User login
Time Management and the Hospitalist
Hospital medicine groups are becoming an integral part of healthcare delivery in the US. Since the term hospitalist was coined in 1996 by Robert Wachter, the U.S. has witnessed an amazing growth and development of inpatient programs. Physicians going into inpatient medicine experience impressive fluctuations in patient volume when new programs begin and when existing programs expand their primary referral base or comanage patients with subspecialists and surgeons.
Ideal patient volume numbers vary from group to group but range, on average, from 15 to 18 patients per hospitalist. Layered on the management of patients in the hospital is a myriad of duties the hospitalist must perform to effectively care for patients. Depending on program layout, hospitalists will also be involved in committee work, end-of-life discussions, protocol development, and measurement of data that links improvement of care when hospitalists are involved in caring for patients.
A good reason to talk about inpatient time management is that without it physicians can become overstressed. Physician burnout, job dissatisfaction, and high turnover with hospital medicine groups are major concerns, due in part to the increased demands placed on hospitalists. Small programs, especially, can experience great fluctuations in volume as they define their patient referral base, and deficient physician time management skills can be the main reason a program does not gain momentum.
Early in my training, I wondered if there was a better way to see patients and not feel stressed when new patients were admitted to my service. But it wasn’t until I started work with a healthcare organization in Wisconsin that I noticed there was a way to gain control of my busy day. I was introduced to time management principles by physicians who exercised this important skill everyday. These physicians did not seem stressed when the day seemed to be getting “out of control.” Their time management skills allowed them to stay efficient. After a few busy days, it didn’t take long for me to seek out information on time management and begin my own journey of self-assessment. At its core, that’s what time management is: an honest assessment of yourself. After learning about time management, I created a plan to assist me in getting through my day. Now, time management is automatic, an integral part of my ability to function on a busy inpatient floor. Time management is important for anyone who wants to achieve more control of his or her day, improve on work efficiency, set personal and professional goals, and, in my opinion, extend himself or herself in ways that don’t seem possible.
Some important terms to review include “goal,” “objective,” and “priority.” Goals are long-range and provide overall direction for an individual or a group. A good goal for a hospital medicine group is to be the premiere group in their state or their region. A good goal for a hospitalist is to implement an inpatient time management strategy. An objective is a clear-cut description of how to achieve a goal, and priorities are the ranked items in a goal or objective list. Priorities must be assigned to time management objectives. An exact order will ensure nothing is missed when working on a given objective.
The best way to tackle inpatient time management is to see how the day is laid out by keeping a time log and by performing an internal review of how a typical day marches out. When I performed my internal review I realized I looked at my day chopped into sections that were spent rounding, teaching, and discharging. I never discharged a patient in the morning. I saved all my discharges until the afternoon. I knew discharges required more time, and I felt better seeing patients first and then going back and doing discharges. I wasn’t being efficient with this method, because I always felt tired in the afternoon.
There were different categories of patients: new admits from the previous night, discharges, routine patients, and critical patients. Critical patients received my highest priority, and discharges received the least priority. I was looking at critical patients differently than my discharges. Processing the ICU patients meant more thinking, diagnosing, and reviewing, whereas discharging meant dictating, writing prescriptions, educating patients, and making PCP call-backs. I wasn’t looking at each process in terms of time; rather, I was looking at discharges as a final step and the ICU as a place where all my energy had to be placed. I wasn’t making the connection with time and how I was comparing patients being discharged with patients in the ICU.
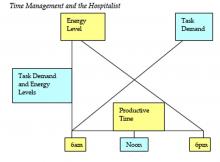
Energy level and task demands, in relationship to productive time, can be graphed (Figure 1). Energy level is highest in the morning, and tasks march out throughout the day. At the intersection, the time is usually noon for hospitalists. Energy level begins to dip after this time. The most productive time is in the early morning with a plateau around noon. This is why I felt tired in the afternoon, having important discharges to finish.
Once I made the connection that discharges take time and ICU patients take time, I knew I had to revamp how I saw patients. The most time-consuming patients need to be seen first when my energy level is high.
