User login
Around the world in 24 hours: A snapshot of COVID’s global havoc
Some medical societies feature sessions at their annual meetings that feel like they’re 24 hours long, yet few have the courage to schedule a session that actually runs all day and all night. But the five societies sponsoring the IDWeek conference had that courage. The first 24 hours of the meeting was devoted to the most pressing infectious-disease crisis of the last 100 years: the COVID-19 pandemic. They called it “COVID-19: Chasing the Sun.”
Dr. Fauci predicts a vaccine answer in mid-November
In the first segment, at 10 am Eastern time, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases and the nation’s top infectious-disease expert, began the day by noting that five of the six companies the US invested in to develop a vaccine are conducting phase 3 trials. He said, “we feel confident that we will have an answer likely in mid-November to the beginning of December as to whether we have a safe and effective vaccine”. He added he was “cautiously optimistic” that “we will have a safe and effective vaccine by the end of the year, which we can begin to distribute as we go into 2021.” He highlighted the COVID-19 Prevention Network website for more information on the trials.
Glaring racial health disparities in U.S.
Some of the most glaring health disparities surrounding COVID-19 in the United States were described by Carlos del Rio, MD, professor of medicine at Emory University in Atlanta, Georgia. He pointed out that while white people have about 23 cases per 10,000 population, Blacks have about 62 cases per 10,000, and Latinos have 73 cases per 10,000. While whites don’t see a huge jump in cases until age 80, he said, “among Blacks and Latinos you start seeing that huge increase at a younger age. In fact, starting at age 20, you start seeing a major, major change.”
COVID-19 diagnostics
Audrey Odom John, MD, PhD, chief of pediatric infectious diseases at Children’s Hospital of Philadelphia, is working on a new way of diagnosing COVID-19 infection in children by testing their breath. “We’re really taking advantage of a fundamental biological fact, which is that people stink,” she said. Breath shows the health of the body as a whole, “and it’s easy to see how breath volatiles might arise from a respiratory infection.” Testing breath is easy and inexpensive, which makes it particularly attractive as a potential test globally, she said.
Long-term effects of COVID-19
Post-COVID illness threatens to overwhelm the health system in the United States, even if only 1% of the 8 million people who have been infected have some sort of long-term deficit, “which would be a very conservative estimate,” said John O’Horo, MD, MPH, with the Mayo Clinic in Rochester, Minn. Neurologic dysfunction is going to be a “fairly significant thing to keep an eye on,” he added. Preeti Malani, MD, chief health officer in infectious diseases at the University of Michigan, Ann Arbor, said the emotional aspects of the illness are “striking” and may be the major long-term effect for most patients.
Challenging cases in COVID-19: Through fire and water
In a case presented to panelists during an afternoon session, a Mexican-born woman, 42, presents to urgent care with fever, dyspnea, dry cough, and pleuritic pain, for over a week. Multiple family members have had recent respiratory illness as well. She is obese, on no medications, was not traveling. She’s a nonsmoker and lives in a multigenerational household in the Mission District of San Francisco. Her heart rate is 116, respiratory rate is 36, and her oxygen saturation on room air is 77%. She is admitted to a local hospital and quickly declines, is intubated and started on hydroxychloroquine (HCQ). One day later she is transferred to a hospital for consideration of extracorporeal membrane oxygenation (ECMO).
Panelists were asked a variety of questions about how they would treat this patient. For example, would they continue HCQ? Ravina Kullar, PharmD, MPH, an infectious disease expert from Newport Beach, Calif., answered that she would not continue the HCQ because of lack of evidence and potential harms. Asked whether she would start remdesivir, Dr. Kullar said she would steer her away from that if the patient developed renal failure. Co-moderator Peter Chin-Hong, MD, a medical educator with the University of California, San Francisco, noted that contact tracing will be important as the patient returns to her housing-dense community.
In-hospital infection prevention
The CDC acknowledged aerosol spread of COVID-19 this month, but David Weber, MD, MPH, professor in infectious diseases at the University of North Carolina at Chapel Hill, said, “this does not change anything we need to do in the hospital,” as long as protective pandemic protocols continue to be followed.
There is no evidence, he noted, that SARS-CoV-2 is transmitted far enough that a hospitalized patient could infect people in other rooms or corridors or floors. Opening windows in COVID-19 patients’ rooms is “not an option,” he said, and could be harmful as fungal elements in outside air may introduce new pathogens. The degree to which improved ventilation systems reduce transmission has not been identified and studies are needed to look at that, he said.
Preventing COVID transmission in the community
Mary-Margaret Fill, MD, deputy state epidemiologist in Tennessee, highlighted COVID-19’s spread in prisons. As of mid-October, she said, there are more than 147,000 cases among the U.S. prison population and there have been 1,246 deaths. This translates to a case rate of about 9800 cases per 100,000 people, she said, “double the highest case rate for any state in the country and over three times greater than our national case rate of about 2,500 cases per 100,000 persons.”
Testing varies widely, she noted. For instance, some states test only new prisoners, and some test only when they are symptomatic. One of the strategies to fight this spread is having staff, who go in and out of the community, be assigned to work with only certain groups at a prison. Another is widespread testing of all prisoners. And when prisoners have to leave the prison for care or court dates, a third strategy would be quarantining them upon their return.
COVID-19 vaccines
As the session stretched into the evening in the United States, Mary Marovich, MD, director of vaccine research, AIDS division, with the National Institute of Allergy and Infectious Diseases and the National Institutes of Health, said while each of the government-funded vaccine studies has its own trial, there are standardized objectives for direct comparisons. The studies are being conducted within the same clinical trial networks, and collaborative laboratories apply the same immunoassays and define the infections in the same way. They are all randomized, placebo-controlled trials and all but one have a 30,000-volunteer sample size. She said that while a vaccine is the goal to end the pandemic, monoclonal antibodies, such as those in convalescent plasma, “may serve as a critical bridge.”
The good, the bad, and the ugly during COVID-19 in Latin America
Latin America and the Caribbean are currently the regions hardest hit by COVID-19. Gustavo D. Lopardo, of the Asociacion Panamericana de Infectologia, noted that even before the pandemic Latin America suffered from widespread poverty and inequality. While overcrowding and poverty are determining factors in the spread of the virus, diabetes and obesity – both highly prevalent – are worsening COVID outcomes.
The countries of the region have dealt with asynchronous waves of transmission within their borders by implementing different containment strategies, with dissimilar results. The presenters covered the spectrum of the pandemic, from the “ugly” in Peru, which has the highest mortality rate in the region, to the “good” in Uruguay, where testing is “winning against COVID-19.” Paradoxically, Chile has both the highest cumulative incidence and the lowest case fatality rate of COVID-19 in the region.
In the social and political turmoil imposed by COVID-19, Clóvis Arns da Cunha, MD, president of the Brazilian Society of Infectious Diseases and professor at the Federal University of Paraná, pointed out that “fake news [has become] a public health problem in Brazil” and elsewhere.
Diagnostics and therapeutics in Latin America
Eleven of the 15 countries with the highest death rate in the world are located in Latin America or the Caribbean. Dr. Arns de Cunha pointed out that tests are hard to come by and inadequate diagnostic testing is a major problem. Latin American countries have not been able to compete with the United States and Europe in purchasing polymerase chain reaction test kits from China and South Korea. The test is the best diagnostic tool in the first week of symptoms, but its scale-up has proved to be a challenge in Latin America.
Furthermore, the most sensitive serological markers, CLIA and ECLIA, which perform best after 2 weeks of symptom onset, are not widely available in Latin America where many patients do not have access to the public health system. The detection of silent hypoxemia in symptomatic patients with COVID-19 can save lives; hence, Arns da Cunha praised the program that distributed 100,000 digital oximeters to hundreds of cities in Brazil, targeting vulnerable populations.
The COVID-19 experience in Japan
Takuya Yamagishi, MD, PhD, chief of the Antimicrobial Resistance Research Center at the National Institute of Infectious Diseases in Japan, played an instrumental role in the epidemiological investigation that took place on the Diamond Princess Cruise Ship in February 2020. That COVID-19 outbreak is the largest disease outbreak involving a cruise ship to date, with 712 confirmed COVID-19 cases and 13 deaths.
The ship-based quarantine prompted a massive public health response with unique challenges. In those early days, investigators uncovered important facts about COVID-19 epidemiology, generating hot debates regarding the public health strategy at the time. Notably, the majority of asymptomatically infected persons remained asymptomatic throughout the course of the infection, transmission from asymptomatic cases was almost as likely as transmission from symptomatic cases, and isolation of passengers in their cabins prevented inter-cabin transmission but not intra-cabin transmission.
Swift response in Asia Pacific region
Infectious-disease experts from Taiwan, Singapore, and Australia, who have been at the forefront of clinical care, research, and policy-making, spoke about their experiences.
Taiwan was one of the first countries to adopt a swift response to COVID-19, shortly after they recognized an outbreak of pneumonia of unknown etiology in China and long before the WHO declared a public health emergency, said Ping-Ing Lee, MD, PhD, from the National Taiwan University Children’s Hospital.
The country began onboard health checks on flights from Wuhan as early as Dec. 31, 2019. Dr. Lee attributed Taiwan’s success in prevention and control of COVID-19 to the rigorous use of face masks and environmental disinfection procedures. Regarding the country’s antilockdown stance, he said, “Lockdown may be effective; however, it is associated with a tremendous economic loss.”
In his presentation on remdesivir vs corticosteroids, David Lye, MBBS, said, “I think remdesivir as an antiviral seems to work well given early, but steroids will need to be studied further in terms of its conflicting evidence in multiple well-designed RCTs as well as [their] potential side effects.” He is director of the Infectious Disease Research and Training Office, National Centre for Infectious Diseases, Singapore.
Allen C. Cheng, MBBS, PhD, of Monash University in Melbourne, noted that “control is possible. We seemed to have controlled this twice at the moment with fairly draconian action, but every day does matter.”
China past the first wave
China has already passed the first wave, explained Lei Zhou, MD, of the Chinese Center for Disease Control and Prevention, but there are still some small-scale resurgences. So far a total of four waves have been identified. She also mentioned that contact tracing is intense and highlighted the case of Xinfadi Market in Beijing, the site of an outbreak in June 2020.
Gui-Qiang Wang, MD, from the Department of Infectious Disease, Peking University First Hospital, emphasized the importance of a chest CT for the diagnosis of COVID-19. “In the early stage of the disease, patients may not show any symptoms; however, on CT scan you can see pneumonia. Also, early intervention of high-risk groups and monitoring of warning indicators for disease progression is extremely important,” he said.
“Early antiviral therapy is expected to stop progression, but still needs evaluation,” he said. “Convalescent plasma is safe and effective, but its source is limited; steroid therapy needs to explore appropriate population and timing; and thymosin α is safe, and its effect on outcomes needs large-sample clinical trial.”
Time to Call for an ‘Arab CDC?’
The eastern Mediterranean is geographically, politically, economically, and religiously a very distinct and sensitive region, and “COVID-19 is an added insult to this already frail region of the world,” said Zaid Haddadin, MD, Vanderbilt University Medical Center, Nashville, Tenn.
Poor healthcare and poor public health services are a consequence of weak and fragile governments and infrastructure, the result of war and regional conflicts in many countries. Millions of war refugees live in camps with high population densities and shared facilities, which makes social distancing and community mitigation very challenging. Moreover, the culture includes frequent large social gatherings. Millions of pilgrims visit holy sites in different cities in these countries. There is also movement due to trade and tourism. Travel restrictions are challenging, and there is limited comprehension of precautionary measures.
Najwa Khuri-Bulos, professor of pediatrics and infectious diseases at the University of Jordan, was part of a task force headed by the country’s Ministry of Health. A lockdown was implemented, which helped flatten the curve, but the loosening of restrictions has led to a recent increase in cases. She said, “No country can succeed in controlling spread without the regional collaboration. Perhaps it is time to adopt the call for an Arab CDC.”
Africa is “not out of the woods yet”
The Africa CDC has three key pillars as the foundation for their COVID-19 strategy: preventing transmission, preventing deaths, and preventing social harm, according to Raji Tajudeen, MBBS, FWACP, MPH, head of the agency’s Public Health Institutes and Research Division. Africa, with 1.5 million cases of COVID-19, accounts for 5% of global cases. With a recovery rate of 83% and a case fatality rate of 2.4%, the African continent has fared much better than the rest of the world. “Significant improvements have been made, but we are not out of the woods yet,” he cautioned.
Richard Lessells, PhD, from the University of KwaZulu-Natal, agreed. “Unfortunately, South Africa has not been spared from the worst effects of this pandemic despite what you might read in the press and scientific coverage.” He added, “Over 50% of cases and up to two thirds of the deaths in the African region are coming from South Africa.” A bigger challenge for South Africa has been maintaining essential health services during the COVID-19 pandemic, especially since it is also at the heart of the HIV pandemic. On the brighter side, HIV itself has not emerged as a risk factor for COVID-19 infection or severe disease in South Africa.
Dimie Ogoina, MBBS, FWACP, president of the Nigerian Infectious Diseases Society, stated that COVID-19 has significantly affected access to healthcare in Nigeria, particularly immunizations and antenatal care. Immunization uptake is likely to have dropped by 50% in the country.
Diagnostic pitfalls in COVID-19
Technical errors associated with the SARS-CoV-2 diagnostic pipeline are a major source of variations in diagnosis, explained Jim Huggett, PhD, senior lecturer, analytical microbiology, University of Surrey, Guildford, England. He believes that PCR assays are currently too biased for a single cutoff to be broadly used, and false-positive signals are most likely because of contamination.
Dana Wolf, MD, Clinical Virology Unit, Hadassah Hebrew University Medical Center in Israel, presented a large-scale data analysis of more than 133,000 pooled samples. Such a pooling strategy appeared to be highly efficient for a wide range of prevalence rates (<1% to 6%). “Our empirical evidence strongly projects on the feasibility and benefits of pooling in the current pandemic setting, to enhance continued surveillance, control, and community reopening,” she said.
Corine Geurts van Kessel, MD, PhD, Department of Virology, Erasmus University Rotterdam (the Netherlands), discussing antibodies testing for SARS-CoV-2, pointed out that disease severity can affect testing accuracy. “Reinfection cases tell us that we cannot rely on immunity acquired by natural infection to confer herd immunity,” she said.
Misinformation in the first digital pandemic
The world is not only facing a devastating pandemic, but also an alarming “infodemic” of misinformation. Between January and March 2020, a new COVID-19–related tweet appeared on Twitter every 45 milliseconds. Müge Çevik, MD, MSc, MRCP, an infectious disease clinician, scientist, and science communicator, said that “the greatest challenge for science communication is reaching the audience.”
People have always been skeptical of science reporting by journalists and would rather have scientists communicate with them directly, she noted. Science communication plays a dual role. “On one hand is the need to promote science to a wide audience in order to inform and educate and inspire the next generation of scientists, and on the other hand there is also a need to engage effectively in public dialogue,” she added. Dr. Çevik and colleagues think that “The responsibility of academics should not end with finding the truth. It should end after communicating it.”
Treatment in the ICU
Matteo Bassetti, MD, with the University of Genoa (Italy), who was asked about when to use remdesivir in the intensive care unit and for how long, said, “In the majority of cases, 5 days is probably enough.” However, if there is high viremia, he said, physicians may choose to continue the regimen beyond 5 days. Data show it is important to prescribe this drug for patients with oxygen support in an early phase, within 10 days of the first symptoms, he added. “In the late phase, there is a very limited role for remdesivir, as we know that we are already out of the viremic phase.” He also emphasized that there is no role for hydroxychloroquine or lopinavir-ritonavir.
Breaking the chains of transmission
During the wrap-up session, former US CDC Director Tom Frieden, MD, said, “We’re not even halfway through it” about the pandemic trajectory. “And we have to be very clear that the risk of explosive spread will not end with a vaccine.” He is now president and CEO of Resolve to Save Lives.
Different parts of the world will have very different experiences, Dr. Frieden said, noting that Africa, where 4% of the population is older than 65, has a very different risk level than Europe and the United States, where 10%-20% of people are in older age groups.
“We need a one-two punch,” he noted, first preventing spread, and when it does happen, boxing it in. Mask wearing is essential. “States in the US that mandated universal mask-wearing experienced much more rapid declines (in cases) for every 5 days the mandate was in place.”
