User login
A-fib and rate control: Don’t go too low
Aim for a heart rate of <110 beats per minute (bpm) in patients with permanent atrial fibrillation. Maintaining this rate requires less medication than more stringent rate control, resulting in fewer side effects and no increased risk of cardiovascular events.1
STRENGTH OF RECOMMENDATION
B: Based on 1 long-term randomized controlled trial (RCT).
Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362: 1363-1373.
Illustrative case
A 67-year-old man comes in for a follow-up visit after being hospitalized for atrial fibrillation with a rapid ventricular rate. Before being discharged, he was put on warfarin and metoprolol, and his heart rate today is 96 bpm. You consider increasing the dose of his beta-blocker. What should his target heart rate be?
Atrial fibrillation, the most common sustained arrhythmia,2 can lead to life-threatening events such as heart failure and stroke. Studies, including the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) and Rate Control versus Electrical Cardioversion (RACE) trials, have found no difference in morbidity or mortality between rate control and rhythm control strategies.2,3 Thus, rate control is usually preferred for patients with atrial fibrillation because of adverse effects associated with antiarrhythmic drugs.
Guidelines cite stringent targets
The American College of Cardiology/American Heart Association Task Force/European Society of Cardiology (ACC/AHA/ESC) guidelines make no definite recommendations about heart rate targets. The guidelines do indicate, however, that rate control criteria vary based on age, “but usually involve achieving ventricular rates between 60 and 80 [bpm] at rest and between 90 and 115 [bpm] during moderate exercise.”4
This guidance is based on data from epidemiologic studies suggesting that faster heart rates in sinus rhythm may increase mortality from cardiovascular causes.5 However, strict control often requires higher doses of rate-controlling medications, which can lead to adverse events such as symptomatic bradycardia, dizziness, and syncope, as well as pacemaker implantation.
Pooled data suggest a more relaxed rate is better
A retrospective analysis of pooled data from the rate-control arms of the AFFIRM and RACE trials found no difference in all-cause mortality between the more stringent rate-control group in AFFIRM and the more lenient control in RACE.6 This finding suggested that more lenient heart rate targets may be preferred to avoid the adverse effects often associated with the higher doses of rate-controlling drugs needed to achieve strict control. The Rate Control Efficacy in Permanent Atrial Fibrillation: a Comparison between Lenient versus Strict Rate Control II (RACE II) study we report on here provides strong evidence in favor of lenient rate control.
STUDY SUMMARY: Lenient control is as effective, easier to achieve
RACE II was the first RCT to directly compare lenient rate control (resting heart rate <110 bpm) with strict rate control (resting heart rate <80 bpm, and <110 bpm during moderate exercise). This prospective, multi-center study in Holland randomized patients with permanent atrial fibrillation (N=614) to either a lenient or strict rate-control group. Eligibility criteria were (1) permanent atrial fibrillation for up to 12 months; (2) ≤80 years of age (3) mean resting heart rate >80 bpm; and (4) current use of oral anticoagulation therapy (or aspirin, in the absence of risk factors for thromboembolic complications).
Patients received various doses of beta-blockers, nondihydropyridine calcium-channel blockers, or digoxin, singly or in combination as needed to reach the target heart rate. In both groups, the resting heart rate was determined by 12-lead electrocardiogram after the patient remained in a supine position for 2 to 3 minutes. In the strict-control group, heart rate was also measured during moderate exercise on a stationary bicycle after the resting rate goal had been achieved. In addition, patients in the strict-control group wore a Holter monitor for 24 hours to check for bradycardia.
Participants in both groups were seen every 2 weeks until their heart rate goals were achieved, with follow-up at 1, 2, and 3 years. The primary composite outcome included death from cardiovascular causes; hospitalization for heart failure, stroke, systemic embolism, major bleeding, or life-threatening adverse effects of rate-control drugs; arrhythmic events, including sustained ventricular tachycardia, syncope, or cardiac arrest; and implantation of a pacemaker or cardioverter-defibrillator.
At the end of 3 years, the estimated cumulative incidence of the primary outcome was 12.9% in the lenient-control group vs 14.9% in the strict-control group. The absolute difference was -2.0 (90% confidence interval [CI], -7.6 to 3.5); a 90% CI was acceptable because the study only tested whether lenient control was worse than strict control. The frequency of reported symptoms and adverse events was similar between the 2 groups, but the lenient-control group had fewer visits for rate control (75 vs 684; P<.001), required fewer medications, and took lower doses of some medications.
Heart rate targets were met in 97.7% of patients in the lenient-control group, compared with 67% in the strict-control group (P<.001). Of those not meeting the strict control targets, 25% were due to an adverse medication event. There were no differences between the 2 groups in symptoms or in New York Heart Association functional class status.
WHAT'S NEW: Now we know: It doesn’t pay to go too low
A heart rate <80 at rest and <110 during exercise is difficult to maintain. This more stringent target often requires high dosages of drugs and/or multiple medications, which may lead to adverse effects. This RCT—the first to compare outcomes in patients with lenient vs strict heart rate control—found that morbidity and mortality were similar between the 2 groups. This means that, in many cases, patients will need less medication—leading to a reduction in risk of side effects and interactions.
CAVEATS: Unblinded study excluded very old, high risk
This was not a blinded study, so both patients and providers knew the target heart rates. However, the major outcomes were determined with relative objectivity and were not different between the 2 groups, so it is unlikely that this knowledge would have a major effect on the results. Nonetheless, this is a single study, and the findings are not yet supported by other large, prospective studies.
