User login
Erythematous Verrucous Plaque on the Hand
The Diagnosis: Chromomycosis
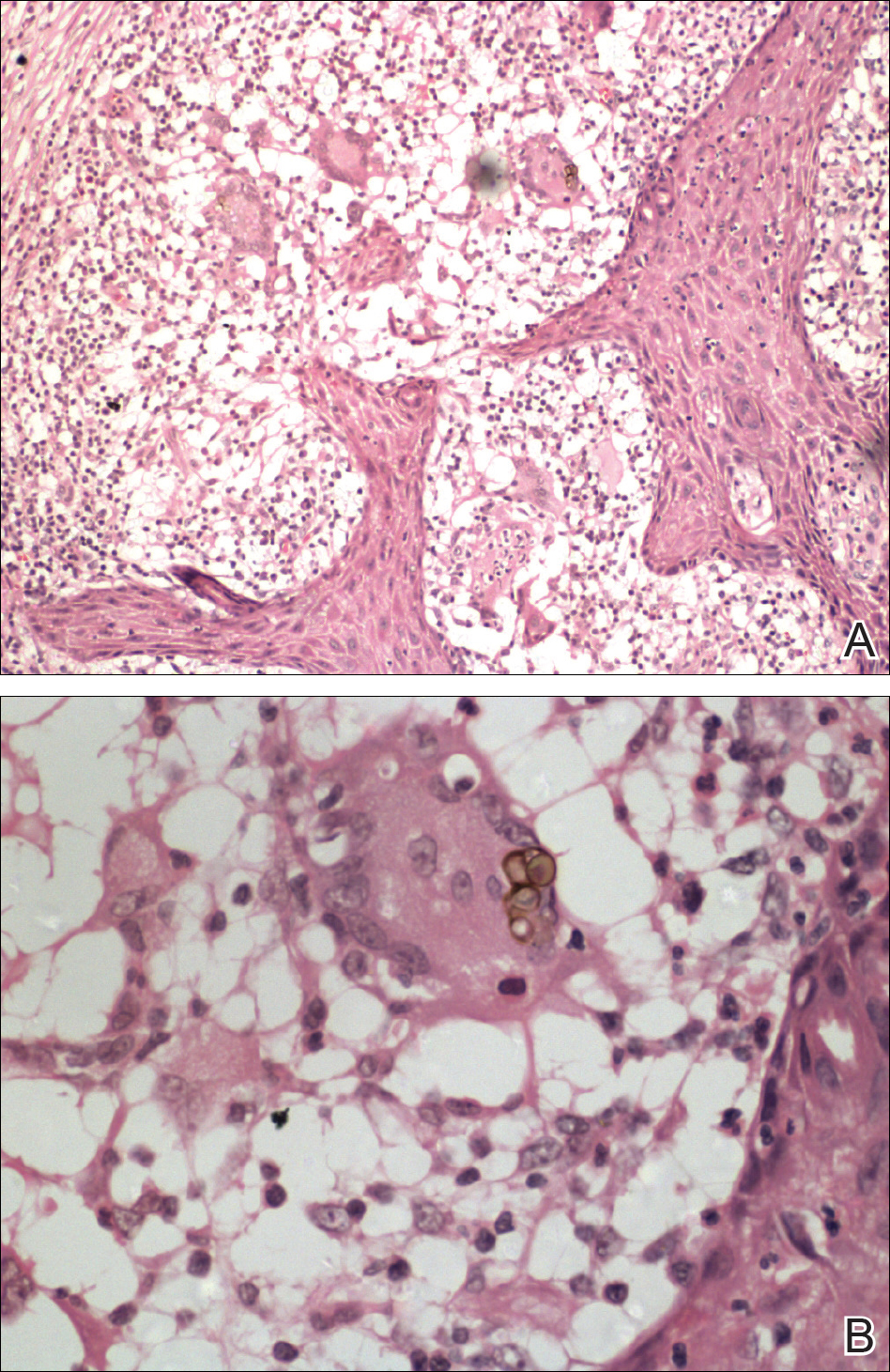
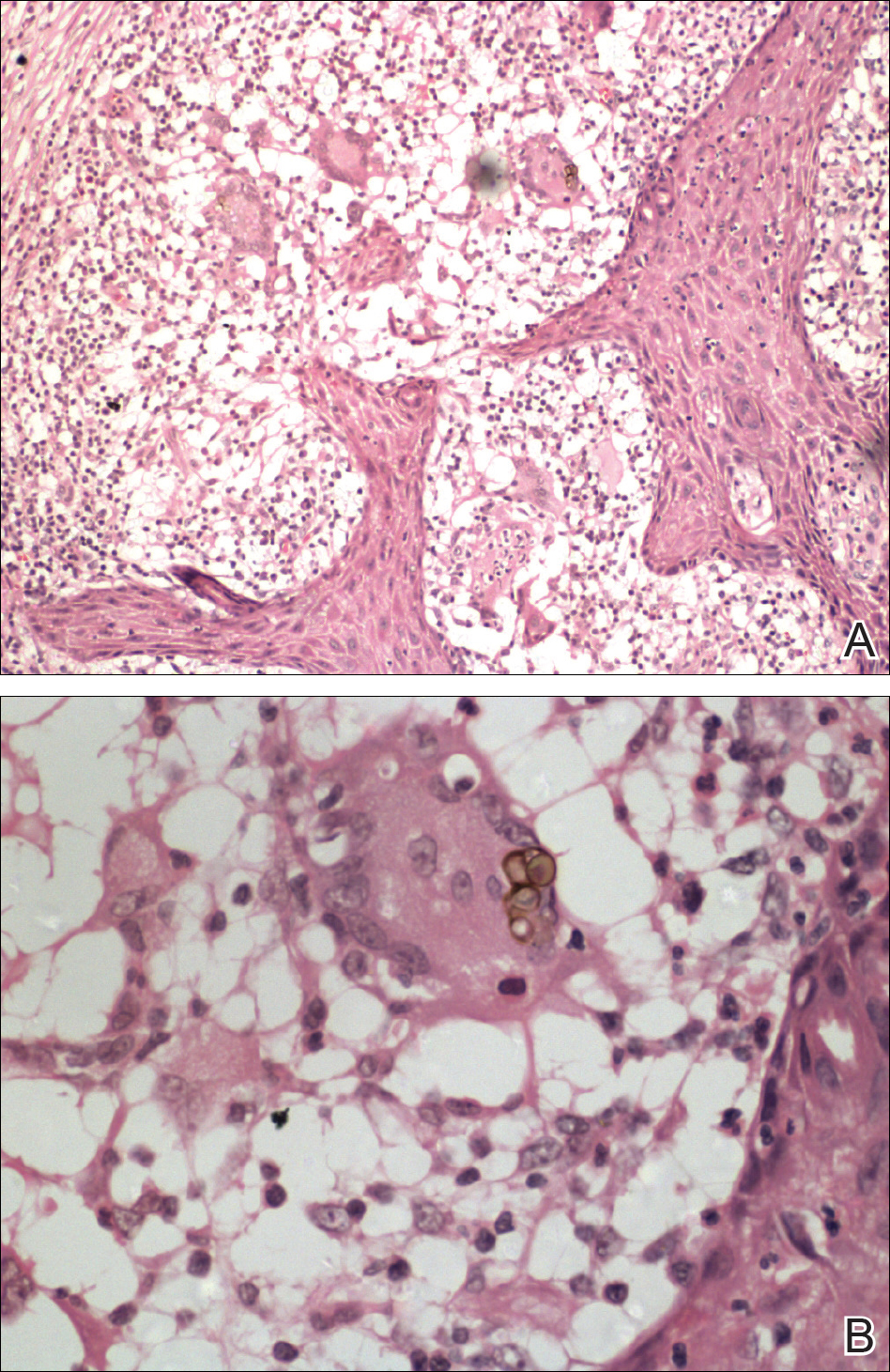
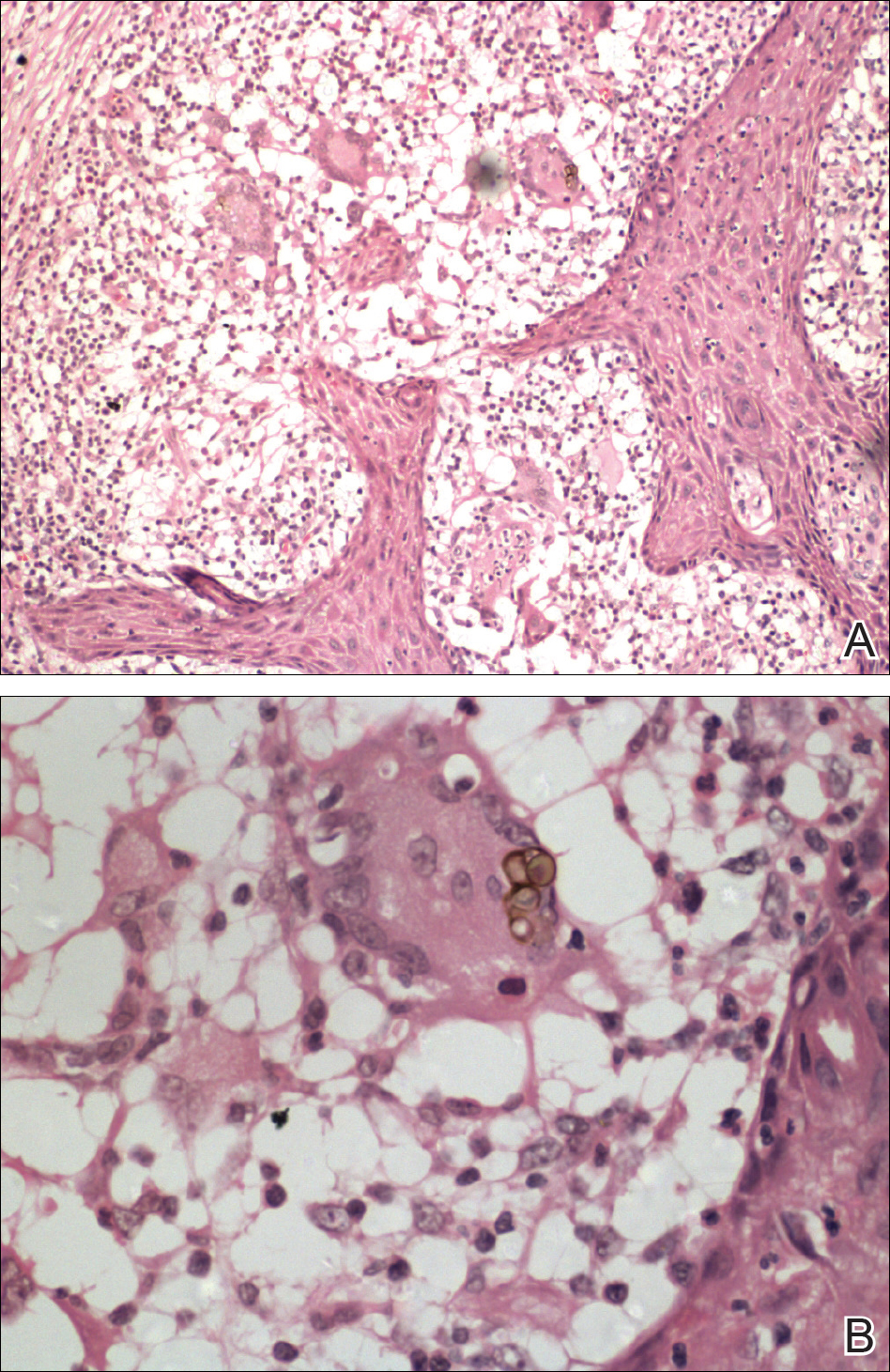
Skin scrapings revealed brownish sclerotic bodies. A review of the skin biopsy performed 4 years prior showed florid pseudoepitheliomatous hyperplasia overlying dense mixed inflammatory infiltrates of predominantly granulomatous microabscesses in the dermis. Numerous sclerotic bodies were evident within multinucleated giant cells and scattered among epidermal and dermal microabscesses (Figure). Few atypical basal keratinocytes were noted, but frank pleomorphism and aberrant mitosis was absent.
