User login
ED Intervention Modestly Alters Teens' Behaviors
Major Finding: At baseline 83% of the therapist group, 76% of the computer group, and 78% of the control group reported severe peer aggression during the past year. At 6 months the percentages were 45%, 49%, and 49%, respectively. At baseline 53% of the therapist group, 49% of the computer group, and 54% of the control group reported binge drinking. At 6 months the percentages declined to 33%, 33%, and 34%.
Data Source: Randomized, controlled trial of 726 adolescents, aged 14–18 years, who reported both past-year aggression and alcohol consumption.
Disclosures: The study was supported by the National Institute on Alcohol Abuse and Alcoholism. The authors reported no financial conflicts.
A brief intervention in the emergency department resulted in modest reductions in violence and alcohol use, according to a randomized, controlled trial involving 726 adolescents.
The teenagers, all of whom reported violence and alcohol abuse during the past year, were randomized to receive either a brochure (the control condition) or a 35-minute intervention delivered via computer or by a therapist. Both interventions were targeted at alcohol use and violence and were based on motivational interviewing techniques and skills training. The interventions included a review of goals, tailored feedback, a decisional balance exercise, role plays, and referrals, wrote Maureen A. Walton, Ph.D., of the University of Michigan, Ann Arbor, and her colleagues (JAMA 2010;304:527–35).
On every violence-related measure, all three groups, including the control group, showed substantial declines from baseline at 3 months and again at 6 months. For example, at baseline 83% of the therapist group, 76% of the computer group, and 78% of the control group reported severe peer aggression during the past year. At 3 months the percentages reporting aggression were 48%, 54%, and 62%, respectively, and at 6 months they were 45%, 49%, and 49%.
Similarly, all three groups showed substantial declines in every alcohol-related measure at 3 months and additional declines in most alcohol-related measures at 6 months. For example, at baseline 53% of the therapist group, 49% of the computer group, and 54% of the control group reported binge drinking. At 3 months the percentages declined to 34%, 29%, and 35%, respectively, and at 6 months they were 33%, 33%, and 34%.
Included in the study were adolescents aged 14–18 years who were being seen in a level I trauma center for a variety of reasons. Excluded were teens experiencing suicidal ideation, abnormal vital signs, insufficient cognitive orientation, and several other conditions. Of 3,764 patients approached for screening, 446 refused and 2,509 did not meet inclusion criteria, the most important of which was reported alcohol use and reported violence within the past year. More than 100 others refused participation, leaving 726 to be randomized. A total of 626 completed the 6-month assessment.
Several of the between-group differences were statistically significant. Compared with those in the control group, teenagers in the therapist group were significantly less likely to report severe peer aggression, an experience of peer violence, or consequences of violence at 3 months. None of those differences were statistically significant at 6 months. At 6 months, but not at 3 months, those in the therapist group reported significantly fewer alcohol consequences than controls.
The investigators reported several encouraging results from a number-needed-to-treat analysis. For example, only eight at-risk adolescents would need to receive the therapist intervention to prevent severe peer aggression in one adolescent. Ten at-risk adolescents would need to receive the therapist intervention to prevent one from being victimized by a peer. And 17 adolescents would need to receive the therapist intervention to prevent alcohol consequences in 1 teen.
In an accompanying editorial, Dr. Richard Saitz and Dr. Timothy S. Naimi of Boston University criticized several aspects of the study. They noted that the study's trial registration suggested that the investigators measured quite a few additional primary outcomes that they did not mention in their report, including drug use, injury, delinquency, and weapon carrying.
The fact that the investigators measured so many primary outcomes raises the concern of type I experimental error because of multiple comparisons. “If this study had measured more objective outcomes such as physician-documented injury events or school-based reports of violent incidents, rather than self-reported risk behaviors, the findings might have been more convincing,” they wrote.
In addition, Dr. Saitz and Dr. Naimi suggested that participants in face-to-face counseling might be less likely to report unsafe or undesirable behaviors at follow-up (JAMA 2010;304:575–7).
Dr. Saitz reported having been a consultant for online alcohol-related screening and brief intervention education projects supported by National Institutes of Health grants. He also has been compensated by Beth Israel Deaconess Hospital and the National Institute on Alcohol Abuse and Alcoholism for serving on data and safety monitoring boards. He has been or expects to be compensated as a speaker or consultant on alcohol and drug topics by multiple government agencies, academic institutions, professional societies, and private companies.
Dr. Naimi reported currently receiving NIH grant support.
Major Finding: At baseline 83% of the therapist group, 76% of the computer group, and 78% of the control group reported severe peer aggression during the past year. At 6 months the percentages were 45%, 49%, and 49%, respectively. At baseline 53% of the therapist group, 49% of the computer group, and 54% of the control group reported binge drinking. At 6 months the percentages declined to 33%, 33%, and 34%.
Data Source: Randomized, controlled trial of 726 adolescents, aged 14–18 years, who reported both past-year aggression and alcohol consumption.
Disclosures: The study was supported by the National Institute on Alcohol Abuse and Alcoholism. The authors reported no financial conflicts.
A brief intervention in the emergency department resulted in modest reductions in violence and alcohol use, according to a randomized, controlled trial involving 726 adolescents.
The teenagers, all of whom reported violence and alcohol abuse during the past year, were randomized to receive either a brochure (the control condition) or a 35-minute intervention delivered via computer or by a therapist. Both interventions were targeted at alcohol use and violence and were based on motivational interviewing techniques and skills training. The interventions included a review of goals, tailored feedback, a decisional balance exercise, role plays, and referrals, wrote Maureen A. Walton, Ph.D., of the University of Michigan, Ann Arbor, and her colleagues (JAMA 2010;304:527–35).
On every violence-related measure, all three groups, including the control group, showed substantial declines from baseline at 3 months and again at 6 months. For example, at baseline 83% of the therapist group, 76% of the computer group, and 78% of the control group reported severe peer aggression during the past year. At 3 months the percentages reporting aggression were 48%, 54%, and 62%, respectively, and at 6 months they were 45%, 49%, and 49%.
Similarly, all three groups showed substantial declines in every alcohol-related measure at 3 months and additional declines in most alcohol-related measures at 6 months. For example, at baseline 53% of the therapist group, 49% of the computer group, and 54% of the control group reported binge drinking. At 3 months the percentages declined to 34%, 29%, and 35%, respectively, and at 6 months they were 33%, 33%, and 34%.
Included in the study were adolescents aged 14–18 years who were being seen in a level I trauma center for a variety of reasons. Excluded were teens experiencing suicidal ideation, abnormal vital signs, insufficient cognitive orientation, and several other conditions. Of 3,764 patients approached for screening, 446 refused and 2,509 did not meet inclusion criteria, the most important of which was reported alcohol use and reported violence within the past year. More than 100 others refused participation, leaving 726 to be randomized. A total of 626 completed the 6-month assessment.
Several of the between-group differences were statistically significant. Compared with those in the control group, teenagers in the therapist group were significantly less likely to report severe peer aggression, an experience of peer violence, or consequences of violence at 3 months. None of those differences were statistically significant at 6 months. At 6 months, but not at 3 months, those in the therapist group reported significantly fewer alcohol consequences than controls.
The investigators reported several encouraging results from a number-needed-to-treat analysis. For example, only eight at-risk adolescents would need to receive the therapist intervention to prevent severe peer aggression in one adolescent. Ten at-risk adolescents would need to receive the therapist intervention to prevent one from being victimized by a peer. And 17 adolescents would need to receive the therapist intervention to prevent alcohol consequences in 1 teen.
In an accompanying editorial, Dr. Richard Saitz and Dr. Timothy S. Naimi of Boston University criticized several aspects of the study. They noted that the study's trial registration suggested that the investigators measured quite a few additional primary outcomes that they did not mention in their report, including drug use, injury, delinquency, and weapon carrying.
The fact that the investigators measured so many primary outcomes raises the concern of type I experimental error because of multiple comparisons. “If this study had measured more objective outcomes such as physician-documented injury events or school-based reports of violent incidents, rather than self-reported risk behaviors, the findings might have been more convincing,” they wrote.
In addition, Dr. Saitz and Dr. Naimi suggested that participants in face-to-face counseling might be less likely to report unsafe or undesirable behaviors at follow-up (JAMA 2010;304:575–7).
Dr. Saitz reported having been a consultant for online alcohol-related screening and brief intervention education projects supported by National Institutes of Health grants. He also has been compensated by Beth Israel Deaconess Hospital and the National Institute on Alcohol Abuse and Alcoholism for serving on data and safety monitoring boards. He has been or expects to be compensated as a speaker or consultant on alcohol and drug topics by multiple government agencies, academic institutions, professional societies, and private companies.
Dr. Naimi reported currently receiving NIH grant support.
Major Finding: At baseline 83% of the therapist group, 76% of the computer group, and 78% of the control group reported severe peer aggression during the past year. At 6 months the percentages were 45%, 49%, and 49%, respectively. At baseline 53% of the therapist group, 49% of the computer group, and 54% of the control group reported binge drinking. At 6 months the percentages declined to 33%, 33%, and 34%.
Data Source: Randomized, controlled trial of 726 adolescents, aged 14–18 years, who reported both past-year aggression and alcohol consumption.
Disclosures: The study was supported by the National Institute on Alcohol Abuse and Alcoholism. The authors reported no financial conflicts.
A brief intervention in the emergency department resulted in modest reductions in violence and alcohol use, according to a randomized, controlled trial involving 726 adolescents.
The teenagers, all of whom reported violence and alcohol abuse during the past year, were randomized to receive either a brochure (the control condition) or a 35-minute intervention delivered via computer or by a therapist. Both interventions were targeted at alcohol use and violence and were based on motivational interviewing techniques and skills training. The interventions included a review of goals, tailored feedback, a decisional balance exercise, role plays, and referrals, wrote Maureen A. Walton, Ph.D., of the University of Michigan, Ann Arbor, and her colleagues (JAMA 2010;304:527–35).
On every violence-related measure, all three groups, including the control group, showed substantial declines from baseline at 3 months and again at 6 months. For example, at baseline 83% of the therapist group, 76% of the computer group, and 78% of the control group reported severe peer aggression during the past year. At 3 months the percentages reporting aggression were 48%, 54%, and 62%, respectively, and at 6 months they were 45%, 49%, and 49%.
Similarly, all three groups showed substantial declines in every alcohol-related measure at 3 months and additional declines in most alcohol-related measures at 6 months. For example, at baseline 53% of the therapist group, 49% of the computer group, and 54% of the control group reported binge drinking. At 3 months the percentages declined to 34%, 29%, and 35%, respectively, and at 6 months they were 33%, 33%, and 34%.