Michael Ryan, MD, executive director for the WHO’s Health Emergencies Programme, added, “We need to collectively recommit to winning this game. We know how to break the chains of transmission. We need recommitment to a scientific, societal, and political strategy, and an alliance – a contract – between those entities to try to move us forward.”
This article first appeared on Medscape.com.
Some medical societies feature sessions at their annual meetings that feel like they’re 24 hours long, yet few have the courage to schedule a session that actually runs all day and all night. But the five societies sponsoring the IDWeek conference had that courage. The first 24 hours of the meeting was devoted to the most pressing infectious-disease crisis of the last 100 years: the COVID-19 pandemic. They called it “COVID-19: Chasing the Sun.”
Dr. Fauci predicts a vaccine answer in mid-November
In the first segment, at 10 am Eastern time, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases and the nation’s top infectious-disease expert, began the day by noting that five of the six companies the US invested in to develop a vaccine are conducting phase 3 trials. He said, “we feel confident that we will have an answer likely in mid-November to the beginning of December as to whether we have a safe and effective vaccine”. He added he was “cautiously optimistic” that “we will have a safe and effective vaccine by the end of the year, which we can begin to distribute as we go into 2021.” He highlighted the COVID-19 Prevention Network website for more information on the trials.
Glaring racial health disparities in U.S.
Some of the most glaring health disparities surrounding COVID-19 in the United States were described by Carlos del Rio, MD, professor of medicine at Emory University in Atlanta, Georgia. He pointed out that while white people have about 23 cases per 10,000 population, Blacks have about 62 cases per 10,000, and Latinos have 73 cases per 10,000. While whites don’t see a huge jump in cases until age 80, he said, “among Blacks and Latinos you start seeing that huge increase at a younger age. In fact, starting at age 20, you start seeing a major, major change.”
COVID-19 diagnostics
Audrey Odom John, MD, PhD, chief of pediatric infectious diseases at Children’s Hospital of Philadelphia, is working on a new way of diagnosing COVID-19 infection in children by testing their breath. “We’re really taking advantage of a fundamental biological fact, which is that people stink,” she said. Breath shows the health of the body as a whole, “and it’s easy to see how breath volatiles might arise from a respiratory infection.” Testing breath is easy and inexpensive, which makes it particularly attractive as a potential test globally, she said.
Long-term effects of COVID-19
Post-COVID illness threatens to overwhelm the health system in the United States, even if only 1% of the 8 million people who have been infected have some sort of long-term deficit, “which would be a very conservative estimate,” said John O’Horo, MD, MPH, with the Mayo Clinic in Rochester, Minn. Neurologic dysfunction is going to be a “fairly significant thing to keep an eye on,” he added. Preeti Malani, MD, chief health officer in infectious diseases at the University of Michigan, Ann Arbor, said the emotional aspects of the illness are “striking” and may be the major long-term effect for most patients.
Challenging cases in COVID-19: Through fire and water
In a case presented to panelists during an afternoon session, a Mexican-born woman, 42, presents to urgent care with fever, dyspnea, dry cough, and pleuritic pain, for over a week. Multiple family members have had recent respiratory illness as well. She is obese, on no medications, was not traveling. She’s a nonsmoker and lives in a multigenerational household in the Mission District of San Francisco. Her heart rate is 116, respiratory rate is 36, and her oxygen saturation on room air is 77%. She is admitted to a local hospital and quickly declines, is intubated and started on hydroxychloroquine (HCQ). One day later she is transferred to a hospital for consideration of extracorporeal membrane oxygenation (ECMO).
Panelists were asked a variety of questions about how they would treat this patient. For example, would they continue HCQ? Ravina Kullar, PharmD, MPH, an infectious disease expert from Newport Beach, Calif., answered that she would not continue the HCQ because of lack of evidence and potential harms. Asked whether she would start remdesivir, Dr. Kullar said she would steer her away from that if the patient developed renal failure. Co-moderator Peter Chin-Hong, MD, a medical educator with the University of California, San Francisco, noted that contact tracing will be important as the patient returns to her housing-dense community.
In-hospital infection prevention
The CDC acknowledged aerosol spread of COVID-19 this month, but David Weber, MD, MPH, professor in infectious diseases at the University of North Carolina at Chapel Hill, said, “this does not change anything we need to do in the hospital,” as long as protective pandemic protocols continue to be followed.
There is no evidence, he noted, that SARS-CoV-2 is transmitted far enough that a hospitalized patient could infect people in other rooms or corridors or floors. Opening windows in COVID-19 patients’ rooms is “not an option,” he said, and could be harmful as fungal elements in outside air may introduce new pathogens. The degree to which improved ventilation systems reduce transmission has not been identified and studies are needed to look at that, he said.
Preventing COVID transmission in the community
Mary-Margaret Fill, MD, deputy state epidemiologist in Tennessee, highlighted COVID-19’s spread in prisons. As of mid-October, she said, there are more than 147,000 cases among the U.S. prison population and there have been 1,246 deaths. This translates to a case rate of about 9800 cases per 100,000 people, she said, “double the highest case rate for any state in the country and over three times greater than our national case rate of about 2,500 cases per 100,000 persons.”
Testing varies widely, she noted. For instance, some states test only new prisoners, and some test only when they are symptomatic. One of the strategies to fight this spread is having staff, who go in and out of the community, be assigned to work with only certain groups at a prison. Another is widespread testing of all prisoners. And when prisoners have to leave the prison for care or court dates, a third strategy would be quarantining them upon their return.
COVID-19 vaccines
As the session stretched into the evening in the United States, Mary Marovich, MD, director of vaccine research, AIDS division, with the National Institute of Allergy and Infectious Diseases and the National Institutes of Health, said while each of the government-funded vaccine studies has its own trial, there are standardized objectives for direct comparisons. The studies are being conducted within the same clinical trial networks, and collaborative laboratories apply the same immunoassays and define the infections in the same way. They are all randomized, placebo-controlled trials and all but one have a 30,000-volunteer sample size. She said that while a vaccine is the goal to end the pandemic, monoclonal antibodies, such as those in convalescent plasma, “may serve as a critical bridge.”
The good, the bad, and the ugly during COVID-19 in Latin America
Latin America and the Caribbean are currently the regions hardest hit by COVID-19. Gustavo D. Lopardo, of the Asociacion Panamericana de Infectologia, noted that even before the pandemic Latin America suffered from widespread poverty and inequality. While overcrowding and poverty are determining factors in the spread of the virus, diabetes and obesity – both highly prevalent – are worsening COVID outcomes.
The countries of the region have dealt with asynchronous waves of transmission within their borders by implementing different containment strategies, with dissimilar results. The presenters covered the spectrum of the pandemic, from the “ugly” in Peru, which has the highest mortality rate in the region, to the “good” in Uruguay, where testing is “winning against COVID-19.” Paradoxically, Chile has both the highest cumulative incidence and the lowest case fatality rate of COVID-19 in the region.
In the social and political turmoil imposed by COVID-19, Clóvis Arns da Cunha, MD, president of the Brazilian Society of Infectious Diseases and professor at the Federal University of Paraná, pointed out that “fake news [has become] a public health problem in Brazil” and elsewhere.
Diagnostics and therapeutics in Latin America
Eleven of the 15 countries with the highest death rate in the world are located in Latin America or the Caribbean. Dr. Arns de Cunha pointed out that tests are hard to come by and inadequate diagnostic testing is a major problem. Latin American countries have not been able to compete with the United States and Europe in purchasing polymerase chain reaction test kits from China and South Korea. The test is the best diagnostic tool in the first week of symptoms, but its scale-up has proved to be a challenge in Latin America.
Furthermore, the most sensitive serological markers, CLIA and ECLIA, which perform best after 2 weeks of symptom onset, are not widely available in Latin America where many patients do not have access to the public health system. The detection of silent hypoxemia in symptomatic patients with COVID-19 can save lives; hence, Arns da Cunha praised the program that distributed 100,000 digital oximeters to hundreds of cities in Brazil, targeting vulnerable populations.
The COVID-19 experience in Japan
Takuya Yamagishi, MD, PhD, chief of the Antimicrobial Resistance Research Center at the National Institute of Infectious Diseases in Japan, played an instrumental role in the epidemiological investigation that took place on the Diamond Princess Cruise Ship in February 2020. That COVID-19 outbreak is the largest disease outbreak involving a cruise ship to date, with 712 confirmed COVID-19 cases and 13 deaths.
The ship-based quarantine prompted a massive public health response with unique challenges. In those early days, investigators uncovered important facts about COVID-19 epidemiology, generating hot debates regarding the public health strategy at the time. Notably, the majority of asymptomatically infected persons remained asymptomatic throughout the course of the infection, transmission from asymptomatic cases was almost as likely as transmission from symptomatic cases, and isolation of passengers in their cabins prevented inter-cabin transmission but not intra-cabin transmission.
Swift response in Asia Pacific region
Infectious-disease experts from Taiwan, Singapore, and Australia, who have been at the forefront of clinical care, research, and policy-making, spoke about their experiences.
Taiwan was one of the first countries to adopt a swift response to COVID-19, shortly after they recognized an outbreak of pneumonia of unknown etiology in China and long before the WHO declared a public health emergency, said Ping-Ing Lee, MD, PhD, from the National Taiwan University Children’s Hospital.
The country began onboard health checks on flights from Wuhan as early as Dec. 31, 2019. Dr. Lee attributed Taiwan’s success in prevention and control of COVID-19 to the rigorous use of face masks and environmental disinfection procedures. Regarding the country’s antilockdown stance, he said, “Lockdown may be effective; however, it is associated with a tremendous economic loss.”
In his presentation on remdesivir vs corticosteroids, David Lye, MBBS, said, “I think remdesivir as an antiviral seems to work well given early, but steroids will need to be studied further in terms of its conflicting evidence in multiple well-designed RCTs as well as [their] potential side effects.” He is director of the Infectious Disease Research and Training Office, National Centre for Infectious Diseases, Singapore.
Allen C. Cheng, MBBS, PhD, of Monash University in Melbourne, noted that “control is possible. We seemed to have controlled this twice at the moment with fairly draconian action, but every day does matter.”
China past the first wave
China has already passed the first wave, explained Lei Zhou, MD, of the Chinese Center for Disease Control and Prevention, but there are still some small-scale resurgences. So far a total of four waves have been identified. She also mentioned that contact tracing is intense and highlighted the case of Xinfadi Market in Beijing, the site of an outbreak in June 2020.
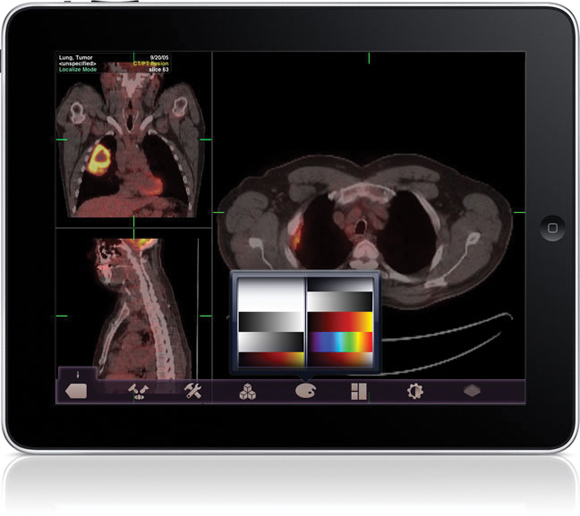
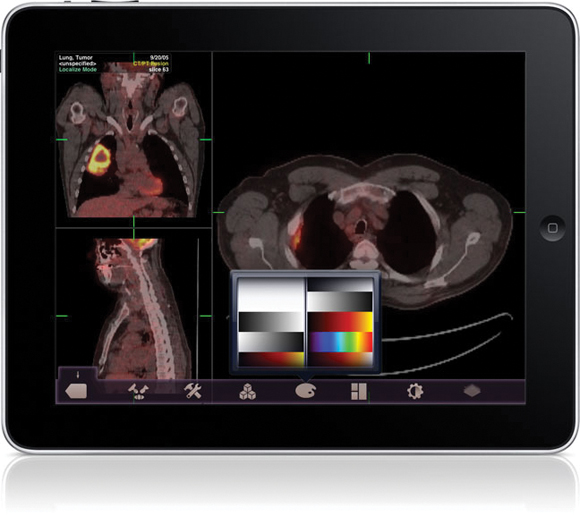
Gui-Qiang Wang, MD, from the Department of Infectious Disease, Peking University First Hospital, emphasized the importance of a chest CT for the diagnosis of COVID-19. “In the early stage of the disease, patients may not show any symptoms; however, on CT scan you can see pneumonia. Also, early intervention of high-risk groups and monitoring of warning indicators for disease progression is extremely important,” he said.
“Early antiviral therapy is expected to stop progression, but still needs evaluation,” he said. “Convalescent plasma is safe and effective, but its source is limited; steroid therapy needs to explore appropriate population and timing; and thymosin α is safe, and its effect on outcomes needs large-sample clinical trial.”
Time to Call for an ‘Arab CDC?’
The eastern Mediterranean is geographically, politically, economically, and religiously a very distinct and sensitive region, and “COVID-19 is an added insult to this already frail region of the world,” said Zaid Haddadin, MD, Vanderbilt University Medical Center, Nashville, Tenn.
Poor healthcare and poor public health services are a consequence of weak and fragile governments and infrastructure, the result of war and regional conflicts in many countries. Millions of war refugees live in camps with high population densities and shared facilities, which makes social distancing and community mitigation very challenging. Moreover, the culture includes frequent large social gatherings. Millions of pilgrims visit holy sites in different cities in these countries. There is also movement due to trade and tourism. Travel restrictions are challenging, and there is limited comprehension of precautionary measures.
Najwa Khuri-Bulos, professor of pediatrics and infectious diseases at the University of Jordan, was part of a task force headed by the country’s Ministry of Health. A lockdown was implemented, which helped flatten the curve, but the loosening of restrictions has led to a recent increase in cases. She said, “No country can succeed in controlling spread without the regional collaboration. Perhaps it is time to adopt the call for an Arab CDC.”
Africa is “not out of the woods yet”
The Africa CDC has three key pillars as the foundation for their COVID-19 strategy: preventing transmission, preventing deaths, and preventing social harm, according to Raji Tajudeen, MBBS, FWACP, MPH, head of the agency’s Public Health Institutes and Research Division. Africa, with 1.5 million cases of COVID-19, accounts for 5% of global cases. With a recovery rate of 83% and a case fatality rate of 2.4%, the African continent has fared much better than the rest of the world. “Significant improvements have been made, but we are not out of the woods yet,” he cautioned.
Richard Lessells, PhD, from the University of KwaZulu-Natal, agreed. “Unfortunately, South Africa has not been spared from the worst effects of this pandemic despite what you might read in the press and scientific coverage.” He added, “Over 50% of cases and up to two thirds of the deaths in the African region are coming from South Africa.” A bigger challenge for South Africa has been maintaining essential health services during the COVID-19 pandemic, especially since it is also at the heart of the HIV pandemic. On the brighter side, HIV itself has not emerged as a risk factor for COVID-19 infection or severe disease in South Africa.
Dimie Ogoina, MBBS, FWACP, president of the Nigerian Infectious Diseases Society, stated that COVID-19 has significantly affected access to healthcare in Nigeria, particularly immunizations and antenatal care. Immunization uptake is likely to have dropped by 50% in the country.
Diagnostic pitfalls in COVID-19
Technical errors associated with the SARS-CoV-2 diagnostic pipeline are a major source of variations in diagnosis, explained Jim Huggett, PhD, senior lecturer, analytical microbiology, University of Surrey, Guildford, England. He believes that PCR assays are currently too biased for a single cutoff to be broadly used, and false-positive signals are most likely because of contamination.
Dana Wolf, MD, Clinical Virology Unit, Hadassah Hebrew University Medical Center in Israel, presented a large-scale data analysis of more than 133,000 pooled samples. Such a pooling strategy appeared to be highly efficient for a wide range of prevalence rates (<1% to 6%). “Our empirical evidence strongly projects on the feasibility and benefits of pooling in the current pandemic setting, to enhance continued surveillance, control, and community reopening,” she said.
Corine Geurts van Kessel, MD, PhD, Department of Virology, Erasmus University Rotterdam (the Netherlands), discussing antibodies testing for SARS-CoV-2, pointed out that disease severity can affect testing accuracy. “Reinfection cases tell us that we cannot rely on immunity acquired by natural infection to confer herd immunity,” she said.
