User login
Antihypertensive Therapy and BP Control
Current recommendations for blood pressure (BP) control focus on chronic management of ambulatory patients; however, treatment guidelines for hospitalized patients who have acute increases in BP or simply uncontrolled BP lack clarity regarding appropriate therapeutic options and short‐term treatment goals.[1, 2] For patients with a history of hypertension, management in the hospital setting typically involves continuation of home therapies. In the inpatient setting, uncontrolled hypertension can be categorized as hypertensive emergency, hypertensive urgency, or asymptomatic poor BP control.[3] Asymptomatic BP elevations occur when the BP is not at goal (but not inordinately high) and the patient has no signs of new or worsening end‐organ damage.[4, 5, 6]
Published data have not demonstrated that aggressive treatment of asymptomatic hypertension in the inpatient setting improves short‐ or long‐term outcomes; however, such aggressive treatment may be associated with iatrogenic adverse effects.[5, 7, 8] Despite the lack of evidence of patient benefit, there is a tendency to treat hospitalized patients with asymptomatic BP elevations aggressively by prescribing IV antihypertensive agents on an as‐needed basis.[9] Intravenous hydralazine and labetalol are frequently used, although these agents are not recommended as initial therapy in consensus recommendations for asymptomatic uncontrolled hypertension in either the inpatient or outpatient setting.[10]
We therefore undertook the present study to determine the type and frequency of ordered and administered episodic intravenous (IV) antihypertensive drug therapy, the BP thresholds triggering such administration, and subsequent in‐hospital clinical outcomes after administration of IV antihypertensive drugs. Accordingly, we evaluated a series of hospitalized patients, in noncritical care settings with no evidence of new or worsening target‐organ injury, who were treated with episodic (either as needed or 1 time only) IV antihypertensive therapy.
METHODS
This study is a retrospective review. Between November 1, 2010 and January 31, 2011 we reviewed the charts of all patients who had at least 1 dose of IV hydralazine, enalaprilat, labetalol, or metoprolol ordered, regardless of previous oral antihypertensive treatment or hypertension diagnosis. Other IV antihypertensive agents were not evaluated in this study, as they are only available in critical care units at our institution. This study took place at an 806‐bed urban hospital that utilizes 100% computer prescriber order entry and bar code technology to document medication administration. The institutional review boards of the Detroit Medical Center and Wayne State University, Detroit, Michigan approved this study.
Patient Identification
Patients were identified through a list of all 1‐time‐only and as‐needed orders for IV hydralazine, enalaprilat, labetolol, or metoprolol. The list was generated daily through the hospital electronic medical record system (Cerner Powerchart, North Kansas City, MO). Patients were excluded if they were younger than 18 or older than 89 years of age, admitted to the intensive care or coronary care unit, were receiving nothing by mouth, pregnant, received a renal transplant in the past 3 months, or if there was any clinical manifestation of new or worsening target‐organ injury consistent with the diagnosis of hypertensive emergency.
Data Collection
The following data were collected for all patients: basic demographic information including factors that have been specifically associated with differences in hypertension risk (ie, age, sex, race, weight, and renal function), antihypertensive regimen (if any) prior to admission, changes to oral antihypertensive therapy during admission, order for sodium‐restricted diet, baseline and discharge laboratory values and vital signs. In addition, the details of their antihypertensive therapy order and administration were collected, including prescriber type (attending, resident, or physician extender), service of prescriber, criteria for use, and date and time of drug administration categorized by shift (morning shift, 7 am to 3 pm; afternoon shift, 3 pm to 11 pm; and night shift, 11 pm to 7 am). To analyze the outcomes of administering episodic IV antihypertensive therapy, the following data were collected: changes in average BP within 30 minutes to 6 hours after drug administration and occurrence of antihypertensive therapy‐related adverse events, including any interventions required after administration and adjustments to oral antihypertensive therapy during admission or upon discharge. In cases where BP data were not available (either just prior to or within 6 hours following administration of an IV antihypertensive), the data were not included in the analysis. To determine whether an antihypertensive drug regimen had been intensified, a therapeutic intensity score (TIS) was calculated for the oral antihypertensive regimen on admission and again at discharge. The antihypertensive TIS was calculated by dividing the total daily dose of each antihypertensive medication by the maximum US Food and Drug Administrationapproved daily dose.[11]
Adverse Outcomes Definition
We defined an adverse outcome as a 25% decrease in systolic or diastolic BP within 6 hours and/or intervention to treat symptoms of hypotension. This definition is consistent with Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) recommendations to assure safety when lowering BP in the setting of hypertensive emergency.[6] Although the patients in this study were not experiencing hypertensive emergency, this definition is supported by reports of negative sequelae from overzealous lowering of BP,[12, 13, 14] and it reflects criteria used in other trials.[10] Hypotension was deemed to have occurred if any of the following were documented: as IV fluid administration; scheduled BP medication held (at either the nurses discretion or per physician order); change in level of care; change in mental status; or transient ischemic attack, stroke, or chest pain within 30 minutes to 6 hours after administration. Heart rate changes were also considered to be adverse outcomes, including tachycardia (heart rate >100 beats per minute [bpm] or increase 20 bpm from baseline) or bradycardia (heart rate <50 bpm).
Analysis
Descriptive statistics were performed for all variables. Continuous data were summarized using means and standard deviations. Categorical variables were summarized as counts and percentages. Paired t tests were used to contrast changes from baseline for continuous variables pre‐ and post‐BP, and heart rate changes were evaluated only for the first episode of IV antihypertensive drug administration in patients receiving multiple doses of antihypertensive medication to avoid the bias created by repeated or clustered measures in a given patient. 2 tests were used to test differences in categorical variables. All statistical testing was considered significant when 2‐tailed P values were <0.05. Analyses were generated using SAS software version 9.4 (SAS Institute Inc., Cary, NC).
RESULTS
Patients
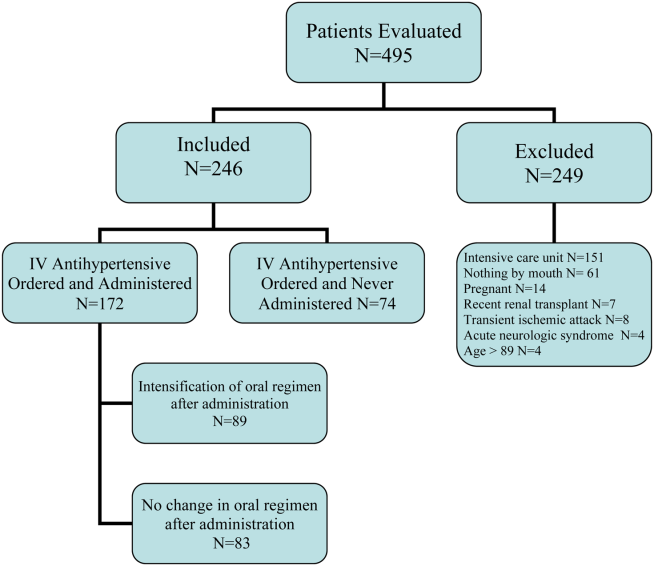
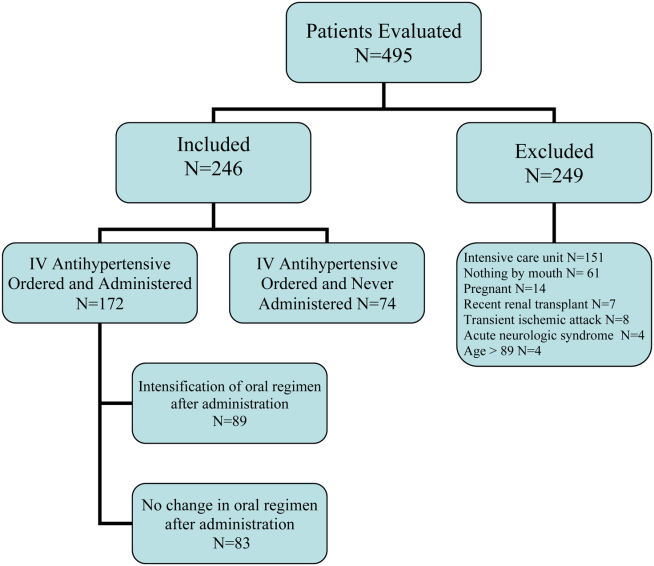
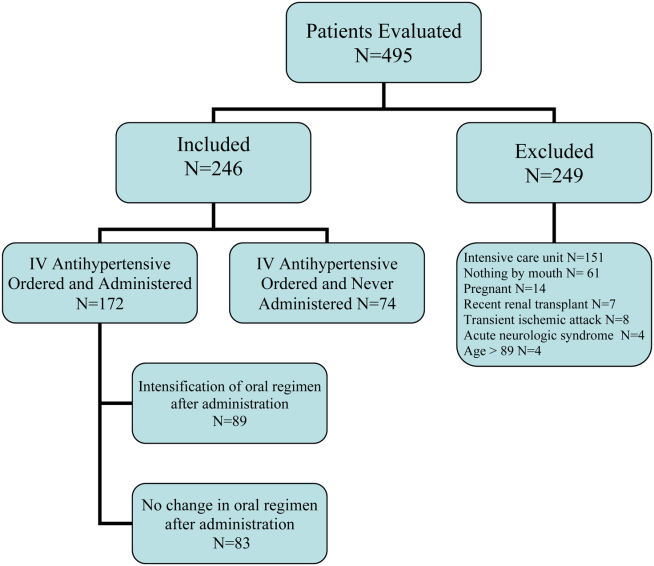
During the study period, there were 6133 inpatient adult admissions. Of 495 patients who had at least 1 order for IV hydralazine, enalaprilat, labetolol, or metoprolol, 246 were included in the analysis after applying the exclusion criteria (Figure 1). Patients were divided into 2 groups. One group had an order for an IV antihypertensive that was not administered (n = 74), and the other had an order for an IV antihypertensive and received at least 1 dose (n = 172). The demographic characteristics of the 2 groups are compared in Table 1. Patients who had their chronic oral antihypertensive regimens intensified after receiving IV antihypertensive medications were more often African American, leaner, more intensively treated, and had higher baseline BP.