My new routine was to see the ICU patients first, new admissions second, and discharges third, all before noon. This new plan allowed me to begin seeing routine patients earlier. For my routine patients, I review the chart, look at lab and imaging tests ordered, and then go into the room and examine the patient. The difference with these patients is that I wait to write my final impression and discussion section until after I’ve seen all the routine patients. Then I go back and write my final notes. The rest of the day is concentrated on finishing notes, PCP call-backs, billing, family conferences, new admissions, and emergencies.
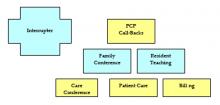
A good way to look at inpatient work is in sets of blocks. (Figure 2) Within each block are the duties of the hospitalist. Blocks are prioritized in order of importance. Within the prioritized blocks are the “absolute” duties that a hospitalist must perform each day. They include patient care (new and existing), billing capture, and multidisciplinary care conferences. After the absolutes come duties that are routinely performed, including patient and nonpatient functions such as PCP call-backs, family conferencing, resident teaching, and time interrupters. Inpatient blocks can be stacked, with the first layer containing the absolutes and the subsequent layers containing the regular duties or tasks.
Interrupters are time delays that take a busy hospitalist away from absolute and regular work tasks. They are polygonal and can be placed anywhere along the blocks. Interrupters may be new patients, an established patient with an emergency, an outside physician trying to contact the service, a spouse, the medical records department, a funeral home inquiring about a death certificate, a home health agency trying to get certification for a patient’s wheelchair or a subspecialist, for example.
An ideal day shows the blocks in perfect formation, pyramid style. A day with interruptions will result in the blocks appearing disorganized. The ability to recognize time interrupters and to have a plan to deal with them is the key to managing a busy inpatient service. Any plan developed must use patient care as the focus. Everything the hospitalist does is centered on this block, and priorities can be developed to keep it focused.
Interruptions are a part of any busy inpatient service. Interrupters need to be prioritized, and a system needs to be in place for handling them with any good time management plan. Code Blue response, emergency patient need, and new patients on the floor rank high in priority for interrupters. Phone interruptions and nursing questions are ranked based on urgency and patient impact. One of the best ways to avoid too many phone interruptions is to have a coordinator or secretary assist with filtering incoming calls. This person will have specific instructions on how calls are to be handled. Emergency calls and incoming calls from physicians are given priority. A call from a drug representative or friend can be postponed.
A good rule to have when seeing new patients on the floor is to visualize each new patient coming onto the service. ER physicians visualize each patient coming into the ED arena. By direct visualization of incoming patients, ER physicians determine what their level of involvement will be. A patient who appears ill will get a quicker evaluation than a patient who appears stable. Principles that underlie patient triage include meeting the patient and identifying oneself as the responsible physician, visualization of the patient even while interviewing others, and communication and delegation of work.
Talking to an ED physician about a patient or to a PCP at an outreach facility is helpful, but the direct visualization of the patient by the hospitalist when he or she arrives on the ward is key to managing floor time. This method allows for patients to be prioritized based on acuity. Direct visualization can also be performed before resident contact is initiated. A quick look at the patient and his or her vitals provides reassurance that nothing immediate needs to be performed. A brief hospitalist introduction gives comfort to the patient and family. Patients are impressed when you meet them in their room when they arrive.
Critical patients require more attention, and care can be started with a primary survey. Trauma services have modes of triage care and initial evaluations of trauma patients that can be modified by hospitalists.
The objectives of initial trauma care include 1) stabilization, 2) identification of life-threatening injuries and initiation of adequate supportive therapy, and 3) efficient and rapid organization of either definitive therapy or transfer to a facility that provides definite therapy. Within this set of objectives is a triage objective to prioritize patients with a high likelihood of early deterioration.
Direct hospitalist visualization of every patient coming onto the service accomplishes the objectives of initial care and triage. Of course, the hospitalist isn’t prioritizing a gunshot wound patient, but the principles are the same: visualizing the patient, determining a level of involvement, and initiating a primary survey for critical patients. This approach to patients can be adopted in the hospitalist patient-care repertoire.
