User login
Online Entry-Level Education: The Jury Is Still Out!
I consider my role as an editorialist to be to inform, persuade, or—sometimes—just comment on current issues that affect PAs and NPs. There have been many opportunities in recent years to address “hot” topics, and this is certainly one of them: the rise of distance entry-level education for health professions students.
The catalyst for this discussion? Earlier this year, Yale University announced it was launching an online entry-level PA program.1 Within minutes of that announcement, there was a conflagration of criticism from the profession, alumni, and the general public. Most of the backlash centered on concerns about adequate delivery of such intense content—including how to instill or enhance professional behaviors and attitudes, or teach hands-on procedures, objective structured clinical examinations (OSCEs), and physical exam techniques—from a distance.
In our professions, we tend to be fairly conservative when it comes to change—particularly in terms of innovations in our education programs. But as e-learning, simulations, and distance education modalities become ever more prevalent across the spectrum of higher learning, we require an improved understanding of how these methods will transform entry-level education for health care providers.
Until recently, there has been minimal data on the impact of these technologic advances and teaching methods in health professions education, although this is changing.2 We do have a research gap when it comes to the effect of learning style on NP and PA students’ perceptions of online instruction (despite the rapidly increasing use of it). We also have not firmly established how this delivery method affects professional development (ie, how effectively it prepares clinicians to provide care to patients). None of this has prevented the proliferation of these concepts.
While many were stunned by the Yale venture, it should be noted that the idea is not new. Rather, such programs have steadily become part of health professions education (particularly nursing) in recent years.3 Yale itself was an early adopter of “bridge” programs; for example, someone with a Bachelor of Science in any field could enter the NP program, becoming an RN in one year and an NP in the second.
As far as “distance learning,” offering graduate degrees in a health profession to remote students dates back to at least the early 1990s, when the University of Pennsylvania offered a videoconference-based master’s in nurse-midwifery. Since then, of course, technology has advanced to a level that allows individuals to view videos and “conference” online via personal electronic devices of one kind or another—a vast improvement on the expensive and inflexible room-scale video presentations of 20 years ago.
As these technologic limitations have fallen by the wayside and alterations to our educational structure have become more feasible, more colleges and universities are exploring their options. The PA programs at the University of North Dakota and the University of Wisconsin–Madison have experimented with blended online learning environments. My own university has an interest in moving to ever-higher levels of distant interaction.
Major criticism of distance education includes the perception that it is a “watered-down” version of the “real thing.” There is also concern that educational institutions might be motivated purely by money, if the sole impetus for distance learning is to significantly increase enrollment. And some critics, while not opposed to online courses per se, do not want an NP or PA seeing patients if his/her degree was earned online—not even in part!
Perhaps the larger issue we’re struggling with is that a new paradigm of teaching is emerging: We are moving away from the traditional Socratic method to more interactive modalities, such as flipped classrooms (settings in which students collaborate via online discussion). Synchronous classes can be delivered seminar-style, with each student able to hear the others and instructors able to share content and even give control of a class to a student for questions or presentations. Asynchronous courses offer opportunities for students to study on their own time and at their own pace. Many suggest that more comprehensive learning, including the development of critical thinking skills, occurs in programs of this design than in traditional education programs.4
I think there is little argument that the educational content (didactics) of a program can be successfully delivered through a nonresidential venue. The concern, rightly so, in health professional education is how to adequately deliver the practical and cocurricular experiences at a distance. Some of us may have a difficult time understanding how this new method of teaching can create the kind of clinicians that are needed, particularly in the relatively short period in which PAs and NPs are prepared for their roles.
Proponents insist that these programs can be successful, as long as they are accredited by the appropriate agency and demonstrate high educational standards (comparable to traditional programs). Programs also need to provide clinical experiences in which the students observe and actually work with patients in order to develop skills in the art of history taking and physical examination, establishment of a differential diagnosis, creation of a plan of action, and appropriate decision-making with regard to available tests and treatment options. Advocates of distance learning also agree that students must be observed by peer clinicians who can confirm that they are ethical and competent to practice, have good bedside manners, and demonstrate respect for the profession and for life.
And who knows? Distance learning may create opportunities to improve access to care in remote, rural, and underserved areas, as these could become fertile training grounds for NPs and PAs (a return to our roots, in a sense). In this age of successful telemedicine, why shouldn’t “tele-education” be the next success story? Although the jury is still out on this concept, the proverbial cat has already been let out of the bag! Only time will tell what results we will see. But I think with the significant enhancement of technology, and participation of committed educators who are willing to step into the arena to ensure that competency-based education persists, we will be pleasantly surprised by the success of this venture.
I would be interested in your views. Please email me at PAEditor@frontlinemedcom.com.
REFERENCES
1. Monir M. Yale to offer full-time master’s program online. USA Today. www.usatoday.com/story/news/nation/2015/03/12/yale-full-time-online-masters-program/70163994. Accessed May 2, 2015.
2. Kushniruk AW. Advances in health education applying e-learning, simulations and distance technologies [editorial]. Knowledge Manage E-Learning Int J. 2011;3(1):1-4.
3. Robley LR, Farnsworth BJ, Flynn JB, Horne CD. This new house: building knowledge through online learning. J Prof Nurs. 2004;20(5):333-343.
4. Yang YTC, Chou HA. Beyond critical thinking skills: investigating the relationship between critical thinking skills and dispositions through different online instructional strategies. Br J Educ Technol. 2008;39(4):666-684.
I consider my role as an editorialist to be to inform, persuade, or—sometimes—just comment on current issues that affect PAs and NPs. There have been many opportunities in recent years to address “hot” topics, and this is certainly one of them: the rise of distance entry-level education for health professions students.
The catalyst for this discussion? Earlier this year, Yale University announced it was launching an online entry-level PA program.1 Within minutes of that announcement, there was a conflagration of criticism from the profession, alumni, and the general public. Most of the backlash centered on concerns about adequate delivery of such intense content—including how to instill or enhance professional behaviors and attitudes, or teach hands-on procedures, objective structured clinical examinations (OSCEs), and physical exam techniques—from a distance.
In our professions, we tend to be fairly conservative when it comes to change—particularly in terms of innovations in our education programs. But as e-learning, simulations, and distance education modalities become ever more prevalent across the spectrum of higher learning, we require an improved understanding of how these methods will transform entry-level education for health care providers.
Until recently, there has been minimal data on the impact of these technologic advances and teaching methods in health professions education, although this is changing.2 We do have a research gap when it comes to the effect of learning style on NP and PA students’ perceptions of online instruction (despite the rapidly increasing use of it). We also have not firmly established how this delivery method affects professional development (ie, how effectively it prepares clinicians to provide care to patients). None of this has prevented the proliferation of these concepts.
While many were stunned by the Yale venture, it should be noted that the idea is not new. Rather, such programs have steadily become part of health professions education (particularly nursing) in recent years.3 Yale itself was an early adopter of “bridge” programs; for example, someone with a Bachelor of Science in any field could enter the NP program, becoming an RN in one year and an NP in the second.
As far as “distance learning,” offering graduate degrees in a health profession to remote students dates back to at least the early 1990s, when the University of Pennsylvania offered a videoconference-based master’s in nurse-midwifery. Since then, of course, technology has advanced to a level that allows individuals to view videos and “conference” online via personal electronic devices of one kind or another—a vast improvement on the expensive and inflexible room-scale video presentations of 20 years ago.
As these technologic limitations have fallen by the wayside and alterations to our educational structure have become more feasible, more colleges and universities are exploring their options. The PA programs at the University of North Dakota and the University of Wisconsin–Madison have experimented with blended online learning environments. My own university has an interest in moving to ever-higher levels of distant interaction.
Major criticism of distance education includes the perception that it is a “watered-down” version of the “real thing.” There is also concern that educational institutions might be motivated purely by money, if the sole impetus for distance learning is to significantly increase enrollment. And some critics, while not opposed to online courses per se, do not want an NP or PA seeing patients if his/her degree was earned online—not even in part!
Perhaps the larger issue we’re struggling with is that a new paradigm of teaching is emerging: We are moving away from the traditional Socratic method to more interactive modalities, such as flipped classrooms (settings in which students collaborate via online discussion). Synchronous classes can be delivered seminar-style, with each student able to hear the others and instructors able to share content and even give control of a class to a student for questions or presentations. Asynchronous courses offer opportunities for students to study on their own time and at their own pace. Many suggest that more comprehensive learning, including the development of critical thinking skills, occurs in programs of this design than in traditional education programs.4
I think there is little argument that the educational content (didactics) of a program can be successfully delivered through a nonresidential venue. The concern, rightly so, in health professional education is how to adequately deliver the practical and cocurricular experiences at a distance. Some of us may have a difficult time understanding how this new method of teaching can create the kind of clinicians that are needed, particularly in the relatively short period in which PAs and NPs are prepared for their roles.
Proponents insist that these programs can be successful, as long as they are accredited by the appropriate agency and demonstrate high educational standards (comparable to traditional programs). Programs also need to provide clinical experiences in which the students observe and actually work with patients in order to develop skills in the art of history taking and physical examination, establishment of a differential diagnosis, creation of a plan of action, and appropriate decision-making with regard to available tests and treatment options. Advocates of distance learning also agree that students must be observed by peer clinicians who can confirm that they are ethical and competent to practice, have good bedside manners, and demonstrate respect for the profession and for life.
And who knows? Distance learning may create opportunities to improve access to care in remote, rural, and underserved areas, as these could become fertile training grounds for NPs and PAs (a return to our roots, in a sense). In this age of successful telemedicine, why shouldn’t “tele-education” be the next success story? Although the jury is still out on this concept, the proverbial cat has already been let out of the bag! Only time will tell what results we will see. But I think with the significant enhancement of technology, and participation of committed educators who are willing to step into the arena to ensure that competency-based education persists, we will be pleasantly surprised by the success of this venture.
I would be interested in your views. Please email me at PAEditor@frontlinemedcom.com.
REFERENCES
1. Monir M. Yale to offer full-time master’s program online. USA Today. www.usatoday.com/story/news/nation/2015/03/12/yale-full-time-online-masters-program/70163994. Accessed May 2, 2015.
2. Kushniruk AW. Advances in health education applying e-learning, simulations and distance technologies [editorial]. Knowledge Manage E-Learning Int J. 2011;3(1):1-4.
3. Robley LR, Farnsworth BJ, Flynn JB, Horne CD. This new house: building knowledge through online learning. J Prof Nurs. 2004;20(5):333-343.
4. Yang YTC, Chou HA. Beyond critical thinking skills: investigating the relationship between critical thinking skills and dispositions through different online instructional strategies. Br J Educ Technol. 2008;39(4):666-684.
I consider my role as an editorialist to be to inform, persuade, or—sometimes—just comment on current issues that affect PAs and NPs. There have been many opportunities in recent years to address “hot” topics, and this is certainly one of them: the rise of distance entry-level education for health professions students.
The catalyst for this discussion? Earlier this year, Yale University announced it was launching an online entry-level PA program.1 Within minutes of that announcement, there was a conflagration of criticism from the profession, alumni, and the general public. Most of the backlash centered on concerns about adequate delivery of such intense content—including how to instill or enhance professional behaviors and attitudes, or teach hands-on procedures, objective structured clinical examinations (OSCEs), and physical exam techniques—from a distance.
In our professions, we tend to be fairly conservative when it comes to change—particularly in terms of innovations in our education programs. But as e-learning, simulations, and distance education modalities become ever more prevalent across the spectrum of higher learning, we require an improved understanding of how these methods will transform entry-level education for health care providers.
Until recently, there has been minimal data on the impact of these technologic advances and teaching methods in health professions education, although this is changing.2 We do have a research gap when it comes to the effect of learning style on NP and PA students’ perceptions of online instruction (despite the rapidly increasing use of it). We also have not firmly established how this delivery method affects professional development (ie, how effectively it prepares clinicians to provide care to patients). None of this has prevented the proliferation of these concepts.
While many were stunned by the Yale venture, it should be noted that the idea is not new. Rather, such programs have steadily become part of health professions education (particularly nursing) in recent years.3 Yale itself was an early adopter of “bridge” programs; for example, someone with a Bachelor of Science in any field could enter the NP program, becoming an RN in one year and an NP in the second.
As far as “distance learning,” offering graduate degrees in a health profession to remote students dates back to at least the early 1990s, when the University of Pennsylvania offered a videoconference-based master’s in nurse-midwifery. Since then, of course, technology has advanced to a level that allows individuals to view videos and “conference” online via personal electronic devices of one kind or another—a vast improvement on the expensive and inflexible room-scale video presentations of 20 years ago.
As these technologic limitations have fallen by the wayside and alterations to our educational structure have become more feasible, more colleges and universities are exploring their options. The PA programs at the University of North Dakota and the University of Wisconsin–Madison have experimented with blended online learning environments. My own university has an interest in moving to ever-higher levels of distant interaction.
Major criticism of distance education includes the perception that it is a “watered-down” version of the “real thing.” There is also concern that educational institutions might be motivated purely by money, if the sole impetus for distance learning is to significantly increase enrollment. And some critics, while not opposed to online courses per se, do not want an NP or PA seeing patients if his/her degree was earned online—not even in part!
Perhaps the larger issue we’re struggling with is that a new paradigm of teaching is emerging: We are moving away from the traditional Socratic method to more interactive modalities, such as flipped classrooms (settings in which students collaborate via online discussion). Synchronous classes can be delivered seminar-style, with each student able to hear the others and instructors able to share content and even give control of a class to a student for questions or presentations. Asynchronous courses offer opportunities for students to study on their own time and at their own pace. Many suggest that more comprehensive learning, including the development of critical thinking skills, occurs in programs of this design than in traditional education programs.4
I think there is little argument that the educational content (didactics) of a program can be successfully delivered through a nonresidential venue. The concern, rightly so, in health professional education is how to adequately deliver the practical and cocurricular experiences at a distance. Some of us may have a difficult time understanding how this new method of teaching can create the kind of clinicians that are needed, particularly in the relatively short period in which PAs and NPs are prepared for their roles.
Proponents insist that these programs can be successful, as long as they are accredited by the appropriate agency and demonstrate high educational standards (comparable to traditional programs). Programs also need to provide clinical experiences in which the students observe and actually work with patients in order to develop skills in the art of history taking and physical examination, establishment of a differential diagnosis, creation of a plan of action, and appropriate decision-making with regard to available tests and treatment options. Advocates of distance learning also agree that students must be observed by peer clinicians who can confirm that they are ethical and competent to practice, have good bedside manners, and demonstrate respect for the profession and for life.
And who knows? Distance learning may create opportunities to improve access to care in remote, rural, and underserved areas, as these could become fertile training grounds for NPs and PAs (a return to our roots, in a sense). In this age of successful telemedicine, why shouldn’t “tele-education” be the next success story? Although the jury is still out on this concept, the proverbial cat has already been let out of the bag! Only time will tell what results we will see. But I think with the significant enhancement of technology, and participation of committed educators who are willing to step into the arena to ensure that competency-based education persists, we will be pleasantly surprised by the success of this venture.
I would be interested in your views. Please email me at PAEditor@frontlinemedcom.com.
REFERENCES
1. Monir M. Yale to offer full-time master’s program online. USA Today. www.usatoday.com/story/news/nation/2015/03/12/yale-full-time-online-masters-program/70163994. Accessed May 2, 2015.
2. Kushniruk AW. Advances in health education applying e-learning, simulations and distance technologies [editorial]. Knowledge Manage E-Learning Int J. 2011;3(1):1-4.
3. Robley LR, Farnsworth BJ, Flynn JB, Horne CD. This new house: building knowledge through online learning. J Prof Nurs. 2004;20(5):333-343.
4. Yang YTC, Chou HA. Beyond critical thinking skills: investigating the relationship between critical thinking skills and dispositions through different online instructional strategies. Br J Educ Technol. 2008;39(4):666-684.
It's All About the Spit!
Remember eighth grade, when you were taught the correlation between pH and saliva? You learned that testing saliva provides information on whether the mouth is an acidic, basic, or neutral environment. But did you ever suspect then that saliva would become a formidable instrument for medical diagnosis, health, and research?
It’s true, friends and colleagues: Spit is the latest, greatest trend in health care! This important physiologic fluid, which contains a highly complex assortment of substances, is rapidly gaining notice as a diagnostic tool. Don’t believe it? Read on!
