User login
Childhood alopecia areata: What treatment works best?
IT’S UNCLEAR; there are no validated effective treatments for alopecia areata (AA). Topical immunotherapy (squaric acid dibutylester [SADBE] and diphenylcyclopropenone [DPCP]) induces the most signifi cant short-term hair regrowth in children with severe AA (strength of recommendation [SOR]: C, 4 small individual cohort studies and 1 moderately sized retrospective case review). Intralesional steroids can induce hair regrowth greater than 50% in children with limited AA (SOR: C, 1 retrospective cohort study).
Other commonly used treatments—topical and oral corticosteroids, topical cyclosporine, photodynamic therapy, and topical minoxidil—have no benefit over placebo (SOR: A, 14 randomized controlled trials [RCTs] and 3 within-patient studies).
Evidence summary
AA is a common inflammatory condition that causes hair loss and subsequent social consequences. Spontaneous remission occurs in 34% to 50% of patients within 1 year.1 Many trials of commonly used AA treatments have identified no significant patient benefits. A 2008 Cochrane review that examined 17 studies (14 RCTs and 3 within-patient studies) of AA interventions in 540 participants found no clinically significant hair regrowth (>50%) when patients were treated with topical corticosteroids, cyclosporine, minoxidil, photodynamic therapy, or oral corticosteroids.2
Documenting patient outcomes is problematic because of spontaneous resolution and frequent relapses.2 Moreover, few quality-controlled trials have studied children, and no long-term, randomized outcome trials of AA treatments exist.
Intralesional steroids and SADBE show results
In a moderately sized retrospective cohort study in Singapore (392 patients <16 years), 57% of patients experienced more than 50% improvement after 12 weeks of intralesional steroids for limited AA, and 75% showed similar improvement after 24 weeks. Of 43 children treated with anthralin, only 10 with limited AA showed more than 50% clinical improvement within 6 months.3 Fifty-four patients with extensive AA received SADBE; 74% experienced greater than 50% hair regrowth at 6 months.3
SADBE effects aren’t long-lived
A 1996 individual cohort study of 33 children (6*#8211;14 years of age) with extensive AA who were treated with SADBE once a week for a year showed a complete regrowth rate of 30.3%. Only 9% of the children maintained total or partial regrowth during long-term follow-up (mean 6 years), however.4
In another individual cohort study, 28 pediatric patients with extensive AA had mixed results with 2% SADBE used once a week for a year.5 Nine patients (32.1%) showed total or acceptable hair growth; 6 (21.4%) had diffuse regrowth but thinner than normal hair. Eighty-seven percent of patients relapsed within 6 months of discontinuing therapy.5
Studies of DPCP are too small
A 1996 small individual cohort investigation recorded a 40% response rate (90%–100% regrowth) to DPCP in 10 pediatric patients with extensive AA who were treated for an average of 8.6 months. The same study found cosmetically acceptable growth in 27% of patients (4 of 15 patients 4–15 years of age) treated for an average of 9.6 months.6
A small individual study of DPCP reported complete regrowth in 4 of 12 (33%) children with extensive AA; growth persisted at 6 months in 3 of the 4 responders.7 Another cohort study reported a 50% response rate (>80% regrowth) using DPCP in 10 patients (11–14 years of age) with extensive disease.8
Use SADBE and DPCP with caution
SADBE and DPCP are unlicensed treatments that can cause occipital and cervical lymphadenopathy, severe dermatitis (minimized by careful titration), urticaria, and hypo- or hyperpigmentation disorders (especially in racially pigmented patients). These agents shouldn’t be used during pregnancy and should be applied using gloves and aprons to avoid allergic contact dermatitis.
In light of these cautions, and handling and storage limitations, SADBE and DPCP should be reserved for patients with extensive disease (after obtaining signed informed consent). Patients should avoid ultraviolet light for 24 to 48 hours after application to avoid degradation of the medication.
Recommendations
The National Alopecia Areata Foundation and the American Academy of Dermatology recommend corticosteroids, topical minoxidil, and anthralin to treat AA.9,10
The British Association of Dermatologists’ guidelines for managing AA advise using intralesional corticosteroids for limited AA and contact immunotherapy for more extensive disease.1 They also note that intralesional corticosteroids are poorly tolerated and clinicians are reluctant to use contact immunotherapy in children.
Acknowledgements
The opinions and assertions contained herein are the private views of the author and are not to be construed as official, or as reflecting the views of the United States Air Force Medical Service or the US Air Force at large.
1. MacDonald Hull SP, Wood ML, Hutchinson PE, et al. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149:692-699.
2. Delamere FM, Sladden MJ, Dobbins HM, et al. Interventions for alopecia areata. Cochrane Database Syst Rev. 2008;(2):CD004413.-
3. Tan E, Tay YK, Giam YC. A clinical study of childhood alopecia areata in Singapore. Pediatr Dermatol. 2002;19:298-301.
4. Tosti A, Guidetti MS, Bardazzi F, et al. Long-term results of topical immunotherapy in children with alopecia totalis or alopecia universalis. J Am Acad Dermatol. 1996;35:199-201.
5. Orecchia G, Malagoli P, Santagostino L. Treatment of severe alopecia areata with squaric acid dibutylester in pediatric patients. Pediatr Dermatol. 1994;11:65-68.
6. Schuttelaar ML, Hamstra JJ, Plinck EP, et al. Alopecia areata in children: treatment with diphencyprone. Br J Dermatol. 1996;135:581-585.
7. Hull SM, Pepall L, Cunliffe WJ. Alopecia areata in children: response to treatment with diphencyprone. Br J Dermatol. 1991;125:164-168.
8. Sotiriadis D, Patsatsi A, Lazaridou E, et al. Topical immunotherapy with diphenylcyclopropenone in the treatment of chronic extensive alopecia areata. Clin Exp Dermatol. 2007;32:48-51.
9. National Alopecia Areata Foundation. Treatment recommendations. Available at: www.naaf.org/site/PageServer?pagename=about_alopecia_treatment.html. Accessed December 17, 2010.
10. American Academy of Dermatology. Alopecia areata. Available at: http://www.aad.org/public/publications/pamphlets/common_alopecia.html. Accessed December 17, 2010.
IT’S UNCLEAR; there are no validated effective treatments for alopecia areata (AA). Topical immunotherapy (squaric acid dibutylester [SADBE] and diphenylcyclopropenone [DPCP]) induces the most signifi cant short-term hair regrowth in children with severe AA (strength of recommendation [SOR]: C, 4 small individual cohort studies and 1 moderately sized retrospective case review). Intralesional steroids can induce hair regrowth greater than 50% in children with limited AA (SOR: C, 1 retrospective cohort study).
Other commonly used treatments—topical and oral corticosteroids, topical cyclosporine, photodynamic therapy, and topical minoxidil—have no benefit over placebo (SOR: A, 14 randomized controlled trials [RCTs] and 3 within-patient studies).
Evidence summary
AA is a common inflammatory condition that causes hair loss and subsequent social consequences. Spontaneous remission occurs in 34% to 50% of patients within 1 year.1 Many trials of commonly used AA treatments have identified no significant patient benefits. A 2008 Cochrane review that examined 17 studies (14 RCTs and 3 within-patient studies) of AA interventions in 540 participants found no clinically significant hair regrowth (>50%) when patients were treated with topical corticosteroids, cyclosporine, minoxidil, photodynamic therapy, or oral corticosteroids.2
Documenting patient outcomes is problematic because of spontaneous resolution and frequent relapses.2 Moreover, few quality-controlled trials have studied children, and no long-term, randomized outcome trials of AA treatments exist.
Intralesional steroids and SADBE show results
In a moderately sized retrospective cohort study in Singapore (392 patients <16 years), 57% of patients experienced more than 50% improvement after 12 weeks of intralesional steroids for limited AA, and 75% showed similar improvement after 24 weeks. Of 43 children treated with anthralin, only 10 with limited AA showed more than 50% clinical improvement within 6 months.3 Fifty-four patients with extensive AA received SADBE; 74% experienced greater than 50% hair regrowth at 6 months.3
SADBE effects aren’t long-lived
A 1996 individual cohort study of 33 children (6*#8211;14 years of age) with extensive AA who were treated with SADBE once a week for a year showed a complete regrowth rate of 30.3%. Only 9% of the children maintained total or partial regrowth during long-term follow-up (mean 6 years), however.4
In another individual cohort study, 28 pediatric patients with extensive AA had mixed results with 2% SADBE used once a week for a year.5 Nine patients (32.1%) showed total or acceptable hair growth; 6 (21.4%) had diffuse regrowth but thinner than normal hair. Eighty-seven percent of patients relapsed within 6 months of discontinuing therapy.5
Studies of DPCP are too small
A 1996 small individual cohort investigation recorded a 40% response rate (90%–100% regrowth) to DPCP in 10 pediatric patients with extensive AA who were treated for an average of 8.6 months. The same study found cosmetically acceptable growth in 27% of patients (4 of 15 patients 4–15 years of age) treated for an average of 9.6 months.6
A small individual study of DPCP reported complete regrowth in 4 of 12 (33%) children with extensive AA; growth persisted at 6 months in 3 of the 4 responders.7 Another cohort study reported a 50% response rate (>80% regrowth) using DPCP in 10 patients (11–14 years of age) with extensive disease.8
Use SADBE and DPCP with caution
SADBE and DPCP are unlicensed treatments that can cause occipital and cervical lymphadenopathy, severe dermatitis (minimized by careful titration), urticaria, and hypo- or hyperpigmentation disorders (especially in racially pigmented patients). These agents shouldn’t be used during pregnancy and should be applied using gloves and aprons to avoid allergic contact dermatitis.
In light of these cautions, and handling and storage limitations, SADBE and DPCP should be reserved for patients with extensive disease (after obtaining signed informed consent). Patients should avoid ultraviolet light for 24 to 48 hours after application to avoid degradation of the medication.
Recommendations
The National Alopecia Areata Foundation and the American Academy of Dermatology recommend corticosteroids, topical minoxidil, and anthralin to treat AA.9,10
The British Association of Dermatologists’ guidelines for managing AA advise using intralesional corticosteroids for limited AA and contact immunotherapy for more extensive disease.1 They also note that intralesional corticosteroids are poorly tolerated and clinicians are reluctant to use contact immunotherapy in children.
Acknowledgements
The opinions and assertions contained herein are the private views of the author and are not to be construed as official, or as reflecting the views of the United States Air Force Medical Service or the US Air Force at large.
IT’S UNCLEAR; there are no validated effective treatments for alopecia areata (AA). Topical immunotherapy (squaric acid dibutylester [SADBE] and diphenylcyclopropenone [DPCP]) induces the most signifi cant short-term hair regrowth in children with severe AA (strength of recommendation [SOR]: C, 4 small individual cohort studies and 1 moderately sized retrospective case review). Intralesional steroids can induce hair regrowth greater than 50% in children with limited AA (SOR: C, 1 retrospective cohort study).
Other commonly used treatments—topical and oral corticosteroids, topical cyclosporine, photodynamic therapy, and topical minoxidil—have no benefit over placebo (SOR: A, 14 randomized controlled trials [RCTs] and 3 within-patient studies).
Evidence summary
AA is a common inflammatory condition that causes hair loss and subsequent social consequences. Spontaneous remission occurs in 34% to 50% of patients within 1 year.1 Many trials of commonly used AA treatments have identified no significant patient benefits. A 2008 Cochrane review that examined 17 studies (14 RCTs and 3 within-patient studies) of AA interventions in 540 participants found no clinically significant hair regrowth (>50%) when patients were treated with topical corticosteroids, cyclosporine, minoxidil, photodynamic therapy, or oral corticosteroids.2
Documenting patient outcomes is problematic because of spontaneous resolution and frequent relapses.2 Moreover, few quality-controlled trials have studied children, and no long-term, randomized outcome trials of AA treatments exist.
Intralesional steroids and SADBE show results
In a moderately sized retrospective cohort study in Singapore (392 patients <16 years), 57% of patients experienced more than 50% improvement after 12 weeks of intralesional steroids for limited AA, and 75% showed similar improvement after 24 weeks. Of 43 children treated with anthralin, only 10 with limited AA showed more than 50% clinical improvement within 6 months.3 Fifty-four patients with extensive AA received SADBE; 74% experienced greater than 50% hair regrowth at 6 months.3
SADBE effects aren’t long-lived
A 1996 individual cohort study of 33 children (6*#8211;14 years of age) with extensive AA who were treated with SADBE once a week for a year showed a complete regrowth rate of 30.3%. Only 9% of the children maintained total or partial regrowth during long-term follow-up (mean 6 years), however.4
In another individual cohort study, 28 pediatric patients with extensive AA had mixed results with 2% SADBE used once a week for a year.5 Nine patients (32.1%) showed total or acceptable hair growth; 6 (21.4%) had diffuse regrowth but thinner than normal hair. Eighty-seven percent of patients relapsed within 6 months of discontinuing therapy.5
Studies of DPCP are too small
A 1996 small individual cohort investigation recorded a 40% response rate (90%–100% regrowth) to DPCP in 10 pediatric patients with extensive AA who were treated for an average of 8.6 months. The same study found cosmetically acceptable growth in 27% of patients (4 of 15 patients 4–15 years of age) treated for an average of 9.6 months.6
A small individual study of DPCP reported complete regrowth in 4 of 12 (33%) children with extensive AA; growth persisted at 6 months in 3 of the 4 responders.7 Another cohort study reported a 50% response rate (>80% regrowth) using DPCP in 10 patients (11–14 years of age) with extensive disease.8
Use SADBE and DPCP with caution
SADBE and DPCP are unlicensed treatments that can cause occipital and cervical lymphadenopathy, severe dermatitis (minimized by careful titration), urticaria, and hypo- or hyperpigmentation disorders (especially in racially pigmented patients). These agents shouldn’t be used during pregnancy and should be applied using gloves and aprons to avoid allergic contact dermatitis.
In light of these cautions, and handling and storage limitations, SADBE and DPCP should be reserved for patients with extensive disease (after obtaining signed informed consent). Patients should avoid ultraviolet light for 24 to 48 hours after application to avoid degradation of the medication.
Recommendations
The National Alopecia Areata Foundation and the American Academy of Dermatology recommend corticosteroids, topical minoxidil, and anthralin to treat AA.9,10
The British Association of Dermatologists’ guidelines for managing AA advise using intralesional corticosteroids for limited AA and contact immunotherapy for more extensive disease.1 They also note that intralesional corticosteroids are poorly tolerated and clinicians are reluctant to use contact immunotherapy in children.
Acknowledgements
The opinions and assertions contained herein are the private views of the author and are not to be construed as official, or as reflecting the views of the United States Air Force Medical Service or the US Air Force at large.
1. MacDonald Hull SP, Wood ML, Hutchinson PE, et al. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149:692-699.
2. Delamere FM, Sladden MJ, Dobbins HM, et al. Interventions for alopecia areata. Cochrane Database Syst Rev. 2008;(2):CD004413.-
3. Tan E, Tay YK, Giam YC. A clinical study of childhood alopecia areata in Singapore. Pediatr Dermatol. 2002;19:298-301.
4. Tosti A, Guidetti MS, Bardazzi F, et al. Long-term results of topical immunotherapy in children with alopecia totalis or alopecia universalis. J Am Acad Dermatol. 1996;35:199-201.
5. Orecchia G, Malagoli P, Santagostino L. Treatment of severe alopecia areata with squaric acid dibutylester in pediatric patients. Pediatr Dermatol. 1994;11:65-68.
6. Schuttelaar ML, Hamstra JJ, Plinck EP, et al. Alopecia areata in children: treatment with diphencyprone. Br J Dermatol. 1996;135:581-585.
7. Hull SM, Pepall L, Cunliffe WJ. Alopecia areata in children: response to treatment with diphencyprone. Br J Dermatol. 1991;125:164-168.
8. Sotiriadis D, Patsatsi A, Lazaridou E, et al. Topical immunotherapy with diphenylcyclopropenone in the treatment of chronic extensive alopecia areata. Clin Exp Dermatol. 2007;32:48-51.
9. National Alopecia Areata Foundation. Treatment recommendations. Available at: www.naaf.org/site/PageServer?pagename=about_alopecia_treatment.html. Accessed December 17, 2010.
10. American Academy of Dermatology. Alopecia areata. Available at: http://www.aad.org/public/publications/pamphlets/common_alopecia.html. Accessed December 17, 2010.
1. MacDonald Hull SP, Wood ML, Hutchinson PE, et al. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149:692-699.
2. Delamere FM, Sladden MJ, Dobbins HM, et al. Interventions for alopecia areata. Cochrane Database Syst Rev. 2008;(2):CD004413.-
3. Tan E, Tay YK, Giam YC. A clinical study of childhood alopecia areata in Singapore. Pediatr Dermatol. 2002;19:298-301.
4. Tosti A, Guidetti MS, Bardazzi F, et al. Long-term results of topical immunotherapy in children with alopecia totalis or alopecia universalis. J Am Acad Dermatol. 1996;35:199-201.
5. Orecchia G, Malagoli P, Santagostino L. Treatment of severe alopecia areata with squaric acid dibutylester in pediatric patients. Pediatr Dermatol. 1994;11:65-68.
6. Schuttelaar ML, Hamstra JJ, Plinck EP, et al. Alopecia areata in children: treatment with diphencyprone. Br J Dermatol. 1996;135:581-585.
7. Hull SM, Pepall L, Cunliffe WJ. Alopecia areata in children: response to treatment with diphencyprone. Br J Dermatol. 1991;125:164-168.
8. Sotiriadis D, Patsatsi A, Lazaridou E, et al. Topical immunotherapy with diphenylcyclopropenone in the treatment of chronic extensive alopecia areata. Clin Exp Dermatol. 2007;32:48-51.
9. National Alopecia Areata Foundation. Treatment recommendations. Available at: www.naaf.org/site/PageServer?pagename=about_alopecia_treatment.html. Accessed December 17, 2010.
10. American Academy of Dermatology. Alopecia areata. Available at: http://www.aad.org/public/publications/pamphlets/common_alopecia.html. Accessed December 17, 2010.
Evidence-based answers from the Family Physicians Inquiries Network
How does electronic fetal heart rate monitoring affect labor and delivery outcomes?
CONTINUOUS ELECTRONIC FETAL MONITORING (EFM) REDUCES THE RISK OF NEONATAL SEIZURE BY 50% compared with intermittent auscultation (IA) (strength of recommendation [SOR]: A, systematic review of randomized controlled trials [RCTs]).
EFM increases the incidence of cesarean section by 66% and the incidence of operative vaginal delivery by 16% (SOR: A, systematic review of RCTs). It has no effect on the rates of cerebral palsy or neonatal mortality (SOR: A, systematic review of RCTs).
An estimate from a Cochrane meta-analysis suggests that a cohort of 628 women receiving EFM could expect to experience 1 less neonatal seizure and 11 more cesarean sections compared with IA controls.
Evidence summary
Continuous EFM is designed to detect early fetal hypoxia and thereby decrease neonatal morbidity and mortality compared with IA. IA is defined as auscultation of the fetal heart rate for at least 60 seconds every 15 minutes during the first stage of labor and every 5 minutes during the second stage of labor.
A decrease in seizures, but not deaths or cerebral palsy
A 2006 Cochrane systematic review examined 12 RCTs (with >37,000 women) that compared continuous EFM with IA.1 Continuous EFM reduced the risk of neonatal seizure by 50% (relative risk [RR]=0.50; 95% confidence interval [CI], 0.31-0.80), but had no effect on the rate of neonatal death (RR=0.85; 95% CI, 0.59-1.23) or development of cerebral palsy (RR=1.74; 95% CI, 0.97-3.11).
Reduction of seizures was consistent across all trials. However, a subgroup analysis of high-risk pregnancies (advanced maternal age, diabetes mellitus, chronic hypertension, renal disease, preeclampsia, cardiac disease, renal disease, previous delivery of a low-birth-weight infant) didn’t find a statistically significant decrease in seizures.
Cesarean deliveries rise, regardless of patient risk status
Continuous EFM raised the rates of cesarean delivery (RR=1.66; 95% CI, 1.30-2.13) and instrumental vaginal deliveries (RR=1.16; 95% CI, 1.01-1.32). The increased rate of cesarean section in the EFM group was consistent regardless of clinical risk status (low- vs high-risk women). One additional cesarean section was performed for every 58 women monitored continuously. For “high-risk” women, 1 additional cesarean section was performed for every 12 women monitored continuously.1
Cesarean section rates varied widely among the individual trials (2.3%-35%). Analysis suggested that studies with higher baseline rates showed the greatest increases with continuous EFM. The rate for all studies combined was just 4.3%; 69% of patients included in the meta-analysis were contributed by the Dublin trial, which had an average cesarean rate of 2.3%.1 By comparison, the US Division of Vital Statistics reported a cesarean rate of 32.3% in 2008.2
EFM reduces death from fetal hypoxia
A 1995 meta-analysis, including 9 of the Cochrane review studies with a total of 18,561 women, evaluated the additional outcome of death resulting from fetal hypoxia.3 Compared with IA, EFM was associated with a 59% reduction in death from fetal hypoxia (RR=0.41; 95% CI, 0.17-0.98). Continuous EFM prevented 1 perinatal death per 1000 births. The reduction in perinatal mortality was offset by a 53% increase in cesarean deliveries and a 23% increase in operative vaginal deliveries.3
Recommendations
The American College of Obstetricians and Gynecologists (ACOG) doesn’t recommend for or against continuous fetal heart rate monitoring in uncomplicated labor, recognizing either EFM or IA as acceptable in uncomplicated patients.4 ACOG does recommend continuous EFM for women with high-risk conditions (suspected fetal growth restriction, preeclampsia, and type 1 diabetes mellitus).
The US Preventive Services Task Force doesn’t support routine intrapartum EFM for low-risk woman. The Task Force found insufficient evidence for using EFM in high-risk pregnancies.5
The Royal College of Obstetricians and Gynaecologists and the Royal Australian and New Zealand College of Obstetricians and Gynecologists both recommend continuous EFM for high-risk women and IA for low-risk patients.6,7
Acknowledgements
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the US Army Medical Department or the US Army at large.
1. Alfirevic Z, Devane D, Gyte GM. Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database Syst Rev. 2006;(3):CD006066.-
2. Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2008. Natl Vital Stat Rep. 2010;58(16):1-18.
3. Vintzileos AM, Nochimson DJ, Guzman ER, et al. Intrapartum electronic heart rate monitoring versus intermittent auscultation: a meta-analysis. Obstet Gynecol. 1995;85:149-155.
4. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin. Clinical Management Guidelines for Obstetrician-Gynecologists, Number 106, July 2009. Intrapartum fetal heart rate monitoring: Nomenclature, interpretation, and general management principles. Obstet Gynecol. 2009;114:192-202.
5. US Preventive Services Task Force. Screening for intrapartum electronic fetal monitoring. Rockville, MD: Agency for Healthcare Research and Quality; 1996. Available at: www.ahrq.gov/clinic/uspstf/uspsiefm.htm. Accessed March 7, 2010.
6. National Institute for Health and Clinical Excellence (NICE). Intrapartum Care: Management and Delivery of Care to Women in Labour. London: NICE; 2007.
7. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Clinical Guidelines. Intrapartum Fetal Surveillance Guidelines. May 2006. Available at: www.ranzcog.edu.au/publications/womenshealth.shtml. Accessed December 9, 2008.
CONTINUOUS ELECTRONIC FETAL MONITORING (EFM) REDUCES THE RISK OF NEONATAL SEIZURE BY 50% compared with intermittent auscultation (IA) (strength of recommendation [SOR]: A, systematic review of randomized controlled trials [RCTs]).
EFM increases the incidence of cesarean section by 66% and the incidence of operative vaginal delivery by 16% (SOR: A, systematic review of RCTs). It has no effect on the rates of cerebral palsy or neonatal mortality (SOR: A, systematic review of RCTs).
An estimate from a Cochrane meta-analysis suggests that a cohort of 628 women receiving EFM could expect to experience 1 less neonatal seizure and 11 more cesarean sections compared with IA controls.
Evidence summary
Continuous EFM is designed to detect early fetal hypoxia and thereby decrease neonatal morbidity and mortality compared with IA. IA is defined as auscultation of the fetal heart rate for at least 60 seconds every 15 minutes during the first stage of labor and every 5 minutes during the second stage of labor.
A decrease in seizures, but not deaths or cerebral palsy
A 2006 Cochrane systematic review examined 12 RCTs (with >37,000 women) that compared continuous EFM with IA.1 Continuous EFM reduced the risk of neonatal seizure by 50% (relative risk [RR]=0.50; 95% confidence interval [CI], 0.31-0.80), but had no effect on the rate of neonatal death (RR=0.85; 95% CI, 0.59-1.23) or development of cerebral palsy (RR=1.74; 95% CI, 0.97-3.11).
