User login
Rapid-Response Teams Help Hospitalists Manage Non-Medical Distress
A team that could respond quickly to social and behavioral concerns—and not medical issues per se—would have tremendous benefits for patients and caregivers.
I think there has been a steady increase, over the last 20 years or so, in the number of very unhappy, angry, or misbehaving patients (e.g. abusive/threatening to staff). In some cases, the hospital and caregivers have failed the patient. In other cases, their frustration arises out of things outside the hospital’s direct control, such as Medicare observation status, or perhaps the patient or family is just unreasonable or suffering from a psychiatric or substance abuse disorder.
I’m not talking about the common occurrence of a disappointed patient or family who might calmly complain about something. Instead, I want to focus on those patients who, whether we perceive them as justifiably unhappy or not, are so angry that they become very time consuming and distressing to deal with. Maybe they shout about how their lawyer will be suing us and the newspaper will be writing a story about how awful we are. Or they shout and throw things, and staff become afraid of them.
In my May 2013 column, I discussed care plans for patients like this who are admitted frequently, but such plans are not sufficient in every case.
A Haphazard Approach
Most hospitals have an informal process of dealing with these patients; it starts with the bedside nurse and/or doctor trying to apologize or make adjustments to satisfy and calm the patient. If that fails, then perhaps the manager of the nursing unit gets involved. Others may be recruited, such as someone from the hospital’s risk management or “patient advocate” departments and hospital executives such as the CNO, CMO, or CEO. Sometimes several of these people may meet as a group in an effort to come up with a plan to address the situation. But, most institutions do not have a clear and consistent approach to this important work, so the hospital personnel involved end up “reinventing the wheel” each time.
The growing awareness that hospital personnel don’t seem to have a robust and confident approach to addressing this type of situation can increase a patient’s distress, and it may embolden some to become even more demanding or threatening.
And all of this takes a significant toll on bedside caregivers, who often spend so much time dealing with the angry patient that they have less time to devote to other patients, who are in turn at least a little more likely to become unhappy or suffer as a result of a distressed and busy caregiver.
A Consistent Approach: RRT for Non-Medical Distress
I think the potential benefit for patients and caregivers is significant enough that hospitals should develop a standardized approach to managing such patients, and rapid response teams (RRTs) could serve as a model. To be clear, I’m not advocating that RRTs add management of very angry or distressed patients to their current role. Let’s call it an “RRT for non-medical distress.” And, while I think it is a worthwhile idea, and I am in the early steps of trying to develop it at “my” hospital, I’m not aware of any such team in place anywhere now.
To make it practical, I think this team should be available only during weekday business hours and would comprise something like six to 10 people with clinical backgrounds who do mostly administrative work. For example, the team members could include two nursing unit directors, a risk manager, a patient advocate (or patient satisfaction “czar”), a psychiatrist, the hospitalist medical director, the chief medical officer, and a few other individuals selected for their communication skills.
One of the team members would be on call for a day or week at a time and would carry the team’s pager during business hours. Any hospital caregiver could send a page requesting the team’s assistance, and the on-call team member would respond immediately by phone or, if possible, in person. After the on-call team member’s initial assessment, the whole team would meet later the same day or early the next day. On most days, a few members of the team would be off and unable to attend the meeting. So, if the team has eight members, each meeting of the team might average about five participants.
Non-Medical Distress RRT Processes
When meeting to establish a plan for addressing an extraordinarily distressed patient/family, the team should follow a standardized written approach. A designated person should lead the conversation—perhaps the on-call team member who responded first—and another should take notes. Using a form developed for this purpose, the note-taker would capture a standardized data set that is likely to be useful in determining a course of action, as well as valuable in helping the team fine-tune its approach by reviewing trends in aggregate data. The form might include things like patient demographics; the patient’s complaints and demands; potential complicating patient issues such as substance abuse, psychoactive drugs, or psychiatric history; location in the hospital; and names of bedside caregivers. Every effort should be made to keep the meetings efficient and as brief as practical—typically 30-60 minutes.
I’m convinced that when deciding how to respond to the situation, the team should try to limit itself to choosing one or more of eight to 10 standard interventions, rather than aiming for an entirely customized response in every case. Among the standardized interventions:
- Service recovery tools, such as a handwritten apology letter;
- A meeting between the patient/family and the hospital CEO or CMO;
- Security guard(s) at the door, on “high alert” to help if called; or
- A behavioral contract specifying the expectations for both patient and hospital staff behavior.
You might think of additional “tools” this team could have in their standardized response set.
Why limit the team as much as possible to a small set of standardized interventions? Developing customized responses in each situation is time consuming and, arguably, has a higher risk of failure, since it will be difficult to ensure that all staff caring for the patient can understand and execute them effectively. And the small set of interventions will make it easier to track their effectiveness over multiple patients so that the whole process can be improved over time.
Set a High Bar
The team should not be activated for every unhappy or difficult patient; that would be overkill and would result in many activations requiring dedicated staff with no other duties to serve on the team each day. Instead, I think the team should be activated only for the most difficult and distressing cases, at least for the first few years. In a 300-bed hospital, this would be approximately one to 1.5 activations per week.
Bedside caregivers would likely feel some reassurance knowing that they can reliably get help managing the most difficult patients, and, if the plan is executed well, these patients may get care that is safer for both themselves and staff. Who knows, medical outcomes might be improved for these patients also.

A team that could respond quickly to social and behavioral concerns—and not medical issues per se—would have tremendous benefits for patients and caregivers.
I think there has been a steady increase, over the last 20 years or so, in the number of very unhappy, angry, or misbehaving patients (e.g. abusive/threatening to staff). In some cases, the hospital and caregivers have failed the patient. In other cases, their frustration arises out of things outside the hospital’s direct control, such as Medicare observation status, or perhaps the patient or family is just unreasonable or suffering from a psychiatric or substance abuse disorder.
I’m not talking about the common occurrence of a disappointed patient or family who might calmly complain about something. Instead, I want to focus on those patients who, whether we perceive them as justifiably unhappy or not, are so angry that they become very time consuming and distressing to deal with. Maybe they shout about how their lawyer will be suing us and the newspaper will be writing a story about how awful we are. Or they shout and throw things, and staff become afraid of them.
In my May 2013 column, I discussed care plans for patients like this who are admitted frequently, but such plans are not sufficient in every case.
A Haphazard Approach
Most hospitals have an informal process of dealing with these patients; it starts with the bedside nurse and/or doctor trying to apologize or make adjustments to satisfy and calm the patient. If that fails, then perhaps the manager of the nursing unit gets involved. Others may be recruited, such as someone from the hospital’s risk management or “patient advocate” departments and hospital executives such as the CNO, CMO, or CEO. Sometimes several of these people may meet as a group in an effort to come up with a plan to address the situation. But, most institutions do not have a clear and consistent approach to this important work, so the hospital personnel involved end up “reinventing the wheel” each time.
The growing awareness that hospital personnel don’t seem to have a robust and confident approach to addressing this type of situation can increase a patient’s distress, and it may embolden some to become even more demanding or threatening.
And all of this takes a significant toll on bedside caregivers, who often spend so much time dealing with the angry patient that they have less time to devote to other patients, who are in turn at least a little more likely to become unhappy or suffer as a result of a distressed and busy caregiver.
A Consistent Approach: RRT for Non-Medical Distress
I think the potential benefit for patients and caregivers is significant enough that hospitals should develop a standardized approach to managing such patients, and rapid response teams (RRTs) could serve as a model. To be clear, I’m not advocating that RRTs add management of very angry or distressed patients to their current role. Let’s call it an “RRT for non-medical distress.” And, while I think it is a worthwhile idea, and I am in the early steps of trying to develop it at “my” hospital, I’m not aware of any such team in place anywhere now.
To make it practical, I think this team should be available only during weekday business hours and would comprise something like six to 10 people with clinical backgrounds who do mostly administrative work. For example, the team members could include two nursing unit directors, a risk manager, a patient advocate (or patient satisfaction “czar”), a psychiatrist, the hospitalist medical director, the chief medical officer, and a few other individuals selected for their communication skills.
One of the team members would be on call for a day or week at a time and would carry the team’s pager during business hours. Any hospital caregiver could send a page requesting the team’s assistance, and the on-call team member would respond immediately by phone or, if possible, in person. After the on-call team member’s initial assessment, the whole team would meet later the same day or early the next day. On most days, a few members of the team would be off and unable to attend the meeting. So, if the team has eight members, each meeting of the team might average about five participants.
Non-Medical Distress RRT Processes
When meeting to establish a plan for addressing an extraordinarily distressed patient/family, the team should follow a standardized written approach. A designated person should lead the conversation—perhaps the on-call team member who responded first—and another should take notes. Using a form developed for this purpose, the note-taker would capture a standardized data set that is likely to be useful in determining a course of action, as well as valuable in helping the team fine-tune its approach by reviewing trends in aggregate data. The form might include things like patient demographics; the patient’s complaints and demands; potential complicating patient issues such as substance abuse, psychoactive drugs, or psychiatric history; location in the hospital; and names of bedside caregivers. Every effort should be made to keep the meetings efficient and as brief as practical—typically 30-60 minutes.
I’m convinced that when deciding how to respond to the situation, the team should try to limit itself to choosing one or more of eight to 10 standard interventions, rather than aiming for an entirely customized response in every case. Among the standardized interventions:
- Service recovery tools, such as a handwritten apology letter;
- A meeting between the patient/family and the hospital CEO or CMO;
- Security guard(s) at the door, on “high alert” to help if called; or
- A behavioral contract specifying the expectations for both patient and hospital staff behavior.
You might think of additional “tools” this team could have in their standardized response set.
Why limit the team as much as possible to a small set of standardized interventions? Developing customized responses in each situation is time consuming and, arguably, has a higher risk of failure, since it will be difficult to ensure that all staff caring for the patient can understand and execute them effectively. And the small set of interventions will make it easier to track their effectiveness over multiple patients so that the whole process can be improved over time.
Set a High Bar
The team should not be activated for every unhappy or difficult patient; that would be overkill and would result in many activations requiring dedicated staff with no other duties to serve on the team each day. Instead, I think the team should be activated only for the most difficult and distressing cases, at least for the first few years. In a 300-bed hospital, this would be approximately one to 1.5 activations per week.
Bedside caregivers would likely feel some reassurance knowing that they can reliably get help managing the most difficult patients, and, if the plan is executed well, these patients may get care that is safer for both themselves and staff. Who knows, medical outcomes might be improved for these patients also.

A team that could respond quickly to social and behavioral concerns—and not medical issues per se—would have tremendous benefits for patients and caregivers.
I think there has been a steady increase, over the last 20 years or so, in the number of very unhappy, angry, or misbehaving patients (e.g. abusive/threatening to staff). In some cases, the hospital and caregivers have failed the patient. In other cases, their frustration arises out of things outside the hospital’s direct control, such as Medicare observation status, or perhaps the patient or family is just unreasonable or suffering from a psychiatric or substance abuse disorder.
I’m not talking about the common occurrence of a disappointed patient or family who might calmly complain about something. Instead, I want to focus on those patients who, whether we perceive them as justifiably unhappy or not, are so angry that they become very time consuming and distressing to deal with. Maybe they shout about how their lawyer will be suing us and the newspaper will be writing a story about how awful we are. Or they shout and throw things, and staff become afraid of them.
In my May 2013 column, I discussed care plans for patients like this who are admitted frequently, but such plans are not sufficient in every case.
A Haphazard Approach
Most hospitals have an informal process of dealing with these patients; it starts with the bedside nurse and/or doctor trying to apologize or make adjustments to satisfy and calm the patient. If that fails, then perhaps the manager of the nursing unit gets involved. Others may be recruited, such as someone from the hospital’s risk management or “patient advocate” departments and hospital executives such as the CNO, CMO, or CEO. Sometimes several of these people may meet as a group in an effort to come up with a plan to address the situation. But, most institutions do not have a clear and consistent approach to this important work, so the hospital personnel involved end up “reinventing the wheel” each time.
The growing awareness that hospital personnel don’t seem to have a robust and confident approach to addressing this type of situation can increase a patient’s distress, and it may embolden some to become even more demanding or threatening.
And all of this takes a significant toll on bedside caregivers, who often spend so much time dealing with the angry patient that they have less time to devote to other patients, who are in turn at least a little more likely to become unhappy or suffer as a result of a distressed and busy caregiver.
A Consistent Approach: RRT for Non-Medical Distress
I think the potential benefit for patients and caregivers is significant enough that hospitals should develop a standardized approach to managing such patients, and rapid response teams (RRTs) could serve as a model. To be clear, I’m not advocating that RRTs add management of very angry or distressed patients to their current role. Let’s call it an “RRT for non-medical distress.” And, while I think it is a worthwhile idea, and I am in the early steps of trying to develop it at “my” hospital, I’m not aware of any such team in place anywhere now.
To make it practical, I think this team should be available only during weekday business hours and would comprise something like six to 10 people with clinical backgrounds who do mostly administrative work. For example, the team members could include two nursing unit directors, a risk manager, a patient advocate (or patient satisfaction “czar”), a psychiatrist, the hospitalist medical director, the chief medical officer, and a few other individuals selected for their communication skills.
One of the team members would be on call for a day or week at a time and would carry the team’s pager during business hours. Any hospital caregiver could send a page requesting the team’s assistance, and the on-call team member would respond immediately by phone or, if possible, in person. After the on-call team member’s initial assessment, the whole team would meet later the same day or early the next day. On most days, a few members of the team would be off and unable to attend the meeting. So, if the team has eight members, each meeting of the team might average about five participants.
Non-Medical Distress RRT Processes
When meeting to establish a plan for addressing an extraordinarily distressed patient/family, the team should follow a standardized written approach. A designated person should lead the conversation—perhaps the on-call team member who responded first—and another should take notes. Using a form developed for this purpose, the note-taker would capture a standardized data set that is likely to be useful in determining a course of action, as well as valuable in helping the team fine-tune its approach by reviewing trends in aggregate data. The form might include things like patient demographics; the patient’s complaints and demands; potential complicating patient issues such as substance abuse, psychoactive drugs, or psychiatric history; location in the hospital; and names of bedside caregivers. Every effort should be made to keep the meetings efficient and as brief as practical—typically 30-60 minutes.
I’m convinced that when deciding how to respond to the situation, the team should try to limit itself to choosing one or more of eight to 10 standard interventions, rather than aiming for an entirely customized response in every case. Among the standardized interventions:
- Service recovery tools, such as a handwritten apology letter;
- A meeting between the patient/family and the hospital CEO or CMO;
- Security guard(s) at the door, on “high alert” to help if called; or
- A behavioral contract specifying the expectations for both patient and hospital staff behavior.
You might think of additional “tools” this team could have in their standardized response set.
Why limit the team as much as possible to a small set of standardized interventions? Developing customized responses in each situation is time consuming and, arguably, has a higher risk of failure, since it will be difficult to ensure that all staff caring for the patient can understand and execute them effectively. And the small set of interventions will make it easier to track their effectiveness over multiple patients so that the whole process can be improved over time.
Set a High Bar
The team should not be activated for every unhappy or difficult patient; that would be overkill and would result in many activations requiring dedicated staff with no other duties to serve on the team each day. Instead, I think the team should be activated only for the most difficult and distressing cases, at least for the first few years. In a 300-bed hospital, this would be approximately one to 1.5 activations per week.
Bedside caregivers would likely feel some reassurance knowing that they can reliably get help managing the most difficult patients, and, if the plan is executed well, these patients may get care that is safer for both themselves and staff. Who knows, medical outcomes might be improved for these patients also.

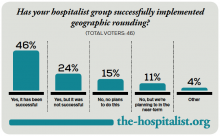
Geographic Rounding of Hospital Nurses Challenges Unit-Based Theory
Nurses, of course, have always been assigned by unit—that is, geographically. So it should come as no surprise that searching “unit-based” at the-hospitalist.org returns many articles about assigning hospitalists geographically, but not nurses, partly because few would consider it a new idea. But this article is about a new wrinkle in assigning nurses.
Although there likely are a number of hospitals doing something similar, I’ll describe a place I was lucky enough to see up close.
Bassett Medical Center
On a cold day last December, I was part of a team that spent a few days in Cooperstown, N.Y. This is a place that is so pretty that I didn’t immediately recognize we had arrived at the Bassett Medical Center Campus, since the entrance we used looked more like a library topped by a pretty cupola and warmly decorated for the holidays. We met so many nice people, including Kai Mebust, MD, FHM, who I’m convinced works full-time for the local Chamber of Commerce and tourism industry. If he doesn’t, then they should put him on their payroll.