The researchers did not enroll patients >80 years, who have a higher incidence of atrial fibrillation and are less likely than younger patients to tolerate higher doses of rate-controlling medications. Also excluded were sedentary patients and those with a history of stroke, which resulted in a lower-risk study population. However, 40% of the subjects had a CHADS score ≥2 (an indication of high risk of stroke in patients with atrial fibrillation), and subgroup analysis found that the results applied to higher-risk groups.
Finally, it is possible that it may take longer than 3 years (the duration of study follow-up) for higher ventricular rates to result in adverse cardiovascular outcomes and that there could be a benefit of strict rate control over a longer period of time.
CHALLENGES TO IMPLEMENTATION: Guidelines do not reflect these findings
These findings are not yet incorporated into the ACC/AHA/ESC guidelines or those issued by other organizations. Clinical inertia may stop some physicians from reducing medications for patients with atrial fibrillation, but in general, both doctors and patients should welcome an easing of the drug burden.
Click here to view PURL METHODOLOGY
1. Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362:1363-1373.
2. Wyse DG, Waldo AL, DiMarco JP, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347:1825-1833.
3. Hagens VE, Ranchor AV, Van SE, et al. Effect of rate or rhythm control on quality of life in persistent atrial fibrillation. Results from the Rate Control Versus Electrical Cardioversion (RACE) Study. J Am Coll Cardiol. 2004;43:241-247.
4. Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e257-e354.
5. Dorian P. Rate control in atrial fibrillation. N Engl J Med. 2010;362:1439-1441.
6. Van Gelder IC, Wyse DG, Chandler ML, et al. Does intensity of rate-control influence outcome in atrial fibrillation? An analysis of pooled data from the RACE and AFFIRM studies. Europace. 2006;8:935-942.
Aim for a heart rate of <110 beats per minute (bpm) in patients with permanent atrial fibrillation. Maintaining this rate requires less medication than more stringent rate control, resulting in fewer side effects and no increased risk of cardiovascular events.1
STRENGTH OF RECOMMENDATION
B: Based on 1 long-term randomized controlled trial (RCT).
Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362: 1363-1373.
Illustrative case
A 67-year-old man comes in for a follow-up visit after being hospitalized for atrial fibrillation with a rapid ventricular rate. Before being discharged, he was put on warfarin and metoprolol, and his heart rate today is 96 bpm. You consider increasing the dose of his beta-blocker. What should his target heart rate be?
Atrial fibrillation, the most common sustained arrhythmia,2 can lead to life-threatening events such as heart failure and stroke. Studies, including the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) and Rate Control versus Electrical Cardioversion (RACE) trials, have found no difference in morbidity or mortality between rate control and rhythm control strategies.2,3 Thus, rate control is usually preferred for patients with atrial fibrillation because of adverse effects associated with antiarrhythmic drugs.
Guidelines cite stringent targets
The American College of Cardiology/American Heart Association Task Force/European Society of Cardiology (ACC/AHA/ESC) guidelines make no definite recommendations about heart rate targets. The guidelines do indicate, however, that rate control criteria vary based on age, “but usually involve achieving ventricular rates between 60 and 80 [bpm] at rest and between 90 and 115 [bpm] during moderate exercise.”4
This guidance is based on data from epidemiologic studies suggesting that faster heart rates in sinus rhythm may increase mortality from cardiovascular causes.5 However, strict control often requires higher doses of rate-controlling medications, which can lead to adverse events such as symptomatic bradycardia, dizziness, and syncope, as well as pacemaker implantation.
Pooled data suggest a more relaxed rate is better
A retrospective analysis of pooled data from the rate-control arms of the AFFIRM and RACE trials found no difference in all-cause mortality between the more stringent rate-control group in AFFIRM and the more lenient control in RACE.6 This finding suggested that more lenient heart rate targets may be preferred to avoid the adverse effects often associated with the higher doses of rate-controlling drugs needed to achieve strict control. The Rate Control Efficacy in Permanent Atrial Fibrillation: a Comparison between Lenient versus Strict Rate Control II (RACE II) study we report on here provides strong evidence in favor of lenient rate control.
STUDY SUMMARY: Lenient control is as effective, easier to achieve
RACE II was the first RCT to directly compare lenient rate control (resting heart rate <110 bpm) with strict rate control (resting heart rate <80 bpm, and <110 bpm during moderate exercise). This prospective, multi-center study in Holland randomized patients with permanent atrial fibrillation (N=614) to either a lenient or strict rate-control group. Eligibility criteria were (1) permanent atrial fibrillation for up to 12 months; (2) ≤80 years of age (3) mean resting heart rate >80 bpm; and (4) current use of oral anticoagulation therapy (or aspirin, in the absence of risk factors for thromboembolic complications).
Patients received various doses of beta-blockers, nondihydropyridine calcium-channel blockers, or digoxin, singly or in combination as needed to reach the target heart rate. In both groups, the resting heart rate was determined by 12-lead electrocardiogram after the patient remained in a supine position for 2 to 3 minutes. In the strict-control group, heart rate was also measured during moderate exercise on a stationary bicycle after the resting rate goal had been achieved. In addition, patients in the strict-control group wore a Holter monitor for 24 hours to check for bradycardia.
Participants in both groups were seen every 2 weeks until their heart rate goals were achieved, with follow-up at 1, 2, and 3 years. The primary composite outcome included death from cardiovascular causes; hospitalization for heart failure, stroke, systemic embolism, major bleeding, or life-threatening adverse effects of rate-control drugs; arrhythmic events, including sustained ventricular tachycardia, syncope, or cardiac arrest; and implantation of a pacemaker or cardioverter-defibrillator.
