User login
What is the best way to manage phantom limb pain?
No single best therapy for phantom limb pain (PLP) exists. Treatment requires a coordinated application of conservative, pharmacologic, and adjuvant therapies.
Evaluative management (including prosthesis adjustment, treatment of referred pain, and residual limb care) should be tried initially (strength of recommendation [SOR]: C, expert opinion). Other first-line treatments such as transcutaneous electrical nerve stimulation (TENS) (SOR: A, multiple high-quality randomized, control trials [RCTs]), and biofeedback (SOR: B, numerous case studies) can reduce PLP. Pharmacotherapy, including opioids, anticonvulsants (gabapentin), and nonsteroidal anti-inflammatory drugs (NSAIDs), can also relieve pain (SOR: B, initial RCTs and inconsistent findings).
Adjuvant therapies (mirror box therapy, acupuncture, calcitonin, and N-methyl d-aspartate receptor antagonists) haven’t been rigorously investigated for alleviating PLP, but can be considered for patients who have failed other treatments.
Evidence summary
An estimated 1.7 million people in the United States are living with limb loss. The number is expected to increase because of ongoing military conflicts.1 The incidence of PLP is 60% to 80% among amputees.1
A multidisciplinary approach
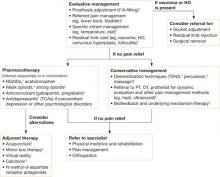
A lack of comparative clinical trials of therapies for PLP has led health-care providers to adopt a multidisciplinary approach that combines evaluative management, desensitization, psychotherapy, and pharmacotherapy (FIGURE).
Evaluative management, based largely on expert opinion, includes assessing the fit of the prosthesis, treating referred pain, and assessing aggravating factors. Because residual limb pain can exacerbate PLP, adjusting a poorly fitting prosthesis or providing the patient with NSAIDs when there is evidence of stump inflammation may adequately control pain.2,3 Anatomically distant pain syndromes, such as hip or lower back pain, can also aggravate PLP and should be managed to provide optimal pain relief.2
Desensitization, using TENS, has reduced PLP in multiple placebo-controlled trials and epidemiologic surveys.2-5 TENS is an easy-to-use, low-cost, noninvasive, first-line therapy.5 Its long-term effectiveness in alleviating PLP remains unknown.2 Some experts suggest that pain reductions after 1 year of treatment are comparable to placebo.2 Other forms of desensitization (percussion and massage) are supported only by anecdotal reports.
Psychotherapy, including biofeedback, has been found in several case studies to effectively treat chronic PLP.2,5 Psychotherapy can reportedly reveal the underlying mechanisms (muscle spasm, vascular insufficiency) and therefore direct therapeutic interventions by biofeedback or other focus techniques.2
FIGURE Management of phantom limb pain1-10
*Expert opinion.
†Case studies.
‡Randomized controlled trials or cohort studies.
Pharmacotherapy is best used as an adjunct to other treatments.2 Although PLP is typically treated as neuropathic pain, only a few medications have been critically evaluated for treating it.6 Morphine (number needed to treat [NNT]=2.5; 95% confidence interval [CI], 1.9-3.4) and other opioids, including tramadol (NNT=3.9; 95% CI, 2.7-6.7 in neuropathic pain) help some patients.6,7 Despite the proven benefit of tricyclic antidepressants (TCAs) in other neuropathic pain conditions, a recent RCT demonstrated no benefit of TCAs over placebo in PLP.8 Anticonvulsants, including gabapentin, have documented benefit in neuropathic pain modalities and are often used for PLP.6 However, their value in reducing PLP is still under investigation.6 One 2002 RCT showed benefit regarding an improvement of the visual analog scale by an average of 3 points (on a 10-point scale) after 6 weeks of gabapentin therapy.9 A similarly designed 2006 RCT of gabapentin, however did not identify significant pain reductions.10
Promising adjuvant therapies use mirroring techniques
Of the adjuvant treatments mentioned previously, only mirror box therapy has shown promise. This technique allows the amputee to perceive the missing limb by focusing on the reflection of the remaining limb during specific movements and activities. Theoretically, this perception allows reconfiguration of the amputee’s sensory cortex.
Virtual reality therapy employs similar techniques based on the idea that the brain can be deceived. Initial case studies are promising and have prompted further research.11
Recommendations
The US Department of Veterans Affairs and Department of Defense recently issued clinical guidelines for rehabilitating lower-limb amputees that include a segment on pain management.12 The guidelines stress the importance of an interdisciplinary team approach that addresses each pathology plaguing the amputee.
