User login
New Data Add to Debate Over Optimal Transfusion Ratio
CHICAGO – A fresh frozen plasma–to–red blood cells ratio greater than 0.4:1 can stanch bleeding without causing organ failure, a small single-center study of 185 patients has found.
Trauma surgeons have long grappled with the ideal fresh frozen plasma–to–red blood cells (FFP:RBC) ratio for transfusion in severely injured patients because a 1:1 ratio may stop bleeding but cause respiratory distress. Results of the new study, presented by Dr. Charles E. Lucas at the annual meeting of the American Association for the Surgery of Trauma, shed some light on this question and identified some key recommendations for how level I trauma centers should manage massive transfusions.
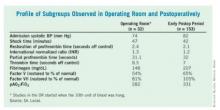
Dr. Lucas of the department of surgery at Wayne State University, Detroit, and his colleagues tracked serial measurements in 185 injured patients who received an average of 1,064 mL of FFP and 17.1 U of RBC, along with 12.6 L of crystalloids.
Observing patients during and after surgery, they compared levels of fibrinogen and labile factors V and VIII, standard clotting times, PaO2:FiO2 ratios for acute respiratory distress syndrome, and shock times. The average operation time was 8.1 hours. Studies in the operating room started when the 10th unit of blood was hung, he said.
"During the operative observation, we found the higher [the] level of FFP, the better [the] clotting times – the relationship of FFP ratio to coagulants again showing [that a] greater number of units of plasma given per red cells affects the procoagulant level," Dr. Lucas said. Moreover, the PaO2:FiO2 and FFP:RBC ratios showed no correlation in the operative or postoperative groups.
In the early postoperative group, at an average of 17 hours after admission, the relationship between clotting times and FFP:RBC ratio went away; factor V was the only factor that coordinated directly with FFP ratio, Dr. Lucas said. "This means that the increase in procoagulants at 17 hours after the patient arrives can no longer be related to the FFP:RBC ratio, but is due to increased synthesis of these factors by the liver and relocation of these factors from the interstitial fluid space," he said.
On the basis of the study results, the investigators offered the following four recommendations for level I centers responding to level I activation:
• Have 4 units of sex-specific O-negative RBC without plasma on hand.
• Use an FFP:RBC ratio of 2:4 if more plasma is needed.
• If plasma can be available in 10 minutes, use FFP when rapid thawing capabilities are available; otherwise, use prethawed plasma.
• Maintain a subsequent FFP:RBC ratio of 2:4 with ongoing monitoring of the coagulation test.
Dr. Ernest E. Moore Jr., the discussion leader for the paper, acknowledged that in the decades-long debate about the optimal FFP:RBC ratio, trauma surgeons have seen recommendations go from 1:4 to 1:5 and, more recently, to 1:2 or 1:3. Prothrombin and partial prothrombin times represent only the first 5% of activity in thrombin generation, noted Dr. Moore of Denver Health Medical Center.
"That’s true if you look at all the factors that are being evaluated by the clotting system," Dr. Lucas replied, "but with all the clotting tests, the end point is the conversion of fibrinogen to fibrin, so in that sense, it represents 100% of what’s happening."
Dr. Moore also asked whether the investigators detected any effect of FFP on renal, hepatic, or cardiac function.
The study evaluated several markers for those organs, Dr. Lucas noted. Among patients who received higher levels of plasma, the investigators found a slight increase in bilirubin in the operative group; in the postoperative group, they identified a significant increase in the level of FiO2 needed to achieve the desired PaO2 levels.
Dr. Lucas had no relevant disclosures.
CHICAGO – A fresh frozen plasma–to–red blood cells ratio greater than 0.4:1 can stanch bleeding without causing organ failure, a small single-center study of 185 patients has found.
Trauma surgeons have long grappled with the ideal fresh frozen plasma–to–red blood cells (FFP:RBC) ratio for transfusion in severely injured patients because a 1:1 ratio may stop bleeding but cause respiratory distress. Results of the new study, presented by Dr. Charles E. Lucas at the annual meeting of the American Association for the Surgery of Trauma, shed some light on this question and identified some key recommendations for how level I trauma centers should manage massive transfusions.
Dr. Lucas of the department of surgery at Wayne State University, Detroit, and his colleagues tracked serial measurements in 185 injured patients who received an average of 1,064 mL of FFP and 17.1 U of RBC, along with 12.6 L of crystalloids.
Observing patients during and after surgery, they compared levels of fibrinogen and labile factors V and VIII, standard clotting times, PaO2:FiO2 ratios for acute respiratory distress syndrome, and shock times. The average operation time was 8.1 hours. Studies in the operating room started when the 10th unit of blood was hung, he said.
"During the operative observation, we found the higher [the] level of FFP, the better [the] clotting times – the relationship of FFP ratio to coagulants again showing [that a] greater number of units of plasma given per red cells affects the procoagulant level," Dr. Lucas said. Moreover, the PaO2:FiO2 and FFP:RBC ratios showed no correlation in the operative or postoperative groups.
In the early postoperative group, at an average of 17 hours after admission, the relationship between clotting times and FFP:RBC ratio went away; factor V was the only factor that coordinated directly with FFP ratio, Dr. Lucas said. "This means that the increase in procoagulants at 17 hours after the patient arrives can no longer be related to the FFP:RBC ratio, but is due to increased synthesis of these factors by the liver and relocation of these factors from the interstitial fluid space," he said.
On the basis of the study results, the investigators offered the following four recommendations for level I centers responding to level I activation:
• Have 4 units of sex-specific O-negative RBC without plasma on hand.
• Use an FFP:RBC ratio of 2:4 if more plasma is needed.
• If plasma can be available in 10 minutes, use FFP when rapid thawing capabilities are available; otherwise, use prethawed plasma.
• Maintain a subsequent FFP:RBC ratio of 2:4 with ongoing monitoring of the coagulation test.
Dr. Ernest E. Moore Jr., the discussion leader for the paper, acknowledged that in the decades-long debate about the optimal FFP:RBC ratio, trauma surgeons have seen recommendations go from 1:4 to 1:5 and, more recently, to 1:2 or 1:3. Prothrombin and partial prothrombin times represent only the first 5% of activity in thrombin generation, noted Dr. Moore of Denver Health Medical Center.
"That’s true if you look at all the factors that are being evaluated by the clotting system," Dr. Lucas replied, "but with all the clotting tests, the end point is the conversion of fibrinogen to fibrin, so in that sense, it represents 100% of what’s happening."
Dr. Moore also asked whether the investigators detected any effect of FFP on renal, hepatic, or cardiac function.
The study evaluated several markers for those organs, Dr. Lucas noted. Among patients who received higher levels of plasma, the investigators found a slight increase in bilirubin in the operative group; in the postoperative group, they identified a significant increase in the level of FiO2 needed to achieve the desired PaO2 levels.
Dr. Lucas had no relevant disclosures.
CHICAGO – A fresh frozen plasma–to–red blood cells ratio greater than 0.4:1 can stanch bleeding without causing organ failure, a small single-center study of 185 patients has found.
Trauma surgeons have long grappled with the ideal fresh frozen plasma–to–red blood cells (FFP:RBC) ratio for transfusion in severely injured patients because a 1:1 ratio may stop bleeding but cause respiratory distress. Results of the new study, presented by Dr. Charles E. Lucas at the annual meeting of the American Association for the Surgery of Trauma, shed some light on this question and identified some key recommendations for how level I trauma centers should manage massive transfusions.
Dr. Lucas of the department of surgery at Wayne State University, Detroit, and his colleagues tracked serial measurements in 185 injured patients who received an average of 1,064 mL of FFP and 17.1 U of RBC, along with 12.6 L of crystalloids.
Observing patients during and after surgery, they compared levels of fibrinogen and labile factors V and VIII, standard clotting times, PaO2:FiO2 ratios for acute respiratory distress syndrome, and shock times. The average operation time was 8.1 hours. Studies in the operating room started when the 10th unit of blood was hung, he said.
"During the operative observation, we found the higher [the] level of FFP, the better [the] clotting times – the relationship of FFP ratio to coagulants again showing [that a] greater number of units of plasma given per red cells affects the procoagulant level," Dr. Lucas said. Moreover, the PaO2:FiO2 and FFP:RBC ratios showed no correlation in the operative or postoperative groups.
In the early postoperative group, at an average of 17 hours after admission, the relationship between clotting times and FFP:RBC ratio went away; factor V was the only factor that coordinated directly with FFP ratio, Dr. Lucas said. "This means that the increase in procoagulants at 17 hours after the patient arrives can no longer be related to the FFP:RBC ratio, but is due to increased synthesis of these factors by the liver and relocation of these factors from the interstitial fluid space," he said.
On the basis of the study results, the investigators offered the following four recommendations for level I centers responding to level I activation:
• Have 4 units of sex-specific O-negative RBC without plasma on hand.
• Use an FFP:RBC ratio of 2:4 if more plasma is needed.
• If plasma can be available in 10 minutes, use FFP when rapid thawing capabilities are available; otherwise, use prethawed plasma.
• Maintain a subsequent FFP:RBC ratio of 2:4 with ongoing monitoring of the coagulation test.
Dr. Ernest E. Moore Jr., the discussion leader for the paper, acknowledged that in the decades-long debate about the optimal FFP:RBC ratio, trauma surgeons have seen recommendations go from 1:4 to 1:5 and, more recently, to 1:2 or 1:3. Prothrombin and partial prothrombin times represent only the first 5% of activity in thrombin generation, noted Dr. Moore of Denver Health Medical Center.
"That’s true if you look at all the factors that are being evaluated by the clotting system," Dr. Lucas replied, "but with all the clotting tests, the end point is the conversion of fibrinogen to fibrin, so in that sense, it represents 100% of what’s happening."
Dr. Moore also asked whether the investigators detected any effect of FFP on renal, hepatic, or cardiac function.
The study evaluated several markers for those organs, Dr. Lucas noted. Among patients who received higher levels of plasma, the investigators found a slight increase in bilirubin in the operative group; in the postoperative group, they identified a significant increase in the level of FiO2 needed to achieve the desired PaO2 levels.
Dr. Lucas had no relevant disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THE SURGERY OF TRAUMA
Trauma Funding Cuts May Jeopardize Care of Immigrants
CHICAGO – Funding sources to cover care for undocumented immigrants have pulled back since 2008 and will continue to do so after the Patient Protection and Affordable Care Act takes full effect. Although the legislation strives to provide nearly universal health insurance coverage by 2014, undocumented immigrants are not included, and one hospital’s experience with dwindling reimbursement portends a cloudy future for paying for care in this patient population.
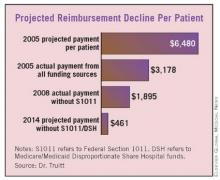
Even when the Affordable Care Act takes full effect, about 22 million people will still lack coverage – 10-15 million of whom will be undocumented immigrants, according to Dr. Michael S. Truitt of Methodist Dallas Medical Center. The Affordable Care Act will cut Medicare/Medicaid Disproportionate Share Hospital (DSH) funds by about 75% between 2014 and 2019.
"We have serious and specific concerns about how the cut in DSH funding could affect trauma centers and safety net hospitals," Dr. Truitt said at the annual meeting of the American Association for the Surgery of Trauma. "On a per-patient basis at our institution, projected payments decrease from $6,480 in 2005 to $461 in 2014."
He presented a study that evaluated retrospectively 183,000 visits to his hospital’s emergency department from 2005 to 2008. Of those, 6,691 were undocumented immigrants, and about 20% of their visits were trauma related, he said.
The study focused on the four main funding mechanisms for the care of undocumented immigrants in Texas: self-payment; the Texas Driver Responsibility Program (DRP), which uses motor vehicle fines; federal Section 1011 funds; and DSH funds.
The state DRP program distributes $70 million to $90 million to Texas hospitals annually, Dr. Truitt said, but even that has been problematic. "Significantly more has been collected each year and earmarked for trauma, but disbursement from the state has not always been consistent," he said.
Section 1011 distributed about $1 billion from 2005 to 2008, one-third of which went to the eight states bordering Mexico, but that program has been unfunded since 2008, according to Dr. Truitt. Medicare/Medicaid DSH funds distributed $19.1 billion to U.S. hospitals in 2009, but these funds are used to subsidize numerous programs and are not specific to care of indigent trauma patients.
From May 2005 to May 2008, Methodist Dallas Medical Center actually collected about $4.2 million from these varied sources for uncompensated undocumented immigrant trauma care – about $4.9 million less than the hospital’s usual fees, Dr. Truitt said. These funds were shared by the hospital, ED physicians, and trauma surgeons, he noted.
"In the end, this may be just another call for fiscal responsibility on the part of trauma centers to reduce unnecessary charges and waste, such as robust use of CT scans, laboratory tests, etc. – not just for the undocumented immigrant trauma patients, but for all compensated and uncompensated patients," said Dr. Thomas Esposito of Loyola University, Chicago. He asked whether the authors had any suggestions for alternative funding sources, and whether states and trauma systems should take it upon themselves to establish or increase revenue from sources similar to the Texas Driver Responsibility Program.
Dr. Truitt called on policy makers to prioritize funding for trauma centers and safety net hospitals. "If it’s a federal responsibility, so be it, but it should be supported by a program that is not subject to the political winds. If it’s a state responsibility, the states should have the authority to collect these funds and ensure they are disbursed to the intended recipients expeditiously and consistently."
Dr. Truitt and his colleagues had no relevant financial disclosures.
CHICAGO – Funding sources to cover care for undocumented immigrants have pulled back since 2008 and will continue to do so after the Patient Protection and Affordable Care Act takes full effect. Although the legislation strives to provide nearly universal health insurance coverage by 2014, undocumented immigrants are not included, and one hospital’s experience with dwindling reimbursement portends a cloudy future for paying for care in this patient population.
Even when the Affordable Care Act takes full effect, about 22 million people will still lack coverage – 10-15 million of whom will be undocumented immigrants, according to Dr. Michael S. Truitt of Methodist Dallas Medical Center. The Affordable Care Act will cut Medicare/Medicaid Disproportionate Share Hospital (DSH) funds by about 75% between 2014 and 2019.
