User login
There’s No Place Like Home… for Carbon Monoxide Poisoning
Case
An 84-year-old woman with a history of hypertension and dyslipidemia and her husband, an 88-year-old man with a history of dementia and coronary artery disease, presented to the ED via EMS after neighbors discovered the woman lying on her living room floor, responding only to painful stimuli. Earlier in the evening, the same neighbors had helped the husband to bed after noticing that he had become lethargic. The EMS report indicated that a car had been left running in a closed garage of the patients’ home. The fire department identified an ambient carbon monoxide (CO) concentration of 88 ppm.
Upon arrival to the ED, the woman’s vital signs were: blood pressure (BP), 130/74 mm Hg; heart rate (HR), 63 beats/minute; respiratory rate (RR), 16 breaths/minute; temperature, 99°F. Oxygen saturation was 99% on room air. Her husband’s vital signs were: BP, 150/66 mm Hg; HR, 59 beats/minute; RR, 19 breaths/minute; temperature, 98°F; oxygen saturation was 98% on room air.
What is carbon monoxide poisoning?
Carbon monoxide is a colorless and odorless toxic gas produced by incomplete combustion of carbon-based fuel. Common sources in the United States include portable generators, gas-powered furnaces, cooking appliances, poorly ventilated home-heating systems, and motor vehicles (Box 1).1
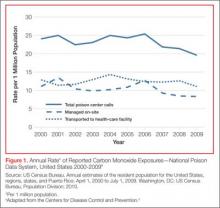
Carbon monoxide is the leading cause of unintentional poisoning deaths in the United States,1 resulting in more than 20,000 ED visits and 2,000 hospital admissions. Nearly three-fourths of these deaths are due to exposures in the home, with more than half occurring during the months of November through February.2,3 The average cost of a hospital admission for confirmed CO poisoning is over $11,000, with a cumulative nationwide total cost of over $26 million per year. While the hospitalization rate for persons aged 18 to 44 years is only 6.7%, the admittance rates for persons aged 65 to 84 years and older than 85 years are 33% and 43%, respectively.3 Although there has been a slight decline in the incidence of CO poisoning over the past 10 years, it is still a public health concern (Figure 1).2
Who is most susceptible to motor vehicle-related carbon monoxide poisoning?
The US Centers for Disease Control and Prevention (CDC) reports that motor vehicles are the second most common source of CO exposure.4 A study of US news media reports covering a 2.5-year period revealed that 8% of such poisonings were the result of a motor vehicle left running in a garage—the overall mortality rate of which is suggested to be significantly higher than that of other sources of CO exposure.5
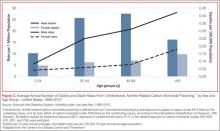
Approximately 430 deaths per year are caused by unintentional, nonfire-related CO poisoning,6 and the CDC reports the death rate is highest in persons older than age 65 years.1 The death rate from these exposures is more than three times higher in men than women (Figure 2).6 In addition, older patients are disproportionately affected: In US news media-reported cases of CO poisoning that included patient age, 29% occurred in persons older than age 80 years.5 Moreover, in approximately one-third of motor vehicle-related deaths due to CO poisoning, nearly all of patients older than age 80 years were found dead at the scene of exposure. These reports suggest that the elderly are at greater risk for CO exposure due to age-related cognitive changes, physical inability to escape a toxic environment once becoming symptomatic, and a greater susceptibility to poisoning due to comorbid conditions.5
Case Continued
The husband and wife’s initial carboxyhemoglobin concentrations in this case were 35% and 13%, respectively. Both were treated with hyperbaric oxygen (HBO) without complication. During their inpatient stay, the woman noted that their home did not have a CO detector.
What is the role of hyperbaric oxygen therapy as a treatment option for CO poisoning?
