User login
Arthroscopic SLAP IIb Repair Using Knot-Tying Versus Knotless Suture Anchors: Is There a Difference?
ABSTRACT
The use of knotless suture anchors has increased in popularity; however, there is a paucity of literature examining the difference in clinical outcomes with traditional knotted fixation. It was hypothesized that knotless fixation would provide superior clinical outcomes, improved return to play (RTP), and lower revision rates as compared with traditional knotted fixation in the repair of SLAP IIb tears. Seventy-four athletes who underwent arthroscopic SLAP IIb repair with traditional (n = 42) and knotless anchors (n = 32) by a single surgeon were evaluated after a minimum 2-year follow. Demographic and surgical data, RTP, Kerlan-Jobe Orthopaedic Clinic (KJOC) score, American Shoulder and Elbow Surgeons (ASES) score, stability, strength, and pain scores were compared. Knotless anchors had slightly higher RTP (93.5% vs 90.2%, P = .94) and RTP at the same level (58.1% vs 53.7% P = .81) compared with knotted fixation, but the difference did not reach statistical significance. Knotless anchors were less likely to require revision surgery than traditional anchors (9% vs 17%, P = .50), but the difference was not statistically significant. When comparing knotless and traditional knotted suture anchor repair of type llb SLAP tears, knotless fixation required less revision surgery and had higher RTP, ASES, and KJOC scores; however, statistical significance was not achieved in this relatively small cohort.
Continue to: Injury of the anterosuperior...
Injury of the anterosuperior labrum near the biceps origin was first described by Andrews and colleagues in 1985 in overhead athletes.1 The term SLAP, or a tear in the superior labrum anterior to posterior, was coined a few years later by Snyder and colleagues.2 They described an injury to the superior labrum beginning posteriorly and extending anteriorly, including the “anchor” of the biceps tendon to the labrum. Snyder further delineated SLAP lesions into 4 subtypes, the most common being type II, which he described as “degenerative fraying of the labrum with additional detachment of the superior labrum and biceps from the glenoid resulting in an unstable labral anchor.”2,3 Type II tears are of particular importance as they are the most common SLAP lesions, with an incidence of 55%, and comprise nearly 75% of SLAP repairs performed.2,4
Morgan and colleagues further delineated type II SLAP tears into IIa (anterior), IIb (posterior), and IIc (combined). Their group found that SLAP IIb tears were the most common type in overhead throwers, accounting for 47% of overhead athletes with type II tears.5 Further, type IIb tears can have a significant impact in throwers, in part due to greater shoulder instability as well as anterior pseudolaxity.5 SLAP injuries typically have been difficult to successfully treat nonoperatively in overhead athletes.6 A study by Edwards and colleagues6 examined 39 patients with all types of SLAP tears. Although, in their study, nonoperative management failed in 20 patients and they required surgery, 10 of the 15 overhead athletes in whom nonoperative treatment did not fail initially returned to sport at a level equal to or better than their pre-injury level, indicating that nonoperative treatment may play a role in some patients’ recovery.6
Surgical outcomes of SLAP IIb repairs have traditionally been less predictable than those of other shoulder injuries. Some believe that traditional knotted anchors may be partially to blame by abrading the rotator cuff, possibly leading to rotator cuff tears and pain. Further, knotted anchors are typically bulkier and require more experience with tying and tensioning and, therefore, may lead to less consistent results.7 The purpose of this study was to investigate if knotless anchors result in more favorable outcomes in repair of type IIb SLAP lesions when compared with traditional knotted anchors. It was hypothesized that knotless fixation will provide superior clinical outcomes, improved return to play (RTP), and lower revision rates as compared with traditional knotted fixation in the repair of SLAP IIb tears.
METHODS
PATIENT SELECTION
The authors retrospectively reviewed SLAP tears repaired by the senior author from June 2000 to September 2015. The inclusion criteria consisted of all athletes at any level who were diagnosed intraoperatively with a type IIb SLAP tear as defined by Morgan and colleagues5 with a minimum 2-year follow-up. The exclusion criteria were any patients with a previous shoulder surgery and the presence of any labral pathology aside from a SLAP IIb tear. Patients with rotator cuff or biceps pathologies were included. In all included patients, an initial course of preoperative physical therapy, including strengthening and stabilization of the scapulothoracic joint, had failed. Patient-directed surveys evaluated RTP, as well as the Kerlan-Jobe Orthopaedic Clinic (KJOC) score, American Shoulder and Elbow Surgeons (ASES) score, stability, range of motion (ROM), strength, and pain scores, as previously described.8-10 Institutional Review Board and informed consent approval were acquired prior to initiation of the study.
PATIENT EVALUATION
An appropriate preoperative history was taken, and physical examinations were performed, including evaluation of the scapulothoracic joint, as well as tests to evaluate the presence of a SLAP tear, anterior instability, posterior instability, multi-directional instability, and rotator cuff tears, as previously described.11 Patients with a history and physical examination concerning SLAP pathology underwent an magnetic resonance imaging (MRI) arthrogram, which was used in conjunction with intraoperative findings to diagnose type IIb SLAP tears.
Continue to: SURGICAL TECHNIQUE
SURGICAL TECHNIQUE
All surgeries were performed arthroscopically with the patient in the lateral decubitus position. The SLAP lesions were subsequently repaired using a technique similar to that described by Burkhart and colleagues.12 The traditional knotted fixation incorporated the use of 3.0 Bio-FASTak (Arthrex) with #2 FiberWire (Arthrex). Knotless anchor fixation was performed using 2.9 mm × 12.5 mm or 2.4 mm × 11.3 mm BioComposite PushLock (Arthrex) suture anchors, based on the size of the glenoid, with LabralTape or SutureTape (Arthrex). Patients who had surgery before January 1, 2013 underwent fixation with traditional knotted fixation; after that date, patients underwent fixation with knotless anchors.
POSTOPERATIVE REHABILITATION
Patients underwent a strict postoperative protocol in which they were kept in a sling with an abduction pillow for the first 6 weeks and performed pendulum exercises and passive motion only. A formal physical therapy regimen started at 4 weeks with passive ROM, passive posterior capsular and internal rotation stretching, scapulothoracic mobility, and biceps, rotator cuff, and capsular stabilizer strengthening. At 10 weeks, patients began biceps, rotator cuff, and scapular stabilizer resistance exercises, and at 16 weeks, throwing athletes began an interval throwing program. Patients were first eligible to return to sport without limitation at 9 months.
STATISTICAL ANALYSIS
Return to play, KJOC, ASES, stability, ROM, strength, and pain scores were analyzed and compared using Fisher exact test, the Kruskal-Wallis test, and the Wilcoxon rank sum test, where appropriate. The level of statistical significance was α = 0.05.
RESULTS
Table 1. Patient Demographics | |
Athletes (N) | 74 |
Age (yr) | 30.1 (14-64) |
Knotless anchors | 32 (43.2%) |
Knotted anchors | 42 (56.8%) |
Overhead athletes | 53 (72%) |
Throwing athletes | 29 (39%) |
Follow-up (yr) | 6.5 (2-12) |
Of the 74 athletes who met inclusion criteria, 28 were female (37.8%) and 46 (62.2%) were male. The average follow-up was 6.5 years with a minimum of 2 years and a maximum of 12 years. Forty-two (56.8%) patients underwent traditional knotted suture anchor fixation and 32 (43.2%) underwent knotless anchor fixation. The average age was 30.1 +/– 13.6 years, with a range of 14 to 64 years. The majority of athletes were right hand dominant (79.9%). Fifty-three (72%) were overhead athletes and 29 (39%) were throwing athletes (Table 1). The average age in the knotted group was 33.3 years: 29 of 42 (69%) were overhead athletes and 20 (47.6%) were throwing athletes. In the knotless group, the average age was 25.8 years: 24 of 32 (75.0%) were overhead athletes and 9 (28.1%) were throwing athletes. Primary sports at the time of injury are listed in Table 2. The average number of anchors used was 3.1, with 17 patients (23.0%) requiring ≤2 anchors, 39 (52.7%) requiring 3 anchors, and 18 (24.3%) requiring ≥4 anchors for repair. The number of anchors used was determined intraoperatively by the surgeon on the basis of the size and extent of the tear. Of the entire group of 74 patients, 91.9% returned to sport, 56.8% returned to the same level, 35.1% returned at a lower capacity, and 8.1% were unable to return to sport. Knotless anchors had a slightly higher overall RTP compared with traditional anchors (93.5% vs 90.2%, P = .94), as well as a higher RTP at the same level (58.1% vs 53.7%, P = .81). These differences were, however, not statistically significant (Table 3).
Table 2. Primary Sport at Time of SLAP IIb Injury | |
Primary Sport | n (%) |
Baseball | 14 (19.7%) |
Softball | 8 (11.3%) |
Volleyball | 6 (8.5%) |
Basketball | 5 (7.0%) |
Golf | 5 (7.0%) |
Other Sport | 33 (46.5%) |
No Primary Sport | 3 (4.1%) |
Abbreviation: SLAP, superior labrum anterior to posterior.
Knotless anchors were less likely to require revision surgery than traditional anchors (9% vs 17%, P = .50), but this difference was not statistically significant (Table 3). In the knotted group, 5 patients had revision surgery for rotator cuff tears, and 2 patients had recurrent SLAP tears. In the knotless group, 2 patients had revision surgeries for a torn rotator cuff, and 1 patient had a snapping scapula. A power analysis found that it would take over 300 athletes in each group to detect a significant difference in the revision rate between knotless and traditional anchors.
Table 3. Comparison of Anchor Type in Surgical Fixation of SLAP IIb Tears | |||||
| RTP | RTP Same Level | ASES | KJOC | Revision Rate |
Knotless anchors (n = 32) | 93.5% | 58.1% | 86.3 + 10.5 | 66.1 + 29.6 | 9% |
Traditional anchors (n = 42) | 90.2% | 53.7% | 85.3 + 15.6 | 65.6 + 27.2 | 17% |
P-value | .94 | .81 | .79 | .61 | .50 |
Abbreviations: ASES, American Shoulder and Elbow Surgeons; KJOC, Kerlan-Jobe Orthopaedic Clinic; RTP: return to play. | |||||
Continue to: Although KJOC...
Although KJOC (66.1 vs 65.6 P = .61) and ASES (86.3 vs 85.3 P = .79) scores were also superior with knotless anchors, these differences in scores were not statistically significant (Table 3). Pain was the only variable that was linked to decreased RTP, as patients who rated higher on a pain scale of 0 to 10 were less likely to return to their sport (P < .0001). There was no correlation in outcome measures or RTP with gender, age, number of anchors, or sport type (P > .05). There was no statistically significant difference in RTP, KJOC, or ASES scores between non-overhead and overhead athletes (Table 4). Overall return to sport in throwers was 85.7% (24/28), while 39.3% (11/28) returned at the same level, 46.4% (13/28) at a lower level, and 14.3% (4/28) did not return to sport.
Table 4. Overhead vs Non-Overhead Athletes After Surgical Fixation of SLAP IIb Tears | |||||
| RTP | RTP Same Level | ASES | ASES Good-Excellent | KJOC |
Overhead | 90.6% | 52.3% | 91.7 + 14.1 | 98.1% | 64.6 + 25.7 |
Non-Overhead | 95.5% | 72.7% | 86.7 + 12.7 | 100% | 88.5 + 29.6 |
P value | 0.1 | 0.29 | 0.76 | 0.50 | 0.49 |
Abbreviations: ASES, American Shoulder and Elbow Surgeons; KJOC, Kerlan-Jobe Orthopaedic Clinic; RTP: return to play. | |||||
DISCUSSION
There was no significant difference between knotted and knotless fixation in clinical outcomes or return to sport in the repair of SLAP IIb tears; however, there was a trend toward knotless anchors requiring less revision surgery and having higher RTP, ASES, and KJOC scores than knotted fixation. Despite the inclusion of 74 patients, this study was significantly underpowered, as a power analysis calculated that over 300 athletes would be required in each group to detect a difference in the revision rate.
SLAP tears, traditionally treated with knotted suture anchors, have yielded varying results in the literature, with good to excellent results being reported in 65% to 94% of patients.13-17 The success of SLAP repairs in athletes, especially overhead athletes, remains a difficult problem, as they are common injuries, and RTP is less predictable. Studies differ with regard to the percentage of overhead athletes who are able to return to their previous level of sport, with ranges being reported from 22% to 92%.16,18,19 In a systematic review of 198 patients, Sayde and colleagues16 found that 63% of overhead athletes treated with anchor fixation, tacks, or staples were able to return to their previous level of play. Morgan and colleagues5 found a higher return to sport when compared with other studies, reporting that 83% of patients undergoing SLAP repairs using traditional suture anchors had excellent results, and 87% of the 53 overhead athletes had excellent results based on UCLA shoulder scores. Further, 37 of the 44 pitchers examined (84%) were able to return to their pre-injury levels.5 This is in contrast to Friel and colleagues20 who found that in 48 patients with type II SLAP tears treated with traditional anchors, 23% reported excellent and 56% reported good results in regards to UCLA shoulder scores. Friel and colleagues also found that 62% of all athletes and 59% of overhead athletes were able to return to their previous levels of sport, which is similar to the current study.20 The large discrepancy in RTP at the pre-injury level between this study and that of Morgan and colleagues5 may be due to the shorter minimum follow-up of 1 year as well as the inclusion of all subtypes of SLAP II tears in the latter. The current study had a minimum 2-year follow-up period, with an average of 6.5 years, and was limited to SLAP IIb tears. With a longer follow-up period, patient outcomes and RTP, particularly in overhead sports, may deteriorate; therefore, the current study likely shows a more complete and accurate result.
Knotless anchors were originally introduced as a less time consuming, lower profile, and simpler device to learn and use for arthroscopic procedures.21 Kocaoglu and colleagues22 found that in Bankart repairs, the mean time per anchor placement for knotted anchors was 380 seconds, whereas placement of knotless anchors took on average 225 seconds. A learning curve also exists for proper and efficient knot tying.7 There is also variation in knot tying between surgeons, as evidenced by a wide range in both load to failure and knot height.7 A study performed by Hanypsiak and colleagues7 found that the surgical knot was the weakest portion of the suture-anchor construct, as the knot’s load to failure was less than the pullout strength of the anchor.
There is also concern for the added height associated with traditional knotted fixation, which has been supported by case reports of knot-induced glenoid erosion after arthroscopic fixation of a SLAP tear.23 Hanypsiak and colleagues7 also found that the average knot height occupied 50% to 95% of the space between the humeral head and the acromion when the shoulder is in a neutral position, indicating that the higher profile knotted anchors may contact the undersurface of the acromion, which could affect the labral repair as well as cause rotator cuff injury. Abrasion of the rotator cuff by a prominent knot may cause pain, tearing, and disability. A recent study by Park and colleagues24 reported on 11 patients with knot-induced pain after type II SLAP repair. All complained of sharp pain, with 64% also complaining of clicking. Knot location did not seem to matter, as there was no difference in preoperative symptoms, with 5 of the 11 patients having knots on the glenoid side of the repair on repeat arthroscopy. Patients with knots on the labral side did, however, have humeral head cartilage damage. The knots appeared to be the cause of pain and clicking, as after arthroscopic knot removal, dramatic pain relief was seen, with Constant and UCLA scores significantly improving in all 11 patients. All patients also had positive preoperative compression-rotation testing, and at 6 weeks after surgical knot removal, all were negative.24
Continue to: Further, as shown by Dines and colleagues...
Further, as shown by Dines and colleagues25, knotless anchors may help to better restore the meniscoid anatomy of the superior labrum better than knotted suture anchors. With regards to fixation strength, Uggen and colleagues26, using a cadaveric model, found no difference in initial fixation strength of knotless and traditional suture anchor repair of SLAP II tears, and both restored glenohumeral rotation without over-constraining the shoulder.
Despite the shorter operative time, lower profile, and more consistent tensioning with knotless anchors, the literature is limited with regard to evaluating patient outcomes. In a study by Yung and colleagues13 14 of the 16 patients with type II SLAP tears were treated with knotless anchors, and the authors found that 31.3% of patients had an excellent UCLA score while 43.8% had a good score. This is similar to the outcomes illustrated in studies by both Friel and colleagues20 and Sayde and colleagues.16 In a more recent study, Yang and colleagues27 did find some benefit in regard to ROM with knotless fixation. Their study consisted of 21 patients who underwent surgery with traditional knotted anchor fixation and 20 who underwent knotless horizontal mattress fixation. They found an average UCLA score of 37.6 and ASES score of 91.5 in patients undergoing knotless fixation, and the knotless fixation group had 5% greater total ROM, 15.6% more internal rotation at abduction, and 11.4% more external rotation at the side as compared with patients undergoing the traditional knotted technique. When compared with the current study, this study also had a significantly shorter follow-up period of 3 years.27 In a 2017 study, Bents and colleagues28 compared 44 patients who underwent knotless and 119 who underwent knotted fixation of SLAP tears. They found no statistically significant difference between knotless and knotted fixation in the ASES score, Visual Analog Scale (VAS), ASES, or Veterans RAND 12-Item Health Survey (VR-12) at 1 year postoperatively. Their outcomes were similar to those of the current study, but as in other mentioned literature, the study by Bents and colleagues28 included multiple surgeons with different postoperative protocols, was not limited to SLAP IIb tears, and also had a shorter follow-up of 1 year. Like Kocaoglu and colleagues22, Bents and colleagues did find knotless anchors to be more efficient, as operative time was reduced by 5.3 minutes per anchor. This likely would have a significant impact on surgical cost and surgeon productivity.28
One limitation of the current study was that despite the inclusion of >70 patients, the study was still significantly underpowered. It was determined that >300 patients in each group would be required to detect a significant difference in the revision rate between the 2 anchor types. Also, due to the retrospective nature of this study, no preoperative scores were collected. The inclusion of objective clinical measurements and follow-up imaging evaluating the rotator cuff and other anatomy would also be of interest.
Although statistical significance was not achieved, there was a trend toward knotless fixation requiring less revision surgery and having higher RTP, ASES, and KJOC scores when compared with traditional knotted fixation at 6.5-year follow-up. Larger studies with longer follow-up periods are necessary to determine the effects of knotted and knotless anchors on rotator cuff tears, patient reported outcomes, and RTP. These complications have been shown in the literature, mostly in case reports, and typically develop over a longer period.23 Despite this, other advantages of knotless fixation, such as its lower profile, the ability to better provide consistent tensioning, and decreased surgical time are important to consider.
1. Andrews JR, Carson WG, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13(5):337-341. doi:10.1177/036354658501300508.
2. Snyder SJ, Karzel RP, Pizzo WD, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthrosc J Arthrosc Relat Surg. 1990;6(4):274-279. doi:10.1016/0749-8063(90)90056-J.
3. Ahsan ZS, Hsu JE, Gee AO. The Snyder classification of superior labrum anterior and posterior (SLAP) lesions. Clin Orthop. 2016;474(9):2075-2078. doi:10.1007/s11999-016-4826-z.
4. Erickson BJ, Jain A, Abrams GD, et al. SLAP Lesions: Trends in treatment. Arthrosc J Arthrosc Relat Surg. 2016;32(6):976-981. doi:10.1016/j.arthro.2015.11.044.
5. Morgan C, Burkhart S, Palmeri M, Gillespie M. Type II SLAP lesions: three subtypes and their relationships to superior instability and rotator cuff tears. Arthrosc J Arthrosc Relat Surg. 1998;14(6):553-565. doi:10.1016/S0749-8063(98)70049-0.
6. Edwards SL, Lee JA, Bell J-E, et al. nonoperative treatment of superior labrum anterior posterior tears: Improvements in pain, function, and quality of life. Am J Sports Med. 2010;38(7):1456-1461. doi:10.1177/0363546510370937.
7. Hanypsiak BT, DeLong JM, Simmons L, Lowe W, Burkhart S. Knot strength varies widely among expert arthroscopists. Am J Sports Med. 2014;42(8):1978-1984. doi:10.1177/0363546514535554.
8. Alberta FG, ElAttrache NS, Bissell S, et al. The development and validation of a functional assessment tool for the upper extremity in the overhead athlete. Am J Sports Med. 2010;38(5):903-911. doi:10.1177/0363546509355642.
9. Bradley JP, McClincy MP, Arner JW, Tejwani SG. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 200 shoulders. Am J Sports Med. 2013;41(9):2005-2014. doi:10.1177/0363546513493599.
10. Michener LA, McClure PW, Sennett BJ. American shoulder and elbow surgeons standardized shoulder assessment form, patient self-report section: Reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587-594. doi:10.1067/mse.2002.127096.
11. Cook C, Hegedus EJ. Orthopedic Physical Examination Tests: An Evidence-Based Approach. Upper Saddle River, NJ: PearsonPrentice Hall; 2008.
12. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: Spectrum of pathology part I: Pathoanatomy and biomechanics. Arthrosc J Arthrosc Relat Surg. 2003;19(4):404-420. doi:10.1053/jars.2003.50128.
13. Yung PS-H, Fong DT-P, Kong M-F, et al. Arthroscopic repair of isolated type II superior labrum anterior–posterior lesion. Knee Surg Sports Traumatol Arthrosc. 2008;16(12):1151-1157. doi:10.1007/s00167-008-0629-4.
14. Brockmeier SF, Voos JE, Williams RJ, Altchek DW, Cordasco FA, Allen AA. Outcomes After Arthroscopic Repair of Type-II SLAP Lesions: J Bone Jt Surg-Am Vol. 2009;91(7):1595-1603. doi:10.2106/JBJS.H.00205.
15. Galano GJ, Ahmad CS, Bigliani L, Levine W. Percutaneous SLAP lesion repair technique is an effective alternative to portal of Wilmington. Orthopedics. 2010;33(11). doi:10.3928/01477447-20100924-15.
16. Sayde WM, Cohen SB, Ciccotti MG, Dodson CC. Return to play after type II superior labral anterior-posterior lesion repairs in athletes: A systematic review. Clin Orthop Relat Res. 2012;470(6):1595-1600. doi:10.1007/s11999-012-2295-6.
17. Kim K-H, Bin S-I, Kim J-M. The correlation between posterior tibial slope and maximal angle of flexion after total knee arthroplasty. Knee Surg Relat Res. 2012;24(3):158-163. doi:10.5792/ksrr.2012.24.3.158.
18. Kim S-H, Ha K-I, Kim S-H, Choi H-J. Results of arthroscopic treatment of superior labral lesions. J Bone Joint Surg Am. 2002;84-A(6):981-985.
19. Pagnani MJ, Speer KP, Altchek DW, Warren RF, Dines DM. Arthroscopic fixation of superior labral lesions using a biodegradable implant: a preliminary report. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 1995;11(2):194-198.
20. Friel NA, Karas V, Slabaugh MA, Cole BJ. Outcomes of type II superior labrum, anterior to posterior (SLAP) repair: Prospective evaluation at a minimum two-year follow-up. J Shoulder Elbow Surg. 2010;19(6):859-867. doi:10.1016/j.jse.2010.03.004.
21. Thal R. A knotless suture anchor. Arthrosc J Arthrosc Relat Surg. 2001;17(2):213-218. doi:10.1053/jars.2001.20666.
22. Kocaoglu B, Guven O, Nalbantoglu U, Aydin N, Haklar U. No difference between knotless sutures and suture anchors in arthroscopic repair of Bankart lesions in collision athletes. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):844-849. doi:10.1007/s00167-009-0811-3.
23. Rhee YG, Ha JH. Knot-induced glenoid erosion after arthroscopic fixation for unstable superior labrum anterior-posterior lesion: Case report. J Shoulder Elbow Surg. 2006;15(3):391-393. doi:10.1016/j.jse.2005.03.010.
24. Park JG, Cho NS, Kim JY, Song JH, Hong SJ, Rhee YG. Arthroscopic Knot Removal for Failed Superior Labrum Anterior-Posterior Repair Secondary to Knot-Induced Pain. Am J Sports Med. 2017;45(11):2563-2568. doi:10.1177/0363546517713662.
25. Dines JS, ElAttrache NS. Horizontal Mattress With a Knotless Anchor to Better Recreate the Normal Superior Labrum Anatomy. Arthrosc J Arthrosc Relat Surg. 2008;24(12):1422-1425. doi:10.1016/j.arthro.2008.06.012.
26. Uggen C, Wei A, Glousman RE, et al. Biomechanical Comparison of Knotless Anchor Repair Versus Simple Suture Repair for Type II SLAP Lesions. Arthrosc J Arthrosc Relat Surg. 2009;25(10):1085-1092. doi:10.1016/j.arthro.2009.03.022.
27. Yang HJ, Yoon K, Jin H, Song HS. Clinical outcome of arthroscopic SLAP repair: conventional vertical knot versus knotless horizontal mattress sutures. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):464-469. doi:10.1007/s00167-014-3449-8.
28. Bents EJ, Brady PC, Adams CR, Tokish JM, Higgins LD, Denard PJ. Patient-reported outcomes of knotted and knotless glenohumeral labral repairs are equivalent. Am J Orthop. 2017;46(6):279-283.
