User login
When should you treat scabies empirically?
Empirically treat patients when they have pruritus and lesions typical of scabies in at least 2 places—even if there is no known household contact diagnosed with scabies, and even if the diagnosis cannot be confirmed by light microscopy (strength of recommendation [SOR]: B, based on a single large cohort study). Also give empiric treatment to all sexual and household contacts of anyone diagnosed with scabies (SOR: C, based on expert opinion).
In institutional settings such as hospitals, nursing homes, or residential facilities, treat the entire at-risk population empirically to prevent epidemics (SOR: C, based on expert opinion). In hospital settings, give empiric treatment to health care workers with skin exposure to patients with scabies (SOR: B, based on case-control study).
Treating empirically saves money (and unnecessary itching)
Barbara Walker, DO
New Hanover regional Medical Center residency in Family Medicine, University of North Carolina, Wilmington
During my medical training and years in the military, I have seen patients who suffered prolonged itching because they had no microscopic confirmation of scabies, but who cleared quickly with treatment after a skin biopsy identified scabies. This has given me a “short fuse” for treating empirically in my own clinics.
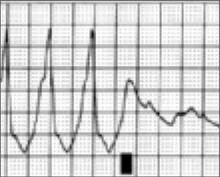
Though I always encourage the residents to do a scraping—since the microscopic confirmation is one of those “oh, wow!” findings when it is positive (FIGURE)—it is reassuring to know that evidence exists for opting to treat without confirmation. It also saves the patient the cost of the skin scraping and microscopy—important for the increasing numbers of cash-paying, uninsured patients.
Permethrin is relatively safe (rated category B in pregnancy), usually affordable, and well-tolerated; the hardest part of the empiric treatment may be the emotional impact on the patient who is told his skin has a “parasitic infestation.” (I’m itching at the thought!)
Evidence summary
Clinical diagnosis of scabies begins with pruritus, typical lesions in a distribution consistent with scabies—finger webs, wrists, axillae, elbows, buttocks, genitalia of men, breasts of women—and possible exposure. Clinical diagnosis can be confirmed by skin scrapings from characteristic lesions, such as burrows. When these scrapings are examined under light microscopy, they can show mites, eggs, or feces from the mites (FIGURE). However, this technique depends greatly on operator experience and skill, and a lack of light microscopy findings does not rule out scabies.1
The only study we found that investigated the sensitivity of clinical features in diagnosing scabies was done in sub-Saharan Africa.2 In this study, the presence of diffuse itching, plus lesions in at least 2 locations typical with scabies or a household member with itch, had 100% sensitivity and 96.9% specificity for scabies infection. This study used the evaluation of a dermatologist as a gold standard. The authors propose that treatment based on clinical findings with or without microscopic confirmation is appropriate; however, it is not clear how these data translate to a primary care population with a lower prevalence of scabies.
FIGURE
The “Oh, wow!” test
I always encourage residents to do a scraping, since the microscopic confirmation is one of those “oh, wow!” findings when it is positive.
It is reassuring to know that evidence exists for opting to treat without confirmation. It also saves the patient the cost of the skin scraping and microscopy—important for the increasing numbers of cash-paying, uninsured patients.
—Barbara Walker, Do
Long stretches without symptoms play role in treatment
To date, no controlled trials address whether empiric treatment of asymptomatic contacts or family members of those with scabies decreases its spread. However, it is known that an initial infestation with scabies will not lead to pruritus for up to 4 to 6 weeks.1 Asymptomatic contacts can be infected with scabies, and can transmit this infection to others before symptoms even occur.
Given the long period of asymptomatic infestation, prevention of epidemics in institutions such as hospitals, nursing homes, and residential facilities is of particular importance. One case-control study, performed at a large tertiary-care teaching hospital, demonstrated that health care workers on a service having a patient with undiagnosed scabies were 5.3 times more likely to develop a pruritic rash than those in other units.3
Health care workers with more skin-to-skin contact with the patients (nurses, nursing students, and physical therapists) were 4.5 times more likely to develop scabies compared with those in less physical contact (physicians, medical students, and occupational therapists). Among the symptomatic health care workers, 17% of their household contacts developed scabies, too.
Permethrin vs lindane? Which is better?
A 2000 Cochrane review, updated in 2002, concluded that permethrin was superior to lindane for topical treatment of scabies.4,5 Combining 4 trials with 718 patients, permethrin 5% appeared better than lindane 1% (odds ratio=0.66; 95% confidence interval, 0.46–0.95). However, there was significant heterogeneity between the studies, and the largest trial (n=467) found no difference.
Oral ivermectin, though costly, is an effective alternative for those who do not tolerate topical treatment. See the TABLE for a summary of treatment recommendations.
TABLE
Recommended treatment for scabies infection
| DIAGNOSIS | RECOMMENDED THERAPY | SOR |
|---|---|---|
| High-risk individual with exposure | Permethrin 5% topical solution (single overnight application) | A |
| Typical scabies infection | Permethrin 5% topical solution (single overnight application) | A |
| Crusted (Norwegian) scabies | oral ivermectin 200 mcg/kg single dose repeated in 14 days | B |
| Scabies in patient with HIV | Oral ivermectin 200 mcg/kg single dose repeated in 14 days | B |
| Data taken from 2000 Cochrane Systematic Review.4 and 2002 update5 | ||
| SOR, strength of recommendation. | ||
Recommendations from others
Guidelines released by the Centers for Disease Control and Prevention in 2002 regarding the treatment of sexually transmitted diseases state that both sexual and close personal or household contacts of patients diagnosed with scabies within the preceding month should be examined and treated.6
Another guideline, developed by the British Association of Sexual Health and HIV, recommends empiric treatment of sexual, household, and institutional contacts of those with scabies. This guideline recommends treating those who were in contact with the scabies patient within 2 months of his diagnosis; this time frame, though, is arbitrary.7 No evidence grading was given for these recommendations, which are based on expert opinion.
1. Orion E, Marcos B, Davidovici B, Wolf R. Itch and scratch: scabies and pediculosis. Clin Dermatol 2006;24:168-175.
2. Mahe A, Faye O, N’Diaye HT, et al. Definition of an algorithm for the management of common skin diseases at primary health care level in sub-Saharan Africa. Trans R Soc Trop Med Hyg 2005;99:39-47.
3. Obasanjo OO, Wu P, Conlon M, et al. An outbreak of scabies in a teaching hospital: lessons learned. Infect Control Hosp Epidemiol 2001;22:13-18.
4. Walker GJA, Johnstone PW. Interventions for treating scabies. Cochrane Database Syst Rev 2000;(3):CD000320.
5. Walker G, Johnstone P. Scabies. Clin Evid 2002;8:1745-1752.
6. Ectoparasitic infections. Sexually transmitted diseases treatment guidelines 2002. Centers for Disease Control and Prevention. MMWR Recomm Rep 2002;51:6709.
7. Scott G. 2002 National Guideline on the management of scabies. Clinical Effectiveness Group. Developed by British Association of Sexual Health and HIV–Medical Specialty Society 2002.
