User login
Restoring Function in Veterans With Complex Chronic Pain
According to the International Association for the Study of Pain (IASP), pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”1 Chronic pain (pain lasting more than 3 months) has a high prevalence in the U.S. veteran population. In a recently published article by Richard Nahin, PhD, of the National Institutes of Health, 65.5% of U.S. veterans reported pain in the previous 3 months with 9.1% classified as having severe pain (defined as “which occurs most days or every day and bothers the individual a lot”) compared with 6.4% among nonveterans.2 In addition, male veterans were more likely to report severe pain, 9%, compared with male nonveterans, 4.7%.2 Veterans make up about 6.2% of the U.S. population; therefore, the number of veterans negatively impacted by pain is substantial.3,4 Compared with individuals with other chronic diseases, such as heart disease, chronic obstructive pulmonary disease, or diabetes mellitus, a recent population-based, matched cohort study reported that only patients with Alzheimer disease have a poorer quality of life (QOL) than do those with chronic pain.5
Background
When comparing veterans to nonveterans, Nahin also reported that younger veterans aged 18 to 39 years had significantly higher rates for severe pain, compared with similarly aged nonveterans, 7.8% vs 3.2%, respectively. The prevalence of severe pain was significantly higher among veterans than it was for nonveterans experiencing the following: back pain, 21.6% vs 16.7% among nonveterans; jaw pain, 37.5% vs 22.9%, respectively; severe migraine and headaches, 26.4% vs 15.9%, respectively; and neck pain, 27.7% vs 21.9%, respectively. The veterans also were more likely than were nonveterans to have joint pain, 43.6% vs 31.5% , respectively.2
A study by Kerns and colleagues noted that almost 50% of older veterans (mean age 65.6 years) experience chronic pain regularly.6 Based on responses of 685 veterans to the Health-Risk Behavior Screening Questionnaire (HRBSQ), this study also found that the presence of pain was strongly associated with patient reports of worsening health and emotional distress. Rollin Gallagher, MD, of the Philadelphia VAMC, reported that veterans who experienced pain tended to have more personal problems due to higher rates of psychiatric and social comorbidities, such as substance abuse, depression, posttraumatic stress syndrome, and early work disabilities.7 Gallagher also has noted that the number of veterans seeking pain treatment has grown steadily over the past 2 decades due to the aging veteran population retiring and seeking VA care for chronic illness management.
In January 2017, the VA released an analysis of health care use among recent Operation Iraqi Freedom (OIF), Operation Enduring Freedom (OEF), and Operation New Dawn (OND) veterans from October 2001 through June 2015.8 The VA noted that 1,965,534 veterans have become eligible for VA health care since fiscal year 2002. Of the 1,218,857 OIF/OEF/OND veterans treated during this period, 62.3% (759,850) were treated for diseases of the musculoskeletal system and connective tissue, 58.1% (708,062) were treated for mental disorders, and 58.7% (715,263) were treated for “symptoms, signs and ill-defined conditions.”
According to the VA, “the ICD-9-CM diagnostic category ‘Symptoms, Signs and Ill-Defined Conditions’ is a diverse, catch-all category that consists of 160 sub-categories and includes primarily symptoms that do not yet have an identified cause and clinical findings that are not coded elsewhere.” The most frequently reported codes in this category, in order of magnitude are General Symptoms (ICD-9-CM 780), Symptoms Involving Respiratory System and Other Chest Symptoms (ICD-9-CM 786), and Symptoms Involving Head and Neck (ICD-9-CM 784).
Musculoskeletal ailments (ie, joint and back disorders), mental health disorders and symptoms, signs, and ill-defined conditions are the 3 most frequently coded diagnoses related to medical treatment in OEF/OIF/OND veterans. This demonstrates the high rate of pain-related conditions with comorbid mental health diagnoses.
Public Health Challenge
Recognizing that pain is a public health challenge, the National Academy of Sciences published the landmark study Relieving Pain in America.9 The study reported that pain affects at least 100 million Americans, greatly reducing quality of life. In addition, annual financial costs to society are estimated at $560 to $635 billion, with federal and state costs almost $100 billion annually. Given the challenges of addressing chronic pain, especially in the U.S. veteran population, the VHA has likewise outlined 6 recommendations for transforming VA pain care:
- Educate veterans/families to promote self-efficacy and shared decision making, provide access to all relevant sources;
- Educate/train all team members to their discipline-specific competencies, including team-based care;
- Develop and integrate nonpharmacologic modalities into care plans;
- Institute evidence-based medication prescribing, use of pain procedures, and safe opioid use (universal precautions);
- Implement approaches for bringing the veteran’s whole team together, such as virtual pain consulting (SCAN-ECHO, e-consults, telehealth, clinical video teleconsultation and education) and for maintaining ongoing communication between team members; and
- Establish metrics to monitor pain care and outcomes at both the individual level and population level.10
The American Pain Society (APS) differentiates multidisciplinary care vs interdisciplinary pain care.11 Multidisciplinary pain care is provided by several disciplines that may not be coordinated. Treatment may occur with different goals and in parallel rather than with an integrated approach. The APS suggests that professional identities are clearly defined, team membership is a secondary consideration in multidisciplinary care, and the leadership is typically hierarchical with a physician in charge. In this model of care, each team member has a “clearly defined place in the overall care of the patient, contributing their expertise in relative isolation from one another.”11
In contrast, according to APS, interdisciplinary teams have complementary roles that enhance patient care. Each discipline has valuable knowledge and a set of skills that complement other team members who are collaborative partners. The interdisciplinary approach encourages complementary roles and responsibilities, conjoint problem solving, and shared accountability. Treatment decisions are consensus based.
