User login
Is Patient Satisfaction the Same Immediately After the First Visit Compared to Two Weeks Later?
From the Department of Surgery and Perioperative Care, Dell Medical School, The University of Texas at Austin, Austin, TX (Dr. Kortlever, Ms. Haidar, Dr. Reichel, Dr. Driscoll, Dr. Ring, and Dr. Vagner) and University Medical Center Utrecht, Utrecht, The Netherlands (Dr. Teunis).
Abstract
- Objective: Patient satisfaction is considered a quality measure. Satisfaction is typically measured directly after an in-person visit in research and 2 weeks later in practice surveys. We assessed if there was a difference in immediate and delayed measurement of satisfaction.
- Questions: (1) There is no difference in patient satisfaction (measured by Numerical Rating Scale [NRS]) and (2) perceived empathy (measured by the Jefferson Scale of Patient Perceptions of Physician Empathy [JSPPPE]) immediately after the initial visit compared to 2 weeks later. (3) Change in disability (measured by the Patient-Reported Outcome Measurement Information System Physical Function-Upper Extremity [PROMIS PF-UE]) is not independently associated with change in satisfaction and (4) empathy after the initial visit compared to 2 weeks later.
- Methods: 150 new patients completed a survey of demographics, satisfaction with the surgeon, rating of the surgeon’s empathy, and upper extremity specific limitations. The satisfaction, empathy, and limitation questionnaires were repeated 2 weeks later.
- Results: We found a slight but significant decrease in satisfaction 2 weeks after the in-person visit (–0.41, P = 0.001). There was no significant change in perceived empathy (–0.71, P = 0.19). Change in limitations did not account for a change in satisfaction (P = 0.79) or perceived empathy (P = 0.93).
- Conclusion: Satisfaction and perceived empathy are relatively stable constructs that can be measured immediately after the visit.
Keywords: satisfaction, empathy, change, upper extremity, disability.
Patient satisfaction is increasingly being used as a performance measure to evaluate quality of care.1-8 Patient satisfaction correlates with adherence with recommended treatment.1,6,8-10 Satisfaction measured on an 11-point ordinal scale immediately after the visit correlates strongly with the perception of clinician empathy.2,3 Indeed, some satisfaction questionnaires such as the Medical Interview Satisfaction Scale (MISS)11,12 have questions very similar to empathy questionnaires. It may be that satisfaction is a construct similar to feeling that your doctor listened and cared about you as an individual (perceived physician empathy).
Higher ratings of satisfaction also seem to be related to a physician’s communication style.1,4,7-10 One study of 13 fertility doctors found that training in effective communication strategies led to improved patient satisfaction.7 A qualitative study of 36 patients, health professionals, and clinical support staff in an orthopaedic outpatient setting held interviews and focus group sessions to identify themes influencing patient satisfaction.4 Communication and expectation were among the 7 themes identified. We have noticed a high ceiling effect (maximum scores) with measures of patient satisfaction and perceived empathy.2,3 Another study also noted a high ceiling effect when using an ordinal scale.5 It may be that people with a positive feeling shortly after a health care encounter give top ratings out of politeness or gratefulness. It is also possible they will feel differently a few weeks after they leave the office. Furthermore, ratings of satisfaction gathered by a practice or health care system for practice assessment/improvement are often obtained several days to weeks after the visit, while research often obtains satisfaction ratings immediately after the visit for practical reasons. There may be differences between immediate and delayed measurement of satisfaction beyond the mentioned social norms.
Therefore, this study tested the primary null hypothesis that there is no difference in patient satisfaction (measured by Numerical Rating Scale [NRS]) immediately after the initial visit compared to 2 weeks later. Additionally, we assessed the difference in perceived empathy immediately after the initial visit compared to 2 weeks later, and whether change in disability was independently associated with change in satisfaction and empathy after the initial visit compared to 2 weeks later.
Methods
Study Design
After Institutional Review Board approval of this prospective, longitudinal, observational cohort study, we prospectively enrolled 150 adult patients between November 29, 2017 and January 10, 2018. Patients were seen at 5 orthopaedic clinics in a large urban area. We included all new English-speaking patients aged 18 to 89 years who were visiting 1 of 6 participating orthopaedic surgeons for any upper extremity problem and who were able to provide informed consent. We excluded follow-up visits and patients who were unable to speak and understand English. Four research assistants who were not involved with patient treatment described the study to patients before or after the visit with the surgeon. We were granted a waiver of written informed consent; patients indicated their consent by completing the surveys.
Patients could choose either phone or email as their preferred mode of contact for follow-up in this study. For patients who selected email as the preferred mode of contact, the follow-up survey was sent automatically 2 weeks after completion date, and a maximum of 3 reminder emails with 2-day time intervals between them were sent to those who did not respond to the initial invitation. For patients who selected phone as the preferred mode of contact, the follow-up survey was done by an English-speaking research assistant who was not involved with patient treatment. When a response was not obtained on the initial phone call, 3 additional phone calls were made (1 later that same day and 2 the next day). One patient declined participation because he was not interested in the study and had no time after his visit.