As an example, I was asked to consult on a patient with a subarachnoid bleed to manage hypertension. The patient was already admitted into the ICU by the neurosurgeon. Subarachnoid bleed and hypertension are 2 urgent needs, and this was a new patient on my service. I went to visualize the patient. I finished my brief survey and was writing down some orders when the nurse came over to me and told me the patient was not responding to her the way he had earlier. The patient’s admitting blood pressure was 180/100 and when the nurse reported the change to me, the blood pressure was 230/106. The patient was obtunded and unable to protect his airway. In addition to intubating the patient and hyperventilating him, I contacted the neurosurgeon to notify him of the change in status, started intravenous mannitol, established large bore venous access, and started nitroprusside. The surgeon returned to the ICU and took the patient for corrective surgery.
When the nurse alerted me to the change in status with the patient, I performed actions based on my survey, stabilized the patient, identified a threat, provided supportive care, and contacted the person who would be able to provide definitive treatment. I was able to do this because of the discipline provided to me with time management and by prioritizing an interrupter.
Developing a system to flexibly see new patients and provide quick surveys should be a focus for any hospitalist. By doing this, the hospitalist is providing the plan for how the day will flow, regardless of interruptions. The plan, the objectives, and the priorities are there to ensure a day happens the way the physician wants it to happen.
Time management courses and books usually recommend that people complete a daily log of how and what they do in the course of their day. (Figure 3) The daily log is an honest portrayal of the day as it unfolds and how one responds to events as they happen. Logs include phone calls to friends, stockbrokers, and spouses. Each hospitalist’s log notes when a patient or family conference occurred, when interruptions occurred, and how they were handled. Taking coffee breaks, reading a paper, and talking to a partner are all fair game in the log. Everything needs to be put in the log. Keeping a log for 1 or 2 days is a great exercise with endless ways of showing people where their time and energy is going. I encourage physicians who ask me what some of my secrets are to getting done early to read a book on time management or attend a course.
When I took my first time management course in 1998, I became an instant student of my time and an observer of how others mange their time. I didn’t realize how incredible a force time management was, because I thought it was mainly for business people. A course may range from the implementation of a few basic strategies to a complete revamp of how the day is structured, but any hospitalist can benefit from time management techniques.
Dr. Houser can be contacted at houserr@siouxvalley.org.
Reading List
- Mackenzie A. The Time Trap: The Classic Book on Time Management. New York, NY: AMACOM; 1997.
- Lane, B and Rierdan, R. Managing People-A Practical Guide. Oasis Press. 2001.
- Wachter R. The emerging role of “hospitalists” in the American health care system, N Engl J Me. 1996;335:514-7.
- Dries DJ. Initial evaluation of the trauma patient. www.eMedicine.com, 2004.
Hospital medicine groups are becoming an integral part of healthcare delivery in the US. Since the term hospitalist was coined in 1996 by Robert Wachter, the U.S. has witnessed an amazing growth and development of inpatient programs. Physicians going into inpatient medicine experience impressive fluctuations in patient volume when new programs begin and when existing programs expand their primary referral base or comanage patients with subspecialists and surgeons.
Ideal patient volume numbers vary from group to group but range, on average, from 15 to 18 patients per hospitalist. Layered on the management of patients in the hospital is a myriad of duties the hospitalist must perform to effectively care for patients. Depending on program layout, hospitalists will also be involved in committee work, end-of-life discussions, protocol development, and measurement of data that links improvement of care when hospitalists are involved in caring for patients.
A good reason to talk about inpatient time management is that without it physicians can become overstressed. Physician burnout, job dissatisfaction, and high turnover with hospital medicine groups are major concerns, due in part to the increased demands placed on hospitalists. Small programs, especially, can experience great fluctuations in volume as they define their patient referral base, and deficient physician time management skills can be the main reason a program does not gain momentum.
