User login
Team Rapid
The origin of the RRT can be found in medical emergency teams (METs). METs began in Australia as a result of the realization that earlier intervention could lead to better outcomes.1 In December 2004, in response to persistent problems with patient safety, the Institute for Healthcare Improvement launched its “100,000 Lives Campaign.”2 The Institute’s key plan for saving some of these 100,000 lives was to create RRTs at every participating medical center. Participating facilities would also submit data on mortality.
Olive View-UCLA Medical Center (OV-UCLA) signed on to participate in the campaign, and part of that effort was the creation and implementation of an RRT. We joined a University Health Consortium “Commit to Action” team, which assisted us by providing support as we began the creation and implementation of the RRT. What follows is the story of how we created an RRT.
We chose team members from all disciplines that were to be part of the RRT response—both at and behind the scenes: RNs, nursing administrators, hospital administrators, ICU attendings, house staff, laboratory personnel, nursing educators, radiology technicians, and hospital operators. The group was further organized into specific teams to solve problems and present solutions. At this point we learned our first important lesson: We needed to meet individually with all inpatient department chairs to discuss the effect of RRTs.
Activation and Notification
How would the RRT call be activated—overhead or beeper? Who could call, and what would the indications be? The OV-UCLA activation and notification team decided that the RRT could be activated by any staff member. Criteria, including vital signs, mental status, or simply “concern about the patient,” were created and posted. A telephone line in the ICU (X4415) was dedicated for RRT calls, and all other activation was overhead due to the lack of an adequate beeper system. (Other than code pagers, our beeper system can’t be simultaneously activated, and ancillaries don’t have beepers.)
The primary nurse’s responsibilities included calling the primary team or cross-covering team and obtaining a fingerstick glucose on all patients while waiting for the team. In discussions the primary team, we learned our second important lesson: As we presented the RRT to the hospital staff, everyone was concerned about the primary team. Ensuring that a mechanism for notifying the primary team was in place and reassuring staff that the primary team would be involved emerged as essential tasks. It was also imperative to identify the chain of command.
With this need in mind, we decided the primary team would always be the captain and would, therefore, have the authority to dismiss whomever they wanted from the RRT. An ICU attending was assigned to RRT call as supervision for the ICU resident responder. At OV-UCLA, our attending is not in-house and, to date, has not been called.
Documentation
The OV-UCLA documentation team was called on to answer the following questions: How would the RRT call be documented? How would medication orders be sent to the pharmacy? How would quality indicators (QI) and data be collected on the calls?
The team’s solution involved creating a one-page, primarily check-based document. The ICU nurse who answered the X4415 telephone in the ICU would begin documentation, which included the time of the call and the chief complaint. When the RRT reached the patient, however, the documentation duties were transferred to the primary RN. All providers were to document on the same page—similar to a code sheet. The RRT nurse and the attending doctor were to check vitals and perform the physical exam, as all information was called out to the documenter.
Medications were to be verbally ordered by the doctor, then read back and verified by the nurses documenting and administering for the RRT. For the most part, medication orders were restricted to what was carried in the RRT bag. The document was eventually copied three times: The original was placed in the chart, one copy was sent to the pharmacy for a record of medication, and the other was saved for QI. The primary team was expected to write a note in the chart’s disposition and time of disposition were to be included in this message.
Equipment
The OV-UCLA equipment team had one important question to answer: What supplies did we need at the bedside?
Although equipment and medications are readily available outside the ICU, the team didn’t want to spend time looking for equipment during an RRT call. “I don’t want a quick RRT call to evolve into a three-hour scavenger hunt,” says one team member.
Because OV-UCLA does not have a 24-hour pharmacist, the group felt it essential to bring medications to the bedside to avoid delays. Our solution to this potential problem was simple. The medication box is prepared by the pharmacy and sealed with one expiration date. Once the box is opened, it is exchanged for a new sealed box. The team chose a rolling duffle to store and transport the supplies, which are compartmentalized into the following sections: infection control, medications, airway and respiratory, IV access and blood draw, and IV start. Medications include respiratory treatments, antibiotics, furosemide, nitroglycerin, metoprolol, heparin and low molecular weight heparin, naloxone, ephedrine, dopamine, glucose, glucagons, and so on. The bag is restocked upon its return to the ICU.