They recommend narcotics during the immediate postoperative period, followed by transition to a non-narcotic medical regimen during the rehabilitation process. The guidelines don’t support a single, specific pain control method over others; they recommend the following approaches to PLP:
- pharmacologic treatment, which may include antiseizure medications, tricyclic antidepressants, selective serotonin reuptake inhibitors, NSAIDs, dextromethorathane, or long-acting narcotics
- epidural analgesia, patient-controlled analgesia, or regional analgesia
- nonpharmacologic therapies, including TENS, desensitization, scar mobilization, relaxation, and biofeedback.
Acknowledgements
The opinions and assertions contained herein are the private views of the authors and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
1. Ziegler-Graham K, MacKenzie EI, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422-429.
2. Sherman RA. Postamputation pain. In: Jensen TS, Wilson PR, Rice AS, eds. Clinical Pain Management: Chronic Pain. London: Hodder Arnold Publishing; 2002;32:427-436.
3. Wartan SW, Hamann W, Wedley JR, et al. Phantom pain and sensation among British veteran amputees. Br J Anaesth. 1997;78:652-659.
4. Halbert J, Crotty M, Cameron ID. Evidence for the optimal management of acute and chronic phantom pain: a systematic review. Clin J Pain. 2002;18:84-92.
5. Baron R, Wasner G, Lindner V. Optimal treatment of phantom limb pain in the elderly. Drugs Aging. 1998;12:361-376.
6. Finnerup NB, Otto M, McQuay HJ, et al. Algorithm for neuropathic pain treatment: an evidence-based proposal. Pain. 2005;118:289-305.
7. Huse E, Larbig W, Flor H, et al. The effect of opioids on phantom limb pain and cortical reorganization. Pain. 2001;90:47-55.
8. Robinson LR, Czerniecki JM, Ehde DM, et al. Trial of amitriptyline for relief of pain in amputees: results of a randomized controlled study. Arch Phys Med Rehabil. 2004;85:1-6.
9. Bone M, Critchley P, Buggy DJ. Gabapentin in postamputation phantom limb pain: a randomized, double-blind, placebo-controlled, cross-over study. Reg Anesth Pain Med. 2002;27:481-486.
10. Nikolajsen L, Finnerup NB, Kramp S, et al. A randomized study of the effects of gabapentin on post-amputation pain. Anesthesiology. 2006;105:1008-1015.
11. Chan BL, Witt R, Charrow AP, et al. Mirror therapy for phantom limb pain. N Engl J Med. 2007;357:2206-2207.
12. Department of Veterans Affairs/Department of Defense. VA/DoD clinical practice guideline for rehabilitation of lower amputation. Washington, DC: Department of Veterans Affairs, Department of Defense; 2007:1-55. Available at: www.guideline.gov/summary/summary.aspx?doc_id=11758&nbr=006060&string=amputation. Accessed December 13, 2008.
No single best therapy for phantom limb pain (PLP) exists. Treatment requires a coordinated application of conservative, pharmacologic, and adjuvant therapies.
Evaluative management (including prosthesis adjustment, treatment of referred pain, and residual limb care) should be tried initially (strength of recommendation [SOR]: C, expert opinion). Other first-line treatments such as transcutaneous electrical nerve stimulation (TENS) (SOR: A, multiple high-quality randomized, control trials [RCTs]), and biofeedback (SOR: B, numerous case studies) can reduce PLP. Pharmacotherapy, including opioids, anticonvulsants (gabapentin), and nonsteroidal anti-inflammatory drugs (NSAIDs), can also relieve pain (SOR: B, initial RCTs and inconsistent findings).
Adjuvant therapies (mirror box therapy, acupuncture, calcitonin, and N-methyl d-aspartate receptor antagonists) haven’t been rigorously investigated for alleviating PLP, but can be considered for patients who have failed other treatments.
Evidence summary
An estimated 1.7 million people in the United States are living with limb loss. The number is expected to increase because of ongoing military conflicts.1 The incidence of PLP is 60% to 80% among amputees.1
A multidisciplinary approach
A lack of comparative clinical trials of therapies for PLP has led health-care providers to adopt a multidisciplinary approach that combines evaluative management, desensitization, psychotherapy, and pharmacotherapy (FIGURE).