Empirically treat patients when they have pruritus and lesions typical of scabies in at least 2 places—even if there is no known household contact diagnosed with scabies, and even if the diagnosis cannot be confirmed by light microscopy (strength of recommendation [SOR]: B, based on a single large cohort study). Also give empiric treatment to all sexual and household contacts of anyone diagnosed with scabies (SOR: C, based on expert opinion).
In institutional settings such as hospitals, nursing homes, or residential facilities, treat the entire at-risk population empirically to prevent epidemics (SOR: C, based on expert opinion). In hospital settings, give empiric treatment to health care workers with skin exposure to patients with scabies (SOR: B, based on case-control study).
Treating empirically saves money (and unnecessary itching)
Barbara Walker, DO
New Hanover regional Medical Center residency in Family Medicine, University of North Carolina, Wilmington
During my medical training and years in the military, I have seen patients who suffered prolonged itching because they had no microscopic confirmation of scabies, but who cleared quickly with treatment after a skin biopsy identified scabies. This has given me a “short fuse” for treating empirically in my own clinics.
Though I always encourage the residents to do a scraping—since the microscopic confirmation is one of those “oh, wow!” findings when it is positive (FIGURE)—it is reassuring to know that evidence exists for opting to treat without confirmation. It also saves the patient the cost of the skin scraping and microscopy—important for the increasing numbers of cash-paying, uninsured patients.
Permethrin is relatively safe (rated category B in pregnancy), usually affordable, and well-tolerated; the hardest part of the empiric treatment may be the emotional impact on the patient who is told his skin has a “parasitic infestation.” (I’m itching at the thought!)
Evidence summary
Clinical diagnosis of scabies begins with pruritus, typical lesions in a distribution consistent with scabies—finger webs, wrists, axillae, elbows, buttocks, genitalia of men, breasts of women—and possible exposure. Clinical diagnosis can be confirmed by skin scrapings from characteristic lesions, such as burrows. When these scrapings are examined under light microscopy, they can show mites, eggs, or feces from the mites (FIGURE). However, this technique depends greatly on operator experience and skill, and a lack of light microscopy findings does not rule out scabies.1
The only study we found that investigated the sensitivity of clinical features in diagnosing scabies was done in sub-Saharan Africa.2 In this study, the presence of diffuse itching, plus lesions in at least 2 locations typical with scabies or a household member with itch, had 100% sensitivity and 96.9% specificity for scabies infection. This study used the evaluation of a dermatologist as a gold standard. The authors propose that treatment based on clinical findings with or without microscopic confirmation is appropriate; however, it is not clear how these data translate to a primary care population with a lower prevalence of scabies.
FIGURE
The “Oh, wow!” test
I always encourage residents to do a scraping, since the microscopic confirmation is one of those “oh, wow!” findings when it is positive.
It is reassuring to know that evidence exists for opting to treat without confirmation. It also saves the patient the cost of the skin scraping and microscopy—important for the increasing numbers of cash-paying, uninsured patients.
—Barbara Walker, Do
Long stretches without symptoms play role in treatment
To date, no controlled trials address whether empiric treatment of asymptomatic contacts or family members of those with scabies decreases its spread. However, it is known that an initial infestation with scabies will not lead to pruritus for up to 4 to 6 weeks.1 Asymptomatic contacts can be infected with scabies, and can transmit this infection to others before symptoms even occur.
Given the long period of asymptomatic infestation, prevention of epidemics in institutions such as hospitals, nursing homes, and residential facilities is of particular importance. One case-control study, performed at a large tertiary-care teaching hospital, demonstrated that health care workers on a service having a patient with undiagnosed scabies were 5.3 times more likely to develop a pruritic rash than those in other units.3
Health care workers with more skin-to-skin contact with the patients (nurses, nursing students, and physical therapists) were 4.5 times more likely to develop scabies compared with those in less physical contact (physicians, medical students, and occupational therapists). Among the symptomatic health care workers, 17% of their household contacts developed scabies, too.
Permethrin vs lindane? Which is better?
A 2000 Cochrane review, updated in 2002, concluded that permethrin was superior to lindane for topical treatment of scabies.4,5 Combining 4 trials with 718 patients, permethrin 5% appeared better than lindane 1% (odds ratio=0.66; 95% confidence interval, 0.46–0.95). However, there was significant heterogeneity between the studies, and the largest trial (n=467) found no difference.
Oral ivermectin, though costly, is an effective alternative for those who do not tolerate topical treatment. See the TABLE for a summary of treatment recommendations.
TABLE
Recommended treatment for scabies infection
| DIAGNOSIS | RECOMMENDED THERAPY | SOR |
|---|---|---|
| High-risk individual with exposure | Permethrin 5% topical solution (single overnight application) | A |
| Typical scabies infection | Permethrin 5% topical solution (single overnight application) | A |
| Crusted (Norwegian) scabies | oral ivermectin 200 mcg/kg single dose repeated in 14 days | B |
| Scabies in patient with HIV | Oral ivermectin 200 mcg/kg single dose repeated in 14 days | B |
| Data taken from 2000 Cochrane Systematic Review.4 and 2002 update5 | ||
| SOR, strength of recommendation. | ||
Recommendations from others
Guidelines released by the Centers for Disease Control and Prevention in 2002 regarding the treatment of sexually transmitted diseases state that both sexual and close personal or household contacts of patients diagnosed with scabies within the preceding month should be examined and treated.6
Another guideline, developed by the British Association of Sexual Health and HIV, recommends empiric treatment of sexual, household, and institutional contacts of those with scabies. This guideline recommends treating those who were in contact with the scabies patient within 2 months of his diagnosis; this time frame, though, is arbitrary.7 No evidence grading was given for these recommendations, which are based on expert opinion.
Empirically treat patients when they have pruritus and lesions typical of scabies in at least 2 places—even if there is no known household contact diagnosed with scabies, and even if the diagnosis cannot be confirmed by light microscopy (strength of recommendation [SOR]: B, based on a single large cohort study). Also give empiric treatment to all sexual and household contacts of anyone diagnosed with scabies (SOR: C, based on expert opinion).
In institutional settings such as hospitals, nursing homes, or residential facilities, treat the entire at-risk population empirically to prevent epidemics (SOR: C, based on expert opinion). In hospital settings, give empiric treatment to health care workers with skin exposure to patients with scabies (SOR: B, based on case-control study).
Treating empirically saves money (and unnecessary itching)
Barbara Walker, DO
New Hanover regional Medical Center residency in Family Medicine, University of North Carolina, Wilmington
During my medical training and years in the military, I have seen patients who suffered prolonged itching because they had no microscopic confirmation of scabies, but who cleared quickly with treatment after a skin biopsy identified scabies. This has given me a “short fuse” for treating empirically in my own clinics.
Though I always encourage the residents to do a scraping—since the microscopic confirmation is one of those “oh, wow!” findings when it is positive (FIGURE)—it is reassuring to know that evidence exists for opting to treat without confirmation. It also saves the patient the cost of the skin scraping and microscopy—important for the increasing numbers of cash-paying, uninsured patients.
Permethrin is relatively safe (rated category B in pregnancy), usually affordable, and well-tolerated; the hardest part of the empiric treatment may be the emotional impact on the patient who is told his skin has a “parasitic infestation.” (I’m itching at the thought!)