"We have serious and specific concerns about how the cut in DSH funding could affect trauma centers and safety net hospitals," Dr. Truitt said at the annual meeting of the American Association for the Surgery of Trauma. "On a per-patient basis at our institution, projected payments decrease from $6,480 in 2005 to $461 in 2014."
He presented a study that evaluated retrospectively 183,000 visits to his hospital’s emergency department from 2005 to 2008. Of those, 6,691 were undocumented immigrants, and about 20% of their visits were trauma related, he said.
The study focused on the four main funding mechanisms for the care of undocumented immigrants in Texas: self-payment; the Texas Driver Responsibility Program (DRP), which uses motor vehicle fines; federal Section 1011 funds; and DSH funds.
The state DRP program distributes $70 million to $90 million to Texas hospitals annually, Dr. Truitt said, but even that has been problematic. "Significantly more has been collected each year and earmarked for trauma, but disbursement from the state has not always been consistent," he said.
Section 1011 distributed about $1 billion from 2005 to 2008, one-third of which went to the eight states bordering Mexico, but that program has been unfunded since 2008, according to Dr. Truitt. Medicare/Medicaid DSH funds distributed $19.1 billion to U.S. hospitals in 2009, but these funds are used to subsidize numerous programs and are not specific to care of indigent trauma patients.
From May 2005 to May 2008, Methodist Dallas Medical Center actually collected about $4.2 million from these varied sources for uncompensated undocumented immigrant trauma care – about $4.9 million less than the hospital’s usual fees, Dr. Truitt said. These funds were shared by the hospital, ED physicians, and trauma surgeons, he noted.
"In the end, this may be just another call for fiscal responsibility on the part of trauma centers to reduce unnecessary charges and waste, such as robust use of CT scans, laboratory tests, etc. – not just for the undocumented immigrant trauma patients, but for all compensated and uncompensated patients," said Dr. Thomas Esposito of Loyola University, Chicago. He asked whether the authors had any suggestions for alternative funding sources, and whether states and trauma systems should take it upon themselves to establish or increase revenue from sources similar to the Texas Driver Responsibility Program.
Dr. Truitt called on policy makers to prioritize funding for trauma centers and safety net hospitals. "If it’s a federal responsibility, so be it, but it should be supported by a program that is not subject to the political winds. If it’s a state responsibility, the states should have the authority to collect these funds and ensure they are disbursed to the intended recipients expeditiously and consistently."
Dr. Truitt and his colleagues had no relevant financial disclosures.
CHICAGO – Funding sources to cover care for undocumented immigrants have pulled back since 2008 and will continue to do so after the Patient Protection and Affordable Care Act takes full effect. Although the legislation strives to provide nearly universal health insurance coverage by 2014, undocumented immigrants are not included, and one hospital’s experience with dwindling reimbursement portends a cloudy future for paying for care in this patient population.
Even when the Affordable Care Act takes full effect, about 22 million people will still lack coverage – 10-15 million of whom will be undocumented immigrants, according to Dr. Michael S. Truitt of Methodist Dallas Medical Center. The Affordable Care Act will cut Medicare/Medicaid Disproportionate Share Hospital (DSH) funds by about 75% between 2014 and 2019.
"We have serious and specific concerns about how the cut in DSH funding could affect trauma centers and safety net hospitals," Dr. Truitt said at the annual meeting of the American Association for the Surgery of Trauma. "On a per-patient basis at our institution, projected payments decrease from $6,480 in 2005 to $461 in 2014."
He presented a study that evaluated retrospectively 183,000 visits to his hospital’s emergency department from 2005 to 2008. Of those, 6,691 were undocumented immigrants, and about 20% of their visits were trauma related, he said.
The study focused on the four main funding mechanisms for the care of undocumented immigrants in Texas: self-payment; the Texas Driver Responsibility Program (DRP), which uses motor vehicle fines; federal Section 1011 funds; and DSH funds.
The state DRP program distributes $70 million to $90 million to Texas hospitals annually, Dr. Truitt said, but even that has been problematic. "Significantly more has been collected each year and earmarked for trauma, but disbursement from the state has not always been consistent," he said.
Section 1011 distributed about $1 billion from 2005 to 2008, one-third of which went to the eight states bordering Mexico, but that program has been unfunded since 2008, according to Dr. Truitt. Medicare/Medicaid DSH funds distributed $19.1 billion to U.S. hospitals in 2009, but these funds are used to subsidize numerous programs and are not specific to care of indigent trauma patients.
From May 2005 to May 2008, Methodist Dallas Medical Center actually collected about $4.2 million from these varied sources for uncompensated undocumented immigrant trauma care – about $4.9 million less than the hospital’s usual fees, Dr. Truitt said. These funds were shared by the hospital, ED physicians, and trauma surgeons, he noted.
"In the end, this may be just another call for fiscal responsibility on the part of trauma centers to reduce unnecessary charges and waste, such as robust use of CT scans, laboratory tests, etc. – not just for the undocumented immigrant trauma patients, but for all compensated and uncompensated patients," said Dr. Thomas Esposito of Loyola University, Chicago. He asked whether the authors had any suggestions for alternative funding sources, and whether states and trauma systems should take it upon themselves to establish or increase revenue from sources similar to the Texas Driver Responsibility Program.
Dr. Truitt called on policy makers to prioritize funding for trauma centers and safety net hospitals. "If it’s a federal responsibility, so be it, but it should be supported by a program that is not subject to the political winds. If it’s a state responsibility, the states should have the authority to collect these funds and ensure they are disbursed to the intended recipients expeditiously and consistently."
Dr. Truitt and his colleagues had no relevant financial disclosures.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THE SURGERY OF TRAUMA
Survival Trends Promising in Geriatric Trauma Patients
CHICAGO – Long-term survival in severely injured geriatric trauma patients may not be as poor as once thought, according to a study at a level 1 trauma center in Pennsylvania that followed these patients for up to 10 years after discharge.
The retrospective study presented at the annual meeting of the American Association for the Surgery of Trauma showed an overall death rate of 33% in elderly patients with brain injury, and almost two-thirds of the patients who survived their initial hospitalization were alive at the conclusion of the study, according to Dr. Ulunna Ofurum of St. Luke’s Hospital in Bethlehem, Pa.
Dr. Ofurum and her colleagues undertook their study to learn whether aggressive care in this population was futile. Trauma patients aged 65 and older with an Injury Severity Score of 30 or higher were assigned to two groups based on the presence or absence of brain injury, with an Abbreviated Injury Scale score of 3 or higher as the cutoff. The Social Security Death Index database was used to determine survival status.
"The initial drop in survivorship was most pronounced in the patients with severe head injury," she said. Overall, 97 of the 145 patients survived hospital discharge, but nearly a third died after hospital discharge. That left 65 for analysis of current living status, Dr. Ofurum said. Of those, 52 patients in the head-injured group had a median survival of 33 months, and 13 of the patients without head injury had a median survival of 49 months.
Of the 65 who were still alive when the study ended, 47 were contacted by phone to determine their living arrangements. Overall, 31 (65%) were at home, 11 (23%) were in skilled nursing facilities, four (8%) were at assisted living centers, and one (2%) was in a rehabilitation center.
"The most significant finding of this study is that severely injured geriatric trauma patients who survive their hospitalization have appreciable long-term survival and that a surprising number return home," Dr. Ofurum said. "This study showed that the 5-year survival is almost 20%, which is similar to that of many cancer diagnoses."
She noted that she and her coinvestigators did not apply a uniform approach to the resuscitation variable in all geriatric trauma patients; instead, they used a case-by-case approach. "There is a preselection bias for patients with the most devastating injuries, as we tend not to treat them," she said.
Dr. Ofurum acknowledged some limitations of the study, including its retrospective nature, the small sample size, and the lack of data on cause of death, comorbidities, and survivors’ functional status.
"However, in our practice, it’s been noted that about one-third of deaths that occur in geriatric trauma patients are associated with immediate withdrawal of care," she said. This makes managing complications critical in this patient group. "When patients have complications such as renal failure, families may tend to withdraw care," she said.
With the exponential growth of the elderly population, this and similar studies are notable, said discussion leader Dr. Roxie Albrecht of the University of Oklahoma in Oklahoma City. "Studies such as this do give us a glimmer of hope that not every patient over the age of 65 has the Grim Reaper standing over them, predicting that they will either die in the hospital or never return to their prehospital living status," she said. She noted that the St. Luke’s study is consistent with other reports on elderly trauma (J. Trauma 1998;44:618-23; J. Trauma 2002;52:242-6).
Dr. Ofurum had no conflicts to disclose.
CHICAGO – Long-term survival in severely injured geriatric trauma patients may not be as poor as once thought, according to a study at a level 1 trauma center in Pennsylvania that followed these patients for up to 10 years after discharge.
The retrospective study presented at the annual meeting of the American Association for the Surgery of Trauma showed an overall death rate of 33% in elderly patients with brain injury, and almost two-thirds of the patients who survived their initial hospitalization were alive at the conclusion of the study, according to Dr. Ulunna Ofurum of St. Luke’s Hospital in Bethlehem, Pa.
Dr. Ofurum and her colleagues undertook their study to learn whether aggressive care in this population was futile. Trauma patients aged 65 and older with an Injury Severity Score of 30 or higher were assigned to two groups based on the presence or absence of brain injury, with an Abbreviated Injury Scale score of 3 or higher as the cutoff. The Social Security Death Index database was used to determine survival status.
"The initial drop in survivorship was most pronounced in the patients with severe head injury," she said. Overall, 97 of the 145 patients survived hospital discharge, but nearly a third died after hospital discharge. That left 65 for analysis of current living status, Dr. Ofurum said. Of those, 52 patients in the head-injured group had a median survival of 33 months, and 13 of the patients without head injury had a median survival of 49 months.
Of the 65 who were still alive when the study ended, 47 were contacted by phone to determine their living arrangements. Overall, 31 (65%) were at home, 11 (23%) were in skilled nursing facilities, four (8%) were at assisted living centers, and one (2%) was in a rehabilitation center.
"The most significant finding of this study is that severely injured geriatric trauma patients who survive their hospitalization have appreciable long-term survival and that a surprising number return home," Dr. Ofurum said. "This study showed that the 5-year survival is almost 20%, which is similar to that of many cancer diagnoses."
She noted that she and her coinvestigators did not apply a uniform approach to the resuscitation variable in all geriatric trauma patients; instead, they used a case-by-case approach. "There is a preselection bias for patients with the most devastating injuries, as we tend not to treat them," she said.
Dr. Ofurum acknowledged some limitations of the study, including its retrospective nature, the small sample size, and the lack of data on cause of death, comorbidities, and survivors’ functional status.
"However, in our practice, it’s been noted that about one-third of deaths that occur in geriatric trauma patients are associated with immediate withdrawal of care," she said. This makes managing complications critical in this patient group. "When patients have complications such as renal failure, families may tend to withdraw care," she said.
With the exponential growth of the elderly population, this and similar studies are notable, said discussion leader Dr. Roxie Albrecht of the University of Oklahoma in Oklahoma City. "Studies such as this do give us a glimmer of hope that not every patient over the age of 65 has the Grim Reaper standing over them, predicting that they will either die in the hospital or never return to their prehospital living status," she said. She noted that the St. Luke’s study is consistent with other reports on elderly trauma (J. Trauma 1998;44:618-23; J. Trauma 2002;52:242-6).
Dr. Ofurum had no conflicts to disclose.
CHICAGO – Long-term survival in severely injured geriatric trauma patients may not be as poor as once thought, according to a study at a level 1 trauma center in Pennsylvania that followed these patients for up to 10 years after discharge.
The retrospective study presented at the annual meeting of the American Association for the Surgery of Trauma showed an overall death rate of 33% in elderly patients with brain injury, and almost two-thirds of the patients who survived their initial hospitalization were alive at the conclusion of the study, according to Dr. Ulunna Ofurum of St. Luke’s Hospital in Bethlehem, Pa.
Dr. Ofurum and her colleagues undertook their study to learn whether aggressive care in this population was futile. Trauma patients aged 65 and older with an Injury Severity Score of 30 or higher were assigned to two groups based on the presence or absence of brain injury, with an Abbreviated Injury Scale score of 3 or higher as the cutoff. The Social Security Death Index database was used to determine survival status.
"The initial drop in survivorship was most pronounced in the patients with severe head injury," she said. Overall, 97 of the 145 patients survived hospital discharge, but nearly a third died after hospital discharge. That left 65 for analysis of current living status, Dr. Ofurum said. Of those, 52 patients in the head-injured group had a median survival of 33 months, and 13 of the patients without head injury had a median survival of 49 months.
Of the 65 who were still alive when the study ended, 47 were contacted by phone to determine their living arrangements. Overall, 31 (65%) were at home, 11 (23%) were in skilled nursing facilities, four (8%) were at assisted living centers, and one (2%) was in a rehabilitation center.
"The most significant finding of this study is that severely injured geriatric trauma patients who survive their hospitalization have appreciable long-term survival and that a surprising number return home," Dr. Ofurum said. "This study showed that the 5-year survival is almost 20%, which is similar to that of many cancer diagnoses."
She noted that she and her coinvestigators did not apply a uniform approach to the resuscitation variable in all geriatric trauma patients; instead, they used a case-by-case approach. "There is a preselection bias for patients with the most devastating injuries, as we tend not to treat them," she said.
Dr. Ofurum acknowledged some limitations of the study, including its retrospective nature, the small sample size, and the lack of data on cause of death, comorbidities, and survivors’ functional status.
"However, in our practice, it’s been noted that about one-third of deaths that occur in geriatric trauma patients are associated with immediate withdrawal of care," she said. This makes managing complications critical in this patient group. "When patients have complications such as renal failure, families may tend to withdraw care," she said.