Evaluative management, based largely on expert opinion, includes assessing the fit of the prosthesis, treating referred pain, and assessing aggravating factors. Because residual limb pain can exacerbate PLP, adjusting a poorly fitting prosthesis or providing the patient with NSAIDs when there is evidence of stump inflammation may adequately control pain.2,3 Anatomically distant pain syndromes, such as hip or lower back pain, can also aggravate PLP and should be managed to provide optimal pain relief.2
Desensitization, using TENS, has reduced PLP in multiple placebo-controlled trials and epidemiologic surveys.2-5 TENS is an easy-to-use, low-cost, noninvasive, first-line therapy.5 Its long-term effectiveness in alleviating PLP remains unknown.2 Some experts suggest that pain reductions after 1 year of treatment are comparable to placebo.2 Other forms of desensitization (percussion and massage) are supported only by anecdotal reports.
Psychotherapy, including biofeedback, has been found in several case studies to effectively treat chronic PLP.2,5 Psychotherapy can reportedly reveal the underlying mechanisms (muscle spasm, vascular insufficiency) and therefore direct therapeutic interventions by biofeedback or other focus techniques.2
FIGURE Management of phantom limb pain1-10
*Expert opinion.
†Case studies.
‡Randomized controlled trials or cohort studies.
Pharmacotherapy is best used as an adjunct to other treatments.2 Although PLP is typically treated as neuropathic pain, only a few medications have been critically evaluated for treating it.6 Morphine (number needed to treat [NNT]=2.5; 95% confidence interval [CI], 1.9-3.4) and other opioids, including tramadol (NNT=3.9; 95% CI, 2.7-6.7 in neuropathic pain) help some patients.6,7 Despite the proven benefit of tricyclic antidepressants (TCAs) in other neuropathic pain conditions, a recent RCT demonstrated no benefit of TCAs over placebo in PLP.8 Anticonvulsants, including gabapentin, have documented benefit in neuropathic pain modalities and are often used for PLP.6 However, their value in reducing PLP is still under investigation.6 One 2002 RCT showed benefit regarding an improvement of the visual analog scale by an average of 3 points (on a 10-point scale) after 6 weeks of gabapentin therapy.9 A similarly designed 2006 RCT of gabapentin, however did not identify significant pain reductions.10
Promising adjuvant therapies use mirroring techniques
Of the adjuvant treatments mentioned previously, only mirror box therapy has shown promise. This technique allows the amputee to perceive the missing limb by focusing on the reflection of the remaining limb during specific movements and activities. Theoretically, this perception allows reconfiguration of the amputee’s sensory cortex.
Virtual reality therapy employs similar techniques based on the idea that the brain can be deceived. Initial case studies are promising and have prompted further research.11
Recommendations
The US Department of Veterans Affairs and Department of Defense recently issued clinical guidelines for rehabilitating lower-limb amputees that include a segment on pain management.12 The guidelines stress the importance of an interdisciplinary team approach that addresses each pathology plaguing the amputee.
They recommend narcotics during the immediate postoperative period, followed by transition to a non-narcotic medical regimen during the rehabilitation process. The guidelines don’t support a single, specific pain control method over others; they recommend the following approaches to PLP:
- pharmacologic treatment, which may include antiseizure medications, tricyclic antidepressants, selective serotonin reuptake inhibitors, NSAIDs, dextromethorathane, or long-acting narcotics
- epidural analgesia, patient-controlled analgesia, or regional analgesia
- nonpharmacologic therapies, including TENS, desensitization, scar mobilization, relaxation, and biofeedback.
Acknowledgements
The opinions and assertions contained herein are the private views of the authors and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
No single best therapy for phantom limb pain (PLP) exists. Treatment requires a coordinated application of conservative, pharmacologic, and adjuvant therapies.
Evaluative management (including prosthesis adjustment, treatment of referred pain, and residual limb care) should be tried initially (strength of recommendation [SOR]: C, expert opinion). Other first-line treatments such as transcutaneous electrical nerve stimulation (TENS) (SOR: A, multiple high-quality randomized, control trials [RCTs]), and biofeedback (SOR: B, numerous case studies) can reduce PLP. Pharmacotherapy, including opioids, anticonvulsants (gabapentin), and nonsteroidal anti-inflammatory drugs (NSAIDs), can also relieve pain (SOR: B, initial RCTs and inconsistent findings).
