User login
Emergency Imaging
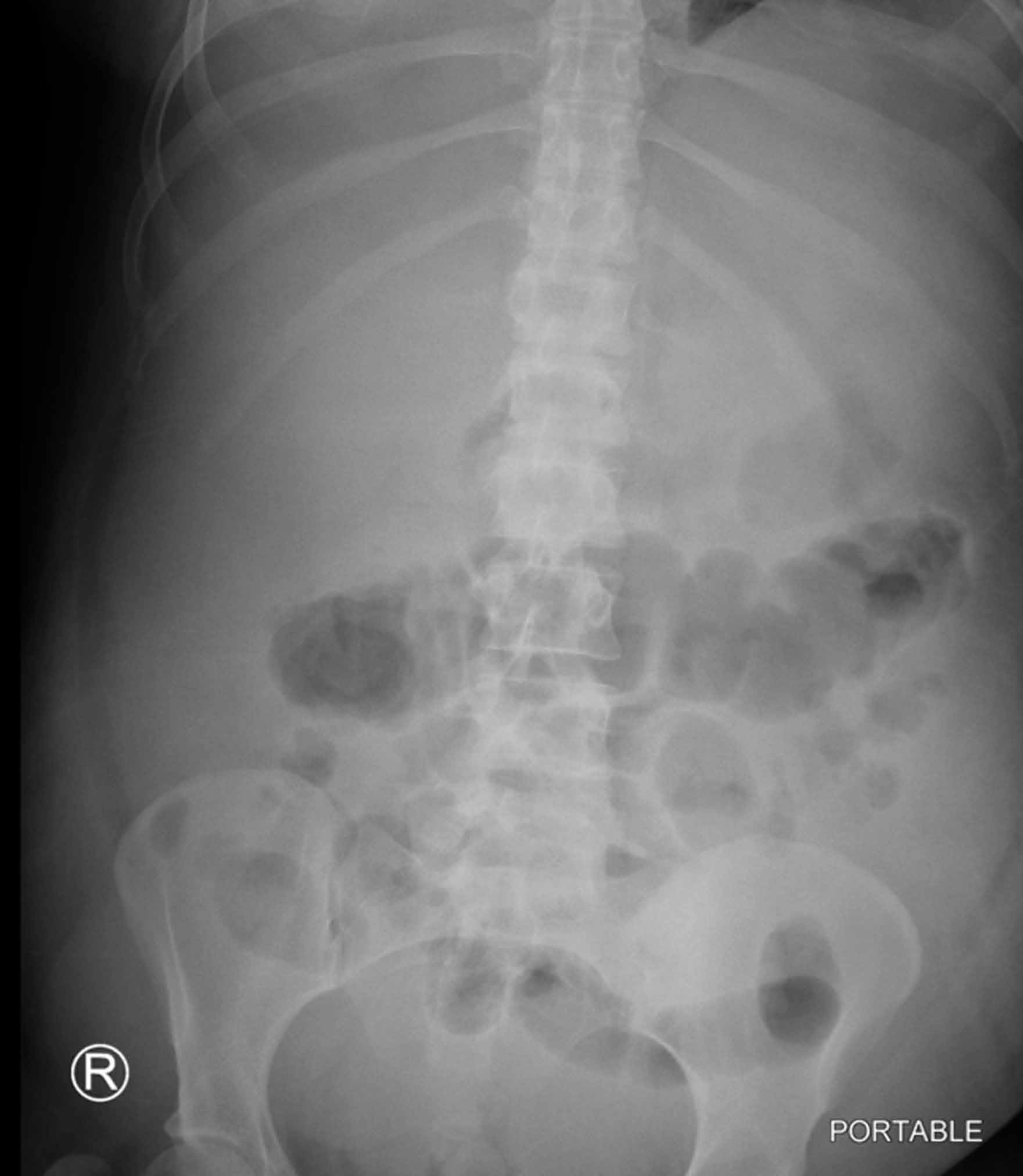
30-year-old woman with a history of alcoholism and anxiety presented to the ED for evaluation of abdominal distension and pain. She reported new social stressors at home and increased alcohol consumption. She also noted gradually increasing abdominal distension over the past several weeks. As patient’s liver function tests were elevated, supine radiographs of the abdomen were acquired for further evaluation; a representative image is presented below (Figure 1a).
