User login
How can you help prevent a recurrence of diverticulitis?
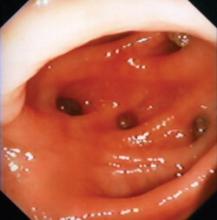
A high-fiber diet may help; available evidence doesn’t support other interventions. A high-fiber diet is often prescribed after recovery from acute diverticulitis, based on extrapolation from epidemiologic data showing an association between low-fiber diets and diverticulosis (strength of recommendation [SOR]: C, expert opinion). No direct evidence establishes a role for fiber in preventing recurrent diverticulitis, however.
No evidence supports the common advice to avoid nuts and seeds to prevent diverticulitis. Eating nuts, corn, and popcorn doesn’t increase the risk; in fact, nuts and popcorn may have a protective effect (SOR: B, large cohort study).
There isn’t enough evidence to recommend the anti-inflammatory drug mesalamine or a polybacterial lysate for immunostimulation. Retrospective data don’t support routine prophylactic colectomy after 1 or 2 episodes of acute diverticulitis (SOR: B, observational studies).
Evidence summary
A 2006 Family Physicians Inquiries Network Clinical Inquiry on diverticulosis found inconsistent evidence that fiber decreases the risk of symptomatic diverticular disease (SOR: C, case control studies and a large prospective cohort study).1
A 2007 literature review found no systematic reviews or randomized controlled trials (RCTs) of fiber for preventing complications of diverticular disease. The reviewers noted that observational studies have found less diverticulosis in populations with higher fiber consumption.2
Nuts, popcorn may be protective
A trial conducted as part of a large prospective cohort study—the Health Professionals Follow-up Study—followed 47,228 male health professionals in the United States, ages 40 to 75 years, from 1986 to 2004.3 The subjects, all of whom returned a food-frequency questionnaire, were at baseline free of diverticulosis and related complications, cancer, and inflammatory bowel disease. During the follow-up period, 801 cases of diverticulitis and 383 cases of diverticular bleeding (the main outcome measures) occurred.
The investigators found an inverse association between consumption of nuts and popcorn and risk of diverticulitis. Men with the highest intake of each food (at least twice per week) compared with men with the lowest intake (less than once per month) had a hazard ratio of 0.80 (95% confidence interval [CI], 0.63-1.01; P for trend=.04) for nuts and 0.72 (95% CI, 0.56-0.92; P for trend=.007) for popcorn. No association was noted between corn consumption and diverticulitis or between nut, corn, or popcorn consumption and diverticular bleeding or uncomplicated diverticulosis.
Mesalamine’s efficacy is unknown
A 2007 systematic review found 1 RCT of the anti-inflammatory drug mesalamine (mesalazine, 5-aminosalicylic acid) for preventing diverticulitis. Mesalamine reduced the recurrence rate of diverticulitis from 46% to 15% among 166 subjects.
The reviewers judged the study to be flawed by unreported diagnostic criteria and a high withdrawal rate. They concluded that the effectiveness of mesalamine remains unknown.2
1 small study of oral enterovaccine
An oral polybacterial lysate suspension designed to stimulate gut secretion of immunoglobulin A was investigated in a study of 83 patients with recurrent diverticulitis. In the treated group, 4.6% (2/43) of patients had recurrent diverticulitis during the 3 months of the study, compared with 12.5% (5/40) of the untreated group (P<.05).4
Prophylactic surgery rarely helps
No randomized trials have compared surgical with medical therapy to prevent recurrent diverticulitis. Extensive retrospective literature fails to support elective surgery after a second episode. Sixty-eight percent to 96% of patients requiring surgery for diverticulitis-associated perforation or abscess had no previous symptoms and couldn’t be helped by prophylactic surgery,5 and diverticulitis symptoms persisted after bowel resection in 27% to 33% of patients.5
One large retrospective study followed 3165 patients for 6 to 12 years after hospitalization for diverticulitis. Of the patients treated nonoperatively, 13% had a single recurrence and 4% had multiple recurrences; the annual recurrence rate was approximately 2%. The authors concluded that routine elective colectomy is rarely indicated after a first episode of uncomplicated acute diverticulitis.6
A decision analysis using a Markov model found that performing a colectomy after a fourth, rather than a second, episode of diverticulitis would result in somewhat fewer deaths and colostomies, equivalent quality-adjusted years of life, and cost savings per patient of $1035 to $5429. The results held for both older and younger patients.7
Recommendations
The American Society of Colon and Rectal Surgeons (ASCRS) concludes that recommendations for elective sigmoid colectomy after recovery from acute diverticulitis should be made on a case-by-case basis.8 Computed tomography to grade the severity of a first attack may help determine the need for surgery. The ASCRS guidelines mention that long-term fiber supplementation may prevent recurrences of diverticulitis in most patients.