Reduction of seizures was consistent across all trials. However, a subgroup analysis of high-risk pregnancies (advanced maternal age, diabetes mellitus, chronic hypertension, renal disease, preeclampsia, cardiac disease, renal disease, previous delivery of a low-birth-weight infant) didn’t find a statistically significant decrease in seizures.
Cesarean deliveries rise, regardless of patient risk status
Continuous EFM raised the rates of cesarean delivery (RR=1.66; 95% CI, 1.30-2.13) and instrumental vaginal deliveries (RR=1.16; 95% CI, 1.01-1.32). The increased rate of cesarean section in the EFM group was consistent regardless of clinical risk status (low- vs high-risk women). One additional cesarean section was performed for every 58 women monitored continuously. For “high-risk” women, 1 additional cesarean section was performed for every 12 women monitored continuously.1
Cesarean section rates varied widely among the individual trials (2.3%-35%). Analysis suggested that studies with higher baseline rates showed the greatest increases with continuous EFM. The rate for all studies combined was just 4.3%; 69% of patients included in the meta-analysis were contributed by the Dublin trial, which had an average cesarean rate of 2.3%.1 By comparison, the US Division of Vital Statistics reported a cesarean rate of 32.3% in 2008.2
EFM reduces death from fetal hypoxia
A 1995 meta-analysis, including 9 of the Cochrane review studies with a total of 18,561 women, evaluated the additional outcome of death resulting from fetal hypoxia.3 Compared with IA, EFM was associated with a 59% reduction in death from fetal hypoxia (RR=0.41; 95% CI, 0.17-0.98). Continuous EFM prevented 1 perinatal death per 1000 births. The reduction in perinatal mortality was offset by a 53% increase in cesarean deliveries and a 23% increase in operative vaginal deliveries.3
Recommendations
The American College of Obstetricians and Gynecologists (ACOG) doesn’t recommend for or against continuous fetal heart rate monitoring in uncomplicated labor, recognizing either EFM or IA as acceptable in uncomplicated patients.4 ACOG does recommend continuous EFM for women with high-risk conditions (suspected fetal growth restriction, preeclampsia, and type 1 diabetes mellitus).
The US Preventive Services Task Force doesn’t support routine intrapartum EFM for low-risk woman. The Task Force found insufficient evidence for using EFM in high-risk pregnancies.5
The Royal College of Obstetricians and Gynaecologists and the Royal Australian and New Zealand College of Obstetricians and Gynecologists both recommend continuous EFM for high-risk women and IA for low-risk patients.6,7
Acknowledgements
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the US Army Medical Department or the US Army at large.
CONTINUOUS ELECTRONIC FETAL MONITORING (EFM) REDUCES THE RISK OF NEONATAL SEIZURE BY 50% compared with intermittent auscultation (IA) (strength of recommendation [SOR]: A, systematic review of randomized controlled trials [RCTs]).
EFM increases the incidence of cesarean section by 66% and the incidence of operative vaginal delivery by 16% (SOR: A, systematic review of RCTs). It has no effect on the rates of cerebral palsy or neonatal mortality (SOR: A, systematic review of RCTs).
An estimate from a Cochrane meta-analysis suggests that a cohort of 628 women receiving EFM could expect to experience 1 less neonatal seizure and 11 more cesarean sections compared with IA controls.
Evidence summary
Continuous EFM is designed to detect early fetal hypoxia and thereby decrease neonatal morbidity and mortality compared with IA. IA is defined as auscultation of the fetal heart rate for at least 60 seconds every 15 minutes during the first stage of labor and every 5 minutes during the second stage of labor.
A decrease in seizures, but not deaths or cerebral palsy
A 2006 Cochrane systematic review examined 12 RCTs (with >37,000 women) that compared continuous EFM with IA.1 Continuous EFM reduced the risk of neonatal seizure by 50% (relative risk [RR]=0.50; 95% confidence interval [CI], 0.31-0.80), but had no effect on the rate of neonatal death (RR=0.85; 95% CI, 0.59-1.23) or development of cerebral palsy (RR=1.74; 95% CI, 0.97-3.11).
Reduction of seizures was consistent across all trials. However, a subgroup analysis of high-risk pregnancies (advanced maternal age, diabetes mellitus, chronic hypertension, renal disease, preeclampsia, cardiac disease, renal disease, previous delivery of a low-birth-weight infant) didn’t find a statistically significant decrease in seizures.
Cesarean deliveries rise, regardless of patient risk status
Continuous EFM raised the rates of cesarean delivery (RR=1.66; 95% CI, 1.30-2.13) and instrumental vaginal deliveries (RR=1.16; 95% CI, 1.01-1.32). The increased rate of cesarean section in the EFM group was consistent regardless of clinical risk status (low- vs high-risk women). One additional cesarean section was performed for every 58 women monitored continuously. For “high-risk” women, 1 additional cesarean section was performed for every 12 women monitored continuously.1
Cesarean section rates varied widely among the individual trials (2.3%-35%). Analysis suggested that studies with higher baseline rates showed the greatest increases with continuous EFM. The rate for all studies combined was just 4.3%; 69% of patients included in the meta-analysis were contributed by the Dublin trial, which had an average cesarean rate of 2.3%.1 By comparison, the US Division of Vital Statistics reported a cesarean rate of 32.3% in 2008.2
EFM reduces death from fetal hypoxia
A 1995 meta-analysis, including 9 of the Cochrane review studies with a total of 18,561 women, evaluated the additional outcome of death resulting from fetal hypoxia.3 Compared with IA, EFM was associated with a 59% reduction in death from fetal hypoxia (RR=0.41; 95% CI, 0.17-0.98). Continuous EFM prevented 1 perinatal death per 1000 births. The reduction in perinatal mortality was offset by a 53% increase in cesarean deliveries and a 23% increase in operative vaginal deliveries.3
Recommendations
The American College of Obstetricians and Gynecologists (ACOG) doesn’t recommend for or against continuous fetal heart rate monitoring in uncomplicated labor, recognizing either EFM or IA as acceptable in uncomplicated patients.4 ACOG does recommend continuous EFM for women with high-risk conditions (suspected fetal growth restriction, preeclampsia, and type 1 diabetes mellitus).
The US Preventive Services Task Force doesn’t support routine intrapartum EFM for low-risk woman. The Task Force found insufficient evidence for using EFM in high-risk pregnancies.5
The Royal College of Obstetricians and Gynaecologists and the Royal Australian and New Zealand College of Obstetricians and Gynecologists both recommend continuous EFM for high-risk women and IA for low-risk patients.6,7
Acknowledgements
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the US Army Medical Department or the US Army at large.
1. Alfirevic Z, Devane D, Gyte GM. Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database Syst Rev. 2006;(3):CD006066.-
2. Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2008. Natl Vital Stat Rep. 2010;58(16):1-18.
3. Vintzileos AM, Nochimson DJ, Guzman ER, et al. Intrapartum electronic heart rate monitoring versus intermittent auscultation: a meta-analysis. Obstet Gynecol. 1995;85:149-155.
4. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin. Clinical Management Guidelines for Obstetrician-Gynecologists, Number 106, July 2009. Intrapartum fetal heart rate monitoring: Nomenclature, interpretation, and general management principles. Obstet Gynecol. 2009;114:192-202.
5. US Preventive Services Task Force. Screening for intrapartum electronic fetal monitoring. Rockville, MD: Agency for Healthcare Research and Quality; 1996. Available at: www.ahrq.gov/clinic/uspstf/uspsiefm.htm. Accessed March 7, 2010.
6. National Institute for Health and Clinical Excellence (NICE). Intrapartum Care: Management and Delivery of Care to Women in Labour. London: NICE; 2007.
7. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Clinical Guidelines. Intrapartum Fetal Surveillance Guidelines. May 2006. Available at: www.ranzcog.edu.au/publications/womenshealth.shtml. Accessed December 9, 2008.
1. Alfirevic Z, Devane D, Gyte GM. Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database Syst Rev. 2006;(3):CD006066.-
2. Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2008. Natl Vital Stat Rep. 2010;58(16):1-18.
3. Vintzileos AM, Nochimson DJ, Guzman ER, et al. Intrapartum electronic heart rate monitoring versus intermittent auscultation: a meta-analysis. Obstet Gynecol. 1995;85:149-155.
4. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin. Clinical Management Guidelines for Obstetrician-Gynecologists, Number 106, July 2009. Intrapartum fetal heart rate monitoring: Nomenclature, interpretation, and general management principles. Obstet Gynecol. 2009;114:192-202.
5. US Preventive Services Task Force. Screening for intrapartum electronic fetal monitoring. Rockville, MD: Agency for Healthcare Research and Quality; 1996. Available at: www.ahrq.gov/clinic/uspstf/uspsiefm.htm. Accessed March 7, 2010.
6. National Institute for Health and Clinical Excellence (NICE). Intrapartum Care: Management and Delivery of Care to Women in Labour. London: NICE; 2007.
7. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Clinical Guidelines. Intrapartum Fetal Surveillance Guidelines. May 2006. Available at: www.ranzcog.edu.au/publications/womenshealth.shtml. Accessed December 9, 2008.
Evidence-based answers from the Family Physicians Inquiries Network
Which drugs should post-MI patients routinely receive?
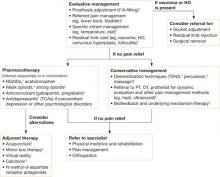
PATIENTS SHOULD BE PLACED ON THE FOLLOWING MEDICATIONS :
- antiplatelet agents (strength of recommendation [SOR]: A, meta-analysis for aspirin; A, multiple randomized controlled trials [RCTs] for aspirin plus clopidogrel)
- a statin; atorvastatin has the best evidence (SOR: B, a single RCT)
- a beta-blocker (SOR: A, meta-analysis)
- renin-angiotensin-aldosterone system blockers, whether or not the ejection fraction is diminished after myocardial infarction (MI) (SOR: A, meta-analysis for angiotensin-converting enzyme [ACE] inhibitor; B, single RCT for ACE inhibitor plus aldosterone blocker). ( TABLE )
Evidence summary
A systematic review of 9 RCTs demonstrated that aspirin (75-325 mg) started soon after the onset of acute MI significantly reduced mortality, reinfarction, and stroke at 1 month compared with placebo (absolute risk reduction [ARR]=3.8%; number needed to treat [NNT]=26; 95% confidence interval [CI], 23-30).1
One large RCT involving 17,187 patients with suspected acute MI showed that 162 mg aspirin given on the day of the MI resulted in a 2.6% ARR (NNT=38; 95% CI, 29-63) in vascular deaths at 35 days compared with placebo.2 The survival benefit persisted for as long as 10 years. The RCT also found no significant difference between aspirin and placebo in rates of cerebral hemorrhage or bleeding requiring transfusions.
Patients who have had an MI without ST segment elevation should take clopidogrel (75 mg/d) and aspirin (81 mg/d) for 12 months. The combination has been shown to result in a 2.1% ARR (NNT=48) in deaths, recurrent MI, and stroke compared with aspirin alone.3 Patients who have had an ST segment elevation MI should take clopidogrel in combination with aspirin for at least 2 weeks.4
TABLE
Recommended drugs for post-MI patients
| Drug type | Examples | Precautions | Contraindications |
|---|---|---|---|
| Antiplatelet agents | Aspirin 81 mg/d; clopidogrel 75 mg/d | Risk for bleeding; use caution in patients taking warfarin | Active bleeding; hypersensitivity |
| RAAS blockers | Lisinopril 20 mg/d; losartan 50 mg/d; eplerenone 50 mg/d | Hypotension, hyperkalemia, renal failure Use eplerenone only with decreased ejection fraction | Hypersensitivity; systolic blood pressure <90 mm Hg |
| Beta-blockers | Metoprolol 100 mg bid | Hypotension, bradycardia, reactive airways | Systolic blood pressure <90 mm Hg; pulse rate <50 bpm |
| Statins | Atorvastatin 80 mg/d | Elevated AST/ALT, myositis | Active liver disease; pregnancy/nursing |
| ALT, alanine aminotransferase; AST, aspartate aminotransferase; BPM, beats per minute; RAAS, renin-angiotensin-aldosterone system. | |||
Intensive atorvastatin therapy lowers risk of death
The PROVE IT-TIMI 22 trial showed the benefit of early intensive therapy with the hydroxymethyl glutaryl coenzyme A reductase inhibitor atorvastatin to lower low-density lipoprotein <70 mg/dL post-MI.5 At 30 days after the event, atorvastatin 80 mg daily resulted in a 1.2% ARR in death and recurrent acute coronary syndrome (NNT=83; hazard ratio [HR]=0.72; 95% CI, 0.52-0.99). From 6 months to 24 months after the event, the ARR was 2.6% (NNT=38; HR=0.82; 95% CI, 0.69-0.99).
Beta-blockers significantly decrease late mortality
One systematic review of 63 RCTs showed that, in long-term trials, use of a beta-blocker significantly reduced the late mortality rate (NNT=48; odds ratio [OR]=0.77; 95% CI, 0.70-0.85).6 In another review of 82 RCTs, the mortality rate between 6 months and 4 years after MI decreased markedly in patients receiving a beta-blocker (OR=0.77; 95% CI, 0.69-0.85).7
ACE inhibitors decrease overall mortality, sudden cardiac death
An ACE inhibitor should be started regardless of the ejection fraction or the presence or absence of left ventricular systolic dysfunction. One systematic review that compared long-term mortality rates of patients started on an ACE inhibitor within 14 days of acute MI versus placebo found that ACE inhibitors significantly decreased overall mortality and sudden cardiac deaths between 2 and 42 months after the MI (NNT=42; OR=0.83; 95% CI, 0.71-0.97).8
Eplerenone + ACE inhibitor benefit patients with post-MI heart failure
The selective aldosterone blocker eplerenone appears to benefit patients with a decreased ejection fraction post-MI. The EPHESUS study demonstrated that eplerenone, when added to an ACE inhibitor, reduced all-cause mortality (ARR=1.4%; NNT=71; 95% CI, 47-200; RR=0.69; 95% CI, 0.54-0.89) and sudden cardiac death (ARR=0.5%; NNT=200; 95% CI, 125-∞; RR=0.63; 95% CI, 0.40-1.00) up to 30 days in patients with post-MI heart failure. Benefits were also seen after 16 months of treatment.9
Recommendations
The American College of Cardiology (ACC) and American Heart Association (AHA) provide the following recommendations in their joint 2006 Guidelines for Secondary Prevention for Patients with Coronary and Other Atherosclerotic Vascular Disease:10
- Low-dose aspirin should be used, as well as clopidogrel in combination with aspirin for up to 12 months after a non-ST elevation MI
- ACE inhibitors or angiotensin receptor blockers should be considered in all patients, and an aldosterone antagonist should be prescribed for patients with a diminished ejection fraction post-MI
- Beta-blockers should be used in all post-MI patients without contraindications.
The ACC/AHA 2007 Guidelines for the Management of Patients with Unstable Angina/Non–ST-Elevation Myocardial Infarction recommend the same medication combinations.11 So does the 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction, with the exception that clopidogrel in combination with aspirin is recommended for at least 14 days.12
Similarly, the British National Institute for Clinical Excellence Clinical Guideline 48 recommends that all post-MI patients be offered a combination of an ACE inhibitor, aspirin with clopidogrel, a beta-blocker, and a statin.13
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and should not be construed as official or as reflecting the views of the US Department of the Navy or the Department of Defense.
1. Collaborative overview of randomized trials of antiplatelet therapy: prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of people. Antiplatelet Trialists’ Collaboration. BMJ. 1994;308:81-106.
2. Randomized trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Second International Study of Infarct Survival (ISIS-2) Collaborative Group. Lancet. 1988;2:349-360.
3. Yusuf S, Zhao F, Mehta SR, et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345:494-502.
4. Chen ZM, Jiang LX, Chen YP, et al. Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo-controlled trial. Lancet. 2005;366:1607-1621.
5. Ray KK, Cannon CP, McCabe CH, et al. Early and late benefits of high-dose atorvastatin in patients with acute coronary syndromes: results from the PROVE IT-TIMI 22 trial. J Am Coll Cardiol. 2005;46:1405-1410.
6. Yusuf S, Peto R, Lewis J, et al. Beta-blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis. 1985;27:335-371.
7. Freemantle N, Cleland J, Young P, et al. Beta blockade after myocardial infarction: systematic review and meta regression analysis. BMJ. 1999;318:1730-1737.
8. Domanski MJ, Exner DV, Borkowf CB, et al. Effect of angiotensin converting enzyme inhibition on sudden cardiac death in patients following acute myocardial infarction. A meta-analysis of randomized clinical trials. J Am Coll Cardiol. 1999;33:598-604.
9. Pitt B, White H, Nicolau J, et al. Eplerenone reduces mortality 30 days post-randomization following acute myocardial infarction in patients with left ventricular systolic dysfunction and heart failure. J Am Coll Cardiol. 2005;46:425-431.
10. Smith SC, Jr, Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006;113:2363-2372.
11. Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non–ST-elevation myocardial infarction. J Am Coll Cardiol. 2007;50:e1-e157.
12. Antman EM, Hand M, Armstron PW, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2008;51:210-247.
13. National Institute for Health and Clinical Excellence (NICE). Clinical guideline 48. Secondary prevention in primary and secondary care for patients following a myocardial infarction. London: NICE; 2007. Available at: http://guidance.nice.org.uk/CG48. Accessed March 7, 2010.
PATIENTS SHOULD BE PLACED ON THE FOLLOWING MEDICATIONS :
- antiplatelet agents (strength of recommendation [SOR]: A, meta-analysis for aspirin; A, multiple randomized controlled trials [RCTs] for aspirin plus clopidogrel)
- a statin; atorvastatin has the best evidence (SOR: B, a single RCT)
- a beta-blocker (SOR: A, meta-analysis)
- renin-angiotensin-aldosterone system blockers, whether or not the ejection fraction is diminished after myocardial infarction (MI) (SOR: A, meta-analysis for angiotensin-converting enzyme [ACE] inhibitor; B, single RCT for ACE inhibitor plus aldosterone blocker). ( TABLE )
Evidence summary
A systematic review of 9 RCTs demonstrated that aspirin (75-325 mg) started soon after the onset of acute MI significantly reduced mortality, reinfarction, and stroke at 1 month compared with placebo (absolute risk reduction [ARR]=3.8%; number needed to treat [NNT]=26; 95% confidence interval [CI], 23-30).1
One large RCT involving 17,187 patients with suspected acute MI showed that 162 mg aspirin given on the day of the MI resulted in a 2.6% ARR (NNT=38; 95% CI, 29-63) in vascular deaths at 35 days compared with placebo.2 The survival benefit persisted for as long as 10 years. The RCT also found no significant difference between aspirin and placebo in rates of cerebral hemorrhage or bleeding requiring transfusions.
Patients who have had an MI without ST segment elevation should take clopidogrel (75 mg/d) and aspirin (81 mg/d) for 12 months. The combination has been shown to result in a 2.1% ARR (NNT=48) in deaths, recurrent MI, and stroke compared with aspirin alone.3 Patients who have had an ST segment elevation MI should take clopidogrel in combination with aspirin for at least 2 weeks.4
TABLE
Recommended drugs for post-MI patients
| Drug type | Examples | Precautions | Contraindications |
|---|---|---|---|
| Antiplatelet agents | Aspirin 81 mg/d; clopidogrel 75 mg/d | Risk for bleeding; use caution in patients taking warfarin | Active bleeding; hypersensitivity |
| RAAS blockers | Lisinopril 20 mg/d; losartan 50 mg/d; eplerenone 50 mg/d | Hypotension, hyperkalemia, renal failure Use eplerenone only with decreased ejection fraction | Hypersensitivity; systolic blood pressure <90 mm Hg |
| Beta-blockers | Metoprolol 100 mg bid | Hypotension, bradycardia, reactive airways | Systolic blood pressure <90 mm Hg; pulse rate <50 bpm |
| Statins | Atorvastatin 80 mg/d | Elevated AST/ALT, myositis | Active liver disease; pregnancy/nursing |
| ALT, alanine aminotransferase; AST, aspartate aminotransferase; BPM, beats per minute; RAAS, renin-angiotensin-aldosterone system. | |||
Intensive atorvastatin therapy lowers risk of death
The PROVE IT-TIMI 22 trial showed the benefit of early intensive therapy with the hydroxymethyl glutaryl coenzyme A reductase inhibitor atorvastatin to lower low-density lipoprotein <70 mg/dL post-MI.5 At 30 days after the event, atorvastatin 80 mg daily resulted in a 1.2% ARR in death and recurrent acute coronary syndrome (NNT=83; hazard ratio [HR]=0.72; 95% CI, 0.52-0.99). From 6 months to 24 months after the event, the ARR was 2.6% (NNT=38; HR=0.82; 95% CI, 0.69-0.99).
Beta-blockers significantly decrease late mortality
One systematic review of 63 RCTs showed that, in long-term trials, use of a beta-blocker significantly reduced the late mortality rate (NNT=48; odds ratio [OR]=0.77; 95% CI, 0.70-0.85).6 In another review of 82 RCTs, the mortality rate between 6 months and 4 years after MI decreased markedly in patients receiving a beta-blocker (OR=0.77; 95% CI, 0.69-0.85).7
ACE inhibitors decrease overall mortality, sudden cardiac death
An ACE inhibitor should be started regardless of the ejection fraction or the presence or absence of left ventricular systolic dysfunction. One systematic review that compared long-term mortality rates of patients started on an ACE inhibitor within 14 days of acute MI versus placebo found that ACE inhibitors significantly decreased overall mortality and sudden cardiac deaths between 2 and 42 months after the MI (NNT=42; OR=0.83; 95% CI, 0.71-0.97).8
Eplerenone + ACE inhibitor benefit patients with post-MI heart failure
The selective aldosterone blocker eplerenone appears to benefit patients with a decreased ejection fraction post-MI. The EPHESUS study demonstrated that eplerenone, when added to an ACE inhibitor, reduced all-cause mortality (ARR=1.4%; NNT=71; 95% CI, 47-200; RR=0.69; 95% CI, 0.54-0.89) and sudden cardiac death (ARR=0.5%; NNT=200; 95% CI, 125-∞; RR=0.63; 95% CI, 0.40-1.00) up to 30 days in patients with post-MI heart failure. Benefits were also seen after 16 months of treatment.9
Recommendations
The American College of Cardiology (ACC) and American Heart Association (AHA) provide the following recommendations in their joint 2006 Guidelines for Secondary Prevention for Patients with Coronary and Other Atherosclerotic Vascular Disease:10
- Low-dose aspirin should be used, as well as clopidogrel in combination with aspirin for up to 12 months after a non-ST elevation MI
- ACE inhibitors or angiotensin receptor blockers should be considered in all patients, and an aldosterone antagonist should be prescribed for patients with a diminished ejection fraction post-MI
- Beta-blockers should be used in all post-MI patients without contraindications.
The ACC/AHA 2007 Guidelines for the Management of Patients with Unstable Angina/Non–ST-Elevation Myocardial Infarction recommend the same medication combinations.11 So does the 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction, with the exception that clopidogrel in combination with aspirin is recommended for at least 14 days.12
Similarly, the British National Institute for Clinical Excellence Clinical Guideline 48 recommends that all post-MI patients be offered a combination of an ACE inhibitor, aspirin with clopidogrel, a beta-blocker, and a statin.13
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and should not be construed as official or as reflecting the views of the US Department of the Navy or the Department of Defense.
PATIENTS SHOULD BE PLACED ON THE FOLLOWING MEDICATIONS :
- antiplatelet agents (strength of recommendation [SOR]: A, meta-analysis for aspirin; A, multiple randomized controlled trials [RCTs] for aspirin plus clopidogrel)
- a statin; atorvastatin has the best evidence (SOR: B, a single RCT)
- a beta-blocker (SOR: A, meta-analysis)
- renin-angiotensin-aldosterone system blockers, whether or not the ejection fraction is diminished after myocardial infarction (MI) (SOR: A, meta-analysis for angiotensin-converting enzyme [ACE] inhibitor; B, single RCT for ACE inhibitor plus aldosterone blocker). ( TABLE )
Evidence summary
A systematic review of 9 RCTs demonstrated that aspirin (75-325 mg) started soon after the onset of acute MI significantly reduced mortality, reinfarction, and stroke at 1 month compared with placebo (absolute risk reduction [ARR]=3.8%; number needed to treat [NNT]=26; 95% confidence interval [CI], 23-30).1
One large RCT involving 17,187 patients with suspected acute MI showed that 162 mg aspirin given on the day of the MI resulted in a 2.6% ARR (NNT=38; 95% CI, 29-63) in vascular deaths at 35 days compared with placebo.2 The survival benefit persisted for as long as 10 years. The RCT also found no significant difference between aspirin and placebo in rates of cerebral hemorrhage or bleeding requiring transfusions.
