User login
Pediatric Hospitalist Comanagement
As the field of pediatric hospital medicine has emerged, so too has evidence that hospitalist management of pediatric medical patients in the tertiary‐care setting is associated with decreased length of stay (LOS).13 The American Academy of Pediatrics Committee on Hospital Care has recommended hospitalist consultation for pediatric surgical patients being managed by adult surgeons.4 In one survey of pediatric hospitalists, 66% of community hospitalists and 47% of academic hospitalists reported comanaging surgical patients.5 However, little work has been published on the effect of hospitalist comanagement of pediatric surgical patients.
Since June 2000 patients undergoing spinal fusion surgery at the Children's Hospital in Denver, Colorado have been screened by a spine nurse for medical complexity. Medically complex patients undergoing preoperative multispecialty evaluation and their perioperative care are coordinated by the spine nurse.6 Introduction of a general pediatric hospitalist to aid with pre‐ and perioperative management of the most complicated patients in December 2004 provided us with an opportunity to study hospitalist comanagement of medically complex pediatric patients undergoing spine fusion surgery.
Our objectives were (1) to describe comanagement activities and (2) to determine the association of hospitalist comanagement on LOS following spinal fusion surgery. We hypothesized that by addressing a variety of pre‐ and perioperative medical issues, hospitalist comanagement would be associated with a decreased LOS for medically complex pediatric patients undergoing spinal fusion surgery.
METHODS
Design and Population
A retrospective analysis of the orthopedic surgeons' log at the Children's Hospital in Denver, Colorado, a tertiary‐care academic pediatric hospital serving the Rocky Mountain region, was performed. Patients included were those underwent their first episode of spinal fusion surgery between July 1, 2000, and October 1, 2005 (n = 759); exclusion criteria included diagnoses of spondylolisthesis or spondylolysis. The study was approved by the Colorado Multiple Institutional Review Board and exempted from ongoing review, and informed consent was not required.
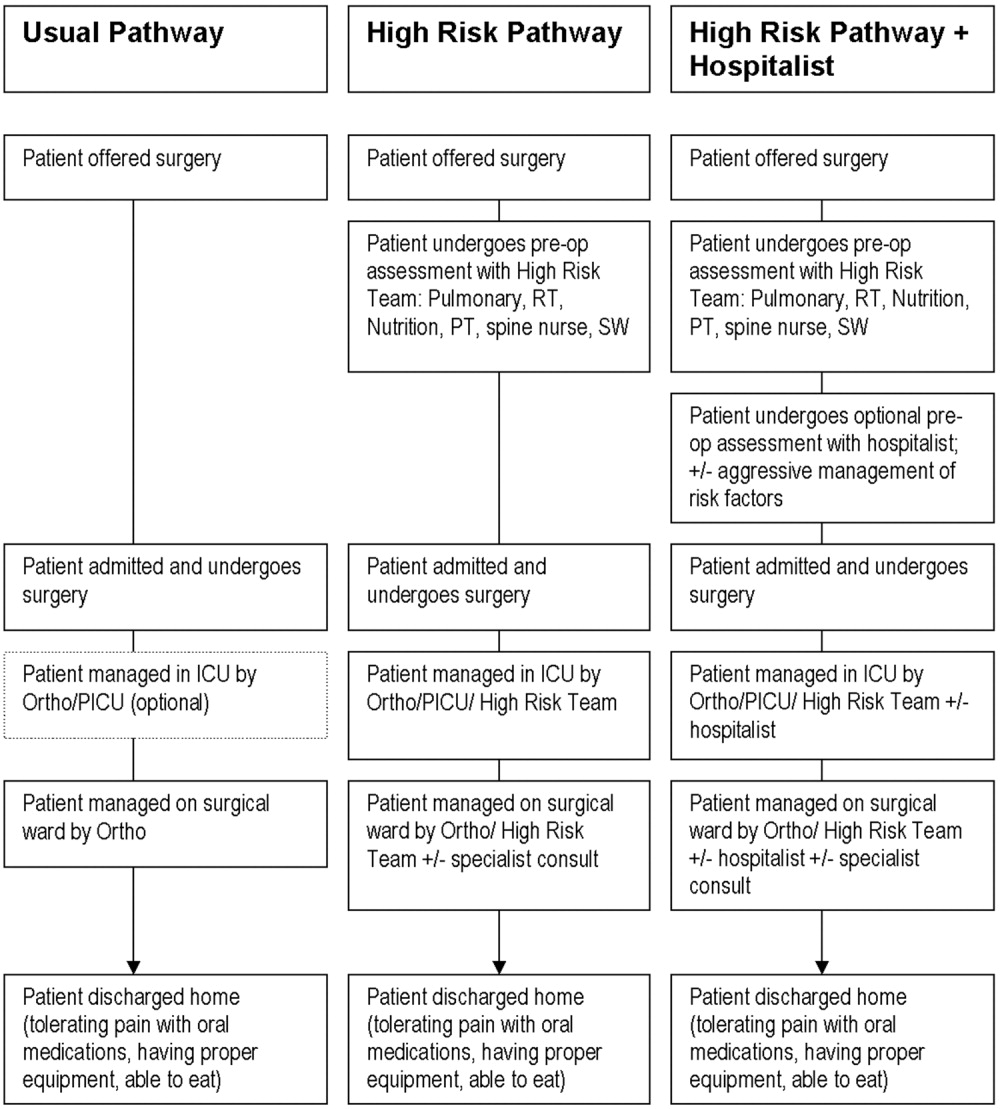
Intervention: Pre‐ and Perioperative High‐Risk Pathway
Since June 2000 medically complex patients undergoing spinal fusion surgery at the Children's Hospital in Denver, Colorado have been referred by either the orthopedic surgeon or the rehabilitation physician to the spine surgery nurse. This nurse, an RN, BSN with more than a decade of experience with spinal fusion patients, then coordinates preoperative multispecialty evaluation (Fig. 1, column 2). Patients are seen by a pulmonologist pre‐operatively, and undergo pulmonary function tests, chest radiograph, venous blood gas, and, at times, a polysomnogram and electrocardiography. A cardiology consult is obtained for patients with muscle disease. Gastroenterology and neurology may be consulted if there are significant feeding and/or neurological issues that the primary care physician needs assistance addressing preoperatively. Shortly before the scheduled surgery, the patient is evaluated at a discharge planning meeting by a nutritionist, respiratory therapist, physical therapist, social worker (at times), and the spinal surgery nurse for discharge equipment planning. Immediately before surgery, in addition to teaching, surgical consent and a surgical history and physical are obtained, as well as laboratory studies that include a complete blood cell count, type, and cross, coagulation studies, and spine radiographs.5 Medically complex patients are managed in the intensive care unit for at least 24 hours after surgery. In addition, standardized order sets developed in 2001 and edited in July 2005 are used to streamline management of the intensive care unit and the orthopedic ward.

Since December 2004, a hospitalist has aided pre‐ and perioperative evaluation and management (Fig. 1, column 3). The patients seen and comanaged by the hospitalist have been those who have significant medical issues in addition to neuromuscular disease, including multiple medications, seizure disorders, nutritional concerns, and/or significant social concerns. Whereas patients with a multitude of different diagnoses were referred to the spinal surgery nurse for a variety of reasons, patients comanaged by hospitalists were generally children with multiple medical conditions who had neuromuscular scoliosis.
Data Sources
The primary data source used was the surgeons' log. The surgeons' log is a record of patients undergoing spinal fusion surgery maintained concurrently by 2 individuals (the spine surgery nurse and her assistant). From January 2000 on, patient data were manually input into an Excel spreadsheet regularly and were cross‐referenced weekly with the surgery schedule. Data entered include: patient name, medical record number, date of surgery, date of discharge (from hospital admission information), underlying diagnosis, type of procedure, primary surgeon (from operative and/or discharge summaries), and LOS (calculated from dates of discharge and surgery). If either underlying diagnosis or type of procedure needed clarification, the spine surgery nurse discussed it with the primary surgeon. We verified the completeness of the surgeons' log for first spinal fusion surgeries by cross‐referencing with billing records; of 572 surgeries performed by 5 surgeons, 571 were recorded (99.8%) in the surgeons' log.
To perform the descriptive analysis of hospitalist activities, the first author (T.S.) performed a retrospective review of the charts of patients she had seen in her role as hospitalist from December 1, 2004, to October 1, 2005. Prepared in advance was a checklist of pre‐ and perioperative activities, modeled on prior work reporting clinical activities.7 Activities either mentioned in the daily progress note or ordered were recorded as completed and entered into an Excel spreadsheet.
Data Collection
The outcome measure was LOS, log‐transformed for analyses. Covariates included were: patient age, underlying diagnosis, procedure type, and surgeon. Underlying diagnoses were subdivided on the basis of the manually input Excel spreadsheet entries into 5 categories: idiopathic, congenital, neuromuscular, osteogenic, and other. The major diagnoses in the idiopathic category were infantile, juvenile, and adolescent idiopathic scoliosis; in the congenital category were congenital scoliosis, congenital kyphoscoliosis; in the neuromuscular category were cerebral palsy, Duchenne's muscular dystrophy, spina bifida, brain injury, spinal cord injury, and chromosomal anomalies; and in the osteogenic category were Scheuermann's kyphosis, trauma, tumor, kyphoscoliosis, and bone disease. Procedures were subdivided according to the manually input Excel spreadsheet entries into 3 categories: posterior only, anterior/ posterior, and anterior spinal fusion only.
After our initial analysis demonstrated a decline in LOS after December 2004 in both idiopathic and neuromuscular patients, we asked the orthopedic surgeons and spine surgery nurse to determine cointerventions that may have occurred around December 2004. We attempted to contact each surgeon who performed surgery during the study period and asked, What changes did you make on or around November 2004 in your management of spinal fusion patients? We received e‐mail and verbal responses from the spine surgery nurse and from 6 surgeons who had performed 646 of the procedures (78%) over the study period.
Increased use of intrathecal morphine was raised as a possible confounding cointervention. To characterize use of intrathecal morphine, we reviewed the charts of all the patients categorized as idiopathic or neuromuscular patients who underwent surgery after December 2004 and a random sample of 20% of these patients who underwent surgery before December 2004.