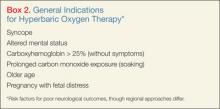
Hyperbaric oxygen therapy greatly accelerates the dissociation of hemoglobin from CO, reduces free radical-related cellular damage, and may have a role in preventing adverse neurological sequelae in the setting of CO poisoning. Although controversy exists, HBO therapy is generally indicated in select patients with elevated CO levels and abnormal neurological findings, cardiovascular findings, or persistent metabolic acidosis. While few ED patients with CO exposure receive HBO therapy, over 20% of patients requiring inpatient hospitalization receive treatment.3
What preventive measures can be taken to reduce motor vehicle-related CO poisoning?
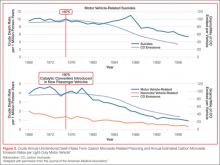
The literature supports the enforcement of motor vehicle emissions standards and the proper use of home CO detectors as primary preventive strategies. Computerized data from the CDC, US Census Bureau, and US Environmental Protection Agency from 1968 to 1998 were used to evaluate the influence of national vehicle emissions policies on CO-related mortality. The Clean Air Act of 1970 set environmental limits on CO emissions from automobiles at 15.0 g/mile in 1975; the EPA further reduced this standard to 3.4 g/mile for automobiles manufactured after 1981. After the enforcement of standards set forth by the Clean Air Act and the introduction of the catalytic converter in 1975, CO emissions from automobiles decreased by an estimated 76.3%, and unintentional motor vehicle-related CO deaths declined by 81.3% (Figure 3).7 (Catalytic converters contain elements [eg, platinum] that catalyze the oxidation of CO to carbon dioxide.)
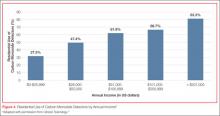
Since CO exposure occurs primarily in the home, the installation of battery-powered or battery-backed CO alarms—both in the home and garage—can prevent poisoning. These detectors are inexpensive and available at common retail stores. Unfortunately, despite the easy availability and access to CO detectors, only 39 states currently have legislation mandating their use, and approximately two-thirds of the states with existing legislation only require CO detectors in newly built structures.8
In 2010, the state of New York enacted legislation known as “Amanda’s Law,” (named after a teenaged girl whose death was caused by CO poisoning from a defective boiler) mandating CO detectors in all one- and two-family homes with heating sources that may emit CO or have attached garages. However, an industry survey in 2011 found that nearly half of New York families were not aware of this law.9 The two largest surveys on home CO detector use—those conducted by the US Census Bureau and CDC—estimate the national rate of having a working CO detector in a home is 32% to 40%, with a lower prevalence among those living in manufactured housing, renting a home, or living below the poverty level.10
What is the utilization of CO detectors by ED patients?
Case conclusion
After hospital admission and treatment, both patients were discharged on hospital day 2 with a return to a baseline mental status. Neither patient reported neurological sequelae or new cognitive changes when a follow up call was placed more than 6 months after HBO treatment. The couple furthermore reported that they installed a CO detector upon their return home.
Dr West is a resident, department of emergency medicine, Albert Einstein College of Medicine, Bronx, New York.
Dr McGregor is a resident, department of emergency medicine, Albert Einstein College of Medicine, Bronx, New York.
Dr Touger is an associate professor of clinical emergency medicine, department of emergency medicine, Albert Einstein College of Medicine, Bronx, New York. He is also medical director of the Jacobi Medical Center hyperbaric chamber.
Dr Nelson, editor of “Case Studies in Toxicology,” is a professor in the department of emergency medicine and director of the medical toxicology fellowship program at New York University School of Medicine and New York City Poison Control Center. He is also associate editor, toxicology, of the EMERGENCY MEDICINE editorial board.
- Centers for Disease Control and Prevention. Carbon monoxide-related deaths—United States, 1999-2004. MMWR Morb Mortal Wkly Rep. 2007;56(50):1309-1312.
- Centers for Disease Control and Prevention. Carbon mononoxide exposures—United States, 2000-2009. MMWR Morb Mortal Wkly Rep. 2011;60(30):1014-1017.