With the exponential growth of the elderly population, this and similar studies are notable, said discussion leader Dr. Roxie Albrecht of the University of Oklahoma in Oklahoma City. "Studies such as this do give us a glimmer of hope that not every patient over the age of 65 has the Grim Reaper standing over them, predicting that they will either die in the hospital or never return to their prehospital living status," she said. She noted that the St. Luke’s study is consistent with other reports on elderly trauma (J. Trauma 1998;44:618-23; J. Trauma 2002;52:242-6).
Dr. Ofurum had no conflicts to disclose.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THE SURGERY OF TRAUMA
Major Finding: Long-term survival in geriatric trauma patients may not be as poor as once thought. Almost two-thirds of the patients who survived their initial hospitalization were alive at the conclusion of the study.
Data Source: A 10-year retrospective study of 145 severely injured geriatric trauma patients at a level 1 trauma center.
Disclosures: Dr. Ofurum had no conflicts to disclose.
Doubt Cast on Protocol for VAP Resolution
CHICAGO – Use of the Clinical Pulmonary Infection Score to guide therapy for ventilator-associated pneumonia in critically ill patients has had mixed results, and a recent study has raised further questions about whether CPIS can accurately determine resolution of the infection in critically injured trauma ICU patients.
"Using CPIS to determine the appropriate duration of antimicrobial therapy in trauma patients could potentially be harmful by unnecessarily prolonging exposure to antibiotics," Dr. Nancy A. Parks said at the annual meeting of the American Association for the Surgery of Trauma. It could also lead to undertreatment, resulting in relapse, she noted.
Conventional diagnosis of ventilator-assisted pneumonia (VAP) has been based on a CPIS of 6 or higher, but her 6-year study of 1,028 critically ill patients diagnosed with VAP showed resolution of VAP in patients with higher CPIS scores.
Dr. Parks, of the Elvis Presley Memorial Trauma Center in Memphis, cited previously published work that questioned the ability of the CPIS to help differentiate the infection of VAP from posttraumatic systemic inflammatory response syndrome (J. Trauma 2006;60:523-8). While this study explored the efficacy of CPIS for initiating antibiotic therapy, it left unanswered the question of whether CPIS could help determine when to end therapy.
Dr. Parks and her coinvestigators answered that in the negative.
Their protocol to confirm VAP involved using bronchoscopy with bronchoalveolar lavage (BAL) in patients with a clinical suspicion of VAP based on three of four elements in the CPIS: body temperature, white cell count, purulent secretions, or new or changing infiltrate on chest x-ray. The investigators started patients on antibiotics empirically, then adjusted treatment if BAL effluent was 105 colony-forming units (CFU) per milliliter or higher. The investigators considered VAP resolved if repeat BAL showed a reading of 103 CFU/mL or less on day 4 of therapy. If repeat BAL was done within 2 weeks, they considered any findings greater than 105 CFU/mL as a recurrence.
The study population, which had an average Injury Severity Score of 31 and an average base deficit of 4.4, was composed primarily of blunt trauma patients, Dr. Parks reported. Overall mortality was 9.4%. Slightly more than half of the patients had community-acquired pathogens (50% methicillin-sensitive Staphylococcus aureus [MSSA], the remainder split between streptococcus and haemophilus), and slightly fewer had hospital-acquired infections (including about 19% methicillin-resistant Staphylococcus aureus [MRSA] and 27% pseudomonas). The recurrence rate was 1% overall.
A CPIS score of 6 or greater is considered positive for VAP, but this study showed resolution of VAP at CPIS scores above that. "The average CPIS on discontinuation of antibiotics was 6.9 in the community-acquired group and 6.3 in the hospital-acquired group – both well above our clinical cutoff of 6," Dr. Parks said.
"If we had used CPIS to guide treatment, we would have seen a sensitivity of 69% in our community-acquired group and 72% in our hospital-acquired group," Dr. Parks said. "Specificity would have been 51% and 53%, respectively. Our positive predictive value was 59% and 61%, and negative predictive value 62% and 66%. If we were to use CPIS to guide therapy, 59% of our patients would have had antibiotics continued inappropriately."
"This disparity – that CPIS may be potentially beneficial and useful in medical patients but not in trauma patients – is very important," said Dr. Lena Napolitano, a discussant at the meeting. "It will have important implications, particularly as we strive nationally to modify the definition of VAP and optimize duration of microbial therapy for VAP, hoping to move toward more short-term antimicrobial therapy and hopefully not lead to greater prevalence of recurrent pneumonia," said Dr. Napolitano, of the University of Michigan, Ann Arbor.
Dr. Parks had no disclosures, and the study received no outside funding.
CHICAGO – Use of the Clinical Pulmonary Infection Score to guide therapy for ventilator-associated pneumonia in critically ill patients has had mixed results, and a recent study has raised further questions about whether CPIS can accurately determine resolution of the infection in critically injured trauma ICU patients.
"Using CPIS to determine the appropriate duration of antimicrobial therapy in trauma patients could potentially be harmful by unnecessarily prolonging exposure to antibiotics," Dr. Nancy A. Parks said at the annual meeting of the American Association for the Surgery of Trauma. It could also lead to undertreatment, resulting in relapse, she noted.
Conventional diagnosis of ventilator-assisted pneumonia (VAP) has been based on a CPIS of 6 or higher, but her 6-year study of 1,028 critically ill patients diagnosed with VAP showed resolution of VAP in patients with higher CPIS scores.
Dr. Parks, of the Elvis Presley Memorial Trauma Center in Memphis, cited previously published work that questioned the ability of the CPIS to help differentiate the infection of VAP from posttraumatic systemic inflammatory response syndrome (J. Trauma 2006;60:523-8). While this study explored the efficacy of CPIS for initiating antibiotic therapy, it left unanswered the question of whether CPIS could help determine when to end therapy.
Dr. Parks and her coinvestigators answered that in the negative.
Their protocol to confirm VAP involved using bronchoscopy with bronchoalveolar lavage (BAL) in patients with a clinical suspicion of VAP based on three of four elements in the CPIS: body temperature, white cell count, purulent secretions, or new or changing infiltrate on chest x-ray. The investigators started patients on antibiotics empirically, then adjusted treatment if BAL effluent was 105 colony-forming units (CFU) per milliliter or higher. The investigators considered VAP resolved if repeat BAL showed a reading of 103 CFU/mL or less on day 4 of therapy. If repeat BAL was done within 2 weeks, they considered any findings greater than 105 CFU/mL as a recurrence.
The study population, which had an average Injury Severity Score of 31 and an average base deficit of 4.4, was composed primarily of blunt trauma patients, Dr. Parks reported. Overall mortality was 9.4%. Slightly more than half of the patients had community-acquired pathogens (50% methicillin-sensitive Staphylococcus aureus [MSSA], the remainder split between streptococcus and haemophilus), and slightly fewer had hospital-acquired infections (including about 19% methicillin-resistant Staphylococcus aureus [MRSA] and 27% pseudomonas). The recurrence rate was 1% overall.
A CPIS score of 6 or greater is considered positive for VAP, but this study showed resolution of VAP at CPIS scores above that. "The average CPIS on discontinuation of antibiotics was 6.9 in the community-acquired group and 6.3 in the hospital-acquired group – both well above our clinical cutoff of 6," Dr. Parks said.
"If we had used CPIS to guide treatment, we would have seen a sensitivity of 69% in our community-acquired group and 72% in our hospital-acquired group," Dr. Parks said. "Specificity would have been 51% and 53%, respectively. Our positive predictive value was 59% and 61%, and negative predictive value 62% and 66%. If we were to use CPIS to guide therapy, 59% of our patients would have had antibiotics continued inappropriately."
"This disparity – that CPIS may be potentially beneficial and useful in medical patients but not in trauma patients – is very important," said Dr. Lena Napolitano, a discussant at the meeting. "It will have important implications, particularly as we strive nationally to modify the definition of VAP and optimize duration of microbial therapy for VAP, hoping to move toward more short-term antimicrobial therapy and hopefully not lead to greater prevalence of recurrent pneumonia," said Dr. Napolitano, of the University of Michigan, Ann Arbor.
Dr. Parks had no disclosures, and the study received no outside funding.
CHICAGO – Use of the Clinical Pulmonary Infection Score to guide therapy for ventilator-associated pneumonia in critically ill patients has had mixed results, and a recent study has raised further questions about whether CPIS can accurately determine resolution of the infection in critically injured trauma ICU patients.
"Using CPIS to determine the appropriate duration of antimicrobial therapy in trauma patients could potentially be harmful by unnecessarily prolonging exposure to antibiotics," Dr. Nancy A. Parks said at the annual meeting of the American Association for the Surgery of Trauma. It could also lead to undertreatment, resulting in relapse, she noted.
Conventional diagnosis of ventilator-assisted pneumonia (VAP) has been based on a CPIS of 6 or higher, but her 6-year study of 1,028 critically ill patients diagnosed with VAP showed resolution of VAP in patients with higher CPIS scores.
Dr. Parks, of the Elvis Presley Memorial Trauma Center in Memphis, cited previously published work that questioned the ability of the CPIS to help differentiate the infection of VAP from posttraumatic systemic inflammatory response syndrome (J. Trauma 2006;60:523-8). While this study explored the efficacy of CPIS for initiating antibiotic therapy, it left unanswered the question of whether CPIS could help determine when to end therapy.
Dr. Parks and her coinvestigators answered that in the negative.
Their protocol to confirm VAP involved using bronchoscopy with bronchoalveolar lavage (BAL) in patients with a clinical suspicion of VAP based on three of four elements in the CPIS: body temperature, white cell count, purulent secretions, or new or changing infiltrate on chest x-ray. The investigators started patients on antibiotics empirically, then adjusted treatment if BAL effluent was 105 colony-forming units (CFU) per milliliter or higher. The investigators considered VAP resolved if repeat BAL showed a reading of 103 CFU/mL or less on day 4 of therapy. If repeat BAL was done within 2 weeks, they considered any findings greater than 105 CFU/mL as a recurrence.
The study population, which had an average Injury Severity Score of 31 and an average base deficit of 4.4, was composed primarily of blunt trauma patients, Dr. Parks reported. Overall mortality was 9.4%. Slightly more than half of the patients had community-acquired pathogens (50% methicillin-sensitive Staphylococcus aureus [MSSA], the remainder split between streptococcus and haemophilus), and slightly fewer had hospital-acquired infections (including about 19% methicillin-resistant Staphylococcus aureus [MRSA] and 27% pseudomonas). The recurrence rate was 1% overall.
A CPIS score of 6 or greater is considered positive for VAP, but this study showed resolution of VAP at CPIS scores above that. "The average CPIS on discontinuation of antibiotics was 6.9 in the community-acquired group and 6.3 in the hospital-acquired group – both well above our clinical cutoff of 6," Dr. Parks said.
"If we had used CPIS to guide treatment, we would have seen a sensitivity of 69% in our community-acquired group and 72% in our hospital-acquired group," Dr. Parks said. "Specificity would have been 51% and 53%, respectively. Our positive predictive value was 59% and 61%, and negative predictive value 62% and 66%. If we were to use CPIS to guide therapy, 59% of our patients would have had antibiotics continued inappropriately."
"This disparity – that CPIS may be potentially beneficial and useful in medical patients but not in trauma patients – is very important," said Dr. Lena Napolitano, a discussant at the meeting. "It will have important implications, particularly as we strive nationally to modify the definition of VAP and optimize duration of microbial therapy for VAP, hoping to move toward more short-term antimicrobial therapy and hopefully not lead to greater prevalence of recurrent pneumonia," said Dr. Napolitano, of the University of Michigan, Ann Arbor.
Dr. Parks had no disclosures, and the study received no outside funding.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THE SURGERY OF TRAUMA
Are Benchmarks the Problem for High VAP Rates?
CHICAGO – Payers are relying ever more on tying physician and hospital payments to quality measures, but what happens if the benchmarks they use vary among institutions or are flawed? Such may be the case with ventilator-associated pneumonia and large trauma centers, as a recent study shows VAP rates at such facilities exceed national benchmarks, which some say are inadequate for comparison.
Dr. Christopher P. Michetti of Inova Fairfax Hospital in Falls Church, Va., presented a retrospective study designed to determine VAP rates at major trauma centers and to lay groundwork for more accurate benchmarking that relies less on National Health Safety Network data, he said. He spoke at the annual meeting of the American Association for Surgery in Trauma. The study was performed through the AAST Multi-Institutional Trials Committee.
"Hospitals are under pressure to reduce their VAP rates, yet a direct association between VAP rates and quality of care or outcomes has not been demonstrated," he remarked.
"VAP rates ...are remarkably variable," Dr. Michetti said. "It is not appropriate to measure all trauma centers against a single benchmark, nor does an actual benchmark appear to exist at this point." Comparing VAP rates between different trauma centers is "like comparing apples and oranges," he said.
The study looked at VAP rates at 47 level I and II trauma centers for 2008 and 2009 with an average of 3,000 trauma evaluations a year. The average VAP rate for the study group was 17.2/1,000 ventilator days, compared with 8.1/1,000 for NHSN data. "In fact, the 90th-percentile rate for NHSN was still below the mean rate from our study," Dr. Michetti said. Across all 47 centers in the study, VAP rates ranged from a low of 1.8/1,000 ventilator days to a high of 57.6/1,000 ventilator days.
The case mix at the trauma centers did not auger well for lower VAP rates, as 88% of the cases were blunt trauma, Dr. Michetti noted. "VAP rates are generally higher for blunt-trauma patients, at about 17/1,000 ventilator days, compared with penetrating trauma at 11/1,000," he said.
Most other variables among the centers in the study – such as having a closed or open ICU, or using a bacteriologic vs. a clinical strategy to diagnose VAP – showed little impact on the pneumonia rates. VAP rates did not correlate with the size or level of trauma center, injury severity or type of ICU, he said.
Among the problems he noted with the NHSN data on VAP rates are the lack of source hospital identification, population risk, or injury severity stratification. "In addition, the NHSN rates are substantially lower than other published rates among trauma patients," he said.
