User login
Sleepiness in Critical Care Nurses
Current practice patterns among nurses show they are working longer than they ever have.14 The effect of these long hours is that many nurses work in the midst of severe lethargy and sleep deprivation.5 Sleep deprivation jeopardizes not only patient safety but also the safety and general health of the nurses themselves.46 Numerous studies of shift workers in other professions have been done to assess sleepiness using subjective and objective data and also the effect of shift work on work and health.710 Despite the Accreditation Council for Graduate Medical Education (ACGME) mandating work‐hour limitations for medical residents, recent data suggest that sleepiness continues to be a significant issue for medical residents.11 There is a paucity of objective information about the sleepiness and performance of nurses, especially now that most nurses in the United States are working 12‐hour shifts. We hypothesized that nurses working a 12‐hour night shift would have a significant degree of sleepiness. Our objective was to assess the daytime sleepiness of post‐night‐shift nurses using both subjective measures (Epworth Sleepiness Scale [ESS]) and objective testing (Multiple Sleep Latency Test [MSLT]).
MATERIALS AND METHODS
The study was initiated after we obtained institutional review board approval.
Setting
The setting of the study was a community hospital in Corpus Christi, Texas.
Design
The study was a prospective pilot study.
Subjects
Twenty adult nurses (age > 18 years) assigned to duty on general floors (both medical and surgical) and the intensive care unit (ICU) who consented to participate in the study were included. Exclusion criteria included recent or ongoing use of sedative, hypnotic, stimulant drugs; illnesses such as cardiac disease; narcolepsy and other primary sleep disorders; being pregnant or lactating, and being obese (body mass index [BMI] > 30).
Protocol
Floor nurses (n = 10) constituted the control group, and ICU nurses (n = 10) formed the study group. Both groups of nurses came on duty at 7 PM and completed their duty at 7 AM. The MSLT test was performed in the morning following either the third or fourth night shift. All nurses maintained a detailed sleep diary for the week prior to the day of the test that included a detailed record of their bedtimes, wake times, and daytime naps and also included comments about nocturnal awakenings and subjective sleepiness. All nurses were asked to fill out the ESS prior to undergoing the MSLT. ESS is a well‐standardized and validated measure of subjective sleepiness.12 The score was established based on the questionnaire about their chances of falling asleep in 6 different scenarios. A score greater than 8 was considered abnormal. A modified protocol for MSLT was used, which consisted of only 2 nap opportunities. This was done to enable these nurses to go home at a reasonable time in order to catch up on their sleep after having spent the previous night at work. The MSLT procedure was explained to nurses before the start of study, and the MSLT was done at 7:15 AM and 8:30 AM. Standard guidelines for the test were followed.13 Nurses were given $25 gift certificates on completion of the study.
Statistical Analysis
Standard software was used for computation of all data. The t test was used for comparison of means, and Fisher's exact analysis was used to compare proportions. All P values are 2 sided. The term significant indicates a P value < .05. Computations were performed using Microsoft Excel software.
RESULTS
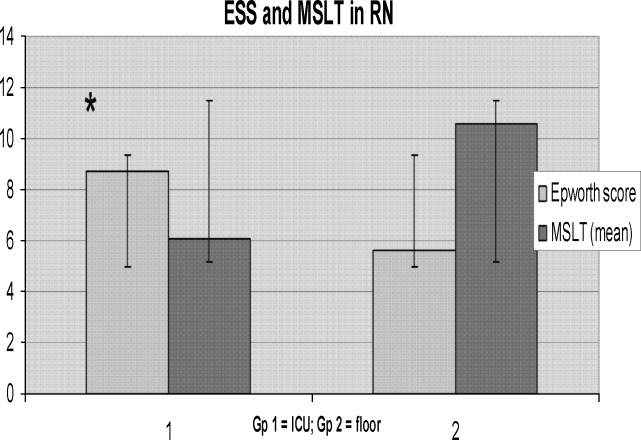
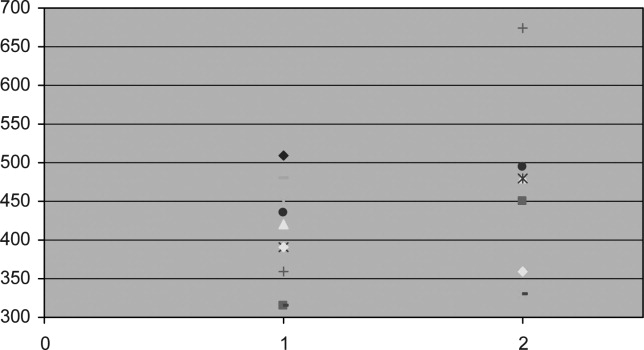
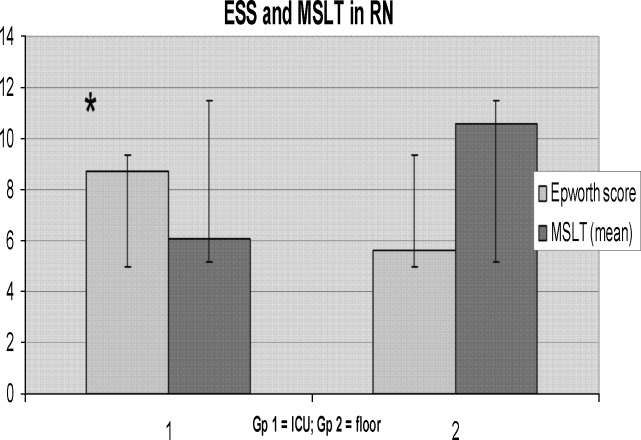
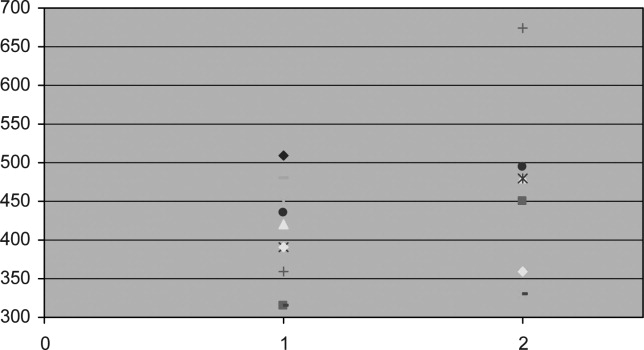
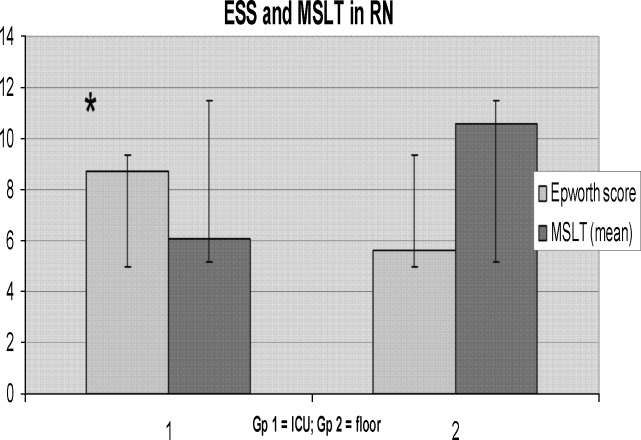
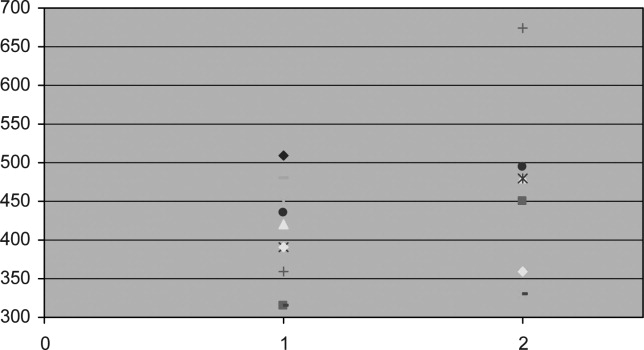
Baseline data are shown in Table 1. Nurses in the 2 groups were matched for age, sex, and marital and offspring status. There was a small but statistically significant difference between the 2 groups in BMI (see Table 1). There was no difference between the 2 groups in the average time slept (per night) in the week preceding the test. Seven of 10 ICU nurses had an abnormal ESS (>8) compared with 2 of 10 floor nurses. Mean ESS of ICU nurses was also higher (5.6 2.1 vs. 8.7 3.9 minutes, respectively, P = .042). Nine of 10 ICU nurses had sleep latency values in the severe pathologic range (<5 minutes) for the first sleep period, compared with only 2 of 10 in the floor group. Mean sleep latency in the nap 1 period differed significantly between the 2 groups (Table 2). Overall, however, mean MSLT value did not differ between the ICU nurses and the control group (6.1 3.8 vs. 10.6 7.5 minutes; Table 2 and Fig. 1). Also, during MSLT, the nurses were unaware of their sleep onset in 10 of the 32 periods (31.3%).