Included in the study were adolescents aged 14–18 years who were being seen in a level I trauma center for a variety of reasons. Excluded were teens experiencing suicidal ideation, abnormal vital signs, insufficient cognitive orientation, and several other conditions. Of 3,764 patients approached for screening, 446 refused and 2,509 did not meet inclusion criteria, the most important of which was reported alcohol use and reported violence within the past year. More than 100 others refused participation, leaving 726 to be randomized. A total of 626 completed the 6-month assessment.
Several of the between-group differences were statistically significant. Compared with those in the control group, teenagers in the therapist group were significantly less likely to report severe peer aggression, an experience of peer violence, or consequences of violence at 3 months. None of those differences were statistically significant at 6 months. At 6 months, but not at 3 months, those in the therapist group reported significantly fewer alcohol consequences than controls.
The investigators reported several encouraging results from a number-needed-to-treat analysis. For example, only eight at-risk adolescents would need to receive the therapist intervention to prevent severe peer aggression in one adolescent. Ten at-risk adolescents would need to receive the therapist intervention to prevent one from being victimized by a peer. And 17 adolescents would need to receive the therapist intervention to prevent alcohol consequences in 1 teen.
In an accompanying editorial, Dr. Richard Saitz and Dr. Timothy S. Naimi of Boston University criticized several aspects of the study. They noted that the study's trial registration suggested that the investigators measured quite a few additional primary outcomes that they did not mention in their report, including drug use, injury, delinquency, and weapon carrying.
The fact that the investigators measured so many primary outcomes raises the concern of type I experimental error because of multiple comparisons. “If this study had measured more objective outcomes such as physician-documented injury events or school-based reports of violent incidents, rather than self-reported risk behaviors, the findings might have been more convincing,” they wrote.
In addition, Dr. Saitz and Dr. Naimi suggested that participants in face-to-face counseling might be less likely to report unsafe or undesirable behaviors at follow-up (JAMA 2010;304:575–7).
Dr. Saitz reported having been a consultant for online alcohol-related screening and brief intervention education projects supported by National Institutes of Health grants. He also has been compensated by Beth Israel Deaconess Hospital and the National Institute on Alcohol Abuse and Alcoholism for serving on data and safety monitoring boards. He has been or expects to be compensated as a speaker or consultant on alcohol and drug topics by multiple government agencies, academic institutions, professional societies, and private companies.
Dr. Naimi reported currently receiving NIH grant support.
Drug-Resistant Klebsiella Pneumoniae a Growing Problem
VANCOUVER, B.C. - There’s a new bad bug on the block, and it appears to be making appearances in long-term care facilities, at least in the Chicago area, according to a recent study presented at the annual meeting of the Infectious Diseases Society of America.
Carbapenem-resistant Enterobacteriaceae, particularly those that produce Klebsiella pneumoniae carbapenemase (KPC), are becoming increasingly problematic in the Chicago area, Dr. Mary K. Hayden said during a press briefing. The first case appeared in Chicago in December 2007, but by March 2009 an Internet-based survey of infection preventionists revealed that 26 of 53 facilities (49%) had reported one case, and the mean number of cases per facility was 3.8.
In a subsequent survey in February 2010, 37 of 57 facilities (65%) had reported at least one case, and the mean number of cases per facility was 10.2.
According to the 2009 survey, 81% of the affected patients had been transferred from a long-term care facility or a long-term acute care hospital. In 2010, 75% of patients came from such facilities.
Dr. Hayden, of Rush University Medical Center, Chicago, declined to refer to KPC as a "superbug," a term favored in the popular press, but she did say, "I think it is an organism that should be identified as requiring particular attention. [It] can cause serious, life-threatening infections in hospitalized patients."
These organisms, aerobic gram-negative bacilli, produce infections that are particularly difficult to treat because they’re resistant to most and sometimes to all available antibiotics.
"This rapid increase in KPC is not unique to the Chicago area," Dr. Hayden said. "KPC was first identified in North Carolina in the late 1990s, and over the next 10 years remained restricted to the East Coast, causing significant morbidity and mortality in areas such as Brooklyn, N.Y. But in the last couple of years, KPC has spread globally, with reports now from multiple areas in the United States and from South America, Europe, and Asia. An extreme example was seen in Israel, which reported a nationwide outbreak of KPC only about 2 years after their first case was identified."
Dr. Hayden said that her team believes their findings point to the need for a regional approach to KPC control. "It will require coordinated collaboration between acute care hospitals, long-term care facilities, and public health [departments]," she said.
VANCOUVER, B.C. - There’s a new bad bug on the block, and it appears to be making appearances in long-term care facilities, at least in the Chicago area, according to a recent study presented at the annual meeting of the Infectious Diseases Society of America.
Carbapenem-resistant Enterobacteriaceae, particularly those that produce Klebsiella pneumoniae carbapenemase (KPC), are becoming increasingly problematic in the Chicago area, Dr. Mary K. Hayden said during a press briefing. The first case appeared in Chicago in December 2007, but by March 2009 an Internet-based survey of infection preventionists revealed that 26 of 53 facilities (49%) had reported one case, and the mean number of cases per facility was 3.8.
In a subsequent survey in February 2010, 37 of 57 facilities (65%) had reported at least one case, and the mean number of cases per facility was 10.2.
According to the 2009 survey, 81% of the affected patients had been transferred from a long-term care facility or a long-term acute care hospital. In 2010, 75% of patients came from such facilities.
Dr. Hayden, of Rush University Medical Center, Chicago, declined to refer to KPC as a "superbug," a term favored in the popular press, but she did say, "I think it is an organism that should be identified as requiring particular attention. [It] can cause serious, life-threatening infections in hospitalized patients."
These organisms, aerobic gram-negative bacilli, produce infections that are particularly difficult to treat because they’re resistant to most and sometimes to all available antibiotics.
"This rapid increase in KPC is not unique to the Chicago area," Dr. Hayden said. "KPC was first identified in North Carolina in the late 1990s, and over the next 10 years remained restricted to the East Coast, causing significant morbidity and mortality in areas such as Brooklyn, N.Y. But in the last couple of years, KPC has spread globally, with reports now from multiple areas in the United States and from South America, Europe, and Asia. An extreme example was seen in Israel, which reported a nationwide outbreak of KPC only about 2 years after their first case was identified."
Dr. Hayden said that her team believes their findings point to the need for a regional approach to KPC control. "It will require coordinated collaboration between acute care hospitals, long-term care facilities, and public health [departments]," she said.
VANCOUVER, B.C. - There’s a new bad bug on the block, and it appears to be making appearances in long-term care facilities, at least in the Chicago area, according to a recent study presented at the annual meeting of the Infectious Diseases Society of America.
Carbapenem-resistant Enterobacteriaceae, particularly those that produce Klebsiella pneumoniae carbapenemase (KPC), are becoming increasingly problematic in the Chicago area, Dr. Mary K. Hayden said during a press briefing. The first case appeared in Chicago in December 2007, but by March 2009 an Internet-based survey of infection preventionists revealed that 26 of 53 facilities (49%) had reported one case, and the mean number of cases per facility was 3.8.
In a subsequent survey in February 2010, 37 of 57 facilities (65%) had reported at least one case, and the mean number of cases per facility was 10.2.
According to the 2009 survey, 81% of the affected patients had been transferred from a long-term care facility or a long-term acute care hospital. In 2010, 75% of patients came from such facilities.
Dr. Hayden, of Rush University Medical Center, Chicago, declined to refer to KPC as a "superbug," a term favored in the popular press, but she did say, "I think it is an organism that should be identified as requiring particular attention. [It] can cause serious, life-threatening infections in hospitalized patients."
These organisms, aerobic gram-negative bacilli, produce infections that are particularly difficult to treat because they’re resistant to most and sometimes to all available antibiotics.
"This rapid increase in KPC is not unique to the Chicago area," Dr. Hayden said. "KPC was first identified in North Carolina in the late 1990s, and over the next 10 years remained restricted to the East Coast, causing significant morbidity and mortality in areas such as Brooklyn, N.Y. But in the last couple of years, KPC has spread globally, with reports now from multiple areas in the United States and from South America, Europe, and Asia. An extreme example was seen in Israel, which reported a nationwide outbreak of KPC only about 2 years after their first case was identified."
Dr. Hayden said that her team believes their findings point to the need for a regional approach to KPC control. "It will require coordinated collaboration between acute care hospitals, long-term care facilities, and public health [departments]," she said.
FROM THE ANNUAL MEETING OF THE INFECTIOUS DISEASES SOCIETY OF AMERICA
Major Finding: Between December 2007 and February 2010, Chicago went from a single case of resistant Klebsiella pneumoniae in one health care facility to an average of about 10 cases in each of 37 different facilities.
Data Source: Two Internet-based surveys administered to Chicago-area infection preventionists.
Disclosures: The authors had no disclosures.
Drug-Resistant Klebsiella pneumoniae a Growing Problem
VANCOUVER, B.C. – There’s a new bad bug on the block, and it appears to be making appearances in long-term care facilities, at least in the Chicago area, according to a recent study presented at the annual meeting of the Infectious Diseases Society of America.
Carbapenem-resistant Enterobacteriaceae, particularly those that produce Klebsiella pneumoniae carbapenemase (KPC), are becoming increasingly problematic in the Chicago area, Dr. Mary K. Hayden said during a press briefing. The first case appeared in Chicago in December 2007, but by March 2009 an Internet-based survey of infection preventionists revealed that 26 of 53 facilities (49%) had reported one case, and the mean number of cases per facility was 3.8.
In a subsequent survey in February 2010, 37 of 57 facilities (65%) had reported at least one case, and the mean number of cases per facility was 10.2.
According to the 2009 survey, 81% of the affected patients had been transferred from a long-term care facility or a long-term acute care hospital. In 2010, 75% of patients came from such facilities.
Dr. Hayden, of Rush University Medical Center, Chicago, declined to refer to KPC as a "superbug," a term favored in the popular press, but she did say, "I think it is an organism that should be identified as requiring particular attention. [It] can cause serious, life-threatening infections in hospitalized patients."
These organisms, aerobic gram-negative bacilli, produce infections that are particularly difficult to treat because they’re resistant to most and sometimes to all available antibiotics.