Analyses
All quantitative analyses (ie, those of the surgeons' log) were performed in a blinded manner, whereas the chart review was not blinded. Univariate analyses of hospitalist activities and univariate and bivariate analyses of the surgeons' log were performed using SAS 9.1. Mean LOS after log back‐transformation along with 95% confidence interval is reported. The chi square test of equality of variance was used to analyze whether the variances differed.
The multifaceted approach to the care of spinal fusion patients is a tiered approach, with 3 major patient groups (Fig. 1): (1) patients with scoliosis, generally idiopathic, and no or minimal medical conditions, who receive care by the usual pathway and do not receive care by the high‐risk pathway or do not have a hospitalist; (2) patients with scoliosis with any underlying diagnosis and some medical conditions, who receive care by high‐risk pathway; and (3) patients with scoliosis, usually neuromuscular scoliosis, and multiple medical conditions, who receive care by the high‐risk pathway and have hospitalist comanagement. Because of selection bias in the receipt of hospitalist comanagement (ie, the most complicated patients), we cannot reasonably compare hospitalist patients to nonhospitalist patients after December 2004. Instead, we compared all neuromuscular patients before and after hospitalist comanagement with a control group of idiopathic patients.
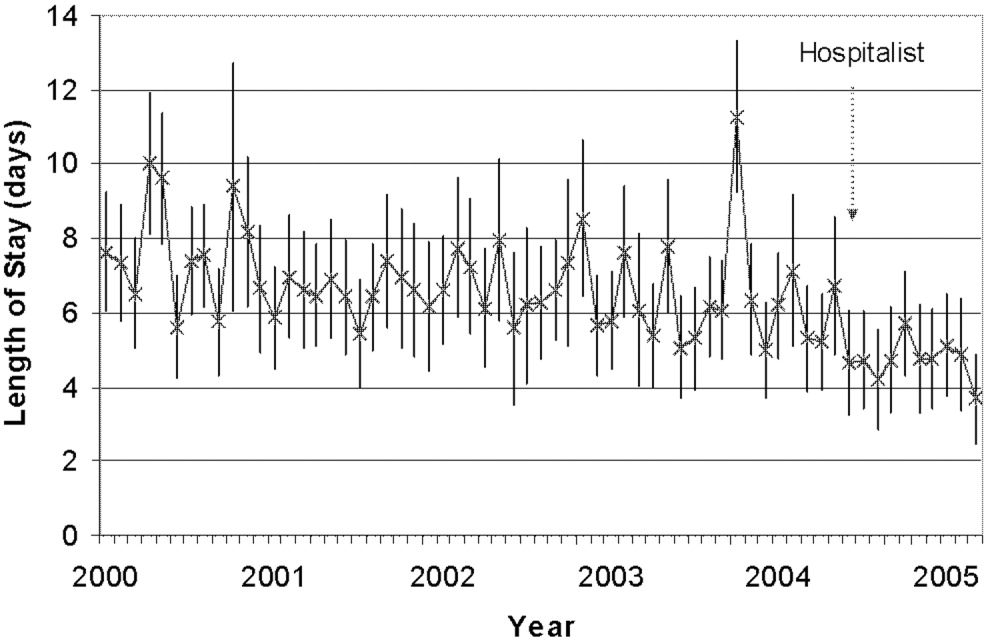
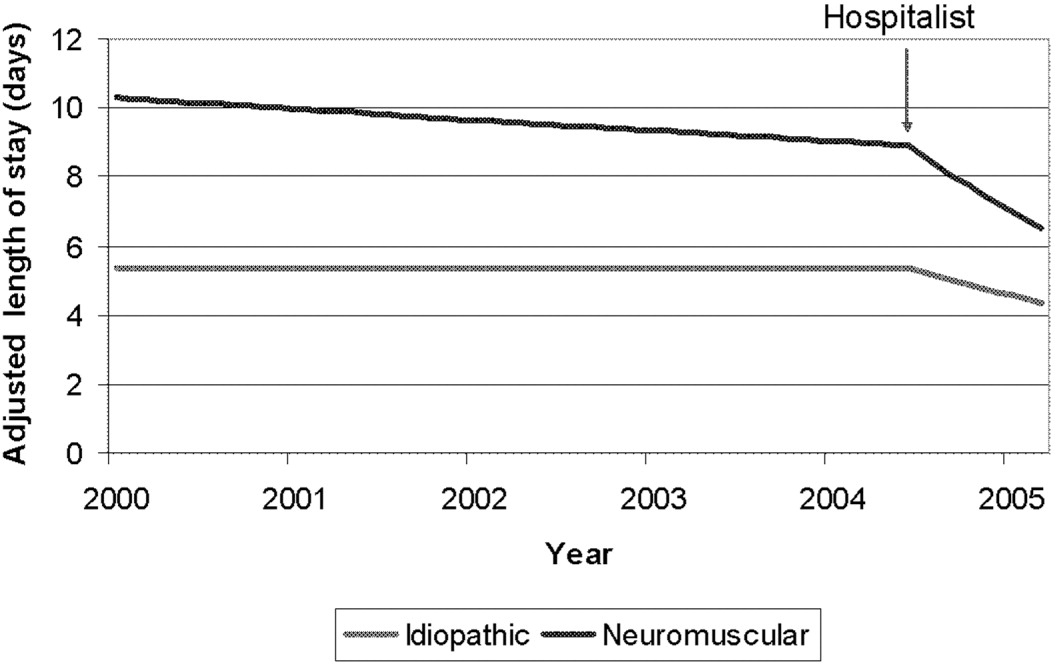
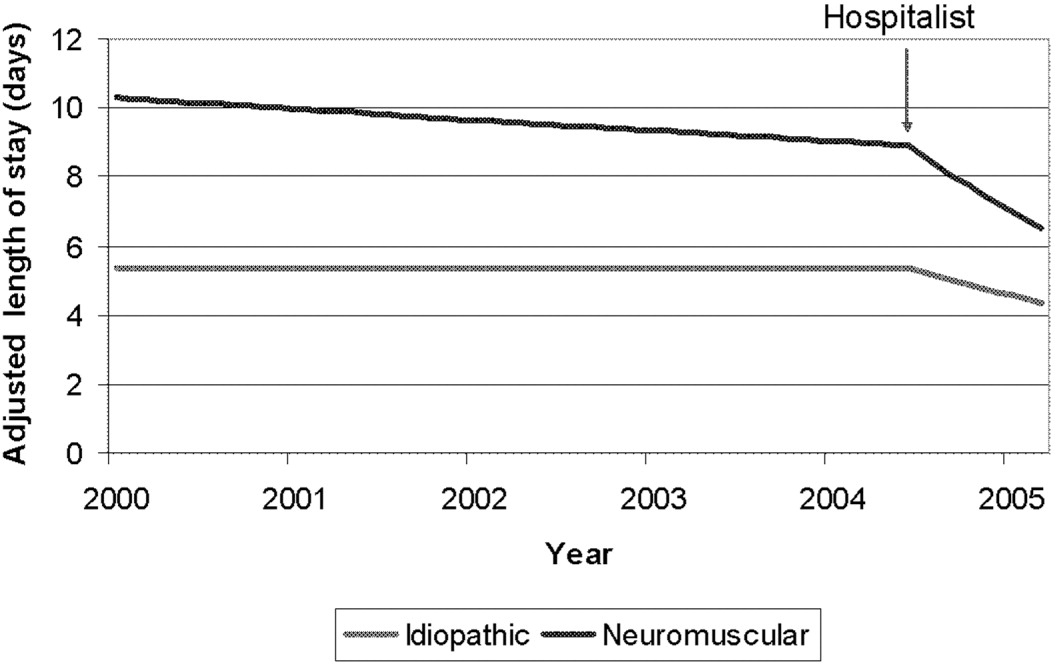
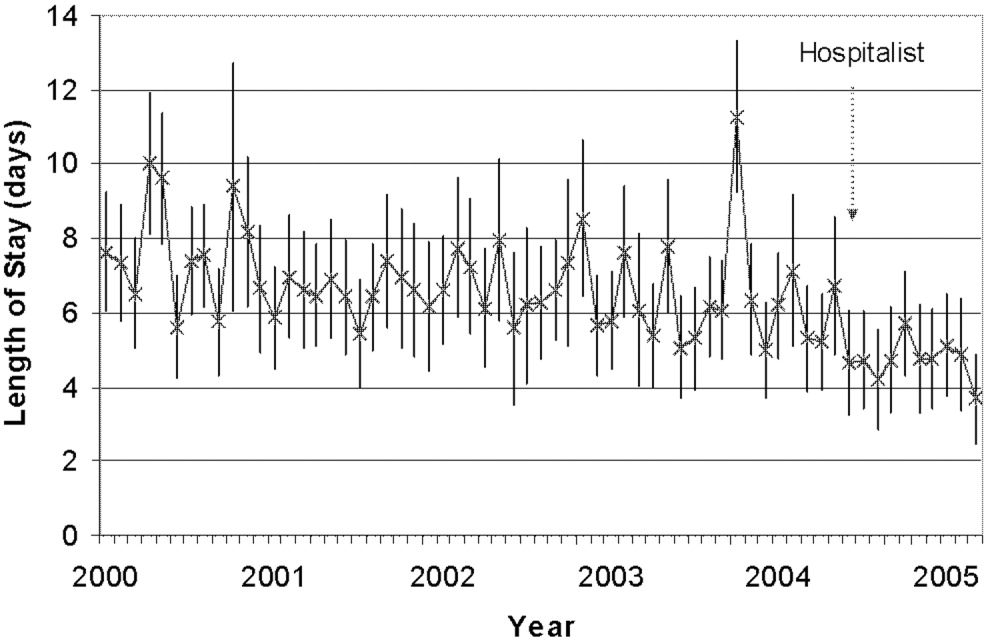
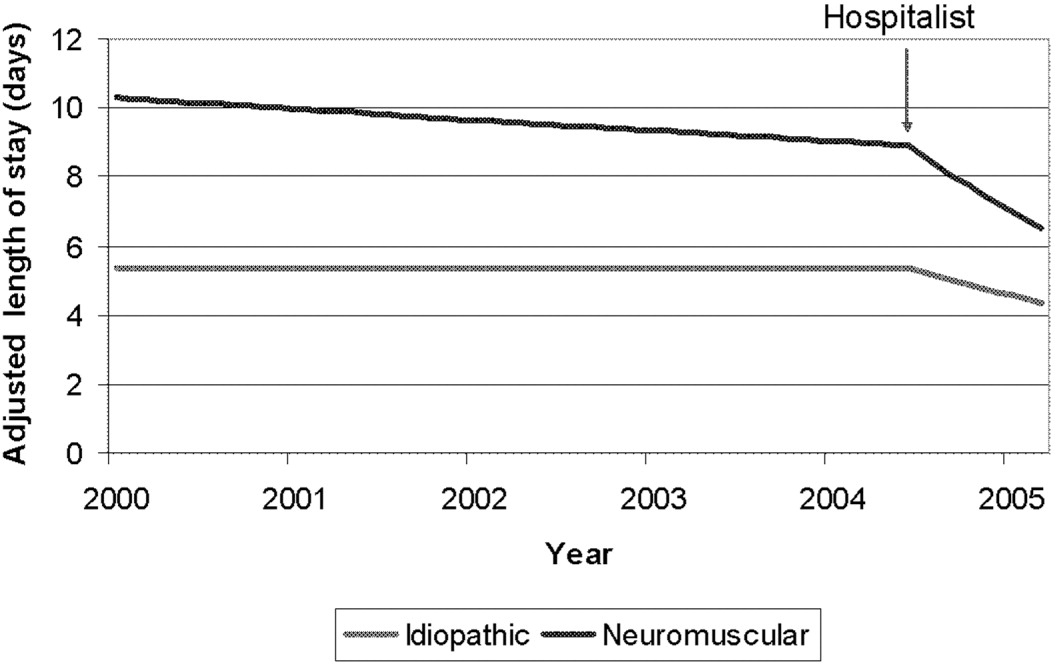
Initial examination of mean monthly LOS from June 2000 to October 2005 (Fig. 2) suggested a possible decline in both mean LOS and variability in LOS after December 2004, when hospitalist comanagement was initiated. To determine the trend in LOS over time before and after December 2004, we performed a mixed‐effects piecewise Poisson regression, adjusting for patient covariates (patient age, underlying diagnosis, procedure type, and intrathecal morphine [for idiopathic and neuromuscular patients]) and clustering by surgeon (as a random effect). We used the model to estimate 2 slopes to represent the linear trend before and after December 2004 (when hospitalist comanagement started). After regression modeling generated beta coefficients for each covariate, the average covariates were entered into the model to generate an average adjusted LOS as shown in Figure 3.