ABSTRACT
The use of knotless suture anchors has increased in popularity; however, there is a paucity of literature examining the difference in clinical outcomes with traditional knotted fixation. It was hypothesized that knotless fixation would provide superior clinical outcomes, improved return to play (RTP), and lower revision rates as compared with traditional knotted fixation in the repair of SLAP IIb tears. Seventy-four athletes who underwent arthroscopic SLAP IIb repair with traditional (n = 42) and knotless anchors (n = 32) by a single surgeon were evaluated after a minimum 2-year follow. Demographic and surgical data, RTP, Kerlan-Jobe Orthopaedic Clinic (KJOC) score, American Shoulder and Elbow Surgeons (ASES) score, stability, strength, and pain scores were compared. Knotless anchors had slightly higher RTP (93.5% vs 90.2%, P = .94) and RTP at the same level (58.1% vs 53.7% P = .81) compared with knotted fixation, but the difference did not reach statistical significance. Knotless anchors were less likely to require revision surgery than traditional anchors (9% vs 17%, P = .50), but the difference was not statistically significant. When comparing knotless and traditional knotted suture anchor repair of type llb SLAP tears, knotless fixation required less revision surgery and had higher RTP, ASES, and KJOC scores; however, statistical significance was not achieved in this relatively small cohort.
Continue to: Injury of the anterosuperior...
Injury of the anterosuperior labrum near the biceps origin was first described by Andrews and colleagues in 1985 in overhead athletes.1 The term SLAP, or a tear in the superior labrum anterior to posterior, was coined a few years later by Snyder and colleagues.2 They described an injury to the superior labrum beginning posteriorly and extending anteriorly, including the “anchor” of the biceps tendon to the labrum. Snyder further delineated SLAP lesions into 4 subtypes, the most common being type II, which he described as “degenerative fraying of the labrum with additional detachment of the superior labrum and biceps from the glenoid resulting in an unstable labral anchor.”2,3 Type II tears are of particular importance as they are the most common SLAP lesions, with an incidence of 55%, and comprise nearly 75% of SLAP repairs performed.2,4
Morgan and colleagues further delineated type II SLAP tears into IIa (anterior), IIb (posterior), and IIc (combined). Their group found that SLAP IIb tears were the most common type in overhead throwers, accounting for 47% of overhead athletes with type II tears.5 Further, type IIb tears can have a significant impact in throwers, in part due to greater shoulder instability as well as anterior pseudolaxity.5 SLAP injuries typically have been difficult to successfully treat nonoperatively in overhead athletes.6 A study by Edwards and colleagues6 examined 39 patients with all types of SLAP tears. Although, in their study, nonoperative management failed in 20 patients and they required surgery, 10 of the 15 overhead athletes in whom nonoperative treatment did not fail initially returned to sport at a level equal to or better than their pre-injury level, indicating that nonoperative treatment may play a role in some patients’ recovery.6
Surgical outcomes of SLAP IIb repairs have traditionally been less predictable than those of other shoulder injuries. Some believe that traditional knotted anchors may be partially to blame by abrading the rotator cuff, possibly leading to rotator cuff tears and pain. Further, knotted anchors are typically bulkier and require more experience with tying and tensioning and, therefore, may lead to less consistent results.7 The purpose of this study was to investigate if knotless anchors result in more favorable outcomes in repair of type IIb SLAP lesions when compared with traditional knotted anchors. It was hypothesized that knotless fixation will provide superior clinical outcomes, improved return to play (RTP), and lower revision rates as compared with traditional knotted fixation in the repair of SLAP IIb tears.
METHODS
PATIENT SELECTION
The authors retrospectively reviewed SLAP tears repaired by the senior author from June 2000 to September 2015. The inclusion criteria consisted of all athletes at any level who were diagnosed intraoperatively with a type IIb SLAP tear as defined by Morgan and colleagues5 with a minimum 2-year follow-up. The exclusion criteria were any patients with a previous shoulder surgery and the presence of any labral pathology aside from a SLAP IIb tear. Patients with rotator cuff or biceps pathologies were included. In all included patients, an initial course of preoperative physical therapy, including strengthening and stabilization of the scapulothoracic joint, had failed. Patient-directed surveys evaluated RTP, as well as the Kerlan-Jobe Orthopaedic Clinic (KJOC) score, American Shoulder and Elbow Surgeons (ASES) score, stability, range of motion (ROM), strength, and pain scores, as previously described.8-10 Institutional Review Board and informed consent approval were acquired prior to initiation of the study.
PATIENT EVALUATION
An appropriate preoperative history was taken, and physical examinations were performed, including evaluation of the scapulothoracic joint, as well as tests to evaluate the presence of a SLAP tear, anterior instability, posterior instability, multi-directional instability, and rotator cuff tears, as previously described.11 Patients with a history and physical examination concerning SLAP pathology underwent an magnetic resonance imaging (MRI) arthrogram, which was used in conjunction with intraoperative findings to diagnose type IIb SLAP tears.
Continue to: SURGICAL TECHNIQUE
SURGICAL TECHNIQUE
All surgeries were performed arthroscopically with the patient in the lateral decubitus position. The SLAP lesions were subsequently repaired using a technique similar to that described by Burkhart and colleagues.12 The traditional knotted fixation incorporated the use of 3.0 Bio-FASTak (Arthrex) with #2 FiberWire (Arthrex). Knotless anchor fixation was performed using 2.9 mm × 12.5 mm or 2.4 mm × 11.3 mm BioComposite PushLock (Arthrex) suture anchors, based on the size of the glenoid, with LabralTape or SutureTape (Arthrex). Patients who had surgery before January 1, 2013 underwent fixation with traditional knotted fixation; after that date, patients underwent fixation with knotless anchors.
POSTOPERATIVE REHABILITATION
Patients underwent a strict postoperative protocol in which they were kept in a sling with an abduction pillow for the first 6 weeks and performed pendulum exercises and passive motion only. A formal physical therapy regimen started at 4 weeks with passive ROM, passive posterior capsular and internal rotation stretching, scapulothoracic mobility, and biceps, rotator cuff, and capsular stabilizer strengthening. At 10 weeks, patients began biceps, rotator cuff, and scapular stabilizer resistance exercises, and at 16 weeks, throwing athletes began an interval throwing program. Patients were first eligible to return to sport without limitation at 9 months.
STATISTICAL ANALYSIS
Return to play, KJOC, ASES, stability, ROM, strength, and pain scores were analyzed and compared using Fisher exact test, the Kruskal-Wallis test, and the Wilcoxon rank sum test, where appropriate. The level of statistical significance was α = 0.05.
RESULTS
Table 1. Patient Demographics | |
Athletes (N) | 74 |
Age (yr) | 30.1 (14-64) |
Knotless anchors | 32 (43.2%) |
Knotted anchors | 42 (56.8%) |
Overhead athletes | 53 (72%) |
Throwing athletes | 29 (39%) |
Follow-up (yr) | 6.5 (2-12) |
Of the 74 athletes who met inclusion criteria, 28 were female (37.8%) and 46 (62.2%) were male. The average follow-up was 6.5 years with a minimum of 2 years and a maximum of 12 years. Forty-two (56.8%) patients underwent traditional knotted suture anchor fixation and 32 (43.2%) underwent knotless anchor fixation. The average age was 30.1 +/– 13.6 years, with a range of 14 to 64 years. The majority of athletes were right hand dominant (79.9%). Fifty-three (72%) were overhead athletes and 29 (39%) were throwing athletes (Table 1). The average age in the knotted group was 33.3 years: 29 of 42 (69%) were overhead athletes and 20 (47.6%) were throwing athletes. In the knotless group, the average age was 25.8 years: 24 of 32 (75.0%) were overhead athletes and 9 (28.1%) were throwing athletes. Primary sports at the time of injury are listed in Table 2. The average number of anchors used was 3.1, with 17 patients (23.0%) requiring ≤2 anchors, 39 (52.7%) requiring 3 anchors, and 18 (24.3%) requiring ≥4 anchors for repair. The number of anchors used was determined intraoperatively by the surgeon on the basis of the size and extent of the tear. Of the entire group of 74 patients, 91.9% returned to sport, 56.8% returned to the same level, 35.1% returned at a lower capacity, and 8.1% were unable to return to sport. Knotless anchors had a slightly higher overall RTP compared with traditional anchors (93.5% vs 90.2%, P = .94), as well as a higher RTP at the same level (58.1% vs 53.7%, P = .81). These differences were, however, not statistically significant (Table 3).
Table 2. Primary Sport at Time of SLAP IIb Injury | |
Primary Sport | n (%) |
Baseball | 14 (19.7%) |
Softball | 8 (11.3%) |
Volleyball | 6 (8.5%) |
Basketball | 5 (7.0%) |
Golf | 5 (7.0%) |
Other Sport | 33 (46.5%) |
No Primary Sport | 3 (4.1%) |
Abbreviation: SLAP, superior labrum anterior to posterior.
Knotless anchors were less likely to require revision surgery than traditional anchors (9% vs 17%, P = .50), but this difference was not statistically significant (Table 3). In the knotted group, 5 patients had revision surgery for rotator cuff tears, and 2 patients had recurrent SLAP tears. In the knotless group, 2 patients had revision surgeries for a torn rotator cuff, and 1 patient had a snapping scapula. A power analysis found that it would take over 300 athletes in each group to detect a significant difference in the revision rate between knotless and traditional anchors.
Table 3. Comparison of Anchor Type in Surgical Fixation of SLAP IIb Tears | |||||
| RTP | RTP Same Level | ASES | KJOC | Revision Rate |
Knotless anchors (n = 32) | 93.5% | 58.1% | 86.3 + 10.5 | 66.1 + 29.6 | 9% |
Traditional anchors (n = 42) | 90.2% | 53.7% | 85.3 + 15.6 | 65.6 + 27.2 | 17% |
P-value | .94 | .81 | .79 | .61 | .50 |
Abbreviations: ASES, American Shoulder and Elbow Surgeons; KJOC, Kerlan-Jobe Orthopaedic Clinic; RTP: return to play. | |||||
Continue to: Although KJOC...
Although KJOC (66.1 vs 65.6 P = .61) and ASES (86.3 vs 85.3 P = .79) scores were also superior with knotless anchors, these differences in scores were not statistically significant (Table 3). Pain was the only variable that was linked to decreased RTP, as patients who rated higher on a pain scale of 0 to 10 were less likely to return to their sport (P < .0001). There was no correlation in outcome measures or RTP with gender, age, number of anchors, or sport type (P > .05). There was no statistically significant difference in RTP, KJOC, or ASES scores between non-overhead and overhead athletes (Table 4). Overall return to sport in throwers was 85.7% (24/28), while 39.3% (11/28) returned at the same level, 46.4% (13/28) at a lower level, and 14.3% (4/28) did not return to sport.
Table 4. Overhead vs Non-Overhead Athletes After Surgical Fixation of SLAP IIb Tears | |||||
| RTP | RTP Same Level | ASES | ASES Good-Excellent | KJOC |
Overhead | 90.6% | 52.3% | 91.7 + 14.1 | 98.1% | 64.6 + 25.7 |
Non-Overhead | 95.5% | 72.7% | 86.7 + 12.7 | 100% | 88.5 + 29.6 |
P value | 0.1 | 0.29 | 0.76 | 0.50 | 0.49 |
Abbreviations: ASES, American Shoulder and Elbow Surgeons; KJOC, Kerlan-Jobe Orthopaedic Clinic; RTP: return to play. | |||||
DISCUSSION
There was no significant difference between knotted and knotless fixation in clinical outcomes or return to sport in the repair of SLAP IIb tears; however, there was a trend toward knotless anchors requiring less revision surgery and having higher RTP, ASES, and KJOC scores than knotted fixation. Despite the inclusion of 74 patients, this study was significantly underpowered, as a power analysis calculated that over 300 athletes would be required in each group to detect a difference in the revision rate.
SLAP tears, traditionally treated with knotted suture anchors, have yielded varying results in the literature, with good to excellent results being reported in 65% to 94% of patients.13-17 The success of SLAP repairs in athletes, especially overhead athletes, remains a difficult problem, as they are common injuries, and RTP is less predictable. Studies differ with regard to the percentage of overhead athletes who are able to return to their previous level of sport, with ranges being reported from 22% to 92%.16,18,19 In a systematic review of 198 patients, Sayde and colleagues16 found that 63% of overhead athletes treated with anchor fixation, tacks, or staples were able to return to their previous level of play. Morgan and colleagues5 found a higher return to sport when compared with other studies, reporting that 83% of patients undergoing SLAP repairs using traditional suture anchors had excellent results, and 87% of the 53 overhead athletes had excellent results based on UCLA shoulder scores. Further, 37 of the 44 pitchers examined (84%) were able to return to their pre-injury levels.5 This is in contrast to Friel and colleagues20 who found that in 48 patients with type II SLAP tears treated with traditional anchors, 23% reported excellent and 56% reported good results in regards to UCLA shoulder scores. Friel and colleagues also found that 62% of all athletes and 59% of overhead athletes were able to return to their previous levels of sport, which is similar to the current study.20 The large discrepancy in RTP at the pre-injury level between this study and that of Morgan and colleagues5 may be due to the shorter minimum follow-up of 1 year as well as the inclusion of all subtypes of SLAP II tears in the latter. The current study had a minimum 2-year follow-up period, with an average of 6.5 years, and was limited to SLAP IIb tears. With a longer follow-up period, patient outcomes and RTP, particularly in overhead sports, may deteriorate; therefore, the current study likely shows a more complete and accurate result.
Knotless anchors were originally introduced as a less time consuming, lower profile, and simpler device to learn and use for arthroscopic procedures.21 Kocaoglu and colleagues22 found that in Bankart repairs, the mean time per anchor placement for knotted anchors was 380 seconds, whereas placement of knotless anchors took on average 225 seconds. A learning curve also exists for proper and efficient knot tying.7 There is also variation in knot tying between surgeons, as evidenced by a wide range in both load to failure and knot height.7 A study performed by Hanypsiak and colleagues7 found that the surgical knot was the weakest portion of the suture-anchor construct, as the knot’s load to failure was less than the pullout strength of the anchor.
There is also concern for the added height associated with traditional knotted fixation, which has been supported by case reports of knot-induced glenoid erosion after arthroscopic fixation of a SLAP tear.23 Hanypsiak and colleagues7 also found that the average knot height occupied 50% to 95% of the space between the humeral head and the acromion when the shoulder is in a neutral position, indicating that the higher profile knotted anchors may contact the undersurface of the acromion, which could affect the labral repair as well as cause rotator cuff injury. Abrasion of the rotator cuff by a prominent knot may cause pain, tearing, and disability. A recent study by Park and colleagues24 reported on 11 patients with knot-induced pain after type II SLAP repair. All complained of sharp pain, with 64% also complaining of clicking. Knot location did not seem to matter, as there was no difference in preoperative symptoms, with 5 of the 11 patients having knots on the glenoid side of the repair on repeat arthroscopy. Patients with knots on the labral side did, however, have humeral head cartilage damage. The knots appeared to be the cause of pain and clicking, as after arthroscopic knot removal, dramatic pain relief was seen, with Constant and UCLA scores significantly improving in all 11 patients. All patients also had positive preoperative compression-rotation testing, and at 6 weeks after surgical knot removal, all were negative.24
Continue to: Further, as shown by Dines and colleagues...
Further, as shown by Dines and colleagues25, knotless anchors may help to better restore the meniscoid anatomy of the superior labrum better than knotted suture anchors. With regards to fixation strength, Uggen and colleagues26, using a cadaveric model, found no difference in initial fixation strength of knotless and traditional suture anchor repair of SLAP II tears, and both restored glenohumeral rotation without over-constraining the shoulder.
Despite the shorter operative time, lower profile, and more consistent tensioning with knotless anchors, the literature is limited with regard to evaluating patient outcomes. In a study by Yung and colleagues13 14 of the 16 patients with type II SLAP tears were treated with knotless anchors, and the authors found that 31.3% of patients had an excellent UCLA score while 43.8% had a good score. This is similar to the outcomes illustrated in studies by both Friel and colleagues20 and Sayde and colleagues.16 In a more recent study, Yang and colleagues27 did find some benefit in regard to ROM with knotless fixation. Their study consisted of 21 patients who underwent surgery with traditional knotted anchor fixation and 20 who underwent knotless horizontal mattress fixation. They found an average UCLA score of 37.6 and ASES score of 91.5 in patients undergoing knotless fixation, and the knotless fixation group had 5% greater total ROM, 15.6% more internal rotation at abduction, and 11.4% more external rotation at the side as compared with patients undergoing the traditional knotted technique. When compared with the current study, this study also had a significantly shorter follow-up period of 3 years.27 In a 2017 study, Bents and colleagues28 compared 44 patients who underwent knotless and 119 who underwent knotted fixation of SLAP tears. They found no statistically significant difference between knotless and knotted fixation in the ASES score, Visual Analog Scale (VAS), ASES, or Veterans RAND 12-Item Health Survey (VR-12) at 1 year postoperatively. Their outcomes were similar to those of the current study, but as in other mentioned literature, the study by Bents and colleagues28 included multiple surgeons with different postoperative protocols, was not limited to SLAP IIb tears, and also had a shorter follow-up of 1 year. Like Kocaoglu and colleagues22, Bents and colleagues did find knotless anchors to be more efficient, as operative time was reduced by 5.3 minutes per anchor. This likely would have a significant impact on surgical cost and surgeon productivity.28
One limitation of the current study was that despite the inclusion of >70 patients, the study was still significantly underpowered. It was determined that >300 patients in each group would be required to detect a significant difference in the revision rate between the 2 anchor types. Also, due to the retrospective nature of this study, no preoperative scores were collected. The inclusion of objective clinical measurements and follow-up imaging evaluating the rotator cuff and other anatomy would also be of interest.
Although statistical significance was not achieved, there was a trend toward knotless fixation requiring less revision surgery and having higher RTP, ASES, and KJOC scores when compared with traditional knotted fixation at 6.5-year follow-up. Larger studies with longer follow-up periods are necessary to determine the effects of knotted and knotless anchors on rotator cuff tears, patient reported outcomes, and RTP. These complications have been shown in the literature, mostly in case reports, and typically develop over a longer period.23 Despite this, other advantages of knotless fixation, such as its lower profile, the ability to better provide consistent tensioning, and decreased surgical time are important to consider.
ABSTRACT
The use of knotless suture anchors has increased in popularity; however, there is a paucity of literature examining the difference in clinical outcomes with traditional knotted fixation. It was hypothesized that knotless fixation would provide superior clinical outcomes, improved return to play (RTP), and lower revision rates as compared with traditional knotted fixation in the repair of SLAP IIb tears. Seventy-four athletes who underwent arthroscopic SLAP IIb repair with traditional (n = 42) and knotless anchors (n = 32) by a single surgeon were evaluated after a minimum 2-year follow. Demographic and surgical data, RTP, Kerlan-Jobe Orthopaedic Clinic (KJOC) score, American Shoulder and Elbow Surgeons (ASES) score, stability, strength, and pain scores were compared. Knotless anchors had slightly higher RTP (93.5% vs 90.2%, P = .94) and RTP at the same level (58.1% vs 53.7% P = .81) compared with knotted fixation, but the difference did not reach statistical significance. Knotless anchors were less likely to require revision surgery than traditional anchors (9% vs 17%, P = .50), but the difference was not statistically significant. When comparing knotless and traditional knotted suture anchor repair of type llb SLAP tears, knotless fixation required less revision surgery and had higher RTP, ASES, and KJOC scores; however, statistical significance was not achieved in this relatively small cohort.
Continue to: Injury of the anterosuperior...
Injury of the anterosuperior labrum near the biceps origin was first described by Andrews and colleagues in 1985 in overhead athletes.1 The term SLAP, or a tear in the superior labrum anterior to posterior, was coined a few years later by Snyder and colleagues.2 They described an injury to the superior labrum beginning posteriorly and extending anteriorly, including the “anchor” of the biceps tendon to the labrum. Snyder further delineated SLAP lesions into 4 subtypes, the most common being type II, which he described as “degenerative fraying of the labrum with additional detachment of the superior labrum and biceps from the glenoid resulting in an unstable labral anchor.”2,3 Type II tears are of particular importance as they are the most common SLAP lesions, with an incidence of 55%, and comprise nearly 75% of SLAP repairs performed.2,4
Morgan and colleagues further delineated type II SLAP tears into IIa (anterior), IIb (posterior), and IIc (combined). Their group found that SLAP IIb tears were the most common type in overhead throwers, accounting for 47% of overhead athletes with type II tears.5 Further, type IIb tears can have a significant impact in throwers, in part due to greater shoulder instability as well as anterior pseudolaxity.5 SLAP injuries typically have been difficult to successfully treat nonoperatively in overhead athletes.6 A study by Edwards and colleagues6 examined 39 patients with all types of SLAP tears. Although, in their study, nonoperative management failed in 20 patients and they required surgery, 10 of the 15 overhead athletes in whom nonoperative treatment did not fail initially returned to sport at a level equal to or better than their pre-injury level, indicating that nonoperative treatment may play a role in some patients’ recovery.6
Surgical outcomes of SLAP IIb repairs have traditionally been less predictable than those of other shoulder injuries. Some believe that traditional knotted anchors may be partially to blame by abrading the rotator cuff, possibly leading to rotator cuff tears and pain. Further, knotted anchors are typically bulkier and require more experience with tying and tensioning and, therefore, may lead to less consistent results.7 The purpose of this study was to investigate if knotless anchors result in more favorable outcomes in repair of type IIb SLAP lesions when compared with traditional knotted anchors. It was hypothesized that knotless fixation will provide superior clinical outcomes, improved return to play (RTP), and lower revision rates as compared with traditional knotted fixation in the repair of SLAP IIb tears.
METHODS
PATIENT SELECTION
The authors retrospectively reviewed SLAP tears repaired by the senior author from June 2000 to September 2015. The inclusion criteria consisted of all athletes at any level who were diagnosed intraoperatively with a type IIb SLAP tear as defined by Morgan and colleagues5 with a minimum 2-year follow-up. The exclusion criteria were any patients with a previous shoulder surgery and the presence of any labral pathology aside from a SLAP IIb tear. Patients with rotator cuff or biceps pathologies were included. In all included patients, an initial course of preoperative physical therapy, including strengthening and stabilization of the scapulothoracic joint, had failed. Patient-directed surveys evaluated RTP, as well as the Kerlan-Jobe Orthopaedic Clinic (KJOC) score, American Shoulder and Elbow Surgeons (ASES) score, stability, range of motion (ROM), strength, and pain scores, as previously described.8-10 Institutional Review Board and informed consent approval were acquired prior to initiation of the study.
PATIENT EVALUATION
An appropriate preoperative history was taken, and physical examinations were performed, including evaluation of the scapulothoracic joint, as well as tests to evaluate the presence of a SLAP tear, anterior instability, posterior instability, multi-directional instability, and rotator cuff tears, as previously described.11 Patients with a history and physical examination concerning SLAP pathology underwent an magnetic resonance imaging (MRI) arthrogram, which was used in conjunction with intraoperative findings to diagnose type IIb SLAP tears.
Continue to: SURGICAL TECHNIQUE
SURGICAL TECHNIQUE
All surgeries were performed arthroscopically with the patient in the lateral decubitus position. The SLAP lesions were subsequently repaired using a technique similar to that described by Burkhart and colleagues.12 The traditional knotted fixation incorporated the use of 3.0 Bio-FASTak (Arthrex) with #2 FiberWire (Arthrex). Knotless anchor fixation was performed using 2.9 mm × 12.5 mm or 2.4 mm × 11.3 mm BioComposite PushLock (Arthrex) suture anchors, based on the size of the glenoid, with LabralTape or SutureTape (Arthrex). Patients who had surgery before January 1, 2013 underwent fixation with traditional knotted fixation; after that date, patients underwent fixation with knotless anchors.
POSTOPERATIVE REHABILITATION
Patients underwent a strict postoperative protocol in which they were kept in a sling with an abduction pillow for the first 6 weeks and performed pendulum exercises and passive motion only. A formal physical therapy regimen started at 4 weeks with passive ROM, passive posterior capsular and internal rotation stretching, scapulothoracic mobility, and biceps, rotator cuff, and capsular stabilizer strengthening. At 10 weeks, patients began biceps, rotator cuff, and scapular stabilizer resistance exercises, and at 16 weeks, throwing athletes began an interval throwing program. Patients were first eligible to return to sport without limitation at 9 months.
STATISTICAL ANALYSIS
Return to play, KJOC, ASES, stability, ROM, strength, and pain scores were analyzed and compared using Fisher exact test, the Kruskal-Wallis test, and the Wilcoxon rank sum test, where appropriate. The level of statistical significance was α = 0.05.
RESULTS
Table 1. Patient Demographics | |
Athletes (N) | 74 |
Age (yr) | 30.1 (14-64) |
Knotless anchors | 32 (43.2%) |
Knotted anchors | 42 (56.8%) |
Overhead athletes | 53 (72%) |
Throwing athletes | 29 (39%) |
Follow-up (yr) | 6.5 (2-12) |
Of the 74 athletes who met inclusion criteria, 28 were female (37.8%) and 46 (62.2%) were male. The average follow-up was 6.5 years with a minimum of 2 years and a maximum of 12 years. Forty-two (56.8%) patients underwent traditional knotted suture anchor fixation and 32 (43.2%) underwent knotless anchor fixation. The average age was 30.1 +/– 13.6 years, with a range of 14 to 64 years. The majority of athletes were right hand dominant (79.9%). Fifty-three (72%) were overhead athletes and 29 (39%) were throwing athletes (Table 1). The average age in the knotted group was 33.3 years: 29 of 42 (69%) were overhead athletes and 20 (47.6%) were throwing athletes. In the knotless group, the average age was 25.8 years: 24 of 32 (75.0%) were overhead athletes and 9 (28.1%) were throwing athletes. Primary sports at the time of injury are listed in Table 2. The average number of anchors used was 3.1, with 17 patients (23.0%) requiring ≤2 anchors, 39 (52.7%) requiring 3 anchors, and 18 (24.3%) requiring ≥4 anchors for repair. The number of anchors used was determined intraoperatively by the surgeon on the basis of the size and extent of the tear. Of the entire group of 74 patients, 91.9% returned to sport, 56.8% returned to the same level, 35.1% returned at a lower capacity, and 8.1% were unable to return to sport. Knotless anchors had a slightly higher overall RTP compared with traditional anchors (93.5% vs 90.2%, P = .94), as well as a higher RTP at the same level (58.1% vs 53.7%, P = .81). These differences were, however, not statistically significant (Table 3).