"This rapid increase in KPC is not unique to the Chicago area," Dr. Hayden said. "KPC was first identified in North Carolina in the late 1990s, and over the next 10 years remained restricted to the East Coast, causing significant morbidity and mortality in areas such as Brooklyn, N.Y. But in the last couple of years, KPC has spread globally, with reports now from multiple areas in the United States and from South America, Europe, and Asia. An extreme example was seen in Israel, which reported a nationwide outbreak of KPC only about 2 years after their first case was identified."
Dr. Hayden said that her team believes their findings point to the need for a regional approach to KPC control. "It will require coordinated collaboration between acute care hospitals, long-term care facilities, and public health [departments]," she said.
Dr. Hayden stated that she had no disclosures related to her study.
VANCOUVER, B.C. – There’s a new bad bug on the block, and it appears to be making appearances in long-term care facilities, at least in the Chicago area, according to a recent study presented at the annual meeting of the Infectious Diseases Society of America.
Carbapenem-resistant Enterobacteriaceae, particularly those that produce Klebsiella pneumoniae carbapenemase (KPC), are becoming increasingly problematic in the Chicago area, Dr. Mary K. Hayden said during a press briefing. The first case appeared in Chicago in December 2007, but by March 2009 an Internet-based survey of infection preventionists revealed that 26 of 53 facilities (49%) had reported one case, and the mean number of cases per facility was 3.8.
In a subsequent survey in February 2010, 37 of 57 facilities (65%) had reported at least one case, and the mean number of cases per facility was 10.2.
According to the 2009 survey, 81% of the affected patients had been transferred from a long-term care facility or a long-term acute care hospital. In 2010, 75% of patients came from such facilities.
Dr. Hayden, of Rush University Medical Center, Chicago, declined to refer to KPC as a "superbug," a term favored in the popular press, but she did say, "I think it is an organism that should be identified as requiring particular attention. [It] can cause serious, life-threatening infections in hospitalized patients."
These organisms, aerobic gram-negative bacilli, produce infections that are particularly difficult to treat because they’re resistant to most and sometimes to all available antibiotics.
"This rapid increase in KPC is not unique to the Chicago area," Dr. Hayden said. "KPC was first identified in North Carolina in the late 1990s, and over the next 10 years remained restricted to the East Coast, causing significant morbidity and mortality in areas such as Brooklyn, N.Y. But in the last couple of years, KPC has spread globally, with reports now from multiple areas in the United States and from South America, Europe, and Asia. An extreme example was seen in Israel, which reported a nationwide outbreak of KPC only about 2 years after their first case was identified."
Dr. Hayden said that her team believes their findings point to the need for a regional approach to KPC control. "It will require coordinated collaboration between acute care hospitals, long-term care facilities, and public health [departments]," she said.
Dr. Hayden stated that she had no disclosures related to her study.
VANCOUVER, B.C. – There’s a new bad bug on the block, and it appears to be making appearances in long-term care facilities, at least in the Chicago area, according to a recent study presented at the annual meeting of the Infectious Diseases Society of America.
Carbapenem-resistant Enterobacteriaceae, particularly those that produce Klebsiella pneumoniae carbapenemase (KPC), are becoming increasingly problematic in the Chicago area, Dr. Mary K. Hayden said during a press briefing. The first case appeared in Chicago in December 2007, but by March 2009 an Internet-based survey of infection preventionists revealed that 26 of 53 facilities (49%) had reported one case, and the mean number of cases per facility was 3.8.
In a subsequent survey in February 2010, 37 of 57 facilities (65%) had reported at least one case, and the mean number of cases per facility was 10.2.
According to the 2009 survey, 81% of the affected patients had been transferred from a long-term care facility or a long-term acute care hospital. In 2010, 75% of patients came from such facilities.
Dr. Hayden, of Rush University Medical Center, Chicago, declined to refer to KPC as a "superbug," a term favored in the popular press, but she did say, "I think it is an organism that should be identified as requiring particular attention. [It] can cause serious, life-threatening infections in hospitalized patients."
These organisms, aerobic gram-negative bacilli, produce infections that are particularly difficult to treat because they’re resistant to most and sometimes to all available antibiotics.
"This rapid increase in KPC is not unique to the Chicago area," Dr. Hayden said. "KPC was first identified in North Carolina in the late 1990s, and over the next 10 years remained restricted to the East Coast, causing significant morbidity and mortality in areas such as Brooklyn, N.Y. But in the last couple of years, KPC has spread globally, with reports now from multiple areas in the United States and from South America, Europe, and Asia. An extreme example was seen in Israel, which reported a nationwide outbreak of KPC only about 2 years after their first case was identified."
Dr. Hayden said that her team believes their findings point to the need for a regional approach to KPC control. "It will require coordinated collaboration between acute care hospitals, long-term care facilities, and public health [departments]," she said.
Dr. Hayden stated that she had no disclosures related to her study.
FROM THE ANNUAL MEETING OF THE INFECTIOUS DISEASES SOCIETY OF AMERICA
Drug-Resistant Klebsiella pneumoniae a Growing Problem
VANCOUVER, B.C. – There’s a new bad bug on the block, and it appears to be making appearances in long-term care facilities, at least in the Chicago area, according to a recent study presented at the annual meeting of the Infectious Diseases Society of America.
Carbapenem-resistant Enterobacteriaceae, particularly those that produce Klebsiella pneumoniae carbapenemase (KPC), are becoming increasingly problematic in the Chicago area, Dr. Mary K. Hayden said during a press briefing. The first case appeared in Chicago in December 2007, but by March 2009 an Internet-based survey of infection preventionists revealed that 26 of 53 facilities (49%) had reported one case, and the mean number of cases per facility was 3.8.
In a subsequent survey in February 2010, 37 of 57 facilities (65%) had reported at least one case, and the mean number of cases per facility was 10.2.
According to the 2009 survey, 81% of the affected patients had been transferred from a long-term care facility or a long-term acute care hospital. In 2010, 75% of patients came from such facilities.
Dr. Hayden, of Rush University Medical Center, Chicago, declined to refer to KPC as a "superbug," a term favored in the popular press, but she did say, "I think it is an organism that should be identified as requiring particular attention. [It] can cause serious, life-threatening infections in hospitalized patients."
These organisms, aerobic gram-negative bacilli, produce infections that are particularly difficult to treat because they’re resistant to most and sometimes to all available antibiotics.
"This rapid increase in KPC is not unique to the Chicago area," Dr. Hayden said. "KPC was first identified in North Carolina in the late 1990s, and over the next 10 years remained restricted to the East Coast, causing significant morbidity and mortality in areas such as Brooklyn, N.Y. But in the last couple of years, KPC has spread globally, with reports now from multiple areas in the United States and from South America, Europe, and Asia. An extreme example was seen in Israel, which reported a nationwide outbreak of KPC only about 2 years after their first case was identified."
Dr. Hayden said that her team believes their findings point to the need for a regional approach to KPC control. "It will require coordinated collaboration between acute care hospitals, long-term care facilities, and public health [departments]," she said.
Dr. Hayden stated that she had no disclosures related to her study.
VANCOUVER, B.C. – There’s a new bad bug on the block, and it appears to be making appearances in long-term care facilities, at least in the Chicago area, according to a recent study presented at the annual meeting of the Infectious Diseases Society of America.
Carbapenem-resistant Enterobacteriaceae, particularly those that produce Klebsiella pneumoniae carbapenemase (KPC), are becoming increasingly problematic in the Chicago area, Dr. Mary K. Hayden said during a press briefing. The first case appeared in Chicago in December 2007, but by March 2009 an Internet-based survey of infection preventionists revealed that 26 of 53 facilities (49%) had reported one case, and the mean number of cases per facility was 3.8.
In a subsequent survey in February 2010, 37 of 57 facilities (65%) had reported at least one case, and the mean number of cases per facility was 10.2.
According to the 2009 survey, 81% of the affected patients had been transferred from a long-term care facility or a long-term acute care hospital. In 2010, 75% of patients came from such facilities.
Dr. Hayden, of Rush University Medical Center, Chicago, declined to refer to KPC as a "superbug," a term favored in the popular press, but she did say, "I think it is an organism that should be identified as requiring particular attention. [It] can cause serious, life-threatening infections in hospitalized patients."
These organisms, aerobic gram-negative bacilli, produce infections that are particularly difficult to treat because they’re resistant to most and sometimes to all available antibiotics.
"This rapid increase in KPC is not unique to the Chicago area," Dr. Hayden said. "KPC was first identified in North Carolina in the late 1990s, and over the next 10 years remained restricted to the East Coast, causing significant morbidity and mortality in areas such as Brooklyn, N.Y. But in the last couple of years, KPC has spread globally, with reports now from multiple areas in the United States and from South America, Europe, and Asia. An extreme example was seen in Israel, which reported a nationwide outbreak of KPC only about 2 years after their first case was identified."
Dr. Hayden said that her team believes their findings point to the need for a regional approach to KPC control. "It will require coordinated collaboration between acute care hospitals, long-term care facilities, and public health [departments]," she said.
Dr. Hayden stated that she had no disclosures related to her study.
VANCOUVER, B.C. – There’s a new bad bug on the block, and it appears to be making appearances in long-term care facilities, at least in the Chicago area, according to a recent study presented at the annual meeting of the Infectious Diseases Society of America.
Carbapenem-resistant Enterobacteriaceae, particularly those that produce Klebsiella pneumoniae carbapenemase (KPC), are becoming increasingly problematic in the Chicago area, Dr. Mary K. Hayden said during a press briefing. The first case appeared in Chicago in December 2007, but by March 2009 an Internet-based survey of infection preventionists revealed that 26 of 53 facilities (49%) had reported one case, and the mean number of cases per facility was 3.8.
In a subsequent survey in February 2010, 37 of 57 facilities (65%) had reported at least one case, and the mean number of cases per facility was 10.2.
According to the 2009 survey, 81% of the affected patients had been transferred from a long-term care facility or a long-term acute care hospital. In 2010, 75% of patients came from such facilities.
Dr. Hayden, of Rush University Medical Center, Chicago, declined to refer to KPC as a "superbug," a term favored in the popular press, but she did say, "I think it is an organism that should be identified as requiring particular attention. [It] can cause serious, life-threatening infections in hospitalized patients."
These organisms, aerobic gram-negative bacilli, produce infections that are particularly difficult to treat because they’re resistant to most and sometimes to all available antibiotics.