RESULTS
A total of 759 patients underwent initial spinal fusion surgery between July 1, 2000, and October 1, 2005644 before and 115 after December 2004, when hospitalist involvement started. After December 2004, 12% (14 of 115) of all spinal fusion surgery patients were comanaged by a hospitalist. Most comanaged patients (14 of 15, 93%) had neuromuscular scoliosis, and comanaged patients represented 37% (13 of 35) of all neuromuscular patients (Table 1). Over the course of the study, the number of more invasive and complicated anterior/posterior spinal fusion surgeries declined, whereas the number of posterior spinal fusion surgeries increased significantly because of the introduction of new technology (data not shown).
| LOS Days (95% CI) | ||||
|---|---|---|---|---|
| All Surgeries | Preintervention (July 2000December 2004) | Postintervention (December 2004September 2005) | Hospitalist Comanaged (December 2004September 2005) | |
| ||||
| Number of surgeries | 759 | 644 | 115 | 14* |
| Age (years), mean (SD) | 13.6 (3.4) | 13.7 (3.4) | 13.1 (3.4) | 12.6 (4.0) |
| Diagnosis | ||||
| Idiopathic | 328 (43%) | 277 (43%) | 51 (44%) | 1 (7%) |
| Neuromuscular | 247 (32%) | 212 (33%) | 35 (30%) | 13 (93%) |
| Congenital | 66 (9%) | 55 (8%) | 11 (10%) | |
| Osteogenic | 96 (13%) | 81 (13%) | 15 (13%) | |
| Other | 22 (3%) | 19 (3%) | 3 (3%) | |
| Procedure | ||||
| Posterior | 470 (62%) | 365 (57%) | 105 (91%) | 13 (93%) |
| Ant/post | 227 (30%) | 217 (34%) | 10 (8%) | 1 (7%) |
| Anterior | 62 (8%) | 62 (9%) | ||
| Intrathecal morphine use | ||||
| Idiopathic | 30/50 (60%) | 45/51 (88%) | 0 (0%) | |
| Neuromuscular | 10/42 (24%) | 21/35 (62%) | 5/13 (38%) | |
The 15 patients seen by the hospitalist received a total of 60 visits by the hospitalist. The hospitalist saw 9 patients preoperatively. Of the 15 patients comanaged in the hospital, 5 (33%) were seen once, 8 (53%) were seen between 2 and 5 times, and 2 (14%) were seen more than 10 times. Patients were seen both in the ICU and on the surgical ward. Among the patients seen preoperatively, the hospitalist recommended nutritional interventions for 5 patients (33%), bowel regimens for 4 patients (27%), and preoperative hospitalization for 1 patient for 5 days to optimize nutritional intake, address reflux, and modify bowel regimen, as well as facilitate multispecialty evaluation. Postoperative involvement generally addressed a variety of issues, but 20% of patients had no changes in their management (Table 2).
| Hospitalist Activity | Number of Patients (%) (n = 15) |
|---|---|
| |
| Care coordination | |
| Updated family | 11 (73%) |
| Coordinated discharge | 8 (53%) |
| Updated PCP | 7 (47%) |
| Transfer facilitated | 4 (27%) |
| Consulted pulmonary | 3 (20%) |
| Consulted GI | 2 (13%) |
| Type of recommendation | |
| Home medications reviewed | 14 (93%) |
| Nutritional (ie, feed changes) | 11 (73%) |
| Pain medications reviewed | 11 (73%) |
| Bowel regimen | 10 (67%) |
| New medical issues* | 10 (67%) |
| Pain medications modified | 9 (60%) |
| Foley removed | 7 (46%) |
| Unnecessary medication removed | 6 (40%) |
| Central line removed | 4 (27%) |
| No changes in management | 3 (20%) |
| TPN | 2 (13%) |
| Harmful medications removed | 0 (0%) |
Initial examination of mean monthly LOS from June 2000 to October 2005 suggested a possible decline in both mean LOS and variability in LOS after hospitalist comanagement was initiated (Fig. 2). Mean LOS for all initial spinal fusion surgeries decreased from 6.5 days (95% CI: 6.26.7) to 4.8 days (95% CI: 4.55.1) after December 2004. The standard deviation in LOS for all initial spinal fusion surgeries decreased from 1.64 to 1.39 days (P < .0001; Table 3). In the 52 months prior to hospitalist comanagement, there was no change in adjusted LOS over time (slope = 0.009 days/month, P = .3997). After December 2004, there was a significant decline in average adjusted LOS (slope = 0.2 days/month; P < .0001).
| Before Hospitalist 7/0012/04 n=644 | After Hospitalist After 12/04 n=115 | p value | |
|---|---|---|---|
| LOS Days (95% CI) | |||
| All Initial Spinal Fusion Surgeries | 6.5 (6.26.7) | 4.8 (4.55.1) | |
| Idiopathic | 5.2 (5.05.4) | 4.1(3.94.4) | |
| Neuromuscular | 8.6 (8.09.2) | 6.25 (5.56.9) | |
| Standard Deviation Days | |||
| All Initial Spinal Fusion Surgeries | 1.64 | 1.39 | <0.0001 |
| Idiopathic | 1.35 | 1.26 | 0.03 |
| Neuromuscular | 1.70 | 1.41 | 0.002 |
Mean and adjusted LOS of patients in the 2 main diagnostic categories, idiopathic and neuromuscular scoliosis, decreased. The absolute mean LOS decreased more for neuromuscular patients (8.6 days [95% CI: 8.09.2] to 6.2 days [95% CI: 5.56.9]) than for idiopathic patients (5.2 days [95% CI: 5.05.4] to 4.1 days [95% CI: 3.94.4]). The standard deviation in LOS decreased more for the neuromuscular patients, from 1.70 to 1.41 days (P = .002), as shown in Table 3. In the 52 months prior to hospitalist comanagement, there was no change in adjusted LOS over time (neuromuscular slope = 0.024 to 0.027 days/month, P = .49; idiopathic slope = 0.0005 days/month, P = .96). After December 2004, there was a significant decline in average adjusted LOS (neuromuscular slope = 0.23 to 0.31 days/month, P = .0075; idiopathic slope = 0.10 to 0.12 days/month; P = .0007), as demonstrated in Figure 3. A survey of the orthopedic surgical staff demonstrated no known specific changes in surgical or postoperative management initiated around December 2004 other than intrathecal morphine use. Some surgeons performed fewer surgeries, particularly of idiopathic patients.
DISCUSSION
The introduction of hospitalist comanagement to ongoing multispecialty evaluation for medically complex spinal fusion surgery patients was associated with a decrease in mean LOS among all patients undergoing initial spinal fusion surgery. A greater magnitude of decline in LOS was seen among children with neuromuscular scoliosis, who were often comanaged, than among children with idiopathic scoliosis, who were rarely comanaged. Variability in LOS also decreased following initiation of hospitalist comanagement, particularly in the more complex patients. The decreases in LOS persisted after adjustment for patient age, diagnosis, procedure type, intrathecal morphine use, and surgeon. This study provides support for the hypothesis that selective hospitalist comanagement of pediatric surgical patients in the tertiary‐care setting is associated with decreased LOS and decreased variability in LOS.
Analysis of a nationally representative data set demonstrated that 4504 children with idiopathic scoliosis and 1570 children with neuromuscular scoliosis underwent spinal fusion surgery in the United States in 2000.8 The average LOS for children with neuromuscular scoliosis was 9.2 days versus 6.1 days for those with idiopathic scoliosis. The LOS of both our patient populations, those before hospitalist comanagement and those after hospitalist comanagement, was less than the national estimates. Multidisciplinary management strategies with or without hospitalist comanagement may be associated with decreases in LOS for neuromuscular scoliosis patients undergoing spinal fusion surgery.