The American College of Gastroenterology Practice Parameters Committee states that prophylactic surgery may be recommended for recurrent attacks of diverticulitis, but generally isn’t indicated after a single uncomplicated episode.9 The group also notes that high-fiber diets may decrease the development of colonic diverticulosis, but no consistent data exist regarding fiber to prevent recurrent diverticulitis.
1. Eglash A, Lane CH, Schneider D. What is the most beneficial diet for patients with diverticulosis? J Fam Pract. 2006;55:813-815.
2. Humes D, Simpson J, Spiller R. Colonic diverticular disease. BMJ Clin Evid. 2008;01:405-416.
3. Strate LL, Liu YL, Syngal S, et al. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300:907-914.
4. Dughera L, Serra AM, Battaglia E, et al. Acute recurrent diverticulitis is prevented by oral administration of a polybacterial lysate suspension. Minerva Gastroenterol Dietol. 2004;50:149-153.
5. Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg. 2005;92:133-142.
6. Broderick-Villa G, Burchette RJ, Collins JC, et al. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576-581.
7. Salem L, Veenstra DL, Sullivan SD, et al. The timing of elective colectomy in diverticulitis: a decision analysis. J Am Coll Surg. 2004;199:904-912.
8. Rafferty J, Shellito P, Hyman NH, et al. Standards Committee of the American Society of Colon and Rectal Surgeons. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939-944.
9. Stollman N, Raskin L. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121.
A high-fiber diet may help; available evidence doesn’t support other interventions. A high-fiber diet is often prescribed after recovery from acute diverticulitis, based on extrapolation from epidemiologic data showing an association between low-fiber diets and diverticulosis (strength of recommendation [SOR]: C, expert opinion). No direct evidence establishes a role for fiber in preventing recurrent diverticulitis, however.
No evidence supports the common advice to avoid nuts and seeds to prevent diverticulitis. Eating nuts, corn, and popcorn doesn’t increase the risk; in fact, nuts and popcorn may have a protective effect (SOR: B, large cohort study).
There isn’t enough evidence to recommend the anti-inflammatory drug mesalamine or a polybacterial lysate for immunostimulation. Retrospective data don’t support routine prophylactic colectomy after 1 or 2 episodes of acute diverticulitis (SOR: B, observational studies).
Evidence summary
A 2006 Family Physicians Inquiries Network Clinical Inquiry on diverticulosis found inconsistent evidence that fiber decreases the risk of symptomatic diverticular disease (SOR: C, case control studies and a large prospective cohort study).1
A 2007 literature review found no systematic reviews or randomized controlled trials (RCTs) of fiber for preventing complications of diverticular disease. The reviewers noted that observational studies have found less diverticulosis in populations with higher fiber consumption.2
Nuts, popcorn may be protective
A trial conducted as part of a large prospective cohort study—the Health Professionals Follow-up Study—followed 47,228 male health professionals in the United States, ages 40 to 75 years, from 1986 to 2004.3 The subjects, all of whom returned a food-frequency questionnaire, were at baseline free of diverticulosis and related complications, cancer, and inflammatory bowel disease. During the follow-up period, 801 cases of diverticulitis and 383 cases of diverticular bleeding (the main outcome measures) occurred.
The investigators found an inverse association between consumption of nuts and popcorn and risk of diverticulitis. Men with the highest intake of each food (at least twice per week) compared with men with the lowest intake (less than once per month) had a hazard ratio of 0.80 (95% confidence interval [CI], 0.63-1.01; P for trend=.04) for nuts and 0.72 (95% CI, 0.56-0.92; P for trend=.007) for popcorn. No association was noted between corn consumption and diverticulitis or between nut, corn, or popcorn consumption and diverticular bleeding or uncomplicated diverticulosis.
Mesalamine’s efficacy is unknown
A 2007 systematic review found 1 RCT of the anti-inflammatory drug mesalamine (mesalazine, 5-aminosalicylic acid) for preventing diverticulitis. Mesalamine reduced the recurrence rate of diverticulitis from 46% to 15% among 166 subjects.