At the end of 3 years, the estimated cumulative incidence of the primary outcome was 12.9% in the lenient-control group vs 14.9% in the strict-control group. The absolute difference was -2.0 (90% confidence interval [CI], -7.6 to 3.5); a 90% CI was acceptable because the study only tested whether lenient control was worse than strict control. The frequency of reported symptoms and adverse events was similar between the 2 groups, but the lenient-control group had fewer visits for rate control (75 vs 684; P<.001), required fewer medications, and took lower doses of some medications.
Heart rate targets were met in 97.7% of patients in the lenient-control group, compared with 67% in the strict-control group (P<.001). Of those not meeting the strict control targets, 25% were due to an adverse medication event. There were no differences between the 2 groups in symptoms or in New York Heart Association functional class status.
WHAT'S NEW: Now we know: It doesn’t pay to go too low
A heart rate <80 at rest and <110 during exercise is difficult to maintain. This more stringent target often requires high dosages of drugs and/or multiple medications, which may lead to adverse effects. This RCT—the first to compare outcomes in patients with lenient vs strict heart rate control—found that morbidity and mortality were similar between the 2 groups. This means that, in many cases, patients will need less medication—leading to a reduction in risk of side effects and interactions.
CAVEATS: Unblinded study excluded very old, high risk
This was not a blinded study, so both patients and providers knew the target heart rates. However, the major outcomes were determined with relative objectivity and were not different between the 2 groups, so it is unlikely that this knowledge would have a major effect on the results. Nonetheless, this is a single study, and the findings are not yet supported by other large, prospective studies.
The researchers did not enroll patients >80 years, who have a higher incidence of atrial fibrillation and are less likely than younger patients to tolerate higher doses of rate-controlling medications. Also excluded were sedentary patients and those with a history of stroke, which resulted in a lower-risk study population. However, 40% of the subjects had a CHADS score ≥2 (an indication of high risk of stroke in patients with atrial fibrillation), and subgroup analysis found that the results applied to higher-risk groups.
Finally, it is possible that it may take longer than 3 years (the duration of study follow-up) for higher ventricular rates to result in adverse cardiovascular outcomes and that there could be a benefit of strict rate control over a longer period of time.
CHALLENGES TO IMPLEMENTATION: Guidelines do not reflect these findings
These findings are not yet incorporated into the ACC/AHA/ESC guidelines or those issued by other organizations. Clinical inertia may stop some physicians from reducing medications for patients with atrial fibrillation, but in general, both doctors and patients should welcome an easing of the drug burden.
Click here to view PURL METHODOLOGY
Aim for a heart rate of <110 beats per minute (bpm) in patients with permanent atrial fibrillation. Maintaining this rate requires less medication than more stringent rate control, resulting in fewer side effects and no increased risk of cardiovascular events.1
STRENGTH OF RECOMMENDATION
B: Based on 1 long-term randomized controlled trial (RCT).
Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362: 1363-1373.
Illustrative case
A 67-year-old man comes in for a follow-up visit after being hospitalized for atrial fibrillation with a rapid ventricular rate. Before being discharged, he was put on warfarin and metoprolol, and his heart rate today is 96 bpm. You consider increasing the dose of his beta-blocker. What should his target heart rate be?
Atrial fibrillation, the most common sustained arrhythmia,2 can lead to life-threatening events such as heart failure and stroke. Studies, including the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) and Rate Control versus Electrical Cardioversion (RACE) trials, have found no difference in morbidity or mortality between rate control and rhythm control strategies.2,3 Thus, rate control is usually preferred for patients with atrial fibrillation because of adverse effects associated with antiarrhythmic drugs.
Guidelines cite stringent targets
The American College of Cardiology/American Heart Association Task Force/European Society of Cardiology (ACC/AHA/ESC) guidelines make no definite recommendations about heart rate targets. The guidelines do indicate, however, that rate control criteria vary based on age, “but usually involve achieving ventricular rates between 60 and 80 [bpm] at rest and between 90 and 115 [bpm] during moderate exercise.”4
This guidance is based on data from epidemiologic studies suggesting that faster heart rates in sinus rhythm may increase mortality from cardiovascular causes.5 However, strict control often requires higher doses of rate-controlling medications, which can lead to adverse events such as symptomatic bradycardia, dizziness, and syncope, as well as pacemaker implantation.
Pooled data suggest a more relaxed rate is better
A retrospective analysis of pooled data from the rate-control arms of the AFFIRM and RACE trials found no difference in all-cause mortality between the more stringent rate-control group in AFFIRM and the more lenient control in RACE.6 This finding suggested that more lenient heart rate targets may be preferred to avoid the adverse effects often associated with the higher doses of rate-controlling drugs needed to achieve strict control. The Rate Control Efficacy in Permanent Atrial Fibrillation: a Comparison between Lenient versus Strict Rate Control II (RACE II) study we report on here provides strong evidence in favor of lenient rate control.
STUDY SUMMARY: Lenient control is as effective, easier to achieve
RACE II was the first RCT to directly compare lenient rate control (resting heart rate <110 bpm) with strict rate control (resting heart rate <80 bpm, and <110 bpm during moderate exercise). This prospective, multi-center study in Holland randomized patients with permanent atrial fibrillation (N=614) to either a lenient or strict rate-control group. Eligibility criteria were (1) permanent atrial fibrillation for up to 12 months; (2) ≤80 years of age (3) mean resting heart rate >80 bpm; and (4) current use of oral anticoagulation therapy (or aspirin, in the absence of risk factors for thromboembolic complications).