Table 2. Primary Sport at Time of SLAP IIb Injury | |
Primary Sport | n (%) |
Baseball | 14 (19.7%) |
Softball | 8 (11.3%) |
Volleyball | 6 (8.5%) |
Basketball | 5 (7.0%) |
Golf | 5 (7.0%) |
Other Sport | 33 (46.5%) |
No Primary Sport | 3 (4.1%) |
Abbreviation: SLAP, superior labrum anterior to posterior.
Knotless anchors were less likely to require revision surgery than traditional anchors (9% vs 17%, P = .50), but this difference was not statistically significant (Table 3). In the knotted group, 5 patients had revision surgery for rotator cuff tears, and 2 patients had recurrent SLAP tears. In the knotless group, 2 patients had revision surgeries for a torn rotator cuff, and 1 patient had a snapping scapula. A power analysis found that it would take over 300 athletes in each group to detect a significant difference in the revision rate between knotless and traditional anchors.
Table 3. Comparison of Anchor Type in Surgical Fixation of SLAP IIb Tears | |||||
| RTP | RTP Same Level | ASES | KJOC | Revision Rate |
Knotless anchors (n = 32) | 93.5% | 58.1% | 86.3 + 10.5 | 66.1 + 29.6 | 9% |
Traditional anchors (n = 42) | 90.2% | 53.7% | 85.3 + 15.6 | 65.6 + 27.2 | 17% |
P-value | .94 | .81 | .79 | .61 | .50 |
Abbreviations: ASES, American Shoulder and Elbow Surgeons; KJOC, Kerlan-Jobe Orthopaedic Clinic; RTP: return to play. | |||||
Continue to: Although KJOC...
Although KJOC (66.1 vs 65.6 P = .61) and ASES (86.3 vs 85.3 P = .79) scores were also superior with knotless anchors, these differences in scores were not statistically significant (Table 3). Pain was the only variable that was linked to decreased RTP, as patients who rated higher on a pain scale of 0 to 10 were less likely to return to their sport (P < .0001). There was no correlation in outcome measures or RTP with gender, age, number of anchors, or sport type (P > .05). There was no statistically significant difference in RTP, KJOC, or ASES scores between non-overhead and overhead athletes (Table 4). Overall return to sport in throwers was 85.7% (24/28), while 39.3% (11/28) returned at the same level, 46.4% (13/28) at a lower level, and 14.3% (4/28) did not return to sport.
Table 4. Overhead vs Non-Overhead Athletes After Surgical Fixation of SLAP IIb Tears | |||||
| RTP | RTP Same Level | ASES | ASES Good-Excellent | KJOC |
Overhead | 90.6% | 52.3% | 91.7 + 14.1 | 98.1% | 64.6 + 25.7 |
Non-Overhead | 95.5% | 72.7% | 86.7 + 12.7 | 100% | 88.5 + 29.6 |
P value | 0.1 | 0.29 | 0.76 | 0.50 | 0.49 |
Abbreviations: ASES, American Shoulder and Elbow Surgeons; KJOC, Kerlan-Jobe Orthopaedic Clinic; RTP: return to play. | |||||
DISCUSSION
There was no significant difference between knotted and knotless fixation in clinical outcomes or return to sport in the repair of SLAP IIb tears; however, there was a trend toward knotless anchors requiring less revision surgery and having higher RTP, ASES, and KJOC scores than knotted fixation. Despite the inclusion of 74 patients, this study was significantly underpowered, as a power analysis calculated that over 300 athletes would be required in each group to detect a difference in the revision rate.
SLAP tears, traditionally treated with knotted suture anchors, have yielded varying results in the literature, with good to excellent results being reported in 65% to 94% of patients.13-17 The success of SLAP repairs in athletes, especially overhead athletes, remains a difficult problem, as they are common injuries, and RTP is less predictable. Studies differ with regard to the percentage of overhead athletes who are able to return to their previous level of sport, with ranges being reported from 22% to 92%.16,18,19 In a systematic review of 198 patients, Sayde and colleagues16 found that 63% of overhead athletes treated with anchor fixation, tacks, or staples were able to return to their previous level of play. Morgan and colleagues5 found a higher return to sport when compared with other studies, reporting that 83% of patients undergoing SLAP repairs using traditional suture anchors had excellent results, and 87% of the 53 overhead athletes had excellent results based on UCLA shoulder scores. Further, 37 of the 44 pitchers examined (84%) were able to return to their pre-injury levels.5 This is in contrast to Friel and colleagues20 who found that in 48 patients with type II SLAP tears treated with traditional anchors, 23% reported excellent and 56% reported good results in regards to UCLA shoulder scores. Friel and colleagues also found that 62% of all athletes and 59% of overhead athletes were able to return to their previous levels of sport, which is similar to the current study.20 The large discrepancy in RTP at the pre-injury level between this study and that of Morgan and colleagues5 may be due to the shorter minimum follow-up of 1 year as well as the inclusion of all subtypes of SLAP II tears in the latter. The current study had a minimum 2-year follow-up period, with an average of 6.5 years, and was limited to SLAP IIb tears. With a longer follow-up period, patient outcomes and RTP, particularly in overhead sports, may deteriorate; therefore, the current study likely shows a more complete and accurate result.
Knotless anchors were originally introduced as a less time consuming, lower profile, and simpler device to learn and use for arthroscopic procedures.21 Kocaoglu and colleagues22 found that in Bankart repairs, the mean time per anchor placement for knotted anchors was 380 seconds, whereas placement of knotless anchors took on average 225 seconds. A learning curve also exists for proper and efficient knot tying.7 There is also variation in knot tying between surgeons, as evidenced by a wide range in both load to failure and knot height.7 A study performed by Hanypsiak and colleagues7 found that the surgical knot was the weakest portion of the suture-anchor construct, as the knot’s load to failure was less than the pullout strength of the anchor.
There is also concern for the added height associated with traditional knotted fixation, which has been supported by case reports of knot-induced glenoid erosion after arthroscopic fixation of a SLAP tear.23 Hanypsiak and colleagues7 also found that the average knot height occupied 50% to 95% of the space between the humeral head and the acromion when the shoulder is in a neutral position, indicating that the higher profile knotted anchors may contact the undersurface of the acromion, which could affect the labral repair as well as cause rotator cuff injury. Abrasion of the rotator cuff by a prominent knot may cause pain, tearing, and disability. A recent study by Park and colleagues24 reported on 11 patients with knot-induced pain after type II SLAP repair. All complained of sharp pain, with 64% also complaining of clicking. Knot location did not seem to matter, as there was no difference in preoperative symptoms, with 5 of the 11 patients having knots on the glenoid side of the repair on repeat arthroscopy. Patients with knots on the labral side did, however, have humeral head cartilage damage. The knots appeared to be the cause of pain and clicking, as after arthroscopic knot removal, dramatic pain relief was seen, with Constant and UCLA scores significantly improving in all 11 patients. All patients also had positive preoperative compression-rotation testing, and at 6 weeks after surgical knot removal, all were negative.24
Continue to: Further, as shown by Dines and colleagues...
Further, as shown by Dines and colleagues25, knotless anchors may help to better restore the meniscoid anatomy of the superior labrum better than knotted suture anchors. With regards to fixation strength, Uggen and colleagues26, using a cadaveric model, found no difference in initial fixation strength of knotless and traditional suture anchor repair of SLAP II tears, and both restored glenohumeral rotation without over-constraining the shoulder.
Despite the shorter operative time, lower profile, and more consistent tensioning with knotless anchors, the literature is limited with regard to evaluating patient outcomes. In a study by Yung and colleagues13 14 of the 16 patients with type II SLAP tears were treated with knotless anchors, and the authors found that 31.3% of patients had an excellent UCLA score while 43.8% had a good score. This is similar to the outcomes illustrated in studies by both Friel and colleagues20 and Sayde and colleagues.16 In a more recent study, Yang and colleagues27 did find some benefit in regard to ROM with knotless fixation. Their study consisted of 21 patients who underwent surgery with traditional knotted anchor fixation and 20 who underwent knotless horizontal mattress fixation. They found an average UCLA score of 37.6 and ASES score of 91.5 in patients undergoing knotless fixation, and the knotless fixation group had 5% greater total ROM, 15.6% more internal rotation at abduction, and 11.4% more external rotation at the side as compared with patients undergoing the traditional knotted technique. When compared with the current study, this study also had a significantly shorter follow-up period of 3 years.27 In a 2017 study, Bents and colleagues28 compared 44 patients who underwent knotless and 119 who underwent knotted fixation of SLAP tears. They found no statistically significant difference between knotless and knotted fixation in the ASES score, Visual Analog Scale (VAS), ASES, or Veterans RAND 12-Item Health Survey (VR-12) at 1 year postoperatively. Their outcomes were similar to those of the current study, but as in other mentioned literature, the study by Bents and colleagues28 included multiple surgeons with different postoperative protocols, was not limited to SLAP IIb tears, and also had a shorter follow-up of 1 year. Like Kocaoglu and colleagues22, Bents and colleagues did find knotless anchors to be more efficient, as operative time was reduced by 5.3 minutes per anchor. This likely would have a significant impact on surgical cost and surgeon productivity.28
One limitation of the current study was that despite the inclusion of >70 patients, the study was still significantly underpowered. It was determined that >300 patients in each group would be required to detect a significant difference in the revision rate between the 2 anchor types. Also, due to the retrospective nature of this study, no preoperative scores were collected. The inclusion of objective clinical measurements and follow-up imaging evaluating the rotator cuff and other anatomy would also be of interest.
Although statistical significance was not achieved, there was a trend toward knotless fixation requiring less revision surgery and having higher RTP, ASES, and KJOC scores when compared with traditional knotted fixation at 6.5-year follow-up. Larger studies with longer follow-up periods are necessary to determine the effects of knotted and knotless anchors on rotator cuff tears, patient reported outcomes, and RTP. These complications have been shown in the literature, mostly in case reports, and typically develop over a longer period.23 Despite this, other advantages of knotless fixation, such as its lower profile, the ability to better provide consistent tensioning, and decreased surgical time are important to consider.
1. Andrews JR, Carson WG, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13(5):337-341. doi:10.1177/036354658501300508.
2. Snyder SJ, Karzel RP, Pizzo WD, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthrosc J Arthrosc Relat Surg. 1990;6(4):274-279. doi:10.1016/0749-8063(90)90056-J.
3. Ahsan ZS, Hsu JE, Gee AO. The Snyder classification of superior labrum anterior and posterior (SLAP) lesions. Clin Orthop. 2016;474(9):2075-2078. doi:10.1007/s11999-016-4826-z.
4. Erickson BJ, Jain A, Abrams GD, et al. SLAP Lesions: Trends in treatment. Arthrosc J Arthrosc Relat Surg. 2016;32(6):976-981. doi:10.1016/j.arthro.2015.11.044.
5. Morgan C, Burkhart S, Palmeri M, Gillespie M. Type II SLAP lesions: three subtypes and their relationships to superior instability and rotator cuff tears. Arthrosc J Arthrosc Relat Surg. 1998;14(6):553-565. doi:10.1016/S0749-8063(98)70049-0.
6. Edwards SL, Lee JA, Bell J-E, et al. nonoperative treatment of superior labrum anterior posterior tears: Improvements in pain, function, and quality of life. Am J Sports Med. 2010;38(7):1456-1461. doi:10.1177/0363546510370937.
7. Hanypsiak BT, DeLong JM, Simmons L, Lowe W, Burkhart S. Knot strength varies widely among expert arthroscopists. Am J Sports Med. 2014;42(8):1978-1984. doi:10.1177/0363546514535554.
8. Alberta FG, ElAttrache NS, Bissell S, et al. The development and validation of a functional assessment tool for the upper extremity in the overhead athlete. Am J Sports Med. 2010;38(5):903-911. doi:10.1177/0363546509355642.
9. Bradley JP, McClincy MP, Arner JW, Tejwani SG. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 200 shoulders. Am J Sports Med. 2013;41(9):2005-2014. doi:10.1177/0363546513493599.
10. Michener LA, McClure PW, Sennett BJ. American shoulder and elbow surgeons standardized shoulder assessment form, patient self-report section: Reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587-594. doi:10.1067/mse.2002.127096.
11. Cook C, Hegedus EJ. Orthopedic Physical Examination Tests: An Evidence-Based Approach. Upper Saddle River, NJ: PearsonPrentice Hall; 2008.
12. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: Spectrum of pathology part I: Pathoanatomy and biomechanics. Arthrosc J Arthrosc Relat Surg. 2003;19(4):404-420. doi:10.1053/jars.2003.50128.
13. Yung PS-H, Fong DT-P, Kong M-F, et al. Arthroscopic repair of isolated type II superior labrum anterior–posterior lesion. Knee Surg Sports Traumatol Arthrosc. 2008;16(12):1151-1157. doi:10.1007/s00167-008-0629-4.
14. Brockmeier SF, Voos JE, Williams RJ, Altchek DW, Cordasco FA, Allen AA. Outcomes After Arthroscopic Repair of Type-II SLAP Lesions: J Bone Jt Surg-Am Vol. 2009;91(7):1595-1603. doi:10.2106/JBJS.H.00205.
15. Galano GJ, Ahmad CS, Bigliani L, Levine W. Percutaneous SLAP lesion repair technique is an effective alternative to portal of Wilmington. Orthopedics. 2010;33(11). doi:10.3928/01477447-20100924-15.
16. Sayde WM, Cohen SB, Ciccotti MG, Dodson CC. Return to play after type II superior labral anterior-posterior lesion repairs in athletes: A systematic review. Clin Orthop Relat Res. 2012;470(6):1595-1600. doi:10.1007/s11999-012-2295-6.
17. Kim K-H, Bin S-I, Kim J-M. The correlation between posterior tibial slope and maximal angle of flexion after total knee arthroplasty. Knee Surg Relat Res. 2012;24(3):158-163. doi:10.5792/ksrr.2012.24.3.158.
18. Kim S-H, Ha K-I, Kim S-H, Choi H-J. Results of arthroscopic treatment of superior labral lesions. J Bone Joint Surg Am. 2002;84-A(6):981-985.
19. Pagnani MJ, Speer KP, Altchek DW, Warren RF, Dines DM. Arthroscopic fixation of superior labral lesions using a biodegradable implant: a preliminary report. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 1995;11(2):194-198.
20. Friel NA, Karas V, Slabaugh MA, Cole BJ. Outcomes of type II superior labrum, anterior to posterior (SLAP) repair: Prospective evaluation at a minimum two-year follow-up. J Shoulder Elbow Surg. 2010;19(6):859-867. doi:10.1016/j.jse.2010.03.004.
21. Thal R. A knotless suture anchor. Arthrosc J Arthrosc Relat Surg. 2001;17(2):213-218. doi:10.1053/jars.2001.20666.
22. Kocaoglu B, Guven O, Nalbantoglu U, Aydin N, Haklar U. No difference between knotless sutures and suture anchors in arthroscopic repair of Bankart lesions in collision athletes. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):844-849. doi:10.1007/s00167-009-0811-3.
23. Rhee YG, Ha JH. Knot-induced glenoid erosion after arthroscopic fixation for unstable superior labrum anterior-posterior lesion: Case report. J Shoulder Elbow Surg. 2006;15(3):391-393. doi:10.1016/j.jse.2005.03.010.
24. Park JG, Cho NS, Kim JY, Song JH, Hong SJ, Rhee YG. Arthroscopic Knot Removal for Failed Superior Labrum Anterior-Posterior Repair Secondary to Knot-Induced Pain. Am J Sports Med. 2017;45(11):2563-2568. doi:10.1177/0363546517713662.
25. Dines JS, ElAttrache NS. Horizontal Mattress With a Knotless Anchor to Better Recreate the Normal Superior Labrum Anatomy. Arthrosc J Arthrosc Relat Surg. 2008;24(12):1422-1425. doi:10.1016/j.arthro.2008.06.012.
26. Uggen C, Wei A, Glousman RE, et al. Biomechanical Comparison of Knotless Anchor Repair Versus Simple Suture Repair for Type II SLAP Lesions. Arthrosc J Arthrosc Relat Surg. 2009;25(10):1085-1092. doi:10.1016/j.arthro.2009.03.022.
27. Yang HJ, Yoon K, Jin H, Song HS. Clinical outcome of arthroscopic SLAP repair: conventional vertical knot versus knotless horizontal mattress sutures. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):464-469. doi:10.1007/s00167-014-3449-8.
28. Bents EJ, Brady PC, Adams CR, Tokish JM, Higgins LD, Denard PJ. Patient-reported outcomes of knotted and knotless glenohumeral labral repairs are equivalent. Am J Orthop. 2017;46(6):279-283.
1. Andrews JR, Carson WG, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13(5):337-341. doi:10.1177/036354658501300508.
2. Snyder SJ, Karzel RP, Pizzo WD, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthrosc J Arthrosc Relat Surg. 1990;6(4):274-279. doi:10.1016/0749-8063(90)90056-J.
3. Ahsan ZS, Hsu JE, Gee AO. The Snyder classification of superior labrum anterior and posterior (SLAP) lesions. Clin Orthop. 2016;474(9):2075-2078. doi:10.1007/s11999-016-4826-z.
4. Erickson BJ, Jain A, Abrams GD, et al. SLAP Lesions: Trends in treatment. Arthrosc J Arthrosc Relat Surg. 2016;32(6):976-981. doi:10.1016/j.arthro.2015.11.044.
5. Morgan C, Burkhart S, Palmeri M, Gillespie M. Type II SLAP lesions: three subtypes and their relationships to superior instability and rotator cuff tears. Arthrosc J Arthrosc Relat Surg. 1998;14(6):553-565. doi:10.1016/S0749-8063(98)70049-0.
6. Edwards SL, Lee JA, Bell J-E, et al. nonoperative treatment of superior labrum anterior posterior tears: Improvements in pain, function, and quality of life. Am J Sports Med. 2010;38(7):1456-1461. doi:10.1177/0363546510370937.
7. Hanypsiak BT, DeLong JM, Simmons L, Lowe W, Burkhart S. Knot strength varies widely among expert arthroscopists. Am J Sports Med. 2014;42(8):1978-1984. doi:10.1177/0363546514535554.
8. Alberta FG, ElAttrache NS, Bissell S, et al. The development and validation of a functional assessment tool for the upper extremity in the overhead athlete. Am J Sports Med. 2010;38(5):903-911. doi:10.1177/0363546509355642.
9. Bradley JP, McClincy MP, Arner JW, Tejwani SG. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 200 shoulders. Am J Sports Med. 2013;41(9):2005-2014. doi:10.1177/0363546513493599.
10. Michener LA, McClure PW, Sennett BJ. American shoulder and elbow surgeons standardized shoulder assessment form, patient self-report section: Reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587-594. doi:10.1067/mse.2002.127096.
11. Cook C, Hegedus EJ. Orthopedic Physical Examination Tests: An Evidence-Based Approach. Upper Saddle River, NJ: PearsonPrentice Hall; 2008.
12. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: Spectrum of pathology part I: Pathoanatomy and biomechanics. Arthrosc J Arthrosc Relat Surg. 2003;19(4):404-420. doi:10.1053/jars.2003.50128.
13. Yung PS-H, Fong DT-P, Kong M-F, et al. Arthroscopic repair of isolated type II superior labrum anterior–posterior lesion. Knee Surg Sports Traumatol Arthrosc. 2008;16(12):1151-1157. doi:10.1007/s00167-008-0629-4.
14. Brockmeier SF, Voos JE, Williams RJ, Altchek DW, Cordasco FA, Allen AA. Outcomes After Arthroscopic Repair of Type-II SLAP Lesions: J Bone Jt Surg-Am Vol. 2009;91(7):1595-1603. doi:10.2106/JBJS.H.00205.
15. Galano GJ, Ahmad CS, Bigliani L, Levine W. Percutaneous SLAP lesion repair technique is an effective alternative to portal of Wilmington. Orthopedics. 2010;33(11). doi:10.3928/01477447-20100924-15.
16. Sayde WM, Cohen SB, Ciccotti MG, Dodson CC. Return to play after type II superior labral anterior-posterior lesion repairs in athletes: A systematic review. Clin Orthop Relat Res. 2012;470(6):1595-1600. doi:10.1007/s11999-012-2295-6.
17. Kim K-H, Bin S-I, Kim J-M. The correlation between posterior tibial slope and maximal angle of flexion after total knee arthroplasty. Knee Surg Relat Res. 2012;24(3):158-163. doi:10.5792/ksrr.2012.24.3.158.
18. Kim S-H, Ha K-I, Kim S-H, Choi H-J. Results of arthroscopic treatment of superior labral lesions. J Bone Joint Surg Am. 2002;84-A(6):981-985.
19. Pagnani MJ, Speer KP, Altchek DW, Warren RF, Dines DM. Arthroscopic fixation of superior labral lesions using a biodegradable implant: a preliminary report. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 1995;11(2):194-198.
20. Friel NA, Karas V, Slabaugh MA, Cole BJ. Outcomes of type II superior labrum, anterior to posterior (SLAP) repair: Prospective evaluation at a minimum two-year follow-up. J Shoulder Elbow Surg. 2010;19(6):859-867. doi:10.1016/j.jse.2010.03.004.
21. Thal R. A knotless suture anchor. Arthrosc J Arthrosc Relat Surg. 2001;17(2):213-218. doi:10.1053/jars.2001.20666.
22. Kocaoglu B, Guven O, Nalbantoglu U, Aydin N, Haklar U. No difference between knotless sutures and suture anchors in arthroscopic repair of Bankart lesions in collision athletes. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):844-849. doi:10.1007/s00167-009-0811-3.
23. Rhee YG, Ha JH. Knot-induced glenoid erosion after arthroscopic fixation for unstable superior labrum anterior-posterior lesion: Case report. J Shoulder Elbow Surg. 2006;15(3):391-393. doi:10.1016/j.jse.2005.03.010.
24. Park JG, Cho NS, Kim JY, Song JH, Hong SJ, Rhee YG. Arthroscopic Knot Removal for Failed Superior Labrum Anterior-Posterior Repair Secondary to Knot-Induced Pain. Am J Sports Med. 2017;45(11):2563-2568. doi:10.1177/0363546517713662.
25. Dines JS, ElAttrache NS. Horizontal Mattress With a Knotless Anchor to Better Recreate the Normal Superior Labrum Anatomy. Arthrosc J Arthrosc Relat Surg. 2008;24(12):1422-1425. doi:10.1016/j.arthro.2008.06.012.
26. Uggen C, Wei A, Glousman RE, et al. Biomechanical Comparison of Knotless Anchor Repair Versus Simple Suture Repair for Type II SLAP Lesions. Arthrosc J Arthrosc Relat Surg. 2009;25(10):1085-1092. doi:10.1016/j.arthro.2009.03.022.
27. Yang HJ, Yoon K, Jin H, Song HS. Clinical outcome of arthroscopic SLAP repair: conventional vertical knot versus knotless horizontal mattress sutures. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):464-469. doi:10.1007/s00167-014-3449-8.
28. Bents EJ, Brady PC, Adams CR, Tokish JM, Higgins LD, Denard PJ. Patient-reported outcomes of knotted and knotless glenohumeral labral repairs are equivalent. Am J Orthop. 2017;46(6):279-283.
TAKE-HOME POINTS
- SLAP IIb tears are common injuries in overhead athletes, yet surgical outcomes are variable, with throwers commonly having difficulty with return to play at the same level.
- In this study, 92% of athletes returned to play post-operatively, yet only around 55% returned at the same level.
- In overhead athletes, overall return to play was 85.7%, yet only 39.3% returned at the same level.
- Knotless fixation required less revision surgery and had higher outcome scores and return to play when compared to knotted fixation; however, this did not reach statistical significance.
- Knotless fixation should be considered in SLAP IIb repairs given their lower profile leading to less rotator cuff irritation, the ability to better provide more consistent tensioning, and decreased surgical time.
In Throwers With Posterior Instability, Rotator Cuff Tears Are Common but Do Not Affect Surgical Outcomes
ABSTRACT
In a previous study, compared with throwing athletes with superior labral anterior posterior (SLAP) tears, those with concomitant SLAP tears and rotator cuff tears (RCTs) had significantly poorer outcome scores and return to play. Posterior shoulder instability also occurs in throwing athletes, but no studies currently exist regarding outcomes of these patients with concomitant RCTs.
The authors hypothesized that throwing athletes treated with arthroscopic capsulolabral repair for posterior shoulder instability with coexistent rotator cuff pathology would have poorer outcome scores and return to play.
Fifty-six consecutive throwing athletes with unidirectional posterior shoulder instability underwent arthroscopic capsulolabral repair. Preoperative and postoperative patient-centered outcomes of pain, stability, function, range of motion, strength, and American Shoulder and Elbow Surgeons Shoulder (ASES) scores, as well as return to play, were evaluated. Patients with and without rotator cuff pathology were compared.
Forty-three percent (24/56) of throwing athletes had rotator cuff pathology in addition to posterior capsulolabral pathology. All RCTs were débrided. At a mean of 3 years, there were no differences in preoperative and postoperative patient-centered outcomes between those with and without RCTs. Return-to-play rates showed no between-group differences; 92% (22/24) of athletes with concomitant RCTs returned to sport (P = .414) and 67% (16/24) returned to the same level (P = .430).