- Iqbal S, Law HZ, Clower JH, Yip FY, Elixhauser A. Hospital burden of unintentional carbon monoxide poisoning in the United States, 2007. Am J Emerg Med. 2012;30(5):657-664.
- Centers for Disease Control and Prevention. Nonfatal, unintentional, non-fire-related carbon monoxide exposures—United States, 2004-2006. MMWR Morb Mortal Wkly Rep. 2008;57(33):896-899.
- Hampson NB. Residential carbon monoxide poisoning from motor vehicles. Am J Emerg Med. 2011;29(1):75-77.
- Centers for Disease Control and Prevention. Average annual number of deaths and death rates from unintentional, non-fire-related carbon monoxide poisoning, by sex and age group—United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2014;63(3):65.
- Mott JA, Wolfe MI, Alverson CJ, et al. National vehicle emissions policies and practices and declining US carbon monoxide-related mortality. JAMA. 2002;288(8):988-995.
- Carbon monoxide detectors: state statutes. National Conference of State Legislatures Web site. http://www.ncsl.org/research/environment-and-natural-resources/carbon-monoxide-detectors-state-statutes.aspx. Accessed March 11, 2014.
- Survey results: New York homeowners and the risk of carbon monoxide poisoning. Kidde Web site. http://www.kidde.com/PressRoom/Pages/SurveyResultsNYHomeownersCORisks.aspx. Accessed March 11, 2014.
- Iqbal S, Clower JH, King M, Bell J, Yip YF. National carbon monoxide poisoning surveillance framework and recent estimates. Public Health Rep. 2012;127(5):486-496.
- Johnson-Arbor K, Liebman DL, Carter EM. A survey of residential carbon monoxide detector utilization among Connecticut Emergency Department patients. Clin Toxicol (Phila). 2012;50(5):384-389.
Case
An 84-year-old woman with a history of hypertension and dyslipidemia and her husband, an 88-year-old man with a history of dementia and coronary artery disease, presented to the ED via EMS after neighbors discovered the woman lying on her living room floor, responding only to painful stimuli. Earlier in the evening, the same neighbors had helped the husband to bed after noticing that he had become lethargic. The EMS report indicated that a car had been left running in a closed garage of the patients’ home. The fire department identified an ambient carbon monoxide (CO) concentration of 88 ppm.
Upon arrival to the ED, the woman’s vital signs were: blood pressure (BP), 130/74 mm Hg; heart rate (HR), 63 beats/minute; respiratory rate (RR), 16 breaths/minute; temperature, 99°F. Oxygen saturation was 99% on room air. Her husband’s vital signs were: BP, 150/66 mm Hg; HR, 59 beats/minute; RR, 19 breaths/minute; temperature, 98°F; oxygen saturation was 98% on room air.
What is carbon monoxide poisoning?
Carbon monoxide is a colorless and odorless toxic gas produced by incomplete combustion of carbon-based fuel. Common sources in the United States include portable generators, gas-powered furnaces, cooking appliances, poorly ventilated home-heating systems, and motor vehicles (Box 1).1
Carbon monoxide is the leading cause of unintentional poisoning deaths in the United States,1 resulting in more than 20,000 ED visits and 2,000 hospital admissions. Nearly three-fourths of these deaths are due to exposures in the home, with more than half occurring during the months of November through February.2,3 The average cost of a hospital admission for confirmed CO poisoning is over $11,000, with a cumulative nationwide total cost of over $26 million per year. While the hospitalization rate for persons aged 18 to 44 years is only 6.7%, the admittance rates for persons aged 65 to 84 years and older than 85 years are 33% and 43%, respectively.3 Although there has been a slight decline in the incidence of CO poisoning over the past 10 years, it is still a public health concern (Figure 1).2
Who is most susceptible to motor vehicle-related carbon monoxide poisoning?