Measurements
Patients were asked to complete a set of questionnaires at the end of their visit:
1. A demographic questionnaire consisting of preferred mode of contact for follow-up (phone or email), age, sex, race/ethnicity, marital status, education status, work status, insurance status, and type of visit (first visit or second opinion);
2. An 11-point ordinal measure of satisfaction with the surgeon, with scores ranging from 0 (Worst Surgeon Possible) to 10 (Best Surgeon Possible);
3. The patient’s rating of the surgeon’s empathy, measured by the Jefferson Scale of Patient Perceptions of Physician Empathy (JSPPPE).13 The JSPPPE is a 5-item questionnaire, measured on a 7-point Likert scale, with scores ranging from 1 (Strongly Disagree) to 7 (Strongly Agree), that assesses agreement with statements about the physician. The total score is the sum of all item scores (5-35), with higher scores representing a higher degree of perceived physician empathy.
4. Upper extremity disability, measured by the Patient-Reported Outcomes Measurement Information System Physical Function-Upper Extremity (PROMIS PF-UE) Computer Adaptive Test (CAT).14-16 This is a measure of physical limitations in the upper extremity. It can be completed with as few as 4 questions while still achieving high precision in scoring and thereby decreasing survey burden. PROMIS presents a continuous T-score with a mean of 50 and standard deviation (SD) of 10, with higher scores reflecting better physical function compared to the average of the US general population.15
After completing the initial questionnaire, the research assistant filled out the office and surgeon name and asked the surgeon to complete the diagnosis. All questionnaires were administered on an encrypted tablet via the secure, HIPAA-compliant electronic platform REDCap (Research Electronic Data Capture), a web-based application for building and managing online surveys and databases.17 The follow-up survey was sent automatically or was done by phone call as previously described. The follow-up survey consisted of (1) the 11-point ordinal measure of satisfaction with the surgeon, (2) the JSPPPE for perceived empathy, and (3) the PROMIS PF-UE for physical limitations in the upper extremity.