The hospitalist performed a variety of activities in comanaging the medically complex pediatric orthopedic patients. Hospitalist comanagement may have been associated with reduction in LOS for several reasons: preoperative prevention of medical problems, early postoperative identification of and intervention on medical complications, improved coordination of care, or simply consistency of postoperative medical care.
These findings are consistent with the pediatric nonsurgical literature, which suggests that hospitalist management of pediatric medical patients in the tertiary‐care setting is associated with decreased LOS.13 Hospitalist comanagement of adult orthopedic patients has been better studied than has been comanagement of pediatric patients. Elderly patients undergoing elective hip or knee arthroplasty were randomized to hospitalist care versus traditional orthopedic care after surgery. Both sets of patients were managed by the same nursing staff according to standardized care pathways. The mean LOS did not differ between the 2 groups, but the adjusted LOS was lower in the group that received hospitalist care.9 When the same center examined outcomes in hip fracture patients before and after implementation of a hospitalist care model, there was a decrease in LOS and no change in readmission or deaths.10 As in these studies, spinal fusion surgery management is highly standardized in our center. Nonetheless, hospitalist comanagement still was associated with a decreased LOS.
This study found a decline in LOS among all patients undergoing spinal fusion surgery, even among children with idiopathic scoliosis, of whom only 1 was comanaged. This finding may suggest hospitalist comanagement had a global, or indirect, effect on the management of all postoperative patients. However, the time‐series design could have been biased by a cointervention implemented at the same time as hospitalist care. Some surgeons performed fewer surgeries on their idiopathic patients over the course of the study; however, we adjusted for that surgeon in our analysis. Intrathecal morphine use is the only known change in postoperative management that may have affected care starting in December 2004; we also adjusted for intrathecal morphine use in our analysis. There may be other changes of which we are unaware. Nonetheless, the decline in LOS seen in the idiopathic population was exceeded by the decline in LOS in the comanaged neuromuscular population.
Unlike earlier reported studies, which examined hospitalist management among pediatric medical patients, this study did not assess complications (such as pneumonia, respiratory failure, urinary tract infection, gastric ulcers, pathologic fractures, poor wound healing, nutritional compromise, and readmission),7, 11, 12 costs, or patient and provider satisfaction with hospitalist comanagement.13 This assessment is critical to defining the value of these services to patients and providers. In addition, because we did not collect information on severity of disability, we were unable to control for disability. These are other covariates and outcomes of interest that should be assessed in future studies. Furthermore, there was potential bias introduced by having the lead author both conducting the study and performing the intervention; this was minimized by having different individuals responsible for primary data collection and having the analyses performed in a blinded fashion. In addition, although this study provided promising initial evidence that selective hospitalist comanagement along with multispecialty evaluation of spinal fusion surgery patients may lead to a significant decrease in LOS, this evidence needs to be replicated in other surgical patient populations and hospital settings. Ideally, the impact of hospitalist comanagement should be more fully evaluated in a randomized controlled trial. Hospitalist comanagement is a promising technique for improving the care of children undergoing spinal fusion surgery, particularly those with complex medical conditions.
Acknowledgements
The authors acknowledge the contributions of Heidi Gullord of University Physician, Incorporated, for assistance with obtaining billing records. We also appreciate the ongoing input of the Children's Hospital Department of Epidemiology, including Lorna Dyk, BSN, MBA; Michael Rannie, RN, MS; Meghan Birkholz, MSPH; and Michael Kahn, MD, PhD. We appreciate the willingness of the Department of Orthopedics to cooperate with this study, including (but not limited to) Mark Erickson, MD; Frank Chang, MD; and Gaia Georgopoulos, MD. In addition, we acknowledge the ongoing efforts of the care providers involved in the High Risk Pathway at the Children's Hospital, including Carol Page, PT; Alice Radic, PTA; Sarah Hack Baltazar, RD; Monte Leidholm, RRT; Cloy Vaneman, RRT; Gail Shattuck, MSW; and Lynn Katz, MSW, as well as the Divisions of Pulmonary Medicine and Intensive Care of the Department of Pediatrics. We also thank Heather Ramey, BS, BA, for her assistance with organizing the multispecialty evaluation of patients undergoing surgery. We also appreciate the efforts of the fellows and faculty of the Primary Care Research Fellowship and appreciate their assistance in crafting this research.
- ,.Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges.Pediatrics.2000;105:478–484.
- ,,, et al.Impact of a health maintenance organization hospitalist system in academic pediatrics.Pediatrics.2002;110:720–728.
- ,,,.Evaluation of a staff‐only hospitalist system in a tertiary care, academic children's hospital.Pediatrics.2004;114:1545–1549.
- and theCommittee on Hospital Care.Physicians' roles in coordinating care of hospitalized children.Pediatrics.2003;111:707–709.
- and.Differences in work environment, responsibilities, and training need between community hospital and academic center hospitalists. E‐PAS2006:59:4128.3.
- ,.Development and implementation of a spine fusion high risk pathway. 5th Annual Pre‐Brandon Carrell Pediatric Orthopaedic Symposium for Nursing and Allied Healthcare Professionals, Texas Scottish Rite Hospital for Children, Dallas, Texas, June 26,2003.
- ,,,.Reducing delirium after hip fracture: a randomized trial.J Am Geriatr Soc.2001;49:516–522.
- ,,, et al.Spinal fusion in children with idiopathic and neuromuscular scoliosis: what's the difference?J Pediatr Orthop.2006;26(2):216–220.
- ,,, et al.Medical and surgical comanagement after elective hip and knee arthroplasty.Ann Intern Med.2004;141:28–38.
- ,,, et al.Effects of a hospitalist model on elderly patients with hip fracture.Arch Intern Med2005;165:796–801.
- ,,, et al.Factors predicting post‐operative complications following spinal fusion in children with cerebral palsy.J Spinal Disord.1999;12:297–305.
- ,,, et al.Neuromuscular scoliosis: clinical evaluation pre‐ and post‐operative.J Pediatr Orthop..2000;9(4):217–220.
As the field of pediatric hospital medicine has emerged, so too has evidence that hospitalist management of pediatric medical patients in the tertiary‐care setting is associated with decreased length of stay (LOS).13 The American Academy of Pediatrics Committee on Hospital Care has recommended hospitalist consultation for pediatric surgical patients being managed by adult surgeons.4 In one survey of pediatric hospitalists, 66% of community hospitalists and 47% of academic hospitalists reported comanaging surgical patients.5 However, little work has been published on the effect of hospitalist comanagement of pediatric surgical patients.
Since June 2000 patients undergoing spinal fusion surgery at the Children's Hospital in Denver, Colorado have been screened by a spine nurse for medical complexity. Medically complex patients undergoing preoperative multispecialty evaluation and their perioperative care are coordinated by the spine nurse.6 Introduction of a general pediatric hospitalist to aid with pre‐ and perioperative management of the most complicated patients in December 2004 provided us with an opportunity to study hospitalist comanagement of medically complex pediatric patients undergoing spine fusion surgery.
Our objectives were (1) to describe comanagement activities and (2) to determine the association of hospitalist comanagement on LOS following spinal fusion surgery. We hypothesized that by addressing a variety of pre‐ and perioperative medical issues, hospitalist comanagement would be associated with a decreased LOS for medically complex pediatric patients undergoing spinal fusion surgery.
METHODS
Design and Population
A retrospective analysis of the orthopedic surgeons' log at the Children's Hospital in Denver, Colorado, a tertiary‐care academic pediatric hospital serving the Rocky Mountain region, was performed. Patients included were those underwent their first episode of spinal fusion surgery between July 1, 2000, and October 1, 2005 (n = 759); exclusion criteria included diagnoses of spondylolisthesis or spondylolysis. The study was approved by the Colorado Multiple Institutional Review Board and exempted from ongoing review, and informed consent was not required.
Intervention: Pre‐ and Perioperative High‐Risk Pathway
Since June 2000 medically complex patients undergoing spinal fusion surgery at the Children's Hospital in Denver, Colorado have been referred by either the orthopedic surgeon or the rehabilitation physician to the spine surgery nurse. This nurse, an RN, BSN with more than a decade of experience with spinal fusion patients, then coordinates preoperative multispecialty evaluation (Fig. 1, column 2). Patients are seen by a pulmonologist pre‐operatively, and undergo pulmonary function tests, chest radiograph, venous blood gas, and, at times, a polysomnogram and electrocardiography. A cardiology consult is obtained for patients with muscle disease. Gastroenterology and neurology may be consulted if there are significant feeding and/or neurological issues that the primary care physician needs assistance addressing preoperatively. Shortly before the scheduled surgery, the patient is evaluated at a discharge planning meeting by a nutritionist, respiratory therapist, physical therapist, social worker (at times), and the spinal surgery nurse for discharge equipment planning. Immediately before surgery, in addition to teaching, surgical consent and a surgical history and physical are obtained, as well as laboratory studies that include a complete blood cell count, type, and cross, coagulation studies, and spine radiographs.5 Medically complex patients are managed in the intensive care unit for at least 24 hours after surgery. In addition, standardized order sets developed in 2001 and edited in July 2005 are used to streamline management of the intensive care unit and the orthopedic ward.

Since December 2004, a hospitalist has aided pre‐ and perioperative evaluation and management (Fig. 1, column 3). The patients seen and comanaged by the hospitalist have been those who have significant medical issues in addition to neuromuscular disease, including multiple medications, seizure disorders, nutritional concerns, and/or significant social concerns. Whereas patients with a multitude of different diagnoses were referred to the spinal surgery nurse for a variety of reasons, patients comanaged by hospitalists were generally children with multiple medical conditions who had neuromuscular scoliosis.