The US Centers for Disease Control and Prevention (CDC) reports that motor vehicles are the second most common source of CO exposure.4 A study of US news media reports covering a 2.5-year period revealed that 8% of such poisonings were the result of a motor vehicle left running in a garage—the overall mortality rate of which is suggested to be significantly higher than that of other sources of CO exposure.5
Approximately 430 deaths per year are caused by unintentional, nonfire-related CO poisoning,6 and the CDC reports the death rate is highest in persons older than age 65 years.1 The death rate from these exposures is more than three times higher in men than women (Figure 2).6 In addition, older patients are disproportionately affected: In US news media-reported cases of CO poisoning that included patient age, 29% occurred in persons older than age 80 years.5 Moreover, in approximately one-third of motor vehicle-related deaths due to CO poisoning, nearly all of patients older than age 80 years were found dead at the scene of exposure. These reports suggest that the elderly are at greater risk for CO exposure due to age-related cognitive changes, physical inability to escape a toxic environment once becoming symptomatic, and a greater susceptibility to poisoning due to comorbid conditions.5
Case Continued
The husband and wife’s initial carboxyhemoglobin concentrations in this case were 35% and 13%, respectively. Both were treated with hyperbaric oxygen (HBO) without complication. During their inpatient stay, the woman noted that their home did not have a CO detector.
What is the role of hyperbaric oxygen therapy as a treatment option for CO poisoning?
Hyperbaric oxygen therapy greatly accelerates the dissociation of hemoglobin from CO, reduces free radical-related cellular damage, and may have a role in preventing adverse neurological sequelae in the setting of CO poisoning. Although controversy exists, HBO therapy is generally indicated in select patients with elevated CO levels and abnormal neurological findings, cardiovascular findings, or persistent metabolic acidosis. While few ED patients with CO exposure receive HBO therapy, over 20% of patients requiring inpatient hospitalization receive treatment.3
What preventive measures can be taken to reduce motor vehicle-related CO poisoning?
The literature supports the enforcement of motor vehicle emissions standards and the proper use of home CO detectors as primary preventive strategies. Computerized data from the CDC, US Census Bureau, and US Environmental Protection Agency from 1968 to 1998 were used to evaluate the influence of national vehicle emissions policies on CO-related mortality. The Clean Air Act of 1970 set environmental limits on CO emissions from automobiles at 15.0 g/mile in 1975; the EPA further reduced this standard to 3.4 g/mile for automobiles manufactured after 1981. After the enforcement of standards set forth by the Clean Air Act and the introduction of the catalytic converter in 1975, CO emissions from automobiles decreased by an estimated 76.3%, and unintentional motor vehicle-related CO deaths declined by 81.3% (Figure 3).7 (Catalytic converters contain elements [eg, platinum] that catalyze the oxidation of CO to carbon dioxide.)
Since CO exposure occurs primarily in the home, the installation of battery-powered or battery-backed CO alarms—both in the home and garage—can prevent poisoning. These detectors are inexpensive and available at common retail stores. Unfortunately, despite the easy availability and access to CO detectors, only 39 states currently have legislation mandating their use, and approximately two-thirds of the states with existing legislation only require CO detectors in newly built structures.8
In 2010, the state of New York enacted legislation known as “Amanda’s Law,” (named after a teenaged girl whose death was caused by CO poisoning from a defective boiler) mandating CO detectors in all one- and two-family homes with heating sources that may emit CO or have attached garages. However, an industry survey in 2011 found that nearly half of New York families were not aware of this law.9 The two largest surveys on home CO detector use—those conducted by the US Census Bureau and CDC—estimate the national rate of having a working CO detector in a home is 32% to 40%, with a lower prevalence among those living in manufactured housing, renting a home, or living below the poverty level.10
What is the utilization of CO detectors by ED patients?
Case conclusion
After hospital admission and treatment, both patients were discharged on hospital day 2 with a return to a baseline mental status. Neither patient reported neurological sequelae or new cognitive changes when a follow up call was placed more than 6 months after HBO treatment. The couple furthermore reported that they installed a CO detector upon their return home.