However, the investigators did isolate a few variables that may influence VAP rates: Among centers where the trauma service alone made the diagnosis, the average VAP rate was 27.5/1,000 ventilator days. When the infection control, quality, or epidemiology department made the call, the average VAP rate was 11.9/1,000 days. Centers that excluded patients also had rates about 30% lower than those that did not. This variability raises questions about using VAP as a quality measure, Dr. Michetti said. "Before we take that leap, diagnostic and reporting standards are necessary."
The heightened attention on VAP as a quality measure for critical care is having other implications, he said. "As pressure to reduce VAP rates grows, an increasing number of patients are being labeled as having ventilator-associated tracheobronchitis or excluded for reasons such as aspiration," he said.
Discussant Dr. Karen J. Brasel of the Medical College of Wisconsin in, Milwaukee, acknowledged the need for the study, but raised the question: "Are the benchmarks the problem, or are we the problem?"
"I think the answer is yes, both," Dr. Michetti said. "I’m not sure that an adequate benchmark exists probably because no representative sample of trauma centers has been done to set that benchmark." He noted that the CDC’s Healthcare Infection Control Practices Advisory Committee does not recommend reporting of VAP, which argues against using that as a benchmark. Meanwhile, across individual centers no reporting standards exist, "so centers can’t agree on what is VAP," Dr. Michetti said.
Dr. Michetti had no disclosures, and the study received no outside funding.
CHICAGO – Payers are relying ever more on tying physician and hospital payments to quality measures, but what happens if the benchmarks they use vary among institutions or are flawed? Such may be the case with ventilator-associated pneumonia and large trauma centers, as a recent study shows VAP rates at such facilities exceed national benchmarks, which some say are inadequate for comparison.
Dr. Christopher P. Michetti of Inova Fairfax Hospital in Falls Church, Va., presented a retrospective study designed to determine VAP rates at major trauma centers and to lay groundwork for more accurate benchmarking that relies less on National Health Safety Network data, he said. He spoke at the annual meeting of the American Association for Surgery in Trauma. The study was performed through the AAST Multi-Institutional Trials Committee.
"Hospitals are under pressure to reduce their VAP rates, yet a direct association between VAP rates and quality of care or outcomes has not been demonstrated," he remarked.
"VAP rates ...are remarkably variable," Dr. Michetti said. "It is not appropriate to measure all trauma centers against a single benchmark, nor does an actual benchmark appear to exist at this point." Comparing VAP rates between different trauma centers is "like comparing apples and oranges," he said.
The study looked at VAP rates at 47 level I and II trauma centers for 2008 and 2009 with an average of 3,000 trauma evaluations a year. The average VAP rate for the study group was 17.2/1,000 ventilator days, compared with 8.1/1,000 for NHSN data. "In fact, the 90th-percentile rate for NHSN was still below the mean rate from our study," Dr. Michetti said. Across all 47 centers in the study, VAP rates ranged from a low of 1.8/1,000 ventilator days to a high of 57.6/1,000 ventilator days.
The case mix at the trauma centers did not auger well for lower VAP rates, as 88% of the cases were blunt trauma, Dr. Michetti noted. "VAP rates are generally higher for blunt-trauma patients, at about 17/1,000 ventilator days, compared with penetrating trauma at 11/1,000," he said.
Most other variables among the centers in the study – such as having a closed or open ICU, or using a bacteriologic vs. a clinical strategy to diagnose VAP – showed little impact on the pneumonia rates. VAP rates did not correlate with the size or level of trauma center, injury severity or type of ICU, he said.
Among the problems he noted with the NHSN data on VAP rates are the lack of source hospital identification, population risk, or injury severity stratification. "In addition, the NHSN rates are substantially lower than other published rates among trauma patients," he said.
However, the investigators did isolate a few variables that may influence VAP rates: Among centers where the trauma service alone made the diagnosis, the average VAP rate was 27.5/1,000 ventilator days. When the infection control, quality, or epidemiology department made the call, the average VAP rate was 11.9/1,000 days. Centers that excluded patients also had rates about 30% lower than those that did not. This variability raises questions about using VAP as a quality measure, Dr. Michetti said. "Before we take that leap, diagnostic and reporting standards are necessary."
The heightened attention on VAP as a quality measure for critical care is having other implications, he said. "As pressure to reduce VAP rates grows, an increasing number of patients are being labeled as having ventilator-associated tracheobronchitis or excluded for reasons such as aspiration," he said.
Discussant Dr. Karen J. Brasel of the Medical College of Wisconsin in, Milwaukee, acknowledged the need for the study, but raised the question: "Are the benchmarks the problem, or are we the problem?"
"I think the answer is yes, both," Dr. Michetti said. "I’m not sure that an adequate benchmark exists probably because no representative sample of trauma centers has been done to set that benchmark." He noted that the CDC’s Healthcare Infection Control Practices Advisory Committee does not recommend reporting of VAP, which argues against using that as a benchmark. Meanwhile, across individual centers no reporting standards exist, "so centers can’t agree on what is VAP," Dr. Michetti said.
Dr. Michetti had no disclosures, and the study received no outside funding.
CHICAGO – Payers are relying ever more on tying physician and hospital payments to quality measures, but what happens if the benchmarks they use vary among institutions or are flawed? Such may be the case with ventilator-associated pneumonia and large trauma centers, as a recent study shows VAP rates at such facilities exceed national benchmarks, which some say are inadequate for comparison.
Dr. Christopher P. Michetti of Inova Fairfax Hospital in Falls Church, Va., presented a retrospective study designed to determine VAP rates at major trauma centers and to lay groundwork for more accurate benchmarking that relies less on National Health Safety Network data, he said. He spoke at the annual meeting of the American Association for Surgery in Trauma. The study was performed through the AAST Multi-Institutional Trials Committee.
"Hospitals are under pressure to reduce their VAP rates, yet a direct association between VAP rates and quality of care or outcomes has not been demonstrated," he remarked.
"VAP rates ...are remarkably variable," Dr. Michetti said. "It is not appropriate to measure all trauma centers against a single benchmark, nor does an actual benchmark appear to exist at this point." Comparing VAP rates between different trauma centers is "like comparing apples and oranges," he said.
The study looked at VAP rates at 47 level I and II trauma centers for 2008 and 2009 with an average of 3,000 trauma evaluations a year. The average VAP rate for the study group was 17.2/1,000 ventilator days, compared with 8.1/1,000 for NHSN data. "In fact, the 90th-percentile rate for NHSN was still below the mean rate from our study," Dr. Michetti said. Across all 47 centers in the study, VAP rates ranged from a low of 1.8/1,000 ventilator days to a high of 57.6/1,000 ventilator days.
The case mix at the trauma centers did not auger well for lower VAP rates, as 88% of the cases were blunt trauma, Dr. Michetti noted. "VAP rates are generally higher for blunt-trauma patients, at about 17/1,000 ventilator days, compared with penetrating trauma at 11/1,000," he said.
Most other variables among the centers in the study – such as having a closed or open ICU, or using a bacteriologic vs. a clinical strategy to diagnose VAP – showed little impact on the pneumonia rates. VAP rates did not correlate with the size or level of trauma center, injury severity or type of ICU, he said.
Among the problems he noted with the NHSN data on VAP rates are the lack of source hospital identification, population risk, or injury severity stratification. "In addition, the NHSN rates are substantially lower than other published rates among trauma patients," he said.
However, the investigators did isolate a few variables that may influence VAP rates: Among centers where the trauma service alone made the diagnosis, the average VAP rate was 27.5/1,000 ventilator days. When the infection control, quality, or epidemiology department made the call, the average VAP rate was 11.9/1,000 days. Centers that excluded patients also had rates about 30% lower than those that did not. This variability raises questions about using VAP as a quality measure, Dr. Michetti said. "Before we take that leap, diagnostic and reporting standards are necessary."
The heightened attention on VAP as a quality measure for critical care is having other implications, he said. "As pressure to reduce VAP rates grows, an increasing number of patients are being labeled as having ventilator-associated tracheobronchitis or excluded for reasons such as aspiration," he said.
Discussant Dr. Karen J. Brasel of the Medical College of Wisconsin in, Milwaukee, acknowledged the need for the study, but raised the question: "Are the benchmarks the problem, or are we the problem?"
"I think the answer is yes, both," Dr. Michetti said. "I’m not sure that an adequate benchmark exists probably because no representative sample of trauma centers has been done to set that benchmark." He noted that the CDC’s Healthcare Infection Control Practices Advisory Committee does not recommend reporting of VAP, which argues against using that as a benchmark. Meanwhile, across individual centers no reporting standards exist, "so centers can’t agree on what is VAP," Dr. Michetti said.
Dr. Michetti had no disclosures, and the study received no outside funding.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THE SURGERY OF TRAUMA
Major Finding: AAST study shows major trauma centers have higher VAP rates than do national benchmark data.
Data Source: Retrospective analysis of trauma admissions at 47 Level I and II centers sponsored by AAST Multi-Institutional Trials Committee
Disclosures: Dr. Michetti had no disclosures and the study received no outside funding.
r-TEG Test Helps Pinpoint Likelihood of PE
CHICAGO – Performing rapid thromboelastography on admission can help trauma surgeons determine which patients are at greatest risk of developing pulmonary embolism, judging by results of a study of more than 8,000 patients.
The incidence of pulmonary embolism (PE), although still below 0.5%, has more than doubled in recent years, according to a recent report using data from the National Trauma Data Bank (Ann. Surg. 2011 Aug. 24 [E-pub ahead of print]).
"Despite this increasing knowledge of risk factors, despite increasing chemoprophylaxis – we’re getting more aggressive with head injuries in starting enoxaparin and heparin, and more aggressive with our spine and solid organ injuries – despite all this, the incidence of PE is increasing," Dr. Bryan A. Cotton said at the annual meeting of the American Association for the Surgery of Trauma.
To learn whether rapid thromboelastography (r-TEG), using a maximum amplitude (mA) greater than 65 mm, could identify patients at risk of developing PE during their hospital stay, Dr. Cotton and his colleagues at the University of Texas Health Science Center in Houston evaluated the use of r-TEG upon admission to the trauma bay for 8,330 total trauma patients over an 18-month period.
"Recent data from multiple institutions have shown an increase in vascular complications following these states if the mA values and certain other portions of TEG values are elevated," Dr. Cotton said. Besides PE and venous thromboembolism (VTE), complications including stroke and postoperative MI have been shown to increase with postoperative and postinjury r-TEG values, he added.
In the Houston study, r-TEG was obtained on 2,070 consecutive trauma patients. Of those, 2.5% went on to develop PE. These patients tended to be older and were more likely to be white and more severely injured than the other patients, and to have only blunt injuries.
"We found the admission mA, which is the highest amplitude of the clot, was associated with risk of developing PE during hospital stay," Dr. Cotton said.
The median time to development of PE was 6 days (duration, 2-31 days), he noted. The investigators also analyzed other factors, and when controlling for male sex, Injury Severity Score, and age, they found that an individual with an mA greater than 65 mm at the time of admission had a 3.5-fold greater odds of developing PE during the hospital stay, Dr. Cotton said. When they raised the threshold to an mA of 72 mm or higher, the risk profile increased sixfold, he said.
"An mA of 65 [mm] or greater is just as good as traditionally noted high-risk factors," Dr. Cotton said. "These include pelvic factures and lower extremity spine and head injuries. When mA is greater than 72 [mm], it exceeds or equals the odds ratio for very-high-risk factors such as prolonged ventilation and venous injuries."
Dr. Preston Miller of Wake Forest University in Winston-Salem, N.C., said that the study "answers some questions and creates a lot of questions as to what we’re doing in respect to PE and VTE prophylaxis in our patients." He asked whether the study accounted for intrinsic or genetic hypercoagulable states in the PE population.
"On TEG, maximal amplitude is mostly reflective of platelet activity; the elevated mA associated with pulmonary embolism may argue that platelet dysfunction is a problem," said Dr. Miller. "Does this argue for a potential role for antiplatelet agents for potential PE and thromboembolism prophylaxis in trauma patients?"
Dr. Cotton acknowledged that further studies are needed to determine whether anticoagulation protocols should be more aggressive. However, at his institution, these patients now get 30 mg of enoxaparin or 5,000 cc of heparin on admission unless they have traumatic brain injury. The investigators said the next step is to develop an algorithm and a guideline based on initiating aspirin along with enoxaparin.
Dr. Steven R. Shackford, who practices in San Diego, offered a likely explanation for the rising incidence of PE in trauma patients: "We have CT now, and instead of getting a pulmonary angiogram, we can now get a CT scan, which is much easier to get," he said.
Dr. Cotton disclosed that although the study received no direct funding, he has done work for Haemonetics Corp., which markets automated blood-processing systems.
Venous thromboembolism (VTE) is a common, morbid, costly, and oftentimes fatal complication of hospitalization or trauma/surgery. Yet, proven and effective thromboprophylaxis strategies are often underutilized which has fostered regulatory initiatives to improve VTE prevention efforts. For example, current Joint Commission performance measures endorse VTE risk assessment for all patients at the time of admission. Yet, our current ability to tailor thromboprophylaxis strategies to individualized patient specific risk is limited.
Consequently, we approach VTE prevention with a “pack mentality,” initiating the same strategy for all patients who fall within broad risk groups. The concept of more tailored and personalized approaches such as individualized risk assessment methods including clinical features, genetics, results of biomarkers, and/or coagulation parameters such as rapid thromboelastography (TEG) as studied by Dr Cotton, is intriguing and could have the potential to allow for the targeting of the most aggressive prevention efforts to those at the highest risk while obviating the need for thromboprophylaxis in identified low risk patients. Yet, these tailored approaches would add complexity and may increase the cost to patient care without improving outcomes.
Only through validation of tools such as the TEG along with the completion of prospective comparative effectiveness clinical studies will we be able to determine their utility. In the meantime, as it relates to VTE prevention, clinicians should continue to ensure that VTE risk is broadly performed on all hospital admissions and that proven thromboprophylaxis strategies are delivered to those groups identified at being at increased risk.
ROBERT PENDLETON, M.D., is associate professor of medicine in the general internal medicine division at the University of Utah in Salt Lake City. He reported having no disclosures.