Patients received various doses of beta-blockers, nondihydropyridine calcium-channel blockers, or digoxin, singly or in combination as needed to reach the target heart rate. In both groups, the resting heart rate was determined by 12-lead electrocardiogram after the patient remained in a supine position for 2 to 3 minutes. In the strict-control group, heart rate was also measured during moderate exercise on a stationary bicycle after the resting rate goal had been achieved. In addition, patients in the strict-control group wore a Holter monitor for 24 hours to check for bradycardia.
Participants in both groups were seen every 2 weeks until their heart rate goals were achieved, with follow-up at 1, 2, and 3 years. The primary composite outcome included death from cardiovascular causes; hospitalization for heart failure, stroke, systemic embolism, major bleeding, or life-threatening adverse effects of rate-control drugs; arrhythmic events, including sustained ventricular tachycardia, syncope, or cardiac arrest; and implantation of a pacemaker or cardioverter-defibrillator.
At the end of 3 years, the estimated cumulative incidence of the primary outcome was 12.9% in the lenient-control group vs 14.9% in the strict-control group. The absolute difference was -2.0 (90% confidence interval [CI], -7.6 to 3.5); a 90% CI was acceptable because the study only tested whether lenient control was worse than strict control. The frequency of reported symptoms and adverse events was similar between the 2 groups, but the lenient-control group had fewer visits for rate control (75 vs 684; P<.001), required fewer medications, and took lower doses of some medications.
Heart rate targets were met in 97.7% of patients in the lenient-control group, compared with 67% in the strict-control group (P<.001). Of those not meeting the strict control targets, 25% were due to an adverse medication event. There were no differences between the 2 groups in symptoms or in New York Heart Association functional class status.
WHAT'S NEW: Now we know: It doesn’t pay to go too low
A heart rate <80 at rest and <110 during exercise is difficult to maintain. This more stringent target often requires high dosages of drugs and/or multiple medications, which may lead to adverse effects. This RCT—the first to compare outcomes in patients with lenient vs strict heart rate control—found that morbidity and mortality were similar between the 2 groups. This means that, in many cases, patients will need less medication—leading to a reduction in risk of side effects and interactions.
CAVEATS: Unblinded study excluded very old, high risk
This was not a blinded study, so both patients and providers knew the target heart rates. However, the major outcomes were determined with relative objectivity and were not different between the 2 groups, so it is unlikely that this knowledge would have a major effect on the results. Nonetheless, this is a single study, and the findings are not yet supported by other large, prospective studies.
The researchers did not enroll patients >80 years, who have a higher incidence of atrial fibrillation and are less likely than younger patients to tolerate higher doses of rate-controlling medications. Also excluded were sedentary patients and those with a history of stroke, which resulted in a lower-risk study population. However, 40% of the subjects had a CHADS score ≥2 (an indication of high risk of stroke in patients with atrial fibrillation), and subgroup analysis found that the results applied to higher-risk groups.
Finally, it is possible that it may take longer than 3 years (the duration of study follow-up) for higher ventricular rates to result in adverse cardiovascular outcomes and that there could be a benefit of strict rate control over a longer period of time.
CHALLENGES TO IMPLEMENTATION: Guidelines do not reflect these findings
These findings are not yet incorporated into the ACC/AHA/ESC guidelines or those issued by other organizations. Clinical inertia may stop some physicians from reducing medications for patients with atrial fibrillation, but in general, both doctors and patients should welcome an easing of the drug burden.
Click here to view PURL METHODOLOGY
1. Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362:1363-1373.
2. Wyse DG, Waldo AL, DiMarco JP, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347:1825-1833.
3. Hagens VE, Ranchor AV, Van SE, et al. Effect of rate or rhythm control on quality of life in persistent atrial fibrillation. Results from the Rate Control Versus Electrical Cardioversion (RACE) Study. J Am Coll Cardiol. 2004;43:241-247.
4. Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e257-e354.
5. Dorian P. Rate control in atrial fibrillation. N Engl J Med. 2010;362:1439-1441.
6. Van Gelder IC, Wyse DG, Chandler ML, et al. Does intensity of rate-control influence outcome in atrial fibrillation? An analysis of pooled data from the RACE and AFFIRM studies. Europace. 2006;8:935-942.
1. Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010;362:1363-1373.
2. Wyse DG, Waldo AL, DiMarco JP, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347:1825-1833.
3. Hagens VE, Ranchor AV, Van SE, et al. Effect of rate or rhythm control on quality of life in persistent atrial fibrillation. Results from the Rate Control Versus Electrical Cardioversion (RACE) Study. J Am Coll Cardiol. 2004;43:241-247.
4. Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e257-e354.
5. Dorian P. Rate control in atrial fibrillation. N Engl J Med. 2010;362:1439-1441.
6. Van Gelder IC, Wyse DG, Chandler ML, et al. Does intensity of rate-control influence outcome in atrial fibrillation? An analysis of pooled data from the RACE and AFFIRM studies. Europace. 2006;8:935-942.
Copyright © 2010 The Family Physicians Inquiries Network. All rights reserved.
Help smokers quit: Tell them their “lung age”
ILLUSTRATIVE CASE
A 48-year-old man comes to your office for a routine physical. He has a 30 pack-year smoking history. When you talk to him about smoking cessation, he tells you he’s tried to stop more than once, but he can’t seem to stay motivated. You find no evidence of chronic lung disease and do not perform spirometry screening. (The US Preventive Services Task Force does not recommend spirometry for asymptomatic patients.) But could spirometry have therapeutic value in this case?