The oral cavity, according to Dr. Jack Dillenberg, the inaugural dean of the Arizona School of Dentistry and Oral Health (ASDOH), “is the gateway and window into health in our body. The signs of nutritional deficiencies, general infections, and systemic diseases that affect the entire body may first become apparent in the oral cavity via lesions or other oral problems. Saliva plays a significant role in maintaining oral health and has a strong correlation to tooth decay.”1
Yes, we’ve known for a while that an adequate amount of saliva serves as a pH buffer; when plaque pH drops below 5.5, dental caries can occur. But according to researchers at The Johns Hopkins University’s Center for Interdisciplinary Salivary Bioscience Research (yes, a research center dedicated to spit!), saliva holds a wealth of data that is easily collected and economically analyzed and may be a key to many mysteries of human biology and genetics, as well as a helpful tool to combat disease. “There’s lots of potential in exploring what’s in saliva,” according to Dr. Doug Granger, the center’s director and a psychoneuroendocrinologist (what a mouthful—pun intended!) at Arizona State University.2
Saliva in the mouth forms a thin film that protects against dental caries, erosion, attrition, abrasion, periodontal diseases, candidiasis, and abrasive mucosal lesions. Studies suggest saliva may be useful in detecting heart disease, acid reflux, and diabetes; it is already being used for rapid HIV testing.3-5 Researchers have also reported encouraging results in the use of saliva for the diagnosis of autoimmune disorders, breast cancer, oral cancers, gum disease, and cardiovascular, endocrine, and infectious diseases.6,7
Is saliva screening the new "blood test"?
So is saliva screening the new “blood test”? Blood testing, performed as an aid to diagnosis, has its drawbacks: Samples are often uncomfortable to obtain, a lab visit may be necessary, and processing takes time. Finding a reasonable alternative would be beneficial, but there are several steps to such a process.
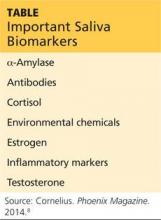
The capacity to monitor health status, disease onset and progression, and treatment outcomes through noninvasive means is a goal in health care promotion and delivery. For this to occur, three things must happen: first, specific biomarkers associated with a health or disease state must be established; second, a noninvasive manner to detect and monitor those biomarkers must be developed; and third, a mechanism to differentiate between the results is needed. Dr. Granger’s team has been studying the possibilities for several years now. Some of the key biomarkers measurable via saliva are listed in the Table below.8
Meanwhile, Dr. Tony Hashemian and colleagues at the ASDOH have developed a diagnostic tool based on pH. The purpose of their pH of Oral Health (pH2OH) initiative is to deliver new technology for pH saliva testing.9 This innovation uses a mobile phone application to capture time-sensitive data and to communicate with a server (in compliance with HIPAA regulations, of course).
Next page: Saliva-testing examination tool >>
A saliva-testing examination tool is used by the dental team to educate patients, inform preventive treatment planning, and assist with proper selection of dental materials to initiate changes in the patient’s oral hygiene. Dental teams measure saliva pH with test strips—the litmus paper we used even as kids in school. It is simply a strip of colored paper that, when soaked in sample saliva, turns a different color depending on the pH level. The color scale ranges from red (indicating a strong acidic state [pH < 3]) to dark blue or purple (indicating a strong alkaline state [pH > 11]).
The free iPhone or Android app developed by Dr. Hashemian’s team is designed to capture the pH value for a patient. The app can manually set the value, or you can take a picture of a test strip and auto-calculate the pH using color-coding analysis. Once set, the app will allow you to save the data and track improvements to oral pH over time.9
With improvements in immunology, microbiology, and biochemistry, salivary testing—in both research and clinical settings—may prove to be an applied and reliable means of recognizing oral signs of systemic illness and exposure to risk factors.10 Salivary diagnostics will be the next great breakthrough in improving the general health of the public. Stay tuned.
What are your thoughts about how “spit” could be applied clinically? Contact me at PAEditor@frontlinemedcom.com.
REFERENCES
1. Personal communication. February 17, 2015.
2. Walker AK. Researchers eye saliva for patient testing. Baltimore Sun. May 23, 2012.
3. Devi TJ. Saliva: a potential diagnostic tool. J Dental Med Sci. 2014;13(2):52-57.
4. Giannobile WV, Beikler T, Kinney JS, et al. Saliva as a diagnostic tool for periodontal disease: current state and future directions. Periodontol 2000. 2009;50:52-64.
5. Gopinath VK, Arzreanne AR. Saliva as a diagnostic tool for assessment of dental caries. Arch Orofacial Sci. 2006;1:57-59.
6. Streckfus CF, Bigler LR. Salivary glands and saliva: saliva as a diagnostic fluid. Oral Dis. 2002;8:69-76.
7. Lee JM, Garon E, Wong DR. Salivary diagnostics. Orthod Cranioffac Res. 2009;12:206211.
8. Cornelius K. Spit, polished. Phoenix Magazine. November 2014; 38.
9. AT Still University, Arizona School of Dentistry and Oral Health. pH2OH. www.ph2oh.com/apps/. Accessed March 21, 2015.
10. Lawrence HP. Salivary markers of systemic disease: noninvasive diagnosis of disease and monitoring of general health. J Can Dent Assoc. 2002;68(3):170-174.
Remember eighth grade, when you were taught the correlation between pH and saliva? You learned that testing saliva provides information on whether the mouth is an acidic, basic, or neutral environment. But did you ever suspect then that saliva would become a formidable instrument for medical diagnosis, health, and research?
It’s true, friends and colleagues: Spit is the latest, greatest trend in health care! This important physiologic fluid, which contains a highly complex assortment of substances, is rapidly gaining notice as a diagnostic tool. Don’t believe it? Read on!
The oral cavity, according to Dr. Jack Dillenberg, the inaugural dean of the Arizona School of Dentistry and Oral Health (ASDOH), “is the gateway and window into health in our body. The signs of nutritional deficiencies, general infections, and systemic diseases that affect the entire body may first become apparent in the oral cavity via lesions or other oral problems. Saliva plays a significant role in maintaining oral health and has a strong correlation to tooth decay.”1
Yes, we’ve known for a while that an adequate amount of saliva serves as a pH buffer; when plaque pH drops below 5.5, dental caries can occur. But according to researchers at The Johns Hopkins University’s Center for Interdisciplinary Salivary Bioscience Research (yes, a research center dedicated to spit!), saliva holds a wealth of data that is easily collected and economically analyzed and may be a key to many mysteries of human biology and genetics, as well as a helpful tool to combat disease. “There’s lots of potential in exploring what’s in saliva,” according to Dr. Doug Granger, the center’s director and a psychoneuroendocrinologist (what a mouthful—pun intended!) at Arizona State University.2
Saliva in the mouth forms a thin film that protects against dental caries, erosion, attrition, abrasion, periodontal diseases, candidiasis, and abrasive mucosal lesions. Studies suggest saliva may be useful in detecting heart disease, acid reflux, and diabetes; it is already being used for rapid HIV testing.3-5 Researchers have also reported encouraging results in the use of saliva for the diagnosis of autoimmune disorders, breast cancer, oral cancers, gum disease, and cardiovascular, endocrine, and infectious diseases.6,7
Is saliva screening the new "blood test"?
So is saliva screening the new “blood test”? Blood testing, performed as an aid to diagnosis, has its drawbacks: Samples are often uncomfortable to obtain, a lab visit may be necessary, and processing takes time. Finding a reasonable alternative would be beneficial, but there are several steps to such a process.
The capacity to monitor health status, disease onset and progression, and treatment outcomes through noninvasive means is a goal in health care promotion and delivery. For this to occur, three things must happen: first, specific biomarkers associated with a health or disease state must be established; second, a noninvasive manner to detect and monitor those biomarkers must be developed; and third, a mechanism to differentiate between the results is needed. Dr. Granger’s team has been studying the possibilities for several years now. Some of the key biomarkers measurable via saliva are listed in the Table below.8
Meanwhile, Dr. Tony Hashemian and colleagues at the ASDOH have developed a diagnostic tool based on pH. The purpose of their pH of Oral Health (pH2OH) initiative is to deliver new technology for pH saliva testing.9 This innovation uses a mobile phone application to capture time-sensitive data and to communicate with a server (in compliance with HIPAA regulations, of course).
Next page: Saliva-testing examination tool >>
A saliva-testing examination tool is used by the dental team to educate patients, inform preventive treatment planning, and assist with proper selection of dental materials to initiate changes in the patient’s oral hygiene. Dental teams measure saliva pH with test strips—the litmus paper we used even as kids in school. It is simply a strip of colored paper that, when soaked in sample saliva, turns a different color depending on the pH level. The color scale ranges from red (indicating a strong acidic state [pH < 3]) to dark blue or purple (indicating a strong alkaline state [pH > 11]).
The free iPhone or Android app developed by Dr. Hashemian’s team is designed to capture the pH value for a patient. The app can manually set the value, or you can take a picture of a test strip and auto-calculate the pH using color-coding analysis. Once set, the app will allow you to save the data and track improvements to oral pH over time.9
With improvements in immunology, microbiology, and biochemistry, salivary testing—in both research and clinical settings—may prove to be an applied and reliable means of recognizing oral signs of systemic illness and exposure to risk factors.10 Salivary diagnostics will be the next great breakthrough in improving the general health of the public. Stay tuned.
What are your thoughts about how “spit” could be applied clinically? Contact me at PAEditor@frontlinemedcom.com.
REFERENCES
1. Personal communication. February 17, 2015.
2. Walker AK. Researchers eye saliva for patient testing. Baltimore Sun. May 23, 2012.
3. Devi TJ. Saliva: a potential diagnostic tool. J Dental Med Sci. 2014;13(2):52-57.
4. Giannobile WV, Beikler T, Kinney JS, et al. Saliva as a diagnostic tool for periodontal disease: current state and future directions. Periodontol 2000. 2009;50:52-64.
5. Gopinath VK, Arzreanne AR. Saliva as a diagnostic tool for assessment of dental caries. Arch Orofacial Sci. 2006;1:57-59.
6. Streckfus CF, Bigler LR. Salivary glands and saliva: saliva as a diagnostic fluid. Oral Dis. 2002;8:69-76.
7. Lee JM, Garon E, Wong DR. Salivary diagnostics. Orthod Cranioffac Res. 2009;12:206211.
8. Cornelius K. Spit, polished. Phoenix Magazine. November 2014; 38.
9. AT Still University, Arizona School of Dentistry and Oral Health. pH2OH. www.ph2oh.com/apps/. Accessed March 21, 2015.
10. Lawrence HP. Salivary markers of systemic disease: noninvasive diagnosis of disease and monitoring of general health. J Can Dent Assoc. 2002;68(3):170-174.
Remember eighth grade, when you were taught the correlation between pH and saliva? You learned that testing saliva provides information on whether the mouth is an acidic, basic, or neutral environment. But did you ever suspect then that saliva would become a formidable instrument for medical diagnosis, health, and research?
It’s true, friends and colleagues: Spit is the latest, greatest trend in health care! This important physiologic fluid, which contains a highly complex assortment of substances, is rapidly gaining notice as a diagnostic tool. Don’t believe it? Read on!
The oral cavity, according to Dr. Jack Dillenberg, the inaugural dean of the Arizona School of Dentistry and Oral Health (ASDOH), “is the gateway and window into health in our body. The signs of nutritional deficiencies, general infections, and systemic diseases that affect the entire body may first become apparent in the oral cavity via lesions or other oral problems. Saliva plays a significant role in maintaining oral health and has a strong correlation to tooth decay.”1
Yes, we’ve known for a while that an adequate amount of saliva serves as a pH buffer; when plaque pH drops below 5.5, dental caries can occur. But according to researchers at The Johns Hopkins University’s Center for Interdisciplinary Salivary Bioscience Research (yes, a research center dedicated to spit!), saliva holds a wealth of data that is easily collected and economically analyzed and may be a key to many mysteries of human biology and genetics, as well as a helpful tool to combat disease. “There’s lots of potential in exploring what’s in saliva,” according to Dr. Doug Granger, the center’s director and a psychoneuroendocrinologist (what a mouthful—pun intended!) at Arizona State University.2
Saliva in the mouth forms a thin film that protects against dental caries, erosion, attrition, abrasion, periodontal diseases, candidiasis, and abrasive mucosal lesions. Studies suggest saliva may be useful in detecting heart disease, acid reflux, and diabetes; it is already being used for rapid HIV testing.3-5 Researchers have also reported encouraging results in the use of saliva for the diagnosis of autoimmune disorders, breast cancer, oral cancers, gum disease, and cardiovascular, endocrine, and infectious diseases.6,7
Is saliva screening the new "blood test"?
So is saliva screening the new “blood test”? Blood testing, performed as an aid to diagnosis, has its drawbacks: Samples are often uncomfortable to obtain, a lab visit may be necessary, and processing takes time. Finding a reasonable alternative would be beneficial, but there are several steps to such a process.
The capacity to monitor health status, disease onset and progression, and treatment outcomes through noninvasive means is a goal in health care promotion and delivery. For this to occur, three things must happen: first, specific biomarkers associated with a health or disease state must be established; second, a noninvasive manner to detect and monitor those biomarkers must be developed; and third, a mechanism to differentiate between the results is needed. Dr. Granger’s team has been studying the possibilities for several years now. Some of the key biomarkers measurable via saliva are listed in the Table below.8
Meanwhile, Dr. Tony Hashemian and colleagues at the ASDOH have developed a diagnostic tool based on pH. The purpose of their pH of Oral Health (pH2OH) initiative is to deliver new technology for pH saliva testing.9 This innovation uses a mobile phone application to capture time-sensitive data and to communicate with a server (in compliance with HIPAA regulations, of course).
Next page: Saliva-testing examination tool >>
A saliva-testing examination tool is used by the dental team to educate patients, inform preventive treatment planning, and assist with proper selection of dental materials to initiate changes in the patient’s oral hygiene. Dental teams measure saliva pH with test strips—the litmus paper we used even as kids in school. It is simply a strip of colored paper that, when soaked in sample saliva, turns a different color depending on the pH level. The color scale ranges from red (indicating a strong acidic state [pH < 3]) to dark blue or purple (indicating a strong alkaline state [pH > 11]).
The free iPhone or Android app developed by Dr. Hashemian’s team is designed to capture the pH value for a patient. The app can manually set the value, or you can take a picture of a test strip and auto-calculate the pH using color-coding analysis. Once set, the app will allow you to save the data and track improvements to oral pH over time.9
With improvements in immunology, microbiology, and biochemistry, salivary testing—in both research and clinical settings—may prove to be an applied and reliable means of recognizing oral signs of systemic illness and exposure to risk factors.10 Salivary diagnostics will be the next great breakthrough in improving the general health of the public. Stay tuned.
What are your thoughts about how “spit” could be applied clinically? Contact me at PAEditor@frontlinemedcom.com.
REFERENCES
1. Personal communication. February 17, 2015.
2. Walker AK. Researchers eye saliva for patient testing. Baltimore Sun. May 23, 2012.
3. Devi TJ. Saliva: a potential diagnostic tool. J Dental Med Sci. 2014;13(2):52-57.
4. Giannobile WV, Beikler T, Kinney JS, et al. Saliva as a diagnostic tool for periodontal disease: current state and future directions. Periodontol 2000. 2009;50:52-64.
5. Gopinath VK, Arzreanne AR. Saliva as a diagnostic tool for assessment of dental caries. Arch Orofacial Sci. 2006;1:57-59.
6. Streckfus CF, Bigler LR. Salivary glands and saliva: saliva as a diagnostic fluid. Oral Dis. 2002;8:69-76.
7. Lee JM, Garon E, Wong DR. Salivary diagnostics. Orthod Cranioffac Res. 2009;12:206211.
8. Cornelius K. Spit, polished. Phoenix Magazine. November 2014; 38.
9. AT Still University, Arizona School of Dentistry and Oral Health. pH2OH. www.ph2oh.com/apps/. Accessed March 21, 2015.
10. Lawrence HP. Salivary markers of systemic disease: noninvasive diagnosis of disease and monitoring of general health. J Can Dent Assoc. 2002;68(3):170-174.
The Complexities of Competency
Rarely do I post online as a knee-jerk reaction! But recently, a topic hit me right in the middle of the forehead. I received an email from a colleague who asked:
“Is there any study looking at how long a PA or NP needs after completing his/her training to be fully competent? I’m at a hospital board meeting and one member is suggesting ‘midlevels’ need three more years of training, at the expense of the institution hiring them.”
I must admit that I was at a loss as to how to respond! (Not least because I dislike the term midlevel.) Lately, competency has been a hot topic as hospitals and large health care organizations hire more new graduates and want to know how long it will take for them to get up to speed within the institution. Competence is thus defined as how long it takes these PAs/NPs to become fully functional in a particular setting. It’s a narrow, specific question rather than a broad, philosophical one—but it begs the competency question, does it not?
Let’s start with the definition of competency. I had to laugh when I consulted Merriam-Webster, which says competency is “the quality or state of being functionally adequate.” Now, that is what I strive to be … “adequate”!