Pain Programs
In a review of 4 interdisciplinary pain programs (Mayo Clinic Pain Rehabilitation Center, the Brooks Rehabilitation Pain Rehabilitation Program, the Rehabilitation Institute of Chicago Center for Pain Management, and the Cleveland Clinic Foundation Chronic Pain Rehabilitation Program), Stanos found that the compositions of the staff were similar.12 In general, staff consisted of pain management physicians, pain psychologists, physical and occupational therapists, and nurse coordinators. The Mayo Clinic had more personnel, including a clinical pharmacist, the Brooks program had an additional biofeedback specialist, and the Cleveland Clinic had a tai chi instructor. The programs ranged from 3 to 5 weeks of daily programming. The duration of services provided were dependent on the payers. Stanos concluded that functional status, as measured by the Pain Disability Index, improved on discharge, 6 months, and 1 year after treatment at the Cleveland Clinic.
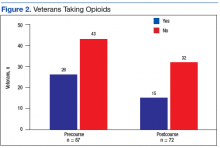
Cosio and Lin described their experience in a multidisciplinary outpatient pain clinic at Jesse Brown VAMC in Chicago.13 Their study noted that the number of veterans in their multidisciplinary pain clinic on chronic opioids significantly decreased, the degree of pain relief increased, and veterans reported improvements in mobility and ability to complete activities of daily living (ADLs). Overall veteran satisfaction with this pain program was reportedly high.
Cosio and Lin also published a study of the effect of complementary alternative medicine (CAM) utilization at a VAMC, which included a 12-week pain education school that was offered to all veterans and families.14 They noted that veterans began using at least 1 more CAM modality before the completion of the pain education program. However, it is unclear from the 2 studies whether the pain education program was incorporated into their multidisciplinary pain clinic.
Outpatient Functional Restoration Program
Given the challenges of addressing chronic pain and at the same time fostering an interdisciplinary approach to management, the VA Puget Sound Health Care System (VAPSHCS) team initiated a program development and quality improvement process for addressing pain and restoring function for veteran patients.
The VA Northwest Health Network (VISN 20) offers health care services for veterans located in the states of Alaska, Idaho, Oregon, Washington, and parts of California and Montana. VISN 20 has 8 parent facilities, which include the Seattle and American Lake divisions of the VAPSHCS. The VAPSHCS has established a comprehensive, interdisciplinary functional restoration pain program that integrates medical, psychosocial, and complementary alternative medicine.
The Outpatient Functional Restoration Program (OFRPP) pain team consists of a chief who is board certified in pain medicine and addiction medicine; a board-certified pain medicine physician; 2 physician assistants, one of whom has formal training in acupuncture and another who is trained in tai chi, qigong, hypnosis, and mindfulness; nurse care coordinators; a pain psychologist with training in acceptance and commitment therapy, cognitive behavioral therapy, yoga nidra, and hypnosis; a second pain psychologist who has a background in rehabilitation psychology; a physical therapist; and a pain clinical pharmacy specialist.
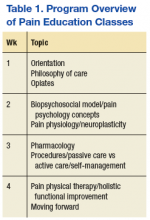
Prior to participation in OFRPP, veterans were required to attend 4 weekly pain education classes for 4 consecutive weeks. The classes educate veterans and their families on the complexity of managing chronic pain. Topics cover medical, pharmacologic and nonpharmacologic approaches to pain, including CAM and psychological modalities (Table 1). The pain orientation classes introduce veterans to available treatment options, and in some cases, veterans decide committing to a more intensive pain rehabilitation program is a good fit.
The program is based on the biopsychosocial model of pain care and Commission on Accreditation for Rehabilitation Facilities (CARF) interdisciplinary pain rehabilitation program standards. The length of the program was determined after reviewing data from existing VA outpatient pain rehabilitation programs; Pain Clinic staff availability, training and experience; and survey responses from veterans completing the 4-week education. This survey asked veterans whether they would be interested in an outpatient pain rehabilitation program and their preference for length of the program and treatment modalities.
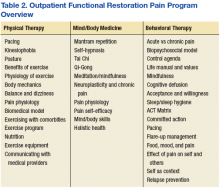
Since its inception, OFRPP has earned a 3-year CARF accreditation. Veterans participate in VAPSHCS American Lake division OFRPP education twice weekly for 4 hours for a total of 8 weeks (Table 2). Each week of programming includes 2 hours of physical therapy didactics, 2 hours of physical therapy (eg, paced cardio exercise, stretching, and core strength and conditioning), 2 hours of mind-body medicine (eg, mantram repetition and neuroplasticity education), and 2 hours of psychology education (behavioral interventions and psychological strategies for pain self-management of pain).
There is also 1 hour of pharmacotherapy education regarding commonly prescribed pain medications and how to take medications safely to avoid common adverse events. The nurse is responsible for care coordination and analysis of outcome measures, data collection, and quality improvement.
Program Effectiveness
Program effectiveness is measured using the POQ-VA (Pain Outcomes Questionnaire-VA). The POQ results and participant feedback are used to ensure ongoing program evaluation and improvement. This outcome measure was selected as the POQ-VA evaluates intervention effectiveness of all the major pain outcomes domains. This questionnaire was developed and validated by the VA.