Arthroscopic capsulolabral reconstruction is successful in throwing athletes with RCTs treated with arthroscopic débridement. Unlike the previous study evaluating throwers outcomes after surgical treatment for concomitant SLAP tears and RCTs, the authors found no difference in patient-reported outcome measures or return to play for throwing athletes with concomitant posterior shoulder instability and RCTs. In throwing athletes with concomitant posterior instability and RCTs, arthroscopic posterior capsulolabral repair with rotator cuff débridement is successful.
Continue to: Posterior shoulder instability...
Posterior shoulder instability is an important and increasingly recognized pathology among throwers. Like the superior labrum, the posterior capsulolabral complex is also susceptible to injury during the throwing motion; the posterior labrum being most at risk during the late cocking and follow-through phases. Recent studies have found that arthroscopic capsulolabral reconstruction in posterior shoulder instability is successful in allowing athletes to return to their preinjury sports activities, with 2 studies detailing outcomes in throwing athletes.1-4 However, superior labral anterior posterior (SLAP) tears are common in throwing athletes and have been treated with varying and limited success. Further, in a study of outcomes of arthroscopic repair of SLAP lesions, Neri and colleagues5 found that, compared with throwing athletes with SLAP tears, throwing athletes with concomitant SLAP tears and partial-thickness rotator cuff tears (RCTs) had significantly poorer outcomes and return-to-play rates after surgical repair.
The purpose of this study was to determine outcome scores and return to play of throwing athletes treated with arthroscopic capsulolabral repair for posterior shoulder instability with coexistent RCTs and to compare them with outcome scores as well as return to play of throwing athletes with isolated posterior shoulder instability. It was hypothesized that throwing athletes with a combination of posterior shoulder instability and RCT would have poorer outcomes and poorer return to play after surgery.5
METHODS
PATIENT SELECTION
After Institutional Review Board approval, informed consent was obtained, and consecutive throwing athletes who underwent arthroscopic posterior capsulolabral reconstruction for posterior shoulder instability were followed in the perioperative period. Inclusion criteria were throwing athletes participating in competitive sports at the high school, collegiate, or professional level, minimum 1-year follow-up, presence of unidirectional posterior instability, and absence of symptoms of instability in any direction other than posterior. Patients with inferior instability, SLAP pathology on examination and on magnetic resonance imaging, multidirectional instability, or habitual or psychogenic voluntary shoulder subluxations were excluded. Patients with diagnoses of both posterior shoulder instability and impingement treated with subacromial decompression and distal clavicle resection were also excluded.
After this cohort was identified, patient records were reviewed for pertinent operative data, such as procedure, complications, and evidence of RCT by operative report and arthroscopic photographs. A partial RCT was defined as a tear of 10% to 50%; those with rotator cuff fraying were determined not to be significant.
PATIENT EVALUATION
Surgeries were performed between January 1998 and December 2009 by the senior author (JPB). All patients were followed with clinical examinations, radiographs, and subjective grading scales. Recorded patient demographic data included age, sex, sport, position, competition level, and follow-up duration.
Continue to: All patients had...
All patients had symptomatic posterior shoulder instability, including posterior shoulder pain, clicking, a sensation of subluxation, or instability/apprehension with motion. Each athlete’s shoulder was palpated for tenderness and tested for impingement. Specific posterior glenohumeral instability tests, including the Kim test,6 the circumduction test, the jerk test,7 the posterior load-and-shift test,8 and the posterior stress test,9 were performed on all patients. Patients with multidirectional instability on the sulcus test, as well as provocative tests indicating SLAP pathology, such as the Crank test and the active compression test, were not included. Standard radiography and magnetic resonance arthrography (MRA) were performed to further narrow inclusion and exclusion criteria.
Both before surgery and at latest follow-up, patient outcomes were evaluated using the American Shoulder and Elbow Surgeons (ASES) score (range, 0-100) which combines a subjective functional scale measuring activities of daily living (0-3 for each of 10 tasks, with a total of 0-30) and a subjective pain scale (0-10, with 10 being worst pain). Values >80 were described as excellent, and failures were defined as scores <60 after surgery.10 A subjective stability scale (0-10, with 0 indicating completely stable and 10 completely unstable), strength scale (0-3, with 0 indicating none, 1 markedly decreased, 2 slightly decreased, and 3 normal), and ROM scale (0-3, with 0 indicating poor, 1 limited, 2 satisfactory, and 3 full) were evaluated both before surgery and at the latest follow-up. A stability score >5 after surgery was defined as a failure.1,2,11 Patients were also asked if, based on their current state, they would undergo surgery again. Intraoperative findings and specific surgical procedures performed were correlated with the aforementioned subjective and objective outcome scores.
OPERATIVE TREATMENT
Throwing athletes who met inclusion criteria and failed nonoperative management underwent surgery by the senior author (JPB). Each patient was examined under anesthesia and, with the patient in the lateral decubitus position, a diagnostic arthroscopy was performed to identify posterior capsulolabral complex pathology, including a patulous capsule, capsular tears, labral fraying, and labral tears. A careful examination for rotator cuff pathology was also performed. Based on preoperative clinical examination, MRA, examination under anesthesia, pathologic findings at diagnostic arthroscopic surgery, and surgeon experience, capsulolabral plication was performed with or without suture anchors.2,5 After capsulolabral repair, the capsule was evaluated for residual laxity, and additional plication sutures were placed, as indicated, with care to avoid overconstraint in these throwing athletes.1 Posterior glenohumeral stability restoration was judged by removing traction and performing posterior load-and-shift and posterior stress tests. Any RCT with <50% thickness was débrided. Postoperative care and rehabilitation were carried out as previously described and were not altered by the presence or absence of a RCT.3
STATISTICAL ANALYSIS
Preoperative and latest follow-up ASES scores, stability scores, functional scores, and pain-level findings were compared using paired-samples Comparisons between groups, including throwing athletes with and without rotator cuff pathology, were done using the Student t test. Outcome comparisons between multiple groups, which included intraoperative findings and surgical fixation methods, were analyzed with c2 modeling for nonparametric data. Statistical significance was set at P < .05. A power analysis found that this study was able to detect a meaningful difference of 10 ASES points.
RESULTS
PATIENT DEMOGRAPHIC CHARACTERISTICS
Of the 56 throwing athletes who met the inclusion criteria, 24 were found to have rotator cuff pathology in addition to posterior capsulolabral pathology, while 32 were found to have capsulolabral pathology alone. Demographic data are listed in Table 1. Mean age was 20.1 years for patients with rotator cuff pathology and 17.8 years for patients without RCTs. All 24 athletes with rotator cuff pathology were treated with arthroscopic débridement. Mean follow-up was 38.6 months (range, 16.5-63.6 months) for patients with RCTs and 39.1 months (range, 12-98.8 months) for patients without RCTs. No significant difference was found in age, sports level, or follow-up between groups.
Table 1. Demographic Data for Athletes With Posterior Instability With and Without Rotator Cuff Tears (N = 56 Shoulders)a
Characteristic | Rotator Cuff Tears | |
Yes | No | |
| Total | 24 | 32 |
| Sex | ||
| Male | 16 | 27 |
| Female | 8 | 5 |
| Mean age, y | 20.1 | 17.8 |
| Mean follow up, mo | 38.6 | 39.1 |
| Participation level | ||
| Professional | 1 | 0 |
| College | 4 | 4 |
| High school | 17 | 26 |
| Recreational | 2 | 2 |
aThe majority of athletes were males in high school and their mean follow-up was 3 years.
Continue to: Outcomes
OUTCOMES
Table 2 lists the preoperative and postoperative scores for shoulder performance in throwing athletes with posterior shoulder instability, with and without RCTs.
Table 2. Preoperative and Postoperative Scores for Shoulder Performance in Throwing Athletes With Posterior Shoulder Instability With and Without Rotator Cuff Tearsa
| With Rotator Cuff Tears (n=24 shoulders) | Without Rotator Cuff Tears (n=32 shoulders) | |||||||||
| Preoperative | Latest Follow-Up | Preoperative | Latest Follow-Up | |||||||
| Outcome Measure | Mean Score | Range | Mean Score | Range | P | Mean Score | Range | Mean Score | Range | P |
ASES 0-100 0 = worst | 41.8 | 20-70 | 85.4 | 67-100 | <.05 | 49.7 | 20-85 | 83.1 | 25-100 | <.05 |
Stability 0-10 0 = most stable | 6.7 | 2-10 | 2.4 | 0-6 | <.05 | 7.8 | 0-10 | 2.4 | 0-8 | <.05 |
Pain 0-10 10 = worst | 7.6 | 5-10 | 1.9 | 0-5 | <.05 | 6.3 | 0-10 | 2.2 | 0-7 | <.05 |
Function 0-30 0 = worst | 18.5 | 6-27 | 27 | 16-30 | <.05 | 19.0 | 8-26 | 26.4 | 6-30 | <.05 |
aThere was no difference in ASES, stability, pain, or functional scores between athletes with posterior instability alone compared with patients with concomitant rotator cuff tears.
Abbreviation: ASES, American Shoulder and Elbow Surgeons.
ASES Scores. Mean preoperative ASES scores for patients with RCTs improved significantly (t = –13.8, P < .001), as did those for patients without rotator cuff pathology (t = –8.9, P < .001). No significant differences in ASES score were found between patients with and without rotator cuff pathology before or after surgery (t = 1.9, P = .07; t = .58, P = .06). In addition, 70.8% (17/24) of throwing athletes with rotator cuff pathology had an excellent postoperative outcome (ASES score >80), and 29.2% (7/24) had a satisfactory outcome (ASES score, 60-80). Thus, 100% of those with concomitant posterior shoulder instability and RCTs had a good or excellent outcome after surgical intervention. In those without rotator cuff pathology, 78.1% (25/32) had an excellent outcome, 12.5% (4/32) had a satisfactory outcome, and 9.4% (3/32) had a poor outcome. Thus, 91% of those without rotator cuff pathology had a good or excellent outcome after surgery.
Stability. Preoperative stability scores improved significantly after surgery in both groups (t = 7.2, P < .001; t = 10.5, P < .001). There were no statistical differences between preoperative or postoperative stability scores in those with or without rotator cuff pathology (t = 1.7, P = .095; t = .03, P = .975). Of throwing athletes with RCTs, 54.2% (13/24) had an excellent outcome, 33.3% (8/24) a good outcome, and 12.5% (3/24) a satisfactory outcome. Thus, 87.5% (21/24) of those with RCTs had a good or excellent outcome in terms of stability. In those without rotator cuff pathology, 46.9% (15/32) had excellent stability, 46.9% (15/32) had good stability, and 3.1% (1/32) had satisfactory stability after surgery. Thus, 93.8% (30/32) of throwing athletes without rotator cuff pathology had good or excellent stability after surgery.
Pain. Mean preoperative pain scores for those with and without rotator cuff pathology improved significantly (t = 13.4, P < .001; t = 7.1, P < .001). There was no statistical difference in preoperative or postoperative pain scores between those with and without rotator cuff pathology (t = 1.99, P = .051; t = .49, P = .627).
Function. Mean preoperative function scores for both groups improved significantly (t = 7.7, P < .001; t = 8.0, P < .001). There was no difference in improvement in functional scores between the two groups before or after surgery (t = .36, P = .721; t = .5, P = .622).
Continue to: ROM
ROM. Of those with rotator cuff pathology, 54% (13/24) had normal ROM, 42% (10/24) had satisfactory ROM, and 4% (1/24) had limited ROM. In throwing athletes without rotator cuff pathology, 34% (11/32) had normal ROM, 53.1% (17/32) had satisfactory ROM, and 9% (3/32) had limited ROM after surgery. There was no significant difference in ROM between the groups (c2 = 2.7, P = .260).
Strength. Of those with RCTs, 67% (16/24) reported normal strength, 29% (7/24) slightly decreased strength, and 4% (1/24) markedly decreased strength. Of those throwing athletes without rotator cuff pathology, 50% (16/32) had normal strength, 41% (13/32) had slightly decreased strength, and 9% (3/32) had markedly decreased strength. No statistical difference was noted between the two groups (c2 = 1.7, P = .429).
Return to Sport. Of those with RCTs, 92% (22/24) returned to sport while 84% (27/32) of throwing athletes without RCTs returned to sport. There was no difference between the two groups (c2 = .667, P = .414). Sixty-seven percent (16/24) of those with RCTs and 56% (18/32) of those without RCTs returned to the same level of sport. No statistical difference was found in return to play between throwing athletes with and without rotator cuff pathology (c2 = .624, P = .430).
Failures. According to ASES scores, no throwers with RCTs failed, while 9.4% (3/32) with posterior instability alone failed. Regarding stability, 8.3% (2/24) of athletes with RCTs failed, while 6.3% (2/32) with posterior instability alone failed.
SURGICAL FINDINGS AND PROCEDURES
Of the 24 throwing athletes with rotator cuff pathology, 92% (22/24) had labral tears, while 78% (25/32) of those without RCTs had labral tears. The majority of RCTs were in the posterior supraspinatus and anterior infraspinatus regions. This was not significantly different between groups (c2 = 1.86, P = .172). All labral pathology was posterior-inferior, and all RCTs were <50% thickness, and therefore were débrided. Fifty-four percent (13/24) of those with RCTs had a patulous capsule and 63% (20/32) of throwing athletes without rotator cuff pathology had a patulous capsule. There was no significant difference between groups (c2 = .393, P = .530). Of those with RCTs, 92% (22/24) had surgical fixation with anchors, while 78% (25/32) of those without rotator cuff pathology underwent repair with anchor fixation. There was no statistically significant difference in anchor use between groups (c2 = 1.86, P = .172).
Continue to: Discussion
DISCUSSION
Throwing athletes with and without RCTs had similar rates of recovery and return to play after arthroscopic capsular labral repair, with rotator cuff débridement if a tear was present. The mean follow-up was 3.2 years. Further, there was no difference in return to play (92% vs 84%), ASES score, stability, pain, function, ROM, or strength between the 2 groups before or after surgery. In this cohort of 56 patients, 24 throwing athletes (43%) were found to have RCTs.
Return-to-play rates showed no between-group differences; 92% (22/24) of athletes with concomitant RCTs returned to sport, and 67% (16/24) returned to the same level. Eight percent of throwing athletes with RCTs were unable to return to sport after surgery. These return-to-play rates are an improvement over most previously reported rates in throwing athletes and in posterior shoulder instability in general.1-4,11 When these athletes are compared with their counterparts with combined SLAP tears and RCTs, return-to-play rates are notably higher. There may be discrepancies in interpreting return-to-play between the two studies, but in the current study, 67% of those with concomitant RCTs achieved return to preinjury level of play. This is 10% higher than the rate reported in athletes with SLAP tears alone (57%) and even higher than in those with concomitant SLAP and RCTs. It is also essential to note that a number of this cohort’s athletes who did not return to play did so for factors (eg, graduation) unrelated to the shoulder. However, the study by Neri and colleagues5 included professional athletes who likely all attempted to return to play and, if unable to perform at the same level, likely were unable to continue their professional career.5
All patients with RCTs had a good or excellent outcome (ASES score), and 70.8% had an excellent outcome. Similarly, 97% of those without rotator cuff pathology had a good or excellent outcome, and 81.3% had an excellent outcome. There was no significant difference between the two groups. These results parallel those of Neri and colleagues’5 study of SLAP tears with RCTs, where 96% (22/23) of throwing athletes had a good or excellent outcome. Despite these high outcome scores in patients with SLAP tears, only 57% were able to return to elite pitching.5 In the current study, pain was slightly higher for those with rotator cuff pathology before surgery—a finding consistent with pain frequently being found in patients with isolated partial-thickness RCTs. Their postoperative pain scores were actually lower on average than those of patients without RCTs, which suggests simple débridement of undersurface tears adequately addressed the pathology. The authors theorize that the main pain generator in this population may be posterior instability, and that the rotator cuff has less of an influence. In the SLAP population, the main pain generator likely is the RCT.
Failures by ASES score or strength were fairly rare in this cohort. Many patients opted to have revision surgery because of continued instability, pain, decreased function, or reinjury. One potential cause of failure in this cohort is inadequate capsular shift. However, capsular plication in throwing athletes is difficult to address, as overtensioning the repair can lead to the inability to adequately perform overhead activites.3,4 This cannot be overemphasized, particularly with pitchers.
Partial-thickness RCTs, particularly those on the articular side, are common in throwing athletes because of high tensile and compressive loads.12 Despite the known risk of RCTs with posterior shoulder instability in throwing athletes, the authors are unaware of reports of the incidence or treatment of this pathology. RCTs in this posterior instability group likely represent a pathology other than internal impingement. The high proportion of throwing athletes with RCTs in this study (43%) indicates a need for close evaluation of rotator cuff pathology in young throwing athletes. Ide et al found that 75% of patients with SLAP tears had partial articular-sided RCTs.13 In the current study, all RCTs were small partial tears, and arthroscopic débridement was performed. It is unknown whether repair of these RCTs would impact return to play. However, rotator cuff repair in this population has been shown to have poor outcomes. Tear thickness typically is used to determine treatment, with débridement performed if <50% tendon thickness is affected. More recently, many have advocated having greater tendon involvement in throwers before repair, because of poor outcomes. Although studies are limited, tear size does seem to correlate with outcomes.14
Continue to: Study Limitations
STUDY LIMITATIONS
Limitations of this study include its small number of professional throwing athletes, with the majority being high school athletes. Further, although ASES scores are consistently used in posterior shoulder instability studies, these scores are influenced highly by pain scores, and some argue that other scoring systems may provide more useful information. However, none of the more modern scoring systems have been studied extensively in posterior glenohumeral instability. Further, because the authors used the present scoring systems previously,1-4 they were continued to be used for comparison and consistency. Outcomes such as ROM and strength may carry more weight if measured and documented by clinical examination. Further testing, such as clinical evaluation of the jerk test or the posterior load-and-shift test, and their comparison before and after surgery may provide more objective data.
CONCLUSION
Arthroscopic capsulolabral reconstruction is successful in throwing athletes with RCTs treated with arthroscopic débridement. Unlike a previous study of throwing athletes’ outcomes after surgery for concomitant SLAP tears and RCTs,5 this study of throwing athletes with concomitant posterior shoulder instability and RCTs found no difference in patient-reported outcome measures or return to play. In throwing athletes with posterior instability and RCTs, arthroscopic posterior capsulolabral repair with rotator cuff débridement is successful.
1. Bradley JP, Baker CL 3rd, Kline AJ, Armfield DR, Chhabra A. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 100 shoulders. Am J Sports Med. 2006;34(7):1061-1071.
2. Bradley JP, McClincy MP, Arner JW, Tejwani SG. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 200 shoulders. Am J Sports Med. 2013;41(9):2005-2014.
3. McClincy MP, Arner JW, Bradley JP. Posterior shoulder instability in throwing athletes: a case-matched comparison of throwers and non-throwers. Arthroscopy. 2015;31(6):1041-1051.
4. Radkowski CA, Chhabra A, Baker CL 3rd, Tejwani SG, Bradley JP. Arthroscopic capsulolabral repair for posterior shoulder instability in throwing athletes compared with nonthrowing athletes. Am J Sports Med. 2008;36(4):693-699.
5. Neri BR, ElAttrache NS, Owsley KC, Mohr K, Yocum LA. Outcome of type II superior labral anterior posterior repairs in elite overhead athletes: effect of concomitant partial-thickness rotator cuff tears. Am J Sports Med. 2011;39(1):114-120.
6. Kim SH, Park JS, Jeong WK, Shin SK. The Kim test: a novel test for posteroinferior labral lesion of the shoulder—a comparison to the jerk test. Am J Sports Med. 2005;33(8):1188-1192.
7. Antoniou J, Duckworth DT, Harryman DT 2nd. Capsulolabral augmentation for the management of posteroinferior instability of the shoulder. J Bone Joint Surg Am. 2000;82(9):1220-1230.
8. Altchek DW, Hobbs WR. Evaluation and management of shoulder instability in the elite overhead thrower. Orthop Clin North Am. 2001;32(3):423-430, viii.
9. Fuchs B, Jost B, Gerber C. Posterior-inferior capsular shift for the treatment of recurrent, voluntary posterior subluxation of the shoulder. J Bone Joint Surg Am. 2000;82(1):16-25.
10. Richards RR, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3(6):347-352.
11. Arner JW, McClincy MP, Bradley JP. Arthroscopic stabilization of posterior shoulder instability is successful in American football players. Arthroscopy. 2015;31(8):1466-1471.
12. Mazoue CG, Andrews JR. Repair of full-thickness rotator cuff tears in professional baseball players. Am J Sports Med. 2006;34(2):182-189.
13. Ide J, Maeda S, Takagi K. Sports activity after arthroscopic superior labral repair using suture anchors in overhead-throwing athletes. Am J Sports Med. 2005;33(4):507-514.
14. Economopoulos KJ, Brockmeier SF. Rotator cuff tears in overhead athletes. Clin Sports Med. 2012;31(4):675-692.
ABSTRACT
In a previous study, compared with throwing athletes with superior labral anterior posterior (SLAP) tears, those with concomitant SLAP tears and rotator cuff tears (RCTs) had significantly poorer outcome scores and return to play. Posterior shoulder instability also occurs in throwing athletes, but no studies currently exist regarding outcomes of these patients with concomitant RCTs.
The authors hypothesized that throwing athletes treated with arthroscopic capsulolabral repair for posterior shoulder instability with coexistent rotator cuff pathology would have poorer outcome scores and return to play.
Fifty-six consecutive throwing athletes with unidirectional posterior shoulder instability underwent arthroscopic capsulolabral repair. Preoperative and postoperative patient-centered outcomes of pain, stability, function, range of motion, strength, and American Shoulder and Elbow Surgeons Shoulder (ASES) scores, as well as return to play, were evaluated. Patients with and without rotator cuff pathology were compared.
Forty-three percent (24/56) of throwing athletes had rotator cuff pathology in addition to posterior capsulolabral pathology. All RCTs were débrided. At a mean of 3 years, there were no differences in preoperative and postoperative patient-centered outcomes between those with and without RCTs. Return-to-play rates showed no between-group differences; 92% (22/24) of athletes with concomitant RCTs returned to sport (P = .414) and 67% (16/24) returned to the same level (P = .430).
Arthroscopic capsulolabral reconstruction is successful in throwing athletes with RCTs treated with arthroscopic débridement. Unlike the previous study evaluating throwers outcomes after surgical treatment for concomitant SLAP tears and RCTs, the authors found no difference in patient-reported outcome measures or return to play for throwing athletes with concomitant posterior shoulder instability and RCTs. In throwing athletes with concomitant posterior instability and RCTs, arthroscopic posterior capsulolabral repair with rotator cuff débridement is successful.
Continue to: Posterior shoulder instability...
Posterior shoulder instability is an important and increasingly recognized pathology among throwers. Like the superior labrum, the posterior capsulolabral complex is also susceptible to injury during the throwing motion; the posterior labrum being most at risk during the late cocking and follow-through phases. Recent studies have found that arthroscopic capsulolabral reconstruction in posterior shoulder instability is successful in allowing athletes to return to their preinjury sports activities, with 2 studies detailing outcomes in throwing athletes.1-4 However, superior labral anterior posterior (SLAP) tears are common in throwing athletes and have been treated with varying and limited success. Further, in a study of outcomes of arthroscopic repair of SLAP lesions, Neri and colleagues5 found that, compared with throwing athletes with SLAP tears, throwing athletes with concomitant SLAP tears and partial-thickness rotator cuff tears (RCTs) had significantly poorer outcomes and return-to-play rates after surgical repair.
The purpose of this study was to determine outcome scores and return to play of throwing athletes treated with arthroscopic capsulolabral repair for posterior shoulder instability with coexistent RCTs and to compare them with outcome scores as well as return to play of throwing athletes with isolated posterior shoulder instability. It was hypothesized that throwing athletes with a combination of posterior shoulder instability and RCT would have poorer outcomes and poorer return to play after surgery.5
METHODS
PATIENT SELECTION
After Institutional Review Board approval, informed consent was obtained, and consecutive throwing athletes who underwent arthroscopic posterior capsulolabral reconstruction for posterior shoulder instability were followed in the perioperative period. Inclusion criteria were throwing athletes participating in competitive sports at the high school, collegiate, or professional level, minimum 1-year follow-up, presence of unidirectional posterior instability, and absence of symptoms of instability in any direction other than posterior. Patients with inferior instability, SLAP pathology on examination and on magnetic resonance imaging, multidirectional instability, or habitual or psychogenic voluntary shoulder subluxations were excluded. Patients with diagnoses of both posterior shoulder instability and impingement treated with subacromial decompression and distal clavicle resection were also excluded.
After this cohort was identified, patient records were reviewed for pertinent operative data, such as procedure, complications, and evidence of RCT by operative report and arthroscopic photographs. A partial RCT was defined as a tear of 10% to 50%; those with rotator cuff fraying were determined not to be significant.
PATIENT EVALUATION
Surgeries were performed between January 1998 and December 2009 by the senior author (JPB). All patients were followed with clinical examinations, radiographs, and subjective grading scales. Recorded patient demographic data included age, sex, sport, position, competition level, and follow-up duration.
Continue to: All patients had...