"This rapid increase in KPC is not unique to the Chicago area," Dr. Hayden said. "KPC was first identified in North Carolina in the late 1990s, and over the next 10 years remained restricted to the East Coast, causing significant morbidity and mortality in areas such as Brooklyn, N.Y. But in the last couple of years, KPC has spread globally, with reports now from multiple areas in the United States and from South America, Europe, and Asia. An extreme example was seen in Israel, which reported a nationwide outbreak of KPC only about 2 years after their first case was identified."
Dr. Hayden said that her team believes their findings point to the need for a regional approach to KPC control. "It will require coordinated collaboration between acute care hospitals, long-term care facilities, and public health [departments]," she said.
Dr. Hayden stated that she had no disclosures related to her study.
FROM THE ANNUAL MEETING OF THE INFECTIOUS DISEASES SOCIETY OF AMERICA
Major Finding: Between December 2007 and February 2010, Chicago went from a single case of resistant Klebsiella pneumoniae in one health care facility to an average of about 10 cases in each of 37 different facilities.
Data Source: Two Internet-based surveys administered to Chicago-area infection preventionists.
Disclosures: The authors had no disclosures.
FDA Program Aims to Improve External Defibrillators
A new initiative aimed at improving the reliability of external defibrillators has been launched by the Food and Drug Administration, the agency announced Nov. 15.
The initiative includes external defibrillators used by medical professionals as well as automated external defibrillators (AEDs) intended for use by members of the public.
According to the FDA, the agency’s Center for Devices and Radiological Health (CDRH) has received more than 28,000 reports of device failures associated with external defibrillators during the past 5 years. Manufacturers have conducted 68 recalls from Jan. 1, 2005 to July 10, 2010.
During a news briefing, Dr. Jeffrey Shuren, director of CDRH, said that 700 deaths had been associated with device failures, but that it’s difficult to determine how many of those resulted directly from malfunctions of the devices. Having suffered cardiac defibrillation, the patients were, of course, very ill, and many would probably have died even if the devices had worked correctly.
The problems the FDA identified range across all manufacturers of the devices. They involve shortcomings in engineering, design practices, and manufacturing practices, poor communication to users, and lack of adverse event reporting.
For example, some manufacturers have used a "fix-on-fail" strategy for dealing with problems. "Fix on fail" refers to the practice of identifying and fixing problems with individual devices on a case-by-case basis instead of informing all users of the problems as part of a recall.
Under the new initiative, the agency will collaborate with manufacturers and others to facilitate the development of the next generation of defibrillators. To further these efforts, the agency will hold a public workshop on Dec. 15-16, intended to bring together government, industry, academia, and clinicians.
The FDA also will work with manufacturers to improve the way they respond to user complaints, conduct recalls, and report adverse events.
Finally, the FDA will propose changes to the classification of AEDs and changes to the premarket regulatory pathway of these devices. The agency plans to announce those proposed changes in 2011.
"I think it’s important to reiterate that we consider these to be lifesaving technologies" Dr. Shuren said during the press briefing. "We’re not taking any of these devices off the market. We’re strongly encouraging people to continue to use them and to use them according to guidelines. And we think that these technologies can improve to reduce the rate of failures that we’ve seen."
A new FDA initiative intended to improve the reliability of external defibrillators will address manufacturing and engineering design practices, poor communication to users, and lack of adverse event reporting.
A new initiative aimed at improving the reliability of external defibrillators has been launched by the Food and Drug Administration, the agency announced Nov. 15.
The initiative includes external defibrillators used by medical professionals as well as automated external defibrillators (AEDs) intended for use by members of the public.
According to the FDA, the agency’s Center for Devices and Radiological Health (CDRH) has received more than 28,000 reports of device failures associated with external defibrillators during the past 5 years. Manufacturers have conducted 68 recalls from Jan. 1, 2005 to July 10, 2010.
During a news briefing, Dr. Jeffrey Shuren, director of CDRH, said that 700 deaths had been associated with device failures, but that it’s difficult to determine how many of those resulted directly from malfunctions of the devices. Having suffered cardiac defibrillation, the patients were, of course, very ill, and many would probably have died even if the devices had worked correctly.
The problems the FDA identified range across all manufacturers of the devices. They involve shortcomings in engineering, design practices, and manufacturing practices, poor communication to users, and lack of adverse event reporting.
For example, some manufacturers have used a "fix-on-fail" strategy for dealing with problems. "Fix on fail" refers to the practice of identifying and fixing problems with individual devices on a case-by-case basis instead of informing all users of the problems as part of a recall.
Under the new initiative, the agency will collaborate with manufacturers and others to facilitate the development of the next generation of defibrillators. To further these efforts, the agency will hold a public workshop on Dec. 15-16, intended to bring together government, industry, academia, and clinicians.
The FDA also will work with manufacturers to improve the way they respond to user complaints, conduct recalls, and report adverse events.
Finally, the FDA will propose changes to the classification of AEDs and changes to the premarket regulatory pathway of these devices. The agency plans to announce those proposed changes in 2011.
"I think it’s important to reiterate that we consider these to be lifesaving technologies" Dr. Shuren said during the press briefing. "We’re not taking any of these devices off the market. We’re strongly encouraging people to continue to use them and to use them according to guidelines. And we think that these technologies can improve to reduce the rate of failures that we’ve seen."
A new FDA initiative intended to improve the reliability of external defibrillators will address manufacturing and engineering design practices, poor communication to users, and lack of adverse event reporting.
A new initiative aimed at improving the reliability of external defibrillators has been launched by the Food and Drug Administration, the agency announced Nov. 15.
The initiative includes external defibrillators used by medical professionals as well as automated external defibrillators (AEDs) intended for use by members of the public.
According to the FDA, the agency’s Center for Devices and Radiological Health (CDRH) has received more than 28,000 reports of device failures associated with external defibrillators during the past 5 years. Manufacturers have conducted 68 recalls from Jan. 1, 2005 to July 10, 2010.
During a news briefing, Dr. Jeffrey Shuren, director of CDRH, said that 700 deaths had been associated with device failures, but that it’s difficult to determine how many of those resulted directly from malfunctions of the devices. Having suffered cardiac defibrillation, the patients were, of course, very ill, and many would probably have died even if the devices had worked correctly.
The problems the FDA identified range across all manufacturers of the devices. They involve shortcomings in engineering, design practices, and manufacturing practices, poor communication to users, and lack of adverse event reporting.
For example, some manufacturers have used a "fix-on-fail" strategy for dealing with problems. "Fix on fail" refers to the practice of identifying and fixing problems with individual devices on a case-by-case basis instead of informing all users of the problems as part of a recall.
Under the new initiative, the agency will collaborate with manufacturers and others to facilitate the development of the next generation of defibrillators. To further these efforts, the agency will hold a public workshop on Dec. 15-16, intended to bring together government, industry, academia, and clinicians.
The FDA also will work with manufacturers to improve the way they respond to user complaints, conduct recalls, and report adverse events.
Finally, the FDA will propose changes to the classification of AEDs and changes to the premarket regulatory pathway of these devices. The agency plans to announce those proposed changes in 2011.
"I think it’s important to reiterate that we consider these to be lifesaving technologies" Dr. Shuren said during the press briefing. "We’re not taking any of these devices off the market. We’re strongly encouraging people to continue to use them and to use them according to guidelines. And we think that these technologies can improve to reduce the rate of failures that we’ve seen."
A new FDA initiative intended to improve the reliability of external defibrillators will address manufacturing and engineering design practices, poor communication to users, and lack of adverse event reporting.
FROM AN FDA TELEBRIEFING
FDA Program Aims to Improve External Defibrillators
A new initiative aimed at improving the reliability of external defibrillators has been launched by the Food and Drug Administration, the agency announced Nov. 15.
The initiative includes external defibrillators used by medical professionals as well as automated external defibrillators (AEDs) intended for use by members of the public.
According to the FDA, the agency’s Center for Devices and Radiological Health (CDRH) has received more than 28,000 reports of device failures associated with external defibrillators during the past 5 years. Manufacturers have conducted 68 recalls from Jan. 1, 2005 to July 10, 2010.
During a news briefing, Dr. Jeffrey Shuren, director of CDRH, said that 700 deaths had been associated with device failures, but that it’s difficult to determine how many of those resulted directly from malfunctions of the devices. Having suffered cardiac defibrillation, the patients were, of course, very ill, and many would probably have died even if the devices had worked correctly.
The problems the FDA identified range across all manufacturers of the devices. They involve shortcomings in engineering, design practices, and manufacturing practices, poor communication to users, and lack of adverse event reporting.
For example, some manufacturers have used a "fix-on-fail" strategy for dealing with problems. "Fix on fail" refers to the practice of identifying and fixing problems with individual devices on a case-by-case basis instead of informing all users of the problems as part of a recall.
Under the new initiative, the agency will collaborate with manufacturers and others to facilitate the development of the next generation of defibrillators. To further these efforts, the agency will hold a public workshop on Dec. 15-16, intended to bring together government, industry, academia, and clinicians.
The FDA also will work with manufacturers to improve the way they respond to user complaints, conduct recalls, and report adverse events.
Finally, the FDA will propose changes to the classification of AEDs and changes to the premarket regulatory pathway of these devices. The agency plans to announce those proposed changes in 2011.
"I think it’s important to reiterate that we consider these to be lifesaving technologies" Dr. Shuren said during the press briefing. "We’re not taking any of these devices off the market. We’re strongly encouraging people to continue to use them and to use them according to guidelines. And we think that these technologies can improve to reduce the rate of failures that we’ve seen."
A new FDA initiative intended to improve the reliability of external defibrillators will address manufacturing and engineering design practices, poor communication to users, and lack of adverse event reporting.
A new initiative aimed at improving the reliability of external defibrillators has been launched by the Food and Drug Administration, the agency announced Nov. 15.
The initiative includes external defibrillators used by medical professionals as well as automated external defibrillators (AEDs) intended for use by members of the public.
According to the FDA, the agency’s Center for Devices and Radiological Health (CDRH) has received more than 28,000 reports of device failures associated with external defibrillators during the past 5 years. Manufacturers have conducted 68 recalls from Jan. 1, 2005 to July 10, 2010.
During a news briefing, Dr. Jeffrey Shuren, director of CDRH, said that 700 deaths had been associated with device failures, but that it’s difficult to determine how many of those resulted directly from malfunctions of the devices. Having suffered cardiac defibrillation, the patients were, of course, very ill, and many would probably have died even if the devices had worked correctly.
The problems the FDA identified range across all manufacturers of the devices. They involve shortcomings in engineering, design practices, and manufacturing practices, poor communication to users, and lack of adverse event reporting.