I prefer Norman’s definition of professional competence: “The habitual and judicious use of communication, knowledge, technical skills, clinical reasoning, emotions, values, and reflection in daily practice for the benefit of the individual and community being served. Competence builds on a foundation of basic clinical skills, scientific knowledge, and moral development.”1
He goes on to say that competence has multiple functions: cognitive (using acquired knowledge to solve real-life problems); integrative (using biomedical and psychosocial data in clinical reasoning); relational (communicating effectively with patients and colleagues); and affective/moral (the willingness, patience, and emotional awareness to use these skills judiciously and humanely). I was particularly struck by a final comment that competence is “developmental, impermanent, and context-dependent.”1 Competence is certainly developmental in the context of lifelong learning. If it is indeed impermanent (temporary, transient, transitory, passing, fleeting), then it must be evaluated frequently. There is no argument that it is context-dependent, whether by level of care, specialty knowledge required, or institution.
Clearly, competence is complex. While the PA and NP professions have developed and published clinical competencies in the past decade (which mirror and parallel those of our physician colleagues), how do we actually demonstrate them?
Continue for competency definitions >>
Patricia Benner developed one of the best-known competency definitions in 1982 with her Novice to Expert model, which applied the Dreyfus Model of Skill Acquisition to nursing. It has been widely used as a tool to determine “expertise.”2,3 Her model describes the five levels of expertise as
• Novice: A beginner with little to no experience. Novices face the inability to use discretionary judgment and require significant supervision.
• Advanced beginner: Able to demonstrate marginally acceptable performance based on some real-life experience.
• Competent: Has usually been on the job for two to three years. At this level, the clinician has a sense of mastery and the ability to cope with and manage many aspects of patient care.
• Proficient: Able to grasp clinical solutions quicker and able to hone in on accurate regions of the problem faster.
• Expert: No longer relies on analytics to connect to understanding of the problem but has an intuitive grasp and is able to zero in on all aspects of the problem at hand without any wasteful or unfruitful possibilities.3
Benner maintains that knowledge accrues over time in clinical practice and is developed through dialogue in relationship and situational contexts.4 Of note, clinical experience is not the mere passage of time or longevity within a clinical experience but rather the actual level of clinical interaction. The clinician, therefore, may move forward or backward, depending on the situation.
In 2011, Chuck defined six levels of competency, postulating that for each we find ways to scale the learning curve. It is where we are on the curve that determines our competence in a skill set. His six levels include
• Naïve/Newcomer: Exhibits little observable knowledge, skill, or sincere interest
• Intermediate: Has received minimal but not sufficient training to exhibit a core set of knowledge, skills, or interest
• Proficient: Has completed sufficient training (usually through a set of required classes) to reliably reproduce a core set of knowledge and skills, but requires further training when confronted with situations in which it needs to be applied
• Confident: Has above-average knowledge and skills and demonstrates appropriate confidence in adapting to new situations that challenge those skills
• Master: Demonstrates consistent excellence in knowledge and skills and can appropriately seek affirmation and criticism to independently develop additional skills
• Expert: Has received external validation of superior quality knowledge and skills and is considered an innovator, leader, or authority in a specific area.5
In the Chuck model, levels 1 and 2 would be prematriculants and students. You can see variations of this learning curve in different situations, whether it is a new clinician in the emergency department (ED) or an experienced clinician moving to a new practice.
So when is a clinician (specifically, a PA or NP) fully competent to see patients? This question is undoubtedly being asked more than we realize, and both professions should develop a serious answer to it. Are we doing enough research to make an objective argument in response? No matter how we answer, I think it is important to note that our respective professions have excellent patient care outcomes, even when taking into account the particular clinician level (novice through expert).
This is a challenging topic because what we do requires factual knowledge and the consistent, appropriate application of that knowledge. We know how to measure factual knowledge, more or less, but assuredly we don’t know how to measure the latter (possibly the more important part). In my opinion, we need a pragmatic approach to determine whether a clinician is competent and continues to be so.
One method is to do what is known as a 360 survey. Here’s how it might work: All coworkers of a particular clinician would be surveyed on the perceived elements of clinical competence, including knowledge, application of knowledge, efficiency, ability to make decisions, and attitude toward patients. Every person in the department—say, the ED—could anonymously complete the survey. (This would include nurses, techs, other PAs/NPs, housekeeping, on-call members of the medical staff—literally everybody, although not all of them will be capable of making some of these determinations.) Then the ED director would let the clinician review and discuss the feedback. Everyone in the department would know he or she would be similarly evaluated.6
This is the most brutal, yet fair and efficient, way to assess competency in its broadest sense. Will all opinions be factually substantiated? No! But what better technique do we have, at least for now?
But wait! Perhaps competence is not the end game. Perhaps competence is really a minimum standard. Competence (albeit novice) is measured by completion of the PA or NP curricula (meeting the course objectives) and passage of board/licensure exams, just as, essentially, physician competence is.
Most, if not all, would agree that mastery is achieved by the acquisition of knowledge coupled with sound practice and experience. Mastery or expertise, some say, is what we should focus on, the achievement of which is quite individual. All clinicians can move toward mastery, but not all will actually achieve it. Therefore, how can we mandate a minimum standard, beyond competence, for PAs and NPs but not for other providers?
So, after all the rhetorical ranting about when a PA or NP becomes fully competent, the answer is … It depends! There are too many moving parts. I would suggest that competency is the starting point and mastery (expertise) is a journey.
What do you think? Share your thoughts with me via PAEditor@frontlinemedcom.com.
REFERENCES
1. Norman GR. Defining competence: a methodological review. In: Neufeld VR, Norman GR, eds. Assessing Clinical Competence. New York, NY: Springer; 1985:15-35.
2. Gentile DL. Applying the novice-to-expert model to infusion nursing. J Infus Nurs. 2012;35(2):101-107.
3. Benner P. From novice to expert. Am J Nurs. 1982;82(3):402-407.
4. Brykczynski KA. Patricia Benner: caring, clinical wisdom, and ethics in nursing practice. In: Alligood MR, ed. Nursing Theorists and Their Work. 8th ed. St Louis, MO: Elsevier. 2014; 120-146.
5. Chuck E. The competency manifesto: part 3. The Student Doctor Network. www.student doctor.net/2011/04/the-competency-mani festo-part-3. Accessed November 11, 2014.
6. Lepsinger R, Luca AD. The Art and Science of 360-Degree Feedback. 2nd ed. San Francisco, CA: Jossey-Bass; 2009.
Rarely do I post online as a knee-jerk reaction! But recently, a topic hit me right in the middle of the forehead. I received an email from a colleague who asked:
“Is there any study looking at how long a PA or NP needs after completing his/her training to be fully competent? I’m at a hospital board meeting and one member is suggesting ‘midlevels’ need three more years of training, at the expense of the institution hiring them.”
I must admit that I was at a loss as to how to respond! (Not least because I dislike the term midlevel.) Lately, competency has been a hot topic as hospitals and large health care organizations hire more new graduates and want to know how long it will take for them to get up to speed within the institution. Competence is thus defined as how long it takes these PAs/NPs to become fully functional in a particular setting. It’s a narrow, specific question rather than a broad, philosophical one—but it begs the competency question, does it not?
Let’s start with the definition of competency. I had to laugh when I consulted Merriam-Webster, which says competency is “the quality or state of being functionally adequate.” Now, that is what I strive to be … “adequate”!
I prefer Norman’s definition of professional competence: “The habitual and judicious use of communication, knowledge, technical skills, clinical reasoning, emotions, values, and reflection in daily practice for the benefit of the individual and community being served. Competence builds on a foundation of basic clinical skills, scientific knowledge, and moral development.”1
He goes on to say that competence has multiple functions: cognitive (using acquired knowledge to solve real-life problems); integrative (using biomedical and psychosocial data in clinical reasoning); relational (communicating effectively with patients and colleagues); and affective/moral (the willingness, patience, and emotional awareness to use these skills judiciously and humanely). I was particularly struck by a final comment that competence is “developmental, impermanent, and context-dependent.”1 Competence is certainly developmental in the context of lifelong learning. If it is indeed impermanent (temporary, transient, transitory, passing, fleeting), then it must be evaluated frequently. There is no argument that it is context-dependent, whether by level of care, specialty knowledge required, or institution.
Clearly, competence is complex. While the PA and NP professions have developed and published clinical competencies in the past decade (which mirror and parallel those of our physician colleagues), how do we actually demonstrate them?
Continue for competency definitions >>
Patricia Benner developed one of the best-known competency definitions in 1982 with her Novice to Expert model, which applied the Dreyfus Model of Skill Acquisition to nursing. It has been widely used as a tool to determine “expertise.”2,3 Her model describes the five levels of expertise as
• Novice: A beginner with little to no experience. Novices face the inability to use discretionary judgment and require significant supervision.
• Advanced beginner: Able to demonstrate marginally acceptable performance based on some real-life experience.
• Competent: Has usually been on the job for two to three years. At this level, the clinician has a sense of mastery and the ability to cope with and manage many aspects of patient care.
• Proficient: Able to grasp clinical solutions quicker and able to hone in on accurate regions of the problem faster.
• Expert: No longer relies on analytics to connect to understanding of the problem but has an intuitive grasp and is able to zero in on all aspects of the problem at hand without any wasteful or unfruitful possibilities.3
Benner maintains that knowledge accrues over time in clinical practice and is developed through dialogue in relationship and situational contexts.4 Of note, clinical experience is not the mere passage of time or longevity within a clinical experience but rather the actual level of clinical interaction. The clinician, therefore, may move forward or backward, depending on the situation.
In 2011, Chuck defined six levels of competency, postulating that for each we find ways to scale the learning curve. It is where we are on the curve that determines our competence in a skill set. His six levels include
• Naïve/Newcomer: Exhibits little observable knowledge, skill, or sincere interest
• Intermediate: Has received minimal but not sufficient training to exhibit a core set of knowledge, skills, or interest
• Proficient: Has completed sufficient training (usually through a set of required classes) to reliably reproduce a core set of knowledge and skills, but requires further training when confronted with situations in which it needs to be applied
• Confident: Has above-average knowledge and skills and demonstrates appropriate confidence in adapting to new situations that challenge those skills
• Master: Demonstrates consistent excellence in knowledge and skills and can appropriately seek affirmation and criticism to independently develop additional skills
• Expert: Has received external validation of superior quality knowledge and skills and is considered an innovator, leader, or authority in a specific area.5
In the Chuck model, levels 1 and 2 would be prematriculants and students. You can see variations of this learning curve in different situations, whether it is a new clinician in the emergency department (ED) or an experienced clinician moving to a new practice.
So when is a clinician (specifically, a PA or NP) fully competent to see patients? This question is undoubtedly being asked more than we realize, and both professions should develop a serious answer to it. Are we doing enough research to make an objective argument in response? No matter how we answer, I think it is important to note that our respective professions have excellent patient care outcomes, even when taking into account the particular clinician level (novice through expert).
This is a challenging topic because what we do requires factual knowledge and the consistent, appropriate application of that knowledge. We know how to measure factual knowledge, more or less, but assuredly we don’t know how to measure the latter (possibly the more important part). In my opinion, we need a pragmatic approach to determine whether a clinician is competent and continues to be so.
One method is to do what is known as a 360 survey. Here’s how it might work: All coworkers of a particular clinician would be surveyed on the perceived elements of clinical competence, including knowledge, application of knowledge, efficiency, ability to make decisions, and attitude toward patients. Every person in the department—say, the ED—could anonymously complete the survey. (This would include nurses, techs, other PAs/NPs, housekeeping, on-call members of the medical staff—literally everybody, although not all of them will be capable of making some of these determinations.) Then the ED director would let the clinician review and discuss the feedback. Everyone in the department would know he or she would be similarly evaluated.6
This is the most brutal, yet fair and efficient, way to assess competency in its broadest sense. Will all opinions be factually substantiated? No! But what better technique do we have, at least for now?
But wait! Perhaps competence is not the end game. Perhaps competence is really a minimum standard. Competence (albeit novice) is measured by completion of the PA or NP curricula (meeting the course objectives) and passage of board/licensure exams, just as, essentially, physician competence is.
Most, if not all, would agree that mastery is achieved by the acquisition of knowledge coupled with sound practice and experience. Mastery or expertise, some say, is what we should focus on, the achievement of which is quite individual. All clinicians can move toward mastery, but not all will actually achieve it. Therefore, how can we mandate a minimum standard, beyond competence, for PAs and NPs but not for other providers?
So, after all the rhetorical ranting about when a PA or NP becomes fully competent, the answer is … It depends! There are too many moving parts. I would suggest that competency is the starting point and mastery (expertise) is a journey.
What do you think? Share your thoughts with me via PAEditor@frontlinemedcom.com.
REFERENCES
1. Norman GR. Defining competence: a methodological review. In: Neufeld VR, Norman GR, eds. Assessing Clinical Competence. New York, NY: Springer; 1985:15-35.
2. Gentile DL. Applying the novice-to-expert model to infusion nursing. J Infus Nurs. 2012;35(2):101-107.
3. Benner P. From novice to expert. Am J Nurs. 1982;82(3):402-407.
4. Brykczynski KA. Patricia Benner: caring, clinical wisdom, and ethics in nursing practice. In: Alligood MR, ed. Nursing Theorists and Their Work. 8th ed. St Louis, MO: Elsevier. 2014; 120-146.
5. Chuck E. The competency manifesto: part 3. The Student Doctor Network. www.student doctor.net/2011/04/the-competency-mani festo-part-3. Accessed November 11, 2014.
6. Lepsinger R, Luca AD. The Art and Science of 360-Degree Feedback. 2nd ed. San Francisco, CA: Jossey-Bass; 2009.
Rarely do I post online as a knee-jerk reaction! But recently, a topic hit me right in the middle of the forehead. I received an email from a colleague who asked:
“Is there any study looking at how long a PA or NP needs after completing his/her training to be fully competent? I’m at a hospital board meeting and one member is suggesting ‘midlevels’ need three more years of training, at the expense of the institution hiring them.”
I must admit that I was at a loss as to how to respond! (Not least because I dislike the term midlevel.) Lately, competency has been a hot topic as hospitals and large health care organizations hire more new graduates and want to know how long it will take for them to get up to speed within the institution. Competence is thus defined as how long it takes these PAs/NPs to become fully functional in a particular setting. It’s a narrow, specific question rather than a broad, philosophical one—but it begs the competency question, does it not?
Let’s start with the definition of competency. I had to laugh when I consulted Merriam-Webster, which says competency is “the quality or state of being functionally adequate.” Now, that is what I strive to be … “adequate”!
I prefer Norman’s definition of professional competence: “The habitual and judicious use of communication, knowledge, technical skills, clinical reasoning, emotions, values, and reflection in daily practice for the benefit of the individual and community being served. Competence builds on a foundation of basic clinical skills, scientific knowledge, and moral development.”1
He goes on to say that competence has multiple functions: cognitive (using acquired knowledge to solve real-life problems); integrative (using biomedical and psychosocial data in clinical reasoning); relational (communicating effectively with patients and colleagues); and affective/moral (the willingness, patience, and emotional awareness to use these skills judiciously and humanely). I was particularly struck by a final comment that competence is “developmental, impermanent, and context-dependent.”1 Competence is certainly developmental in the context of lifelong learning. If it is indeed impermanent (temporary, transient, transitory, passing, fleeting), then it must be evaluated frequently. There is no argument that it is context-dependent, whether by level of care, specialty knowledge required, or institution.
Clearly, competence is complex. While the PA and NP professions have developed and published clinical competencies in the past decade (which mirror and parallel those of our physician colleagues), how do we actually demonstrate them?
Continue for competency definitions >>
Patricia Benner developed one of the best-known competency definitions in 1982 with her Novice to Expert model, which applied the Dreyfus Model of Skill Acquisition to nursing. It has been widely used as a tool to determine “expertise.”2,3 Her model describes the five levels of expertise as
• Novice: A beginner with little to no experience. Novices face the inability to use discretionary judgment and require significant supervision.
• Advanced beginner: Able to demonstrate marginally acceptable performance based on some real-life experience.
• Competent: Has usually been on the job for two to three years. At this level, the clinician has a sense of mastery and the ability to cope with and manage many aspects of patient care.
• Proficient: Able to grasp clinical solutions quicker and able to hone in on accurate regions of the problem faster.
• Expert: No longer relies on analytics to connect to understanding of the problem but has an intuitive grasp and is able to zero in on all aspects of the problem at hand without any wasteful or unfruitful possibilities.3
Benner maintains that knowledge accrues over time in clinical practice and is developed through dialogue in relationship and situational contexts.4 Of note, clinical experience is not the mere passage of time or longevity within a clinical experience but rather the actual level of clinical interaction. The clinician, therefore, may move forward or backward, depending on the situation.