Misinformation in the first digital pandemic
The world is not only facing a devastating pandemic, but also an alarming “infodemic” of misinformation. Between January and March 2020, a new COVID-19–related tweet appeared on Twitter every 45 milliseconds. Müge Çevik, MD, MSc, MRCP, an infectious disease clinician, scientist, and science communicator, said that “the greatest challenge for science communication is reaching the audience.”
People have always been skeptical of science reporting by journalists and would rather have scientists communicate with them directly, she noted. Science communication plays a dual role. “On one hand is the need to promote science to a wide audience in order to inform and educate and inspire the next generation of scientists, and on the other hand there is also a need to engage effectively in public dialogue,” she added. Dr. Çevik and colleagues think that “The responsibility of academics should not end with finding the truth. It should end after communicating it.”
Treatment in the ICU
Matteo Bassetti, MD, with the University of Genoa (Italy), who was asked about when to use remdesivir in the intensive care unit and for how long, said, “In the majority of cases, 5 days is probably enough.” However, if there is high viremia, he said, physicians may choose to continue the regimen beyond 5 days. Data show it is important to prescribe this drug for patients with oxygen support in an early phase, within 10 days of the first symptoms, he added. “In the late phase, there is a very limited role for remdesivir, as we know that we are already out of the viremic phase.” He also emphasized that there is no role for hydroxychloroquine or lopinavir-ritonavir.
Breaking the chains of transmission
During the wrap-up session, former US CDC Director Tom Frieden, MD, said, “We’re not even halfway through it” about the pandemic trajectory. “And we have to be very clear that the risk of explosive spread will not end with a vaccine.” He is now president and CEO of Resolve to Save Lives.
Different parts of the world will have very different experiences, Dr. Frieden said, noting that Africa, where 4% of the population is older than 65, has a very different risk level than Europe and the United States, where 10%-20% of people are in older age groups.
“We need a one-two punch,” he noted, first preventing spread, and when it does happen, boxing it in. Mask wearing is essential. “States in the US that mandated universal mask-wearing experienced much more rapid declines (in cases) for every 5 days the mandate was in place.”
Michael Ryan, MD, executive director for the WHO’s Health Emergencies Programme, added, “We need to collectively recommit to winning this game. We know how to break the chains of transmission. We need recommitment to a scientific, societal, and political strategy, and an alliance – a contract – between those entities to try to move us forward.”
This article first appeared on Medscape.com.
Some medical societies feature sessions at their annual meetings that feel like they’re 24 hours long, yet few have the courage to schedule a session that actually runs all day and all night. But the five societies sponsoring the IDWeek conference had that courage. The first 24 hours of the meeting was devoted to the most pressing infectious-disease crisis of the last 100 years: the COVID-19 pandemic. They called it “COVID-19: Chasing the Sun.”
Dr. Fauci predicts a vaccine answer in mid-November
In the first segment, at 10 am Eastern time, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases and the nation’s top infectious-disease expert, began the day by noting that five of the six companies the US invested in to develop a vaccine are conducting phase 3 trials. He said, “we feel confident that we will have an answer likely in mid-November to the beginning of December as to whether we have a safe and effective vaccine”. He added he was “cautiously optimistic” that “we will have a safe and effective vaccine by the end of the year, which we can begin to distribute as we go into 2021.” He highlighted the COVID-19 Prevention Network website for more information on the trials.
Glaring racial health disparities in U.S.
Some of the most glaring health disparities surrounding COVID-19 in the United States were described by Carlos del Rio, MD, professor of medicine at Emory University in Atlanta, Georgia. He pointed out that while white people have about 23 cases per 10,000 population, Blacks have about 62 cases per 10,000, and Latinos have 73 cases per 10,000. While whites don’t see a huge jump in cases until age 80, he said, “among Blacks and Latinos you start seeing that huge increase at a younger age. In fact, starting at age 20, you start seeing a major, major change.”
COVID-19 diagnostics
Audrey Odom John, MD, PhD, chief of pediatric infectious diseases at Children’s Hospital of Philadelphia, is working on a new way of diagnosing COVID-19 infection in children by testing their breath. “We’re really taking advantage of a fundamental biological fact, which is that people stink,” she said. Breath shows the health of the body as a whole, “and it’s easy to see how breath volatiles might arise from a respiratory infection.” Testing breath is easy and inexpensive, which makes it particularly attractive as a potential test globally, she said.
Long-term effects of COVID-19
Post-COVID illness threatens to overwhelm the health system in the United States, even if only 1% of the 8 million people who have been infected have some sort of long-term deficit, “which would be a very conservative estimate,” said John O’Horo, MD, MPH, with the Mayo Clinic in Rochester, Minn. Neurologic dysfunction is going to be a “fairly significant thing to keep an eye on,” he added. Preeti Malani, MD, chief health officer in infectious diseases at the University of Michigan, Ann Arbor, said the emotional aspects of the illness are “striking” and may be the major long-term effect for most patients.
Challenging cases in COVID-19: Through fire and water
In a case presented to panelists during an afternoon session, a Mexican-born woman, 42, presents to urgent care with fever, dyspnea, dry cough, and pleuritic pain, for over a week. Multiple family members have had recent respiratory illness as well. She is obese, on no medications, was not traveling. She’s a nonsmoker and lives in a multigenerational household in the Mission District of San Francisco. Her heart rate is 116, respiratory rate is 36, and her oxygen saturation on room air is 77%. She is admitted to a local hospital and quickly declines, is intubated and started on hydroxychloroquine (HCQ). One day later she is transferred to a hospital for consideration of extracorporeal membrane oxygenation (ECMO).
Panelists were asked a variety of questions about how they would treat this patient. For example, would they continue HCQ? Ravina Kullar, PharmD, MPH, an infectious disease expert from Newport Beach, Calif., answered that she would not continue the HCQ because of lack of evidence and potential harms. Asked whether she would start remdesivir, Dr. Kullar said she would steer her away from that if the patient developed renal failure. Co-moderator Peter Chin-Hong, MD, a medical educator with the University of California, San Francisco, noted that contact tracing will be important as the patient returns to her housing-dense community.
In-hospital infection prevention
The CDC acknowledged aerosol spread of COVID-19 this month, but David Weber, MD, MPH, professor in infectious diseases at the University of North Carolina at Chapel Hill, said, “this does not change anything we need to do in the hospital,” as long as protective pandemic protocols continue to be followed.
There is no evidence, he noted, that SARS-CoV-2 is transmitted far enough that a hospitalized patient could infect people in other rooms or corridors or floors. Opening windows in COVID-19 patients’ rooms is “not an option,” he said, and could be harmful as fungal elements in outside air may introduce new pathogens. The degree to which improved ventilation systems reduce transmission has not been identified and studies are needed to look at that, he said.
Preventing COVID transmission in the community
Mary-Margaret Fill, MD, deputy state epidemiologist in Tennessee, highlighted COVID-19’s spread in prisons. As of mid-October, she said, there are more than 147,000 cases among the U.S. prison population and there have been 1,246 deaths. This translates to a case rate of about 9800 cases per 100,000 people, she said, “double the highest case rate for any state in the country and over three times greater than our national case rate of about 2,500 cases per 100,000 persons.”
Testing varies widely, she noted. For instance, some states test only new prisoners, and some test only when they are symptomatic. One of the strategies to fight this spread is having staff, who go in and out of the community, be assigned to work with only certain groups at a prison. Another is widespread testing of all prisoners. And when prisoners have to leave the prison for care or court dates, a third strategy would be quarantining them upon their return.
COVID-19 vaccines
As the session stretched into the evening in the United States, Mary Marovich, MD, director of vaccine research, AIDS division, with the National Institute of Allergy and Infectious Diseases and the National Institutes of Health, said while each of the government-funded vaccine studies has its own trial, there are standardized objectives for direct comparisons. The studies are being conducted within the same clinical trial networks, and collaborative laboratories apply the same immunoassays and define the infections in the same way. They are all randomized, placebo-controlled trials and all but one have a 30,000-volunteer sample size. She said that while a vaccine is the goal to end the pandemic, monoclonal antibodies, such as those in convalescent plasma, “may serve as a critical bridge.”
The good, the bad, and the ugly during COVID-19 in Latin America
Latin America and the Caribbean are currently the regions hardest hit by COVID-19. Gustavo D. Lopardo, of the Asociacion Panamericana de Infectologia, noted that even before the pandemic Latin America suffered from widespread poverty and inequality. While overcrowding and poverty are determining factors in the spread of the virus, diabetes and obesity – both highly prevalent – are worsening COVID outcomes.
The countries of the region have dealt with asynchronous waves of transmission within their borders by implementing different containment strategies, with dissimilar results. The presenters covered the spectrum of the pandemic, from the “ugly” in Peru, which has the highest mortality rate in the region, to the “good” in Uruguay, where testing is “winning against COVID-19.” Paradoxically, Chile has both the highest cumulative incidence and the lowest case fatality rate of COVID-19 in the region.
In the social and political turmoil imposed by COVID-19, Clóvis Arns da Cunha, MD, president of the Brazilian Society of Infectious Diseases and professor at the Federal University of Paraná, pointed out that “fake news [has become] a public health problem in Brazil” and elsewhere.
Diagnostics and therapeutics in Latin America
Eleven of the 15 countries with the highest death rate in the world are located in Latin America or the Caribbean. Dr. Arns de Cunha pointed out that tests are hard to come by and inadequate diagnostic testing is a major problem. Latin American countries have not been able to compete with the United States and Europe in purchasing polymerase chain reaction test kits from China and South Korea. The test is the best diagnostic tool in the first week of symptoms, but its scale-up has proved to be a challenge in Latin America.
Furthermore, the most sensitive serological markers, CLIA and ECLIA, which perform best after 2 weeks of symptom onset, are not widely available in Latin America where many patients do not have access to the public health system. The detection of silent hypoxemia in symptomatic patients with COVID-19 can save lives; hence, Arns da Cunha praised the program that distributed 100,000 digital oximeters to hundreds of cities in Brazil, targeting vulnerable populations.
The COVID-19 experience in Japan
Takuya Yamagishi, MD, PhD, chief of the Antimicrobial Resistance Research Center at the National Institute of Infectious Diseases in Japan, played an instrumental role in the epidemiological investigation that took place on the Diamond Princess Cruise Ship in February 2020. That COVID-19 outbreak is the largest disease outbreak involving a cruise ship to date, with 712 confirmed COVID-19 cases and 13 deaths.
The ship-based quarantine prompted a massive public health response with unique challenges. In those early days, investigators uncovered important facts about COVID-19 epidemiology, generating hot debates regarding the public health strategy at the time. Notably, the majority of asymptomatically infected persons remained asymptomatic throughout the course of the infection, transmission from asymptomatic cases was almost as likely as transmission from symptomatic cases, and isolation of passengers in their cabins prevented inter-cabin transmission but not intra-cabin transmission.
Swift response in Asia Pacific region
Infectious-disease experts from Taiwan, Singapore, and Australia, who have been at the forefront of clinical care, research, and policy-making, spoke about their experiences.
Taiwan was one of the first countries to adopt a swift response to COVID-19, shortly after they recognized an outbreak of pneumonia of unknown etiology in China and long before the WHO declared a public health emergency, said Ping-Ing Lee, MD, PhD, from the National Taiwan University Children’s Hospital.
The country began onboard health checks on flights from Wuhan as early as Dec. 31, 2019. Dr. Lee attributed Taiwan’s success in prevention and control of COVID-19 to the rigorous use of face masks and environmental disinfection procedures. Regarding the country’s antilockdown stance, he said, “Lockdown may be effective; however, it is associated with a tremendous economic loss.”
In his presentation on remdesivir vs corticosteroids, David Lye, MBBS, said, “I think remdesivir as an antiviral seems to work well given early, but steroids will need to be studied further in terms of its conflicting evidence in multiple well-designed RCTs as well as [their] potential side effects.” He is director of the Infectious Disease Research and Training Office, National Centre for Infectious Diseases, Singapore.
Allen C. Cheng, MBBS, PhD, of Monash University in Melbourne, noted that “control is possible. We seemed to have controlled this twice at the moment with fairly draconian action, but every day does matter.”
China past the first wave
China has already passed the first wave, explained Lei Zhou, MD, of the Chinese Center for Disease Control and Prevention, but there are still some small-scale resurgences. So far a total of four waves have been identified. She also mentioned that contact tracing is intense and highlighted the case of Xinfadi Market in Beijing, the site of an outbreak in June 2020.
Gui-Qiang Wang, MD, from the Department of Infectious Disease, Peking University First Hospital, emphasized the importance of a chest CT for the diagnosis of COVID-19. “In the early stage of the disease, patients may not show any symptoms; however, on CT scan you can see pneumonia. Also, early intervention of high-risk groups and monitoring of warning indicators for disease progression is extremely important,” he said.
“Early antiviral therapy is expected to stop progression, but still needs evaluation,” he said. “Convalescent plasma is safe and effective, but its source is limited; steroid therapy needs to explore appropriate population and timing; and thymosin α is safe, and its effect on outcomes needs large-sample clinical trial.”
Time to Call for an ‘Arab CDC?’
The eastern Mediterranean is geographically, politically, economically, and religiously a very distinct and sensitive region, and “COVID-19 is an added insult to this already frail region of the world,” said Zaid Haddadin, MD, Vanderbilt University Medical Center, Nashville, Tenn.
Poor healthcare and poor public health services are a consequence of weak and fragile governments and infrastructure, the result of war and regional conflicts in many countries. Millions of war refugees live in camps with high population densities and shared facilities, which makes social distancing and community mitigation very challenging. Moreover, the culture includes frequent large social gatherings. Millions of pilgrims visit holy sites in different cities in these countries. There is also movement due to trade and tourism. Travel restrictions are challenging, and there is limited comprehension of precautionary measures.
Najwa Khuri-Bulos, professor of pediatrics and infectious diseases at the University of Jordan, was part of a task force headed by the country’s Ministry of Health. A lockdown was implemented, which helped flatten the curve, but the loosening of restrictions has led to a recent increase in cases. She said, “No country can succeed in controlling spread without the regional collaboration. Perhaps it is time to adopt the call for an Arab CDC.”
Africa is “not out of the woods yet”
The Africa CDC has three key pillars as the foundation for their COVID-19 strategy: preventing transmission, preventing deaths, and preventing social harm, according to Raji Tajudeen, MBBS, FWACP, MPH, head of the agency’s Public Health Institutes and Research Division. Africa, with 1.5 million cases of COVID-19, accounts for 5% of global cases. With a recovery rate of 83% and a case fatality rate of 2.4%, the African continent has fared much better than the rest of the world. “Significant improvements have been made, but we are not out of the woods yet,” he cautioned.
Richard Lessells, PhD, from the University of KwaZulu-Natal, agreed. “Unfortunately, South Africa has not been spared from the worst effects of this pandemic despite what you might read in the press and scientific coverage.” He added, “Over 50% of cases and up to two thirds of the deaths in the African region are coming from South Africa.” A bigger challenge for South Africa has been maintaining essential health services during the COVID-19 pandemic, especially since it is also at the heart of the HIV pandemic. On the brighter side, HIV itself has not emerged as a risk factor for COVID-19 infection or severe disease in South Africa.
Dimie Ogoina, MBBS, FWACP, president of the Nigerian Infectious Diseases Society, stated that COVID-19 has significantly affected access to healthcare in Nigeria, particularly immunizations and antenatal care. Immunization uptake is likely to have dropped by 50% in the country.
Diagnostic pitfalls in COVID-19
Technical errors associated with the SARS-CoV-2 diagnostic pipeline are a major source of variations in diagnosis, explained Jim Huggett, PhD, senior lecturer, analytical microbiology, University of Surrey, Guildford, England. He believes that PCR assays are currently too biased for a single cutoff to be broadly used, and false-positive signals are most likely because of contamination.
Dana Wolf, MD, Clinical Virology Unit, Hadassah Hebrew University Medical Center in Israel, presented a large-scale data analysis of more than 133,000 pooled samples. Such a pooling strategy appeared to be highly efficient for a wide range of prevalence rates (<1% to 6%). “Our empirical evidence strongly projects on the feasibility and benefits of pooling in the current pandemic setting, to enhance continued surveillance, control, and community reopening,” she said.
Corine Geurts van Kessel, MD, PhD, Department of Virology, Erasmus University Rotterdam (the Netherlands), discussing antibodies testing for SARS-CoV-2, pointed out that disease severity can affect testing accuracy. “Reinfection cases tell us that we cannot rely on immunity acquired by natural infection to confer herd immunity,” she said.