For example, some manufacturers have used a "fix-on-fail" strategy for dealing with problems. "Fix on fail" refers to the practice of identifying and fixing problems with individual devices on a case-by-case basis instead of informing all users of the problems as part of a recall.
Under the new initiative, the agency will collaborate with manufacturers and others to facilitate the development of the next generation of defibrillators. To further these efforts, the agency will hold a public workshop on Dec. 15-16, intended to bring together government, industry, academia, and clinicians.
The FDA also will work with manufacturers to improve the way they respond to user complaints, conduct recalls, and report adverse events.
Finally, the FDA will propose changes to the classification of AEDs and changes to the premarket regulatory pathway of these devices. The agency plans to announce those proposed changes in 2011.
"I think it’s important to reiterate that we consider these to be lifesaving technologies" Dr. Shuren said during the press briefing. "We’re not taking any of these devices off the market. We’re strongly encouraging people to continue to use them and to use them according to guidelines. And we think that these technologies can improve to reduce the rate of failures that we’ve seen."
A new FDA initiative intended to improve the reliability of external defibrillators will address manufacturing and engineering design practices, poor communication to users, and lack of adverse event reporting.
A new initiative aimed at improving the reliability of external defibrillators has been launched by the Food and Drug Administration, the agency announced Nov. 15.
The initiative includes external defibrillators used by medical professionals as well as automated external defibrillators (AEDs) intended for use by members of the public.
According to the FDA, the agency’s Center for Devices and Radiological Health (CDRH) has received more than 28,000 reports of device failures associated with external defibrillators during the past 5 years. Manufacturers have conducted 68 recalls from Jan. 1, 2005 to July 10, 2010.
During a news briefing, Dr. Jeffrey Shuren, director of CDRH, said that 700 deaths had been associated with device failures, but that it’s difficult to determine how many of those resulted directly from malfunctions of the devices. Having suffered cardiac defibrillation, the patients were, of course, very ill, and many would probably have died even if the devices had worked correctly.
The problems the FDA identified range across all manufacturers of the devices. They involve shortcomings in engineering, design practices, and manufacturing practices, poor communication to users, and lack of adverse event reporting.
For example, some manufacturers have used a "fix-on-fail" strategy for dealing with problems. "Fix on fail" refers to the practice of identifying and fixing problems with individual devices on a case-by-case basis instead of informing all users of the problems as part of a recall.
Under the new initiative, the agency will collaborate with manufacturers and others to facilitate the development of the next generation of defibrillators. To further these efforts, the agency will hold a public workshop on Dec. 15-16, intended to bring together government, industry, academia, and clinicians.
The FDA also will work with manufacturers to improve the way they respond to user complaints, conduct recalls, and report adverse events.
Finally, the FDA will propose changes to the classification of AEDs and changes to the premarket regulatory pathway of these devices. The agency plans to announce those proposed changes in 2011.
"I think it’s important to reiterate that we consider these to be lifesaving technologies" Dr. Shuren said during the press briefing. "We’re not taking any of these devices off the market. We’re strongly encouraging people to continue to use them and to use them according to guidelines. And we think that these technologies can improve to reduce the rate of failures that we’ve seen."
A new FDA initiative intended to improve the reliability of external defibrillators will address manufacturing and engineering design practices, poor communication to users, and lack of adverse event reporting.
FROM AN FDA TELEBRIEFING
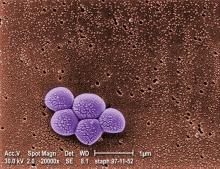
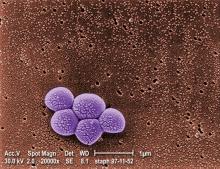
Agents in Pipeline May Help Combat MRSA
Major Finding: Fusidic acid inhibited 99.6% of 7,340 isolates of Staphylococcus aureus. Tested against 511 S. aureus isolates, JNJ-Q2 was 16 times more potent than moxifloxacin, 64 times more potent than levofloxacin, and 128 times more potent than ciprofloxacin. Ceftaroline is highly active against methicillin-resistant S. aureus itself, but when combined with NXL104 it is also at least as active as carbapenems and fourth-generation cephalosporins against Enterobacteriaceae producing derepressed AmpC beta-lactamase.
Data Source: Three separate in vitro studies.
Disclosures: The study on CXL104 was supported by Forest Laboratories, and the study on JNJ-Q2 was supported by Furiex Pharmaceuticals. JMI Laboratories conducts studies supported by Forest, Furiex, and other pharmaceutical companies.
VANCOUVER, B.C. – New compounds in preclinical stages of testing may eventually help combat the surge in methicillin-resistant Staphylococcus aureus and other multidrug-resistant organisms, Dr. Ronald N. Jones said at the meeting.
Fusidic acid was discovered in the 1960s and used widely in Europe, Australia, and Canada. However because it was never released in the United States, domestic MRSA strains have built up little resistance to it, which makes it something of “an old drug in new clothing,” said the chief executive officer of JMI Laboratories, a contract research organization in North Liberty, Iowa.
Dr. Jones and his colleagues tested the compound against 7,340 S. aureus isolates collected from 51 hospitals in every region of the country. Fusidic acid inhibited 99.6% of the isolates at a concentration of 1 mcg/mL or less. The compound also showed comparable activity against S. aureus strains in eight different resistance groups, including strains resistant to five or more other compounds including oxacillin, erythromycin, clindamycin, and the fluoroquinolones.
“This is pretty exciting, because it also has no cross-resistance with any other class of antibiotic,” Dr. Jones said. “It could be used widely if we could deliver it in such a way that would prevent any emerging resistance from happening in what I call the naïve population of United States Staph aureus.”
In addition, Dr. Jones said, “it's been conservatively stated that tens of millions of patients have been treated with fusidic acid over the period of the 4-plus decades. The drug is considered safe, and it's usually administered orally for the treatment of serious staphylococcal infections. It also has been applied in some countries topically.”
A second agent, JNJ-Q2, is a broad-spectrum fluoroquinolone developed by Johnson & Johnson and Furiex Pharmaceuticals.
“One of the things that was noted very early on is that quinolone resistance, particularly among methicillin-resistant staphylococci, became quite common over a decade ago,” Dr. Jones said. “New compounds have been tried for a number of years, [but] what's novel about this is it's 16 times more potent than the best of the existing marketed fluoroquinolones.”
JNJ-Q2 is moving into phase II and phase III clinical trials. In preclinical studies, “We challenged it with the worst of the MRSA and the fluoroquinolone-resistant MRSA that we could find in our surveillance systems all around the planet. And this new compound came out quite well and covered essentially 90%-100% of the strains, depending upon the geography.”
Compared with other fluoroquinolones, JNJ-Q2 was 16 times more potent than moxifloxacin, 64 times more potent than levofloxacin, and 128 times more potent than ciprofloxacin when tested against 511 S. aureus isolates.
A third agent, ceftaroline, is a broad-spectrum cephalosporin from Forest Laboratories. It is being tested in combination with NXL104, a beta-lactamase inhibitor being developed by Novexel.
Dr. Jones pointed out that ceftaroline alone is active against MRSA and multidrug-resistant pneumococci, but when combined with NXL104, it could also be used against the growing population of Enterobacteriaceae that produce derepressed AmpC beta-lactamase.
In studies, Dr. Jones and his colleagues determined that the combination, which they refer to as CXL104, inhibited 96% of ceftazidime-resistant strains of Enterobacter, Citrobacter, and Serratia at concentrations of 4 mcg/mL or lower.
“It's probably not going to be on the market until 2013 or 2014, [but will probably have labeling] against a large number of indications if everything goes well in clinical trials,” Dr. Jones said.
Major Finding: Fusidic acid inhibited 99.6% of 7,340 isolates of Staphylococcus aureus. Tested against 511 S. aureus isolates, JNJ-Q2 was 16 times more potent than moxifloxacin, 64 times more potent than levofloxacin, and 128 times more potent than ciprofloxacin. Ceftaroline is highly active against methicillin-resistant S. aureus itself, but when combined with NXL104 it is also at least as active as carbapenems and fourth-generation cephalosporins against Enterobacteriaceae producing derepressed AmpC beta-lactamase.
Data Source: Three separate in vitro studies.
Disclosures: The study on CXL104 was supported by Forest Laboratories, and the study on JNJ-Q2 was supported by Furiex Pharmaceuticals. JMI Laboratories conducts studies supported by Forest, Furiex, and other pharmaceutical companies.
VANCOUVER, B.C. – New compounds in preclinical stages of testing may eventually help combat the surge in methicillin-resistant Staphylococcus aureus and other multidrug-resistant organisms, Dr. Ronald N. Jones said at the meeting.
Fusidic acid was discovered in the 1960s and used widely in Europe, Australia, and Canada. However because it was never released in the United States, domestic MRSA strains have built up little resistance to it, which makes it something of “an old drug in new clothing,” said the chief executive officer of JMI Laboratories, a contract research organization in North Liberty, Iowa.
Dr. Jones and his colleagues tested the compound against 7,340 S. aureus isolates collected from 51 hospitals in every region of the country. Fusidic acid inhibited 99.6% of the isolates at a concentration of 1 mcg/mL or less. The compound also showed comparable activity against S. aureus strains in eight different resistance groups, including strains resistant to five or more other compounds including oxacillin, erythromycin, clindamycin, and the fluoroquinolones.
“This is pretty exciting, because it also has no cross-resistance with any other class of antibiotic,” Dr. Jones said. “It could be used widely if we could deliver it in such a way that would prevent any emerging resistance from happening in what I call the naïve population of United States Staph aureus.”
In addition, Dr. Jones said, “it's been conservatively stated that tens of millions of patients have been treated with fusidic acid over the period of the 4-plus decades. The drug is considered safe, and it's usually administered orally for the treatment of serious staphylococcal infections. It also has been applied in some countries topically.”
A second agent, JNJ-Q2, is a broad-spectrum fluoroquinolone developed by Johnson & Johnson and Furiex Pharmaceuticals.
“One of the things that was noted very early on is that quinolone resistance, particularly among methicillin-resistant staphylococci, became quite common over a decade ago,” Dr. Jones said. “New compounds have been tried for a number of years, [but] what's novel about this is it's 16 times more potent than the best of the existing marketed fluoroquinolones.”
JNJ-Q2 is moving into phase II and phase III clinical trials. In preclinical studies, “We challenged it with the worst of the MRSA and the fluoroquinolone-resistant MRSA that we could find in our surveillance systems all around the planet. And this new compound came out quite well and covered essentially 90%-100% of the strains, depending upon the geography.”