| Did Not Receive IV Antihypertensive (n = 74) | Did Receive IV Antihypertensive (n = 172) | P | |
|---|---|---|---|
| |||
| Age, y | 61.6 13.9 | 60.6 13.7 | |
| Male sex | 51% | 47% | |
| African American | 74% | 87% | 0.008 |
| Weight, kg | 94.6 33.2 | 88.5 27.7 | |
| Admit systolic BP | 148 23 | 163 32 | <0.0001 |
| Admit diastolic BP | 82 13 | 87 18 | 0.009 |
| Admit heart rate | 87 18 | 82 20 | 0.069 |
| Admit TIS | 0.84 0.72 | 1.08 0.88 | 0.026 |
| Baseline SCr | 1.78 2.00 | 2.74 3.30 | 0.006 |
| Baseline AST | 26.5 12.5 | 65 126.2 | 0.046 |
| Low‐sodium diet order | 65% | 83% | 0.002 |
| Ordering service | |||
| Cardiology | 14% | 19% | |
| Internal medicine | 49% | 47% | |
| Nephrology | 0% | 6% | |
| Other services | 37% | 28% | |
| Prescriber type | |||
| Resident | 30% | 49% | |
| Physician extender | 53% | 35% | |
| Attending | 17% | 16% | |
| 1‐time‐only order | 5% | 19% | |
| As‐needed order | 95% | 81% | |
Prescribing Patterns
Medical residents prescribed nearly half (49%) of the orders for episodic IV antihypertensives. Attending physicians were responsible for 16% of episodic antihypertensive orders and physician extenders (physician's assistants and nurse practitioners) for 35%. A total of 321 orders were prescribed for the 246 patients in the study. Hydralazine was the preferred antihypertensive agent (80.1%), with IV ‐blockers prescribed less frequently (labetalol 15.6% and metoprolol 4.4%). There were no orders for IV enalaprilat. BP parameters were included in 181 (56%) of the episodic IV antihypertensive orders. Of the IV antihypertensive orders containing criteria, 153 (84.5%) had systolic BP threshold for administration <180 mm Hg (Table 2).
| BP Criteria for Administration of IV Antihypertensive Contained in Order, mm Hg | Did Not Receive IV Antihypertensive, n (%), n = 71* | Did Receive IV Antihypertensive, n (%), n = 133* |
|---|---|---|
| ||
| SBP >120 | 2 (2.8) | 1 (0.7) |
| SBP >130 | 2 (2.8) | 9 (6.8) |
| SBP >140 | 2 (2.8) | 5 (3.8) |
| SBP >150 | 4 (5.6) | 8 (6) |
| SBP >160 | 27 (38) | 58 (43.7) |
| SBP >170 | 26 (36.6) | 29 (21.8) |
| SBP >180 | 8 (11.4) | 18 (13.5) |
| SBP >200 | 4 (3) | |
| DBP >100 | 1 (0.7) | |
Drug Administration and Short‐term Data
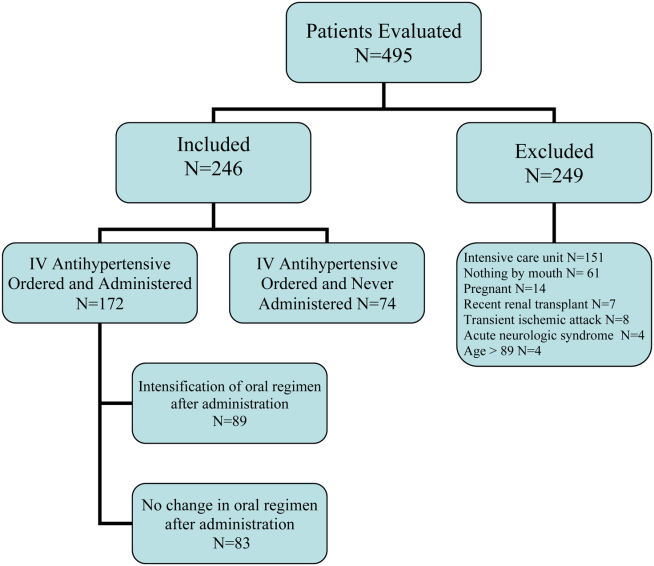
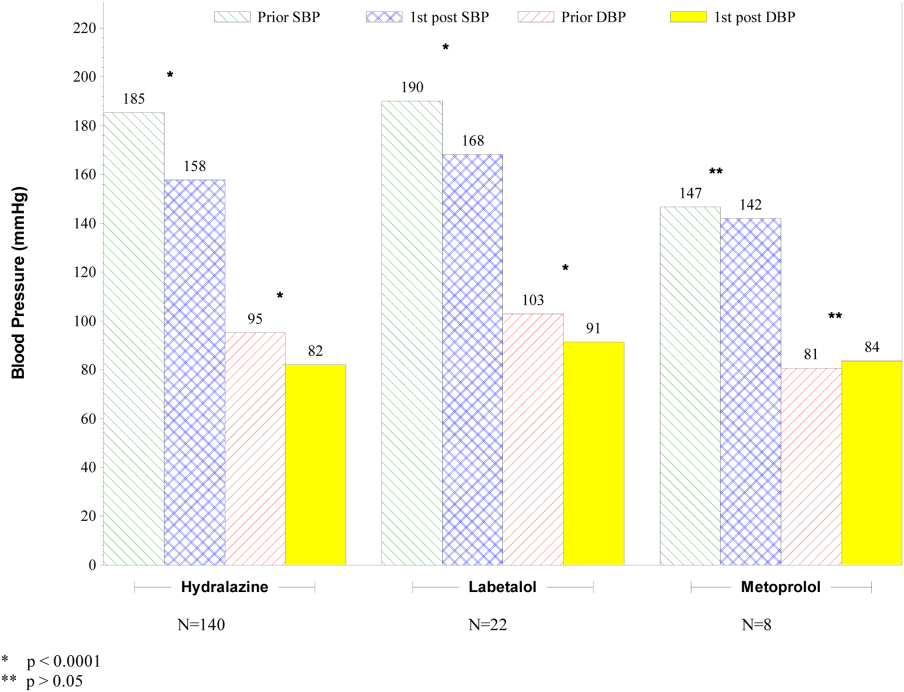
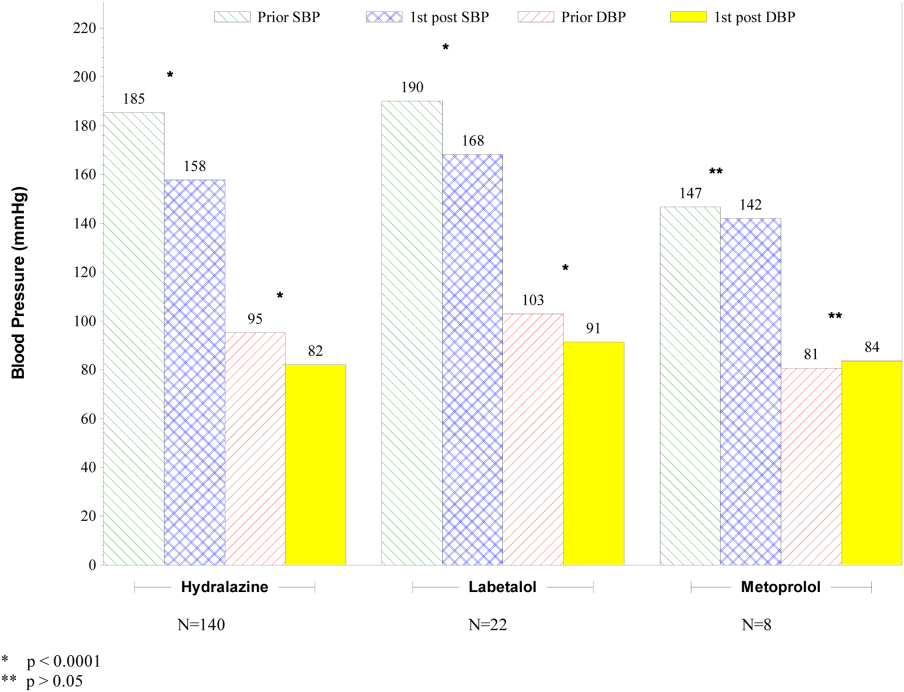
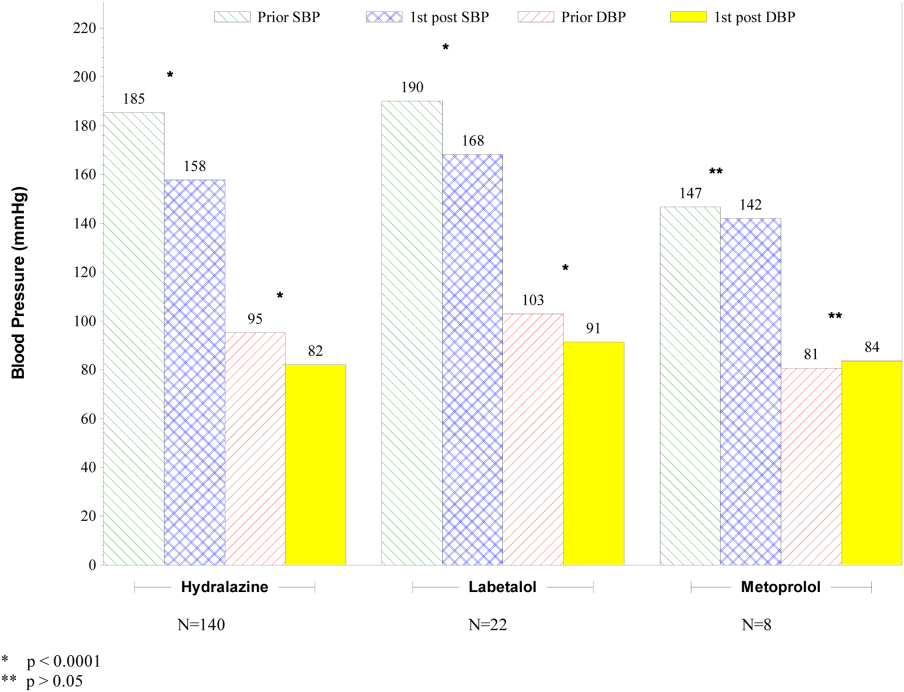
Table 2 indicates the BP criteria specified in the episodic IV antihypertensive orders. For the 74 patients who did not receive an episodic IV antihypertensive agent, despite having an order, the nurses caring for the patients determined that their BPs never met the criteria for administration of the IV antihypertensive agent. The remainder of the results apply only to the 172 patients who actually received episodic IV antihypertensive therapy. Two of these patients did not have BP data available and were not included in the short‐term BP analysis. Almost half (48%) of the patients received 1 dose of episodic IV antihypertensive, 26% received 2 doses, and 11% received 3 doses. One patient received 10 doses. Hydralazine significantly lowered BP, whereas metoprolol did not (Figure 2).