Venous thromboembolism (VTE) is a common, morbid, costly, and oftentimes fatal complication of hospitalization or trauma/surgery. Yet, proven and effective thromboprophylaxis strategies are often underutilized which has fostered regulatory initiatives to improve VTE prevention efforts. For example, current Joint Commission performance measures endorse VTE risk assessment for all patients at the time of admission. Yet, our current ability to tailor thromboprophylaxis strategies to individualized patient specific risk is limited.
Consequently, we approach VTE prevention with a “pack mentality,” initiating the same strategy for all patients who fall within broad risk groups. The concept of more tailored and personalized approaches such as individualized risk assessment methods including clinical features, genetics, results of biomarkers, and/or coagulation parameters such as rapid thromboelastography (TEG) as studied by Dr Cotton, is intriguing and could have the potential to allow for the targeting of the most aggressive prevention efforts to those at the highest risk while obviating the need for thromboprophylaxis in identified low risk patients. Yet, these tailored approaches would add complexity and may increase the cost to patient care without improving outcomes.
Only through validation of tools such as the TEG along with the completion of prospective comparative effectiveness clinical studies will we be able to determine their utility. In the meantime, as it relates to VTE prevention, clinicians should continue to ensure that VTE risk is broadly performed on all hospital admissions and that proven thromboprophylaxis strategies are delivered to those groups identified at being at increased risk.
ROBERT PENDLETON, M.D., is associate professor of medicine in the general internal medicine division at the University of Utah in Salt Lake City. He reported having no disclosures.
Venous thromboembolism (VTE) is a common, morbid, costly, and oftentimes fatal complication of hospitalization or trauma/surgery. Yet, proven and effective thromboprophylaxis strategies are often underutilized which has fostered regulatory initiatives to improve VTE prevention efforts. For example, current Joint Commission performance measures endorse VTE risk assessment for all patients at the time of admission. Yet, our current ability to tailor thromboprophylaxis strategies to individualized patient specific risk is limited.
Consequently, we approach VTE prevention with a “pack mentality,” initiating the same strategy for all patients who fall within broad risk groups. The concept of more tailored and personalized approaches such as individualized risk assessment methods including clinical features, genetics, results of biomarkers, and/or coagulation parameters such as rapid thromboelastography (TEG) as studied by Dr Cotton, is intriguing and could have the potential to allow for the targeting of the most aggressive prevention efforts to those at the highest risk while obviating the need for thromboprophylaxis in identified low risk patients. Yet, these tailored approaches would add complexity and may increase the cost to patient care without improving outcomes.
Only through validation of tools such as the TEG along with the completion of prospective comparative effectiveness clinical studies will we be able to determine their utility. In the meantime, as it relates to VTE prevention, clinicians should continue to ensure that VTE risk is broadly performed on all hospital admissions and that proven thromboprophylaxis strategies are delivered to those groups identified at being at increased risk.
ROBERT PENDLETON, M.D., is associate professor of medicine in the general internal medicine division at the University of Utah in Salt Lake City. He reported having no disclosures.
CHICAGO – Performing rapid thromboelastography on admission can help trauma surgeons determine which patients are at greatest risk of developing pulmonary embolism, judging by results of a study of more than 8,000 patients.
The incidence of pulmonary embolism (PE), although still below 0.5%, has more than doubled in recent years, according to a recent report using data from the National Trauma Data Bank (Ann. Surg. 2011 Aug. 24 [E-pub ahead of print]).
"Despite this increasing knowledge of risk factors, despite increasing chemoprophylaxis – we’re getting more aggressive with head injuries in starting enoxaparin and heparin, and more aggressive with our spine and solid organ injuries – despite all this, the incidence of PE is increasing," Dr. Bryan A. Cotton said at the annual meeting of the American Association for the Surgery of Trauma.
To learn whether rapid thromboelastography (r-TEG), using a maximum amplitude (mA) greater than 65 mm, could identify patients at risk of developing PE during their hospital stay, Dr. Cotton and his colleagues at the University of Texas Health Science Center in Houston evaluated the use of r-TEG upon admission to the trauma bay for 8,330 total trauma patients over an 18-month period.
"Recent data from multiple institutions have shown an increase in vascular complications following these states if the mA values and certain other portions of TEG values are elevated," Dr. Cotton said. Besides PE and venous thromboembolism (VTE), complications including stroke and postoperative MI have been shown to increase with postoperative and postinjury r-TEG values, he added.
In the Houston study, r-TEG was obtained on 2,070 consecutive trauma patients. Of those, 2.5% went on to develop PE. These patients tended to be older and were more likely to be white and more severely injured than the other patients, and to have only blunt injuries.
"We found the admission mA, which is the highest amplitude of the clot, was associated with risk of developing PE during hospital stay," Dr. Cotton said.
The median time to development of PE was 6 days (duration, 2-31 days), he noted. The investigators also analyzed other factors, and when controlling for male sex, Injury Severity Score, and age, they found that an individual with an mA greater than 65 mm at the time of admission had a 3.5-fold greater odds of developing PE during the hospital stay, Dr. Cotton said. When they raised the threshold to an mA of 72 mm or higher, the risk profile increased sixfold, he said.
"An mA of 65 [mm] or greater is just as good as traditionally noted high-risk factors," Dr. Cotton said. "These include pelvic factures and lower extremity spine and head injuries. When mA is greater than 72 [mm], it exceeds or equals the odds ratio for very-high-risk factors such as prolonged ventilation and venous injuries."
Dr. Preston Miller of Wake Forest University in Winston-Salem, N.C., said that the study "answers some questions and creates a lot of questions as to what we’re doing in respect to PE and VTE prophylaxis in our patients." He asked whether the study accounted for intrinsic or genetic hypercoagulable states in the PE population.
"On TEG, maximal amplitude is mostly reflective of platelet activity; the elevated mA associated with pulmonary embolism may argue that platelet dysfunction is a problem," said Dr. Miller. "Does this argue for a potential role for antiplatelet agents for potential PE and thromboembolism prophylaxis in trauma patients?"
Dr. Cotton acknowledged that further studies are needed to determine whether anticoagulation protocols should be more aggressive. However, at his institution, these patients now get 30 mg of enoxaparin or 5,000 cc of heparin on admission unless they have traumatic brain injury. The investigators said the next step is to develop an algorithm and a guideline based on initiating aspirin along with enoxaparin.
Dr. Steven R. Shackford, who practices in San Diego, offered a likely explanation for the rising incidence of PE in trauma patients: "We have CT now, and instead of getting a pulmonary angiogram, we can now get a CT scan, which is much easier to get," he said.
Dr. Cotton disclosed that although the study received no direct funding, he has done work for Haemonetics Corp., which markets automated blood-processing systems.
CHICAGO – Performing rapid thromboelastography on admission can help trauma surgeons determine which patients are at greatest risk of developing pulmonary embolism, judging by results of a study of more than 8,000 patients.
The incidence of pulmonary embolism (PE), although still below 0.5%, has more than doubled in recent years, according to a recent report using data from the National Trauma Data Bank (Ann. Surg. 2011 Aug. 24 [E-pub ahead of print]).
"Despite this increasing knowledge of risk factors, despite increasing chemoprophylaxis – we’re getting more aggressive with head injuries in starting enoxaparin and heparin, and more aggressive with our spine and solid organ injuries – despite all this, the incidence of PE is increasing," Dr. Bryan A. Cotton said at the annual meeting of the American Association for the Surgery of Trauma.
To learn whether rapid thromboelastography (r-TEG), using a maximum amplitude (mA) greater than 65 mm, could identify patients at risk of developing PE during their hospital stay, Dr. Cotton and his colleagues at the University of Texas Health Science Center in Houston evaluated the use of r-TEG upon admission to the trauma bay for 8,330 total trauma patients over an 18-month period.
"Recent data from multiple institutions have shown an increase in vascular complications following these states if the mA values and certain other portions of TEG values are elevated," Dr. Cotton said. Besides PE and venous thromboembolism (VTE), complications including stroke and postoperative MI have been shown to increase with postoperative and postinjury r-TEG values, he added.
In the Houston study, r-TEG was obtained on 2,070 consecutive trauma patients. Of those, 2.5% went on to develop PE. These patients tended to be older and were more likely to be white and more severely injured than the other patients, and to have only blunt injuries.
"We found the admission mA, which is the highest amplitude of the clot, was associated with risk of developing PE during hospital stay," Dr. Cotton said.
The median time to development of PE was 6 days (duration, 2-31 days), he noted. The investigators also analyzed other factors, and when controlling for male sex, Injury Severity Score, and age, they found that an individual with an mA greater than 65 mm at the time of admission had a 3.5-fold greater odds of developing PE during the hospital stay, Dr. Cotton said. When they raised the threshold to an mA of 72 mm or higher, the risk profile increased sixfold, he said.
"An mA of 65 [mm] or greater is just as good as traditionally noted high-risk factors," Dr. Cotton said. "These include pelvic factures and lower extremity spine and head injuries. When mA is greater than 72 [mm], it exceeds or equals the odds ratio for very-high-risk factors such as prolonged ventilation and venous injuries."
Dr. Preston Miller of Wake Forest University in Winston-Salem, N.C., said that the study "answers some questions and creates a lot of questions as to what we’re doing in respect to PE and VTE prophylaxis in our patients." He asked whether the study accounted for intrinsic or genetic hypercoagulable states in the PE population.
"On TEG, maximal amplitude is mostly reflective of platelet activity; the elevated mA associated with pulmonary embolism may argue that platelet dysfunction is a problem," said Dr. Miller. "Does this argue for a potential role for antiplatelet agents for potential PE and thromboembolism prophylaxis in trauma patients?"
Dr. Cotton acknowledged that further studies are needed to determine whether anticoagulation protocols should be more aggressive. However, at his institution, these patients now get 30 mg of enoxaparin or 5,000 cc of heparin on admission unless they have traumatic brain injury. The investigators said the next step is to develop an algorithm and a guideline based on initiating aspirin along with enoxaparin.
Dr. Steven R. Shackford, who practices in San Diego, offered a likely explanation for the rising incidence of PE in trauma patients: "We have CT now, and instead of getting a pulmonary angiogram, we can now get a CT scan, which is much easier to get," he said.
Dr. Cotton disclosed that although the study received no direct funding, he has done work for Haemonetics Corp., which markets automated blood-processing systems.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THE SURGERY OF TRAUMA
Observation Period for Gunshot Wounds Clarified
CHICAGO – Nonoperative management of gunshot wounds has become an accepted practice at many trauma centers despite a slightly heightened risk of complications, but the time frame for safe discharge of these patients is still uncertain.
The minimum seems to be 24 hours, according to Dr. Kenji Inaba, the lead investigator of a prospective trial from the University of Southern California in Los Angeles. Defining an appropriate observation period for nonoperative management is important, he said, "because we can expect that up to 6.2% of these patients will require delayed laparotomy." He described nonoperative management as a "resource-intensive process requiring serial examinations and serial laboratory evaluations."
At the annual meeting of the American Association for Surgery in Trauma, Dr. Inaba presented results for 270 patients who sustained torso gunshot wounds (GSW) over a 2-year period. Of those, 25 (9.3%) died in the emergency department, leaving 245 for analysis. All subjects were aged 15 years or older.
The prospective results he presented are the second phase of his group’s research. Last year, the researchers published a retrospective study of 787 patients. Of the 636 patients who underwent a trial of nonoperative management in that study, 4.6% of patients failed and had to undergo laparotomy (J. Trauma 2010;68:1301-4). Of the 4.6% patients who had laparotomy, 97% had failed nonoperative management within 12 hours, and the rest failed within 24 hours.
Avoiding nontherapeutic laparotomy is noteworthy, he said, because it has been associated with complication rates ranging from 9% to 26%. The goal of the prospective study was to validate this observation period, he said.
The protocol for the prospective study indicated surgery for GSW victims who were unstable or eviscerated, could not be evaluated, or had peritonitis – 115 in all. The remaining 130 patients got a CT scan. Of those, 39 (30%) had positive findings: mostly hollow-viscus injuries, followed by solid-organ injury, vascular injury, and bladder injuries, according to Dr. Inaba of the department of surgery at USC. These patients had surgery. Among the remaining patients who got a CT scan, 44 (34%) had a negative scan and 47 (36%) had an equivocal finding. All patients in the latter two groups were put under observation.
The CT scans were read by the resident on call and checked for concordance with a radiologist, Dr Inaba said; discordant findings did not impact clinical management.
Among those who had a negative or equivocal CT scan, about 9% (all of whom had equivocal findings on CT) went for laparotomy later on, Dr. Inaba said. The most common earliest sign of failure was tachycardia; the most common latest sign was peritonitis, Dr. Inaba said.
In all, 75% of the surgical procedures were therapeutic. Among the patients who had therapeutic laparotomy, the operation revealed injuries of the stomach, colon, and rectum. The mean time for proceeding to laparotomy was 2 hours 43 minutes, according to Dr. Inaba, with 50% having failed nonoperative management by 6 hours, 75% by 12 hours, and 100% by 24 hours.
"According to this study, the clinical examination was seen yet again to very effectively identify those with gunshot wounds that required an immediate trip to the OR," Dr. Inaba said. "For all other remaining patients who didn’t go immediately to the OR, the CT was of value. If CT was positive, there was very high yield for taking that trip to the OR. If it was negative, it was very unlikely there would’ve been a missed injury."
For those with an equivocal CT scan, observation was "very important," Dr. Inaba said, because it was key for eventually distinguishing who needed laparotomy. "We feel it’s important that [at a minimum] these patients be watched for at least 24 hours before they are safely discharged home," he said.
Dr. Timothy C. Fabian of the University of Tennessee, Memphis, questioned the rigor of follow-up after discharge. "Follow-up is extremely important in order to completely put nonoperative management into perspective," he said.
Dr. Peter Rhee of the University of Arizona, Tucson, echoed that concern: "When I worked in Los Angeles for 5 years, follow-up was nonexistent," he said. "Of the people you didn’t operate on, were you able to state [definitively that] they had no injuries?"
Dr. Inaba acknowledged that the follow-up was problematic, as the investigators had no data on what happened to these patients after discharge.