Evidence summary
Clinical diagnosis of scabies begins with pruritus, typical lesions in a distribution consistent with scabies—finger webs, wrists, axillae, elbows, buttocks, genitalia of men, breasts of women—and possible exposure. Clinical diagnosis can be confirmed by skin scrapings from characteristic lesions, such as burrows. When these scrapings are examined under light microscopy, they can show mites, eggs, or feces from the mites (FIGURE). However, this technique depends greatly on operator experience and skill, and a lack of light microscopy findings does not rule out scabies.1
The only study we found that investigated the sensitivity of clinical features in diagnosing scabies was done in sub-Saharan Africa.2 In this study, the presence of diffuse itching, plus lesions in at least 2 locations typical with scabies or a household member with itch, had 100% sensitivity and 96.9% specificity for scabies infection. This study used the evaluation of a dermatologist as a gold standard. The authors propose that treatment based on clinical findings with or without microscopic confirmation is appropriate; however, it is not clear how these data translate to a primary care population with a lower prevalence of scabies.
FIGURE
The “Oh, wow!” test
I always encourage residents to do a scraping, since the microscopic confirmation is one of those “oh, wow!” findings when it is positive.
It is reassuring to know that evidence exists for opting to treat without confirmation. It also saves the patient the cost of the skin scraping and microscopy—important for the increasing numbers of cash-paying, uninsured patients.
—Barbara Walker, Do
Long stretches without symptoms play role in treatment
To date, no controlled trials address whether empiric treatment of asymptomatic contacts or family members of those with scabies decreases its spread. However, it is known that an initial infestation with scabies will not lead to pruritus for up to 4 to 6 weeks.1 Asymptomatic contacts can be infected with scabies, and can transmit this infection to others before symptoms even occur.
Given the long period of asymptomatic infestation, prevention of epidemics in institutions such as hospitals, nursing homes, and residential facilities is of particular importance. One case-control study, performed at a large tertiary-care teaching hospital, demonstrated that health care workers on a service having a patient with undiagnosed scabies were 5.3 times more likely to develop a pruritic rash than those in other units.3
Health care workers with more skin-to-skin contact with the patients (nurses, nursing students, and physical therapists) were 4.5 times more likely to develop scabies compared with those in less physical contact (physicians, medical students, and occupational therapists). Among the symptomatic health care workers, 17% of their household contacts developed scabies, too.
Permethrin vs lindane? Which is better?
A 2000 Cochrane review, updated in 2002, concluded that permethrin was superior to lindane for topical treatment of scabies.4,5 Combining 4 trials with 718 patients, permethrin 5% appeared better than lindane 1% (odds ratio=0.66; 95% confidence interval, 0.46–0.95). However, there was significant heterogeneity between the studies, and the largest trial (n=467) found no difference.
Oral ivermectin, though costly, is an effective alternative for those who do not tolerate topical treatment. See the TABLE for a summary of treatment recommendations.
TABLE
Recommended treatment for scabies infection
| DIAGNOSIS | RECOMMENDED THERAPY | SOR |
|---|---|---|
| High-risk individual with exposure | Permethrin 5% topical solution (single overnight application) | A |
| Typical scabies infection | Permethrin 5% topical solution (single overnight application) | A |
| Crusted (Norwegian) scabies | oral ivermectin 200 mcg/kg single dose repeated in 14 days | B |
| Scabies in patient with HIV | Oral ivermectin 200 mcg/kg single dose repeated in 14 days | B |
| Data taken from 2000 Cochrane Systematic Review.4 and 2002 update5 | ||
| SOR, strength of recommendation. | ||
Recommendations from others
Guidelines released by the Centers for Disease Control and Prevention in 2002 regarding the treatment of sexually transmitted diseases state that both sexual and close personal or household contacts of patients diagnosed with scabies within the preceding month should be examined and treated.6
Another guideline, developed by the British Association of Sexual Health and HIV, recommends empiric treatment of sexual, household, and institutional contacts of those with scabies. This guideline recommends treating those who were in contact with the scabies patient within 2 months of his diagnosis; this time frame, though, is arbitrary.7 No evidence grading was given for these recommendations, which are based on expert opinion.
1. Orion E, Marcos B, Davidovici B, Wolf R. Itch and scratch: scabies and pediculosis. Clin Dermatol 2006;24:168-175.
2. Mahe A, Faye O, N’Diaye HT, et al. Definition of an algorithm for the management of common skin diseases at primary health care level in sub-Saharan Africa. Trans R Soc Trop Med Hyg 2005;99:39-47.
3. Obasanjo OO, Wu P, Conlon M, et al. An outbreak of scabies in a teaching hospital: lessons learned. Infect Control Hosp Epidemiol 2001;22:13-18.
4. Walker GJA, Johnstone PW. Interventions for treating scabies. Cochrane Database Syst Rev 2000;(3):CD000320.
5. Walker G, Johnstone P. Scabies. Clin Evid 2002;8:1745-1752.
6. Ectoparasitic infections. Sexually transmitted diseases treatment guidelines 2002. Centers for Disease Control and Prevention. MMWR Recomm Rep 2002;51:6709.
7. Scott G. 2002 National Guideline on the management of scabies. Clinical Effectiveness Group. Developed by British Association of Sexual Health and HIV–Medical Specialty Society 2002.
1. Orion E, Marcos B, Davidovici B, Wolf R. Itch and scratch: scabies and pediculosis. Clin Dermatol 2006;24:168-175.
2. Mahe A, Faye O, N’Diaye HT, et al. Definition of an algorithm for the management of common skin diseases at primary health care level in sub-Saharan Africa. Trans R Soc Trop Med Hyg 2005;99:39-47.
3. Obasanjo OO, Wu P, Conlon M, et al. An outbreak of scabies in a teaching hospital: lessons learned. Infect Control Hosp Epidemiol 2001;22:13-18.
4. Walker GJA, Johnstone PW. Interventions for treating scabies. Cochrane Database Syst Rev 2000;(3):CD000320.
5. Walker G, Johnstone P. Scabies. Clin Evid 2002;8:1745-1752.
6. Ectoparasitic infections. Sexually transmitted diseases treatment guidelines 2002. Centers for Disease Control and Prevention. MMWR Recomm Rep 2002;51:6709.
7. Scott G. 2002 National Guideline on the management of scabies. Clinical Effectiveness Group. Developed by British Association of Sexual Health and HIV–Medical Specialty Society 2002.
Evidence-based answers from the Family Physicians Inquiries Network
Should you restrict your cardiac patient from driving?
That depends, of course, on your patient’s particular condition, but your decision can be guided by various cardiovascular society consensus conferences, such as the one from the Canadian Cardiovascular society (TABLE), since no evidence-based guidelines exist. It seems sensible to say, though, that impairment of consciousness associated with any heart disease needs further evaluation, with a complete restriction of driving for at least 6 months (strength of recommendation [SOR]: C, based on expert opinion and extrapolation from observational studies).