All patients had symptomatic posterior shoulder instability, including posterior shoulder pain, clicking, a sensation of subluxation, or instability/apprehension with motion. Each athlete’s shoulder was palpated for tenderness and tested for impingement. Specific posterior glenohumeral instability tests, including the Kim test,6 the circumduction test, the jerk test,7 the posterior load-and-shift test,8 and the posterior stress test,9 were performed on all patients. Patients with multidirectional instability on the sulcus test, as well as provocative tests indicating SLAP pathology, such as the Crank test and the active compression test, were not included. Standard radiography and magnetic resonance arthrography (MRA) were performed to further narrow inclusion and exclusion criteria.
Both before surgery and at latest follow-up, patient outcomes were evaluated using the American Shoulder and Elbow Surgeons (ASES) score (range, 0-100) which combines a subjective functional scale measuring activities of daily living (0-3 for each of 10 tasks, with a total of 0-30) and a subjective pain scale (0-10, with 10 being worst pain). Values >80 were described as excellent, and failures were defined as scores <60 after surgery.10 A subjective stability scale (0-10, with 0 indicating completely stable and 10 completely unstable), strength scale (0-3, with 0 indicating none, 1 markedly decreased, 2 slightly decreased, and 3 normal), and ROM scale (0-3, with 0 indicating poor, 1 limited, 2 satisfactory, and 3 full) were evaluated both before surgery and at the latest follow-up. A stability score >5 after surgery was defined as a failure.1,2,11 Patients were also asked if, based on their current state, they would undergo surgery again. Intraoperative findings and specific surgical procedures performed were correlated with the aforementioned subjective and objective outcome scores.
OPERATIVE TREATMENT
Throwing athletes who met inclusion criteria and failed nonoperative management underwent surgery by the senior author (JPB). Each patient was examined under anesthesia and, with the patient in the lateral decubitus position, a diagnostic arthroscopy was performed to identify posterior capsulolabral complex pathology, including a patulous capsule, capsular tears, labral fraying, and labral tears. A careful examination for rotator cuff pathology was also performed. Based on preoperative clinical examination, MRA, examination under anesthesia, pathologic findings at diagnostic arthroscopic surgery, and surgeon experience, capsulolabral plication was performed with or without suture anchors.2,5 After capsulolabral repair, the capsule was evaluated for residual laxity, and additional plication sutures were placed, as indicated, with care to avoid overconstraint in these throwing athletes.1 Posterior glenohumeral stability restoration was judged by removing traction and performing posterior load-and-shift and posterior stress tests. Any RCT with <50% thickness was débrided. Postoperative care and rehabilitation were carried out as previously described and were not altered by the presence or absence of a RCT.3
STATISTICAL ANALYSIS
Preoperative and latest follow-up ASES scores, stability scores, functional scores, and pain-level findings were compared using paired-samples Comparisons between groups, including throwing athletes with and without rotator cuff pathology, were done using the Student t test. Outcome comparisons between multiple groups, which included intraoperative findings and surgical fixation methods, were analyzed with c2 modeling for nonparametric data. Statistical significance was set at P < .05. A power analysis found that this study was able to detect a meaningful difference of 10 ASES points.
RESULTS
PATIENT DEMOGRAPHIC CHARACTERISTICS
Of the 56 throwing athletes who met the inclusion criteria, 24 were found to have rotator cuff pathology in addition to posterior capsulolabral pathology, while 32 were found to have capsulolabral pathology alone. Demographic data are listed in Table 1. Mean age was 20.1 years for patients with rotator cuff pathology and 17.8 years for patients without RCTs. All 24 athletes with rotator cuff pathology were treated with arthroscopic débridement. Mean follow-up was 38.6 months (range, 16.5-63.6 months) for patients with RCTs and 39.1 months (range, 12-98.8 months) for patients without RCTs. No significant difference was found in age, sports level, or follow-up between groups.
Table 1. Demographic Data for Athletes With Posterior Instability With and Without Rotator Cuff Tears (N = 56 Shoulders)a
Characteristic | Rotator Cuff Tears | |
Yes | No | |
| Total | 24 | 32 |
| Sex | ||
| Male | 16 | 27 |
| Female | 8 | 5 |
| Mean age, y | 20.1 | 17.8 |
| Mean follow up, mo | 38.6 | 39.1 |
| Participation level | ||
| Professional | 1 | 0 |
| College | 4 | 4 |
| High school | 17 | 26 |
| Recreational | 2 | 2 |
aThe majority of athletes were males in high school and their mean follow-up was 3 years.
Continue to: Outcomes
OUTCOMES
Table 2 lists the preoperative and postoperative scores for shoulder performance in throwing athletes with posterior shoulder instability, with and without RCTs.
Table 2. Preoperative and Postoperative Scores for Shoulder Performance in Throwing Athletes With Posterior Shoulder Instability With and Without Rotator Cuff Tearsa
| With Rotator Cuff Tears (n=24 shoulders) | Without Rotator Cuff Tears (n=32 shoulders) | |||||||||
| Preoperative | Latest Follow-Up | Preoperative | Latest Follow-Up | |||||||
| Outcome Measure | Mean Score | Range | Mean Score | Range | P | Mean Score | Range | Mean Score | Range | P |
ASES 0-100 0 = worst | 41.8 | 20-70 | 85.4 | 67-100 | <.05 | 49.7 | 20-85 | 83.1 | 25-100 | <.05 |
Stability 0-10 0 = most stable | 6.7 | 2-10 | 2.4 | 0-6 | <.05 | 7.8 | 0-10 | 2.4 | 0-8 | <.05 |
Pain 0-10 10 = worst | 7.6 | 5-10 | 1.9 | 0-5 | <.05 | 6.3 | 0-10 | 2.2 | 0-7 | <.05 |
Function 0-30 0 = worst | 18.5 | 6-27 | 27 | 16-30 | <.05 | 19.0 | 8-26 | 26.4 | 6-30 | <.05 |
aThere was no difference in ASES, stability, pain, or functional scores between athletes with posterior instability alone compared with patients with concomitant rotator cuff tears.
Abbreviation: ASES, American Shoulder and Elbow Surgeons.
ASES Scores. Mean preoperative ASES scores for patients with RCTs improved significantly (t = –13.8, P < .001), as did those for patients without rotator cuff pathology (t = –8.9, P < .001). No significant differences in ASES score were found between patients with and without rotator cuff pathology before or after surgery (t = 1.9, P = .07; t = .58, P = .06). In addition, 70.8% (17/24) of throwing athletes with rotator cuff pathology had an excellent postoperative outcome (ASES score >80), and 29.2% (7/24) had a satisfactory outcome (ASES score, 60-80). Thus, 100% of those with concomitant posterior shoulder instability and RCTs had a good or excellent outcome after surgical intervention. In those without rotator cuff pathology, 78.1% (25/32) had an excellent outcome, 12.5% (4/32) had a satisfactory outcome, and 9.4% (3/32) had a poor outcome. Thus, 91% of those without rotator cuff pathology had a good or excellent outcome after surgery.
Stability. Preoperative stability scores improved significantly after surgery in both groups (t = 7.2, P < .001; t = 10.5, P < .001). There were no statistical differences between preoperative or postoperative stability scores in those with or without rotator cuff pathology (t = 1.7, P = .095; t = .03, P = .975). Of throwing athletes with RCTs, 54.2% (13/24) had an excellent outcome, 33.3% (8/24) a good outcome, and 12.5% (3/24) a satisfactory outcome. Thus, 87.5% (21/24) of those with RCTs had a good or excellent outcome in terms of stability. In those without rotator cuff pathology, 46.9% (15/32) had excellent stability, 46.9% (15/32) had good stability, and 3.1% (1/32) had satisfactory stability after surgery. Thus, 93.8% (30/32) of throwing athletes without rotator cuff pathology had good or excellent stability after surgery.
Pain. Mean preoperative pain scores for those with and without rotator cuff pathology improved significantly (t = 13.4, P < .001; t = 7.1, P < .001). There was no statistical difference in preoperative or postoperative pain scores between those with and without rotator cuff pathology (t = 1.99, P = .051; t = .49, P = .627).
Function. Mean preoperative function scores for both groups improved significantly (t = 7.7, P < .001; t = 8.0, P < .001). There was no difference in improvement in functional scores between the two groups before or after surgery (t = .36, P = .721; t = .5, P = .622).
Continue to: ROM
ROM. Of those with rotator cuff pathology, 54% (13/24) had normal ROM, 42% (10/24) had satisfactory ROM, and 4% (1/24) had limited ROM. In throwing athletes without rotator cuff pathology, 34% (11/32) had normal ROM, 53.1% (17/32) had satisfactory ROM, and 9% (3/32) had limited ROM after surgery. There was no significant difference in ROM between the groups (c2 = 2.7, P = .260).
Strength. Of those with RCTs, 67% (16/24) reported normal strength, 29% (7/24) slightly decreased strength, and 4% (1/24) markedly decreased strength. Of those throwing athletes without rotator cuff pathology, 50% (16/32) had normal strength, 41% (13/32) had slightly decreased strength, and 9% (3/32) had markedly decreased strength. No statistical difference was noted between the two groups (c2 = 1.7, P = .429).
Return to Sport. Of those with RCTs, 92% (22/24) returned to sport while 84% (27/32) of throwing athletes without RCTs returned to sport. There was no difference between the two groups (c2 = .667, P = .414). Sixty-seven percent (16/24) of those with RCTs and 56% (18/32) of those without RCTs returned to the same level of sport. No statistical difference was found in return to play between throwing athletes with and without rotator cuff pathology (c2 = .624, P = .430).
Failures. According to ASES scores, no throwers with RCTs failed, while 9.4% (3/32) with posterior instability alone failed. Regarding stability, 8.3% (2/24) of athletes with RCTs failed, while 6.3% (2/32) with posterior instability alone failed.
SURGICAL FINDINGS AND PROCEDURES
Of the 24 throwing athletes with rotator cuff pathology, 92% (22/24) had labral tears, while 78% (25/32) of those without RCTs had labral tears. The majority of RCTs were in the posterior supraspinatus and anterior infraspinatus regions. This was not significantly different between groups (c2 = 1.86, P = .172). All labral pathology was posterior-inferior, and all RCTs were <50% thickness, and therefore were débrided. Fifty-four percent (13/24) of those with RCTs had a patulous capsule and 63% (20/32) of throwing athletes without rotator cuff pathology had a patulous capsule. There was no significant difference between groups (c2 = .393, P = .530). Of those with RCTs, 92% (22/24) had surgical fixation with anchors, while 78% (25/32) of those without rotator cuff pathology underwent repair with anchor fixation. There was no statistically significant difference in anchor use between groups (c2 = 1.86, P = .172).
Continue to: Discussion
DISCUSSION
Throwing athletes with and without RCTs had similar rates of recovery and return to play after arthroscopic capsular labral repair, with rotator cuff débridement if a tear was present. The mean follow-up was 3.2 years. Further, there was no difference in return to play (92% vs 84%), ASES score, stability, pain, function, ROM, or strength between the 2 groups before or after surgery. In this cohort of 56 patients, 24 throwing athletes (43%) were found to have RCTs.
Return-to-play rates showed no between-group differences; 92% (22/24) of athletes with concomitant RCTs returned to sport, and 67% (16/24) returned to the same level. Eight percent of throwing athletes with RCTs were unable to return to sport after surgery. These return-to-play rates are an improvement over most previously reported rates in throwing athletes and in posterior shoulder instability in general.1-4,11 When these athletes are compared with their counterparts with combined SLAP tears and RCTs, return-to-play rates are notably higher. There may be discrepancies in interpreting return-to-play between the two studies, but in the current study, 67% of those with concomitant RCTs achieved return to preinjury level of play. This is 10% higher than the rate reported in athletes with SLAP tears alone (57%) and even higher than in those with concomitant SLAP and RCTs. It is also essential to note that a number of this cohort’s athletes who did not return to play did so for factors (eg, graduation) unrelated to the shoulder. However, the study by Neri and colleagues5 included professional athletes who likely all attempted to return to play and, if unable to perform at the same level, likely were unable to continue their professional career.5
All patients with RCTs had a good or excellent outcome (ASES score), and 70.8% had an excellent outcome. Similarly, 97% of those without rotator cuff pathology had a good or excellent outcome, and 81.3% had an excellent outcome. There was no significant difference between the two groups. These results parallel those of Neri and colleagues’5 study of SLAP tears with RCTs, where 96% (22/23) of throwing athletes had a good or excellent outcome. Despite these high outcome scores in patients with SLAP tears, only 57% were able to return to elite pitching.5 In the current study, pain was slightly higher for those with rotator cuff pathology before surgery—a finding consistent with pain frequently being found in patients with isolated partial-thickness RCTs. Their postoperative pain scores were actually lower on average than those of patients without RCTs, which suggests simple débridement of undersurface tears adequately addressed the pathology. The authors theorize that the main pain generator in this population may be posterior instability, and that the rotator cuff has less of an influence. In the SLAP population, the main pain generator likely is the RCT.
Failures by ASES score or strength were fairly rare in this cohort. Many patients opted to have revision surgery because of continued instability, pain, decreased function, or reinjury. One potential cause of failure in this cohort is inadequate capsular shift. However, capsular plication in throwing athletes is difficult to address, as overtensioning the repair can lead to the inability to adequately perform overhead activites.3,4 This cannot be overemphasized, particularly with pitchers.
Partial-thickness RCTs, particularly those on the articular side, are common in throwing athletes because of high tensile and compressive loads.12 Despite the known risk of RCTs with posterior shoulder instability in throwing athletes, the authors are unaware of reports of the incidence or treatment of this pathology. RCTs in this posterior instability group likely represent a pathology other than internal impingement. The high proportion of throwing athletes with RCTs in this study (43%) indicates a need for close evaluation of rotator cuff pathology in young throwing athletes. Ide et al found that 75% of patients with SLAP tears had partial articular-sided RCTs.13 In the current study, all RCTs were small partial tears, and arthroscopic débridement was performed. It is unknown whether repair of these RCTs would impact return to play. However, rotator cuff repair in this population has been shown to have poor outcomes. Tear thickness typically is used to determine treatment, with débridement performed if <50% tendon thickness is affected. More recently, many have advocated having greater tendon involvement in throwers before repair, because of poor outcomes. Although studies are limited, tear size does seem to correlate with outcomes.14
Continue to: Study Limitations
STUDY LIMITATIONS
Limitations of this study include its small number of professional throwing athletes, with the majority being high school athletes. Further, although ASES scores are consistently used in posterior shoulder instability studies, these scores are influenced highly by pain scores, and some argue that other scoring systems may provide more useful information. However, none of the more modern scoring systems have been studied extensively in posterior glenohumeral instability. Further, because the authors used the present scoring systems previously,1-4 they were continued to be used for comparison and consistency. Outcomes such as ROM and strength may carry more weight if measured and documented by clinical examination. Further testing, such as clinical evaluation of the jerk test or the posterior load-and-shift test, and their comparison before and after surgery may provide more objective data.
CONCLUSION
Arthroscopic capsulolabral reconstruction is successful in throwing athletes with RCTs treated with arthroscopic débridement. Unlike a previous study of throwing athletes’ outcomes after surgery for concomitant SLAP tears and RCTs,5 this study of throwing athletes with concomitant posterior shoulder instability and RCTs found no difference in patient-reported outcome measures or return to play. In throwing athletes with posterior instability and RCTs, arthroscopic posterior capsulolabral repair with rotator cuff débridement is successful.
ABSTRACT
In a previous study, compared with throwing athletes with superior labral anterior posterior (SLAP) tears, those with concomitant SLAP tears and rotator cuff tears (RCTs) had significantly poorer outcome scores and return to play. Posterior shoulder instability also occurs in throwing athletes, but no studies currently exist regarding outcomes of these patients with concomitant RCTs.
The authors hypothesized that throwing athletes treated with arthroscopic capsulolabral repair for posterior shoulder instability with coexistent rotator cuff pathology would have poorer outcome scores and return to play.
Fifty-six consecutive throwing athletes with unidirectional posterior shoulder instability underwent arthroscopic capsulolabral repair. Preoperative and postoperative patient-centered outcomes of pain, stability, function, range of motion, strength, and American Shoulder and Elbow Surgeons Shoulder (ASES) scores, as well as return to play, were evaluated. Patients with and without rotator cuff pathology were compared.
Forty-three percent (24/56) of throwing athletes had rotator cuff pathology in addition to posterior capsulolabral pathology. All RCTs were débrided. At a mean of 3 years, there were no differences in preoperative and postoperative patient-centered outcomes between those with and without RCTs. Return-to-play rates showed no between-group differences; 92% (22/24) of athletes with concomitant RCTs returned to sport (P = .414) and 67% (16/24) returned to the same level (P = .430).
Arthroscopic capsulolabral reconstruction is successful in throwing athletes with RCTs treated with arthroscopic débridement. Unlike the previous study evaluating throwers outcomes after surgical treatment for concomitant SLAP tears and RCTs, the authors found no difference in patient-reported outcome measures or return to play for throwing athletes with concomitant posterior shoulder instability and RCTs. In throwing athletes with concomitant posterior instability and RCTs, arthroscopic posterior capsulolabral repair with rotator cuff débridement is successful.
Continue to: Posterior shoulder instability...
Posterior shoulder instability is an important and increasingly recognized pathology among throwers. Like the superior labrum, the posterior capsulolabral complex is also susceptible to injury during the throwing motion; the posterior labrum being most at risk during the late cocking and follow-through phases. Recent studies have found that arthroscopic capsulolabral reconstruction in posterior shoulder instability is successful in allowing athletes to return to their preinjury sports activities, with 2 studies detailing outcomes in throwing athletes.1-4 However, superior labral anterior posterior (SLAP) tears are common in throwing athletes and have been treated with varying and limited success. Further, in a study of outcomes of arthroscopic repair of SLAP lesions, Neri and colleagues5 found that, compared with throwing athletes with SLAP tears, throwing athletes with concomitant SLAP tears and partial-thickness rotator cuff tears (RCTs) had significantly poorer outcomes and return-to-play rates after surgical repair.
The purpose of this study was to determine outcome scores and return to play of throwing athletes treated with arthroscopic capsulolabral repair for posterior shoulder instability with coexistent RCTs and to compare them with outcome scores as well as return to play of throwing athletes with isolated posterior shoulder instability. It was hypothesized that throwing athletes with a combination of posterior shoulder instability and RCT would have poorer outcomes and poorer return to play after surgery.5
METHODS
PATIENT SELECTION
After Institutional Review Board approval, informed consent was obtained, and consecutive throwing athletes who underwent arthroscopic posterior capsulolabral reconstruction for posterior shoulder instability were followed in the perioperative period. Inclusion criteria were throwing athletes participating in competitive sports at the high school, collegiate, or professional level, minimum 1-year follow-up, presence of unidirectional posterior instability, and absence of symptoms of instability in any direction other than posterior. Patients with inferior instability, SLAP pathology on examination and on magnetic resonance imaging, multidirectional instability, or habitual or psychogenic voluntary shoulder subluxations were excluded. Patients with diagnoses of both posterior shoulder instability and impingement treated with subacromial decompression and distal clavicle resection were also excluded.
After this cohort was identified, patient records were reviewed for pertinent operative data, such as procedure, complications, and evidence of RCT by operative report and arthroscopic photographs. A partial RCT was defined as a tear of 10% to 50%; those with rotator cuff fraying were determined not to be significant.
PATIENT EVALUATION
Surgeries were performed between January 1998 and December 2009 by the senior author (JPB). All patients were followed with clinical examinations, radiographs, and subjective grading scales. Recorded patient demographic data included age, sex, sport, position, competition level, and follow-up duration.
Continue to: All patients had...
All patients had symptomatic posterior shoulder instability, including posterior shoulder pain, clicking, a sensation of subluxation, or instability/apprehension with motion. Each athlete’s shoulder was palpated for tenderness and tested for impingement. Specific posterior glenohumeral instability tests, including the Kim test,6 the circumduction test, the jerk test,7 the posterior load-and-shift test,8 and the posterior stress test,9 were performed on all patients. Patients with multidirectional instability on the sulcus test, as well as provocative tests indicating SLAP pathology, such as the Crank test and the active compression test, were not included. Standard radiography and magnetic resonance arthrography (MRA) were performed to further narrow inclusion and exclusion criteria.
Both before surgery and at latest follow-up, patient outcomes were evaluated using the American Shoulder and Elbow Surgeons (ASES) score (range, 0-100) which combines a subjective functional scale measuring activities of daily living (0-3 for each of 10 tasks, with a total of 0-30) and a subjective pain scale (0-10, with 10 being worst pain). Values >80 were described as excellent, and failures were defined as scores <60 after surgery.10 A subjective stability scale (0-10, with 0 indicating completely stable and 10 completely unstable), strength scale (0-3, with 0 indicating none, 1 markedly decreased, 2 slightly decreased, and 3 normal), and ROM scale (0-3, with 0 indicating poor, 1 limited, 2 satisfactory, and 3 full) were evaluated both before surgery and at the latest follow-up. A stability score >5 after surgery was defined as a failure.1,2,11 Patients were also asked if, based on their current state, they would undergo surgery again. Intraoperative findings and specific surgical procedures performed were correlated with the aforementioned subjective and objective outcome scores.
OPERATIVE TREATMENT
Throwing athletes who met inclusion criteria and failed nonoperative management underwent surgery by the senior author (JPB). Each patient was examined under anesthesia and, with the patient in the lateral decubitus position, a diagnostic arthroscopy was performed to identify posterior capsulolabral complex pathology, including a patulous capsule, capsular tears, labral fraying, and labral tears. A careful examination for rotator cuff pathology was also performed. Based on preoperative clinical examination, MRA, examination under anesthesia, pathologic findings at diagnostic arthroscopic surgery, and surgeon experience, capsulolabral plication was performed with or without suture anchors.2,5 After capsulolabral repair, the capsule was evaluated for residual laxity, and additional plication sutures were placed, as indicated, with care to avoid overconstraint in these throwing athletes.1 Posterior glenohumeral stability restoration was judged by removing traction and performing posterior load-and-shift and posterior stress tests. Any RCT with <50% thickness was débrided. Postoperative care and rehabilitation were carried out as previously described and were not altered by the presence or absence of a RCT.3
STATISTICAL ANALYSIS
Preoperative and latest follow-up ASES scores, stability scores, functional scores, and pain-level findings were compared using paired-samples Comparisons between groups, including throwing athletes with and without rotator cuff pathology, were done using the Student t test. Outcome comparisons between multiple groups, which included intraoperative findings and surgical fixation methods, were analyzed with c2 modeling for nonparametric data. Statistical significance was set at P < .05. A power analysis found that this study was able to detect a meaningful difference of 10 ASES points.
RESULTS
PATIENT DEMOGRAPHIC CHARACTERISTICS
Of the 56 throwing athletes who met the inclusion criteria, 24 were found to have rotator cuff pathology in addition to posterior capsulolabral pathology, while 32 were found to have capsulolabral pathology alone. Demographic data are listed in Table 1. Mean age was 20.1 years for patients with rotator cuff pathology and 17.8 years for patients without RCTs. All 24 athletes with rotator cuff pathology were treated with arthroscopic débridement. Mean follow-up was 38.6 months (range, 16.5-63.6 months) for patients with RCTs and 39.1 months (range, 12-98.8 months) for patients without RCTs. No significant difference was found in age, sports level, or follow-up between groups.
Table 1. Demographic Data for Athletes With Posterior Instability With and Without Rotator Cuff Tears (N = 56 Shoulders)a
Characteristic | Rotator Cuff Tears | |
Yes | No | |
| Total | 24 | 32 |
| Sex | ||
| Male | 16 | 27 |
| Female | 8 | 5 |
| Mean age, y | 20.1 | 17.8 |
| Mean follow up, mo | 38.6 | 39.1 |
| Participation level | ||
| Professional | 1 | 0 |
| College | 4 | 4 |
| High school | 17 | 26 |
| Recreational | 2 | 2 |
aThe majority of athletes were males in high school and their mean follow-up was 3 years.
Continue to: Outcomes
OUTCOMES
Table 2 lists the preoperative and postoperative scores for shoulder performance in throwing athletes with posterior shoulder instability, with and without RCTs.
Table 2. Preoperative and Postoperative Scores for Shoulder Performance in Throwing Athletes With Posterior Shoulder Instability With and Without Rotator Cuff Tearsa
| With Rotator Cuff Tears (n=24 shoulders) | Without Rotator Cuff Tears (n=32 shoulders) | |||||||||
| Preoperative | Latest Follow-Up | Preoperative | Latest Follow-Up | |||||||
| Outcome Measure | Mean Score | Range | Mean Score | Range | P | Mean Score | Range | Mean Score | Range | P |
ASES 0-100 0 = worst | 41.8 | 20-70 | 85.4 | 67-100 | <.05 | 49.7 | 20-85 | 83.1 | 25-100 | <.05 |
Stability 0-10 0 = most stable | 6.7 | 2-10 | 2.4 | 0-6 | <.05 | 7.8 | 0-10 | 2.4 | 0-8 | <.05 |
Pain 0-10 10 = worst | 7.6 | 5-10 | 1.9 | 0-5 | <.05 | 6.3 | 0-10 | 2.2 | 0-7 | <.05 |
Function 0-30 0 = worst | 18.5 | 6-27 | 27 | 16-30 | <.05 | 19.0 | 8-26 | 26.4 | 6-30 | <.05 |
aThere was no difference in ASES, stability, pain, or functional scores between athletes with posterior instability alone compared with patients with concomitant rotator cuff tears.
Abbreviation: ASES, American Shoulder and Elbow Surgeons.