What is the suspected diagnosis?
Is any additional imaging required?
Answer
Centralization of bowel is suggestive of abdominopelvic ascites.1 Additional radiographic findings that may be seen with ascites include diffusely increased density of the abdomen and bulging of the peritoneal fat stripes/flanks. In the average adult, a minimum of approximately 800 mL of ascitic fluid is required to medially displace bowel loops or abdominal viscera.2 While there are many causes of ascites, the radiograph in this case suggests the underlying etiology of cirrhosis. Although the top of the liver is not visualized on the radiograph, the liver contour appears enlarged (red arrow, Figure 1b).
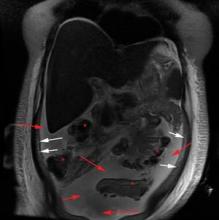
In the ED, ultrasound is the imaging modality of choice to confirm the presence of ascites as it is widely available, quick, relatively inexpensive, and does not require ionizing radiation. Ultrasound is also useful when examining the abdominal viscera since it may detect the underlying cause of ascites.3 The ultrasound image of the abdominal viscera in this case demonstrated a hypoechoic (dark) signal (red arrow, Figure 1c) between the abdominal wall (red asterisk, Figure 1c) and bowel loops (letter ‘B,” Figure 1c). This finding confirmed the presence of ascites because simple fluid does not reflect the ultrasound beam, but instead results in the hypoechoic signal seen in Figure 1c. An additional sonographic image confirmed the presence of an enlarged liver (white asterisk, Figure 1d) and ascites in the right upper quadrant (red arrow, Figure 1d).
The patient was admitted for further workup and treatment of alcoholic cirrhosis. A
Dr Lyons is a resident in the department of radiology at New York Presbyterian Hospital/Weill Cornell Medical College in New York City. Dr Wladyka is an assistant professor of radiology at Weill Cornell Medical College in New York City and an assistant attending radiologist at NewYork-Presbyterian Hospital/Weill Cornell Medical Center. Dr Hentel is an associate professor of clinical radiology at Weill Cornell Medical College in New York City. He is also chief of emergency/musculoskeletal imaging and executive vice-chairman for the department of radiology at New York-
- Meschan I. Analysis of Roentgen Signs in General Radiology. Philadelphia, PA: Saunders; 1973:1231.
- Keeffee EJ, Gagliardi RA, Pfister RC. The roentgenographic evaluation of ascites. Am J Roentgenol. 1967;101(2):388-396.
- Goldberg BB, Goodman GA, Clearfield HR. Evaluation of ascites by ultrasound. Radiology. 1970;96(1):15-22.
30-year-old woman with a history of alcoholism and anxiety presented to the ED for evaluation of abdominal distension and pain. She reported new social stressors at home and increased alcohol consumption. She also noted gradually increasing abdominal distension over the past several weeks. As patient’s liver function tests were elevated, supine radiographs of the abdomen were acquired for further evaluation; a representative image is presented below (Figure 1a).
What is the suspected diagnosis?
Is any additional imaging required?
Answer
Centralization of bowel is suggestive of abdominopelvic ascites.1 Additional radiographic findings that may be seen with ascites include diffusely increased density of the abdomen and bulging of the peritoneal fat stripes/flanks. In the average adult, a minimum of approximately 800 mL of ascitic fluid is required to medially displace bowel loops or abdominal viscera.2 While there are many causes of ascites, the radiograph in this case suggests the underlying etiology of cirrhosis. Although the top of the liver is not visualized on the radiograph, the liver contour appears enlarged (red arrow, Figure 1b).