Helpful guide stratifies risk
Drew Malloy, MD
University of California Santa Cruz Student Health Service
This review points out the lack of evidence for a common clinical problem. Evidence is scant, but the TABLE helps the busy clinician stratify risks for different types of heart disease and provides some rational basis for the duration of restrictions. The existing expert consensus guidelines are sensible and useful when discussing this important issue with patients and their families after diagnosis of heart disease. However, to be quite frank, when I am driving I am more worried about the teenager on a cell phone behind the wheel of an SUV than my grandmother with an ICD.
Evidence summary
Our search identified no randomized controlled trials, no systematic reviews, 6 observational studies, and 3 consensus panel guidelines on risks from driving and cardiovascular disease. No studies deal specifically with coronary artery disease, congestive heart failure, or valvular heart disease and the risk of motor vehicle crashes for patients with these conditions. A population-based case control study of 5204 male drivers ages 45 to 70 in Quebec found no increased risk of crash for drivers with unspecified cardiovascular disease.1
Car accidents among ICD patients are low
The most studied patients are those with life-threatening ventricular arrhythmias—particularly those with implantable cardioverter-defibrillators (ICDs). Based on observational studies of patients and their physicians, patients with ventricular arrhythmias treated with ICDs do not have an increased risk of motor vehicle crashes.2-4 The largest of the studies2 prospectively and anonymously surveyed 627 patients from the Antiarrhythmics vs Implantable Defibrillators Trial. During follow-up, 2% of patients had a syncopal episode while driving, and 11% had dizziness or palpitations that required stopping the vehicle.
Of the 55 car crashes that occurred during 1619 patient-years after resumption of driving, 11% were preceded by a possible symptom of arrhythmia (0.4% per patient per year). The annual incidence of car accidents for patients with an ICD was 3.4% per patient-year. This is substantially lower than the 7.1% rate among the general driving population in the US.
Recommendations from others
Expert panel guidelines regarding fitness to drive for patients with heart disease are available from the Canadian Cardiovascular Society (CCS),5 the European Society of Cardiology, the American Heart Association, the North American Society of Pacing and Physiology,6 and the Cardiac Society of Australia and New Zealand.7 The 2004 CCS guidelines are the most recent and include a “Risk of Harm” formula that attempts to assign a quantitative level of risk to drivers with heart disease. These guidelines appear sensible but are not evidence-based (TABLE).
TABLE
Should your heart patient get behind the wheel? A helpful guide
| CONDITIONS | TIME TO RESUME DRIVING |
|---|---|
| Coronary artery disease | |
| Coronary bypass graft | 1 month after discharge |
| ST elevation myocardial infarction | 1 month after discharge |
| Unstable angina | |
| – PCI during hospital stay | 48 hours after PCI |
| – PCI not done during hospital stay | 7 days after discharge |
| Ventricular arrhythmias | |
| Non-sustained VT with no loss of consciousness | No restriction |
| VF or unstable VT | 6 months after event |
| Implantable cardioverter defibrillator | |
| For VF or VT with decreased level of consciousness | 6 months after event |
| Rhythm disturbances | |
| Atrial flutter (without impaired level of consciousness) | No restriction |
| Supraventricular tachycardia | No restriction |
| Atrial fibrillation | No restriction |
| Heart block | |
| First- and second-degree atrioventricular block, Mobitz Type 1 (without impairment of consciousness) | No restriction |
| Second-degree atrioventricular block, Mobitz Type II | No driving |
| Permanent pacemaker | |
| All patients | 1 week after implant; normal pacer function; no impaired level of consciousness |
| Congestive heart failure | |
| NYHA Classes I–III | No restriction |
| NYHA Classes IV | No driving |
| Adapted from Canadian Cardiovascular Society Consensus Conference 2003.5 | |
| PCI, percutaneous coronary intervention; VF, ventricular fibrillation; | |
| VT, ventricular tachycardia; NYHA, New York Heart Association | |
1. Guibert R, Potvin L, Ciampi A, Loiselle J, Philibert L, Franco ED. Are drivers with CVD more at risk for motor vehicle crashes? Study of men aged 45 to 70. Can Fam Physician 1998;44:770-776.
2. Akiyama T, Powell JL, Mitchell LB, Ehlert FA, Baessler C. Resumption of driving after life-threatening ventricular tachyarrhythmia. N Engl J Med 2001;345:391-397.
3. Trappe HJ, Wenzlaff P, Grellman G. Should patients with implantable cardioverter defibrillators be allowed to drive? Observations in 291 patients from a single center over an 11-year period. J Interv Card Electrophysiol 1998;2:193-201.
4. Curtis AB, Conti JB, Tucker KJ, Kubilis PS, Reilly RE, Woodard DA. Motor vehicle accidents in patients with an implantable cardioverter-defibrillator. J Am Coll Cardiol 1995;26:180-184.
5. CCS Consensus Conference 2003: Assessment of the cardiac patient fitness to drive and fly—executive summary. Can J Cardiol 2004;20:1313-1323.
6. Epstein AE, Miles WM, Benditt DG, et al. Personal and public safety issues related to arrhythmias that may affect consciousness: Implications for regulation and physician recommendations. A medical/scientific statement from the American Heart Association and the North American Society of Pacing and Electrophysiology. Circulation 1996;94:1147-1166.
7. Cardiac Society of Australia and New Zealand. Cardiovascular Disease and Driving 2002. Available at: www.csanz.edu.au/guidelines/practice/Drivegl2002.pdf. Accessed on April 3, 2007.
That depends, of course, on your patient’s particular condition, but your decision can be guided by various cardiovascular society consensus conferences, such as the one from the Canadian Cardiovascular society (TABLE), since no evidence-based guidelines exist. It seems sensible to say, though, that impairment of consciousness associated with any heart disease needs further evaluation, with a complete restriction of driving for at least 6 months (strength of recommendation [SOR]: C, based on expert opinion and extrapolation from observational studies).
Helpful guide stratifies risk
Drew Malloy, MD
University of California Santa Cruz Student Health Service
This review points out the lack of evidence for a common clinical problem. Evidence is scant, but the TABLE helps the busy clinician stratify risks for different types of heart disease and provides some rational basis for the duration of restrictions. The existing expert consensus guidelines are sensible and useful when discussing this important issue with patients and their families after diagnosis of heart disease. However, to be quite frank, when I am driving I am more worried about the teenager on a cell phone behind the wheel of an SUV than my grandmother with an ICD.
Evidence summary
Our search identified no randomized controlled trials, no systematic reviews, 6 observational studies, and 3 consensus panel guidelines on risks from driving and cardiovascular disease. No studies deal specifically with coronary artery disease, congestive heart failure, or valvular heart disease and the risk of motor vehicle crashes for patients with these conditions. A population-based case control study of 5204 male drivers ages 45 to 70 in Quebec found no increased risk of crash for drivers with unspecified cardiovascular disease.1
Car accidents among ICD patients are low
The most studied patients are those with life-threatening ventricular arrhythmias—particularly those with implantable cardioverter-defibrillators (ICDs). Based on observational studies of patients and their physicians, patients with ventricular arrhythmias treated with ICDs do not have an increased risk of motor vehicle crashes.2-4 The largest of the studies2 prospectively and anonymously surveyed 627 patients from the Antiarrhythmics vs Implantable Defibrillators Trial. During follow-up, 2% of patients had a syncopal episode while driving, and 11% had dizziness or palpitations that required stopping the vehicle.