Because of the stress involved in maintaining emergency equipment, we opted to call the supplies a “convenience bag.” This label ensured that only the sealed medication box would require a mandatory check; the rest of the equipment would be monitored on a more informal basis. Because all equipment is available on every floor, and because any RRT call can be converted to a code blue, the team felt that this was reasonable. The committee also purchased a five-pound patient monitor that has a screen for a cardiac tracing, a pulse oximeter, a noninvasive blood pressure monitor, and a temperature probe. This monitor fits easily in a pocket of the duffle.
Education and Publicity
How would staff know to call the RRT? The OV-UCLA team, anticipating that the majority of RRT calls would be activated by the primary RNs, decided that educating all nursing staff was essential.
The hospital nursing education office trained all nurses on all shifts in a short period of time. All nursing staff were taught to use SBAR (situation, background, assessment, and recommendation) communication and to identify early warning signs.1 The importance of recognizing the early warning signs was stressed during the nursing and physician training sessions. Staff were reassured that they didn’t have to know what was wrong with the patient to know that something was wrong and that help was required.
Publicity was accomplished in a variety of ways. The facility purchased pencils in our official color—lime green—that said “Rapid Response Team X4415.” The duffle was wheeled to all nursing stations so that staff could see it. We also ordered custom green-and-white M&M candy (available at www.mms.com) labeled “RRT X4415” to give as a promotional gift when an RRT was called.
Staffing
One last question remained for our team members: Who would respond to the RRT?
The committee felt strongly that an ICU nurse, an ICU resident, and a respiratory therapist should respond. Many physicians on the team did not want a doctor to respond, mostly due to concerns over chain of command. Who would be responsible for decisions made by the RRT? What if an ICU R2 disagreed with a surgery R4? Could they write a “do not call RRT order?” Nursing, on the other hand, wanted physician response; they wanted to be able to stabilize the patient.
Standardized protocols were discussed, but the team felt that the they would unreasonably delay the start. Radiology, which has no code blue response, volunteered to respond to all calls and hand-deliver the film to a computerized viewing system. The lab volunteered to run all RRT labs—designated with a lime green sticker—as quickly as possible.
The medical staff wanted to pilot the RRT, but because we are a small facility (220 beds) and to avoid confusion we launched the RRT for all inpatients. We went live in October 2005. The original plan was to staff an ICU nurse/RRT position. This RRT RN would relieve ICU nurses for breaks to maintain staffing ratios and provide RRT coverage. Because of the omnipresent nursing shortage, however, the RRT position is often pulled and the charge nurse must cover calls. Nurses sign up for RRT overtime and get pulled for patient care duties.
Mock RRT Calls
We performed three RRT drills to determine problem areas. For the first call, we involved a physician who had been vocal about the need for an RRT. The call was for a patient with shortness of breath. Two problems occurred during this drill: The primary team was never called, and there was no overhead page. So a member of our team worked with the hospital operator on our committee and clarified our protocols.
At the second drill, the main problem was documentation. The ICU nurse was so busy documenting that he wasn’t involved with the patient. Because the expertise of the ICU nurse is essential (in fact, there are times when this RN is the most experienced person on the team) we restructured the response so that the primary nurse would document and the ICU nurse was free to provide the hands-on care required.
At the final mock RRT, the major problem was again communication; that is, everyone spoke at once. The team members were encouraged to direct all comments to the team leader and keep any other conversation to a minimum.
A Successful RRT
The following case example, which describes the successful use of our OV-UCLA’s RRT, provides an illuminating look at its effectiveness. In this case, the RRT comprised the ICU nurse, the ICU physician, and the respiratory therapist. The team carried the following equipment: a patient monitor, medications, an IV start, blood sampling tubes, a central line, oxygen masks, and suctioning equipment.
The case began when the primary nurse activated the call. The patient—a 36-year-old HIV-positive male with acute rectal bleeding—was found to have a systolic blood pressure (SBP) reading of 70 and a heart rate of 144. The patient was admitted for anal warts but was noted to have acute bright red blood per rectum. The primary physician team had been called, but had not yet arrived. The primary nurse used the bedside phone to call X4415, and the RRT arrived within three minutes.
Upon arrival, the RRT started a wide bore IV and a central line. The team then called for O-negative blood from the blood bank. The transfusion began seven minutes after the team’s arrival in the patient’s room. The patient was transferred to the ICU and was discharged to the floor the following day.