Smoking is the leading modifiable risk factor for mortality in the United States,2 and smoking cessation is the most effective intervention. Nortriptyline, bupropion, nicotine replacement agents, and varenicline are effective pharmacological treatments.3 Adding counseling to medication significantly improves quit rates (estimated odds ratio [OR]=1.4; 95% confidence interval [CI], 1.2-1.6).3 Nonetheless, physicians’ efforts to help patients stop smoking frequently fail.
But another option has caught—and held—the attention of researchers.
The promise of biomarkers
It has long been suspected that presenting smokers with evidence of tobacco’s harmful effect on their bodies—biomarkers—might encourage them to stop. Biomarkers that have been tested in randomized controlled trials (RCTs) include spirometry, exhaled carbon monoxide measurement, ultrasonography of carotid and femoral arteries, and genetic susceptibility to lung cancer, as well as combinations of these markers. But the results of most biomarker studies have been disappointing. A 2005 Cochrane Database review found insufficient evidence of the effectiveness of these markers in boosting quit rates.4
Lung age, a biomarker that’s easily understood
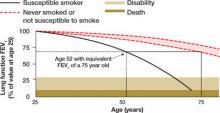
Lung age, a clever presentation of spirometry results, had not been tested in an RCT prior to the study we summarize below. Defined in 1985, lung age refers to the average age of a nonsmoker with a forced expiratory volume at 1 second (FEV1) equal to that of the person being tested ( FIGURE 1 ). The primary purpose was to make spirometry results easier for patients to understand, but researchers also envisioned it as a way to demonstrate the premature lung damage suffered as a consequence of smoking.5
FIGURE 1
Translating FEV1 into lung age1
STUDY SUMMARY: Graphic display more effective than FEV1 results
This study was a well-done, multicenter RCT evaluating the effect on tobacco quit rates of informing adult smokers of their lung age.1 Smokers ages 35 and older from 5 general practices in England were invited to participate. The authors excluded patients using oxygen and those with a history of tuberculosis, lung cancer, asbestosis, bronchiectasis, silicosis, or pneumonectomy. The study included 561 participants with an average of 33 pack-years of smoking, who underwent spirometry before being divided into an intervention or a control group. The researchers used standardized instruments to confirm the baseline comparability of the 2 groups.
Subjects in both groups were given information about local smoking cessation clinics and strongly encouraged to quit. All were told that their lung function would be retested in 12 months.
The controls received letters with their spirometry results presented as FEV1. In contrast, participants in the intervention group received the results in the form of a computer-generated graphic display of lung age ( FIGURE 2 ), which was further explained by a health care worker. They also received a letter within 1 month containing the same data. Participants were evaluated for smoking cessation at 12 months, and those who reported quitting received confirmatory carbon monoxide breath testing and salivary cotinine testing. Eleven percent of the subjects were lost to follow-up.
FIGURE 2
Lung age helps spirometry pack a bigger punch
Drawing a vertical line from the patient’s age (on the horizontal axis) to reach the solid curve representing the lung function of the “susceptible smoker” and extending the line horizontally to reach the curve with the broken lines representing “never smokers” graphically shows the patient’s lung age and the accelerated decline in lung function associated with smoking. The patient shown here is a 52-year-old smoker with FEV1 equivalent to a 75-year-old nonsmoker.
Source: Parkes G et al. BMJ. 2008;336:598-600. Reproduced with permission from the BMJ Publishing Group.
Quit rates higher when patients know lung age
At 1 year, verified quit rates were 13.6% in the intervention group and 6.4% in the control group (a difference of 7.2%, 95% CI, 2.2%-12.1%; P=.005). This means that for every 14 smokers who are told their lung age and shown a graphic display of this biomarker, 1 additional smoker will quit after 1 year.
Contrary to what might be expected, the investigators found that quitting did not depend on the degree of lung damage. Patients with both normal and abnormal lung age quit smoking at similar rates.
WHAT’S NEW: Lung age resonates more than spirometry alone
This is the first RCT demonstrating that informing smokers of their lung age can help them quit, and the first well-designed study to demonstrate improved cessation rates using a physiological biomarker. The research also suggests that successful quitting may have less to do with spirometry results—the level of severity of lung damage it shows—than with the way the results are presented. Giving patients information about their lung function in an easily understandable format, the authors observe, appears to result in higher quit rates.
CAVEATS: Young smokers weren’t studied
The study did not test to see if this intervention would work in younger adults, as only those 35 years of age and older were enrolled. This is a single study, and it is possible that the findings cannot be generalized to other groups or are due to unmeasured confounding factors. However, the intervention is unlikely to cause any significant harm, so we see no risks associated with it other than the cost of spirometry.
CHALLENGES TO IMPLEMENTATION: Time and expense of spirometry
We suspect the biggest challenges to implementing this recommendation in clinical practice are the expense of obtaining a spirometer ( TABLE ), staff training for those practices without one, and the time needed for the intervention. The average time to perform spirometry on study participants was 30 minutes; a health care worker spent, on average, another 15 minutes reviewing results with each member of the intervention group.
Another challenge: Not all spirometers calculate lung age or can create a graphic similar to FIGURE 2 . However, any FEV1 measurement, whether it is generated by formal pulmonary function testing or by an inexpensive hand-held meter, can easily be converted to lung age using the formula shown in FIGURE 1 . If desired, the same elements—the patient’s age, height, and gender as well as FEV1—could also be used to create a computer-generated graphic display.