The number of IV antihypertensive doses (for which BP data are available) administered during the night shift (n = 75) was numerically higher than the morning (n = 54) and the afternoon (n = 41) shifts. The mean BPs that triggered administration of IV antihypertensives did not differ among shifts (night shift 183/93, morning shift 184/99, afternoon shift 182/97).
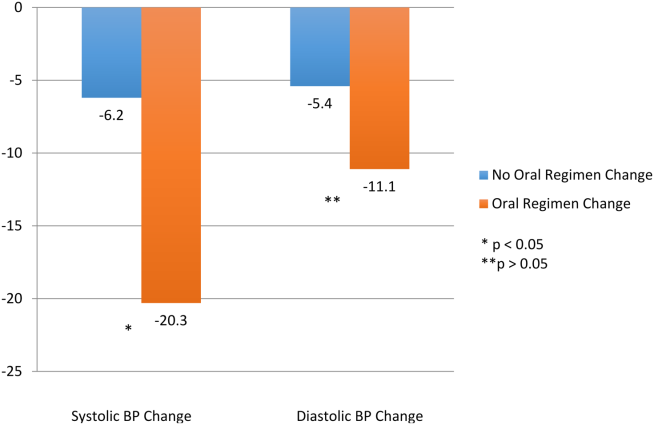
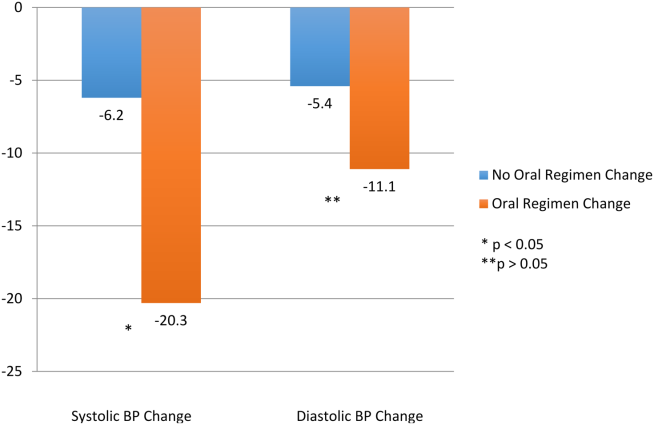
Changes to Oral Antihypertensive Regimen After Administration of IV Antihypertensive Drugs
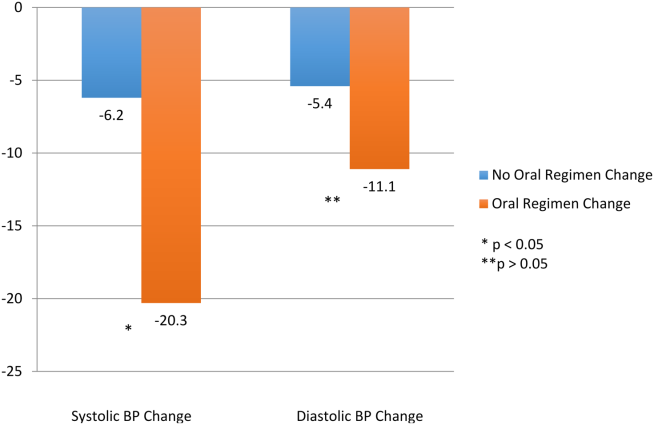
After administration of an episodic IV antihypertensive, the inpatient oral medication regimen was intensified in only 89 patients (52%). The BP reduction from admission to discharge in patients who had their inpatient oral medication regimen adjusted versus those who did not have an inpatient oral regimen adjustment after receiving IV antihypertensive medication is shown in Figure 3. Patients with intensification of their oral medications had a greater reduction in systolic BP from admission to discharge, compared to patients who received episodic IV antihypertensives but had no subsequent change to their inpatient oral antihypertensive regimen (Figure 3).
Adverse Events
Fifty‐six patients (32.6%) demonstrated BP reductions of more than 25% within 6 hours of antihypertensive administration. Of these patients, 2 received IV fluids, and 6 (3.5%) had a scheduled oral BP medication held. Of the patients who received IV hydralazine, 13 (4.4%) had an increase in heart rate >20 bpm, with 7 having a heart rate >100 bpm. One patient who received labetolol experienced bradycardia. No patient required a higher level of care (transfer to an intensive care unit) because of hemodynamic instability. In addition, no patient experienced a change in mental status, transient ischemic attack, stroke, or chest pain within 30 minutes to 6 hours after administration.
DISCUSSION
The overwhelming majority of administrations of costly episodic IV antihypertensive drugs among this low‐risk population were in patients with modest BP elevations who may have merited no more, at most, than intensification of their oral antihypertensive drug regimen or observation. Such administration was infrequently followed by intensification of the oral antihypertensive drug regimen, and a significant number of patients experienced a potentially adverse clinical event. Excessive reduction of BP resulting in withholding of oral agents or administering IV fluids (as seen in 8 patients) is clinically relevant, especially in a setting where rapid lowering of BP with IV antihypertensives have no proven clinical benefit. There were differences between patients who did and did not received IV antihypertensive drug therapy, as those receiving therapy were higher‐risk patients. Of the patients initially evaluated for inclusion in this analysis, approximately half had a clear indication for IV antihypertensive therapy and were not included in this analysis. It should also be noted that one‐third of the patients included in the study did not subsequently receive an IV antihypertensive agent.
Recently updated hypertensive guidelines do not address the treatment of hypertensive urgency and emergency, whereas the JNC 7 addressed hypertensive urgency but did not provide a specific BP definition or goals because of concerns about overly aggressive management of severe asymptomatic hypertension.[2, 6] For patients with chronically elevated BP, its rapid reduction, even to levels that remain in the frankly hypertensive range, can be associated with negative clinical sequelae, attributable to decreased target organ perfusion causing clinically manifest ischemia.[3] Accordingly, there have been reports of ischemic events related to unwarranted and overzealous BP lowering.[12, 13, 14] In such patients, resistance vessel remodeling causes a rightward shift of the entire pressure/flow auto regulatory curve in critical arterial beds (eg, cerebral, coronary, and renal). Higher systemic pressure is necessary to maintain adequate perfusion in the target organ, at least over the short‐term. Thus, rapid, aggressive BP reduction can result in the aforementioned negative sequelae because remodeled resistance arterioles are not capable of vasodilating enough to ensure adequate blood flow when systemic pressure falls precipitously.
The patients in this study had no evidence of new or worsening pressure‐related end‐organ damage; therefore, there appeared to be no medical justification for emergent BP lowering via the IV route (a very small minority may have had BP high enough to have justified being diagnosed with hypertensive urgency in which fast‐acting oral therapy would be used). Despite the paucity of data to support this practice, it does, however, appear to be relatively common.[9] The high prevalence of IV hydralazine use in this inpatient study is consistent with the retrospective study reported by Weder and Erickson at the University of Michigan.[9]
Even among those with hypertensive urgencies, oral medication is the preferred route (assuming the patient can eat and swallow without difficulty and does not manifest an altered sensorium). Furthermore, the risks associated with overzealous BP lowering can be devastating. The likelihood of target‐organ ischemia (eg, angina pectoris, myocardial infarction, azotemia, stroke, transient ischemic attack) is most strongly correlated to the rapidity of the BP reduction, even to levels within the hypertensive range, in patients with persistent poor BP control.[4, 15, 16] Thus, the justification for considering a >25% drop in systolic BP within 6 hours of the administration of the IV antihypertensive agent as a potential adverse event, especially because there was only a very small immediate risk for adverse cardiovascular sequelae at the BP levels triggering administration of IV antihypertensive drug therapy.