In the ED, ultrasound is the imaging modality of choice to confirm the presence of ascites as it is widely available, quick, relatively inexpensive, and does not require ionizing radiation. Ultrasound is also useful when examining the abdominal viscera since it may detect the underlying cause of ascites.3 The ultrasound image of the abdominal viscera in this case demonstrated a hypoechoic (dark) signal (red arrow, Figure 1c) between the abdominal wall (red asterisk, Figure 1c) and bowel loops (letter ‘B,” Figure 1c). This finding confirmed the presence of ascites because simple fluid does not reflect the ultrasound beam, but instead results in the hypoechoic signal seen in Figure 1c. An additional sonographic image confirmed the presence of an enlarged liver (white asterisk, Figure 1d) and ascites in the right upper quadrant (red arrow, Figure 1d).
The patient was admitted for further workup and treatment of alcoholic cirrhosis. A
Dr Lyons is a resident in the department of radiology at New York Presbyterian Hospital/Weill Cornell Medical College in New York City. Dr Wladyka is an assistant professor of radiology at Weill Cornell Medical College in New York City and an assistant attending radiologist at NewYork-Presbyterian Hospital/Weill Cornell Medical Center. Dr Hentel is an associate professor of clinical radiology at Weill Cornell Medical College in New York City. He is also chief of emergency/musculoskeletal imaging and executive vice-chairman for the department of radiology at New York-
30-year-old woman with a history of alcoholism and anxiety presented to the ED for evaluation of abdominal distension and pain. She reported new social stressors at home and increased alcohol consumption. She also noted gradually increasing abdominal distension over the past several weeks. As patient’s liver function tests were elevated, supine radiographs of the abdomen were acquired for further evaluation; a representative image is presented below (Figure 1a).
What is the suspected diagnosis?
Is any additional imaging required?
Answer
Centralization of bowel is suggestive of abdominopelvic ascites.1 Additional radiographic findings that may be seen with ascites include diffusely increased density of the abdomen and bulging of the peritoneal fat stripes/flanks. In the average adult, a minimum of approximately 800 mL of ascitic fluid is required to medially displace bowel loops or abdominal viscera.2 While there are many causes of ascites, the radiograph in this case suggests the underlying etiology of cirrhosis. Although the top of the liver is not visualized on the radiograph, the liver contour appears enlarged (red arrow, Figure 1b).
In the ED, ultrasound is the imaging modality of choice to confirm the presence of ascites as it is widely available, quick, relatively inexpensive, and does not require ionizing radiation. Ultrasound is also useful when examining the abdominal viscera since it may detect the underlying cause of ascites.3 The ultrasound image of the abdominal viscera in this case demonstrated a hypoechoic (dark) signal (red arrow, Figure 1c) between the abdominal wall (red asterisk, Figure 1c) and bowel loops (letter ‘B,” Figure 1c). This finding confirmed the presence of ascites because simple fluid does not reflect the ultrasound beam, but instead results in the hypoechoic signal seen in Figure 1c. An additional sonographic image confirmed the presence of an enlarged liver (white asterisk, Figure 1d) and ascites in the right upper quadrant (red arrow, Figure 1d).
The patient was admitted for further workup and treatment of alcoholic cirrhosis. A
Dr Lyons is a resident in the department of radiology at New York Presbyterian Hospital/Weill Cornell Medical College in New York City. Dr Wladyka is an assistant professor of radiology at Weill Cornell Medical College in New York City and an assistant attending radiologist at NewYork-Presbyterian Hospital/Weill Cornell Medical Center. Dr Hentel is an associate professor of clinical radiology at Weill Cornell Medical College in New York City. He is also chief of emergency/musculoskeletal imaging and executive vice-chairman for the department of radiology at New York-
- Meschan I. Analysis of Roentgen Signs in General Radiology. Philadelphia, PA: Saunders; 1973:1231.
- Keeffee EJ, Gagliardi RA, Pfister RC. The roentgenographic evaluation of ascites. Am J Roentgenol. 1967;101(2):388-396.
- Goldberg BB, Goodman GA, Clearfield HR. Evaluation of ascites by ultrasound. Radiology. 1970;96(1):15-22.