Of the 55 car crashes that occurred during 1619 patient-years after resumption of driving, 11% were preceded by a possible symptom of arrhythmia (0.4% per patient per year). The annual incidence of car accidents for patients with an ICD was 3.4% per patient-year. This is substantially lower than the 7.1% rate among the general driving population in the US.
Recommendations from others
Expert panel guidelines regarding fitness to drive for patients with heart disease are available from the Canadian Cardiovascular Society (CCS),5 the European Society of Cardiology, the American Heart Association, the North American Society of Pacing and Physiology,6 and the Cardiac Society of Australia and New Zealand.7 The 2004 CCS guidelines are the most recent and include a “Risk of Harm” formula that attempts to assign a quantitative level of risk to drivers with heart disease. These guidelines appear sensible but are not evidence-based (TABLE).
TABLE
Should your heart patient get behind the wheel? A helpful guide
| CONDITIONS | TIME TO RESUME DRIVING |
|---|---|
| Coronary artery disease | |
| Coronary bypass graft | 1 month after discharge |
| ST elevation myocardial infarction | 1 month after discharge |
| Unstable angina | |
| – PCI during hospital stay | 48 hours after PCI |
| – PCI not done during hospital stay | 7 days after discharge |
| Ventricular arrhythmias | |
| Non-sustained VT with no loss of consciousness | No restriction |
| VF or unstable VT | 6 months after event |
| Implantable cardioverter defibrillator | |
| For VF or VT with decreased level of consciousness | 6 months after event |
| Rhythm disturbances | |
| Atrial flutter (without impaired level of consciousness) | No restriction |
| Supraventricular tachycardia | No restriction |
| Atrial fibrillation | No restriction |
| Heart block | |
| First- and second-degree atrioventricular block, Mobitz Type 1 (without impairment of consciousness) | No restriction |
| Second-degree atrioventricular block, Mobitz Type II | No driving |
| Permanent pacemaker | |
| All patients | 1 week after implant; normal pacer function; no impaired level of consciousness |
| Congestive heart failure | |
| NYHA Classes I–III | No restriction |
| NYHA Classes IV | No driving |
| Adapted from Canadian Cardiovascular Society Consensus Conference 2003.5 | |
| PCI, percutaneous coronary intervention; VF, ventricular fibrillation; | |
| VT, ventricular tachycardia; NYHA, New York Heart Association | |
That depends, of course, on your patient’s particular condition, but your decision can be guided by various cardiovascular society consensus conferences, such as the one from the Canadian Cardiovascular society (TABLE), since no evidence-based guidelines exist. It seems sensible to say, though, that impairment of consciousness associated with any heart disease needs further evaluation, with a complete restriction of driving for at least 6 months (strength of recommendation [SOR]: C, based on expert opinion and extrapolation from observational studies).
Helpful guide stratifies risk
Drew Malloy, MD
University of California Santa Cruz Student Health Service
This review points out the lack of evidence for a common clinical problem. Evidence is scant, but the TABLE helps the busy clinician stratify risks for different types of heart disease and provides some rational basis for the duration of restrictions. The existing expert consensus guidelines are sensible and useful when discussing this important issue with patients and their families after diagnosis of heart disease. However, to be quite frank, when I am driving I am more worried about the teenager on a cell phone behind the wheel of an SUV than my grandmother with an ICD.
Evidence summary
Our search identified no randomized controlled trials, no systematic reviews, 6 observational studies, and 3 consensus panel guidelines on risks from driving and cardiovascular disease. No studies deal specifically with coronary artery disease, congestive heart failure, or valvular heart disease and the risk of motor vehicle crashes for patients with these conditions. A population-based case control study of 5204 male drivers ages 45 to 70 in Quebec found no increased risk of crash for drivers with unspecified cardiovascular disease.1
Car accidents among ICD patients are low
The most studied patients are those with life-threatening ventricular arrhythmias—particularly those with implantable cardioverter-defibrillators (ICDs). Based on observational studies of patients and their physicians, patients with ventricular arrhythmias treated with ICDs do not have an increased risk of motor vehicle crashes.2-4 The largest of the studies2 prospectively and anonymously surveyed 627 patients from the Antiarrhythmics vs Implantable Defibrillators Trial. During follow-up, 2% of patients had a syncopal episode while driving, and 11% had dizziness or palpitations that required stopping the vehicle.
Of the 55 car crashes that occurred during 1619 patient-years after resumption of driving, 11% were preceded by a possible symptom of arrhythmia (0.4% per patient per year). The annual incidence of car accidents for patients with an ICD was 3.4% per patient-year. This is substantially lower than the 7.1% rate among the general driving population in the US.
Recommendations from others
Expert panel guidelines regarding fitness to drive for patients with heart disease are available from the Canadian Cardiovascular Society (CCS),5 the European Society of Cardiology, the American Heart Association, the North American Society of Pacing and Physiology,6 and the Cardiac Society of Australia and New Zealand.7 The 2004 CCS guidelines are the most recent and include a “Risk of Harm” formula that attempts to assign a quantitative level of risk to drivers with heart disease. These guidelines appear sensible but are not evidence-based (TABLE).
TABLE
Should your heart patient get behind the wheel? A helpful guide
| CONDITIONS | TIME TO RESUME DRIVING |
|---|---|
| Coronary artery disease | |
| Coronary bypass graft | 1 month after discharge |
| ST elevation myocardial infarction | 1 month after discharge |
| Unstable angina | |
| – PCI during hospital stay | 48 hours after PCI |
| – PCI not done during hospital stay | 7 days after discharge |
| Ventricular arrhythmias | |
| Non-sustained VT with no loss of consciousness | No restriction |
| VF or unstable VT | 6 months after event |
| Implantable cardioverter defibrillator | |
| For VF or VT with decreased level of consciousness | 6 months after event |
| Rhythm disturbances | |
| Atrial flutter (without impaired level of consciousness) | No restriction |
| Supraventricular tachycardia | No restriction |
| Atrial fibrillation | No restriction |
| Heart block | |
| First- and second-degree atrioventricular block, Mobitz Type 1 (without impairment of consciousness) | No restriction |
| Second-degree atrioventricular block, Mobitz Type II | No driving |
| Permanent pacemaker | |
| All patients | 1 week after implant; normal pacer function; no impaired level of consciousness |
| Congestive heart failure | |
| NYHA Classes I–III | No restriction |
| NYHA Classes IV | No driving |
| Adapted from Canadian Cardiovascular Society Consensus Conference 2003.5 | |
| PCI, percutaneous coronary intervention; VF, ventricular fibrillation; | |
| VT, ventricular tachycardia; NYHA, New York Heart Association | |
1. Guibert R, Potvin L, Ciampi A, Loiselle J, Philibert L, Franco ED. Are drivers with CVD more at risk for motor vehicle crashes? Study of men aged 45 to 70. Can Fam Physician 1998;44:770-776.