Although we found that residents and physician assistants prescribed most IV antihypertensives, the practice of prescribing IV antihypertensive therapy appears to be common among all prescriber types. A recent survey assessing the attitudes and practices of resident physicians regarding hypertension in the inpatient setting found that 44% of respondents would treat acute asymptomatic, moderately elevated BP (182/100 mm Hg) with either an oral or intravenous agent.[17]
In addition to there being no proven clinical benefit in this setting, the use of unnecessary IV antihypertensives is associated with unnecessary risks and excess cost. Another report of IV hydralazine in asymptomatic patients found that 17 of 94 patients experienced an adverse effect after administration.[18] Not only is the drug acquisition cost for IV antihypertensives greater than their oral counterparts, often by a factor of 10 to 100, the intravenous route requires additional care to monitor their effects, adding to the human resource expense. Finally, the onset of action of intravenous agents is generally more rapid, which increases the risk of inducing hypotension and therefore target‐organ ischemia.
This study does, however, have limitations. This is a single‐center study, so the findings may not be generalizable to different hospital settings. The findings of this study depend on the accuracy and completeness of the medical record as recorded during routine clinical care; therefore, errors and omissions of data input and documentation may affect the quality of the data. Omissions and errors in the medication history can affect inpatient management as well as appropriateness of discharge medications. BP values before and after administration of an IV antihypertensive were not always available, limiting some of the short‐term outcomes data that were available. The impact of acuity of illness and concomitant disease states of patients were not assessed, which could also affect outcomes. The outcomes measured in this investigation were all short‐term outcomes and did not include important clinical outcomes (long‐term BP control, rehospitalization rates, or patient morbidity or mortality).
We speculate that the practice of episodic IV antihypertensive therapy has developed out of convenience for the practitioner and is likely commonplace across the country.[17] Healthcare systems should examine practices locally and address them as appropriate. To assist in promoting evidence‐based practice that is safe, prudent, and clinically appropriate, we propose that national BP organizations and consensus development groups consider placing priority on developing recommendations for inpatient hypertension treatment algorithms beyond those for hypertensive emergencies. In many cases, adjustments to a patient's oral regimen or observation of the patient are the only interventions that are needed. In addition, appropriate coordination of ambulatory follow‐up care upon discharge is prudent. Finally, individual healthcare systems might need to identify formal programs to modify institutional behavior of both medical and nursing staff to eliminate or limit this practice that is not supported by clinical evidence and potentially places the patient at risk.
CONCLUSIONS
Our study found that the practice of prescribing episodic IV antihypertensive agents at our institution occurred across all prescriber types. Hydralazine was the most frequently ordered agent. The majority of orders containing systolic BP criteria for administration of an episodic IV antihypertensive agent were well below the BP level associated with immediate or near‐immediate cardiovascular risk. Administration of episodic IV antihypertensive agents, without subsequent intensification of the patient's chronic oral antihypertensive regimen was nearly as likely to occur as subsequent intensification of the oral regimen in our study. The absence of evidence‐based guidelines, combined with the results of this evaluation, provide a rationale for implementing hospital‐ and health systembased policies limiting the use of episodic IV antihypertensive agents in asymptomatic patients with uncontrolled BP in noncritical care settings in the absence of new or worsening target‐organ injury.
Disclosure: Nothing to report.
- , , , et al. Treatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation. 2007;115(21):2761–2788.
- , , , et al. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520.
- , . Hypertensive crises: challenges and management. Chest. 2007;131(6):1949–1962.
- , . Severely increased blood pressure in the emergency department. Ann Emerg Med. 2003;41(4):513–529.
- , , , , ; American College of Emergency Physicians Clinical Policies Subcommittee on Asymptomatic Hypertension in the ED. Clinical policy: critical issues in the evaluation and management of adult patients with asymptomatic hypertension in the emergency department. Ann Emerg Med.2006;47(3):237–249.
- , , , et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572.
- , . Best Evidence on management of asymptomatic hypertension in ED patients. J Emerg Nurs. 2011;37(2):174–178.
- , , , et al. A novel pathway for the management of hypertension for hospitalized patients. Crit Pathw Cardiol. 2007;6(4):150–160.
- , . Treatment of hypertension in the inpatient setting: use of intravenous labetalol and hydralazine. J Clin Hypertens (Greenwich). 2010;12(1):29–33.
- , , , et al. Patterns of antihypertensive treatment in patients with acute severe hypertension from a nonneurologic cause: Studying the Treatment of Acute Hypertension (STAT) registry. Pharmacotherapy. 2010;30(11):1087–1096.
- , , , , . Does earlier attainment of blood pressure goal translate into fewer cardiovascular events? Curr Hypertens Rep. 2008;10(5):398–404.
- . Symptomatic hypotension induced by nifedipine in the acute treatment of severe hypertension. Arch Intern Med. 1987;147(3):556–558.
- , , . Rapid reduction of severe asymptomatic hypertension. A prospective, controlled trial. Arch Intern Med. 1989;149(10):2186–2189.
- , , . Nifedipine‐associated myocardial ischemia or infarction in the treatment of hypertensive urgencies. Ann Intern Med. 1987;107(2):185–186.
- , , , , . Stroke precipitated by moderate blood pressure reduction. J Emerg Med. 2000;9(4):339–346.
- , , , . Adverse events associated with aggressive treatment of increased blood pressure. Int J Clin Prac. 2004;58(5):517–519.
- , , , et al. Attitudes and practices of resident physicians regarding hypertension in the inpatient setting. J Clin Hypertens. 2010;12(9):698–705.
- , , , . Intravenous hydralazine for blood pressure management in the hospitalized patient: its use is often unjustified. J Am Soc Hypertens. 2011;5(6):473–477.
Current recommendations for blood pressure (BP) control focus on chronic management of ambulatory patients; however, treatment guidelines for hospitalized patients who have acute increases in BP or simply uncontrolled BP lack clarity regarding appropriate therapeutic options and short‐term treatment goals.[1, 2] For patients with a history of hypertension, management in the hospital setting typically involves continuation of home therapies. In the inpatient setting, uncontrolled hypertension can be categorized as hypertensive emergency, hypertensive urgency, or asymptomatic poor BP control.[3] Asymptomatic BP elevations occur when the BP is not at goal (but not inordinately high) and the patient has no signs of new or worsening end‐organ damage.[4, 5, 6]
Published data have not demonstrated that aggressive treatment of asymptomatic hypertension in the inpatient setting improves short‐ or long‐term outcomes; however, such aggressive treatment may be associated with iatrogenic adverse effects.[5, 7, 8] Despite the lack of evidence of patient benefit, there is a tendency to treat hospitalized patients with asymptomatic BP elevations aggressively by prescribing IV antihypertensive agents on an as‐needed basis.[9] Intravenous hydralazine and labetalol are frequently used, although these agents are not recommended as initial therapy in consensus recommendations for asymptomatic uncontrolled hypertension in either the inpatient or outpatient setting.[10]
We therefore undertook the present study to determine the type and frequency of ordered and administered episodic intravenous (IV) antihypertensive drug therapy, the BP thresholds triggering such administration, and subsequent in‐hospital clinical outcomes after administration of IV antihypertensive drugs. Accordingly, we evaluated a series of hospitalized patients, in noncritical care settings with no evidence of new or worsening target‐organ injury, who were treated with episodic (either as needed or 1 time only) IV antihypertensive therapy.
METHODS
This study is a retrospective review. Between November 1, 2010 and January 31, 2011 we reviewed the charts of all patients who had at least 1 dose of IV hydralazine, enalaprilat, labetalol, or metoprolol ordered, regardless of previous oral antihypertensive treatment or hypertension diagnosis. Other IV antihypertensive agents were not evaluated in this study, as they are only available in critical care units at our institution. This study took place at an 806‐bed urban hospital that utilizes 100% computer prescriber order entry and bar code technology to document medication administration. The institutional review boards of the Detroit Medical Center and Wayne State University, Detroit, Michigan approved this study.
Patient Identification
Patients were identified through a list of all 1‐time‐only and as‐needed orders for IV hydralazine, enalaprilat, labetolol, or metoprolol. The list was generated daily through the hospital electronic medical record system (Cerner Powerchart, North Kansas City, MO). Patients were excluded if they were younger than 18 or older than 89 years of age, admitted to the intensive care or coronary care unit, were receiving nothing by mouth, pregnant, received a renal transplant in the past 3 months, or if there was any clinical manifestation of new or worsening target‐organ injury consistent with the diagnosis of hypertensive emergency.