- Meschan I. Analysis of Roentgen Signs in General Radiology. Philadelphia, PA: Saunders; 1973:1231.
- Keeffee EJ, Gagliardi RA, Pfister RC. The roentgenographic evaluation of ascites. Am J Roentgenol. 1967;101(2):388-396.
- Goldberg BB, Goodman GA, Clearfield HR. Evaluation of ascites by ultrasound. Radiology. 1970;96(1):15-22.
Emergency Imaging: Wrist injury in a woman with multiple sclerosis
Case
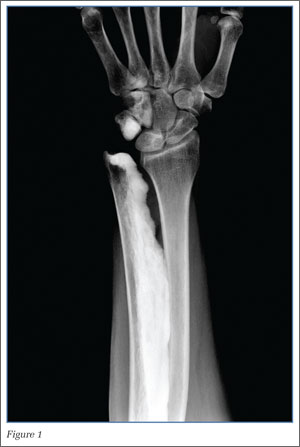
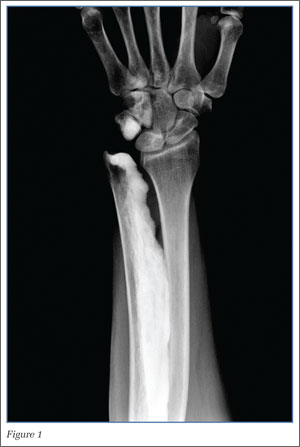
A 54-year-old woman with history of active multiple sclerosis (MS) presented to the ED with left wrist pain after sustaining a mechanical fall 9 days earlier. On physical examination, the patient had minimal left wrist swelling with circumferential tenderness to palpation at both the distal radius and distal ulna, as well as snuff-box tenderness. Posterioranterior and lateral radiographs of the wrist were obtained (Figures 1 and 2).
|
|
|
What is the diagnosis?
Radiographs of the left wrist demonstrated cortically based sclerosis of the ulna, triquetrum, and hamate; no fracture or dislocation was seen. This pattern of cortical bone formation, described as the “dripping candle wax” sign, is characteristic for melorheostosis, a rare nonhereditary mixed sclerosing bone dysplasia.
|
|
|
Sclerosing bone dysplasias include a wide range of both hereditary and nonhereditary skeletal abnormalities that result from a disturbance in the bone ossification pathway. These dysplasias can be categorized as disruptions in endochondral bone formation, disruptions in intramembranous bone formation, or mixed. First described by Leri and Joanny in 1922, there have been approximately 400 reported cases of melorheostosis since its initial identification.1,2
In melorheostosis, the distribution of lesions follows sclerotomes, skeletal regions supplied by a single spinal sensory nerve. The condition manifests as cortical and medullary hyperostosis involving one side of the bone (eg, medial or lateral) with a clear distinction between affected bone and the adjacent normal bone. As in this case, the radiographic appearance of melorheostosis is almost always sufficient for diagnosis.
Melorheostosis has no gender predilection and is usually diagnosed in late adolescence or early adulthood.5 While the etiology is unknown, genetic analyses have found a common loss-of-function mutation on chromosome 12q (LEMD3) associated with several sclerosing bone dysplasias, including melorheostosis, suggesting a common etiology.3 In addition, since melorheostosis typically has a sclerotomal distribution, some theories postulate that it represents an acquired defect of the spinal sensory nerves.1
Patients generally present with pain, stiffness, and occasionally joint swelling in the involved regions. Although any bone can be involved, the extremities are most often affected, with the disease frequently polyostotic, but rarely bilateral.4,5 In hyperostosis involving a joint, muscular atrophy, tendon and ligament shortening, and muscle contractures may be seen, which can limit range of motion.6 Some cases of leg-length discrepancy have also been described. Skeletal lesions may progress, but there is no reported risk of pathological fracture or malignant degeneration.7
Treatment is dependent on the patient’s age, location of involved bone, and specific symptoms. The major goals of treatment are pain relief and preserving or restoring full range of motion. Therapy is generally focused on conservative techniques such as analgesics, braces, and physical therapy. Occasionally, surgical treatment is necessary, including soft-tissue release, fasciotomy, tendon lengthening, and arthroplasty.8
In the ED setting, it is important to recognize melorheostosis as the source of pain as this condition may be confused with osseous neoplasm. Based on this patient’s underlying partially treated MS flare and the potential for recurring fall, admission was recommended for intravenous corticosteroids. The patient, however, was only amenable to a wrist splint and refused further treatment.
