User login
Spondylolysis and Spondylolisthesis Primary Care Clinicians' Role
CE/CME No: CR-1410
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Identify risk factors for the development of spondylolysis and spondylolisthesis
• Discuss the differential diagnoses associated with low back pain
• Describe physical examination findings consistent with spondylolysis and spondylolisthesis
• List the imaging modalities that may be used to confirm these diagnoses and explain the indications for each
• Identify when a pediatric patient with low back pain should be referred to an orthopedic or neurologic specialist for further evaluation and treatment
FACULTY
Shannon P. More is a pediatric nurse practitioner in New York City. Rita Marie John is a Professor at the Columbia University School of Nursing in New York City. The authors have no significant financial relationships to disclose.
ACCREDITATION STATEMENT
Article begins on next page >>
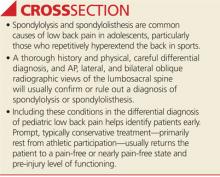
The most common causes of low back pain in adolescents, spondylolysis and spondylolisthesis can be tricky to diagnose. The primary care clinician plays a key role in optimal management so that full recovery, in most cases, is achieved.
Spondylolysis, the most common cause of low back pain in adolescents, occurs in approximately 8% to 14% of adolescent athletes.1 It is estimated that 15% to 25% of patients with spondylolysis will develop spondylolisthesis.2 This article discusses the definitions, pathophysiology, risk factors, differential diagnosis, and clinical presentation of spondylolysis and spondylolisthesis, including a review of diagnostic imaging, treatment, and the primary care clinician’s role in the optimal management of affected patients.
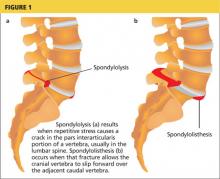
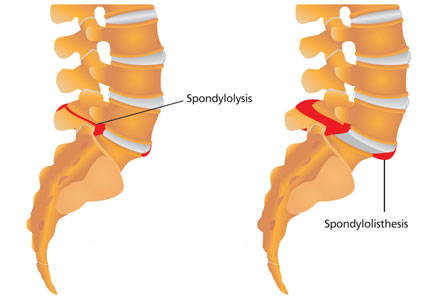
Spondylolysis is a congenital or acquired unilateral or bilateral defect in the portion of a vertebra—usually L5—called the pars interarticularis, the bony area between the superior and inferior articulating facets (see Figure 1a). Recurrent trauma, such as repeated flexion, hyperextension, or twisting, can weaken the pars interarticularis. During these movements, the inferior articular process of the cranial (upper) vertebra can come into contact with the pars interarticularis of the caudal (lower) vertebra. When this happens repeatedly, a stress reaction may occur in the pars interarticularis, which can result in a stress or complete nonunion fracture.
The paraspinal muscles around the lumbar spine may adjust to accommodate the weakened vertebra, resulting in postural alterations. This can predispose patients to further spinal injury because normal muscular control of that portion of the spine is impaired.3
When the break in the pars interarticularis causes slippage, or forward movement, of the upper vertebra (again, usually L5) over the vertebra (ie, S1) below it, spondylolisthesis occurs (see Figure 1b, above).2,4 This happens more frequently with bilateral spondylolysis and is often associated with an adolescent growth spurt.5
Spondylolisthesis can manifest anywhere in the spine but is most common in the lumbosacral region, with most (71% to 95%) cases occurring at L5 and the remainder at L4.6 Some patients develop these conditions spontaneously through strenuous activity or injury; others are predisposed but remain asymptomatic until the condition is exacerbated through athletic activities.
Wiltse first described spondylolisthesis in 1962 and 10 years later published a classification system based on etiology and anatomy; his research is still used today as the basis for diagnosis.7,8 The five types of spondylolisthesis are
• Type 1, dysplastic (congenital)
• Type 2, isthmic (defect in pars interarticularis)
• Type 3, degenerative (arthritic changes in older patients)
• Type 4, traumatic (acute injury)
• Type 5, pathologic (bone disease).8
Types 1 and 2 occur in pediatric patients, with 85% of such cases classified as type 2.4
The classification is further refined according to degree of severity, defined as the percentage of slippage of the upper over the lower vertebra. Grade 1 (first degree) entails a slippage of less than 25%; grade 2 (second degree), 26% to 50%; grade 3 (third degree), 51% to 75%; and grade 4 (fourth degree), greater than 75%.5
Risk Factors
In general, women are at greater risk for stress fractures than men are.9 Yet while pars interarticularis defects are twice as common in men as in women, women are more likely to progress to spondylolisthesis.10 Similarly, in patients with bilateral spondylolysis, women are significantly more likely than men (90.9% vs 66.2%) to develop spondylolisthesis.11 In general, those who repetitively hyperextend the lower back (eg, football players, rowers, dancers, gymnasts, soccer players, swimmers) are at increased risk for both spondylolysis and spondylolisthesis.
While a patient’s activities and environmental stressors play a role in the development of spondylolysis and spondylolisthesis, a genetic predisposition is believed to be a factor as well: A five-fold increase in the incidence of defects of the pars interarticularis has been noted in near relatives of patients with spondylolisthesis.7 In addition, patients with conditions such as spina bifida occulta, severe scoliosis, and osteogenesis imperfecta are at increased risk for these conditions.6,12
Differential DiagnosIs
Both spondylolysis and spondylolisthesis manifest as low back pain, for which the differential diagnosis is extensive. Pathologic causes of low back pain are much less common than causes related to structural weakness or trauma; however, carefully differentiating these is important so that pathology is identified promptly and treated appropriately.13
The differential diagnosis for low back pain in pediatric patients, by type of pain, includes
• Pain at night or with fever or other generalized symptoms: tumor or infection
• Acute pain: herniated disk, slipped apophysis, spondylolysis, vertebral fracture, or muscle strain
• Chronic pain: Scheuermann kyphosis, inflammatory spondyloarthropathies, or psychological problems
• Pain with spinal forward flexion: herniated disk or slipped apophysis
• Pain with spinal extension: spondylolysis, spondylolisthesis, or lesion or injury in the pedicle or lamina (posterior arch)
• Pain with recent-onset scoliosis: tumor, infection, herniated disk, syrinx, or idiopathic scoliosis
• Other pain: pyelonephritis or sickle cell crisis.13
Clinical Presentation
A systematic approach to a patient with a chief concern of low back pain is recommended. An initial assessment of the patient’s vital signs and growth parameters should be compared to those from previous visits to determine if there have been any changes in the usual pattern.
History
Use the standard HEEADSSS (Home, Education, Eating, Activities, Drugs, Sexuality, Suicide, Safety) adolescent psychosocial assessment as part of the patient history.14 In particular, focus on details about the physical activities and sports in which the patient participates and obtain data on the amount of time spent on each. When taking the family history, pay particular attention to any predisposition to musculoskeletal disorders. In the review of systems, note any history of traumatic injury.
Next, ask the patient to point with one finger to the location at which the pain is felt; in spondylolysis and spondylolisthesis, pain localizes to the waist. Obtain a detailed history of the pain, including onset, duration, frequency, location, and all alleviating or exacerbating factors.15
Physical examination
A brief summary of key features to assess during the physical examination is presented in Table 1. When completing the physical assessment, follow the typical head-to-toe approach, with special attention to evaluation of the presenting back pain.
Visual inspection. A visual inspection of the spine for scoliosis and kyphosis is key; also be sure to examine posture, assess symmetry, and observe for any midline defects.13 Hemangiomas, a line of hairy patches, or other abnormal markings along the body’s vertical axis may suggest an intraspinal anomaly.
Palpation. The entire spine should be palpated to confirm the location of the pain as identified by the patient. In particular, note if tenderness is felt over bony structures of the spine or in the paraspinal musculature.