Data Collection
The following data were collected for all patients: basic demographic information including factors that have been specifically associated with differences in hypertension risk (ie, age, sex, race, weight, and renal function), antihypertensive regimen (if any) prior to admission, changes to oral antihypertensive therapy during admission, order for sodium‐restricted diet, baseline and discharge laboratory values and vital signs. In addition, the details of their antihypertensive therapy order and administration were collected, including prescriber type (attending, resident, or physician extender), service of prescriber, criteria for use, and date and time of drug administration categorized by shift (morning shift, 7 am to 3 pm; afternoon shift, 3 pm to 11 pm; and night shift, 11 pm to 7 am). To analyze the outcomes of administering episodic IV antihypertensive therapy, the following data were collected: changes in average BP within 30 minutes to 6 hours after drug administration and occurrence of antihypertensive therapy‐related adverse events, including any interventions required after administration and adjustments to oral antihypertensive therapy during admission or upon discharge. In cases where BP data were not available (either just prior to or within 6 hours following administration of an IV antihypertensive), the data were not included in the analysis. To determine whether an antihypertensive drug regimen had been intensified, a therapeutic intensity score (TIS) was calculated for the oral antihypertensive regimen on admission and again at discharge. The antihypertensive TIS was calculated by dividing the total daily dose of each antihypertensive medication by the maximum US Food and Drug Administrationapproved daily dose.[11]
Adverse Outcomes Definition
We defined an adverse outcome as a 25% decrease in systolic or diastolic BP within 6 hours and/or intervention to treat symptoms of hypotension. This definition is consistent with Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) recommendations to assure safety when lowering BP in the setting of hypertensive emergency.[6] Although the patients in this study were not experiencing hypertensive emergency, this definition is supported by reports of negative sequelae from overzealous lowering of BP,[12, 13, 14] and it reflects criteria used in other trials.[10] Hypotension was deemed to have occurred if any of the following were documented: as IV fluid administration; scheduled BP medication held (at either the nurses discretion or per physician order); change in level of care; change in mental status; or transient ischemic attack, stroke, or chest pain within 30 minutes to 6 hours after administration. Heart rate changes were also considered to be adverse outcomes, including tachycardia (heart rate >100 beats per minute [bpm] or increase 20 bpm from baseline) or bradycardia (heart rate <50 bpm).
Analysis
Descriptive statistics were performed for all variables. Continuous data were summarized using means and standard deviations. Categorical variables were summarized as counts and percentages. Paired t tests were used to contrast changes from baseline for continuous variables pre‐ and post‐BP, and heart rate changes were evaluated only for the first episode of IV antihypertensive drug administration in patients receiving multiple doses of antihypertensive medication to avoid the bias created by repeated or clustered measures in a given patient. 2 tests were used to test differences in categorical variables. All statistical testing was considered significant when 2‐tailed P values were <0.05. Analyses were generated using SAS software version 9.4 (SAS Institute Inc., Cary, NC).
RESULTS
Patients
During the study period, there were 6133 inpatient adult admissions. Of 495 patients who had at least 1 order for IV hydralazine, enalaprilat, labetolol, or metoprolol, 246 were included in the analysis after applying the exclusion criteria (Figure 1). Patients were divided into 2 groups. One group had an order for an IV antihypertensive that was not administered (n = 74), and the other had an order for an IV antihypertensive and received at least 1 dose (n = 172). The demographic characteristics of the 2 groups are compared in Table 1. Patients who had their chronic oral antihypertensive regimens intensified after receiving IV antihypertensive medications were more often African American, leaner, more intensively treated, and had higher baseline BP.
| Did Not Receive IV Antihypertensive (n = 74) | Did Receive IV Antihypertensive (n = 172) | P | |
|---|---|---|---|
| |||
| Age, y | 61.6 13.9 | 60.6 13.7 | |
| Male sex | 51% | 47% | |
| African American | 74% | 87% | 0.008 |
| Weight, kg | 94.6 33.2 | 88.5 27.7 | |
| Admit systolic BP | 148 23 | 163 32 | <0.0001 |
| Admit diastolic BP | 82 13 | 87 18 | 0.009 |
| Admit heart rate | 87 18 | 82 20 | 0.069 |
| Admit TIS | 0.84 0.72 | 1.08 0.88 | 0.026 |
| Baseline SCr | 1.78 2.00 | 2.74 3.30 | 0.006 |
| Baseline AST | 26.5 12.5 | 65 126.2 | 0.046 |
| Low‐sodium diet order | 65% | 83% | 0.002 |
| Ordering service | |||
| Cardiology | 14% | 19% | |
| Internal medicine | 49% | 47% | |
| Nephrology | 0% | 6% | |
| Other services | 37% | 28% | |
| Prescriber type | |||
| Resident | 30% | 49% | |
| Physician extender | 53% | 35% | |
| Attending | 17% | 16% | |
| 1‐time‐only order | 5% | 19% | |
| As‐needed order | 95% | 81% | |
Prescribing Patterns
Medical residents prescribed nearly half (49%) of the orders for episodic IV antihypertensives. Attending physicians were responsible for 16% of episodic antihypertensive orders and physician extenders (physician's assistants and nurse practitioners) for 35%. A total of 321 orders were prescribed for the 246 patients in the study. Hydralazine was the preferred antihypertensive agent (80.1%), with IV ‐blockers prescribed less frequently (labetalol 15.6% and metoprolol 4.4%). There were no orders for IV enalaprilat. BP parameters were included in 181 (56%) of the episodic IV antihypertensive orders. Of the IV antihypertensive orders containing criteria, 153 (84.5%) had systolic BP threshold for administration <180 mm Hg (Table 2).
| BP Criteria for Administration of IV Antihypertensive Contained in Order, mm Hg | Did Not Receive IV Antihypertensive, n (%), n = 71* | Did Receive IV Antihypertensive, n (%), n = 133* |
|---|---|---|
| ||
| SBP >120 | 2 (2.8) | 1 (0.7) |
| SBP >130 | 2 (2.8) | 9 (6.8) |
| SBP >140 | 2 (2.8) | 5 (3.8) |
| SBP >150 | 4 (5.6) | 8 (6) |
| SBP >160 | 27 (38) | 58 (43.7) |
| SBP >170 | 26 (36.6) | 29 (21.8) |
| SBP >180 | 8 (11.4) | 18 (13.5) |
| SBP >200 | 4 (3) | |
| DBP >100 | 1 (0.7) | |
Drug Administration and Short‐term Data
Table 2 indicates the BP criteria specified in the episodic IV antihypertensive orders. For the 74 patients who did not receive an episodic IV antihypertensive agent, despite having an order, the nurses caring for the patients determined that their BPs never met the criteria for administration of the IV antihypertensive agent. The remainder of the results apply only to the 172 patients who actually received episodic IV antihypertensive therapy. Two of these patients did not have BP data available and were not included in the short‐term BP analysis. Almost half (48%) of the patients received 1 dose of episodic IV antihypertensive, 26% received 2 doses, and 11% received 3 doses. One patient received 10 doses. Hydralazine significantly lowered BP, whereas metoprolol did not (Figure 2).
The number of IV antihypertensive doses (for which BP data are available) administered during the night shift (n = 75) was numerically higher than the morning (n = 54) and the afternoon (n = 41) shifts. The mean BPs that triggered administration of IV antihypertensives did not differ among shifts (night shift 183/93, morning shift 184/99, afternoon shift 182/97).
Changes to Oral Antihypertensive Regimen After Administration of IV Antihypertensive Drugs
After administration of an episodic IV antihypertensive, the inpatient oral medication regimen was intensified in only 89 patients (52%). The BP reduction from admission to discharge in patients who had their inpatient oral medication regimen adjusted versus those who did not have an inpatient oral regimen adjustment after receiving IV antihypertensive medication is shown in Figure 3. Patients with intensification of their oral medications had a greater reduction in systolic BP from admission to discharge, compared to patients who received episodic IV antihypertensives but had no subsequent change to their inpatient oral antihypertensive regimen (Figure 3).
Adverse Events
Fifty‐six patients (32.6%) demonstrated BP reductions of more than 25% within 6 hours of antihypertensive administration. Of these patients, 2 received IV fluids, and 6 (3.5%) had a scheduled oral BP medication held. Of the patients who received IV hydralazine, 13 (4.4%) had an increase in heart rate >20 bpm, with 7 having a heart rate >100 bpm. One patient who received labetolol experienced bradycardia. No patient required a higher level of care (transfer to an intensive care unit) because of hemodynamic instability. In addition, no patient experienced a change in mental status, transient ischemic attack, stroke, or chest pain within 30 minutes to 6 hours after administration.
DISCUSSION
The overwhelming majority of administrations of costly episodic IV antihypertensive drugs among this low‐risk population were in patients with modest BP elevations who may have merited no more, at most, than intensification of their oral antihypertensive drug regimen or observation. Such administration was infrequently followed by intensification of the oral antihypertensive drug regimen, and a significant number of patients experienced a potentially adverse clinical event. Excessive reduction of BP resulting in withholding of oral agents or administering IV fluids (as seen in 8 patients) is clinically relevant, especially in a setting where rapid lowering of BP with IV antihypertensives have no proven clinical benefit. There were differences between patients who did and did not received IV antihypertensive drug therapy, as those receiving therapy were higher‐risk patients. Of the patients initially evaluated for inclusion in this analysis, approximately half had a clear indication for IV antihypertensive therapy and were not included in this analysis. It should also be noted that one‐third of the patients included in the study did not subsequently receive an IV antihypertensive agent.