| Variable | ICU nurses (n = 10) | Floor nurses (n = 10) | P value |
|---|---|---|---|
| |||
| Age (years) | 37.1 7.53 | 34.6 7.19 | .45 |
| Sex (M:F) | 4:6 | 1:9 | .118 |
| BMI* | 24.9 3.5 | 21.6 1.9 | .02 |
| Married | 5 | 6 | .315 |
| With Children | 6 | 5 | .315 |
| Variable | ICU nurses (n = 10) | Floor nurses (n = 10) | P value |
|---|---|---|---|
| |||
| Sleep time (minutes) | 405.2 36.6 | 416.1 84.73 | .72 |
| ESS score* | 8.7 3.9 | 5.6 2.1 | .042 |
| Abnormal ESS (>8)* | 7 | 2 | .032 |
| MSLT (min) | 6.1 3.8 | 1.6 7.5 | .19 |
| First‐period sleep latency < 5 minutes* | 9 | 2 | <.005 |
| First nap MSLT | 4.65 5.56 | 1.85 7.44 | .025 |
DISCUSSION
Our study shows that nurses working night shifts have a pathologic degree of sleepiness. This was especially severe in the ICU nurses as determined by both the ESS and the MSLT studies.
To our knowledge, ours is the first study that has comprehensively evaluated the issue of sleepiness in nurses working night shifts using both the ESS and the MSLT. Previous studies have evaluated subjective sleepiness in nurses. In a cross‐sectional study in 8 large hospitals in Japan, Suzuki et al. found that an estimated 26% of the 4407 nurses surveyed reported excess sleepiness.14 They found key associations of daytime sleepiness with motor vehicle accidents, medication errors, and incorrect operation of medical equipment. Scott et al. randomly surveyed 502 critical care nurses across the US and found that almost two thirds reported struggling to stay awake at least once during the study period and that 22% fell asleep at least once during their work shift.2 Sleep deprivation resulting in impairment in cognitive and psychomotor performance and its association with medical errors have now been well documented in medical residents.1517 This has resulted in the Accreditation Council for Graduate Medical Education mandating a reduction in resident work hours.18 No state or federal regulations restrict the number of hours a nurse may voluntarily work in a 24‐hour or a 7‐day period. Bills prohibiting mandatory overtime for nurses have passed only in California, Maine, New Jersey, and Oregon. No measure, either proposed or enacted, addresses how long nurses may work voluntarily. The recent Institute of Medicine (IOM) report, Keeping Patients Safe, explicitly recommends that nurses' shifts be limited to 12 hours in a 24‐hour period, 60 hours per week, and that voluntary overtime be limited.19
Even with the current ACGME‐mandated reduction in work hours, we and others have reported that sleepiness in medical residents continues to be a major issue.11, 20 In the first year following implementation of the ACGME duty‐hour standards, as many as 43% of interns reported noncompliance with these requirements.21 This demonstrates that mandating work‐hour reductions is only the first step in what is likely to be a long process of effecting change in nurse work hours and fatigue and, in turn, improving patient safety. However, initiating this process is going to be crucial, given the impact even small changes in nursing fatigue could have on patient‐care outcomes.
A nationwide nursing shortage has placed enormous stress on the delivery of patient care in our hospitals. Demands of nursing care requirements have also increased in today's health care scenario because of a variety of socioeconomic factors, and this in turn has forced hospitals to encourage and in many instances insist on nurses working overtime and longer shifts. Rogers et al. examined logbooks completed by 393 hospital staff nurses and found that 40% of the 5317 work shifts they logged exceeded 12 hours. The risk of making an error was significantly increased when the work shift was longer than 12 hours, when overtime was worked, and when the workweek was more than 40 hours.5 There are good data comparing 8‐ and 12‐hour shift lengths among other occupational groups that demonstrate, particularly for the night shift, greater sleepiness during a 12‐hour night shift than during an 8‐hour night shift.22 Emergency room physicians overwhelmingly prefer shifts to last 8 and 10 hours than 12 hours, and longer shifts have been shown to impair their triage decisions in simulation studies.23 The problem is compounded for female nurses, as they also have to carry out their responsibilities as partner and parent along with working, resulting in chronic fatigue and sleep deprivation.24 From these results together with the results of the present study, we suggest enforcing a shift length of no longer than 10 hours for nurses working the night shift in a critical care environment.