Range of motion. After the locus of the pain is confirmed, instruct the patient to flex and extend the spine to assess for worsening pain. If noted, this finding is pathognomonic for spondylolysis and spondylolisthesis.13
Also useful for making the diagnosis is the one-leg hyperextension test, in which the patient is asked to raise one leg off the ground and lean backward. Pain elicited during this movement is indicative of back injury, including spondylolysis or spondylolisthesis. A positive result with the one-leg hyperextension test alone, however, is not a clinical marker for spondylolysis. Not only may the test elicit pain stemming from other pathologies, but the results are dependent on the patient’s subjective reporting of pain.16
Muscular signs and symptoms. Hamstring tightness is present in 80% of symptomatic patients.5 Consequently, the patient may have a somewhat waddling gait due to the inability to flex the hips and extend the knee simultaneously. For this reason, physical examination for spondylolysis and spondylolisthesis includes gait assessment. Other clinical signs of spondylolisthesis include a weak and drooping abdominal wall, paravertebral muscle hypertrophy, increased lumbar lordosis, hamstring muscle spasm, and pain during lateral trunk flexion/extension and double leg raising.17
Motor and sensory function. It is important to assess motor and sensory function to differentiate neurologic from orthopedic conditions. Deep tendon reflexes and lower extremity motor strength and sensory capabilities also need careful assessment.13 Sensation in the region of the cauda equinus requires further evaluation due to the possibility of cauda equinus compression. Hyperreflexia indicates an upper motor lesion, whereas hyporeflexia indicates a lower motor lesion—neither of which would be expected in spondylolisthesis or spondylolysis.
A patient with any positive neurologic signs should be referred to a neurologic specialist.
Diagnostic TESTING
Unfortunately, rigorous comparative research is lacking on which to base clinical practice guidelines for diagnosis (as well as treatment) of spondylolysis and spondylolisthesis.18 Nevertheless, current standards call for a detailed physical examination as an effective diagnostic tool and recommend radiologic evaluation for a definitive diagnosis.17,18 Lateral radiographs are also useful for identifying the degree of vertebral slippage when spondylolisthesis is diagnosed.17 The specialist may choose to utilize such diagnostic modalities as CT, single-photon-emission CT (SPECT), or MRI.
Radiologic evaluation
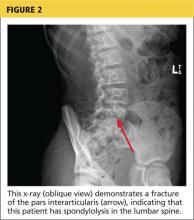
For complete radiologic evaluation, four x-ray views of the spine are necessary: anterior-posterior (AP), lateral, and bilateral oblique views. A fracture seen in the pars interarticularis is called the Scotty dog sign because it looks like a collar around the neck of a Scottish terrier (see Figures 2 and 3).2
Since treatment for nonspecific back pain and spondylolysis is essentially the same, it could be argued that radiographic imaging to confirm the clinical diagnosis exposes the patient to unnecessary radiation (a particular concern in the pediatric population). But a definitive diagnosis also rules out other pathologies that would require more aggressive treatment.
If x-rays reveal abnormalities, refer the patient to an orthopedic specialist for further evaluation. Referral to orthopedics should also be prompted if spondylolysis or spondylolisthesis is suspected but x-rays are insufficient to make the diagnosis.
CT and SPECT
Standaert and Herring suggest that CT combined with SPECT is the standard for diagnosis of a pars interarticularis lesion1; in many reported cases, CT test results may be negative even when SPECT results are abnormal, suggesting that both studies are needed. In other cases, CT can help identify the origin of an abnormality seen on SPECT.
The disadvantage to using both modalities is that the patient is exposed to additional ionizing radiation. If only one method is to be used, SPECT may be preferred; it exposes the patient to less ionizing radiation and seldom requires sedation.19
Magnetic resonance imaging
In terms of radiation exposure, MRI is preferred to CT and SPECT because it does not utilize ionizing radiation; unfortunately, it is also less effective at detection of spondylolysis and spondylolisthesis. A review of the literature indicates that MRI is not as sensitive as SPECT in identifying stress on the pars interarticularis.16,19
In general, MRI is superior for visualizing soft tissue pathology (eg, disk disease, nerve root compression, inflammation), while CT is superior for visualization of bone. In the context of back pain, MRI may be informative when etiologies other than spondylolysis and spondylolisthesis are suspected; Feldman et al recommend MRI for patients with constant back pain, radicular pain, nighttime pain, and/or abnormal neurologic examination results.16
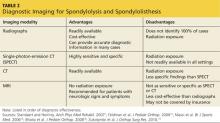
The advantages and disadvantages of x-rays, SPECT, CT, and MRI for the diagnosis of spondylolysis and spondylolisthesis are summarized in Table 2.1,15,16,18,19
Laboratory studies
There are no laboratory tests to confirm the diagnosis of spondylolysis or spondylolisthesis. To eliminate other diagnoses, however, it is appropriate to order certain laboratory tests. In addition to radiographs, Bernstein and Cozen recommend a complete blood count, an erythrocyte sedimentation rate, and a C-reactive protein test as part of the diagnostic work-up if the history and physical are suspicious for underlying pathology, such as infection.13
Management and Treatment Options
Treatment for spondylolysis or spondylolisthesis ranges from basic strengthening programs to surgical intervention and is based on the severity of the patient’s condition. The goal is to alleviate symptoms and facilitate a return to normal activities. Treatment should be individualized based on the patient’s age, athletic level and demands, and severity of symptoms.10
Nonsurgical treatment
Conservative treatment options include rest, physical therapy, core strengthening, and antilordotic bracing for several months (eg, eight to 12 weeks).5 Most grade 1 and 2 cases can be successfully treated nonsurgically.
Studies of nonsurgical treatment of children and young adults with spondylolysis and/or mild spondylolisthesis (up to 25% slippage) were evaluated in a meta-analysis.20 The authors found that approximately 84% of such patients were pain free or nearly pain free with unrestricted activities within one year of treatment. While nonsurgical treatment does not usually resolve the pars interarticularis defect, it alleviates symptoms and enables the patient’s return to unrestricted activities. Further, the authors found no significant difference in outcomes between patients who were treated with or without bracing.20
In contrast, another study demonstrated that patients who wore braces achieved higher functional outcomes than those who did not.21 However, the patients who were braced were restricted from physical activity longer than were those who were not braced, so it could not be definitively determined if bracing or additional rest was the reason for the improved outcomes.
A significant limitation of bracing is that it is a restrictive and sometimes uncomfortable treatment, especially for an active child or adolescent. If clinicians can treat these patients effectively without bracing, greater compliance with treatment may result.
This study also found a strong correlation between early intervention and an increased incidence of bony healing. The researchers recommend the early use of sensitive diagnostic imaging so that treatment can begin early, increasing the possibility that the fracture will heal.20
Skeletally immature patients should be followed clinically at six-month to one-year intervals, including use of lateral x-rays for spinal evaluation, to ensure that progressive spondylolisthesis does not develop. Once skeletal development is complete, follow-up is no longer necessary because progressive spondylolisthesis is unlikely at or near skeletal maturity.10
Surgical treatment
When conservative treatment fails to alleviate the pediatric patient’s pain, if daily functioning is impaired, or if the spondylolisthesis is of a more severe grade or progresses, surgical correction to repair the pars interarticularis defect or laminectomy and spinal fusion may be necessary.5 Adolescent patients treated surgically are likely to have good long-term results but may still experience symptoms, including back pain, into adulthood.22 The procedure used in a particular case depends on the degree of severity and the patient’s specific presentation.
PRIMARY CARE IS KEY
As stated earlier, referral to an orthopedic specialist is indicated when spondylolysis or spondylolisthesis is suspected or confirmed or to a neurologic specialist when any neurologic signs are positive or deficits are noted. In these instances, the primary care clinician is key to early diagnosis and prompt treatment.