Recently updated hypertensive guidelines do not address the treatment of hypertensive urgency and emergency, whereas the JNC 7 addressed hypertensive urgency but did not provide a specific BP definition or goals because of concerns about overly aggressive management of severe asymptomatic hypertension.[2, 6] For patients with chronically elevated BP, its rapid reduction, even to levels that remain in the frankly hypertensive range, can be associated with negative clinical sequelae, attributable to decreased target organ perfusion causing clinically manifest ischemia.[3] Accordingly, there have been reports of ischemic events related to unwarranted and overzealous BP lowering.[12, 13, 14] In such patients, resistance vessel remodeling causes a rightward shift of the entire pressure/flow auto regulatory curve in critical arterial beds (eg, cerebral, coronary, and renal). Higher systemic pressure is necessary to maintain adequate perfusion in the target organ, at least over the short‐term. Thus, rapid, aggressive BP reduction can result in the aforementioned negative sequelae because remodeled resistance arterioles are not capable of vasodilating enough to ensure adequate blood flow when systemic pressure falls precipitously.
The patients in this study had no evidence of new or worsening pressure‐related end‐organ damage; therefore, there appeared to be no medical justification for emergent BP lowering via the IV route (a very small minority may have had BP high enough to have justified being diagnosed with hypertensive urgency in which fast‐acting oral therapy would be used). Despite the paucity of data to support this practice, it does, however, appear to be relatively common.[9] The high prevalence of IV hydralazine use in this inpatient study is consistent with the retrospective study reported by Weder and Erickson at the University of Michigan.[9]
Even among those with hypertensive urgencies, oral medication is the preferred route (assuming the patient can eat and swallow without difficulty and does not manifest an altered sensorium). Furthermore, the risks associated with overzealous BP lowering can be devastating. The likelihood of target‐organ ischemia (eg, angina pectoris, myocardial infarction, azotemia, stroke, transient ischemic attack) is most strongly correlated to the rapidity of the BP reduction, even to levels within the hypertensive range, in patients with persistent poor BP control.[4, 15, 16] Thus, the justification for considering a >25% drop in systolic BP within 6 hours of the administration of the IV antihypertensive agent as a potential adverse event, especially because there was only a very small immediate risk for adverse cardiovascular sequelae at the BP levels triggering administration of IV antihypertensive drug therapy.
Although we found that residents and physician assistants prescribed most IV antihypertensives, the practice of prescribing IV antihypertensive therapy appears to be common among all prescriber types. A recent survey assessing the attitudes and practices of resident physicians regarding hypertension in the inpatient setting found that 44% of respondents would treat acute asymptomatic, moderately elevated BP (182/100 mm Hg) with either an oral or intravenous agent.[17]
In addition to there being no proven clinical benefit in this setting, the use of unnecessary IV antihypertensives is associated with unnecessary risks and excess cost. Another report of IV hydralazine in asymptomatic patients found that 17 of 94 patients experienced an adverse effect after administration.[18] Not only is the drug acquisition cost for IV antihypertensives greater than their oral counterparts, often by a factor of 10 to 100, the intravenous route requires additional care to monitor their effects, adding to the human resource expense. Finally, the onset of action of intravenous agents is generally more rapid, which increases the risk of inducing hypotension and therefore target‐organ ischemia.
This study does, however, have limitations. This is a single‐center study, so the findings may not be generalizable to different hospital settings. The findings of this study depend on the accuracy and completeness of the medical record as recorded during routine clinical care; therefore, errors and omissions of data input and documentation may affect the quality of the data. Omissions and errors in the medication history can affect inpatient management as well as appropriateness of discharge medications. BP values before and after administration of an IV antihypertensive were not always available, limiting some of the short‐term outcomes data that were available. The impact of acuity of illness and concomitant disease states of patients were not assessed, which could also affect outcomes. The outcomes measured in this investigation were all short‐term outcomes and did not include important clinical outcomes (long‐term BP control, rehospitalization rates, or patient morbidity or mortality).
We speculate that the practice of episodic IV antihypertensive therapy has developed out of convenience for the practitioner and is likely commonplace across the country.[17] Healthcare systems should examine practices locally and address them as appropriate. To assist in promoting evidence‐based practice that is safe, prudent, and clinically appropriate, we propose that national BP organizations and consensus development groups consider placing priority on developing recommendations for inpatient hypertension treatment algorithms beyond those for hypertensive emergencies. In many cases, adjustments to a patient's oral regimen or observation of the patient are the only interventions that are needed. In addition, appropriate coordination of ambulatory follow‐up care upon discharge is prudent. Finally, individual healthcare systems might need to identify formal programs to modify institutional behavior of both medical and nursing staff to eliminate or limit this practice that is not supported by clinical evidence and potentially places the patient at risk.
CONCLUSIONS
Our study found that the practice of prescribing episodic IV antihypertensive agents at our institution occurred across all prescriber types. Hydralazine was the most frequently ordered agent. The majority of orders containing systolic BP criteria for administration of an episodic IV antihypertensive agent were well below the BP level associated with immediate or near‐immediate cardiovascular risk. Administration of episodic IV antihypertensive agents, without subsequent intensification of the patient's chronic oral antihypertensive regimen was nearly as likely to occur as subsequent intensification of the oral regimen in our study. The absence of evidence‐based guidelines, combined with the results of this evaluation, provide a rationale for implementing hospital‐ and health systembased policies limiting the use of episodic IV antihypertensive agents in asymptomatic patients with uncontrolled BP in noncritical care settings in the absence of new or worsening target‐organ injury.
Disclosure: Nothing to report.
Current recommendations for blood pressure (BP) control focus on chronic management of ambulatory patients; however, treatment guidelines for hospitalized patients who have acute increases in BP or simply uncontrolled BP lack clarity regarding appropriate therapeutic options and short‐term treatment goals.[1, 2] For patients with a history of hypertension, management in the hospital setting typically involves continuation of home therapies. In the inpatient setting, uncontrolled hypertension can be categorized as hypertensive emergency, hypertensive urgency, or asymptomatic poor BP control.[3] Asymptomatic BP elevations occur when the BP is not at goal (but not inordinately high) and the patient has no signs of new or worsening end‐organ damage.[4, 5, 6]
Published data have not demonstrated that aggressive treatment of asymptomatic hypertension in the inpatient setting improves short‐ or long‐term outcomes; however, such aggressive treatment may be associated with iatrogenic adverse effects.[5, 7, 8] Despite the lack of evidence of patient benefit, there is a tendency to treat hospitalized patients with asymptomatic BP elevations aggressively by prescribing IV antihypertensive agents on an as‐needed basis.[9] Intravenous hydralazine and labetalol are frequently used, although these agents are not recommended as initial therapy in consensus recommendations for asymptomatic uncontrolled hypertension in either the inpatient or outpatient setting.[10]
We therefore undertook the present study to determine the type and frequency of ordered and administered episodic intravenous (IV) antihypertensive drug therapy, the BP thresholds triggering such administration, and subsequent in‐hospital clinical outcomes after administration of IV antihypertensive drugs. Accordingly, we evaluated a series of hospitalized patients, in noncritical care settings with no evidence of new or worsening target‐organ injury, who were treated with episodic (either as needed or 1 time only) IV antihypertensive therapy.
METHODS
This study is a retrospective review. Between November 1, 2010 and January 31, 2011 we reviewed the charts of all patients who had at least 1 dose of IV hydralazine, enalaprilat, labetalol, or metoprolol ordered, regardless of previous oral antihypertensive treatment or hypertension diagnosis. Other IV antihypertensive agents were not evaluated in this study, as they are only available in critical care units at our institution. This study took place at an 806‐bed urban hospital that utilizes 100% computer prescriber order entry and bar code technology to document medication administration. The institutional review boards of the Detroit Medical Center and Wayne State University, Detroit, Michigan approved this study.
Patient Identification
Patients were identified through a list of all 1‐time‐only and as‐needed orders for IV hydralazine, enalaprilat, labetolol, or metoprolol. The list was generated daily through the hospital electronic medical record system (Cerner Powerchart, North Kansas City, MO). Patients were excluded if they were younger than 18 or older than 89 years of age, admitted to the intensive care or coronary care unit, were receiving nothing by mouth, pregnant, received a renal transplant in the past 3 months, or if there was any clinical manifestation of new or worsening target‐organ injury consistent with the diagnosis of hypertensive emergency.
Data Collection
The following data were collected for all patients: basic demographic information including factors that have been specifically associated with differences in hypertension risk (ie, age, sex, race, weight, and renal function), antihypertensive regimen (if any) prior to admission, changes to oral antihypertensive therapy during admission, order for sodium‐restricted diet, baseline and discharge laboratory values and vital signs. In addition, the details of their antihypertensive therapy order and administration were collected, including prescriber type (attending, resident, or physician extender), service of prescriber, criteria for use, and date and time of drug administration categorized by shift (morning shift, 7 am to 3 pm; afternoon shift, 3 pm to 11 pm; and night shift, 11 pm to 7 am). To analyze the outcomes of administering episodic IV antihypertensive therapy, the following data were collected: changes in average BP within 30 minutes to 6 hours after drug administration and occurrence of antihypertensive therapy‐related adverse events, including any interventions required after administration and adjustments to oral antihypertensive therapy during admission or upon discharge. In cases where BP data were not available (either just prior to or within 6 hours following administration of an IV antihypertensive), the data were not included in the analysis. To determine whether an antihypertensive drug regimen had been intensified, a therapeutic intensity score (TIS) was calculated for the oral antihypertensive regimen on admission and again at discharge. The antihypertensive TIS was calculated by dividing the total daily dose of each antihypertensive medication by the maximum US Food and Drug Administrationapproved daily dose.[11]
Adverse Outcomes Definition
We defined an adverse outcome as a 25% decrease in systolic or diastolic BP within 6 hours and/or intervention to treat symptoms of hypotension. This definition is consistent with Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) recommendations to assure safety when lowering BP in the setting of hypertensive emergency.[6] Although the patients in this study were not experiencing hypertensive emergency, this definition is supported by reports of negative sequelae from overzealous lowering of BP,[12, 13, 14] and it reflects criteria used in other trials.[10] Hypotension was deemed to have occurred if any of the following were documented: as IV fluid administration; scheduled BP medication held (at either the nurses discretion or per physician order); change in level of care; change in mental status; or transient ischemic attack, stroke, or chest pain within 30 minutes to 6 hours after administration. Heart rate changes were also considered to be adverse outcomes, including tachycardia (heart rate >100 beats per minute [bpm] or increase 20 bpm from baseline) or bradycardia (heart rate <50 bpm).