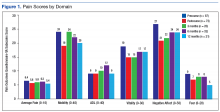
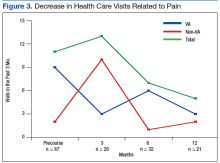
The sample size was 957 veterans.15 The POQ-VA is reverse scored, meaning lower scores indicate improvement. Eighty-seven veterans have completed the program with 20 participants completing the 3-month outcome measures, 31 participants completing 6-month outcome measures, and 17 participants completing 12-month outcome measures.
The pain score decreased close to 1 point at 12 months. The mobility gains were maintained at 12 months. The ADL did not improve much after 1 year (Figure 1).
In the other POQ-VA subscales, vitality improved somewhat.
Limitations
Only a small sample size of veterans with chronic pain participated in the functional restoration pain program. Long-term follow-up of participants who successfully completed the program also is desired.
Conclusion
Veterans experiencing complex chronic noncancer pain present a challenge for the VA health care system. Successful management of this requires cooperation among different disciplines and fostering a multimodal and interdisciplinary approach. Functional restoration pain programs have existed for a while and have shown clear evidence of their superiority over monotherapies for patients with chronic noncancer pain.
This functional restoration pain program incorporated various evidence-based medical, rehabilitative, psychological interventions with mind body medicine, mindfulness and integrative pain modalities. The authors continually meet and assess the success of the program. Although the initial outcome measures are encouraging, increased veteran participation in answering their post program completion surveys is desired. The goal is to improve veterans’ self-management of their chronic pain, leading to reductions in pain symptoms, medication, and health care provider use, as well as improve veterans’ function and overall QOL.
1. International Association for the Study of Pain. IASP taxonomy. https://www.iasp-pain.org/Taxonomy#Pain. Updated May 22, 2012. Accessed August 31, 2017.
2. Nahin RL. Severe pain in veterans: the effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254.
3. U.S. Census Bureau. 2011-2015 American community services 5-year estimates. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_15_5YRB21002&prodType=table. Accessed August 31, 2017.
4. U.S. Census Bureau, population division. Annual estimates of the resident population: April 1, 2010 to July 1, 2016. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview .xhtml?pid=PEP_2016_PEPANNRES&SPC=pt. Accessed August 31, 2017.
5. Hogan ME, Taddio A, Katz J, Shah V, Krahn M. Health utilities in people with chronic pain using a population level survey and linked health care administrative data. Pain. 2017;158(3):408-416.
6. Kerns RD, Otis J, Rosenberg R, Reid MC. Veterans reports of pain and associations with ratings of health, health risk-behaviors, affective distress and use of the healthcare system. J Rehabil Res Dev. 2003;40(5):371-379.
7. Gallagher RM. Advancing the pain agenda in the veteran population. Anesthesiol Clin. 2016;34(2):357-378.
8. U.S. Department of Veterans Affairs. Analysis of VA health care utilization among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) veterans. https://www.publichealth.va.gov/docs/epidemiol ogy/healthcare-utilization-report-fy2015-qtr3.pdf. Published January 2017. Accessed August 31, 2017.
9. National Academies of Science. Institute of Medicine: Relieving pain in America: a blueprint for transforming prevention care, education, and research. https://iprcc.nih.gov/docs/032712_mtg _presentations/iom_pain_report_508comp.pdf. Published June 29, 2011. Accessed August 31, 2017.
10. U.S. Department of Veterans Affairs. Transforming VA pain care. https://www.va.gov/painmanagement/Updated August 17, 2017. Accessed August 31, 2017.
11. American Pain Society. Interdisciplinary pain management. http://americanpainsociety.org/uploads/about/position-statements/interdisciplinary-white -paper.pdf. Accessed August 31, 2017.
12. Stanos S. Focused review of interdisciplinary pain rehabilitation programs for chronic pain management. Curr Pain Headache Rep. 2012;16(2):147-152.
13. Cosio D, Lin EH. (538) Efficacy of an outpatient, multidisciplinary VA pain management clinic: findings from a one-year outcome study. Pain. 2014;15(4):S110.
14. Cosio D, Lin EH. Effects of a pain education program in complementary and alternative medicine treatment utilization at a VA medical center. Complement Ther Med. 2015;23(3):413-422.
15. Clark ME, Gironda RJ, Young RW. Development and validation of the pain outcomes questionnaire-VA. J Rehabil Res Dev. 2003;40(5)-381-395.
According to the International Association for the Study of Pain (IASP), pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”1 Chronic pain (pain lasting more than 3 months) has a high prevalence in the U.S. veteran population. In a recently published article by Richard Nahin, PhD, of the National Institutes of Health, 65.5% of U.S. veterans reported pain in the previous 3 months with 9.1% classified as having severe pain (defined as “which occurs most days or every day and bothers the individual a lot”) compared with 6.4% among nonveterans.2 In addition, male veterans were more likely to report severe pain, 9%, compared with male nonveterans, 4.7%.2 Veterans make up about 6.2% of the U.S. population; therefore, the number of veterans negatively impacted by pain is substantial.3,4 Compared with individuals with other chronic diseases, such as heart disease, chronic obstructive pulmonary disease, or diabetes mellitus, a recent population-based, matched cohort study reported that only patients with Alzheimer disease have a poorer quality of life (QOL) than do those with chronic pain.5
Background
When comparing veterans to nonveterans, Nahin also reported that younger veterans aged 18 to 39 years had significantly higher rates for severe pain, compared with similarly aged nonveterans, 7.8% vs 3.2%, respectively. The prevalence of severe pain was significantly higher among veterans than it was for nonveterans experiencing the following: back pain, 21.6% vs 16.7% among nonveterans; jaw pain, 37.5% vs 22.9%, respectively; severe migraine and headaches, 26.4% vs 15.9%, respectively; and neck pain, 27.7% vs 21.9%, respectively. The veterans also were more likely than were nonveterans to have joint pain, 43.6% vs 31.5% , respectively.2
A study by Kerns and colleagues noted that almost 50% of older veterans (mean age 65.6 years) experience chronic pain regularly.6 Based on responses of 685 veterans to the Health-Risk Behavior Screening Questionnaire (HRBSQ), this study also found that the presence of pain was strongly associated with patient reports of worsening health and emotional distress. Rollin Gallagher, MD, of the Philadelphia VAMC, reported that veterans who experienced pain tended to have more personal problems due to higher rates of psychiatric and social comorbidities, such as substance abuse, depression, posttraumatic stress syndrome, and early work disabilities.7 Gallagher also has noted that the number of veterans seeking pain treatment has grown steadily over the past 2 decades due to the aging veteran population retiring and seeking VA care for chronic illness management.