Results
In four-and-a-half months, we have had 43 calls. The warning signs that precipitated the calls include:
- Respiratory distress: 14 (resulting in eight intubations);
- Cardiac problems: six;
- Altered mental status: four;
- Hypotension: four;
- Post-procedure oversedation: three;
- Vomiting: two;
- Bleeding: two;
- Gastrointestinal: one;
- Mouth bleeding: one;
- Hypoglycemia: one; and
- Unclear etiology: five. TH
Dr. Stein is the medical director, Intensive Care Unit/SDU, at Olive View UCLA Medical Center.
References
- Bellomo R, Goldsmith D, Uchino S, et al. A prospective before-and-after trial of a medical emergency team. Med J Aust. 2003 Sep 15:179(6):283-287
- The Institute for Healthcare Improvement’s 100,000 Lives Campaign. Available at: www.ihi.org. Last accessed July 10, 2006.
- Leonard MS, Graham S, Taggart B. The human factor: effective teamwork and communication in patient strategy. In: Leonard M, Frankel A, Simmonds T, eds. Achieving safe and reliable health care strategies and solutions. 1st ed. ACHE Management Series; 2004. p.37-65.
- Schein RM, Hazday N, Pena M, et al. Clinical antecedents to in-hospital cardiopulmonary arrests. Chest. 1990;98:1388-1392.
- Franklin C, Matthew J. Developing strategies to prevent-in hospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med. 1994;22(2):244-247.
The origin of the RRT can be found in medical emergency teams (METs). METs began in Australia as a result of the realization that earlier intervention could lead to better outcomes.1 In December 2004, in response to persistent problems with patient safety, the Institute for Healthcare Improvement launched its “100,000 Lives Campaign.”2 The Institute’s key plan for saving some of these 100,000 lives was to create RRTs at every participating medical center. Participating facilities would also submit data on mortality.
Olive View-UCLA Medical Center (OV-UCLA) signed on to participate in the campaign, and part of that effort was the creation and implementation of an RRT. We joined a University Health Consortium “Commit to Action” team, which assisted us by providing support as we began the creation and implementation of the RRT. What follows is the story of how we created an RRT.
We chose team members from all disciplines that were to be part of the RRT response—both at and behind the scenes: RNs, nursing administrators, hospital administrators, ICU attendings, house staff, laboratory personnel, nursing educators, radiology technicians, and hospital operators. The group was further organized into specific teams to solve problems and present solutions. At this point we learned our first important lesson: We needed to meet individually with all inpatient department chairs to discuss the effect of RRTs.
Activation and Notification
How would the RRT call be activated—overhead or beeper? Who could call, and what would the indications be? The OV-UCLA activation and notification team decided that the RRT could be activated by any staff member. Criteria, including vital signs, mental status, or simply “concern about the patient,” were created and posted. A telephone line in the ICU (X4415) was dedicated for RRT calls, and all other activation was overhead due to the lack of an adequate beeper system. (Other than code pagers, our beeper system can’t be simultaneously activated, and ancillaries don’t have beepers.)
The primary nurse’s responsibilities included calling the primary team or cross-covering team and obtaining a fingerstick glucose on all patients while waiting for the team. In discussions the primary team, we learned our second important lesson: As we presented the RRT to the hospital staff, everyone was concerned about the primary team. Ensuring that a mechanism for notifying the primary team was in place and reassuring staff that the primary team would be involved emerged as essential tasks. It was also imperative to identify the chain of command.
With this need in mind, we decided the primary team would always be the captain and would, therefore, have the authority to dismiss whomever they wanted from the RRT. An ICU attending was assigned to RRT call as supervision for the ICU resident responder. At OV-UCLA, our attending is not in-house and, to date, has not been called.
Documentation
The OV-UCLA documentation team was called on to answer the following questions: How would the RRT call be documented? How would medication orders be sent to the pharmacy? How would quality indicators (QI) and data be collected on the calls?
The team’s solution involved creating a one-page, primarily check-based document. The ICU nurse who answered the X4415 telephone in the ICU would begin documentation, which included the time of the call and the chief complaint. When the RRT reached the patient, however, the documentation duties were transferred to the primary RN. All providers were to document on the same page—similar to a code sheet. The RRT nurse and the attending doctor were to check vitals and perform the physical exam, as all information was called out to the documenter.