Misinformation in the first digital pandemic
The world is not only facing a devastating pandemic, but also an alarming “infodemic” of misinformation. Between January and March 2020, a new COVID-19–related tweet appeared on Twitter every 45 milliseconds. Müge Çevik, MD, MSc, MRCP, an infectious disease clinician, scientist, and science communicator, said that “the greatest challenge for science communication is reaching the audience.”
People have always been skeptical of science reporting by journalists and would rather have scientists communicate with them directly, she noted. Science communication plays a dual role. “On one hand is the need to promote science to a wide audience in order to inform and educate and inspire the next generation of scientists, and on the other hand there is also a need to engage effectively in public dialogue,” she added. Dr. Çevik and colleagues think that “The responsibility of academics should not end with finding the truth. It should end after communicating it.”
Treatment in the ICU
Matteo Bassetti, MD, with the University of Genoa (Italy), who was asked about when to use remdesivir in the intensive care unit and for how long, said, “In the majority of cases, 5 days is probably enough.” However, if there is high viremia, he said, physicians may choose to continue the regimen beyond 5 days. Data show it is important to prescribe this drug for patients with oxygen support in an early phase, within 10 days of the first symptoms, he added. “In the late phase, there is a very limited role for remdesivir, as we know that we are already out of the viremic phase.” He also emphasized that there is no role for hydroxychloroquine or lopinavir-ritonavir.
Breaking the chains of transmission
During the wrap-up session, former US CDC Director Tom Frieden, MD, said, “We’re not even halfway through it” about the pandemic trajectory. “And we have to be very clear that the risk of explosive spread will not end with a vaccine.” He is now president and CEO of Resolve to Save Lives.
Different parts of the world will have very different experiences, Dr. Frieden said, noting that Africa, where 4% of the population is older than 65, has a very different risk level than Europe and the United States, where 10%-20% of people are in older age groups.
“We need a one-two punch,” he noted, first preventing spread, and when it does happen, boxing it in. Mask wearing is essential. “States in the US that mandated universal mask-wearing experienced much more rapid declines (in cases) for every 5 days the mandate was in place.”
Michael Ryan, MD, executive director for the WHO’s Health Emergencies Programme, added, “We need to collectively recommit to winning this game. We know how to break the chains of transmission. We need recommitment to a scientific, societal, and political strategy, and an alliance – a contract – between those entities to try to move us forward.”
This article first appeared on Medscape.com.
FROM IDWEEK 2020
Islatravir + doravirine maintains HIV viral suppression
according to new data.
ISL is a first-in-class nucleoside reverse transcriptase translocation inhibitor (NRTTI), Jean-Michel Molina, MD, PhD, of Saint‐Louis and Lariboisière Hospitals in Paris, explained at the annual HIV drug therapy meeting in Glasgow, Scotland. The randomized, double-blind, dose‐ranging trial compared ISL+DOR to a fixed‐dose combination of DOR, lamivudine, and tenofovir disoproxil fumarate (DOR/3TC/TDF) daily in 121 patients.
Patients in the ISL+DOR group initially received 0.25, 0.75, or 2.25 mg of ISL along with 100 mg of DOR and 200 mg of 3TC. Beginning at week 20, participants achieving HIV viral loads of 50 copies/mL or less discontinued 3TC but continued on their assigned dose of ISL+DOR for at least 24 weeks. At that point the investigators noted a greater number of discontinuations in the 2.25-mg group and settled on the 0.75-mg ISL dose. All patients in the ISL group were transitioned to that dose between weeks 60 and 72.
At week 96, 81.1% of the patients in the combined ISL group maintained viral loads <50 copies/mL, comparable to the 80.6% of those in the DOR/3TC/TDF group.
ISL+DOR appeared to be “well tolerated,” the investigators noted. They found drug-related adverse events in 7.8% of the patients in the ISL+DOR group compared with 22.6% of patients in the DOR/3TC/TDF group. In addition, among the 90 patients in the ISL+DOR group, no more than 5% of participants experienced any specific drug-related adverse event.
Source: HIV Glasgow 2020 Virtual Conference: Abstract O415. Oct. 5-8, 2020.
A version of this article originally appeared on Medscape.com.
according to new data.
ISL is a first-in-class nucleoside reverse transcriptase translocation inhibitor (NRTTI), Jean-Michel Molina, MD, PhD, of Saint‐Louis and Lariboisière Hospitals in Paris, explained at the annual HIV drug therapy meeting in Glasgow, Scotland. The randomized, double-blind, dose‐ranging trial compared ISL+DOR to a fixed‐dose combination of DOR, lamivudine, and tenofovir disoproxil fumarate (DOR/3TC/TDF) daily in 121 patients.
Patients in the ISL+DOR group initially received 0.25, 0.75, or 2.25 mg of ISL along with 100 mg of DOR and 200 mg of 3TC. Beginning at week 20, participants achieving HIV viral loads of 50 copies/mL or less discontinued 3TC but continued on their assigned dose of ISL+DOR for at least 24 weeks. At that point the investigators noted a greater number of discontinuations in the 2.25-mg group and settled on the 0.75-mg ISL dose. All patients in the ISL group were transitioned to that dose between weeks 60 and 72.
At week 96, 81.1% of the patients in the combined ISL group maintained viral loads <50 copies/mL, comparable to the 80.6% of those in the DOR/3TC/TDF group.
ISL+DOR appeared to be “well tolerated,” the investigators noted. They found drug-related adverse events in 7.8% of the patients in the ISL+DOR group compared with 22.6% of patients in the DOR/3TC/TDF group. In addition, among the 90 patients in the ISL+DOR group, no more than 5% of participants experienced any specific drug-related adverse event.
Source: HIV Glasgow 2020 Virtual Conference: Abstract O415. Oct. 5-8, 2020.
A version of this article originally appeared on Medscape.com.
according to new data.
ISL is a first-in-class nucleoside reverse transcriptase translocation inhibitor (NRTTI), Jean-Michel Molina, MD, PhD, of Saint‐Louis and Lariboisière Hospitals in Paris, explained at the annual HIV drug therapy meeting in Glasgow, Scotland. The randomized, double-blind, dose‐ranging trial compared ISL+DOR to a fixed‐dose combination of DOR, lamivudine, and tenofovir disoproxil fumarate (DOR/3TC/TDF) daily in 121 patients.
Patients in the ISL+DOR group initially received 0.25, 0.75, or 2.25 mg of ISL along with 100 mg of DOR and 200 mg of 3TC. Beginning at week 20, participants achieving HIV viral loads of 50 copies/mL or less discontinued 3TC but continued on their assigned dose of ISL+DOR for at least 24 weeks. At that point the investigators noted a greater number of discontinuations in the 2.25-mg group and settled on the 0.75-mg ISL dose. All patients in the ISL group were transitioned to that dose between weeks 60 and 72.
At week 96, 81.1% of the patients in the combined ISL group maintained viral loads <50 copies/mL, comparable to the 80.6% of those in the DOR/3TC/TDF group.
ISL+DOR appeared to be “well tolerated,” the investigators noted. They found drug-related adverse events in 7.8% of the patients in the ISL+DOR group compared with 22.6% of patients in the DOR/3TC/TDF group. In addition, among the 90 patients in the ISL+DOR group, no more than 5% of participants experienced any specific drug-related adverse event.
Source: HIV Glasgow 2020 Virtual Conference: Abstract O415. Oct. 5-8, 2020.
A version of this article originally appeared on Medscape.com.
Low-Dose Lamotrigine Safest Anti-Epileptic Drug in Pregnancy
Dose selection is as critical as is the choice of antiepileptic drug for avoiding birth defects in women with epilepsy, according to a large observational cohort study published online June 6 in The Lancet Neurology.
In a comparison of the four most commonly prescribed antiepileptic drugs, lamotrigine at a dose of less than 300 mg/day at the time of conception was the least likely to be associated with birth defects. Valproic acid at 1,500 mg/day or more was 16 times more likely to be associated with birth defects, according to the results of the multivariate analysis. Carbamazepine and phenobarbital carried intermediate levels of risk, depending on the dose.
The results came from an observational cohort study of 3,909 pregnancies representing 3,521 women in 42 countries between 1999 and 2010. All the women had epilepsy and were taking one of the four drugs at conception.
The investigators, led by Dr. Torbjörn Tomson of the Karolinska Institute, Stockholm, excluded pregnancies in women whose antiepilepsy prescription was changed during the first trimester, those who were exposed to antiepileptic polytherapy or to other potentially teratogenic medications, and women with comorbidities such as diabetes, toxoplasmosis, and HIV that are known to increase the risk of congenital malformations (Lancet Neurology 2011 June 6 [doi:10.1016/S1474-4422(11)70107-7]).
In their multivariate analysis, the investigators controlled for a host of potential confounders. These included maternal age, sex of child, parental history of major congenital malformations, geographical region, parity, type of epilepsy, generalized tonic-clonic seizures during the first trimester, parental education, and the use of folic acid.
The overall rate of birth defects among women taking one of the four drugs was 6%. The lowest doses of lamotrigine carried the lowest absolute risk of birth defects 17 of 836 pregnancies (2%). The highest doses of valproic acid carried the highest absolute risk; 24 of 99 pregnancies (24%) resulted in major congenital malformations.
The investigators compared all drugs and doses to lamotrigine at less than 300 mg/day. Lamotrigine at more than 300 mg/day carried 2.2 times the risk of birth defects.
The lowest dose of carbamazepine (less than 400 mg/day) was not statistically more risky than was low-dose lamotrigine. An intermediate dose of carbamazepine was associated with a 2.5-fold increase in risk, and carbamazepine at 1,000 mg/day or more was associated with a 4.6-fold increase in risk.
Phenobarbital at less than 150 mg/day was 2.5 times as risky as was low-dose lamotrigine, and phenobarbital at 150 mg/day or greater was 8.2 times as risky.
Valproic acid at less than 700 mg/day was 2.8 times as risky as was low-dose lamotrigine, intermediate doses of valproic acid were 5.8 times as risky, and doses of 1,500 mg/day or more were 16.1 times as risky.
Except for the lowest dose of carbamazepine, all increases in risk associated with the drugs were statistically significant when compared to low-dose lamotrigine.
The only nondrug covariates that proved to carry a significant increase in risk were folate supplementation and a parental history of major congenital malformations. Inappropriate folicate use increased the risk of birth defects by 40%, compared with appropriate use. A parental history of birth defects carried a 4.4-fold increase in risk compared to pregnancies without that characteristic.
"Our findings show that the risk of major congenital malformations increases dose-dependently with all assessed antiepileptic drugs," the investigators wrote. "The approach generally accepted by physicians so far has been to identify, before conception, the lowest effective dose of the drug that is most appropriate for the woman’s epilepsy. Our study gives the prescriber the possibility of assessing how teratogenic risks at that dose compare with the risks associated with alternative treatments at various doses. Our data suggest that many women can enter pregnancy at low doses and maintain seizure control, although in many such cases dose adjustment might be needed later in pregnancy."
The study was funded by Eisai, GlaxoSmithKline, Janssen-Cilag, Novartis, Pfizer, Sanofi-Aventis, UCB, Netherlands Epilepsy Foundation, Stockholm County Council, and ALF. All but one of the eight investigators reported relationships with numerous pharmaceutical companies. The authors stated that the sponsors had no role in study design, data collection, data analysis, data interpretation, or writing the report.
"The findings are important to the clinician treating people with epilepsy because they provide specific information not only on the drug but also on the dose. It is easy to recommend against use of a specific drug (valproic acid, for instance) because of a higher risk of malformations, but if seizure control is not possible with alternative therapeutic regimens, such recommendations are difficult to implement. The data provide another reason for use of the lowest dose of a drug associated with optimum seizure control. Incidence of major congenital malformations associated with a low dose of a higher-risk drug might be lower than that associated with a high dose of a lower-risk drug."
Dr. W. Allen Hauser is professor of neurology and epidemiology at the Columbia University College of Physicians and Surgeons in New York. His comments come from an editorial accompanying the report in The Lancet Neurology (2011 June 6 [doi:10.1016/S1474-4422(11)70129-6]).
"The findings are important to the clinician treating people with epilepsy because they provide specific information not only on the drug but also on the dose. It is easy to recommend against use of a specific drug (valproic acid, for instance) because of a higher risk of malformations, but if seizure control is not possible with alternative therapeutic regimens, such recommendations are difficult to implement. The data provide another reason for use of the lowest dose of a drug associated with optimum seizure control. Incidence of major congenital malformations associated with a low dose of a higher-risk drug might be lower than that associated with a high dose of a lower-risk drug."
Dr. W. Allen Hauser is professor of neurology and epidemiology at the Columbia University College of Physicians and Surgeons in New York. His comments come from an editorial accompanying the report in The Lancet Neurology (2011 June 6 [doi:10.1016/S1474-4422(11)70129-6]).
"The findings are important to the clinician treating people with epilepsy because they provide specific information not only on the drug but also on the dose. It is easy to recommend against use of a specific drug (valproic acid, for instance) because of a higher risk of malformations, but if seizure control is not possible with alternative therapeutic regimens, such recommendations are difficult to implement. The data provide another reason for use of the lowest dose of a drug associated with optimum seizure control. Incidence of major congenital malformations associated with a low dose of a higher-risk drug might be lower than that associated with a high dose of a lower-risk drug."
Dr. W. Allen Hauser is professor of neurology and epidemiology at the Columbia University College of Physicians and Surgeons in New York. His comments come from an editorial accompanying the report in The Lancet Neurology (2011 June 6 [doi:10.1016/S1474-4422(11)70129-6]).
Dose selection is as critical as is the choice of antiepileptic drug for avoiding birth defects in women with epilepsy, according to a large observational cohort study published online June 6 in The Lancet Neurology.
In a comparison of the four most commonly prescribed antiepileptic drugs, lamotrigine at a dose of less than 300 mg/day at the time of conception was the least likely to be associated with birth defects. Valproic acid at 1,500 mg/day or more was 16 times more likely to be associated with birth defects, according to the results of the multivariate analysis. Carbamazepine and phenobarbital carried intermediate levels of risk, depending on the dose.
The results came from an observational cohort study of 3,909 pregnancies representing 3,521 women in 42 countries between 1999 and 2010. All the women had epilepsy and were taking one of the four drugs at conception.
The investigators, led by Dr. Torbjörn Tomson of the Karolinska Institute, Stockholm, excluded pregnancies in women whose antiepilepsy prescription was changed during the first trimester, those who were exposed to antiepileptic polytherapy or to other potentially teratogenic medications, and women with comorbidities such as diabetes, toxoplasmosis, and HIV that are known to increase the risk of congenital malformations (Lancet Neurology 2011 June 6 [doi:10.1016/S1474-4422(11)70107-7]).
In their multivariate analysis, the investigators controlled for a host of potential confounders. These included maternal age, sex of child, parental history of major congenital malformations, geographical region, parity, type of epilepsy, generalized tonic-clonic seizures during the first trimester, parental education, and the use of folic acid.
The overall rate of birth defects among women taking one of the four drugs was 6%. The lowest doses of lamotrigine carried the lowest absolute risk of birth defects 17 of 836 pregnancies (2%). The highest doses of valproic acid carried the highest absolute risk; 24 of 99 pregnancies (24%) resulted in major congenital malformations.
The investigators compared all drugs and doses to lamotrigine at less than 300 mg/day. Lamotrigine at more than 300 mg/day carried 2.2 times the risk of birth defects.
The lowest dose of carbamazepine (less than 400 mg/day) was not statistically more risky than was low-dose lamotrigine. An intermediate dose of carbamazepine was associated with a 2.5-fold increase in risk, and carbamazepine at 1,000 mg/day or more was associated with a 4.6-fold increase in risk.
Phenobarbital at less than 150 mg/day was 2.5 times as risky as was low-dose lamotrigine, and phenobarbital at 150 mg/day or greater was 8.2 times as risky.
Valproic acid at less than 700 mg/day was 2.8 times as risky as was low-dose lamotrigine, intermediate doses of valproic acid were 5.8 times as risky, and doses of 1,500 mg/day or more were 16.1 times as risky.
Except for the lowest dose of carbamazepine, all increases in risk associated with the drugs were statistically significant when compared to low-dose lamotrigine.
The only nondrug covariates that proved to carry a significant increase in risk were folate supplementation and a parental history of major congenital malformations. Inappropriate folicate use increased the risk of birth defects by 40%, compared with appropriate use. A parental history of birth defects carried a 4.4-fold increase in risk compared to pregnancies without that characteristic.
