hosp Med. 2001;62:169–171.
- , , , , , . The impact of nonphysician clinicians: do they improve the quality and cost‐effectiveness of health care services? Med Care Res Rev. 2009;66(6 suppl):36S–89S.
- . Will the NP workforce grow in the future? New forecasts and implications for healthcare delivery. Med Care. 2012;50(7):606–610.
- , , . The certified physician assistant iin the United States: a 2011 snapshot. JAAPA. 2012;25(4):58.
- , , . The use of nonphysician providers in adult intensive care units. Am J Respir Crit Care Med. 2012;185(6):600–605.
- American Academy of Physician Assistants. State law issues: supervision of PAs: access and excellence in patient care. October 2011. Available at: http://www.aapa.org/WorkArea/DownloadAsset.aspx?id=632. Accessed on June 22, 2014.
- Centers for Medicare 5(2):99–102.
- , , , . Physician assistant and nurse practitioner utilization in academic medical centers. Am J Med Qual. 2011;26(6):452–460.
- , , , et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361–368.
- American Academy of Physician Assistants. 2010 AAPA Physician Assistant Census. Alexandria, VA, 2011. Available at: http://www.aapa.org/WorkArea/DownloadAsset.aspx?id=838. Accessed on June 22, 2014.
- . 2009–2010 AANP national nurse practitioner sample survey: an overview. J Am Acad Nurse Pract. 2011;23(5):266–268.
- , . Physician assistants working in the Department of Veterans Affairs. JAAPA 2010;23(11):41–44.
- National Center for Veterans Analysis and Statistics. Selected Veterans Health Administration Characteristics: FY2002 to FY2012. 2013; http://www.va.gov/vetdata/docs/Utilization/VHAStats.xls. Accessed January 7, 2014.
- , , , . The physician assistant profession and military veterans. Mil Med. 2011;176(2):197–203.
- , , , . Veterans' perceptions of care by nurse practitioners, physician assistants, and physicians: a comparison from satisfaction surveys. J Am Acad Nurse Pract. 2010;22(3):170–176.
- , , , . Nurse practitioners as primary care providers within the VA. Mil Med. 2011;176(7):791–797.
- . Federally employed physician assistants. Mil Med. 2008;173(9):895–899.
- , , , , . Variations in nurse practitioner use in Veterans Affairs primary care practices. Health Serv Res. 2004;39(4 pt 1):887–904.
- , , , , . The association of hospital characteristics and quality improvement activities in inpatient medical services. J Gen Intern Med. 2014;29(5):715–722.
- , , , . Effect of a multidisciplinary intervention on communication and collaboration among physicians and nurses. Am J Crit Care. 2005;14(1):71–77.
- , , , , . Utilization‐focused evaluation of acute care nurse practitioner role. Outcomes Manag Nurs Pract. 1998;2(4):152–160; quiz 160–151.
- , , , , . Factors affecting the use of patient survey data for quality improvement in the Veterans Health Administration. BMC Health Serv Res. 2011;11:334.
- , , , . Patients' perception of hospital care in the United States. N Engl J Med. 2008;359(18):1921–1931.
- , , , et al. Nurse staffing and patient outcomes in Veterans Affairs hospitals. J Nurs Adm. 2005;35(10):459–466.
- . Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002;25(3):176–188.
- , , , . Broadening the scope of nursing practice. N Engl J Med. 2011;364(3):193–196.
- . Expanding the role of advanced nurse practitioners—risks and rewards. N Engl J Med. 2013;368(20):1935–1941.
- , , , et al. The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs. J Nurs Adm. 2006;36(2):79–85.
- , , , . Description of a nurse practitioner inpatient service in a public teaching hospital. J Gen Intern Med. 1993;8(1):29–30.
- , . Acute care nurse practitioners: creating and implementing a model of care for an inpatient general medical service. Am J Crit Care. 2002;11(5):448–458.
- , , , , . Improving resource utilization in a teaching hospital: development of a nonteaching service for chest pain admissions. Acad Med. 2006;81(5):432–435.
- , , , et al. Care activities and outcomes of patients cared for by acute care nurse practitioners, physician assistants, and resident physicians: a comparison. Am J Crit Care. 1998;7(4):267–281.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- , , . Resource use by physician assistant services versus teaching services. JAAPA 2002;15(1):33–38, 40, 42.
- . Physician assistants in hospital medicine. In: Ballweg R, Sullivan EM, Brown D, Vetrosky D, eds. Physician Assistant: A Guide to Clinical Practice. 5th ed. Philadelphia, PA: W.B. Saunders; 2013:450–455.
- , , . Factors contributing to nurse job satisfaction in the acute hospital setting: a review of recent literature. J Nurs Manage. 2010;18(7):804–814.
- , , , , . Outcomes of care managed by an acute care nurse practitioner/attending physician team in a subacute medical intensive care unit. Am J Crit Care. 2005;14(2):121–130; quiz 131–132.
- , . The organizational and performance effects of nurse practitioner roles. J Adv Nurs. 2004;47(6):672–681.
- , , . Gaps in the supply of physicians, advance practice nurses, and physician assistants. J Am Coll Surg. 2011;212(6):991–999.
- . Advanced nurse practitioners and physician assistants: what is the difference? Comparing the USA and UK. Hosp Med. 2001;62:169–171.