Chromomycosis is a chronic subcutaneous fungal infection caused by pigmented (dematiaceous) fungi growing in soil, decaying vegetables, and rotting wood. Infection usually occurs via traumatic inoculation from splinters and thorns. Some of the agents responsible include Fonsecaea pedrosoi, Cladophialophora carrionii, and Phialophora verrucosa.1
Diverse cutaneous manifestations have been observed with 5 different clinical forms: nodules, verrucous hyperkeratotic plaques, cicatricial lesions with central sparing, scaly plaques, and tumoral (cauliflowerlike) lesions.2 Of these clinical presentations, verrucous hyperkeratotic plaques are the most common, as seen in our patient. However, this presentation is not exclusive to chromomycosis because many conditions appear similarly, including sporotrichosis, nontuberculous mycobacterial infection, tuberculosis verrucosa cutis, and squamous cell carcinoma (SCC). The presence of small ulcerations may appear as the black dots seen on the plaques of chromomycosis, distinguishing chromomycosis from other conditions. Although this feature may be a fundamental clue for diagnosis, it should be emphasized that in many occasions, clinical differences between chromomycosis and its differentials are subtle. A study involving 9 patients with chromomycosis reported that only 1 was given the initial diagnosis of mycosis. Six patients initially were diagnosed with cutaneous malignancies, 1 patient with viral warts, and another patient with ganglion.3 Therefore, unless there is a high index of suspicion, these conditions may easily be mistaken for others by clinicians who are unfamiliar with their presentations, particularly in the setting of a busy clinic.
Chromomycosis routinely is diagnosed based on histologic examination and culture. Apart from sclerotic bodies, other histopathologic features include an inflammatory infiltrate characterized by neutrophilic microabscesses, multinucleated cells, fibrosis, acanthosis, papillomatosis, hyperkeratosis, and pseudoepitheliomatous hyperplasia (PEH).2 Pseudoepitheliomatous hyperplasia is an exaggerated proliferation of the epidermis, usually secondary to chronic inflammatory skin conditions.4 Because most verrucous lesions are thought to be neoplastic and carcinomas more commonly are seen and expected in dermatopathology, PEH can sometimes be mistaken for SCC. At times, the squamous epithelium of PEH can appear infiltrative, giving the illusion of well-differentiated SCC.5 However, absence of marked cellular atypia and abnormal mitotic activity should suggest otherwise. Thorough scrutiny for a concomitant infective process is necessary to avoid the overdiagnosis of SCC. Special stains for infectious agents such as periodic acid-Schiff and Grocott-Gomori methenamine-silver for fungal spores and Ziehl-Neelsen for acid-fast bacilli may reveal infectious organisms. Multilevel sections of deeper levels also may be essential to uncover sparse organisms.6
There is no standard treatment of chromomycosis. Some treatment options are available based on few open clinical studies and expert opinions. Systemic antifungals such as itraconazole or terbinafine most commonly are used with 15% to 80% cure rates.7 In invasive refractory cases, a combination of itraconazole and terbinafine has been employed as salvage therapy. Recently, the use of newer azoles such as posaconazole is favored due to its expanded-spectrum profile along with better pharmacodynamics and pharmacokinetic profile versus itraconazole. Physical methods such as cryotherapy, heat therapy, laser therapy, and photodynamic therapy frequently are practiced in conjunction with systemic antifungal therapy.8 Surgical procedures such as photocoagulation, Mohs micrographic surgery, and curettage sometimes are recommended for smaller well-defined lesions. Amputation, however, is rarely ever indicated, as there rarely is deep tissue involvement.2
Our case highlights the importance of clinicopathologic correlation in diagnosing squamous epithelial lesions. A high index of clinical suspicion and a wider list of differential diagnoses of verrucous plaques are necessary to minimize pitfalls in diagnosing lesions with squamous proliferation and therefore reduces the need for unnecessary interventions.
- Queiroz-Telles F, Esterre P, Perez-Blanco M, et al. Chromoblastomycosis: an overview of clinical manifestations, diagnosis and treatment. Med Mycol. 2009;47:3-15.
- Krzyściak PM, Pindycka-Piaszczyńska M, Piaszczyński M. Chromoblastomycosis. Postepy Dermatol Allergol. 2014;31:310-321.
- Jayalakshmi P, Looi LM, Soo-Hoo TS. Chromoblastomycosis in Malaysia. Mycopathologica. 1990;109:27-31.