Dr Escalon is second-year postgraduate resident, the department of radiology, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Dr Loftus is an assistant professor of radiology, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Dr Hentel is an associate professor of clinical radiology, Weill Cornell Medical College in New York City. He is also chief of emergency/musculoskeletal imaging and executive vice-chairman for the department of radiology, New York-Presbyterian Hospital/Weill Cornell Medical Center. He is associate editor, imaging, of the EMERGENCY MEDICINE editorial board.
- Ihde LL, Forrester DM, Gottsegen CJ, Masih S, et al. Sclerosing bone dysplasias: review and differentiation from other causes of osteosclerosis. Radiographics. 2011;31(7):1865-1882.
- Suresh S, Muthukumar T, Saifuddin A. Classical and unusual imaging appearances of melorheostosis. Clin Radiol. 2010;65(8):593-600.
- Bansal A. The dripping candle wax sign. Radiology. 2008;246(2):638-640.
- Birtane M, Eryavuz M, Unalan H, Tüzün F. Melorheostosis: report of a new case with linear seleroderma. Clin Rheumatol. 1998;17(6):543-545.
- Siegel A, Williams H. Linear scleroderma and melorheostosis. Br J Radiol. 1992;65(771):266-268.
- Tekin L, Akarsu S, Durmuş O, Kiralp MZ. Melorheostosis in the hand and forearm. Am J Phys Med Rehabil. 2012;91(1):96.
- Soffa DJ, Sire DJ, Dodson JH. Melorheostosis with Linear Sclerodermatous Skin Changes. Radiology. 1975;114(3):577,578.
- Jain VK, Arya RK, Bharadwaj M, Kumar S. Melorheostosis: clinicopathological features, diagnosis, and management. Orthopedics. 2009;32(7):512
Case
A 54-year-old woman with history of active multiple sclerosis (MS) presented to the ED with left wrist pain after sustaining a mechanical fall 9 days earlier. On physical examination, the patient had minimal left wrist swelling with circumferential tenderness to palpation at both the distal radius and distal ulna, as well as snuff-box tenderness. Posterioranterior and lateral radiographs of the wrist were obtained (Figures 1 and 2).
|
|
|
What is the diagnosis?
Radiographs of the left wrist demonstrated cortically based sclerosis of the ulna, triquetrum, and hamate; no fracture or dislocation was seen. This pattern of cortical bone formation, described as the “dripping candle wax” sign, is characteristic for melorheostosis, a rare nonhereditary mixed sclerosing bone dysplasia.
|
|
|
Sclerosing bone dysplasias include a wide range of both hereditary and nonhereditary skeletal abnormalities that result from a disturbance in the bone ossification pathway. These dysplasias can be categorized as disruptions in endochondral bone formation, disruptions in intramembranous bone formation, or mixed. First described by Leri and Joanny in 1922, there have been approximately 400 reported cases of melorheostosis since its initial identification.1,2
In melorheostosis, the distribution of lesions follows sclerotomes, skeletal regions supplied by a single spinal sensory nerve. The condition manifests as cortical and medullary hyperostosis involving one side of the bone (eg, medial or lateral) with a clear distinction between affected bone and the adjacent normal bone. As in this case, the radiographic appearance of melorheostosis is almost always sufficient for diagnosis.