Dr West is a resident, department of emergency medicine, Albert Einstein College of Medicine, Bronx, New York.
Dr McGregor is a resident, department of emergency medicine, Albert Einstein College of Medicine, Bronx, New York.
Dr Touger is an associate professor of clinical emergency medicine, department of emergency medicine, Albert Einstein College of Medicine, Bronx, New York. He is also medical director of the Jacobi Medical Center hyperbaric chamber.
Dr Nelson, editor of “Case Studies in Toxicology,” is a professor in the department of emergency medicine and director of the medical toxicology fellowship program at New York University School of Medicine and New York City Poison Control Center. He is also associate editor, toxicology, of the EMERGENCY MEDICINE editorial board.
Case
An 84-year-old woman with a history of hypertension and dyslipidemia and her husband, an 88-year-old man with a history of dementia and coronary artery disease, presented to the ED via EMS after neighbors discovered the woman lying on her living room floor, responding only to painful stimuli. Earlier in the evening, the same neighbors had helped the husband to bed after noticing that he had become lethargic. The EMS report indicated that a car had been left running in a closed garage of the patients’ home. The fire department identified an ambient carbon monoxide (CO) concentration of 88 ppm.
Upon arrival to the ED, the woman’s vital signs were: blood pressure (BP), 130/74 mm Hg; heart rate (HR), 63 beats/minute; respiratory rate (RR), 16 breaths/minute; temperature, 99°F. Oxygen saturation was 99% on room air. Her husband’s vital signs were: BP, 150/66 mm Hg; HR, 59 beats/minute; RR, 19 breaths/minute; temperature, 98°F; oxygen saturation was 98% on room air.
What is carbon monoxide poisoning?
Carbon monoxide is a colorless and odorless toxic gas produced by incomplete combustion of carbon-based fuel. Common sources in the United States include portable generators, gas-powered furnaces, cooking appliances, poorly ventilated home-heating systems, and motor vehicles (Box 1).1
Carbon monoxide is the leading cause of unintentional poisoning deaths in the United States,1 resulting in more than 20,000 ED visits and 2,000 hospital admissions. Nearly three-fourths of these deaths are due to exposures in the home, with more than half occurring during the months of November through February.2,3 The average cost of a hospital admission for confirmed CO poisoning is over $11,000, with a cumulative nationwide total cost of over $26 million per year. While the hospitalization rate for persons aged 18 to 44 years is only 6.7%, the admittance rates for persons aged 65 to 84 years and older than 85 years are 33% and 43%, respectively.3 Although there has been a slight decline in the incidence of CO poisoning over the past 10 years, it is still a public health concern (Figure 1).2
Who is most susceptible to motor vehicle-related carbon monoxide poisoning?
The US Centers for Disease Control and Prevention (CDC) reports that motor vehicles are the second most common source of CO exposure.4 A study of US news media reports covering a 2.5-year period revealed that 8% of such poisonings were the result of a motor vehicle left running in a garage—the overall mortality rate of which is suggested to be significantly higher than that of other sources of CO exposure.5
Approximately 430 deaths per year are caused by unintentional, nonfire-related CO poisoning,6 and the CDC reports the death rate is highest in persons older than age 65 years.1 The death rate from these exposures is more than three times higher in men than women (Figure 2).6 In addition, older patients are disproportionately affected: In US news media-reported cases of CO poisoning that included patient age, 29% occurred in persons older than age 80 years.5 Moreover, in approximately one-third of motor vehicle-related deaths due to CO poisoning, nearly all of patients older than age 80 years were found dead at the scene of exposure. These reports suggest that the elderly are at greater risk for CO exposure due to age-related cognitive changes, physical inability to escape a toxic environment once becoming symptomatic, and a greater susceptibility to poisoning due to comorbid conditions.5
Case Continued
The husband and wife’s initial carboxyhemoglobin concentrations in this case were 35% and 13%, respectively. Both were treated with hyperbaric oxygen (HBO) without complication. During their inpatient stay, the woman noted that their home did not have a CO detector.