Adjuvant therapies (mirror box therapy, acupuncture, calcitonin, and N-methyl d-aspartate receptor antagonists) haven’t been rigorously investigated for alleviating PLP, but can be considered for patients who have failed other treatments.
Evidence summary
An estimated 1.7 million people in the United States are living with limb loss. The number is expected to increase because of ongoing military conflicts.1 The incidence of PLP is 60% to 80% among amputees.1
A multidisciplinary approach
A lack of comparative clinical trials of therapies for PLP has led health-care providers to adopt a multidisciplinary approach that combines evaluative management, desensitization, psychotherapy, and pharmacotherapy (FIGURE).
Evaluative management, based largely on expert opinion, includes assessing the fit of the prosthesis, treating referred pain, and assessing aggravating factors. Because residual limb pain can exacerbate PLP, adjusting a poorly fitting prosthesis or providing the patient with NSAIDs when there is evidence of stump inflammation may adequately control pain.2,3 Anatomically distant pain syndromes, such as hip or lower back pain, can also aggravate PLP and should be managed to provide optimal pain relief.2
Desensitization, using TENS, has reduced PLP in multiple placebo-controlled trials and epidemiologic surveys.2-5 TENS is an easy-to-use, low-cost, noninvasive, first-line therapy.5 Its long-term effectiveness in alleviating PLP remains unknown.2 Some experts suggest that pain reductions after 1 year of treatment are comparable to placebo.2 Other forms of desensitization (percussion and massage) are supported only by anecdotal reports.
Psychotherapy, including biofeedback, has been found in several case studies to effectively treat chronic PLP.2,5 Psychotherapy can reportedly reveal the underlying mechanisms (muscle spasm, vascular insufficiency) and therefore direct therapeutic interventions by biofeedback or other focus techniques.2
FIGURE Management of phantom limb pain1-10
*Expert opinion.
†Case studies.
‡Randomized controlled trials or cohort studies.
Pharmacotherapy is best used as an adjunct to other treatments.2 Although PLP is typically treated as neuropathic pain, only a few medications have been critically evaluated for treating it.6 Morphine (number needed to treat [NNT]=2.5; 95% confidence interval [CI], 1.9-3.4) and other opioids, including tramadol (NNT=3.9; 95% CI, 2.7-6.7 in neuropathic pain) help some patients.6,7 Despite the proven benefit of tricyclic antidepressants (TCAs) in other neuropathic pain conditions, a recent RCT demonstrated no benefit of TCAs over placebo in PLP.8 Anticonvulsants, including gabapentin, have documented benefit in neuropathic pain modalities and are often used for PLP.6 However, their value in reducing PLP is still under investigation.6 One 2002 RCT showed benefit regarding an improvement of the visual analog scale by an average of 3 points (on a 10-point scale) after 6 weeks of gabapentin therapy.9 A similarly designed 2006 RCT of gabapentin, however did not identify significant pain reductions.10
Promising adjuvant therapies use mirroring techniques
Of the adjuvant treatments mentioned previously, only mirror box therapy has shown promise. This technique allows the amputee to perceive the missing limb by focusing on the reflection of the remaining limb during specific movements and activities. Theoretically, this perception allows reconfiguration of the amputee’s sensory cortex.
Virtual reality therapy employs similar techniques based on the idea that the brain can be deceived. Initial case studies are promising and have prompted further research.11
Recommendations
The US Department of Veterans Affairs and Department of Defense recently issued clinical guidelines for rehabilitating lower-limb amputees that include a segment on pain management.12 The guidelines stress the importance of an interdisciplinary team approach that addresses each pathology plaguing the amputee.
They recommend narcotics during the immediate postoperative period, followed by transition to a non-narcotic medical regimen during the rehabilitation process. The guidelines don’t support a single, specific pain control method over others; they recommend the following approaches to PLP:
- pharmacologic treatment, which may include antiseizure medications, tricyclic antidepressants, selective serotonin reuptake inhibitors, NSAIDs, dextromethorathane, or long-acting narcotics
- epidural analgesia, patient-controlled analgesia, or regional analgesia
- nonpharmacologic therapies, including TENS, desensitization, scar mobilization, relaxation, and biofeedback.
Acknowledgements
The opinions and assertions contained herein are the private views of the authors and not to be construed as official, or as reflecting the views of the US Air Force Medical Service or the US Air Force at large.