In 2011, Chuck defined six levels of competency, postulating that for each we find ways to scale the learning curve. It is where we are on the curve that determines our competence in a skill set. His six levels include
• Naïve/Newcomer: Exhibits little observable knowledge, skill, or sincere interest
• Intermediate: Has received minimal but not sufficient training to exhibit a core set of knowledge, skills, or interest
• Proficient: Has completed sufficient training (usually through a set of required classes) to reliably reproduce a core set of knowledge and skills, but requires further training when confronted with situations in which it needs to be applied
• Confident: Has above-average knowledge and skills and demonstrates appropriate confidence in adapting to new situations that challenge those skills
• Master: Demonstrates consistent excellence in knowledge and skills and can appropriately seek affirmation and criticism to independently develop additional skills
• Expert: Has received external validation of superior quality knowledge and skills and is considered an innovator, leader, or authority in a specific area.5
In the Chuck model, levels 1 and 2 would be prematriculants and students. You can see variations of this learning curve in different situations, whether it is a new clinician in the emergency department (ED) or an experienced clinician moving to a new practice.
So when is a clinician (specifically, a PA or NP) fully competent to see patients? This question is undoubtedly being asked more than we realize, and both professions should develop a serious answer to it. Are we doing enough research to make an objective argument in response? No matter how we answer, I think it is important to note that our respective professions have excellent patient care outcomes, even when taking into account the particular clinician level (novice through expert).
This is a challenging topic because what we do requires factual knowledge and the consistent, appropriate application of that knowledge. We know how to measure factual knowledge, more or less, but assuredly we don’t know how to measure the latter (possibly the more important part). In my opinion, we need a pragmatic approach to determine whether a clinician is competent and continues to be so.
One method is to do what is known as a 360 survey. Here’s how it might work: All coworkers of a particular clinician would be surveyed on the perceived elements of clinical competence, including knowledge, application of knowledge, efficiency, ability to make decisions, and attitude toward patients. Every person in the department—say, the ED—could anonymously complete the survey. (This would include nurses, techs, other PAs/NPs, housekeeping, on-call members of the medical staff—literally everybody, although not all of them will be capable of making some of these determinations.) Then the ED director would let the clinician review and discuss the feedback. Everyone in the department would know he or she would be similarly evaluated.6
This is the most brutal, yet fair and efficient, way to assess competency in its broadest sense. Will all opinions be factually substantiated? No! But what better technique do we have, at least for now?
But wait! Perhaps competence is not the end game. Perhaps competence is really a minimum standard. Competence (albeit novice) is measured by completion of the PA or NP curricula (meeting the course objectives) and passage of board/licensure exams, just as, essentially, physician competence is.
Most, if not all, would agree that mastery is achieved by the acquisition of knowledge coupled with sound practice and experience. Mastery or expertise, some say, is what we should focus on, the achievement of which is quite individual. All clinicians can move toward mastery, but not all will actually achieve it. Therefore, how can we mandate a minimum standard, beyond competence, for PAs and NPs but not for other providers?
So, after all the rhetorical ranting about when a PA or NP becomes fully competent, the answer is … It depends! There are too many moving parts. I would suggest that competency is the starting point and mastery (expertise) is a journey.
What do you think? Share your thoughts with me via PAEditor@frontlinemedcom.com.
REFERENCES
1. Norman GR. Defining competence: a methodological review. In: Neufeld VR, Norman GR, eds. Assessing Clinical Competence. New York, NY: Springer; 1985:15-35.
2. Gentile DL. Applying the novice-to-expert model to infusion nursing. J Infus Nurs. 2012;35(2):101-107.
3. Benner P. From novice to expert. Am J Nurs. 1982;82(3):402-407.
4. Brykczynski KA. Patricia Benner: caring, clinical wisdom, and ethics in nursing practice. In: Alligood MR, ed. Nursing Theorists and Their Work. 8th ed. St Louis, MO: Elsevier. 2014; 120-146.
5. Chuck E. The competency manifesto: part 3. The Student Doctor Network. www.student doctor.net/2011/04/the-competency-mani festo-part-3. Accessed November 11, 2014.
6. Lepsinger R, Luca AD. The Art and Science of 360-Degree Feedback. 2nd ed. San Francisco, CA: Jossey-Bass; 2009.
I’ve Been Framed!
Making a correct diagnosis is the central cognitive endeavor of every clinician, since an accurate diagnosis usually leads to appropriate treatment. As PAs and NPs, we dread missing a diagnosis: jaw pain that turns out to be angina or back pain that ends up being an aortic aneurysm. And then of course, there are preventable infections and medication errors.
Several studies in the medical literature indicate that misdiagnosis occurs in 15% to 20% of all cases; in half of these, the patient is harmed. The vast majority of misdiagnoses, about 80%, are due to cognitive errors—in other words, errors in thinking!
This was recently brought home to me through an online course required by my malpractice insurance carrier. The focus was cognitive errors in diagnosis. Prior to starting, I expected it to be a no brainer. After all, every clinician knows what malpractice entails and how best to avoid it, right? We have attended CME courses and read plenty of articles on the topic.
Well, this course was different and had a rather sobering effect on me. As a result, I started to ponder the process we go through to establish a diagnosis.
For the most part, formulating a diagnosis is largely subconscious, and our ability to do it increases with experience.1 The normative model is Bayes’ theorem, an application of conditional probabilities. Clinicians use information on the prevalence of various clinical features in different disease entities to determine the probability that a particular condition is present. The theorem is considered a milestone in logical reasoning and a conquest of statistical inference, although it is still treated with suspicion by most clinicians.
What makes this method potentially impractical is the complexity of the calculations and the fact that not all required information may be readily available. Would you agree that it is impossible to search for and consider all required information or evaluate all possible hypotheses? Therefore, the search for the correct clinical diagnosis is limited to satisfactory explanations within the constraints of the clinical environment.2
Another model for clinical diagnosis is the hypothetico-deductive model. Clinicians achieve a diagnosis by generating multiple competing hypotheses from initial patient cues and collecting data to confirm or refute each. This model has been validated through empirical studies.3 Most clinicians, in my experience, use a combination of intuitive, reflective, and analytical problem solving, with some approaches given more emphasis than others.
On the next page: Categories of diagnostic errors >>
According to Graber et al4, diagnostic errors fall into three categories:
“No-Fault” Errors: The illness is silent, masked, or unusual in its presentation, or the patient misrepresents symptoms.
System-Related: This includes erroneous information in the patient record, technical and/or equipment failures, incorrect test results, poor coordination, and organizational flaws.
Cognitive: Herein lies faulty data collection, interpretation/reasoning, or incomplete knowledge on the part of the clinician. The information necessary to draw the right conclusion is available, or easily found, but the wrong conclusion is reached.4
What really intrigued me is the cognitive framing effect. This is when the diagnosis is unduly influenced by collateral information. There is considerable evidence that we make irrational or biased decisions based on how the expected outcome is framed.
Shortly after taking the malpractice course, I was working in an allergy and asthma practice and had an immunotherapy patient on my schedule who was listed as “same day/sick.” I entered the room thinking her symptoms could be related to her allergic rhinitis or extrinsic asthma or perhaps an adverse reaction to that week’s allergy shot. What I found was a 38-year-old woman with a three-day history of a 103°F fever, severe neck pain, headache, and severe malaise. Sparing all other information, suffice it to say she was sent directly to the emergency department (ED), where she was admitted.
I am also aware of a case in which a patient with shortness of breath was treated in an ED with an erroneous diagnosis of COPD with a “long-standing benign murmur.” She was in a room with nebulizers on the nightstand and a diagnosis of “COPD exacerbation” and later died of aortic stenosis. Sometimes, inaccurate prior information or collateral evidence frames a problem as pulmonary when it is really cardiac.
Essentially, clinicians may be influenced by the way in which the problem is framed. For example, perceptions of risk to the patient may be influenced by the possible outcome (eg, is the patient likely to die?), the type of clinic, or even the time of day.5 Framing may also occur when another clinician presents a case to you that is influenced by his or her own bias.
On the next page: How to avoid framing bias >>
There are some remedies to avoid framing bias:
• Acknowledge that framing bias may exist, and be on the lookout for it.
• Improve your knowledge and experience through use of simulations, improved feedback on decision outcomes, and focused CME on known pitfalls in specific diseases/scenarios.
• Improve your clinical reasoning through reflective practices. Slow down (easy for me to say) and think. Perform a metacognitive review, and recognize the traps associated with relying on rules-of-thumb.
• Provide cognitive help through technological support and algorithms (eg, through electronic medical record prompts), and ensure access to second opinions from colleagues.
• Reduce the “cognitive load” by modifying work schedules and the number of patients to be seen. Reduce distractions and interruptions in the work environment.6
With the time constraints and frenzied nature of modern health care, there is, I believe, value in stopping to reflect on our thinking, particularly when an original presumption about a diagnosis appears not to succeed in explaining the complaint or empiric therapy does not improve the patient’s symptoms. At these times, drawing on both intuitive and deliberative thinking can be fundamental in avoiding thought traps and moving us onto a better diagnostic path.
I have not meant to oversimplify an obviously complex topic, but I would love to hear from you on your opinion about this topic. Contact me at PAEditor@frontlinemedcom.com.
REFERENCES
1. Nkanginieme KEO. Clinical diagnosis as
a dynamic cognitive process: application
of Bloom’s taxonomy for educational objectives in the cognitive domain. Med Educ Online [serial online]. 1997;2:1. www.msu.edu/~dsolomon/f0000007.pdf. Accessed May 14, 2014.
2. Phua DH, Tan NC. Cognitive aspect of diagnostic errors. Ann Acad Med Singapore. 2013; 42(1):33-41.
3. Charlin B, Tardif J, Boshuizen HP. Scripts and medical diagnostic knowledge: theory and applications for clinical reasoning instruction and research. Acad Med. 2000;75(2):182-190.
4. Graber ML, Franklin N, Gordoin R. Diagnostic error in internal medicine. Arch Intern Med. 2005;165(13):1493-1499.
5. Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med. 2003;78(8):775-780.
6. Perkocha L. Cognitive error in medical diagnosis: what we now know. Presented at University of Hawaii John A Burns School of Medicine Reunion, July 27, 2013. https://jabsom.hawaii.edu/JABSOM/departments/CME/doc/Perkocha.pdf. Accessed May 14, 2014. 5, 2014.
Making a correct diagnosis is the central cognitive endeavor of every clinician, since an accurate diagnosis usually leads to appropriate treatment. As PAs and NPs, we dread missing a diagnosis: jaw pain that turns out to be angina or back pain that ends up being an aortic aneurysm. And then of course, there are preventable infections and medication errors.
Several studies in the medical literature indicate that misdiagnosis occurs in 15% to 20% of all cases; in half of these, the patient is harmed. The vast majority of misdiagnoses, about 80%, are due to cognitive errors—in other words, errors in thinking!
This was recently brought home to me through an online course required by my malpractice insurance carrier. The focus was cognitive errors in diagnosis. Prior to starting, I expected it to be a no brainer. After all, every clinician knows what malpractice entails and how best to avoid it, right? We have attended CME courses and read plenty of articles on the topic.
Well, this course was different and had a rather sobering effect on me. As a result, I started to ponder the process we go through to establish a diagnosis.
For the most part, formulating a diagnosis is largely subconscious, and our ability to do it increases with experience.1 The normative model is Bayes’ theorem, an application of conditional probabilities. Clinicians use information on the prevalence of various clinical features in different disease entities to determine the probability that a particular condition is present. The theorem is considered a milestone in logical reasoning and a conquest of statistical inference, although it is still treated with suspicion by most clinicians.
What makes this method potentially impractical is the complexity of the calculations and the fact that not all required information may be readily available. Would you agree that it is impossible to search for and consider all required information or evaluate all possible hypotheses? Therefore, the search for the correct clinical diagnosis is limited to satisfactory explanations within the constraints of the clinical environment.2
Another model for clinical diagnosis is the hypothetico-deductive model. Clinicians achieve a diagnosis by generating multiple competing hypotheses from initial patient cues and collecting data to confirm or refute each. This model has been validated through empirical studies.3 Most clinicians, in my experience, use a combination of intuitive, reflective, and analytical problem solving, with some approaches given more emphasis than others.
On the next page: Categories of diagnostic errors >>
According to Graber et al4, diagnostic errors fall into three categories:
“No-Fault” Errors: The illness is silent, masked, or unusual in its presentation, or the patient misrepresents symptoms.
System-Related: This includes erroneous information in the patient record, technical and/or equipment failures, incorrect test results, poor coordination, and organizational flaws.
Cognitive: Herein lies faulty data collection, interpretation/reasoning, or incomplete knowledge on the part of the clinician. The information necessary to draw the right conclusion is available, or easily found, but the wrong conclusion is reached.4
What really intrigued me is the cognitive framing effect. This is when the diagnosis is unduly influenced by collateral information. There is considerable evidence that we make irrational or biased decisions based on how the expected outcome is framed.
Shortly after taking the malpractice course, I was working in an allergy and asthma practice and had an immunotherapy patient on my schedule who was listed as “same day/sick.” I entered the room thinking her symptoms could be related to her allergic rhinitis or extrinsic asthma or perhaps an adverse reaction to that week’s allergy shot. What I found was a 38-year-old woman with a three-day history of a 103°F fever, severe neck pain, headache, and severe malaise. Sparing all other information, suffice it to say she was sent directly to the emergency department (ED), where she was admitted.
I am also aware of a case in which a patient with shortness of breath was treated in an ED with an erroneous diagnosis of COPD with a “long-standing benign murmur.” She was in a room with nebulizers on the nightstand and a diagnosis of “COPD exacerbation” and later died of aortic stenosis. Sometimes, inaccurate prior information or collateral evidence frames a problem as pulmonary when it is really cardiac.
Essentially, clinicians may be influenced by the way in which the problem is framed. For example, perceptions of risk to the patient may be influenced by the possible outcome (eg, is the patient likely to die?), the type of clinic, or even the time of day.5 Framing may also occur when another clinician presents a case to you that is influenced by his or her own bias.
On the next page: How to avoid framing bias >>
There are some remedies to avoid framing bias:
• Acknowledge that framing bias may exist, and be on the lookout for it.
• Improve your knowledge and experience through use of simulations, improved feedback on decision outcomes, and focused CME on known pitfalls in specific diseases/scenarios.
• Improve your clinical reasoning through reflective practices. Slow down (easy for me to say) and think. Perform a metacognitive review, and recognize the traps associated with relying on rules-of-thumb.
• Provide cognitive help through technological support and algorithms (eg, through electronic medical record prompts), and ensure access to second opinions from colleagues.
• Reduce the “cognitive load” by modifying work schedules and the number of patients to be seen. Reduce distractions and interruptions in the work environment.6
With the time constraints and frenzied nature of modern health care, there is, I believe, value in stopping to reflect on our thinking, particularly when an original presumption about a diagnosis appears not to succeed in explaining the complaint or empiric therapy does not improve the patient’s symptoms. At these times, drawing on both intuitive and deliberative thinking can be fundamental in avoiding thought traps and moving us onto a better diagnostic path.
I have not meant to oversimplify an obviously complex topic, but I would love to hear from you on your opinion about this topic. Contact me at PAEditor@frontlinemedcom.com.
REFERENCES
1. Nkanginieme KEO. Clinical diagnosis as
a dynamic cognitive process: application
of Bloom’s taxonomy for educational objectives in the cognitive domain. Med Educ Online [serial online]. 1997;2:1. www.msu.edu/~dsolomon/f0000007.pdf. Accessed May 14, 2014.
2. Phua DH, Tan NC. Cognitive aspect of diagnostic errors. Ann Acad Med Singapore. 2013; 42(1):33-41.
3. Charlin B, Tardif J, Boshuizen HP. Scripts and medical diagnostic knowledge: theory and applications for clinical reasoning instruction and research. Acad Med. 2000;75(2):182-190.
4. Graber ML, Franklin N, Gordoin R. Diagnostic error in internal medicine. Arch Intern Med. 2005;165(13):1493-1499.
5. Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med. 2003;78(8):775-780.
6. Perkocha L. Cognitive error in medical diagnosis: what we now know. Presented at University of Hawaii John A Burns School of Medicine Reunion, July 27, 2013. https://jabsom.hawaii.edu/JABSOM/departments/CME/doc/Perkocha.pdf. Accessed May 14, 2014. 5, 2014.
Making a correct diagnosis is the central cognitive endeavor of every clinician, since an accurate diagnosis usually leads to appropriate treatment. As PAs and NPs, we dread missing a diagnosis: jaw pain that turns out to be angina or back pain that ends up being an aortic aneurysm. And then of course, there are preventable infections and medication errors.
Several studies in the medical literature indicate that misdiagnosis occurs in 15% to 20% of all cases; in half of these, the patient is harmed. The vast majority of misdiagnoses, about 80%, are due to cognitive errors—in other words, errors in thinking!
This was recently brought home to me through an online course required by my malpractice insurance carrier. The focus was cognitive errors in diagnosis. Prior to starting, I expected it to be a no brainer. After all, every clinician knows what malpractice entails and how best to avoid it, right? We have attended CME courses and read plenty of articles on the topic.