Not long after our arrival, Dr. Mebust led us outside in the winter air without our coats to see the very beautiful view from the patio adjacent to the hospital cafeteria. And before we left for home he climbed in our car to direct us on a tour of the town. I’m sold. What a beautiful place. So much more than the Baseball Hall of Fame for which Cooperstown is known.
When not promoting his town’s tourism or enthusiastically describing his eighth-grade son playing with the Preservation Hall Jazz Band in New Orleans, he seems to find time to serve as the chief of this academic hospital’s hospital medicine practice. He was the principal engineer of the geographic assignment of nurses and describes it with an enthusiasm that matches his service as tour guide.
Geographic Care: Single RN Caring for Five Adjacent Patients
The idea is simple and best described using an illustration. A single nurse cares for five patients in adjacent rooms referred to as a “pod.” A second nurse is responsible for the next pod of five consecutive patients, and a single hospitalist cares for all 10 in both pods. There are currently four pods on a single floor of 36 beds; however, they hope to expand this system to most of the medical-surgical beds in the hospital.
The nurses eligible to care for patients in these pods are all trained to be able to provide “step down” level of care, meaning patients don’t need to transfer to a different location for more frequent monitoring and such therapies as vasopressors, mask ventilation, and the like.
Each hospitalist caring for two pods of 10 adjacent patients will typically have additional patients in other locations. This is the hospital’s way of finding the sweet spot between the competing interests of “load leveling” patient volume across hospitalists and rigidly assigning each doctor to a single location, though if they succeed in expanding the model through most of the hospital, the hospitalists will likely need to figure out how to assign themselves more rigidly to three or four pods.
Additional Components
Each morning, the hospitalist meets with the two pod nurses. They briefly discuss overnight events and plans for the day.
Much later in the morning, they also conduct daily multidisciplinary rounds involving nurse, case manager, pharmacist, dietician, social worker, respiratory therapist, and hospitalist. These follow a standard format, which is posted on the wall, and are done in a workroom that allows most participants to be in front of a computer, so they can enter notes and orders into the electronic health record (EHR) as they discuss patients.
What Is the Big Deal Here?
A lot of smart people have developed and written about systems that assign hospitalists geographically, but in most cases this has not been accompanied by adjustments in the way nurses are assigned. On nursing units at most hospitals, this means that even if a hospitalist has all of her patients on the same floor, she is still interacting with five to seven nurses caring for her patients. That usually means the hospitalist and nurse have less awareness of each other’s thinking and doing than if the ratio is reduced to no more than three or four nurses for a single hospitalist.
Dr. Mebust provided a document enumerating the goals for the program:
- Improve communication;
- Reduce patient bed moves;
- Improve patient and staff satisfaction; and
- Provide more efficient care as measured in time-of-discharge, decreased physician time-per-patient, and possibly length of stay.
Because of a number of problems teasing out the effects of this program and its limited duration to this point, Dr. Mebust and staff can’t provide robust statistics to document success in these goals. But anecdotal information is very encouraging, and clearly the nurses love it.
A major barrier to assigning nurses based rigidly on patients in adjacent rooms is the inability to ensure that each nurse has a workload of roughly equivalent complexity, but they’ve found this is a much less significant problem than feared. The nurse I spoke with said any risk of ending up with unusually complex and time-consuming patients is essentially offset by the efficiency gained by having the same attending hospitalist for all of her patients.
In fact, the nurses love it so much that they much prefer being assigned to a pod rather than a traditional assortment of patients with different attending physicians, even if the latter offers a chance to address uneven acuity.
The Big Picture
I’ve often wished that I could incorporate into hospitalist work some of the efficient ways a doctor and nurse can work together seeing scheduled patients in an outpatient setting. Surely assigning hospitalists geographically does this to some degree and has a number of advantages that others have written about. But it comes at the cost of difficult tradeoffs for hospitalists, and I know of many groups that have abandoned it after concluding that the challenges of the system exceeded its benefits.
But when it is coupled with assigning nurses geographically, I think the benefits are even greater, not only for the hospitalists, but also for patients, nurses, and other hospital staff.
Next time you’re in Cooperstown, be sure you don’t just visit the Baseball Hall of Fame. Look up Dr. Mebust, Komron Ostovar, MD, and their colleagues at Bassett Medical Center. I betcha you’ll be persuaded to see the value of their geographic model.
And maybe you’ll even fall so far under the spell of how they all talk about where they work and live that you’ll be ready to move there and join them.

Nurses, of course, have always been assigned by unit—that is, geographically. So it should come as no surprise that searching “unit-based” at the-hospitalist.org returns many articles about assigning hospitalists geographically, but not nurses, partly because few would consider it a new idea. But this article is about a new wrinkle in assigning nurses.
Although there likely are a number of hospitals doing something similar, I’ll describe a place I was lucky enough to see up close.
Bassett Medical Center
On a cold day last December, I was part of a team that spent a few days in Cooperstown, N.Y. This is a place that is so pretty that I didn’t immediately recognize we had arrived at the Bassett Medical Center Campus, since the entrance we used looked more like a library topped by a pretty cupola and warmly decorated for the holidays. We met so many nice people, including Kai Mebust, MD, FHM, who I’m convinced works full-time for the local Chamber of Commerce and tourism industry. If he doesn’t, then they should put him on their payroll.
Not long after our arrival, Dr. Mebust led us outside in the winter air without our coats to see the very beautiful view from the patio adjacent to the hospital cafeteria. And before we left for home he climbed in our car to direct us on a tour of the town. I’m sold. What a beautiful place. So much more than the Baseball Hall of Fame for which Cooperstown is known.
When not promoting his town’s tourism or enthusiastically describing his eighth-grade son playing with the Preservation Hall Jazz Band in New Orleans, he seems to find time to serve as the chief of this academic hospital’s hospital medicine practice. He was the principal engineer of the geographic assignment of nurses and describes it with an enthusiasm that matches his service as tour guide.
Geographic Care: Single RN Caring for Five Adjacent Patients
The idea is simple and best described using an illustration. A single nurse cares for five patients in adjacent rooms referred to as a “pod.” A second nurse is responsible for the next pod of five consecutive patients, and a single hospitalist cares for all 10 in both pods. There are currently four pods on a single floor of 36 beds; however, they hope to expand this system to most of the medical-surgical beds in the hospital.
The nurses eligible to care for patients in these pods are all trained to be able to provide “step down” level of care, meaning patients don’t need to transfer to a different location for more frequent monitoring and such therapies as vasopressors, mask ventilation, and the like.
Each hospitalist caring for two pods of 10 adjacent patients will typically have additional patients in other locations. This is the hospital’s way of finding the sweet spot between the competing interests of “load leveling” patient volume across hospitalists and rigidly assigning each doctor to a single location, though if they succeed in expanding the model through most of the hospital, the hospitalists will likely need to figure out how to assign themselves more rigidly to three or four pods.
Additional Components
Each morning, the hospitalist meets with the two pod nurses. They briefly discuss overnight events and plans for the day.
Much later in the morning, they also conduct daily multidisciplinary rounds involving nurse, case manager, pharmacist, dietician, social worker, respiratory therapist, and hospitalist. These follow a standard format, which is posted on the wall, and are done in a workroom that allows most participants to be in front of a computer, so they can enter notes and orders into the electronic health record (EHR) as they discuss patients.
What Is the Big Deal Here?
A lot of smart people have developed and written about systems that assign hospitalists geographically, but in most cases this has not been accompanied by adjustments in the way nurses are assigned. On nursing units at most hospitals, this means that even if a hospitalist has all of her patients on the same floor, she is still interacting with five to seven nurses caring for her patients. That usually means the hospitalist and nurse have less awareness of each other’s thinking and doing than if the ratio is reduced to no more than three or four nurses for a single hospitalist.
Dr. Mebust provided a document enumerating the goals for the program:
- Improve communication;
- Reduce patient bed moves;
- Improve patient and staff satisfaction; and
- Provide more efficient care as measured in time-of-discharge, decreased physician time-per-patient, and possibly length of stay.
Because of a number of problems teasing out the effects of this program and its limited duration to this point, Dr. Mebust and staff can’t provide robust statistics to document success in these goals. But anecdotal information is very encouraging, and clearly the nurses love it.
A major barrier to assigning nurses based rigidly on patients in adjacent rooms is the inability to ensure that each nurse has a workload of roughly equivalent complexity, but they’ve found this is a much less significant problem than feared. The nurse I spoke with said any risk of ending up with unusually complex and time-consuming patients is essentially offset by the efficiency gained by having the same attending hospitalist for all of her patients.
In fact, the nurses love it so much that they much prefer being assigned to a pod rather than a traditional assortment of patients with different attending physicians, even if the latter offers a chance to address uneven acuity.
The Big Picture
I’ve often wished that I could incorporate into hospitalist work some of the efficient ways a doctor and nurse can work together seeing scheduled patients in an outpatient setting. Surely assigning hospitalists geographically does this to some degree and has a number of advantages that others have written about. But it comes at the cost of difficult tradeoffs for hospitalists, and I know of many groups that have abandoned it after concluding that the challenges of the system exceeded its benefits.
But when it is coupled with assigning nurses geographically, I think the benefits are even greater, not only for the hospitalists, but also for patients, nurses, and other hospital staff.
Next time you’re in Cooperstown, be sure you don’t just visit the Baseball Hall of Fame. Look up Dr. Mebust, Komron Ostovar, MD, and their colleagues at Bassett Medical Center. I betcha you’ll be persuaded to see the value of their geographic model.
And maybe you’ll even fall so far under the spell of how they all talk about where they work and live that you’ll be ready to move there and join them.

Nurses, of course, have always been assigned by unit—that is, geographically. So it should come as no surprise that searching “unit-based” at the-hospitalist.org returns many articles about assigning hospitalists geographically, but not nurses, partly because few would consider it a new idea. But this article is about a new wrinkle in assigning nurses.
Although there likely are a number of hospitals doing something similar, I’ll describe a place I was lucky enough to see up close.
Bassett Medical Center
On a cold day last December, I was part of a team that spent a few days in Cooperstown, N.Y. This is a place that is so pretty that I didn’t immediately recognize we had arrived at the Bassett Medical Center Campus, since the entrance we used looked more like a library topped by a pretty cupola and warmly decorated for the holidays. We met so many nice people, including Kai Mebust, MD, FHM, who I’m convinced works full-time for the local Chamber of Commerce and tourism industry. If he doesn’t, then they should put him on their payroll.
Not long after our arrival, Dr. Mebust led us outside in the winter air without our coats to see the very beautiful view from the patio adjacent to the hospital cafeteria. And before we left for home he climbed in our car to direct us on a tour of the town. I’m sold. What a beautiful place. So much more than the Baseball Hall of Fame for which Cooperstown is known.
When not promoting his town’s tourism or enthusiastically describing his eighth-grade son playing with the Preservation Hall Jazz Band in New Orleans, he seems to find time to serve as the chief of this academic hospital’s hospital medicine practice. He was the principal engineer of the geographic assignment of nurses and describes it with an enthusiasm that matches his service as tour guide.
Geographic Care: Single RN Caring for Five Adjacent Patients
The idea is simple and best described using an illustration. A single nurse cares for five patients in adjacent rooms referred to as a “pod.” A second nurse is responsible for the next pod of five consecutive patients, and a single hospitalist cares for all 10 in both pods. There are currently four pods on a single floor of 36 beds; however, they hope to expand this system to most of the medical-surgical beds in the hospital.
The nurses eligible to care for patients in these pods are all trained to be able to provide “step down” level of care, meaning patients don’t need to transfer to a different location for more frequent monitoring and such therapies as vasopressors, mask ventilation, and the like.
Each hospitalist caring for two pods of 10 adjacent patients will typically have additional patients in other locations. This is the hospital’s way of finding the sweet spot between the competing interests of “load leveling” patient volume across hospitalists and rigidly assigning each doctor to a single location, though if they succeed in expanding the model through most of the hospital, the hospitalists will likely need to figure out how to assign themselves more rigidly to three or four pods.
Additional Components
Each morning, the hospitalist meets with the two pod nurses. They briefly discuss overnight events and plans for the day.
Much later in the morning, they also conduct daily multidisciplinary rounds involving nurse, case manager, pharmacist, dietician, social worker, respiratory therapist, and hospitalist. These follow a standard format, which is posted on the wall, and are done in a workroom that allows most participants to be in front of a computer, so they can enter notes and orders into the electronic health record (EHR) as they discuss patients.
What Is the Big Deal Here?
A lot of smart people have developed and written about systems that assign hospitalists geographically, but in most cases this has not been accompanied by adjustments in the way nurses are assigned. On nursing units at most hospitals, this means that even if a hospitalist has all of her patients on the same floor, she is still interacting with five to seven nurses caring for her patients. That usually means the hospitalist and nurse have less awareness of each other’s thinking and doing than if the ratio is reduced to no more than three or four nurses for a single hospitalist.
Dr. Mebust provided a document enumerating the goals for the program:
- Improve communication;
- Reduce patient bed moves;
- Improve patient and staff satisfaction; and
- Provide more efficient care as measured in time-of-discharge, decreased physician time-per-patient, and possibly length of stay.
Because of a number of problems teasing out the effects of this program and its limited duration to this point, Dr. Mebust and staff can’t provide robust statistics to document success in these goals. But anecdotal information is very encouraging, and clearly the nurses love it.
A major barrier to assigning nurses based rigidly on patients in adjacent rooms is the inability to ensure that each nurse has a workload of roughly equivalent complexity, but they’ve found this is a much less significant problem than feared. The nurse I spoke with said any risk of ending up with unusually complex and time-consuming patients is essentially offset by the efficiency gained by having the same attending hospitalist for all of her patients.
In fact, the nurses love it so much that they much prefer being assigned to a pod rather than a traditional assortment of patients with different attending physicians, even if the latter offers a chance to address uneven acuity.
The Big Picture
I’ve often wished that I could incorporate into hospitalist work some of the efficient ways a doctor and nurse can work together seeing scheduled patients in an outpatient setting. Surely assigning hospitalists geographically does this to some degree and has a number of advantages that others have written about. But it comes at the cost of difficult tradeoffs for hospitalists, and I know of many groups that have abandoned it after concluding that the challenges of the system exceeded its benefits.
But when it is coupled with assigning nurses geographically, I think the benefits are even greater, not only for the hospitalists, but also for patients, nurses, and other hospital staff.
Next time you’re in Cooperstown, be sure you don’t just visit the Baseball Hall of Fame. Look up Dr. Mebust, Komron Ostovar, MD, and their colleagues at Bassett Medical Center. I betcha you’ll be persuaded to see the value of their geographic model.
And maybe you’ll even fall so far under the spell of how they all talk about where they work and live that you’ll be ready to move there and join them.

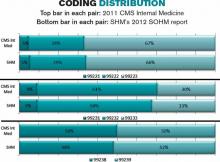
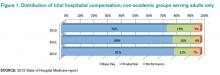
How to Use Hospitalist Productivity, Compensation Survey Data
The 2014 State of Hospital Medicine report (SOHM), published by SHM in the fall of even years, is unquestionably the most robust and informative data available to understand the hospitalist workforce marketplace. And if you are the person who returned a completed survey for your practice, you get a free copy of the report mailed to you.
Keep in mind that the Medical Group Management Association (MGMA) surveys and reports data on hospitalist productivity and compensation every year. And the data acquired by MGMA in even years is simply folded into the SOHM, along with a ton of additional information added by a separate SHM survey, including things like the amount of financial support provided to hospitalist groups by hospitals (now up to a median of $156, 063 per full-time equivalent, or FTE).
I’ve written previously about some of the ways that the data reported in both of these surveys can be tricky to interpret (September 2013 and October 2013), and in this column I’ll go a little deeper into how to use the data reported on number of shifts worked and productivity.
A Common Question
Assume that, to address a staffing shortage or simply as a way to boost their income, some of the doctors in your group are willing to work more shifts than required for full-time status. And, in your group, some portion of a doctor’s compensation is a function of their individual work relevant value unit (wRVU) productivity—for example, a bonus for wRVUs above a certain threshold. You want to know whether the wRVU productivity generated by a doctor on their extra shifts should factor into compensation the same way it does for “regular” shifts.
You might turn to the MGMA and SOHM surveys to see how other groups handle this issue. But here is where it gets tricky.
First, you need to realize that the MGMA surveys, and similar ones from the American Medical Group Association and others, report wRVUs and compensation per physician, not per FTE. So wRVUs generated by these doctors on extra shifts are included, and you can’t tell from the aggregate data what portion of wRVUs came from regular shifts and what portion came from extra shifts.