Analysis
Descriptive statistics were performed for all variables. Continuous data were summarized using means and standard deviations. Categorical variables were summarized as counts and percentages. Paired t tests were used to contrast changes from baseline for continuous variables pre‐ and post‐BP, and heart rate changes were evaluated only for the first episode of IV antihypertensive drug administration in patients receiving multiple doses of antihypertensive medication to avoid the bias created by repeated or clustered measures in a given patient. 2 tests were used to test differences in categorical variables. All statistical testing was considered significant when 2‐tailed P values were <0.05. Analyses were generated using SAS software version 9.4 (SAS Institute Inc., Cary, NC).
RESULTS
Patients
During the study period, there were 6133 inpatient adult admissions. Of 495 patients who had at least 1 order for IV hydralazine, enalaprilat, labetolol, or metoprolol, 246 were included in the analysis after applying the exclusion criteria (Figure 1). Patients were divided into 2 groups. One group had an order for an IV antihypertensive that was not administered (n = 74), and the other had an order for an IV antihypertensive and received at least 1 dose (n = 172). The demographic characteristics of the 2 groups are compared in Table 1. Patients who had their chronic oral antihypertensive regimens intensified after receiving IV antihypertensive medications were more often African American, leaner, more intensively treated, and had higher baseline BP.
| Did Not Receive IV Antihypertensive (n = 74) | Did Receive IV Antihypertensive (n = 172) | P | |
|---|---|---|---|
| |||
| Age, y | 61.6 13.9 | 60.6 13.7 | |
| Male sex | 51% | 47% | |
| African American | 74% | 87% | 0.008 |
| Weight, kg | 94.6 33.2 | 88.5 27.7 | |
| Admit systolic BP | 148 23 | 163 32 | <0.0001 |
| Admit diastolic BP | 82 13 | 87 18 | 0.009 |
| Admit heart rate | 87 18 | 82 20 | 0.069 |
| Admit TIS | 0.84 0.72 | 1.08 0.88 | 0.026 |
| Baseline SCr | 1.78 2.00 | 2.74 3.30 | 0.006 |
| Baseline AST | 26.5 12.5 | 65 126.2 | 0.046 |
| Low‐sodium diet order | 65% | 83% | 0.002 |
| Ordering service | |||
| Cardiology | 14% | 19% | |
| Internal medicine | 49% | 47% | |
| Nephrology | 0% | 6% | |
| Other services | 37% | 28% | |
| Prescriber type | |||
| Resident | 30% | 49% | |
| Physician extender | 53% | 35% | |
| Attending | 17% | 16% | |
| 1‐time‐only order | 5% | 19% | |
| As‐needed order | 95% | 81% | |
Prescribing Patterns
Medical residents prescribed nearly half (49%) of the orders for episodic IV antihypertensives. Attending physicians were responsible for 16% of episodic antihypertensive orders and physician extenders (physician's assistants and nurse practitioners) for 35%. A total of 321 orders were prescribed for the 246 patients in the study. Hydralazine was the preferred antihypertensive agent (80.1%), with IV ‐blockers prescribed less frequently (labetalol 15.6% and metoprolol 4.4%). There were no orders for IV enalaprilat. BP parameters were included in 181 (56%) of the episodic IV antihypertensive orders. Of the IV antihypertensive orders containing criteria, 153 (84.5%) had systolic BP threshold for administration <180 mm Hg (Table 2).
| BP Criteria for Administration of IV Antihypertensive Contained in Order, mm Hg | Did Not Receive IV Antihypertensive, n (%), n = 71* | Did Receive IV Antihypertensive, n (%), n = 133* |
|---|---|---|
| ||
| SBP >120 | 2 (2.8) | 1 (0.7) |
| SBP >130 | 2 (2.8) | 9 (6.8) |
| SBP >140 | 2 (2.8) | 5 (3.8) |
| SBP >150 | 4 (5.6) | 8 (6) |
| SBP >160 | 27 (38) | 58 (43.7) |
| SBP >170 | 26 (36.6) | 29 (21.8) |
| SBP >180 | 8 (11.4) | 18 (13.5) |
| SBP >200 | 4 (3) | |
| DBP >100 | 1 (0.7) | |
Drug Administration and Short‐term Data
Table 2 indicates the BP criteria specified in the episodic IV antihypertensive orders. For the 74 patients who did not receive an episodic IV antihypertensive agent, despite having an order, the nurses caring for the patients determined that their BPs never met the criteria for administration of the IV antihypertensive agent. The remainder of the results apply only to the 172 patients who actually received episodic IV antihypertensive therapy. Two of these patients did not have BP data available and were not included in the short‐term BP analysis. Almost half (48%) of the patients received 1 dose of episodic IV antihypertensive, 26% received 2 doses, and 11% received 3 doses. One patient received 10 doses. Hydralazine significantly lowered BP, whereas metoprolol did not (Figure 2).
The number of IV antihypertensive doses (for which BP data are available) administered during the night shift (n = 75) was numerically higher than the morning (n = 54) and the afternoon (n = 41) shifts. The mean BPs that triggered administration of IV antihypertensives did not differ among shifts (night shift 183/93, morning shift 184/99, afternoon shift 182/97).
Changes to Oral Antihypertensive Regimen After Administration of IV Antihypertensive Drugs
After administration of an episodic IV antihypertensive, the inpatient oral medication regimen was intensified in only 89 patients (52%). The BP reduction from admission to discharge in patients who had their inpatient oral medication regimen adjusted versus those who did not have an inpatient oral regimen adjustment after receiving IV antihypertensive medication is shown in Figure 3. Patients with intensification of their oral medications had a greater reduction in systolic BP from admission to discharge, compared to patients who received episodic IV antihypertensives but had no subsequent change to their inpatient oral antihypertensive regimen (Figure 3).
Adverse Events
Fifty‐six patients (32.6%) demonstrated BP reductions of more than 25% within 6 hours of antihypertensive administration. Of these patients, 2 received IV fluids, and 6 (3.5%) had a scheduled oral BP medication held. Of the patients who received IV hydralazine, 13 (4.4%) had an increase in heart rate >20 bpm, with 7 having a heart rate >100 bpm. One patient who received labetolol experienced bradycardia. No patient required a higher level of care (transfer to an intensive care unit) because of hemodynamic instability. In addition, no patient experienced a change in mental status, transient ischemic attack, stroke, or chest pain within 30 minutes to 6 hours after administration.
DISCUSSION
The overwhelming majority of administrations of costly episodic IV antihypertensive drugs among this low‐risk population were in patients with modest BP elevations who may have merited no more, at most, than intensification of their oral antihypertensive drug regimen or observation. Such administration was infrequently followed by intensification of the oral antihypertensive drug regimen, and a significant number of patients experienced a potentially adverse clinical event. Excessive reduction of BP resulting in withholding of oral agents or administering IV fluids (as seen in 8 patients) is clinically relevant, especially in a setting where rapid lowering of BP with IV antihypertensives have no proven clinical benefit. There were differences between patients who did and did not received IV antihypertensive drug therapy, as those receiving therapy were higher‐risk patients. Of the patients initially evaluated for inclusion in this analysis, approximately half had a clear indication for IV antihypertensive therapy and were not included in this analysis. It should also be noted that one‐third of the patients included in the study did not subsequently receive an IV antihypertensive agent.
Recently updated hypertensive guidelines do not address the treatment of hypertensive urgency and emergency, whereas the JNC 7 addressed hypertensive urgency but did not provide a specific BP definition or goals because of concerns about overly aggressive management of severe asymptomatic hypertension.[2, 6] For patients with chronically elevated BP, its rapid reduction, even to levels that remain in the frankly hypertensive range, can be associated with negative clinical sequelae, attributable to decreased target organ perfusion causing clinically manifest ischemia.[3] Accordingly, there have been reports of ischemic events related to unwarranted and overzealous BP lowering.[12, 13, 14] In such patients, resistance vessel remodeling causes a rightward shift of the entire pressure/flow auto regulatory curve in critical arterial beds (eg, cerebral, coronary, and renal). Higher systemic pressure is necessary to maintain adequate perfusion in the target organ, at least over the short‐term. Thus, rapid, aggressive BP reduction can result in the aforementioned negative sequelae because remodeled resistance arterioles are not capable of vasodilating enough to ensure adequate blood flow when systemic pressure falls precipitously.