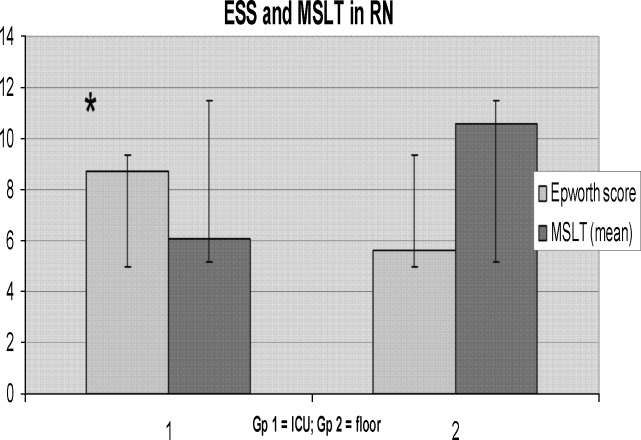
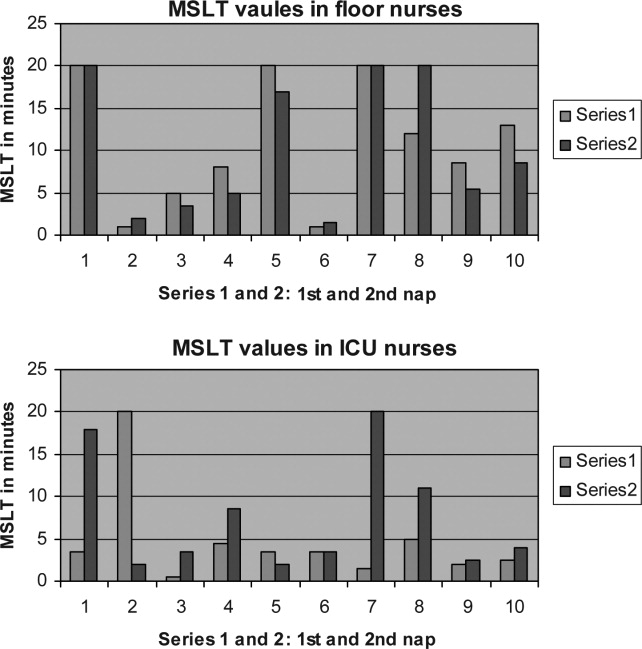
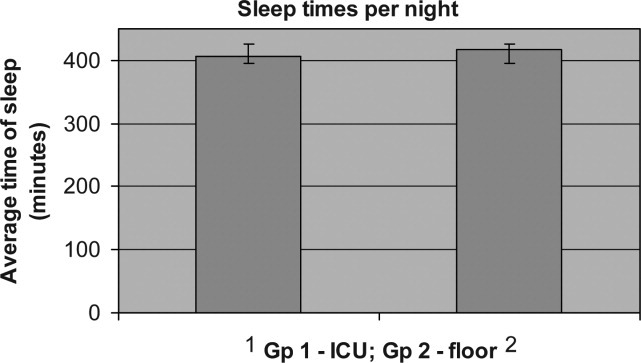
In our study, ICU nurses were found to be more sleepy than floor nurses. Sleep quantity in the week prior to the study day did not differ between the 2 groups (405.2 36.6 vs. 416.1 84.73 minutes; P = .364; Fig. 2). For the 24 hours prior to the night shift that was studied, the average amount of sleep was not different between the 2 groups (406 65 minutes for the ICU group vs. 432 107 minutes for the control group; P = .265; Fig. 4). Sleep quality could certainly be markedly different between the 2 groups. A recent study has reported that nearly a third of ICU nurses had severe burnout syndrome, and this has been associated with profound sleep disturbances.25, 26 This could also be attributed to the floor nurses having a less demanding schedule than the ICU nurses.
Our study had some limitations. Our sample size was small, and larger studies may be needed to validate the results of this pilot study. Although our 2 groups were matched for age and sex, the BMI of ICU nurses was slightly but statistically significantly higher than that of floor nurses. Although the mean BMI of ICU nurses was still not in the obese range (one of the exclusion criteria was a BMI > 30), we still cannot definitively rule out that the higher BMI may have conferred a risk of increased upper airway resistance and sleep‐disordered breathing. The control group consisted of RNs in different settingsmedical and surgicaland because of the small numbers of nurses studied, we are unable to further dissect this group and identify differences in degrees of sleepiness. For example, sleep deprivation effects have been shown to be less pronounced in nurses regularly and permanently working night shifts than in nurses working to rotating shifts,27 perhaps a consequence of circadian misalignment being more severe in the latter group, and this factor was not controlled for. We also measured sleepiness after the shift was completed and not during the shift. Not only is this likely reflective of the nurses' sleepiness toward the latter portion of their shift, it also has direct implications for the driving safety of nurses at the end of a shift.
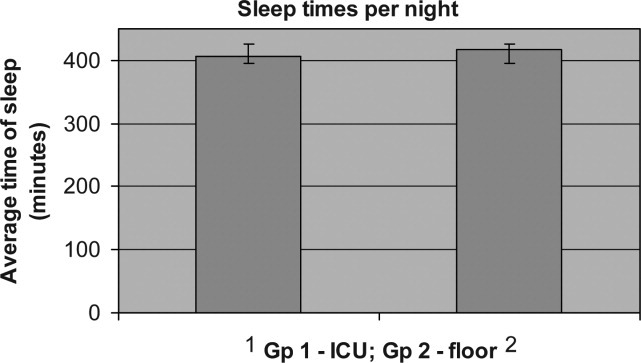
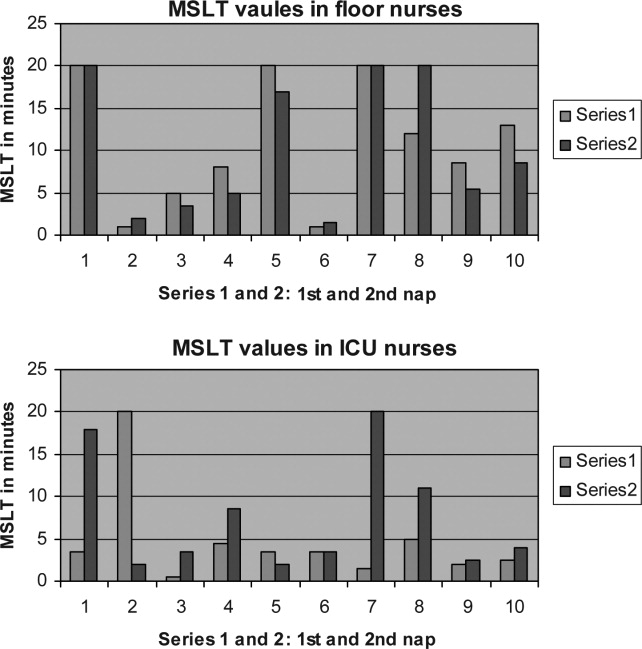
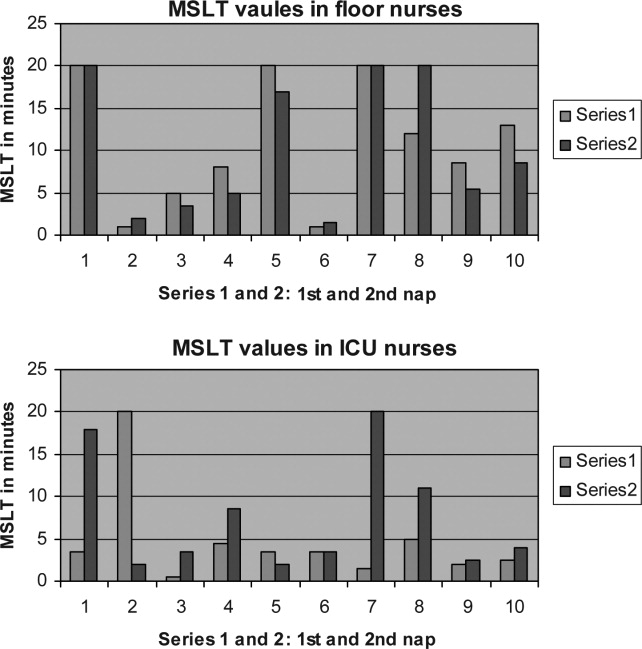
Our MSLT data showed significant differences only for nap 1 but not when combined for the 2 nap periods. We speculate that the reason for this could be that some alertness was recovered by the first nap, as 9 of 10 in the ICU group had at least 15 minutes of sleep during the first nap opportunity compared with only 2 of 10 nurses in the floor group. Incidentally, the only nurse in the ICU group who had no sleep during the first nap period had a sleep latency of 2 minutes during the second nap period (see Fig. 3).