- , , , , , . The impact of nonphysician clinicians: do they improve the quality and cost‐effectiveness of health care services? Med Care Res Rev. 2009;66(6 suppl):36S–89S.
- . Will the NP workforce grow in the future? New forecasts and implications for healthcare delivery. Med Care. 2012;50(7):606–610.
- , , . The certified physician assistant iin the United States: a 2011 snapshot. JAAPA. 2012;25(4):58.
- , , . The use of nonphysician providers in adult intensive care units. Am J Respir Crit Care Med. 2012;185(6):600–605.
- American Academy of Physician Assistants. State law issues: supervision of PAs: access and excellence in patient care. October 2011. Available at: http://www.aapa.org/WorkArea/DownloadAsset.aspx?id=632. Accessed on June 22, 2014.
- Centers for Medicare 5(2):99–102.
- , , , . Physician assistant and nurse practitioner utilization in academic medical centers. Am J Med Qual. 2011;26(6):452–460.
- , , , et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361–368.
- American Academy of Physician Assistants. 2010 AAPA Physician Assistant Census. Alexandria, VA, 2011. Available at: http://www.aapa.org/WorkArea/DownloadAsset.aspx?id=838. Accessed on June 22, 2014.
- . 2009–2010 AANP national nurse practitioner sample survey: an overview. J Am Acad Nurse Pract. 2011;23(5):266–268.
- , . Physician assistants working in the Department of Veterans Affairs. JAAPA 2010;23(11):41–44.
- National Center for Veterans Analysis and Statistics. Selected Veterans Health Administration Characteristics: FY2002 to FY2012. 2013; http://www.va.gov/vetdata/docs/Utilization/VHAStats.xls. Accessed January 7, 2014.
- , , , . The physician assistant profession and military veterans. Mil Med. 2011;176(2):197–203.
- , , , . Veterans' perceptions of care by nurse practitioners, physician assistants, and physicians: a comparison from satisfaction surveys. J Am Acad Nurse Pract. 2010;22(3):170–176.
- , , , . Nurse practitioners as primary care providers within the VA. Mil Med. 2011;176(7):791–797.
- . Federally employed physician assistants. Mil Med. 2008;173(9):895–899.
- , , , , . Variations in nurse practitioner use in Veterans Affairs primary care practices. Health Serv Res. 2004;39(4 pt 1):887–904.
- , , , , . The association of hospital characteristics and quality improvement activities in inpatient medical services. J Gen Intern Med. 2014;29(5):715–722.
- , , , . Effect of a multidisciplinary intervention on communication and collaboration among physicians and nurses. Am J Crit Care. 2005;14(1):71–77.
- , , , , . Utilization‐focused evaluation of acute care nurse practitioner role. Outcomes Manag Nurs Pract. 1998;2(4):152–160; quiz 160–151.
- , , , , . Factors affecting the use of patient survey data for quality improvement in the Veterans Health Administration. BMC Health Serv Res. 2011;11:334.
- , , , . Patients' perception of hospital care in the United States. N Engl J Med. 2008;359(18):1921–1931.
- , , , et al. Nurse staffing and patient outcomes in Veterans Affairs hospitals. J Nurs Adm. 2005;35(10):459–466.
- . Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002;25(3):176–188.
- , , , . Broadening the scope of nursing practice. N Engl J Med. 2011;364(3):193–196.
- . Expanding the role of advanced nurse practitioners—risks and rewards. N Engl J Med. 2013;368(20):1935–1941.
- , , , et al. The effect of a multidisciplinary hospitalist/physician and advanced practice nurse collaboration on hospital costs. J Nurs Adm. 2006;36(2):79–85.
- , , , . Description of a nurse practitioner inpatient service in a public teaching hospital. J Gen Intern Med. 1993;8(1):29–30.
- , . Acute care nurse practitioners: creating and implementing a model of care for an inpatient general medical service. Am J Crit Care. 2002;11(5):448–458.
- , , , , . Improving resource utilization in a teaching hospital: development of a nonteaching service for chest pain admissions. Acad Med. 2006;81(5):432–435.
- , , , et al. Care activities and outcomes of patients cared for by acute care nurse practitioners, physician assistants, and resident physicians: a comparison. Am J Crit Care. 1998;7(4):267–281.
- , , , et al. Impact of localizing general medical teams to a single nursing unit. J Hosp Med. 2012;7(7):551–556.
- , , . Resource use by physician assistant services versus teaching services. JAAPA 2002;15(1):33–38, 40, 42.
- . Physician assistants in hospital medicine. In: Ballweg R, Sullivan EM, Brown D, Vetrosky D, eds. Physician Assistant: A Guide to Clinical Practice. 5th ed. Philadelphia, PA: W.B. Saunders; 2013:450–455.
- , , . Factors contributing to nurse job satisfaction in the acute hospital setting: a review of recent literature. J Nurs Manage. 2010;18(7):804–814.
- , , , , . Outcomes of care managed by an acute care nurse practitioner/attending physician team in a subacute medical intensive care unit. Am J Crit Care. 2005;14(2):121–130; quiz 131–132.
- , . The organizational and performance effects of nurse practitioner roles. J Adv Nurs. 2004;47(6):672–681.
- , , . Gaps in the supply of physicians, advance practice nurses, and physician assistants. J Am Coll Surg. 2011;212(6):991–999.
© 2014 Society of Hospital Medicine