What is the role of hyperbaric oxygen therapy as a treatment option for CO poisoning?
Hyperbaric oxygen therapy greatly accelerates the dissociation of hemoglobin from CO, reduces free radical-related cellular damage, and may have a role in preventing adverse neurological sequelae in the setting of CO poisoning. Although controversy exists, HBO therapy is generally indicated in select patients with elevated CO levels and abnormal neurological findings, cardiovascular findings, or persistent metabolic acidosis. While few ED patients with CO exposure receive HBO therapy, over 20% of patients requiring inpatient hospitalization receive treatment.3
What preventive measures can be taken to reduce motor vehicle-related CO poisoning?
The literature supports the enforcement of motor vehicle emissions standards and the proper use of home CO detectors as primary preventive strategies. Computerized data from the CDC, US Census Bureau, and US Environmental Protection Agency from 1968 to 1998 were used to evaluate the influence of national vehicle emissions policies on CO-related mortality. The Clean Air Act of 1970 set environmental limits on CO emissions from automobiles at 15.0 g/mile in 1975; the EPA further reduced this standard to 3.4 g/mile for automobiles manufactured after 1981. After the enforcement of standards set forth by the Clean Air Act and the introduction of the catalytic converter in 1975, CO emissions from automobiles decreased by an estimated 76.3%, and unintentional motor vehicle-related CO deaths declined by 81.3% (Figure 3).7 (Catalytic converters contain elements [eg, platinum] that catalyze the oxidation of CO to carbon dioxide.)
Since CO exposure occurs primarily in the home, the installation of battery-powered or battery-backed CO alarms—both in the home and garage—can prevent poisoning. These detectors are inexpensive and available at common retail stores. Unfortunately, despite the easy availability and access to CO detectors, only 39 states currently have legislation mandating their use, and approximately two-thirds of the states with existing legislation only require CO detectors in newly built structures.8
In 2010, the state of New York enacted legislation known as “Amanda’s Law,” (named after a teenaged girl whose death was caused by CO poisoning from a defective boiler) mandating CO detectors in all one- and two-family homes with heating sources that may emit CO or have attached garages. However, an industry survey in 2011 found that nearly half of New York families were not aware of this law.9 The two largest surveys on home CO detector use—those conducted by the US Census Bureau and CDC—estimate the national rate of having a working CO detector in a home is 32% to 40%, with a lower prevalence among those living in manufactured housing, renting a home, or living below the poverty level.10
What is the utilization of CO detectors by ED patients?
Case conclusion
After hospital admission and treatment, both patients were discharged on hospital day 2 with a return to a baseline mental status. Neither patient reported neurological sequelae or new cognitive changes when a follow up call was placed more than 6 months after HBO treatment. The couple furthermore reported that they installed a CO detector upon their return home.
Dr West is a resident, department of emergency medicine, Albert Einstein College of Medicine, Bronx, New York.
Dr McGregor is a resident, department of emergency medicine, Albert Einstein College of Medicine, Bronx, New York.
Dr Touger is an associate professor of clinical emergency medicine, department of emergency medicine, Albert Einstein College of Medicine, Bronx, New York. He is also medical director of the Jacobi Medical Center hyperbaric chamber.
Dr Nelson, editor of “Case Studies in Toxicology,” is a professor in the department of emergency medicine and director of the medical toxicology fellowship program at New York University School of Medicine and New York City Poison Control Center. He is also associate editor, toxicology, of the EMERGENCY MEDICINE editorial board.
- Centers for Disease Control and Prevention. Carbon monoxide-related deaths—United States, 1999-2004. MMWR Morb Mortal Wkly Rep. 2007;56(50):1309-1312.
- Centers for Disease Control and Prevention. Carbon mononoxide exposures—United States, 2000-2009. MMWR Morb Mortal Wkly Rep. 2011;60(30):1014-1017.