Well, this course was different and had a rather sobering effect on me. As a result, I started to ponder the process we go through to establish a diagnosis.
For the most part, formulating a diagnosis is largely subconscious, and our ability to do it increases with experience.1 The normative model is Bayes’ theorem, an application of conditional probabilities. Clinicians use information on the prevalence of various clinical features in different disease entities to determine the probability that a particular condition is present. The theorem is considered a milestone in logical reasoning and a conquest of statistical inference, although it is still treated with suspicion by most clinicians.
What makes this method potentially impractical is the complexity of the calculations and the fact that not all required information may be readily available. Would you agree that it is impossible to search for and consider all required information or evaluate all possible hypotheses? Therefore, the search for the correct clinical diagnosis is limited to satisfactory explanations within the constraints of the clinical environment.2
Another model for clinical diagnosis is the hypothetico-deductive model. Clinicians achieve a diagnosis by generating multiple competing hypotheses from initial patient cues and collecting data to confirm or refute each. This model has been validated through empirical studies.3 Most clinicians, in my experience, use a combination of intuitive, reflective, and analytical problem solving, with some approaches given more emphasis than others.
On the next page: Categories of diagnostic errors >>
According to Graber et al4, diagnostic errors fall into three categories:
“No-Fault” Errors: The illness is silent, masked, or unusual in its presentation, or the patient misrepresents symptoms.
System-Related: This includes erroneous information in the patient record, technical and/or equipment failures, incorrect test results, poor coordination, and organizational flaws.
Cognitive: Herein lies faulty data collection, interpretation/reasoning, or incomplete knowledge on the part of the clinician. The information necessary to draw the right conclusion is available, or easily found, but the wrong conclusion is reached.4
What really intrigued me is the cognitive framing effect. This is when the diagnosis is unduly influenced by collateral information. There is considerable evidence that we make irrational or biased decisions based on how the expected outcome is framed.
Shortly after taking the malpractice course, I was working in an allergy and asthma practice and had an immunotherapy patient on my schedule who was listed as “same day/sick.” I entered the room thinking her symptoms could be related to her allergic rhinitis or extrinsic asthma or perhaps an adverse reaction to that week’s allergy shot. What I found was a 38-year-old woman with a three-day history of a 103°F fever, severe neck pain, headache, and severe malaise. Sparing all other information, suffice it to say she was sent directly to the emergency department (ED), where she was admitted.
I am also aware of a case in which a patient with shortness of breath was treated in an ED with an erroneous diagnosis of COPD with a “long-standing benign murmur.” She was in a room with nebulizers on the nightstand and a diagnosis of “COPD exacerbation” and later died of aortic stenosis. Sometimes, inaccurate prior information or collateral evidence frames a problem as pulmonary when it is really cardiac.
Essentially, clinicians may be influenced by the way in which the problem is framed. For example, perceptions of risk to the patient may be influenced by the possible outcome (eg, is the patient likely to die?), the type of clinic, or even the time of day.5 Framing may also occur when another clinician presents a case to you that is influenced by his or her own bias.
On the next page: How to avoid framing bias >>
There are some remedies to avoid framing bias:
• Acknowledge that framing bias may exist, and be on the lookout for it.
• Improve your knowledge and experience through use of simulations, improved feedback on decision outcomes, and focused CME on known pitfalls in specific diseases/scenarios.
• Improve your clinical reasoning through reflective practices. Slow down (easy for me to say) and think. Perform a metacognitive review, and recognize the traps associated with relying on rules-of-thumb.
• Provide cognitive help through technological support and algorithms (eg, through electronic medical record prompts), and ensure access to second opinions from colleagues.
• Reduce the “cognitive load” by modifying work schedules and the number of patients to be seen. Reduce distractions and interruptions in the work environment.6
With the time constraints and frenzied nature of modern health care, there is, I believe, value in stopping to reflect on our thinking, particularly when an original presumption about a diagnosis appears not to succeed in explaining the complaint or empiric therapy does not improve the patient’s symptoms. At these times, drawing on both intuitive and deliberative thinking can be fundamental in avoiding thought traps and moving us onto a better diagnostic path.
I have not meant to oversimplify an obviously complex topic, but I would love to hear from you on your opinion about this topic. Contact me at PAEditor@frontlinemedcom.com.
REFERENCES
1. Nkanginieme KEO. Clinical diagnosis as
a dynamic cognitive process: application
of Bloom’s taxonomy for educational objectives in the cognitive domain. Med Educ Online [serial online]. 1997;2:1. www.msu.edu/~dsolomon/f0000007.pdf. Accessed May 14, 2014.
2. Phua DH, Tan NC. Cognitive aspect of diagnostic errors. Ann Acad Med Singapore. 2013; 42(1):33-41.
3. Charlin B, Tardif J, Boshuizen HP. Scripts and medical diagnostic knowledge: theory and applications for clinical reasoning instruction and research. Acad Med. 2000;75(2):182-190.
4. Graber ML, Franklin N, Gordoin R. Diagnostic error in internal medicine. Arch Intern Med. 2005;165(13):1493-1499.
5. Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med. 2003;78(8):775-780.
6. Perkocha L. Cognitive error in medical diagnosis: what we now know. Presented at University of Hawaii John A Burns School of Medicine Reunion, July 27, 2013. https://jabsom.hawaii.edu/JABSOM/departments/CME/doc/Perkocha.pdf. Accessed May 14, 2014. 5, 2014.
Do You Love Your Job? Survey Says …
There is no doubt that nurse practitioners and physician assistants are in demand in the US workforce. A 2013 survey of more than 300 large multispecialty health care organizations indicated that about two-thirds of them had increased their NP/PA workforce and were projecting additional hiring in the next 12 months. Also of note: 31% of these organizations reported having an NP/PA in an administrative role (an increase from 20% in 2012).1
But along with being in demand, our jobs have become increasingly demanding. Health care is changing, not least because of a shortage of primary care physicians, baby boomers increasing their consumption of health care, an increase in chronic disease care, and the growing complexity of health care management. Historically, large studies by our national professional organizations have indicated that NPs and PAs are predominantly satisfied with their role and their future professional prospects. But is that still the case today?
With that question in mind, a quasi-scientific nationwide survey was conducted at the behest of NP Editor-in-Chief Marie-Eileen Onieal and myself. We wanted to determine whether PAs and NPs are satisfied with their work and the state of their profession. This survey, fielded over a two-week period in February, involved a self-selected sample derived from an invitation to almost 100,000 PAs and NPs via the Clinician Reviews mailing list, as well as a posting on the Web site. It should be noted here, for my statistician friends, that this sample may not be representative of the population—but it does create the opportunity for discussion. People who respond to these types of surveys tend to feel strongly, one way or another, about the issues; this questionnaire was no exception.
A total of 240 clinicians participated: 145 NPs (60%) and 95 PAs (40%). The majority (88% of NPs and 86% of PAs) reported being in clinical practice, and 29% of NP respondents and 45% of PA respondents indicated that they have been in their profession for more than 20 years.
Demographically, more women than men participated (NPs, 94%; PAs, 58%), 71% of respondents were between ages 50 and 69, and almost 90% were white. The last item begs the question of the professional satisfaction of nonwhite NPs and PAs. As in other medical fields, the NP and PA professions do not currently emulate the diversity of the US population—which is something we should strive for (perhaps a topic for a future editorial).
Most respondents had “very positive” feelings about their profession (NPs, 73%; PAs, 65%), and many reported feeling “somewhat positive” (NPs, 23%; PAs, 28%). Only 4% of NPs and 7% of PAs expressed negative feelings about the current state of their profession. Perhaps not surprisingly, the majority of both NPs (58%) and PAs (65%) also indicated feeling “very positive” about the future of their profession. Overall, 66% of NPs and 60% of PAs said they would choose the same profession if they had the opportunity again.
So what, if any, are the drawbacks to being a PA or NP? Well, with regard to workload, participants most commonly endorsed the response that they were working at full capacity but not overextended or overworked (NPs, 43%; PAs, 51%), and the majority felt they were adequately compensated for their work (NPs, 69%; PAs, 73%). However, a significant portion of the remaining respondents had less positive feelings on both subjects; Table 1 and Table 2 provide full data.
Continued on next page >>
The fact that almost one-third of NPs and one-fourth of PAs feel they are overextended and overworked is not lost here. This information is interesting in light of the projection that the workloads of NPs and PAs will increase with the introduction and expansion of team-based health care and with the implementation in primary care of the “medical home” practice model.
Participants were invited to append comments to their responses; these, while of course anecdotal, were rather illuminating of the mindset “in the trenches.” Many clinicians commented on the satisfaction they achieve from providing care and education to patients, their independence as practitioners, and the intellectual and instinctual challenges of diagnosis.
However, several voiced the opinion that NP and PA education programs are no longer as “competitive” as they used to be, noting that the expansion of such programs has led to a perceived attitude of “If you have the dough, you can go.” (As the dean of a PA program, I am of course concerned by this perspective.) This view of the educational system was also reflected in the response to a question about pursuit of a clinical doctorate, with 67% of NPs and 86% of PAs indicating they felt it would not enhance their ability to practice. (On the other hand, one wonders if this is because the majority of respondents are older and have been in the profession longer.)
A similar study by Jackson Healthcare (2012-2013) also noted high levels of job satisfaction among NPs and PAs, with only 5% reporting that they were “very dissatisfied.” In that survey, the five top drivers of NP/PA satisfaction included work environment (37%), patients (28%), compensation (27%), autonomy (21%), and growth opportunities (14%).2
In the same study, NPs and PAs were asked about negative aspects of their jobs. Respondents voiced concern over patient confusion with the NP/PA role, increased administrative duties, and problems with electronic medical records. A significant number mentioned a lack of understanding by physicians and others about the role PAs and NPs play in health care.2
The Jackson study corroborates our findings that overall, NPs and PAs are satisfied with our role and the future of our professions. Our professions continue to be critically important in responding to the converging trends in health care, so it is heartening to see that they continue to offer attractive, fulfilling opportunities to serve tomorrow’s health care needs. At the same time, it is evident that there are some areas with room for improvement. What are your thoughts (good and bad)?
Email me at PAEditor@frontlinemedcom.com.
REFERENCES
1. American Medical Group Association. Survey Reveals Advanced Practice Clinician Workforce Continues to Grow and Incentive Pay Is an Increasing Part of the Compensation Mix [press release]. February 12, 2014. www.amga.org/AboutAMGA/News/article_news.asp?k=727. Accessed February 28, 2014.
2. Jackson Healthcare. Advanced Practice Trends 2012-2013: An Attitude & Outlook on Nurse Practitioners and Physician Assistants. www.jacksonhealthcare.com/media/182734/advancedpracticetrendsreport_ebook0313_lr.pdf. Accessed March 21, 2014.
There is no doubt that nurse practitioners and physician assistants are in demand in the US workforce. A 2013 survey of more than 300 large multispecialty health care organizations indicated that about two-thirds of them had increased their NP/PA workforce and were projecting additional hiring in the next 12 months. Also of note: 31% of these organizations reported having an NP/PA in an administrative role (an increase from 20% in 2012).1
But along with being in demand, our jobs have become increasingly demanding. Health care is changing, not least because of a shortage of primary care physicians, baby boomers increasing their consumption of health care, an increase in chronic disease care, and the growing complexity of health care management. Historically, large studies by our national professional organizations have indicated that NPs and PAs are predominantly satisfied with their role and their future professional prospects. But is that still the case today?
With that question in mind, a quasi-scientific nationwide survey was conducted at the behest of NP Editor-in-Chief Marie-Eileen Onieal and myself. We wanted to determine whether PAs and NPs are satisfied with their work and the state of their profession. This survey, fielded over a two-week period in February, involved a self-selected sample derived from an invitation to almost 100,000 PAs and NPs via the Clinician Reviews mailing list, as well as a posting on the Web site. It should be noted here, for my statistician friends, that this sample may not be representative of the population—but it does create the opportunity for discussion. People who respond to these types of surveys tend to feel strongly, one way or another, about the issues; this questionnaire was no exception.
A total of 240 clinicians participated: 145 NPs (60%) and 95 PAs (40%). The majority (88% of NPs and 86% of PAs) reported being in clinical practice, and 29% of NP respondents and 45% of PA respondents indicated that they have been in their profession for more than 20 years.
Demographically, more women than men participated (NPs, 94%; PAs, 58%), 71% of respondents were between ages 50 and 69, and almost 90% were white. The last item begs the question of the professional satisfaction of nonwhite NPs and PAs. As in other medical fields, the NP and PA professions do not currently emulate the diversity of the US population—which is something we should strive for (perhaps a topic for a future editorial).
Most respondents had “very positive” feelings about their profession (NPs, 73%; PAs, 65%), and many reported feeling “somewhat positive” (NPs, 23%; PAs, 28%). Only 4% of NPs and 7% of PAs expressed negative feelings about the current state of their profession. Perhaps not surprisingly, the majority of both NPs (58%) and PAs (65%) also indicated feeling “very positive” about the future of their profession. Overall, 66% of NPs and 60% of PAs said they would choose the same profession if they had the opportunity again.
So what, if any, are the drawbacks to being a PA or NP? Well, with regard to workload, participants most commonly endorsed the response that they were working at full capacity but not overextended or overworked (NPs, 43%; PAs, 51%), and the majority felt they were adequately compensated for their work (NPs, 69%; PAs, 73%). However, a significant portion of the remaining respondents had less positive feelings on both subjects; Table 1 and Table 2 provide full data.
Continued on next page >>
The fact that almost one-third of NPs and one-fourth of PAs feel they are overextended and overworked is not lost here. This information is interesting in light of the projection that the workloads of NPs and PAs will increase with the introduction and expansion of team-based health care and with the implementation in primary care of the “medical home” practice model.
Participants were invited to append comments to their responses; these, while of course anecdotal, were rather illuminating of the mindset “in the trenches.” Many clinicians commented on the satisfaction they achieve from providing care and education to patients, their independence as practitioners, and the intellectual and instinctual challenges of diagnosis.
However, several voiced the opinion that NP and PA education programs are no longer as “competitive” as they used to be, noting that the expansion of such programs has led to a perceived attitude of “If you have the dough, you can go.” (As the dean of a PA program, I am of course concerned by this perspective.) This view of the educational system was also reflected in the response to a question about pursuit of a clinical doctorate, with 67% of NPs and 86% of PAs indicating they felt it would not enhance their ability to practice. (On the other hand, one wonders if this is because the majority of respondents are older and have been in the profession longer.)
A similar study by Jackson Healthcare (2012-2013) also noted high levels of job satisfaction among NPs and PAs, with only 5% reporting that they were “very dissatisfied.” In that survey, the five top drivers of NP/PA satisfaction included work environment (37%), patients (28%), compensation (27%), autonomy (21%), and growth opportunities (14%).2
In the same study, NPs and PAs were asked about negative aspects of their jobs. Respondents voiced concern over patient confusion with the NP/PA role, increased administrative duties, and problems with electronic medical records. A significant number mentioned a lack of understanding by physicians and others about the role PAs and NPs play in health care.2
The Jackson study corroborates our findings that overall, NPs and PAs are satisfied with our role and the future of our professions. Our professions continue to be critically important in responding to the converging trends in health care, so it is heartening to see that they continue to offer attractive, fulfilling opportunities to serve tomorrow’s health care needs. At the same time, it is evident that there are some areas with room for improvement. What are your thoughts (good and bad)?
Email me at PAEditor@frontlinemedcom.com.
REFERENCES
1. American Medical Group Association. Survey Reveals Advanced Practice Clinician Workforce Continues to Grow and Incentive Pay Is an Increasing Part of the Compensation Mix [press release]. February 12, 2014. www.amga.org/AboutAMGA/News/article_news.asp?k=727. Accessed February 28, 2014.
2. Jackson Healthcare. Advanced Practice Trends 2012-2013: An Attitude & Outlook on Nurse Practitioners and Physician Assistants. www.jacksonhealthcare.com/media/182734/advancedpracticetrendsreport_ebook0313_lr.pdf. Accessed March 21, 2014.
There is no doubt that nurse practitioners and physician assistants are in demand in the US workforce. A 2013 survey of more than 300 large multispecialty health care organizations indicated that about two-thirds of them had increased their NP/PA workforce and were projecting additional hiring in the next 12 months. Also of note: 31% of these organizations reported having an NP/PA in an administrative role (an increase from 20% in 2012).1
But along with being in demand, our jobs have become increasingly demanding. Health care is changing, not least because of a shortage of primary care physicians, baby boomers increasing their consumption of health care, an increase in chronic disease care, and the growing complexity of health care management. Historically, large studies by our national professional organizations have indicated that NPs and PAs are predominantly satisfied with their role and their future professional prospects. But is that still the case today?