Data Sources
The primary data source used was the surgeons' log. The surgeons' log is a record of patients undergoing spinal fusion surgery maintained concurrently by 2 individuals (the spine surgery nurse and her assistant). From January 2000 on, patient data were manually input into an Excel spreadsheet regularly and were cross‐referenced weekly with the surgery schedule. Data entered include: patient name, medical record number, date of surgery, date of discharge (from hospital admission information), underlying diagnosis, type of procedure, primary surgeon (from operative and/or discharge summaries), and LOS (calculated from dates of discharge and surgery). If either underlying diagnosis or type of procedure needed clarification, the spine surgery nurse discussed it with the primary surgeon. We verified the completeness of the surgeons' log for first spinal fusion surgeries by cross‐referencing with billing records; of 572 surgeries performed by 5 surgeons, 571 were recorded (99.8%) in the surgeons' log.
To perform the descriptive analysis of hospitalist activities, the first author (T.S.) performed a retrospective review of the charts of patients she had seen in her role as hospitalist from December 1, 2004, to October 1, 2005. Prepared in advance was a checklist of pre‐ and perioperative activities, modeled on prior work reporting clinical activities.7 Activities either mentioned in the daily progress note or ordered were recorded as completed and entered into an Excel spreadsheet.
Data Collection
The outcome measure was LOS, log‐transformed for analyses. Covariates included were: patient age, underlying diagnosis, procedure type, and surgeon. Underlying diagnoses were subdivided on the basis of the manually input Excel spreadsheet entries into 5 categories: idiopathic, congenital, neuromuscular, osteogenic, and other. The major diagnoses in the idiopathic category were infantile, juvenile, and adolescent idiopathic scoliosis; in the congenital category were congenital scoliosis, congenital kyphoscoliosis; in the neuromuscular category were cerebral palsy, Duchenne's muscular dystrophy, spina bifida, brain injury, spinal cord injury, and chromosomal anomalies; and in the osteogenic category were Scheuermann's kyphosis, trauma, tumor, kyphoscoliosis, and bone disease. Procedures were subdivided according to the manually input Excel spreadsheet entries into 3 categories: posterior only, anterior/ posterior, and anterior spinal fusion only.
After our initial analysis demonstrated a decline in LOS after December 2004 in both idiopathic and neuromuscular patients, we asked the orthopedic surgeons and spine surgery nurse to determine cointerventions that may have occurred around December 2004. We attempted to contact each surgeon who performed surgery during the study period and asked, What changes did you make on or around November 2004 in your management of spinal fusion patients? We received e‐mail and verbal responses from the spine surgery nurse and from 6 surgeons who had performed 646 of the procedures (78%) over the study period.
Increased use of intrathecal morphine was raised as a possible confounding cointervention. To characterize use of intrathecal morphine, we reviewed the charts of all the patients categorized as idiopathic or neuromuscular patients who underwent surgery after December 2004 and a random sample of 20% of these patients who underwent surgery before December 2004.
Analyses
All quantitative analyses (ie, those of the surgeons' log) were performed in a blinded manner, whereas the chart review was not blinded. Univariate analyses of hospitalist activities and univariate and bivariate analyses of the surgeons' log were performed using SAS 9.1. Mean LOS after log back‐transformation along with 95% confidence interval is reported. The chi square test of equality of variance was used to analyze whether the variances differed.
The multifaceted approach to the care of spinal fusion patients is a tiered approach, with 3 major patient groups (Fig. 1): (1) patients with scoliosis, generally idiopathic, and no or minimal medical conditions, who receive care by the usual pathway and do not receive care by the high‐risk pathway or do not have a hospitalist; (2) patients with scoliosis with any underlying diagnosis and some medical conditions, who receive care by high‐risk pathway; and (3) patients with scoliosis, usually neuromuscular scoliosis, and multiple medical conditions, who receive care by the high‐risk pathway and have hospitalist comanagement. Because of selection bias in the receipt of hospitalist comanagement (ie, the most complicated patients), we cannot reasonably compare hospitalist patients to nonhospitalist patients after December 2004. Instead, we compared all neuromuscular patients before and after hospitalist comanagement with a control group of idiopathic patients.
Initial examination of mean monthly LOS from June 2000 to October 2005 (Fig. 2) suggested a possible decline in both mean LOS and variability in LOS after December 2004, when hospitalist comanagement was initiated. To determine the trend in LOS over time before and after December 2004, we performed a mixed‐effects piecewise Poisson regression, adjusting for patient covariates (patient age, underlying diagnosis, procedure type, and intrathecal morphine [for idiopathic and neuromuscular patients]) and clustering by surgeon (as a random effect). We used the model to estimate 2 slopes to represent the linear trend before and after December 2004 (when hospitalist comanagement started). After regression modeling generated beta coefficients for each covariate, the average covariates were entered into the model to generate an average adjusted LOS as shown in Figure 3.
RESULTS
A total of 759 patients underwent initial spinal fusion surgery between July 1, 2000, and October 1, 2005644 before and 115 after December 2004, when hospitalist involvement started. After December 2004, 12% (14 of 115) of all spinal fusion surgery patients were comanaged by a hospitalist. Most comanaged patients (14 of 15, 93%) had neuromuscular scoliosis, and comanaged patients represented 37% (13 of 35) of all neuromuscular patients (Table 1). Over the course of the study, the number of more invasive and complicated anterior/posterior spinal fusion surgeries declined, whereas the number of posterior spinal fusion surgeries increased significantly because of the introduction of new technology (data not shown).
| LOS Days (95% CI) | ||||
|---|---|---|---|---|
| All Surgeries | Preintervention (July 2000December 2004) | Postintervention (December 2004September 2005) | Hospitalist Comanaged (December 2004September 2005) | |
| ||||
| Number of surgeries | 759 | 644 | 115 | 14* |
| Age (years), mean (SD) | 13.6 (3.4) | 13.7 (3.4) | 13.1 (3.4) | 12.6 (4.0) |
| Diagnosis | ||||
| Idiopathic | 328 (43%) | 277 (43%) | 51 (44%) | 1 (7%) |
| Neuromuscular | 247 (32%) | 212 (33%) | 35 (30%) | 13 (93%) |
| Congenital | 66 (9%) | 55 (8%) | 11 (10%) | |
| Osteogenic | 96 (13%) | 81 (13%) | 15 (13%) | |
| Other | 22 (3%) | 19 (3%) | 3 (3%) | |
| Procedure | ||||
| Posterior | 470 (62%) | 365 (57%) | 105 (91%) | 13 (93%) |
| Ant/post | 227 (30%) | 217 (34%) | 10 (8%) | 1 (7%) |
| Anterior | 62 (8%) | 62 (9%) | ||
| Intrathecal morphine use | ||||
| Idiopathic | 30/50 (60%) | 45/51 (88%) | 0 (0%) | |
| Neuromuscular | 10/42 (24%) | 21/35 (62%) | 5/13 (38%) | |
The 15 patients seen by the hospitalist received a total of 60 visits by the hospitalist. The hospitalist saw 9 patients preoperatively. Of the 15 patients comanaged in the hospital, 5 (33%) were seen once, 8 (53%) were seen between 2 and 5 times, and 2 (14%) were seen more than 10 times. Patients were seen both in the ICU and on the surgical ward. Among the patients seen preoperatively, the hospitalist recommended nutritional interventions for 5 patients (33%), bowel regimens for 4 patients (27%), and preoperative hospitalization for 1 patient for 5 days to optimize nutritional intake, address reflux, and modify bowel regimen, as well as facilitate multispecialty evaluation. Postoperative involvement generally addressed a variety of issues, but 20% of patients had no changes in their management (Table 2).
| Hospitalist Activity | Number of Patients (%) (n = 15) |
|---|---|
| |
| Care coordination | |
| Updated family | 11 (73%) |
| Coordinated discharge | 8 (53%) |
| Updated PCP | 7 (47%) |
| Transfer facilitated | 4 (27%) |
| Consulted pulmonary | 3 (20%) |
| Consulted GI | 2 (13%) |
| Type of recommendation | |
| Home medications reviewed | 14 (93%) |
| Nutritional (ie, feed changes) | 11 (73%) |
| Pain medications reviewed | 11 (73%) |
| Bowel regimen | 10 (67%) |
| New medical issues* | 10 (67%) |
| Pain medications modified | 9 (60%) |
| Foley removed | 7 (46%) |
| Unnecessary medication removed | 6 (40%) |
| Central line removed | 4 (27%) |
| No changes in management | 3 (20%) |
| TPN | 2 (13%) |
| Harmful medications removed | 0 (0%) |
Initial examination of mean monthly LOS from June 2000 to October 2005 suggested a possible decline in both mean LOS and variability in LOS after hospitalist comanagement was initiated (Fig. 2). Mean LOS for all initial spinal fusion surgeries decreased from 6.5 days (95% CI: 6.26.7) to 4.8 days (95% CI: 4.55.1) after December 2004. The standard deviation in LOS for all initial spinal fusion surgeries decreased from 1.64 to 1.39 days (P < .0001; Table 3). In the 52 months prior to hospitalist comanagement, there was no change in adjusted LOS over time (slope = 0.009 days/month, P = .3997). After December 2004, there was a significant decline in average adjusted LOS (slope = 0.2 days/month; P < .0001).
| Before Hospitalist 7/0012/04 n=644 | After Hospitalist After 12/04 n=115 | p value | |
|---|---|---|---|
| LOS Days (95% CI) | |||
| All Initial Spinal Fusion Surgeries | 6.5 (6.26.7) | 4.8 (4.55.1) | |
| Idiopathic | 5.2 (5.05.4) | 4.1(3.94.4) | |
| Neuromuscular | 8.6 (8.09.2) | 6.25 (5.56.9) | |
| Standard Deviation Days | |||
| All Initial Spinal Fusion Surgeries | 1.64 | 1.39 | <0.0001 |
| Idiopathic | 1.35 | 1.26 | 0.03 |
| Neuromuscular | 1.70 | 1.41 | 0.002 |
Mean and adjusted LOS of patients in the 2 main diagnostic categories, idiopathic and neuromuscular scoliosis, decreased. The absolute mean LOS decreased more for neuromuscular patients (8.6 days [95% CI: 8.09.2] to 6.2 days [95% CI: 5.56.9]) than for idiopathic patients (5.2 days [95% CI: 5.05.4] to 4.1 days [95% CI: 3.94.4]). The standard deviation in LOS decreased more for the neuromuscular patients, from 1.70 to 1.41 days (P = .002), as shown in Table 3. In the 52 months prior to hospitalist comanagement, there was no change in adjusted LOS over time (neuromuscular slope = 0.024 to 0.027 days/month, P = .49; idiopathic slope = 0.0005 days/month, P = .96). After December 2004, there was a significant decline in average adjusted LOS (neuromuscular slope = 0.23 to 0.31 days/month, P = .0075; idiopathic slope = 0.10 to 0.12 days/month; P = .0007), as demonstrated in Figure 3. A survey of the orthopedic surgical staff demonstrated no known specific changes in surgical or postoperative management initiated around December 2004 other than intrathecal morphine use. Some surgeons performed fewer surgeries, particularly of idiopathic patients.