TABLE
Spirometry: equipment costs
| The initial cost of a spirometer varies widely, depending on the sophistication of the equipment and the available options and features. Additional costs—for disposable mouthpieces, line filters, nose clips, and hoses, for example—are low. A sampling of reasonably priced models well suited for office use is shown below. All of these models meet American Thoracic Society criteria for spirometry, and all calculate lung age. | ||
|---|---|---|
| SPIROMETER MANUFACTURER/MODEL | PRICE | SUPPLIER |
| Futuremed Discovery-2 | $2,125 | medsupplier.com |
| Micro Medical MicroLoop | $1,780 | Miami-med.com |
| Micro Medical SpiroUSB | $1,580 | Miami-med.com |
| NDD EasyOne Frontline | $1,000 | medsupplier.com |
| SDI Diagnostics Spirolab II | $2,600 | med-electronics.com |
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
PURL METHODOLOGY
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Parkes G, Greenhalgh T, Griffin M, Dent R. Effect on smoking quit rate of telling patients their lung age: the Step2quit randomised controlled trial. BMJ. 2008;336:598-600.
2. Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238-1245.
3. Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical practice guideline. Rockville, MD: US Department of Health and Human Services, Public Health Service; May 2008. Available at: http://www.surgeongeneral.gov/tobacco/treating_tobacco_use08.pdf. Accessed July 6, 2008.
4. Bize R, Burnand B, Mueller Y, Cornuz J. Biomedical risk assessment as an aid for smoking cessation. Cochrane Database Syst Rev. 2005;(4):CD004705.-
5. Morris JF, Temple W. Spirometric “lung age” estimation for motivating smoking cessation. Prev Med. 1985;14:655-662.
ILLUSTRATIVE CASE
A 48-year-old man comes to your office for a routine physical. He has a 30 pack-year smoking history. When you talk to him about smoking cessation, he tells you he’s tried to stop more than once, but he can’t seem to stay motivated. You find no evidence of chronic lung disease and do not perform spirometry screening. (The US Preventive Services Task Force does not recommend spirometry for asymptomatic patients.) But could spirometry have therapeutic value in this case?
Smoking is the leading modifiable risk factor for mortality in the United States,2 and smoking cessation is the most effective intervention. Nortriptyline, bupropion, nicotine replacement agents, and varenicline are effective pharmacological treatments.3 Adding counseling to medication significantly improves quit rates (estimated odds ratio [OR]=1.4; 95% confidence interval [CI], 1.2-1.6).3 Nonetheless, physicians’ efforts to help patients stop smoking frequently fail.
But another option has caught—and held—the attention of researchers.
The promise of biomarkers
It has long been suspected that presenting smokers with evidence of tobacco’s harmful effect on their bodies—biomarkers—might encourage them to stop. Biomarkers that have been tested in randomized controlled trials (RCTs) include spirometry, exhaled carbon monoxide measurement, ultrasonography of carotid and femoral arteries, and genetic susceptibility to lung cancer, as well as combinations of these markers. But the results of most biomarker studies have been disappointing. A 2005 Cochrane Database review found insufficient evidence of the effectiveness of these markers in boosting quit rates.4
Lung age, a biomarker that’s easily understood
Lung age, a clever presentation of spirometry results, had not been tested in an RCT prior to the study we summarize below. Defined in 1985, lung age refers to the average age of a nonsmoker with a forced expiratory volume at 1 second (FEV1) equal to that of the person being tested ( FIGURE 1 ). The primary purpose was to make spirometry results easier for patients to understand, but researchers also envisioned it as a way to demonstrate the premature lung damage suffered as a consequence of smoking.5
FIGURE 1
Translating FEV1 into lung age1
STUDY SUMMARY: Graphic display more effective than FEV1 results
This study was a well-done, multicenter RCT evaluating the effect on tobacco quit rates of informing adult smokers of their lung age.1 Smokers ages 35 and older from 5 general practices in England were invited to participate. The authors excluded patients using oxygen and those with a history of tuberculosis, lung cancer, asbestosis, bronchiectasis, silicosis, or pneumonectomy. The study included 561 participants with an average of 33 pack-years of smoking, who underwent spirometry before being divided into an intervention or a control group. The researchers used standardized instruments to confirm the baseline comparability of the 2 groups.
Subjects in both groups were given information about local smoking cessation clinics and strongly encouraged to quit. All were told that their lung function would be retested in 12 months.
The controls received letters with their spirometry results presented as FEV1. In contrast, participants in the intervention group received the results in the form of a computer-generated graphic display of lung age ( FIGURE 2 ), which was further explained by a health care worker. They also received a letter within 1 month containing the same data. Participants were evaluated for smoking cessation at 12 months, and those who reported quitting received confirmatory carbon monoxide breath testing and salivary cotinine testing. Eleven percent of the subjects were lost to follow-up.
FIGURE 2
Lung age helps spirometry pack a bigger punch
Drawing a vertical line from the patient’s age (on the horizontal axis) to reach the solid curve representing the lung function of the “susceptible smoker” and extending the line horizontally to reach the curve with the broken lines representing “never smokers” graphically shows the patient’s lung age and the accelerated decline in lung function associated with smoking. The patient shown here is a 52-year-old smoker with FEV1 equivalent to a 75-year-old nonsmoker.
Source: Parkes G et al. BMJ. 2008;336:598-600. Reproduced with permission from the BMJ Publishing Group.