In January 2017, the VA released an analysis of health care use among recent Operation Iraqi Freedom (OIF), Operation Enduring Freedom (OEF), and Operation New Dawn (OND) veterans from October 2001 through June 2015.8 The VA noted that 1,965,534 veterans have become eligible for VA health care since fiscal year 2002. Of the 1,218,857 OIF/OEF/OND veterans treated during this period, 62.3% (759,850) were treated for diseases of the musculoskeletal system and connective tissue, 58.1% (708,062) were treated for mental disorders, and 58.7% (715,263) were treated for “symptoms, signs and ill-defined conditions.”
According to the VA, “the ICD-9-CM diagnostic category ‘Symptoms, Signs and Ill-Defined Conditions’ is a diverse, catch-all category that consists of 160 sub-categories and includes primarily symptoms that do not yet have an identified cause and clinical findings that are not coded elsewhere.” The most frequently reported codes in this category, in order of magnitude are General Symptoms (ICD-9-CM 780), Symptoms Involving Respiratory System and Other Chest Symptoms (ICD-9-CM 786), and Symptoms Involving Head and Neck (ICD-9-CM 784).
Musculoskeletal ailments (ie, joint and back disorders), mental health disorders and symptoms, signs, and ill-defined conditions are the 3 most frequently coded diagnoses related to medical treatment in OEF/OIF/OND veterans. This demonstrates the high rate of pain-related conditions with comorbid mental health diagnoses.
Public Health Challenge
Recognizing that pain is a public health challenge, the National Academy of Sciences published the landmark study Relieving Pain in America.9 The study reported that pain affects at least 100 million Americans, greatly reducing quality of life. In addition, annual financial costs to society are estimated at $560 to $635 billion, with federal and state costs almost $100 billion annually. Given the challenges of addressing chronic pain, especially in the U.S. veteran population, the VHA has likewise outlined 6 recommendations for transforming VA pain care:
- Educate veterans/families to promote self-efficacy and shared decision making, provide access to all relevant sources;
- Educate/train all team members to their discipline-specific competencies, including team-based care;
- Develop and integrate nonpharmacologic modalities into care plans;
- Institute evidence-based medication prescribing, use of pain procedures, and safe opioid use (universal precautions);
- Implement approaches for bringing the veteran’s whole team together, such as virtual pain consulting (SCAN-ECHO, e-consults, telehealth, clinical video teleconsultation and education) and for maintaining ongoing communication between team members; and
- Establish metrics to monitor pain care and outcomes at both the individual level and population level.10
The American Pain Society (APS) differentiates multidisciplinary care vs interdisciplinary pain care.11 Multidisciplinary pain care is provided by several disciplines that may not be coordinated. Treatment may occur with different goals and in parallel rather than with an integrated approach. The APS suggests that professional identities are clearly defined, team membership is a secondary consideration in multidisciplinary care, and the leadership is typically hierarchical with a physician in charge. In this model of care, each team member has a “clearly defined place in the overall care of the patient, contributing their expertise in relative isolation from one another.”11
In contrast, according to APS, interdisciplinary teams have complementary roles that enhance patient care. Each discipline has valuable knowledge and a set of skills that complement other team members who are collaborative partners. The interdisciplinary approach encourages complementary roles and responsibilities, conjoint problem solving, and shared accountability. Treatment decisions are consensus based.
Pain Programs
In a review of 4 interdisciplinary pain programs (Mayo Clinic Pain Rehabilitation Center, the Brooks Rehabilitation Pain Rehabilitation Program, the Rehabilitation Institute of Chicago Center for Pain Management, and the Cleveland Clinic Foundation Chronic Pain Rehabilitation Program), Stanos found that the compositions of the staff were similar.12 In general, staff consisted of pain management physicians, pain psychologists, physical and occupational therapists, and nurse coordinators. The Mayo Clinic had more personnel, including a clinical pharmacist, the Brooks program had an additional biofeedback specialist, and the Cleveland Clinic had a tai chi instructor. The programs ranged from 3 to 5 weeks of daily programming. The duration of services provided were dependent on the payers. Stanos concluded that functional status, as measured by the Pain Disability Index, improved on discharge, 6 months, and 1 year after treatment at the Cleveland Clinic.
Cosio and Lin described their experience in a multidisciplinary outpatient pain clinic at Jesse Brown VAMC in Chicago.13 Their study noted that the number of veterans in their multidisciplinary pain clinic on chronic opioids significantly decreased, the degree of pain relief increased, and veterans reported improvements in mobility and ability to complete activities of daily living (ADLs). Overall veteran satisfaction with this pain program was reportedly high.