Dr. Inaba had no disclosures to report.
CHICAGO – Nonoperative management of gunshot wounds has become an accepted practice at many trauma centers despite a slightly heightened risk of complications, but the time frame for safe discharge of these patients is still uncertain.
The minimum seems to be 24 hours, according to Dr. Kenji Inaba, the lead investigator of a prospective trial from the University of Southern California in Los Angeles. Defining an appropriate observation period for nonoperative management is important, he said, "because we can expect that up to 6.2% of these patients will require delayed laparotomy." He described nonoperative management as a "resource-intensive process requiring serial examinations and serial laboratory evaluations."
At the annual meeting of the American Association for Surgery in Trauma, Dr. Inaba presented results for 270 patients who sustained torso gunshot wounds (GSW) over a 2-year period. Of those, 25 (9.3%) died in the emergency department, leaving 245 for analysis. All subjects were aged 15 years or older.
The prospective results he presented are the second phase of his group’s research. Last year, the researchers published a retrospective study of 787 patients. Of the 636 patients who underwent a trial of nonoperative management in that study, 4.6% of patients failed and had to undergo laparotomy (J. Trauma 2010;68:1301-4). Of the 4.6% patients who had laparotomy, 97% had failed nonoperative management within 12 hours, and the rest failed within 24 hours.
Avoiding nontherapeutic laparotomy is noteworthy, he said, because it has been associated with complication rates ranging from 9% to 26%. The goal of the prospective study was to validate this observation period, he said.
The protocol for the prospective study indicated surgery for GSW victims who were unstable or eviscerated, could not be evaluated, or had peritonitis – 115 in all. The remaining 130 patients got a CT scan. Of those, 39 (30%) had positive findings: mostly hollow-viscus injuries, followed by solid-organ injury, vascular injury, and bladder injuries, according to Dr. Inaba of the department of surgery at USC. These patients had surgery. Among the remaining patients who got a CT scan, 44 (34%) had a negative scan and 47 (36%) had an equivocal finding. All patients in the latter two groups were put under observation.
The CT scans were read by the resident on call and checked for concordance with a radiologist, Dr Inaba said; discordant findings did not impact clinical management.
Among those who had a negative or equivocal CT scan, about 9% (all of whom had equivocal findings on CT) went for laparotomy later on, Dr. Inaba said. The most common earliest sign of failure was tachycardia; the most common latest sign was peritonitis, Dr. Inaba said.
In all, 75% of the surgical procedures were therapeutic. Among the patients who had therapeutic laparotomy, the operation revealed injuries of the stomach, colon, and rectum. The mean time for proceeding to laparotomy was 2 hours 43 minutes, according to Dr. Inaba, with 50% having failed nonoperative management by 6 hours, 75% by 12 hours, and 100% by 24 hours.
"According to this study, the clinical examination was seen yet again to very effectively identify those with gunshot wounds that required an immediate trip to the OR," Dr. Inaba said. "For all other remaining patients who didn’t go immediately to the OR, the CT was of value. If CT was positive, there was very high yield for taking that trip to the OR. If it was negative, it was very unlikely there would’ve been a missed injury."
For those with an equivocal CT scan, observation was "very important," Dr. Inaba said, because it was key for eventually distinguishing who needed laparotomy. "We feel it’s important that [at a minimum] these patients be watched for at least 24 hours before they are safely discharged home," he said.
Dr. Timothy C. Fabian of the University of Tennessee, Memphis, questioned the rigor of follow-up after discharge. "Follow-up is extremely important in order to completely put nonoperative management into perspective," he said.
Dr. Peter Rhee of the University of Arizona, Tucson, echoed that concern: "When I worked in Los Angeles for 5 years, follow-up was nonexistent," he said. "Of the people you didn’t operate on, were you able to state [definitively that] they had no injuries?"
Dr. Inaba acknowledged that the follow-up was problematic, as the investigators had no data on what happened to these patients after discharge.
Dr. Inaba had no disclosures to report.
CHICAGO – Nonoperative management of gunshot wounds has become an accepted practice at many trauma centers despite a slightly heightened risk of complications, but the time frame for safe discharge of these patients is still uncertain.
The minimum seems to be 24 hours, according to Dr. Kenji Inaba, the lead investigator of a prospective trial from the University of Southern California in Los Angeles. Defining an appropriate observation period for nonoperative management is important, he said, "because we can expect that up to 6.2% of these patients will require delayed laparotomy." He described nonoperative management as a "resource-intensive process requiring serial examinations and serial laboratory evaluations."
At the annual meeting of the American Association for Surgery in Trauma, Dr. Inaba presented results for 270 patients who sustained torso gunshot wounds (GSW) over a 2-year period. Of those, 25 (9.3%) died in the emergency department, leaving 245 for analysis. All subjects were aged 15 years or older.
The prospective results he presented are the second phase of his group’s research. Last year, the researchers published a retrospective study of 787 patients. Of the 636 patients who underwent a trial of nonoperative management in that study, 4.6% of patients failed and had to undergo laparotomy (J. Trauma 2010;68:1301-4). Of the 4.6% patients who had laparotomy, 97% had failed nonoperative management within 12 hours, and the rest failed within 24 hours.
Avoiding nontherapeutic laparotomy is noteworthy, he said, because it has been associated with complication rates ranging from 9% to 26%. The goal of the prospective study was to validate this observation period, he said.
The protocol for the prospective study indicated surgery for GSW victims who were unstable or eviscerated, could not be evaluated, or had peritonitis – 115 in all. The remaining 130 patients got a CT scan. Of those, 39 (30%) had positive findings: mostly hollow-viscus injuries, followed by solid-organ injury, vascular injury, and bladder injuries, according to Dr. Inaba of the department of surgery at USC. These patients had surgery. Among the remaining patients who got a CT scan, 44 (34%) had a negative scan and 47 (36%) had an equivocal finding. All patients in the latter two groups were put under observation.
The CT scans were read by the resident on call and checked for concordance with a radiologist, Dr Inaba said; discordant findings did not impact clinical management.
Among those who had a negative or equivocal CT scan, about 9% (all of whom had equivocal findings on CT) went for laparotomy later on, Dr. Inaba said. The most common earliest sign of failure was tachycardia; the most common latest sign was peritonitis, Dr. Inaba said.
In all, 75% of the surgical procedures were therapeutic. Among the patients who had therapeutic laparotomy, the operation revealed injuries of the stomach, colon, and rectum. The mean time for proceeding to laparotomy was 2 hours 43 minutes, according to Dr. Inaba, with 50% having failed nonoperative management by 6 hours, 75% by 12 hours, and 100% by 24 hours.
"According to this study, the clinical examination was seen yet again to very effectively identify those with gunshot wounds that required an immediate trip to the OR," Dr. Inaba said. "For all other remaining patients who didn’t go immediately to the OR, the CT was of value. If CT was positive, there was very high yield for taking that trip to the OR. If it was negative, it was very unlikely there would’ve been a missed injury."
For those with an equivocal CT scan, observation was "very important," Dr. Inaba said, because it was key for eventually distinguishing who needed laparotomy. "We feel it’s important that [at a minimum] these patients be watched for at least 24 hours before they are safely discharged home," he said.
Dr. Timothy C. Fabian of the University of Tennessee, Memphis, questioned the rigor of follow-up after discharge. "Follow-up is extremely important in order to completely put nonoperative management into perspective," he said.
Dr. Peter Rhee of the University of Arizona, Tucson, echoed that concern: "When I worked in Los Angeles for 5 years, follow-up was nonexistent," he said. "Of the people you didn’t operate on, were you able to state [definitively that] they had no injuries?"
Dr. Inaba acknowledged that the follow-up was problematic, as the investigators had no data on what happened to these patients after discharge.
Dr. Inaba had no disclosures to report.
FROM THE ANNUAL MEETING OF THE AMERICAN ASSOCIATION FOR THE SURGERY OF TRAUMA
Team Care Improves Hypertension Control
NEW YORK – When it comes to getting hypertensive patients to take their medications and to achieve improvements in their blood pressures, it takes a village – or at least a really motivated pharmacist, according to Barry Carter, Pharm. D.
“Team-based care interventions are one of the most potent strategies to achieve blood pressure control, even for those patients with difficult-to-control blood pressure,” said Dr. Carter, professor and associate head for research in the department of family medicine at the University of Iowa, Iowa City. “While improving adherence is one key reason for the success,” it's also important to step-up the intensity of the medical management by increasing the number of patient encounters and the intensity of blood pressure monitoring. It's “one of the most important strategies we've seen” to help overcome “clinical inertia.”
In a 2009 systematic review of controlled clinical trials, Dr. Carter and associates showed the potency of using pharmacists and nurses in hypertension management. In studies in which the pharmacist made recommendations to the physician, there was an average reduction of 9.3 mm Hg in systolic BP, compared with settings that did not use team-based care (Arch. Intern. Med. 2009;169:1748-55).
By comparison, in studies in which the nurse did the intervention, the reduction in systolic blood pressure was 4.8 mm Hg greater than in the non–team-based care. Both results were statistically significant, he said at the meeting. (See graph.)
Home-based blood pressure monitoring in other studies and systematic reviews showed an average blood pressure reduction of 2.4 mm Hg, according to Dr. Carter. “When added to team-based care, home-based blood pressure monitoring is much more effective than home monitoring alone,” he said.
Dr. Carter also commented on preliminary results from HINTS (Hypertension Intervention Nurse Telemedicine Study). This Veterans Affairs study involved four arms: a control group that received usual care, nurse-administered behavioral intervention, nurse-administered medication management, and a combination of the nurse-administered behavioral and medical management interventions.
“The proportion achieving blood pressure control at 12 months started out around 59%, and in the intervention groups it was near 70%,” Dr. Carter said. But by 18 months, the between-group differences had tapered off (Am. Heart J. 2009;157:450-6). A limitation of the study is that about half the patients had uncontrolled blood pressure when they entered the trial. “There was a statistically significant improvement in the odds ratio of blood pressure being controlled with nurse management,” Dr. Carter added.
A 2008 study of 778 patients showed that adding Web-based pharmacist care to a protocol of home blood pressure monitoring and Web training significantly increased the percentage of patients with controlled blood pressure (JAMA 2008;299: 2857-67).
At baseline, all patients had systolic BPs in the low 150–mm Hg range, he said. After 12 months, the usual-care arm had an average reduction in systolic blood pressure of 5 mm Hg, and the arm with home blood pressure monitoring and patient interaction via the Web showed an average reduction of 8 mm Hg. By contrast, the group that received home-based monitoring and Web-based assistance by the pharmacist had an average reduction in systolic blood pressure of 14 mm Hg, he said.
Reimbursement issues are among the most significant barriers to a team-based approach for hypertension management, Dr. Carter acknowledged. “The business model has really been a critical problem,” he said. “The reason the Kaiser-Permanentes, Group Health, and the VAs can do this is because they don't operate on a fee-for-service model.” Although Medicare Part D allows for team-based management of hypertension, Medicare itself has not yet completed a relative-value unit for the service, he said.
Dr. Carter is currently leading the CAPTION (Collaboration Among Pharmacists and Physicians to Improve Outcomes Now) trial, the purpose of which is to determine if the face-to-face physician-pharmacist collaborative model will be adopted in typical practice settings, funded by the National Institutes of Health.
Dr. Carter had no relevant conflicts of interest.
'When added to team-based care, home-based [BP] monitoring is much more effective than home monitoring alone.'
Source Dr. carter
Source Elsevier Global Medical News
NEW YORK – When it comes to getting hypertensive patients to take their medications and to achieve improvements in their blood pressures, it takes a village – or at least a really motivated pharmacist, according to Barry Carter, Pharm. D.
“Team-based care interventions are one of the most potent strategies to achieve blood pressure control, even for those patients with difficult-to-control blood pressure,” said Dr. Carter, professor and associate head for research in the department of family medicine at the University of Iowa, Iowa City. “While improving adherence is one key reason for the success,” it's also important to step-up the intensity of the medical management by increasing the number of patient encounters and the intensity of blood pressure monitoring. It's “one of the most important strategies we've seen” to help overcome “clinical inertia.”
In a 2009 systematic review of controlled clinical trials, Dr. Carter and associates showed the potency of using pharmacists and nurses in hypertension management. In studies in which the pharmacist made recommendations to the physician, there was an average reduction of 9.3 mm Hg in systolic BP, compared with settings that did not use team-based care (Arch. Intern. Med. 2009;169:1748-55).
By comparison, in studies in which the nurse did the intervention, the reduction in systolic blood pressure was 4.8 mm Hg greater than in the non–team-based care. Both results were statistically significant, he said at the meeting. (See graph.)
Home-based blood pressure monitoring in other studies and systematic reviews showed an average blood pressure reduction of 2.4 mm Hg, according to Dr. Carter. “When added to team-based care, home-based blood pressure monitoring is much more effective than home monitoring alone,” he said.
Dr. Carter also commented on preliminary results from HINTS (Hypertension Intervention Nurse Telemedicine Study). This Veterans Affairs study involved four arms: a control group that received usual care, nurse-administered behavioral intervention, nurse-administered medication management, and a combination of the nurse-administered behavioral and medical management interventions.
“The proportion achieving blood pressure control at 12 months started out around 59%, and in the intervention groups it was near 70%,” Dr. Carter said. But by 18 months, the between-group differences had tapered off (Am. Heart J. 2009;157:450-6). A limitation of the study is that about half the patients had uncontrolled blood pressure when they entered the trial. “There was a statistically significant improvement in the odds ratio of blood pressure being controlled with nurse management,” Dr. Carter added.
A 2008 study of 778 patients showed that adding Web-based pharmacist care to a protocol of home blood pressure monitoring and Web training significantly increased the percentage of patients with controlled blood pressure (JAMA 2008;299: 2857-67).
At baseline, all patients had systolic BPs in the low 150–mm Hg range, he said. After 12 months, the usual-care arm had an average reduction in systolic blood pressure of 5 mm Hg, and the arm with home blood pressure monitoring and patient interaction via the Web showed an average reduction of 8 mm Hg. By contrast, the group that received home-based monitoring and Web-based assistance by the pharmacist had an average reduction in systolic blood pressure of 14 mm Hg, he said.