ASES Scores. Mean preoperative ASES scores for patients with RCTs improved significantly (t = –13.8, P < .001), as did those for patients without rotator cuff pathology (t = –8.9, P < .001). No significant differences in ASES score were found between patients with and without rotator cuff pathology before or after surgery (t = 1.9, P = .07; t = .58, P = .06). In addition, 70.8% (17/24) of throwing athletes with rotator cuff pathology had an excellent postoperative outcome (ASES score >80), and 29.2% (7/24) had a satisfactory outcome (ASES score, 60-80). Thus, 100% of those with concomitant posterior shoulder instability and RCTs had a good or excellent outcome after surgical intervention. In those without rotator cuff pathology, 78.1% (25/32) had an excellent outcome, 12.5% (4/32) had a satisfactory outcome, and 9.4% (3/32) had a poor outcome. Thus, 91% of those without rotator cuff pathology had a good or excellent outcome after surgery.
Stability. Preoperative stability scores improved significantly after surgery in both groups (t = 7.2, P < .001; t = 10.5, P < .001). There were no statistical differences between preoperative or postoperative stability scores in those with or without rotator cuff pathology (t = 1.7, P = .095; t = .03, P = .975). Of throwing athletes with RCTs, 54.2% (13/24) had an excellent outcome, 33.3% (8/24) a good outcome, and 12.5% (3/24) a satisfactory outcome. Thus, 87.5% (21/24) of those with RCTs had a good or excellent outcome in terms of stability. In those without rotator cuff pathology, 46.9% (15/32) had excellent stability, 46.9% (15/32) had good stability, and 3.1% (1/32) had satisfactory stability after surgery. Thus, 93.8% (30/32) of throwing athletes without rotator cuff pathology had good or excellent stability after surgery.
Pain. Mean preoperative pain scores for those with and without rotator cuff pathology improved significantly (t = 13.4, P < .001; t = 7.1, P < .001). There was no statistical difference in preoperative or postoperative pain scores between those with and without rotator cuff pathology (t = 1.99, P = .051; t = .49, P = .627).
Function. Mean preoperative function scores for both groups improved significantly (t = 7.7, P < .001; t = 8.0, P < .001). There was no difference in improvement in functional scores between the two groups before or after surgery (t = .36, P = .721; t = .5, P = .622).
Continue to: ROM
ROM. Of those with rotator cuff pathology, 54% (13/24) had normal ROM, 42% (10/24) had satisfactory ROM, and 4% (1/24) had limited ROM. In throwing athletes without rotator cuff pathology, 34% (11/32) had normal ROM, 53.1% (17/32) had satisfactory ROM, and 9% (3/32) had limited ROM after surgery. There was no significant difference in ROM between the groups (c2 = 2.7, P = .260).
Strength. Of those with RCTs, 67% (16/24) reported normal strength, 29% (7/24) slightly decreased strength, and 4% (1/24) markedly decreased strength. Of those throwing athletes without rotator cuff pathology, 50% (16/32) had normal strength, 41% (13/32) had slightly decreased strength, and 9% (3/32) had markedly decreased strength. No statistical difference was noted between the two groups (c2 = 1.7, P = .429).
Return to Sport. Of those with RCTs, 92% (22/24) returned to sport while 84% (27/32) of throwing athletes without RCTs returned to sport. There was no difference between the two groups (c2 = .667, P = .414). Sixty-seven percent (16/24) of those with RCTs and 56% (18/32) of those without RCTs returned to the same level of sport. No statistical difference was found in return to play between throwing athletes with and without rotator cuff pathology (c2 = .624, P = .430).
Failures. According to ASES scores, no throwers with RCTs failed, while 9.4% (3/32) with posterior instability alone failed. Regarding stability, 8.3% (2/24) of athletes with RCTs failed, while 6.3% (2/32) with posterior instability alone failed.
SURGICAL FINDINGS AND PROCEDURES
Of the 24 throwing athletes with rotator cuff pathology, 92% (22/24) had labral tears, while 78% (25/32) of those without RCTs had labral tears. The majority of RCTs were in the posterior supraspinatus and anterior infraspinatus regions. This was not significantly different between groups (c2 = 1.86, P = .172). All labral pathology was posterior-inferior, and all RCTs were <50% thickness, and therefore were débrided. Fifty-four percent (13/24) of those with RCTs had a patulous capsule and 63% (20/32) of throwing athletes without rotator cuff pathology had a patulous capsule. There was no significant difference between groups (c2 = .393, P = .530). Of those with RCTs, 92% (22/24) had surgical fixation with anchors, while 78% (25/32) of those without rotator cuff pathology underwent repair with anchor fixation. There was no statistically significant difference in anchor use between groups (c2 = 1.86, P = .172).
Continue to: Discussion
DISCUSSION
Throwing athletes with and without RCTs had similar rates of recovery and return to play after arthroscopic capsular labral repair, with rotator cuff débridement if a tear was present. The mean follow-up was 3.2 years. Further, there was no difference in return to play (92% vs 84%), ASES score, stability, pain, function, ROM, or strength between the 2 groups before or after surgery. In this cohort of 56 patients, 24 throwing athletes (43%) were found to have RCTs.
Return-to-play rates showed no between-group differences; 92% (22/24) of athletes with concomitant RCTs returned to sport, and 67% (16/24) returned to the same level. Eight percent of throwing athletes with RCTs were unable to return to sport after surgery. These return-to-play rates are an improvement over most previously reported rates in throwing athletes and in posterior shoulder instability in general.1-4,11 When these athletes are compared with their counterparts with combined SLAP tears and RCTs, return-to-play rates are notably higher. There may be discrepancies in interpreting return-to-play between the two studies, but in the current study, 67% of those with concomitant RCTs achieved return to preinjury level of play. This is 10% higher than the rate reported in athletes with SLAP tears alone (57%) and even higher than in those with concomitant SLAP and RCTs. It is also essential to note that a number of this cohort’s athletes who did not return to play did so for factors (eg, graduation) unrelated to the shoulder. However, the study by Neri and colleagues5 included professional athletes who likely all attempted to return to play and, if unable to perform at the same level, likely were unable to continue their professional career.5
All patients with RCTs had a good or excellent outcome (ASES score), and 70.8% had an excellent outcome. Similarly, 97% of those without rotator cuff pathology had a good or excellent outcome, and 81.3% had an excellent outcome. There was no significant difference between the two groups. These results parallel those of Neri and colleagues’5 study of SLAP tears with RCTs, where 96% (22/23) of throwing athletes had a good or excellent outcome. Despite these high outcome scores in patients with SLAP tears, only 57% were able to return to elite pitching.5 In the current study, pain was slightly higher for those with rotator cuff pathology before surgery—a finding consistent with pain frequently being found in patients with isolated partial-thickness RCTs. Their postoperative pain scores were actually lower on average than those of patients without RCTs, which suggests simple débridement of undersurface tears adequately addressed the pathology. The authors theorize that the main pain generator in this population may be posterior instability, and that the rotator cuff has less of an influence. In the SLAP population, the main pain generator likely is the RCT.
Failures by ASES score or strength were fairly rare in this cohort. Many patients opted to have revision surgery because of continued instability, pain, decreased function, or reinjury. One potential cause of failure in this cohort is inadequate capsular shift. However, capsular plication in throwing athletes is difficult to address, as overtensioning the repair can lead to the inability to adequately perform overhead activites.3,4 This cannot be overemphasized, particularly with pitchers.
Partial-thickness RCTs, particularly those on the articular side, are common in throwing athletes because of high tensile and compressive loads.12 Despite the known risk of RCTs with posterior shoulder instability in throwing athletes, the authors are unaware of reports of the incidence or treatment of this pathology. RCTs in this posterior instability group likely represent a pathology other than internal impingement. The high proportion of throwing athletes with RCTs in this study (43%) indicates a need for close evaluation of rotator cuff pathology in young throwing athletes. Ide et al found that 75% of patients with SLAP tears had partial articular-sided RCTs.13 In the current study, all RCTs were small partial tears, and arthroscopic débridement was performed. It is unknown whether repair of these RCTs would impact return to play. However, rotator cuff repair in this population has been shown to have poor outcomes. Tear thickness typically is used to determine treatment, with débridement performed if <50% tendon thickness is affected. More recently, many have advocated having greater tendon involvement in throwers before repair, because of poor outcomes. Although studies are limited, tear size does seem to correlate with outcomes.14
Continue to: Study Limitations
STUDY LIMITATIONS
Limitations of this study include its small number of professional throwing athletes, with the majority being high school athletes. Further, although ASES scores are consistently used in posterior shoulder instability studies, these scores are influenced highly by pain scores, and some argue that other scoring systems may provide more useful information. However, none of the more modern scoring systems have been studied extensively in posterior glenohumeral instability. Further, because the authors used the present scoring systems previously,1-4 they were continued to be used for comparison and consistency. Outcomes such as ROM and strength may carry more weight if measured and documented by clinical examination. Further testing, such as clinical evaluation of the jerk test or the posterior load-and-shift test, and their comparison before and after surgery may provide more objective data.
CONCLUSION
Arthroscopic capsulolabral reconstruction is successful in throwing athletes with RCTs treated with arthroscopic débridement. Unlike a previous study of throwing athletes’ outcomes after surgery for concomitant SLAP tears and RCTs,5 this study of throwing athletes with concomitant posterior shoulder instability and RCTs found no difference in patient-reported outcome measures or return to play. In throwing athletes with posterior instability and RCTs, arthroscopic posterior capsulolabral repair with rotator cuff débridement is successful.
1. Bradley JP, Baker CL 3rd, Kline AJ, Armfield DR, Chhabra A. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 100 shoulders. Am J Sports Med. 2006;34(7):1061-1071.
2. Bradley JP, McClincy MP, Arner JW, Tejwani SG. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 200 shoulders. Am J Sports Med. 2013;41(9):2005-2014.
3. McClincy MP, Arner JW, Bradley JP. Posterior shoulder instability in throwing athletes: a case-matched comparison of throwers and non-throwers. Arthroscopy. 2015;31(6):1041-1051.
4. Radkowski CA, Chhabra A, Baker CL 3rd, Tejwani SG, Bradley JP. Arthroscopic capsulolabral repair for posterior shoulder instability in throwing athletes compared with nonthrowing athletes. Am J Sports Med. 2008;36(4):693-699.
5. Neri BR, ElAttrache NS, Owsley KC, Mohr K, Yocum LA. Outcome of type II superior labral anterior posterior repairs in elite overhead athletes: effect of concomitant partial-thickness rotator cuff tears. Am J Sports Med. 2011;39(1):114-120.
6. Kim SH, Park JS, Jeong WK, Shin SK. The Kim test: a novel test for posteroinferior labral lesion of the shoulder—a comparison to the jerk test. Am J Sports Med. 2005;33(8):1188-1192.
7. Antoniou J, Duckworth DT, Harryman DT 2nd. Capsulolabral augmentation for the management of posteroinferior instability of the shoulder. J Bone Joint Surg Am. 2000;82(9):1220-1230.
8. Altchek DW, Hobbs WR. Evaluation and management of shoulder instability in the elite overhead thrower. Orthop Clin North Am. 2001;32(3):423-430, viii.
9. Fuchs B, Jost B, Gerber C. Posterior-inferior capsular shift for the treatment of recurrent, voluntary posterior subluxation of the shoulder. J Bone Joint Surg Am. 2000;82(1):16-25.
10. Richards RR, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3(6):347-352.
11. Arner JW, McClincy MP, Bradley JP. Arthroscopic stabilization of posterior shoulder instability is successful in American football players. Arthroscopy. 2015;31(8):1466-1471.
12. Mazoue CG, Andrews JR. Repair of full-thickness rotator cuff tears in professional baseball players. Am J Sports Med. 2006;34(2):182-189.
13. Ide J, Maeda S, Takagi K. Sports activity after arthroscopic superior labral repair using suture anchors in overhead-throwing athletes. Am J Sports Med. 2005;33(4):507-514.
14. Economopoulos KJ, Brockmeier SF. Rotator cuff tears in overhead athletes. Clin Sports Med. 2012;31(4):675-692.
1. Bradley JP, Baker CL 3rd, Kline AJ, Armfield DR, Chhabra A. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 100 shoulders. Am J Sports Med. 2006;34(7):1061-1071.
2. Bradley JP, McClincy MP, Arner JW, Tejwani SG. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 200 shoulders. Am J Sports Med. 2013;41(9):2005-2014.
3. McClincy MP, Arner JW, Bradley JP. Posterior shoulder instability in throwing athletes: a case-matched comparison of throwers and non-throwers. Arthroscopy. 2015;31(6):1041-1051.
4. Radkowski CA, Chhabra A, Baker CL 3rd, Tejwani SG, Bradley JP. Arthroscopic capsulolabral repair for posterior shoulder instability in throwing athletes compared with nonthrowing athletes. Am J Sports Med. 2008;36(4):693-699.
5. Neri BR, ElAttrache NS, Owsley KC, Mohr K, Yocum LA. Outcome of type II superior labral anterior posterior repairs in elite overhead athletes: effect of concomitant partial-thickness rotator cuff tears. Am J Sports Med. 2011;39(1):114-120.
6. Kim SH, Park JS, Jeong WK, Shin SK. The Kim test: a novel test for posteroinferior labral lesion of the shoulder—a comparison to the jerk test. Am J Sports Med. 2005;33(8):1188-1192.
7. Antoniou J, Duckworth DT, Harryman DT 2nd. Capsulolabral augmentation for the management of posteroinferior instability of the shoulder. J Bone Joint Surg Am. 2000;82(9):1220-1230.
8. Altchek DW, Hobbs WR. Evaluation and management of shoulder instability in the elite overhead thrower. Orthop Clin North Am. 2001;32(3):423-430, viii.
9. Fuchs B, Jost B, Gerber C. Posterior-inferior capsular shift for the treatment of recurrent, voluntary posterior subluxation of the shoulder. J Bone Joint Surg Am. 2000;82(1):16-25.
10. Richards RR, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3(6):347-352.
11. Arner JW, McClincy MP, Bradley JP. Arthroscopic stabilization of posterior shoulder instability is successful in American football players. Arthroscopy. 2015;31(8):1466-1471.
12. Mazoue CG, Andrews JR. Repair of full-thickness rotator cuff tears in professional baseball players. Am J Sports Med. 2006;34(2):182-189.
13. Ide J, Maeda S, Takagi K. Sports activity after arthroscopic superior labral repair using suture anchors in overhead-throwing athletes. Am J Sports Med. 2005;33(4):507-514.
14. Economopoulos KJ, Brockmeier SF. Rotator cuff tears in overhead athletes. Clin Sports Med. 2012;31(4):675-692.
TAKE-HOME POINTS
- Arthroscopic capsulolabral reconstruction is successful in throwing athletes with concomitant RCTs treated with arthroscopic débridement.
- A previous study of throwing athletes found poor outcomes after surgery for concomitant SLAP tears and RCTs.
- Throwing athletes with concomitant posterior shoulder instability and RCTs were no different in patient-reported outcomes or return to play.
- The high proportion of throwing athletes with partial thickness RCTs in this study (43%) indicates a need for close evaluation of rotator cuff pathology in young throwing athletes.
- The authors theorize the main pain generator in this population may be posterior instability and that the rotator cuff has less of an influence.
Arthroscopic Anterior Ankle Decompression Is Successful in National Football League Players
ABSTRACT
Anterior ankle impingement is a frequent cause of pain and disability in athletes with impingement of soft-tissue or osseous structures along the anterior margin of the tibiotalar joint during dorsiflexion.
In this study, we hypothesized that arthroscopic decompression of anterior ankle impingement would result in significant, reliable, and durable improvement in pain and range of motion (ROM), and would allow National Football League (NFL) players to return to their preoperative level of play.
We reviewed 29 arthroscopic ankle débridements performed by a single surgeon. Each NFL player underwent arthroscopic débridement of pathologic soft tissue and of tibial and talar osteophytes in the anterior ankle. Preoperative and postoperative visual analog scale (VAS) pain scores, American Orthopaedic Foot and Ankle Society (AOFAS) hindfoot scores, and ankle ROM were compared; time to return to play (RTP), events missed secondary to surgery, and complications were recorded.
All athletes returned to the same level of NFL play at a mean (SD) of 8.4 (4.1) weeks after surgery and continued playing for a mean (SD) of 3.43 (2.57) years after surgery. Mean (SD) VAS pain scores decreased significantly (P < .001), to 0.38 (0.89) from 4.21 (1.52). Mean (SD) active ankle dorsiflexion increased significantly (P < .001), to 18.86° (2.62°) from 8.28° (4.14°). Mean (SD) AOFAS hindfoot scores increased significantly (P < .001), to 97.45 (4.72) from 70.62 (10.39). Degree of arthritis (r = 0.305) and age (r = 0.106) were poorly correlated to time to RTP.
In all cases, arthroscopic débridement of anterior ankle impingement resulted in RTP at the same level at a mean of 2 months after surgery. There were significant improvements in VAS pain scores, AOFAS hindfoot scores, and ROM.
Arthroscopic débridement of anterior ankle impingement relieves pain, restores ROM and function, and results in reliable RTP in professional football players.
Continue to: Anterior ankle impingement...
Anterior ankle impingement is a frequent cause of disability in athletes.1 This condition results from repetitive trauma over time, which leads to osseous and soft-tissue impingement, pain, and decreased ankle range of motion (ROM).
First termed footballer’s ankle, this condition is linked to repeated, forceful plantarflexion,2 though later studies attributed the phenomenon to repeated dorsiflexion resulting in periosteal hemorrhage.3 Both osseous and soft-tissue structures can cause impingement at the tibiotalar joint, often with osteophytes anteromedially at the tibial talar joint. Soft-tissue structures, including hypertrophic synovium, meniscoid lesions, and a thickened anterior talofibular ligament, more often cause anterolateral impingement.4-6 This process results in pain in extreme dorsiflexion, which comes into play in almost all football maneuvers, including sprinting, back-peddling, and offensive and defensive stances. Therefore, maintenance of pain-free dorsiflexion is required for high-level football. Decreased ROM can lead to decreased ability to perform these high-level athletic functions and can limit performance.
Arthroscopic débridement improves functional outcomes and functional motion in both athletes and nonathletes.7,8 In addition, findings of a recent systematic review provide support for arthroscopic treatment of ankle impingement.9 Although arthroscopic treatment is effective in nonathletes and recreational athletes,10 there is a paucity of data on the efficacy of this procedure and on time to return to play (RTP) in professional football players.
We conducted a study to evaluate the outcomes (pain, ROM, RTP) of arthroscopic débridement for anterior ankle impingement in National Football League (NFL) players. We hypothesized that arthroscopic decompression of anterior ankle impingement would result in significant, reliable, and durable improvement in pain and ROM, and would allow NFL players to return to their preoperative level of play.
METHODS
After this study was granted Institutional Review Board approval, we retrospectively reviewed a consecutive series of arthroscopically treated anterior ankle impingement athletes by a single surgeon (JPB). Indications for surgery were anterior ankle impingement resulting in ankle pain and decreased ROM that interfered with sport. Active NFL players who underwent ankle arthroscopy for symptomatic anterior ankle impingement were included. Excluded were players who underwent surgery after retirement or who retired before returning to play for reasons unrelated to the ankle. Medical records, operative reports, and rehabilitation reports were reviewed.
Continue to: Preoperative and postoperative...
Preoperative and postoperative visual analog scale (VAS) pain scores, American Orthopaedic Foot and Ankle Society (AOFAS) hindfoot scores, and ankle ROM were compared; time to RTP, events missed secondary to surgery, and complications were recorded. These preoperative and postoperative variables were compared with paired Student 2-way t tests for continuous variables. Pearson correlation coefficients were calculated.
PROCEDURE
Ankle arthroscopy was performed with the patient supine after spinal or general anesthesia was induced. Prophylactic antibiotics were given in each case. Arthroscopy was performed with standard anterolateral and anteromedial portals. First, an incision was made through skin only, followed by blunt subcutaneous dissection down to the ankle capsule. A capsulotomy was then made bluntly. Care was taken to avoid all neurovascular structures. Posterior portals were not used. A 2.7-mm arthroscope was inserted and alternated between the anteromedial and anterolateral portals to maximally visualize the ankle joint. Diagnostic arthroscopy was performed to document synovitis, chondral injury, osseous, and soft-tissue impingement and any other noted pathology (Figures 1A-1C).
A full radius resector was then used to perform a synovectomy and débridement of impinging soft tissue from the anterior talofibular ligament or anterior inferior talofibular ligament. All patients underwent arthroscopic débridement of pathologic soft tissue and of tibial and talar osteophytes in the anterior ankle. A small burr was used to débride and remove the osteophytes on the talus and/or tibia. Soft-tissue and osseous structures were resected until the contours of the talus and tibia were normal. Any unstable articular defects were débrided and loose bodies were removed. Ankle ROM was checked to confirm complete resolution of impingement (Figures 2A-2D). Patients were not immobilized and were allowed progressive weight-bearing as tolerated. Crutches were used for assisted ambulation the first 3 to 5 postoperative days.
Physical therapy progressed through 3 phases: (1) inflammation control and ROM restoration, (2) initiation of ankle strengthening, including eversion and inversion, and (3) agility, proprioception, and functional rehabilitation.
RESULTS
Twenty-five NFL players (29 surgeries) were included in the study. Two players were excluded because they had retired at the end of the season before the surgery for reasons unrelated to the operative ankle. Mean (SD) age was 28.1 (2.9) years. Six included players had a history of ankle sprains, 1 had a history of ipsilateral ankle fracture, and 1 had a history of ipsilateral ankle dislocation. Table 1 lists the positions of players who underwent ankle arthroscopic decompression.
Table 1. Positions of National Football League Players Who Underwent Ankle Arthroscopic Decompression for Anterior Ankle Impingement
Position | Surgeries, n |
| Offensive line | 8 |
| Defensive line | 8 |
| Wide receiver | 4 |
| Running back | 4 |
| Linebacker | 3 |
| Quarterback | 1 |
| Defensive back | 1 |
Continue to: During diagnostic arthroscopy...
During diagnostic arthroscopy, changes to the articular cartilage were noted: grade 0 in 38% of patients, grade 1 in 17%, grade 2 in 21%, grade 3 in 21%, and grade 4 in 3%. Four patients had an osteochondral lesion (<1 cm in each case), which was treated with chondroplasty without microfracture.
Each included patient returned to NFL play. Mean (SD) time to RTP without restrictions was 8.4 (4.1) weeks after surgery (range, 2-20 weeks). There was a poor correlation between degree of chondrosis and time to RTP (r = 0.305). In addition, there was a poor correlation between age and time to RTP (r = 0.106).
Dorsiflexion improved significantly (P < .001), patients had significantly less pain after surgery (P < .001), and AOFAS hindfoot scores improved significantly (P < .001) (Table 2).
Table 2. Preoperative and Postoperative Dorsiflexion, Pain, and AOFAS Score Before and After Arthroscopic Débridement of Anterior Ankle Impingementa
| Mean (SD) | ||
|---|---|---|
| Preoperative | Postoperative | |
| Dorsiflexion | 8.28º (4.14º) | 18.86° (2.62°) |
| VAS pain score | 4.21 (1.52) | 0.38 (0.89) |
| AOFAS score | 70.62 (10.39) | 97.45 (4.72) |
aAll values were significantly improved after surgery (P < .001).
Abbreviations: AOFAS, American Orthopaedic Foot and Ankle Society; VAS, visual analog scale.
The athletes played in the NFL for a mean (SD) of 3.43 (2.57) years after surgery (range, 1-10 seasons). These players included 6 who were still active at time of publication. No patient required revision surgery or additional surgery on the ipsilateral ankle. The one patient who was treated for superficial thrombophlebitis after surgery reported symptoms before surgery as well.
DISCUSSION
Arthroscopic decompression of anterior ankle impingement is safe and significantly improves pain and ROM in professional American football players. The procedure results in reliable RTP at an elite level, with durable results over the time remaining in their NFL careers.
Continue to: before the 1988 study by Hawkins...
Before the 1988 study by Hawkins,11 ankle spurs were removed with open procedures. Hawkins11 used arthroscopy for better and safer visualization of the ankle joint and used a burr for less painful removal of spurs from the tibia and the talus. In 2002, a series of 105 patients (median age, 35 years) had reduced pain and improved function a minimum of 2 years after arthroscopic débridement.12 These patients had a mix of pathology, including soft-tissue impingement, bony impingement, chondral lesions, loose bodies, and osteoarthritis.
For many elite athletes, anterior ankle impingement can cause significant limitation. Reduced ankle dorsiflexion can alter all limb mechanics and predispose athletes to injury.13 In addition, because NFL players’ ankle ROM often approaches or exceeds normal physiologic limits,14 an ankle ROM limitation will often hinder their performance.
Miyamoto and colleagues15 studied a series of 9 professional athletes (6 soccer players, 1 baseball pitcher, 1 mixed martial artist, 1 golfer) who underwent decompression of both anterior and posterior impingement. With regard to anterior impingement, they found anterior osteophytes in all the ankles, as was seen in the present study. Furthermore, they noted that mean dorsiflexion improved from 10° before surgery to 15° after surgery and that their athletes returned to play 12 to 15 weeks after surgery. Their results are similar to ours, though we noted more improvement in dorsiflexion, from 8.28° before surgery to 18.86° after surgery.
One of the most important metrics in evaluating treatment options for professional athletes is time from surgery to RTP without restrictions. Mean time to full RTP was shorter in our study (8.4 weeks) than in the study by Miyamoto and colleagues15 (up to 20 weeks). However, many of their procedures were performed during the off-season, when there was no need to expeditiously clear patients for full sports participation. In addition, the patients in their study had both anterior and posterior pathology.