2. Akiyama T, Powell JL, Mitchell LB, Ehlert FA, Baessler C. Resumption of driving after life-threatening ventricular tachyarrhythmia. N Engl J Med 2001;345:391-397.
3. Trappe HJ, Wenzlaff P, Grellman G. Should patients with implantable cardioverter defibrillators be allowed to drive? Observations in 291 patients from a single center over an 11-year period. J Interv Card Electrophysiol 1998;2:193-201.
4. Curtis AB, Conti JB, Tucker KJ, Kubilis PS, Reilly RE, Woodard DA. Motor vehicle accidents in patients with an implantable cardioverter-defibrillator. J Am Coll Cardiol 1995;26:180-184.
5. CCS Consensus Conference 2003: Assessment of the cardiac patient fitness to drive and fly—executive summary. Can J Cardiol 2004;20:1313-1323.
6. Epstein AE, Miles WM, Benditt DG, et al. Personal and public safety issues related to arrhythmias that may affect consciousness: Implications for regulation and physician recommendations. A medical/scientific statement from the American Heart Association and the North American Society of Pacing and Electrophysiology. Circulation 1996;94:1147-1166.
7. Cardiac Society of Australia and New Zealand. Cardiovascular Disease and Driving 2002. Available at: www.csanz.edu.au/guidelines/practice/Drivegl2002.pdf. Accessed on April 3, 2007.
1. Guibert R, Potvin L, Ciampi A, Loiselle J, Philibert L, Franco ED. Are drivers with CVD more at risk for motor vehicle crashes? Study of men aged 45 to 70. Can Fam Physician 1998;44:770-776.
2. Akiyama T, Powell JL, Mitchell LB, Ehlert FA, Baessler C. Resumption of driving after life-threatening ventricular tachyarrhythmia. N Engl J Med 2001;345:391-397.
3. Trappe HJ, Wenzlaff P, Grellman G. Should patients with implantable cardioverter defibrillators be allowed to drive? Observations in 291 patients from a single center over an 11-year period. J Interv Card Electrophysiol 1998;2:193-201.
4. Curtis AB, Conti JB, Tucker KJ, Kubilis PS, Reilly RE, Woodard DA. Motor vehicle accidents in patients with an implantable cardioverter-defibrillator. J Am Coll Cardiol 1995;26:180-184.
5. CCS Consensus Conference 2003: Assessment of the cardiac patient fitness to drive and fly—executive summary. Can J Cardiol 2004;20:1313-1323.
6. Epstein AE, Miles WM, Benditt DG, et al. Personal and public safety issues related to arrhythmias that may affect consciousness: Implications for regulation and physician recommendations. A medical/scientific statement from the American Heart Association and the North American Society of Pacing and Electrophysiology. Circulation 1996;94:1147-1166.
7. Cardiac Society of Australia and New Zealand. Cardiovascular Disease and Driving 2002. Available at: www.csanz.edu.au/guidelines/practice/Drivegl2002.pdf. Accessed on April 3, 2007.
Evidence-based answers from the Family Physicians Inquiries Network
What is the appropriate evaluation and treatment of children who are “toe walkers”?
The evaluation of toe-walking focuses on differentiating normal children from those with mild cerebral palsy. Gait analysis may be a useful diagnostic tool, but further investigation is needed to confirm its reliability (strength of recommendation [SOR]: C, based on case series).
Observation alone is generally as successful as serial casting and surgery in decreasing the frequency of toe-walking at follow-up (SOR: C, based on case series).
Avoid overmedicalizing a problem that appears to run a benign course
Vince Winkler-Prins, MD
Michigan State University, East Lansing
The challenge with idiopathic toe-walking appears to be how to discriminate it from the more serious entities of cerebral palsy and muscular dystrophy. Idiopathic toe-walking should be evident in an otherwise healthy child as he or she begins to walk. It should be bilateral, there should be no spasticity and reflexes should not be overly brisk. A few follow-up visits at 3- or 6-month intervals should reassure all that this problem is nonprogressive. I have seen many toe-walking children over the years but no toe-walking adults without cerebral palsy or muscular dystrophy. This seems to confirm this review’s findings that observation appears to be as useful as casting or surgery. Until there is a natural history study of toe-walking, we need to be watchful to not overmedicalize a problem that appears to run a benign course.
Evidence summary
Idiopathic toe-walking is a childhood condition of unknown cause characterized by persistence of a tiptoe gait pattern without evidence of neurologic, orthopedic, or psychiatric disease.1 The incidence in the general population is not known. Children with idiopathic toe-walking usually have limited ankle dorsiflexion and are able to walk with a heel-strike for short periods when asked to do so. Longitudinal data is lacking to determine whether ankle equinus is the primary cause of idiopathic toe-walking or is a consequence of chronically walking on tiptoes. A family history of toe-walking ranges from 30% to 71% in the literature and is considered a characteristic of idiopathic toe walking.2-4
Evaluation. An important element of the evaluation of idiopathic toe-walking is to distinguish it from neuromuscular disorders associated with toe-walking, such as mild cerebral palsy. Case series with small numbers of subjects (range=27–41) have used gait electromyography (EMG) to distinguish cerebral palsy from idiopathic toe-walking.4-6 The overlap in gait EMG values in cerebral palsy and idiopathic toe-walking precludes its use as a differentiating diagnostic test.
The only aspect of EMG testing that has been useful in differentiating cerebral palsy from idiopathic toe-walking is gastrocnemius coactivation during resisted knee extension—a finding indicative of neurologic pathology.5,6 Kinematic analysis and observation of gait and measurement of ankle range of motion have been studied as diagnostic tools to differentiate idiopathic toe-walking from cerebral palsy.5-8 In the largest of these 4 studies (23 children with mild cerebral palsy and 22 with idiopathic toe-walking), maximal knee extension occurred at ground contact in the idiopathic toe-walking group whereas in the mild cerebral palsy group, the knee was flexed at ground contact.7 Measurement of ankle range of motion is not reliable in distinguishing between idiopathic toe-walking and cerebral palsy groups.5-7
Treatment. Simple observation, physical therapy, serial casting, and Achilles tendon lengthening surgery have been studied in the treatment of idiopathic toe-walking.2,3,9-11 In the largest case series (n=136),10 the frequency of toe-walking decreased in 51% of those in both the observation and casted groups. In this same study, the surgical group had lower rates of toe-walking, but no direct comparisons could be made to the nonsurgical groups because the patients in the surgical group were older and had longer follow-up than the other groups.
In a retrospective comparison3 of observation (which included physical therapy and special shoes), casting, and surgery among 80 children with idiopathic toe-walking, surgery resulted in significantly higher parental satisfaction (satisfied was defined as “child rarely walks on tiptoe”), 67% vs 25% and 24% for observation and casting groups respectively (P<.05). Three smaller studies (from 13 to 18 subjects) also showed decreased toe-walking at follow-up, regardless of treatment.2,9,11
There is no convincing evidence that treatment is necessary for this condition. We found no randomized trials of treatment for idiopathic toe-walking and no follow-up studies of sufficient size and duration that evaluate long-term effects of toe walking on the patient later in life.
Recommendations from others
No recommendations or guidelines were found.