With that question in mind, a quasi-scientific nationwide survey was conducted at the behest of NP Editor-in-Chief Marie-Eileen Onieal and myself. We wanted to determine whether PAs and NPs are satisfied with their work and the state of their profession. This survey, fielded over a two-week period in February, involved a self-selected sample derived from an invitation to almost 100,000 PAs and NPs via the Clinician Reviews mailing list, as well as a posting on the Web site. It should be noted here, for my statistician friends, that this sample may not be representative of the population—but it does create the opportunity for discussion. People who respond to these types of surveys tend to feel strongly, one way or another, about the issues; this questionnaire was no exception.
A total of 240 clinicians participated: 145 NPs (60%) and 95 PAs (40%). The majority (88% of NPs and 86% of PAs) reported being in clinical practice, and 29% of NP respondents and 45% of PA respondents indicated that they have been in their profession for more than 20 years.
Demographically, more women than men participated (NPs, 94%; PAs, 58%), 71% of respondents were between ages 50 and 69, and almost 90% were white. The last item begs the question of the professional satisfaction of nonwhite NPs and PAs. As in other medical fields, the NP and PA professions do not currently emulate the diversity of the US population—which is something we should strive for (perhaps a topic for a future editorial).
Most respondents had “very positive” feelings about their profession (NPs, 73%; PAs, 65%), and many reported feeling “somewhat positive” (NPs, 23%; PAs, 28%). Only 4% of NPs and 7% of PAs expressed negative feelings about the current state of their profession. Perhaps not surprisingly, the majority of both NPs (58%) and PAs (65%) also indicated feeling “very positive” about the future of their profession. Overall, 66% of NPs and 60% of PAs said they would choose the same profession if they had the opportunity again.
So what, if any, are the drawbacks to being a PA or NP? Well, with regard to workload, participants most commonly endorsed the response that they were working at full capacity but not overextended or overworked (NPs, 43%; PAs, 51%), and the majority felt they were adequately compensated for their work (NPs, 69%; PAs, 73%). However, a significant portion of the remaining respondents had less positive feelings on both subjects; Table 1 and Table 2 provide full data.
Continued on next page >>
The fact that almost one-third of NPs and one-fourth of PAs feel they are overextended and overworked is not lost here. This information is interesting in light of the projection that the workloads of NPs and PAs will increase with the introduction and expansion of team-based health care and with the implementation in primary care of the “medical home” practice model.
Participants were invited to append comments to their responses; these, while of course anecdotal, were rather illuminating of the mindset “in the trenches.” Many clinicians commented on the satisfaction they achieve from providing care and education to patients, their independence as practitioners, and the intellectual and instinctual challenges of diagnosis.
However, several voiced the opinion that NP and PA education programs are no longer as “competitive” as they used to be, noting that the expansion of such programs has led to a perceived attitude of “If you have the dough, you can go.” (As the dean of a PA program, I am of course concerned by this perspective.) This view of the educational system was also reflected in the response to a question about pursuit of a clinical doctorate, with 67% of NPs and 86% of PAs indicating they felt it would not enhance their ability to practice. (On the other hand, one wonders if this is because the majority of respondents are older and have been in the profession longer.)
A similar study by Jackson Healthcare (2012-2013) also noted high levels of job satisfaction among NPs and PAs, with only 5% reporting that they were “very dissatisfied.” In that survey, the five top drivers of NP/PA satisfaction included work environment (37%), patients (28%), compensation (27%), autonomy (21%), and growth opportunities (14%).2
In the same study, NPs and PAs were asked about negative aspects of their jobs. Respondents voiced concern over patient confusion with the NP/PA role, increased administrative duties, and problems with electronic medical records. A significant number mentioned a lack of understanding by physicians and others about the role PAs and NPs play in health care.2
The Jackson study corroborates our findings that overall, NPs and PAs are satisfied with our role and the future of our professions. Our professions continue to be critically important in responding to the converging trends in health care, so it is heartening to see that they continue to offer attractive, fulfilling opportunities to serve tomorrow’s health care needs. At the same time, it is evident that there are some areas with room for improvement. What are your thoughts (good and bad)?
Email me at PAEditor@frontlinemedcom.com.
REFERENCES
1. American Medical Group Association. Survey Reveals Advanced Practice Clinician Workforce Continues to Grow and Incentive Pay Is an Increasing Part of the Compensation Mix [press release]. February 12, 2014. www.amga.org/AboutAMGA/News/article_news.asp?k=727. Accessed February 28, 2014.
2. Jackson Healthcare. Advanced Practice Trends 2012-2013: An Attitude & Outlook on Nurse Practitioners and Physician Assistants. www.jacksonhealthcare.com/media/182734/advancedpracticetrendsreport_ebook0313_lr.pdf. Accessed March 21, 2014.
Swimming With Sharks
Not too long ago, I was sitting with a couple of my best friends talking about people in our lives whom we admired and who have made a difference. Family members and close relatives were discussed, as were others unknown to us personally. We talked about John F. Kennedy, Norman Schwarzkopf, and Nelson Mandela. Well, after reading a bit about her, I have decided to add Diana Nyad to my list.
Nyad is the woman who, at age 64, swam in shark- and jellyfish-infested waters (without a shark cage) from Cuba to Key West last year.1 When asked if she was afraid of the sharks and jellyfish, she said she just swam past them—they were afraid of her.
If that isn’t impressive enough, you should know that she first started this quest (inside a shark cage) in 1978 at age 28 and was nearly 42 hours in before her team doctors demanded she end her journey. She tried again many years later, in 2010, 2011, and 2012, with each of those attempts curtailed by bad weather and/or jellyfish and Portuguese man-of-war stings. But she was determined not to quit, even though, given her age, no one would have blamed her for just retiring. After all, the greatest swimmers in the world had attempted this feat without success since 1950.
After hearing about her adventures, some have dismissed her as a thrill-seeker and narcissist. Why, they ask, was she willing to risk her life repeatedly to accomplish something that ultimately “amounts to a stunt”?2 But whether others can understand it or not, her quest to swim the 110 miles of treacherous open waters from Cuba to Florida gave her purpose. It was her raison d’être.
Why did Nyad attempt the impossible for a fifth time? She said she awoke one day wondering how much of her life was left and realized she could still fulfill her dream. In an interview,1 Nyad said it was not the 53 hours of swimming to attain the record that was significant to her; it was the previous 30 years of never abandoning her dreams—even when neurologists, endurance experts, and her own team said it couldn’t be done “at her age.” The team mantra for this final effort was “Find a Way!”
And in that we have a valuable lesson about perseverance. So much of everyday life is about showing up, working hard, and making sacrifices. In the struggle and the chaos, we often lose track of our goals and dreams. What Diana Nyad has shown us is that we should never stop believing that our dreams are achievable. She has also shown us, however, that they cannot be accomplished without persistence and hard work.
Without question, what she accomplished is remarkable for anyone. The fact that she was 64 when she made her final, successful attempt—an age at which most of us are expected to be thinking about retirement—is extraordinary. But we don’t have to attempt to match her feat to achieve a sense of satisfaction and purpose. Most of us will never actually swim with sharks, but we can take Nyad’s example as a metaphor for how we should live our lives—always striving, always believing, and always learning as much (if not more) from our failures as from our successes.
As any of the individuals mentioned earlier (Kennedy, Schwarzkopf, Mandela) would surely attest, failure is a vital part of success that makes accomplishments so satisfying. Every day is epic! What matters is taking what we have to work with and making the most of it.
One of my favorite quotes by Teddy Roosevelt is:
It is not the critic who counts; not the man who points out how the strong man stumbles, or where the doer of deeds could have done them better. The credit belongs to the man who is actually in the arena, whose face is marred by dust and sweat and blood; who strives valiantly; who errs, who comes short again and again, because there is no effort without error and shortcoming; but who does actually strive to do the deeds; who knows great enthusiasms, the great devotions; who spends himself in a worthy cause; who at the best knows in the end the triumph of high achievement, and who at the worst, if he fails, at least fails while daring greatly, so that his place shall never be with those cold and timid souls who neither know victory nor defeat.3
If there is anything to be said about the PA and NP professions, it is that we are resilient! I’m not suggesting we are swimming with sharks—but I am suggesting we should be proud of our professions and remain resilient and always “Find a Way!” Please share your thoughts with me at PAEditor@frontlinemedcom.com.
References
1. TED. Diana Nyad: Never, ever give up [video]. www.ted.com/talks/diana_nyad_never_ever_give_up.html. Accessed January 10, 2014.
2. Diana Nyad’s life lesson for the rest of us [editorial]. Dallas Morning News. September 3, 2013. www.dallasnews.com/opinion/editorials/20130903-editorial-diana-nyads-life-lesson-for-the-rest-of-us.ece. Accessed January 10, 2014.
3. Roosevelt T. Excerpt from “Citizenship in a Republic” [speech]; April 23, 1910. www.theodore-roosevelt.com/trsorbonnespeech.html. Accessed January 13, 2014
Not too long ago, I was sitting with a couple of my best friends talking about people in our lives whom we admired and who have made a difference. Family members and close relatives were discussed, as were others unknown to us personally. We talked about John F. Kennedy, Norman Schwarzkopf, and Nelson Mandela. Well, after reading a bit about her, I have decided to add Diana Nyad to my list.
Nyad is the woman who, at age 64, swam in shark- and jellyfish-infested waters (without a shark cage) from Cuba to Key West last year.1 When asked if she was afraid of the sharks and jellyfish, she said she just swam past them—they were afraid of her.
If that isn’t impressive enough, you should know that she first started this quest (inside a shark cage) in 1978 at age 28 and was nearly 42 hours in before her team doctors demanded she end her journey. She tried again many years later, in 2010, 2011, and 2012, with each of those attempts curtailed by bad weather and/or jellyfish and Portuguese man-of-war stings. But she was determined not to quit, even though, given her age, no one would have blamed her for just retiring. After all, the greatest swimmers in the world had attempted this feat without success since 1950.
After hearing about her adventures, some have dismissed her as a thrill-seeker and narcissist. Why, they ask, was she willing to risk her life repeatedly to accomplish something that ultimately “amounts to a stunt”?2 But whether others can understand it or not, her quest to swim the 110 miles of treacherous open waters from Cuba to Florida gave her purpose. It was her raison d’être.
Why did Nyad attempt the impossible for a fifth time? She said she awoke one day wondering how much of her life was left and realized she could still fulfill her dream. In an interview,1 Nyad said it was not the 53 hours of swimming to attain the record that was significant to her; it was the previous 30 years of never abandoning her dreams—even when neurologists, endurance experts, and her own team said it couldn’t be done “at her age.” The team mantra for this final effort was “Find a Way!”
And in that we have a valuable lesson about perseverance. So much of everyday life is about showing up, working hard, and making sacrifices. In the struggle and the chaos, we often lose track of our goals and dreams. What Diana Nyad has shown us is that we should never stop believing that our dreams are achievable. She has also shown us, however, that they cannot be accomplished without persistence and hard work.
Without question, what she accomplished is remarkable for anyone. The fact that she was 64 when she made her final, successful attempt—an age at which most of us are expected to be thinking about retirement—is extraordinary. But we don’t have to attempt to match her feat to achieve a sense of satisfaction and purpose. Most of us will never actually swim with sharks, but we can take Nyad’s example as a metaphor for how we should live our lives—always striving, always believing, and always learning as much (if not more) from our failures as from our successes.
As any of the individuals mentioned earlier (Kennedy, Schwarzkopf, Mandela) would surely attest, failure is a vital part of success that makes accomplishments so satisfying. Every day is epic! What matters is taking what we have to work with and making the most of it.
One of my favorite quotes by Teddy Roosevelt is:
It is not the critic who counts; not the man who points out how the strong man stumbles, or where the doer of deeds could have done them better. The credit belongs to the man who is actually in the arena, whose face is marred by dust and sweat and blood; who strives valiantly; who errs, who comes short again and again, because there is no effort without error and shortcoming; but who does actually strive to do the deeds; who knows great enthusiasms, the great devotions; who spends himself in a worthy cause; who at the best knows in the end the triumph of high achievement, and who at the worst, if he fails, at least fails while daring greatly, so that his place shall never be with those cold and timid souls who neither know victory nor defeat.3
If there is anything to be said about the PA and NP professions, it is that we are resilient! I’m not suggesting we are swimming with sharks—but I am suggesting we should be proud of our professions and remain resilient and always “Find a Way!” Please share your thoughts with me at PAEditor@frontlinemedcom.com.
References
1. TED. Diana Nyad: Never, ever give up [video]. www.ted.com/talks/diana_nyad_never_ever_give_up.html. Accessed January 10, 2014.
2. Diana Nyad’s life lesson for the rest of us [editorial]. Dallas Morning News. September 3, 2013. www.dallasnews.com/opinion/editorials/20130903-editorial-diana-nyads-life-lesson-for-the-rest-of-us.ece. Accessed January 10, 2014.
3. Roosevelt T. Excerpt from “Citizenship in a Republic” [speech]; April 23, 1910. www.theodore-roosevelt.com/trsorbonnespeech.html. Accessed January 13, 2014
Not too long ago, I was sitting with a couple of my best friends talking about people in our lives whom we admired and who have made a difference. Family members and close relatives were discussed, as were others unknown to us personally. We talked about John F. Kennedy, Norman Schwarzkopf, and Nelson Mandela. Well, after reading a bit about her, I have decided to add Diana Nyad to my list.
Nyad is the woman who, at age 64, swam in shark- and jellyfish-infested waters (without a shark cage) from Cuba to Key West last year.1 When asked if she was afraid of the sharks and jellyfish, she said she just swam past them—they were afraid of her.
If that isn’t impressive enough, you should know that she first started this quest (inside a shark cage) in 1978 at age 28 and was nearly 42 hours in before her team doctors demanded she end her journey. She tried again many years later, in 2010, 2011, and 2012, with each of those attempts curtailed by bad weather and/or jellyfish and Portuguese man-of-war stings. But she was determined not to quit, even though, given her age, no one would have blamed her for just retiring. After all, the greatest swimmers in the world had attempted this feat without success since 1950.
After hearing about her adventures, some have dismissed her as a thrill-seeker and narcissist. Why, they ask, was she willing to risk her life repeatedly to accomplish something that ultimately “amounts to a stunt”?2 But whether others can understand it or not, her quest to swim the 110 miles of treacherous open waters from Cuba to Florida gave her purpose. It was her raison d’être.
Why did Nyad attempt the impossible for a fifth time? She said she awoke one day wondering how much of her life was left and realized she could still fulfill her dream. In an interview,1 Nyad said it was not the 53 hours of swimming to attain the record that was significant to her; it was the previous 30 years of never abandoning her dreams—even when neurologists, endurance experts, and her own team said it couldn’t be done “at her age.” The team mantra for this final effort was “Find a Way!”
And in that we have a valuable lesson about perseverance. So much of everyday life is about showing up, working hard, and making sacrifices. In the struggle and the chaos, we often lose track of our goals and dreams. What Diana Nyad has shown us is that we should never stop believing that our dreams are achievable. She has also shown us, however, that they cannot be accomplished without persistence and hard work.
Without question, what she accomplished is remarkable for anyone. The fact that she was 64 when she made her final, successful attempt—an age at which most of us are expected to be thinking about retirement—is extraordinary. But we don’t have to attempt to match her feat to achieve a sense of satisfaction and purpose. Most of us will never actually swim with sharks, but we can take Nyad’s example as a metaphor for how we should live our lives—always striving, always believing, and always learning as much (if not more) from our failures as from our successes.
As any of the individuals mentioned earlier (Kennedy, Schwarzkopf, Mandela) would surely attest, failure is a vital part of success that makes accomplishments so satisfying. Every day is epic! What matters is taking what we have to work with and making the most of it.
One of my favorite quotes by Teddy Roosevelt is:
It is not the critic who counts; not the man who points out how the strong man stumbles, or where the doer of deeds could have done them better. The credit belongs to the man who is actually in the arena, whose face is marred by dust and sweat and blood; who strives valiantly; who errs, who comes short again and again, because there is no effort without error and shortcoming; but who does actually strive to do the deeds; who knows great enthusiasms, the great devotions; who spends himself in a worthy cause; who at the best knows in the end the triumph of high achievement, and who at the worst, if he fails, at least fails while daring greatly, so that his place shall never be with those cold and timid souls who neither know victory nor defeat.3
If there is anything to be said about the PA and NP professions, it is that we are resilient! I’m not suggesting we are swimming with sharks—but I am suggesting we should be proud of our professions and remain resilient and always “Find a Way!” Please share your thoughts with me at PAEditor@frontlinemedcom.com.
References
1. TED. Diana Nyad: Never, ever give up [video]. www.ted.com/talks/diana_nyad_never_ever_give_up.html. Accessed January 10, 2014.