Patients who have had an MI without ST segment elevation should take clopidogrel (75 mg/d) and aspirin (81 mg/d) for 12 months. The combination has been shown to result in a 2.1% ARR (NNT=48) in deaths, recurrent MI, and stroke compared with aspirin alone.3 Patients who have had an ST segment elevation MI should take clopidogrel in combination with aspirin for at least 2 weeks.4
TABLE
Recommended drugs for post-MI patients
| Drug type | Examples | Precautions | Contraindications |
|---|---|---|---|
| Antiplatelet agents | Aspirin 81 mg/d; clopidogrel 75 mg/d | Risk for bleeding; use caution in patients taking warfarin | Active bleeding; hypersensitivity |
| RAAS blockers | Lisinopril 20 mg/d; losartan 50 mg/d; eplerenone 50 mg/d | Hypotension, hyperkalemia, renal failure Use eplerenone only with decreased ejection fraction | Hypersensitivity; systolic blood pressure <90 mm Hg |
| Beta-blockers | Metoprolol 100 mg bid | Hypotension, bradycardia, reactive airways | Systolic blood pressure <90 mm Hg; pulse rate <50 bpm |
| Statins | Atorvastatin 80 mg/d | Elevated AST/ALT, myositis | Active liver disease; pregnancy/nursing |
| ALT, alanine aminotransferase; AST, aspartate aminotransferase; BPM, beats per minute; RAAS, renin-angiotensin-aldosterone system. | |||
Intensive atorvastatin therapy lowers risk of death
The PROVE IT-TIMI 22 trial showed the benefit of early intensive therapy with the hydroxymethyl glutaryl coenzyme A reductase inhibitor atorvastatin to lower low-density lipoprotein <70 mg/dL post-MI.5 At 30 days after the event, atorvastatin 80 mg daily resulted in a 1.2% ARR in death and recurrent acute coronary syndrome (NNT=83; hazard ratio [HR]=0.72; 95% CI, 0.52-0.99). From 6 months to 24 months after the event, the ARR was 2.6% (NNT=38; HR=0.82; 95% CI, 0.69-0.99).
Beta-blockers significantly decrease late mortality
One systematic review of 63 RCTs showed that, in long-term trials, use of a beta-blocker significantly reduced the late mortality rate (NNT=48; odds ratio [OR]=0.77; 95% CI, 0.70-0.85).6 In another review of 82 RCTs, the mortality rate between 6 months and 4 years after MI decreased markedly in patients receiving a beta-blocker (OR=0.77; 95% CI, 0.69-0.85).7
ACE inhibitors decrease overall mortality, sudden cardiac death
An ACE inhibitor should be started regardless of the ejection fraction or the presence or absence of left ventricular systolic dysfunction. One systematic review that compared long-term mortality rates of patients started on an ACE inhibitor within 14 days of acute MI versus placebo found that ACE inhibitors significantly decreased overall mortality and sudden cardiac deaths between 2 and 42 months after the MI (NNT=42; OR=0.83; 95% CI, 0.71-0.97).8
Eplerenone + ACE inhibitor benefit patients with post-MI heart failure
The selective aldosterone blocker eplerenone appears to benefit patients with a decreased ejection fraction post-MI. The EPHESUS study demonstrated that eplerenone, when added to an ACE inhibitor, reduced all-cause mortality (ARR=1.4%; NNT=71; 95% CI, 47-200; RR=0.69; 95% CI, 0.54-0.89) and sudden cardiac death (ARR=0.5%; NNT=200; 95% CI, 125-∞; RR=0.63; 95% CI, 0.40-1.00) up to 30 days in patients with post-MI heart failure. Benefits were also seen after 16 months of treatment.9
Recommendations
The American College of Cardiology (ACC) and American Heart Association (AHA) provide the following recommendations in their joint 2006 Guidelines for Secondary Prevention for Patients with Coronary and Other Atherosclerotic Vascular Disease:10
- Low-dose aspirin should be used, as well as clopidogrel in combination with aspirin for up to 12 months after a non-ST elevation MI
- ACE inhibitors or angiotensin receptor blockers should be considered in all patients, and an aldosterone antagonist should be prescribed for patients with a diminished ejection fraction post-MI
- Beta-blockers should be used in all post-MI patients without contraindications.
The ACC/AHA 2007 Guidelines for the Management of Patients with Unstable Angina/Non–ST-Elevation Myocardial Infarction recommend the same medication combinations.11 So does the 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction, with the exception that clopidogrel in combination with aspirin is recommended for at least 14 days.12
Similarly, the British National Institute for Clinical Excellence Clinical Guideline 48 recommends that all post-MI patients be offered a combination of an ACE inhibitor, aspirin with clopidogrel, a beta-blocker, and a statin.13
Acknowledgement
The opinions and assertions contained herein are the private views of the authors and should not be construed as official or as reflecting the views of the US Department of the Navy or the Department of Defense.
1. Collaborative overview of randomized trials of antiplatelet therapy: prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of people. Antiplatelet Trialists’ Collaboration. BMJ. 1994;308:81-106.
2. Randomized trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Second International Study of Infarct Survival (ISIS-2) Collaborative Group. Lancet. 1988;2:349-360.
3. Yusuf S, Zhao F, Mehta SR, et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345:494-502.
4. Chen ZM, Jiang LX, Chen YP, et al. Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo-controlled trial. Lancet. 2005;366:1607-1621.
5. Ray KK, Cannon CP, McCabe CH, et al. Early and late benefits of high-dose atorvastatin in patients with acute coronary syndromes: results from the PROVE IT-TIMI 22 trial. J Am Coll Cardiol. 2005;46:1405-1410.
6. Yusuf S, Peto R, Lewis J, et al. Beta-blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis. 1985;27:335-371.
7. Freemantle N, Cleland J, Young P, et al. Beta blockade after myocardial infarction: systematic review and meta regression analysis. BMJ. 1999;318:1730-1737.
8. Domanski MJ, Exner DV, Borkowf CB, et al. Effect of angiotensin converting enzyme inhibition on sudden cardiac death in patients following acute myocardial infarction. A meta-analysis of randomized clinical trials. J Am Coll Cardiol. 1999;33:598-604.
9. Pitt B, White H, Nicolau J, et al. Eplerenone reduces mortality 30 days post-randomization following acute myocardial infarction in patients with left ventricular systolic dysfunction and heart failure. J Am Coll Cardiol. 2005;46:425-431.
10. Smith SC, Jr, Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006;113:2363-2372.
11. Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non–ST-elevation myocardial infarction. J Am Coll Cardiol. 2007;50:e1-e157.
12. Antman EM, Hand M, Armstron PW, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2008;51:210-247.
13. National Institute for Health and Clinical Excellence (NICE). Clinical guideline 48. Secondary prevention in primary and secondary care for patients following a myocardial infarction. London: NICE; 2007. Available at: http://guidance.nice.org.uk/CG48. Accessed March 7, 2010.
1. Collaborative overview of randomized trials of antiplatelet therapy: prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of people. Antiplatelet Trialists’ Collaboration. BMJ. 1994;308:81-106.
2. Randomized trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Second International Study of Infarct Survival (ISIS-2) Collaborative Group. Lancet. 1988;2:349-360.
3. Yusuf S, Zhao F, Mehta SR, et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345:494-502.
4. Chen ZM, Jiang LX, Chen YP, et al. Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo-controlled trial. Lancet. 2005;366:1607-1621.
5. Ray KK, Cannon CP, McCabe CH, et al. Early and late benefits of high-dose atorvastatin in patients with acute coronary syndromes: results from the PROVE IT-TIMI 22 trial. J Am Coll Cardiol. 2005;46:1405-1410.
6. Yusuf S, Peto R, Lewis J, et al. Beta-blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis. 1985;27:335-371.
7. Freemantle N, Cleland J, Young P, et al. Beta blockade after myocardial infarction: systematic review and meta regression analysis. BMJ. 1999;318:1730-1737.
8. Domanski MJ, Exner DV, Borkowf CB, et al. Effect of angiotensin converting enzyme inhibition on sudden cardiac death in patients following acute myocardial infarction. A meta-analysis of randomized clinical trials. J Am Coll Cardiol. 1999;33:598-604.
9. Pitt B, White H, Nicolau J, et al. Eplerenone reduces mortality 30 days post-randomization following acute myocardial infarction in patients with left ventricular systolic dysfunction and heart failure. J Am Coll Cardiol. 2005;46:425-431.
10. Smith SC, Jr, Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006;113:2363-2372.
11. Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non–ST-elevation myocardial infarction. J Am Coll Cardiol. 2007;50:e1-e157.
12. Antman EM, Hand M, Armstron PW, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2008;51:210-247.
13. National Institute for Health and Clinical Excellence (NICE). Clinical guideline 48. Secondary prevention in primary and secondary care for patients following a myocardial infarction. London: NICE; 2007. Available at: http://guidance.nice.org.uk/CG48. Accessed March 7, 2010.
Evidence-based answers from the Family Physicians Inquiries Network
What’s the best way to manage upper extremity venous thrombosis?
STANDARD MANAGEMENT IS BEST: Start with unfractionated heparin or low-molecular-weight heparin and follow with long-term therapy with a vitamin K antagonist (strength of recommendation [SOR]: C, expert consensus and case reports). Some evidence supports thrombolytic therapy, placement of a superior vena cava filter, or surgical thrombectomy in selected patients (SOR: C, expert consensus and case reports). Whether to remove venous catheters during initial treatment for catheter-induced venous thrombosis remains unclear, because limited studies address this issue specifically (SOR: C, expert consensus and case reports).
Evidence summary
Upper extremity venous thrombosis (UEVT)—which typically refers to thrombosis of the brachial, axillary, or subclavian veins—accounts for approximately 10% of all cases of venous thromboembolism.1 UEVT can occur spontaneously (Paget-Schroetter syndrome) or develop as a complication of cancer or in-dwelling medical devices (such as long-term central venous catheters).
Although significant evidence-based data exist on treatment of lower extremity venous thrombosis, no good-quality studies specifically address management of UEVT. Review of the current literature revealed several small studies that compared various treatment strategies.
Thrombolytics may work better than anticoagulants in some patients
A small retrospective study randomized 20 patients with UEVT to either treatment with anticoagulant therapy with heparin and warfarin (n=11) or thrombolytic therapy (n=9).2 After a mean follow-up period of 81.7 months for the anticoagulation group and 52.1 months for the thrombolytic group, 4 more patients in the thrombolytic group achieved complete clinical recovery and vein patency than in the anticoagulant group (P=.04). When patients who recovered completely were added to those who showed some clinical improvement, 89% of the thrombolytic therapy group had satisfactory outcomes, compared with 36% of the anticoagulant group (P=.028).
Another small retrospective study looked at 10 consecutive patients with UEVT who were treated with either anticoagulant therapy (n=6) or thrombolytics (n=4).3 Fifty percent of patients treated with anticoagulants experienced partial or complete improvement in symptoms, whereas 100% of patients treated with thrombolytics had partial or complete resolution of both symptoms and thrombi.
Overall, both studies raise the possibility that thrombolytic therapy is more effective than anticoagulation therapy in certain patients. The studies evaluated only active patients, 23 to 58 years of age, who had no contraindications to thrombolytic therapy. Neither study reported data on long-term outcomes such as recurrences, bleeding, or post-thrombotic sequelae.
Surgery may avoid long-term anticoagulation
Two case studies evaluated treatment of UEVT with thrombolytic therapy followed by various surgical interventions (angioplasty, thrombectomy, decompression via first rib resection or anterior scalenectomy, and venous bypass).4,5 The first study reported that 8 of 9 patients who underwent first-rib resection and 1 of 2 who underwent scalenectomy were free of residual symptoms at follow-up (mean 2 years, range 6 months to 5 years).4 All patients were treated with thrombolytics before surgery.
The second study demonstrated that 50% of the patients treated with a surgical intervention without thrombolysis had complete symptom relief, while the remaining 50% reported relief from pain but still had occasional swelling.5 Although more invasive, surgery may eliminate the need for long-term anticoagulation therapy and enable a more rapid return to normal activities.
Data on vena cava filters are limited
Data supporting superior vena cava Green-field filters to treat UEVT are extremely limited. Of 6 patients with contraindications to anticoagulation therapy who were treated with a Greenfield filter, none had clinical evidence of pulmonary embolism at 14 months.6 The study reported no data regarding long-term sequelae or effects of the UEVT on the patients’ upper extremity.6
When in doubt, don’t (necessarily) take it out
For patients with central venous catheter-related deep vein thrombosis, taking out the catheter as part of treatment is controversial and should depend on clinical symptoms, the reason for the catheter, and duration of use, as well as physician judgment.7 No RCTs have studied the effects of catheter removal as part of initial treatment. Current guidelines recommend removing the catheter from patients with persistent symptoms who have failed anticoagulant or thrombolytic treatment.1
Recommendations
The American College of Chest Physicians recommends therapeutic doses of intravenous unfractionated heparin, low-molecular-weight heparin, or fondaparinux for initial treatment of UEVT, followed by at least 3 months of treatment with a vitamin K antagonist.1 The organization also suggests that surgical thrombectomy, superior vena caval filters, thrombolytic therapy, or catheter extraction may benefit selected patients.
Acknowledgement
The opinions and assertions contained herein are the private views of the author and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
1. Hirsh J, Guyatt G, Albers GW, et al. Executive summary: American College of Chest Physicians evidence-based clinical practice guidelines, 8th ed. Chest. 2008;133(6 suppl):71S-109S.
2. Petrakis IE, Katsamouris A, Kafassis E, et al. Two different therapeutic modalities in the treatment of the upper extremity deep vein thrombosis: preliminary investigation with 20 case reports. Int J Angiol. 2000;9:46-50.
3. AbuRahma AF, Sadler D, Stuart P, et al. Conventional versus thrombolytic therapy in spontaneous (effort) axillary-subclavian vein thrombosis. Am J Surg. 1991;161:459-465.
4. Lee MC, Grassi CJ, Belkin M, et al. Early operative intervention after thrombolytic therapy for primary subclavian vein thrombosis: an effective treatment approach. J Vasc Surg. 1998;27:1101-1107.
5. Sanders RJ, Cooper MA. Surgical management of subclavian vein obstruction, including six cases of subclavian vein bypass. Surgery. 1995;118:856-863.
6. Ascer E, Gennaro M, Lorensen E, et al. Superior vena caval Green-field filters: indications, techniques, and results. J Vasc Surg. 1996;23:498-503.
7. Verso M, Agnelli G. Venous thromboembolism associated with long-term use of central venous catheters in cancer patients. J Clin Oncol. 2003;21:3665-3675.
STANDARD MANAGEMENT IS BEST: Start with unfractionated heparin or low-molecular-weight heparin and follow with long-term therapy with a vitamin K antagonist (strength of recommendation [SOR]: C, expert consensus and case reports). Some evidence supports thrombolytic therapy, placement of a superior vena cava filter, or surgical thrombectomy in selected patients (SOR: C, expert consensus and case reports). Whether to remove venous catheters during initial treatment for catheter-induced venous thrombosis remains unclear, because limited studies address this issue specifically (SOR: C, expert consensus and case reports).
Evidence summary
Upper extremity venous thrombosis (UEVT)—which typically refers to thrombosis of the brachial, axillary, or subclavian veins—accounts for approximately 10% of all cases of venous thromboembolism.1 UEVT can occur spontaneously (Paget-Schroetter syndrome) or develop as a complication of cancer or in-dwelling medical devices (such as long-term central venous catheters).
Although significant evidence-based data exist on treatment of lower extremity venous thrombosis, no good-quality studies specifically address management of UEVT. Review of the current literature revealed several small studies that compared various treatment strategies.
Thrombolytics may work better than anticoagulants in some patients
A small retrospective study randomized 20 patients with UEVT to either treatment with anticoagulant therapy with heparin and warfarin (n=11) or thrombolytic therapy (n=9).2 After a mean follow-up period of 81.7 months for the anticoagulation group and 52.1 months for the thrombolytic group, 4 more patients in the thrombolytic group achieved complete clinical recovery and vein patency than in the anticoagulant group (P=.04). When patients who recovered completely were added to those who showed some clinical improvement, 89% of the thrombolytic therapy group had satisfactory outcomes, compared with 36% of the anticoagulant group (P=.028).
Another small retrospective study looked at 10 consecutive patients with UEVT who were treated with either anticoagulant therapy (n=6) or thrombolytics (n=4).3 Fifty percent of patients treated with anticoagulants experienced partial or complete improvement in symptoms, whereas 100% of patients treated with thrombolytics had partial or complete resolution of both symptoms and thrombi.
Overall, both studies raise the possibility that thrombolytic therapy is more effective than anticoagulation therapy in certain patients. The studies evaluated only active patients, 23 to 58 years of age, who had no contraindications to thrombolytic therapy. Neither study reported data on long-term outcomes such as recurrences, bleeding, or post-thrombotic sequelae.
Surgery may avoid long-term anticoagulation
Two case studies evaluated treatment of UEVT with thrombolytic therapy followed by various surgical interventions (angioplasty, thrombectomy, decompression via first rib resection or anterior scalenectomy, and venous bypass).4,5 The first study reported that 8 of 9 patients who underwent first-rib resection and 1 of 2 who underwent scalenectomy were free of residual symptoms at follow-up (mean 2 years, range 6 months to 5 years).4 All patients were treated with thrombolytics before surgery.
The second study demonstrated that 50% of the patients treated with a surgical intervention without thrombolysis had complete symptom relief, while the remaining 50% reported relief from pain but still had occasional swelling.5 Although more invasive, surgery may eliminate the need for long-term anticoagulation therapy and enable a more rapid return to normal activities.
Data on vena cava filters are limited
Data supporting superior vena cava Green-field filters to treat UEVT are extremely limited. Of 6 patients with contraindications to anticoagulation therapy who were treated with a Greenfield filter, none had clinical evidence of pulmonary embolism at 14 months.6 The study reported no data regarding long-term sequelae or effects of the UEVT on the patients’ upper extremity.6
When in doubt, don’t (necessarily) take it out
For patients with central venous catheter-related deep vein thrombosis, taking out the catheter as part of treatment is controversial and should depend on clinical symptoms, the reason for the catheter, and duration of use, as well as physician judgment.7 No RCTs have studied the effects of catheter removal as part of initial treatment. Current guidelines recommend removing the catheter from patients with persistent symptoms who have failed anticoagulant or thrombolytic treatment.1
Recommendations
The American College of Chest Physicians recommends therapeutic doses of intravenous unfractionated heparin, low-molecular-weight heparin, or fondaparinux for initial treatment of UEVT, followed by at least 3 months of treatment with a vitamin K antagonist.1 The organization also suggests that surgical thrombectomy, superior vena caval filters, thrombolytic therapy, or catheter extraction may benefit selected patients.
Acknowledgement
The opinions and assertions contained herein are the private views of the author and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
STANDARD MANAGEMENT IS BEST: Start with unfractionated heparin or low-molecular-weight heparin and follow with long-term therapy with a vitamin K antagonist (strength of recommendation [SOR]: C, expert consensus and case reports). Some evidence supports thrombolytic therapy, placement of a superior vena cava filter, or surgical thrombectomy in selected patients (SOR: C, expert consensus and case reports). Whether to remove venous catheters during initial treatment for catheter-induced venous thrombosis remains unclear, because limited studies address this issue specifically (SOR: C, expert consensus and case reports).
Evidence summary
Upper extremity venous thrombosis (UEVT)—which typically refers to thrombosis of the brachial, axillary, or subclavian veins—accounts for approximately 10% of all cases of venous thromboembolism.1 UEVT can occur spontaneously (Paget-Schroetter syndrome) or develop as a complication of cancer or in-dwelling medical devices (such as long-term central venous catheters).
Although significant evidence-based data exist on treatment of lower extremity venous thrombosis, no good-quality studies specifically address management of UEVT. Review of the current literature revealed several small studies that compared various treatment strategies.
Thrombolytics may work better than anticoagulants in some patients
A small retrospective study randomized 20 patients with UEVT to either treatment with anticoagulant therapy with heparin and warfarin (n=11) or thrombolytic therapy (n=9).2 After a mean follow-up period of 81.7 months for the anticoagulation group and 52.1 months for the thrombolytic group, 4 more patients in the thrombolytic group achieved complete clinical recovery and vein patency than in the anticoagulant group (P=.04). When patients who recovered completely were added to those who showed some clinical improvement, 89% of the thrombolytic therapy group had satisfactory outcomes, compared with 36% of the anticoagulant group (P=.028).
Another small retrospective study looked at 10 consecutive patients with UEVT who were treated with either anticoagulant therapy (n=6) or thrombolytics (n=4).3 Fifty percent of patients treated with anticoagulants experienced partial or complete improvement in symptoms, whereas 100% of patients treated with thrombolytics had partial or complete resolution of both symptoms and thrombi.
Overall, both studies raise the possibility that thrombolytic therapy is more effective than anticoagulation therapy in certain patients. The studies evaluated only active patients, 23 to 58 years of age, who had no contraindications to thrombolytic therapy. Neither study reported data on long-term outcomes such as recurrences, bleeding, or post-thrombotic sequelae.
Surgery may avoid long-term anticoagulation
Two case studies evaluated treatment of UEVT with thrombolytic therapy followed by various surgical interventions (angioplasty, thrombectomy, decompression via first rib resection or anterior scalenectomy, and venous bypass).4,5 The first study reported that 8 of 9 patients who underwent first-rib resection and 1 of 2 who underwent scalenectomy were free of residual symptoms at follow-up (mean 2 years, range 6 months to 5 years).4 All patients were treated with thrombolytics before surgery.
The second study demonstrated that 50% of the patients treated with a surgical intervention without thrombolysis had complete symptom relief, while the remaining 50% reported relief from pain but still had occasional swelling.5 Although more invasive, surgery may eliminate the need for long-term anticoagulation therapy and enable a more rapid return to normal activities.
Data on vena cava filters are limited
Data supporting superior vena cava Green-field filters to treat UEVT are extremely limited. Of 6 patients with contraindications to anticoagulation therapy who were treated with a Greenfield filter, none had clinical evidence of pulmonary embolism at 14 months.6 The study reported no data regarding long-term sequelae or effects of the UEVT on the patients’ upper extremity.6
When in doubt, don’t (necessarily) take it out
For patients with central venous catheter-related deep vein thrombosis, taking out the catheter as part of treatment is controversial and should depend on clinical symptoms, the reason for the catheter, and duration of use, as well as physician judgment.7 No RCTs have studied the effects of catheter removal as part of initial treatment. Current guidelines recommend removing the catheter from patients with persistent symptoms who have failed anticoagulant or thrombolytic treatment.1
Recommendations
The American College of Chest Physicians recommends therapeutic doses of intravenous unfractionated heparin, low-molecular-weight heparin, or fondaparinux for initial treatment of UEVT, followed by at least 3 months of treatment with a vitamin K antagonist.1 The organization also suggests that surgical thrombectomy, superior vena caval filters, thrombolytic therapy, or catheter extraction may benefit selected patients.
Acknowledgement
The opinions and assertions contained herein are the private views of the author and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
1. Hirsh J, Guyatt G, Albers GW, et al. Executive summary: American College of Chest Physicians evidence-based clinical practice guidelines, 8th ed. Chest. 2008;133(6 suppl):71S-109S.
2. Petrakis IE, Katsamouris A, Kafassis E, et al. Two different therapeutic modalities in the treatment of the upper extremity deep vein thrombosis: preliminary investigation with 20 case reports. Int J Angiol. 2000;9:46-50.
3. AbuRahma AF, Sadler D, Stuart P, et al. Conventional versus thrombolytic therapy in spontaneous (effort) axillary-subclavian vein thrombosis. Am J Surg. 1991;161:459-465.
4. Lee MC, Grassi CJ, Belkin M, et al. Early operative intervention after thrombolytic therapy for primary subclavian vein thrombosis: an effective treatment approach. J Vasc Surg. 1998;27:1101-1107.
5. Sanders RJ, Cooper MA. Surgical management of subclavian vein obstruction, including six cases of subclavian vein bypass. Surgery. 1995;118:856-863.
6. Ascer E, Gennaro M, Lorensen E, et al. Superior vena caval Green-field filters: indications, techniques, and results. J Vasc Surg. 1996;23:498-503.
7. Verso M, Agnelli G. Venous thromboembolism associated with long-term use of central venous catheters in cancer patients. J Clin Oncol. 2003;21:3665-3675.
1. Hirsh J, Guyatt G, Albers GW, et al. Executive summary: American College of Chest Physicians evidence-based clinical practice guidelines, 8th ed. Chest. 2008;133(6 suppl):71S-109S.
2. Petrakis IE, Katsamouris A, Kafassis E, et al. Two different therapeutic modalities in the treatment of the upper extremity deep vein thrombosis: preliminary investigation with 20 case reports. Int J Angiol. 2000;9:46-50.
3. AbuRahma AF, Sadler D, Stuart P, et al. Conventional versus thrombolytic therapy in spontaneous (effort) axillary-subclavian vein thrombosis. Am J Surg. 1991;161:459-465.