1. Hall JE, Salter RB, Bhalla SK. Congenital short tendo calcaneus. J Bone Joint Surg Br 1967;49B:695-697.
2. Hirsch G, Wagner B. The natural history of idiopathic toe-walking: a long-term follow-up of fourteen conservatively treated children. Acta Paediatr 2004;93:196-199.
3. Stricker SJ, Angulo JC. Idiopathic toe walking: a comparison of treatment methods. J Pediatr Orthop 1998;18:289-293.
4. Kalen V, Adler N, Bleck EE. Electromyography of idiopathic toe walking. J Pediatr Orthop 1986;6:31-33.
5. Policy JF, Torburn L, Rinsky LA, Rose J. Electromyographic test to differentiate mild diplegic cerebral palsy and idiopathic toe-walking. J Pediatr Orthop 2001;21:784-789.
6. Rose J, Martin JG, Torburn L, Rinsky LA, Gamble JG. Electromyographic differentiation of diplegic cerebral palsy from idiopathic toe walking: involuntary coactivation of the quadriceps and gastrocnemius. J Pediatr Orthop 1999;19:677-682.
7. Kelly IP, Jenkinson A, Stephens M, O’Brien T. The kinematic patterns of toe-walkers. J Pediatr Orthop 1997;17:478-480.
8. Hicks R, Durinick N, Gage JR. Differentiation of idiopathic toe-walking and cerebral palsy. J Pediatr Orthop 1988;8:160-163.
9. Stott NS, Walt SE, Lobb GA, Reynolds N, Nicol RO. Treatment for idiopathic toe-walking: results at skeletal maturity. J Pediatr Orthop 2004;24:63-69.
10. Eastwood DM, Menelaus MB, Dickens DR, Broughton NS, Cole WG. Idiopathic toe-walking: does treatment alter the natural history. J Pediatr Orthop B 2000;9:47-49.
11. Brouwer B, Davidson LK, Olney SJ. Serial casting in idiopathic toe-walkers and children with spastic cerebral palsy. J Pediatr Orthop 2000;20:221-225.
The evaluation of toe-walking focuses on differentiating normal children from those with mild cerebral palsy. Gait analysis may be a useful diagnostic tool, but further investigation is needed to confirm its reliability (strength of recommendation [SOR]: C, based on case series).
Observation alone is generally as successful as serial casting and surgery in decreasing the frequency of toe-walking at follow-up (SOR: C, based on case series).
Avoid overmedicalizing a problem that appears to run a benign course
Vince Winkler-Prins, MD
Michigan State University, East Lansing
The challenge with idiopathic toe-walking appears to be how to discriminate it from the more serious entities of cerebral palsy and muscular dystrophy. Idiopathic toe-walking should be evident in an otherwise healthy child as he or she begins to walk. It should be bilateral, there should be no spasticity and reflexes should not be overly brisk. A few follow-up visits at 3- or 6-month intervals should reassure all that this problem is nonprogressive. I have seen many toe-walking children over the years but no toe-walking adults without cerebral palsy or muscular dystrophy. This seems to confirm this review’s findings that observation appears to be as useful as casting or surgery. Until there is a natural history study of toe-walking, we need to be watchful to not overmedicalize a problem that appears to run a benign course.
Evidence summary
Idiopathic toe-walking is a childhood condition of unknown cause characterized by persistence of a tiptoe gait pattern without evidence of neurologic, orthopedic, or psychiatric disease.1 The incidence in the general population is not known. Children with idiopathic toe-walking usually have limited ankle dorsiflexion and are able to walk with a heel-strike for short periods when asked to do so. Longitudinal data is lacking to determine whether ankle equinus is the primary cause of idiopathic toe-walking or is a consequence of chronically walking on tiptoes. A family history of toe-walking ranges from 30% to 71% in the literature and is considered a characteristic of idiopathic toe walking.2-4
Evaluation. An important element of the evaluation of idiopathic toe-walking is to distinguish it from neuromuscular disorders associated with toe-walking, such as mild cerebral palsy. Case series with small numbers of subjects (range=27–41) have used gait electromyography (EMG) to distinguish cerebral palsy from idiopathic toe-walking.4-6 The overlap in gait EMG values in cerebral palsy and idiopathic toe-walking precludes its use as a differentiating diagnostic test.
The only aspect of EMG testing that has been useful in differentiating cerebral palsy from idiopathic toe-walking is gastrocnemius coactivation during resisted knee extension—a finding indicative of neurologic pathology.5,6 Kinematic analysis and observation of gait and measurement of ankle range of motion have been studied as diagnostic tools to differentiate idiopathic toe-walking from cerebral palsy.5-8 In the largest of these 4 studies (23 children with mild cerebral palsy and 22 with idiopathic toe-walking), maximal knee extension occurred at ground contact in the idiopathic toe-walking group whereas in the mild cerebral palsy group, the knee was flexed at ground contact.7 Measurement of ankle range of motion is not reliable in distinguishing between idiopathic toe-walking and cerebral palsy groups.5-7
Treatment. Simple observation, physical therapy, serial casting, and Achilles tendon lengthening surgery have been studied in the treatment of idiopathic toe-walking.2,3,9-11 In the largest case series (n=136),10 the frequency of toe-walking decreased in 51% of those in both the observation and casted groups. In this same study, the surgical group had lower rates of toe-walking, but no direct comparisons could be made to the nonsurgical groups because the patients in the surgical group were older and had longer follow-up than the other groups.
In a retrospective comparison3 of observation (which included physical therapy and special shoes), casting, and surgery among 80 children with idiopathic toe-walking, surgery resulted in significantly higher parental satisfaction (satisfied was defined as “child rarely walks on tiptoe”), 67% vs 25% and 24% for observation and casting groups respectively (P<.05). Three smaller studies (from 13 to 18 subjects) also showed decreased toe-walking at follow-up, regardless of treatment.2,9,11
There is no convincing evidence that treatment is necessary for this condition. We found no randomized trials of treatment for idiopathic toe-walking and no follow-up studies of sufficient size and duration that evaluate long-term effects of toe walking on the patient later in life.
Recommendations from others
No recommendations or guidelines were found.
The evaluation of toe-walking focuses on differentiating normal children from those with mild cerebral palsy. Gait analysis may be a useful diagnostic tool, but further investigation is needed to confirm its reliability (strength of recommendation [SOR]: C, based on case series).
Observation alone is generally as successful as serial casting and surgery in decreasing the frequency of toe-walking at follow-up (SOR: C, based on case series).
Avoid overmedicalizing a problem that appears to run a benign course
Vince Winkler-Prins, MD
Michigan State University, East Lansing
The challenge with idiopathic toe-walking appears to be how to discriminate it from the more serious entities of cerebral palsy and muscular dystrophy. Idiopathic toe-walking should be evident in an otherwise healthy child as he or she begins to walk. It should be bilateral, there should be no spasticity and reflexes should not be overly brisk. A few follow-up visits at 3- or 6-month intervals should reassure all that this problem is nonprogressive. I have seen many toe-walking children over the years but no toe-walking adults without cerebral palsy or muscular dystrophy. This seems to confirm this review’s findings that observation appears to be as useful as casting or surgery. Until there is a natural history study of toe-walking, we need to be watchful to not overmedicalize a problem that appears to run a benign course.