Medications were to be verbally ordered by the doctor, then read back and verified by the nurses documenting and administering for the RRT. For the most part, medication orders were restricted to what was carried in the RRT bag. The document was eventually copied three times: The original was placed in the chart, one copy was sent to the pharmacy for a record of medication, and the other was saved for QI. The primary team was expected to write a note in the chart’s disposition and time of disposition were to be included in this message.
Equipment
The OV-UCLA equipment team had one important question to answer: What supplies did we need at the bedside?
Although equipment and medications are readily available outside the ICU, the team didn’t want to spend time looking for equipment during an RRT call. “I don’t want a quick RRT call to evolve into a three-hour scavenger hunt,” says one team member.
Because OV-UCLA does not have a 24-hour pharmacist, the group felt it essential to bring medications to the bedside to avoid delays. Our solution to this potential problem was simple. The medication box is prepared by the pharmacy and sealed with one expiration date. Once the box is opened, it is exchanged for a new sealed box. The team chose a rolling duffle to store and transport the supplies, which are compartmentalized into the following sections: infection control, medications, airway and respiratory, IV access and blood draw, and IV start. Medications include respiratory treatments, antibiotics, furosemide, nitroglycerin, metoprolol, heparin and low molecular weight heparin, naloxone, ephedrine, dopamine, glucose, glucagons, and so on. The bag is restocked upon its return to the ICU.
Because of the stress involved in maintaining emergency equipment, we opted to call the supplies a “convenience bag.” This label ensured that only the sealed medication box would require a mandatory check; the rest of the equipment would be monitored on a more informal basis. Because all equipment is available on every floor, and because any RRT call can be converted to a code blue, the team felt that this was reasonable. The committee also purchased a five-pound patient monitor that has a screen for a cardiac tracing, a pulse oximeter, a noninvasive blood pressure monitor, and a temperature probe. This monitor fits easily in a pocket of the duffle.
Education and Publicity
How would staff know to call the RRT? The OV-UCLA team, anticipating that the majority of RRT calls would be activated by the primary RNs, decided that educating all nursing staff was essential.
The hospital nursing education office trained all nurses on all shifts in a short period of time. All nursing staff were taught to use SBAR (situation, background, assessment, and recommendation) communication and to identify early warning signs.1 The importance of recognizing the early warning signs was stressed during the nursing and physician training sessions. Staff were reassured that they didn’t have to know what was wrong with the patient to know that something was wrong and that help was required.
Publicity was accomplished in a variety of ways. The facility purchased pencils in our official color—lime green—that said “Rapid Response Team X4415.” The duffle was wheeled to all nursing stations so that staff could see it. We also ordered custom green-and-white M&M candy (available at www.mms.com) labeled “RRT X4415” to give as a promotional gift when an RRT was called.
Staffing
One last question remained for our team members: Who would respond to the RRT?
The committee felt strongly that an ICU nurse, an ICU resident, and a respiratory therapist should respond. Many physicians on the team did not want a doctor to respond, mostly due to concerns over chain of command. Who would be responsible for decisions made by the RRT? What if an ICU R2 disagreed with a surgery R4? Could they write a “do not call RRT order?” Nursing, on the other hand, wanted physician response; they wanted to be able to stabilize the patient.
Standardized protocols were discussed, but the team felt that the they would unreasonably delay the start. Radiology, which has no code blue response, volunteered to respond to all calls and hand-deliver the film to a computerized viewing system. The lab volunteered to run all RRT labs—designated with a lime green sticker—as quickly as possible.
The medical staff wanted to pilot the RRT, but because we are a small facility (220 beds) and to avoid confusion we launched the RRT for all inpatients. We went live in October 2005. The original plan was to staff an ICU nurse/RRT position. This RRT RN would relieve ICU nurses for breaks to maintain staffing ratios and provide RRT coverage. Because of the omnipresent nursing shortage, however, the RRT position is often pulled and the charge nurse must cover calls. Nurses sign up for RRT overtime and get pulled for patient care duties.
Mock RRT Calls
We performed three RRT drills to determine problem areas. For the first call, we involved a physician who had been vocal about the need for an RRT. The call was for a patient with shortness of breath. Two problems occurred during this drill: The primary team was never called, and there was no overhead page. So a member of our team worked with the hospital operator on our committee and clarified our protocols.