Cosio and Lin also published a study of the effect of complementary alternative medicine (CAM) utilization at a VAMC, which included a 12-week pain education school that was offered to all veterans and families.14 They noted that veterans began using at least 1 more CAM modality before the completion of the pain education program. However, it is unclear from the 2 studies whether the pain education program was incorporated into their multidisciplinary pain clinic.
Outpatient Functional Restoration Program
Given the challenges of addressing chronic pain and at the same time fostering an interdisciplinary approach to management, the VA Puget Sound Health Care System (VAPSHCS) team initiated a program development and quality improvement process for addressing pain and restoring function for veteran patients.
The VA Northwest Health Network (VISN 20) offers health care services for veterans located in the states of Alaska, Idaho, Oregon, Washington, and parts of California and Montana. VISN 20 has 8 parent facilities, which include the Seattle and American Lake divisions of the VAPSHCS. The VAPSHCS has established a comprehensive, interdisciplinary functional restoration pain program that integrates medical, psychosocial, and complementary alternative medicine.
The Outpatient Functional Restoration Program (OFRPP) pain team consists of a chief who is board certified in pain medicine and addiction medicine; a board-certified pain medicine physician; 2 physician assistants, one of whom has formal training in acupuncture and another who is trained in tai chi, qigong, hypnosis, and mindfulness; nurse care coordinators; a pain psychologist with training in acceptance and commitment therapy, cognitive behavioral therapy, yoga nidra, and hypnosis; a second pain psychologist who has a background in rehabilitation psychology; a physical therapist; and a pain clinical pharmacy specialist.
Prior to participation in OFRPP, veterans were required to attend 4 weekly pain education classes for 4 consecutive weeks. The classes educate veterans and their families on the complexity of managing chronic pain. Topics cover medical, pharmacologic and nonpharmacologic approaches to pain, including CAM and psychological modalities (Table 1). The pain orientation classes introduce veterans to available treatment options, and in some cases, veterans decide committing to a more intensive pain rehabilitation program is a good fit.
The program is based on the biopsychosocial model of pain care and Commission on Accreditation for Rehabilitation Facilities (CARF) interdisciplinary pain rehabilitation program standards. The length of the program was determined after reviewing data from existing VA outpatient pain rehabilitation programs; Pain Clinic staff availability, training and experience; and survey responses from veterans completing the 4-week education. This survey asked veterans whether they would be interested in an outpatient pain rehabilitation program and their preference for length of the program and treatment modalities.
Since its inception, OFRPP has earned a 3-year CARF accreditation. Veterans participate in VAPSHCS American Lake division OFRPP education twice weekly for 4 hours for a total of 8 weeks (Table 2). Each week of programming includes 2 hours of physical therapy didactics, 2 hours of physical therapy (eg, paced cardio exercise, stretching, and core strength and conditioning), 2 hours of mind-body medicine (eg, mantram repetition and neuroplasticity education), and 2 hours of psychology education (behavioral interventions and psychological strategies for pain self-management of pain).
There is also 1 hour of pharmacotherapy education regarding commonly prescribed pain medications and how to take medications safely to avoid common adverse events. The nurse is responsible for care coordination and analysis of outcome measures, data collection, and quality improvement.
Program Effectiveness
Program effectiveness is measured using the POQ-VA (Pain Outcomes Questionnaire-VA). The POQ results and participant feedback are used to ensure ongoing program evaluation and improvement. This outcome measure was selected as the POQ-VA evaluates intervention effectiveness of all the major pain outcomes domains. This questionnaire was developed and validated by the VA.
The sample size was 957 veterans.15 The POQ-VA is reverse scored, meaning lower scores indicate improvement. Eighty-seven veterans have completed the program with 20 participants completing the 3-month outcome measures, 31 participants completing 6-month outcome measures, and 17 participants completing 12-month outcome measures.
The pain score decreased close to 1 point at 12 months. The mobility gains were maintained at 12 months. The ADL did not improve much after 1 year (Figure 1).
In the other POQ-VA subscales, vitality improved somewhat.
Limitations
Only a small sample size of veterans with chronic pain participated in the functional restoration pain program. Long-term follow-up of participants who successfully completed the program also is desired.
Conclusion
Veterans experiencing complex chronic noncancer pain present a challenge for the VA health care system. Successful management of this requires cooperation among different disciplines and fostering a multimodal and interdisciplinary approach. Functional restoration pain programs have existed for a while and have shown clear evidence of their superiority over monotherapies for patients with chronic noncancer pain.
This functional restoration pain program incorporated various evidence-based medical, rehabilitative, psychological interventions with mind body medicine, mindfulness and integrative pain modalities. The authors continually meet and assess the success of the program. Although the initial outcome measures are encouraging, increased veteran participation in answering their post program completion surveys is desired. The goal is to improve veterans’ self-management of their chronic pain, leading to reductions in pain symptoms, medication, and health care provider use, as well as improve veterans’ function and overall QOL.