The reviewers judged the study to be flawed by unreported diagnostic criteria and a high withdrawal rate. They concluded that the effectiveness of mesalamine remains unknown.2
1 small study of oral enterovaccine
An oral polybacterial lysate suspension designed to stimulate gut secretion of immunoglobulin A was investigated in a study of 83 patients with recurrent diverticulitis. In the treated group, 4.6% (2/43) of patients had recurrent diverticulitis during the 3 months of the study, compared with 12.5% (5/40) of the untreated group (P<.05).4
Prophylactic surgery rarely helps
No randomized trials have compared surgical with medical therapy to prevent recurrent diverticulitis. Extensive retrospective literature fails to support elective surgery after a second episode. Sixty-eight percent to 96% of patients requiring surgery for diverticulitis-associated perforation or abscess had no previous symptoms and couldn’t be helped by prophylactic surgery,5 and diverticulitis symptoms persisted after bowel resection in 27% to 33% of patients.5
One large retrospective study followed 3165 patients for 6 to 12 years after hospitalization for diverticulitis. Of the patients treated nonoperatively, 13% had a single recurrence and 4% had multiple recurrences; the annual recurrence rate was approximately 2%. The authors concluded that routine elective colectomy is rarely indicated after a first episode of uncomplicated acute diverticulitis.6
A decision analysis using a Markov model found that performing a colectomy after a fourth, rather than a second, episode of diverticulitis would result in somewhat fewer deaths and colostomies, equivalent quality-adjusted years of life, and cost savings per patient of $1035 to $5429. The results held for both older and younger patients.7
Recommendations
The American Society of Colon and Rectal Surgeons (ASCRS) concludes that recommendations for elective sigmoid colectomy after recovery from acute diverticulitis should be made on a case-by-case basis.8 Computed tomography to grade the severity of a first attack may help determine the need for surgery. The ASCRS guidelines mention that long-term fiber supplementation may prevent recurrences of diverticulitis in most patients.
The American College of Gastroenterology Practice Parameters Committee states that prophylactic surgery may be recommended for recurrent attacks of diverticulitis, but generally isn’t indicated after a single uncomplicated episode.9 The group also notes that high-fiber diets may decrease the development of colonic diverticulosis, but no consistent data exist regarding fiber to prevent recurrent diverticulitis.
A high-fiber diet may help; available evidence doesn’t support other interventions. A high-fiber diet is often prescribed after recovery from acute diverticulitis, based on extrapolation from epidemiologic data showing an association between low-fiber diets and diverticulosis (strength of recommendation [SOR]: C, expert opinion). No direct evidence establishes a role for fiber in preventing recurrent diverticulitis, however.
No evidence supports the common advice to avoid nuts and seeds to prevent diverticulitis. Eating nuts, corn, and popcorn doesn’t increase the risk; in fact, nuts and popcorn may have a protective effect (SOR: B, large cohort study).
There isn’t enough evidence to recommend the anti-inflammatory drug mesalamine or a polybacterial lysate for immunostimulation. Retrospective data don’t support routine prophylactic colectomy after 1 or 2 episodes of acute diverticulitis (SOR: B, observational studies).
Evidence summary
A 2006 Family Physicians Inquiries Network Clinical Inquiry on diverticulosis found inconsistent evidence that fiber decreases the risk of symptomatic diverticular disease (SOR: C, case control studies and a large prospective cohort study).1
A 2007 literature review found no systematic reviews or randomized controlled trials (RCTs) of fiber for preventing complications of diverticular disease. The reviewers noted that observational studies have found less diverticulosis in populations with higher fiber consumption.2
Nuts, popcorn may be protective
A trial conducted as part of a large prospective cohort study—the Health Professionals Follow-up Study—followed 47,228 male health professionals in the United States, ages 40 to 75 years, from 1986 to 2004.3 The subjects, all of whom returned a food-frequency questionnaire, were at baseline free of diverticulosis and related complications, cancer, and inflammatory bowel disease. During the follow-up period, 801 cases of diverticulitis and 383 cases of diverticular bleeding (the main outcome measures) occurred.
The investigators found an inverse association between consumption of nuts and popcorn and risk of diverticulitis. Men with the highest intake of each food (at least twice per week) compared with men with the lowest intake (less than once per month) had a hazard ratio of 0.80 (95% confidence interval [CI], 0.63-1.01; P for trend=.04) for nuts and 0.72 (95% CI, 0.56-0.92; P for trend=.007) for popcorn. No association was noted between corn consumption and diverticulitis or between nut, corn, or popcorn consumption and diverticular bleeding or uncomplicated diverticulosis.
Mesalamine’s efficacy is unknown
A 2007 systematic review found 1 RCT of the anti-inflammatory drug mesalamine (mesalazine, 5-aminosalicylic acid) for preventing diverticulitis. Mesalamine reduced the recurrence rate of diverticulitis from 46% to 15% among 166 subjects.