Primary health care practitioners are in a position to contribute to the management of spondylolysis or spondylolisthesis in a way that will help facilitate a full recovery. For example, the patient and parent or guardian should be counseled about the need for the child to refrain from athletic activity while awaiting an orthopedic or neurologic evaluation. Restriction of activity will prevent exacerbation of the injury and increased pain. Suggest OTC NSAIDs, taken with food to prevent gastrointestinal adverse effects, for pain relief.13
It can also be helpful to assess the patient’s psychosocial status to determine whether he or she might face barriers to recovery. Often a major obstacle in treating these conditions is pressure from parents, coaches, or the patients themselves to continue athletic activities despite pain and injury.
Clinicians can offer support by reinforcing the message that limiting physical activity is essential to recovery; it should not be compromised because of patient, parental, coach, or peer pressure. At the same time, it is important to recognize that a leave of absence from a competitive sport, no matter how short, can affect the patient’s mental health. If the patient feels angry or depressed about the diagnosis, mental health counseling options can be discussed.
Educating patients and parents about the numerous treatments for acute low back pain that have been proven to offer little benefit can be informative and reassuring. For example, adding spinal manipulation and chiropractic techniques to established medical treatments does not improve outcomes. Neither does the use of oral corticosteroids, acupuncture, massage, traction, or exercise programs. Bed rest should be avoided.23
Conclusion
In the primary care setting, low back pain is a common complaint with an extensive differential diagnosis. If a thorough history and physical examination prompt suspicion for spondylolysis or spondylolisthesis, x-rays will usually confirm the diagnosis. If the patient is referred to an orthopedic specialist, the primary care clinician can supplement and reinforce the treatment plan through patient and parent education about the diagnosis and its treatment. Compliance with conservative nonsurgical treatment may enable the patient to make a speedier return to his or her usual physical activities.
The authors would like to thank Jennifer Tareco, MD, and Robert More, MD, for their revisions and support in the completion of this article.
1. Standaert CJ, Herring SA. Expert opinion and controversies in sports and musculoskeletal medicine: the diagnosis and treatment of spondylolysis in adolescent athletes. Arch Phys Med Rehabil. 2007;88(4):537-540.
2. Spiegel DA, Dormans JP. Spondylolysis and spondylolisthesis. In: Kliegman RM, Stanton BF, Schor NF, St. Geme III JW, Behrman RE, eds. Nelson Textbook of Pediatrics. Philadelphia, PA: Elsevier; 2011:1561-1571.
3. Smith J. Moving beyond the neutral spine: stabilizing the dancer with lumbar extension dysfunction. J Dance Med Sci. 2009;13(3):73-82.
4. Hu SS, Tribus CB, Diab M, Ghanayem AJ. Spondylolisthesis and spondylolysis. J Bone Joint Surg Am. 2008;90(3):656-671.
5. Wicker A. Spondylolysis and spondylolisthesis in sports. Int Sports Med J. 2008;9(2):74-78.
6. McCleary MD, Congeni JA. Current concepts in the diagnosis and treatment of spondylolysis in young athletes. Curr Sports Med Rep. 2007; 6(1):62-66.
7. Wiltse LL. The etiology of spondylolisthesis. J Bone Joint Surg Am. 1962;44-A:539-560.
8. Wiltse LL, Newman PH, Macnab I. Classification of spondylolysis and spondylolisthesis. Clin Orthop Relat Res. 1976;117:23-29.
9. Ivkovic A, Franic M, Bojanic I, Pecina M. Overuse injuries in female athletes. Croat Med J. 2007;48:767-778.
10. Tallarico RA, Madom IA, Palumbo MA. Spondylolysis and spondylolisthesis in the athlete. Sports Med Arthrosc. 2008;16(1):32-38.
11. Takao S, Sakai T, Sairyo K, et al. Radiographic comparison between male and female patients with lumbar spondylolysis. J Med Invest. 2010;57 (1-2):133-137.
12. Hatz D, Esposito PW, Schroeder B, et al. The incidence of spondylolysis and spondylolisthesis in children with osteogenesis imperfecta. J Pediatr Orthop. 2011;31(6):655-660.
13. Bernstein RM, Cozen H. Evaluation of back pain in children and adolescents. Am Fam Physician. 2007;76(11):1669-1676.
14. Klein DA, Goldenring JM, Adelman WP. HEEADSSS 3.0: The psychosocial interview for adolescents updated for a new century fueled by media. Contemp Pediatr. 2014;1:16-28.
15. Feldman DS, Straight JJ, Badra MI, et al. Evaluation of an algorithmic approach to pediatric back pain. J Pediatr Orthop. 2006;26(3):353-357.
16. Masci L, Pike J, Malara F, et al. Use of the one-legged hyperextension test and magnetic resonance imaging in the diagnosis of active spondylolysis. Br J Sports Med. 2006;40(11):940-946.
17. Kalpakcioglu B, Altinbilek T, Senel K. Determination of spondylolisthesis in low back pain by clinical evaluation. J Back Musculoskelet Rehabil. 2009;22(1):27-32.
18. Bhatia NN, Chow G, Timon SJ, Watts HG. Diagnostic modalities for the evaluation of pediatric back pain: a prospective study. J Pediatr Orthop. 2008;28(2):230-233.
19. Zukotynski K, Curtis C, Grant FD, et al. The value of SPECT in the detection of stress injury to the pars interarticularis in patients with low back pain. J Orthop Surg Res. 2010;5(13):1-6.
20. Klein G, Mehlman CT, McCarty M. Nonoperative treatment of spondylolysis and grade I spondylolisthesis in children and young adults. J Pediatr Orthop. 2009;29(2):146-156.
21. Alvarez-Diaz P, Alentorn-Geli E, Steinbacher G, et al. Conservative treatment of lumbar spondylolysis in young soccer players. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2111-2114.
22. Helenius I, Remes V, Lamberg T, et al. Long-term health-related quality of life after surgery for adolescent idiopathic scoliosis and spondylolisthesis. J Bone Joint Surg Am. 2008;90(6):1231-1239.
23. Casazza BA. Diagnosis and treatment of acute low back pain. Am Fam Physician. 2012;85(4):343-350.
CE/CME No: CR-1410
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Identify risk factors for the development of spondylolysis and spondylolisthesis
• Discuss the differential diagnoses associated with low back pain
• Describe physical examination findings consistent with spondylolysis and spondylolisthesis
• List the imaging modalities that may be used to confirm these diagnoses and explain the indications for each
• Identify when a pediatric patient with low back pain should be referred to an orthopedic or neurologic specialist for further evaluation and treatment
FACULTY
Shannon P. More is a pediatric nurse practitioner in New York City. Rita Marie John is a Professor at the Columbia University School of Nursing in New York City. The authors have no significant financial relationships to disclose.
ACCREDITATION STATEMENT
Article begins on next page >>
The most common causes of low back pain in adolescents, spondylolysis and spondylolisthesis can be tricky to diagnose. The primary care clinician plays a key role in optimal management so that full recovery, in most cases, is achieved.
Spondylolysis, the most common cause of low back pain in adolescents, occurs in approximately 8% to 14% of adolescent athletes.1 It is estimated that 15% to 25% of patients with spondylolysis will develop spondylolisthesis.2 This article discusses the definitions, pathophysiology, risk factors, differential diagnosis, and clinical presentation of spondylolysis and spondylolisthesis, including a review of diagnostic imaging, treatment, and the primary care clinician’s role in the optimal management of affected patients.
Spondylolysis is a congenital or acquired unilateral or bilateral defect in the portion of a vertebra—usually L5—called the pars interarticularis, the bony area between the superior and inferior articulating facets (see Figure 1a). Recurrent trauma, such as repeated flexion, hyperextension, or twisting, can weaken the pars interarticularis. During these movements, the inferior articular process of the cranial (upper) vertebra can come into contact with the pars interarticularis of the caudal (lower) vertebra. When this happens repeatedly, a stress reaction may occur in the pars interarticularis, which can result in a stress or complete nonunion fracture.