Compared with other fluoroquinolones, JNJ-Q2 was 16 times more potent than moxifloxacin, 64 times more potent than levofloxacin, and 128 times more potent than ciprofloxacin when tested against 511 S. aureus isolates.
A third agent, ceftaroline, is a broad-spectrum cephalosporin from Forest Laboratories. It is being tested in combination with NXL104, a beta-lactamase inhibitor being developed by Novexel.
Dr. Jones pointed out that ceftaroline alone is active against MRSA and multidrug-resistant pneumococci, but when combined with NXL104, it could also be used against the growing population of Enterobacteriaceae that produce derepressed AmpC beta-lactamase.
In studies, Dr. Jones and his colleagues determined that the combination, which they refer to as CXL104, inhibited 96% of ceftazidime-resistant strains of Enterobacter, Citrobacter, and Serratia at concentrations of 4 mcg/mL or lower.
“It's probably not going to be on the market until 2013 or 2014, [but will probably have labeling] against a large number of indications if everything goes well in clinical trials,” Dr. Jones said.
Major Finding: Fusidic acid inhibited 99.6% of 7,340 isolates of Staphylococcus aureus. Tested against 511 S. aureus isolates, JNJ-Q2 was 16 times more potent than moxifloxacin, 64 times more potent than levofloxacin, and 128 times more potent than ciprofloxacin. Ceftaroline is highly active against methicillin-resistant S. aureus itself, but when combined with NXL104 it is also at least as active as carbapenems and fourth-generation cephalosporins against Enterobacteriaceae producing derepressed AmpC beta-lactamase.
Data Source: Three separate in vitro studies.
Disclosures: The study on CXL104 was supported by Forest Laboratories, and the study on JNJ-Q2 was supported by Furiex Pharmaceuticals. JMI Laboratories conducts studies supported by Forest, Furiex, and other pharmaceutical companies.
VANCOUVER, B.C. – New compounds in preclinical stages of testing may eventually help combat the surge in methicillin-resistant Staphylococcus aureus and other multidrug-resistant organisms, Dr. Ronald N. Jones said at the meeting.
Fusidic acid was discovered in the 1960s and used widely in Europe, Australia, and Canada. However because it was never released in the United States, domestic MRSA strains have built up little resistance to it, which makes it something of “an old drug in new clothing,” said the chief executive officer of JMI Laboratories, a contract research organization in North Liberty, Iowa.
Dr. Jones and his colleagues tested the compound against 7,340 S. aureus isolates collected from 51 hospitals in every region of the country. Fusidic acid inhibited 99.6% of the isolates at a concentration of 1 mcg/mL or less. The compound also showed comparable activity against S. aureus strains in eight different resistance groups, including strains resistant to five or more other compounds including oxacillin, erythromycin, clindamycin, and the fluoroquinolones.
“This is pretty exciting, because it also has no cross-resistance with any other class of antibiotic,” Dr. Jones said. “It could be used widely if we could deliver it in such a way that would prevent any emerging resistance from happening in what I call the naïve population of United States Staph aureus.”
In addition, Dr. Jones said, “it's been conservatively stated that tens of millions of patients have been treated with fusidic acid over the period of the 4-plus decades. The drug is considered safe, and it's usually administered orally for the treatment of serious staphylococcal infections. It also has been applied in some countries topically.”
A second agent, JNJ-Q2, is a broad-spectrum fluoroquinolone developed by Johnson & Johnson and Furiex Pharmaceuticals.
“One of the things that was noted very early on is that quinolone resistance, particularly among methicillin-resistant staphylococci, became quite common over a decade ago,” Dr. Jones said. “New compounds have been tried for a number of years, [but] what's novel about this is it's 16 times more potent than the best of the existing marketed fluoroquinolones.”
JNJ-Q2 is moving into phase II and phase III clinical trials. In preclinical studies, “We challenged it with the worst of the MRSA and the fluoroquinolone-resistant MRSA that we could find in our surveillance systems all around the planet. And this new compound came out quite well and covered essentially 90%-100% of the strains, depending upon the geography.”
Compared with other fluoroquinolones, JNJ-Q2 was 16 times more potent than moxifloxacin, 64 times more potent than levofloxacin, and 128 times more potent than ciprofloxacin when tested against 511 S. aureus isolates.
A third agent, ceftaroline, is a broad-spectrum cephalosporin from Forest Laboratories. It is being tested in combination with NXL104, a beta-lactamase inhibitor being developed by Novexel.
Dr. Jones pointed out that ceftaroline alone is active against MRSA and multidrug-resistant pneumococci, but when combined with NXL104, it could also be used against the growing population of Enterobacteriaceae that produce derepressed AmpC beta-lactamase.
In studies, Dr. Jones and his colleagues determined that the combination, which they refer to as CXL104, inhibited 96% of ceftazidime-resistant strains of Enterobacter, Citrobacter, and Serratia at concentrations of 4 mcg/mL or lower.
“It's probably not going to be on the market until 2013 or 2014, [but will probably have labeling] against a large number of indications if everything goes well in clinical trials,” Dr. Jones said.
Cure Rates Similar for Mesh/No Mesh Prolapse Repair
LONG BEACH, CALIF. – A randomized controlled trial found no advantage for vaginal prolapse repair using mesh colpopexy compared with no-mesh repair, said Dr. Andrew I. Sokol of Washington (D.C.) Hospital Center.
After a mean follow-up of 14.7 months in this study of 65 women, 96% of women having mesh colpopexy with Prolift and 92% of women undergoing vaginal colpopexy without mesh were free of bulge symptoms; 25% of the mesh group and 22% of the no-mesh group experienced recurrent prolapse beyond the hymen. Neither of these differences was significant.
A total of 38% of women in the mesh group, compared with 30% of women in the no-mesh group, achieved optimal scores (stage 1 or below) on the pelvic organ prolapse quantification (POP-Q) scale, a difference that was not significant.
On the other hand, the vaginal mesh erosion rate was relatively high at 15.6%, and the data safety monitoring board terminated the study early because of this, Dr. Sokol said at the meeting.
In addition, there were three reoperations for erosion and three reoperations for prolapse among patients in the mesh group, compared with no reoperations in the no-mesh group, a significant difference.
In October 2008 the Food and Drug Administration issued a formal notification on reported complications from mesh use. Recognizing the high complication rate, mesh manufacturers have developed lighter-weight and mixed composite meshes.
The study included 65 women who were at POP-Q stages 2-4 uterovaginal or vaginal prolapse and who desired vaginal reconstructive surgery; the mean age in both groups was 64 years.
The study was supported by research grants from the AUGS Foundation and the MedStar Health Research Institute. Ethicon Women's Health and Urology donated the Prolift mesh kits for this study.
Dr. Sokol stated that he had no conflicts of interest.
LONG BEACH, CALIF. – A randomized controlled trial found no advantage for vaginal prolapse repair using mesh colpopexy compared with no-mesh repair, said Dr. Andrew I. Sokol of Washington (D.C.) Hospital Center.
After a mean follow-up of 14.7 months in this study of 65 women, 96% of women having mesh colpopexy with Prolift and 92% of women undergoing vaginal colpopexy without mesh were free of bulge symptoms; 25% of the mesh group and 22% of the no-mesh group experienced recurrent prolapse beyond the hymen. Neither of these differences was significant.
A total of 38% of women in the mesh group, compared with 30% of women in the no-mesh group, achieved optimal scores (stage 1 or below) on the pelvic organ prolapse quantification (POP-Q) scale, a difference that was not significant.
On the other hand, the vaginal mesh erosion rate was relatively high at 15.6%, and the data safety monitoring board terminated the study early because of this, Dr. Sokol said at the meeting.
In addition, there were three reoperations for erosion and three reoperations for prolapse among patients in the mesh group, compared with no reoperations in the no-mesh group, a significant difference.
In October 2008 the Food and Drug Administration issued a formal notification on reported complications from mesh use. Recognizing the high complication rate, mesh manufacturers have developed lighter-weight and mixed composite meshes.
The study included 65 women who were at POP-Q stages 2-4 uterovaginal or vaginal prolapse and who desired vaginal reconstructive surgery; the mean age in both groups was 64 years.
The study was supported by research grants from the AUGS Foundation and the MedStar Health Research Institute. Ethicon Women's Health and Urology donated the Prolift mesh kits for this study.
Dr. Sokol stated that he had no conflicts of interest.
LONG BEACH, CALIF. – A randomized controlled trial found no advantage for vaginal prolapse repair using mesh colpopexy compared with no-mesh repair, said Dr. Andrew I. Sokol of Washington (D.C.) Hospital Center.
After a mean follow-up of 14.7 months in this study of 65 women, 96% of women having mesh colpopexy with Prolift and 92% of women undergoing vaginal colpopexy without mesh were free of bulge symptoms; 25% of the mesh group and 22% of the no-mesh group experienced recurrent prolapse beyond the hymen. Neither of these differences was significant.
A total of 38% of women in the mesh group, compared with 30% of women in the no-mesh group, achieved optimal scores (stage 1 or below) on the pelvic organ prolapse quantification (POP-Q) scale, a difference that was not significant.
On the other hand, the vaginal mesh erosion rate was relatively high at 15.6%, and the data safety monitoring board terminated the study early because of this, Dr. Sokol said at the meeting.
In addition, there were three reoperations for erosion and three reoperations for prolapse among patients in the mesh group, compared with no reoperations in the no-mesh group, a significant difference.
In October 2008 the Food and Drug Administration issued a formal notification on reported complications from mesh use. Recognizing the high complication rate, mesh manufacturers have developed lighter-weight and mixed composite meshes.
The study included 65 women who were at POP-Q stages 2-4 uterovaginal or vaginal prolapse and who desired vaginal reconstructive surgery; the mean age in both groups was 64 years.
The study was supported by research grants from the AUGS Foundation and the MedStar Health Research Institute. Ethicon Women's Health and Urology donated the Prolift mesh kits for this study.
Dr. Sokol stated that he had no conflicts of interest.
Agents in Pipeline May Help Combat MRSA
VANCOUVER, B.C. – New compounds in preclinical stages of testing may eventually help combat the surge in methicillin-resistant Staphylococcus aureus and other multidrug resistant organisms, Dr. Ronald N. Jones said at the annual meeting of the Infectious Diseases Society of America.
Fusidic acid was discovered in the 1960s and used widely in Europe, Australia, and Canada. However because it was never released in the United States, domestic MRSA strains have built up little resistance to it, which makes it something of "an old drug in new clothing," said the chief executive officer of JMI Laboratories, a contract research organization in North Liberty, Iowa.