According to the International Association for the Study of Pain (IASP), pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”1 Chronic pain (pain lasting more than 3 months) has a high prevalence in the U.S. veteran population. In a recently published article by Richard Nahin, PhD, of the National Institutes of Health, 65.5% of U.S. veterans reported pain in the previous 3 months with 9.1% classified as having severe pain (defined as “which occurs most days or every day and bothers the individual a lot”) compared with 6.4% among nonveterans.2 In addition, male veterans were more likely to report severe pain, 9%, compared with male nonveterans, 4.7%.2 Veterans make up about 6.2% of the U.S. population; therefore, the number of veterans negatively impacted by pain is substantial.3,4 Compared with individuals with other chronic diseases, such as heart disease, chronic obstructive pulmonary disease, or diabetes mellitus, a recent population-based, matched cohort study reported that only patients with Alzheimer disease have a poorer quality of life (QOL) than do those with chronic pain.5
Background
When comparing veterans to nonveterans, Nahin also reported that younger veterans aged 18 to 39 years had significantly higher rates for severe pain, compared with similarly aged nonveterans, 7.8% vs 3.2%, respectively. The prevalence of severe pain was significantly higher among veterans than it was for nonveterans experiencing the following: back pain, 21.6% vs 16.7% among nonveterans; jaw pain, 37.5% vs 22.9%, respectively; severe migraine and headaches, 26.4% vs 15.9%, respectively; and neck pain, 27.7% vs 21.9%, respectively. The veterans also were more likely than were nonveterans to have joint pain, 43.6% vs 31.5% , respectively.2
A study by Kerns and colleagues noted that almost 50% of older veterans (mean age 65.6 years) experience chronic pain regularly.6 Based on responses of 685 veterans to the Health-Risk Behavior Screening Questionnaire (HRBSQ), this study also found that the presence of pain was strongly associated with patient reports of worsening health and emotional distress. Rollin Gallagher, MD, of the Philadelphia VAMC, reported that veterans who experienced pain tended to have more personal problems due to higher rates of psychiatric and social comorbidities, such as substance abuse, depression, posttraumatic stress syndrome, and early work disabilities.7 Gallagher also has noted that the number of veterans seeking pain treatment has grown steadily over the past 2 decades due to the aging veteran population retiring and seeking VA care for chronic illness management.
In January 2017, the VA released an analysis of health care use among recent Operation Iraqi Freedom (OIF), Operation Enduring Freedom (OEF), and Operation New Dawn (OND) veterans from October 2001 through June 2015.8 The VA noted that 1,965,534 veterans have become eligible for VA health care since fiscal year 2002. Of the 1,218,857 OIF/OEF/OND veterans treated during this period, 62.3% (759,850) were treated for diseases of the musculoskeletal system and connective tissue, 58.1% (708,062) were treated for mental disorders, and 58.7% (715,263) were treated for “symptoms, signs and ill-defined conditions.”
According to the VA, “the ICD-9-CM diagnostic category ‘Symptoms, Signs and Ill-Defined Conditions’ is a diverse, catch-all category that consists of 160 sub-categories and includes primarily symptoms that do not yet have an identified cause and clinical findings that are not coded elsewhere.” The most frequently reported codes in this category, in order of magnitude are General Symptoms (ICD-9-CM 780), Symptoms Involving Respiratory System and Other Chest Symptoms (ICD-9-CM 786), and Symptoms Involving Head and Neck (ICD-9-CM 784).
Musculoskeletal ailments (ie, joint and back disorders), mental health disorders and symptoms, signs, and ill-defined conditions are the 3 most frequently coded diagnoses related to medical treatment in OEF/OIF/OND veterans. This demonstrates the high rate of pain-related conditions with comorbid mental health diagnoses.
Public Health Challenge
Recognizing that pain is a public health challenge, the National Academy of Sciences published the landmark study Relieving Pain in America.9 The study reported that pain affects at least 100 million Americans, greatly reducing quality of life. In addition, annual financial costs to society are estimated at $560 to $635 billion, with federal and state costs almost $100 billion annually. Given the challenges of addressing chronic pain, especially in the U.S. veteran population, the VHA has likewise outlined 6 recommendations for transforming VA pain care:
- Educate veterans/families to promote self-efficacy and shared decision making, provide access to all relevant sources;
- Educate/train all team members to their discipline-specific competencies, including team-based care;
- Develop and integrate nonpharmacologic modalities into care plans;
- Institute evidence-based medication prescribing, use of pain procedures, and safe opioid use (universal precautions);
- Implement approaches for bringing the veteran’s whole team together, such as virtual pain consulting (SCAN-ECHO, e-consults, telehealth, clinical video teleconsultation and education) and for maintaining ongoing communication between team members; and
- Establish metrics to monitor pain care and outcomes at both the individual level and population level.10
The American Pain Society (APS) differentiates multidisciplinary care vs interdisciplinary pain care.11 Multidisciplinary pain care is provided by several disciplines that may not be coordinated. Treatment may occur with different goals and in parallel rather than with an integrated approach. The APS suggests that professional identities are clearly defined, team membership is a secondary consideration in multidisciplinary care, and the leadership is typically hierarchical with a physician in charge. In this model of care, each team member has a “clearly defined place in the overall care of the patient, contributing their expertise in relative isolation from one another.”11
In contrast, according to APS, interdisciplinary teams have complementary roles that enhance patient care. Each discipline has valuable knowledge and a set of skills that complement other team members who are collaborative partners. The interdisciplinary approach encourages complementary roles and responsibilities, conjoint problem solving, and shared accountability. Treatment decisions are consensus based.
Pain Programs
In a review of 4 interdisciplinary pain programs (Mayo Clinic Pain Rehabilitation Center, the Brooks Rehabilitation Pain Rehabilitation Program, the Rehabilitation Institute of Chicago Center for Pain Management, and the Cleveland Clinic Foundation Chronic Pain Rehabilitation Program), Stanos found that the compositions of the staff were similar.12 In general, staff consisted of pain management physicians, pain psychologists, physical and occupational therapists, and nurse coordinators. The Mayo Clinic had more personnel, including a clinical pharmacist, the Brooks program had an additional biofeedback specialist, and the Cleveland Clinic had a tai chi instructor. The programs ranged from 3 to 5 weeks of daily programming. The duration of services provided were dependent on the payers. Stanos concluded that functional status, as measured by the Pain Disability Index, improved on discharge, 6 months, and 1 year after treatment at the Cleveland Clinic.