2. Diana Nyad’s life lesson for the rest of us [editorial]. Dallas Morning News. September 3, 2013. www.dallasnews.com/opinion/editorials/20130903-editorial-diana-nyads-life-lesson-for-the-rest-of-us.ece. Accessed January 10, 2014.
3. Roosevelt T. Excerpt from “Citizenship in a Republic” [speech]; April 23, 1910. www.theodore-roosevelt.com/trsorbonnespeech.html. Accessed January 13, 2014
I’d Like to Write a Medical Article, But…
For almost 10 years, I have had the privilege of teaching an online medical writing course for two health science universities. The premise is that health professionals must be able to present their work clearly and proficiently. Excellent educational material and important research data, however, are sometimes buried in poorly written papers.
The truth is, writing a good medical paper is a complex task. It requires inspired energy, quiet reflection, and yes, time in which to do it. Now that I’ve lost most of you (ha ha) ….
The first question I ask my students is what prevents them from writing. The six biggest impediments are time constraints and/or competing interests; limited experience in writing/inadequate knowledge of the process; fear of inadequacy; lack of passion; procrastination; and lack of mentorship. If this sounds familiar, and you’d like to break through these barriers, please allow me to offer some guidance derived from more than 30 years’ experience.
The first question we have to answer is: Why write, anyway? There are many reasons; six are listed in the box below.
Once you’ve decided you want to try your hand at medical writing, it is essential to develop a plan for carrying it out. It can be a long and arduous process, but without a strategy, it is nearly impossible to complete. Following are eight steps to ease the process—or at least make it palatable.
1. Find the topic that you are most passionate about, whether it is a particular case that you want to share with others or a topic you want to learn more about. The first article I wrote (circa 1979) was on Hodgkin’s disease. My father had recently died of that condition, and I wanted to better understand it. Topics, of course, should be of relevance from either a medical, practice, or academic standpoint. Be creative but realistic—topics should be focused and feasible. Above all, you should have something interesting to say.
2. Look at past issues of your professional journals to see what types of articles they accept. Some may not accept original research, while for others that is the primary focus. Also, visit the “Instructions for Authors” page (CR’s can be found at http://bit.ly/16OmNW9) and review that information. You should follow the guidelines to the letter unless otherwise instructed by the editor. In fact, it is a good idea to contact the editor and share your idea before you begin your work.
3. Start writing. A blank page is very intimidating. Get your ideas down on paper early (giving yourself permission to revise later!). Think about the main message of your article and what you hope to achieve by writing it. What is the one provocative thought you would like to leave with your audience? And who is that audience: the general public or medical professionals? Create a general outline with an introduction, discussion, and conclusion.
4. Perform a focused literature review. A literature review—basically an account of what has been published on a topic by accredited scholars and researchers—can help you narrow your focus. It also gives the reader confidence that you have understood the main theoretical positions of the subject matter and can integrate that material coherently into your own article. The literature review also provides an idea of the scope of published work in your field, enabling you to identify gaps in knowledge and avoid repetition—lending greater credibility to your work.2
5. Revise! Good papers are the product of many revisions—usually in response to feedback from others. That means you need to get over your fear of criticism and ask colleagues for advice. (I have two trusted colleagues—they know who they are!—who are critical to a fault of my drafts. But I thank them for it!) Since readability is crucial, you might even want to read your work out loud to determine whether your points are clearly made and easily understood.3 Then give yourself time to step back, digest your colleagues’ feedback, and re-read with a new perspective.
Revision also entails checking for consistency, eliminating redundancy, and deleting unnecessary information. Make sure every sentence and paragraph has a purpose. Yes, it’s time-consuming, and time is often at a premium. But if you undertake to write an article, make the time to do it correctly. Don’t rush the process.
6. Create your “accessories.” The title and abstract are the first—possibly the only—parts of your paper that an editor (and, if you’re successful, a reader) will read. Spend some quality time developing them so they accurately and adequately express the focus of your article, as well as why the subject matter is beneficial to readers. Another key element is figures and tables; visuals draw attention, so ensure you have some compelling data to present in this format. They can also be vital “take-aways” for readers to refer to in the future.
7. Submit your article to your chosen journal—and be prepared to wait! Compose a cover letter indicating why you chose this particular journal and confirming that you have not submitted the manuscript elsewhere (which is considered a conflict) and that your work is original. Then get ready to wait, because the review process takes time. First, there will likely be an in-house editorial review to determine whether the manuscript meets the publication’s needs. If it passes this first “test,” it will be sent (blinded) to two or three peer reviewers who will provide detailed feedback on the clinical validity and relevance of the topic and your presentation of it. Finally, the editor will review that feedback to determine whether the article will be accepted outright (which is rare), accepted pending revision, or rejected.
8. Deal with rejection. Nothing ventured, nothing gained. Review the feedback you receive and consider how you could rewrite the article or even approach the topic differently, hopefully with a more positive outcome. And if you mange to skip step 8—all the better! Bravo!
I hope this editorial has been a helpful introduction to the wonders of writing. There are great resources out there, including a text by Furman and Kinn4 that I encourage you to aquire.
Writing will always be hard work—but if you stick to it, it will be a rewarding and essential part of your professional life. I would love to hear your experiences in writing (both good and bad). Direct your responses to me at PAeditor@frontlinemedcom.com.
References
1. Richardson L. Writing: a method of inquiry. In: Denzin NK, Lincoln YS (eds). Handbook of Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage. 2000;923-948.
2. Parsell G, Bligh J. AMEE guide 17: writing for journal publication. Medical Teacher. 1999;21 (5):457-468.
3. Welch HG, Froehlich GW. Perspectives: strategies in writing for a physician audience. JGIM. 1996;11:50-55.
4. Furman R, Kinn JT. Practical Tips for Publishing Scholarly Articles: Writing and Publishing in the Helping Professions. 2nd ed. Chicago, IL: Lyceum Books, Inc; 2012.
For almost 10 years, I have had the privilege of teaching an online medical writing course for two health science universities. The premise is that health professionals must be able to present their work clearly and proficiently. Excellent educational material and important research data, however, are sometimes buried in poorly written papers.
The truth is, writing a good medical paper is a complex task. It requires inspired energy, quiet reflection, and yes, time in which to do it. Now that I’ve lost most of you (ha ha) ….
The first question I ask my students is what prevents them from writing. The six biggest impediments are time constraints and/or competing interests; limited experience in writing/inadequate knowledge of the process; fear of inadequacy; lack of passion; procrastination; and lack of mentorship. If this sounds familiar, and you’d like to break through these barriers, please allow me to offer some guidance derived from more than 30 years’ experience.
The first question we have to answer is: Why write, anyway? There are many reasons; six are listed in the box below.
Once you’ve decided you want to try your hand at medical writing, it is essential to develop a plan for carrying it out. It can be a long and arduous process, but without a strategy, it is nearly impossible to complete. Following are eight steps to ease the process—or at least make it palatable.
1. Find the topic that you are most passionate about, whether it is a particular case that you want to share with others or a topic you want to learn more about. The first article I wrote (circa 1979) was on Hodgkin’s disease. My father had recently died of that condition, and I wanted to better understand it. Topics, of course, should be of relevance from either a medical, practice, or academic standpoint. Be creative but realistic—topics should be focused and feasible. Above all, you should have something interesting to say.
2. Look at past issues of your professional journals to see what types of articles they accept. Some may not accept original research, while for others that is the primary focus. Also, visit the “Instructions for Authors” page (CR’s can be found at http://bit.ly/16OmNW9) and review that information. You should follow the guidelines to the letter unless otherwise instructed by the editor. In fact, it is a good idea to contact the editor and share your idea before you begin your work.
3. Start writing. A blank page is very intimidating. Get your ideas down on paper early (giving yourself permission to revise later!). Think about the main message of your article and what you hope to achieve by writing it. What is the one provocative thought you would like to leave with your audience? And who is that audience: the general public or medical professionals? Create a general outline with an introduction, discussion, and conclusion.
4. Perform a focused literature review. A literature review—basically an account of what has been published on a topic by accredited scholars and researchers—can help you narrow your focus. It also gives the reader confidence that you have understood the main theoretical positions of the subject matter and can integrate that material coherently into your own article. The literature review also provides an idea of the scope of published work in your field, enabling you to identify gaps in knowledge and avoid repetition—lending greater credibility to your work.2
5. Revise! Good papers are the product of many revisions—usually in response to feedback from others. That means you need to get over your fear of criticism and ask colleagues for advice. (I have two trusted colleagues—they know who they are!—who are critical to a fault of my drafts. But I thank them for it!) Since readability is crucial, you might even want to read your work out loud to determine whether your points are clearly made and easily understood.3 Then give yourself time to step back, digest your colleagues’ feedback, and re-read with a new perspective.
Revision also entails checking for consistency, eliminating redundancy, and deleting unnecessary information. Make sure every sentence and paragraph has a purpose. Yes, it’s time-consuming, and time is often at a premium. But if you undertake to write an article, make the time to do it correctly. Don’t rush the process.
6. Create your “accessories.” The title and abstract are the first—possibly the only—parts of your paper that an editor (and, if you’re successful, a reader) will read. Spend some quality time developing them so they accurately and adequately express the focus of your article, as well as why the subject matter is beneficial to readers. Another key element is figures and tables; visuals draw attention, so ensure you have some compelling data to present in this format. They can also be vital “take-aways” for readers to refer to in the future.
7. Submit your article to your chosen journal—and be prepared to wait! Compose a cover letter indicating why you chose this particular journal and confirming that you have not submitted the manuscript elsewhere (which is considered a conflict) and that your work is original. Then get ready to wait, because the review process takes time. First, there will likely be an in-house editorial review to determine whether the manuscript meets the publication’s needs. If it passes this first “test,” it will be sent (blinded) to two or three peer reviewers who will provide detailed feedback on the clinical validity and relevance of the topic and your presentation of it. Finally, the editor will review that feedback to determine whether the article will be accepted outright (which is rare), accepted pending revision, or rejected.
8. Deal with rejection. Nothing ventured, nothing gained. Review the feedback you receive and consider how you could rewrite the article or even approach the topic differently, hopefully with a more positive outcome. And if you mange to skip step 8—all the better! Bravo!
I hope this editorial has been a helpful introduction to the wonders of writing. There are great resources out there, including a text by Furman and Kinn4 that I encourage you to aquire.
Writing will always be hard work—but if you stick to it, it will be a rewarding and essential part of your professional life. I would love to hear your experiences in writing (both good and bad). Direct your responses to me at PAeditor@frontlinemedcom.com.
References
1. Richardson L. Writing: a method of inquiry. In: Denzin NK, Lincoln YS (eds). Handbook of Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage. 2000;923-948.
2. Parsell G, Bligh J. AMEE guide 17: writing for journal publication. Medical Teacher. 1999;21 (5):457-468.
3. Welch HG, Froehlich GW. Perspectives: strategies in writing for a physician audience. JGIM. 1996;11:50-55.
4. Furman R, Kinn JT. Practical Tips for Publishing Scholarly Articles: Writing and Publishing in the Helping Professions. 2nd ed. Chicago, IL: Lyceum Books, Inc; 2012.
For almost 10 years, I have had the privilege of teaching an online medical writing course for two health science universities. The premise is that health professionals must be able to present their work clearly and proficiently. Excellent educational material and important research data, however, are sometimes buried in poorly written papers.
The truth is, writing a good medical paper is a complex task. It requires inspired energy, quiet reflection, and yes, time in which to do it. Now that I’ve lost most of you (ha ha) ….
The first question I ask my students is what prevents them from writing. The six biggest impediments are time constraints and/or competing interests; limited experience in writing/inadequate knowledge of the process; fear of inadequacy; lack of passion; procrastination; and lack of mentorship. If this sounds familiar, and you’d like to break through these barriers, please allow me to offer some guidance derived from more than 30 years’ experience.
The first question we have to answer is: Why write, anyway? There are many reasons; six are listed in the box below.
Once you’ve decided you want to try your hand at medical writing, it is essential to develop a plan for carrying it out. It can be a long and arduous process, but without a strategy, it is nearly impossible to complete. Following are eight steps to ease the process—or at least make it palatable.
1. Find the topic that you are most passionate about, whether it is a particular case that you want to share with others or a topic you want to learn more about. The first article I wrote (circa 1979) was on Hodgkin’s disease. My father had recently died of that condition, and I wanted to better understand it. Topics, of course, should be of relevance from either a medical, practice, or academic standpoint. Be creative but realistic—topics should be focused and feasible. Above all, you should have something interesting to say.
2. Look at past issues of your professional journals to see what types of articles they accept. Some may not accept original research, while for others that is the primary focus. Also, visit the “Instructions for Authors” page (CR’s can be found at http://bit.ly/16OmNW9) and review that information. You should follow the guidelines to the letter unless otherwise instructed by the editor. In fact, it is a good idea to contact the editor and share your idea before you begin your work.
3. Start writing. A blank page is very intimidating. Get your ideas down on paper early (giving yourself permission to revise later!). Think about the main message of your article and what you hope to achieve by writing it. What is the one provocative thought you would like to leave with your audience? And who is that audience: the general public or medical professionals? Create a general outline with an introduction, discussion, and conclusion.
4. Perform a focused literature review. A literature review—basically an account of what has been published on a topic by accredited scholars and researchers—can help you narrow your focus. It also gives the reader confidence that you have understood the main theoretical positions of the subject matter and can integrate that material coherently into your own article. The literature review also provides an idea of the scope of published work in your field, enabling you to identify gaps in knowledge and avoid repetition—lending greater credibility to your work.2
5. Revise! Good papers are the product of many revisions—usually in response to feedback from others. That means you need to get over your fear of criticism and ask colleagues for advice. (I have two trusted colleagues—they know who they are!—who are critical to a fault of my drafts. But I thank them for it!) Since readability is crucial, you might even want to read your work out loud to determine whether your points are clearly made and easily understood.3 Then give yourself time to step back, digest your colleagues’ feedback, and re-read with a new perspective.
Revision also entails checking for consistency, eliminating redundancy, and deleting unnecessary information. Make sure every sentence and paragraph has a purpose. Yes, it’s time-consuming, and time is often at a premium. But if you undertake to write an article, make the time to do it correctly. Don’t rush the process.
6. Create your “accessories.” The title and abstract are the first—possibly the only—parts of your paper that an editor (and, if you’re successful, a reader) will read. Spend some quality time developing them so they accurately and adequately express the focus of your article, as well as why the subject matter is beneficial to readers. Another key element is figures and tables; visuals draw attention, so ensure you have some compelling data to present in this format. They can also be vital “take-aways” for readers to refer to in the future.
7. Submit your article to your chosen journal—and be prepared to wait! Compose a cover letter indicating why you chose this particular journal and confirming that you have not submitted the manuscript elsewhere (which is considered a conflict) and that your work is original. Then get ready to wait, because the review process takes time. First, there will likely be an in-house editorial review to determine whether the manuscript meets the publication’s needs. If it passes this first “test,” it will be sent (blinded) to two or three peer reviewers who will provide detailed feedback on the clinical validity and relevance of the topic and your presentation of it. Finally, the editor will review that feedback to determine whether the article will be accepted outright (which is rare), accepted pending revision, or rejected.
8. Deal with rejection. Nothing ventured, nothing gained. Review the feedback you receive and consider how you could rewrite the article or even approach the topic differently, hopefully with a more positive outcome. And if you mange to skip step 8—all the better! Bravo!
I hope this editorial has been a helpful introduction to the wonders of writing. There are great resources out there, including a text by Furman and Kinn4 that I encourage you to aquire.
Writing will always be hard work—but if you stick to it, it will be a rewarding and essential part of your professional life. I would love to hear your experiences in writing (both good and bad). Direct your responses to me at PAeditor@frontlinemedcom.com.
References
1. Richardson L. Writing: a method of inquiry. In: Denzin NK, Lincoln YS (eds). Handbook of Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage. 2000;923-948.
2. Parsell G, Bligh J. AMEE guide 17: writing for journal publication. Medical Teacher. 1999;21 (5):457-468.
3. Welch HG, Froehlich GW. Perspectives: strategies in writing for a physician audience. JGIM. 1996;11:50-55.
4. Furman R, Kinn JT. Practical Tips for Publishing Scholarly Articles: Writing and Publishing in the Helping Professions. 2nd ed. Chicago, IL: Lyceum Books, Inc; 2012.
Humor: The Best Rx You Can Write
I recently attended a fundraiser for a free clinic, at which a comedian was the main entertainment. I remember smirking a bit, anticipating a quick five- or 10-minute stand-up program with a few chuckles after dinner. I was amazed, however, when the comedian, Greg Schwem, spoke for almost an hour and had the 250 people in attendance in stitches. His premise is that every group needs to laugh at itself. The presentation was clean and motivational, and it was obvious he had done his homework for this particular medical group.