4. Lee MC, Grassi CJ, Belkin M, et al. Early operative intervention after thrombolytic therapy for primary subclavian vein thrombosis: an effective treatment approach. J Vasc Surg. 1998;27:1101-1107.
5. Sanders RJ, Cooper MA. Surgical management of subclavian vein obstruction, including six cases of subclavian vein bypass. Surgery. 1995;118:856-863.
6. Ascer E, Gennaro M, Lorensen E, et al. Superior vena caval Green-field filters: indications, techniques, and results. J Vasc Surg. 1996;23:498-503.
7. Verso M, Agnelli G. Venous thromboembolism associated with long-term use of central venous catheters in cancer patients. J Clin Oncol. 2003;21:3665-3675.
Evidence-based answers from the Family Physicians Inquiries Network
How can you help prevent a recurrence of diverticulitis?
A high-fiber diet may help; available evidence doesn’t support other interventions. A high-fiber diet is often prescribed after recovery from acute diverticulitis, based on extrapolation from epidemiologic data showing an association between low-fiber diets and diverticulosis (strength of recommendation [SOR]: C, expert opinion). No direct evidence establishes a role for fiber in preventing recurrent diverticulitis, however.
No evidence supports the common advice to avoid nuts and seeds to prevent diverticulitis. Eating nuts, corn, and popcorn doesn’t increase the risk; in fact, nuts and popcorn may have a protective effect (SOR: B, large cohort study).
There isn’t enough evidence to recommend the anti-inflammatory drug mesalamine or a polybacterial lysate for immunostimulation. Retrospective data don’t support routine prophylactic colectomy after 1 or 2 episodes of acute diverticulitis (SOR: B, observational studies).
Evidence summary
A 2006 Family Physicians Inquiries Network Clinical Inquiry on diverticulosis found inconsistent evidence that fiber decreases the risk of symptomatic diverticular disease (SOR: C, case control studies and a large prospective cohort study).1
A 2007 literature review found no systematic reviews or randomized controlled trials (RCTs) of fiber for preventing complications of diverticular disease. The reviewers noted that observational studies have found less diverticulosis in populations with higher fiber consumption.2
Nuts, popcorn may be protective
A trial conducted as part of a large prospective cohort study—the Health Professionals Follow-up Study—followed 47,228 male health professionals in the United States, ages 40 to 75 years, from 1986 to 2004.3 The subjects, all of whom returned a food-frequency questionnaire, were at baseline free of diverticulosis and related complications, cancer, and inflammatory bowel disease. During the follow-up period, 801 cases of diverticulitis and 383 cases of diverticular bleeding (the main outcome measures) occurred.
The investigators found an inverse association between consumption of nuts and popcorn and risk of diverticulitis. Men with the highest intake of each food (at least twice per week) compared with men with the lowest intake (less than once per month) had a hazard ratio of 0.80 (95% confidence interval [CI], 0.63-1.01; P for trend=.04) for nuts and 0.72 (95% CI, 0.56-0.92; P for trend=.007) for popcorn. No association was noted between corn consumption and diverticulitis or between nut, corn, or popcorn consumption and diverticular bleeding or uncomplicated diverticulosis.
Mesalamine’s efficacy is unknown
A 2007 systematic review found 1 RCT of the anti-inflammatory drug mesalamine (mesalazine, 5-aminosalicylic acid) for preventing diverticulitis. Mesalamine reduced the recurrence rate of diverticulitis from 46% to 15% among 166 subjects.
The reviewers judged the study to be flawed by unreported diagnostic criteria and a high withdrawal rate. They concluded that the effectiveness of mesalamine remains unknown.2
1 small study of oral enterovaccine
An oral polybacterial lysate suspension designed to stimulate gut secretion of immunoglobulin A was investigated in a study of 83 patients with recurrent diverticulitis. In the treated group, 4.6% (2/43) of patients had recurrent diverticulitis during the 3 months of the study, compared with 12.5% (5/40) of the untreated group (P<.05).4
Prophylactic surgery rarely helps
No randomized trials have compared surgical with medical therapy to prevent recurrent diverticulitis. Extensive retrospective literature fails to support elective surgery after a second episode. Sixty-eight percent to 96% of patients requiring surgery for diverticulitis-associated perforation or abscess had no previous symptoms and couldn’t be helped by prophylactic surgery,5 and diverticulitis symptoms persisted after bowel resection in 27% to 33% of patients.5
One large retrospective study followed 3165 patients for 6 to 12 years after hospitalization for diverticulitis. Of the patients treated nonoperatively, 13% had a single recurrence and 4% had multiple recurrences; the annual recurrence rate was approximately 2%. The authors concluded that routine elective colectomy is rarely indicated after a first episode of uncomplicated acute diverticulitis.6
A decision analysis using a Markov model found that performing a colectomy after a fourth, rather than a second, episode of diverticulitis would result in somewhat fewer deaths and colostomies, equivalent quality-adjusted years of life, and cost savings per patient of $1035 to $5429. The results held for both older and younger patients.7
Recommendations
The American Society of Colon and Rectal Surgeons (ASCRS) concludes that recommendations for elective sigmoid colectomy after recovery from acute diverticulitis should be made on a case-by-case basis.8 Computed tomography to grade the severity of a first attack may help determine the need for surgery. The ASCRS guidelines mention that long-term fiber supplementation may prevent recurrences of diverticulitis in most patients.
The American College of Gastroenterology Practice Parameters Committee states that prophylactic surgery may be recommended for recurrent attacks of diverticulitis, but generally isn’t indicated after a single uncomplicated episode.9 The group also notes that high-fiber diets may decrease the development of colonic diverticulosis, but no consistent data exist regarding fiber to prevent recurrent diverticulitis.
1. Eglash A, Lane CH, Schneider D. What is the most beneficial diet for patients with diverticulosis? J Fam Pract. 2006;55:813-815.
2. Humes D, Simpson J, Spiller R. Colonic diverticular disease. BMJ Clin Evid. 2008;01:405-416.
3. Strate LL, Liu YL, Syngal S, et al. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300:907-914.
4. Dughera L, Serra AM, Battaglia E, et al. Acute recurrent diverticulitis is prevented by oral administration of a polybacterial lysate suspension. Minerva Gastroenterol Dietol. 2004;50:149-153.
5. Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg. 2005;92:133-142.
6. Broderick-Villa G, Burchette RJ, Collins JC, et al. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576-581.
7. Salem L, Veenstra DL, Sullivan SD, et al. The timing of elective colectomy in diverticulitis: a decision analysis. J Am Coll Surg. 2004;199:904-912.
8. Rafferty J, Shellito P, Hyman NH, et al. Standards Committee of the American Society of Colon and Rectal Surgeons. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939-944.
9. Stollman N, Raskin L. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121.
A high-fiber diet may help; available evidence doesn’t support other interventions. A high-fiber diet is often prescribed after recovery from acute diverticulitis, based on extrapolation from epidemiologic data showing an association between low-fiber diets and diverticulosis (strength of recommendation [SOR]: C, expert opinion). No direct evidence establishes a role for fiber in preventing recurrent diverticulitis, however.
No evidence supports the common advice to avoid nuts and seeds to prevent diverticulitis. Eating nuts, corn, and popcorn doesn’t increase the risk; in fact, nuts and popcorn may have a protective effect (SOR: B, large cohort study).
There isn’t enough evidence to recommend the anti-inflammatory drug mesalamine or a polybacterial lysate for immunostimulation. Retrospective data don’t support routine prophylactic colectomy after 1 or 2 episodes of acute diverticulitis (SOR: B, observational studies).
Evidence summary
A 2006 Family Physicians Inquiries Network Clinical Inquiry on diverticulosis found inconsistent evidence that fiber decreases the risk of symptomatic diverticular disease (SOR: C, case control studies and a large prospective cohort study).1
A 2007 literature review found no systematic reviews or randomized controlled trials (RCTs) of fiber for preventing complications of diverticular disease. The reviewers noted that observational studies have found less diverticulosis in populations with higher fiber consumption.2
Nuts, popcorn may be protective
A trial conducted as part of a large prospective cohort study—the Health Professionals Follow-up Study—followed 47,228 male health professionals in the United States, ages 40 to 75 years, from 1986 to 2004.3 The subjects, all of whom returned a food-frequency questionnaire, were at baseline free of diverticulosis and related complications, cancer, and inflammatory bowel disease. During the follow-up period, 801 cases of diverticulitis and 383 cases of diverticular bleeding (the main outcome measures) occurred.
The investigators found an inverse association between consumption of nuts and popcorn and risk of diverticulitis. Men with the highest intake of each food (at least twice per week) compared with men with the lowest intake (less than once per month) had a hazard ratio of 0.80 (95% confidence interval [CI], 0.63-1.01; P for trend=.04) for nuts and 0.72 (95% CI, 0.56-0.92; P for trend=.007) for popcorn. No association was noted between corn consumption and diverticulitis or between nut, corn, or popcorn consumption and diverticular bleeding or uncomplicated diverticulosis.
Mesalamine’s efficacy is unknown
A 2007 systematic review found 1 RCT of the anti-inflammatory drug mesalamine (mesalazine, 5-aminosalicylic acid) for preventing diverticulitis. Mesalamine reduced the recurrence rate of diverticulitis from 46% to 15% among 166 subjects.
The reviewers judged the study to be flawed by unreported diagnostic criteria and a high withdrawal rate. They concluded that the effectiveness of mesalamine remains unknown.2
1 small study of oral enterovaccine
An oral polybacterial lysate suspension designed to stimulate gut secretion of immunoglobulin A was investigated in a study of 83 patients with recurrent diverticulitis. In the treated group, 4.6% (2/43) of patients had recurrent diverticulitis during the 3 months of the study, compared with 12.5% (5/40) of the untreated group (P<.05).4
Prophylactic surgery rarely helps
No randomized trials have compared surgical with medical therapy to prevent recurrent diverticulitis. Extensive retrospective literature fails to support elective surgery after a second episode. Sixty-eight percent to 96% of patients requiring surgery for diverticulitis-associated perforation or abscess had no previous symptoms and couldn’t be helped by prophylactic surgery,5 and diverticulitis symptoms persisted after bowel resection in 27% to 33% of patients.5
One large retrospective study followed 3165 patients for 6 to 12 years after hospitalization for diverticulitis. Of the patients treated nonoperatively, 13% had a single recurrence and 4% had multiple recurrences; the annual recurrence rate was approximately 2%. The authors concluded that routine elective colectomy is rarely indicated after a first episode of uncomplicated acute diverticulitis.6
A decision analysis using a Markov model found that performing a colectomy after a fourth, rather than a second, episode of diverticulitis would result in somewhat fewer deaths and colostomies, equivalent quality-adjusted years of life, and cost savings per patient of $1035 to $5429. The results held for both older and younger patients.7
Recommendations
The American Society of Colon and Rectal Surgeons (ASCRS) concludes that recommendations for elective sigmoid colectomy after recovery from acute diverticulitis should be made on a case-by-case basis.8 Computed tomography to grade the severity of a first attack may help determine the need for surgery. The ASCRS guidelines mention that long-term fiber supplementation may prevent recurrences of diverticulitis in most patients.
The American College of Gastroenterology Practice Parameters Committee states that prophylactic surgery may be recommended for recurrent attacks of diverticulitis, but generally isn’t indicated after a single uncomplicated episode.9 The group also notes that high-fiber diets may decrease the development of colonic diverticulosis, but no consistent data exist regarding fiber to prevent recurrent diverticulitis.
A high-fiber diet may help; available evidence doesn’t support other interventions. A high-fiber diet is often prescribed after recovery from acute diverticulitis, based on extrapolation from epidemiologic data showing an association between low-fiber diets and diverticulosis (strength of recommendation [SOR]: C, expert opinion). No direct evidence establishes a role for fiber in preventing recurrent diverticulitis, however.
No evidence supports the common advice to avoid nuts and seeds to prevent diverticulitis. Eating nuts, corn, and popcorn doesn’t increase the risk; in fact, nuts and popcorn may have a protective effect (SOR: B, large cohort study).
There isn’t enough evidence to recommend the anti-inflammatory drug mesalamine or a polybacterial lysate for immunostimulation. Retrospective data don’t support routine prophylactic colectomy after 1 or 2 episodes of acute diverticulitis (SOR: B, observational studies).
Evidence summary
A 2006 Family Physicians Inquiries Network Clinical Inquiry on diverticulosis found inconsistent evidence that fiber decreases the risk of symptomatic diverticular disease (SOR: C, case control studies and a large prospective cohort study).1
A 2007 literature review found no systematic reviews or randomized controlled trials (RCTs) of fiber for preventing complications of diverticular disease. The reviewers noted that observational studies have found less diverticulosis in populations with higher fiber consumption.2
Nuts, popcorn may be protective
A trial conducted as part of a large prospective cohort study—the Health Professionals Follow-up Study—followed 47,228 male health professionals in the United States, ages 40 to 75 years, from 1986 to 2004.3 The subjects, all of whom returned a food-frequency questionnaire, were at baseline free of diverticulosis and related complications, cancer, and inflammatory bowel disease. During the follow-up period, 801 cases of diverticulitis and 383 cases of diverticular bleeding (the main outcome measures) occurred.
The investigators found an inverse association between consumption of nuts and popcorn and risk of diverticulitis. Men with the highest intake of each food (at least twice per week) compared with men with the lowest intake (less than once per month) had a hazard ratio of 0.80 (95% confidence interval [CI], 0.63-1.01; P for trend=.04) for nuts and 0.72 (95% CI, 0.56-0.92; P for trend=.007) for popcorn. No association was noted between corn consumption and diverticulitis or between nut, corn, or popcorn consumption and diverticular bleeding or uncomplicated diverticulosis.
Mesalamine’s efficacy is unknown
A 2007 systematic review found 1 RCT of the anti-inflammatory drug mesalamine (mesalazine, 5-aminosalicylic acid) for preventing diverticulitis. Mesalamine reduced the recurrence rate of diverticulitis from 46% to 15% among 166 subjects.
The reviewers judged the study to be flawed by unreported diagnostic criteria and a high withdrawal rate. They concluded that the effectiveness of mesalamine remains unknown.2
1 small study of oral enterovaccine
An oral polybacterial lysate suspension designed to stimulate gut secretion of immunoglobulin A was investigated in a study of 83 patients with recurrent diverticulitis. In the treated group, 4.6% (2/43) of patients had recurrent diverticulitis during the 3 months of the study, compared with 12.5% (5/40) of the untreated group (P<.05).4
Prophylactic surgery rarely helps
No randomized trials have compared surgical with medical therapy to prevent recurrent diverticulitis. Extensive retrospective literature fails to support elective surgery after a second episode. Sixty-eight percent to 96% of patients requiring surgery for diverticulitis-associated perforation or abscess had no previous symptoms and couldn’t be helped by prophylactic surgery,5 and diverticulitis symptoms persisted after bowel resection in 27% to 33% of patients.5
One large retrospective study followed 3165 patients for 6 to 12 years after hospitalization for diverticulitis. Of the patients treated nonoperatively, 13% had a single recurrence and 4% had multiple recurrences; the annual recurrence rate was approximately 2%. The authors concluded that routine elective colectomy is rarely indicated after a first episode of uncomplicated acute diverticulitis.6
A decision analysis using a Markov model found that performing a colectomy after a fourth, rather than a second, episode of diverticulitis would result in somewhat fewer deaths and colostomies, equivalent quality-adjusted years of life, and cost savings per patient of $1035 to $5429. The results held for both older and younger patients.7
Recommendations
The American Society of Colon and Rectal Surgeons (ASCRS) concludes that recommendations for elective sigmoid colectomy after recovery from acute diverticulitis should be made on a case-by-case basis.8 Computed tomography to grade the severity of a first attack may help determine the need for surgery. The ASCRS guidelines mention that long-term fiber supplementation may prevent recurrences of diverticulitis in most patients.
The American College of Gastroenterology Practice Parameters Committee states that prophylactic surgery may be recommended for recurrent attacks of diverticulitis, but generally isn’t indicated after a single uncomplicated episode.9 The group also notes that high-fiber diets may decrease the development of colonic diverticulosis, but no consistent data exist regarding fiber to prevent recurrent diverticulitis.
1. Eglash A, Lane CH, Schneider D. What is the most beneficial diet for patients with diverticulosis? J Fam Pract. 2006;55:813-815.
2. Humes D, Simpson J, Spiller R. Colonic diverticular disease. BMJ Clin Evid. 2008;01:405-416.
3. Strate LL, Liu YL, Syngal S, et al. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300:907-914.
4. Dughera L, Serra AM, Battaglia E, et al. Acute recurrent diverticulitis is prevented by oral administration of a polybacterial lysate suspension. Minerva Gastroenterol Dietol. 2004;50:149-153.
5. Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg. 2005;92:133-142.
6. Broderick-Villa G, Burchette RJ, Collins JC, et al. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576-581.
7. Salem L, Veenstra DL, Sullivan SD, et al. The timing of elective colectomy in diverticulitis: a decision analysis. J Am Coll Surg. 2004;199:904-912.
8. Rafferty J, Shellito P, Hyman NH, et al. Standards Committee of the American Society of Colon and Rectal Surgeons. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939-944.
9. Stollman N, Raskin L. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121.
1. Eglash A, Lane CH, Schneider D. What is the most beneficial diet for patients with diverticulosis? J Fam Pract. 2006;55:813-815.
2. Humes D, Simpson J, Spiller R. Colonic diverticular disease. BMJ Clin Evid. 2008;01:405-416.
3. Strate LL, Liu YL, Syngal S, et al. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300:907-914.
4. Dughera L, Serra AM, Battaglia E, et al. Acute recurrent diverticulitis is prevented by oral administration of a polybacterial lysate suspension. Minerva Gastroenterol Dietol. 2004;50:149-153.
5. Janes S, Meagher A, Frizelle FA. Elective surgery after acute diverticulitis. Br J Surg. 2005;92:133-142.
6. Broderick-Villa G, Burchette RJ, Collins JC, et al. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576-581.
7. Salem L, Veenstra DL, Sullivan SD, et al. The timing of elective colectomy in diverticulitis: a decision analysis. J Am Coll Surg. 2004;199:904-912.
8. Rafferty J, Shellito P, Hyman NH, et al. Standards Committee of the American Society of Colon and Rectal Surgeons. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939-944.
9. Stollman N, Raskin L. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121.
Evidence-based answers from the Family Physicians Inquiries Network
Do abnormal fetal kick counts predict intrauterine death in average-risk pregnancies?
No. Structured daily monitoring of fetal movement doesn’t decrease the rate of all-cause antenatal death in average-risk pregnancies (strength of recommendation [SOR]: B, single good-quality, randomized controlled trial [RCT]). Although maternal perception of decreased fetal movement may herald fetal death, it isn’t specific for poor neonatal outcome (SOR: B, single good-quality, diagnostic cohort study). Monitoring fetal movement increases the frequency of non-stress-test monitoring (SOR: B, single good-quality RCT).
A rare tragedy that monitoring can’t prevent
Johanna Warren, MD
Oregon Health and Sciences University, Portland
Fetal movement is a marker of well-being. We draw on our experience with fetal monitoring to know that in healthy fetuses, movement increases sympathetic response and accelerates heart rate. Fetuses with severe acid-base disorders can’t oxygenate their muscles adequately and don’t move. Fetal movement, therefore, is a relatively simple indirect means of fetal assessment that indicates a lack of significant acidosis.
Intrauterine fetal demise (IUFD) is a rare but devastating event in an uncomplicated term pregnancy; it occurs in about 5000 of nearly 4 million us births each year (0.125). As the authors of this Clinical Inquiry state, nearly half of term IUFDs are unexpected and unexplained. Although it may be a logical extension to apply our knowledge of fetal physiology in an attempt to prevent IUFD, no conclusive evidence suggests that daily monitoring of fetal movement improves fetal or neonatal outcomes. We can hope that, with more accurate dating methods and more aggressive control of hypertension, diabetes, and anemia in pregnancy, the number of term IUFDs will continue to fall.
Evidence summary
Nearly 50% of late-pregnancy IUFDs have no associated risk factors. Fetal demise, however, may be heralded by decreased fetal movement followed by cessation of movement at least 12 hours before death.1 Maternal monitoring of fetal movement by kick counts has been proposed as a method to verify fetal well-being and decrease the rate of IUFD in the general obstetric population.
Counting doesn’t reduce antenatal death, large study shows
A well-done RCT randomized 68,654 women to either usual care or structured, daily monitoring of fetal movement using the count-to-10 method—daily maternal documentation of the amount of time it takes to perceive 10 fetal movements. Usual care was comprised of a query about fetal movement at antenatal visits and instruction to perform fetal movement monitoring at the provider’s discretion. Mothers were told to visit their health-care provider for evaluation if they felt no movement in 24 hours or fewer than 10 movements in 10 hours during a 48-hour period. The trial showed no benefit from monitoring in reducing the rate of antenatal death from all causes.
The rate of all fetal deaths in the counting group was 2.9 per 1000 normally formed, live, singleton births; the rate in the control group was 2.67 (absolute risk reduction=0.24; 95% confidence interval [CI], –0.5 to 0.98). Women in the counting group spent an average of 160 hours counting during pregnancy and had a statistically significant increase in fetal non-stress-test (NST) monitoring (odds ratio [OR]=1.39; 95% CI, 1.31-1.49; number needed to harm [NNH]=50 to cause 1 additional NST). A statistically insignificant trend toward increased antepartum admissions was also noted in the counting group.2
Maternal perception of less movement not linked to fetal outcome
A retrospective cohort study of 6793 patients compared pregnancy outcomes of 463 women who presented for evaluation of decreased fetal movement with outcomes among the general obstetric population. The study excluded women who reported complete cessation of fetal movement.
Pregnancies evaluated for decreased fetal movement were less likely to have an Apgar score <7 at 5 minutes (relative risk [RR]=0.56; 95% CI, 0.29-0.96; P=.05) and less likely to be preterm (RR=0.68; 95% CI, 0.48-0.94; P=.02). No significant difference in cesarean section for fetal distress or admission to the neonatal intensive care unit was noted between the study and control groups. The study suggests that maternal perception of decreased fetal movement is not associated with poor fetal outcome.3
A recent rigorous systematic review yielded no significant outcome effect related to fetal kick counts.4 A prospective cohort study of 4383 births in California, using historical controls, found a drop in fetal mortality from 8.7 to 2.1 deaths/1000. The historical control rate was higher than statewide data from the same time period, however. The overall weaker design of the study and probable effect of regression to the mean significantly limit the interpretation of outcomes.5
Recommendations
The American College of Obstetrics and Gynecology (ACOG) makes no recommendation for or against assessing daily fetal movement in routine pregnancies. ACOG notes that no consistent evidence suggests that formal assessment of fetal movement decreases IUFD.6
The Institute for Clinical Systems Improvement recommends instructing patients on “daily identification of fetal movement at the 28-week visit.” The institute doesn’t recommend specific criteria for evaluating fetal movements or offer recommendations for follow-up of a maternal report of decreased fetal movement.1 The National Institute for Clinical Excellence in Great Britain recommends against routine formal fetal-movement counting.7
1. Institute for Clinical systems Improvement. Routine Prenatal Care. 12th ed. August 2008. Available at: http://www.icsi.org/prenatal_care_4/prenatal_care__routine__full_version__2.html. Accessed november 7, 2008.
2. Grant A, Elbourne D, Valentin L, et al. Routine formal fetal movement counting and risk of antepartum late death in normally formed singletons. Lancet. 1989;2:345-349.
3. Harrington K, Thompson O, Jordan L, et al. Obstetric outcome in women who present with a reduction in fetal movements in the third trimester of pregnancy. J Perinat Med. 1998;26:77-82.
4. Mangesi L, Hofmeyr GJ. Fetal movement counting for assessment of fetal wellbeing. Cochrane Database Syst Rev. 2007;(1):CD004909.-
5. Moore TR, Piacquadio K. A prospective evaluation of fetal movement screening to reduce the incidence of antepartum fetal death. Am J Obstet Gynecol. 1989;160:1075-1080.
6. ACOG. Antepartum Fetal Surveillance. ACOG Practice Bulletin, Number 9. Washington, DC: American College of Obstetrics and Gynecology; October 1999.
7. National Institute for Clinical Excellence. Antenatal Care: Routine Care for the Healthy Pregnant Woman. Clinical Guideline 62. London: National Institute for Health and Clinical Excellence; March 2008.
No. Structured daily monitoring of fetal movement doesn’t decrease the rate of all-cause antenatal death in average-risk pregnancies (strength of recommendation [SOR]: B, single good-quality, randomized controlled trial [RCT]). Although maternal perception of decreased fetal movement may herald fetal death, it isn’t specific for poor neonatal outcome (SOR: B, single good-quality, diagnostic cohort study). Monitoring fetal movement increases the frequency of non-stress-test monitoring (SOR: B, single good-quality RCT).