Dr. Jones and his colleagues tested the compound against 7,340 S. aureus isolates collected from 51 hospitals in every region of the country. Fusidic acid inhibited 99.6% of the isolates at a concentration of 1 mcg/mL or less. The compound also showed comparable activity against S. aureus strains in eight different resistance groups, including strains resistant to five or more other compounds including oxacillin, erythromycin, clindamycin, and the fluoroquinolones.
"This is pretty exciting, because it also has no cross-resistance with any other class of antibiotic," Dr. Jones said. "It could be used widely if we could deliver it in such a way that would prevent any emerging resistance from happening in what I call the naïve population of United States Staph aureus."
In addition, Dr. Jones said, "it's been conservatively stated that tens of millions of patients have been treated with fusidic acid over the period of the four-plus decades. The drug is considered safe, and it's usually administered orally for the treatment of serious staphylococcal infections. It also has been applied in some countries topically."
A second agent, JNJ-Q2, is a broad-spectrum fluoroquinolone developed by Johnson & Johnson and Furiex Pharmaceuticals.
"One of the things that was noted very early on is that quinolone resistance, particularly among methicillin-resistant staphylococci, became quite common over a decade ago," Dr. Jones said. "New compounds have been tried for a number of years, [but] what's novel about this is it’s 16 times more potent than the best of the existing marketed fluoroquinolones."
JNJ-Q2 is moving into phase II and phase III clinical trials. In preclinical studies, "We challenged it with the worst of the MRSA and the fluoroquinolone-resistant MRSA that we could find in our surveillance systems all around the planet. And this new compound came out quite well and covered essentially 90%-100% of the strains, depending upon the geography."
In comparison to other fluoroquinolones, JNJ-Q2 was 16 times more potent than moxifloxacin, 64 times more potent than levofloxacin, and 128 times more potent than ciprofloxacin when tested against 511 S. aureus isolates.
A third agent, ceftaroline, is a broad-spectrum cephalosporin from Forest Laboratories. It is being tested in combination with NXL104, a beta-lactamase inhibitor being developed by Novexel.
Dr. Jones pointed out that ceftaroline alone is active against MRSA and multidrug resistant pneumococci, but when combined with NXL104, it could also be used against the growing population of Enterobacteriaceae that produce derepressed AmpC beta-lactamase.
In studies, Dr. Jones and his colleagues determined that the combination, which they refer to as CXL104, inhibited 96% of ceftazidime-resistant strains of Enterobacter, Citrobacter, and Serratia at concentrations of 4 mcg/mL or lower.
"It's probably not going to be on the market until 2013 or 2014, [but will probably have labeling] against a large number of indications if everything goes well in clinical trials," Dr. Jones said.
The study on CXL104 was supported by Forest Laboratories, and the study on JNJ-Q2 was supported by Furiex Pharmaceuticals. JMI Laboratories conducts studies supported by Forest, Furiex, and other pharmaceutical companies.
VANCOUVER, B.C. – New compounds in preclinical stages of testing may eventually help combat the surge in methicillin-resistant Staphylococcus aureus and other multidrug resistant organisms, Dr. Ronald N. Jones said at the annual meeting of the Infectious Diseases Society of America.
Fusidic acid was discovered in the 1960s and used widely in Europe, Australia, and Canada. However because it was never released in the United States, domestic MRSA strains have built up little resistance to it, which makes it something of "an old drug in new clothing," said the chief executive officer of JMI Laboratories, a contract research organization in North Liberty, Iowa.
Dr. Jones and his colleagues tested the compound against 7,340 S. aureus isolates collected from 51 hospitals in every region of the country. Fusidic acid inhibited 99.6% of the isolates at a concentration of 1 mcg/mL or less. The compound also showed comparable activity against S. aureus strains in eight different resistance groups, including strains resistant to five or more other compounds including oxacillin, erythromycin, clindamycin, and the fluoroquinolones.
"This is pretty exciting, because it also has no cross-resistance with any other class of antibiotic," Dr. Jones said. "It could be used widely if we could deliver it in such a way that would prevent any emerging resistance from happening in what I call the naïve population of United States Staph aureus."
In addition, Dr. Jones said, "it's been conservatively stated that tens of millions of patients have been treated with fusidic acid over the period of the four-plus decades. The drug is considered safe, and it's usually administered orally for the treatment of serious staphylococcal infections. It also has been applied in some countries topically."
A second agent, JNJ-Q2, is a broad-spectrum fluoroquinolone developed by Johnson & Johnson and Furiex Pharmaceuticals.
"One of the things that was noted very early on is that quinolone resistance, particularly among methicillin-resistant staphylococci, became quite common over a decade ago," Dr. Jones said. "New compounds have been tried for a number of years, [but] what's novel about this is it’s 16 times more potent than the best of the existing marketed fluoroquinolones."
JNJ-Q2 is moving into phase II and phase III clinical trials. In preclinical studies, "We challenged it with the worst of the MRSA and the fluoroquinolone-resistant MRSA that we could find in our surveillance systems all around the planet. And this new compound came out quite well and covered essentially 90%-100% of the strains, depending upon the geography."
In comparison to other fluoroquinolones, JNJ-Q2 was 16 times more potent than moxifloxacin, 64 times more potent than levofloxacin, and 128 times more potent than ciprofloxacin when tested against 511 S. aureus isolates.
A third agent, ceftaroline, is a broad-spectrum cephalosporin from Forest Laboratories. It is being tested in combination with NXL104, a beta-lactamase inhibitor being developed by Novexel.
Dr. Jones pointed out that ceftaroline alone is active against MRSA and multidrug resistant pneumococci, but when combined with NXL104, it could also be used against the growing population of Enterobacteriaceae that produce derepressed AmpC beta-lactamase.
In studies, Dr. Jones and his colleagues determined that the combination, which they refer to as CXL104, inhibited 96% of ceftazidime-resistant strains of Enterobacter, Citrobacter, and Serratia at concentrations of 4 mcg/mL or lower.
"It's probably not going to be on the market until 2013 or 2014, [but will probably have labeling] against a large number of indications if everything goes well in clinical trials," Dr. Jones said.
The study on CXL104 was supported by Forest Laboratories, and the study on JNJ-Q2 was supported by Furiex Pharmaceuticals. JMI Laboratories conducts studies supported by Forest, Furiex, and other pharmaceutical companies.
VANCOUVER, B.C. – New compounds in preclinical stages of testing may eventually help combat the surge in methicillin-resistant Staphylococcus aureus and other multidrug resistant organisms, Dr. Ronald N. Jones said at the annual meeting of the Infectious Diseases Society of America.
Fusidic acid was discovered in the 1960s and used widely in Europe, Australia, and Canada. However because it was never released in the United States, domestic MRSA strains have built up little resistance to it, which makes it something of "an old drug in new clothing," said the chief executive officer of JMI Laboratories, a contract research organization in North Liberty, Iowa.
Dr. Jones and his colleagues tested the compound against 7,340 S. aureus isolates collected from 51 hospitals in every region of the country. Fusidic acid inhibited 99.6% of the isolates at a concentration of 1 mcg/mL or less. The compound also showed comparable activity against S. aureus strains in eight different resistance groups, including strains resistant to five or more other compounds including oxacillin, erythromycin, clindamycin, and the fluoroquinolones.
"This is pretty exciting, because it also has no cross-resistance with any other class of antibiotic," Dr. Jones said. "It could be used widely if we could deliver it in such a way that would prevent any emerging resistance from happening in what I call the naïve population of United States Staph aureus."
In addition, Dr. Jones said, "it's been conservatively stated that tens of millions of patients have been treated with fusidic acid over the period of the four-plus decades. The drug is considered safe, and it's usually administered orally for the treatment of serious staphylococcal infections. It also has been applied in some countries topically."
A second agent, JNJ-Q2, is a broad-spectrum fluoroquinolone developed by Johnson & Johnson and Furiex Pharmaceuticals.
"One of the things that was noted very early on is that quinolone resistance, particularly among methicillin-resistant staphylococci, became quite common over a decade ago," Dr. Jones said. "New compounds have been tried for a number of years, [but] what's novel about this is it’s 16 times more potent than the best of the existing marketed fluoroquinolones."
JNJ-Q2 is moving into phase II and phase III clinical trials. In preclinical studies, "We challenged it with the worst of the MRSA and the fluoroquinolone-resistant MRSA that we could find in our surveillance systems all around the planet. And this new compound came out quite well and covered essentially 90%-100% of the strains, depending upon the geography."
In comparison to other fluoroquinolones, JNJ-Q2 was 16 times more potent than moxifloxacin, 64 times more potent than levofloxacin, and 128 times more potent than ciprofloxacin when tested against 511 S. aureus isolates.
A third agent, ceftaroline, is a broad-spectrum cephalosporin from Forest Laboratories. It is being tested in combination with NXL104, a beta-lactamase inhibitor being developed by Novexel.
Dr. Jones pointed out that ceftaroline alone is active against MRSA and multidrug resistant pneumococci, but when combined with NXL104, it could also be used against the growing population of Enterobacteriaceae that produce derepressed AmpC beta-lactamase.
In studies, Dr. Jones and his colleagues determined that the combination, which they refer to as CXL104, inhibited 96% of ceftazidime-resistant strains of Enterobacter, Citrobacter, and Serratia at concentrations of 4 mcg/mL or lower.
"It's probably not going to be on the market until 2013 or 2014, [but will probably have labeling] against a large number of indications if everything goes well in clinical trials," Dr. Jones said.
The study on CXL104 was supported by Forest Laboratories, and the study on JNJ-Q2 was supported by Furiex Pharmaceuticals. JMI Laboratories conducts studies supported by Forest, Furiex, and other pharmaceutical companies.
FROM THE ANNUAL MEETING OF THE INFECTIOUS DISEASES SOCIETY OF AMERICA
Major Finding: Fusidic acid inhibited 99.6% of 7,340 isolates of Staphylococcus aureus. Tested against 511 S. aureus isolates, JNJ-Q2 was 16 times more potent than moxifloxacin, 64 times more potent than levofloxacin, and 128 times more potent than ciprofloxacin. Ceftaroline is highly active against methicillin-resistant S. aureus itself, but when combined with NXL104 it is also at least as active as carbapenems and fourth-generation cephalosporins against Enterobacteriaceae producing derepressed AmpC beta-lactamase.
Data Source: Three separate in vitro studies.