- Zayour M, Lazova R. Pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2011;33:112-126.
- El-Khoury J, Kibbi AG, Abbas O. Mucocutaneous pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2012;34:165-175.
- Tan KB, Tan SH, Aw DC, et al. Simulators of squamous cell carcinoma of the skin: diagnostic challenges on small biopsies and clinicopathological correlation [published online June 25, 2013]. J Skin Cancer. 2013;2013:752864.
- Queiroz-Telles F, Santos DW. Challenges in the therapy of chromoblastomycosis. Mycopathologia. 2013;175:477-488.
- Queiroz-Telles F, de Hoog S, Santos DW, et al. Chromoblastomycosis. Clin Microbiol Rev. 2017;30:233-276.
The Diagnosis: Chromomycosis
Skin scrapings revealed brownish sclerotic bodies. A review of the skin biopsy performed 4 years prior showed florid pseudoepitheliomatous hyperplasia overlying dense mixed inflammatory infiltrates of predominantly granulomatous microabscesses in the dermis. Numerous sclerotic bodies were evident within multinucleated giant cells and scattered among epidermal and dermal microabscesses (Figure). Few atypical basal keratinocytes were noted, but frank pleomorphism and aberrant mitosis was absent.
Chromomycosis is a chronic subcutaneous fungal infection caused by pigmented (dematiaceous) fungi growing in soil, decaying vegetables, and rotting wood. Infection usually occurs via traumatic inoculation from splinters and thorns. Some of the agents responsible include Fonsecaea pedrosoi, Cladophialophora carrionii, and Phialophora verrucosa.1
Diverse cutaneous manifestations have been observed with 5 different clinical forms: nodules, verrucous hyperkeratotic plaques, cicatricial lesions with central sparing, scaly plaques, and tumoral (cauliflowerlike) lesions.2 Of these clinical presentations, verrucous hyperkeratotic plaques are the most common, as seen in our patient. However, this presentation is not exclusive to chromomycosis because many conditions appear similarly, including sporotrichosis, nontuberculous mycobacterial infection, tuberculosis verrucosa cutis, and squamous cell carcinoma (SCC). The presence of small ulcerations may appear as the black dots seen on the plaques of chromomycosis, distinguishing chromomycosis from other conditions. Although this feature may be a fundamental clue for diagnosis, it should be emphasized that in many occasions, clinical differences between chromomycosis and its differentials are subtle. A study involving 9 patients with chromomycosis reported that only 1 was given the initial diagnosis of mycosis. Six patients initially were diagnosed with cutaneous malignancies, 1 patient with viral warts, and another patient with ganglion.3 Therefore, unless there is a high index of suspicion, these conditions may easily be mistaken for others by clinicians who are unfamiliar with their presentations, particularly in the setting of a busy clinic.
Chromomycosis routinely is diagnosed based on histologic examination and culture. Apart from sclerotic bodies, other histopathologic features include an inflammatory infiltrate characterized by neutrophilic microabscesses, multinucleated cells, fibrosis, acanthosis, papillomatosis, hyperkeratosis, and pseudoepitheliomatous hyperplasia (PEH).2 Pseudoepitheliomatous hyperplasia is an exaggerated proliferation of the epidermis, usually secondary to chronic inflammatory skin conditions.4 Because most verrucous lesions are thought to be neoplastic and carcinomas more commonly are seen and expected in dermatopathology, PEH can sometimes be mistaken for SCC. At times, the squamous epithelium of PEH can appear infiltrative, giving the illusion of well-differentiated SCC.5 However, absence of marked cellular atypia and abnormal mitotic activity should suggest otherwise. Thorough scrutiny for a concomitant infective process is necessary to avoid the overdiagnosis of SCC. Special stains for infectious agents such as periodic acid-Schiff and Grocott-Gomori methenamine-silver for fungal spores and Ziehl-Neelsen for acid-fast bacilli may reveal infectious organisms. Multilevel sections of deeper levels also may be essential to uncover sparse organisms.6
There is no standard treatment of chromomycosis. Some treatment options are available based on few open clinical studies and expert opinions. Systemic antifungals such as itraconazole or terbinafine most commonly are used with 15% to 80% cure rates.7 In invasive refractory cases, a combination of itraconazole and terbinafine has been employed as salvage therapy. Recently, the use of newer azoles such as posaconazole is favored due to its expanded-spectrum profile along with better pharmacodynamics and pharmacokinetic profile versus itraconazole. Physical methods such as cryotherapy, heat therapy, laser therapy, and photodynamic therapy frequently are practiced in conjunction with systemic antifungal therapy.8 Surgical procedures such as photocoagulation, Mohs micrographic surgery, and curettage sometimes are recommended for smaller well-defined lesions. Amputation, however, is rarely ever indicated, as there rarely is deep tissue involvement.2
Our case highlights the importance of clinicopathologic correlation in diagnosing squamous epithelial lesions. A high index of clinical suspicion and a wider list of differential diagnoses of verrucous plaques are necessary to minimize pitfalls in diagnosing lesions with squamous proliferation and therefore reduces the need for unnecessary interventions.