The paraspinal muscles around the lumbar spine may adjust to accommodate the weakened vertebra, resulting in postural alterations. This can predispose patients to further spinal injury because normal muscular control of that portion of the spine is impaired.3
When the break in the pars interarticularis causes slippage, or forward movement, of the upper vertebra (again, usually L5) over the vertebra (ie, S1) below it, spondylolisthesis occurs (see Figure 1b, above).2,4 This happens more frequently with bilateral spondylolysis and is often associated with an adolescent growth spurt.5
Spondylolisthesis can manifest anywhere in the spine but is most common in the lumbosacral region, with most (71% to 95%) cases occurring at L5 and the remainder at L4.6 Some patients develop these conditions spontaneously through strenuous activity or injury; others are predisposed but remain asymptomatic until the condition is exacerbated through athletic activities.
Wiltse first described spondylolisthesis in 1962 and 10 years later published a classification system based on etiology and anatomy; his research is still used today as the basis for diagnosis.7,8 The five types of spondylolisthesis are
• Type 1, dysplastic (congenital)
• Type 2, isthmic (defect in pars interarticularis)
• Type 3, degenerative (arthritic changes in older patients)
• Type 4, traumatic (acute injury)
• Type 5, pathologic (bone disease).8
Types 1 and 2 occur in pediatric patients, with 85% of such cases classified as type 2.4
The classification is further refined according to degree of severity, defined as the percentage of slippage of the upper over the lower vertebra. Grade 1 (first degree) entails a slippage of less than 25%; grade 2 (second degree), 26% to 50%; grade 3 (third degree), 51% to 75%; and grade 4 (fourth degree), greater than 75%.5
Risk Factors
In general, women are at greater risk for stress fractures than men are.9 Yet while pars interarticularis defects are twice as common in men as in women, women are more likely to progress to spondylolisthesis.10 Similarly, in patients with bilateral spondylolysis, women are significantly more likely than men (90.9% vs 66.2%) to develop spondylolisthesis.11 In general, those who repetitively hyperextend the lower back (eg, football players, rowers, dancers, gymnasts, soccer players, swimmers) are at increased risk for both spondylolysis and spondylolisthesis.
While a patient’s activities and environmental stressors play a role in the development of spondylolysis and spondylolisthesis, a genetic predisposition is believed to be a factor as well: A five-fold increase in the incidence of defects of the pars interarticularis has been noted in near relatives of patients with spondylolisthesis.7 In addition, patients with conditions such as spina bifida occulta, severe scoliosis, and osteogenesis imperfecta are at increased risk for these conditions.6,12
Differential DiagnosIs
Both spondylolysis and spondylolisthesis manifest as low back pain, for which the differential diagnosis is extensive. Pathologic causes of low back pain are much less common than causes related to structural weakness or trauma; however, carefully differentiating these is important so that pathology is identified promptly and treated appropriately.13
The differential diagnosis for low back pain in pediatric patients, by type of pain, includes
• Pain at night or with fever or other generalized symptoms: tumor or infection
• Acute pain: herniated disk, slipped apophysis, spondylolysis, vertebral fracture, or muscle strain
• Chronic pain: Scheuermann kyphosis, inflammatory spondyloarthropathies, or psychological problems
• Pain with spinal forward flexion: herniated disk or slipped apophysis
• Pain with spinal extension: spondylolysis, spondylolisthesis, or lesion or injury in the pedicle or lamina (posterior arch)
• Pain with recent-onset scoliosis: tumor, infection, herniated disk, syrinx, or idiopathic scoliosis
• Other pain: pyelonephritis or sickle cell crisis.13
Clinical Presentation
A systematic approach to a patient with a chief concern of low back pain is recommended. An initial assessment of the patient’s vital signs and growth parameters should be compared to those from previous visits to determine if there have been any changes in the usual pattern.
History
Use the standard HEEADSSS (Home, Education, Eating, Activities, Drugs, Sexuality, Suicide, Safety) adolescent psychosocial assessment as part of the patient history.14 In particular, focus on details about the physical activities and sports in which the patient participates and obtain data on the amount of time spent on each. When taking the family history, pay particular attention to any predisposition to musculoskeletal disorders. In the review of systems, note any history of traumatic injury.
Next, ask the patient to point with one finger to the location at which the pain is felt; in spondylolysis and spondylolisthesis, pain localizes to the waist. Obtain a detailed history of the pain, including onset, duration, frequency, location, and all alleviating or exacerbating factors.15
Physical examination
A brief summary of key features to assess during the physical examination is presented in Table 1. When completing the physical assessment, follow the typical head-to-toe approach, with special attention to evaluation of the presenting back pain.
Visual inspection. A visual inspection of the spine for scoliosis and kyphosis is key; also be sure to examine posture, assess symmetry, and observe for any midline defects.13 Hemangiomas, a line of hairy patches, or other abnormal markings along the body’s vertical axis may suggest an intraspinal anomaly.
Palpation. The entire spine should be palpated to confirm the location of the pain as identified by the patient. In particular, note if tenderness is felt over bony structures of the spine or in the paraspinal musculature.
Range of motion. After the locus of the pain is confirmed, instruct the patient to flex and extend the spine to assess for worsening pain. If noted, this finding is pathognomonic for spondylolysis and spondylolisthesis.13
Also useful for making the diagnosis is the one-leg hyperextension test, in which the patient is asked to raise one leg off the ground and lean backward. Pain elicited during this movement is indicative of back injury, including spondylolysis or spondylolisthesis. A positive result with the one-leg hyperextension test alone, however, is not a clinical marker for spondylolysis. Not only may the test elicit pain stemming from other pathologies, but the results are dependent on the patient’s subjective reporting of pain.16
Muscular signs and symptoms. Hamstring tightness is present in 80% of symptomatic patients.5 Consequently, the patient may have a somewhat waddling gait due to the inability to flex the hips and extend the knee simultaneously. For this reason, physical examination for spondylolysis and spondylolisthesis includes gait assessment. Other clinical signs of spondylolisthesis include a weak and drooping abdominal wall, paravertebral muscle hypertrophy, increased lumbar lordosis, hamstring muscle spasm, and pain during lateral trunk flexion/extension and double leg raising.17
Motor and sensory function. It is important to assess motor and sensory function to differentiate neurologic from orthopedic conditions. Deep tendon reflexes and lower extremity motor strength and sensory capabilities also need careful assessment.13 Sensation in the region of the cauda equinus requires further evaluation due to the possibility of cauda equinus compression. Hyperreflexia indicates an upper motor lesion, whereas hyporeflexia indicates a lower motor lesion—neither of which would be expected in spondylolisthesis or spondylolysis.
A patient with any positive neurologic signs should be referred to a neurologic specialist.
Diagnostic TESTING
Unfortunately, rigorous comparative research is lacking on which to base clinical practice guidelines for diagnosis (as well as treatment) of spondylolysis and spondylolisthesis.18 Nevertheless, current standards call for a detailed physical examination as an effective diagnostic tool and recommend radiologic evaluation for a definitive diagnosis.17,18 Lateral radiographs are also useful for identifying the degree of vertebral slippage when spondylolisthesis is diagnosed.17 The specialist may choose to utilize such diagnostic modalities as CT, single-photon-emission CT (SPECT), or MRI.
Radiologic evaluation
For complete radiologic evaluation, four x-ray views of the spine are necessary: anterior-posterior (AP), lateral, and bilateral oblique views. A fracture seen in the pars interarticularis is called the Scotty dog sign because it looks like a collar around the neck of a Scottish terrier (see Figures 2 and 3).2
Since treatment for nonspecific back pain and spondylolysis is essentially the same, it could be argued that radiographic imaging to confirm the clinical diagnosis exposes the patient to unnecessary radiation (a particular concern in the pediatric population). But a definitive diagnosis also rules out other pathologies that would require more aggressive treatment.
If x-rays reveal abnormalities, refer the patient to an orthopedic specialist for further evaluation. Referral to orthopedics should also be prompted if spondylolysis or spondylolisthesis is suspected but x-rays are insufficient to make the diagnosis.