Early in my training, I wondered if there was a better way to see patients and not feel stressed when new patients were admitted to my service. But it wasn’t until I started work with a healthcare organization in Wisconsin that I noticed there was a way to gain control of my busy day. I was introduced to time management principles by physicians who exercised this important skill everyday. These physicians did not seem stressed when the day seemed to be getting “out of control.” Their time management skills allowed them to stay efficient. After a few busy days, it didn’t take long for me to seek out information on time management and begin my own journey of self-assessment. At its core, that’s what time management is: an honest assessment of yourself. After learning about time management, I created a plan to assist me in getting through my day. Now, time management is automatic, an integral part of my ability to function on a busy inpatient floor. Time management is important for anyone who wants to achieve more control of his or her day, improve on work efficiency, set personal and professional goals, and, in my opinion, extend himself or herself in ways that don’t seem possible.
Some important terms to review include “goal,” “objective,” and “priority.” Goals are long-range and provide overall direction for an individual or a group. A good goal for a hospital medicine group is to be the premiere group in their state or their region. A good goal for a hospitalist is to implement an inpatient time management strategy. An objective is a clear-cut description of how to achieve a goal, and priorities are the ranked items in a goal or objective list. Priorities must be assigned to time management objectives. An exact order will ensure nothing is missed when working on a given objective.
The best way to tackle inpatient time management is to see how the day is laid out by keeping a time log and by performing an internal review of how a typical day marches out. When I performed my internal review I realized I looked at my day chopped into sections that were spent rounding, teaching, and discharging. I never discharged a patient in the morning. I saved all my discharges until the afternoon. I knew discharges required more time, and I felt better seeing patients first and then going back and doing discharges. I wasn’t being efficient with this method, because I always felt tired in the afternoon.
There were different categories of patients: new admits from the previous night, discharges, routine patients, and critical patients. Critical patients received my highest priority, and discharges received the least priority. I was looking at critical patients differently than my discharges. Processing the ICU patients meant more thinking, diagnosing, and reviewing, whereas discharging meant dictating, writing prescriptions, educating patients, and making PCP call-backs. I wasn’t looking at each process in terms of time; rather, I was looking at discharges as a final step and the ICU as a place where all my energy had to be placed. I wasn’t making the connection with time and how I was comparing patients being discharged with patients in the ICU.
Energy level and task demands, in relationship to productive time, can be graphed (Figure 1). Energy level is highest in the morning, and tasks march out throughout the day. At the intersection, the time is usually noon for hospitalists. Energy level begins to dip after this time. The most productive time is in the early morning with a plateau around noon. This is why I felt tired in the afternoon, having important discharges to finish.
Once I made the connection that discharges take time and ICU patients take time, I knew I had to revamp how I saw patients. The most time-consuming patients need to be seen first when my energy level is high.
My new routine was to see the ICU patients first, new admissions second, and discharges third, all before noon. This new plan allowed me to begin seeing routine patients earlier. For my routine patients, I review the chart, look at lab and imaging tests ordered, and then go into the room and examine the patient. The difference with these patients is that I wait to write my final impression and discussion section until after I’ve seen all the routine patients. Then I go back and write my final notes. The rest of the day is concentrated on finishing notes, PCP call-backs, billing, family conferences, new admissions, and emergencies.
A good way to look at inpatient work is in sets of blocks. (Figure 2) Within each block are the duties of the hospitalist. Blocks are prioritized in order of importance. Within the prioritized blocks are the “absolute” duties that a hospitalist must perform each day. They include patient care (new and existing), billing capture, and multidisciplinary care conferences. After the absolutes come duties that are routinely performed, including patient and nonpatient functions such as PCP call-backs, family conferencing, resident teaching, and time interrupters. Inpatient blocks can be stacked, with the first layer containing the absolutes and the subsequent layers containing the regular duties or tasks.
Interrupters are time delays that take a busy hospitalist away from absolute and regular work tasks. They are polygonal and can be placed anywhere along the blocks. Interrupters may be new patients, an established patient with an emergency, an outside physician trying to contact the service, a spouse, the medical records department, a funeral home inquiring about a death certificate, a home health agency trying to get certification for a patient’s wheelchair or a subspecialist, for example.