Reimbursement issues are among the most significant barriers to a team-based approach for hypertension management, Dr. Carter acknowledged. “The business model has really been a critical problem,” he said. “The reason the Kaiser-Permanentes, Group Health, and the VAs can do this is because they don't operate on a fee-for-service model.” Although Medicare Part D allows for team-based management of hypertension, Medicare itself has not yet completed a relative-value unit for the service, he said.
Dr. Carter is currently leading the CAPTION (Collaboration Among Pharmacists and Physicians to Improve Outcomes Now) trial, the purpose of which is to determine if the face-to-face physician-pharmacist collaborative model will be adopted in typical practice settings, funded by the National Institutes of Health.
Dr. Carter had no relevant conflicts of interest.
'When added to team-based care, home-based [BP] monitoring is much more effective than home monitoring alone.'
Source Dr. carter
Source Elsevier Global Medical News
NEW YORK – When it comes to getting hypertensive patients to take their medications and to achieve improvements in their blood pressures, it takes a village – or at least a really motivated pharmacist, according to Barry Carter, Pharm. D.
“Team-based care interventions are one of the most potent strategies to achieve blood pressure control, even for those patients with difficult-to-control blood pressure,” said Dr. Carter, professor and associate head for research in the department of family medicine at the University of Iowa, Iowa City. “While improving adherence is one key reason for the success,” it's also important to step-up the intensity of the medical management by increasing the number of patient encounters and the intensity of blood pressure monitoring. It's “one of the most important strategies we've seen” to help overcome “clinical inertia.”
In a 2009 systematic review of controlled clinical trials, Dr. Carter and associates showed the potency of using pharmacists and nurses in hypertension management. In studies in which the pharmacist made recommendations to the physician, there was an average reduction of 9.3 mm Hg in systolic BP, compared with settings that did not use team-based care (Arch. Intern. Med. 2009;169:1748-55).
By comparison, in studies in which the nurse did the intervention, the reduction in systolic blood pressure was 4.8 mm Hg greater than in the non–team-based care. Both results were statistically significant, he said at the meeting. (See graph.)
Home-based blood pressure monitoring in other studies and systematic reviews showed an average blood pressure reduction of 2.4 mm Hg, according to Dr. Carter. “When added to team-based care, home-based blood pressure monitoring is much more effective than home monitoring alone,” he said.
Dr. Carter also commented on preliminary results from HINTS (Hypertension Intervention Nurse Telemedicine Study). This Veterans Affairs study involved four arms: a control group that received usual care, nurse-administered behavioral intervention, nurse-administered medication management, and a combination of the nurse-administered behavioral and medical management interventions.
“The proportion achieving blood pressure control at 12 months started out around 59%, and in the intervention groups it was near 70%,” Dr. Carter said. But by 18 months, the between-group differences had tapered off (Am. Heart J. 2009;157:450-6). A limitation of the study is that about half the patients had uncontrolled blood pressure when they entered the trial. “There was a statistically significant improvement in the odds ratio of blood pressure being controlled with nurse management,” Dr. Carter added.
A 2008 study of 778 patients showed that adding Web-based pharmacist care to a protocol of home blood pressure monitoring and Web training significantly increased the percentage of patients with controlled blood pressure (JAMA 2008;299: 2857-67).
At baseline, all patients had systolic BPs in the low 150–mm Hg range, he said. After 12 months, the usual-care arm had an average reduction in systolic blood pressure of 5 mm Hg, and the arm with home blood pressure monitoring and patient interaction via the Web showed an average reduction of 8 mm Hg. By contrast, the group that received home-based monitoring and Web-based assistance by the pharmacist had an average reduction in systolic blood pressure of 14 mm Hg, he said.
Reimbursement issues are among the most significant barriers to a team-based approach for hypertension management, Dr. Carter acknowledged. “The business model has really been a critical problem,” he said. “The reason the Kaiser-Permanentes, Group Health, and the VAs can do this is because they don't operate on a fee-for-service model.” Although Medicare Part D allows for team-based management of hypertension, Medicare itself has not yet completed a relative-value unit for the service, he said.
Dr. Carter is currently leading the CAPTION (Collaboration Among Pharmacists and Physicians to Improve Outcomes Now) trial, the purpose of which is to determine if the face-to-face physician-pharmacist collaborative model will be adopted in typical practice settings, funded by the National Institutes of Health.
Dr. Carter had no relevant conflicts of interest.
'When added to team-based care, home-based [BP] monitoring is much more effective than home monitoring alone.'
Source Dr. carter
Source Elsevier Global Medical News
KEEP Results Show Promise of New Equation
Major Finding: KEEP data have shown an uptick in overall blood pressure control among patients with early-stage kidney disease or hypertension, from 45% at the initial screening to 49% at rescreening.
Data Source: Preliminary results from the National Kidney Foundation's screening initiative.
Disclosures: KEEP is funded by Amgen, Abbott, Siemens, Astellas, Genzyme, Fresenius Medical Care, Pfizer, Nephroceuticals and the LifeScan unit of Johnson & Johnson. Panel participants disclosed affiliations with a variety of device and pharmaceutical companies.
NEW YORK – Boosting patient awareness and use of a new equation for measuring glomerular filtration rate are showing early signs of being the cornerstones to the prevention of chronic kidney disease among people at risk for the disease, according to preliminary results from the National Kidney Foundation's nationwide screening initiative.
The Kidney Early Evaluation Program (KEEP) has enrolled 150,000 people so far, making it the nation's largest perpetual chronic kidney disease screening program, according to Dr. Joseph Vassalotti, chief medical officer of the National Kidney Foundation and a faculty member at Mount Sinai School of Medicine, New York.
The point is to identify “individuals in the community with kidney disease along with the risk factors that go with it,” said Dr. George Bakris, professor of medicine at the University of Chicago Medical Center and a former KEEP principal investigator.
All of the participants have some stage of kidney disease or hypertension and are referred to the registry by physicians. Enrollment is voluntary and participants complete a questionnaire and undergo a medical evaluation that includes standard panels plus testing for calcium, phosphorus, and parathyroid hormone. The program does not accept people who have had a kidney transplant or are on dialysis, he said.
Under the program, a new method for estimating glomerular filtration rate (eGFR), known as the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation, has been used. This equation is more accurate in determining kidney function than is the Modification of Diet in Renal Disease (MDRD) Study equation, said Dr. Lesley Stevens of Tufts Medical Center, Boston.
“The use of the CKD-EPI equation more accurately reflects measured GFR and results in a lower prevalence of eGFR below 60 mL/min per 1.73 m
According to Dr. Stevens, the equation has been validated in two clinical studies (Am. J. Kidney Dis. 2010;55:648-59 and Am. J. Kidney Dis. 2010;55:660-70).
One of the goals of KEEP is to determine factors that help slow the slide into chronic kidney disease, as well as the loss of kidney function over time, Dr. Vassalotti said.
“Multiple trials on systolic blood pressure show that untreated hypertension results in a loss of 10-12 mL/min per 1.73 m
Managing blood pressure early in kidney disease is critical because as eGFR declines, hypertension becomes more difficult to control, Dr. Vassalotti said. Thus, self-reported hypertension is one of the qualifiers for KEEP enrollment, he said. He cited early data from KEEP that showed prevalence, awareness and treatment of hypertension increased with stage of chronic kidney disease, but that didn't necessarily translate to control with severe disease. Among those with stage 3 disease, only 82% were undergoing treatment, compared with 92% of those with stage 4 disease. However, 38% of the stage 3 group had systolic blood pressure below 140 mm Hg, while only 35% of the stage 4 group did (Am. J. Med. 2008; 121:332-40).
KEEP data have shown an uptick in overall blood pressure control, from 45% at the initial screening to 49% at rescreening, Dr. Vassalotti said, and even some improvement in control without medication. “But I wouldn't overstate this.”
The project involves merging data with the National Death Index and the United States Renal Data System to track survival and chronic kidney failure outcomes, respectively. Future goals include additional data links with Medicare Parts B and D to gain clarity on morbidity and medication use, Dr. Vassalotti said. “Preliminary longitudinal data show that community screening appears to influence hypertension despite progression of chronic kidney disease,” he said.
Patient awareness is the cornerstone of hypertension management, noted Dr. Adam Whaley-Connell of the University of Missouri. “Awareness has a very important role in not only understanding blood pressure control, especially in the context of the early stages of kidney disease, but in improving kidney related patient outcomes,” he said.
However, Dr. Whaley-Connell noted that awareness of kidney disease, particularly in its early stages, “is alarmingly low.” He noted that KEEP data on awareness reflect that of National Health and Nutrition Examination Survey and other chronic kidney disease cohort studies:
Only about 5% of those with stages 1-3 are aware of their disease. “Roughly 95% of individuals entering into the screening program are unaware they have chronic kidney disease,” Dr. Whaley-Connell said.
The point is to identify persons 'in the community with kidney disease along with the risk factors that go with it.'
Source DR. BAKRIS
'Community screening appears to influence hypertension despite progression' of CKD.
Source DR. VASSALOTTI
Major Finding: KEEP data have shown an uptick in overall blood pressure control among patients with early-stage kidney disease or hypertension, from 45% at the initial screening to 49% at rescreening.
Data Source: Preliminary results from the National Kidney Foundation's screening initiative.
Disclosures: KEEP is funded by Amgen, Abbott, Siemens, Astellas, Genzyme, Fresenius Medical Care, Pfizer, Nephroceuticals and the LifeScan unit of Johnson & Johnson. Panel participants disclosed affiliations with a variety of device and pharmaceutical companies.
NEW YORK – Boosting patient awareness and use of a new equation for measuring glomerular filtration rate are showing early signs of being the cornerstones to the prevention of chronic kidney disease among people at risk for the disease, according to preliminary results from the National Kidney Foundation's nationwide screening initiative.
The Kidney Early Evaluation Program (KEEP) has enrolled 150,000 people so far, making it the nation's largest perpetual chronic kidney disease screening program, according to Dr. Joseph Vassalotti, chief medical officer of the National Kidney Foundation and a faculty member at Mount Sinai School of Medicine, New York.
The point is to identify “individuals in the community with kidney disease along with the risk factors that go with it,” said Dr. George Bakris, professor of medicine at the University of Chicago Medical Center and a former KEEP principal investigator.
All of the participants have some stage of kidney disease or hypertension and are referred to the registry by physicians. Enrollment is voluntary and participants complete a questionnaire and undergo a medical evaluation that includes standard panels plus testing for calcium, phosphorus, and parathyroid hormone. The program does not accept people who have had a kidney transplant or are on dialysis, he said.
Under the program, a new method for estimating glomerular filtration rate (eGFR), known as the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation, has been used. This equation is more accurate in determining kidney function than is the Modification of Diet in Renal Disease (MDRD) Study equation, said Dr. Lesley Stevens of Tufts Medical Center, Boston.
“The use of the CKD-EPI equation more accurately reflects measured GFR and results in a lower prevalence of eGFR below 60 mL/min per 1.73 m
According to Dr. Stevens, the equation has been validated in two clinical studies (Am. J. Kidney Dis. 2010;55:648-59 and Am. J. Kidney Dis. 2010;55:660-70).
One of the goals of KEEP is to determine factors that help slow the slide into chronic kidney disease, as well as the loss of kidney function over time, Dr. Vassalotti said.
“Multiple trials on systolic blood pressure show that untreated hypertension results in a loss of 10-12 mL/min per 1.73 m
Managing blood pressure early in kidney disease is critical because as eGFR declines, hypertension becomes more difficult to control, Dr. Vassalotti said. Thus, self-reported hypertension is one of the qualifiers for KEEP enrollment, he said. He cited early data from KEEP that showed prevalence, awareness and treatment of hypertension increased with stage of chronic kidney disease, but that didn't necessarily translate to control with severe disease. Among those with stage 3 disease, only 82% were undergoing treatment, compared with 92% of those with stage 4 disease. However, 38% of the stage 3 group had systolic blood pressure below 140 mm Hg, while only 35% of the stage 4 group did (Am. J. Med. 2008; 121:332-40).
KEEP data have shown an uptick in overall blood pressure control, from 45% at the initial screening to 49% at rescreening, Dr. Vassalotti said, and even some improvement in control without medication. “But I wouldn't overstate this.”
The project involves merging data with the National Death Index and the United States Renal Data System to track survival and chronic kidney failure outcomes, respectively. Future goals include additional data links with Medicare Parts B and D to gain clarity on morbidity and medication use, Dr. Vassalotti said. “Preliminary longitudinal data show that community screening appears to influence hypertension despite progression of chronic kidney disease,” he said.
Patient awareness is the cornerstone of hypertension management, noted Dr. Adam Whaley-Connell of the University of Missouri. “Awareness has a very important role in not only understanding blood pressure control, especially in the context of the early stages of kidney disease, but in improving kidney related patient outcomes,” he said.
However, Dr. Whaley-Connell noted that awareness of kidney disease, particularly in its early stages, “is alarmingly low.” He noted that KEEP data on awareness reflect that of National Health and Nutrition Examination Survey and other chronic kidney disease cohort studies:
Only about 5% of those with stages 1-3 are aware of their disease. “Roughly 95% of individuals entering into the screening program are unaware they have chronic kidney disease,” Dr. Whaley-Connell said.
The point is to identify persons 'in the community with kidney disease along with the risk factors that go with it.'
Source DR. BAKRIS
'Community screening appears to influence hypertension despite progression' of CKD.
Source DR. VASSALOTTI
Major Finding: KEEP data have shown an uptick in overall blood pressure control among patients with early-stage kidney disease or hypertension, from 45% at the initial screening to 49% at rescreening.
Data Source: Preliminary results from the National Kidney Foundation's screening initiative.
Disclosures: KEEP is funded by Amgen, Abbott, Siemens, Astellas, Genzyme, Fresenius Medical Care, Pfizer, Nephroceuticals and the LifeScan unit of Johnson & Johnson. Panel participants disclosed affiliations with a variety of device and pharmaceutical companies.