Cosio and Lin described their experience in a multidisciplinary outpatient pain clinic at Jesse Brown VAMC in Chicago.13 Their study noted that the number of veterans in their multidisciplinary pain clinic on chronic opioids significantly decreased, the degree of pain relief increased, and veterans reported improvements in mobility and ability to complete activities of daily living (ADLs). Overall veteran satisfaction with this pain program was reportedly high.
Cosio and Lin also published a study of the effect of complementary alternative medicine (CAM) utilization at a VAMC, which included a 12-week pain education school that was offered to all veterans and families.14 They noted that veterans began using at least 1 more CAM modality before the completion of the pain education program. However, it is unclear from the 2 studies whether the pain education program was incorporated into their multidisciplinary pain clinic.
Outpatient Functional Restoration Program
Given the challenges of addressing chronic pain and at the same time fostering an interdisciplinary approach to management, the VA Puget Sound Health Care System (VAPSHCS) team initiated a program development and quality improvement process for addressing pain and restoring function for veteran patients.
The VA Northwest Health Network (VISN 20) offers health care services for veterans located in the states of Alaska, Idaho, Oregon, Washington, and parts of California and Montana. VISN 20 has 8 parent facilities, which include the Seattle and American Lake divisions of the VAPSHCS. The VAPSHCS has established a comprehensive, interdisciplinary functional restoration pain program that integrates medical, psychosocial, and complementary alternative medicine.
The Outpatient Functional Restoration Program (OFRPP) pain team consists of a chief who is board certified in pain medicine and addiction medicine; a board-certified pain medicine physician; 2 physician assistants, one of whom has formal training in acupuncture and another who is trained in tai chi, qigong, hypnosis, and mindfulness; nurse care coordinators; a pain psychologist with training in acceptance and commitment therapy, cognitive behavioral therapy, yoga nidra, and hypnosis; a second pain psychologist who has a background in rehabilitation psychology; a physical therapist; and a pain clinical pharmacy specialist.
Prior to participation in OFRPP, veterans were required to attend 4 weekly pain education classes for 4 consecutive weeks. The classes educate veterans and their families on the complexity of managing chronic pain. Topics cover medical, pharmacologic and nonpharmacologic approaches to pain, including CAM and psychological modalities (Table 1). The pain orientation classes introduce veterans to available treatment options, and in some cases, veterans decide committing to a more intensive pain rehabilitation program is a good fit.
The program is based on the biopsychosocial model of pain care and Commission on Accreditation for Rehabilitation Facilities (CARF) interdisciplinary pain rehabilitation program standards. The length of the program was determined after reviewing data from existing VA outpatient pain rehabilitation programs; Pain Clinic staff availability, training and experience; and survey responses from veterans completing the 4-week education. This survey asked veterans whether they would be interested in an outpatient pain rehabilitation program and their preference for length of the program and treatment modalities.
Since its inception, OFRPP has earned a 3-year CARF accreditation. Veterans participate in VAPSHCS American Lake division OFRPP education twice weekly for 4 hours for a total of 8 weeks (Table 2). Each week of programming includes 2 hours of physical therapy didactics, 2 hours of physical therapy (eg, paced cardio exercise, stretching, and core strength and conditioning), 2 hours of mind-body medicine (eg, mantram repetition and neuroplasticity education), and 2 hours of psychology education (behavioral interventions and psychological strategies for pain self-management of pain).
There is also 1 hour of pharmacotherapy education regarding commonly prescribed pain medications and how to take medications safely to avoid common adverse events. The nurse is responsible for care coordination and analysis of outcome measures, data collection, and quality improvement.
Program Effectiveness
Program effectiveness is measured using the POQ-VA (Pain Outcomes Questionnaire-VA). The POQ results and participant feedback are used to ensure ongoing program evaluation and improvement. This outcome measure was selected as the POQ-VA evaluates intervention effectiveness of all the major pain outcomes domains. This questionnaire was developed and validated by the VA.
The sample size was 957 veterans.15 The POQ-VA is reverse scored, meaning lower scores indicate improvement. Eighty-seven veterans have completed the program with 20 participants completing the 3-month outcome measures, 31 participants completing 6-month outcome measures, and 17 participants completing 12-month outcome measures.
The pain score decreased close to 1 point at 12 months. The mobility gains were maintained at 12 months. The ADL did not improve much after 1 year (Figure 1).
In the other POQ-VA subscales, vitality improved somewhat.
Limitations
Only a small sample size of veterans with chronic pain participated in the functional restoration pain program. Long-term follow-up of participants who successfully completed the program also is desired.
Conclusion
Veterans experiencing complex chronic noncancer pain present a challenge for the VA health care system. Successful management of this requires cooperation among different disciplines and fostering a multimodal and interdisciplinary approach. Functional restoration pain programs have existed for a while and have shown clear evidence of their superiority over monotherapies for patients with chronic noncancer pain.
This functional restoration pain program incorporated various evidence-based medical, rehabilitative, psychological interventions with mind body medicine, mindfulness and integrative pain modalities. The authors continually meet and assess the success of the program. Although the initial outcome measures are encouraging, increased veteran participation in answering their post program completion surveys is desired. The goal is to improve veterans’ self-management of their chronic pain, leading to reductions in pain symptoms, medication, and health care provider use, as well as improve veterans’ function and overall QOL.