At the second drill, the main problem was documentation. The ICU nurse was so busy documenting that he wasn’t involved with the patient. Because the expertise of the ICU nurse is essential (in fact, there are times when this RN is the most experienced person on the team) we restructured the response so that the primary nurse would document and the ICU nurse was free to provide the hands-on care required.
At the final mock RRT, the major problem was again communication; that is, everyone spoke at once. The team members were encouraged to direct all comments to the team leader and keep any other conversation to a minimum.
A Successful RRT
The following case example, which describes the successful use of our OV-UCLA’s RRT, provides an illuminating look at its effectiveness. In this case, the RRT comprised the ICU nurse, the ICU physician, and the respiratory therapist. The team carried the following equipment: a patient monitor, medications, an IV start, blood sampling tubes, a central line, oxygen masks, and suctioning equipment.
The case began when the primary nurse activated the call. The patient—a 36-year-old HIV-positive male with acute rectal bleeding—was found to have a systolic blood pressure (SBP) reading of 70 and a heart rate of 144. The patient was admitted for anal warts but was noted to have acute bright red blood per rectum. The primary physician team had been called, but had not yet arrived. The primary nurse used the bedside phone to call X4415, and the RRT arrived within three minutes.
Upon arrival, the RRT started a wide bore IV and a central line. The team then called for O-negative blood from the blood bank. The transfusion began seven minutes after the team’s arrival in the patient’s room. The patient was transferred to the ICU and was discharged to the floor the following day.
Results
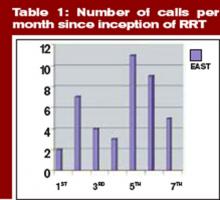
In four-and-a-half months, we have had 43 calls. The warning signs that precipitated the calls include:
- Respiratory distress: 14 (resulting in eight intubations);
- Cardiac problems: six;
- Altered mental status: four;
- Hypotension: four;
- Post-procedure oversedation: three;
- Vomiting: two;
- Bleeding: two;
- Gastrointestinal: one;
- Mouth bleeding: one;
- Hypoglycemia: one; and
- Unclear etiology: five. TH
Dr. Stein is the medical director, Intensive Care Unit/SDU, at Olive View UCLA Medical Center.
References
- Bellomo R, Goldsmith D, Uchino S, et al. A prospective before-and-after trial of a medical emergency team. Med J Aust. 2003 Sep 15:179(6):283-287
- The Institute for Healthcare Improvement’s 100,000 Lives Campaign. Available at: www.ihi.org. Last accessed July 10, 2006.
- Leonard MS, Graham S, Taggart B. The human factor: effective teamwork and communication in patient strategy. In: Leonard M, Frankel A, Simmonds T, eds. Achieving safe and reliable health care strategies and solutions. 1st ed. ACHE Management Series; 2004. p.37-65.
- Schein RM, Hazday N, Pena M, et al. Clinical antecedents to in-hospital cardiopulmonary arrests. Chest. 1990;98:1388-1392.
- Franklin C, Matthew J. Developing strategies to prevent-in hospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med. 1994;22(2):244-247.
The origin of the RRT can be found in medical emergency teams (METs). METs began in Australia as a result of the realization that earlier intervention could lead to better outcomes.1 In December 2004, in response to persistent problems with patient safety, the Institute for Healthcare Improvement launched its “100,000 Lives Campaign.”2 The Institute’s key plan for saving some of these 100,000 lives was to create RRTs at every participating medical center. Participating facilities would also submit data on mortality.
Olive View-UCLA Medical Center (OV-UCLA) signed on to participate in the campaign, and part of that effort was the creation and implementation of an RRT. We joined a University Health Consortium “Commit to Action” team, which assisted us by providing support as we began the creation and implementation of the RRT. What follows is the story of how we created an RRT.
We chose team members from all disciplines that were to be part of the RRT response—both at and behind the scenes: RNs, nursing administrators, hospital administrators, ICU attendings, house staff, laboratory personnel, nursing educators, radiology technicians, and hospital operators. The group was further organized into specific teams to solve problems and present solutions. At this point we learned our first important lesson: We needed to meet individually with all inpatient department chairs to discuss the effect of RRTs.
Activation and Notification
How would the RRT call be activated—overhead or beeper? Who could call, and what would the indications be? The OV-UCLA activation and notification team decided that the RRT could be activated by any staff member. Criteria, including vital signs, mental status, or simply “concern about the patient,” were created and posted. A telephone line in the ICU (X4415) was dedicated for RRT calls, and all other activation was overhead due to the lack of an adequate beeper system. (Other than code pagers, our beeper system can’t be simultaneously activated, and ancillaries don’t have beepers.)