The Diagnosis: Chromomycosis
Skin scrapings revealed brownish sclerotic bodies. A review of the skin biopsy performed 4 years prior showed florid pseudoepitheliomatous hyperplasia overlying dense mixed inflammatory infiltrates of predominantly granulomatous microabscesses in the dermis. Numerous sclerotic bodies were evident within multinucleated giant cells and scattered among epidermal and dermal microabscesses (Figure). Few atypical basal keratinocytes were noted, but frank pleomorphism and aberrant mitosis was absent.
Chromomycosis is a chronic subcutaneous fungal infection caused by pigmented (dematiaceous) fungi growing in soil, decaying vegetables, and rotting wood. Infection usually occurs via traumatic inoculation from splinters and thorns. Some of the agents responsible include Fonsecaea pedrosoi, Cladophialophora carrionii, and Phialophora verrucosa.1
Diverse cutaneous manifestations have been observed with 5 different clinical forms: nodules, verrucous hyperkeratotic plaques, cicatricial lesions with central sparing, scaly plaques, and tumoral (cauliflowerlike) lesions.2 Of these clinical presentations, verrucous hyperkeratotic plaques are the most common, as seen in our patient. However, this presentation is not exclusive to chromomycosis because many conditions appear similarly, including sporotrichosis, nontuberculous mycobacterial infection, tuberculosis verrucosa cutis, and squamous cell carcinoma (SCC). The presence of small ulcerations may appear as the black dots seen on the plaques of chromomycosis, distinguishing chromomycosis from other conditions. Although this feature may be a fundamental clue for diagnosis, it should be emphasized that in many occasions, clinical differences between chromomycosis and its differentials are subtle. A study involving 9 patients with chromomycosis reported that only 1 was given the initial diagnosis of mycosis. Six patients initially were diagnosed with cutaneous malignancies, 1 patient with viral warts, and another patient with ganglion.3 Therefore, unless there is a high index of suspicion, these conditions may easily be mistaken for others by clinicians who are unfamiliar with their presentations, particularly in the setting of a busy clinic.
Chromomycosis routinely is diagnosed based on histologic examination and culture. Apart from sclerotic bodies, other histopathologic features include an inflammatory infiltrate characterized by neutrophilic microabscesses, multinucleated cells, fibrosis, acanthosis, papillomatosis, hyperkeratosis, and pseudoepitheliomatous hyperplasia (PEH).2 Pseudoepitheliomatous hyperplasia is an exaggerated proliferation of the epidermis, usually secondary to chronic inflammatory skin conditions.4 Because most verrucous lesions are thought to be neoplastic and carcinomas more commonly are seen and expected in dermatopathology, PEH can sometimes be mistaken for SCC. At times, the squamous epithelium of PEH can appear infiltrative, giving the illusion of well-differentiated SCC.5 However, absence of marked cellular atypia and abnormal mitotic activity should suggest otherwise. Thorough scrutiny for a concomitant infective process is necessary to avoid the overdiagnosis of SCC. Special stains for infectious agents such as periodic acid-Schiff and Grocott-Gomori methenamine-silver for fungal spores and Ziehl-Neelsen for acid-fast bacilli may reveal infectious organisms. Multilevel sections of deeper levels also may be essential to uncover sparse organisms.6
There is no standard treatment of chromomycosis. Some treatment options are available based on few open clinical studies and expert opinions. Systemic antifungals such as itraconazole or terbinafine most commonly are used with 15% to 80% cure rates.7 In invasive refractory cases, a combination of itraconazole and terbinafine has been employed as salvage therapy. Recently, the use of newer azoles such as posaconazole is favored due to its expanded-spectrum profile along with better pharmacodynamics and pharmacokinetic profile versus itraconazole. Physical methods such as cryotherapy, heat therapy, laser therapy, and photodynamic therapy frequently are practiced in conjunction with systemic antifungal therapy.8 Surgical procedures such as photocoagulation, Mohs micrographic surgery, and curettage sometimes are recommended for smaller well-defined lesions. Amputation, however, is rarely ever indicated, as there rarely is deep tissue involvement.2
Our case highlights the importance of clinicopathologic correlation in diagnosing squamous epithelial lesions. A high index of clinical suspicion and a wider list of differential diagnoses of verrucous plaques are necessary to minimize pitfalls in diagnosing lesions with squamous proliferation and therefore reduces the need for unnecessary interventions.