CT and SPECT
Standaert and Herring suggest that CT combined with SPECT is the standard for diagnosis of a pars interarticularis lesion1; in many reported cases, CT test results may be negative even when SPECT results are abnormal, suggesting that both studies are needed. In other cases, CT can help identify the origin of an abnormality seen on SPECT.
The disadvantage to using both modalities is that the patient is exposed to additional ionizing radiation. If only one method is to be used, SPECT may be preferred; it exposes the patient to less ionizing radiation and seldom requires sedation.19
Magnetic resonance imaging
In terms of radiation exposure, MRI is preferred to CT and SPECT because it does not utilize ionizing radiation; unfortunately, it is also less effective at detection of spondylolysis and spondylolisthesis. A review of the literature indicates that MRI is not as sensitive as SPECT in identifying stress on the pars interarticularis.16,19
In general, MRI is superior for visualizing soft tissue pathology (eg, disk disease, nerve root compression, inflammation), while CT is superior for visualization of bone. In the context of back pain, MRI may be informative when etiologies other than spondylolysis and spondylolisthesis are suspected; Feldman et al recommend MRI for patients with constant back pain, radicular pain, nighttime pain, and/or abnormal neurologic examination results.16
The advantages and disadvantages of x-rays, SPECT, CT, and MRI for the diagnosis of spondylolysis and spondylolisthesis are summarized in Table 2.1,15,16,18,19
Laboratory studies
There are no laboratory tests to confirm the diagnosis of spondylolysis or spondylolisthesis. To eliminate other diagnoses, however, it is appropriate to order certain laboratory tests. In addition to radiographs, Bernstein and Cozen recommend a complete blood count, an erythrocyte sedimentation rate, and a C-reactive protein test as part of the diagnostic work-up if the history and physical are suspicious for underlying pathology, such as infection.13
Management and Treatment Options
Treatment for spondylolysis or spondylolisthesis ranges from basic strengthening programs to surgical intervention and is based on the severity of the patient’s condition. The goal is to alleviate symptoms and facilitate a return to normal activities. Treatment should be individualized based on the patient’s age, athletic level and demands, and severity of symptoms.10
Nonsurgical treatment
Conservative treatment options include rest, physical therapy, core strengthening, and antilordotic bracing for several months (eg, eight to 12 weeks).5 Most grade 1 and 2 cases can be successfully treated nonsurgically.
Studies of nonsurgical treatment of children and young adults with spondylolysis and/or mild spondylolisthesis (up to 25% slippage) were evaluated in a meta-analysis.20 The authors found that approximately 84% of such patients were pain free or nearly pain free with unrestricted activities within one year of treatment. While nonsurgical treatment does not usually resolve the pars interarticularis defect, it alleviates symptoms and enables the patient’s return to unrestricted activities. Further, the authors found no significant difference in outcomes between patients who were treated with or without bracing.20
In contrast, another study demonstrated that patients who wore braces achieved higher functional outcomes than those who did not.21 However, the patients who were braced were restricted from physical activity longer than were those who were not braced, so it could not be definitively determined if bracing or additional rest was the reason for the improved outcomes.
A significant limitation of bracing is that it is a restrictive and sometimes uncomfortable treatment, especially for an active child or adolescent. If clinicians can treat these patients effectively without bracing, greater compliance with treatment may result.
This study also found a strong correlation between early intervention and an increased incidence of bony healing. The researchers recommend the early use of sensitive diagnostic imaging so that treatment can begin early, increasing the possibility that the fracture will heal.20
Skeletally immature patients should be followed clinically at six-month to one-year intervals, including use of lateral x-rays for spinal evaluation, to ensure that progressive spondylolisthesis does not develop. Once skeletal development is complete, follow-up is no longer necessary because progressive spondylolisthesis is unlikely at or near skeletal maturity.10
Surgical treatment
When conservative treatment fails to alleviate the pediatric patient’s pain, if daily functioning is impaired, or if the spondylolisthesis is of a more severe grade or progresses, surgical correction to repair the pars interarticularis defect or laminectomy and spinal fusion may be necessary.5 Adolescent patients treated surgically are likely to have good long-term results but may still experience symptoms, including back pain, into adulthood.22 The procedure used in a particular case depends on the degree of severity and the patient’s specific presentation.
PRIMARY CARE IS KEY
As stated earlier, referral to an orthopedic specialist is indicated when spondylolysis or spondylolisthesis is suspected or confirmed or to a neurologic specialist when any neurologic signs are positive or deficits are noted. In these instances, the primary care clinician is key to early diagnosis and prompt treatment.
Primary health care practitioners are in a position to contribute to the management of spondylolysis or spondylolisthesis in a way that will help facilitate a full recovery. For example, the patient and parent or guardian should be counseled about the need for the child to refrain from athletic activity while awaiting an orthopedic or neurologic evaluation. Restriction of activity will prevent exacerbation of the injury and increased pain. Suggest OTC NSAIDs, taken with food to prevent gastrointestinal adverse effects, for pain relief.13
It can also be helpful to assess the patient’s psychosocial status to determine whether he or she might face barriers to recovery. Often a major obstacle in treating these conditions is pressure from parents, coaches, or the patients themselves to continue athletic activities despite pain and injury.
Clinicians can offer support by reinforcing the message that limiting physical activity is essential to recovery; it should not be compromised because of patient, parental, coach, or peer pressure. At the same time, it is important to recognize that a leave of absence from a competitive sport, no matter how short, can affect the patient’s mental health. If the patient feels angry or depressed about the diagnosis, mental health counseling options can be discussed.
Educating patients and parents about the numerous treatments for acute low back pain that have been proven to offer little benefit can be informative and reassuring. For example, adding spinal manipulation and chiropractic techniques to established medical treatments does not improve outcomes. Neither does the use of oral corticosteroids, acupuncture, massage, traction, or exercise programs. Bed rest should be avoided.23
Conclusion
In the primary care setting, low back pain is a common complaint with an extensive differential diagnosis. If a thorough history and physical examination prompt suspicion for spondylolysis or spondylolisthesis, x-rays will usually confirm the diagnosis. If the patient is referred to an orthopedic specialist, the primary care clinician can supplement and reinforce the treatment plan through patient and parent education about the diagnosis and its treatment. Compliance with conservative nonsurgical treatment may enable the patient to make a speedier return to his or her usual physical activities.
The authors would like to thank Jennifer Tareco, MD, and Robert More, MD, for their revisions and support in the completion of this article.
CE/CME No: CR-1410
PROGRAM OVERVIEW
Earn credit by reading this article and successfully completing the posttest and evaluation. Successful completion is defined as a cumulative score of at least 70% correct.
EDUCATIONAL OBJECTIVES
• Identify risk factors for the development of spondylolysis and spondylolisthesis
• Discuss the differential diagnoses associated with low back pain
• Describe physical examination findings consistent with spondylolysis and spondylolisthesis
• List the imaging modalities that may be used to confirm these diagnoses and explain the indications for each
• Identify when a pediatric patient with low back pain should be referred to an orthopedic or neurologic specialist for further evaluation and treatment
FACULTY
Shannon P. More is a pediatric nurse practitioner in New York City. Rita Marie John is a Professor at the Columbia University School of Nursing in New York City. The authors have no significant financial relationships to disclose.
ACCREDITATION STATEMENT
Article begins on next page >>
The most common causes of low back pain in adolescents, spondylolysis and spondylolisthesis can be tricky to diagnose. The primary care clinician plays a key role in optimal management so that full recovery, in most cases, is achieved.
Spondylolysis, the most common cause of low back pain in adolescents, occurs in approximately 8% to 14% of adolescent athletes.1 It is estimated that 15% to 25% of patients with spondylolysis will develop spondylolisthesis.2 This article discusses the definitions, pathophysiology, risk factors, differential diagnosis, and clinical presentation of spondylolysis and spondylolisthesis, including a review of diagnostic imaging, treatment, and the primary care clinician’s role in the optimal management of affected patients.