The primary nurse’s responsibilities included calling the primary team or cross-covering team and obtaining a fingerstick glucose on all patients while waiting for the team. In discussions the primary team, we learned our second important lesson: As we presented the RRT to the hospital staff, everyone was concerned about the primary team. Ensuring that a mechanism for notifying the primary team was in place and reassuring staff that the primary team would be involved emerged as essential tasks. It was also imperative to identify the chain of command.
With this need in mind, we decided the primary team would always be the captain and would, therefore, have the authority to dismiss whomever they wanted from the RRT. An ICU attending was assigned to RRT call as supervision for the ICU resident responder. At OV-UCLA, our attending is not in-house and, to date, has not been called.
Documentation
The OV-UCLA documentation team was called on to answer the following questions: How would the RRT call be documented? How would medication orders be sent to the pharmacy? How would quality indicators (QI) and data be collected on the calls?
The team’s solution involved creating a one-page, primarily check-based document. The ICU nurse who answered the X4415 telephone in the ICU would begin documentation, which included the time of the call and the chief complaint. When the RRT reached the patient, however, the documentation duties were transferred to the primary RN. All providers were to document on the same page—similar to a code sheet. The RRT nurse and the attending doctor were to check vitals and perform the physical exam, as all information was called out to the documenter.
Medications were to be verbally ordered by the doctor, then read back and verified by the nurses documenting and administering for the RRT. For the most part, medication orders were restricted to what was carried in the RRT bag. The document was eventually copied three times: The original was placed in the chart, one copy was sent to the pharmacy for a record of medication, and the other was saved for QI. The primary team was expected to write a note in the chart’s disposition and time of disposition were to be included in this message.
Equipment
The OV-UCLA equipment team had one important question to answer: What supplies did we need at the bedside?
Although equipment and medications are readily available outside the ICU, the team didn’t want to spend time looking for equipment during an RRT call. “I don’t want a quick RRT call to evolve into a three-hour scavenger hunt,” says one team member.
Because OV-UCLA does not have a 24-hour pharmacist, the group felt it essential to bring medications to the bedside to avoid delays. Our solution to this potential problem was simple. The medication box is prepared by the pharmacy and sealed with one expiration date. Once the box is opened, it is exchanged for a new sealed box. The team chose a rolling duffle to store and transport the supplies, which are compartmentalized into the following sections: infection control, medications, airway and respiratory, IV access and blood draw, and IV start. Medications include respiratory treatments, antibiotics, furosemide, nitroglycerin, metoprolol, heparin and low molecular weight heparin, naloxone, ephedrine, dopamine, glucose, glucagons, and so on. The bag is restocked upon its return to the ICU.
Because of the stress involved in maintaining emergency equipment, we opted to call the supplies a “convenience bag.” This label ensured that only the sealed medication box would require a mandatory check; the rest of the equipment would be monitored on a more informal basis. Because all equipment is available on every floor, and because any RRT call can be converted to a code blue, the team felt that this was reasonable. The committee also purchased a five-pound patient monitor that has a screen for a cardiac tracing, a pulse oximeter, a noninvasive blood pressure monitor, and a temperature probe. This monitor fits easily in a pocket of the duffle.
Education and Publicity
How would staff know to call the RRT? The OV-UCLA team, anticipating that the majority of RRT calls would be activated by the primary RNs, decided that educating all nursing staff was essential.
The hospital nursing education office trained all nurses on all shifts in a short period of time. All nursing staff were taught to use SBAR (situation, background, assessment, and recommendation) communication and to identify early warning signs.1 The importance of recognizing the early warning signs was stressed during the nursing and physician training sessions. Staff were reassured that they didn’t have to know what was wrong with the patient to know that something was wrong and that help was required.
Publicity was accomplished in a variety of ways. The facility purchased pencils in our official color—lime green—that said “Rapid Response Team X4415.” The duffle was wheeled to all nursing stations so that staff could see it. We also ordered custom green-and-white M&M candy (available at www.mms.com) labeled “RRT X4415” to give as a promotional gift when an RRT was called.
Staffing
One last question remained for our team members: Who would respond to the RRT?