A rare tragedy that monitoring can’t prevent
Johanna Warren, MD
Oregon Health and Sciences University, Portland
Fetal movement is a marker of well-being. We draw on our experience with fetal monitoring to know that in healthy fetuses, movement increases sympathetic response and accelerates heart rate. Fetuses with severe acid-base disorders can’t oxygenate their muscles adequately and don’t move. Fetal movement, therefore, is a relatively simple indirect means of fetal assessment that indicates a lack of significant acidosis.
Intrauterine fetal demise (IUFD) is a rare but devastating event in an uncomplicated term pregnancy; it occurs in about 5000 of nearly 4 million us births each year (0.125). As the authors of this Clinical Inquiry state, nearly half of term IUFDs are unexpected and unexplained. Although it may be a logical extension to apply our knowledge of fetal physiology in an attempt to prevent IUFD, no conclusive evidence suggests that daily monitoring of fetal movement improves fetal or neonatal outcomes. We can hope that, with more accurate dating methods and more aggressive control of hypertension, diabetes, and anemia in pregnancy, the number of term IUFDs will continue to fall.
Evidence summary
Nearly 50% of late-pregnancy IUFDs have no associated risk factors. Fetal demise, however, may be heralded by decreased fetal movement followed by cessation of movement at least 12 hours before death.1 Maternal monitoring of fetal movement by kick counts has been proposed as a method to verify fetal well-being and decrease the rate of IUFD in the general obstetric population.
Counting doesn’t reduce antenatal death, large study shows
A well-done RCT randomized 68,654 women to either usual care or structured, daily monitoring of fetal movement using the count-to-10 method—daily maternal documentation of the amount of time it takes to perceive 10 fetal movements. Usual care was comprised of a query about fetal movement at antenatal visits and instruction to perform fetal movement monitoring at the provider’s discretion. Mothers were told to visit their health-care provider for evaluation if they felt no movement in 24 hours or fewer than 10 movements in 10 hours during a 48-hour period. The trial showed no benefit from monitoring in reducing the rate of antenatal death from all causes.
The rate of all fetal deaths in the counting group was 2.9 per 1000 normally formed, live, singleton births; the rate in the control group was 2.67 (absolute risk reduction=0.24; 95% confidence interval [CI], –0.5 to 0.98). Women in the counting group spent an average of 160 hours counting during pregnancy and had a statistically significant increase in fetal non-stress-test (NST) monitoring (odds ratio [OR]=1.39; 95% CI, 1.31-1.49; number needed to harm [NNH]=50 to cause 1 additional NST). A statistically insignificant trend toward increased antepartum admissions was also noted in the counting group.2
Maternal perception of less movement not linked to fetal outcome
A retrospective cohort study of 6793 patients compared pregnancy outcomes of 463 women who presented for evaluation of decreased fetal movement with outcomes among the general obstetric population. The study excluded women who reported complete cessation of fetal movement.
Pregnancies evaluated for decreased fetal movement were less likely to have an Apgar score <7 at 5 minutes (relative risk [RR]=0.56; 95% CI, 0.29-0.96; P=.05) and less likely to be preterm (RR=0.68; 95% CI, 0.48-0.94; P=.02). No significant difference in cesarean section for fetal distress or admission to the neonatal intensive care unit was noted between the study and control groups. The study suggests that maternal perception of decreased fetal movement is not associated with poor fetal outcome.3
A recent rigorous systematic review yielded no significant outcome effect related to fetal kick counts.4 A prospective cohort study of 4383 births in California, using historical controls, found a drop in fetal mortality from 8.7 to 2.1 deaths/1000. The historical control rate was higher than statewide data from the same time period, however. The overall weaker design of the study and probable effect of regression to the mean significantly limit the interpretation of outcomes.5
Recommendations
The American College of Obstetrics and Gynecology (ACOG) makes no recommendation for or against assessing daily fetal movement in routine pregnancies. ACOG notes that no consistent evidence suggests that formal assessment of fetal movement decreases IUFD.6
The Institute for Clinical Systems Improvement recommends instructing patients on “daily identification of fetal movement at the 28-week visit.” The institute doesn’t recommend specific criteria for evaluating fetal movements or offer recommendations for follow-up of a maternal report of decreased fetal movement.1 The National Institute for Clinical Excellence in Great Britain recommends against routine formal fetal-movement counting.7
No. Structured daily monitoring of fetal movement doesn’t decrease the rate of all-cause antenatal death in average-risk pregnancies (strength of recommendation [SOR]: B, single good-quality, randomized controlled trial [RCT]). Although maternal perception of decreased fetal movement may herald fetal death, it isn’t specific for poor neonatal outcome (SOR: B, single good-quality, diagnostic cohort study). Monitoring fetal movement increases the frequency of non-stress-test monitoring (SOR: B, single good-quality RCT).
A rare tragedy that monitoring can’t prevent
Johanna Warren, MD
Oregon Health and Sciences University, Portland
Fetal movement is a marker of well-being. We draw on our experience with fetal monitoring to know that in healthy fetuses, movement increases sympathetic response and accelerates heart rate. Fetuses with severe acid-base disorders can’t oxygenate their muscles adequately and don’t move. Fetal movement, therefore, is a relatively simple indirect means of fetal assessment that indicates a lack of significant acidosis.
Intrauterine fetal demise (IUFD) is a rare but devastating event in an uncomplicated term pregnancy; it occurs in about 5000 of nearly 4 million us births each year (0.125). As the authors of this Clinical Inquiry state, nearly half of term IUFDs are unexpected and unexplained. Although it may be a logical extension to apply our knowledge of fetal physiology in an attempt to prevent IUFD, no conclusive evidence suggests that daily monitoring of fetal movement improves fetal or neonatal outcomes. We can hope that, with more accurate dating methods and more aggressive control of hypertension, diabetes, and anemia in pregnancy, the number of term IUFDs will continue to fall.
Evidence summary
Nearly 50% of late-pregnancy IUFDs have no associated risk factors. Fetal demise, however, may be heralded by decreased fetal movement followed by cessation of movement at least 12 hours before death.1 Maternal monitoring of fetal movement by kick counts has been proposed as a method to verify fetal well-being and decrease the rate of IUFD in the general obstetric population.
Counting doesn’t reduce antenatal death, large study shows
A well-done RCT randomized 68,654 women to either usual care or structured, daily monitoring of fetal movement using the count-to-10 method—daily maternal documentation of the amount of time it takes to perceive 10 fetal movements. Usual care was comprised of a query about fetal movement at antenatal visits and instruction to perform fetal movement monitoring at the provider’s discretion. Mothers were told to visit their health-care provider for evaluation if they felt no movement in 24 hours or fewer than 10 movements in 10 hours during a 48-hour period. The trial showed no benefit from monitoring in reducing the rate of antenatal death from all causes.
The rate of all fetal deaths in the counting group was 2.9 per 1000 normally formed, live, singleton births; the rate in the control group was 2.67 (absolute risk reduction=0.24; 95% confidence interval [CI], –0.5 to 0.98). Women in the counting group spent an average of 160 hours counting during pregnancy and had a statistically significant increase in fetal non-stress-test (NST) monitoring (odds ratio [OR]=1.39; 95% CI, 1.31-1.49; number needed to harm [NNH]=50 to cause 1 additional NST). A statistically insignificant trend toward increased antepartum admissions was also noted in the counting group.2
Maternal perception of less movement not linked to fetal outcome
A retrospective cohort study of 6793 patients compared pregnancy outcomes of 463 women who presented for evaluation of decreased fetal movement with outcomes among the general obstetric population. The study excluded women who reported complete cessation of fetal movement.
Pregnancies evaluated for decreased fetal movement were less likely to have an Apgar score <7 at 5 minutes (relative risk [RR]=0.56; 95% CI, 0.29-0.96; P=.05) and less likely to be preterm (RR=0.68; 95% CI, 0.48-0.94; P=.02). No significant difference in cesarean section for fetal distress or admission to the neonatal intensive care unit was noted between the study and control groups. The study suggests that maternal perception of decreased fetal movement is not associated with poor fetal outcome.3
A recent rigorous systematic review yielded no significant outcome effect related to fetal kick counts.4 A prospective cohort study of 4383 births in California, using historical controls, found a drop in fetal mortality from 8.7 to 2.1 deaths/1000. The historical control rate was higher than statewide data from the same time period, however. The overall weaker design of the study and probable effect of regression to the mean significantly limit the interpretation of outcomes.5
Recommendations
The American College of Obstetrics and Gynecology (ACOG) makes no recommendation for or against assessing daily fetal movement in routine pregnancies. ACOG notes that no consistent evidence suggests that formal assessment of fetal movement decreases IUFD.6
The Institute for Clinical Systems Improvement recommends instructing patients on “daily identification of fetal movement at the 28-week visit.” The institute doesn’t recommend specific criteria for evaluating fetal movements or offer recommendations for follow-up of a maternal report of decreased fetal movement.1 The National Institute for Clinical Excellence in Great Britain recommends against routine formal fetal-movement counting.7
1. Institute for Clinical systems Improvement. Routine Prenatal Care. 12th ed. August 2008. Available at: http://www.icsi.org/prenatal_care_4/prenatal_care__routine__full_version__2.html. Accessed november 7, 2008.
2. Grant A, Elbourne D, Valentin L, et al. Routine formal fetal movement counting and risk of antepartum late death in normally formed singletons. Lancet. 1989;2:345-349.
3. Harrington K, Thompson O, Jordan L, et al. Obstetric outcome in women who present with a reduction in fetal movements in the third trimester of pregnancy. J Perinat Med. 1998;26:77-82.
4. Mangesi L, Hofmeyr GJ. Fetal movement counting for assessment of fetal wellbeing. Cochrane Database Syst Rev. 2007;(1):CD004909.-
5. Moore TR, Piacquadio K. A prospective evaluation of fetal movement screening to reduce the incidence of antepartum fetal death. Am J Obstet Gynecol. 1989;160:1075-1080.
6. ACOG. Antepartum Fetal Surveillance. ACOG Practice Bulletin, Number 9. Washington, DC: American College of Obstetrics and Gynecology; October 1999.
7. National Institute for Clinical Excellence. Antenatal Care: Routine Care for the Healthy Pregnant Woman. Clinical Guideline 62. London: National Institute for Health and Clinical Excellence; March 2008.
1. Institute for Clinical systems Improvement. Routine Prenatal Care. 12th ed. August 2008. Available at: http://www.icsi.org/prenatal_care_4/prenatal_care__routine__full_version__2.html. Accessed november 7, 2008.
2. Grant A, Elbourne D, Valentin L, et al. Routine formal fetal movement counting and risk of antepartum late death in normally formed singletons. Lancet. 1989;2:345-349.
3. Harrington K, Thompson O, Jordan L, et al. Obstetric outcome in women who present with a reduction in fetal movements in the third trimester of pregnancy. J Perinat Med. 1998;26:77-82.
4. Mangesi L, Hofmeyr GJ. Fetal movement counting for assessment of fetal wellbeing. Cochrane Database Syst Rev. 2007;(1):CD004909.-
5. Moore TR, Piacquadio K. A prospective evaluation of fetal movement screening to reduce the incidence of antepartum fetal death. Am J Obstet Gynecol. 1989;160:1075-1080.
6. ACOG. Antepartum Fetal Surveillance. ACOG Practice Bulletin, Number 9. Washington, DC: American College of Obstetrics and Gynecology; October 1999.
7. National Institute for Clinical Excellence. Antenatal Care: Routine Care for the Healthy Pregnant Woman. Clinical Guideline 62. London: National Institute for Health and Clinical Excellence; March 2008.
Evidence-based answers from the Family Physicians Inquiries Network
What is the best way to manage phantom limb pain?
No single best therapy for phantom limb pain (PLP) exists. Treatment requires a coordinated application of conservative, pharmacologic, and adjuvant therapies.
Evaluative management (including prosthesis adjustment, treatment of referred pain, and residual limb care) should be tried initially (strength of recommendation [SOR]: C, expert opinion). Other first-line treatments such as transcutaneous electrical nerve stimulation (TENS) (SOR: A, multiple high-quality randomized, control trials [RCTs]), and biofeedback (SOR: B, numerous case studies) can reduce PLP. Pharmacotherapy, including opioids, anticonvulsants (gabapentin), and nonsteroidal anti-inflammatory drugs (NSAIDs), can also relieve pain (SOR: B, initial RCTs and inconsistent findings).
Adjuvant therapies (mirror box therapy, acupuncture, calcitonin, and N-methyl d-aspartate receptor antagonists) haven’t been rigorously investigated for alleviating PLP, but can be considered for patients who have failed other treatments.
Evidence summary
An estimated 1.7 million people in the United States are living with limb loss. The number is expected to increase because of ongoing military conflicts.1 The incidence of PLP is 60% to 80% among amputees.1
A multidisciplinary approach
A lack of comparative clinical trials of therapies for PLP has led health-care providers to adopt a multidisciplinary approach that combines evaluative management, desensitization, psychotherapy, and pharmacotherapy (FIGURE).
Evaluative management, based largely on expert opinion, includes assessing the fit of the prosthesis, treating referred pain, and assessing aggravating factors. Because residual limb pain can exacerbate PLP, adjusting a poorly fitting prosthesis or providing the patient with NSAIDs when there is evidence of stump inflammation may adequately control pain.2,3 Anatomically distant pain syndromes, such as hip or lower back pain, can also aggravate PLP and should be managed to provide optimal pain relief.2
Desensitization, using TENS, has reduced PLP in multiple placebo-controlled trials and epidemiologic surveys.2-5 TENS is an easy-to-use, low-cost, noninvasive, first-line therapy.5 Its long-term effectiveness in alleviating PLP remains unknown.2 Some experts suggest that pain reductions after 1 year of treatment are comparable to placebo.2 Other forms of desensitization (percussion and massage) are supported only by anecdotal reports.
Psychotherapy, including biofeedback, has been found in several case studies to effectively treat chronic PLP.2,5 Psychotherapy can reportedly reveal the underlying mechanisms (muscle spasm, vascular insufficiency) and therefore direct therapeutic interventions by biofeedback or other focus techniques.2
FIGURE Management of phantom limb pain1-10
*Expert opinion.
†Case studies.
‡Randomized controlled trials or cohort studies.
Pharmacotherapy is best used as an adjunct to other treatments.2 Although PLP is typically treated as neuropathic pain, only a few medications have been critically evaluated for treating it.6 Morphine (number needed to treat [NNT]=2.5; 95% confidence interval [CI], 1.9-3.4) and other opioids, including tramadol (NNT=3.9; 95% CI, 2.7-6.7 in neuropathic pain) help some patients.6,7 Despite the proven benefit of tricyclic antidepressants (TCAs) in other neuropathic pain conditions, a recent RCT demonstrated no benefit of TCAs over placebo in PLP.8 Anticonvulsants, including gabapentin, have documented benefit in neuropathic pain modalities and are often used for PLP.6 However, their value in reducing PLP is still under investigation.6 One 2002 RCT showed benefit regarding an improvement of the visual analog scale by an average of 3 points (on a 10-point scale) after 6 weeks of gabapentin therapy.9 A similarly designed 2006 RCT of gabapentin, however did not identify significant pain reductions.10
Promising adjuvant therapies use mirroring techniques
Of the adjuvant treatments mentioned previously, only mirror box therapy has shown promise. This technique allows the amputee to perceive the missing limb by focusing on the reflection of the remaining limb during specific movements and activities. Theoretically, this perception allows reconfiguration of the amputee’s sensory cortex.
Virtual reality therapy employs similar techniques based on the idea that the brain can be deceived. Initial case studies are promising and have prompted further research.11
Recommendations
The US Department of Veterans Affairs and Department of Defense recently issued clinical guidelines for rehabilitating lower-limb amputees that include a segment on pain management.12 The guidelines stress the importance of an interdisciplinary team approach that addresses each pathology plaguing the amputee.
They recommend narcotics during the immediate postoperative period, followed by transition to a non-narcotic medical regimen during the rehabilitation process. The guidelines don’t support a single, specific pain control method over others; they recommend the following approaches to PLP:
- pharmacologic treatment, which may include antiseizure medications, tricyclic antidepressants, selective serotonin reuptake inhibitors, NSAIDs, dextromethorathane, or long-acting narcotics
- epidural analgesia, patient-controlled analgesia, or regional analgesia
- nonpharmacologic therapies, including TENS, desensitization, scar mobilization, relaxation, and biofeedback.
Acknowledgements
The opinions and assertions contained herein are the private views of the authors and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
1. Ziegler-Graham K, MacKenzie EI, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422-429.
2. Sherman RA. Postamputation pain. In: Jensen TS, Wilson PR, Rice AS, eds. Clinical Pain Management: Chronic Pain. London: Hodder Arnold Publishing; 2002;32:427-436.
3. Wartan SW, Hamann W, Wedley JR, et al. Phantom pain and sensation among British veteran amputees. Br J Anaesth. 1997;78:652-659.
4. Halbert J, Crotty M, Cameron ID. Evidence for the optimal management of acute and chronic phantom pain: a systematic review. Clin J Pain. 2002;18:84-92.
5. Baron R, Wasner G, Lindner V. Optimal treatment of phantom limb pain in the elderly. Drugs Aging. 1998;12:361-376.
6. Finnerup NB, Otto M, McQuay HJ, et al. Algorithm for neuropathic pain treatment: an evidence-based proposal. Pain. 2005;118:289-305.
7. Huse E, Larbig W, Flor H, et al. The effect of opioids on phantom limb pain and cortical reorganization. Pain. 2001;90:47-55.
8. Robinson LR, Czerniecki JM, Ehde DM, et al. Trial of amitriptyline for relief of pain in amputees: results of a randomized controlled study. Arch Phys Med Rehabil. 2004;85:1-6.
9. Bone M, Critchley P, Buggy DJ. Gabapentin in postamputation phantom limb pain: a randomized, double-blind, placebo-controlled, cross-over study. Reg Anesth Pain Med. 2002;27:481-486.
10. Nikolajsen L, Finnerup NB, Kramp S, et al. A randomized study of the effects of gabapentin on post-amputation pain. Anesthesiology. 2006;105:1008-1015.
11. Chan BL, Witt R, Charrow AP, et al. Mirror therapy for phantom limb pain. N Engl J Med. 2007;357:2206-2207.
12. Department of Veterans Affairs/Department of Defense. VA/DoD clinical practice guideline for rehabilitation of lower amputation. Washington, DC: Department of Veterans Affairs, Department of Defense; 2007:1-55. Available at: www.guideline.gov/summary/summary.aspx?doc_id=11758&nbr=006060&string=amputation. Accessed December 13, 2008.
No single best therapy for phantom limb pain (PLP) exists. Treatment requires a coordinated application of conservative, pharmacologic, and adjuvant therapies.
Evaluative management (including prosthesis adjustment, treatment of referred pain, and residual limb care) should be tried initially (strength of recommendation [SOR]: C, expert opinion). Other first-line treatments such as transcutaneous electrical nerve stimulation (TENS) (SOR: A, multiple high-quality randomized, control trials [RCTs]), and biofeedback (SOR: B, numerous case studies) can reduce PLP. Pharmacotherapy, including opioids, anticonvulsants (gabapentin), and nonsteroidal anti-inflammatory drugs (NSAIDs), can also relieve pain (SOR: B, initial RCTs and inconsistent findings).
Adjuvant therapies (mirror box therapy, acupuncture, calcitonin, and N-methyl d-aspartate receptor antagonists) haven’t been rigorously investigated for alleviating PLP, but can be considered for patients who have failed other treatments.
Evidence summary
An estimated 1.7 million people in the United States are living with limb loss. The number is expected to increase because of ongoing military conflicts.1 The incidence of PLP is 60% to 80% among amputees.1
A multidisciplinary approach
A lack of comparative clinical trials of therapies for PLP has led health-care providers to adopt a multidisciplinary approach that combines evaluative management, desensitization, psychotherapy, and pharmacotherapy (FIGURE).
Evaluative management, based largely on expert opinion, includes assessing the fit of the prosthesis, treating referred pain, and assessing aggravating factors. Because residual limb pain can exacerbate PLP, adjusting a poorly fitting prosthesis or providing the patient with NSAIDs when there is evidence of stump inflammation may adequately control pain.2,3 Anatomically distant pain syndromes, such as hip or lower back pain, can also aggravate PLP and should be managed to provide optimal pain relief.2
Desensitization, using TENS, has reduced PLP in multiple placebo-controlled trials and epidemiologic surveys.2-5 TENS is an easy-to-use, low-cost, noninvasive, first-line therapy.5 Its long-term effectiveness in alleviating PLP remains unknown.2 Some experts suggest that pain reductions after 1 year of treatment are comparable to placebo.2 Other forms of desensitization (percussion and massage) are supported only by anecdotal reports.
Psychotherapy, including biofeedback, has been found in several case studies to effectively treat chronic PLP.2,5 Psychotherapy can reportedly reveal the underlying mechanisms (muscle spasm, vascular insufficiency) and therefore direct therapeutic interventions by biofeedback or other focus techniques.2
FIGURE Management of phantom limb pain1-10
*Expert opinion.
†Case studies.
‡Randomized controlled trials or cohort studies.
Pharmacotherapy is best used as an adjunct to other treatments.2 Although PLP is typically treated as neuropathic pain, only a few medications have been critically evaluated for treating it.6 Morphine (number needed to treat [NNT]=2.5; 95% confidence interval [CI], 1.9-3.4) and other opioids, including tramadol (NNT=3.9; 95% CI, 2.7-6.7 in neuropathic pain) help some patients.6,7 Despite the proven benefit of tricyclic antidepressants (TCAs) in other neuropathic pain conditions, a recent RCT demonstrated no benefit of TCAs over placebo in PLP.8 Anticonvulsants, including gabapentin, have documented benefit in neuropathic pain modalities and are often used for PLP.6 However, their value in reducing PLP is still under investigation.6 One 2002 RCT showed benefit regarding an improvement of the visual analog scale by an average of 3 points (on a 10-point scale) after 6 weeks of gabapentin therapy.9 A similarly designed 2006 RCT of gabapentin, however did not identify significant pain reductions.10
Promising adjuvant therapies use mirroring techniques
Of the adjuvant treatments mentioned previously, only mirror box therapy has shown promise. This technique allows the amputee to perceive the missing limb by focusing on the reflection of the remaining limb during specific movements and activities. Theoretically, this perception allows reconfiguration of the amputee’s sensory cortex.
Virtual reality therapy employs similar techniques based on the idea that the brain can be deceived. Initial case studies are promising and have prompted further research.11
Recommendations
The US Department of Veterans Affairs and Department of Defense recently issued clinical guidelines for rehabilitating lower-limb amputees that include a segment on pain management.12 The guidelines stress the importance of an interdisciplinary team approach that addresses each pathology plaguing the amputee.
They recommend narcotics during the immediate postoperative period, followed by transition to a non-narcotic medical regimen during the rehabilitation process. The guidelines don’t support a single, specific pain control method over others; they recommend the following approaches to PLP:
- pharmacologic treatment, which may include antiseizure medications, tricyclic antidepressants, selective serotonin reuptake inhibitors, NSAIDs, dextromethorathane, or long-acting narcotics
- epidural analgesia, patient-controlled analgesia, or regional analgesia
- nonpharmacologic therapies, including TENS, desensitization, scar mobilization, relaxation, and biofeedback.
Acknowledgements
The opinions and assertions contained herein are the private views of the authors and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
No single best therapy for phantom limb pain (PLP) exists. Treatment requires a coordinated application of conservative, pharmacologic, and adjuvant therapies.
Evaluative management (including prosthesis adjustment, treatment of referred pain, and residual limb care) should be tried initially (strength of recommendation [SOR]: C, expert opinion). Other first-line treatments such as transcutaneous electrical nerve stimulation (TENS) (SOR: A, multiple high-quality randomized, control trials [RCTs]), and biofeedback (SOR: B, numerous case studies) can reduce PLP. Pharmacotherapy, including opioids, anticonvulsants (gabapentin), and nonsteroidal anti-inflammatory drugs (NSAIDs), can also relieve pain (SOR: B, initial RCTs and inconsistent findings).
Adjuvant therapies (mirror box therapy, acupuncture, calcitonin, and N-methyl d-aspartate receptor antagonists) haven’t been rigorously investigated for alleviating PLP, but can be considered for patients who have failed other treatments.
Evidence summary
An estimated 1.7 million people in the United States are living with limb loss. The number is expected to increase because of ongoing military conflicts.1 The incidence of PLP is 60% to 80% among amputees.1
A multidisciplinary approach
A lack of comparative clinical trials of therapies for PLP has led health-care providers to adopt a multidisciplinary approach that combines evaluative management, desensitization, psychotherapy, and pharmacotherapy (FIGURE).