Faster return to high-level athletics was supported in a study of 11 elite ballet dancers,16 whose pain and dance performance improved after arthroscopic débridement. Of the 11 patients, 9 returned to dance at a mean of 7 weeks after surgery; the other 2 required reoperation. Although the pathology differed in their study of elite professional soccer players, Calder and colleagues17 found that mean time to RTP after ankle arthroscopy for posterior impingement was 5 weeks.
Continue to: For the NFL players in our study...
For the NFL players in our study, RTP at their elite level was 100% after arthroscopic débridement of anterior ankle impingement. In the literature, time to RTP varies. Table 3 lists RTP rates for recreational athletes in published studies.18-27 In their recent systematic literature review, Zwiers and colleagues10 noted that 24% to 96.4% of recreational athletes returned to play after arthroscopic treatment for anterior ankle impingement. The percentage was significantly higher for the professional athletes in our study. Historical comparison supports an evolution in the indications and techniques for this procedure, with more recent literature suggesting a RTP rate much higher than earlier rates. In addition, compared with recreational athletes, professional athletes have strong financial incentives to return to their sports. Furthermore, our professional cohort was significantly younger than the recreational cohorts in those studies.
Table 3. Frequency of Recreational Athletes’ Return to Play After Arthroscopic Débridement of Anterior Ankle Impingement, as Reported in the Literature
| Study | Year | Journal | Return to Play | |
|---|---|---|---|---|
| n/N | % | |||
| Akseki et al18 | 1999 | Acta Orthop Scand | 10/11 | 91 |
| Baums et al19 | 2006 | Knee Surg Sports Traumatol Arthrosc | 25/26 | 96 |
| Branca et al20 | 1997 | Foot Ankle Int | 13/27 | 48 |
| Di Palma et al21 | 1999 | J Sports Traumatol Relat Res | 21/32 | 66 |
| Ferkel et al22 | 1991 | Am J Sports Med | 27/31 | 87.1 |
| Hassan23 | 2007 | Knee Surg Sports Traumatol Arthrosc | 9/11 | 82 |
| Jerosch et al24 | 1994 | Knee Surg Sports Traumatol Arthrosc | 9/38 | 24 |
| Murawski & Kennedy25 | 2010 | Am J Sports Med | 27/28 | 96.4 |
| Ogilvie-Harris et al26 | 1993 | J Bone Joint Surg Br | 21/28 | 75 |
| Rouvillain et al27 | 2014 | Eur J Orthop Surg Traumatol | 10/11 | 90 |
Total | 172/243 | 70 | ||
Current recommendations for recreational athletes include initial conservative treatment with rest, ankle bracing, and avoidance of jumping and other repetitive dorsiflexing activities. Physical therapy should include joint mobilization and work along the entire kinetic chain. Night splints or a removable walking boot can be used temporarily, as can a single intra-articular corticosteroid injection to reduce inflammation and evaluate improvement in more refractory cases.28 Commonly, conservative treatments fail if patients remain active, and soft tissue and/or osteophytes can be resected, though resection typically is reserved for recreational athletes for whom nonoperative treatments have been exhausted.29,30
This study had several limitations, including its retrospective nature and lack of control group. In addition, follow-up was relatively short, and we did not use more recently described outcome measures, such as the Sports subscale of the Foot and Ankle Ability Measure, which may be more sensitive in describing function in elite athletes. However, many of the cases in our study predated these measures, but the rate of RTP at the NFL level requires a very high degree of postoperative ankle function, making this outcome the most meaningful. In the context of professional athletes, specifically the length of their careers, our study results provide valuable information regarding expectations about RTP and the durability of arthroscopic débridement of anterior ankle impingement in a high-demand setting.
CONCLUSION
For all the NFL players in this study, arthroscopic débridement of anterior ankle impingement resulted in return to preoperative level of play at a mean of 2 months after surgery. There were significant improvements in VAS pain scores, AOFAS hindfoot scores, and ROM. Arthroscopic débridement of anterior ankle impingement relieves pain, restores ROM and function, and results in reliable RTP in professional football players.
1. Lubowitz JH. Editorial commentary: ankle anterior impingement is common in athletes and could be under-recognized. Arthroscopy. 2015;31(8):1597.
2. Mcdougall A. Footballer’s ankle. Lancet. 1955;269(6902):1219-1220.
3. Kleiger B. Anterior tibiotalar impingement syndromes in dancers. Foot Ankle. 1982;3(2):69-73.
4. Bassett FH 3rd, Gates HS 3rd, Billys JB, Morris HB, Nikolaou PK. Talar impingement by the anteroinferior tibiofibular ligament. A cause of chronic pain in the ankle after inversion sprain. J Bone Joint Surg Am. 1990;72(1):55-59.
5. Liu SH, Raskin A, Osti L, et al. Arthroscopic treatment of anterolateral ankle impingement. Arthroscopy. 1994;10(2):215-218.
6. Thein R, Eichenblat M. Arthroscopic treatment of sports-related synovitis of the ankle. Am J Sports Med. 1992;20(5):496-498.
7. Arnold H. Posttraumatic impingement syndrome of the ankle—indication and results of arthroscopic therapy. Foot Ankle Surg. 2011;17(2):85-88.
8. Walsh SJ, Twaddle BC, Rosenfeldt MP, Boyle MJ. Arthroscopic treatment of anterior ankle impingement: a prospective study of 46 patients with 5-year follow-up. Am J Sports Med. 2014;42(11):2722-2726.
9. Glazebrook MA, Ganapathy V, Bridge MA, Stone JW, Allard JP. Evidence-based indications for ankle arthroscopy. Arthroscopy. 2009;25(12):1478-1490.
10. Zwiers R, Wiegerinck JI, Murawski CD, Fraser EJ, Kennedy JG, van Dijk CN. Arthroscopic treatment for anterior ankle impingement: a systematic review of the current literature. Arthroscopy. 2015;31(8):1585-1596.
11. Hawkins RB. Arthroscopic treatment of sports-related anterior osteophytes in the ankle. Foot Ankle. 1988;9(2):87-90.
12. Rasmussen S, Hjorth Jensen C. Arthroscopic treatment of impingement of the ankle reduces pain and enhances function. Scand J Med Sci Sports. 2002;12(2):69-72.
13. Mason-Mackay AR, Whatman C, Reid D. The effect of reduced ankle dorsiflexion on lower extremity mechanics during landing: a systematic review. J Sci Med Sport. 2017;20(5):451-458.
14. Riley PO, Kent RW, Dierks TA, Lievers WB, Frimenko RE, Crandall JR. Foot kinematics and loading of professional athletes in American football-specific tasks. Gait Posture. 2013;38(4):563-569.
15. Miyamoto W, Takao M, Matsui K, Matsushita T. Simultaneous ankle arthroscopy and hindfoot endoscopy for combined anterior and posterior ankle impingement syndrome in professional athletes. J Orthop Sci. 2015;20(4):642-648.
16. Nihal A, Rose DJ, Trepman E. Arthroscopic treatment of anterior ankle impingement syndrome in dancers. Foot Ankle Int. 2005;26(11):908-912.
17. Calder JD, Sexton SA, Pearce CJ. Return to training and playing after posterior ankle arthroscopy for posterior impingement in elite professional soccer. Am J Sports Med. 2010;38(1):120-124.
18. Akseki D, Pinar H, Bozkurt M, Yaldiz K, Arag S. The distal fascicle of the anterior inferior tibiofibular ligament as a cause of anterolateral ankle impingement: results of arthroscopic resection. Acta Orthop Scand. 1999;70(5):478-482.
19. Baums MH, Kahl E, Schultz W, Klinger HM. Clinical outcome of the arthroscopic management of sports-related “anterior ankle pain”: a prospective study. Knee Surg Sports Traumatol Arthrosc. 2006;14(5):482-486.
20. Branca A, Di Palma L, Bucca C, Visconti CS, Di Mille M. Arthroscopic treatment of anterior ankle impingement. Foot Ankle Int. 1997;18(7):418-423.
21. Di Palma L, Bucca C, Di Mille M, Branca A. Diagnosis and arthroscopic treatment of fibrous impingement of the ankle. J Sports Traumatol Relat Res. 1999;21:170-177.
22. Ferkel RD, Karzel RP, Del Pizzo W, Friedman MJ, Fischer SP. Arthroscopic treatment of anterolateral impingement of the ankle. Am J Sports Med. 1991;19(5):440-446.
23. Hassan AH. Treatment of anterolateral impingements of the ankle joint by arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2007;15(9):1150-1154.
24. Jerosch J, Steinbeck J, Schröder M, Halm H. Arthroscopic treatment of anterior synovitis of the ankle in athletes. Knee Surg Sports Traumatol Arthrosc. 1994;2(3):176-181.
25. Murawski CD, Kennedy JG. Anteromedial impingement in the ankle joint: outcomes following arthroscopy. Am J Sports Med. 2010;38(10):2017-2024.
26. Ogilvie-Harris DJ, Mahomed N, Demazière A. Anterior impingement of the ankle treated by arthroscopic removal of bony spurs. J Bone Joint Surg Br. 1993;75(3):437-440.
27. Rouvillain JL, Daoud W, Donica A, Garron E, Uzel AP. Distraction-free ankle arthroscopy for anterolateral impingement. Eur J Orthop Surg Traumatol. 2014;24(6):1019-1023.
28. O’Kane JW, Kadel N. Anterior impingement syndrome in dancers. Curr Rev Musculoskelet Med. 2008;1(1):12-16.
29. Lavery KP, McHale KJ, Rossy WH, Theodore G. Ankle impingement. J Orthop Surg Res. 2016;11(1):97.
30. Talusan PG, Toy J, Perez JL, Milewski MD, Reach JS. Anterior ankle impingement: diagnosis and treatment. J Am Acad Orthop Surg. 2014;22(5):333-339.
ABSTRACT
Anterior ankle impingement is a frequent cause of pain and disability in athletes with impingement of soft-tissue or osseous structures along the anterior margin of the tibiotalar joint during dorsiflexion.
In this study, we hypothesized that arthroscopic decompression of anterior ankle impingement would result in significant, reliable, and durable improvement in pain and range of motion (ROM), and would allow National Football League (NFL) players to return to their preoperative level of play.
We reviewed 29 arthroscopic ankle débridements performed by a single surgeon. Each NFL player underwent arthroscopic débridement of pathologic soft tissue and of tibial and talar osteophytes in the anterior ankle. Preoperative and postoperative visual analog scale (VAS) pain scores, American Orthopaedic Foot and Ankle Society (AOFAS) hindfoot scores, and ankle ROM were compared; time to return to play (RTP), events missed secondary to surgery, and complications were recorded.
All athletes returned to the same level of NFL play at a mean (SD) of 8.4 (4.1) weeks after surgery and continued playing for a mean (SD) of 3.43 (2.57) years after surgery. Mean (SD) VAS pain scores decreased significantly (P < .001), to 0.38 (0.89) from 4.21 (1.52). Mean (SD) active ankle dorsiflexion increased significantly (P < .001), to 18.86° (2.62°) from 8.28° (4.14°). Mean (SD) AOFAS hindfoot scores increased significantly (P < .001), to 97.45 (4.72) from 70.62 (10.39). Degree of arthritis (r = 0.305) and age (r = 0.106) were poorly correlated to time to RTP.
In all cases, arthroscopic débridement of anterior ankle impingement resulted in RTP at the same level at a mean of 2 months after surgery. There were significant improvements in VAS pain scores, AOFAS hindfoot scores, and ROM.
Arthroscopic débridement of anterior ankle impingement relieves pain, restores ROM and function, and results in reliable RTP in professional football players.
Continue to: Anterior ankle impingement...
Anterior ankle impingement is a frequent cause of disability in athletes.1 This condition results from repetitive trauma over time, which leads to osseous and soft-tissue impingement, pain, and decreased ankle range of motion (ROM).
First termed footballer’s ankle, this condition is linked to repeated, forceful plantarflexion,2 though later studies attributed the phenomenon to repeated dorsiflexion resulting in periosteal hemorrhage.3 Both osseous and soft-tissue structures can cause impingement at the tibiotalar joint, often with osteophytes anteromedially at the tibial talar joint. Soft-tissue structures, including hypertrophic synovium, meniscoid lesions, and a thickened anterior talofibular ligament, more often cause anterolateral impingement.4-6 This process results in pain in extreme dorsiflexion, which comes into play in almost all football maneuvers, including sprinting, back-peddling, and offensive and defensive stances. Therefore, maintenance of pain-free dorsiflexion is required for high-level football. Decreased ROM can lead to decreased ability to perform these high-level athletic functions and can limit performance.
Arthroscopic débridement improves functional outcomes and functional motion in both athletes and nonathletes.7,8 In addition, findings of a recent systematic review provide support for arthroscopic treatment of ankle impingement.9 Although arthroscopic treatment is effective in nonathletes and recreational athletes,10 there is a paucity of data on the efficacy of this procedure and on time to return to play (RTP) in professional football players.
We conducted a study to evaluate the outcomes (pain, ROM, RTP) of arthroscopic débridement for anterior ankle impingement in National Football League (NFL) players. We hypothesized that arthroscopic decompression of anterior ankle impingement would result in significant, reliable, and durable improvement in pain and ROM, and would allow NFL players to return to their preoperative level of play.
METHODS
After this study was granted Institutional Review Board approval, we retrospectively reviewed a consecutive series of arthroscopically treated anterior ankle impingement athletes by a single surgeon (JPB). Indications for surgery were anterior ankle impingement resulting in ankle pain and decreased ROM that interfered with sport. Active NFL players who underwent ankle arthroscopy for symptomatic anterior ankle impingement were included. Excluded were players who underwent surgery after retirement or who retired before returning to play for reasons unrelated to the ankle. Medical records, operative reports, and rehabilitation reports were reviewed.
Continue to: Preoperative and postoperative...
Preoperative and postoperative visual analog scale (VAS) pain scores, American Orthopaedic Foot and Ankle Society (AOFAS) hindfoot scores, and ankle ROM were compared; time to RTP, events missed secondary to surgery, and complications were recorded. These preoperative and postoperative variables were compared with paired Student 2-way t tests for continuous variables. Pearson correlation coefficients were calculated.
PROCEDURE
Ankle arthroscopy was performed with the patient supine after spinal or general anesthesia was induced. Prophylactic antibiotics were given in each case. Arthroscopy was performed with standard anterolateral and anteromedial portals. First, an incision was made through skin only, followed by blunt subcutaneous dissection down to the ankle capsule. A capsulotomy was then made bluntly. Care was taken to avoid all neurovascular structures. Posterior portals were not used. A 2.7-mm arthroscope was inserted and alternated between the anteromedial and anterolateral portals to maximally visualize the ankle joint. Diagnostic arthroscopy was performed to document synovitis, chondral injury, osseous, and soft-tissue impingement and any other noted pathology (Figures 1A-1C).
A full radius resector was then used to perform a synovectomy and débridement of impinging soft tissue from the anterior talofibular ligament or anterior inferior talofibular ligament. All patients underwent arthroscopic débridement of pathologic soft tissue and of tibial and talar osteophytes in the anterior ankle. A small burr was used to débride and remove the osteophytes on the talus and/or tibia. Soft-tissue and osseous structures were resected until the contours of the talus and tibia were normal. Any unstable articular defects were débrided and loose bodies were removed. Ankle ROM was checked to confirm complete resolution of impingement (Figures 2A-2D). Patients were not immobilized and were allowed progressive weight-bearing as tolerated. Crutches were used for assisted ambulation the first 3 to 5 postoperative days.
Physical therapy progressed through 3 phases: (1) inflammation control and ROM restoration, (2) initiation of ankle strengthening, including eversion and inversion, and (3) agility, proprioception, and functional rehabilitation.
RESULTS
Twenty-five NFL players (29 surgeries) were included in the study. Two players were excluded because they had retired at the end of the season before the surgery for reasons unrelated to the operative ankle. Mean (SD) age was 28.1 (2.9) years. Six included players had a history of ankle sprains, 1 had a history of ipsilateral ankle fracture, and 1 had a history of ipsilateral ankle dislocation. Table 1 lists the positions of players who underwent ankle arthroscopic decompression.
Table 1. Positions of National Football League Players Who Underwent Ankle Arthroscopic Decompression for Anterior Ankle Impingement
Position | Surgeries, n |
| Offensive line | 8 |
| Defensive line | 8 |
| Wide receiver | 4 |
| Running back | 4 |
| Linebacker | 3 |
| Quarterback | 1 |
| Defensive back | 1 |
Continue to: During diagnostic arthroscopy...
During diagnostic arthroscopy, changes to the articular cartilage were noted: grade 0 in 38% of patients, grade 1 in 17%, grade 2 in 21%, grade 3 in 21%, and grade 4 in 3%. Four patients had an osteochondral lesion (<1 cm in each case), which was treated with chondroplasty without microfracture.
Each included patient returned to NFL play. Mean (SD) time to RTP without restrictions was 8.4 (4.1) weeks after surgery (range, 2-20 weeks). There was a poor correlation between degree of chondrosis and time to RTP (r = 0.305). In addition, there was a poor correlation between age and time to RTP (r = 0.106).
Dorsiflexion improved significantly (P < .001), patients had significantly less pain after surgery (P < .001), and AOFAS hindfoot scores improved significantly (P < .001) (Table 2).
Table 2. Preoperative and Postoperative Dorsiflexion, Pain, and AOFAS Score Before and After Arthroscopic Débridement of Anterior Ankle Impingementa
| Mean (SD) | ||
|---|---|---|
| Preoperative | Postoperative | |
| Dorsiflexion | 8.28º (4.14º) | 18.86° (2.62°) |
| VAS pain score | 4.21 (1.52) | 0.38 (0.89) |
| AOFAS score | 70.62 (10.39) | 97.45 (4.72) |
aAll values were significantly improved after surgery (P < .001).
Abbreviations: AOFAS, American Orthopaedic Foot and Ankle Society; VAS, visual analog scale.
The athletes played in the NFL for a mean (SD) of 3.43 (2.57) years after surgery (range, 1-10 seasons). These players included 6 who were still active at time of publication. No patient required revision surgery or additional surgery on the ipsilateral ankle. The one patient who was treated for superficial thrombophlebitis after surgery reported symptoms before surgery as well.
DISCUSSION
Arthroscopic decompression of anterior ankle impingement is safe and significantly improves pain and ROM in professional American football players. The procedure results in reliable RTP at an elite level, with durable results over the time remaining in their NFL careers.
Continue to: before the 1988 study by Hawkins...
Before the 1988 study by Hawkins,11 ankle spurs were removed with open procedures. Hawkins11 used arthroscopy for better and safer visualization of the ankle joint and used a burr for less painful removal of spurs from the tibia and the talus. In 2002, a series of 105 patients (median age, 35 years) had reduced pain and improved function a minimum of 2 years after arthroscopic débridement.12 These patients had a mix of pathology, including soft-tissue impingement, bony impingement, chondral lesions, loose bodies, and osteoarthritis.
For many elite athletes, anterior ankle impingement can cause significant limitation. Reduced ankle dorsiflexion can alter all limb mechanics and predispose athletes to injury.13 In addition, because NFL players’ ankle ROM often approaches or exceeds normal physiologic limits,14 an ankle ROM limitation will often hinder their performance.
Miyamoto and colleagues15 studied a series of 9 professional athletes (6 soccer players, 1 baseball pitcher, 1 mixed martial artist, 1 golfer) who underwent decompression of both anterior and posterior impingement. With regard to anterior impingement, they found anterior osteophytes in all the ankles, as was seen in the present study. Furthermore, they noted that mean dorsiflexion improved from 10° before surgery to 15° after surgery and that their athletes returned to play 12 to 15 weeks after surgery. Their results are similar to ours, though we noted more improvement in dorsiflexion, from 8.28° before surgery to 18.86° after surgery.
One of the most important metrics in evaluating treatment options for professional athletes is time from surgery to RTP without restrictions. Mean time to full RTP was shorter in our study (8.4 weeks) than in the study by Miyamoto and colleagues15 (up to 20 weeks). However, many of their procedures were performed during the off-season, when there was no need to expeditiously clear patients for full sports participation. In addition, the patients in their study had both anterior and posterior pathology.
Faster return to high-level athletics was supported in a study of 11 elite ballet dancers,16 whose pain and dance performance improved after arthroscopic débridement. Of the 11 patients, 9 returned to dance at a mean of 7 weeks after surgery; the other 2 required reoperation. Although the pathology differed in their study of elite professional soccer players, Calder and colleagues17 found that mean time to RTP after ankle arthroscopy for posterior impingement was 5 weeks.
Continue to: For the NFL players in our study...
For the NFL players in our study, RTP at their elite level was 100% after arthroscopic débridement of anterior ankle impingement. In the literature, time to RTP varies. Table 3 lists RTP rates for recreational athletes in published studies.18-27 In their recent systematic literature review, Zwiers and colleagues10 noted that 24% to 96.4% of recreational athletes returned to play after arthroscopic treatment for anterior ankle impingement. The percentage was significantly higher for the professional athletes in our study. Historical comparison supports an evolution in the indications and techniques for this procedure, with more recent literature suggesting a RTP rate much higher than earlier rates. In addition, compared with recreational athletes, professional athletes have strong financial incentives to return to their sports. Furthermore, our professional cohort was significantly younger than the recreational cohorts in those studies.
Table 3. Frequency of Recreational Athletes’ Return to Play After Arthroscopic Débridement of Anterior Ankle Impingement, as Reported in the Literature
| Study | Year | Journal | Return to Play | |
|---|---|---|---|---|
| n/N | % | |||
| Akseki et al18 | 1999 | Acta Orthop Scand | 10/11 | 91 |
| Baums et al19 | 2006 | Knee Surg Sports Traumatol Arthrosc | 25/26 | 96 |
| Branca et al20 | 1997 | Foot Ankle Int | 13/27 | 48 |
| Di Palma et al21 | 1999 | J Sports Traumatol Relat Res | 21/32 | 66 |
| Ferkel et al22 | 1991 | Am J Sports Med | 27/31 | 87.1 |
| Hassan23 | 2007 | Knee Surg Sports Traumatol Arthrosc | 9/11 | 82 |
| Jerosch et al24 | 1994 | Knee Surg Sports Traumatol Arthrosc | 9/38 | 24 |
| Murawski & Kennedy25 | 2010 | Am J Sports Med | 27/28 | 96.4 |
| Ogilvie-Harris et al26 | 1993 | J Bone Joint Surg Br | 21/28 | 75 |
| Rouvillain et al27 | 2014 | Eur J Orthop Surg Traumatol | 10/11 | 90 |
Total | 172/243 | 70 | ||
Current recommendations for recreational athletes include initial conservative treatment with rest, ankle bracing, and avoidance of jumping and other repetitive dorsiflexing activities. Physical therapy should include joint mobilization and work along the entire kinetic chain. Night splints or a removable walking boot can be used temporarily, as can a single intra-articular corticosteroid injection to reduce inflammation and evaluate improvement in more refractory cases.28 Commonly, conservative treatments fail if patients remain active, and soft tissue and/or osteophytes can be resected, though resection typically is reserved for recreational athletes for whom nonoperative treatments have been exhausted.29,30
This study had several limitations, including its retrospective nature and lack of control group. In addition, follow-up was relatively short, and we did not use more recently described outcome measures, such as the Sports subscale of the Foot and Ankle Ability Measure, which may be more sensitive in describing function in elite athletes. However, many of the cases in our study predated these measures, but the rate of RTP at the NFL level requires a very high degree of postoperative ankle function, making this outcome the most meaningful. In the context of professional athletes, specifically the length of their careers, our study results provide valuable information regarding expectations about RTP and the durability of arthroscopic débridement of anterior ankle impingement in a high-demand setting.
CONCLUSION
For all the NFL players in this study, arthroscopic débridement of anterior ankle impingement resulted in return to preoperative level of play at a mean of 2 months after surgery. There were significant improvements in VAS pain scores, AOFAS hindfoot scores, and ROM. Arthroscopic débridement of anterior ankle impingement relieves pain, restores ROM and function, and results in reliable RTP in professional football players.
ABSTRACT
Anterior ankle impingement is a frequent cause of pain and disability in athletes with impingement of soft-tissue or osseous structures along the anterior margin of the tibiotalar joint during dorsiflexion.
In this study, we hypothesized that arthroscopic decompression of anterior ankle impingement would result in significant, reliable, and durable improvement in pain and range of motion (ROM), and would allow National Football League (NFL) players to return to their preoperative level of play.
We reviewed 29 arthroscopic ankle débridements performed by a single surgeon. Each NFL player underwent arthroscopic débridement of pathologic soft tissue and of tibial and talar osteophytes in the anterior ankle. Preoperative and postoperative visual analog scale (VAS) pain scores, American Orthopaedic Foot and Ankle Society (AOFAS) hindfoot scores, and ankle ROM were compared; time to return to play (RTP), events missed secondary to surgery, and complications were recorded.
All athletes returned to the same level of NFL play at a mean (SD) of 8.4 (4.1) weeks after surgery and continued playing for a mean (SD) of 3.43 (2.57) years after surgery. Mean (SD) VAS pain scores decreased significantly (P < .001), to 0.38 (0.89) from 4.21 (1.52). Mean (SD) active ankle dorsiflexion increased significantly (P < .001), to 18.86° (2.62°) from 8.28° (4.14°). Mean (SD) AOFAS hindfoot scores increased significantly (P < .001), to 97.45 (4.72) from 70.62 (10.39). Degree of arthritis (r = 0.305) and age (r = 0.106) were poorly correlated to time to RTP.
In all cases, arthroscopic débridement of anterior ankle impingement resulted in RTP at the same level at a mean of 2 months after surgery. There were significant improvements in VAS pain scores, AOFAS hindfoot scores, and ROM.