And it is critical to keep in mind that any doctor who works at least 0.8 FTE as defined by that particular practice is reported as full time. Those working 79% or less of full time are counted by MGMA as part time.
To summarize: The MGMA and similar surveys don’t provide data on wRVU productivity per FTE, even though in most cases that is how everyone describes the data. Instead, the surveys provide data per individual doctor, many of whom work more or less than 1.0 FTE. So, despite the fact that most people, including me, tend to quote data from the surveys as though it is per FTE, as in “The 2014 MGMA data shows median hospitalist compensation is $253,977 per FTE,” we should say “per doctor” instead.
Theoretically, doctors working slightly less than 1.0 FTE should offset the doctors working slightly more than 1.0 FTE. But, while I think that’s a reasonable assumption for most specialties, such a significant portion of hospitalist groups have had chronic staffing shortages that a lot of hospitalists across the country are working extra shifts, probably more than are working between 0.8 and 1.0 FTE. So the hospitalist survey wRVU data is probably at least a little higher than it would be if it were reported per FTE.
Unfortunately, there is no way to confirm my suspicion, because MGMA doesn’t allow any individual doctor to be reported as more than 1.0 FTE, even if he works far more shifts than the number that defines full time for that practice. In other words, extra shifts just aren’t accounted for in the MGMA survey.
Implications of Individual vs. FTE
For most purposes, it probably doesn’t make any difference if you are erroneously thinking about the compensation and productivity survey numbers on a per FTE basis. But, for some purposes, and for those who work significantly more shifts than most hospitalists, it can start to matter.
Now back to the original question. You’re thinking about whether wRVUs generated by the doctors in your group on extra shifts should count toward the wRVU bonus just like those generated on regular shifts. You’d like to handle this the same way as other groups, but, unfortunately, survey data just isn’t helpful here. You’ll have to decide this for yourself.
I think some, but probably not all, extra shift productivity should count toward your wRVU bonus. You might, for example, say that productivity for somewhere between three or five extra shifts per quarter—that’s totally arbitrary, and of course this would be a negotiation between you and hospital leadership—should count toward the productivity target, and the rest wouldn’t, or that those extra shifts above an agreed-upon number would result in an increase in the wRVU target. The biggest problem with this is that it would be a nightmare to administer—essentially impossible for many practices. But you could accomplish the same thing by including the first few shifts per quarter in the “base” FTE calculation and then, after that, adjusting each person’s FTE value up as they work more shifts.
One more thing about productivity targets…
It’s also important to remember that productivity targets make the most sense at the group—not the individual—level. The MGMA data includes hospitalists who work night shifts (including nocturnists) and doctors who work low-production shifts (i.e., pager or ED triage shifts), as well as daytime rounding doctors. So, if you have a doctor who only works days, you would expect him to generate wRVUs in excess of the global target of wRVUs per FTE to make up for the low-productivity shifts that other doctors have to work.
For example, your practice might decide the group as a whole is expected to generate the MGMA yearly median 4,298 wRVUs per doctor, multiplied by the number of FTEs in the group. But the nocturnists would be expected to generate fewer, while those who work most or all of their shifts in a daytime rounder would be expected to generate more. So the threshold to begin paying the wRVU bonus for daytime rounding doctors might be adjusted up to something like 4,500 wRVUs.
The above example is just as an illustration, of course, and there are all kinds of reasons it might be more appropriate to choose different thresholds for your practice. But it’s a good place to start the thinking.

The 2014 State of Hospital Medicine report (SOHM), published by SHM in the fall of even years, is unquestionably the most robust and informative data available to understand the hospitalist workforce marketplace. And if you are the person who returned a completed survey for your practice, you get a free copy of the report mailed to you.
Keep in mind that the Medical Group Management Association (MGMA) surveys and reports data on hospitalist productivity and compensation every year. And the data acquired by MGMA in even years is simply folded into the SOHM, along with a ton of additional information added by a separate SHM survey, including things like the amount of financial support provided to hospitalist groups by hospitals (now up to a median of $156, 063 per full-time equivalent, or FTE).
I’ve written previously about some of the ways that the data reported in both of these surveys can be tricky to interpret (September 2013 and October 2013), and in this column I’ll go a little deeper into how to use the data reported on number of shifts worked and productivity.
A Common Question
Assume that, to address a staffing shortage or simply as a way to boost their income, some of the doctors in your group are willing to work more shifts than required for full-time status. And, in your group, some portion of a doctor’s compensation is a function of their individual work relevant value unit (wRVU) productivity—for example, a bonus for wRVUs above a certain threshold. You want to know whether the wRVU productivity generated by a doctor on their extra shifts should factor into compensation the same way it does for “regular” shifts.
You might turn to the MGMA and SOHM surveys to see how other groups handle this issue. But here is where it gets tricky.
First, you need to realize that the MGMA surveys, and similar ones from the American Medical Group Association and others, report wRVUs and compensation per physician, not per FTE. So wRVUs generated by these doctors on extra shifts are included, and you can’t tell from the aggregate data what portion of wRVUs came from regular shifts and what portion came from extra shifts.
And it is critical to keep in mind that any doctor who works at least 0.8 FTE as defined by that particular practice is reported as full time. Those working 79% or less of full time are counted by MGMA as part time.
To summarize: The MGMA and similar surveys don’t provide data on wRVU productivity per FTE, even though in most cases that is how everyone describes the data. Instead, the surveys provide data per individual doctor, many of whom work more or less than 1.0 FTE. So, despite the fact that most people, including me, tend to quote data from the surveys as though it is per FTE, as in “The 2014 MGMA data shows median hospitalist compensation is $253,977 per FTE,” we should say “per doctor” instead.
Theoretically, doctors working slightly less than 1.0 FTE should offset the doctors working slightly more than 1.0 FTE. But, while I think that’s a reasonable assumption for most specialties, such a significant portion of hospitalist groups have had chronic staffing shortages that a lot of hospitalists across the country are working extra shifts, probably more than are working between 0.8 and 1.0 FTE. So the hospitalist survey wRVU data is probably at least a little higher than it would be if it were reported per FTE.
Unfortunately, there is no way to confirm my suspicion, because MGMA doesn’t allow any individual doctor to be reported as more than 1.0 FTE, even if he works far more shifts than the number that defines full time for that practice. In other words, extra shifts just aren’t accounted for in the MGMA survey.
Implications of Individual vs. FTE
For most purposes, it probably doesn’t make any difference if you are erroneously thinking about the compensation and productivity survey numbers on a per FTE basis. But, for some purposes, and for those who work significantly more shifts than most hospitalists, it can start to matter.
Now back to the original question. You’re thinking about whether wRVUs generated by the doctors in your group on extra shifts should count toward the wRVU bonus just like those generated on regular shifts. You’d like to handle this the same way as other groups, but, unfortunately, survey data just isn’t helpful here. You’ll have to decide this for yourself.
I think some, but probably not all, extra shift productivity should count toward your wRVU bonus. You might, for example, say that productivity for somewhere between three or five extra shifts per quarter—that’s totally arbitrary, and of course this would be a negotiation between you and hospital leadership—should count toward the productivity target, and the rest wouldn’t, or that those extra shifts above an agreed-upon number would result in an increase in the wRVU target. The biggest problem with this is that it would be a nightmare to administer—essentially impossible for many practices. But you could accomplish the same thing by including the first few shifts per quarter in the “base” FTE calculation and then, after that, adjusting each person’s FTE value up as they work more shifts.
One more thing about productivity targets…
It’s also important to remember that productivity targets make the most sense at the group—not the individual—level. The MGMA data includes hospitalists who work night shifts (including nocturnists) and doctors who work low-production shifts (i.e., pager or ED triage shifts), as well as daytime rounding doctors. So, if you have a doctor who only works days, you would expect him to generate wRVUs in excess of the global target of wRVUs per FTE to make up for the low-productivity shifts that other doctors have to work.
For example, your practice might decide the group as a whole is expected to generate the MGMA yearly median 4,298 wRVUs per doctor, multiplied by the number of FTEs in the group. But the nocturnists would be expected to generate fewer, while those who work most or all of their shifts in a daytime rounder would be expected to generate more. So the threshold to begin paying the wRVU bonus for daytime rounding doctors might be adjusted up to something like 4,500 wRVUs.
The above example is just as an illustration, of course, and there are all kinds of reasons it might be more appropriate to choose different thresholds for your practice. But it’s a good place to start the thinking.

The 2014 State of Hospital Medicine report (SOHM), published by SHM in the fall of even years, is unquestionably the most robust and informative data available to understand the hospitalist workforce marketplace. And if you are the person who returned a completed survey for your practice, you get a free copy of the report mailed to you.
Keep in mind that the Medical Group Management Association (MGMA) surveys and reports data on hospitalist productivity and compensation every year. And the data acquired by MGMA in even years is simply folded into the SOHM, along with a ton of additional information added by a separate SHM survey, including things like the amount of financial support provided to hospitalist groups by hospitals (now up to a median of $156, 063 per full-time equivalent, or FTE).
I’ve written previously about some of the ways that the data reported in both of these surveys can be tricky to interpret (September 2013 and October 2013), and in this column I’ll go a little deeper into how to use the data reported on number of shifts worked and productivity.
A Common Question
Assume that, to address a staffing shortage or simply as a way to boost their income, some of the doctors in your group are willing to work more shifts than required for full-time status. And, in your group, some portion of a doctor’s compensation is a function of their individual work relevant value unit (wRVU) productivity—for example, a bonus for wRVUs above a certain threshold. You want to know whether the wRVU productivity generated by a doctor on their extra shifts should factor into compensation the same way it does for “regular” shifts.
You might turn to the MGMA and SOHM surveys to see how other groups handle this issue. But here is where it gets tricky.
First, you need to realize that the MGMA surveys, and similar ones from the American Medical Group Association and others, report wRVUs and compensation per physician, not per FTE. So wRVUs generated by these doctors on extra shifts are included, and you can’t tell from the aggregate data what portion of wRVUs came from regular shifts and what portion came from extra shifts.
And it is critical to keep in mind that any doctor who works at least 0.8 FTE as defined by that particular practice is reported as full time. Those working 79% or less of full time are counted by MGMA as part time.
To summarize: The MGMA and similar surveys don’t provide data on wRVU productivity per FTE, even though in most cases that is how everyone describes the data. Instead, the surveys provide data per individual doctor, many of whom work more or less than 1.0 FTE. So, despite the fact that most people, including me, tend to quote data from the surveys as though it is per FTE, as in “The 2014 MGMA data shows median hospitalist compensation is $253,977 per FTE,” we should say “per doctor” instead.
Theoretically, doctors working slightly less than 1.0 FTE should offset the doctors working slightly more than 1.0 FTE. But, while I think that’s a reasonable assumption for most specialties, such a significant portion of hospitalist groups have had chronic staffing shortages that a lot of hospitalists across the country are working extra shifts, probably more than are working between 0.8 and 1.0 FTE. So the hospitalist survey wRVU data is probably at least a little higher than it would be if it were reported per FTE.
Unfortunately, there is no way to confirm my suspicion, because MGMA doesn’t allow any individual doctor to be reported as more than 1.0 FTE, even if he works far more shifts than the number that defines full time for that practice. In other words, extra shifts just aren’t accounted for in the MGMA survey.
Implications of Individual vs. FTE
For most purposes, it probably doesn’t make any difference if you are erroneously thinking about the compensation and productivity survey numbers on a per FTE basis. But, for some purposes, and for those who work significantly more shifts than most hospitalists, it can start to matter.
Now back to the original question. You’re thinking about whether wRVUs generated by the doctors in your group on extra shifts should count toward the wRVU bonus just like those generated on regular shifts. You’d like to handle this the same way as other groups, but, unfortunately, survey data just isn’t helpful here. You’ll have to decide this for yourself.
I think some, but probably not all, extra shift productivity should count toward your wRVU bonus. You might, for example, say that productivity for somewhere between three or five extra shifts per quarter—that’s totally arbitrary, and of course this would be a negotiation between you and hospital leadership—should count toward the productivity target, and the rest wouldn’t, or that those extra shifts above an agreed-upon number would result in an increase in the wRVU target. The biggest problem with this is that it would be a nightmare to administer—essentially impossible for many practices. But you could accomplish the same thing by including the first few shifts per quarter in the “base” FTE calculation and then, after that, adjusting each person’s FTE value up as they work more shifts.
One more thing about productivity targets…
It’s also important to remember that productivity targets make the most sense at the group—not the individual—level. The MGMA data includes hospitalists who work night shifts (including nocturnists) and doctors who work low-production shifts (i.e., pager or ED triage shifts), as well as daytime rounding doctors. So, if you have a doctor who only works days, you would expect him to generate wRVUs in excess of the global target of wRVUs per FTE to make up for the low-productivity shifts that other doctors have to work.
For example, your practice might decide the group as a whole is expected to generate the MGMA yearly median 4,298 wRVUs per doctor, multiplied by the number of FTEs in the group. But the nocturnists would be expected to generate fewer, while those who work most or all of their shifts in a daytime rounder would be expected to generate more. So the threshold to begin paying the wRVU bonus for daytime rounding doctors might be adjusted up to something like 4,500 wRVUs.
The above example is just as an illustration, of course, and there are all kinds of reasons it might be more appropriate to choose different thresholds for your practice. But it’s a good place to start the thinking.

Hospitals' Observation Status Designation May Trigger Malpractice Claims
I’m convinced that observation status is rapidly becoming a meaningful factor in patients’ decision to file a malpractice lawsuit.
First, let me concede that I don’t know of any hard data to support my claim. I even asked the nation’s largest malpractice insurer about this, and they didn’t have any data on it. I think that is because observation status has only become a really big issue in the last couple of years, and since it typically takes several years for a malpractice suit to conclude, it just hasn’t found its way onto their radar yet.
But I’m pretty sure that will change within the next few years.
Implications
As any seasoned practitioner in our field knows, all outpatient and inpatient physician charges for Medicare patients, along with those of other licensed practitioners, are billed through Medicare Part B. After meeting a deductible, patients with traditional fee-for-service Medicare are generally responsible for 20% of all approved Part B charges, with no upper limit. For patients seen by a large number of providers while hospitalized, this 20% can really add up. Some patients have a secondary insurance that pays for this.
Hospital charges for patients on inpatient status are billed through Medicare Part A. Patients have an annual Part A deductible, and only in the case of very long inpatient stays will they have to pay more than that for inpatient care each year.
But hospital charges for patients on observation status are billed through Part B. And because hospital charges add up so quickly, the 20% of this that the patient is responsible for can be a lot of money—thousands of dollars, even for stays of less than 24 hours. Understandably, patients are not at all happy about this.
Let’s say you’re admitted overnight on observation status and your doctor orders your usual Advair inhaler. You use it once. Most hospitals aren’t able to ensure compliance with regulations around dispensing medications for home use like a pharmacy, so they won’t let you take the inhaler home. A few weeks later you’re stunned to learn that the hospital charged $10,000 for all services provided, and you’re responsible for 20% of the allowable amount PLUS the cost of all “self administered” drugs, like inhalers, eye drops, and calcitonin nasal spray. You look over your bill to see that you’re asked to pay $350 for the inhaler you used once and couldn’t even take home with you! Many self-administered medications, including eye drops and calcitonin nasal spray, result in similarly alarming charges to patients.
On top of the unpleasant surprise of a large hospital bill, Medicare won’t pay for skilled nursing facility (SNF) care for patients who are on observation status. That is, observation is not a “qualifying” stay for beneficiaries to access their SNF benefit.
It is easy to see why patients are unhappy about observation status.
The Media Message
News media are making the public aware of the potentially high financial costs they face if placed on observation status. But, too often, they oversimplify the issue, making it seem as though the choice of observation vs. inpatient status is entirely up to the treating doctor.
Saying that this decision is entirely up to the doctor is a lot like saying it is entirely up to you to determine how fast you drive on a freeway. In a sense that is correct, because no one else is in your car to control how fast you go and, in theory, you could choose to go 100 mph or 30 mph. The only problem is that it wouldn’t be long before you’d be in trouble with the law. So you don’t have complete autonomy to choose your speed; you have to comply with the laws. The same is true for doctors choosing observation status. We must comply with regulations in choosing the status or face legal consequences like fines or accusations of fraud.