DISCUSSION
The introduction of hospitalist comanagement to ongoing multispecialty evaluation for medically complex spinal fusion surgery patients was associated with a decrease in mean LOS among all patients undergoing initial spinal fusion surgery. A greater magnitude of decline in LOS was seen among children with neuromuscular scoliosis, who were often comanaged, than among children with idiopathic scoliosis, who were rarely comanaged. Variability in LOS also decreased following initiation of hospitalist comanagement, particularly in the more complex patients. The decreases in LOS persisted after adjustment for patient age, diagnosis, procedure type, intrathecal morphine use, and surgeon. This study provides support for the hypothesis that selective hospitalist comanagement of pediatric surgical patients in the tertiary‐care setting is associated with decreased LOS and decreased variability in LOS.
Analysis of a nationally representative data set demonstrated that 4504 children with idiopathic scoliosis and 1570 children with neuromuscular scoliosis underwent spinal fusion surgery in the United States in 2000.8 The average LOS for children with neuromuscular scoliosis was 9.2 days versus 6.1 days for those with idiopathic scoliosis. The LOS of both our patient populations, those before hospitalist comanagement and those after hospitalist comanagement, was less than the national estimates. Multidisciplinary management strategies with or without hospitalist comanagement may be associated with decreases in LOS for neuromuscular scoliosis patients undergoing spinal fusion surgery.
The hospitalist performed a variety of activities in comanaging the medically complex pediatric orthopedic patients. Hospitalist comanagement may have been associated with reduction in LOS for several reasons: preoperative prevention of medical problems, early postoperative identification of and intervention on medical complications, improved coordination of care, or simply consistency of postoperative medical care.
These findings are consistent with the pediatric nonsurgical literature, which suggests that hospitalist management of pediatric medical patients in the tertiary‐care setting is associated with decreased LOS.13 Hospitalist comanagement of adult orthopedic patients has been better studied than has been comanagement of pediatric patients. Elderly patients undergoing elective hip or knee arthroplasty were randomized to hospitalist care versus traditional orthopedic care after surgery. Both sets of patients were managed by the same nursing staff according to standardized care pathways. The mean LOS did not differ between the 2 groups, but the adjusted LOS was lower in the group that received hospitalist care.9 When the same center examined outcomes in hip fracture patients before and after implementation of a hospitalist care model, there was a decrease in LOS and no change in readmission or deaths.10 As in these studies, spinal fusion surgery management is highly standardized in our center. Nonetheless, hospitalist comanagement still was associated with a decreased LOS.
This study found a decline in LOS among all patients undergoing spinal fusion surgery, even among children with idiopathic scoliosis, of whom only 1 was comanaged. This finding may suggest hospitalist comanagement had a global, or indirect, effect on the management of all postoperative patients. However, the time‐series design could have been biased by a cointervention implemented at the same time as hospitalist care. Some surgeons performed fewer surgeries on their idiopathic patients over the course of the study; however, we adjusted for that surgeon in our analysis. Intrathecal morphine use is the only known change in postoperative management that may have affected care starting in December 2004; we also adjusted for intrathecal morphine use in our analysis. There may be other changes of which we are unaware. Nonetheless, the decline in LOS seen in the idiopathic population was exceeded by the decline in LOS in the comanaged neuromuscular population.
Unlike earlier reported studies, which examined hospitalist management among pediatric medical patients, this study did not assess complications (such as pneumonia, respiratory failure, urinary tract infection, gastric ulcers, pathologic fractures, poor wound healing, nutritional compromise, and readmission),7, 11, 12 costs, or patient and provider satisfaction with hospitalist comanagement.13 This assessment is critical to defining the value of these services to patients and providers. In addition, because we did not collect information on severity of disability, we were unable to control for disability. These are other covariates and outcomes of interest that should be assessed in future studies. Furthermore, there was potential bias introduced by having the lead author both conducting the study and performing the intervention; this was minimized by having different individuals responsible for primary data collection and having the analyses performed in a blinded fashion. In addition, although this study provided promising initial evidence that selective hospitalist comanagement along with multispecialty evaluation of spinal fusion surgery patients may lead to a significant decrease in LOS, this evidence needs to be replicated in other surgical patient populations and hospital settings. Ideally, the impact of hospitalist comanagement should be more fully evaluated in a randomized controlled trial. Hospitalist comanagement is a promising technique for improving the care of children undergoing spinal fusion surgery, particularly those with complex medical conditions.
Acknowledgements
The authors acknowledge the contributions of Heidi Gullord of University Physician, Incorporated, for assistance with obtaining billing records. We also appreciate the ongoing input of the Children's Hospital Department of Epidemiology, including Lorna Dyk, BSN, MBA; Michael Rannie, RN, MS; Meghan Birkholz, MSPH; and Michael Kahn, MD, PhD. We appreciate the willingness of the Department of Orthopedics to cooperate with this study, including (but not limited to) Mark Erickson, MD; Frank Chang, MD; and Gaia Georgopoulos, MD. In addition, we acknowledge the ongoing efforts of the care providers involved in the High Risk Pathway at the Children's Hospital, including Carol Page, PT; Alice Radic, PTA; Sarah Hack Baltazar, RD; Monte Leidholm, RRT; Cloy Vaneman, RRT; Gail Shattuck, MSW; and Lynn Katz, MSW, as well as the Divisions of Pulmonary Medicine and Intensive Care of the Department of Pediatrics. We also thank Heather Ramey, BS, BA, for her assistance with organizing the multispecialty evaluation of patients undergoing surgery. We also appreciate the efforts of the fellows and faculty of the Primary Care Research Fellowship and appreciate their assistance in crafting this research.
As the field of pediatric hospital medicine has emerged, so too has evidence that hospitalist management of pediatric medical patients in the tertiary‐care setting is associated with decreased length of stay (LOS).13 The American Academy of Pediatrics Committee on Hospital Care has recommended hospitalist consultation for pediatric surgical patients being managed by adult surgeons.4 In one survey of pediatric hospitalists, 66% of community hospitalists and 47% of academic hospitalists reported comanaging surgical patients.5 However, little work has been published on the effect of hospitalist comanagement of pediatric surgical patients.
Since June 2000 patients undergoing spinal fusion surgery at the Children's Hospital in Denver, Colorado have been screened by a spine nurse for medical complexity. Medically complex patients undergoing preoperative multispecialty evaluation and their perioperative care are coordinated by the spine nurse.6 Introduction of a general pediatric hospitalist to aid with pre‐ and perioperative management of the most complicated patients in December 2004 provided us with an opportunity to study hospitalist comanagement of medically complex pediatric patients undergoing spine fusion surgery.
Our objectives were (1) to describe comanagement activities and (2) to determine the association of hospitalist comanagement on LOS following spinal fusion surgery. We hypothesized that by addressing a variety of pre‐ and perioperative medical issues, hospitalist comanagement would be associated with a decreased LOS for medically complex pediatric patients undergoing spinal fusion surgery.
METHODS
Design and Population
A retrospective analysis of the orthopedic surgeons' log at the Children's Hospital in Denver, Colorado, a tertiary‐care academic pediatric hospital serving the Rocky Mountain region, was performed. Patients included were those underwent their first episode of spinal fusion surgery between July 1, 2000, and October 1, 2005 (n = 759); exclusion criteria included diagnoses of spondylolisthesis or spondylolysis. The study was approved by the Colorado Multiple Institutional Review Board and exempted from ongoing review, and informed consent was not required.
Intervention: Pre‐ and Perioperative High‐Risk Pathway
Since June 2000 medically complex patients undergoing spinal fusion surgery at the Children's Hospital in Denver, Colorado have been referred by either the orthopedic surgeon or the rehabilitation physician to the spine surgery nurse. This nurse, an RN, BSN with more than a decade of experience with spinal fusion patients, then coordinates preoperative multispecialty evaluation (Fig. 1, column 2). Patients are seen by a pulmonologist pre‐operatively, and undergo pulmonary function tests, chest radiograph, venous blood gas, and, at times, a polysomnogram and electrocardiography. A cardiology consult is obtained for patients with muscle disease. Gastroenterology and neurology may be consulted if there are significant feeding and/or neurological issues that the primary care physician needs assistance addressing preoperatively. Shortly before the scheduled surgery, the patient is evaluated at a discharge planning meeting by a nutritionist, respiratory therapist, physical therapist, social worker (at times), and the spinal surgery nurse for discharge equipment planning. Immediately before surgery, in addition to teaching, surgical consent and a surgical history and physical are obtained, as well as laboratory studies that include a complete blood cell count, type, and cross, coagulation studies, and spine radiographs.5 Medically complex patients are managed in the intensive care unit for at least 24 hours after surgery. In addition, standardized order sets developed in 2001 and edited in July 2005 are used to streamline management of the intensive care unit and the orthopedic ward.

Since December 2004, a hospitalist has aided pre‐ and perioperative evaluation and management (Fig. 1, column 3). The patients seen and comanaged by the hospitalist have been those who have significant medical issues in addition to neuromuscular disease, including multiple medications, seizure disorders, nutritional concerns, and/or significant social concerns. Whereas patients with a multitude of different diagnoses were referred to the spinal surgery nurse for a variety of reasons, patients comanaged by hospitalists were generally children with multiple medical conditions who had neuromuscular scoliosis.