"Our findings show that the risk of major congenital malformations increases dose-dependently with all assessed antiepileptic drugs," the investigators wrote. "The approach generally accepted by physicians so far has been to identify, before conception, the lowest effective dose of the drug that is most appropriate for the woman’s epilepsy. Our study gives the prescriber the possibility of assessing how teratogenic risks at that dose compare with the risks associated with alternative treatments at various doses. Our data suggest that many women can enter pregnancy at low doses and maintain seizure control, although in many such cases dose adjustment might be needed later in pregnancy."
The study was funded by Eisai, GlaxoSmithKline, Janssen-Cilag, Novartis, Pfizer, Sanofi-Aventis, UCB, Netherlands Epilepsy Foundation, Stockholm County Council, and ALF. All but one of the eight investigators reported relationships with numerous pharmaceutical companies. The authors stated that the sponsors had no role in study design, data collection, data analysis, data interpretation, or writing the report.
Dose selection is as critical as is the choice of antiepileptic drug for avoiding birth defects in women with epilepsy, according to a large observational cohort study published online June 6 in The Lancet Neurology.
In a comparison of the four most commonly prescribed antiepileptic drugs, lamotrigine at a dose of less than 300 mg/day at the time of conception was the least likely to be associated with birth defects. Valproic acid at 1,500 mg/day or more was 16 times more likely to be associated with birth defects, according to the results of the multivariate analysis. Carbamazepine and phenobarbital carried intermediate levels of risk, depending on the dose.
The results came from an observational cohort study of 3,909 pregnancies representing 3,521 women in 42 countries between 1999 and 2010. All the women had epilepsy and were taking one of the four drugs at conception.
The investigators, led by Dr. Torbjörn Tomson of the Karolinska Institute, Stockholm, excluded pregnancies in women whose antiepilepsy prescription was changed during the first trimester, those who were exposed to antiepileptic polytherapy or to other potentially teratogenic medications, and women with comorbidities such as diabetes, toxoplasmosis, and HIV that are known to increase the risk of congenital malformations (Lancet Neurology 2011 June 6 [doi:10.1016/S1474-4422(11)70107-7]).
In their multivariate analysis, the investigators controlled for a host of potential confounders. These included maternal age, sex of child, parental history of major congenital malformations, geographical region, parity, type of epilepsy, generalized tonic-clonic seizures during the first trimester, parental education, and the use of folic acid.
The overall rate of birth defects among women taking one of the four drugs was 6%. The lowest doses of lamotrigine carried the lowest absolute risk of birth defects 17 of 836 pregnancies (2%). The highest doses of valproic acid carried the highest absolute risk; 24 of 99 pregnancies (24%) resulted in major congenital malformations.
The investigators compared all drugs and doses to lamotrigine at less than 300 mg/day. Lamotrigine at more than 300 mg/day carried 2.2 times the risk of birth defects.
The lowest dose of carbamazepine (less than 400 mg/day) was not statistically more risky than was low-dose lamotrigine. An intermediate dose of carbamazepine was associated with a 2.5-fold increase in risk, and carbamazepine at 1,000 mg/day or more was associated with a 4.6-fold increase in risk.
Phenobarbital at less than 150 mg/day was 2.5 times as risky as was low-dose lamotrigine, and phenobarbital at 150 mg/day or greater was 8.2 times as risky.
Valproic acid at less than 700 mg/day was 2.8 times as risky as was low-dose lamotrigine, intermediate doses of valproic acid were 5.8 times as risky, and doses of 1,500 mg/day or more were 16.1 times as risky.
Except for the lowest dose of carbamazepine, all increases in risk associated with the drugs were statistically significant when compared to low-dose lamotrigine.
The only nondrug covariates that proved to carry a significant increase in risk were folate supplementation and a parental history of major congenital malformations. Inappropriate folicate use increased the risk of birth defects by 40%, compared with appropriate use. A parental history of birth defects carried a 4.4-fold increase in risk compared to pregnancies without that characteristic.
"Our findings show that the risk of major congenital malformations increases dose-dependently with all assessed antiepileptic drugs," the investigators wrote. "The approach generally accepted by physicians so far has been to identify, before conception, the lowest effective dose of the drug that is most appropriate for the woman’s epilepsy. Our study gives the prescriber the possibility of assessing how teratogenic risks at that dose compare with the risks associated with alternative treatments at various doses. Our data suggest that many women can enter pregnancy at low doses and maintain seizure control, although in many such cases dose adjustment might be needed later in pregnancy."
The study was funded by Eisai, GlaxoSmithKline, Janssen-Cilag, Novartis, Pfizer, Sanofi-Aventis, UCB, Netherlands Epilepsy Foundation, Stockholm County Council, and ALF. All but one of the eight investigators reported relationships with numerous pharmaceutical companies. The authors stated that the sponsors had no role in study design, data collection, data analysis, data interpretation, or writing the report.
FROM THE LANCET NEUROLOGY
Major Finding: Of four common antiepileptic drugs, lamotrigine at a dose of less than 300 mg/day had the lowest teratogenic potential. Valproic acid at a dose of 1,500 mg/day was 16-fold more likely than was low-dose lamotrigine to cause birth defects.
Data Source: Observational cohort study of 3,909 pregnancies representing 3,521 women.
Disclosures: The study was funded by Eisai, GlaxoSmithKline, Janssen-Cilag, Novartis, Pfizer, Sanofi-Aventis, UCB, Netherlands Epilepsy Foundation, Stockholm County Council, and ALF. All but one of the eight investigators reported relationships with a variety of pharmaceutical companies. The authors stated that the sponsors had no role in study design, data collection, data analysis, data interpretation, or writing the report.
Low-Dose Lamotrigine Safest Anti-Epileptic Drug in Pregnancy
Dose selection is as critical as is the choice of antiepileptic drug for avoiding birth defects in women with epilepsy, according to a large observational cohort study published online June 6 in The Lancet Neurology.
In a comparison of the four most commonly prescribed antiepileptic drugs, lamotrigine at a dose of less than 300 mg/day at the time of conception was the least likely to be associated with birth defects. Valproic acid at 1,500 mg/day or more was 16 times more likely to be associated with birth defects, according to the results of the multivariate analysis. Carbamazepine and phenobarbital carried intermediate levels of risk, depending on the dose.
The results came from an observational cohort study of 3,909 pregnancies representing 3,521 women in 42 countries between 1999 and 2010. All the women had epilepsy and were taking one of the four drugs at conception.
The investigators, led by Dr. Torbjörn Tomson of the Karolinska Institute, Stockholm, excluded pregnancies in women whose antiepilepsy prescription was changed during the first trimester, those who were exposed to antiepileptic polytherapy or to other potentially teratogenic medications, and women with comorbidities such as diabetes, toxoplasmosis, and HIV that are known to increase the risk of congenital malformations (Lancet Neurology 2011 June 6 [doi:10.1016/S1474-4422(11)70107-7]).
In their multivariate analysis, the investigators controlled for a host of potential confounders. These included maternal age, sex of child, parental history of major congenital malformations, geographical region, parity, type of epilepsy, generalized tonic-clonic seizures during the first trimester, parental education, and the use of folic acid.
The overall rate of birth defects among women taking one of the four drugs was 6%. The lowest doses of lamotrigine carried the lowest absolute risk of birth defects 17 of 836 pregnancies (2%). The highest doses of valproic acid carried the highest absolute risk; 24 of 99 pregnancies (24%) resulted in major congenital malformations.
The investigators compared all drugs and doses to lamotrigine at less than 300 mg/day. Lamotrigine at more than 300 mg/day carried 2.2 times the risk of birth defects.
The lowest dose of carbamazepine (less than 400 mg/day) was not statistically more risky than was low-dose lamotrigine. An intermediate dose of carbamazepine was associated with a 2.5-fold increase in risk, and carbamazepine at 1,000 mg/day or more was associated with a 4.6-fold increase in risk.
Phenobarbital at less than 150 mg/day was 2.5 times as risky as was low-dose lamotrigine, and phenobarbital at 150 mg/day or greater was 8.2 times as risky.
Valproic acid at less than 700 mg/day was 2.8 times as risky as was low-dose lamotrigine, intermediate doses of valproic acid were 5.8 times as risky, and doses of 1,500 mg/day or more were 16.1 times as risky.
Except for the lowest dose of carbamazepine, all increases in risk associated with the drugs were statistically significant when compared to low-dose lamotrigine.
The only nondrug covariates that proved to carry a significant increase in risk were folate supplementation and a parental history of major congenital malformations. Inappropriate folicate use increased the risk of birth defects by 40%, compared with appropriate use. A parental history of birth defects carried a 4.4-fold increase in risk compared to pregnancies without that characteristic.
"Our findings show that the risk of major congenital malformations increases dose-dependently with all assessed antiepileptic drugs," the investigators wrote. "The approach generally accepted by physicians so far has been to identify, before conception, the lowest effective dose of the drug that is most appropriate for the woman’s epilepsy. Our study gives the prescriber the possibility of assessing how teratogenic risks at that dose compare with the risks associated with alternative treatments at various doses. Our data suggest that many women can enter pregnancy at low doses and maintain seizure control, although in many such cases dose adjustment might be needed later in pregnancy."
The study was funded by Eisai, GlaxoSmithKline, Janssen-Cilag, Novartis, Pfizer, Sanofi-Aventis, UCB, Netherlands Epilepsy Foundation, Stockholm County Council, and ALF. All but one of the eight investigators reported relationships with numerous pharmaceutical companies. The authors stated that the sponsors had no role in study design, data collection, data analysis, data interpretation, or writing the report.
"The findings are important to the clinician treating people with epilepsy because they provide specific information not only on the drug but also on the dose. It is easy to recommend against use of a specific drug (valproic acid, for instance) because of a higher risk of malformations, but if seizure control is not possible with alternative therapeutic regimens, such recommendations are difficult to implement. The data provide another reason for use of the lowest dose of a drug associated with optimum seizure control. Incidence of major congenital malformations associated with a low dose of a higher-risk drug might be lower than that associated with a high dose of a lower-risk drug."
Dr. W. Allen Hauser is professor of neurology and epidemiology at the Columbia University College of Physicians and Surgeons in New York. His comments come from an editorial accompanying the report in The Lancet Neurology (2011 June 6 [doi:10.1016/S1474-4422(11)70129-6]).
"The findings are important to the clinician treating people with epilepsy because they provide specific information not only on the drug but also on the dose. It is easy to recommend against use of a specific drug (valproic acid, for instance) because of a higher risk of malformations, but if seizure control is not possible with alternative therapeutic regimens, such recommendations are difficult to implement. The data provide another reason for use of the lowest dose of a drug associated with optimum seizure control. Incidence of major congenital malformations associated with a low dose of a higher-risk drug might be lower than that associated with a high dose of a lower-risk drug."
Dr. W. Allen Hauser is professor of neurology and epidemiology at the Columbia University College of Physicians and Surgeons in New York. His comments come from an editorial accompanying the report in The Lancet Neurology (2011 June 6 [doi:10.1016/S1474-4422(11)70129-6]).
"The findings are important to the clinician treating people with epilepsy because they provide specific information not only on the drug but also on the dose. It is easy to recommend against use of a specific drug (valproic acid, for instance) because of a higher risk of malformations, but if seizure control is not possible with alternative therapeutic regimens, such recommendations are difficult to implement. The data provide another reason for use of the lowest dose of a drug associated with optimum seizure control. Incidence of major congenital malformations associated with a low dose of a higher-risk drug might be lower than that associated with a high dose of a lower-risk drug."
Dr. W. Allen Hauser is professor of neurology and epidemiology at the Columbia University College of Physicians and Surgeons in New York. His comments come from an editorial accompanying the report in The Lancet Neurology (2011 June 6 [doi:10.1016/S1474-4422(11)70129-6]).
Dose selection is as critical as is the choice of antiepileptic drug for avoiding birth defects in women with epilepsy, according to a large observational cohort study published online June 6 in The Lancet Neurology.
In a comparison of the four most commonly prescribed antiepileptic drugs, lamotrigine at a dose of less than 300 mg/day at the time of conception was the least likely to be associated with birth defects. Valproic acid at 1,500 mg/day or more was 16 times more likely to be associated with birth defects, according to the results of the multivariate analysis. Carbamazepine and phenobarbital carried intermediate levels of risk, depending on the dose.
The results came from an observational cohort study of 3,909 pregnancies representing 3,521 women in 42 countries between 1999 and 2010. All the women had epilepsy and were taking one of the four drugs at conception.
The investigators, led by Dr. Torbjörn Tomson of the Karolinska Institute, Stockholm, excluded pregnancies in women whose antiepilepsy prescription was changed during the first trimester, those who were exposed to antiepileptic polytherapy or to other potentially teratogenic medications, and women with comorbidities such as diabetes, toxoplasmosis, and HIV that are known to increase the risk of congenital malformations (Lancet Neurology 2011 June 6 [doi:10.1016/S1474-4422(11)70107-7]).
In their multivariate analysis, the investigators controlled for a host of potential confounders. These included maternal age, sex of child, parental history of major congenital malformations, geographical region, parity, type of epilepsy, generalized tonic-clonic seizures during the first trimester, parental education, and the use of folic acid.
The overall rate of birth defects among women taking one of the four drugs was 6%. The lowest doses of lamotrigine carried the lowest absolute risk of birth defects 17 of 836 pregnancies (2%). The highest doses of valproic acid carried the highest absolute risk; 24 of 99 pregnancies (24%) resulted in major congenital malformations.
The investigators compared all drugs and doses to lamotrigine at less than 300 mg/day. Lamotrigine at more than 300 mg/day carried 2.2 times the risk of birth defects.
The lowest dose of carbamazepine (less than 400 mg/day) was not statistically more risky than was low-dose lamotrigine. An intermediate dose of carbamazepine was associated with a 2.5-fold increase in risk, and carbamazepine at 1,000 mg/day or more was associated with a 4.6-fold increase in risk.
Phenobarbital at less than 150 mg/day was 2.5 times as risky as was low-dose lamotrigine, and phenobarbital at 150 mg/day or greater was 8.2 times as risky.
Valproic acid at less than 700 mg/day was 2.8 times as risky as was low-dose lamotrigine, intermediate doses of valproic acid were 5.8 times as risky, and doses of 1,500 mg/day or more were 16.1 times as risky.
Except for the lowest dose of carbamazepine, all increases in risk associated with the drugs were statistically significant when compared to low-dose lamotrigine.
The only nondrug covariates that proved to carry a significant increase in risk were folate supplementation and a parental history of major congenital malformations. Inappropriate folicate use increased the risk of birth defects by 40%, compared with appropriate use. A parental history of birth defects carried a 4.4-fold increase in risk compared to pregnancies without that characteristic.
"Our findings show that the risk of major congenital malformations increases dose-dependently with all assessed antiepileptic drugs," the investigators wrote. "The approach generally accepted by physicians so far has been to identify, before conception, the lowest effective dose of the drug that is most appropriate for the woman’s epilepsy. Our study gives the prescriber the possibility of assessing how teratogenic risks at that dose compare with the risks associated with alternative treatments at various doses. Our data suggest that many women can enter pregnancy at low doses and maintain seizure control, although in many such cases dose adjustment might be needed later in pregnancy."
The study was funded by Eisai, GlaxoSmithKline, Janssen-Cilag, Novartis, Pfizer, Sanofi-Aventis, UCB, Netherlands Epilepsy Foundation, Stockholm County Council, and ALF. All but one of the eight investigators reported relationships with numerous pharmaceutical companies. The authors stated that the sponsors had no role in study design, data collection, data analysis, data interpretation, or writing the report.
Dose selection is as critical as is the choice of antiepileptic drug for avoiding birth defects in women with epilepsy, according to a large observational cohort study published online June 6 in The Lancet Neurology.
In a comparison of the four most commonly prescribed antiepileptic drugs, lamotrigine at a dose of less than 300 mg/day at the time of conception was the least likely to be associated with birth defects. Valproic acid at 1,500 mg/day or more was 16 times more likely to be associated with birth defects, according to the results of the multivariate analysis. Carbamazepine and phenobarbital carried intermediate levels of risk, depending on the dose.
The results came from an observational cohort study of 3,909 pregnancies representing 3,521 women in 42 countries between 1999 and 2010. All the women had epilepsy and were taking one of the four drugs at conception.