The patients in this study had no evidence of new or worsening pressure‐related end‐organ damage; therefore, there appeared to be no medical justification for emergent BP lowering via the IV route (a very small minority may have had BP high enough to have justified being diagnosed with hypertensive urgency in which fast‐acting oral therapy would be used). Despite the paucity of data to support this practice, it does, however, appear to be relatively common.[9] The high prevalence of IV hydralazine use in this inpatient study is consistent with the retrospective study reported by Weder and Erickson at the University of Michigan.[9]
Even among those with hypertensive urgencies, oral medication is the preferred route (assuming the patient can eat and swallow without difficulty and does not manifest an altered sensorium). Furthermore, the risks associated with overzealous BP lowering can be devastating. The likelihood of target‐organ ischemia (eg, angina pectoris, myocardial infarction, azotemia, stroke, transient ischemic attack) is most strongly correlated to the rapidity of the BP reduction, even to levels within the hypertensive range, in patients with persistent poor BP control.[4, 15, 16] Thus, the justification for considering a >25% drop in systolic BP within 6 hours of the administration of the IV antihypertensive agent as a potential adverse event, especially because there was only a very small immediate risk for adverse cardiovascular sequelae at the BP levels triggering administration of IV antihypertensive drug therapy.
Although we found that residents and physician assistants prescribed most IV antihypertensives, the practice of prescribing IV antihypertensive therapy appears to be common among all prescriber types. A recent survey assessing the attitudes and practices of resident physicians regarding hypertension in the inpatient setting found that 44% of respondents would treat acute asymptomatic, moderately elevated BP (182/100 mm Hg) with either an oral or intravenous agent.[17]
In addition to there being no proven clinical benefit in this setting, the use of unnecessary IV antihypertensives is associated with unnecessary risks and excess cost. Another report of IV hydralazine in asymptomatic patients found that 17 of 94 patients experienced an adverse effect after administration.[18] Not only is the drug acquisition cost for IV antihypertensives greater than their oral counterparts, often by a factor of 10 to 100, the intravenous route requires additional care to monitor their effects, adding to the human resource expense. Finally, the onset of action of intravenous agents is generally more rapid, which increases the risk of inducing hypotension and therefore target‐organ ischemia.
This study does, however, have limitations. This is a single‐center study, so the findings may not be generalizable to different hospital settings. The findings of this study depend on the accuracy and completeness of the medical record as recorded during routine clinical care; therefore, errors and omissions of data input and documentation may affect the quality of the data. Omissions and errors in the medication history can affect inpatient management as well as appropriateness of discharge medications. BP values before and after administration of an IV antihypertensive were not always available, limiting some of the short‐term outcomes data that were available. The impact of acuity of illness and concomitant disease states of patients were not assessed, which could also affect outcomes. The outcomes measured in this investigation were all short‐term outcomes and did not include important clinical outcomes (long‐term BP control, rehospitalization rates, or patient morbidity or mortality).
We speculate that the practice of episodic IV antihypertensive therapy has developed out of convenience for the practitioner and is likely commonplace across the country.[17] Healthcare systems should examine practices locally and address them as appropriate. To assist in promoting evidence‐based practice that is safe, prudent, and clinically appropriate, we propose that national BP organizations and consensus development groups consider placing priority on developing recommendations for inpatient hypertension treatment algorithms beyond those for hypertensive emergencies. In many cases, adjustments to a patient's oral regimen or observation of the patient are the only interventions that are needed. In addition, appropriate coordination of ambulatory follow‐up care upon discharge is prudent. Finally, individual healthcare systems might need to identify formal programs to modify institutional behavior of both medical and nursing staff to eliminate or limit this practice that is not supported by clinical evidence and potentially places the patient at risk.
CONCLUSIONS
Our study found that the practice of prescribing episodic IV antihypertensive agents at our institution occurred across all prescriber types. Hydralazine was the most frequently ordered agent. The majority of orders containing systolic BP criteria for administration of an episodic IV antihypertensive agent were well below the BP level associated with immediate or near‐immediate cardiovascular risk. Administration of episodic IV antihypertensive agents, without subsequent intensification of the patient's chronic oral antihypertensive regimen was nearly as likely to occur as subsequent intensification of the oral regimen in our study. The absence of evidence‐based guidelines, combined with the results of this evaluation, provide a rationale for implementing hospital‐ and health systembased policies limiting the use of episodic IV antihypertensive agents in asymptomatic patients with uncontrolled BP in noncritical care settings in the absence of new or worsening target‐organ injury.
Disclosure: Nothing to report.
- , , , et al. Treatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation. 2007;115(21):2761–2788.
- , , , et al. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520.
- , . Hypertensive crises: challenges and management. Chest. 2007;131(6):1949–1962.
- , . Severely increased blood pressure in the emergency department. Ann Emerg Med. 2003;41(4):513–529.
- , , , , ; American College of Emergency Physicians Clinical Policies Subcommittee on Asymptomatic Hypertension in the ED. Clinical policy: critical issues in the evaluation and management of adult patients with asymptomatic hypertension in the emergency department. Ann Emerg Med.2006;47(3):237–249.
- , , , et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572.
- , . Best Evidence on management of asymptomatic hypertension in ED patients. J Emerg Nurs. 2011;37(2):174–178.
- , , , et al. A novel pathway for the management of hypertension for hospitalized patients. Crit Pathw Cardiol. 2007;6(4):150–160.
- , . Treatment of hypertension in the inpatient setting: use of intravenous labetalol and hydralazine. J Clin Hypertens (Greenwich). 2010;12(1):29–33.
- , , , et al. Patterns of antihypertensive treatment in patients with acute severe hypertension from a nonneurologic cause: Studying the Treatment of Acute Hypertension (STAT) registry. Pharmacotherapy. 2010;30(11):1087–1096.
- , , , , . Does earlier attainment of blood pressure goal translate into fewer cardiovascular events? Curr Hypertens Rep. 2008;10(5):398–404.
- . Symptomatic hypotension induced by nifedipine in the acute treatment of severe hypertension. Arch Intern Med. 1987;147(3):556–558.
- , , . Rapid reduction of severe asymptomatic hypertension. A prospective, controlled trial. Arch Intern Med. 1989;149(10):2186–2189.
- , , . Nifedipine‐associated myocardial ischemia or infarction in the treatment of hypertensive urgencies. Ann Intern Med. 1987;107(2):185–186.
- , , , , . Stroke precipitated by moderate blood pressure reduction. J Emerg Med. 2000;9(4):339–346.
- , , , . Adverse events associated with aggressive treatment of increased blood pressure. Int J Clin Prac. 2004;58(5):517–519.
- , , , et al. Attitudes and practices of resident physicians regarding hypertension in the inpatient setting. J Clin Hypertens. 2010;12(9):698–705.
- , , , . Intravenous hydralazine for blood pressure management in the hospitalized patient: its use is often unjustified. J Am Soc Hypertens. 2011;5(6):473–477.
- , , , et al. Treatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation. 2007;115(21):2761–2788.
- , , , et al. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520.
- , . Hypertensive crises: challenges and management. Chest. 2007;131(6):1949–1962.
- , . Severely increased blood pressure in the emergency department. Ann Emerg Med. 2003;41(4):513–529.
- , , , , ; American College of Emergency Physicians Clinical Policies Subcommittee on Asymptomatic Hypertension in the ED. Clinical policy: critical issues in the evaluation and management of adult patients with asymptomatic hypertension in the emergency department. Ann Emerg Med.2006;47(3):237–249.
- , , , et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572.
- , . Best Evidence on management of asymptomatic hypertension in ED patients. J Emerg Nurs. 2011;37(2):174–178.
- , , , et al. A novel pathway for the management of hypertension for hospitalized patients. Crit Pathw Cardiol. 2007;6(4):150–160.
- , . Treatment of hypertension in the inpatient setting: use of intravenous labetalol and hydralazine. J Clin Hypertens (Greenwich). 2010;12(1):29–33.
- , , , et al. Patterns of antihypertensive treatment in patients with acute severe hypertension from a nonneurologic cause: Studying the Treatment of Acute Hypertension (STAT) registry. Pharmacotherapy. 2010;30(11):1087–1096.
- , , , , . Does earlier attainment of blood pressure goal translate into fewer cardiovascular events? Curr Hypertens Rep. 2008;10(5):398–404.
- . Symptomatic hypotension induced by nifedipine in the acute treatment of severe hypertension. Arch Intern Med. 1987;147(3):556–558.
- , , . Rapid reduction of severe asymptomatic hypertension. A prospective, controlled trial. Arch Intern Med. 1989;149(10):2186–2189.
- , , . Nifedipine‐associated myocardial ischemia or infarction in the treatment of hypertensive urgencies. Ann Intern Med. 1987;107(2):185–186.
- , , , , . Stroke precipitated by moderate blood pressure reduction. J Emerg Med. 2000;9(4):339–346.
- , , , . Adverse events associated with aggressive treatment of increased blood pressure. Int J Clin Prac. 2004;58(5):517–519.
- , , , et al. Attitudes and practices of resident physicians regarding hypertension in the inpatient setting. J Clin Hypertens. 2010;12(9):698–705.
- , , , . Intravenous hydralazine for blood pressure management in the hospitalized patient: its use is often unjustified. J Am Soc Hypertens. 2011;5(6):473–477.
© 2015 Society of Hospital Medicine