- Queiroz-Telles F, Esterre P, Perez-Blanco M, et al. Chromoblastomycosis: an overview of clinical manifestations, diagnosis and treatment. Med Mycol. 2009;47:3-15.
- Krzyściak PM, Pindycka-Piaszczyńska M, Piaszczyński M. Chromoblastomycosis. Postepy Dermatol Allergol. 2014;31:310-321.
- Jayalakshmi P, Looi LM, Soo-Hoo TS. Chromoblastomycosis in Malaysia. Mycopathologica. 1990;109:27-31.
- Zayour M, Lazova R. Pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2011;33:112-126.
- El-Khoury J, Kibbi AG, Abbas O. Mucocutaneous pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2012;34:165-175.
- Tan KB, Tan SH, Aw DC, et al. Simulators of squamous cell carcinoma of the skin: diagnostic challenges on small biopsies and clinicopathological correlation [published online June 25, 2013]. J Skin Cancer. 2013;2013:752864.
- Queiroz-Telles F, Santos DW. Challenges in the therapy of chromoblastomycosis. Mycopathologia. 2013;175:477-488.
- Queiroz-Telles F, de Hoog S, Santos DW, et al. Chromoblastomycosis. Clin Microbiol Rev. 2017;30:233-276.
- Queiroz-Telles F, Esterre P, Perez-Blanco M, et al. Chromoblastomycosis: an overview of clinical manifestations, diagnosis and treatment. Med Mycol. 2009;47:3-15.
- Krzyściak PM, Pindycka-Piaszczyńska M, Piaszczyński M. Chromoblastomycosis. Postepy Dermatol Allergol. 2014;31:310-321.
- Jayalakshmi P, Looi LM, Soo-Hoo TS. Chromoblastomycosis in Malaysia. Mycopathologica. 1990;109:27-31.
- Zayour M, Lazova R. Pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2011;33:112-126.
- El-Khoury J, Kibbi AG, Abbas O. Mucocutaneous pseudoepitheliomatous hyperplasia: a review. Am J Dermatopathol. 2012;34:165-175.
- Tan KB, Tan SH, Aw DC, et al. Simulators of squamous cell carcinoma of the skin: diagnostic challenges on small biopsies and clinicopathological correlation [published online June 25, 2013]. J Skin Cancer. 2013;2013:752864.
- Queiroz-Telles F, Santos DW. Challenges in the therapy of chromoblastomycosis. Mycopathologia. 2013;175:477-488.
- Queiroz-Telles F, de Hoog S, Santos DW, et al. Chromoblastomycosis. Clin Microbiol Rev. 2017;30:233-276.

A 75-year-old retired farmer presented with an erythematous verrucous plaque on the dorsal aspect of the left hand of 4 years' duration. Superficial biopsies from the lesion 4 years prior to presentation revealed pseudoepitheliomatous hyperplasia suggestive of squamous cell carcinoma, which led to the excision of the lesion along with 2 digits of the left hand. Despite surgery, the lesions promptly recurred and continued to progress. Physical examination revealed a verrucous plaque with crusting and small ulcerations (black dots) over the extensor aspect of the left hand and forearm.