The investigators, led by Dr. Torbjörn Tomson of the Karolinska Institute, Stockholm, excluded pregnancies in women whose antiepilepsy prescription was changed during the first trimester, those who were exposed to antiepileptic polytherapy or to other potentially teratogenic medications, and women with comorbidities such as diabetes, toxoplasmosis, and HIV that are known to increase the risk of congenital malformations (Lancet Neurology 2011 June 6 [doi:10.1016/S1474-4422(11)70107-7]).
In their multivariate analysis, the investigators controlled for a host of potential confounders. These included maternal age, sex of child, parental history of major congenital malformations, geographical region, parity, type of epilepsy, generalized tonic-clonic seizures during the first trimester, parental education, and the use of folic acid.
The overall rate of birth defects among women taking one of the four drugs was 6%. The lowest doses of lamotrigine carried the lowest absolute risk of birth defects 17 of 836 pregnancies (2%). The highest doses of valproic acid carried the highest absolute risk; 24 of 99 pregnancies (24%) resulted in major congenital malformations.
The investigators compared all drugs and doses to lamotrigine at less than 300 mg/day. Lamotrigine at more than 300 mg/day carried 2.2 times the risk of birth defects.
The lowest dose of carbamazepine (less than 400 mg/day) was not statistically more risky than was low-dose lamotrigine. An intermediate dose of carbamazepine was associated with a 2.5-fold increase in risk, and carbamazepine at 1,000 mg/day or more was associated with a 4.6-fold increase in risk.
Phenobarbital at less than 150 mg/day was 2.5 times as risky as was low-dose lamotrigine, and phenobarbital at 150 mg/day or greater was 8.2 times as risky.
Valproic acid at less than 700 mg/day was 2.8 times as risky as was low-dose lamotrigine, intermediate doses of valproic acid were 5.8 times as risky, and doses of 1,500 mg/day or more were 16.1 times as risky.
Except for the lowest dose of carbamazepine, all increases in risk associated with the drugs were statistically significant when compared to low-dose lamotrigine.
The only nondrug covariates that proved to carry a significant increase in risk were folate supplementation and a parental history of major congenital malformations. Inappropriate folicate use increased the risk of birth defects by 40%, compared with appropriate use. A parental history of birth defects carried a 4.4-fold increase in risk compared to pregnancies without that characteristic.
"Our findings show that the risk of major congenital malformations increases dose-dependently with all assessed antiepileptic drugs," the investigators wrote. "The approach generally accepted by physicians so far has been to identify, before conception, the lowest effective dose of the drug that is most appropriate for the woman’s epilepsy. Our study gives the prescriber the possibility of assessing how teratogenic risks at that dose compare with the risks associated with alternative treatments at various doses. Our data suggest that many women can enter pregnancy at low doses and maintain seizure control, although in many such cases dose adjustment might be needed later in pregnancy."
The study was funded by Eisai, GlaxoSmithKline, Janssen-Cilag, Novartis, Pfizer, Sanofi-Aventis, UCB, Netherlands Epilepsy Foundation, Stockholm County Council, and ALF. All but one of the eight investigators reported relationships with numerous pharmaceutical companies. The authors stated that the sponsors had no role in study design, data collection, data analysis, data interpretation, or writing the report.
FROM THE LANCET NEUROLOGY
Major Finding: Of four common antiepileptic drugs, lamotrigine at a dose of less than 300 mg/day had the lowest teratogenic potential. Valproic acid at a dose of 1,500 mg/day was 16-fold more likely than was low-dose lamotrigine to cause birth defects.
Data Source: Observational cohort study of 3,909 pregnancies representing 3,521 women.
Disclosures: The study was funded by Eisai, GlaxoSmithKline, Janssen-Cilag, Novartis, Pfizer, Sanofi-Aventis, UCB, Netherlands Epilepsy Foundation, Stockholm County Council, and ALF. All but one of the eight investigators reported relationships with a variety of pharmaceutical companies. The authors stated that the sponsors had no role in study design, data collection, data analysis, data interpretation, or writing the report.
Low-Dose Lamotrigine Safest Anti-Epileptic Drug in Pregnancy
Dose selection is as critical as is the choice of antiepileptic drug for avoiding birth defects in women with epilepsy, according to a large observational cohort study published online June 6 in The Lancet Neurology.
In a comparison of the four most commonly prescribed antiepileptic drugs, lamotrigine at a dose of less than 300 mg/day at the time of conception was the least likely to be associated with birth defects. Valproic acid at 1,500 mg/day or more was 16 times more likely to be associated with birth defects, according to the results of the multivariate analysis. Carbamazepine and phenobarbital carried intermediate levels of risk, depending on the dose.
The results came from an observational cohort study of 3,909 pregnancies representing 3,521 women in 42 countries between 1999 and 2010. All the women had epilepsy and were taking one of the four drugs at conception.
The investigators, led by Dr. Torbjörn Tomson of the Karolinska Institute, Stockholm, excluded pregnancies in women whose antiepilepsy prescription was changed during the first trimester, those who were exposed to antiepileptic polytherapy or to other potentially teratogenic medications, and women with comorbidities such as diabetes, toxoplasmosis, and HIV that are known to increase the risk of congenital malformations (Lancet Neurology 2011 June 6 [doi:10.1016/S1474-4422(11)70107-7]).
In their multivariate analysis, the investigators controlled for a host of potential confounders. These included maternal age, sex of child, parental history of major congenital malformations, geographical region, parity, type of epilepsy, generalized tonic-clonic seizures during the first trimester, parental education, and the use of folic acid.
The overall rate of birth defects among women taking one of the four drugs was 6%. The lowest doses of lamotrigine carried the lowest absolute risk of birth defects 17 of 836 pregnancies (2%). The highest doses of valproic acid carried the highest absolute risk; 24 of 99 pregnancies (24%) resulted in major congenital malformations.
The investigators compared all drugs and doses to lamotrigine at less than 300 mg/day. Lamotrigine at more than 300 mg/day carried 2.2 times the risk of birth defects.
The lowest dose of carbamazepine (less than 400 mg/day) was not statistically more risky than was low-dose lamotrigine. An intermediate dose of carbamazepine was associated with a 2.5-fold increase in risk, and carbamazepine at 1,000 mg/day or more was associated with a 4.6-fold increase in risk.
Phenobarbital at less than 150 mg/day was 2.5 times as risky as was low-dose lamotrigine, and phenobarbital at 150 mg/day or greater was 8.2 times as risky.
Valproic acid at less than 700 mg/day was 2.8 times as risky as was low-dose lamotrigine, intermediate doses of valproic acid were 5.8 times as risky, and doses of 1,500 mg/day or more were 16.1 times as risky.
Except for the lowest dose of carbamazepine, all increases in risk associated with the drugs were statistically significant when compared to low-dose lamotrigine.
The only nondrug covariates that proved to carry a significant increase in risk were folate supplementation and a parental history of major congenital malformations. Inappropriate folicate use increased the risk of birth defects by 40%, compared with appropriate use. A parental history of birth defects carried a 4.4-fold increase in risk compared to pregnancies without that characteristic.
"Our findings show that the risk of major congenital malformations increases dose-dependently with all assessed antiepileptic drugs," the investigators wrote. "The approach generally accepted by physicians so far has been to identify, before conception, the lowest effective dose of the drug that is most appropriate for the woman’s epilepsy. Our study gives the prescriber the possibility of assessing how teratogenic risks at that dose compare with the risks associated with alternative treatments at various doses. Our data suggest that many women can enter pregnancy at low doses and maintain seizure control, although in many such cases dose adjustment might be needed later in pregnancy."
The study was funded by Eisai, GlaxoSmithKline, Janssen-Cilag, Novartis, Pfizer, Sanofi-Aventis, UCB, Netherlands Epilepsy Foundation, Stockholm County Council, and ALF. All but one of the eight investigators reported relationships with numerous pharmaceutical companies. The authors stated that the sponsors had no role in study design, data collection, data analysis, data interpretation, or writing the report.
"The findings are important to the clinician treating people with epilepsy because they provide specific information not only on the drug but also on the dose. It is easy to recommend against use of a specific drug (valproic acid, for instance) because of a higher risk of malformations, but if seizure control is not possible with alternative therapeutic regimens, such recommendations are difficult to implement. The data provide another reason for use of the lowest dose of a drug associated with optimum seizure control. Incidence of major congenital malformations associated with a low dose of a higher-risk drug might be lower than that associated with a high dose of a lower-risk drug."
Dr. W. Allen Hauser is professor of neurology and epidemiology at the Columbia University College of Physicians and Surgeons in New York. His comments come from an editorial accompanying the report in The Lancet Neurology (2011 June 6 [doi:10.1016/S1474-4422(11)70129-6]).
"The findings are important to the clinician treating people with epilepsy because they provide specific information not only on the drug but also on the dose. It is easy to recommend against use of a specific drug (valproic acid, for instance) because of a higher risk of malformations, but if seizure control is not possible with alternative therapeutic regimens, such recommendations are difficult to implement. The data provide another reason for use of the lowest dose of a drug associated with optimum seizure control. Incidence of major congenital malformations associated with a low dose of a higher-risk drug might be lower than that associated with a high dose of a lower-risk drug."
Dr. W. Allen Hauser is professor of neurology and epidemiology at the Columbia University College of Physicians and Surgeons in New York. His comments come from an editorial accompanying the report in The Lancet Neurology (2011 June 6 [doi:10.1016/S1474-4422(11)70129-6]).
"The findings are important to the clinician treating people with epilepsy because they provide specific information not only on the drug but also on the dose. It is easy to recommend against use of a specific drug (valproic acid, for instance) because of a higher risk of malformations, but if seizure control is not possible with alternative therapeutic regimens, such recommendations are difficult to implement. The data provide another reason for use of the lowest dose of a drug associated with optimum seizure control. Incidence of major congenital malformations associated with a low dose of a higher-risk drug might be lower than that associated with a high dose of a lower-risk drug."
Dr. W. Allen Hauser is professor of neurology and epidemiology at the Columbia University College of Physicians and Surgeons in New York. His comments come from an editorial accompanying the report in The Lancet Neurology (2011 June 6 [doi:10.1016/S1474-4422(11)70129-6]).
Dose selection is as critical as is the choice of antiepileptic drug for avoiding birth defects in women with epilepsy, according to a large observational cohort study published online June 6 in The Lancet Neurology.
In a comparison of the four most commonly prescribed antiepileptic drugs, lamotrigine at a dose of less than 300 mg/day at the time of conception was the least likely to be associated with birth defects. Valproic acid at 1,500 mg/day or more was 16 times more likely to be associated with birth defects, according to the results of the multivariate analysis. Carbamazepine and phenobarbital carried intermediate levels of risk, depending on the dose.
The results came from an observational cohort study of 3,909 pregnancies representing 3,521 women in 42 countries between 1999 and 2010. All the women had epilepsy and were taking one of the four drugs at conception.
The investigators, led by Dr. Torbjörn Tomson of the Karolinska Institute, Stockholm, excluded pregnancies in women whose antiepilepsy prescription was changed during the first trimester, those who were exposed to antiepileptic polytherapy or to other potentially teratogenic medications, and women with comorbidities such as diabetes, toxoplasmosis, and HIV that are known to increase the risk of congenital malformations (Lancet Neurology 2011 June 6 [doi:10.1016/S1474-4422(11)70107-7]).
In their multivariate analysis, the investigators controlled for a host of potential confounders. These included maternal age, sex of child, parental history of major congenital malformations, geographical region, parity, type of epilepsy, generalized tonic-clonic seizures during the first trimester, parental education, and the use of folic acid.
The overall rate of birth defects among women taking one of the four drugs was 6%. The lowest doses of lamotrigine carried the lowest absolute risk of birth defects 17 of 836 pregnancies (2%). The highest doses of valproic acid carried the highest absolute risk; 24 of 99 pregnancies (24%) resulted in major congenital malformations.
The investigators compared all drugs and doses to lamotrigine at less than 300 mg/day. Lamotrigine at more than 300 mg/day carried 2.2 times the risk of birth defects.
The lowest dose of carbamazepine (less than 400 mg/day) was not statistically more risky than was low-dose lamotrigine. An intermediate dose of carbamazepine was associated with a 2.5-fold increase in risk, and carbamazepine at 1,000 mg/day or more was associated with a 4.6-fold increase in risk.
Phenobarbital at less than 150 mg/day was 2.5 times as risky as was low-dose lamotrigine, and phenobarbital at 150 mg/day or greater was 8.2 times as risky.
Valproic acid at less than 700 mg/day was 2.8 times as risky as was low-dose lamotrigine, intermediate doses of valproic acid were 5.8 times as risky, and doses of 1,500 mg/day or more were 16.1 times as risky.
Except for the lowest dose of carbamazepine, all increases in risk associated with the drugs were statistically significant when compared to low-dose lamotrigine.
The only nondrug covariates that proved to carry a significant increase in risk were folate supplementation and a parental history of major congenital malformations. Inappropriate folicate use increased the risk of birth defects by 40%, compared with appropriate use. A parental history of birth defects carried a 4.4-fold increase in risk compared to pregnancies without that characteristic.
"Our findings show that the risk of major congenital malformations increases dose-dependently with all assessed antiepileptic drugs," the investigators wrote. "The approach generally accepted by physicians so far has been to identify, before conception, the lowest effective dose of the drug that is most appropriate for the woman’s epilepsy. Our study gives the prescriber the possibility of assessing how teratogenic risks at that dose compare with the risks associated with alternative treatments at various doses. Our data suggest that many women can enter pregnancy at low doses and maintain seizure control, although in many such cases dose adjustment might be needed later in pregnancy."
The study was funded by Eisai, GlaxoSmithKline, Janssen-Cilag, Novartis, Pfizer, Sanofi-Aventis, UCB, Netherlands Epilepsy Foundation, Stockholm County Council, and ALF. All but one of the eight investigators reported relationships with numerous pharmaceutical companies. The authors stated that the sponsors had no role in study design, data collection, data analysis, data interpretation, or writing the report.
Dose selection is as critical as is the choice of antiepileptic drug for avoiding birth defects in women with epilepsy, according to a large observational cohort study published online June 6 in The Lancet Neurology.
In a comparison of the four most commonly prescribed antiepileptic drugs, lamotrigine at a dose of less than 300 mg/day at the time of conception was the least likely to be associated with birth defects. Valproic acid at 1,500 mg/day or more was 16 times more likely to be associated with birth defects, according to the results of the multivariate analysis. Carbamazepine and phenobarbital carried intermediate levels of risk, depending on the dose.
The results came from an observational cohort study of 3,909 pregnancies representing 3,521 women in 42 countries between 1999 and 2010. All the women had epilepsy and were taking one of the four drugs at conception.
The investigators, led by Dr. Torbjörn Tomson of the Karolinska Institute, Stockholm, excluded pregnancies in women whose antiepilepsy prescription was changed during the first trimester, those who were exposed to antiepileptic polytherapy or to other potentially teratogenic medications, and women with comorbidities such as diabetes, toxoplasmosis, and HIV that are known to increase the risk of congenital malformations (Lancet Neurology 2011 June 6 [doi:10.1016/S1474-4422(11)70107-7]).
In their multivariate analysis, the investigators controlled for a host of potential confounders. These included maternal age, sex of child, parental history of major congenital malformations, geographical region, parity, type of epilepsy, generalized tonic-clonic seizures during the first trimester, parental education, and the use of folic acid.
The overall rate of birth defects among women taking one of the four drugs was 6%. The lowest doses of lamotrigine carried the lowest absolute risk of birth defects 17 of 836 pregnancies (2%). The highest doses of valproic acid carried the highest absolute risk; 24 of 99 pregnancies (24%) resulted in major congenital malformations.
The investigators compared all drugs and doses to lamotrigine at less than 300 mg/day. Lamotrigine at more than 300 mg/day carried 2.2 times the risk of birth defects.
The lowest dose of carbamazepine (less than 400 mg/day) was not statistically more risky than was low-dose lamotrigine. An intermediate dose of carbamazepine was associated with a 2.5-fold increase in risk, and carbamazepine at 1,000 mg/day or more was associated with a 4.6-fold increase in risk.
Phenobarbital at less than 150 mg/day was 2.5 times as risky as was low-dose lamotrigine, and phenobarbital at 150 mg/day or greater was 8.2 times as risky.
Valproic acid at less than 700 mg/day was 2.8 times as risky as was low-dose lamotrigine, intermediate doses of valproic acid were 5.8 times as risky, and doses of 1,500 mg/day or more were 16.1 times as risky.