Evaluative management, based largely on expert opinion, includes assessing the fit of the prosthesis, treating referred pain, and assessing aggravating factors. Because residual limb pain can exacerbate PLP, adjusting a poorly fitting prosthesis or providing the patient with NSAIDs when there is evidence of stump inflammation may adequately control pain.2,3 Anatomically distant pain syndromes, such as hip or lower back pain, can also aggravate PLP and should be managed to provide optimal pain relief.2
Desensitization, using TENS, has reduced PLP in multiple placebo-controlled trials and epidemiologic surveys.2-5 TENS is an easy-to-use, low-cost, noninvasive, first-line therapy.5 Its long-term effectiveness in alleviating PLP remains unknown.2 Some experts suggest that pain reductions after 1 year of treatment are comparable to placebo.2 Other forms of desensitization (percussion and massage) are supported only by anecdotal reports.
Psychotherapy, including biofeedback, has been found in several case studies to effectively treat chronic PLP.2,5 Psychotherapy can reportedly reveal the underlying mechanisms (muscle spasm, vascular insufficiency) and therefore direct therapeutic interventions by biofeedback or other focus techniques.2
FIGURE Management of phantom limb pain1-10
*Expert opinion.
†Case studies.
‡Randomized controlled trials or cohort studies.
Pharmacotherapy is best used as an adjunct to other treatments.2 Although PLP is typically treated as neuropathic pain, only a few medications have been critically evaluated for treating it.6 Morphine (number needed to treat [NNT]=2.5; 95% confidence interval [CI], 1.9-3.4) and other opioids, including tramadol (NNT=3.9; 95% CI, 2.7-6.7 in neuropathic pain) help some patients.6,7 Despite the proven benefit of tricyclic antidepressants (TCAs) in other neuropathic pain conditions, a recent RCT demonstrated no benefit of TCAs over placebo in PLP.8 Anticonvulsants, including gabapentin, have documented benefit in neuropathic pain modalities and are often used for PLP.6 However, their value in reducing PLP is still under investigation.6 One 2002 RCT showed benefit regarding an improvement of the visual analog scale by an average of 3 points (on a 10-point scale) after 6 weeks of gabapentin therapy.9 A similarly designed 2006 RCT of gabapentin, however did not identify significant pain reductions.10
Promising adjuvant therapies use mirroring techniques
Of the adjuvant treatments mentioned previously, only mirror box therapy has shown promise. This technique allows the amputee to perceive the missing limb by focusing on the reflection of the remaining limb during specific movements and activities. Theoretically, this perception allows reconfiguration of the amputee’s sensory cortex.
Virtual reality therapy employs similar techniques based on the idea that the brain can be deceived. Initial case studies are promising and have prompted further research.11
Recommendations
The US Department of Veterans Affairs and Department of Defense recently issued clinical guidelines for rehabilitating lower-limb amputees that include a segment on pain management.12 The guidelines stress the importance of an interdisciplinary team approach that addresses each pathology plaguing the amputee.
They recommend narcotics during the immediate postoperative period, followed by transition to a non-narcotic medical regimen during the rehabilitation process. The guidelines don’t support a single, specific pain control method over others; they recommend the following approaches to PLP:
- pharmacologic treatment, which may include antiseizure medications, tricyclic antidepressants, selective serotonin reuptake inhibitors, NSAIDs, dextromethorathane, or long-acting narcotics
- epidural analgesia, patient-controlled analgesia, or regional analgesia
- nonpharmacologic therapies, including TENS, desensitization, scar mobilization, relaxation, and biofeedback.
Acknowledgements
The opinions and assertions contained herein are the private views of the authors and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
1. Ziegler-Graham K, MacKenzie EI, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422-429.
2. Sherman RA. Postamputation pain. In: Jensen TS, Wilson PR, Rice AS, eds. Clinical Pain Management: Chronic Pain. London: Hodder Arnold Publishing; 2002;32:427-436.
3. Wartan SW, Hamann W, Wedley JR, et al. Phantom pain and sensation among British veteran amputees. Br J Anaesth. 1997;78:652-659.
4. Halbert J, Crotty M, Cameron ID. Evidence for the optimal management of acute and chronic phantom pain: a systematic review. Clin J Pain. 2002;18:84-92.
5. Baron R, Wasner G, Lindner V. Optimal treatment of phantom limb pain in the elderly. Drugs Aging. 1998;12:361-376.
6. Finnerup NB, Otto M, McQuay HJ, et al. Algorithm for neuropathic pain treatment: an evidence-based proposal. Pain. 2005;118:289-305.
7. Huse E, Larbig W, Flor H, et al. The effect of opioids on phantom limb pain and cortical reorganization. Pain. 2001;90:47-55.
8. Robinson LR, Czerniecki JM, Ehde DM, et al. Trial of amitriptyline for relief of pain in amputees: results of a randomized controlled study. Arch Phys Med Rehabil. 2004;85:1-6.
9. Bone M, Critchley P, Buggy DJ. Gabapentin in postamputation phantom limb pain: a randomized, double-blind, placebo-controlled, cross-over study. Reg Anesth Pain Med. 2002;27:481-486.
10. Nikolajsen L, Finnerup NB, Kramp S, et al. A randomized study of the effects of gabapentin on post-amputation pain. Anesthesiology. 2006;105:1008-1015.
11. Chan BL, Witt R, Charrow AP, et al. Mirror therapy for phantom limb pain. N Engl J Med. 2007;357:2206-2207.
12. Department of Veterans Affairs/Department of Defense. VA/DoD clinical practice guideline for rehabilitation of lower amputation. Washington, DC: Department of Veterans Affairs, Department of Defense; 2007:1-55. Available at: www.guideline.gov/summary/summary.aspx?doc_id=11758&nbr=006060&string=amputation. Accessed December 13, 2008.
1. Ziegler-Graham K, MacKenzie EI, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422-429.
2. Sherman RA. Postamputation pain. In: Jensen TS, Wilson PR, Rice AS, eds. Clinical Pain Management: Chronic Pain. London: Hodder Arnold Publishing; 2002;32:427-436.
3. Wartan SW, Hamann W, Wedley JR, et al. Phantom pain and sensation among British veteran amputees. Br J Anaesth. 1997;78:652-659.
4. Halbert J, Crotty M, Cameron ID. Evidence for the optimal management of acute and chronic phantom pain: a systematic review. Clin J Pain. 2002;18:84-92.
5. Baron R, Wasner G, Lindner V. Optimal treatment of phantom limb pain in the elderly. Drugs Aging. 1998;12:361-376.
6. Finnerup NB, Otto M, McQuay HJ, et al. Algorithm for neuropathic pain treatment: an evidence-based proposal. Pain. 2005;118:289-305.
7. Huse E, Larbig W, Flor H, et al. The effect of opioids on phantom limb pain and cortical reorganization. Pain. 2001;90:47-55.
8. Robinson LR, Czerniecki JM, Ehde DM, et al. Trial of amitriptyline for relief of pain in amputees: results of a randomized controlled study. Arch Phys Med Rehabil. 2004;85:1-6.
9. Bone M, Critchley P, Buggy DJ. Gabapentin in postamputation phantom limb pain: a randomized, double-blind, placebo-controlled, cross-over study. Reg Anesth Pain Med. 2002;27:481-486.
10. Nikolajsen L, Finnerup NB, Kramp S, et al. A randomized study of the effects of gabapentin on post-amputation pain. Anesthesiology. 2006;105:1008-1015.
11. Chan BL, Witt R, Charrow AP, et al. Mirror therapy for phantom limb pain. N Engl J Med. 2007;357:2206-2207.
12. Department of Veterans Affairs/Department of Defense. VA/DoD clinical practice guideline for rehabilitation of lower amputation. Washington, DC: Department of Veterans Affairs, Department of Defense; 2007:1-55. Available at: www.guideline.gov/summary/summary.aspx?doc_id=11758&nbr=006060&string=amputation. Accessed December 13, 2008.
Evidence-based answers from the Family Physicians Inquiries Network
What is the best treatment for oral thrush in healthy infants?
Nystatin oral suspension is a safe first-line therapy; fluconazole is more effective (strength of recommendation [SOR]: B, 1 small randomized controlled trial [RCT]) but has not been approved by the Food and Drug Administration (FDA) for use in immunocompetent infants. Miconazole oral gel is also more effective than nystatin suspension, but is not commercially available in the united states (SOR: B, one small RCT). Gentian violet may be effective, but it stains skin and clothes and is associated with mucosal ulceration (SOR: B, 1 small retrospective cohort study).
Fluconazole isn’t worth the higher cost
Daniel Triezenberg, MD
St. Joseph Regional Medical Center, South Bend, Ind
I reassure parents that oral thrush in infants is rarely a sign of serious illness and recommend nystatin suspension 0.5 cc qid––a smaller dose than reported in this review. Larger doses are more often spit out or swallowed, and at the smaller dose, a 60-mL bottle suppresses the yeast adequately for 2 weeks. My goal is to suppress yeast overgrowth until the infant’s immune system and bacterial flora mature. This review doesn’t convince me that fluconazole, which costs more than nystatin, is worth the added expense. Gentian violet is very messy, and I rarely recommend it. For refractory thrush in breastfed infants, I recommend that the mother apply a topical antifungal to the nipple area.
Evidence summary
Few studies have compared treatment options for oropharyngeal candidiasis in immunocompetent infants. In a survey of 312 health care providers, approximately 75% of the respondents reported treating thrush with oral nystatin, citing fewer side effects and lower cost.1 However, nystatin has proved less effective than either miconazole gel or oral fluconazole.
Nystatin is safe and available, but other options work better
Miconazole vs nystatin. An unblinded RCT assigned 83 immunocompetent infants with culture-positive oral thrush to receive either 25 mg miconazole oral gel (not commercially available in the United States) or nystatin suspension (1 mL of 100,000 IU/mL) qid after meals. The clinical cure rate, defined as absence of plaques by day 12, was significantly higher in the miconazole group (99% for miconazole, 54% for nystatin; P<.0001, number needed to treat [NNT]=2). The eradication rate, confirmed by cultures collected in a blinded manner on the day of clinical cure, was also higher in the miconazole group (55.7% for miconazole, 15.2% for nystatin; P<.0001, NNT=3). In successfully treated patients, infection recurred with similar frequency in both treatment groups within 4 weeks (miconazole, 12.4%; nystatin, 13.0%). Side effects—mostly vomiting and, infrequently, diarrhea—were rare in both groups (miconazole, 4.5%; nystatin 3.5%).2
An earlier, unblinded RCT of 95 infants compared miconazole gel to 2 nystatin oral gels (gel A: 250,000 IU/g with 250,000 IU administered as single dose; gel B: 100,000 IU/g with 50,000 IU administered as single dose). Each medication was given qid over the course of 8 to 14 days. The study confirmed higher clinical cure rates with miconazole gel (85.1% for miconazole vs 42.8% for nystatin gel A [P<.0007, NNT=2] and 48.5% for nystatin gel B [P<.004, NNT=3]).3
Fluconazole vs nystatin. In the only prospective RCT (unblinded) to compare oral suspensions of fluconazole and nystatin, 34 infants were randomized to receive either nystatin (1 mL of 100,000 IU/mL) qid for 10 days or fluconazole (3 mg/kg) once a day for 7 days. Mothers of breastfed infants applied nystatin cream to their nipples twice a day for the duration of the infant’s treatment. The clinical cure rate—defined as absence of oral plaques at the end of therapy (day 10 for the nystatin group, day 7 for the fluconazole group)—was significantly higher in the group treated with fluconazole (100% for fluconazole, 32% for nystatin; P<.0001, NNT=2). The eradication rate was also higher with fluconazole (73.3% for fluconazole, 5.6% for nystatin; P<.0001, NNT=2). The patients treated with fluconazole experienced no side effects.4 Fluconazole has been shown to be effective, safe, and easy to use to treat thrush in immunocompromised children,5 but has not been approved by the FDA for use in healthy infants.
Gentian violet is effective, but messy and irritating
A retrospective cohort study that reviewed 69 cases of oral thrush showed that gentian violet achieved a 75% cure rate in an average of 11 days (compared to 55% in 10 days for nystatin). Both treatments shortened the duration of illness compared with the average of 34 days for untreated children.6 However, gentian violet can stain skin and clothes, and case studies have shown an association with ulceration of the buccal mucosa.7
Recommendations
A thorough literature search through the Cochrane Database Systematic Reviews, Agency for Healthcare Research and Quality, National Guideline Clearinghouse, and Medline did not yield any guidelines or consensus statements from other organizations or specialty groups on treating oropharyngeal candidiasis in infants. Neither the American Academy of Pediatrics nor the Infectious Diseases Society of America has issued applicable practice guidelines.
1. Brent NB. Thrush in the breastfeeding dyad: results of a survey on diagnosis and treatment. Clin Pediatr. 2001;40:503-506.
2. Hoppe JE. Treatment of oropharyngeal candidiasis in immunocompetent infants: a randomized multicenter study of miconazole gel vs. nystatin suspension. The Antifungals Study Group. Pediatr Infect Dis J. 1997;16:288-293.
3. Hoppe JE, Hahn H. Randomized comparison of two nystatin oral gels with miconazole oral gel for treatment of oral thrush in infants. Antimycotics Study Group. Infection. 1996;24:136-139.
4. Goins RA, Ascher D, Waecker N, et al. Comparison of fluconazole and nystatin oral suspensions for treatment of oral candidiasis in infants. Pediatr Infect Dis J. 2002;21:1165-1167.
5. Flynn PM, Cunningham CK, Kerkering T, et al. Oropharyngeal candidiasis in immunocompromised children: a randomized, multicenter study of orally administered fluconazole suspension versus nystatin. The Multicenter Fluconazole Study Group. J Pediatr. 1995;127:322-328.
6. Kozinn PJ, Taschdjian CL, Dragutsky D, et al. Therapy of oral thrush: a comparative evaluation of gentian violet, mycostatin, and amphotericin B. Monographs on Therapy. 1957;2:16-24.
7. Leung AK. Gentian violet in the treatment of oral candidiasis. Pediatr Infect Dis J. 1988;7:304-305.
Nystatin oral suspension is a safe first-line therapy; fluconazole is more effective (strength of recommendation [SOR]: B, 1 small randomized controlled trial [RCT]) but has not been approved by the Food and Drug Administration (FDA) for use in immunocompetent infants. Miconazole oral gel is also more effective than nystatin suspension, but is not commercially available in the united states (SOR: B, one small RCT). Gentian violet may be effective, but it stains skin and clothes and is associated with mucosal ulceration (SOR: B, 1 small retrospective cohort study).
Fluconazole isn’t worth the higher cost
Daniel Triezenberg, MD
St. Joseph Regional Medical Center, South Bend, Ind
I reassure parents that oral thrush in infants is rarely a sign of serious illness and recommend nystatin suspension 0.5 cc qid––a smaller dose than reported in this review. Larger doses are more often spit out or swallowed, and at the smaller dose, a 60-mL bottle suppresses the yeast adequately for 2 weeks. My goal is to suppress yeast overgrowth until the infant’s immune system and bacterial flora mature. This review doesn’t convince me that fluconazole, which costs more than nystatin, is worth the added expense. Gentian violet is very messy, and I rarely recommend it. For refractory thrush in breastfed infants, I recommend that the mother apply a topical antifungal to the nipple area.
Evidence summary
Few studies have compared treatment options for oropharyngeal candidiasis in immunocompetent infants. In a survey of 312 health care providers, approximately 75% of the respondents reported treating thrush with oral nystatin, citing fewer side effects and lower cost.1 However, nystatin has proved less effective than either miconazole gel or oral fluconazole.
Nystatin is safe and available, but other options work better
Miconazole vs nystatin. An unblinded RCT assigned 83 immunocompetent infants with culture-positive oral thrush to receive either 25 mg miconazole oral gel (not commercially available in the United States) or nystatin suspension (1 mL of 100,000 IU/mL) qid after meals. The clinical cure rate, defined as absence of plaques by day 12, was significantly higher in the miconazole group (99% for miconazole, 54% for nystatin; P<.0001, number needed to treat [NNT]=2). The eradication rate, confirmed by cultures collected in a blinded manner on the day of clinical cure, was also higher in the miconazole group (55.7% for miconazole, 15.2% for nystatin; P<.0001, NNT=3). In successfully treated patients, infection recurred with similar frequency in both treatment groups within 4 weeks (miconazole, 12.4%; nystatin, 13.0%). Side effects—mostly vomiting and, infrequently, diarrhea—were rare in both groups (miconazole, 4.5%; nystatin 3.5%).2
An earlier, unblinded RCT of 95 infants compared miconazole gel to 2 nystatin oral gels (gel A: 250,000 IU/g with 250,000 IU administered as single dose; gel B: 100,000 IU/g with 50,000 IU administered as single dose). Each medication was given qid over the course of 8 to 14 days. The study confirmed higher clinical cure rates with miconazole gel (85.1% for miconazole vs 42.8% for nystatin gel A [P<.0007, NNT=2] and 48.5% for nystatin gel B [P<.004, NNT=3]).3
Fluconazole vs nystatin. In the only prospective RCT (unblinded) to compare oral suspensions of fluconazole and nystatin, 34 infants were randomized to receive either nystatin (1 mL of 100,000 IU/mL) qid for 10 days or fluconazole (3 mg/kg) once a day for 7 days. Mothers of breastfed infants applied nystatin cream to their nipples twice a day for the duration of the infant’s treatment. The clinical cure rate—defined as absence of oral plaques at the end of therapy (day 10 for the nystatin group, day 7 for the fluconazole group)—was significantly higher in the group treated with fluconazole (100% for fluconazole, 32% for nystatin; P<.0001, NNT=2). The eradication rate was also higher with fluconazole (73.3% for fluconazole, 5.6% for nystatin; P<.0001, NNT=2). The patients treated with fluconazole experienced no side effects.4 Fluconazole has been shown to be effective, safe, and easy to use to treat thrush in immunocompromised children,5 but has not been approved by the FDA for use in healthy infants.
Gentian violet is effective, but messy and irritating
A retrospective cohort study that reviewed 69 cases of oral thrush showed that gentian violet achieved a 75% cure rate in an average of 11 days (compared to 55% in 10 days for nystatin). Both treatments shortened the duration of illness compared with the average of 34 days for untreated children.6 However, gentian violet can stain skin and clothes, and case studies have shown an association with ulceration of the buccal mucosa.7
Recommendations
A thorough literature search through the Cochrane Database Systematic Reviews, Agency for Healthcare Research and Quality, National Guideline Clearinghouse, and Medline did not yield any guidelines or consensus statements from other organizations or specialty groups on treating oropharyngeal candidiasis in infants. Neither the American Academy of Pediatrics nor the Infectious Diseases Society of America has issued applicable practice guidelines.
Nystatin oral suspension is a safe first-line therapy; fluconazole is more effective (strength of recommendation [SOR]: B, 1 small randomized controlled trial [RCT]) but has not been approved by the Food and Drug Administration (FDA) for use in immunocompetent infants. Miconazole oral gel is also more effective than nystatin suspension, but is not commercially available in the united states (SOR: B, one small RCT). Gentian violet may be effective, but it stains skin and clothes and is associated with mucosal ulceration (SOR: B, 1 small retrospective cohort study).
Fluconazole isn’t worth the higher cost
Daniel Triezenberg, MD
St. Joseph Regional Medical Center, South Bend, Ind
I reassure parents that oral thrush in infants is rarely a sign of serious illness and recommend nystatin suspension 0.5 cc qid––a smaller dose than reported in this review. Larger doses are more often spit out or swallowed, and at the smaller dose, a 60-mL bottle suppresses the yeast adequately for 2 weeks. My goal is to suppress yeast overgrowth until the infant’s immune system and bacterial flora mature. This review doesn’t convince me that fluconazole, which costs more than nystatin, is worth the added expense. Gentian violet is very messy, and I rarely recommend it. For refractory thrush in breastfed infants, I recommend that the mother apply a topical antifungal to the nipple area.
Evidence summary
Few studies have compared treatment options for oropharyngeal candidiasis in immunocompetent infants. In a survey of 312 health care providers, approximately 75% of the respondents reported treating thrush with oral nystatin, citing fewer side effects and lower cost.1 However, nystatin has proved less effective than either miconazole gel or oral fluconazole.
Nystatin is safe and available, but other options work better
Miconazole vs nystatin. An unblinded RCT assigned 83 immunocompetent infants with culture-positive oral thrush to receive either 25 mg miconazole oral gel (not commercially available in the United States) or nystatin suspension (1 mL of 100,000 IU/mL) qid after meals. The clinical cure rate, defined as absence of plaques by day 12, was significantly higher in the miconazole group (99% for miconazole, 54% for nystatin; P<.0001, number needed to treat [NNT]=2). The eradication rate, confirmed by cultures collected in a blinded manner on the day of clinical cure, was also higher in the miconazole group (55.7% for miconazole, 15.2% for nystatin; P<.0001, NNT=3). In successfully treated patients, infection recurred with similar frequency in both treatment groups within 4 weeks (miconazole, 12.4%; nystatin, 13.0%). Side effects—mostly vomiting and, infrequently, diarrhea—were rare in both groups (miconazole, 4.5%; nystatin 3.5%).2
An earlier, unblinded RCT of 95 infants compared miconazole gel to 2 nystatin oral gels (gel A: 250,000 IU/g with 250,000 IU administered as single dose; gel B: 100,000 IU/g with 50,000 IU administered as single dose). Each medication was given qid over the course of 8 to 14 days. The study confirmed higher clinical cure rates with miconazole gel (85.1% for miconazole vs 42.8% for nystatin gel A [P<.0007, NNT=2] and 48.5% for nystatin gel B [P<.004, NNT=3]).3
Fluconazole vs nystatin. In the only prospective RCT (unblinded) to compare oral suspensions of fluconazole and nystatin, 34 infants were randomized to receive either nystatin (1 mL of 100,000 IU/mL) qid for 10 days or fluconazole (3 mg/kg) once a day for 7 days. Mothers of breastfed infants applied nystatin cream to their nipples twice a day for the duration of the infant’s treatment. The clinical cure rate—defined as absence of oral plaques at the end of therapy (day 10 for the nystatin group, day 7 for the fluconazole group)—was significantly higher in the group treated with fluconazole (100% for fluconazole, 32% for nystatin; P<.0001, NNT=2). The eradication rate was also higher with fluconazole (73.3% for fluconazole, 5.6% for nystatin; P<.0001, NNT=2). The patients treated with fluconazole experienced no side effects.4 Fluconazole has been shown to be effective, safe, and easy to use to treat thrush in immunocompromised children,5 but has not been approved by the FDA for use in healthy infants.
Gentian violet is effective, but messy and irritating
A retrospective cohort study that reviewed 69 cases of oral thrush showed that gentian violet achieved a 75% cure rate in an average of 11 days (compared to 55% in 10 days for nystatin). Both treatments shortened the duration of illness compared with the average of 34 days for untreated children.6 However, gentian violet can stain skin and clothes, and case studies have shown an association with ulceration of the buccal mucosa.7
Recommendations
A thorough literature search through the Cochrane Database Systematic Reviews, Agency for Healthcare Research and Quality, National Guideline Clearinghouse, and Medline did not yield any guidelines or consensus statements from other organizations or specialty groups on treating oropharyngeal candidiasis in infants. Neither the American Academy of Pediatrics nor the Infectious Diseases Society of America has issued applicable practice guidelines.
1. Brent NB. Thrush in the breastfeeding dyad: results of a survey on diagnosis and treatment. Clin Pediatr. 2001;40:503-506.
2. Hoppe JE. Treatment of oropharyngeal candidiasis in immunocompetent infants: a randomized multicenter study of miconazole gel vs. nystatin suspension. The Antifungals Study Group. Pediatr Infect Dis J. 1997;16:288-293.
3. Hoppe JE, Hahn H. Randomized comparison of two nystatin oral gels with miconazole oral gel for treatment of oral thrush in infants. Antimycotics Study Group. Infection. 1996;24:136-139.
4. Goins RA, Ascher D, Waecker N, et al. Comparison of fluconazole and nystatin oral suspensions for treatment of oral candidiasis in infants. Pediatr Infect Dis J. 2002;21:1165-1167.
5. Flynn PM, Cunningham CK, Kerkering T, et al. Oropharyngeal candidiasis in immunocompromised children: a randomized, multicenter study of orally administered fluconazole suspension versus nystatin. The Multicenter Fluconazole Study Group. J Pediatr. 1995;127:322-328.
6. Kozinn PJ, Taschdjian CL, Dragutsky D, et al. Therapy of oral thrush: a comparative evaluation of gentian violet, mycostatin, and amphotericin B. Monographs on Therapy. 1957;2:16-24.
7. Leung AK. Gentian violet in the treatment of oral candidiasis. Pediatr Infect Dis J. 1988;7:304-305.
1. Brent NB. Thrush in the breastfeeding dyad: results of a survey on diagnosis and treatment. Clin Pediatr. 2001;40:503-506.