We also did not correlate sleepiness in our study with any clinical performance, and this will be an important variable to focus on in future studies.
In conclusion, our data indicate that nurses working in the ICU are significantly more sleepy than nurses on the floor. Level of sleepiness of ICU nurses is frequently in the pathologic range, comparable to narcolepsy.
- ,.Trends in nurse overtime, 1995–2002.Policy Polit Nurs Pract.2005;6:183–190.
- ,,,.Effects of critical care nurses' work hours on vigilance and patients' safety.Am J Crit Care.2006;15:30–37.
- ,,,,.How long and how much are nurses now working?Am J Nurs.2006;106:60–71.
- ,.Are you tired? Sleep deprivation compromises nurse's health and jeopardizes patients.Am J Nurs.2004;104:36–38.
- ,,,,.The working hours of hospital staff nurses and patient safety.Health Aff (Millwood).2004;23:202–212.
- ,.Twelve‐hour night shifts of healthcare workers: a risk to the patients?Chronobiol Int.2003;20:351–360.
- ,,,,.The sleep of long‐haul truck drivers.N Engl J Med.1997;337:755–761.
- ,,, et al.Subjective and objective measures of adaptation and readaptation to night work on an oil rig in the North Sea.Sleep.2006;29:821–829.
- ,,,,.Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers.Sleep.2004;27:1453–1462.
- ,.Impact of shift work on the health and safety of nurses and patients.Clin J Oncol Nurs.2006;0:465–471.
- ,,,,.Sleepiness in medical residents: Impact of mandated reduction in work hours.Sleep Med.2007;8:90–93.
- .A new method for measuring daytime sleepiness: the Epworth sleepiness scale.Sleep.1991;14:540–545.
- ,,,,,, et al.Standards of practice committee of the American Academy of Sleep Medicine. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test.Sleep.2005;28:113–121.
- ,,,,.Daytime sleepiness, sleep habits and occupational accidents among hospital nurses.J Adv Nurs.2005;52:445–453.
- ,,,,.Neurobehavioral performance of residents after heavy night call vs after alcohol ingestion.JAMA.2005;294:1025–1033.
- .Simulation study of rested versus sleep‐deprived anesthesiologists.Anesthesiology.2003;98:1345–1355.
- ,,,.The risks and implication of excessive daytime sleepiness in resident physicians.Acad Med.2002;77:1019–1025.
- Accreditation Council for Graduate Medical Education. Common program requirements. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_dutyHoursCommonPR.pdf.
- Institute of Medicine.Keeping Patients Safe: Transforming the Work Environment of Nurses.Washington, DC:National Academies Press;2003.
- ,,, et al.Sleep and well‐being of ICU housestaff.Chest.2007;131:1685–1693.
- ,,,,.Interns' compliance with accreditation council for graduate medical education work‐hour limits.JAMA.2006;296:1063–1070.
- ,,, et al.Effects of alternating 8‐ and 12‐hour shifts on sleep, sleepiness, physical effort and performance.Scand J Work Environ Health.1998;24:62–68.
- ,,, et al.Emergency medicine residents' shiftwork tolerance and preference.Acad Emerg Med.2000;7:670–673.
- ,,,.A study of female nurses combining partner and parent roles with working a continuous three‐shift roster: the impact on sleep, fatigue and stress.Contemp Nurse.2002;12:294–302.
- ,,, et al.Burnout syndrome in critical care nursing staff.Am J Respir Crit Care Med2007;175:698–704.
- ,,, et al.Disturbed sleep and fatigue in occupational burnout.Scand J Work Environ Health.2006;32:121.
- .A computer‐aided comparative study of progressive alertness changes in nurses working two different night‐shift rotations.J Adv Nurs.1996;23:1247–1253.
Current practice patterns among nurses show they are working longer than they ever have.14 The effect of these long hours is that many nurses work in the midst of severe lethargy and sleep deprivation.5 Sleep deprivation jeopardizes not only patient safety but also the safety and general health of the nurses themselves.46 Numerous studies of shift workers in other professions have been done to assess sleepiness using subjective and objective data and also the effect of shift work on work and health.710 Despite the Accreditation Council for Graduate Medical Education (ACGME) mandating work‐hour limitations for medical residents, recent data suggest that sleepiness continues to be a significant issue for medical residents.11 There is a paucity of objective information about the sleepiness and performance of nurses, especially now that most nurses in the United States are working 12‐hour shifts. We hypothesized that nurses working a 12‐hour night shift would have a significant degree of sleepiness. Our objective was to assess the daytime sleepiness of post‐night‐shift nurses using both subjective measures (Epworth Sleepiness Scale [ESS]) and objective testing (Multiple Sleep Latency Test [MSLT]).
MATERIALS AND METHODS
The study was initiated after we obtained institutional review board approval.
Setting
The setting of the study was a community hospital in Corpus Christi, Texas.
Design
The study was a prospective pilot study.
Subjects
Twenty adult nurses (age > 18 years) assigned to duty on general floors (both medical and surgical) and the intensive care unit (ICU) who consented to participate in the study were included. Exclusion criteria included recent or ongoing use of sedative, hypnotic, stimulant drugs; illnesses such as cardiac disease; narcolepsy and other primary sleep disorders; being pregnant or lactating, and being obese (body mass index [BMI] > 30).