Except for the lowest dose of carbamazepine, all increases in risk associated with the drugs were statistically significant when compared to low-dose lamotrigine.
The only nondrug covariates that proved to carry a significant increase in risk were folate supplementation and a parental history of major congenital malformations. Inappropriate folicate use increased the risk of birth defects by 40%, compared with appropriate use. A parental history of birth defects carried a 4.4-fold increase in risk compared to pregnancies without that characteristic.
"Our findings show that the risk of major congenital malformations increases dose-dependently with all assessed antiepileptic drugs," the investigators wrote. "The approach generally accepted by physicians so far has been to identify, before conception, the lowest effective dose of the drug that is most appropriate for the woman’s epilepsy. Our study gives the prescriber the possibility of assessing how teratogenic risks at that dose compare with the risks associated with alternative treatments at various doses. Our data suggest that many women can enter pregnancy at low doses and maintain seizure control, although in many such cases dose adjustment might be needed later in pregnancy."
The study was funded by Eisai, GlaxoSmithKline, Janssen-Cilag, Novartis, Pfizer, Sanofi-Aventis, UCB, Netherlands Epilepsy Foundation, Stockholm County Council, and ALF. All but one of the eight investigators reported relationships with numerous pharmaceutical companies. The authors stated that the sponsors had no role in study design, data collection, data analysis, data interpretation, or writing the report.
FROM THE LANCET NEUROLOGY
Major Finding: Of four common antiepileptic drugs, lamotrigine at a dose of less than 300 mg/day had the lowest teratogenic potential. Valproic acid at a dose of 1,500 mg/day was 16-fold more likely than was low-dose lamotrigine to cause birth defects.
Data Source: Observational cohort study of 3,909 pregnancies representing 3,521 women.
Disclosures: The study was funded by Eisai, GlaxoSmithKline, Janssen-Cilag, Novartis, Pfizer, Sanofi-Aventis, UCB, Netherlands Epilepsy Foundation, Stockholm County Council, and ALF. All but one of the eight investigators reported relationships with a variety of pharmaceutical companies. The authors stated that the sponsors had no role in study design, data collection, data analysis, data interpretation, or writing the report.
Prednisone Aids Disease Control in Early RA
The addition of low-dose prednisone to a methotrexate-based, tight-control strategy leads to better outcomes in early rheumatoid arthritis, according to study results reported by Marije F. Bakker, Ph.D.
Compared with patients who received methotrexate (MTX) with placebo, those receiving MTX with 10 mg/day prednisone had better control of their disease and less erosive damage to their joints, Dr. Bakker Said in an interview.”
“The existing strategies leave room for improvement, especially for the number of patients who reach remission,” said Dr. Bakker of University Medical Center Utrecht (the Netherlands) in explaining the study's rationale. “Besides, it is important to determine which strategy steps are useful in the tight-control treatment strategies. Also, it is important to decide at which moment early in the treatment of [rheumatoid arthritis] medication should be added to the strategy.”
The CAMERA-II (Computer-Assisted Management of Early Rheumatoid Arthritis–II) trial was designed specifically to test the hypothesis that the addition of prednisone to a tight-control strategy of early RA using disease-modifying antirheumatic drugs would result in better disease control.
In the randomized, double-blind, placebo-controlled trial, 117 patients received MTX plus prednisone and 119 received MTX with placebo. All patients had early RA, with an onset less than 1 year before enrollment. Patients were at least 18 years old and had no previous DMARD therapy.
Patients were excluded from the trial if they had major comorbidities such as malignancies or severe diabetes mellitus; abnormal liver or kidney function; leukopenia or thrombocytopenia; evidence of drug or alcohol abuse; treatment with cytotoxic or immunosuppressive drugs within 3 months of the study; or osteoporotic vertebral fractures.
The investigators tailored the MTX treatment to each patient with the goal of achieving remission. If patients did not achieve remission with the maximum tolerable oral MTX dose, investigators first switched the patient to subcutaneous MTX and then added adalimumab to the regimen.
After 2 years, patients in the MTX plus prednisone group had significantly less radiographically confirmed erosive joint damage, as measured by their Sharp/van der Heijde scores. Patients on the MTX with prednisone regimen had significantly lower scores on the DAS28 (Disease Activity Score using a 28-joint count) questionnaire, and lower disability scores on the HAQ (Health Assessment Questionnaire).
A significantly lower proportion of patients in the experimental group required biologic treatment, compared with those on placebo (14% vs. 36%). The time to sustained remission was 6 months in the experimental group and 11 months in the control group, a significant difference. In addition, patients in the experimental group appeared to be somewhat more likely to achieve sustained remission, although this result did not achieve statistical significance (72% vs. 61%; P = .09).
Rates of adverse events were similar (29% in the MTX-prednisone group and 35% in the MTX-placebo group).
The trial was supported by the University Medical Center Utrecht and by Abbott. Dr. Bakker stated that she had no relevant financial disclosures.
Time to sustained remission was 6 months in the experimental group and 11 months in the control group.
Source DR. BAKKER
The addition of low-dose prednisone to a methotrexate-based, tight-control strategy leads to better outcomes in early rheumatoid arthritis, according to study results reported by Marije F. Bakker, Ph.D.
Compared with patients who received methotrexate (MTX) with placebo, those receiving MTX with 10 mg/day prednisone had better control of their disease and less erosive damage to their joints, Dr. Bakker Said in an interview.”
“The existing strategies leave room for improvement, especially for the number of patients who reach remission,” said Dr. Bakker of University Medical Center Utrecht (the Netherlands) in explaining the study's rationale. “Besides, it is important to determine which strategy steps are useful in the tight-control treatment strategies. Also, it is important to decide at which moment early in the treatment of [rheumatoid arthritis] medication should be added to the strategy.”
The CAMERA-II (Computer-Assisted Management of Early Rheumatoid Arthritis–II) trial was designed specifically to test the hypothesis that the addition of prednisone to a tight-control strategy of early RA using disease-modifying antirheumatic drugs would result in better disease control.
In the randomized, double-blind, placebo-controlled trial, 117 patients received MTX plus prednisone and 119 received MTX with placebo. All patients had early RA, with an onset less than 1 year before enrollment. Patients were at least 18 years old and had no previous DMARD therapy.
Patients were excluded from the trial if they had major comorbidities such as malignancies or severe diabetes mellitus; abnormal liver or kidney function; leukopenia or thrombocytopenia; evidence of drug or alcohol abuse; treatment with cytotoxic or immunosuppressive drugs within 3 months of the study; or osteoporotic vertebral fractures.
The investigators tailored the MTX treatment to each patient with the goal of achieving remission. If patients did not achieve remission with the maximum tolerable oral MTX dose, investigators first switched the patient to subcutaneous MTX and then added adalimumab to the regimen.
After 2 years, patients in the MTX plus prednisone group had significantly less radiographically confirmed erosive joint damage, as measured by their Sharp/van der Heijde scores. Patients on the MTX with prednisone regimen had significantly lower scores on the DAS28 (Disease Activity Score using a 28-joint count) questionnaire, and lower disability scores on the HAQ (Health Assessment Questionnaire).
A significantly lower proportion of patients in the experimental group required biologic treatment, compared with those on placebo (14% vs. 36%). The time to sustained remission was 6 months in the experimental group and 11 months in the control group, a significant difference. In addition, patients in the experimental group appeared to be somewhat more likely to achieve sustained remission, although this result did not achieve statistical significance (72% vs. 61%; P = .09).
Rates of adverse events were similar (29% in the MTX-prednisone group and 35% in the MTX-placebo group).
The trial was supported by the University Medical Center Utrecht and by Abbott. Dr. Bakker stated that she had no relevant financial disclosures.
Time to sustained remission was 6 months in the experimental group and 11 months in the control group.
Source DR. BAKKER
The addition of low-dose prednisone to a methotrexate-based, tight-control strategy leads to better outcomes in early rheumatoid arthritis, according to study results reported by Marije F. Bakker, Ph.D.
Compared with patients who received methotrexate (MTX) with placebo, those receiving MTX with 10 mg/day prednisone had better control of their disease and less erosive damage to their joints, Dr. Bakker Said in an interview.”
“The existing strategies leave room for improvement, especially for the number of patients who reach remission,” said Dr. Bakker of University Medical Center Utrecht (the Netherlands) in explaining the study's rationale. “Besides, it is important to determine which strategy steps are useful in the tight-control treatment strategies. Also, it is important to decide at which moment early in the treatment of [rheumatoid arthritis] medication should be added to the strategy.”
The CAMERA-II (Computer-Assisted Management of Early Rheumatoid Arthritis–II) trial was designed specifically to test the hypothesis that the addition of prednisone to a tight-control strategy of early RA using disease-modifying antirheumatic drugs would result in better disease control.
In the randomized, double-blind, placebo-controlled trial, 117 patients received MTX plus prednisone and 119 received MTX with placebo. All patients had early RA, with an onset less than 1 year before enrollment. Patients were at least 18 years old and had no previous DMARD therapy.
Patients were excluded from the trial if they had major comorbidities such as malignancies or severe diabetes mellitus; abnormal liver or kidney function; leukopenia or thrombocytopenia; evidence of drug or alcohol abuse; treatment with cytotoxic or immunosuppressive drugs within 3 months of the study; or osteoporotic vertebral fractures.
The investigators tailored the MTX treatment to each patient with the goal of achieving remission. If patients did not achieve remission with the maximum tolerable oral MTX dose, investigators first switched the patient to subcutaneous MTX and then added adalimumab to the regimen.
After 2 years, patients in the MTX plus prednisone group had significantly less radiographically confirmed erosive joint damage, as measured by their Sharp/van der Heijde scores. Patients on the MTX with prednisone regimen had significantly lower scores on the DAS28 (Disease Activity Score using a 28-joint count) questionnaire, and lower disability scores on the HAQ (Health Assessment Questionnaire).
A significantly lower proportion of patients in the experimental group required biologic treatment, compared with those on placebo (14% vs. 36%). The time to sustained remission was 6 months in the experimental group and 11 months in the control group, a significant difference. In addition, patients in the experimental group appeared to be somewhat more likely to achieve sustained remission, although this result did not achieve statistical significance (72% vs. 61%; P = .09).
Rates of adverse events were similar (29% in the MTX-prednisone group and 35% in the MTX-placebo group).
The trial was supported by the University Medical Center Utrecht and by Abbott. Dr. Bakker stated that she had no relevant financial disclosures.
Time to sustained remission was 6 months in the experimental group and 11 months in the control group.
Source DR. BAKKER
Prednisone Added to MTX Improves Control in Early RA
The addition of low-dose prednisone to a methotrexate-based, tight-control strategy leads to better outcomes in early rheumatoid arthritis, according to results from the CAMERA-II trial reported by Marije F. Bakker, Ph.D.
Compared with patients who received methotrexate (MTX) with placebo, those receiving MTX with 10-mg/day prednisone had better control of their disease and less erosive damage to their joints, Dr. Bakker said in an interview.
"The existing strategies leave room for improvement, especially for the number of patients who reach remission," said Dr. Bakker of University Medical Center Utrecht (the Netherlands) in explaining the study’s rationale. "Besides, it is important to determine which strategy steps are useful in the tight-control treatment strategies. Also, it is important to decide at which moment early in the treatment of [rheumatoid arthritis] medication should be added to the strategy."
The CAMERA-II (Computer-Assisted Management of Early Rheumatoid Arthritis–II) trialwas designed specifically to test the hypothesis that the addition of prednisone to a tight-control strategy of early RA using disease-modifying antirheumatic drugs would result in better disease control.
In the randomized, double-blind, placebo-controlled trial, 117 patients received MTX plus prednisone and 119 received MTX with placebo. All patients had early RA, with an onset less than 1 year before enrollment. Patients were at least 18 years old and had no previous DMARD therapy.
Patients were excluded from the trial if they had major comorbidities such as malignancies or severe diabetes mellitus; abnormal liver or kidney function; leukopenia or thrombocytopenia; evidence of drug or alcohol abuse; treatment with cytotoxic or immunosuppressive drugs within 3 months of the study; or osteoporotic vertebral fractures.
Investigators tailored the MTX treatment to each patient with the goal of achieving remission. If patients did not achieve remission with the maximum tolerable oral MTX dose, investigators first switched the patient to subcutaneous MTX and then added adalimumab to the regimen.
After 2 years, patients in the MTX plus prednisone group had significantly less radiographically confirmed erosive joint damage, as measured by their Sharp/van der Heijde scores. Patients on the MTX with prednisone regimen had significantly lower scores on the DAS28 (Disease Activity Score using a 28-joint count) questionnaire, and lower disability scores on the HAQ (Health Assessment Questionnaire).
A significantly lower proportion of patients in the experimental group required biologic treatment, compared with those on placebo (14% vs. 36%). The time to sustained remission was 6 months in the experimental group and 11 months in the control group, a significant difference. In addition, patients in the experimental group appeared to be somewhat more likely to achieve sustained remission, although this result did not achieve statistical significance (72% vs. 61%; P = .09).
Rates of adverse events were similar (29% in the MTX-prednisone group and 35% in the MTX-placebo group).
The trial was supported by the University Medical Center Utrecht and by Abbott. Dr. Bakker stated that she had no relevant financial disclosures.
The addition of low-dose prednisone to a methotrexate-based, tight-control strategy leads to better outcomes in early rheumatoid arthritis, according to results from the CAMERA-II trial reported by Marije F. Bakker, Ph.D.
Compared with patients who received methotrexate (MTX) with placebo, those receiving MTX with 10-mg/day prednisone had better control of their disease and less erosive damage to their joints, Dr. Bakker said in an interview.
"The existing strategies leave room for improvement, especially for the number of patients who reach remission," said Dr. Bakker of University Medical Center Utrecht (the Netherlands) in explaining the study’s rationale. "Besides, it is important to determine which strategy steps are useful in the tight-control treatment strategies. Also, it is important to decide at which moment early in the treatment of [rheumatoid arthritis] medication should be added to the strategy."
The CAMERA-II (Computer-Assisted Management of Early Rheumatoid Arthritis–II) trialwas designed specifically to test the hypothesis that the addition of prednisone to a tight-control strategy of early RA using disease-modifying antirheumatic drugs would result in better disease control.
In the randomized, double-blind, placebo-controlled trial, 117 patients received MTX plus prednisone and 119 received MTX with placebo. All patients had early RA, with an onset less than 1 year before enrollment. Patients were at least 18 years old and had no previous DMARD therapy.
Patients were excluded from the trial if they had major comorbidities such as malignancies or severe diabetes mellitus; abnormal liver or kidney function; leukopenia or thrombocytopenia; evidence of drug or alcohol abuse; treatment with cytotoxic or immunosuppressive drugs within 3 months of the study; or osteoporotic vertebral fractures.
Investigators tailored the MTX treatment to each patient with the goal of achieving remission. If patients did not achieve remission with the maximum tolerable oral MTX dose, investigators first switched the patient to subcutaneous MTX and then added adalimumab to the regimen.
After 2 years, patients in the MTX plus prednisone group had significantly less radiographically confirmed erosive joint damage, as measured by their Sharp/van der Heijde scores. Patients on the MTX with prednisone regimen had significantly lower scores on the DAS28 (Disease Activity Score using a 28-joint count) questionnaire, and lower disability scores on the HAQ (Health Assessment Questionnaire).
A significantly lower proportion of patients in the experimental group required biologic treatment, compared with those on placebo (14% vs. 36%). The time to sustained remission was 6 months in the experimental group and 11 months in the control group, a significant difference. In addition, patients in the experimental group appeared to be somewhat more likely to achieve sustained remission, although this result did not achieve statistical significance (72% vs. 61%; P = .09).
Rates of adverse events were similar (29% in the MTX-prednisone group and 35% in the MTX-placebo group).
The trial was supported by the University Medical Center Utrecht and by Abbott. Dr. Bakker stated that she had no relevant financial disclosures.
The addition of low-dose prednisone to a methotrexate-based, tight-control strategy leads to better outcomes in early rheumatoid arthritis, according to results from the CAMERA-II trial reported by Marije F. Bakker, Ph.D.
Compared with patients who received methotrexate (MTX) with placebo, those receiving MTX with 10-mg/day prednisone had better control of their disease and less erosive damage to their joints, Dr. Bakker said in an interview.