Most news stories, like this one from NBC news (www.nbcnews.com/video/nightly-news/54511352#54511352) in February, are generally accurate but leave out the important fact that hospitals and doctors have little autonomy to choose the status the patient prefers. Instead, media often simply encourage patients on observation status to argue for a change to inpatient status and “be persistent.” More and more often, patients and families are arguing with the treating doctor; in many cases, that is a hospitalist.
Complaints Surge
At the 2014 SHM annual meeting last spring in Las Vegas, I spoke with many hospitalists who said that, increasingly, they are targets of observation-status complaints. One hospitalist group recently had each doctor list his or her top three frustrations with work; difficult and stressful conversations about observation status topped the list.
Patient anger regarding observation status can turn a satisfied patient into an angry one. We all know that unhappy patients are the ones most likely to pursue malpractice lawsuits. While anger over observation status doesn’t equal medical malpractice, it can change a patient’s opinion of our care, which may in some cases result in a malpractice claim.
Solutions
Medicare is unlikely to do away with observation status, so the best way to prevent complaints is to ensure that all its implications are explained to patients and families, ideally before they’re put into the hospital (e.g., while still in the ED). I think it is best if this message is delivered by someone other than the treating doctor(s): For example, a case manager might handle the discussion. Of course, patients and families are often too overwhelmed in the ED to absorb this information, so the message may need to be repeated later.
Maybe everyone should tell observation patients, “We’re going to observe you” without using any form of the word “admission.” And having these patients stay in distinct observation units probably reduces misunderstandings and complaints compared to the common practice of mixing these patients in “regular” hospital floors housing those on inpatient status.
Unfortunately, I couldn’t find research data to support this idea.
I bet some hospitals have even more elegant and effective ways to reduce misunderstandings and complaints around observation status. I’d love to hear from you if you know of any. E-mail me at john.nelson@nelsonflores.com.

I’m convinced that observation status is rapidly becoming a meaningful factor in patients’ decision to file a malpractice lawsuit.
First, let me concede that I don’t know of any hard data to support my claim. I even asked the nation’s largest malpractice insurer about this, and they didn’t have any data on it. I think that is because observation status has only become a really big issue in the last couple of years, and since it typically takes several years for a malpractice suit to conclude, it just hasn’t found its way onto their radar yet.
But I’m pretty sure that will change within the next few years.
Implications
As any seasoned practitioner in our field knows, all outpatient and inpatient physician charges for Medicare patients, along with those of other licensed practitioners, are billed through Medicare Part B. After meeting a deductible, patients with traditional fee-for-service Medicare are generally responsible for 20% of all approved Part B charges, with no upper limit. For patients seen by a large number of providers while hospitalized, this 20% can really add up. Some patients have a secondary insurance that pays for this.
Hospital charges for patients on inpatient status are billed through Medicare Part A. Patients have an annual Part A deductible, and only in the case of very long inpatient stays will they have to pay more than that for inpatient care each year.
But hospital charges for patients on observation status are billed through Part B. And because hospital charges add up so quickly, the 20% of this that the patient is responsible for can be a lot of money—thousands of dollars, even for stays of less than 24 hours. Understandably, patients are not at all happy about this.
Let’s say you’re admitted overnight on observation status and your doctor orders your usual Advair inhaler. You use it once. Most hospitals aren’t able to ensure compliance with regulations around dispensing medications for home use like a pharmacy, so they won’t let you take the inhaler home. A few weeks later you’re stunned to learn that the hospital charged $10,000 for all services provided, and you’re responsible for 20% of the allowable amount PLUS the cost of all “self administered” drugs, like inhalers, eye drops, and calcitonin nasal spray. You look over your bill to see that you’re asked to pay $350 for the inhaler you used once and couldn’t even take home with you! Many self-administered medications, including eye drops and calcitonin nasal spray, result in similarly alarming charges to patients.
On top of the unpleasant surprise of a large hospital bill, Medicare won’t pay for skilled nursing facility (SNF) care for patients who are on observation status. That is, observation is not a “qualifying” stay for beneficiaries to access their SNF benefit.
It is easy to see why patients are unhappy about observation status.
The Media Message
News media are making the public aware of the potentially high financial costs they face if placed on observation status. But, too often, they oversimplify the issue, making it seem as though the choice of observation vs. inpatient status is entirely up to the treating doctor.
Saying that this decision is entirely up to the doctor is a lot like saying it is entirely up to you to determine how fast you drive on a freeway. In a sense that is correct, because no one else is in your car to control how fast you go and, in theory, you could choose to go 100 mph or 30 mph. The only problem is that it wouldn’t be long before you’d be in trouble with the law. So you don’t have complete autonomy to choose your speed; you have to comply with the laws. The same is true for doctors choosing observation status. We must comply with regulations in choosing the status or face legal consequences like fines or accusations of fraud.
Most news stories, like this one from NBC news (www.nbcnews.com/video/nightly-news/54511352#54511352) in February, are generally accurate but leave out the important fact that hospitals and doctors have little autonomy to choose the status the patient prefers. Instead, media often simply encourage patients on observation status to argue for a change to inpatient status and “be persistent.” More and more often, patients and families are arguing with the treating doctor; in many cases, that is a hospitalist.
Complaints Surge
At the 2014 SHM annual meeting last spring in Las Vegas, I spoke with many hospitalists who said that, increasingly, they are targets of observation-status complaints. One hospitalist group recently had each doctor list his or her top three frustrations with work; difficult and stressful conversations about observation status topped the list.
Patient anger regarding observation status can turn a satisfied patient into an angry one. We all know that unhappy patients are the ones most likely to pursue malpractice lawsuits. While anger over observation status doesn’t equal medical malpractice, it can change a patient’s opinion of our care, which may in some cases result in a malpractice claim.
Solutions
Medicare is unlikely to do away with observation status, so the best way to prevent complaints is to ensure that all its implications are explained to patients and families, ideally before they’re put into the hospital (e.g., while still in the ED). I think it is best if this message is delivered by someone other than the treating doctor(s): For example, a case manager might handle the discussion. Of course, patients and families are often too overwhelmed in the ED to absorb this information, so the message may need to be repeated later.
Maybe everyone should tell observation patients, “We’re going to observe you” without using any form of the word “admission.” And having these patients stay in distinct observation units probably reduces misunderstandings and complaints compared to the common practice of mixing these patients in “regular” hospital floors housing those on inpatient status.
Unfortunately, I couldn’t find research data to support this idea.
I bet some hospitals have even more elegant and effective ways to reduce misunderstandings and complaints around observation status. I’d love to hear from you if you know of any. E-mail me at john.nelson@nelsonflores.com.

I’m convinced that observation status is rapidly becoming a meaningful factor in patients’ decision to file a malpractice lawsuit.
First, let me concede that I don’t know of any hard data to support my claim. I even asked the nation’s largest malpractice insurer about this, and they didn’t have any data on it. I think that is because observation status has only become a really big issue in the last couple of years, and since it typically takes several years for a malpractice suit to conclude, it just hasn’t found its way onto their radar yet.
But I’m pretty sure that will change within the next few years.
Implications
As any seasoned practitioner in our field knows, all outpatient and inpatient physician charges for Medicare patients, along with those of other licensed practitioners, are billed through Medicare Part B. After meeting a deductible, patients with traditional fee-for-service Medicare are generally responsible for 20% of all approved Part B charges, with no upper limit. For patients seen by a large number of providers while hospitalized, this 20% can really add up. Some patients have a secondary insurance that pays for this.
Hospital charges for patients on inpatient status are billed through Medicare Part A. Patients have an annual Part A deductible, and only in the case of very long inpatient stays will they have to pay more than that for inpatient care each year.
But hospital charges for patients on observation status are billed through Part B. And because hospital charges add up so quickly, the 20% of this that the patient is responsible for can be a lot of money—thousands of dollars, even for stays of less than 24 hours. Understandably, patients are not at all happy about this.
Let’s say you’re admitted overnight on observation status and your doctor orders your usual Advair inhaler. You use it once. Most hospitals aren’t able to ensure compliance with regulations around dispensing medications for home use like a pharmacy, so they won’t let you take the inhaler home. A few weeks later you’re stunned to learn that the hospital charged $10,000 for all services provided, and you’re responsible for 20% of the allowable amount PLUS the cost of all “self administered” drugs, like inhalers, eye drops, and calcitonin nasal spray. You look over your bill to see that you’re asked to pay $350 for the inhaler you used once and couldn’t even take home with you! Many self-administered medications, including eye drops and calcitonin nasal spray, result in similarly alarming charges to patients.
On top of the unpleasant surprise of a large hospital bill, Medicare won’t pay for skilled nursing facility (SNF) care for patients who are on observation status. That is, observation is not a “qualifying” stay for beneficiaries to access their SNF benefit.
It is easy to see why patients are unhappy about observation status.
The Media Message
News media are making the public aware of the potentially high financial costs they face if placed on observation status. But, too often, they oversimplify the issue, making it seem as though the choice of observation vs. inpatient status is entirely up to the treating doctor.
Saying that this decision is entirely up to the doctor is a lot like saying it is entirely up to you to determine how fast you drive on a freeway. In a sense that is correct, because no one else is in your car to control how fast you go and, in theory, you could choose to go 100 mph or 30 mph. The only problem is that it wouldn’t be long before you’d be in trouble with the law. So you don’t have complete autonomy to choose your speed; you have to comply with the laws. The same is true for doctors choosing observation status. We must comply with regulations in choosing the status or face legal consequences like fines or accusations of fraud.
Most news stories, like this one from NBC news (www.nbcnews.com/video/nightly-news/54511352#54511352) in February, are generally accurate but leave out the important fact that hospitals and doctors have little autonomy to choose the status the patient prefers. Instead, media often simply encourage patients on observation status to argue for a change to inpatient status and “be persistent.” More and more often, patients and families are arguing with the treating doctor; in many cases, that is a hospitalist.
Complaints Surge
At the 2014 SHM annual meeting last spring in Las Vegas, I spoke with many hospitalists who said that, increasingly, they are targets of observation-status complaints. One hospitalist group recently had each doctor list his or her top three frustrations with work; difficult and stressful conversations about observation status topped the list.
Patient anger regarding observation status can turn a satisfied patient into an angry one. We all know that unhappy patients are the ones most likely to pursue malpractice lawsuits. While anger over observation status doesn’t equal medical malpractice, it can change a patient’s opinion of our care, which may in some cases result in a malpractice claim.
Solutions
Medicare is unlikely to do away with observation status, so the best way to prevent complaints is to ensure that all its implications are explained to patients and families, ideally before they’re put into the hospital (e.g., while still in the ED). I think it is best if this message is delivered by someone other than the treating doctor(s): For example, a case manager might handle the discussion. Of course, patients and families are often too overwhelmed in the ED to absorb this information, so the message may need to be repeated later.
Maybe everyone should tell observation patients, “We’re going to observe you” without using any form of the word “admission.” And having these patients stay in distinct observation units probably reduces misunderstandings and complaints compared to the common practice of mixing these patients in “regular” hospital floors housing those on inpatient status.
Unfortunately, I couldn’t find research data to support this idea.
I bet some hospitals have even more elegant and effective ways to reduce misunderstandings and complaints around observation status. I’d love to hear from you if you know of any. E-mail me at john.nelson@nelsonflores.com.

Put Key Principles, Characteristics of Effective Hospital Medicine Groups to Work
I hope you’re already familiar with “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” [www.hospitalmedicine.org/keychar] and have spent at least a few minutes reviewing the list of 10 “principles” and 47 “characteristics” thought to be associated with effective hospital medicine groups (HMGs). (Full disclosure: I was one of the authors of the article published in February 2014 in the Journal of Hospital Medicine.) Most of us are very busy, so the temptation might be high to set the article aside and risk forgetting it. But I hope many in our field, both clinicians and administrators, will look at it more carefully. There are a number of ways you could use the guide to stimulate thinking or change in your practice.
Grading Our Specialty
I just returned from a meeting of about 10 hospitalist leaders from different organizations around the country. Attendees represented the diversity of our field, including hospital-employed HMGs, large hospitalist management companies, and academic programs. We spent a portion of the meeting discussing what grade we as a group would give the whole specialty of hospital medicine on each of the 10 “principles.” Essentially, we generated a report card for the U.S. hospitalist movement.
This wasn’t a rigorous scientific exercise; instead, it was a robust and thought-provoking discussion around what grade to assign. Opinions regarding the appropriate grade varied significantly, but a common theme was that our specialty really “owns” the importance of pursuing many or most of the principles listed in the article and is devoting time and resources to them even if many individual HMGs might have a long way to go to perform optimally.
For example, meeting attendees thought our field has for a long time worked diligently to “support care coordination across the care continuum” (Principle 6). No one thought that all HMGs do this optimally, but the consensus was that most HMGs have invested effort to do it well. And most were concerned that many HMGs still lack “adequate resources” (Principle 3) and sufficiently “engaged hospitalists” (Principle 2)—and that the former contributes to the latter.
The opinion of the hospitalist leaders who happened to attend the meeting where this conversation took place doesn’t represent the final word on how our specialty is performing, but I think all involved found value in having the conversation, hearing different perspectives about what we’re doing well and where we should focus energy and resources to improve.
Grading Your HM Group
You might want to do something similar within your own group, but make it more relevant by grading how your own practice performs on each of the 10 principles. You could do this on your own just to stimulate your thinking, or you could have each member of your HMG generate a report card of your group’s performance—then discuss where there is agreement or disagreement within the group.
You could structure this sort of individual or group assessment simply as an exercise to generate ideas and conversation about the practice, or your group could take a more formal approach and use it as part of a planning process to determine future practice management-related goals. I know of some groups that scheduled strategic planning meetings specifically to discuss which of the elements to make a priority.
Discussion Document for Leadership
In addition to using the article to generate conversation among hospitalists within your group, it can be a really valuable tool in guiding conversations with hospital leaders and the entity that employs the hospitalists. For example, you could use the article to generate or update the job description of the lead hospitalist or practice manager. Or during annual budgeting for the hospitalist practice, the guide could be used as a checklist to think about whether there are important areas that would benefit from more resources.
Of course, there is a risk that hospital leaders or those who employ the hospitalists could use the article primarily to criticize a hospitalist group and its leader for not already having excellent performance on every one of the principles and characteristics listed. That would be pretty unfortunate; there probably isn’t a single group that performs well on every domain, and the real value of the article is to “be aspirational, helping to raise the bar” for each HMG and our specialty as a whole.
And, as discussed in the article, an HMG doesn’t need to be a stellar performer on all 47 characteristics to be effective. Some of the characteristics listed in the article may not apply to all groups, so all involved in the management of any individual HMG should think about whether to set some aside when assessing their own group.
Where to Go from Here
The article is based on expert opinion, with the help of many more people than those listed as author, and I’m hopeful it will stimulate researchers to study some of these principles and characteristics. For many reasons, we will probably never have robust data, but I’d be happy for whatever we can get.
There is a pretty good chance that the evolution in the work we do and the nature of the hospital setting mean that the principles and characteristics may need to be revised periodically. I would love to know how they might be different in 10 or 20 years.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
I hope you’re already familiar with “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” [www.hospitalmedicine.org/keychar] and have spent at least a few minutes reviewing the list of 10 “principles” and 47 “characteristics” thought to be associated with effective hospital medicine groups (HMGs). (Full disclosure: I was one of the authors of the article published in February 2014 in the Journal of Hospital Medicine.) Most of us are very busy, so the temptation might be high to set the article aside and risk forgetting it. But I hope many in our field, both clinicians and administrators, will look at it more carefully. There are a number of ways you could use the guide to stimulate thinking or change in your practice.
Grading Our Specialty
I just returned from a meeting of about 10 hospitalist leaders from different organizations around the country. Attendees represented the diversity of our field, including hospital-employed HMGs, large hospitalist management companies, and academic programs. We spent a portion of the meeting discussing what grade we as a group would give the whole specialty of hospital medicine on each of the 10 “principles.” Essentially, we generated a report card for the U.S. hospitalist movement.
This wasn’t a rigorous scientific exercise; instead, it was a robust and thought-provoking discussion around what grade to assign. Opinions regarding the appropriate grade varied significantly, but a common theme was that our specialty really “owns” the importance of pursuing many or most of the principles listed in the article and is devoting time and resources to them even if many individual HMGs might have a long way to go to perform optimally.
For example, meeting attendees thought our field has for a long time worked diligently to “support care coordination across the care continuum” (Principle 6). No one thought that all HMGs do this optimally, but the consensus was that most HMGs have invested effort to do it well. And most were concerned that many HMGs still lack “adequate resources” (Principle 3) and sufficiently “engaged hospitalists” (Principle 2)—and that the former contributes to the latter.