The reviewers judged the study to be flawed by unreported diagnostic criteria and a high withdrawal rate. They concluded that the effectiveness of mesalamine remains unknown.2
1 small study of oral enterovaccine
An oral polybacterial lysate suspension designed to stimulate gut secretion of immunoglobulin A was investigated in a study of 83 patients with recurrent diverticulitis. In the treated group, 4.6% (2/43) of patients had recurrent diverticulitis during the 3 months of the study, compared with 12.5% (5/40) of the untreated group (P<.05).4
Prophylactic surgery rarely helps
No randomized trials have compared surgical with medical therapy to prevent recurrent diverticulitis. Extensive retrospective literature fails to support elective surgery after a second episode. Sixty-eight percent to 96% of patients requiring surgery for diverticulitis-associated perforation or abscess had no previous symptoms and couldn’t be helped by prophylactic surgery,5 and diverticulitis symptoms persisted after bowel resection in 27% to 33% of patients.5
One large retrospective study followed 3165 patients for 6 to 12 years after hospitalization for diverticulitis. Of the patients treated nonoperatively, 13% had a single recurrence and 4% had multiple recurrences; the annual recurrence rate was approximately 2%. The authors concluded that routine elective colectomy is rarely indicated after a first episode of uncomplicated acute diverticulitis.6
A decision analysis using a Markov model found that performing a colectomy after a fourth, rather than a second, episode of diverticulitis would result in somewhat fewer deaths and colostomies, equivalent quality-adjusted years of life, and cost savings per patient of $1035 to $5429. The results held for both older and younger patients.7
Recommendations
The American Society of Colon and Rectal Surgeons (ASCRS) concludes that recommendations for elective sigmoid colectomy after recovery from acute diverticulitis should be made on a case-by-case basis.8 Computed tomography to grade the severity of a first attack may help determine the need for surgery. The ASCRS guidelines mention that long-term fiber supplementation may prevent recurrences of diverticulitis in most patients.
The American College of Gastroenterology Practice Parameters Committee states that prophylactic surgery may be recommended for recurrent attacks of diverticulitis, but generally isn’t indicated after a single uncomplicated episode.9 The group also notes that high-fiber diets may decrease the development of colonic diverticulosis, but no consistent data exist regarding fiber to prevent recurrent diverticulitis.
1. Eglash A, Lane CH, Schneider D. What is the most beneficial diet for patients with diverticulosis? J Fam Pract. 2006;55:813-815.
2. Humes D, Simpson J, Spiller R. Colonic diverticular disease. BMJ Clin Evid. 2008;01:405-416.
3. Strate LL, Liu YL, Syngal S, et al. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300:907-914.
4. Dughera L, Serra AM, Battaglia E, et al. Acute recurrent diverticulitis is prevented by oral administration of a polybacterial lysate suspension. Minerva Gastroenterol Dietol. 2004;50:149-153.
5. Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg. 2005;92:133-142.
6. Broderick-Villa G, Burchette RJ, Collins JC, et al. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576-581.
7. Salem L, Veenstra DL, Sullivan SD, et al. The timing of elective colectomy in diverticulitis: a decision analysis. J Am Coll Surg. 2004;199:904-912.
8. Rafferty J, Shellito P, Hyman NH, et al. Standards Committee of the American Society of Colon and Rectal Surgeons. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939-944.
9. Stollman N, Raskin L. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121.
1. Eglash A, Lane CH, Schneider D. What is the most beneficial diet for patients with diverticulosis? J Fam Pract. 2006;55:813-815.
2. Humes D, Simpson J, Spiller R. Colonic diverticular disease. BMJ Clin Evid. 2008;01:405-416.
3. Strate LL, Liu YL, Syngal S, et al. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300:907-914.
4. Dughera L, Serra AM, Battaglia E, et al. Acute recurrent diverticulitis is prevented by oral administration of a polybacterial lysate suspension. Minerva Gastroenterol Dietol. 2004;50:149-153.
5. Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg. 2005;92:133-142.
6. Broderick-Villa G, Burchette RJ, Collins JC, et al. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576-581.
7. Salem L, Veenstra DL, Sullivan SD, et al. The timing of elective colectomy in diverticulitis: a decision analysis. J Am Coll Surg. 2004;199:904-912.
8. Rafferty J, Shellito P, Hyman NH, et al. Standards Committee of the American Society of Colon and Rectal Surgeons. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939-944.
9. Stollman N, Raskin L. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121.
Evidence-based answers from the Family Physicians Inquiries Network