1. International Association for the Study of Pain. IASP taxonomy. https://www.iasp-pain.org/Taxonomy#Pain. Updated May 22, 2012. Accessed August 31, 2017.
2. Nahin RL. Severe pain in veterans: the effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254.
3. U.S. Census Bureau. 2011-2015 American community services 5-year estimates. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_15_5YRB21002&prodType=table. Accessed August 31, 2017.
4. U.S. Census Bureau, population division. Annual estimates of the resident population: April 1, 2010 to July 1, 2016. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview .xhtml?pid=PEP_2016_PEPANNRES&SPC=pt. Accessed August 31, 2017.
5. Hogan ME, Taddio A, Katz J, Shah V, Krahn M. Health utilities in people with chronic pain using a population level survey and linked health care administrative data. Pain. 2017;158(3):408-416.
6. Kerns RD, Otis J, Rosenberg R, Reid MC. Veterans reports of pain and associations with ratings of health, health risk-behaviors, affective distress and use of the healthcare system. J Rehabil Res Dev. 2003;40(5):371-379.
7. Gallagher RM. Advancing the pain agenda in the veteran population. Anesthesiol Clin. 2016;34(2):357-378.
8. U.S. Department of Veterans Affairs. Analysis of VA health care utilization among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) veterans. https://www.publichealth.va.gov/docs/epidemiol ogy/healthcare-utilization-report-fy2015-qtr3.pdf. Published January 2017. Accessed August 31, 2017.
9. National Academies of Science. Institute of Medicine: Relieving pain in America: a blueprint for transforming prevention care, education, and research. https://iprcc.nih.gov/docs/032712_mtg _presentations/iom_pain_report_508comp.pdf. Published June 29, 2011. Accessed August 31, 2017.
10. U.S. Department of Veterans Affairs. Transforming VA pain care. https://www.va.gov/painmanagement/Updated August 17, 2017. Accessed August 31, 2017.
11. American Pain Society. Interdisciplinary pain management. http://americanpainsociety.org/uploads/about/position-statements/interdisciplinary-white -paper.pdf. Accessed August 31, 2017.
12. Stanos S. Focused review of interdisciplinary pain rehabilitation programs for chronic pain management. Curr Pain Headache Rep. 2012;16(2):147-152.
13. Cosio D, Lin EH. (538) Efficacy of an outpatient, multidisciplinary VA pain management clinic: findings from a one-year outcome study. Pain. 2014;15(4):S110.
14. Cosio D, Lin EH. Effects of a pain education program in complementary and alternative medicine treatment utilization at a VA medical center. Complement Ther Med. 2015;23(3):413-422.
15. Clark ME, Gironda RJ, Young RW. Development and validation of the pain outcomes questionnaire-VA. J Rehabil Res Dev. 2003;40(5)-381-395.
1. International Association for the Study of Pain. IASP taxonomy. https://www.iasp-pain.org/Taxonomy#Pain. Updated May 22, 2012. Accessed August 31, 2017.
2. Nahin RL. Severe pain in veterans: the effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254.
3. U.S. Census Bureau. 2011-2015 American community services 5-year estimates. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_15_5YRB21002&prodType=table. Accessed August 31, 2017.
4. U.S. Census Bureau, population division. Annual estimates of the resident population: April 1, 2010 to July 1, 2016. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview .xhtml?pid=PEP_2016_PEPANNRES&SPC=pt. Accessed August 31, 2017.
5. Hogan ME, Taddio A, Katz J, Shah V, Krahn M. Health utilities in people with chronic pain using a population level survey and linked health care administrative data. Pain. 2017;158(3):408-416.
6. Kerns RD, Otis J, Rosenberg R, Reid MC. Veterans reports of pain and associations with ratings of health, health risk-behaviors, affective distress and use of the healthcare system. J Rehabil Res Dev. 2003;40(5):371-379.
7. Gallagher RM. Advancing the pain agenda in the veteran population. Anesthesiol Clin. 2016;34(2):357-378.
8. U.S. Department of Veterans Affairs. Analysis of VA health care utilization among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) veterans. https://www.publichealth.va.gov/docs/epidemiol ogy/healthcare-utilization-report-fy2015-qtr3.pdf. Published January 2017. Accessed August 31, 2017.
9. National Academies of Science. Institute of Medicine: Relieving pain in America: a blueprint for transforming prevention care, education, and research. https://iprcc.nih.gov/docs/032712_mtg _presentations/iom_pain_report_508comp.pdf. Published June 29, 2011. Accessed August 31, 2017.
10. U.S. Department of Veterans Affairs. Transforming VA pain care. https://www.va.gov/painmanagement/Updated August 17, 2017. Accessed August 31, 2017.
11. American Pain Society. Interdisciplinary pain management. http://americanpainsociety.org/uploads/about/position-statements/interdisciplinary-white -paper.pdf. Accessed August 31, 2017.
12. Stanos S. Focused review of interdisciplinary pain rehabilitation programs for chronic pain management. Curr Pain Headache Rep. 2012;16(2):147-152.
13. Cosio D, Lin EH. (538) Efficacy of an outpatient, multidisciplinary VA pain management clinic: findings from a one-year outcome study. Pain. 2014;15(4):S110.
14. Cosio D, Lin EH. Effects of a pain education program in complementary and alternative medicine treatment utilization at a VA medical center. Complement Ther Med. 2015;23(3):413-422.
15. Clark ME, Gironda RJ, Young RW. Development and validation of the pain outcomes questionnaire-VA. J Rehabil Res Dev. 2003;40(5)-381-395.