NEW YORK – Boosting patient awareness and use of a new equation for measuring glomerular filtration rate are showing early signs of being the cornerstones to the prevention of chronic kidney disease among people at risk for the disease, according to preliminary results from the National Kidney Foundation's nationwide screening initiative.
The Kidney Early Evaluation Program (KEEP) has enrolled 150,000 people so far, making it the nation's largest perpetual chronic kidney disease screening program, according to Dr. Joseph Vassalotti, chief medical officer of the National Kidney Foundation and a faculty member at Mount Sinai School of Medicine, New York.
The point is to identify “individuals in the community with kidney disease along with the risk factors that go with it,” said Dr. George Bakris, professor of medicine at the University of Chicago Medical Center and a former KEEP principal investigator.
All of the participants have some stage of kidney disease or hypertension and are referred to the registry by physicians. Enrollment is voluntary and participants complete a questionnaire and undergo a medical evaluation that includes standard panels plus testing for calcium, phosphorus, and parathyroid hormone. The program does not accept people who have had a kidney transplant or are on dialysis, he said.
Under the program, a new method for estimating glomerular filtration rate (eGFR), known as the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation, has been used. This equation is more accurate in determining kidney function than is the Modification of Diet in Renal Disease (MDRD) Study equation, said Dr. Lesley Stevens of Tufts Medical Center, Boston.
“The use of the CKD-EPI equation more accurately reflects measured GFR and results in a lower prevalence of eGFR below 60 mL/min per 1.73 m
According to Dr. Stevens, the equation has been validated in two clinical studies (Am. J. Kidney Dis. 2010;55:648-59 and Am. J. Kidney Dis. 2010;55:660-70).
One of the goals of KEEP is to determine factors that help slow the slide into chronic kidney disease, as well as the loss of kidney function over time, Dr. Vassalotti said.
“Multiple trials on systolic blood pressure show that untreated hypertension results in a loss of 10-12 mL/min per 1.73 m
Managing blood pressure early in kidney disease is critical because as eGFR declines, hypertension becomes more difficult to control, Dr. Vassalotti said. Thus, self-reported hypertension is one of the qualifiers for KEEP enrollment, he said. He cited early data from KEEP that showed prevalence, awareness and treatment of hypertension increased with stage of chronic kidney disease, but that didn't necessarily translate to control with severe disease. Among those with stage 3 disease, only 82% were undergoing treatment, compared with 92% of those with stage 4 disease. However, 38% of the stage 3 group had systolic blood pressure below 140 mm Hg, while only 35% of the stage 4 group did (Am. J. Med. 2008; 121:332-40).
KEEP data have shown an uptick in overall blood pressure control, from 45% at the initial screening to 49% at rescreening, Dr. Vassalotti said, and even some improvement in control without medication. “But I wouldn't overstate this.”
The project involves merging data with the National Death Index and the United States Renal Data System to track survival and chronic kidney failure outcomes, respectively. Future goals include additional data links with Medicare Parts B and D to gain clarity on morbidity and medication use, Dr. Vassalotti said. “Preliminary longitudinal data show that community screening appears to influence hypertension despite progression of chronic kidney disease,” he said.
Patient awareness is the cornerstone of hypertension management, noted Dr. Adam Whaley-Connell of the University of Missouri. “Awareness has a very important role in not only understanding blood pressure control, especially in the context of the early stages of kidney disease, but in improving kidney related patient outcomes,” he said.
However, Dr. Whaley-Connell noted that awareness of kidney disease, particularly in its early stages, “is alarmingly low.” He noted that KEEP data on awareness reflect that of National Health and Nutrition Examination Survey and other chronic kidney disease cohort studies:
Only about 5% of those with stages 1-3 are aware of their disease. “Roughly 95% of individuals entering into the screening program are unaware they have chronic kidney disease,” Dr. Whaley-Connell said.
The point is to identify persons 'in the community with kidney disease along with the risk factors that go with it.'
Source DR. BAKRIS
'Community screening appears to influence hypertension despite progression' of CKD.
Source DR. VASSALOTTI
Intensive BP Therapy May Cut Fracture Risk
NEW YORK – Intensive therapy to control systolic blood pressure did not appear to be associated with more falls and fractures in a study of patients under age 80 years with hypertension and type 2 diabetes, based on a report presented at the meeting.
The finding was noted in a subgroup analysis of ACCORD-BONE, an ancillary study of skeletal health in ACCORD study participants. The subgroup analysis looked at ACCORD-BONE participants in the ACCORD Blood Pressure Clinical Trial arm of ACCORD.
For the subgroup analysis, the researchers examined data from 3,282 people who were randomly assigned to standard systolic blood pressure goals of 130-139 mm Hg or to intensive systolic goals of less than 120 mm Hg.
“Intensive control of systolic blood pressure did not result in an increased risk of falls,” reported Dr. Karen Margolis of the Health Partners Research Foundation in Minneapolis. “And fewer intensive than standard group patients developed nonspinal fractures.”
Average blood pressure at entry was 138/75 mm Hg. Those in the intensive therapy group received a thiazide-type diuretic in combination with another class of antihypertensive drug to a goal of 120 mm Hg. The standard intervention group used the same drugs and combinations, but the systolic goal was 130-135 mm Hg and treatment was only intensified if systolic blood pressure rose above 160 mm Hg, according to Dr. Margolis.
Systolic blood pressure averaged 133 mm Hg in the standard treatment group and 119 mm Hg in the intensive treatment group. Subjects' average age was 62 years, and patients over age 80 years were excluded; 44% were women; 66% were white, 26% were black, and 2% Latino. Patients' average body mass index was 32.5 kg/m
With an average follow-up of almost 5 years, ACCORD-BONE study results bucked conventional wisdom about risk of falls, according to Dr. Margolis. “About 20% in the intensive group and 21% in the standard group fell,” she said. The intensive group had a 0.81 relative risk of falling, compared with the standard group. The study found no differences across age, sex, ethnicity, or status of baseline diabetes.
The overall rate of self-reported falls was 70/100 person-years, Dr. Margolis said. “This also was lower in the intensive group at 62/100 person-years vs. the standard group at 74/100.
”With regard to nonspinal fractures, the study identified 273 individuals with at least one fracture, including 63 ankle, 34 humerus, 29 foot, 25 wrist, and 19 hip,” said Dr. Margolis. “Overall, fracture risk was significantly lower in the intensive vs. the standard blood pressure group with a hazard ratio of 0.78,” she said.
Dr. Margolis acknowledged the ACCORD-BONE study had some limits. “One of the most striking findings from the blood pressure treatment data was that there was a very, very large difference in thiazide use – thiazides being known to improve bone density – so that's a very suggestive mechanism,” she said.
Dr. Joseph L. Izzo of the University of Buffalo, N.Y., remarked about obesity in the study group, noting the high average BMI. “I'm not sure that overweight people aren't protected in some way against blood pressure–related falls,” Dr. Izzo said.
Physical activity might also explain why those on intensive therapy were less prone to falls and fractures, noted Dr. Bryan Williams of the University of Leicester, England. “To some extent, falls are not always due to just people getting possible hypotension; they're related to amount of activity,” he said.
Dr. Margolis said that a substudy would further investigate physical activity in this population.
The National Heart, Lung, and Blood Institute and National Institute of Diabetes and Digestive and Kidney Diseases funded the ACCORD-BONE study. Dr. Margolis had no other disclosures to report.
NEW YORK – Intensive therapy to control systolic blood pressure did not appear to be associated with more falls and fractures in a study of patients under age 80 years with hypertension and type 2 diabetes, based on a report presented at the meeting.
The finding was noted in a subgroup analysis of ACCORD-BONE, an ancillary study of skeletal health in ACCORD study participants. The subgroup analysis looked at ACCORD-BONE participants in the ACCORD Blood Pressure Clinical Trial arm of ACCORD.
For the subgroup analysis, the researchers examined data from 3,282 people who were randomly assigned to standard systolic blood pressure goals of 130-139 mm Hg or to intensive systolic goals of less than 120 mm Hg.
“Intensive control of systolic blood pressure did not result in an increased risk of falls,” reported Dr. Karen Margolis of the Health Partners Research Foundation in Minneapolis. “And fewer intensive than standard group patients developed nonspinal fractures.”
Average blood pressure at entry was 138/75 mm Hg. Those in the intensive therapy group received a thiazide-type diuretic in combination with another class of antihypertensive drug to a goal of 120 mm Hg. The standard intervention group used the same drugs and combinations, but the systolic goal was 130-135 mm Hg and treatment was only intensified if systolic blood pressure rose above 160 mm Hg, according to Dr. Margolis.
Systolic blood pressure averaged 133 mm Hg in the standard treatment group and 119 mm Hg in the intensive treatment group. Subjects' average age was 62 years, and patients over age 80 years were excluded; 44% were women; 66% were white, 26% were black, and 2% Latino. Patients' average body mass index was 32.5 kg/m
With an average follow-up of almost 5 years, ACCORD-BONE study results bucked conventional wisdom about risk of falls, according to Dr. Margolis. “About 20% in the intensive group and 21% in the standard group fell,” she said. The intensive group had a 0.81 relative risk of falling, compared with the standard group. The study found no differences across age, sex, ethnicity, or status of baseline diabetes.
The overall rate of self-reported falls was 70/100 person-years, Dr. Margolis said. “This also was lower in the intensive group at 62/100 person-years vs. the standard group at 74/100.
”With regard to nonspinal fractures, the study identified 273 individuals with at least one fracture, including 63 ankle, 34 humerus, 29 foot, 25 wrist, and 19 hip,” said Dr. Margolis. “Overall, fracture risk was significantly lower in the intensive vs. the standard blood pressure group with a hazard ratio of 0.78,” she said.
Dr. Margolis acknowledged the ACCORD-BONE study had some limits. “One of the most striking findings from the blood pressure treatment data was that there was a very, very large difference in thiazide use – thiazides being known to improve bone density – so that's a very suggestive mechanism,” she said.
Dr. Joseph L. Izzo of the University of Buffalo, N.Y., remarked about obesity in the study group, noting the high average BMI. “I'm not sure that overweight people aren't protected in some way against blood pressure–related falls,” Dr. Izzo said.
Physical activity might also explain why those on intensive therapy were less prone to falls and fractures, noted Dr. Bryan Williams of the University of Leicester, England. “To some extent, falls are not always due to just people getting possible hypotension; they're related to amount of activity,” he said.
Dr. Margolis said that a substudy would further investigate physical activity in this population.
The National Heart, Lung, and Blood Institute and National Institute of Diabetes and Digestive and Kidney Diseases funded the ACCORD-BONE study. Dr. Margolis had no other disclosures to report.
NEW YORK – Intensive therapy to control systolic blood pressure did not appear to be associated with more falls and fractures in a study of patients under age 80 years with hypertension and type 2 diabetes, based on a report presented at the meeting.
The finding was noted in a subgroup analysis of ACCORD-BONE, an ancillary study of skeletal health in ACCORD study participants. The subgroup analysis looked at ACCORD-BONE participants in the ACCORD Blood Pressure Clinical Trial arm of ACCORD.
For the subgroup analysis, the researchers examined data from 3,282 people who were randomly assigned to standard systolic blood pressure goals of 130-139 mm Hg or to intensive systolic goals of less than 120 mm Hg.
“Intensive control of systolic blood pressure did not result in an increased risk of falls,” reported Dr. Karen Margolis of the Health Partners Research Foundation in Minneapolis. “And fewer intensive than standard group patients developed nonspinal fractures.”
Average blood pressure at entry was 138/75 mm Hg. Those in the intensive therapy group received a thiazide-type diuretic in combination with another class of antihypertensive drug to a goal of 120 mm Hg. The standard intervention group used the same drugs and combinations, but the systolic goal was 130-135 mm Hg and treatment was only intensified if systolic blood pressure rose above 160 mm Hg, according to Dr. Margolis.
Systolic blood pressure averaged 133 mm Hg in the standard treatment group and 119 mm Hg in the intensive treatment group. Subjects' average age was 62 years, and patients over age 80 years were excluded; 44% were women; 66% were white, 26% were black, and 2% Latino. Patients' average body mass index was 32.5 kg/m
With an average follow-up of almost 5 years, ACCORD-BONE study results bucked conventional wisdom about risk of falls, according to Dr. Margolis. “About 20% in the intensive group and 21% in the standard group fell,” she said. The intensive group had a 0.81 relative risk of falling, compared with the standard group. The study found no differences across age, sex, ethnicity, or status of baseline diabetes.
The overall rate of self-reported falls was 70/100 person-years, Dr. Margolis said. “This also was lower in the intensive group at 62/100 person-years vs. the standard group at 74/100.
”With regard to nonspinal fractures, the study identified 273 individuals with at least one fracture, including 63 ankle, 34 humerus, 29 foot, 25 wrist, and 19 hip,” said Dr. Margolis. “Overall, fracture risk was significantly lower in the intensive vs. the standard blood pressure group with a hazard ratio of 0.78,” she said.
Dr. Margolis acknowledged the ACCORD-BONE study had some limits. “One of the most striking findings from the blood pressure treatment data was that there was a very, very large difference in thiazide use – thiazides being known to improve bone density – so that's a very suggestive mechanism,” she said.
Dr. Joseph L. Izzo of the University of Buffalo, N.Y., remarked about obesity in the study group, noting the high average BMI. “I'm not sure that overweight people aren't protected in some way against blood pressure–related falls,” Dr. Izzo said.
Physical activity might also explain why those on intensive therapy were less prone to falls and fractures, noted Dr. Bryan Williams of the University of Leicester, England. “To some extent, falls are not always due to just people getting possible hypotension; they're related to amount of activity,” he said.
Dr. Margolis said that a substudy would further investigate physical activity in this population.
The National Heart, Lung, and Blood Institute and National Institute of Diabetes and Digestive and Kidney Diseases funded the ACCORD-BONE study. Dr. Margolis had no other disclosures to report.