2. Hoppe JE. Treatment of oropharyngeal candidiasis in immunocompetent infants: a randomized multicenter study of miconazole gel vs. nystatin suspension. The Antifungals Study Group. Pediatr Infect Dis J. 1997;16:288-293.
3. Hoppe JE, Hahn H. Randomized comparison of two nystatin oral gels with miconazole oral gel for treatment of oral thrush in infants. Antimycotics Study Group. Infection. 1996;24:136-139.
4. Goins RA, Ascher D, Waecker N, et al. Comparison of fluconazole and nystatin oral suspensions for treatment of oral candidiasis in infants. Pediatr Infect Dis J. 2002;21:1165-1167.
5. Flynn PM, Cunningham CK, Kerkering T, et al. Oropharyngeal candidiasis in immunocompromised children: a randomized, multicenter study of orally administered fluconazole suspension versus nystatin. The Multicenter Fluconazole Study Group. J Pediatr. 1995;127:322-328.
6. Kozinn PJ, Taschdjian CL, Dragutsky D, et al. Therapy of oral thrush: a comparative evaluation of gentian violet, mycostatin, and amphotericin B. Monographs on Therapy. 1957;2:16-24.
7. Leung AK. Gentian violet in the treatment of oral candidiasis. Pediatr Infect Dis J. 1988;7:304-305.
Evidence-based answers from the Family Physicians Inquiries Network
Do COX-2 inhibitors worsen renal function?
No, COX-2 inhibitors, as a class, do not worsen renal function for those without renal disease. Celecoxib is the only COX-2 inhibitor available, and it is associated with a lower risk of renal dysfunction and hypertension when compared with controls. Available data do not allow for adjusted risk assessment for patients with preexisting renal disease on COX-2 inhibitors (strength of recommendation [SOR]: A, based on meta-analysis).
Use celecoxib cautiously in patients at risk of serious complications
Vincent LO, MD
San Joaquin Family Medicine Residency, French Camp, Calif
Recent studies have raised concerns about the safety of this class of medication. For example, rofecoxib was linked with increased cardiovascular events, leading to it being pulled from the market.1 The claim of decreased gastrointestinal bleeding with long-term use of COX-2 inhibitors has also been questioned.2
Although this Clinical Inquiry concludes that celecoxib does not appear to worsen renal function, it should still be used with caution for patients who are elderly, hospitalized, or at risk of developing serious complications such as acute renal failure, heart failure, and gastrointestinal bleeding.
Evidence summary
A 2006 meta-analysis, including 114 trials and 116,094 patients randomized to either cyclooxygenase-2 (COX-2) inhibitor or control (placebo, nonsteroidal anti-inflammatory drug [NSAID], or mixed), indicated that the COX-2 inhibitors, as a class, had no effect on renal endpoints.3 Trials were reviewed for data on renal endpoints, including peripheral edema, hypertension, and renal dysfunction (defined as significant worsening of serum urea or creatinine, or clinical evidence of kidney disease and renal failure).
When viewed separately, rofecoxib (Vioxx) was associated with a composite relative risk (RR) of 1.53 (95% confidence interval [CI], 1.33–1.76) for all renal endpoints compared with controls. In contrast, the composite RR for the same endpoints among patients taking celecoxib (Celebrex) was 0.97 (95% CI, 0.84–1.12), indicating no effect on renal function. In fact, for the specific outcomes of hypertension and renal dysfunction, celecoxib was associated with a decreased risk compared with controls (TABLE).3
Stratified analysis by type of control (placebo, alternate NSAID, or mixed) yielded consistent results; rofecoxib was uniquely associated with adverse renal outcomes. No effect on renal function was noted for celecoxib compared with the same controls: the RR for adverse renal effects was 0.87 (95% CI, 0.55–1.38), 0.93 (95% CI, 0.70–1.23), and 1.26 (95% CI, 0.94–1.69) for celecoxib vs placebo, NSAID, and mixed controls, respectively. Statistical analysis for heterogeneity showed that the variation in effects on renal function among the COX-2 inhibitors was more likely due to actual differences than due to chance (heterogeneity [I2]=57%; P<.001).
Data were not available to assess the effect of COX-2 agents on patients with pre-existing renal disease, primarily because trials reporting abnormal renal function at baseline were excluded from this meta-analysis.
A recent randomized controlled trial compared standard dosing of diclofenac (75 mg twice daily) and ibuprofen (800 mg 3 times daily) with high-dose celecoxib (400 mg twice daily) for patients with normal kidney function being treated for osteoarthritis and rheumatoid arthritis.4 The mean increase in serum creatinine in the celecoxib arm was less than that noted in the diclofenac controls (0.009 mg/dL vs 0.027 mg/dL; P<.05; number needed to harm [NNH]=56). No difference in mean serum creatinine was seen among those patients using ibuprofen (800 mg 3 times daily) compared with those using high-dose celecoxib.
This evidence further supports the safety of celecoxib vs standard NSAIDs with respect to renal dysfunction.
Recommendations from others The American Pain Society 2002 guideline recommends acetaminophen for mild pain from osteoarthritis.5 For moderate to severe pain and inflammation, a COX-2 inhibitor was the first choice, unless there is significant risk of hypertension or kidney disorder. For active rheumatoid arthritis, the addition of a COX-2 agent to disease-modifying anti-rheumatic drugs (DMARDs) is advised unless there is uncontrolled hypertension or renal disease.6 However, these recommendations came out before the data on the cardiovascular effects of some COX-2 inhibitors.
The American College of rheumatology recommends the use of a COX-2 agent for osteoarthritis or pain unresponsive to acetaminophen. Their 2000 guidelines warn that due to potential renal toxicity, COX-2 inhibitors should not be used for patients with severe renal insufficiency, and used with caution in cases of mild to moderate renal insufficiency.
In 2005, these guidelines were amended to include the recommendation that patients with increased cardiovascular risk be cautioned about the risks associated with COX-2 inhibitor use.7
TABLE
Celecoxib is associated with a decreased risk of hypertension and renal dysfunction
| CELECOXIB | ROFECOXIB | |
|---|---|---|
| Hypertension | 0.83 (95% CI, 0.71–0.97) | 1.55 (95% CI, 1.29–1.85) |
| Peripheral edema | 1.09 (95% CI, 0.91–1.31) | 1.43 (95% CI, 1.23–1.66) |
| Renal dysfunction | 0.61 (95% CI, 0.40–0.94) | 2.31 (95% CI, 1.05–5.07) |
| Source: Zhang J, Ding EL, Song Y, JAMA 2006.3 | ||
1. Bresalier RS, Sandler RS, Quan H, et al. Cardiovascular events associated with rofecoxib in a colorectal adenoma chemoprevention trial. N Engl J Med 2005;352:1092-1102.
2. Hippisley-Cox J, Coupland C, Logan R. Risk of adverse gastrointestinal outcomes in patients taking cyclo-oxygenase-2 inhibitors or conventional non-steroidal anti-inflammatory drugs: population based nested case-control analysis. BMJ 2005;331:1310-1316.
3. Zhang J, Ding EL, Song Y. Adverse effects of cyclooxygenase 2 inhibitors on renal and arrhythmia events. JAMA 2006;296:1619-1632.
4. Whelton A, Lefkowith JL, West CR, Verburg KM. Cardiorenal effects of celecoxib as compared with the nonsteroidal anti-inflammatory drugs diclofenac and ibuprofen. Kidney Intl. 2006;70:1495-1502.
5. Simon LS, Lipman AG, Jacox AK, et al. Pain in Osteoarthritis, Rheumatoid Arthritis and Juvenile Chronic Arthritis. 2nd ed. Glenview, Ill: American Pain society; 2002.
6. American College of Rheumatology (ACR) sub-committee on Osteoarthritis Guidelines. recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. American College of Rheumatology Subcommittee on osteoarthritis Guidelines. Arthritis Rheum. 2000;43:1905-1915.
7. American College of Rheumatology Subcommittee on rheumatoid Arthritis Guidelines. Guidelines for the management of rheumatoid arthritis: 2002 update. Arthritis Rheum. 2002;46:328-346.
No, COX-2 inhibitors, as a class, do not worsen renal function for those without renal disease. Celecoxib is the only COX-2 inhibitor available, and it is associated with a lower risk of renal dysfunction and hypertension when compared with controls. Available data do not allow for adjusted risk assessment for patients with preexisting renal disease on COX-2 inhibitors (strength of recommendation [SOR]: A, based on meta-analysis).
Use celecoxib cautiously in patients at risk of serious complications
Vincent LO, MD
San Joaquin Family Medicine Residency, French Camp, Calif
Recent studies have raised concerns about the safety of this class of medication. For example, rofecoxib was linked with increased cardiovascular events, leading to it being pulled from the market.1 The claim of decreased gastrointestinal bleeding with long-term use of COX-2 inhibitors has also been questioned.2
Although this Clinical Inquiry concludes that celecoxib does not appear to worsen renal function, it should still be used with caution for patients who are elderly, hospitalized, or at risk of developing serious complications such as acute renal failure, heart failure, and gastrointestinal bleeding.
Evidence summary
A 2006 meta-analysis, including 114 trials and 116,094 patients randomized to either cyclooxygenase-2 (COX-2) inhibitor or control (placebo, nonsteroidal anti-inflammatory drug [NSAID], or mixed), indicated that the COX-2 inhibitors, as a class, had no effect on renal endpoints.3 Trials were reviewed for data on renal endpoints, including peripheral edema, hypertension, and renal dysfunction (defined as significant worsening of serum urea or creatinine, or clinical evidence of kidney disease and renal failure).
When viewed separately, rofecoxib (Vioxx) was associated with a composite relative risk (RR) of 1.53 (95% confidence interval [CI], 1.33–1.76) for all renal endpoints compared with controls. In contrast, the composite RR for the same endpoints among patients taking celecoxib (Celebrex) was 0.97 (95% CI, 0.84–1.12), indicating no effect on renal function. In fact, for the specific outcomes of hypertension and renal dysfunction, celecoxib was associated with a decreased risk compared with controls (TABLE).3
Stratified analysis by type of control (placebo, alternate NSAID, or mixed) yielded consistent results; rofecoxib was uniquely associated with adverse renal outcomes. No effect on renal function was noted for celecoxib compared with the same controls: the RR for adverse renal effects was 0.87 (95% CI, 0.55–1.38), 0.93 (95% CI, 0.70–1.23), and 1.26 (95% CI, 0.94–1.69) for celecoxib vs placebo, NSAID, and mixed controls, respectively. Statistical analysis for heterogeneity showed that the variation in effects on renal function among the COX-2 inhibitors was more likely due to actual differences than due to chance (heterogeneity [I2]=57%; P<.001).
Data were not available to assess the effect of COX-2 agents on patients with pre-existing renal disease, primarily because trials reporting abnormal renal function at baseline were excluded from this meta-analysis.
A recent randomized controlled trial compared standard dosing of diclofenac (75 mg twice daily) and ibuprofen (800 mg 3 times daily) with high-dose celecoxib (400 mg twice daily) for patients with normal kidney function being treated for osteoarthritis and rheumatoid arthritis.4 The mean increase in serum creatinine in the celecoxib arm was less than that noted in the diclofenac controls (0.009 mg/dL vs 0.027 mg/dL; P<.05; number needed to harm [NNH]=56). No difference in mean serum creatinine was seen among those patients using ibuprofen (800 mg 3 times daily) compared with those using high-dose celecoxib.
This evidence further supports the safety of celecoxib vs standard NSAIDs with respect to renal dysfunction.
Recommendations from others The American Pain Society 2002 guideline recommends acetaminophen for mild pain from osteoarthritis.5 For moderate to severe pain and inflammation, a COX-2 inhibitor was the first choice, unless there is significant risk of hypertension or kidney disorder. For active rheumatoid arthritis, the addition of a COX-2 agent to disease-modifying anti-rheumatic drugs (DMARDs) is advised unless there is uncontrolled hypertension or renal disease.6 However, these recommendations came out before the data on the cardiovascular effects of some COX-2 inhibitors.
The American College of rheumatology recommends the use of a COX-2 agent for osteoarthritis or pain unresponsive to acetaminophen. Their 2000 guidelines warn that due to potential renal toxicity, COX-2 inhibitors should not be used for patients with severe renal insufficiency, and used with caution in cases of mild to moderate renal insufficiency.
In 2005, these guidelines were amended to include the recommendation that patients with increased cardiovascular risk be cautioned about the risks associated with COX-2 inhibitor use.7
TABLE
Celecoxib is associated with a decreased risk of hypertension and renal dysfunction
| CELECOXIB | ROFECOXIB | |
|---|---|---|
| Hypertension | 0.83 (95% CI, 0.71–0.97) | 1.55 (95% CI, 1.29–1.85) |
| Peripheral edema | 1.09 (95% CI, 0.91–1.31) | 1.43 (95% CI, 1.23–1.66) |
| Renal dysfunction | 0.61 (95% CI, 0.40–0.94) | 2.31 (95% CI, 1.05–5.07) |
| Source: Zhang J, Ding EL, Song Y, JAMA 2006.3 | ||
No, COX-2 inhibitors, as a class, do not worsen renal function for those without renal disease. Celecoxib is the only COX-2 inhibitor available, and it is associated with a lower risk of renal dysfunction and hypertension when compared with controls. Available data do not allow for adjusted risk assessment for patients with preexisting renal disease on COX-2 inhibitors (strength of recommendation [SOR]: A, based on meta-analysis).
Use celecoxib cautiously in patients at risk of serious complications
Vincent LO, MD
San Joaquin Family Medicine Residency, French Camp, Calif
Recent studies have raised concerns about the safety of this class of medication. For example, rofecoxib was linked with increased cardiovascular events, leading to it being pulled from the market.1 The claim of decreased gastrointestinal bleeding with long-term use of COX-2 inhibitors has also been questioned.2
Although this Clinical Inquiry concludes that celecoxib does not appear to worsen renal function, it should still be used with caution for patients who are elderly, hospitalized, or at risk of developing serious complications such as acute renal failure, heart failure, and gastrointestinal bleeding.
Evidence summary
A 2006 meta-analysis, including 114 trials and 116,094 patients randomized to either cyclooxygenase-2 (COX-2) inhibitor or control (placebo, nonsteroidal anti-inflammatory drug [NSAID], or mixed), indicated that the COX-2 inhibitors, as a class, had no effect on renal endpoints.3 Trials were reviewed for data on renal endpoints, including peripheral edema, hypertension, and renal dysfunction (defined as significant worsening of serum urea or creatinine, or clinical evidence of kidney disease and renal failure).
When viewed separately, rofecoxib (Vioxx) was associated with a composite relative risk (RR) of 1.53 (95% confidence interval [CI], 1.33–1.76) for all renal endpoints compared with controls. In contrast, the composite RR for the same endpoints among patients taking celecoxib (Celebrex) was 0.97 (95% CI, 0.84–1.12), indicating no effect on renal function. In fact, for the specific outcomes of hypertension and renal dysfunction, celecoxib was associated with a decreased risk compared with controls (TABLE).3
Stratified analysis by type of control (placebo, alternate NSAID, or mixed) yielded consistent results; rofecoxib was uniquely associated with adverse renal outcomes. No effect on renal function was noted for celecoxib compared with the same controls: the RR for adverse renal effects was 0.87 (95% CI, 0.55–1.38), 0.93 (95% CI, 0.70–1.23), and 1.26 (95% CI, 0.94–1.69) for celecoxib vs placebo, NSAID, and mixed controls, respectively. Statistical analysis for heterogeneity showed that the variation in effects on renal function among the COX-2 inhibitors was more likely due to actual differences than due to chance (heterogeneity [I2]=57%; P<.001).
Data were not available to assess the effect of COX-2 agents on patients with pre-existing renal disease, primarily because trials reporting abnormal renal function at baseline were excluded from this meta-analysis.
A recent randomized controlled trial compared standard dosing of diclofenac (75 mg twice daily) and ibuprofen (800 mg 3 times daily) with high-dose celecoxib (400 mg twice daily) for patients with normal kidney function being treated for osteoarthritis and rheumatoid arthritis.4 The mean increase in serum creatinine in the celecoxib arm was less than that noted in the diclofenac controls (0.009 mg/dL vs 0.027 mg/dL; P<.05; number needed to harm [NNH]=56). No difference in mean serum creatinine was seen among those patients using ibuprofen (800 mg 3 times daily) compared with those using high-dose celecoxib.
This evidence further supports the safety of celecoxib vs standard NSAIDs with respect to renal dysfunction.
Recommendations from others The American Pain Society 2002 guideline recommends acetaminophen for mild pain from osteoarthritis.5 For moderate to severe pain and inflammation, a COX-2 inhibitor was the first choice, unless there is significant risk of hypertension or kidney disorder. For active rheumatoid arthritis, the addition of a COX-2 agent to disease-modifying anti-rheumatic drugs (DMARDs) is advised unless there is uncontrolled hypertension or renal disease.6 However, these recommendations came out before the data on the cardiovascular effects of some COX-2 inhibitors.
The American College of rheumatology recommends the use of a COX-2 agent for osteoarthritis or pain unresponsive to acetaminophen. Their 2000 guidelines warn that due to potential renal toxicity, COX-2 inhibitors should not be used for patients with severe renal insufficiency, and used with caution in cases of mild to moderate renal insufficiency.
In 2005, these guidelines were amended to include the recommendation that patients with increased cardiovascular risk be cautioned about the risks associated with COX-2 inhibitor use.7
TABLE
Celecoxib is associated with a decreased risk of hypertension and renal dysfunction
| CELECOXIB | ROFECOXIB | |
|---|---|---|
| Hypertension | 0.83 (95% CI, 0.71–0.97) | 1.55 (95% CI, 1.29–1.85) |
| Peripheral edema | 1.09 (95% CI, 0.91–1.31) | 1.43 (95% CI, 1.23–1.66) |
| Renal dysfunction | 0.61 (95% CI, 0.40–0.94) | 2.31 (95% CI, 1.05–5.07) |
| Source: Zhang J, Ding EL, Song Y, JAMA 2006.3 | ||
1. Bresalier RS, Sandler RS, Quan H, et al. Cardiovascular events associated with rofecoxib in a colorectal adenoma chemoprevention trial. N Engl J Med 2005;352:1092-1102.
2. Hippisley-Cox J, Coupland C, Logan R. Risk of adverse gastrointestinal outcomes in patients taking cyclo-oxygenase-2 inhibitors or conventional non-steroidal anti-inflammatory drugs: population based nested case-control analysis. BMJ 2005;331:1310-1316.
3. Zhang J, Ding EL, Song Y. Adverse effects of cyclooxygenase 2 inhibitors on renal and arrhythmia events. JAMA 2006;296:1619-1632.
4. Whelton A, Lefkowith JL, West CR, Verburg KM. Cardiorenal effects of celecoxib as compared with the nonsteroidal anti-inflammatory drugs diclofenac and ibuprofen. Kidney Intl. 2006;70:1495-1502.
5. Simon LS, Lipman AG, Jacox AK, et al. Pain in Osteoarthritis, Rheumatoid Arthritis and Juvenile Chronic Arthritis. 2nd ed. Glenview, Ill: American Pain society; 2002.
6. American College of Rheumatology (ACR) sub-committee on Osteoarthritis Guidelines. recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. American College of Rheumatology Subcommittee on osteoarthritis Guidelines. Arthritis Rheum. 2000;43:1905-1915.
7. American College of Rheumatology Subcommittee on rheumatoid Arthritis Guidelines. Guidelines for the management of rheumatoid arthritis: 2002 update. Arthritis Rheum. 2002;46:328-346.
1. Bresalier RS, Sandler RS, Quan H, et al. Cardiovascular events associated with rofecoxib in a colorectal adenoma chemoprevention trial. N Engl J Med 2005;352:1092-1102.
2. Hippisley-Cox J, Coupland C, Logan R. Risk of adverse gastrointestinal outcomes in patients taking cyclo-oxygenase-2 inhibitors or conventional non-steroidal anti-inflammatory drugs: population based nested case-control analysis. BMJ 2005;331:1310-1316.
3. Zhang J, Ding EL, Song Y. Adverse effects of cyclooxygenase 2 inhibitors on renal and arrhythmia events. JAMA 2006;296:1619-1632.
4. Whelton A, Lefkowith JL, West CR, Verburg KM. Cardiorenal effects of celecoxib as compared with the nonsteroidal anti-inflammatory drugs diclofenac and ibuprofen. Kidney Intl. 2006;70:1495-1502.
5. Simon LS, Lipman AG, Jacox AK, et al. Pain in Osteoarthritis, Rheumatoid Arthritis and Juvenile Chronic Arthritis. 2nd ed. Glenview, Ill: American Pain society; 2002.
6. American College of Rheumatology (ACR) sub-committee on Osteoarthritis Guidelines. recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. American College of Rheumatology Subcommittee on osteoarthritis Guidelines. Arthritis Rheum. 2000;43:1905-1915.
7. American College of Rheumatology Subcommittee on rheumatoid Arthritis Guidelines. Guidelines for the management of rheumatoid arthritis: 2002 update. Arthritis Rheum. 2002;46:328-346.
Evidence-based answers from the Family Physicians Inquiries Network
Are DMARDs effective for rheumatologic diseases besides rheumatoid arthritis?
It’s unclear whether disease-modifying antirheumatic agents (DMARDs) as first-line therapy in nonrheumatoid rheumatologic diseases are effective because the question has not been studied. As second-line therapy, the use of some DmArDs appears to be beneficial for patients with psoriatic arthritis (strength of recommendation [SOR]: A, based on systematic reviews of good-quality randomized controlled trials) and ankylosing spondylitis (SOR: B, based on systematic reviews of moderate quality trials). Data on the safety and efficacy of DMARDs as second-line therapy for other arthritic conditions is limited (SOR: C, based on small prospective cohort trials).
There are many options, but remember the risks
Richard Hoffman, MD
Chesterfield Family Medicine Residency, Richmond, Va
Traditionally, nonsteroidal anti-inflammatory agents (NSAIDs) have been the mainstay of treatment for rheumatologic disorders other than rheumatoid arthritis. methotrexate has been used in psoriatic arthritis because it also controls the skin disorder; sulfasalazine has been used in arthritis associated with inflammatory bowel disease, as it helps the bowel disorder itself. However, little evidence shows a definitive benefit for the arthritis.
The advent of tumor necrosis factor (TNF) blockers has changed the direction of research in this area; these agents are being used more and more in inflammatory arthritides. While staying up to date on the TNF antagonists, it’s important to remember the complications associated with them—particularly the increased risk of infections and increased propensity for neoplastic disorders. Consider those on TNF blockers as relatively immunosuppressed (number needed to harm [NNH]=59 for infection and 154 for malignancy).1
Psoriatic arthritis affecting the joints and nails
Evidence summary
The use of DMARDs has become standard of care for rheumatoid arthritis, for both therapy and prevention of progression of this debilitating disease. However, the use of DMARDs in nonrheumatoid rheumatologic disease is still under investigation, and at this point, the use of DMARDs as first-line therapy is not recommended; however, second-line therapy with DMARDs is common.
For psoriatic arthritis, DMARDs are beneficial as a second-line therapy
A Cochrane systematic review identified 13 randomized controlled trials enrolling a combined 1022 patients with psoriatic arthritis randomly assigned to receive a DMARD—methotrexate, sulfasalazine (Azulfidine), azathioprine (Imuran/ Azasan), or etretinate (Tegison; no longer available in the US)—compared with placebo.2 All agents were better than placebo; however, only 2 agents (parenteral high-dose methotrexate and sulfasalazine) had clinically important benefits for more than half the patients. The studies were too small to establish toxicity or to evaluate the other agents.
NSAIDs are still the preferred first-line therapy, concluded a recent publication on the treatment of psoriatic arthritis, which looked at 54 different studies; however, second-line therapy could include methotrexate, sulfasalazine, etanercept (Enbrel), infliximab (Remicade), cyclosporine, or combination therapy.3 Sulfasalazine appeared to be clinically beneficial for peripheral psoriatic arthritis.
Etanercept vs placebo. An initial study (60 patients) of etanercept vs placebo among patients who were permitted to stay on methotrexate or prednisone showed a response rate of 87% vs 23% (P<.0001; number needed to treat [NNT]=1.56).4
Infliximab vs placebo. A study of infliximab vs placebo involving 104 patients had similar results, with good response in 65% vs 10% (NNT=1.81) at 16 weeks; infliximab also inhibited radiographic progression by 22%.5
Cyclosporine. Although it is effective, reserve cyclosporine for patients who do not improve on other regimens, because of its nephrotoxicity.3
DMARDs show some benefit in treating ankylosing spondylitis
Two recent Cochrane systematic reviews on ankylosing spondylitis examined the use of sulfasalazine and methotrexate as second-line agents.6,7 Eleven trials were included in the sulfasalazine analysis, with a total of 895 patients. Sulfasalazine demonstrated some benefit in reducing erythrocyte sedimentation rates (ESRs) and morning stiffness, but there was no evidence that the drug reduced pain or improved physical function, spinal mobility, or rate of enthesitis. Sulfasalazine was well tolerated and may be useful in early mild disease for patients with peripheral arthritis and high ESRs. On the other hand, evidence was insufficient to determine whether methotrexate benefited patients with ankylosing spondylitis.