An ideal day shows the blocks in perfect formation, pyramid style. A day with interruptions will result in the blocks appearing disorganized. The ability to recognize time interrupters and to have a plan to deal with them is the key to managing a busy inpatient service. Any plan developed must use patient care as the focus. Everything the hospitalist does is centered on this block, and priorities can be developed to keep it focused.
Interruptions are a part of any busy inpatient service. Interrupters need to be prioritized, and a system needs to be in place for handling them with any good time management plan. Code Blue response, emergency patient need, and new patients on the floor rank high in priority for interrupters. Phone interruptions and nursing questions are ranked based on urgency and patient impact. One of the best ways to avoid too many phone interruptions is to have a coordinator or secretary assist with filtering incoming calls. This person will have specific instructions on how calls are to be handled. Emergency calls and incoming calls from physicians are given priority. A call from a drug representative or friend can be postponed.
A good rule to have when seeing new patients on the floor is to visualize each new patient coming onto the service. ER physicians visualize each patient coming into the ED arena. By direct visualization of incoming patients, ER physicians determine what their level of involvement will be. A patient who appears ill will get a quicker evaluation than a patient who appears stable. Principles that underlie patient triage include meeting the patient and identifying oneself as the responsible physician, visualization of the patient even while interviewing others, and communication and delegation of work.
Talking to an ED physician about a patient or to a PCP at an outreach facility is helpful, but the direct visualization of the patient by the hospitalist when he or she arrives on the ward is key to managing floor time. This method allows for patients to be prioritized based on acuity. Direct visualization can also be performed before resident contact is initiated. A quick look at the patient and his or her vitals provides reassurance that nothing immediate needs to be performed. A brief hospitalist introduction gives comfort to the patient and family. Patients are impressed when you meet them in their room when they arrive.
Critical patients require more attention, and care can be started with a primary survey. Trauma services have modes of triage care and initial evaluations of trauma patients that can be modified by hospitalists.
The objectives of initial trauma care include 1) stabilization, 2) identification of life-threatening injuries and initiation of adequate supportive therapy, and 3) efficient and rapid organization of either definitive therapy or transfer to a facility that provides definite therapy. Within this set of objectives is a triage objective to prioritize patients with a high likelihood of early deterioration.
Direct hospitalist visualization of every patient coming onto the service accomplishes the objectives of initial care and triage. Of course, the hospitalist isn’t prioritizing a gunshot wound patient, but the principles are the same: visualizing the patient, determining a level of involvement, and initiating a primary survey for critical patients. This approach to patients can be adopted in the hospitalist patient-care repertoire.
As an example, I was asked to consult on a patient with a subarachnoid bleed to manage hypertension. The patient was already admitted into the ICU by the neurosurgeon. Subarachnoid bleed and hypertension are 2 urgent needs, and this was a new patient on my service. I went to visualize the patient. I finished my brief survey and was writing down some orders when the nurse came over to me and told me the patient was not responding to her the way he had earlier. The patient’s admitting blood pressure was 180/100 and when the nurse reported the change to me, the blood pressure was 230/106. The patient was obtunded and unable to protect his airway. In addition to intubating the patient and hyperventilating him, I contacted the neurosurgeon to notify him of the change in status, started intravenous mannitol, established large bore venous access, and started nitroprusside. The surgeon returned to the ICU and took the patient for corrective surgery.
When the nurse alerted me to the change in status with the patient, I performed actions based on my survey, stabilized the patient, identified a threat, provided supportive care, and contacted the person who would be able to provide definitive treatment. I was able to do this because of the discipline provided to me with time management and by prioritizing an interrupter.
Developing a system to flexibly see new patients and provide quick surveys should be a focus for any hospitalist. By doing this, the hospitalist is providing the plan for how the day will flow, regardless of interruptions. The plan, the objectives, and the priorities are there to ensure a day happens the way the physician wants it to happen.
