CHICAGO – A fresh frozen plasma–to–red blood cells ratio greater than 0.4:1 can stanch bleeding without causing organ failure, a small single-center study of 185 patients has found.
Trauma surgeons have long grappled with the ideal fresh frozen plasma–to–red blood cells (FFP:RBC) ratio for transfusion in severely injured patients because a 1:1 ratio may stop bleeding but cause respiratory distress. Results of the new study, presented by Dr. Charles E. Lucas at the annual meeting of the American Association for the Surgery of Trauma, shed some light on this question and identified some key recommendations for how level I trauma centers should manage massive transfusions.
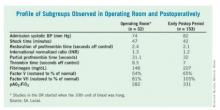
Dr. Lucas of the department of surgery at Wayne State University, Detroit, and his colleagues tracked serial measurements in 185 injured patients who received an average of 1,064 mL of FFP and 17.1 U of RBC, along with 12.6 L of crystalloids.
Observing patients during and after surgery, they compared levels of fibrinogen and labile factors V and VIII, standard clotting times, PaO2:FiO2 ratios for acute respiratory distress syndrome, and shock times. The average operation time was 8.1 hours. Studies in the operating room started when the 10th unit of blood was hung, he said.
"During the operative observation, we found the higher [the] level of FFP, the better [the] clotting times – the relationship of FFP ratio to coagulants again showing [that a] greater number of units of plasma given per red cells affects the procoagulant level," Dr. Lucas said. Moreover, the PaO2:FiO2 and FFP:RBC ratios showed no correlation in the operative or postoperative groups.
In the early postoperative group, at an average of 17 hours after admission, the relationship between clotting times and FFP:RBC ratio went away; factor V was the only factor that coordinated directly with FFP ratio, Dr. Lucas said. "This means that the increase in procoagulants at 17 hours after the patient arrives can no longer be related to the FFP:RBC ratio, but is due to increased synthesis of these factors by the liver and relocation of these factors from the interstitial fluid space," he said.
On the basis of the study results, the investigators offered the following four recommendations for level I centers responding to level I activation:
• Have 4 units of sex-specific O-negative RBC without plasma on hand.
• Use an FFP:RBC ratio of 2:4 if more plasma is needed.
• If plasma can be available in 10 minutes, use FFP when rapid thawing capabilities are available; otherwise, use prethawed plasma.
• Maintain a subsequent FFP:RBC ratio of 2:4 with ongoing monitoring of the coagulation test.
Dr. Ernest E. Moore Jr., the discussion leader for the paper, acknowledged that in the decades-long debate about the optimal FFP:RBC ratio, trauma surgeons have seen recommendations go from 1:4 to 1:5 and, more recently, to 1:2 or 1:3. Prothrombin and partial prothrombin times represent only the first 5% of activity in thrombin generation, noted Dr. Moore of Denver Health Medical Center.
"That’s true if you look at all the factors that are being evaluated by the clotting system," Dr. Lucas replied, "but with all the clotting tests, the end point is the conversion of fibrinogen to fibrin, so in that sense, it represents 100% of what’s happening."
Dr. Moore also asked whether the investigators detected any effect of FFP on renal, hepatic, or cardiac function.
The study evaluated several markers for those organs, Dr. Lucas noted. Among patients who received higher levels of plasma, the investigators found a slight increase in bilirubin in the operative group; in the postoperative group, they identified a significant increase in the level of FiO2 needed to achieve the desired PaO2 levels.
Dr. Lucas had no relevant disclosures.