"The existing strategies leave room for improvement, especially for the number of patients who reach remission," said Dr. Bakker of University Medical Center Utrecht (the Netherlands) in explaining the study’s rationale. "Besides, it is important to determine which strategy steps are useful in the tight-control treatment strategies. Also, it is important to decide at which moment early in the treatment of [rheumatoid arthritis] medication should be added to the strategy."
The CAMERA-II (Computer-Assisted Management of Early Rheumatoid Arthritis–II) trialwas designed specifically to test the hypothesis that the addition of prednisone to a tight-control strategy of early RA using disease-modifying antirheumatic drugs would result in better disease control.
In the randomized, double-blind, placebo-controlled trial, 117 patients received MTX plus prednisone and 119 received MTX with placebo. All patients had early RA, with an onset less than 1 year before enrollment. Patients were at least 18 years old and had no previous DMARD therapy.
Patients were excluded from the trial if they had major comorbidities such as malignancies or severe diabetes mellitus; abnormal liver or kidney function; leukopenia or thrombocytopenia; evidence of drug or alcohol abuse; treatment with cytotoxic or immunosuppressive drugs within 3 months of the study; or osteoporotic vertebral fractures.
Investigators tailored the MTX treatment to each patient with the goal of achieving remission. If patients did not achieve remission with the maximum tolerable oral MTX dose, investigators first switched the patient to subcutaneous MTX and then added adalimumab to the regimen.
After 2 years, patients in the MTX plus prednisone group had significantly less radiographically confirmed erosive joint damage, as measured by their Sharp/van der Heijde scores. Patients on the MTX with prednisone regimen had significantly lower scores on the DAS28 (Disease Activity Score using a 28-joint count) questionnaire, and lower disability scores on the HAQ (Health Assessment Questionnaire).
A significantly lower proportion of patients in the experimental group required biologic treatment, compared with those on placebo (14% vs. 36%). The time to sustained remission was 6 months in the experimental group and 11 months in the control group, a significant difference. In addition, patients in the experimental group appeared to be somewhat more likely to achieve sustained remission, although this result did not achieve statistical significance (72% vs. 61%; P = .09).
Rates of adverse events were similar (29% in the MTX-prednisone group and 35% in the MTX-placebo group).
The trial was supported by the University Medical Center Utrecht and by Abbott. Dr. Bakker stated that she had no relevant financial disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: After 2 years, patients in the MTX plus prednisone group had
significantly less radiographically confirmed erosive joint damage, as
measured by their Sharp/van der Heijde scores. Patients on the MTX with
prednisone regimen had significantly lower scores on the DAS28 questionnaire, and lower
disability scores on the HAQ.
Data Source: A randomized, double-blind, placebo-controlled trial in which 117 patients
received MTX plus prednisone, and 119 received MTX with placebo..
Disclosures: The trial was supported by the University Medical Center Utrecht and by
Abbott. Dr. Bakker stated that she had no relevant financial
disclosures.
Prednisone Added to MTX Improves Control in Early RA
The addition of low-dose prednisone to a methotrexate-based, tight-control strategy leads to better outcomes in early rheumatoid arthritis, according to results from the CAMERA-II trial reported by Marije F. Bakker, Ph.D.
Compared with patients who received methotrexate (MTX) with placebo, those receiving MTX with 10-mg/day prednisone had better control of their disease and less erosive damage to their joints, Dr. Bakker said in an interview.
"The existing strategies leave room for improvement, especially for the number of patients who reach remission," said Dr. Bakker of University Medical Center Utrecht (the Netherlands) in explaining the study’s rationale. "Besides, it is important to determine which strategy steps are useful in the tight-control treatment strategies. Also, it is important to decide at which moment early in the treatment of [rheumatoid arthritis] medication should be added to the strategy."
The CAMERA-II (Computer-Assisted Management of Early Rheumatoid Arthritis–II) trialwas designed specifically to test the hypothesis that the addition of prednisone to a tight-control strategy of early RA using disease-modifying antirheumatic drugs would result in better disease control.
In the randomized, double-blind, placebo-controlled trial, 117 patients received MTX plus prednisone and 119 received MTX with placebo. All patients had early RA, with an onset less than 1 year before enrollment. Patients were at least 18 years old and had no previous DMARD therapy.
Patients were excluded from the trial if they had major comorbidities such as malignancies or severe diabetes mellitus; abnormal liver or kidney function; leukopenia or thrombocytopenia; evidence of drug or alcohol abuse; treatment with cytotoxic or immunosuppressive drugs within 3 months of the study; or osteoporotic vertebral fractures.
Investigators tailored the MTX treatment to each patient with the goal of achieving remission. If patients did not achieve remission with the maximum tolerable oral MTX dose, investigators first switched the patient to subcutaneous MTX and then added adalimumab to the regimen.
After 2 years, patients in the MTX plus prednisone group had significantly less radiographically confirmed erosive joint damage, as measured by their Sharp/van der Heijde scores. Patients on the MTX with prednisone regimen had significantly lower scores on the DAS28 (Disease Activity Score using a 28-joint count) questionnaire, and lower disability scores on the HAQ (Health Assessment Questionnaire).
A significantly lower proportion of patients in the experimental group required biologic treatment, compared with those on placebo (14% vs. 36%). The time to sustained remission was 6 months in the experimental group and 11 months in the control group, a significant difference. In addition, patients in the experimental group appeared to be somewhat more likely to achieve sustained remission, although this result did not achieve statistical significance (72% vs. 61%; P = .09).
Rates of adverse events were similar (29% in the MTX-prednisone group and 35% in the MTX-placebo group).
The trial was supported by the University Medical Center Utrecht and by Abbott. Dr. Bakker stated that she had no relevant financial disclosures.
The addition of low-dose prednisone to a methotrexate-based, tight-control strategy leads to better outcomes in early rheumatoid arthritis, according to results from the CAMERA-II trial reported by Marije F. Bakker, Ph.D.
Compared with patients who received methotrexate (MTX) with placebo, those receiving MTX with 10-mg/day prednisone had better control of their disease and less erosive damage to their joints, Dr. Bakker said in an interview.
"The existing strategies leave room for improvement, especially for the number of patients who reach remission," said Dr. Bakker of University Medical Center Utrecht (the Netherlands) in explaining the study’s rationale. "Besides, it is important to determine which strategy steps are useful in the tight-control treatment strategies. Also, it is important to decide at which moment early in the treatment of [rheumatoid arthritis] medication should be added to the strategy."
The CAMERA-II (Computer-Assisted Management of Early Rheumatoid Arthritis–II) trialwas designed specifically to test the hypothesis that the addition of prednisone to a tight-control strategy of early RA using disease-modifying antirheumatic drugs would result in better disease control.
In the randomized, double-blind, placebo-controlled trial, 117 patients received MTX plus prednisone and 119 received MTX with placebo. All patients had early RA, with an onset less than 1 year before enrollment. Patients were at least 18 years old and had no previous DMARD therapy.
Patients were excluded from the trial if they had major comorbidities such as malignancies or severe diabetes mellitus; abnormal liver or kidney function; leukopenia or thrombocytopenia; evidence of drug or alcohol abuse; treatment with cytotoxic or immunosuppressive drugs within 3 months of the study; or osteoporotic vertebral fractures.
Investigators tailored the MTX treatment to each patient with the goal of achieving remission. If patients did not achieve remission with the maximum tolerable oral MTX dose, investigators first switched the patient to subcutaneous MTX and then added adalimumab to the regimen.
After 2 years, patients in the MTX plus prednisone group had significantly less radiographically confirmed erosive joint damage, as measured by their Sharp/van der Heijde scores. Patients on the MTX with prednisone regimen had significantly lower scores on the DAS28 (Disease Activity Score using a 28-joint count) questionnaire, and lower disability scores on the HAQ (Health Assessment Questionnaire).
A significantly lower proportion of patients in the experimental group required biologic treatment, compared with those on placebo (14% vs. 36%). The time to sustained remission was 6 months in the experimental group and 11 months in the control group, a significant difference. In addition, patients in the experimental group appeared to be somewhat more likely to achieve sustained remission, although this result did not achieve statistical significance (72% vs. 61%; P = .09).
Rates of adverse events were similar (29% in the MTX-prednisone group and 35% in the MTX-placebo group).
The trial was supported by the University Medical Center Utrecht and by Abbott. Dr. Bakker stated that she had no relevant financial disclosures.
The addition of low-dose prednisone to a methotrexate-based, tight-control strategy leads to better outcomes in early rheumatoid arthritis, according to results from the CAMERA-II trial reported by Marije F. Bakker, Ph.D.
Compared with patients who received methotrexate (MTX) with placebo, those receiving MTX with 10-mg/day prednisone had better control of their disease and less erosive damage to their joints, Dr. Bakker said in an interview.
"The existing strategies leave room for improvement, especially for the number of patients who reach remission," said Dr. Bakker of University Medical Center Utrecht (the Netherlands) in explaining the study’s rationale. "Besides, it is important to determine which strategy steps are useful in the tight-control treatment strategies. Also, it is important to decide at which moment early in the treatment of [rheumatoid arthritis] medication should be added to the strategy."
The CAMERA-II (Computer-Assisted Management of Early Rheumatoid Arthritis–II) trialwas designed specifically to test the hypothesis that the addition of prednisone to a tight-control strategy of early RA using disease-modifying antirheumatic drugs would result in better disease control.
In the randomized, double-blind, placebo-controlled trial, 117 patients received MTX plus prednisone and 119 received MTX with placebo. All patients had early RA, with an onset less than 1 year before enrollment. Patients were at least 18 years old and had no previous DMARD therapy.
Patients were excluded from the trial if they had major comorbidities such as malignancies or severe diabetes mellitus; abnormal liver or kidney function; leukopenia or thrombocytopenia; evidence of drug or alcohol abuse; treatment with cytotoxic or immunosuppressive drugs within 3 months of the study; or osteoporotic vertebral fractures.
Investigators tailored the MTX treatment to each patient with the goal of achieving remission. If patients did not achieve remission with the maximum tolerable oral MTX dose, investigators first switched the patient to subcutaneous MTX and then added adalimumab to the regimen.
After 2 years, patients in the MTX plus prednisone group had significantly less radiographically confirmed erosive joint damage, as measured by their Sharp/van der Heijde scores. Patients on the MTX with prednisone regimen had significantly lower scores on the DAS28 (Disease Activity Score using a 28-joint count) questionnaire, and lower disability scores on the HAQ (Health Assessment Questionnaire).
A significantly lower proportion of patients in the experimental group required biologic treatment, compared with those on placebo (14% vs. 36%). The time to sustained remission was 6 months in the experimental group and 11 months in the control group, a significant difference. In addition, patients in the experimental group appeared to be somewhat more likely to achieve sustained remission, although this result did not achieve statistical significance (72% vs. 61%; P = .09).
Rates of adverse events were similar (29% in the MTX-prednisone group and 35% in the MTX-placebo group).
The trial was supported by the University Medical Center Utrecht and by Abbott. Dr. Bakker stated that she had no relevant financial disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: After 2 years, patients in the MTX plus prednisone group had
significantly less radiographically confirmed erosive joint damage, as
measured by their Sharp/van der Heijde scores. Patients on the MTX with
prednisone regimen had significantly lower scores on the DAS28 questionnaire, and lower
disability scores on the HAQ.
Data Source: A randomized, double-blind, placebo-controlled trial in which 117 patients
received MTX plus prednisone, and 119 received MTX with placebo..
Disclosures: The trial was supported by the University Medical Center Utrecht and by
Abbott. Dr. Bakker stated that she had no relevant financial
disclosures.
FDA Clears Imaging App for iPhone/iPad
The Food and Drug Administration gave its first clearance to an application that will allow physicians to review radiology images on Apple's iPad and iPhone in the absence of a standard workstation.
The FDA cleared the Mobile MIM app for viewing images and making diagnoses using computed tomography, magnetic resonance imaging, and positron emission tomography. The agency cautioned that it is not intended to replace standard workstations, and should only be used when one is not available.
The app can measure distance on the image as well as image intensity; it can also display measurement lines, regions of interest, and annotations.
The FDA noted that the luminance displayed by a mobile device can vary greatly, even among identical models. The image's luminance also can vary based on ambient lighting. The app includes an interactive contrast test that will allow a user to determine if he or she can properly distinguish subtle differences in contrast.
The Mobile MIM app was created by Cleveland-based MIM Software Inc. The company said on its Web site Mobile MIM is now available in Apple's App Store.
The Food and Drug Administration gave its first clearance to an application that will allow physicians to review radiology images on Apple's iPad and iPhone in the absence of a standard workstation.
The FDA cleared the Mobile MIM app for viewing images and making diagnoses using computed tomography, magnetic resonance imaging, and positron emission tomography. The agency cautioned that it is not intended to replace standard workstations, and should only be used when one is not available.
The app can measure distance on the image as well as image intensity; it can also display measurement lines, regions of interest, and annotations.
The FDA noted that the luminance displayed by a mobile device can vary greatly, even among identical models. The image's luminance also can vary based on ambient lighting. The app includes an interactive contrast test that will allow a user to determine if he or she can properly distinguish subtle differences in contrast.
The Mobile MIM app was created by Cleveland-based MIM Software Inc. The company said on its Web site Mobile MIM is now available in Apple's App Store.
The Food and Drug Administration gave its first clearance to an application that will allow physicians to review radiology images on Apple's iPad and iPhone in the absence of a standard workstation.
The FDA cleared the Mobile MIM app for viewing images and making diagnoses using computed tomography, magnetic resonance imaging, and positron emission tomography. The agency cautioned that it is not intended to replace standard workstations, and should only be used when one is not available.
The app can measure distance on the image as well as image intensity; it can also display measurement lines, regions of interest, and annotations.
The FDA noted that the luminance displayed by a mobile device can vary greatly, even among identical models. The image's luminance also can vary based on ambient lighting. The app includes an interactive contrast test that will allow a user to determine if he or she can properly distinguish subtle differences in contrast.
The Mobile MIM app was created by Cleveland-based MIM Software Inc. The company said on its Web site Mobile MIM is now available in Apple's App Store.
FDA Clears Imaging App for iPhone/iPad
The Food and Drug Administration gave its first clearance to an application that will allow physicians to review radiology images on Apple's iPad and iPhone in the absence of a standard workstation.
The FDA cleared the Mobile MIM app for viewing images and making diagnoses using computed tomography, magnetic resonance imaging, and positron emission tomography. The agency cautioned that it is not intended to replace standard workstations, and should only be used when one is not available.
The app can measure distance on the image as well as image intensity; it can also display measurement lines, regions of interest, and annotations.
The FDA noted that the luminance displayed by a mobile device can vary greatly, even among identical models. The image's luminance also can vary based on ambient lighting. The app includes an interactive contrast test that will allow a user to determine if he or she can properly distinguish subtle differences in contrast.
The Mobile MIM app was created by Cleveland-based MIM Software Inc. The company said on its Web site Mobile MIM is now available in Apple's App Store.
The Food and Drug Administration gave its first clearance to an application that will allow physicians to review radiology images on Apple's iPad and iPhone in the absence of a standard workstation.
The FDA cleared the Mobile MIM app for viewing images and making diagnoses using computed tomography, magnetic resonance imaging, and positron emission tomography. The agency cautioned that it is not intended to replace standard workstations, and should only be used when one is not available.
The app can measure distance on the image as well as image intensity; it can also display measurement lines, regions of interest, and annotations.
The FDA noted that the luminance displayed by a mobile device can vary greatly, even among identical models. The image's luminance also can vary based on ambient lighting. The app includes an interactive contrast test that will allow a user to determine if he or she can properly distinguish subtle differences in contrast.
The Mobile MIM app was created by Cleveland-based MIM Software Inc. The company said on its Web site Mobile MIM is now available in Apple's App Store.
The Food and Drug Administration gave its first clearance to an application that will allow physicians to review radiology images on Apple's iPad and iPhone in the absence of a standard workstation.
The FDA cleared the Mobile MIM app for viewing images and making diagnoses using computed tomography, magnetic resonance imaging, and positron emission tomography. The agency cautioned that it is not intended to replace standard workstations, and should only be used when one is not available.
The app can measure distance on the image as well as image intensity; it can also display measurement lines, regions of interest, and annotations.
The FDA noted that the luminance displayed by a mobile device can vary greatly, even among identical models. The image's luminance also can vary based on ambient lighting. The app includes an interactive contrast test that will allow a user to determine if he or she can properly distinguish subtle differences in contrast.
The Mobile MIM app was created by Cleveland-based MIM Software Inc. The company said on its Web site Mobile MIM is now available in Apple's App Store.