Quit rates higher when patients know lung age
At 1 year, verified quit rates were 13.6% in the intervention group and 6.4% in the control group (a difference of 7.2%, 95% CI, 2.2%-12.1%; P=.005). This means that for every 14 smokers who are told their lung age and shown a graphic display of this biomarker, 1 additional smoker will quit after 1 year.
Contrary to what might be expected, the investigators found that quitting did not depend on the degree of lung damage. Patients with both normal and abnormal lung age quit smoking at similar rates.
WHAT’S NEW: Lung age resonates more than spirometry alone
This is the first RCT demonstrating that informing smokers of their lung age can help them quit, and the first well-designed study to demonstrate improved cessation rates using a physiological biomarker. The research also suggests that successful quitting may have less to do with spirometry results—the level of severity of lung damage it shows—than with the way the results are presented. Giving patients information about their lung function in an easily understandable format, the authors observe, appears to result in higher quit rates.
CAVEATS: Young smokers weren’t studied
The study did not test to see if this intervention would work in younger adults, as only those 35 years of age and older were enrolled. This is a single study, and it is possible that the findings cannot be generalized to other groups or are due to unmeasured confounding factors. However, the intervention is unlikely to cause any significant harm, so we see no risks associated with it other than the cost of spirometry.
CHALLENGES TO IMPLEMENTATION: Time and expense of spirometry
We suspect the biggest challenges to implementing this recommendation in clinical practice are the expense of obtaining a spirometer ( TABLE ), staff training for those practices without one, and the time needed for the intervention. The average time to perform spirometry on study participants was 30 minutes; a health care worker spent, on average, another 15 minutes reviewing results with each member of the intervention group.
Another challenge: Not all spirometers calculate lung age or can create a graphic similar to FIGURE 2 . However, any FEV1 measurement, whether it is generated by formal pulmonary function testing or by an inexpensive hand-held meter, can easily be converted to lung age using the formula shown in FIGURE 1 . If desired, the same elements—the patient’s age, height, and gender as well as FEV1—could also be used to create a computer-generated graphic display.
TABLE
Spirometry: equipment costs
| The initial cost of a spirometer varies widely, depending on the sophistication of the equipment and the available options and features. Additional costs—for disposable mouthpieces, line filters, nose clips, and hoses, for example—are low. A sampling of reasonably priced models well suited for office use is shown below. All of these models meet American Thoracic Society criteria for spirometry, and all calculate lung age. | ||
|---|---|---|
| SPIROMETER MANUFACTURER/MODEL | PRICE | SUPPLIER |
| Futuremed Discovery-2 | $2,125 | medsupplier.com |
| Micro Medical MicroLoop | $1,780 | Miami-med.com |
| Micro Medical SpiroUSB | $1,580 | Miami-med.com |
| NDD EasyOne Frontline | $1,000 | medsupplier.com |
| SDI Diagnostics Spirolab II | $2,600 | med-electronics.com |
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
PURL METHODOLOGY
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 48-year-old man comes to your office for a routine physical. He has a 30 pack-year smoking history. When you talk to him about smoking cessation, he tells you he’s tried to stop more than once, but he can’t seem to stay motivated. You find no evidence of chronic lung disease and do not perform spirometry screening. (The US Preventive Services Task Force does not recommend spirometry for asymptomatic patients.) But could spirometry have therapeutic value in this case?
Smoking is the leading modifiable risk factor for mortality in the United States,2 and smoking cessation is the most effective intervention. Nortriptyline, bupropion, nicotine replacement agents, and varenicline are effective pharmacological treatments.3 Adding counseling to medication significantly improves quit rates (estimated odds ratio [OR]=1.4; 95% confidence interval [CI], 1.2-1.6).3 Nonetheless, physicians’ efforts to help patients stop smoking frequently fail.
But another option has caught—and held—the attention of researchers.
The promise of biomarkers
It has long been suspected that presenting smokers with evidence of tobacco’s harmful effect on their bodies—biomarkers—might encourage them to stop. Biomarkers that have been tested in randomized controlled trials (RCTs) include spirometry, exhaled carbon monoxide measurement, ultrasonography of carotid and femoral arteries, and genetic susceptibility to lung cancer, as well as combinations of these markers. But the results of most biomarker studies have been disappointing. A 2005 Cochrane Database review found insufficient evidence of the effectiveness of these markers in boosting quit rates.4
Lung age, a biomarker that’s easily understood
Lung age, a clever presentation of spirometry results, had not been tested in an RCT prior to the study we summarize below. Defined in 1985, lung age refers to the average age of a nonsmoker with a forced expiratory volume at 1 second (FEV1) equal to that of the person being tested ( FIGURE 1 ). The primary purpose was to make spirometry results easier for patients to understand, but researchers also envisioned it as a way to demonstrate the premature lung damage suffered as a consequence of smoking.5
FIGURE 1
Translating FEV1 into lung age1
STUDY SUMMARY: Graphic display more effective than FEV1 results
This study was a well-done, multicenter RCT evaluating the effect on tobacco quit rates of informing adult smokers of their lung age.1 Smokers ages 35 and older from 5 general practices in England were invited to participate. The authors excluded patients using oxygen and those with a history of tuberculosis, lung cancer, asbestosis, bronchiectasis, silicosis, or pneumonectomy. The study included 561 participants with an average of 33 pack-years of smoking, who underwent spirometry before being divided into an intervention or a control group. The researchers used standardized instruments to confirm the baseline comparability of the 2 groups.
Subjects in both groups were given information about local smoking cessation clinics and strongly encouraged to quit. All were told that their lung function would be retested in 12 months.