Protocol
Floor nurses (n = 10) constituted the control group, and ICU nurses (n = 10) formed the study group. Both groups of nurses came on duty at 7 PM and completed their duty at 7 AM. The MSLT test was performed in the morning following either the third or fourth night shift. All nurses maintained a detailed sleep diary for the week prior to the day of the test that included a detailed record of their bedtimes, wake times, and daytime naps and also included comments about nocturnal awakenings and subjective sleepiness. All nurses were asked to fill out the ESS prior to undergoing the MSLT. ESS is a well‐standardized and validated measure of subjective sleepiness.12 The score was established based on the questionnaire about their chances of falling asleep in 6 different scenarios. A score greater than 8 was considered abnormal. A modified protocol for MSLT was used, which consisted of only 2 nap opportunities. This was done to enable these nurses to go home at a reasonable time in order to catch up on their sleep after having spent the previous night at work. The MSLT procedure was explained to nurses before the start of study, and the MSLT was done at 7:15 AM and 8:30 AM. Standard guidelines for the test were followed.13 Nurses were given $25 gift certificates on completion of the study.
Statistical Analysis
Standard software was used for computation of all data. The t test was used for comparison of means, and Fisher's exact analysis was used to compare proportions. All P values are 2 sided. The term significant indicates a P value < .05. Computations were performed using Microsoft Excel software.
RESULTS
Baseline data are shown in Table 1. Nurses in the 2 groups were matched for age, sex, and marital and offspring status. There was a small but statistically significant difference between the 2 groups in BMI (see Table 1). There was no difference between the 2 groups in the average time slept (per night) in the week preceding the test. Seven of 10 ICU nurses had an abnormal ESS (>8) compared with 2 of 10 floor nurses. Mean ESS of ICU nurses was also higher (5.6 2.1 vs. 8.7 3.9 minutes, respectively, P = .042). Nine of 10 ICU nurses had sleep latency values in the severe pathologic range (<5 minutes) for the first sleep period, compared with only 2 of 10 in the floor group. Mean sleep latency in the nap 1 period differed significantly between the 2 groups (Table 2). Overall, however, mean MSLT value did not differ between the ICU nurses and the control group (6.1 3.8 vs. 10.6 7.5 minutes; Table 2 and Fig. 1). Also, during MSLT, the nurses were unaware of their sleep onset in 10 of the 32 periods (31.3%).
| Variable | ICU nurses (n = 10) | Floor nurses (n = 10) | P value |
|---|---|---|---|
| |||
| Age (years) | 37.1 7.53 | 34.6 7.19 | .45 |
| Sex (M:F) | 4:6 | 1:9 | .118 |
| BMI* | 24.9 3.5 | 21.6 1.9 | .02 |
| Married | 5 | 6 | .315 |
| With Children | 6 | 5 | .315 |
| Variable | ICU nurses (n = 10) | Floor nurses (n = 10) | P value |
|---|---|---|---|
| |||
| Sleep time (minutes) | 405.2 36.6 | 416.1 84.73 | .72 |
| ESS score* | 8.7 3.9 | 5.6 2.1 | .042 |
| Abnormal ESS (>8)* | 7 | 2 | .032 |
| MSLT (min) | 6.1 3.8 | 1.6 7.5 | .19 |
| First‐period sleep latency < 5 minutes* | 9 | 2 | <.005 |
| First nap MSLT | 4.65 5.56 | 1.85 7.44 | .025 |
DISCUSSION
Our study shows that nurses working night shifts have a pathologic degree of sleepiness. This was especially severe in the ICU nurses as determined by both the ESS and the MSLT studies.
To our knowledge, ours is the first study that has comprehensively evaluated the issue of sleepiness in nurses working night shifts using both the ESS and the MSLT. Previous studies have evaluated subjective sleepiness in nurses. In a cross‐sectional study in 8 large hospitals in Japan, Suzuki et al. found that an estimated 26% of the 4407 nurses surveyed reported excess sleepiness.14 They found key associations of daytime sleepiness with motor vehicle accidents, medication errors, and incorrect operation of medical equipment. Scott et al. randomly surveyed 502 critical care nurses across the US and found that almost two thirds reported struggling to stay awake at least once during the study period and that 22% fell asleep at least once during their work shift.2 Sleep deprivation resulting in impairment in cognitive and psychomotor performance and its association with medical errors have now been well documented in medical residents.1517 This has resulted in the Accreditation Council for Graduate Medical Education mandating a reduction in resident work hours.18 No state or federal regulations restrict the number of hours a nurse may voluntarily work in a 24‐hour or a 7‐day period. Bills prohibiting mandatory overtime for nurses have passed only in California, Maine, New Jersey, and Oregon. No measure, either proposed or enacted, addresses how long nurses may work voluntarily. The recent Institute of Medicine (IOM) report, Keeping Patients Safe, explicitly recommends that nurses' shifts be limited to 12 hours in a 24‐hour period, 60 hours per week, and that voluntary overtime be limited.19
Even with the current ACGME‐mandated reduction in work hours, we and others have reported that sleepiness in medical residents continues to be a major issue.11, 20 In the first year following implementation of the ACGME duty‐hour standards, as many as 43% of interns reported noncompliance with these requirements.21 This demonstrates that mandating work‐hour reductions is only the first step in what is likely to be a long process of effecting change in nurse work hours and fatigue and, in turn, improving patient safety. However, initiating this process is going to be crucial, given the impact even small changes in nursing fatigue could have on patient‐care outcomes.
A nationwide nursing shortage has placed enormous stress on the delivery of patient care in our hospitals. Demands of nursing care requirements have also increased in today's health care scenario because of a variety of socioeconomic factors, and this in turn has forced hospitals to encourage and in many instances insist on nurses working overtime and longer shifts. Rogers et al. examined logbooks completed by 393 hospital staff nurses and found that 40% of the 5317 work shifts they logged exceeded 12 hours. The risk of making an error was significantly increased when the work shift was longer than 12 hours, when overtime was worked, and when the workweek was more than 40 hours.5 There are good data comparing 8‐ and 12‐hour shift lengths among other occupational groups that demonstrate, particularly for the night shift, greater sleepiness during a 12‐hour night shift than during an 8‐hour night shift.22 Emergency room physicians overwhelmingly prefer shifts to last 8 and 10 hours than 12 hours, and longer shifts have been shown to impair their triage decisions in simulation studies.23 The problem is compounded for female nurses, as they also have to carry out their responsibilities as partner and parent along with working, resulting in chronic fatigue and sleep deprivation.24 From these results together with the results of the present study, we suggest enforcing a shift length of no longer than 10 hours for nurses working the night shift in a critical care environment.