Spondylolysis is a congenital or acquired unilateral or bilateral defect in the portion of a vertebra—usually L5—called the pars interarticularis, the bony area between the superior and inferior articulating facets (see Figure 1a). Recurrent trauma, such as repeated flexion, hyperextension, or twisting, can weaken the pars interarticularis. During these movements, the inferior articular process of the cranial (upper) vertebra can come into contact with the pars interarticularis of the caudal (lower) vertebra. When this happens repeatedly, a stress reaction may occur in the pars interarticularis, which can result in a stress or complete nonunion fracture.
The paraspinal muscles around the lumbar spine may adjust to accommodate the weakened vertebra, resulting in postural alterations. This can predispose patients to further spinal injury because normal muscular control of that portion of the spine is impaired.3
When the break in the pars interarticularis causes slippage, or forward movement, of the upper vertebra (again, usually L5) over the vertebra (ie, S1) below it, spondylolisthesis occurs (see Figure 1b, above).2,4 This happens more frequently with bilateral spondylolysis and is often associated with an adolescent growth spurt.5
Spondylolisthesis can manifest anywhere in the spine but is most common in the lumbosacral region, with most (71% to 95%) cases occurring at L5 and the remainder at L4.6 Some patients develop these conditions spontaneously through strenuous activity or injury; others are predisposed but remain asymptomatic until the condition is exacerbated through athletic activities.
Wiltse first described spondylolisthesis in 1962 and 10 years later published a classification system based on etiology and anatomy; his research is still used today as the basis for diagnosis.7,8 The five types of spondylolisthesis are
• Type 1, dysplastic (congenital)
• Type 2, isthmic (defect in pars interarticularis)
• Type 3, degenerative (arthritic changes in older patients)
• Type 4, traumatic (acute injury)
• Type 5, pathologic (bone disease).8
Types 1 and 2 occur in pediatric patients, with 85% of such cases classified as type 2.4
The classification is further refined according to degree of severity, defined as the percentage of slippage of the upper over the lower vertebra. Grade 1 (first degree) entails a slippage of less than 25%; grade 2 (second degree), 26% to 50%; grade 3 (third degree), 51% to 75%; and grade 4 (fourth degree), greater than 75%.5
Risk Factors
In general, women are at greater risk for stress fractures than men are.9 Yet while pars interarticularis defects are twice as common in men as in women, women are more likely to progress to spondylolisthesis.10 Similarly, in patients with bilateral spondylolysis, women are significantly more likely than men (90.9% vs 66.2%) to develop spondylolisthesis.11 In general, those who repetitively hyperextend the lower back (eg, football players, rowers, dancers, gymnasts, soccer players, swimmers) are at increased risk for both spondylolysis and spondylolisthesis.
While a patient’s activities and environmental stressors play a role in the development of spondylolysis and spondylolisthesis, a genetic predisposition is believed to be a factor as well: A five-fold increase in the incidence of defects of the pars interarticularis has been noted in near relatives of patients with spondylolisthesis.7 In addition, patients with conditions such as spina bifida occulta, severe scoliosis, and osteogenesis imperfecta are at increased risk for these conditions.6,12
Differential DiagnosIs
Both spondylolysis and spondylolisthesis manifest as low back pain, for which the differential diagnosis is extensive. Pathologic causes of low back pain are much less common than causes related to structural weakness or trauma; however, carefully differentiating these is important so that pathology is identified promptly and treated appropriately.13
The differential diagnosis for low back pain in pediatric patients, by type of pain, includes
• Pain at night or with fever or other generalized symptoms: tumor or infection
• Acute pain: herniated disk, slipped apophysis, spondylolysis, vertebral fracture, or muscle strain
• Chronic pain: Scheuermann kyphosis, inflammatory spondyloarthropathies, or psychological problems
• Pain with spinal forward flexion: herniated disk or slipped apophysis
• Pain with spinal extension: spondylolysis, spondylolisthesis, or lesion or injury in the pedicle or lamina (posterior arch)
• Pain with recent-onset scoliosis: tumor, infection, herniated disk, syrinx, or idiopathic scoliosis
• Other pain: pyelonephritis or sickle cell crisis.13
Clinical Presentation
A systematic approach to a patient with a chief concern of low back pain is recommended. An initial assessment of the patient’s vital signs and growth parameters should be compared to those from previous visits to determine if there have been any changes in the usual pattern.
History
Use the standard HEEADSSS (Home, Education, Eating, Activities, Drugs, Sexuality, Suicide, Safety) adolescent psychosocial assessment as part of the patient history.14 In particular, focus on details about the physical activities and sports in which the patient participates and obtain data on the amount of time spent on each. When taking the family history, pay particular attention to any predisposition to musculoskeletal disorders. In the review of systems, note any history of traumatic injury.
Next, ask the patient to point with one finger to the location at which the pain is felt; in spondylolysis and spondylolisthesis, pain localizes to the waist. Obtain a detailed history of the pain, including onset, duration, frequency, location, and all alleviating or exacerbating factors.15
Physical examination
A brief summary of key features to assess during the physical examination is presented in Table 1. When completing the physical assessment, follow the typical head-to-toe approach, with special attention to evaluation of the presenting back pain.
Visual inspection. A visual inspection of the spine for scoliosis and kyphosis is key; also be sure to examine posture, assess symmetry, and observe for any midline defects.13 Hemangiomas, a line of hairy patches, or other abnormal markings along the body’s vertical axis may suggest an intraspinal anomaly.
Palpation. The entire spine should be palpated to confirm the location of the pain as identified by the patient. In particular, note if tenderness is felt over bony structures of the spine or in the paraspinal musculature.
Range of motion. After the locus of the pain is confirmed, instruct the patient to flex and extend the spine to assess for worsening pain. If noted, this finding is pathognomonic for spondylolysis and spondylolisthesis.13
Also useful for making the diagnosis is the one-leg hyperextension test, in which the patient is asked to raise one leg off the ground and lean backward. Pain elicited during this movement is indicative of back injury, including spondylolysis or spondylolisthesis. A positive result with the one-leg hyperextension test alone, however, is not a clinical marker for spondylolysis. Not only may the test elicit pain stemming from other pathologies, but the results are dependent on the patient’s subjective reporting of pain.16
Muscular signs and symptoms. Hamstring tightness is present in 80% of symptomatic patients.5 Consequently, the patient may have a somewhat waddling gait due to the inability to flex the hips and extend the knee simultaneously. For this reason, physical examination for spondylolysis and spondylolisthesis includes gait assessment. Other clinical signs of spondylolisthesis include a weak and drooping abdominal wall, paravertebral muscle hypertrophy, increased lumbar lordosis, hamstring muscle spasm, and pain during lateral trunk flexion/extension and double leg raising.17
Motor and sensory function. It is important to assess motor and sensory function to differentiate neurologic from orthopedic conditions. Deep tendon reflexes and lower extremity motor strength and sensory capabilities also need careful assessment.13 Sensation in the region of the cauda equinus requires further evaluation due to the possibility of cauda equinus compression. Hyperreflexia indicates an upper motor lesion, whereas hyporeflexia indicates a lower motor lesion—neither of which would be expected in spondylolisthesis or spondylolysis.
A patient with any positive neurologic signs should be referred to a neurologic specialist.
Diagnostic TESTING
Unfortunately, rigorous comparative research is lacking on which to base clinical practice guidelines for diagnosis (as well as treatment) of spondylolysis and spondylolisthesis.18 Nevertheless, current standards call for a detailed physical examination as an effective diagnostic tool and recommend radiologic evaluation for a definitive diagnosis.17,18 Lateral radiographs are also useful for identifying the degree of vertebral slippage when spondylolisthesis is diagnosed.17 The specialist may choose to utilize such diagnostic modalities as CT, single-photon-emission CT (SPECT), or MRI.