In other trials, infliximab and etanercept showed good potential for benefit in treating ankylosing spondylitis.
One study of infliximab vs placebo showed 61.2% vs 19.2% patients with good clinical benefit at 24 weeks and only mild or moderate adverse events (P<.001; NNT=2.38).8
Similarly, a smaller study (84 patients) showed that 60% of patients on etanercept vs 20% on placebo had good clinical benefit at only 12 weeks (P<.001, NNT=2.5).9
For other rheumatic diseases, studies are mixed
Due to cyclosporine’s toxicity, less toxic DMARDs are being evaluated to replace it for treatment of other rheumatic diseases. A recent randomized controlled trial of 100 patients with antineutrophil cytoplasmic antibody–associated systemic vasculitis showed methotrexate may be able to replace cyclosporine for both induction of remission (methotrexate=89.8% vs cyclosporine=93.5%; P=.041) and maintenance of remission (69.5% vs 46.5% at 18 months; P=.023).10
Initial trials on other rheumatic diseases have been small and have had varied results. There are mixed studies on the effectiveness of adding methotrexate to corticosteroids for giant cell arteritis.11,12
There has been no evidence of efficacy for the new TNF antagonists in either a small study on Sjögren’s syndrome (n=14)13 or a larger study on Wegener’s granulomatosis (n=180).14
The studies for use of DMARDs in lupus or scleroderma are of limited quality.
Recommendations from others
The Italian Society for Rheumatology consensus guidelines recommends TNF antagonists be considered in active psoriatic arthritis resistant to (a) NSAIDs, (b) at least 2 local steroid injections, and (c) at least 2 conventional DMARDs for patients with peripheral arthritis or enthesitis. They also recommend TNF antagonists be considered for psoriatic spondylitis resistant to NSAIDs.15
The Assessment in Ankylosing Spondylitis (ASAS) International Working Group and the European League Against Rheumatism (EULAR) recommendations for the treatment of ankylosing spondylitis, based on a systematic review of the literature and expert opinion, indicate that:
- There is good evidence for using NSAIDs and COX-2 inhibitors for symptomatic treatment.
- Conventional DMARDs are not well supported.
- TNF antagonists show a large benefit in both pain and function.
The ASAS/EULAR recommendation indicate that there is no evidence that any of these treatments actually modify the disease progression.16
Acknowledgments
The opinions and assertions contained herein are the private views of the authors and not to be construed as official, or as reflecting the views of the US Air Force medical service or the US Air Force at large.
1. Bongartz T, sutton AJ, Sweeting MJ, et al. Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. JAMA 2006;295:2275-2285.
2. Jones G, Crotty M, Brooks P. Interventions for treating psoriatic arthritis. Cochrane Database Syst Rev 2000 (3):CD000212.
3. Manadan Am, Sequeira W, Block JA. The treatment of psoriatic arthritis. Am J Ther 2006;13:72-79.
4. Mease PJ, Goffe BS, Metz J, et al. etanercept in the treatment of psoriatic arthritis and psoriasis: a randomized trial. Lancet 2000;356:385-390.
5. Kavanaugh A, Antoni CE, Gladman D, et al. The Infliximab multinational Psoriatic Arthritis Controlled Trial (ImPACT): result of radiographic analyses after 1 year. Ann Rheum Dis 2006;65:1038-1043.
6. Chen J, Liu C. Sulfasalazine for ankylosing spondylitis. Cochrane Database Syst Rev 2005;(2):CD004800.-
7. Chen J, Liu C, Lin J. Methotrexate for ankylosing spondylitis. Cochrane Database Syst Rev 2006;(4):CD004524.-
8. Heijde D, Dijkmans B, Geusens P, et al. efficacy and safety of infliximab in patients with ankylosing spondylitis. Arthritis Rheum 2005;52:582-591.
9. Calin A, Dijkmans BA, Emery P, et al. Outcomes of a multicentre randomized clinical trial of etanercept to treat ankylosing spondylitis. Ann Rheum Dis 2004;63:1594-1600.
10. Grout K, Rasmussen N, Bacon P, et al. randomized trial of cyclophosphamide versus methotrexate for induction of remission in early systemic antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 2005;52:2461-2469.
11. Jover JA, Hernandez-Garcia C, Morado IC, et al. Combined treatment of giant-cell arteritis with methotrexate and prednisone. a randomized, double blinded, placebo-controlled trial. Ann Intern Med 2001;134:106-114.
12. Hoffman GS, Cid MC, Hellmann DB, et al. A multicenter, randomized, double-blind, placebo-controlled trial of adjuvant methotrexate treatment for giant cell arteritis. Arthritis Rheum 2002;46:1309-1318.
13. Sankar V, Brennan MT, Kok MR, et al. etanercept in sjögren’s syndrome: a twelve-week randomized, double-blind, placebo-controlled pilot clinical trial. Arthritis Rheum 2004;50:2240-2245.
14. Wegener’s Granulomatosis etanercept Trial (WGeT) research Group. etanercept plus standard therapy for Wegener’s granulomatosis. N Engl J Med 2005;352:351-361.
15. Salvarani C, Olivieri I, Pipitone N, et al. recommendations of the Italian society for rheumatology for the use of biologic (TNF-alpha blocking) agents in the treatment of psoriatic arthritis. Clin Exp Rheumatol 2006;24:70-78.
16. Zochling J, van der Heijde D, Dougados, et al. Current evidence for the management of ankylosing spondylitis: a systematic literature review for the AsAs/eulAr management recommendations in ankylosing spondylitis. Ann Rheum Dis 2006;65:442-452.
It’s unclear whether disease-modifying antirheumatic agents (DMARDs) as first-line therapy in nonrheumatoid rheumatologic diseases are effective because the question has not been studied. As second-line therapy, the use of some DmArDs appears to be beneficial for patients with psoriatic arthritis (strength of recommendation [SOR]: A, based on systematic reviews of good-quality randomized controlled trials) and ankylosing spondylitis (SOR: B, based on systematic reviews of moderate quality trials). Data on the safety and efficacy of DMARDs as second-line therapy for other arthritic conditions is limited (SOR: C, based on small prospective cohort trials).
There are many options, but remember the risks
Richard Hoffman, MD
Chesterfield Family Medicine Residency, Richmond, Va
Traditionally, nonsteroidal anti-inflammatory agents (NSAIDs) have been the mainstay of treatment for rheumatologic disorders other than rheumatoid arthritis. methotrexate has been used in psoriatic arthritis because it also controls the skin disorder; sulfasalazine has been used in arthritis associated with inflammatory bowel disease, as it helps the bowel disorder itself. However, little evidence shows a definitive benefit for the arthritis.
The advent of tumor necrosis factor (TNF) blockers has changed the direction of research in this area; these agents are being used more and more in inflammatory arthritides. While staying up to date on the TNF antagonists, it’s important to remember the complications associated with them—particularly the increased risk of infections and increased propensity for neoplastic disorders. Consider those on TNF blockers as relatively immunosuppressed (number needed to harm [NNH]=59 for infection and 154 for malignancy).1
Psoriatic arthritis affecting the joints and nails
Evidence summary
The use of DMARDs has become standard of care for rheumatoid arthritis, for both therapy and prevention of progression of this debilitating disease. However, the use of DMARDs in nonrheumatoid rheumatologic disease is still under investigation, and at this point, the use of DMARDs as first-line therapy is not recommended; however, second-line therapy with DMARDs is common.
For psoriatic arthritis, DMARDs are beneficial as a second-line therapy
A Cochrane systematic review identified 13 randomized controlled trials enrolling a combined 1022 patients with psoriatic arthritis randomly assigned to receive a DMARD—methotrexate, sulfasalazine (Azulfidine), azathioprine (Imuran/ Azasan), or etretinate (Tegison; no longer available in the US)—compared with placebo.2 All agents were better than placebo; however, only 2 agents (parenteral high-dose methotrexate and sulfasalazine) had clinically important benefits for more than half the patients. The studies were too small to establish toxicity or to evaluate the other agents.
NSAIDs are still the preferred first-line therapy, concluded a recent publication on the treatment of psoriatic arthritis, which looked at 54 different studies; however, second-line therapy could include methotrexate, sulfasalazine, etanercept (Enbrel), infliximab (Remicade), cyclosporine, or combination therapy.3 Sulfasalazine appeared to be clinically beneficial for peripheral psoriatic arthritis.
Etanercept vs placebo. An initial study (60 patients) of etanercept vs placebo among patients who were permitted to stay on methotrexate or prednisone showed a response rate of 87% vs 23% (P<.0001; number needed to treat [NNT]=1.56).4
Infliximab vs placebo. A study of infliximab vs placebo involving 104 patients had similar results, with good response in 65% vs 10% (NNT=1.81) at 16 weeks; infliximab also inhibited radiographic progression by 22%.5
Cyclosporine. Although it is effective, reserve cyclosporine for patients who do not improve on other regimens, because of its nephrotoxicity.3
DMARDs show some benefit in treating ankylosing spondylitis
Two recent Cochrane systematic reviews on ankylosing spondylitis examined the use of sulfasalazine and methotrexate as second-line agents.6,7 Eleven trials were included in the sulfasalazine analysis, with a total of 895 patients. Sulfasalazine demonstrated some benefit in reducing erythrocyte sedimentation rates (ESRs) and morning stiffness, but there was no evidence that the drug reduced pain or improved physical function, spinal mobility, or rate of enthesitis. Sulfasalazine was well tolerated and may be useful in early mild disease for patients with peripheral arthritis and high ESRs. On the other hand, evidence was insufficient to determine whether methotrexate benefited patients with ankylosing spondylitis.
In other trials, infliximab and etanercept showed good potential for benefit in treating ankylosing spondylitis.
One study of infliximab vs placebo showed 61.2% vs 19.2% patients with good clinical benefit at 24 weeks and only mild or moderate adverse events (P<.001; NNT=2.38).8
Similarly, a smaller study (84 patients) showed that 60% of patients on etanercept vs 20% on placebo had good clinical benefit at only 12 weeks (P<.001, NNT=2.5).9
For other rheumatic diseases, studies are mixed
Due to cyclosporine’s toxicity, less toxic DMARDs are being evaluated to replace it for treatment of other rheumatic diseases. A recent randomized controlled trial of 100 patients with antineutrophil cytoplasmic antibody–associated systemic vasculitis showed methotrexate may be able to replace cyclosporine for both induction of remission (methotrexate=89.8% vs cyclosporine=93.5%; P=.041) and maintenance of remission (69.5% vs 46.5% at 18 months; P=.023).10
Initial trials on other rheumatic diseases have been small and have had varied results. There are mixed studies on the effectiveness of adding methotrexate to corticosteroids for giant cell arteritis.11,12
There has been no evidence of efficacy for the new TNF antagonists in either a small study on Sjögren’s syndrome (n=14)13 or a larger study on Wegener’s granulomatosis (n=180).14
The studies for use of DMARDs in lupus or scleroderma are of limited quality.
Recommendations from others
The Italian Society for Rheumatology consensus guidelines recommends TNF antagonists be considered in active psoriatic arthritis resistant to (a) NSAIDs, (b) at least 2 local steroid injections, and (c) at least 2 conventional DMARDs for patients with peripheral arthritis or enthesitis. They also recommend TNF antagonists be considered for psoriatic spondylitis resistant to NSAIDs.15
The Assessment in Ankylosing Spondylitis (ASAS) International Working Group and the European League Against Rheumatism (EULAR) recommendations for the treatment of ankylosing spondylitis, based on a systematic review of the literature and expert opinion, indicate that:
- There is good evidence for using NSAIDs and COX-2 inhibitors for symptomatic treatment.
- Conventional DMARDs are not well supported.
- TNF antagonists show a large benefit in both pain and function.
The ASAS/EULAR recommendation indicate that there is no evidence that any of these treatments actually modify the disease progression.16
Acknowledgments
The opinions and assertions contained herein are the private views of the authors and not to be construed as official, or as reflecting the views of the US Air Force medical service or the US Air Force at large.
It’s unclear whether disease-modifying antirheumatic agents (DMARDs) as first-line therapy in nonrheumatoid rheumatologic diseases are effective because the question has not been studied. As second-line therapy, the use of some DmArDs appears to be beneficial for patients with psoriatic arthritis (strength of recommendation [SOR]: A, based on systematic reviews of good-quality randomized controlled trials) and ankylosing spondylitis (SOR: B, based on systematic reviews of moderate quality trials). Data on the safety and efficacy of DMARDs as second-line therapy for other arthritic conditions is limited (SOR: C, based on small prospective cohort trials).
There are many options, but remember the risks
Richard Hoffman, MD
Chesterfield Family Medicine Residency, Richmond, Va
Traditionally, nonsteroidal anti-inflammatory agents (NSAIDs) have been the mainstay of treatment for rheumatologic disorders other than rheumatoid arthritis. methotrexate has been used in psoriatic arthritis because it also controls the skin disorder; sulfasalazine has been used in arthritis associated with inflammatory bowel disease, as it helps the bowel disorder itself. However, little evidence shows a definitive benefit for the arthritis.
The advent of tumor necrosis factor (TNF) blockers has changed the direction of research in this area; these agents are being used more and more in inflammatory arthritides. While staying up to date on the TNF antagonists, it’s important to remember the complications associated with them—particularly the increased risk of infections and increased propensity for neoplastic disorders. Consider those on TNF blockers as relatively immunosuppressed (number needed to harm [NNH]=59 for infection and 154 for malignancy).1
Psoriatic arthritis affecting the joints and nails
Evidence summary
The use of DMARDs has become standard of care for rheumatoid arthritis, for both therapy and prevention of progression of this debilitating disease. However, the use of DMARDs in nonrheumatoid rheumatologic disease is still under investigation, and at this point, the use of DMARDs as first-line therapy is not recommended; however, second-line therapy with DMARDs is common.
For psoriatic arthritis, DMARDs are beneficial as a second-line therapy
A Cochrane systematic review identified 13 randomized controlled trials enrolling a combined 1022 patients with psoriatic arthritis randomly assigned to receive a DMARD—methotrexate, sulfasalazine (Azulfidine), azathioprine (Imuran/ Azasan), or etretinate (Tegison; no longer available in the US)—compared with placebo.2 All agents were better than placebo; however, only 2 agents (parenteral high-dose methotrexate and sulfasalazine) had clinically important benefits for more than half the patients. The studies were too small to establish toxicity or to evaluate the other agents.
NSAIDs are still the preferred first-line therapy, concluded a recent publication on the treatment of psoriatic arthritis, which looked at 54 different studies; however, second-line therapy could include methotrexate, sulfasalazine, etanercept (Enbrel), infliximab (Remicade), cyclosporine, or combination therapy.3 Sulfasalazine appeared to be clinically beneficial for peripheral psoriatic arthritis.
Etanercept vs placebo. An initial study (60 patients) of etanercept vs placebo among patients who were permitted to stay on methotrexate or prednisone showed a response rate of 87% vs 23% (P<.0001; number needed to treat [NNT]=1.56).4
Infliximab vs placebo. A study of infliximab vs placebo involving 104 patients had similar results, with good response in 65% vs 10% (NNT=1.81) at 16 weeks; infliximab also inhibited radiographic progression by 22%.5
Cyclosporine. Although it is effective, reserve cyclosporine for patients who do not improve on other regimens, because of its nephrotoxicity.3
DMARDs show some benefit in treating ankylosing spondylitis
Two recent Cochrane systematic reviews on ankylosing spondylitis examined the use of sulfasalazine and methotrexate as second-line agents.6,7 Eleven trials were included in the sulfasalazine analysis, with a total of 895 patients. Sulfasalazine demonstrated some benefit in reducing erythrocyte sedimentation rates (ESRs) and morning stiffness, but there was no evidence that the drug reduced pain or improved physical function, spinal mobility, or rate of enthesitis. Sulfasalazine was well tolerated and may be useful in early mild disease for patients with peripheral arthritis and high ESRs. On the other hand, evidence was insufficient to determine whether methotrexate benefited patients with ankylosing spondylitis.
In other trials, infliximab and etanercept showed good potential for benefit in treating ankylosing spondylitis.
One study of infliximab vs placebo showed 61.2% vs 19.2% patients with good clinical benefit at 24 weeks and only mild or moderate adverse events (P<.001; NNT=2.38).8
Similarly, a smaller study (84 patients) showed that 60% of patients on etanercept vs 20% on placebo had good clinical benefit at only 12 weeks (P<.001, NNT=2.5).9
For other rheumatic diseases, studies are mixed
Due to cyclosporine’s toxicity, less toxic DMARDs are being evaluated to replace it for treatment of other rheumatic diseases. A recent randomized controlled trial of 100 patients with antineutrophil cytoplasmic antibody–associated systemic vasculitis showed methotrexate may be able to replace cyclosporine for both induction of remission (methotrexate=89.8% vs cyclosporine=93.5%; P=.041) and maintenance of remission (69.5% vs 46.5% at 18 months; P=.023).10
Initial trials on other rheumatic diseases have been small and have had varied results. There are mixed studies on the effectiveness of adding methotrexate to corticosteroids for giant cell arteritis.11,12
There has been no evidence of efficacy for the new TNF antagonists in either a small study on Sjögren’s syndrome (n=14)13 or a larger study on Wegener’s granulomatosis (n=180).14
The studies for use of DMARDs in lupus or scleroderma are of limited quality.
Recommendations from others
The Italian Society for Rheumatology consensus guidelines recommends TNF antagonists be considered in active psoriatic arthritis resistant to (a) NSAIDs, (b) at least 2 local steroid injections, and (c) at least 2 conventional DMARDs for patients with peripheral arthritis or enthesitis. They also recommend TNF antagonists be considered for psoriatic spondylitis resistant to NSAIDs.15
The Assessment in Ankylosing Spondylitis (ASAS) International Working Group and the European League Against Rheumatism (EULAR) recommendations for the treatment of ankylosing spondylitis, based on a systematic review of the literature and expert opinion, indicate that:
- There is good evidence for using NSAIDs and COX-2 inhibitors for symptomatic treatment.
- Conventional DMARDs are not well supported.
- TNF antagonists show a large benefit in both pain and function.
The ASAS/EULAR recommendation indicate that there is no evidence that any of these treatments actually modify the disease progression.16
Acknowledgments
The opinions and assertions contained herein are the private views of the authors and not to be construed as official, or as reflecting the views of the US Air Force medical service or the US Air Force at large.
1. Bongartz T, sutton AJ, Sweeting MJ, et al. Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. JAMA 2006;295:2275-2285.
2. Jones G, Crotty M, Brooks P. Interventions for treating psoriatic arthritis. Cochrane Database Syst Rev 2000 (3):CD000212.
3. Manadan Am, Sequeira W, Block JA. The treatment of psoriatic arthritis. Am J Ther 2006;13:72-79.
4. Mease PJ, Goffe BS, Metz J, et al. etanercept in the treatment of psoriatic arthritis and psoriasis: a randomized trial. Lancet 2000;356:385-390.
5. Kavanaugh A, Antoni CE, Gladman D, et al. The Infliximab multinational Psoriatic Arthritis Controlled Trial (ImPACT): result of radiographic analyses after 1 year. Ann Rheum Dis 2006;65:1038-1043.
6. Chen J, Liu C. Sulfasalazine for ankylosing spondylitis. Cochrane Database Syst Rev 2005;(2):CD004800.-
7. Chen J, Liu C, Lin J. Methotrexate for ankylosing spondylitis. Cochrane Database Syst Rev 2006;(4):CD004524.-
8. Heijde D, Dijkmans B, Geusens P, et al. efficacy and safety of infliximab in patients with ankylosing spondylitis. Arthritis Rheum 2005;52:582-591.
9. Calin A, Dijkmans BA, Emery P, et al. Outcomes of a multicentre randomized clinical trial of etanercept to treat ankylosing spondylitis. Ann Rheum Dis 2004;63:1594-1600.
10. Grout K, Rasmussen N, Bacon P, et al. randomized trial of cyclophosphamide versus methotrexate for induction of remission in early systemic antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 2005;52:2461-2469.
11. Jover JA, Hernandez-Garcia C, Morado IC, et al. Combined treatment of giant-cell arteritis with methotrexate and prednisone. a randomized, double blinded, placebo-controlled trial. Ann Intern Med 2001;134:106-114.
12. Hoffman GS, Cid MC, Hellmann DB, et al. A multicenter, randomized, double-blind, placebo-controlled trial of adjuvant methotrexate treatment for giant cell arteritis. Arthritis Rheum 2002;46:1309-1318.
13. Sankar V, Brennan MT, Kok MR, et al. etanercept in sjögren’s syndrome: a twelve-week randomized, double-blind, placebo-controlled pilot clinical trial. Arthritis Rheum 2004;50:2240-2245.
14. Wegener’s Granulomatosis etanercept Trial (WGeT) research Group. etanercept plus standard therapy for Wegener’s granulomatosis. N Engl J Med 2005;352:351-361.
15. Salvarani C, Olivieri I, Pipitone N, et al. recommendations of the Italian society for rheumatology for the use of biologic (TNF-alpha blocking) agents in the treatment of psoriatic arthritis. Clin Exp Rheumatol 2006;24:70-78.
16. Zochling J, van der Heijde D, Dougados, et al. Current evidence for the management of ankylosing spondylitis: a systematic literature review for the AsAs/eulAr management recommendations in ankylosing spondylitis. Ann Rheum Dis 2006;65:442-452.
1. Bongartz T, sutton AJ, Sweeting MJ, et al. Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. JAMA 2006;295:2275-2285.
2. Jones G, Crotty M, Brooks P. Interventions for treating psoriatic arthritis. Cochrane Database Syst Rev 2000 (3):CD000212.
3. Manadan Am, Sequeira W, Block JA. The treatment of psoriatic arthritis. Am J Ther 2006;13:72-79.
4. Mease PJ, Goffe BS, Metz J, et al. etanercept in the treatment of psoriatic arthritis and psoriasis: a randomized trial. Lancet 2000;356:385-390.
5. Kavanaugh A, Antoni CE, Gladman D, et al. The Infliximab multinational Psoriatic Arthritis Controlled Trial (ImPACT): result of radiographic analyses after 1 year. Ann Rheum Dis 2006;65:1038-1043.
6. Chen J, Liu C. Sulfasalazine for ankylosing spondylitis. Cochrane Database Syst Rev 2005;(2):CD004800.-
7. Chen J, Liu C, Lin J. Methotrexate for ankylosing spondylitis. Cochrane Database Syst Rev 2006;(4):CD004524.-
8. Heijde D, Dijkmans B, Geusens P, et al. efficacy and safety of infliximab in patients with ankylosing spondylitis. Arthritis Rheum 2005;52:582-591.
9. Calin A, Dijkmans BA, Emery P, et al. Outcomes of a multicentre randomized clinical trial of etanercept to treat ankylosing spondylitis. Ann Rheum Dis 2004;63:1594-1600.
10. Grout K, Rasmussen N, Bacon P, et al. randomized trial of cyclophosphamide versus methotrexate for induction of remission in early systemic antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum 2005;52:2461-2469.
11. Jover JA, Hernandez-Garcia C, Morado IC, et al. Combined treatment of giant-cell arteritis with methotrexate and prednisone. a randomized, double blinded, placebo-controlled trial. Ann Intern Med 2001;134:106-114.
12. Hoffman GS, Cid MC, Hellmann DB, et al. A multicenter, randomized, double-blind, placebo-controlled trial of adjuvant methotrexate treatment for giant cell arteritis. Arthritis Rheum 2002;46:1309-1318.
13. Sankar V, Brennan MT, Kok MR, et al. etanercept in sjögren’s syndrome: a twelve-week randomized, double-blind, placebo-controlled pilot clinical trial. Arthritis Rheum 2004;50:2240-2245.
14. Wegener’s Granulomatosis etanercept Trial (WGeT) research Group. etanercept plus standard therapy for Wegener’s granulomatosis. N Engl J Med 2005;352:351-361.
15. Salvarani C, Olivieri I, Pipitone N, et al. recommendations of the Italian society for rheumatology for the use of biologic (TNF-alpha blocking) agents in the treatment of psoriatic arthritis. Clin Exp Rheumatol 2006;24:70-78.
16. Zochling J, van der Heijde D, Dougados, et al. Current evidence for the management of ankylosing spondylitis: a systematic literature review for the AsAs/eulAr management recommendations in ankylosing spondylitis. Ann Rheum Dis 2006;65:442-452.
Evidence-based answers from the Family Physicians Inquiries Network