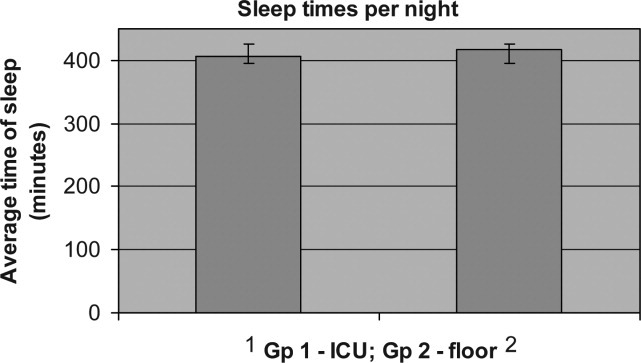
In our study, ICU nurses were found to be more sleepy than floor nurses. Sleep quantity in the week prior to the study day did not differ between the 2 groups (405.2 36.6 vs. 416.1 84.73 minutes; P = .364; Fig. 2). For the 24 hours prior to the night shift that was studied, the average amount of sleep was not different between the 2 groups (406 65 minutes for the ICU group vs. 432 107 minutes for the control group; P = .265; Fig. 4). Sleep quality could certainly be markedly different between the 2 groups. A recent study has reported that nearly a third of ICU nurses had severe burnout syndrome, and this has been associated with profound sleep disturbances.25, 26 This could also be attributed to the floor nurses having a less demanding schedule than the ICU nurses.
Our study had some limitations. Our sample size was small, and larger studies may be needed to validate the results of this pilot study. Although our 2 groups were matched for age and sex, the BMI of ICU nurses was slightly but statistically significantly higher than that of floor nurses. Although the mean BMI of ICU nurses was still not in the obese range (one of the exclusion criteria was a BMI > 30), we still cannot definitively rule out that the higher BMI may have conferred a risk of increased upper airway resistance and sleep‐disordered breathing. The control group consisted of RNs in different settingsmedical and surgicaland because of the small numbers of nurses studied, we are unable to further dissect this group and identify differences in degrees of sleepiness. For example, sleep deprivation effects have been shown to be less pronounced in nurses regularly and permanently working night shifts than in nurses working to rotating shifts,27 perhaps a consequence of circadian misalignment being more severe in the latter group, and this factor was not controlled for. We also measured sleepiness after the shift was completed and not during the shift. Not only is this likely reflective of the nurses' sleepiness toward the latter portion of their shift, it also has direct implications for the driving safety of nurses at the end of a shift.
Our MSLT data showed significant differences only for nap 1 but not when combined for the 2 nap periods. We speculate that the reason for this could be that some alertness was recovered by the first nap, as 9 of 10 in the ICU group had at least 15 minutes of sleep during the first nap opportunity compared with only 2 of 10 nurses in the floor group. Incidentally, the only nurse in the ICU group who had no sleep during the first nap period had a sleep latency of 2 minutes during the second nap period (see Fig. 3).
We also did not correlate sleepiness in our study with any clinical performance, and this will be an important variable to focus on in future studies.
In conclusion, our data indicate that nurses working in the ICU are significantly more sleepy than nurses on the floor. Level of sleepiness of ICU nurses is frequently in the pathologic range, comparable to narcolepsy.
Current practice patterns among nurses show they are working longer than they ever have.14 The effect of these long hours is that many nurses work in the midst of severe lethargy and sleep deprivation.5 Sleep deprivation jeopardizes not only patient safety but also the safety and general health of the nurses themselves.46 Numerous studies of shift workers in other professions have been done to assess sleepiness using subjective and objective data and also the effect of shift work on work and health.710 Despite the Accreditation Council for Graduate Medical Education (ACGME) mandating work‐hour limitations for medical residents, recent data suggest that sleepiness continues to be a significant issue for medical residents.11 There is a paucity of objective information about the sleepiness and performance of nurses, especially now that most nurses in the United States are working 12‐hour shifts. We hypothesized that nurses working a 12‐hour night shift would have a significant degree of sleepiness. Our objective was to assess the daytime sleepiness of post‐night‐shift nurses using both subjective measures (Epworth Sleepiness Scale [ESS]) and objective testing (Multiple Sleep Latency Test [MSLT]).
MATERIALS AND METHODS
The study was initiated after we obtained institutional review board approval.
Setting
The setting of the study was a community hospital in Corpus Christi, Texas.
Design
The study was a prospective pilot study.
Subjects
Twenty adult nurses (age > 18 years) assigned to duty on general floors (both medical and surgical) and the intensive care unit (ICU) who consented to participate in the study were included. Exclusion criteria included recent or ongoing use of sedative, hypnotic, stimulant drugs; illnesses such as cardiac disease; narcolepsy and other primary sleep disorders; being pregnant or lactating, and being obese (body mass index [BMI] > 30).
Protocol
Floor nurses (n = 10) constituted the control group, and ICU nurses (n = 10) formed the study group. Both groups of nurses came on duty at 7 PM and completed their duty at 7 AM. The MSLT test was performed in the morning following either the third or fourth night shift. All nurses maintained a detailed sleep diary for the week prior to the day of the test that included a detailed record of their bedtimes, wake times, and daytime naps and also included comments about nocturnal awakenings and subjective sleepiness. All nurses were asked to fill out the ESS prior to undergoing the MSLT. ESS is a well‐standardized and validated measure of subjective sleepiness.12 The score was established based on the questionnaire about their chances of falling asleep in 6 different scenarios. A score greater than 8 was considered abnormal. A modified protocol for MSLT was used, which consisted of only 2 nap opportunities. This was done to enable these nurses to go home at a reasonable time in order to catch up on their sleep after having spent the previous night at work. The MSLT procedure was explained to nurses before the start of study, and the MSLT was done at 7:15 AM and 8:30 AM. Standard guidelines for the test were followed.13 Nurses were given $25 gift certificates on completion of the study.
Statistical Analysis
Standard software was used for computation of all data. The t test was used for comparison of means, and Fisher's exact analysis was used to compare proportions. All P values are 2 sided. The term significant indicates a P value < .05. Computations were performed using Microsoft Excel software.