- Iqbal S, Law HZ, Clower JH, Yip FY, Elixhauser A. Hospital burden of unintentional carbon monoxide poisoning in the United States, 2007. Am J Emerg Med. 2012;30(5):657-664.
- Centers for Disease Control and Prevention. Nonfatal, unintentional, non-fire-related carbon monoxide exposures—United States, 2004-2006. MMWR Morb Mortal Wkly Rep. 2008;57(33):896-899.
- Hampson NB. Residential carbon monoxide poisoning from motor vehicles. Am J Emerg Med. 2011;29(1):75-77.
- Centers for Disease Control and Prevention. Average annual number of deaths and death rates from unintentional, non-fire-related carbon monoxide poisoning, by sex and age group—United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2014;63(3):65.
- Mott JA, Wolfe MI, Alverson CJ, et al. National vehicle emissions policies and practices and declining US carbon monoxide-related mortality. JAMA. 2002;288(8):988-995.
- Carbon monoxide detectors: state statutes. National Conference of State Legislatures Web site. http://www.ncsl.org/research/environment-and-natural-resources/carbon-monoxide-detectors-state-statutes.aspx. Accessed March 11, 2014.
- Survey results: New York homeowners and the risk of carbon monoxide poisoning. Kidde Web site. http://www.kidde.com/PressRoom/Pages/SurveyResultsNYHomeownersCORisks.aspx. Accessed March 11, 2014.
- Iqbal S, Clower JH, King M, Bell J, Yip YF. National carbon monoxide poisoning surveillance framework and recent estimates. Public Health Rep. 2012;127(5):486-496.
- Johnson-Arbor K, Liebman DL, Carter EM. A survey of residential carbon monoxide detector utilization among Connecticut Emergency Department patients. Clin Toxicol (Phila). 2012;50(5):384-389.
- Centers for Disease Control and Prevention. Carbon monoxide-related deaths—United States, 1999-2004. MMWR Morb Mortal Wkly Rep. 2007;56(50):1309-1312.
- Centers for Disease Control and Prevention. Carbon mononoxide exposures—United States, 2000-2009. MMWR Morb Mortal Wkly Rep. 2011;60(30):1014-1017.
- Iqbal S, Law HZ, Clower JH, Yip FY, Elixhauser A. Hospital burden of unintentional carbon monoxide poisoning in the United States, 2007. Am J Emerg Med. 2012;30(5):657-664.
- Centers for Disease Control and Prevention. Nonfatal, unintentional, non-fire-related carbon monoxide exposures—United States, 2004-2006. MMWR Morb Mortal Wkly Rep. 2008;57(33):896-899.
- Hampson NB. Residential carbon monoxide poisoning from motor vehicles. Am J Emerg Med. 2011;29(1):75-77.
- Centers for Disease Control and Prevention. Average annual number of deaths and death rates from unintentional, non-fire-related carbon monoxide poisoning, by sex and age group—United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2014;63(3):65.
- Mott JA, Wolfe MI, Alverson CJ, et al. National vehicle emissions policies and practices and declining US carbon monoxide-related mortality. JAMA. 2002;288(8):988-995.
- Carbon monoxide detectors: state statutes. National Conference of State Legislatures Web site. http://www.ncsl.org/research/environment-and-natural-resources/carbon-monoxide-detectors-state-statutes.aspx. Accessed March 11, 2014.
- Survey results: New York homeowners and the risk of carbon monoxide poisoning. Kidde Web site. http://www.kidde.com/PressRoom/Pages/SurveyResultsNYHomeownersCORisks.aspx. Accessed March 11, 2014.
- Iqbal S, Clower JH, King M, Bell J, Yip YF. National carbon monoxide poisoning surveillance framework and recent estimates. Public Health Rep. 2012;127(5):486-496.
- Johnson-Arbor K, Liebman DL, Carter EM. A survey of residential carbon monoxide detector utilization among Connecticut Emergency Department patients. Clin Toxicol (Phila). 2012;50(5):384-389.