Data Sources
The primary data source used was the surgeons' log. The surgeons' log is a record of patients undergoing spinal fusion surgery maintained concurrently by 2 individuals (the spine surgery nurse and her assistant). From January 2000 on, patient data were manually input into an Excel spreadsheet regularly and were cross‐referenced weekly with the surgery schedule. Data entered include: patient name, medical record number, date of surgery, date of discharge (from hospital admission information), underlying diagnosis, type of procedure, primary surgeon (from operative and/or discharge summaries), and LOS (calculated from dates of discharge and surgery). If either underlying diagnosis or type of procedure needed clarification, the spine surgery nurse discussed it with the primary surgeon. We verified the completeness of the surgeons' log for first spinal fusion surgeries by cross‐referencing with billing records; of 572 surgeries performed by 5 surgeons, 571 were recorded (99.8%) in the surgeons' log.
To perform the descriptive analysis of hospitalist activities, the first author (T.S.) performed a retrospective review of the charts of patients she had seen in her role as hospitalist from December 1, 2004, to October 1, 2005. Prepared in advance was a checklist of pre‐ and perioperative activities, modeled on prior work reporting clinical activities.7 Activities either mentioned in the daily progress note or ordered were recorded as completed and entered into an Excel spreadsheet.
Data Collection
The outcome measure was LOS, log‐transformed for analyses. Covariates included were: patient age, underlying diagnosis, procedure type, and surgeon. Underlying diagnoses were subdivided on the basis of the manually input Excel spreadsheet entries into 5 categories: idiopathic, congenital, neuromuscular, osteogenic, and other. The major diagnoses in the idiopathic category were infantile, juvenile, and adolescent idiopathic scoliosis; in the congenital category were congenital scoliosis, congenital kyphoscoliosis; in the neuromuscular category were cerebral palsy, Duchenne's muscular dystrophy, spina bifida, brain injury, spinal cord injury, and chromosomal anomalies; and in the osteogenic category were Scheuermann's kyphosis, trauma, tumor, kyphoscoliosis, and bone disease. Procedures were subdivided according to the manually input Excel spreadsheet entries into 3 categories: posterior only, anterior/ posterior, and anterior spinal fusion only.
After our initial analysis demonstrated a decline in LOS after December 2004 in both idiopathic and neuromuscular patients, we asked the orthopedic surgeons and spine surgery nurse to determine cointerventions that may have occurred around December 2004. We attempted to contact each surgeon who performed surgery during the study period and asked, What changes did you make on or around November 2004 in your management of spinal fusion patients? We received e‐mail and verbal responses from the spine surgery nurse and from 6 surgeons who had performed 646 of the procedures (78%) over the study period.
Increased use of intrathecal morphine was raised as a possible confounding cointervention. To characterize use of intrathecal morphine, we reviewed the charts of all the patients categorized as idiopathic or neuromuscular patients who underwent surgery after December 2004 and a random sample of 20% of these patients who underwent surgery before December 2004.
Analyses
All quantitative analyses (ie, those of the surgeons' log) were performed in a blinded manner, whereas the chart review was not blinded. Univariate analyses of hospitalist activities and univariate and bivariate analyses of the surgeons' log were performed using SAS 9.1. Mean LOS after log back‐transformation along with 95% confidence interval is reported. The chi square test of equality of variance was used to analyze whether the variances differed.
The multifaceted approach to the care of spinal fusion patients is a tiered approach, with 3 major patient groups (Fig. 1): (1) patients with scoliosis, generally idiopathic, and no or minimal medical conditions, who receive care by the usual pathway and do not receive care by the high‐risk pathway or do not have a hospitalist; (2) patients with scoliosis with any underlying diagnosis and some medical conditions, who receive care by high‐risk pathway; and (3) patients with scoliosis, usually neuromuscular scoliosis, and multiple medical conditions, who receive care by the high‐risk pathway and have hospitalist comanagement. Because of selection bias in the receipt of hospitalist comanagement (ie, the most complicated patients), we cannot reasonably compare hospitalist patients to nonhospitalist patients after December 2004. Instead, we compared all neuromuscular patients before and after hospitalist comanagement with a control group of idiopathic patients.
Initial examination of mean monthly LOS from June 2000 to October 2005 (Fig. 2) suggested a possible decline in both mean LOS and variability in LOS after December 2004, when hospitalist comanagement was initiated. To determine the trend in LOS over time before and after December 2004, we performed a mixed‐effects piecewise Poisson regression, adjusting for patient covariates (patient age, underlying diagnosis, procedure type, and intrathecal morphine [for idiopathic and neuromuscular patients]) and clustering by surgeon (as a random effect). We used the model to estimate 2 slopes to represent the linear trend before and after December 2004 (when hospitalist comanagement started). After regression modeling generated beta coefficients for each covariate, the average covariates were entered into the model to generate an average adjusted LOS as shown in Figure 3.
RESULTS
A total of 759 patients underwent initial spinal fusion surgery between July 1, 2000, and October 1, 2005644 before and 115 after December 2004, when hospitalist involvement started. After December 2004, 12% (14 of 115) of all spinal fusion surgery patients were comanaged by a hospitalist. Most comanaged patients (14 of 15, 93%) had neuromuscular scoliosis, and comanaged patients represented 37% (13 of 35) of all neuromuscular patients (Table 1). Over the course of the study, the number of more invasive and complicated anterior/posterior spinal fusion surgeries declined, whereas the number of posterior spinal fusion surgeries increased significantly because of the introduction of new technology (data not shown).
| LOS Days (95% CI) | ||||
|---|---|---|---|---|
| All Surgeries | Preintervention (July 2000December 2004) | Postintervention (December 2004September 2005) | Hospitalist Comanaged (December 2004September 2005) | |
| ||||
| Number of surgeries | 759 | 644 | 115 | 14* |
| Age (years), mean (SD) | 13.6 (3.4) | 13.7 (3.4) | 13.1 (3.4) | 12.6 (4.0) |
| Diagnosis | ||||
| Idiopathic | 328 (43%) | 277 (43%) | 51 (44%) | 1 (7%) |
| Neuromuscular | 247 (32%) | 212 (33%) | 35 (30%) | 13 (93%) |
| Congenital | 66 (9%) | 55 (8%) | 11 (10%) | |
| Osteogenic | 96 (13%) | 81 (13%) | 15 (13%) | |
| Other | 22 (3%) | 19 (3%) | 3 (3%) | |
| Procedure | ||||
| Posterior | 470 (62%) | 365 (57%) | 105 (91%) | 13 (93%) |
| Ant/post | 227 (30%) | 217 (34%) | 10 (8%) | 1 (7%) |
| Anterior | 62 (8%) | 62 (9%) | ||
| Intrathecal morphine use | ||||
| Idiopathic | 30/50 (60%) | 45/51 (88%) | 0 (0%) | |
| Neuromuscular | 10/42 (24%) | 21/35 (62%) | 5/13 (38%) | |
The 15 patients seen by the hospitalist received a total of 60 visits by the hospitalist. The hospitalist saw 9 patients preoperatively. Of the 15 patients comanaged in the hospital, 5 (33%) were seen once, 8 (53%) were seen between 2 and 5 times, and 2 (14%) were seen more than 10 times. Patients were seen both in the ICU and on the surgical ward. Among the patients seen preoperatively, the hospitalist recommended nutritional interventions for 5 patients (33%), bowel regimens for 4 patients (27%), and preoperative hospitalization for 1 patient for 5 days to optimize nutritional intake, address reflux, and modify bowel regimen, as well as facilitate multispecialty evaluation. Postoperative involvement generally addressed a variety of issues, but 20% of patients had no changes in their management (Table 2).
| Hospitalist Activity | Number of Patients (%) (n = 15) |
|---|---|
| |
| Care coordination | |
| Updated family | 11 (73%) |
| Coordinated discharge | 8 (53%) |
| Updated PCP | 7 (47%) |
| Transfer facilitated | 4 (27%) |
| Consulted pulmonary | 3 (20%) |
| Consulted GI | 2 (13%) |
| Type of recommendation | |
| Home medications reviewed | 14 (93%) |
| Nutritional (ie, feed changes) | 11 (73%) |
| Pain medications reviewed | 11 (73%) |
| Bowel regimen | 10 (67%) |
| New medical issues* | 10 (67%) |
| Pain medications modified | 9 (60%) |
| Foley removed | 7 (46%) |
| Unnecessary medication removed | 6 (40%) |
| Central line removed | 4 (27%) |
| No changes in management | 3 (20%) |
| TPN | 2 (13%) |
| Harmful medications removed | 0 (0%) |
Initial examination of mean monthly LOS from June 2000 to October 2005 suggested a possible decline in both mean LOS and variability in LOS after hospitalist comanagement was initiated (Fig. 2). Mean LOS for all initial spinal fusion surgeries decreased from 6.5 days (95% CI: 6.26.7) to 4.8 days (95% CI: 4.55.1) after December 2004. The standard deviation in LOS for all initial spinal fusion surgeries decreased from 1.64 to 1.39 days (P < .0001; Table 3). In the 52 months prior to hospitalist comanagement, there was no change in adjusted LOS over time (slope = 0.009 days/month, P = .3997). After December 2004, there was a significant decline in average adjusted LOS (slope = 0.2 days/month; P < .0001).
| Before Hospitalist 7/0012/04 n=644 | After Hospitalist After 12/04 n=115 | p value | |
|---|---|---|---|
| LOS Days (95% CI) | |||
| All Initial Spinal Fusion Surgeries | 6.5 (6.26.7) | 4.8 (4.55.1) | |
| Idiopathic | 5.2 (5.05.4) | 4.1(3.94.4) | |
| Neuromuscular | 8.6 (8.09.2) | 6.25 (5.56.9) | |
| Standard Deviation Days | |||
| All Initial Spinal Fusion Surgeries | 1.64 | 1.39 | <0.0001 |
| Idiopathic | 1.35 | 1.26 | 0.03 |
| Neuromuscular | 1.70 | 1.41 | 0.002 |
Mean and adjusted LOS of patients in the 2 main diagnostic categories, idiopathic and neuromuscular scoliosis, decreased. The absolute mean LOS decreased more for neuromuscular patients (8.6 days [95% CI: 8.09.2] to 6.2 days [95% CI: 5.56.9]) than for idiopathic patients (5.2 days [95% CI: 5.05.4] to 4.1 days [95% CI: 3.94.4]). The standard deviation in LOS decreased more for the neuromuscular patients, from 1.70 to 1.41 days (P = .002), as shown in Table 3. In the 52 months prior to hospitalist comanagement, there was no change in adjusted LOS over time (neuromuscular slope = 0.024 to 0.027 days/month, P = .49; idiopathic slope = 0.0005 days/month, P = .96). After December 2004, there was a significant decline in average adjusted LOS (neuromuscular slope = 0.23 to 0.31 days/month, P = .0075; idiopathic slope = 0.10 to 0.12 days/month; P = .0007), as demonstrated in Figure 3. A survey of the orthopedic surgical staff demonstrated no known specific changes in surgical or postoperative management initiated around December 2004 other than intrathecal morphine use. Some surgeons performed fewer surgeries, particularly of idiopathic patients.