Time management courses and books usually recommend that people complete a daily log of how and what they do in the course of their day. (Figure 3) The daily log is an honest portrayal of the day as it unfolds and how one responds to events as they happen. Logs include phone calls to friends, stockbrokers, and spouses. Each hospitalist’s log notes when a patient or family conference occurred, when interruptions occurred, and how they were handled. Taking coffee breaks, reading a paper, and talking to a partner are all fair game in the log. Everything needs to be put in the log. Keeping a log for 1 or 2 days is a great exercise with endless ways of showing people where their time and energy is going. I encourage physicians who ask me what some of my secrets are to getting done early to read a book on time management or attend a course.
When I took my first time management course in 1998, I became an instant student of my time and an observer of how others mange their time. I didn’t realize how incredible a force time management was, because I thought it was mainly for business people. A course may range from the implementation of a few basic strategies to a complete revamp of how the day is structured, but any hospitalist can benefit from time management techniques.
Dr. Houser can be contacted at houserr@siouxvalley.org.
Reading List
- Mackenzie A. The Time Trap: The Classic Book on Time Management. New York, NY: AMACOM; 1997.
- Lane, B and Rierdan, R. Managing People-A Practical Guide. Oasis Press. 2001.
- Wachter R. The emerging role of “hospitalists” in the American health care system, N Engl J Me. 1996;335:514-7.
- Dries DJ. Initial evaluation of the trauma patient. www.eMedicine.com, 2004.
Hospital medicine groups are becoming an integral part of healthcare delivery in the US. Since the term hospitalist was coined in 1996 by Robert Wachter, the U.S. has witnessed an amazing growth and development of inpatient programs. Physicians going into inpatient medicine experience impressive fluctuations in patient volume when new programs begin and when existing programs expand their primary referral base or comanage patients with subspecialists and surgeons.
Ideal patient volume numbers vary from group to group but range, on average, from 15 to 18 patients per hospitalist. Layered on the management of patients in the hospital is a myriad of duties the hospitalist must perform to effectively care for patients. Depending on program layout, hospitalists will also be involved in committee work, end-of-life discussions, protocol development, and measurement of data that links improvement of care when hospitalists are involved in caring for patients.
A good reason to talk about inpatient time management is that without it physicians can become overstressed. Physician burnout, job dissatisfaction, and high turnover with hospital medicine groups are major concerns, due in part to the increased demands placed on hospitalists. Small programs, especially, can experience great fluctuations in volume as they define their patient referral base, and deficient physician time management skills can be the main reason a program does not gain momentum.
Early in my training, I wondered if there was a better way to see patients and not feel stressed when new patients were admitted to my service. But it wasn’t until I started work with a healthcare organization in Wisconsin that I noticed there was a way to gain control of my busy day. I was introduced to time management principles by physicians who exercised this important skill everyday. These physicians did not seem stressed when the day seemed to be getting “out of control.” Their time management skills allowed them to stay efficient. After a few busy days, it didn’t take long for me to seek out information on time management and begin my own journey of self-assessment. At its core, that’s what time management is: an honest assessment of yourself. After learning about time management, I created a plan to assist me in getting through my day. Now, time management is automatic, an integral part of my ability to function on a busy inpatient floor. Time management is important for anyone who wants to achieve more control of his or her day, improve on work efficiency, set personal and professional goals, and, in my opinion, extend himself or herself in ways that don’t seem possible.
Some important terms to review include “goal,” “objective,” and “priority.” Goals are long-range and provide overall direction for an individual or a group. A good goal for a hospital medicine group is to be the premiere group in their state or their region. A good goal for a hospitalist is to implement an inpatient time management strategy. An objective is a clear-cut description of how to achieve a goal, and priorities are the ranked items in a goal or objective list. Priorities must be assigned to time management objectives. An exact order will ensure nothing is missed when working on a given objective.