The opinion of the hospitalist leaders who happened to attend the meeting where this conversation took place doesn’t represent the final word on how our specialty is performing, but I think all involved found value in having the conversation, hearing different perspectives about what we’re doing well and where we should focus energy and resources to improve.
Grading Your HM Group
You might want to do something similar within your own group, but make it more relevant by grading how your own practice performs on each of the 10 principles. You could do this on your own just to stimulate your thinking, or you could have each member of your HMG generate a report card of your group’s performance—then discuss where there is agreement or disagreement within the group.
You could structure this sort of individual or group assessment simply as an exercise to generate ideas and conversation about the practice, or your group could take a more formal approach and use it as part of a planning process to determine future practice management-related goals. I know of some groups that scheduled strategic planning meetings specifically to discuss which of the elements to make a priority.
Discussion Document for Leadership
In addition to using the article to generate conversation among hospitalists within your group, it can be a really valuable tool in guiding conversations with hospital leaders and the entity that employs the hospitalists. For example, you could use the article to generate or update the job description of the lead hospitalist or practice manager. Or during annual budgeting for the hospitalist practice, the guide could be used as a checklist to think about whether there are important areas that would benefit from more resources.
Of course, there is a risk that hospital leaders or those who employ the hospitalists could use the article primarily to criticize a hospitalist group and its leader for not already having excellent performance on every one of the principles and characteristics listed. That would be pretty unfortunate; there probably isn’t a single group that performs well on every domain, and the real value of the article is to “be aspirational, helping to raise the bar” for each HMG and our specialty as a whole.
And, as discussed in the article, an HMG doesn’t need to be a stellar performer on all 47 characteristics to be effective. Some of the characteristics listed in the article may not apply to all groups, so all involved in the management of any individual HMG should think about whether to set some aside when assessing their own group.
Where to Go from Here
The article is based on expert opinion, with the help of many more people than those listed as author, and I’m hopeful it will stimulate researchers to study some of these principles and characteristics. For many reasons, we will probably never have robust data, but I’d be happy for whatever we can get.
There is a pretty good chance that the evolution in the work we do and the nature of the hospital setting mean that the principles and characteristics may need to be revised periodically. I would love to know how they might be different in 10 or 20 years.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
I hope you’re already familiar with “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists” [www.hospitalmedicine.org/keychar] and have spent at least a few minutes reviewing the list of 10 “principles” and 47 “characteristics” thought to be associated with effective hospital medicine groups (HMGs). (Full disclosure: I was one of the authors of the article published in February 2014 in the Journal of Hospital Medicine.) Most of us are very busy, so the temptation might be high to set the article aside and risk forgetting it. But I hope many in our field, both clinicians and administrators, will look at it more carefully. There are a number of ways you could use the guide to stimulate thinking or change in your practice.
Grading Our Specialty
I just returned from a meeting of about 10 hospitalist leaders from different organizations around the country. Attendees represented the diversity of our field, including hospital-employed HMGs, large hospitalist management companies, and academic programs. We spent a portion of the meeting discussing what grade we as a group would give the whole specialty of hospital medicine on each of the 10 “principles.” Essentially, we generated a report card for the U.S. hospitalist movement.
This wasn’t a rigorous scientific exercise; instead, it was a robust and thought-provoking discussion around what grade to assign. Opinions regarding the appropriate grade varied significantly, but a common theme was that our specialty really “owns” the importance of pursuing many or most of the principles listed in the article and is devoting time and resources to them even if many individual HMGs might have a long way to go to perform optimally.
For example, meeting attendees thought our field has for a long time worked diligently to “support care coordination across the care continuum” (Principle 6). No one thought that all HMGs do this optimally, but the consensus was that most HMGs have invested effort to do it well. And most were concerned that many HMGs still lack “adequate resources” (Principle 3) and sufficiently “engaged hospitalists” (Principle 2)—and that the former contributes to the latter.
The opinion of the hospitalist leaders who happened to attend the meeting where this conversation took place doesn’t represent the final word on how our specialty is performing, but I think all involved found value in having the conversation, hearing different perspectives about what we’re doing well and where we should focus energy and resources to improve.
Grading Your HM Group
You might want to do something similar within your own group, but make it more relevant by grading how your own practice performs on each of the 10 principles. You could do this on your own just to stimulate your thinking, or you could have each member of your HMG generate a report card of your group’s performance—then discuss where there is agreement or disagreement within the group.
You could structure this sort of individual or group assessment simply as an exercise to generate ideas and conversation about the practice, or your group could take a more formal approach and use it as part of a planning process to determine future practice management-related goals. I know of some groups that scheduled strategic planning meetings specifically to discuss which of the elements to make a priority.
Discussion Document for Leadership
In addition to using the article to generate conversation among hospitalists within your group, it can be a really valuable tool in guiding conversations with hospital leaders and the entity that employs the hospitalists. For example, you could use the article to generate or update the job description of the lead hospitalist or practice manager. Or during annual budgeting for the hospitalist practice, the guide could be used as a checklist to think about whether there are important areas that would benefit from more resources.
Of course, there is a risk that hospital leaders or those who employ the hospitalists could use the article primarily to criticize a hospitalist group and its leader for not already having excellent performance on every one of the principles and characteristics listed. That would be pretty unfortunate; there probably isn’t a single group that performs well on every domain, and the real value of the article is to “be aspirational, helping to raise the bar” for each HMG and our specialty as a whole.
And, as discussed in the article, an HMG doesn’t need to be a stellar performer on all 47 characteristics to be effective. Some of the characteristics listed in the article may not apply to all groups, so all involved in the management of any individual HMG should think about whether to set some aside when assessing their own group.
Where to Go from Here
The article is based on expert opinion, with the help of many more people than those listed as author, and I’m hopeful it will stimulate researchers to study some of these principles and characteristics. For many reasons, we will probably never have robust data, but I’d be happy for whatever we can get.
There is a pretty good chance that the evolution in the work we do and the nature of the hospital setting mean that the principles and characteristics may need to be revised periodically. I would love to know how they might be different in 10 or 20 years.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Proper Inpatient Documentation, Coding Essential to Avoid a Medicare Audit
Several years ago we sent a CPT coding auditor 15 chart notes generated by each doctor in our group. Among each doctors’ 15 notes were at least one or two billed as initial hospital care, follow up, discharge, critical care, and so on. This coding expert returned a report showing that, out of all the notes reviewed, a significant portion were not billed at the correct level. Most of the incorrectly billed notes were judged to reflect “up-coding,” and a few were seen as “down-coded.”
This was distressing and hard to believe.
So I took the same set of notes and paid a second coding expert for an independent review. She didn’t know about the first audit but returned a report that showed a nearly identical portion of incorrectly coded notes.
Two independent audits showing nearly the same portion of notes coded incorrectly was alarming. But it was difficult for my partners and me to address, because the auditors didn’t agree on the correct code for many of the notes. In some cases, both flagged a note as incorrectly coded but didn’t agree on the correct code. For a number of the notes, one auditor said the visit was “up-coded,” while the other said it was “down-coded.” There was so little agreement between the two of them that we had a hard time coming up with any firm conclusions about what we should do to improve our performance.
If experts who think about coding all the time can’t agree on the right code for a given note, how can hospitalists be expected to code nearly all of our visits accurately?
RAC: Recovery Audit Contractor
Despite what I believe is poor inter-rater reliability among coding auditors, we need to work diligently to comply with coding guidelines. A 2003 Federal law mandated a program of Recovery Audit Contractors, or RAC for short, to find cases of “up-coding” or other overbilling and require the provider to repay any resulting loss.
A number of companies are in the business of conducting RAC audits (one of them, CGI, is the Canadian company blamed for the failed “Obamacare” exchange websites), and there is a reasonable chance one of these companies has reviewed some of your charges—or those of your hospitalist colleagues.
The RAC auditors review information about your charges, and if they determine that you up-coded or overbilled, they send a “demand letter” summarizing their findings, along with the amount of money they have determined you should pay back. (Theoretically, they could notify you of “under-coding,” so that you can be paid more for past work, but I haven’t yet come across an example of that.)
It is common to appeal the RAC findings, but that can be a long process, and many organizations decide to pay back all the money requested by the RAC as quickly as possible to avoid paying interest on a delayed payment if the appeal is unsuccessful. In the case of a successful appeal, the money previously refunded by the doctor would be returned.
Page 338 of the CMS Fiscal Year 2015 “Justification of Estimates for Appropriations Committees” says that “…about 50 percent of the estimated 43,000 appeals [of adverse RAC audit findings] were fully or partially overturned…” This could mean the RACs are a sort of loose cannon, accusing many providers of overbilling while knowing that some won’t bother to appeal because they don’t understand the process or because the dollar amount involved for a single provider is too small to justify the time and expense of conducting the appeal. In this way, a RAC audit is like the $15 rebate on the last electronic gadget you bought. The seller knows that many people, including me, will fail to do the work required to claim the rebate.
Accuracy Strategies
There are a number of ways to help your group ensure appropriate CPT coding and reduce the chance a RAC will ask for money back.
Education. There are many ways to help providers in your practice understand the elements of documentation and coding. Periodic training classes (e.g. during orientation and annually thereafter) are useful but may not be enough. For me, this is a little like learning a foreign language by going to a couple of classes. Instead, I think “immersion training” is more effective. That might mean a doctor spends a few minutes with a certified coder on most working days for a few weeks. For example, they could meet for 15 minutes near lunchtime and review how the doctor plans to bill visits made that morning. Lastly, consider targeted education for each doctor, based on any problems found in an audit of his/her coding.
Review coding patterns. As I wrote in my August 2007 column, there is value in ensuring that each doctor in the group can see how her coding pattern differs from the group as a whole or any individual in the group. That is, what portion of follow-up visits was billed at the lowest, middle, and highest levels? What about admissions, discharges, and so on? I provided a sample report in that same column.
It also is worth taking the time to compare each doctor’s coding pattern to both the CMS Internal Medicine data and SHM’s State of Hospital Medicine report. The accompanying figure shows the most current data sets available.
Keep in mind that the goal is not to simply ensure that your coding pattern matches these external data sets; knowing where yours differs from these sets can suggest where you might want to investigate further or seek additional education.
Coding audits. Having a certified coder audit your performance at least annually is a good idea. It can help uncover areas in which you’d benefit from further review and training, and if, heaven forbid, questions are ever raised about whether you’re intentionally up-coding (fraud), showing that you’re audited regularly could help demonstrate your efforts to code correctly. In the latter case, it is probably more valuable if the audit is done independently of your employer.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Several years ago we sent a CPT coding auditor 15 chart notes generated by each doctor in our group. Among each doctors’ 15 notes were at least one or two billed as initial hospital care, follow up, discharge, critical care, and so on. This coding expert returned a report showing that, out of all the notes reviewed, a significant portion were not billed at the correct level. Most of the incorrectly billed notes were judged to reflect “up-coding,” and a few were seen as “down-coded.”
This was distressing and hard to believe.
So I took the same set of notes and paid a second coding expert for an independent review. She didn’t know about the first audit but returned a report that showed a nearly identical portion of incorrectly coded notes.
Two independent audits showing nearly the same portion of notes coded incorrectly was alarming. But it was difficult for my partners and me to address, because the auditors didn’t agree on the correct code for many of the notes. In some cases, both flagged a note as incorrectly coded but didn’t agree on the correct code. For a number of the notes, one auditor said the visit was “up-coded,” while the other said it was “down-coded.” There was so little agreement between the two of them that we had a hard time coming up with any firm conclusions about what we should do to improve our performance.
If experts who think about coding all the time can’t agree on the right code for a given note, how can hospitalists be expected to code nearly all of our visits accurately?
RAC: Recovery Audit Contractor
Despite what I believe is poor inter-rater reliability among coding auditors, we need to work diligently to comply with coding guidelines. A 2003 Federal law mandated a program of Recovery Audit Contractors, or RAC for short, to find cases of “up-coding” or other overbilling and require the provider to repay any resulting loss.
A number of companies are in the business of conducting RAC audits (one of them, CGI, is the Canadian company blamed for the failed “Obamacare” exchange websites), and there is a reasonable chance one of these companies has reviewed some of your charges—or those of your hospitalist colleagues.
The RAC auditors review information about your charges, and if they determine that you up-coded or overbilled, they send a “demand letter” summarizing their findings, along with the amount of money they have determined you should pay back. (Theoretically, they could notify you of “under-coding,” so that you can be paid more for past work, but I haven’t yet come across an example of that.)
It is common to appeal the RAC findings, but that can be a long process, and many organizations decide to pay back all the money requested by the RAC as quickly as possible to avoid paying interest on a delayed payment if the appeal is unsuccessful. In the case of a successful appeal, the money previously refunded by the doctor would be returned.
Page 338 of the CMS Fiscal Year 2015 “Justification of Estimates for Appropriations Committees” says that “…about 50 percent of the estimated 43,000 appeals [of adverse RAC audit findings] were fully or partially overturned…” This could mean the RACs are a sort of loose cannon, accusing many providers of overbilling while knowing that some won’t bother to appeal because they don’t understand the process or because the dollar amount involved for a single provider is too small to justify the time and expense of conducting the appeal. In this way, a RAC audit is like the $15 rebate on the last electronic gadget you bought. The seller knows that many people, including me, will fail to do the work required to claim the rebate.
Accuracy Strategies
There are a number of ways to help your group ensure appropriate CPT coding and reduce the chance a RAC will ask for money back.
Education. There are many ways to help providers in your practice understand the elements of documentation and coding. Periodic training classes (e.g. during orientation and annually thereafter) are useful but may not be enough. For me, this is a little like learning a foreign language by going to a couple of classes. Instead, I think “immersion training” is more effective. That might mean a doctor spends a few minutes with a certified coder on most working days for a few weeks. For example, they could meet for 15 minutes near lunchtime and review how the doctor plans to bill visits made that morning. Lastly, consider targeted education for each doctor, based on any problems found in an audit of his/her coding.
Review coding patterns. As I wrote in my August 2007 column, there is value in ensuring that each doctor in the group can see how her coding pattern differs from the group as a whole or any individual in the group. That is, what portion of follow-up visits was billed at the lowest, middle, and highest levels? What about admissions, discharges, and so on? I provided a sample report in that same column.
It also is worth taking the time to compare each doctor’s coding pattern to both the CMS Internal Medicine data and SHM’s State of Hospital Medicine report. The accompanying figure shows the most current data sets available.
Keep in mind that the goal is not to simply ensure that your coding pattern matches these external data sets; knowing where yours differs from these sets can suggest where you might want to investigate further or seek additional education.
Coding audits. Having a certified coder audit your performance at least annually is a good idea. It can help uncover areas in which you’d benefit from further review and training, and if, heaven forbid, questions are ever raised about whether you’re intentionally up-coding (fraud), showing that you’re audited regularly could help demonstrate your efforts to code correctly. In the latter case, it is probably more valuable if the audit is done independently of your employer.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Several years ago we sent a CPT coding auditor 15 chart notes generated by each doctor in our group. Among each doctors’ 15 notes were at least one or two billed as initial hospital care, follow up, discharge, critical care, and so on. This coding expert returned a report showing that, out of all the notes reviewed, a significant portion were not billed at the correct level. Most of the incorrectly billed notes were judged to reflect “up-coding,” and a few were seen as “down-coded.”
This was distressing and hard to believe.
So I took the same set of notes and paid a second coding expert for an independent review. She didn’t know about the first audit but returned a report that showed a nearly identical portion of incorrectly coded notes.
Two independent audits showing nearly the same portion of notes coded incorrectly was alarming. But it was difficult for my partners and me to address, because the auditors didn’t agree on the correct code for many of the notes. In some cases, both flagged a note as incorrectly coded but didn’t agree on the correct code. For a number of the notes, one auditor said the visit was “up-coded,” while the other said it was “down-coded.” There was so little agreement between the two of them that we had a hard time coming up with any firm conclusions about what we should do to improve our performance.
If experts who think about coding all the time can’t agree on the right code for a given note, how can hospitalists be expected to code nearly all of our visits accurately?
RAC: Recovery Audit Contractor
Despite what I believe is poor inter-rater reliability among coding auditors, we need to work diligently to comply with coding guidelines. A 2003 Federal law mandated a program of Recovery Audit Contractors, or RAC for short, to find cases of “up-coding” or other overbilling and require the provider to repay any resulting loss.
A number of companies are in the business of conducting RAC audits (one of them, CGI, is the Canadian company blamed for the failed “Obamacare” exchange websites), and there is a reasonable chance one of these companies has reviewed some of your charges—or those of your hospitalist colleagues.