DISCUSSION
The introduction of hospitalist comanagement to ongoing multispecialty evaluation for medically complex spinal fusion surgery patients was associated with a decrease in mean LOS among all patients undergoing initial spinal fusion surgery. A greater magnitude of decline in LOS was seen among children with neuromuscular scoliosis, who were often comanaged, than among children with idiopathic scoliosis, who were rarely comanaged. Variability in LOS also decreased following initiation of hospitalist comanagement, particularly in the more complex patients. The decreases in LOS persisted after adjustment for patient age, diagnosis, procedure type, intrathecal morphine use, and surgeon. This study provides support for the hypothesis that selective hospitalist comanagement of pediatric surgical patients in the tertiary‐care setting is associated with decreased LOS and decreased variability in LOS.
Analysis of a nationally representative data set demonstrated that 4504 children with idiopathic scoliosis and 1570 children with neuromuscular scoliosis underwent spinal fusion surgery in the United States in 2000.8 The average LOS for children with neuromuscular scoliosis was 9.2 days versus 6.1 days for those with idiopathic scoliosis. The LOS of both our patient populations, those before hospitalist comanagement and those after hospitalist comanagement, was less than the national estimates. Multidisciplinary management strategies with or without hospitalist comanagement may be associated with decreases in LOS for neuromuscular scoliosis patients undergoing spinal fusion surgery.
The hospitalist performed a variety of activities in comanaging the medically complex pediatric orthopedic patients. Hospitalist comanagement may have been associated with reduction in LOS for several reasons: preoperative prevention of medical problems, early postoperative identification of and intervention on medical complications, improved coordination of care, or simply consistency of postoperative medical care.
These findings are consistent with the pediatric nonsurgical literature, which suggests that hospitalist management of pediatric medical patients in the tertiary‐care setting is associated with decreased LOS.13 Hospitalist comanagement of adult orthopedic patients has been better studied than has been comanagement of pediatric patients. Elderly patients undergoing elective hip or knee arthroplasty were randomized to hospitalist care versus traditional orthopedic care after surgery. Both sets of patients were managed by the same nursing staff according to standardized care pathways. The mean LOS did not differ between the 2 groups, but the adjusted LOS was lower in the group that received hospitalist care.9 When the same center examined outcomes in hip fracture patients before and after implementation of a hospitalist care model, there was a decrease in LOS and no change in readmission or deaths.10 As in these studies, spinal fusion surgery management is highly standardized in our center. Nonetheless, hospitalist comanagement still was associated with a decreased LOS.
This study found a decline in LOS among all patients undergoing spinal fusion surgery, even among children with idiopathic scoliosis, of whom only 1 was comanaged. This finding may suggest hospitalist comanagement had a global, or indirect, effect on the management of all postoperative patients. However, the time‐series design could have been biased by a cointervention implemented at the same time as hospitalist care. Some surgeons performed fewer surgeries on their idiopathic patients over the course of the study; however, we adjusted for that surgeon in our analysis. Intrathecal morphine use is the only known change in postoperative management that may have affected care starting in December 2004; we also adjusted for intrathecal morphine use in our analysis. There may be other changes of which we are unaware. Nonetheless, the decline in LOS seen in the idiopathic population was exceeded by the decline in LOS in the comanaged neuromuscular population.
Unlike earlier reported studies, which examined hospitalist management among pediatric medical patients, this study did not assess complications (such as pneumonia, respiratory failure, urinary tract infection, gastric ulcers, pathologic fractures, poor wound healing, nutritional compromise, and readmission),7, 11, 12 costs, or patient and provider satisfaction with hospitalist comanagement.13 This assessment is critical to defining the value of these services to patients and providers. In addition, because we did not collect information on severity of disability, we were unable to control for disability. These are other covariates and outcomes of interest that should be assessed in future studies. Furthermore, there was potential bias introduced by having the lead author both conducting the study and performing the intervention; this was minimized by having different individuals responsible for primary data collection and having the analyses performed in a blinded fashion. In addition, although this study provided promising initial evidence that selective hospitalist comanagement along with multispecialty evaluation of spinal fusion surgery patients may lead to a significant decrease in LOS, this evidence needs to be replicated in other surgical patient populations and hospital settings. Ideally, the impact of hospitalist comanagement should be more fully evaluated in a randomized controlled trial. Hospitalist comanagement is a promising technique for improving the care of children undergoing spinal fusion surgery, particularly those with complex medical conditions.
Acknowledgements
The authors acknowledge the contributions of Heidi Gullord of University Physician, Incorporated, for assistance with obtaining billing records. We also appreciate the ongoing input of the Children's Hospital Department of Epidemiology, including Lorna Dyk, BSN, MBA; Michael Rannie, RN, MS; Meghan Birkholz, MSPH; and Michael Kahn, MD, PhD. We appreciate the willingness of the Department of Orthopedics to cooperate with this study, including (but not limited to) Mark Erickson, MD; Frank Chang, MD; and Gaia Georgopoulos, MD. In addition, we acknowledge the ongoing efforts of the care providers involved in the High Risk Pathway at the Children's Hospital, including Carol Page, PT; Alice Radic, PTA; Sarah Hack Baltazar, RD; Monte Leidholm, RRT; Cloy Vaneman, RRT; Gail Shattuck, MSW; and Lynn Katz, MSW, as well as the Divisions of Pulmonary Medicine and Intensive Care of the Department of Pediatrics. We also thank Heather Ramey, BS, BA, for her assistance with organizing the multispecialty evaluation of patients undergoing surgery. We also appreciate the efforts of the fellows and faculty of the Primary Care Research Fellowship and appreciate their assistance in crafting this research.
- ,.Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges.Pediatrics.2000;105:478–484.
- ,,, et al.Impact of a health maintenance organization hospitalist system in academic pediatrics.Pediatrics.2002;110:720–728.
- ,,,.Evaluation of a staff‐only hospitalist system in a tertiary care, academic children's hospital.Pediatrics.2004;114:1545–1549.
- and theCommittee on Hospital Care.Physicians' roles in coordinating care of hospitalized children.Pediatrics.2003;111:707–709.
- and.Differences in work environment, responsibilities, and training need between community hospital and academic center hospitalists. E‐PAS2006:59:4128.3.
- ,.Development and implementation of a spine fusion high risk pathway. 5th Annual Pre‐Brandon Carrell Pediatric Orthopaedic Symposium for Nursing and Allied Healthcare Professionals, Texas Scottish Rite Hospital for Children, Dallas, Texas, June 26,2003.
- ,,,.Reducing delirium after hip fracture: a randomized trial.J Am Geriatr Soc.2001;49:516–522.
- ,,, et al.Spinal fusion in children with idiopathic and neuromuscular scoliosis: what's the difference?J Pediatr Orthop.2006;26(2):216–220.
- ,,, et al.Medical and surgical comanagement after elective hip and knee arthroplasty.Ann Intern Med.2004;141:28–38.
- ,,, et al.Effects of a hospitalist model on elderly patients with hip fracture.Arch Intern Med2005;165:796–801.
- ,,, et al.Factors predicting post‐operative complications following spinal fusion in children with cerebral palsy.J Spinal Disord.1999;12:297–305.
- ,,, et al.Neuromuscular scoliosis: clinical evaluation pre‐ and post‐operative.J Pediatr Orthop..2000;9(4):217–220.
- ,.Evaluation of a pediatric hospitalist service: impact on length of stay and hospital charges.Pediatrics.2000;105:478–484.
- ,,, et al.Impact of a health maintenance organization hospitalist system in academic pediatrics.Pediatrics.2002;110:720–728.
- ,,,.Evaluation of a staff‐only hospitalist system in a tertiary care, academic children's hospital.Pediatrics.2004;114:1545–1549.
- and theCommittee on Hospital Care.Physicians' roles in coordinating care of hospitalized children.Pediatrics.2003;111:707–709.
- and.Differences in work environment, responsibilities, and training need between community hospital and academic center hospitalists. E‐PAS2006:59:4128.3.
- ,.Development and implementation of a spine fusion high risk pathway. 5th Annual Pre‐Brandon Carrell Pediatric Orthopaedic Symposium for Nursing and Allied Healthcare Professionals, Texas Scottish Rite Hospital for Children, Dallas, Texas, June 26,2003.
- ,,,.Reducing delirium after hip fracture: a randomized trial.J Am Geriatr Soc.2001;49:516–522.
- ,,, et al.Spinal fusion in children with idiopathic and neuromuscular scoliosis: what's the difference?J Pediatr Orthop.2006;26(2):216–220.
- ,,, et al.Medical and surgical comanagement after elective hip and knee arthroplasty.Ann Intern Med.2004;141:28–38.
- ,,, et al.Effects of a hospitalist model on elderly patients with hip fracture.Arch Intern Med2005;165:796–801.
- ,,, et al.Factors predicting post‐operative complications following spinal fusion in children with cerebral palsy.J Spinal Disord.1999;12:297–305.
- ,,, et al.Neuromuscular scoliosis: clinical evaluation pre‐ and post‐operative.J Pediatr Orthop..2000;9(4):217–220.
Copyright © 2007 Society of Hospital Medicine