Radiologic evaluation
For complete radiologic evaluation, four x-ray views of the spine are necessary: anterior-posterior (AP), lateral, and bilateral oblique views. A fracture seen in the pars interarticularis is called the Scotty dog sign because it looks like a collar around the neck of a Scottish terrier (see Figures 2 and 3).2
Since treatment for nonspecific back pain and spondylolysis is essentially the same, it could be argued that radiographic imaging to confirm the clinical diagnosis exposes the patient to unnecessary radiation (a particular concern in the pediatric population). But a definitive diagnosis also rules out other pathologies that would require more aggressive treatment.
If x-rays reveal abnormalities, refer the patient to an orthopedic specialist for further evaluation. Referral to orthopedics should also be prompted if spondylolysis or spondylolisthesis is suspected but x-rays are insufficient to make the diagnosis.
CT and SPECT
Standaert and Herring suggest that CT combined with SPECT is the standard for diagnosis of a pars interarticularis lesion1; in many reported cases, CT test results may be negative even when SPECT results are abnormal, suggesting that both studies are needed. In other cases, CT can help identify the origin of an abnormality seen on SPECT.
The disadvantage to using both modalities is that the patient is exposed to additional ionizing radiation. If only one method is to be used, SPECT may be preferred; it exposes the patient to less ionizing radiation and seldom requires sedation.19
Magnetic resonance imaging
In terms of radiation exposure, MRI is preferred to CT and SPECT because it does not utilize ionizing radiation; unfortunately, it is also less effective at detection of spondylolysis and spondylolisthesis. A review of the literature indicates that MRI is not as sensitive as SPECT in identifying stress on the pars interarticularis.16,19
In general, MRI is superior for visualizing soft tissue pathology (eg, disk disease, nerve root compression, inflammation), while CT is superior for visualization of bone. In the context of back pain, MRI may be informative when etiologies other than spondylolysis and spondylolisthesis are suspected; Feldman et al recommend MRI for patients with constant back pain, radicular pain, nighttime pain, and/or abnormal neurologic examination results.16
The advantages and disadvantages of x-rays, SPECT, CT, and MRI for the diagnosis of spondylolysis and spondylolisthesis are summarized in Table 2.1,15,16,18,19
Laboratory studies
There are no laboratory tests to confirm the diagnosis of spondylolysis or spondylolisthesis. To eliminate other diagnoses, however, it is appropriate to order certain laboratory tests. In addition to radiographs, Bernstein and Cozen recommend a complete blood count, an erythrocyte sedimentation rate, and a C-reactive protein test as part of the diagnostic work-up if the history and physical are suspicious for underlying pathology, such as infection.13
Management and Treatment Options
Treatment for spondylolysis or spondylolisthesis ranges from basic strengthening programs to surgical intervention and is based on the severity of the patient’s condition. The goal is to alleviate symptoms and facilitate a return to normal activities. Treatment should be individualized based on the patient’s age, athletic level and demands, and severity of symptoms.10
Nonsurgical treatment
Conservative treatment options include rest, physical therapy, core strengthening, and antilordotic bracing for several months (eg, eight to 12 weeks).5 Most grade 1 and 2 cases can be successfully treated nonsurgically.
Studies of nonsurgical treatment of children and young adults with spondylolysis and/or mild spondylolisthesis (up to 25% slippage) were evaluated in a meta-analysis.20 The authors found that approximately 84% of such patients were pain free or nearly pain free with unrestricted activities within one year of treatment. While nonsurgical treatment does not usually resolve the pars interarticularis defect, it alleviates symptoms and enables the patient’s return to unrestricted activities. Further, the authors found no significant difference in outcomes between patients who were treated with or without bracing.20
In contrast, another study demonstrated that patients who wore braces achieved higher functional outcomes than those who did not.21 However, the patients who were braced were restricted from physical activity longer than were those who were not braced, so it could not be definitively determined if bracing or additional rest was the reason for the improved outcomes.
A significant limitation of bracing is that it is a restrictive and sometimes uncomfortable treatment, especially for an active child or adolescent. If clinicians can treat these patients effectively without bracing, greater compliance with treatment may result.
This study also found a strong correlation between early intervention and an increased incidence of bony healing. The researchers recommend the early use of sensitive diagnostic imaging so that treatment can begin early, increasing the possibility that the fracture will heal.20
Skeletally immature patients should be followed clinically at six-month to one-year intervals, including use of lateral x-rays for spinal evaluation, to ensure that progressive spondylolisthesis does not develop. Once skeletal development is complete, follow-up is no longer necessary because progressive spondylolisthesis is unlikely at or near skeletal maturity.10
Surgical treatment
When conservative treatment fails to alleviate the pediatric patient’s pain, if daily functioning is impaired, or if the spondylolisthesis is of a more severe grade or progresses, surgical correction to repair the pars interarticularis defect or laminectomy and spinal fusion may be necessary.5 Adolescent patients treated surgically are likely to have good long-term results but may still experience symptoms, including back pain, into adulthood.22 The procedure used in a particular case depends on the degree of severity and the patient’s specific presentation.
PRIMARY CARE IS KEY
As stated earlier, referral to an orthopedic specialist is indicated when spondylolysis or spondylolisthesis is suspected or confirmed or to a neurologic specialist when any neurologic signs are positive or deficits are noted. In these instances, the primary care clinician is key to early diagnosis and prompt treatment.
Primary health care practitioners are in a position to contribute to the management of spondylolysis or spondylolisthesis in a way that will help facilitate a full recovery. For example, the patient and parent or guardian should be counseled about the need for the child to refrain from athletic activity while awaiting an orthopedic or neurologic evaluation. Restriction of activity will prevent exacerbation of the injury and increased pain. Suggest OTC NSAIDs, taken with food to prevent gastrointestinal adverse effects, for pain relief.13
It can also be helpful to assess the patient’s psychosocial status to determine whether he or she might face barriers to recovery. Often a major obstacle in treating these conditions is pressure from parents, coaches, or the patients themselves to continue athletic activities despite pain and injury.
Clinicians can offer support by reinforcing the message that limiting physical activity is essential to recovery; it should not be compromised because of patient, parental, coach, or peer pressure. At the same time, it is important to recognize that a leave of absence from a competitive sport, no matter how short, can affect the patient’s mental health. If the patient feels angry or depressed about the diagnosis, mental health counseling options can be discussed.
Educating patients and parents about the numerous treatments for acute low back pain that have been proven to offer little benefit can be informative and reassuring. For example, adding spinal manipulation and chiropractic techniques to established medical treatments does not improve outcomes. Neither does the use of oral corticosteroids, acupuncture, massage, traction, or exercise programs. Bed rest should be avoided.23
Conclusion
In the primary care setting, low back pain is a common complaint with an extensive differential diagnosis. If a thorough history and physical examination prompt suspicion for spondylolysis or spondylolisthesis, x-rays will usually confirm the diagnosis. If the patient is referred to an orthopedic specialist, the primary care clinician can supplement and reinforce the treatment plan through patient and parent education about the diagnosis and its treatment. Compliance with conservative nonsurgical treatment may enable the patient to make a speedier return to his or her usual physical activities.
The authors would like to thank Jennifer Tareco, MD, and Robert More, MD, for their revisions and support in the completion of this article.
1. Standaert CJ, Herring SA. Expert opinion and controversies in sports and musculoskeletal medicine: the diagnosis and treatment of spondylolysis in adolescent athletes. Arch Phys Med Rehabil. 2007;88(4):537-540.
2. Spiegel DA, Dormans JP. Spondylolysis and spondylolisthesis. In: Kliegman RM, Stanton BF, Schor NF, St. Geme III JW, Behrman RE, eds. Nelson Textbook of Pediatrics. Philadelphia, PA: Elsevier; 2011:1561-1571.