The controls received letters with their spirometry results presented as FEV1. In contrast, participants in the intervention group received the results in the form of a computer-generated graphic display of lung age ( FIGURE 2 ), which was further explained by a health care worker. They also received a letter within 1 month containing the same data. Participants were evaluated for smoking cessation at 12 months, and those who reported quitting received confirmatory carbon monoxide breath testing and salivary cotinine testing. Eleven percent of the subjects were lost to follow-up.
FIGURE 2
Lung age helps spirometry pack a bigger punch
Drawing a vertical line from the patient’s age (on the horizontal axis) to reach the solid curve representing the lung function of the “susceptible smoker” and extending the line horizontally to reach the curve with the broken lines representing “never smokers” graphically shows the patient’s lung age and the accelerated decline in lung function associated with smoking. The patient shown here is a 52-year-old smoker with FEV1 equivalent to a 75-year-old nonsmoker.
Source: Parkes G et al. BMJ. 2008;336:598-600. Reproduced with permission from the BMJ Publishing Group.
Quit rates higher when patients know lung age
At 1 year, verified quit rates were 13.6% in the intervention group and 6.4% in the control group (a difference of 7.2%, 95% CI, 2.2%-12.1%; P=.005). This means that for every 14 smokers who are told their lung age and shown a graphic display of this biomarker, 1 additional smoker will quit after 1 year.
Contrary to what might be expected, the investigators found that quitting did not depend on the degree of lung damage. Patients with both normal and abnormal lung age quit smoking at similar rates.
WHAT’S NEW: Lung age resonates more than spirometry alone
This is the first RCT demonstrating that informing smokers of their lung age can help them quit, and the first well-designed study to demonstrate improved cessation rates using a physiological biomarker. The research also suggests that successful quitting may have less to do with spirometry results—the level of severity of lung damage it shows—than with the way the results are presented. Giving patients information about their lung function in an easily understandable format, the authors observe, appears to result in higher quit rates.
CAVEATS: Young smokers weren’t studied
The study did not test to see if this intervention would work in younger adults, as only those 35 years of age and older were enrolled. This is a single study, and it is possible that the findings cannot be generalized to other groups or are due to unmeasured confounding factors. However, the intervention is unlikely to cause any significant harm, so we see no risks associated with it other than the cost of spirometry.
CHALLENGES TO IMPLEMENTATION: Time and expense of spirometry
We suspect the biggest challenges to implementing this recommendation in clinical practice are the expense of obtaining a spirometer ( TABLE ), staff training for those practices without one, and the time needed for the intervention. The average time to perform spirometry on study participants was 30 minutes; a health care worker spent, on average, another 15 minutes reviewing results with each member of the intervention group.
Another challenge: Not all spirometers calculate lung age or can create a graphic similar to FIGURE 2 . However, any FEV1 measurement, whether it is generated by formal pulmonary function testing or by an inexpensive hand-held meter, can easily be converted to lung age using the formula shown in FIGURE 1 . If desired, the same elements—the patient’s age, height, and gender as well as FEV1—could also be used to create a computer-generated graphic display.
TABLE
Spirometry: equipment costs
| The initial cost of a spirometer varies widely, depending on the sophistication of the equipment and the available options and features. Additional costs—for disposable mouthpieces, line filters, nose clips, and hoses, for example—are low. A sampling of reasonably priced models well suited for office use is shown below. All of these models meet American Thoracic Society criteria for spirometry, and all calculate lung age. | ||
|---|---|---|
| SPIROMETER MANUFACTURER/MODEL | PRICE | SUPPLIER |
| Futuremed Discovery-2 | $2,125 | medsupplier.com |
| Micro Medical MicroLoop | $1,780 | Miami-med.com |
| Micro Medical SpiroUSB | $1,580 | Miami-med.com |
| NDD EasyOne Frontline | $1,000 | medsupplier.com |
| SDI Diagnostics Spirolab II | $2,600 | med-electronics.com |
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
PURL METHODOLOGY
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Parkes G, Greenhalgh T, Griffin M, Dent R. Effect on smoking quit rate of telling patients their lung age: the Step2quit randomised controlled trial. BMJ. 2008;336:598-600.
2. Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238-1245.
3. Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical practice guideline. Rockville, MD: US Department of Health and Human Services, Public Health Service; May 2008. Available at: http://www.surgeongeneral.gov/tobacco/treating_tobacco_use08.pdf. Accessed July 6, 2008.
4. Bize R, Burnand B, Mueller Y, Cornuz J. Biomedical risk assessment as an aid for smoking cessation. Cochrane Database Syst Rev. 2005;(4):CD004705.-
5. Morris JF, Temple W. Spirometric “lung age” estimation for motivating smoking cessation. Prev Med. 1985;14:655-662.
1. Parkes G, Greenhalgh T, Griffin M, Dent R. Effect on smoking quit rate of telling patients their lung age: the Step2quit randomised controlled trial. BMJ. 2008;336:598-600.
2. Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238-1245.
3. Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Clinical practice guideline. Rockville, MD: US Department of Health and Human Services, Public Health Service; May 2008. Available at: http://www.surgeongeneral.gov/tobacco/treating_tobacco_use08.pdf. Accessed July 6, 2008.
4. Bize R, Burnand B, Mueller Y, Cornuz J. Biomedical risk assessment as an aid for smoking cessation. Cochrane Database Syst Rev. 2005;(4):CD004705.-
5. Morris JF, Temple W. Spirometric “lung age” estimation for motivating smoking cessation. Prev Med. 1985;14:655-662.
Copyright © 2008 The Family Physicians Inquiries Network.
All rights reserved.