The RAC auditors review information about your charges, and if they determine that you up-coded or overbilled, they send a “demand letter” summarizing their findings, along with the amount of money they have determined you should pay back. (Theoretically, they could notify you of “under-coding,” so that you can be paid more for past work, but I haven’t yet come across an example of that.)
It is common to appeal the RAC findings, but that can be a long process, and many organizations decide to pay back all the money requested by the RAC as quickly as possible to avoid paying interest on a delayed payment if the appeal is unsuccessful. In the case of a successful appeal, the money previously refunded by the doctor would be returned.
Page 338 of the CMS Fiscal Year 2015 “Justification of Estimates for Appropriations Committees” says that “…about 50 percent of the estimated 43,000 appeals [of adverse RAC audit findings] were fully or partially overturned…” This could mean the RACs are a sort of loose cannon, accusing many providers of overbilling while knowing that some won’t bother to appeal because they don’t understand the process or because the dollar amount involved for a single provider is too small to justify the time and expense of conducting the appeal. In this way, a RAC audit is like the $15 rebate on the last electronic gadget you bought. The seller knows that many people, including me, will fail to do the work required to claim the rebate.
Accuracy Strategies
There are a number of ways to help your group ensure appropriate CPT coding and reduce the chance a RAC will ask for money back.
Education. There are many ways to help providers in your practice understand the elements of documentation and coding. Periodic training classes (e.g. during orientation and annually thereafter) are useful but may not be enough. For me, this is a little like learning a foreign language by going to a couple of classes. Instead, I think “immersion training” is more effective. That might mean a doctor spends a few minutes with a certified coder on most working days for a few weeks. For example, they could meet for 15 minutes near lunchtime and review how the doctor plans to bill visits made that morning. Lastly, consider targeted education for each doctor, based on any problems found in an audit of his/her coding.
Review coding patterns. As I wrote in my August 2007 column, there is value in ensuring that each doctor in the group can see how her coding pattern differs from the group as a whole or any individual in the group. That is, what portion of follow-up visits was billed at the lowest, middle, and highest levels? What about admissions, discharges, and so on? I provided a sample report in that same column.
It also is worth taking the time to compare each doctor’s coding pattern to both the CMS Internal Medicine data and SHM’s State of Hospital Medicine report. The accompanying figure shows the most current data sets available.
Keep in mind that the goal is not to simply ensure that your coding pattern matches these external data sets; knowing where yours differs from these sets can suggest where you might want to investigate further or seek additional education.
Coding audits. Having a certified coder audit your performance at least annually is a good idea. It can help uncover areas in which you’d benefit from further review and training, and if, heaven forbid, questions are ever raised about whether you’re intentionally up-coding (fraud), showing that you’re audited regularly could help demonstrate your efforts to code correctly. In the latter case, it is probably more valuable if the audit is done independently of your employer.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Hospitalists Working Hard to Improve Patient Care
Dear Ms. Bernstein:
I’m writing this letter to let you know about some of the things happening in hospital medicine, to ensure we are always improving the care we provide.
While we talked on New Year’s Eve, you reluctantly told me that you and many of your friends were not happy with the move toward hospital care being provided by hospitalists, rather than the PCP you know. I didn’t respond because we were having a nice lunch and I didn’t want to distract you from praising my kids and talking about your grandbaby and her sibling on the way. So I thought I’d respond by writing this open letter to you on the chance it might also be thought provoking for some of my hospitalist colleagues.
I think your reluctance to share with me the unflattering opinion you and many of your friends have of the hospitalist model of care stemmed from a desire not to offend me rather than any uncertainty in your conclusion. It isn’t difficult to find others, both healthcare providers and consumers, who share your opinion.
As I’ve told you before, outside of my own parents, you and Mr. B. are among the people who had the most influence on my upbringing, and your opinion still matters to me. So I’m writing this hoping to change your view, at least a little.
Updated Numbers of Hospitalists
Our field is now larger than many other specialties, and we are experiencing ever-increasing pressure to “get it right.” A 2012 survey of hospitals conducted by the American Hospital Association found more than 38,000 doctors who identify themselves as hospitalists. This number has been increasing rapidly for more than a decade. The Society of Hospital Medicine (SHM) estimates that the number has grown to more than 44,000 in 2014, and that there are hospitalists in 72% of U.S. hospitals—90% at hospitals with over 200 beds. In 1996, there were fewer than 1,000 hospitalists.
The rapid growth in our field has brought challenges, and we’re lucky to have attracted many dedicated and talented people who are helping all of us make strides to do better, both by providing better technical care (e.g. ensuring careful assessments and ordering the best tests and treatments) and by doing so in a way that ensures patients and their families are highly satisfied.
Tools to Support Ongoing Improvements in Hospitalist Practice
There are many outlets hospitalists can turn to for education on essentially any aspect of their practice. Several years ago, the SHM published “The Core Competencies in Hospital Medicine: A Framework for Curriculum Development,” a publication that continues to be valuable in guiding hospitalists’ professional scope of clinical skills as well as educational curricula for training programs and continuing education. SHM and other organizations generate a great deal of educational content for hospitalists, which is available in many forms, including in-person conferences, webinars, and written materials. And there are several scientific journals that have significant content for hospitalists, including SHM’s own Journal of Hospital Medicine.
Our field encourages and recognizes ongoing commitment to hospitalists’ growth and development in a number of ways. When it is time for a doctor to renew his/her board certification, the American Board of Internal Medicine (ABIM) offers the option to pursue “Focused Practice in Hospital Medicine.” And SHM’s designation of Fellow, Senior Fellow and Master in Hospital Medicine recognizes those who have “demonstrated a commitment to hospital medicine, system change, and quality improvement principles.” Many in our field have achieved one or both of these distinctions, and countless others are pursuing them now.
Through its foundation, the ABIM developed a campaign known as “Choosing Wisely” to “promote conversations between physicians and patients by helping patients choose care that is: supported by evidence, not duplicative of other tests or procedures already received, free from harm, and truly necessary.” SHM joined in this effort by developing separate criteria for hospitalists who care for adults or children.
New Tool Encourages High Performance
In February, an SHM workgroup published “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists,” a document meant to serve as a road map for hospitalist groups to follow to improve their performance. I’m particularly interested in this, since I have spent much of my career thinking about and working with hospitalist groups to improve the way they perform, and I helped develop the characteristics and co-authored the document. But the real value of the document comes from the input of hundreds of people within and outside of SHM who provided thoughtful advice and feedback to identify those attributes of hospitalist groups that are most likely to ensure success.
The document describes 47 characteristics grouped into 10 different categories (“principles”). Some of the principles that you as a patient might be most interested in are ones specifying that a hospitalist group:
— Implements a practice model that is patient- and family-centered, is team-based, and emphasizes care coordination and effective communication.
— Supports care coordination across care settings; and
— Plays a leadership role in addressing key clinical issues in the hospital and/or health system: teaching, quality, safety, efficiency, and the patient/family experience.
Current State of Hospital Medicine
If you’ve had a less than satisfactory experience with care by a hospitalist, the things I’ve described here might not improve your opinion of hospitalists, or that of your friends. But maybe you can take some measure of comfort in knowing that our field as a whole is working hard to continuously improve all aspects of what we do. We’re serious about being good at what we do.
And, since this is published in a magazine read by hospitalists, maybe some of them will be reminded of the many ways our field encourages, supports, and recognizes their professional development.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Dear Ms. Bernstein:
I’m writing this letter to let you know about some of the things happening in hospital medicine, to ensure we are always improving the care we provide.
While we talked on New Year’s Eve, you reluctantly told me that you and many of your friends were not happy with the move toward hospital care being provided by hospitalists, rather than the PCP you know. I didn’t respond because we were having a nice lunch and I didn’t want to distract you from praising my kids and talking about your grandbaby and her sibling on the way. So I thought I’d respond by writing this open letter to you on the chance it might also be thought provoking for some of my hospitalist colleagues.
I think your reluctance to share with me the unflattering opinion you and many of your friends have of the hospitalist model of care stemmed from a desire not to offend me rather than any uncertainty in your conclusion. It isn’t difficult to find others, both healthcare providers and consumers, who share your opinion.
As I’ve told you before, outside of my own parents, you and Mr. B. are among the people who had the most influence on my upbringing, and your opinion still matters to me. So I’m writing this hoping to change your view, at least a little.
Updated Numbers of Hospitalists
Our field is now larger than many other specialties, and we are experiencing ever-increasing pressure to “get it right.” A 2012 survey of hospitals conducted by the American Hospital Association found more than 38,000 doctors who identify themselves as hospitalists. This number has been increasing rapidly for more than a decade. The Society of Hospital Medicine (SHM) estimates that the number has grown to more than 44,000 in 2014, and that there are hospitalists in 72% of U.S. hospitals—90% at hospitals with over 200 beds. In 1996, there were fewer than 1,000 hospitalists.
The rapid growth in our field has brought challenges, and we’re lucky to have attracted many dedicated and talented people who are helping all of us make strides to do better, both by providing better technical care (e.g. ensuring careful assessments and ordering the best tests and treatments) and by doing so in a way that ensures patients and their families are highly satisfied.
Tools to Support Ongoing Improvements in Hospitalist Practice
There are many outlets hospitalists can turn to for education on essentially any aspect of their practice. Several years ago, the SHM published “The Core Competencies in Hospital Medicine: A Framework for Curriculum Development,” a publication that continues to be valuable in guiding hospitalists’ professional scope of clinical skills as well as educational curricula for training programs and continuing education. SHM and other organizations generate a great deal of educational content for hospitalists, which is available in many forms, including in-person conferences, webinars, and written materials. And there are several scientific journals that have significant content for hospitalists, including SHM’s own Journal of Hospital Medicine.
Our field encourages and recognizes ongoing commitment to hospitalists’ growth and development in a number of ways. When it is time for a doctor to renew his/her board certification, the American Board of Internal Medicine (ABIM) offers the option to pursue “Focused Practice in Hospital Medicine.” And SHM’s designation of Fellow, Senior Fellow and Master in Hospital Medicine recognizes those who have “demonstrated a commitment to hospital medicine, system change, and quality improvement principles.” Many in our field have achieved one or both of these distinctions, and countless others are pursuing them now.
Through its foundation, the ABIM developed a campaign known as “Choosing Wisely” to “promote conversations between physicians and patients by helping patients choose care that is: supported by evidence, not duplicative of other tests or procedures already received, free from harm, and truly necessary.” SHM joined in this effort by developing separate criteria for hospitalists who care for adults or children.
New Tool Encourages High Performance
In February, an SHM workgroup published “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists,” a document meant to serve as a road map for hospitalist groups to follow to improve their performance. I’m particularly interested in this, since I have spent much of my career thinking about and working with hospitalist groups to improve the way they perform, and I helped develop the characteristics and co-authored the document. But the real value of the document comes from the input of hundreds of people within and outside of SHM who provided thoughtful advice and feedback to identify those attributes of hospitalist groups that are most likely to ensure success.
The document describes 47 characteristics grouped into 10 different categories (“principles”). Some of the principles that you as a patient might be most interested in are ones specifying that a hospitalist group:
— Implements a practice model that is patient- and family-centered, is team-based, and emphasizes care coordination and effective communication.
— Supports care coordination across care settings; and
— Plays a leadership role in addressing key clinical issues in the hospital and/or health system: teaching, quality, safety, efficiency, and the patient/family experience.
Current State of Hospital Medicine
If you’ve had a less than satisfactory experience with care by a hospitalist, the things I’ve described here might not improve your opinion of hospitalists, or that of your friends. But maybe you can take some measure of comfort in knowing that our field as a whole is working hard to continuously improve all aspects of what we do. We’re serious about being good at what we do.
And, since this is published in a magazine read by hospitalists, maybe some of them will be reminded of the many ways our field encourages, supports, and recognizes their professional development.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Dear Ms. Bernstein:
I’m writing this letter to let you know about some of the things happening in hospital medicine, to ensure we are always improving the care we provide.
While we talked on New Year’s Eve, you reluctantly told me that you and many of your friends were not happy with the move toward hospital care being provided by hospitalists, rather than the PCP you know. I didn’t respond because we were having a nice lunch and I didn’t want to distract you from praising my kids and talking about your grandbaby and her sibling on the way. So I thought I’d respond by writing this open letter to you on the chance it might also be thought provoking for some of my hospitalist colleagues.
I think your reluctance to share with me the unflattering opinion you and many of your friends have of the hospitalist model of care stemmed from a desire not to offend me rather than any uncertainty in your conclusion. It isn’t difficult to find others, both healthcare providers and consumers, who share your opinion.
As I’ve told you before, outside of my own parents, you and Mr. B. are among the people who had the most influence on my upbringing, and your opinion still matters to me. So I’m writing this hoping to change your view, at least a little.
Updated Numbers of Hospitalists
Our field is now larger than many other specialties, and we are experiencing ever-increasing pressure to “get it right.” A 2012 survey of hospitals conducted by the American Hospital Association found more than 38,000 doctors who identify themselves as hospitalists. This number has been increasing rapidly for more than a decade. The Society of Hospital Medicine (SHM) estimates that the number has grown to more than 44,000 in 2014, and that there are hospitalists in 72% of U.S. hospitals—90% at hospitals with over 200 beds. In 1996, there were fewer than 1,000 hospitalists.
The rapid growth in our field has brought challenges, and we’re lucky to have attracted many dedicated and talented people who are helping all of us make strides to do better, both by providing better technical care (e.g. ensuring careful assessments and ordering the best tests and treatments) and by doing so in a way that ensures patients and their families are highly satisfied.
Tools to Support Ongoing Improvements in Hospitalist Practice
There are many outlets hospitalists can turn to for education on essentially any aspect of their practice. Several years ago, the SHM published “The Core Competencies in Hospital Medicine: A Framework for Curriculum Development,” a publication that continues to be valuable in guiding hospitalists’ professional scope of clinical skills as well as educational curricula for training programs and continuing education. SHM and other organizations generate a great deal of educational content for hospitalists, which is available in many forms, including in-person conferences, webinars, and written materials. And there are several scientific journals that have significant content for hospitalists, including SHM’s own Journal of Hospital Medicine.
Our field encourages and recognizes ongoing commitment to hospitalists’ growth and development in a number of ways. When it is time for a doctor to renew his/her board certification, the American Board of Internal Medicine (ABIM) offers the option to pursue “Focused Practice in Hospital Medicine.” And SHM’s designation of Fellow, Senior Fellow and Master in Hospital Medicine recognizes those who have “demonstrated a commitment to hospital medicine, system change, and quality improvement principles.” Many in our field have achieved one or both of these distinctions, and countless others are pursuing them now.
Through its foundation, the ABIM developed a campaign known as “Choosing Wisely” to “promote conversations between physicians and patients by helping patients choose care that is: supported by evidence, not duplicative of other tests or procedures already received, free from harm, and truly necessary.” SHM joined in this effort by developing separate criteria for hospitalists who care for adults or children.
New Tool Encourages High Performance
In February, an SHM workgroup published “The Key Principles and Characteristics of an Effective Hospital Medicine Group: An Assessment Guide for Hospitals and Hospitalists,” a document meant to serve as a road map for hospitalist groups to follow to improve their performance. I’m particularly interested in this, since I have spent much of my career thinking about and working with hospitalist groups to improve the way they perform, and I helped develop the characteristics and co-authored the document. But the real value of the document comes from the input of hundreds of people within and outside of SHM who provided thoughtful advice and feedback to identify those attributes of hospitalist groups that are most likely to ensure success.
The document describes 47 characteristics grouped into 10 different categories (“principles”). Some of the principles that you as a patient might be most interested in are ones specifying that a hospitalist group:
— Implements a practice model that is patient- and family-centered, is team-based, and emphasizes care coordination and effective communication.
— Supports care coordination across care settings; and
— Plays a leadership role in addressing key clinical issues in the hospital and/or health system: teaching, quality, safety, efficiency, and the patient/family experience.
Current State of Hospital Medicine
If you’ve had a less than satisfactory experience with care by a hospitalist, the things I’ve described here might not improve your opinion of hospitalists, or that of your friends. But maybe you can take some measure of comfort in knowing that our field as a whole is working hard to continuously improve all aspects of what we do. We’re serious about being good at what we do.
And, since this is published in a magazine read by hospitalists, maybe some of them will be reminded of the many ways our field encourages, supports, and recognizes their professional development.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Problem Solving In Multi-Site Hospital Medicine Groups
Serving as the lead physician for a hospital medicine group (HMG) makes for challenging work. And the challenges and complexity only increase for anyone who serves as the physician leader for multiple practice sites in the same hospital system. In my November 2013 column on multi-site HMG leaders, I listed a few of the tricky issues they face and will mention a few more here.