Melorheostosis has no gender predilection and is usually diagnosed in late adolescence or early adulthood.5 While the etiology is unknown, genetic analyses have found a common loss-of-function mutation on chromosome 12q (LEMD3) associated with several sclerosing bone dysplasias, including melorheostosis, suggesting a common etiology.3 In addition, since melorheostosis typically has a sclerotomal distribution, some theories postulate that it represents an acquired defect of the spinal sensory nerves.1
Patients generally present with pain, stiffness, and occasionally joint swelling in the involved regions. Although any bone can be involved, the extremities are most often affected, with the disease frequently polyostotic, but rarely bilateral.4,5 In hyperostosis involving a joint, muscular atrophy, tendon and ligament shortening, and muscle contractures may be seen, which can limit range of motion.6 Some cases of leg-length discrepancy have also been described. Skeletal lesions may progress, but there is no reported risk of pathological fracture or malignant degeneration.7
Treatment is dependent on the patient’s age, location of involved bone, and specific symptoms. The major goals of treatment are pain relief and preserving or restoring full range of motion. Therapy is generally focused on conservative techniques such as analgesics, braces, and physical therapy. Occasionally, surgical treatment is necessary, including soft-tissue release, fasciotomy, tendon lengthening, and arthroplasty.8
In the ED setting, it is important to recognize melorheostosis as the source of pain as this condition may be confused with osseous neoplasm. Based on this patient’s underlying partially treated MS flare and the potential for recurring fall, admission was recommended for intravenous corticosteroids. The patient, however, was only amenable to a wrist splint and refused further treatment.
Dr Escalon is second-year postgraduate resident, the department of radiology, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Dr Loftus is an assistant professor of radiology, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Dr Hentel is an associate professor of clinical radiology, Weill Cornell Medical College in New York City. He is also chief of emergency/musculoskeletal imaging and executive vice-chairman for the department of radiology, New York-Presbyterian Hospital/Weill Cornell Medical Center. He is associate editor, imaging, of the EMERGENCY MEDICINE editorial board.
Case
A 54-year-old woman with history of active multiple sclerosis (MS) presented to the ED with left wrist pain after sustaining a mechanical fall 9 days earlier. On physical examination, the patient had minimal left wrist swelling with circumferential tenderness to palpation at both the distal radius and distal ulna, as well as snuff-box tenderness. Posterioranterior and lateral radiographs of the wrist were obtained (Figures 1 and 2).
|
|
|
What is the diagnosis?
Radiographs of the left wrist demonstrated cortically based sclerosis of the ulna, triquetrum, and hamate; no fracture or dislocation was seen. This pattern of cortical bone formation, described as the “dripping candle wax” sign, is characteristic for melorheostosis, a rare nonhereditary mixed sclerosing bone dysplasia.
|
|
|
Sclerosing bone dysplasias include a wide range of both hereditary and nonhereditary skeletal abnormalities that result from a disturbance in the bone ossification pathway. These dysplasias can be categorized as disruptions in endochondral bone formation, disruptions in intramembranous bone formation, or mixed. First described by Leri and Joanny in 1922, there have been approximately 400 reported cases of melorheostosis since its initial identification.1,2
In melorheostosis, the distribution of lesions follows sclerotomes, skeletal regions supplied by a single spinal sensory nerve. The condition manifests as cortical and medullary hyperostosis involving one side of the bone (eg, medial or lateral) with a clear distinction between affected bone and the adjacent normal bone. As in this case, the radiographic appearance of melorheostosis is almost always sufficient for diagnosis.