RESULTS
Baseline data are shown in Table 1. Nurses in the 2 groups were matched for age, sex, and marital and offspring status. There was a small but statistically significant difference between the 2 groups in BMI (see Table 1). There was no difference between the 2 groups in the average time slept (per night) in the week preceding the test. Seven of 10 ICU nurses had an abnormal ESS (>8) compared with 2 of 10 floor nurses. Mean ESS of ICU nurses was also higher (5.6 2.1 vs. 8.7 3.9 minutes, respectively, P = .042). Nine of 10 ICU nurses had sleep latency values in the severe pathologic range (<5 minutes) for the first sleep period, compared with only 2 of 10 in the floor group. Mean sleep latency in the nap 1 period differed significantly between the 2 groups (Table 2). Overall, however, mean MSLT value did not differ between the ICU nurses and the control group (6.1 3.8 vs. 10.6 7.5 minutes; Table 2 and Fig. 1). Also, during MSLT, the nurses were unaware of their sleep onset in 10 of the 32 periods (31.3%).
| Variable | ICU nurses (n = 10) | Floor nurses (n = 10) | P value |
|---|---|---|---|
| |||
| Age (years) | 37.1 7.53 | 34.6 7.19 | .45 |
| Sex (M:F) | 4:6 | 1:9 | .118 |
| BMI* | 24.9 3.5 | 21.6 1.9 | .02 |
| Married | 5 | 6 | .315 |
| With Children | 6 | 5 | .315 |
| Variable | ICU nurses (n = 10) | Floor nurses (n = 10) | P value |
|---|---|---|---|
| |||
| Sleep time (minutes) | 405.2 36.6 | 416.1 84.73 | .72 |
| ESS score* | 8.7 3.9 | 5.6 2.1 | .042 |
| Abnormal ESS (>8)* | 7 | 2 | .032 |
| MSLT (min) | 6.1 3.8 | 1.6 7.5 | .19 |
| First‐period sleep latency < 5 minutes* | 9 | 2 | <.005 |
| First nap MSLT | 4.65 5.56 | 1.85 7.44 | .025 |
DISCUSSION
Our study shows that nurses working night shifts have a pathologic degree of sleepiness. This was especially severe in the ICU nurses as determined by both the ESS and the MSLT studies.
To our knowledge, ours is the first study that has comprehensively evaluated the issue of sleepiness in nurses working night shifts using both the ESS and the MSLT. Previous studies have evaluated subjective sleepiness in nurses. In a cross‐sectional study in 8 large hospitals in Japan, Suzuki et al. found that an estimated 26% of the 4407 nurses surveyed reported excess sleepiness.14 They found key associations of daytime sleepiness with motor vehicle accidents, medication errors, and incorrect operation of medical equipment. Scott et al. randomly surveyed 502 critical care nurses across the US and found that almost two thirds reported struggling to stay awake at least once during the study period and that 22% fell asleep at least once during their work shift.2 Sleep deprivation resulting in impairment in cognitive and psychomotor performance and its association with medical errors have now been well documented in medical residents.1517 This has resulted in the Accreditation Council for Graduate Medical Education mandating a reduction in resident work hours.18 No state or federal regulations restrict the number of hours a nurse may voluntarily work in a 24‐hour or a 7‐day period. Bills prohibiting mandatory overtime for nurses have passed only in California, Maine, New Jersey, and Oregon. No measure, either proposed or enacted, addresses how long nurses may work voluntarily. The recent Institute of Medicine (IOM) report, Keeping Patients Safe, explicitly recommends that nurses' shifts be limited to 12 hours in a 24‐hour period, 60 hours per week, and that voluntary overtime be limited.19
Even with the current ACGME‐mandated reduction in work hours, we and others have reported that sleepiness in medical residents continues to be a major issue.11, 20 In the first year following implementation of the ACGME duty‐hour standards, as many as 43% of interns reported noncompliance with these requirements.21 This demonstrates that mandating work‐hour reductions is only the first step in what is likely to be a long process of effecting change in nurse work hours and fatigue and, in turn, improving patient safety. However, initiating this process is going to be crucial, given the impact even small changes in nursing fatigue could have on patient‐care outcomes.
A nationwide nursing shortage has placed enormous stress on the delivery of patient care in our hospitals. Demands of nursing care requirements have also increased in today's health care scenario because of a variety of socioeconomic factors, and this in turn has forced hospitals to encourage and in many instances insist on nurses working overtime and longer shifts. Rogers et al. examined logbooks completed by 393 hospital staff nurses and found that 40% of the 5317 work shifts they logged exceeded 12 hours. The risk of making an error was significantly increased when the work shift was longer than 12 hours, when overtime was worked, and when the workweek was more than 40 hours.5 There are good data comparing 8‐ and 12‐hour shift lengths among other occupational groups that demonstrate, particularly for the night shift, greater sleepiness during a 12‐hour night shift than during an 8‐hour night shift.22 Emergency room physicians overwhelmingly prefer shifts to last 8 and 10 hours than 12 hours, and longer shifts have been shown to impair their triage decisions in simulation studies.23 The problem is compounded for female nurses, as they also have to carry out their responsibilities as partner and parent along with working, resulting in chronic fatigue and sleep deprivation.24 From these results together with the results of the present study, we suggest enforcing a shift length of no longer than 10 hours for nurses working the night shift in a critical care environment.
In our study, ICU nurses were found to be more sleepy than floor nurses. Sleep quantity in the week prior to the study day did not differ between the 2 groups (405.2 36.6 vs. 416.1 84.73 minutes; P = .364; Fig. 2). For the 24 hours prior to the night shift that was studied, the average amount of sleep was not different between the 2 groups (406 65 minutes for the ICU group vs. 432 107 minutes for the control group; P = .265; Fig. 4). Sleep quality could certainly be markedly different between the 2 groups. A recent study has reported that nearly a third of ICU nurses had severe burnout syndrome, and this has been associated with profound sleep disturbances.25, 26 This could also be attributed to the floor nurses having a less demanding schedule than the ICU nurses.
Our study had some limitations. Our sample size was small, and larger studies may be needed to validate the results of this pilot study. Although our 2 groups were matched for age and sex, the BMI of ICU nurses was slightly but statistically significantly higher than that of floor nurses. Although the mean BMI of ICU nurses was still not in the obese range (one of the exclusion criteria was a BMI > 30), we still cannot definitively rule out that the higher BMI may have conferred a risk of increased upper airway resistance and sleep‐disordered breathing. The control group consisted of RNs in different settingsmedical and surgicaland because of the small numbers of nurses studied, we are unable to further dissect this group and identify differences in degrees of sleepiness. For example, sleep deprivation effects have been shown to be less pronounced in nurses regularly and permanently working night shifts than in nurses working to rotating shifts,27 perhaps a consequence of circadian misalignment being more severe in the latter group, and this factor was not controlled for. We also measured sleepiness after the shift was completed and not during the shift. Not only is this likely reflective of the nurses' sleepiness toward the latter portion of their shift, it also has direct implications for the driving safety of nurses at the end of a shift.
Our MSLT data showed significant differences only for nap 1 but not when combined for the 2 nap periods. We speculate that the reason for this could be that some alertness was recovered by the first nap, as 9 of 10 in the ICU group had at least 15 minutes of sleep during the first nap opportunity compared with only 2 of 10 nurses in the floor group. Incidentally, the only nurse in the ICU group who had no sleep during the first nap period had a sleep latency of 2 minutes during the second nap period (see Fig. 3).
We also did not correlate sleepiness in our study with any clinical performance, and this will be an important variable to focus on in future studies.
In conclusion, our data indicate that nurses working in the ICU are significantly more sleepy than nurses on the floor. Level of sleepiness of ICU nurses is frequently in the pathologic range, comparable to narcolepsy.