Evidence summary
Idiopathic toe-walking is a childhood condition of unknown cause characterized by persistence of a tiptoe gait pattern without evidence of neurologic, orthopedic, or psychiatric disease.1 The incidence in the general population is not known. Children with idiopathic toe-walking usually have limited ankle dorsiflexion and are able to walk with a heel-strike for short periods when asked to do so. Longitudinal data is lacking to determine whether ankle equinus is the primary cause of idiopathic toe-walking or is a consequence of chronically walking on tiptoes. A family history of toe-walking ranges from 30% to 71% in the literature and is considered a characteristic of idiopathic toe walking.2-4
Evaluation. An important element of the evaluation of idiopathic toe-walking is to distinguish it from neuromuscular disorders associated with toe-walking, such as mild cerebral palsy. Case series with small numbers of subjects (range=27–41) have used gait electromyography (EMG) to distinguish cerebral palsy from idiopathic toe-walking.4-6 The overlap in gait EMG values in cerebral palsy and idiopathic toe-walking precludes its use as a differentiating diagnostic test.
The only aspect of EMG testing that has been useful in differentiating cerebral palsy from idiopathic toe-walking is gastrocnemius coactivation during resisted knee extension—a finding indicative of neurologic pathology.5,6 Kinematic analysis and observation of gait and measurement of ankle range of motion have been studied as diagnostic tools to differentiate idiopathic toe-walking from cerebral palsy.5-8 In the largest of these 4 studies (23 children with mild cerebral palsy and 22 with idiopathic toe-walking), maximal knee extension occurred at ground contact in the idiopathic toe-walking group whereas in the mild cerebral palsy group, the knee was flexed at ground contact.7 Measurement of ankle range of motion is not reliable in distinguishing between idiopathic toe-walking and cerebral palsy groups.5-7
Treatment. Simple observation, physical therapy, serial casting, and Achilles tendon lengthening surgery have been studied in the treatment of idiopathic toe-walking.2,3,9-11 In the largest case series (n=136),10 the frequency of toe-walking decreased in 51% of those in both the observation and casted groups. In this same study, the surgical group had lower rates of toe-walking, but no direct comparisons could be made to the nonsurgical groups because the patients in the surgical group were older and had longer follow-up than the other groups.
In a retrospective comparison3 of observation (which included physical therapy and special shoes), casting, and surgery among 80 children with idiopathic toe-walking, surgery resulted in significantly higher parental satisfaction (satisfied was defined as “child rarely walks on tiptoe”), 67% vs 25% and 24% for observation and casting groups respectively (P<.05). Three smaller studies (from 13 to 18 subjects) also showed decreased toe-walking at follow-up, regardless of treatment.2,9,11
There is no convincing evidence that treatment is necessary for this condition. We found no randomized trials of treatment for idiopathic toe-walking and no follow-up studies of sufficient size and duration that evaluate long-term effects of toe walking on the patient later in life.
Recommendations from others
No recommendations or guidelines were found.
1. Hall JE, Salter RB, Bhalla SK. Congenital short tendo calcaneus. J Bone Joint Surg Br 1967;49B:695-697.
2. Hirsch G, Wagner B. The natural history of idiopathic toe-walking: a long-term follow-up of fourteen conservatively treated children. Acta Paediatr 2004;93:196-199.
3. Stricker SJ, Angulo JC. Idiopathic toe walking: a comparison of treatment methods. J Pediatr Orthop 1998;18:289-293.
4. Kalen V, Adler N, Bleck EE. Electromyography of idiopathic toe walking. J Pediatr Orthop 1986;6:31-33.
5. Policy JF, Torburn L, Rinsky LA, Rose J. Electromyographic test to differentiate mild diplegic cerebral palsy and idiopathic toe-walking. J Pediatr Orthop 2001;21:784-789.
6. Rose J, Martin JG, Torburn L, Rinsky LA, Gamble JG. Electromyographic differentiation of diplegic cerebral palsy from idiopathic toe walking: involuntary coactivation of the quadriceps and gastrocnemius. J Pediatr Orthop 1999;19:677-682.
7. Kelly IP, Jenkinson A, Stephens M, O’Brien T. The kinematic patterns of toe-walkers. J Pediatr Orthop 1997;17:478-480.
8. Hicks R, Durinick N, Gage JR. Differentiation of idiopathic toe-walking and cerebral palsy. J Pediatr Orthop 1988;8:160-163.
9. Stott NS, Walt SE, Lobb GA, Reynolds N, Nicol RO. Treatment for idiopathic toe-walking: results at skeletal maturity. J Pediatr Orthop 2004;24:63-69.
10. Eastwood DM, Menelaus MB, Dickens DR, Broughton NS, Cole WG. Idiopathic toe-walking: does treatment alter the natural history. J Pediatr Orthop B 2000;9:47-49.
11. Brouwer B, Davidson LK, Olney SJ. Serial casting in idiopathic toe-walkers and children with spastic cerebral palsy. J Pediatr Orthop 2000;20:221-225.
1. Hall JE, Salter RB, Bhalla SK. Congenital short tendo calcaneus. J Bone Joint Surg Br 1967;49B:695-697.
2. Hirsch G, Wagner B. The natural history of idiopathic toe-walking: a long-term follow-up of fourteen conservatively treated children. Acta Paediatr 2004;93:196-199.
3. Stricker SJ, Angulo JC. Idiopathic toe walking: a comparison of treatment methods. J Pediatr Orthop 1998;18:289-293.
4. Kalen V, Adler N, Bleck EE. Electromyography of idiopathic toe walking. J Pediatr Orthop 1986;6:31-33.
5. Policy JF, Torburn L, Rinsky LA, Rose J. Electromyographic test to differentiate mild diplegic cerebral palsy and idiopathic toe-walking. J Pediatr Orthop 2001;21:784-789.
6. Rose J, Martin JG, Torburn L, Rinsky LA, Gamble JG. Electromyographic differentiation of diplegic cerebral palsy from idiopathic toe walking: involuntary coactivation of the quadriceps and gastrocnemius. J Pediatr Orthop 1999;19:677-682.
7. Kelly IP, Jenkinson A, Stephens M, O’Brien T. The kinematic patterns of toe-walkers. J Pediatr Orthop 1997;17:478-480.
8. Hicks R, Durinick N, Gage JR. Differentiation of idiopathic toe-walking and cerebral palsy. J Pediatr Orthop 1988;8:160-163.
9. Stott NS, Walt SE, Lobb GA, Reynolds N, Nicol RO. Treatment for idiopathic toe-walking: results at skeletal maturity. J Pediatr Orthop 2004;24:63-69.
10. Eastwood DM, Menelaus MB, Dickens DR, Broughton NS, Cole WG. Idiopathic toe-walking: does treatment alter the natural history. J Pediatr Orthop B 2000;9:47-49.
11. Brouwer B, Davidson LK, Olney SJ. Serial casting in idiopathic toe-walkers and children with spastic cerebral palsy. J Pediatr Orthop 2000;20:221-225.
Evidence-based answers from the Family Physicians Inquiries Network