Large-Small Friction
Unfortunately, tension between hospitalists at the big hospital and doctors at the small, “feeder” hospitals seems pretty common, and I think it’s due largely to high stress and a wide variation in workload, neither of which are in our direct control. At facilities where there is significant tension, I’m impressed by how vigorously the hospitalists at both the small and large hospitals argue that their own site faces the most stress and challenges. (This is a little like the endless debate about who works harder, those who work with residents and those who don’t.)
The hospitalists at the small site point out that they work with little or no subspecialty help and might even have to take night call from home while working during the day. Those at the big hospital say they are the ones with the very large scope of clinical practice and that, rather than making their life easier, the presence of lots of subspecialists makes for additional work coordinating care and communicating with all parties.
Where it exists, this tension is most evident during a transfer from one of the small hospitals to the large one. After all, one of the reasons to form a system of hospitals is so that nearly all patient needs can be met at one of the facilities in the system. Yet, for many reasons, the hospitalists at the large hospital are—sometimes—not as receptive to transfers as might be ideal. They might be short staffed or facing a high census or an unusually high number of admissions from their own ED. Or, perhaps, they’re concerned that the subspecialty services for which the patient is being transferred (e.g. to be scoped by a GI doctor) won’t be as helpful or prompt as needed. Or maybe they’ve felt “burned” by their colleagues at the small hospital for past transfers that didn’t seem necessary.
The result can be that the doctors at the smaller hospital complain that the “mother ship” hospitalists often are unfriendly and unreceptive to transfer requests. Although there may not be a definitive “cure” for this issue, there are several ways to help address the problem.
- In my last column, I mentioned the value of one or more in-person meetings between those who tend to be on the sending and receiving end of transfers, to establish some criteria regarding transfers that are appropriate and review the process of requesting a transfer and making the associated arrangements. In most cases there will be value in the parties meeting routinely—perhaps two to four times annually—to review how the system is working and address any difficulties.
- Periodic social meetings among the hospitalists at each site will help to form relationships that can make it less likely that any conversation about transfers will go in an unhelpful direction. Things can be very different when the people on each end of the phone call know each other personally.
- Record the phone calls between those seeking and accepting/declining each transfer. Scott Rissmiller, MD, the lead hospitalist for the 17 practice sites in Carolinas Healthcare, has said that having underperforming doctors listen to recordings of their phone calls about transfers has, in most cases he’s been involved with, proven to be a very effective way to encourage improvement.
Shared Staffing
The small hospitals in many systems sometimes struggle to find a way to provide economical night coverage. Hospitals below a certain size find it very difficult to justify a separate, in-house night provider. Some hospital systems have had success sharing night staffing, with the large hospital’s night hospitalist, nurse practitioner, or physician assistant providing telephone coverage for “cross cover” issues that arise after hours.
For example, when a nurse at the small hospital needs to contact a night hospitalist, staff will page the provider at the big hospital, and, in many cases, the issue can be managed effectively by phone. This works best when both hospitals are on the same electronic medical record, so that the responding provider can look through the record as needed.
The hospitalist at the small hospital typically stays on back-up call and is contacted if bedside attention is required.
Or, if the large and small hospitals are a short drive apart, the night hospitalist at the large facility might make the short drive to the small hospital when needed. In the case of emergencies (i.e., a code blue), the in-house night ED physician is relied on as the first responder.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Serving as the lead physician for a hospital medicine group (HMG) makes for challenging work. And the challenges and complexity only increase for anyone who serves as the physician leader for multiple practice sites in the same hospital system. In my November 2013 column on multi-site HMG leaders, I listed a few of the tricky issues they face and will mention a few more here.
Large-Small Friction
Unfortunately, tension between hospitalists at the big hospital and doctors at the small, “feeder” hospitals seems pretty common, and I think it’s due largely to high stress and a wide variation in workload, neither of which are in our direct control. At facilities where there is significant tension, I’m impressed by how vigorously the hospitalists at both the small and large hospitals argue that their own site faces the most stress and challenges. (This is a little like the endless debate about who works harder, those who work with residents and those who don’t.)
The hospitalists at the small site point out that they work with little or no subspecialty help and might even have to take night call from home while working during the day. Those at the big hospital say they are the ones with the very large scope of clinical practice and that, rather than making their life easier, the presence of lots of subspecialists makes for additional work coordinating care and communicating with all parties.
Where it exists, this tension is most evident during a transfer from one of the small hospitals to the large one. After all, one of the reasons to form a system of hospitals is so that nearly all patient needs can be met at one of the facilities in the system. Yet, for many reasons, the hospitalists at the large hospital are—sometimes—not as receptive to transfers as might be ideal. They might be short staffed or facing a high census or an unusually high number of admissions from their own ED. Or, perhaps, they’re concerned that the subspecialty services for which the patient is being transferred (e.g. to be scoped by a GI doctor) won’t be as helpful or prompt as needed. Or maybe they’ve felt “burned” by their colleagues at the small hospital for past transfers that didn’t seem necessary.
The result can be that the doctors at the smaller hospital complain that the “mother ship” hospitalists often are unfriendly and unreceptive to transfer requests. Although there may not be a definitive “cure” for this issue, there are several ways to help address the problem.
- In my last column, I mentioned the value of one or more in-person meetings between those who tend to be on the sending and receiving end of transfers, to establish some criteria regarding transfers that are appropriate and review the process of requesting a transfer and making the associated arrangements. In most cases there will be value in the parties meeting routinely—perhaps two to four times annually—to review how the system is working and address any difficulties.
- Periodic social meetings among the hospitalists at each site will help to form relationships that can make it less likely that any conversation about transfers will go in an unhelpful direction. Things can be very different when the people on each end of the phone call know each other personally.
- Record the phone calls between those seeking and accepting/declining each transfer. Scott Rissmiller, MD, the lead hospitalist for the 17 practice sites in Carolinas Healthcare, has said that having underperforming doctors listen to recordings of their phone calls about transfers has, in most cases he’s been involved with, proven to be a very effective way to encourage improvement.
Shared Staffing
The small hospitals in many systems sometimes struggle to find a way to provide economical night coverage. Hospitals below a certain size find it very difficult to justify a separate, in-house night provider. Some hospital systems have had success sharing night staffing, with the large hospital’s night hospitalist, nurse practitioner, or physician assistant providing telephone coverage for “cross cover” issues that arise after hours.
For example, when a nurse at the small hospital needs to contact a night hospitalist, staff will page the provider at the big hospital, and, in many cases, the issue can be managed effectively by phone. This works best when both hospitals are on the same electronic medical record, so that the responding provider can look through the record as needed.
The hospitalist at the small hospital typically stays on back-up call and is contacted if bedside attention is required.
Or, if the large and small hospitals are a short drive apart, the night hospitalist at the large facility might make the short drive to the small hospital when needed. In the case of emergencies (i.e., a code blue), the in-house night ED physician is relied on as the first responder.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Serving as the lead physician for a hospital medicine group (HMG) makes for challenging work. And the challenges and complexity only increase for anyone who serves as the physician leader for multiple practice sites in the same hospital system. In my November 2013 column on multi-site HMG leaders, I listed a few of the tricky issues they face and will mention a few more here.
Large-Small Friction
Unfortunately, tension between hospitalists at the big hospital and doctors at the small, “feeder” hospitals seems pretty common, and I think it’s due largely to high stress and a wide variation in workload, neither of which are in our direct control. At facilities where there is significant tension, I’m impressed by how vigorously the hospitalists at both the small and large hospitals argue that their own site faces the most stress and challenges. (This is a little like the endless debate about who works harder, those who work with residents and those who don’t.)
The hospitalists at the small site point out that they work with little or no subspecialty help and might even have to take night call from home while working during the day. Those at the big hospital say they are the ones with the very large scope of clinical practice and that, rather than making their life easier, the presence of lots of subspecialists makes for additional work coordinating care and communicating with all parties.
Where it exists, this tension is most evident during a transfer from one of the small hospitals to the large one. After all, one of the reasons to form a system of hospitals is so that nearly all patient needs can be met at one of the facilities in the system. Yet, for many reasons, the hospitalists at the large hospital are—sometimes—not as receptive to transfers as might be ideal. They might be short staffed or facing a high census or an unusually high number of admissions from their own ED. Or, perhaps, they’re concerned that the subspecialty services for which the patient is being transferred (e.g. to be scoped by a GI doctor) won’t be as helpful or prompt as needed. Or maybe they’ve felt “burned” by their colleagues at the small hospital for past transfers that didn’t seem necessary.
The result can be that the doctors at the smaller hospital complain that the “mother ship” hospitalists often are unfriendly and unreceptive to transfer requests. Although there may not be a definitive “cure” for this issue, there are several ways to help address the problem.
- In my last column, I mentioned the value of one or more in-person meetings between those who tend to be on the sending and receiving end of transfers, to establish some criteria regarding transfers that are appropriate and review the process of requesting a transfer and making the associated arrangements. In most cases there will be value in the parties meeting routinely—perhaps two to four times annually—to review how the system is working and address any difficulties.
- Periodic social meetings among the hospitalists at each site will help to form relationships that can make it less likely that any conversation about transfers will go in an unhelpful direction. Things can be very different when the people on each end of the phone call know each other personally.
- Record the phone calls between those seeking and accepting/declining each transfer. Scott Rissmiller, MD, the lead hospitalist for the 17 practice sites in Carolinas Healthcare, has said that having underperforming doctors listen to recordings of their phone calls about transfers has, in most cases he’s been involved with, proven to be a very effective way to encourage improvement.
Shared Staffing
The small hospitals in many systems sometimes struggle to find a way to provide economical night coverage. Hospitals below a certain size find it very difficult to justify a separate, in-house night provider. Some hospital systems have had success sharing night staffing, with the large hospital’s night hospitalist, nurse practitioner, or physician assistant providing telephone coverage for “cross cover” issues that arise after hours.
For example, when a nurse at the small hospital needs to contact a night hospitalist, staff will page the provider at the big hospital, and, in many cases, the issue can be managed effectively by phone. This works best when both hospitals are on the same electronic medical record, so that the responding provider can look through the record as needed.
The hospitalist at the small hospital typically stays on back-up call and is contacted if bedside attention is required.
Or, if the large and small hospitals are a short drive apart, the night hospitalist at the large facility might make the short drive to the small hospital when needed. In the case of emergencies (i.e., a code blue), the in-house night ED physician is relied on as the first responder.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. Write to him at john.nelson@nelsonflores.com.
Society of Hospital Medicine Creates Self-Assessment Tool for Hospitalist Groups
Are you looking to improve your hospital medicine group (HMG)? Would you like to measure your group against other groups?
The February 2013 issue of the Journal of Hospital Medicine included a seminal article for our specialty, “The Key Principles and Characteristics of an Effective Hospital Medicine Group: an assessment guide for hospitals and hospitalists.” This paper has received a vast amount of attention around the country from hospitalists, hospitalist leaders, HMGs, and hospital executives. The report (www.hospitalmedicine.org/keychar) is a first step for physicians and executives looking to benchmark their practices, and it has stimulated discussions among many HMGs, beginning a process of self-review and considering action.
I am coming up on my 20th year as a hospitalist, and the debate over what makes a high-performing HMG has continued that entire time. In the beginning, there were questions about the mere existence of hospital medicine and HMGs. The discussion about what makes a high-performing HMG started among the physicians, medical groups, and hospitals that signed on early to the HM movement. At conferences, HMG leaders debated how to set up a program. A series of pioneer hospitalists, many with only a few years of experience, roamed the country as consultants giving advice on best practices. A professional society, the National Association of Inpatient Physicians, was born and, later, recast as the Society of Hospital Medicine (SHM)—and the discussion continued.
SHM furthered the debate with such important milestones as The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, white papers on career satisfaction and hospitalist involvement in quality/safety and transitions of care. Different types of practice arrangements developed. Some were hospital-based, some physician practice-centered. Some were local, and others were regional and national. Each of these spawned innovations in HMG processes and contributed to the growing body of best practices.
Over the past five years, a consensus regarding those best practices has seemingly developed, and the discussions are centered on fine details rather than significant differences. To that end, approximately three years ago, a small group of SHM members met and discussed how to capture this information and disseminate it better among hospitalists, HMGs, and hospitals. We had all come to a similar conclusion—high-performing HMGs share common characteristics. Furthermore, every hospital and HMG seeks excellence, striving to be the best that they can be. We settled on a plan to write this up.
After a year of debate, we sought SHM’s help in the development phase and, in early 2012, SHM’s board of directors appointed a workgroup to identify the key principles and characteristics of an effective HMG. The initial group was widened to make sure we included different backgrounds and experiences in hospital medicine. The group had a wide array of involvement in HMG models, including HMG members, HMG leaders, hospital executives, and some involved in consulting. Many of the individuals had multiple experiences. The conversation among these individuals was lively!
The workgroup developed an initial draft of characteristics, which then went through a multi-step process of review and redrafting. More than 200 individuals, representing a broad group of stakeholders in hospital medicine and in the healthcare industry in general, provided comments and feedback. In addition, the workgroup went through a two-step Delphi process to consolidate and/or eliminate characteristics that were redundant or unnecessary.
In the final framework, 47 key characteristics were defined and organized under 10 principles (see Figure 1).
The authors and SHM’s board of directors view this document as an aspirational approach to improvement. We feel it helps to “raise the bar” for the specialty of hospital medicine by laying out a roadmap of potential improvement. These principles and characteristics provide a framework for HMGs seeking to conduct self-assessments, outlining a pathway for improvement, and better defining the central role of hospitalists in coordinating team-based, patient-centered care in the acute care setting.
In enhancing quality, the approach of a gap analysis is a very effective tool. These principles provide an excellent approach to begin that review.
So how do you get started? Hopefully, your HMG has a regular meeting. Take a principle and have a conversation. For example, what do we have? What don’t we have?
Other groups may want to tackle the entire document in a daylong strategy review. Some may want an outside facilitator. Bottom line: It doesn’t matter how you do it; just start with a conversation.
Dr. Cawley is CEO of Medical University of South Carolina Medical Center in Charleston. He is past president of SHM.
Reference
Are you looking to improve your hospital medicine group (HMG)? Would you like to measure your group against other groups?
The February 2013 issue of the Journal of Hospital Medicine included a seminal article for our specialty, “The Key Principles and Characteristics of an Effective Hospital Medicine Group: an assessment guide for hospitals and hospitalists.” This paper has received a vast amount of attention around the country from hospitalists, hospitalist leaders, HMGs, and hospital executives. The report (www.hospitalmedicine.org/keychar) is a first step for physicians and executives looking to benchmark their practices, and it has stimulated discussions among many HMGs, beginning a process of self-review and considering action.
I am coming up on my 20th year as a hospitalist, and the debate over what makes a high-performing HMG has continued that entire time. In the beginning, there were questions about the mere existence of hospital medicine and HMGs. The discussion about what makes a high-performing HMG started among the physicians, medical groups, and hospitals that signed on early to the HM movement. At conferences, HMG leaders debated how to set up a program. A series of pioneer hospitalists, many with only a few years of experience, roamed the country as consultants giving advice on best practices. A professional society, the National Association of Inpatient Physicians, was born and, later, recast as the Society of Hospital Medicine (SHM)—and the discussion continued.
SHM furthered the debate with such important milestones as The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, white papers on career satisfaction and hospitalist involvement in quality/safety and transitions of care. Different types of practice arrangements developed. Some were hospital-based, some physician practice-centered. Some were local, and others were regional and national. Each of these spawned innovations in HMG processes and contributed to the growing body of best practices.
Over the past five years, a consensus regarding those best practices has seemingly developed, and the discussions are centered on fine details rather than significant differences. To that end, approximately three years ago, a small group of SHM members met and discussed how to capture this information and disseminate it better among hospitalists, HMGs, and hospitals. We had all come to a similar conclusion—high-performing HMGs share common characteristics. Furthermore, every hospital and HMG seeks excellence, striving to be the best that they can be. We settled on a plan to write this up.
After a year of debate, we sought SHM’s help in the development phase and, in early 2012, SHM’s board of directors appointed a workgroup to identify the key principles and characteristics of an effective HMG. The initial group was widened to make sure we included different backgrounds and experiences in hospital medicine. The group had a wide array of involvement in HMG models, including HMG members, HMG leaders, hospital executives, and some involved in consulting. Many of the individuals had multiple experiences. The conversation among these individuals was lively!