The best way to tackle inpatient time management is to see how the day is laid out by keeping a time log and by performing an internal review of how a typical day marches out. When I performed my internal review I realized I looked at my day chopped into sections that were spent rounding, teaching, and discharging. I never discharged a patient in the morning. I saved all my discharges until the afternoon. I knew discharges required more time, and I felt better seeing patients first and then going back and doing discharges. I wasn’t being efficient with this method, because I always felt tired in the afternoon.
There were different categories of patients: new admits from the previous night, discharges, routine patients, and critical patients. Critical patients received my highest priority, and discharges received the least priority. I was looking at critical patients differently than my discharges. Processing the ICU patients meant more thinking, diagnosing, and reviewing, whereas discharging meant dictating, writing prescriptions, educating patients, and making PCP call-backs. I wasn’t looking at each process in terms of time; rather, I was looking at discharges as a final step and the ICU as a place where all my energy had to be placed. I wasn’t making the connection with time and how I was comparing patients being discharged with patients in the ICU.
Energy level and task demands, in relationship to productive time, can be graphed (Figure 1). Energy level is highest in the morning, and tasks march out throughout the day. At the intersection, the time is usually noon for hospitalists. Energy level begins to dip after this time. The most productive time is in the early morning with a plateau around noon. This is why I felt tired in the afternoon, having important discharges to finish.
Once I made the connection that discharges take time and ICU patients take time, I knew I had to revamp how I saw patients. The most time-consuming patients need to be seen first when my energy level is high.
My new routine was to see the ICU patients first, new admissions second, and discharges third, all before noon. This new plan allowed me to begin seeing routine patients earlier. For my routine patients, I review the chart, look at lab and imaging tests ordered, and then go into the room and examine the patient. The difference with these patients is that I wait to write my final impression and discussion section until after I’ve seen all the routine patients. Then I go back and write my final notes. The rest of the day is concentrated on finishing notes, PCP call-backs, billing, family conferences, new admissions, and emergencies.
A good way to look at inpatient work is in sets of blocks. (Figure 2) Within each block are the duties of the hospitalist. Blocks are prioritized in order of importance. Within the prioritized blocks are the “absolute” duties that a hospitalist must perform each day. They include patient care (new and existing), billing capture, and multidisciplinary care conferences. After the absolutes come duties that are routinely performed, including patient and nonpatient functions such as PCP call-backs, family conferencing, resident teaching, and time interrupters. Inpatient blocks can be stacked, with the first layer containing the absolutes and the subsequent layers containing the regular duties or tasks.
Interrupters are time delays that take a busy hospitalist away from absolute and regular work tasks. They are polygonal and can be placed anywhere along the blocks. Interrupters may be new patients, an established patient with an emergency, an outside physician trying to contact the service, a spouse, the medical records department, a funeral home inquiring about a death certificate, a home health agency trying to get certification for a patient’s wheelchair or a subspecialist, for example.
An ideal day shows the blocks in perfect formation, pyramid style. A day with interruptions will result in the blocks appearing disorganized. The ability to recognize time interrupters and to have a plan to deal with them is the key to managing a busy inpatient service. Any plan developed must use patient care as the focus. Everything the hospitalist does is centered on this block, and priorities can be developed to keep it focused.
Interruptions are a part of any busy inpatient service. Interrupters need to be prioritized, and a system needs to be in place for handling them with any good time management plan. Code Blue response, emergency patient need, and new patients on the floor rank high in priority for interrupters. Phone interruptions and nursing questions are ranked based on urgency and patient impact. One of the best ways to avoid too many phone interruptions is to have a coordinator or secretary assist with filtering incoming calls. This person will have specific instructions on how calls are to be handled. Emergency calls and incoming calls from physicians are given priority. A call from a drug representative or friend can be postponed.
A good rule to have when seeing new patients on the floor is to visualize each new patient coming onto the service. ER physicians visualize each patient coming into the ED arena. By direct visualization of incoming patients, ER physicians determine what their level of involvement will be. A patient who appears ill will get a quicker evaluation than a patient who appears stable. Principles that underlie patient triage include meeting the patient and identifying oneself as the responsible physician, visualization of the patient even while interviewing others, and communication and delegation of work.