1. Ziegler-Graham K, MacKenzie EI, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422-429.
2. Sherman RA. Postamputation pain. In: Jensen TS, Wilson PR, Rice AS, eds. Clinical Pain Management: Chronic Pain. London: Hodder Arnold Publishing; 2002;32:427-436.
3. Wartan SW, Hamann W, Wedley JR, et al. Phantom pain and sensation among British veteran amputees. Br J Anaesth. 1997;78:652-659.
4. Halbert J, Crotty M, Cameron ID. Evidence for the optimal management of acute and chronic phantom pain: a systematic review. Clin J Pain. 2002;18:84-92.
5. Baron R, Wasner G, Lindner V. Optimal treatment of phantom limb pain in the elderly. Drugs Aging. 1998;12:361-376.
6. Finnerup NB, Otto M, McQuay HJ, et al. Algorithm for neuropathic pain treatment: an evidence-based proposal. Pain. 2005;118:289-305.
7. Huse E, Larbig W, Flor H, et al. The effect of opioids on phantom limb pain and cortical reorganization. Pain. 2001;90:47-55.
8. Robinson LR, Czerniecki JM, Ehde DM, et al. Trial of amitriptyline for relief of pain in amputees: results of a randomized controlled study. Arch Phys Med Rehabil. 2004;85:1-6.
9. Bone M, Critchley P, Buggy DJ. Gabapentin in postamputation phantom limb pain: a randomized, double-blind, placebo-controlled, cross-over study. Reg Anesth Pain Med. 2002;27:481-486.
10. Nikolajsen L, Finnerup NB, Kramp S, et al. A randomized study of the effects of gabapentin on post-amputation pain. Anesthesiology. 2006;105:1008-1015.
11. Chan BL, Witt R, Charrow AP, et al. Mirror therapy for phantom limb pain. N Engl J Med. 2007;357:2206-2207.
12. Department of Veterans Affairs/Department of Defense. VA/DoD clinical practice guideline for rehabilitation of lower amputation. Washington, DC: Department of Veterans Affairs, Department of Defense; 2007:1-55. Available at: www.guideline.gov/summary/summary.aspx?doc_id=11758&nbr=006060&string=amputation. Accessed December 13, 2008.
1. Ziegler-Graham K, MacKenzie EI, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89:422-429.
2. Sherman RA. Postamputation pain. In: Jensen TS, Wilson PR, Rice AS, eds. Clinical Pain Management: Chronic Pain. London: Hodder Arnold Publishing; 2002;32:427-436.
3. Wartan SW, Hamann W, Wedley JR, et al. Phantom pain and sensation among British veteran amputees. Br J Anaesth. 1997;78:652-659.
4. Halbert J, Crotty M, Cameron ID. Evidence for the optimal management of acute and chronic phantom pain: a systematic review. Clin J Pain. 2002;18:84-92.
5. Baron R, Wasner G, Lindner V. Optimal treatment of phantom limb pain in the elderly. Drugs Aging. 1998;12:361-376.
6. Finnerup NB, Otto M, McQuay HJ, et al. Algorithm for neuropathic pain treatment: an evidence-based proposal. Pain. 2005;118:289-305.
7. Huse E, Larbig W, Flor H, et al. The effect of opioids on phantom limb pain and cortical reorganization. Pain. 2001;90:47-55.
8. Robinson LR, Czerniecki JM, Ehde DM, et al. Trial of amitriptyline for relief of pain in amputees: results of a randomized controlled study. Arch Phys Med Rehabil. 2004;85:1-6.
9. Bone M, Critchley P, Buggy DJ. Gabapentin in postamputation phantom limb pain: a randomized, double-blind, placebo-controlled, cross-over study. Reg Anesth Pain Med. 2002;27:481-486.
10. Nikolajsen L, Finnerup NB, Kramp S, et al. A randomized study of the effects of gabapentin on post-amputation pain. Anesthesiology. 2006;105:1008-1015.
11. Chan BL, Witt R, Charrow AP, et al. Mirror therapy for phantom limb pain. N Engl J Med. 2007;357:2206-2207.
12. Department of Veterans Affairs/Department of Defense. VA/DoD clinical practice guideline for rehabilitation of lower amputation. Washington, DC: Department of Veterans Affairs, Department of Defense; 2007:1-55. Available at: www.guideline.gov/summary/summary.aspx?doc_id=11758&nbr=006060&string=amputation. Accessed December 13, 2008.
Evidence-based answers from the Family Physicians Inquiries Network