Disclosures: The study on CXL104 was supported by Forest Laboratories, and the study on JNJ-Q2 was supported by Furiex Pharmaceuticals. JMI Laboratories conducts studies supported by Forest, Furiex, and other pharmaceutical companies.
Agents in Pipeline May Help Combat MRSA
VANCOUVER, B.C. – New compounds in preclinical stages of testing may eventually help combat the surge in methicillin-resistant Staphylococcus aureus and other multidrug resistant organisms, Dr. Ronald N. Jones said at the annual meeting of the Infectious Diseases Society of America .
Fusidic acid was discovered in the 1960s and used widely in Europe, Australia, and Canada. However because it was never released in the United States, domestic MRSA strains have built up little resistance to it, which makes it something of "an old drug in new clothing," said the chief executive officer of JMI Laboratories, a contract research organization in North Liberty, Iowa.
Dr. Jones and his colleagues tested the compound against 7,340 S. aureus isolates collected from 51 hospitals in every region of the country. Fusidic acid inhibited 99.6% of the isolates at a concentration of 1 mcg/mL or less. The compound also showed comparable activity against S. aureus strains in eight different resistance groups, including strains resistant to five or more other compounds including oxacillin, erythromycin, clindamycin, and the fluoroquinolones.
"This is pretty exciting, because it also has no cross-resistance with any other class of antibiotic," Dr. Jones said. "It could be used widely if we could deliver it in such a way that would prevent any emerging resistance from happening in what I call the naïve population of United States Staph aureus."
In addition, Dr. Jones said, "it’s been conservatively stated that tens of millions of patients have been treated with fusidic acid over the period of the four-plus decades. The drug is considered safe, and it’s usually administered orally for the treatment of serious staphylococcal infections. It also has been applied in some countries topically."
A second agent, JNJ-Q2, is a broad-spectrum fluoroquinolone developed by Johnson & Johnson and Furiex Pharmaceuticals.
"One of the things that was noted very early on is that quinolone resistance, particularly among methicillin-resistant staphylococci, became quite common over a decade ago," Dr. Jones said. "New compounds have been tried for a number of years, [but] what’s novel about this is it’s 16 times more potent than the best of the existing marketed fluoroquinolones."
JNJ-Q2 is moving into phase II and phase III clinical trials. In preclinical studies, "We challenged it with the worst of the MRSA and the fluoroquinolone-resistant MRSA that we could find in our surveillance systems all around the planet. And this new compound came out quite well and covered essentially 90%-100% of the strains, depending upon the geography."
In comparison to other fluoroquinolones, JNJ-Q2 was 16 times more potent than moxifloxacin, 64 times more potent than levofloxacin, and 128 times more potent than ciprofloxacin when tested against 511 S. aureus isolates.
A third agent, ceftaroline, is a broad-spectrum cephalosporin from Forest Laboratories. It is being tested in combination with NXL104, a beta-lactamase inhibitor being developed by Novexel.
Dr. Jones pointed out that ceftaroline alone is active against MRSA and multidrug resistant pneumococci, but when combined with NXL104, it could also be used against the growing population of Enterobacteriaceae that produce derepressed AmpC beta-lactamase.
In studies, Dr. Jones and his colleagues determined that the combination, which they refer to as CXL104, inhibited 96% of ceftazidime-resistant strains of Enterobacter, Citrobacter, and Serratia at concentrations of 4 mcg/mL or lower.
"It’s probably not going to be on the market until 2013 or 2014, [but will probably have labeling] against a large number of indications if everything goes well in clinical trials," Dr. Jones said.
The study on CXL104 was supported by Forest Laboratories, and the study on JNJ-Q2 was supported by Furiex Pharmaceuticals. JMI Laboratories conducts studies supported by Forest, Furiex, and other pharmaceutical companies.
VANCOUVER, B.C. – New compounds in preclinical stages of testing may eventually help combat the surge in methicillin-resistant Staphylococcus aureus and other multidrug resistant organisms, Dr. Ronald N. Jones said at the annual meeting of the Infectious Diseases Society of America .
Fusidic acid was discovered in the 1960s and used widely in Europe, Australia, and Canada. However because it was never released in the United States, domestic MRSA strains have built up little resistance to it, which makes it something of "an old drug in new clothing," said the chief executive officer of JMI Laboratories, a contract research organization in North Liberty, Iowa.
Dr. Jones and his colleagues tested the compound against 7,340 S. aureus isolates collected from 51 hospitals in every region of the country. Fusidic acid inhibited 99.6% of the isolates at a concentration of 1 mcg/mL or less. The compound also showed comparable activity against S. aureus strains in eight different resistance groups, including strains resistant to five or more other compounds including oxacillin, erythromycin, clindamycin, and the fluoroquinolones.
"This is pretty exciting, because it also has no cross-resistance with any other class of antibiotic," Dr. Jones said. "It could be used widely if we could deliver it in such a way that would prevent any emerging resistance from happening in what I call the naïve population of United States Staph aureus."
In addition, Dr. Jones said, "it’s been conservatively stated that tens of millions of patients have been treated with fusidic acid over the period of the four-plus decades. The drug is considered safe, and it’s usually administered orally for the treatment of serious staphylococcal infections. It also has been applied in some countries topically."
A second agent, JNJ-Q2, is a broad-spectrum fluoroquinolone developed by Johnson & Johnson and Furiex Pharmaceuticals.
"One of the things that was noted very early on is that quinolone resistance, particularly among methicillin-resistant staphylococci, became quite common over a decade ago," Dr. Jones said. "New compounds have been tried for a number of years, [but] what’s novel about this is it’s 16 times more potent than the best of the existing marketed fluoroquinolones."
JNJ-Q2 is moving into phase II and phase III clinical trials. In preclinical studies, "We challenged it with the worst of the MRSA and the fluoroquinolone-resistant MRSA that we could find in our surveillance systems all around the planet. And this new compound came out quite well and covered essentially 90%-100% of the strains, depending upon the geography."
In comparison to other fluoroquinolones, JNJ-Q2 was 16 times more potent than moxifloxacin, 64 times more potent than levofloxacin, and 128 times more potent than ciprofloxacin when tested against 511 S. aureus isolates.
A third agent, ceftaroline, is a broad-spectrum cephalosporin from Forest Laboratories. It is being tested in combination with NXL104, a beta-lactamase inhibitor being developed by Novexel.
Dr. Jones pointed out that ceftaroline alone is active against MRSA and multidrug resistant pneumococci, but when combined with NXL104, it could also be used against the growing population of Enterobacteriaceae that produce derepressed AmpC beta-lactamase.
In studies, Dr. Jones and his colleagues determined that the combination, which they refer to as CXL104, inhibited 96% of ceftazidime-resistant strains of Enterobacter, Citrobacter, and Serratia at concentrations of 4 mcg/mL or lower.
"It’s probably not going to be on the market until 2013 or 2014, [but will probably have labeling] against a large number of indications if everything goes well in clinical trials," Dr. Jones said.
The study on CXL104 was supported by Forest Laboratories, and the study on JNJ-Q2 was supported by Furiex Pharmaceuticals. JMI Laboratories conducts studies supported by Forest, Furiex, and other pharmaceutical companies.
VANCOUVER, B.C. – New compounds in preclinical stages of testing may eventually help combat the surge in methicillin-resistant Staphylococcus aureus and other multidrug resistant organisms, Dr. Ronald N. Jones said at the annual meeting of the Infectious Diseases Society of America .
Fusidic acid was discovered in the 1960s and used widely in Europe, Australia, and Canada. However because it was never released in the United States, domestic MRSA strains have built up little resistance to it, which makes it something of "an old drug in new clothing," said the chief executive officer of JMI Laboratories, a contract research organization in North Liberty, Iowa.
Dr. Jones and his colleagues tested the compound against 7,340 S. aureus isolates collected from 51 hospitals in every region of the country. Fusidic acid inhibited 99.6% of the isolates at a concentration of 1 mcg/mL or less. The compound also showed comparable activity against S. aureus strains in eight different resistance groups, including strains resistant to five or more other compounds including oxacillin, erythromycin, clindamycin, and the fluoroquinolones.
"This is pretty exciting, because it also has no cross-resistance with any other class of antibiotic," Dr. Jones said. "It could be used widely if we could deliver it in such a way that would prevent any emerging resistance from happening in what I call the naïve population of United States Staph aureus."
In addition, Dr. Jones said, "it’s been conservatively stated that tens of millions of patients have been treated with fusidic acid over the period of the four-plus decades. The drug is considered safe, and it’s usually administered orally for the treatment of serious staphylococcal infections. It also has been applied in some countries topically."
A second agent, JNJ-Q2, is a broad-spectrum fluoroquinolone developed by Johnson & Johnson and Furiex Pharmaceuticals.
"One of the things that was noted very early on is that quinolone resistance, particularly among methicillin-resistant staphylococci, became quite common over a decade ago," Dr. Jones said. "New compounds have been tried for a number of years, [but] what’s novel about this is it’s 16 times more potent than the best of the existing marketed fluoroquinolones."
JNJ-Q2 is moving into phase II and phase III clinical trials. In preclinical studies, "We challenged it with the worst of the MRSA and the fluoroquinolone-resistant MRSA that we could find in our surveillance systems all around the planet. And this new compound came out quite well and covered essentially 90%-100% of the strains, depending upon the geography."
In comparison to other fluoroquinolones, JNJ-Q2 was 16 times more potent than moxifloxacin, 64 times more potent than levofloxacin, and 128 times more potent than ciprofloxacin when tested against 511 S. aureus isolates.
A third agent, ceftaroline, is a broad-spectrum cephalosporin from Forest Laboratories. It is being tested in combination with NXL104, a beta-lactamase inhibitor being developed by Novexel.
Dr. Jones pointed out that ceftaroline alone is active against MRSA and multidrug resistant pneumococci, but when combined with NXL104, it could also be used against the growing population of Enterobacteriaceae that produce derepressed AmpC beta-lactamase.
In studies, Dr. Jones and his colleagues determined that the combination, which they refer to as CXL104, inhibited 96% of ceftazidime-resistant strains of Enterobacter, Citrobacter, and Serratia at concentrations of 4 mcg/mL or lower.
"It’s probably not going to be on the market until 2013 or 2014, [but will probably have labeling] against a large number of indications if everything goes well in clinical trials," Dr. Jones said.
The study on CXL104 was supported by Forest Laboratories, and the study on JNJ-Q2 was supported by Furiex Pharmaceuticals. JMI Laboratories conducts studies supported by Forest, Furiex, and other pharmaceutical companies.