Talking to an ED physician about a patient or to a PCP at an outreach facility is helpful, but the direct visualization of the patient by the hospitalist when he or she arrives on the ward is key to managing floor time. This method allows for patients to be prioritized based on acuity. Direct visualization can also be performed before resident contact is initiated. A quick look at the patient and his or her vitals provides reassurance that nothing immediate needs to be performed. A brief hospitalist introduction gives comfort to the patient and family. Patients are impressed when you meet them in their room when they arrive.
Critical patients require more attention, and care can be started with a primary survey. Trauma services have modes of triage care and initial evaluations of trauma patients that can be modified by hospitalists.
The objectives of initial trauma care include 1) stabilization, 2) identification of life-threatening injuries and initiation of adequate supportive therapy, and 3) efficient and rapid organization of either definitive therapy or transfer to a facility that provides definite therapy. Within this set of objectives is a triage objective to prioritize patients with a high likelihood of early deterioration.
Direct hospitalist visualization of every patient coming onto the service accomplishes the objectives of initial care and triage. Of course, the hospitalist isn’t prioritizing a gunshot wound patient, but the principles are the same: visualizing the patient, determining a level of involvement, and initiating a primary survey for critical patients. This approach to patients can be adopted in the hospitalist patient-care repertoire.
As an example, I was asked to consult on a patient with a subarachnoid bleed to manage hypertension. The patient was already admitted into the ICU by the neurosurgeon. Subarachnoid bleed and hypertension are 2 urgent needs, and this was a new patient on my service. I went to visualize the patient. I finished my brief survey and was writing down some orders when the nurse came over to me and told me the patient was not responding to her the way he had earlier. The patient’s admitting blood pressure was 180/100 and when the nurse reported the change to me, the blood pressure was 230/106. The patient was obtunded and unable to protect his airway. In addition to intubating the patient and hyperventilating him, I contacted the neurosurgeon to notify him of the change in status, started intravenous mannitol, established large bore venous access, and started nitroprusside. The surgeon returned to the ICU and took the patient for corrective surgery.
When the nurse alerted me to the change in status with the patient, I performed actions based on my survey, stabilized the patient, identified a threat, provided supportive care, and contacted the person who would be able to provide definitive treatment. I was able to do this because of the discipline provided to me with time management and by prioritizing an interrupter.
Developing a system to flexibly see new patients and provide quick surveys should be a focus for any hospitalist. By doing this, the hospitalist is providing the plan for how the day will flow, regardless of interruptions. The plan, the objectives, and the priorities are there to ensure a day happens the way the physician wants it to happen.
Time management courses and books usually recommend that people complete a daily log of how and what they do in the course of their day. (Figure 3) The daily log is an honest portrayal of the day as it unfolds and how one responds to events as they happen. Logs include phone calls to friends, stockbrokers, and spouses. Each hospitalist’s log notes when a patient or family conference occurred, when interruptions occurred, and how they were handled. Taking coffee breaks, reading a paper, and talking to a partner are all fair game in the log. Everything needs to be put in the log. Keeping a log for 1 or 2 days is a great exercise with endless ways of showing people where their time and energy is going. I encourage physicians who ask me what some of my secrets are to getting done early to read a book on time management or attend a course.
When I took my first time management course in 1998, I became an instant student of my time and an observer of how others mange their time. I didn’t realize how incredible a force time management was, because I thought it was mainly for business people. A course may range from the implementation of a few basic strategies to a complete revamp of how the day is structured, but any hospitalist can benefit from time management techniques.
Dr. Houser can be contacted at houserr@siouxvalley.org.
Reading List
- Mackenzie A. The Time Trap: The Classic Book on Time Management. New York, NY: AMACOM; 1997.
- Lane, B and Rierdan, R. Managing People-A Practical Guide. Oasis Press. 2001.
- Wachter R. The emerging role of “hospitalists” in the American health care system, N Engl J Me. 1996;335:514-7.
- Dries DJ. Initial evaluation of the trauma patient. www.eMedicine.com, 2004.