The workgroup developed an initial draft of characteristics, which then went through a multi-step process of review and redrafting. More than 200 individuals, representing a broad group of stakeholders in hospital medicine and in the healthcare industry in general, provided comments and feedback. In addition, the workgroup went through a two-step Delphi process to consolidate and/or eliminate characteristics that were redundant or unnecessary.
In the final framework, 47 key characteristics were defined and organized under 10 principles (see Figure 1).
The authors and SHM’s board of directors view this document as an aspirational approach to improvement. We feel it helps to “raise the bar” for the specialty of hospital medicine by laying out a roadmap of potential improvement. These principles and characteristics provide a framework for HMGs seeking to conduct self-assessments, outlining a pathway for improvement, and better defining the central role of hospitalists in coordinating team-based, patient-centered care in the acute care setting.
In enhancing quality, the approach of a gap analysis is a very effective tool. These principles provide an excellent approach to begin that review.
So how do you get started? Hopefully, your HMG has a regular meeting. Take a principle and have a conversation. For example, what do we have? What don’t we have?
Other groups may want to tackle the entire document in a daylong strategy review. Some may want an outside facilitator. Bottom line: It doesn’t matter how you do it; just start with a conversation.
Dr. Cawley is CEO of Medical University of South Carolina Medical Center in Charleston. He is past president of SHM.
Reference
Are you looking to improve your hospital medicine group (HMG)? Would you like to measure your group against other groups?
The February 2013 issue of the Journal of Hospital Medicine included a seminal article for our specialty, “The Key Principles and Characteristics of an Effective Hospital Medicine Group: an assessment guide for hospitals and hospitalists.” This paper has received a vast amount of attention around the country from hospitalists, hospitalist leaders, HMGs, and hospital executives. The report (www.hospitalmedicine.org/keychar) is a first step for physicians and executives looking to benchmark their practices, and it has stimulated discussions among many HMGs, beginning a process of self-review and considering action.
I am coming up on my 20th year as a hospitalist, and the debate over what makes a high-performing HMG has continued that entire time. In the beginning, there were questions about the mere existence of hospital medicine and HMGs. The discussion about what makes a high-performing HMG started among the physicians, medical groups, and hospitals that signed on early to the HM movement. At conferences, HMG leaders debated how to set up a program. A series of pioneer hospitalists, many with only a few years of experience, roamed the country as consultants giving advice on best practices. A professional society, the National Association of Inpatient Physicians, was born and, later, recast as the Society of Hospital Medicine (SHM)—and the discussion continued.
SHM furthered the debate with such important milestones as The Core Competencies in Hospital Medicine: A Framework for Curriculum Development, white papers on career satisfaction and hospitalist involvement in quality/safety and transitions of care. Different types of practice arrangements developed. Some were hospital-based, some physician practice-centered. Some were local, and others were regional and national. Each of these spawned innovations in HMG processes and contributed to the growing body of best practices.
Over the past five years, a consensus regarding those best practices has seemingly developed, and the discussions are centered on fine details rather than significant differences. To that end, approximately three years ago, a small group of SHM members met and discussed how to capture this information and disseminate it better among hospitalists, HMGs, and hospitals. We had all come to a similar conclusion—high-performing HMGs share common characteristics. Furthermore, every hospital and HMG seeks excellence, striving to be the best that they can be. We settled on a plan to write this up.
After a year of debate, we sought SHM’s help in the development phase and, in early 2012, SHM’s board of directors appointed a workgroup to identify the key principles and characteristics of an effective HMG. The initial group was widened to make sure we included different backgrounds and experiences in hospital medicine. The group had a wide array of involvement in HMG models, including HMG members, HMG leaders, hospital executives, and some involved in consulting. Many of the individuals had multiple experiences. The conversation among these individuals was lively!
The workgroup developed an initial draft of characteristics, which then went through a multi-step process of review and redrafting. More than 200 individuals, representing a broad group of stakeholders in hospital medicine and in the healthcare industry in general, provided comments and feedback. In addition, the workgroup went through a two-step Delphi process to consolidate and/or eliminate characteristics that were redundant or unnecessary.
In the final framework, 47 key characteristics were defined and organized under 10 principles (see Figure 1).
The authors and SHM’s board of directors view this document as an aspirational approach to improvement. We feel it helps to “raise the bar” for the specialty of hospital medicine by laying out a roadmap of potential improvement. These principles and characteristics provide a framework for HMGs seeking to conduct self-assessments, outlining a pathway for improvement, and better defining the central role of hospitalists in coordinating team-based, patient-centered care in the acute care setting.
In enhancing quality, the approach of a gap analysis is a very effective tool. These principles provide an excellent approach to begin that review.
So how do you get started? Hopefully, your HMG has a regular meeting. Take a principle and have a conversation. For example, what do we have? What don’t we have?
Other groups may want to tackle the entire document in a daylong strategy review. Some may want an outside facilitator. Bottom line: It doesn’t matter how you do it; just start with a conversation.
Dr. Cawley is CEO of Medical University of South Carolina Medical Center in Charleston. He is past president of SHM.
Reference
Shift from Productivity to Value-Based Compensation Gains Momentum
At the 2011 SHM annual meeting in Dallas, I served on an expert panel that reviewed the latest hospitalist survey data. Included in this review were the latest compensation and productivity figures. As the session concluded, I was satisfied that the panel had discussed important information in an accessible way; however, the keynote speaker who followed us to address an entirely different topic began his talk by pointing out that the data we had reviewed, including things like wRVUs, would very soon have little to do with compensation for any physician, regardless of specialty. He implied, quite persuasively, that we were pretty old school to be talking about wRVUs and compensation based on productivity; everyone should be prepared for and embrace compensation based on value, not production.
I hear a similar sentiment reasonably often. And I agree, but I think many make the mistake of oversimplifying the issue.
Physician Value-Based Payment
Measurement of physician performance using costs, quality, and outcomes has already begun and will influence Medicare payments to doctors beginning in 2015 for large groups (>100 providers with any mix of specialties billing under the same tax ID number) and in 2017 for smaller groups.
If Medicare is moving away from payment based on wRVUs, likely followed soon by other payors, then hospitalist compensation should do the same. But I don’t think that changes the potential role of compensation based on productivity.
Compensation Should Include Performance and Productivity Metrics
Survey data show a move from an essentially fixed annual compensation early in our field to an inclusion of components tied to performance several years before the introduction of the Physician Value-Based Payment Modifier program. Data from SHM’s 2010, 2011, and 2012 State of Hospital Medicine reports (www.hospitalmedicine.org/survey) show that a small, but probably increasing, part of compensation has been tied to performance on things like patient satisfaction and core measures (see “Distribution of Total Hospitalist Compensation,” below). Note that the percentages in the chart refer to the fraction of total compensation dollars allocated to each domain and not the portion of hospitalists who have compensation tied to each domain.
Over the same three years, the percentage of compensation tied to productivity has been decreasing overall, while “private groups are more likely to pay a higher proportion of compensation based on productivity, and hospital-employed groups are more likely to pay a higher proportion of compensation based on performance.”
Matching Performance Compensation to Medicare’s Value-Based Modifier
It makes sense for physician compensation to generally mirror Medicare and other payor professional fee reimbursement formulas. But, in that regard, hospitalists are ahead of the market already, because the portion of dollars allocated to performance (value) in hospitalist compensation plans already exceeds the 2% or less portion of Medicare reimbursement that is influenced by performance.
Medicare will steadily increase the portion of reimbursement allocated to performance (value) and decrease the part tied solely to wRVUs. So it makes sense that hospitalist compensation plans should do the same. Who knows, within the next 5-10 years, hospitalists, and potentially doctors in all specialties, might see 20% to 50% of their compensation tied to performance. I think that might be a good thing, as long as we can come up with effective measures of performance and value—not an easy thing to do in any business or industry.
Future Role of Productivity Compensation
I don’t think all the talk about value-based reimbursement means we should abandon the idea of connecting a portion of compensation to productivity. The first two practice management columns I wrote for The Hospitalist appeared in May 2006 (www.the-hospitalist.org/details/article/252413/The_Sweet_Spot.html) and June 2006 (www.the-hospitalist.org/details/article/246297.html) and recommended tying a meaningful portion of compensation to individual hospitalist productivity, and I think it still makes sense to do so.
Source: 2012 State of Hospital Medicine report
In any business or industry, financial performance is connected to the amount of product produced and its value. In the future, both metrics will determine reimbursement for even the highest performing healthcare providers. The new emphasis on value won’t ever make it unnecessary to produce at a reasonable level.
Unquestionably, there are many high-performing hospitalist practices with little or no productivity component in the compensation formula. So it isn’t an absolute sine qua non for success. But I think many practices dismiss it as a viable option when it might solve problems and liberate individuals in the group to exercise some autonomy in finding their own sweet spot between workload and compensation.
It will be interesting to see if future surveys show that the portion of dollars tied to hospitalist productivity continues to decrease, despite what I see as its potential benefits.

At the 2011 SHM annual meeting in Dallas, I served on an expert panel that reviewed the latest hospitalist survey data. Included in this review were the latest compensation and productivity figures. As the session concluded, I was satisfied that the panel had discussed important information in an accessible way; however, the keynote speaker who followed us to address an entirely different topic began his talk by pointing out that the data we had reviewed, including things like wRVUs, would very soon have little to do with compensation for any physician, regardless of specialty. He implied, quite persuasively, that we were pretty old school to be talking about wRVUs and compensation based on productivity; everyone should be prepared for and embrace compensation based on value, not production.
I hear a similar sentiment reasonably often. And I agree, but I think many make the mistake of oversimplifying the issue.
Physician Value-Based Payment
Measurement of physician performance using costs, quality, and outcomes has already begun and will influence Medicare payments to doctors beginning in 2015 for large groups (>100 providers with any mix of specialties billing under the same tax ID number) and in 2017 for smaller groups.
If Medicare is moving away from payment based on wRVUs, likely followed soon by other payors, then hospitalist compensation should do the same. But I don’t think that changes the potential role of compensation based on productivity.
Compensation Should Include Performance and Productivity Metrics
Survey data show a move from an essentially fixed annual compensation early in our field to an inclusion of components tied to performance several years before the introduction of the Physician Value-Based Payment Modifier program. Data from SHM’s 2010, 2011, and 2012 State of Hospital Medicine reports (www.hospitalmedicine.org/survey) show that a small, but probably increasing, part of compensation has been tied to performance on things like patient satisfaction and core measures (see “Distribution of Total Hospitalist Compensation,” below). Note that the percentages in the chart refer to the fraction of total compensation dollars allocated to each domain and not the portion of hospitalists who have compensation tied to each domain.
Over the same three years, the percentage of compensation tied to productivity has been decreasing overall, while “private groups are more likely to pay a higher proportion of compensation based on productivity, and hospital-employed groups are more likely to pay a higher proportion of compensation based on performance.”
Matching Performance Compensation to Medicare’s Value-Based Modifier
It makes sense for physician compensation to generally mirror Medicare and other payor professional fee reimbursement formulas. But, in that regard, hospitalists are ahead of the market already, because the portion of dollars allocated to performance (value) in hospitalist compensation plans already exceeds the 2% or less portion of Medicare reimbursement that is influenced by performance.
Medicare will steadily increase the portion of reimbursement allocated to performance (value) and decrease the part tied solely to wRVUs. So it makes sense that hospitalist compensation plans should do the same. Who knows, within the next 5-10 years, hospitalists, and potentially doctors in all specialties, might see 20% to 50% of their compensation tied to performance. I think that might be a good thing, as long as we can come up with effective measures of performance and value—not an easy thing to do in any business or industry.
Future Role of Productivity Compensation
I don’t think all the talk about value-based reimbursement means we should abandon the idea of connecting a portion of compensation to productivity. The first two practice management columns I wrote for The Hospitalist appeared in May 2006 (www.the-hospitalist.org/details/article/252413/The_Sweet_Spot.html) and June 2006 (www.the-hospitalist.org/details/article/246297.html) and recommended tying a meaningful portion of compensation to individual hospitalist productivity, and I think it still makes sense to do so.
Source: 2012 State of Hospital Medicine report
In any business or industry, financial performance is connected to the amount of product produced and its value. In the future, both metrics will determine reimbursement for even the highest performing healthcare providers. The new emphasis on value won’t ever make it unnecessary to produce at a reasonable level.
Unquestionably, there are many high-performing hospitalist practices with little or no productivity component in the compensation formula. So it isn’t an absolute sine qua non for success. But I think many practices dismiss it as a viable option when it might solve problems and liberate individuals in the group to exercise some autonomy in finding their own sweet spot between workload and compensation.
It will be interesting to see if future surveys show that the portion of dollars tied to hospitalist productivity continues to decrease, despite what I see as its potential benefits.

At the 2011 SHM annual meeting in Dallas, I served on an expert panel that reviewed the latest hospitalist survey data. Included in this review were the latest compensation and productivity figures. As the session concluded, I was satisfied that the panel had discussed important information in an accessible way; however, the keynote speaker who followed us to address an entirely different topic began his talk by pointing out that the data we had reviewed, including things like wRVUs, would very soon have little to do with compensation for any physician, regardless of specialty. He implied, quite persuasively, that we were pretty old school to be talking about wRVUs and compensation based on productivity; everyone should be prepared for and embrace compensation based on value, not production.
I hear a similar sentiment reasonably often. And I agree, but I think many make the mistake of oversimplifying the issue.
Physician Value-Based Payment
Measurement of physician performance using costs, quality, and outcomes has already begun and will influence Medicare payments to doctors beginning in 2015 for large groups (>100 providers with any mix of specialties billing under the same tax ID number) and in 2017 for smaller groups.
If Medicare is moving away from payment based on wRVUs, likely followed soon by other payors, then hospitalist compensation should do the same. But I don’t think that changes the potential role of compensation based on productivity.
Compensation Should Include Performance and Productivity Metrics
Survey data show a move from an essentially fixed annual compensation early in our field to an inclusion of components tied to performance several years before the introduction of the Physician Value-Based Payment Modifier program. Data from SHM’s 2010, 2011, and 2012 State of Hospital Medicine reports (www.hospitalmedicine.org/survey) show that a small, but probably increasing, part of compensation has been tied to performance on things like patient satisfaction and core measures (see “Distribution of Total Hospitalist Compensation,” below). Note that the percentages in the chart refer to the fraction of total compensation dollars allocated to each domain and not the portion of hospitalists who have compensation tied to each domain.
Over the same three years, the percentage of compensation tied to productivity has been decreasing overall, while “private groups are more likely to pay a higher proportion of compensation based on productivity, and hospital-employed groups are more likely to pay a higher proportion of compensation based on performance.”
Matching Performance Compensation to Medicare’s Value-Based Modifier
It makes sense for physician compensation to generally mirror Medicare and other payor professional fee reimbursement formulas. But, in that regard, hospitalists are ahead of the market already, because the portion of dollars allocated to performance (value) in hospitalist compensation plans already exceeds the 2% or less portion of Medicare reimbursement that is influenced by performance.
Medicare will steadily increase the portion of reimbursement allocated to performance (value) and decrease the part tied solely to wRVUs. So it makes sense that hospitalist compensation plans should do the same. Who knows, within the next 5-10 years, hospitalists, and potentially doctors in all specialties, might see 20% to 50% of their compensation tied to performance. I think that might be a good thing, as long as we can come up with effective measures of performance and value—not an easy thing to do in any business or industry.
Future Role of Productivity Compensation
I don’t think all the talk about value-based reimbursement means we should abandon the idea of connecting a portion of compensation to productivity. The first two practice management columns I wrote for The Hospitalist appeared in May 2006 (www.the-hospitalist.org/details/article/252413/The_Sweet_Spot.html) and June 2006 (www.the-hospitalist.org/details/article/246297.html) and recommended tying a meaningful portion of compensation to individual hospitalist productivity, and I think it still makes sense to do so.
Source: 2012 State of Hospital Medicine report
In any business or industry, financial performance is connected to the amount of product produced and its value. In the future, both metrics will determine reimbursement for even the highest performing healthcare providers. The new emphasis on value won’t ever make it unnecessary to produce at a reasonable level.
Unquestionably, there are many high-performing hospitalist practices with little or no productivity component in the compensation formula. So it isn’t an absolute sine qua non for success. But I think many practices dismiss it as a viable option when it might solve problems and liberate individuals in the group to exercise some autonomy in finding their own sweet spot between workload and compensation.
It will be interesting to see if future surveys show that the portion of dollars tied to hospitalist productivity continues to decrease, despite what I see as its potential benefits.