3. Smith J. Moving beyond the neutral spine: stabilizing the dancer with lumbar extension dysfunction. J Dance Med Sci. 2009;13(3):73-82.
4. Hu SS, Tribus CB, Diab M, Ghanayem AJ. Spondylolisthesis and spondylolysis. J Bone Joint Surg Am. 2008;90(3):656-671.
5. Wicker A. Spondylolysis and spondylolisthesis in sports. Int Sports Med J. 2008;9(2):74-78.
6. McCleary MD, Congeni JA. Current concepts in the diagnosis and treatment of spondylolysis in young athletes. Curr Sports Med Rep. 2007; 6(1):62-66.
7. Wiltse LL. The etiology of spondylolisthesis. J Bone Joint Surg Am. 1962;44-A:539-560.
8. Wiltse LL, Newman PH, Macnab I. Classification of spondylolysis and spondylolisthesis. Clin Orthop Relat Res. 1976;117:23-29.
9. Ivkovic A, Franic M, Bojanic I, Pecina M. Overuse injuries in female athletes. Croat Med J. 2007;48:767-778.
10. Tallarico RA, Madom IA, Palumbo MA. Spondylolysis and spondylolisthesis in the athlete. Sports Med Arthrosc. 2008;16(1):32-38.
11. Takao S, Sakai T, Sairyo K, et al. Radiographic comparison between male and female patients with lumbar spondylolysis. J Med Invest. 2010;57 (1-2):133-137.
12. Hatz D, Esposito PW, Schroeder B, et al. The incidence of spondylolysis and spondylolisthesis in children with osteogenesis imperfecta. J Pediatr Orthop. 2011;31(6):655-660.
13. Bernstein RM, Cozen H. Evaluation of back pain in children and adolescents. Am Fam Physician. 2007;76(11):1669-1676.
14. Klein DA, Goldenring JM, Adelman WP. HEEADSSS 3.0: The psychosocial interview for adolescents updated for a new century fueled by media. Contemp Pediatr. 2014;1:16-28.
15. Feldman DS, Straight JJ, Badra MI, et al. Evaluation of an algorithmic approach to pediatric back pain. J Pediatr Orthop. 2006;26(3):353-357.
16. Masci L, Pike J, Malara F, et al. Use of the one-legged hyperextension test and magnetic resonance imaging in the diagnosis of active spondylolysis. Br J Sports Med. 2006;40(11):940-946.
17. Kalpakcioglu B, Altinbilek T, Senel K. Determination of spondylolisthesis in low back pain by clinical evaluation. J Back Musculoskelet Rehabil. 2009;22(1):27-32.
18. Bhatia NN, Chow G, Timon SJ, Watts HG. Diagnostic modalities for the evaluation of pediatric back pain: a prospective study. J Pediatr Orthop. 2008;28(2):230-233.
19. Zukotynski K, Curtis C, Grant FD, et al. The value of SPECT in the detection of stress injury to the pars interarticularis in patients with low back pain. J Orthop Surg Res. 2010;5(13):1-6.
20. Klein G, Mehlman CT, McCarty M. Nonoperative treatment of spondylolysis and grade I spondylolisthesis in children and young adults. J Pediatr Orthop. 2009;29(2):146-156.
21. Alvarez-Diaz P, Alentorn-Geli E, Steinbacher G, et al. Conservative treatment of lumbar spondylolysis in young soccer players. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2111-2114.
22. Helenius I, Remes V, Lamberg T, et al. Long-term health-related quality of life after surgery for adolescent idiopathic scoliosis and spondylolisthesis. J Bone Joint Surg Am. 2008;90(6):1231-1239.
23. Casazza BA. Diagnosis and treatment of acute low back pain. Am Fam Physician. 2012;85(4):343-350.
1. Standaert CJ, Herring SA. Expert opinion and controversies in sports and musculoskeletal medicine: the diagnosis and treatment of spondylolysis in adolescent athletes. Arch Phys Med Rehabil. 2007;88(4):537-540.
2. Spiegel DA, Dormans JP. Spondylolysis and spondylolisthesis. In: Kliegman RM, Stanton BF, Schor NF, St. Geme III JW, Behrman RE, eds. Nelson Textbook of Pediatrics. Philadelphia, PA: Elsevier; 2011:1561-1571.
3. Smith J. Moving beyond the neutral spine: stabilizing the dancer with lumbar extension dysfunction. J Dance Med Sci. 2009;13(3):73-82.
4. Hu SS, Tribus CB, Diab M, Ghanayem AJ. Spondylolisthesis and spondylolysis. J Bone Joint Surg Am. 2008;90(3):656-671.
5. Wicker A. Spondylolysis and spondylolisthesis in sports. Int Sports Med J. 2008;9(2):74-78.
6. McCleary MD, Congeni JA. Current concepts in the diagnosis and treatment of spondylolysis in young athletes. Curr Sports Med Rep. 2007; 6(1):62-66.
7. Wiltse LL. The etiology of spondylolisthesis. J Bone Joint Surg Am. 1962;44-A:539-560.
8. Wiltse LL, Newman PH, Macnab I. Classification of spondylolysis and spondylolisthesis. Clin Orthop Relat Res. 1976;117:23-29.
9. Ivkovic A, Franic M, Bojanic I, Pecina M. Overuse injuries in female athletes. Croat Med J. 2007;48:767-778.
10. Tallarico RA, Madom IA, Palumbo MA. Spondylolysis and spondylolisthesis in the athlete. Sports Med Arthrosc. 2008;16(1):32-38.
11. Takao S, Sakai T, Sairyo K, et al. Radiographic comparison between male and female patients with lumbar spondylolysis. J Med Invest. 2010;57 (1-2):133-137.
12. Hatz D, Esposito PW, Schroeder B, et al. The incidence of spondylolysis and spondylolisthesis in children with osteogenesis imperfecta. J Pediatr Orthop. 2011;31(6):655-660.
13. Bernstein RM, Cozen H. Evaluation of back pain in children and adolescents. Am Fam Physician. 2007;76(11):1669-1676.
14. Klein DA, Goldenring JM, Adelman WP. HEEADSSS 3.0: The psychosocial interview for adolescents updated for a new century fueled by media. Contemp Pediatr. 2014;1:16-28.
15. Feldman DS, Straight JJ, Badra MI, et al. Evaluation of an algorithmic approach to pediatric back pain. J Pediatr Orthop. 2006;26(3):353-357.
16. Masci L, Pike J, Malara F, et al. Use of the one-legged hyperextension test and magnetic resonance imaging in the diagnosis of active spondylolysis. Br J Sports Med. 2006;40(11):940-946.
17. Kalpakcioglu B, Altinbilek T, Senel K. Determination of spondylolisthesis in low back pain by clinical evaluation. J Back Musculoskelet Rehabil. 2009;22(1):27-32.
18. Bhatia NN, Chow G, Timon SJ, Watts HG. Diagnostic modalities for the evaluation of pediatric back pain: a prospective study. J Pediatr Orthop. 2008;28(2):230-233.
19. Zukotynski K, Curtis C, Grant FD, et al. The value of SPECT in the detection of stress injury to the pars interarticularis in patients with low back pain. J Orthop Surg Res. 2010;5(13):1-6.
20. Klein G, Mehlman CT, McCarty M. Nonoperative treatment of spondylolysis and grade I spondylolisthesis in children and young adults. J Pediatr Orthop. 2009;29(2):146-156.
21. Alvarez-Diaz P, Alentorn-Geli E, Steinbacher G, et al. Conservative treatment of lumbar spondylolysis in young soccer players. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2111-2114.
22. Helenius I, Remes V, Lamberg T, et al. Long-term health-related quality of life after surgery for adolescent idiopathic scoliosis and spondylolisthesis. J Bone Joint Surg Am. 2008;90(6):1231-1239.
23. Casazza BA. Diagnosis and treatment of acute low back pain. Am Fam Physician. 2012;85(4):343-350.