Melorheostosis has no gender predilection and is usually diagnosed in late adolescence or early adulthood.5 While the etiology is unknown, genetic analyses have found a common loss-of-function mutation on chromosome 12q (LEMD3) associated with several sclerosing bone dysplasias, including melorheostosis, suggesting a common etiology.3 In addition, since melorheostosis typically has a sclerotomal distribution, some theories postulate that it represents an acquired defect of the spinal sensory nerves.1
Patients generally present with pain, stiffness, and occasionally joint swelling in the involved regions. Although any bone can be involved, the extremities are most often affected, with the disease frequently polyostotic, but rarely bilateral.4,5 In hyperostosis involving a joint, muscular atrophy, tendon and ligament shortening, and muscle contractures may be seen, which can limit range of motion.6 Some cases of leg-length discrepancy have also been described. Skeletal lesions may progress, but there is no reported risk of pathological fracture or malignant degeneration.7
Treatment is dependent on the patient’s age, location of involved bone, and specific symptoms. The major goals of treatment are pain relief and preserving or restoring full range of motion. Therapy is generally focused on conservative techniques such as analgesics, braces, and physical therapy. Occasionally, surgical treatment is necessary, including soft-tissue release, fasciotomy, tendon lengthening, and arthroplasty.8
In the ED setting, it is important to recognize melorheostosis as the source of pain as this condition may be confused with osseous neoplasm. Based on this patient’s underlying partially treated MS flare and the potential for recurring fall, admission was recommended for intravenous corticosteroids. The patient, however, was only amenable to a wrist splint and refused further treatment.
Dr Escalon is second-year postgraduate resident, the department of radiology, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Dr Loftus is an assistant professor of radiology, New York-Presbyterian Hospital/Weill Cornell Medical College, New York.
Dr Hentel is an associate professor of clinical radiology, Weill Cornell Medical College in New York City. He is also chief of emergency/musculoskeletal imaging and executive vice-chairman for the department of radiology, New York-Presbyterian Hospital/Weill Cornell Medical Center. He is associate editor, imaging, of the EMERGENCY MEDICINE editorial board.
- Ihde LL, Forrester DM, Gottsegen CJ, Masih S, et al. Sclerosing bone dysplasias: review and differentiation from other causes of osteosclerosis. Radiographics. 2011;31(7):1865-1882.
- Suresh S, Muthukumar T, Saifuddin A. Classical and unusual imaging appearances of melorheostosis. Clin Radiol. 2010;65(8):593-600.
- Bansal A. The dripping candle wax sign. Radiology. 2008;246(2):638-640.
- Birtane M, Eryavuz M, Unalan H, Tüzün F. Melorheostosis: report of a new case with linear seleroderma. Clin Rheumatol. 1998;17(6):543-545.
- Siegel A, Williams H. Linear scleroderma and melorheostosis. Br J Radiol. 1992;65(771):266-268.
- Tekin L, Akarsu S, Durmuş O, Kiralp MZ. Melorheostosis in the hand and forearm. Am J Phys Med Rehabil. 2012;91(1):96.
- Soffa DJ, Sire DJ, Dodson JH. Melorheostosis with Linear Sclerodermatous Skin Changes. Radiology. 1975;114(3):577,578.
- Jain VK, Arya RK, Bharadwaj M, Kumar S. Melorheostosis: clinicopathological features, diagnosis, and management. Orthopedics. 2009;32(7):512
- Ihde LL, Forrester DM, Gottsegen CJ, Masih S, et al. Sclerosing bone dysplasias: review and differentiation from other causes of osteosclerosis. Radiographics. 2011;31(7):1865-1882.
- Suresh S, Muthukumar T, Saifuddin A. Classical and unusual imaging appearances of melorheostosis. Clin Radiol. 2010;65(8):593-600.
- Bansal A. The dripping candle wax sign. Radiology. 2008;246(2):638-640.
- Birtane M, Eryavuz M, Unalan H, Tüzün F. Melorheostosis: report of a new case with linear seleroderma. Clin Rheumatol. 1998;17(6):543-545.
- Siegel A, Williams H. Linear scleroderma and melorheostosis. Br J Radiol. 1992;65(771):266-268.
- Tekin L, Akarsu S, Durmuş O, Kiralp MZ. Melorheostosis in the hand and forearm. Am J Phys Med Rehabil. 2012;91(1):96.
- Soffa DJ, Sire DJ, Dodson JH. Melorheostosis with Linear Sclerodermatous Skin Changes. Radiology. 1975;114(3):577,578.
- Jain VK, Arya RK, Bharadwaj M, Kumar S. Melorheostosis: clinicopathological features, diagnosis, and management. Orthopedics. 2009;32(7):512