- ,.Trends in nurse overtime, 1995–2002.Policy Polit Nurs Pract.2005;6:183–190.
- ,,,.Effects of critical care nurses' work hours on vigilance and patients' safety.Am J Crit Care.2006;15:30–37.
- ,,,,.How long and how much are nurses now working?Am J Nurs.2006;106:60–71.
- ,.Are you tired? Sleep deprivation compromises nurse's health and jeopardizes patients.Am J Nurs.2004;104:36–38.
- ,,,,.The working hours of hospital staff nurses and patient safety.Health Aff (Millwood).2004;23:202–212.
- ,.Twelve‐hour night shifts of healthcare workers: a risk to the patients?Chronobiol Int.2003;20:351–360.
- ,,,,.The sleep of long‐haul truck drivers.N Engl J Med.1997;337:755–761.
- ,,, et al.Subjective and objective measures of adaptation and readaptation to night work on an oil rig in the North Sea.Sleep.2006;29:821–829.
- ,,,,.Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers.Sleep.2004;27:1453–1462.
- ,.Impact of shift work on the health and safety of nurses and patients.Clin J Oncol Nurs.2006;0:465–471.
- ,,,,.Sleepiness in medical residents: Impact of mandated reduction in work hours.Sleep Med.2007;8:90–93.
- .A new method for measuring daytime sleepiness: the Epworth sleepiness scale.Sleep.1991;14:540–545.
- ,,,,,, et al.Standards of practice committee of the American Academy of Sleep Medicine. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test.Sleep.2005;28:113–121.
- ,,,,.Daytime sleepiness, sleep habits and occupational accidents among hospital nurses.J Adv Nurs.2005;52:445–453.
- ,,,,.Neurobehavioral performance of residents after heavy night call vs after alcohol ingestion.JAMA.2005;294:1025–1033.
- .Simulation study of rested versus sleep‐deprived anesthesiologists.Anesthesiology.2003;98:1345–1355.
- ,,,.The risks and implication of excessive daytime sleepiness in resident physicians.Acad Med.2002;77:1019–1025.
- Accreditation Council for Graduate Medical Education. Common program requirements. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_dutyHoursCommonPR.pdf.
- Institute of Medicine.Keeping Patients Safe: Transforming the Work Environment of Nurses.Washington, DC:National Academies Press;2003.
- ,,, et al.Sleep and well‐being of ICU housestaff.Chest.2007;131:1685–1693.
- ,,,,.Interns' compliance with accreditation council for graduate medical education work‐hour limits.JAMA.2006;296:1063–1070.
- ,,, et al.Effects of alternating 8‐ and 12‐hour shifts on sleep, sleepiness, physical effort and performance.Scand J Work Environ Health.1998;24:62–68.
- ,,, et al.Emergency medicine residents' shiftwork tolerance and preference.Acad Emerg Med.2000;7:670–673.
- ,,,.A study of female nurses combining partner and parent roles with working a continuous three‐shift roster: the impact on sleep, fatigue and stress.Contemp Nurse.2002;12:294–302.
- ,,, et al.Burnout syndrome in critical care nursing staff.Am J Respir Crit Care Med2007;175:698–704.
- ,,, et al.Disturbed sleep and fatigue in occupational burnout.Scand J Work Environ Health.2006;32:121.
- .A computer‐aided comparative study of progressive alertness changes in nurses working two different night‐shift rotations.J Adv Nurs.1996;23:1247–1253.
- ,.Trends in nurse overtime, 1995–2002.Policy Polit Nurs Pract.2005;6:183–190.
- ,,,.Effects of critical care nurses' work hours on vigilance and patients' safety.Am J Crit Care.2006;15:30–37.
- ,,,,.How long and how much are nurses now working?Am J Nurs.2006;106:60–71.
- ,.Are you tired? Sleep deprivation compromises nurse's health and jeopardizes patients.Am J Nurs.2004;104:36–38.
- ,,,,.The working hours of hospital staff nurses and patient safety.Health Aff (Millwood).2004;23:202–212.
- ,.Twelve‐hour night shifts of healthcare workers: a risk to the patients?Chronobiol Int.2003;20:351–360.
- ,,,,.The sleep of long‐haul truck drivers.N Engl J Med.1997;337:755–761.
- ,,, et al.Subjective and objective measures of adaptation and readaptation to night work on an oil rig in the North Sea.Sleep.2006;29:821–829.
- ,,,,.Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers.Sleep.2004;27:1453–1462.
- ,.Impact of shift work on the health and safety of nurses and patients.Clin J Oncol Nurs.2006;0:465–471.
- ,,,,.Sleepiness in medical residents: Impact of mandated reduction in work hours.Sleep Med.2007;8:90–93.
- .A new method for measuring daytime sleepiness: the Epworth sleepiness scale.Sleep.1991;14:540–545.
- ,,,,,, et al.Standards of practice committee of the American Academy of Sleep Medicine. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test.Sleep.2005;28:113–121.
- ,,,,.Daytime sleepiness, sleep habits and occupational accidents among hospital nurses.J Adv Nurs.2005;52:445–453.
- ,,,,.Neurobehavioral performance of residents after heavy night call vs after alcohol ingestion.JAMA.2005;294:1025–1033.
- .Simulation study of rested versus sleep‐deprived anesthesiologists.Anesthesiology.2003;98:1345–1355.
- ,,,.The risks and implication of excessive daytime sleepiness in resident physicians.Acad Med.2002;77:1019–1025.
- Accreditation Council for Graduate Medical Education. Common program requirements. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_dutyHoursCommonPR.pdf.
- Institute of Medicine.Keeping Patients Safe: Transforming the Work Environment of Nurses.Washington, DC:National Academies Press;2003.
- ,,, et al.Sleep and well‐being of ICU housestaff.Chest.2007;131:1685–1693.
- ,,,,.Interns' compliance with accreditation council for graduate medical education work‐hour limits.JAMA.2006;296:1063–1070.
- ,,, et al.Effects of alternating 8‐ and 12‐hour shifts on sleep, sleepiness, physical effort and performance.Scand J Work Environ Health.1998;24:62–68.
- ,,, et al.Emergency medicine residents' shiftwork tolerance and preference.Acad Emerg Med.2000;7:670–673.
- ,,,.A study of female nurses combining partner and parent roles with working a continuous three‐shift roster: the impact on sleep, fatigue and stress.Contemp Nurse.2002;12:294–302.
- ,,, et al.Burnout syndrome in critical care nursing staff.Am J Respir Crit Care Med2007;175:698–704.
- ,,, et al.Disturbed sleep and fatigue in occupational burnout.Scand J Work Environ Health.2006;32:121.
- .A computer‐aided comparative study of progressive alertness changes in nurses working two different night‐shift rotations.J Adv Nurs.1996;23:1247–1253.
Copyright © 2008 Society of Hospital Medicine