The committee felt strongly that an ICU nurse, an ICU resident, and a respiratory therapist should respond. Many physicians on the team did not want a doctor to respond, mostly due to concerns over chain of command. Who would be responsible for decisions made by the RRT? What if an ICU R2 disagreed with a surgery R4? Could they write a “do not call RRT order?” Nursing, on the other hand, wanted physician response; they wanted to be able to stabilize the patient.
Standardized protocols were discussed, but the team felt that the they would unreasonably delay the start. Radiology, which has no code blue response, volunteered to respond to all calls and hand-deliver the film to a computerized viewing system. The lab volunteered to run all RRT labs—designated with a lime green sticker—as quickly as possible.
The medical staff wanted to pilot the RRT, but because we are a small facility (220 beds) and to avoid confusion we launched the RRT for all inpatients. We went live in October 2005. The original plan was to staff an ICU nurse/RRT position. This RRT RN would relieve ICU nurses for breaks to maintain staffing ratios and provide RRT coverage. Because of the omnipresent nursing shortage, however, the RRT position is often pulled and the charge nurse must cover calls. Nurses sign up for RRT overtime and get pulled for patient care duties.
Mock RRT Calls
We performed three RRT drills to determine problem areas. For the first call, we involved a physician who had been vocal about the need for an RRT. The call was for a patient with shortness of breath. Two problems occurred during this drill: The primary team was never called, and there was no overhead page. So a member of our team worked with the hospital operator on our committee and clarified our protocols.
At the second drill, the main problem was documentation. The ICU nurse was so busy documenting that he wasn’t involved with the patient. Because the expertise of the ICU nurse is essential (in fact, there are times when this RN is the most experienced person on the team) we restructured the response so that the primary nurse would document and the ICU nurse was free to provide the hands-on care required.
At the final mock RRT, the major problem was again communication; that is, everyone spoke at once. The team members were encouraged to direct all comments to the team leader and keep any other conversation to a minimum.
A Successful RRT
The following case example, which describes the successful use of our OV-UCLA’s RRT, provides an illuminating look at its effectiveness. In this case, the RRT comprised the ICU nurse, the ICU physician, and the respiratory therapist. The team carried the following equipment: a patient monitor, medications, an IV start, blood sampling tubes, a central line, oxygen masks, and suctioning equipment.
The case began when the primary nurse activated the call. The patient—a 36-year-old HIV-positive male with acute rectal bleeding—was found to have a systolic blood pressure (SBP) reading of 70 and a heart rate of 144. The patient was admitted for anal warts but was noted to have acute bright red blood per rectum. The primary physician team had been called, but had not yet arrived. The primary nurse used the bedside phone to call X4415, and the RRT arrived within three minutes.
Upon arrival, the RRT started a wide bore IV and a central line. The team then called for O-negative blood from the blood bank. The transfusion began seven minutes after the team’s arrival in the patient’s room. The patient was transferred to the ICU and was discharged to the floor the following day.
Results
In four-and-a-half months, we have had 43 calls. The warning signs that precipitated the calls include:
- Respiratory distress: 14 (resulting in eight intubations);
- Cardiac problems: six;
- Altered mental status: four;
- Hypotension: four;
- Post-procedure oversedation: three;
- Vomiting: two;
- Bleeding: two;
- Gastrointestinal: one;
- Mouth bleeding: one;
- Hypoglycemia: one; and
- Unclear etiology: five. TH
Dr. Stein is the medical director, Intensive Care Unit/SDU, at Olive View UCLA Medical Center.
References
- Bellomo R, Goldsmith D, Uchino S, et al. A prospective before-and-after trial of a medical emergency team. Med J Aust. 2003 Sep 15:179(6):283-287
- The Institute for Healthcare Improvement’s 100,000 Lives Campaign. Available at: www.ihi.org. Last accessed July 10, 2006.
- Leonard MS, Graham S, Taggart B. The human factor: effective teamwork and communication in patient strategy. In: Leonard M, Frankel A, Simmonds T, eds. Achieving safe and reliable health care strategies and solutions. 1st ed. ACHE Management Series; 2004. p.37-65.
- Schein RM, Hazday N, Pena M, et al. Clinical antecedents to in-hospital cardiopulmonary arrests. Chest. 1990;98:1388-1392.
- Franklin C, Matthew J. Developing strategies to prevent-in hospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med. 1994;22(2):244-247.