I have read all the articles, as you have, and know that laughter makes you feel good. Scientists believe it is the physical act of laughing (releasing endorphins and boosting T cells), rather than an intellectual pleasure, that makes laughing feel so right.1,2 The good feeling remains with you even after the laughter wanes. This was certainly true at this event.
One essential characteristic that helps us laugh, as Mr. Schwem suggested, is not taking ourselves too seriously. We all know the classic tight-jawed whiner who regards life with tomblike seriousness and never laughs at anything. You know whom I’m talking about?
This brings to mind the experiences of Ralph, a PA colleague who was excited to finally graduate and start work in a local family practice clinic. The more he worked, the less he enjoyed himself. Although his medical acumen noticeably improved in the subsequent six months, he got angry with himself when he didn’t know something or when he made any little mistake. The clinic atmosphere was filled with stress and negativity, which carried over to the patients. No one was having fun.
Ralph wisely realized that his coworkers were negatively affecting his attitude, so he decided it was time to move on. At his next job, he fortunately worked with colleagues who focused on positive issues and enjoying the moment; as a result, he was less critical of himself.
Work became as enjoyable as he’d hoped it would be. He enjoyed waking up in the morning and seeing patients. The day was filled with smiles and even (appropriate) laughter with staff and patients. He was amazed at how much better his professional relationships became, and this brighter outlook spread to other parts of his life.
Clearly, some events in life are sad and not circumstances for laughter. But most events in life don’t carry an overpowering sense of either sadness or delight. They fall into the gray zone of everyday life—giving you the choice to laugh or not.
That idea was borne out in a great book I read decades ago: Anatomy of an Illness: As Perceived by the Patient, by Norman Cousins.3 (Years later, this story became a movie with Mr. Cousins played by Ed Asner.) Cousins’ book was the first by a patient that spoke to taking charge of our own health. It started the transformation in patients working with their clinicians and using humor to boost their bodies’ capacity for healing.
When the author was diagnosed with ankylosing spondylitis, he forged an unusual alliance with his physician, and together they were able to beat the odds. Told that he had little chance of surviving, Cousins checked himself out of the hospital and into a hotel, where he developed a personal recuperation program incorporating mega-doses of vitamin C alongside a positive attitude, love, hope, and laughter induced by watching multiple Marx Brothers films. He made the jubilant discovery that 10 minutes of genuine belly laughing had a sedative effect and would give him at least two hours of pain-free sleep. He reported that when the painkilling effect of the laughter wore off, he would switch on the projector again—and not infrequently, it would lead to another pain-free interval.
His doctor’s talent was in helping Mr. Cousins use his personal powers of laughter, courage, and persistence. Cousins’ genius was in mobilizing his body’s natural resources, proving what an effective healing tool the mind can be. This remarkable story is truly motivating. Cousins died of heart failure in 1990, having survived years longer than predicted: 10 years after his first heart attack, 26 years after his collagen illness, and 36 years after his doctors first diagnosed his heart disease.
Incorporating more humor and play into our daily relationships can improve the quality of our patient care, as well as our connections with colleagues, family members, and friends. Humor gets us out of our heads and away from our troubles. It allows us to let go of defensiveness and to forget judgments, criticisms, and doubts. It even releases inhibitions and frees us to express our true feelings.
Robert Provine, professor of neuroscience at the University of Maryland and author of Laughter: A Scientific Investigation, was the first researcher to conduct a complete investigation of laughter, taking what is seemingly a frivolous topic into the realm of serious science. Over a span of 10 years, Provine and colleagues hit the streets to document more than 2,000 cases of “naturally occurring laughter.” They compiled some intriguing data, such as: Laughter is an instinctive behavior produced and recognized by people of all cultures, and most laughter is not about humor—it is about relationships between people. According to Provine, we are 30 times more likely to laugh in a social situation than when we are alone.4
How do we invite more laughter and positive emotions into our professional lives? Here are a few ideas5:
• Be OK with laughing at yourself. Share appropriate embarrassing moments. This shows you don’t take yourself too seriously.
• Try to laugh at situations rather than lament them. Look for humor in bad or stressful situations. This will help improve the mood.
• Surround yourself with reminders to lighten up—perhaps humorous sayings on your desk or even screensavers on your computer that make you laugh.
• Keep things in perspective. We all know that many things are beyond our control—particularly the behavior of other people!
• Pay attention to children and emulate them; they are indeed the experts on playing.
• Be more spontaneous. This gets you out of your head at just the right time.
• When you hear laughter—move toward it!
• Hang around people who like to smile and laugh.
Hopefully, you have more suggestions and/or experiences to share. Feel free to contact me about them at PAeditor@frontlinemedcom.com.
References
1. Dunbar RIM, Baron R, Frangou A, et al. Social laughter is correlated with an elevated pain threshold. Proc R Soc B. 2012;279(1731):1161-1167.
2. Berk LS, Felten DL, Tan SA, et al. Modulation of neuroimmune parameters during the eustress of humor-associated mirthful laughter. Altern Ther Health Med. 2001;7(2):62-72, 74-76.
3. Cousins N. Anatomy of an Illness: As Perceived by the Patient (Twentieth Anniversary Edition). W W Norton & Company; 2005.
4. Provine RR. Laughter: A Scientific Investigation. Penguin Books; 2001.
5. Laughter Is the Best Medicine: The Health Benefits of Humor and Laughter. www.helpguide.org/life/humor_laughter_health.htm. Accessed August 30, 2013.
I recently attended a fundraiser for a free clinic, at which a comedian was the main entertainment. I remember smirking a bit, anticipating a quick five- or 10-minute stand-up program with a few chuckles after dinner. I was amazed, however, when the comedian, Greg Schwem, spoke for almost an hour and had the 250 people in attendance in stitches. His premise is that every group needs to laugh at itself. The presentation was clean and motivational, and it was obvious he had done his homework for this particular medical group.
I have read all the articles, as you have, and know that laughter makes you feel good. Scientists believe it is the physical act of laughing (releasing endorphins and boosting T cells), rather than an intellectual pleasure, that makes laughing feel so right.1,2 The good feeling remains with you even after the laughter wanes. This was certainly true at this event.
One essential characteristic that helps us laugh, as Mr. Schwem suggested, is not taking ourselves too seriously. We all know the classic tight-jawed whiner who regards life with tomblike seriousness and never laughs at anything. You know whom I’m talking about?
This brings to mind the experiences of Ralph, a PA colleague who was excited to finally graduate and start work in a local family practice clinic. The more he worked, the less he enjoyed himself. Although his medical acumen noticeably improved in the subsequent six months, he got angry with himself when he didn’t know something or when he made any little mistake. The clinic atmosphere was filled with stress and negativity, which carried over to the patients. No one was having fun.
Ralph wisely realized that his coworkers were negatively affecting his attitude, so he decided it was time to move on. At his next job, he fortunately worked with colleagues who focused on positive issues and enjoying the moment; as a result, he was less critical of himself.
Work became as enjoyable as he’d hoped it would be. He enjoyed waking up in the morning and seeing patients. The day was filled with smiles and even (appropriate) laughter with staff and patients. He was amazed at how much better his professional relationships became, and this brighter outlook spread to other parts of his life.
Clearly, some events in life are sad and not circumstances for laughter. But most events in life don’t carry an overpowering sense of either sadness or delight. They fall into the gray zone of everyday life—giving you the choice to laugh or not.
That idea was borne out in a great book I read decades ago: Anatomy of an Illness: As Perceived by the Patient, by Norman Cousins.3 (Years later, this story became a movie with Mr. Cousins played by Ed Asner.) Cousins’ book was the first by a patient that spoke to taking charge of our own health. It started the transformation in patients working with their clinicians and using humor to boost their bodies’ capacity for healing.
When the author was diagnosed with ankylosing spondylitis, he forged an unusual alliance with his physician, and together they were able to beat the odds. Told that he had little chance of surviving, Cousins checked himself out of the hospital and into a hotel, where he developed a personal recuperation program incorporating mega-doses of vitamin C alongside a positive attitude, love, hope, and laughter induced by watching multiple Marx Brothers films. He made the jubilant discovery that 10 minutes of genuine belly laughing had a sedative effect and would give him at least two hours of pain-free sleep. He reported that when the painkilling effect of the laughter wore off, he would switch on the projector again—and not infrequently, it would lead to another pain-free interval.
His doctor’s talent was in helping Mr. Cousins use his personal powers of laughter, courage, and persistence. Cousins’ genius was in mobilizing his body’s natural resources, proving what an effective healing tool the mind can be. This remarkable story is truly motivating. Cousins died of heart failure in 1990, having survived years longer than predicted: 10 years after his first heart attack, 26 years after his collagen illness, and 36 years after his doctors first diagnosed his heart disease.
Incorporating more humor and play into our daily relationships can improve the quality of our patient care, as well as our connections with colleagues, family members, and friends. Humor gets us out of our heads and away from our troubles. It allows us to let go of defensiveness and to forget judgments, criticisms, and doubts. It even releases inhibitions and frees us to express our true feelings.
Robert Provine, professor of neuroscience at the University of Maryland and author of Laughter: A Scientific Investigation, was the first researcher to conduct a complete investigation of laughter, taking what is seemingly a frivolous topic into the realm of serious science. Over a span of 10 years, Provine and colleagues hit the streets to document more than 2,000 cases of “naturally occurring laughter.” They compiled some intriguing data, such as: Laughter is an instinctive behavior produced and recognized by people of all cultures, and most laughter is not about humor—it is about relationships between people. According to Provine, we are 30 times more likely to laugh in a social situation than when we are alone.4
How do we invite more laughter and positive emotions into our professional lives? Here are a few ideas5:
• Be OK with laughing at yourself. Share appropriate embarrassing moments. This shows you don’t take yourself too seriously.
• Try to laugh at situations rather than lament them. Look for humor in bad or stressful situations. This will help improve the mood.
• Surround yourself with reminders to lighten up—perhaps humorous sayings on your desk or even screensavers on your computer that make you laugh.
• Keep things in perspective. We all know that many things are beyond our control—particularly the behavior of other people!
• Pay attention to children and emulate them; they are indeed the experts on playing.
• Be more spontaneous. This gets you out of your head at just the right time.
• When you hear laughter—move toward it!
• Hang around people who like to smile and laugh.
Hopefully, you have more suggestions and/or experiences to share. Feel free to contact me about them at PAeditor@frontlinemedcom.com.
References
1. Dunbar RIM, Baron R, Frangou A, et al. Social laughter is correlated with an elevated pain threshold. Proc R Soc B. 2012;279(1731):1161-1167.
2. Berk LS, Felten DL, Tan SA, et al. Modulation of neuroimmune parameters during the eustress of humor-associated mirthful laughter. Altern Ther Health Med. 2001;7(2):62-72, 74-76.
3. Cousins N. Anatomy of an Illness: As Perceived by the Patient (Twentieth Anniversary Edition). W W Norton & Company; 2005.
4. Provine RR. Laughter: A Scientific Investigation. Penguin Books; 2001.
5. Laughter Is the Best Medicine: The Health Benefits of Humor and Laughter. www.helpguide.org/life/humor_laughter_health.htm. Accessed August 30, 2013.
I recently attended a fundraiser for a free clinic, at which a comedian was the main entertainment. I remember smirking a bit, anticipating a quick five- or 10-minute stand-up program with a few chuckles after dinner. I was amazed, however, when the comedian, Greg Schwem, spoke for almost an hour and had the 250 people in attendance in stitches. His premise is that every group needs to laugh at itself. The presentation was clean and motivational, and it was obvious he had done his homework for this particular medical group.
I have read all the articles, as you have, and know that laughter makes you feel good. Scientists believe it is the physical act of laughing (releasing endorphins and boosting T cells), rather than an intellectual pleasure, that makes laughing feel so right.1,2 The good feeling remains with you even after the laughter wanes. This was certainly true at this event.
One essential characteristic that helps us laugh, as Mr. Schwem suggested, is not taking ourselves too seriously. We all know the classic tight-jawed whiner who regards life with tomblike seriousness and never laughs at anything. You know whom I’m talking about?
This brings to mind the experiences of Ralph, a PA colleague who was excited to finally graduate and start work in a local family practice clinic. The more he worked, the less he enjoyed himself. Although his medical acumen noticeably improved in the subsequent six months, he got angry with himself when he didn’t know something or when he made any little mistake. The clinic atmosphere was filled with stress and negativity, which carried over to the patients. No one was having fun.
Ralph wisely realized that his coworkers were negatively affecting his attitude, so he decided it was time to move on. At his next job, he fortunately worked with colleagues who focused on positive issues and enjoying the moment; as a result, he was less critical of himself.
Work became as enjoyable as he’d hoped it would be. He enjoyed waking up in the morning and seeing patients. The day was filled with smiles and even (appropriate) laughter with staff and patients. He was amazed at how much better his professional relationships became, and this brighter outlook spread to other parts of his life.
Clearly, some events in life are sad and not circumstances for laughter. But most events in life don’t carry an overpowering sense of either sadness or delight. They fall into the gray zone of everyday life—giving you the choice to laugh or not.
That idea was borne out in a great book I read decades ago: Anatomy of an Illness: As Perceived by the Patient, by Norman Cousins.3 (Years later, this story became a movie with Mr. Cousins played by Ed Asner.) Cousins’ book was the first by a patient that spoke to taking charge of our own health. It started the transformation in patients working with their clinicians and using humor to boost their bodies’ capacity for healing.
When the author was diagnosed with ankylosing spondylitis, he forged an unusual alliance with his physician, and together they were able to beat the odds. Told that he had little chance of surviving, Cousins checked himself out of the hospital and into a hotel, where he developed a personal recuperation program incorporating mega-doses of vitamin C alongside a positive attitude, love, hope, and laughter induced by watching multiple Marx Brothers films. He made the jubilant discovery that 10 minutes of genuine belly laughing had a sedative effect and would give him at least two hours of pain-free sleep. He reported that when the painkilling effect of the laughter wore off, he would switch on the projector again—and not infrequently, it would lead to another pain-free interval.
His doctor’s talent was in helping Mr. Cousins use his personal powers of laughter, courage, and persistence. Cousins’ genius was in mobilizing his body’s natural resources, proving what an effective healing tool the mind can be. This remarkable story is truly motivating. Cousins died of heart failure in 1990, having survived years longer than predicted: 10 years after his first heart attack, 26 years after his collagen illness, and 36 years after his doctors first diagnosed his heart disease.
Incorporating more humor and play into our daily relationships can improve the quality of our patient care, as well as our connections with colleagues, family members, and friends. Humor gets us out of our heads and away from our troubles. It allows us to let go of defensiveness and to forget judgments, criticisms, and doubts. It even releases inhibitions and frees us to express our true feelings.
Robert Provine, professor of neuroscience at the University of Maryland and author of Laughter: A Scientific Investigation, was the first researcher to conduct a complete investigation of laughter, taking what is seemingly a frivolous topic into the realm of serious science. Over a span of 10 years, Provine and colleagues hit the streets to document more than 2,000 cases of “naturally occurring laughter.” They compiled some intriguing data, such as: Laughter is an instinctive behavior produced and recognized by people of all cultures, and most laughter is not about humor—it is about relationships between people. According to Provine, we are 30 times more likely to laugh in a social situation than when we are alone.4
How do we invite more laughter and positive emotions into our professional lives? Here are a few ideas5:
• Be OK with laughing at yourself. Share appropriate embarrassing moments. This shows you don’t take yourself too seriously.
• Try to laugh at situations rather than lament them. Look for humor in bad or stressful situations. This will help improve the mood.
• Surround yourself with reminders to lighten up—perhaps humorous sayings on your desk or even screensavers on your computer that make you laugh.
• Keep things in perspective. We all know that many things are beyond our control—particularly the behavior of other people!
• Pay attention to children and emulate them; they are indeed the experts on playing.
• Be more spontaneous. This gets you out of your head at just the right time.
• When you hear laughter—move toward it!
• Hang around people who like to smile and laugh.
Hopefully, you have more suggestions and/or experiences to share. Feel free to contact me about them at PAeditor@frontlinemedcom.com.
References
1. Dunbar RIM, Baron R, Frangou A, et al. Social laughter is correlated with an elevated pain threshold. Proc R Soc B. 2012;279(1731):1161-1167.
2. Berk LS, Felten DL, Tan SA, et al. Modulation of neuroimmune parameters during the eustress of humor-associated mirthful laughter. Altern Ther Health Med. 2001;7(2):62-72, 74-76.
3. Cousins N. Anatomy of an Illness: As Perceived by the Patient (Twentieth Anniversary Edition). W W Norton & Company; 2005.
4. Provine RR. Laughter: A Scientific Investigation. Penguin Books; 2001.
5. Laughter Is the Best Medicine: The Health Benefits of Humor and Laughter. www.helpguide.org/life/humor_laughter_health.htm. Accessed August 30, 2013.