Arthroscopic débridement of anterior ankle impingement relieves pain, restores ROM and function, and results in reliable RTP in professional football players.
Continue to: Anterior ankle impingement...
Anterior ankle impingement is a frequent cause of disability in athletes.1 This condition results from repetitive trauma over time, which leads to osseous and soft-tissue impingement, pain, and decreased ankle range of motion (ROM).
First termed footballer’s ankle, this condition is linked to repeated, forceful plantarflexion,2 though later studies attributed the phenomenon to repeated dorsiflexion resulting in periosteal hemorrhage.3 Both osseous and soft-tissue structures can cause impingement at the tibiotalar joint, often with osteophytes anteromedially at the tibial talar joint. Soft-tissue structures, including hypertrophic synovium, meniscoid lesions, and a thickened anterior talofibular ligament, more often cause anterolateral impingement.4-6 This process results in pain in extreme dorsiflexion, which comes into play in almost all football maneuvers, including sprinting, back-peddling, and offensive and defensive stances. Therefore, maintenance of pain-free dorsiflexion is required for high-level football. Decreased ROM can lead to decreased ability to perform these high-level athletic functions and can limit performance.
Arthroscopic débridement improves functional outcomes and functional motion in both athletes and nonathletes.7,8 In addition, findings of a recent systematic review provide support for arthroscopic treatment of ankle impingement.9 Although arthroscopic treatment is effective in nonathletes and recreational athletes,10 there is a paucity of data on the efficacy of this procedure and on time to return to play (RTP) in professional football players.
We conducted a study to evaluate the outcomes (pain, ROM, RTP) of arthroscopic débridement for anterior ankle impingement in National Football League (NFL) players. We hypothesized that arthroscopic decompression of anterior ankle impingement would result in significant, reliable, and durable improvement in pain and ROM, and would allow NFL players to return to their preoperative level of play.
METHODS
After this study was granted Institutional Review Board approval, we retrospectively reviewed a consecutive series of arthroscopically treated anterior ankle impingement athletes by a single surgeon (JPB). Indications for surgery were anterior ankle impingement resulting in ankle pain and decreased ROM that interfered with sport. Active NFL players who underwent ankle arthroscopy for symptomatic anterior ankle impingement were included. Excluded were players who underwent surgery after retirement or who retired before returning to play for reasons unrelated to the ankle. Medical records, operative reports, and rehabilitation reports were reviewed.
Continue to: Preoperative and postoperative...
Preoperative and postoperative visual analog scale (VAS) pain scores, American Orthopaedic Foot and Ankle Society (AOFAS) hindfoot scores, and ankle ROM were compared; time to RTP, events missed secondary to surgery, and complications were recorded. These preoperative and postoperative variables were compared with paired Student 2-way t tests for continuous variables. Pearson correlation coefficients were calculated.
PROCEDURE
Ankle arthroscopy was performed with the patient supine after spinal or general anesthesia was induced. Prophylactic antibiotics were given in each case. Arthroscopy was performed with standard anterolateral and anteromedial portals. First, an incision was made through skin only, followed by blunt subcutaneous dissection down to the ankle capsule. A capsulotomy was then made bluntly. Care was taken to avoid all neurovascular structures. Posterior portals were not used. A 2.7-mm arthroscope was inserted and alternated between the anteromedial and anterolateral portals to maximally visualize the ankle joint. Diagnostic arthroscopy was performed to document synovitis, chondral injury, osseous, and soft-tissue impingement and any other noted pathology (Figures 1A-1C).
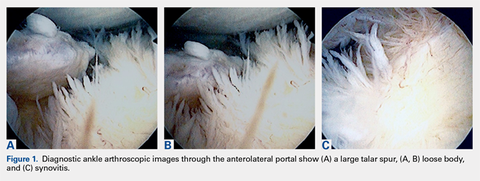
A full radius resector was then used to perform a synovectomy and débridement of impinging soft tissue from the anterior talofibular ligament or anterior inferior talofibular ligament. All patients underwent arthroscopic débridement of pathologic soft tissue and of tibial and talar osteophytes in the anterior ankle. A small burr was used to débride and remove the osteophytes on the talus and/or tibia. Soft-tissue and osseous structures were resected until the contours of the talus and tibia were normal. Any unstable articular defects were débrided and loose bodies were removed. Ankle ROM was checked to confirm complete resolution of impingement (Figures 2A-2D). Patients were not immobilized and were allowed progressive weight-bearing as tolerated. Crutches were used for assisted ambulation the first 3 to 5 postoperative days.
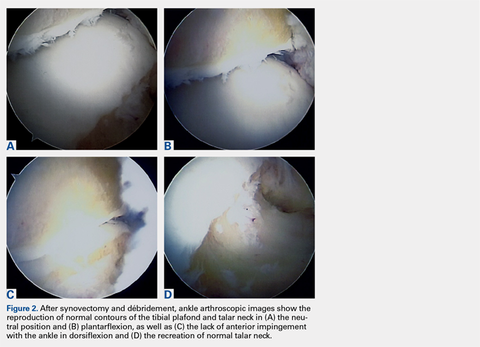
Physical therapy progressed through 3 phases: (1) inflammation control and ROM restoration, (2) initiation of ankle strengthening, including eversion and inversion, and (3) agility, proprioception, and functional rehabilitation.
RESULTS
Twenty-five NFL players (29 surgeries) were included in the study. Two players were excluded because they had retired at the end of the season before the surgery for reasons unrelated to the operative ankle. Mean (SD) age was 28.1 (2.9) years. Six included players had a history of ankle sprains, 1 had a history of ipsilateral ankle fracture, and 1 had a history of ipsilateral ankle dislocation. Table 1 lists the positions of players who underwent ankle arthroscopic decompression.
Table 1. Positions of National Football League Players Who Underwent Ankle Arthroscopic Decompression for Anterior Ankle Impingement
Position | Surgeries, n |
| Offensive line | 8 |
| Defensive line | 8 |
| Wide receiver | 4 |
| Running back | 4 |
| Linebacker | 3 |
| Quarterback | 1 |
| Defensive back | 1 |
Continue to: During diagnostic arthroscopy...
During diagnostic arthroscopy, changes to the articular cartilage were noted: grade 0 in 38% of patients, grade 1 in 17%, grade 2 in 21%, grade 3 in 21%, and grade 4 in 3%. Four patients had an osteochondral lesion (<1 cm in each case), which was treated with chondroplasty without microfracture.
Each included patient returned to NFL play. Mean (SD) time to RTP without restrictions was 8.4 (4.1) weeks after surgery (range, 2-20 weeks). There was a poor correlation between degree of chondrosis and time to RTP (r = 0.305). In addition, there was a poor correlation between age and time to RTP (r = 0.106).
Dorsiflexion improved significantly (P < .001), patients had significantly less pain after surgery (P < .001), and AOFAS hindfoot scores improved significantly (P < .001) (Table 2).
Table 2. Preoperative and Postoperative Dorsiflexion, Pain, and AOFAS Score Before and After Arthroscopic Débridement of Anterior Ankle Impingementa
| Mean (SD) | ||
|---|---|---|
| Preoperative | Postoperative | |
| Dorsiflexion | 8.28º (4.14º) | 18.86° (2.62°) |
| VAS pain score | 4.21 (1.52) | 0.38 (0.89) |
| AOFAS score | 70.62 (10.39) | 97.45 (4.72) |
aAll values were significantly improved after surgery (P < .001).
Abbreviations: AOFAS, American Orthopaedic Foot and Ankle Society; VAS, visual analog scale.
The athletes played in the NFL for a mean (SD) of 3.43 (2.57) years after surgery (range, 1-10 seasons). These players included 6 who were still active at time of publication. No patient required revision surgery or additional surgery on the ipsilateral ankle. The one patient who was treated for superficial thrombophlebitis after surgery reported symptoms before surgery as well.
DISCUSSION
Arthroscopic decompression of anterior ankle impingement is safe and significantly improves pain and ROM in professional American football players. The procedure results in reliable RTP at an elite level, with durable results over the time remaining in their NFL careers.
Continue to: before the 1988 study by Hawkins...
Before the 1988 study by Hawkins,11 ankle spurs were removed with open procedures. Hawkins11 used arthroscopy for better and safer visualization of the ankle joint and used a burr for less painful removal of spurs from the tibia and the talus. In 2002, a series of 105 patients (median age, 35 years) had reduced pain and improved function a minimum of 2 years after arthroscopic débridement.12 These patients had a mix of pathology, including soft-tissue impingement, bony impingement, chondral lesions, loose bodies, and osteoarthritis.
For many elite athletes, anterior ankle impingement can cause significant limitation. Reduced ankle dorsiflexion can alter all limb mechanics and predispose athletes to injury.13 In addition, because NFL players’ ankle ROM often approaches or exceeds normal physiologic limits,14 an ankle ROM limitation will often hinder their performance.
Miyamoto and colleagues15 studied a series of 9 professional athletes (6 soccer players, 1 baseball pitcher, 1 mixed martial artist, 1 golfer) who underwent decompression of both anterior and posterior impingement. With regard to anterior impingement, they found anterior osteophytes in all the ankles, as was seen in the present study. Furthermore, they noted that mean dorsiflexion improved from 10° before surgery to 15° after surgery and that their athletes returned to play 12 to 15 weeks after surgery. Their results are similar to ours, though we noted more improvement in dorsiflexion, from 8.28° before surgery to 18.86° after surgery.
One of the most important metrics in evaluating treatment options for professional athletes is time from surgery to RTP without restrictions. Mean time to full RTP was shorter in our study (8.4 weeks) than in the study by Miyamoto and colleagues15 (up to 20 weeks). However, many of their procedures were performed during the off-season, when there was no need to expeditiously clear patients for full sports participation. In addition, the patients in their study had both anterior and posterior pathology.
Faster return to high-level athletics was supported in a study of 11 elite ballet dancers,16 whose pain and dance performance improved after arthroscopic débridement. Of the 11 patients, 9 returned to dance at a mean of 7 weeks after surgery; the other 2 required reoperation. Although the pathology differed in their study of elite professional soccer players, Calder and colleagues17 found that mean time to RTP after ankle arthroscopy for posterior impingement was 5 weeks.
Continue to: For the NFL players in our study...
For the NFL players in our study, RTP at their elite level was 100% after arthroscopic débridement of anterior ankle impingement. In the literature, time to RTP varies. Table 3 lists RTP rates for recreational athletes in published studies.18-27 In their recent systematic literature review, Zwiers and colleagues10 noted that 24% to 96.4% of recreational athletes returned to play after arthroscopic treatment for anterior ankle impingement. The percentage was significantly higher for the professional athletes in our study. Historical comparison supports an evolution in the indications and techniques for this procedure, with more recent literature suggesting a RTP rate much higher than earlier rates. In addition, compared with recreational athletes, professional athletes have strong financial incentives to return to their sports. Furthermore, our professional cohort was significantly younger than the recreational cohorts in those studies.
Table 3. Frequency of Recreational Athletes’ Return to Play After Arthroscopic Débridement of Anterior Ankle Impingement, as Reported in the Literature
| Study | Year | Journal | Return to Play | |
|---|---|---|---|---|
| n/N | % | |||
| Akseki et al18 | 1999 | Acta Orthop Scand | 10/11 | 91 |
| Baums et al19 | 2006 | Knee Surg Sports Traumatol Arthrosc | 25/26 | 96 |
| Branca et al20 | 1997 | Foot Ankle Int | 13/27 | 48 |
| Di Palma et al21 | 1999 | J Sports Traumatol Relat Res | 21/32 | 66 |
| Ferkel et al22 | 1991 | Am J Sports Med | 27/31 | 87.1 |
| Hassan23 | 2007 | Knee Surg Sports Traumatol Arthrosc | 9/11 | 82 |
| Jerosch et al24 | 1994 | Knee Surg Sports Traumatol Arthrosc | 9/38 | 24 |
| Murawski & Kennedy25 | 2010 | Am J Sports Med | 27/28 | 96.4 |
| Ogilvie-Harris et al26 | 1993 | J Bone Joint Surg Br | 21/28 | 75 |
| Rouvillain et al27 | 2014 | Eur J Orthop Surg Traumatol | 10/11 | 90 |
Total | 172/243 | 70 | ||
Current recommendations for recreational athletes include initial conservative treatment with rest, ankle bracing, and avoidance of jumping and other repetitive dorsiflexing activities. Physical therapy should include joint mobilization and work along the entire kinetic chain. Night splints or a removable walking boot can be used temporarily, as can a single intra-articular corticosteroid injection to reduce inflammation and evaluate improvement in more refractory cases.28 Commonly, conservative treatments fail if patients remain active, and soft tissue and/or osteophytes can be resected, though resection typically is reserved for recreational athletes for whom nonoperative treatments have been exhausted.29,30
This study had several limitations, including its retrospective nature and lack of control group. In addition, follow-up was relatively short, and we did not use more recently described outcome measures, such as the Sports subscale of the Foot and Ankle Ability Measure, which may be more sensitive in describing function in elite athletes. However, many of the cases in our study predated these measures, but the rate of RTP at the NFL level requires a very high degree of postoperative ankle function, making this outcome the most meaningful. In the context of professional athletes, specifically the length of their careers, our study results provide valuable information regarding expectations about RTP and the durability of arthroscopic débridement of anterior ankle impingement in a high-demand setting.
CONCLUSION
For all the NFL players in this study, arthroscopic débridement of anterior ankle impingement resulted in return to preoperative level of play at a mean of 2 months after surgery. There were significant improvements in VAS pain scores, AOFAS hindfoot scores, and ROM. Arthroscopic débridement of anterior ankle impingement relieves pain, restores ROM and function, and results in reliable RTP in professional football players.
1. Lubowitz JH. Editorial commentary: ankle anterior impingement is common in athletes and could be under-recognized. Arthroscopy. 2015;31(8):1597.
2. Mcdougall A. Footballer’s ankle. Lancet. 1955;269(6902):1219-1220.
3. Kleiger B. Anterior tibiotalar impingement syndromes in dancers. Foot Ankle. 1982;3(2):69-73.
4. Bassett FH 3rd, Gates HS 3rd, Billys JB, Morris HB, Nikolaou PK. Talar impingement by the anteroinferior tibiofibular ligament. A cause of chronic pain in the ankle after inversion sprain. J Bone Joint Surg Am. 1990;72(1):55-59.
5. Liu SH, Raskin A, Osti L, et al. Arthroscopic treatment of anterolateral ankle impingement. Arthroscopy. 1994;10(2):215-218.
6. Thein R, Eichenblat M. Arthroscopic treatment of sports-related synovitis of the ankle. Am J Sports Med. 1992;20(5):496-498.
7. Arnold H. Posttraumatic impingement syndrome of the ankle—indication and results of arthroscopic therapy. Foot Ankle Surg. 2011;17(2):85-88.
8. Walsh SJ, Twaddle BC, Rosenfeldt MP, Boyle MJ. Arthroscopic treatment of anterior ankle impingement: a prospective study of 46 patients with 5-year follow-up. Am J Sports Med. 2014;42(11):2722-2726.
9. Glazebrook MA, Ganapathy V, Bridge MA, Stone JW, Allard JP. Evidence-based indications for ankle arthroscopy. Arthroscopy. 2009;25(12):1478-1490.
10. Zwiers R, Wiegerinck JI, Murawski CD, Fraser EJ, Kennedy JG, van Dijk CN. Arthroscopic treatment for anterior ankle impingement: a systematic review of the current literature. Arthroscopy. 2015;31(8):1585-1596.
11. Hawkins RB. Arthroscopic treatment of sports-related anterior osteophytes in the ankle. Foot Ankle. 1988;9(2):87-90.
12. Rasmussen S, Hjorth Jensen C. Arthroscopic treatment of impingement of the ankle reduces pain and enhances function. Scand J Med Sci Sports. 2002;12(2):69-72.
13. Mason-Mackay AR, Whatman C, Reid D. The effect of reduced ankle dorsiflexion on lower extremity mechanics during landing: a systematic review. J Sci Med Sport. 2017;20(5):451-458.
14. Riley PO, Kent RW, Dierks TA, Lievers WB, Frimenko RE, Crandall JR. Foot kinematics and loading of professional athletes in American football-specific tasks. Gait Posture. 2013;38(4):563-569.
15. Miyamoto W, Takao M, Matsui K, Matsushita T. Simultaneous ankle arthroscopy and hindfoot endoscopy for combined anterior and posterior ankle impingement syndrome in professional athletes. J Orthop Sci. 2015;20(4):642-648.
16. Nihal A, Rose DJ, Trepman E. Arthroscopic treatment of anterior ankle impingement syndrome in dancers. Foot Ankle Int. 2005;26(11):908-912.
17. Calder JD, Sexton SA, Pearce CJ. Return to training and playing after posterior ankle arthroscopy for posterior impingement in elite professional soccer. Am J Sports Med. 2010;38(1):120-124.
18. Akseki D, Pinar H, Bozkurt M, Yaldiz K, Arag S. The distal fascicle of the anterior inferior tibiofibular ligament as a cause of anterolateral ankle impingement: results of arthroscopic resection. Acta Orthop Scand. 1999;70(5):478-482.
19. Baums MH, Kahl E, Schultz W, Klinger HM. Clinical outcome of the arthroscopic management of sports-related “anterior ankle pain”: a prospective study. Knee Surg Sports Traumatol Arthrosc. 2006;14(5):482-486.
20. Branca A, Di Palma L, Bucca C, Visconti CS, Di Mille M. Arthroscopic treatment of anterior ankle impingement. Foot Ankle Int. 1997;18(7):418-423.
21. Di Palma L, Bucca C, Di Mille M, Branca A. Diagnosis and arthroscopic treatment of fibrous impingement of the ankle. J Sports Traumatol Relat Res. 1999;21:170-177.
22. Ferkel RD, Karzel RP, Del Pizzo W, Friedman MJ, Fischer SP. Arthroscopic treatment of anterolateral impingement of the ankle. Am J Sports Med. 1991;19(5):440-446.
23. Hassan AH. Treatment of anterolateral impingements of the ankle joint by arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2007;15(9):1150-1154.
24. Jerosch J, Steinbeck J, Schröder M, Halm H. Arthroscopic treatment of anterior synovitis of the ankle in athletes. Knee Surg Sports Traumatol Arthrosc. 1994;2(3):176-181.
25. Murawski CD, Kennedy JG. Anteromedial impingement in the ankle joint: outcomes following arthroscopy. Am J Sports Med. 2010;38(10):2017-2024.
26. Ogilvie-Harris DJ, Mahomed N, Demazière A. Anterior impingement of the ankle treated by arthroscopic removal of bony spurs. J Bone Joint Surg Br. 1993;75(3):437-440.
27. Rouvillain JL, Daoud W, Donica A, Garron E, Uzel AP. Distraction-free ankle arthroscopy for anterolateral impingement. Eur J Orthop Surg Traumatol. 2014;24(6):1019-1023.
28. O’Kane JW, Kadel N. Anterior impingement syndrome in dancers. Curr Rev Musculoskelet Med. 2008;1(1):12-16.
29. Lavery KP, McHale KJ, Rossy WH, Theodore G. Ankle impingement. J Orthop Surg Res. 2016;11(1):97.
30. Talusan PG, Toy J, Perez JL, Milewski MD, Reach JS. Anterior ankle impingement: diagnosis and treatment. J Am Acad Orthop Surg. 2014;22(5):333-339.
1. Lubowitz JH. Editorial commentary: ankle anterior impingement is common in athletes and could be under-recognized. Arthroscopy. 2015;31(8):1597.
2. Mcdougall A. Footballer’s ankle. Lancet. 1955;269(6902):1219-1220.
3. Kleiger B. Anterior tibiotalar impingement syndromes in dancers. Foot Ankle. 1982;3(2):69-73.
4. Bassett FH 3rd, Gates HS 3rd, Billys JB, Morris HB, Nikolaou PK. Talar impingement by the anteroinferior tibiofibular ligament. A cause of chronic pain in the ankle after inversion sprain. J Bone Joint Surg Am. 1990;72(1):55-59.
5. Liu SH, Raskin A, Osti L, et al. Arthroscopic treatment of anterolateral ankle impingement. Arthroscopy. 1994;10(2):215-218.
6. Thein R, Eichenblat M. Arthroscopic treatment of sports-related synovitis of the ankle. Am J Sports Med. 1992;20(5):496-498.
7. Arnold H. Posttraumatic impingement syndrome of the ankle—indication and results of arthroscopic therapy. Foot Ankle Surg. 2011;17(2):85-88.
8. Walsh SJ, Twaddle BC, Rosenfeldt MP, Boyle MJ. Arthroscopic treatment of anterior ankle impingement: a prospective study of 46 patients with 5-year follow-up. Am J Sports Med. 2014;42(11):2722-2726.
9. Glazebrook MA, Ganapathy V, Bridge MA, Stone JW, Allard JP. Evidence-based indications for ankle arthroscopy. Arthroscopy. 2009;25(12):1478-1490.
10. Zwiers R, Wiegerinck JI, Murawski CD, Fraser EJ, Kennedy JG, van Dijk CN. Arthroscopic treatment for anterior ankle impingement: a systematic review of the current literature. Arthroscopy. 2015;31(8):1585-1596.
11. Hawkins RB. Arthroscopic treatment of sports-related anterior osteophytes in the ankle. Foot Ankle. 1988;9(2):87-90.
12. Rasmussen S, Hjorth Jensen C. Arthroscopic treatment of impingement of the ankle reduces pain and enhances function. Scand J Med Sci Sports. 2002;12(2):69-72.
13. Mason-Mackay AR, Whatman C, Reid D. The effect of reduced ankle dorsiflexion on lower extremity mechanics during landing: a systematic review. J Sci Med Sport. 2017;20(5):451-458.
14. Riley PO, Kent RW, Dierks TA, Lievers WB, Frimenko RE, Crandall JR. Foot kinematics and loading of professional athletes in American football-specific tasks. Gait Posture. 2013;38(4):563-569.
15. Miyamoto W, Takao M, Matsui K, Matsushita T. Simultaneous ankle arthroscopy and hindfoot endoscopy for combined anterior and posterior ankle impingement syndrome in professional athletes. J Orthop Sci. 2015;20(4):642-648.
16. Nihal A, Rose DJ, Trepman E. Arthroscopic treatment of anterior ankle impingement syndrome in dancers. Foot Ankle Int. 2005;26(11):908-912.
17. Calder JD, Sexton SA, Pearce CJ. Return to training and playing after posterior ankle arthroscopy for posterior impingement in elite professional soccer. Am J Sports Med. 2010;38(1):120-124.
18. Akseki D, Pinar H, Bozkurt M, Yaldiz K, Arag S. The distal fascicle of the anterior inferior tibiofibular ligament as a cause of anterolateral ankle impingement: results of arthroscopic resection. Acta Orthop Scand. 1999;70(5):478-482.
19. Baums MH, Kahl E, Schultz W, Klinger HM. Clinical outcome of the arthroscopic management of sports-related “anterior ankle pain”: a prospective study. Knee Surg Sports Traumatol Arthrosc. 2006;14(5):482-486.
20. Branca A, Di Palma L, Bucca C, Visconti CS, Di Mille M. Arthroscopic treatment of anterior ankle impingement. Foot Ankle Int. 1997;18(7):418-423.
21. Di Palma L, Bucca C, Di Mille M, Branca A. Diagnosis and arthroscopic treatment of fibrous impingement of the ankle. J Sports Traumatol Relat Res. 1999;21:170-177.
22. Ferkel RD, Karzel RP, Del Pizzo W, Friedman MJ, Fischer SP. Arthroscopic treatment of anterolateral impingement of the ankle. Am J Sports Med. 1991;19(5):440-446.
23. Hassan AH. Treatment of anterolateral impingements of the ankle joint by arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2007;15(9):1150-1154.
24. Jerosch J, Steinbeck J, Schröder M, Halm H. Arthroscopic treatment of anterior synovitis of the ankle in athletes. Knee Surg Sports Traumatol Arthrosc. 1994;2(3):176-181.
25. Murawski CD, Kennedy JG. Anteromedial impingement in the ankle joint: outcomes following arthroscopy. Am J Sports Med. 2010;38(10):2017-2024.
26. Ogilvie-Harris DJ, Mahomed N, Demazière A. Anterior impingement of the ankle treated by arthroscopic removal of bony spurs. J Bone Joint Surg Br. 1993;75(3):437-440.
27. Rouvillain JL, Daoud W, Donica A, Garron E, Uzel AP. Distraction-free ankle arthroscopy for anterolateral impingement. Eur J Orthop Surg Traumatol. 2014;24(6):1019-1023.
28. O’Kane JW, Kadel N. Anterior impingement syndrome in dancers. Curr Rev Musculoskelet Med. 2008;1(1):12-16.
29. Lavery KP, McHale KJ, Rossy WH, Theodore G. Ankle impingement. J Orthop Surg Res. 2016;11(1):97.
30. Talusan PG, Toy J, Perez JL, Milewski MD, Reach JS. Anterior ankle impingement: diagnosis and treatment. J Am Acad Orthop Surg. 2014;22(5):333-339.
TAKE-HOME POINTS
- Anterior ankle impingement can be very debilitating in elite athletes and may lead to significantly decreased performance.
- First line treatment for anterior ankle impingement is conservative which includes rest, ankle bracing, and avoidance of repetitive dorsiflexing activities such as jumping.
- Arthroscopic débridement of anterior ankle impingement reliably relieves pain, and restores ROM and function.
- Arthroscopic débridement of anterior ankle impingement results in reliable RTP in professional football players.
- RTP after arthroscopic anterior ankle débridement for impingement averaged 2 months in professional football players.