Analysis
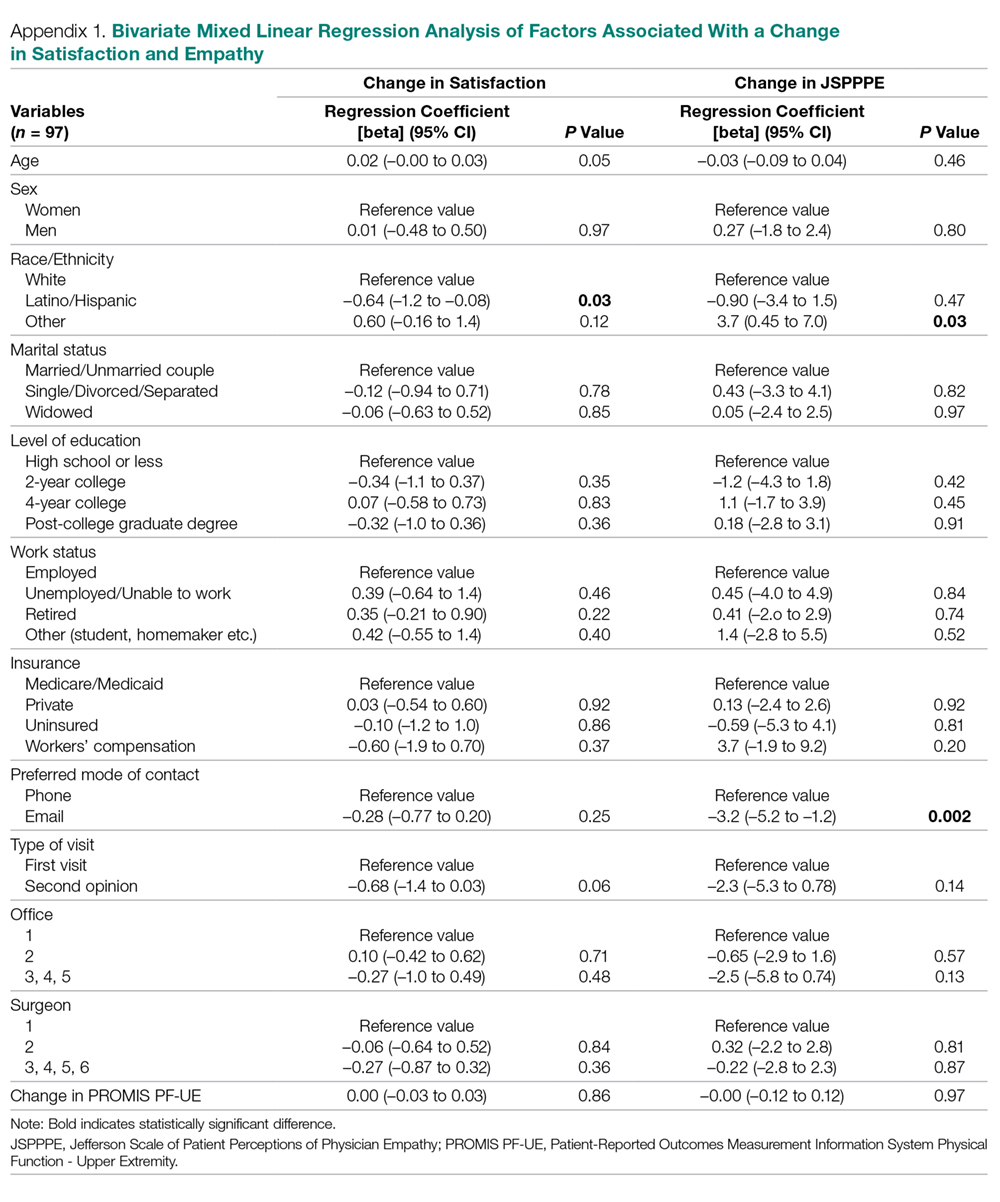
Continuous variables are presented as mean ± SD and discrete data as proportions. We used Student’s t-tests to assess baseline differences between continuous variables and Fisher’s exact tests for discrete variables. To assess differences in satisfaction and perceived empathy after 2 weeks, we used Student’s paired t-tests. We created 2 multilevel multivariable linear regression models to assess factors associated with (1) change in satisfaction with the surgeon and (2) change in perceived physician empathy. These models account for correlation of patients treated by the same surgeon. We selected variables to be included in the final models by running multilevel models with only 1 independent variable of interest (Appendix 1). Variables with P < 0.10 were included in our final models. We also included change in PROMIS PF-UE in both models because this was our variable of interest. We considered P < 0.05 significant.
We performed a power analysis for the difference in patient satisfaction immediately after the first visit compared to 2 weeks later. Based on our pilot data where we found an initial mean satisfaction score of 9.4 and mean satisfaction score after 2 weeks of 9.1 (SD of difference 1.0), a priori power analysis showed that we needed a minimum sample size of 90 patients to detect a difference with power set at 0.80 and alpha set at 0.05. In order to account for loss to follow-up as previously noted,18 we enrolled 67% more patients (total of 150).
Results
Respondent Characteristics
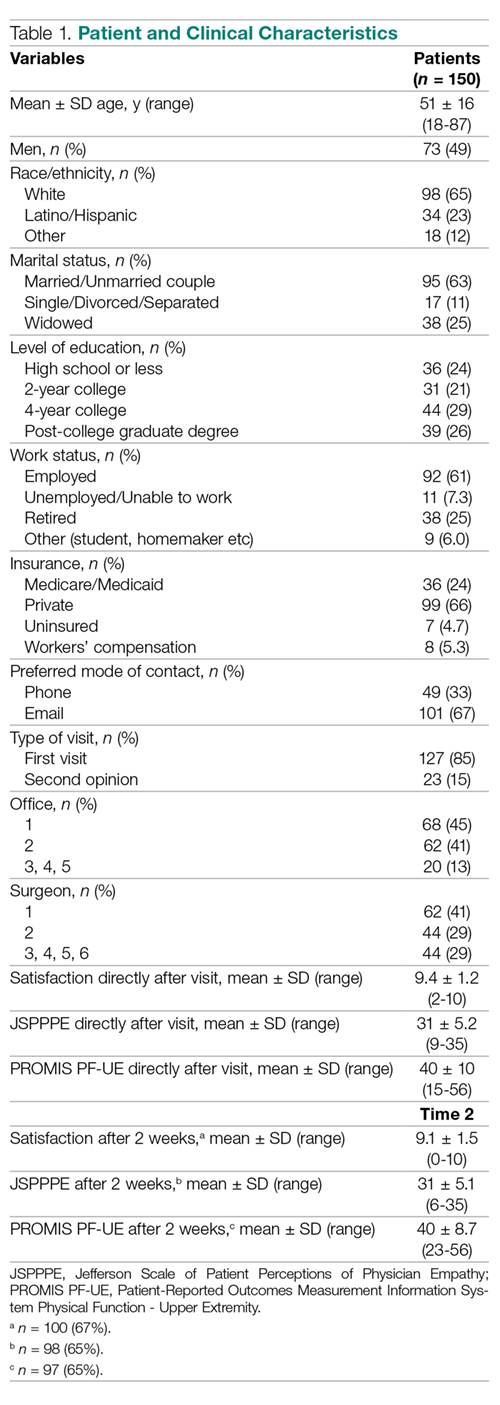
None of the 150 patients were excluded from the analysis. The study patients’ mean age was 51 ± 16 years (range, 18-87 years), and 73 (49%) were men (Table 1). Mean scores directly after the visit were 9.4 ± 1.2 (range, 2-10) for satisfaction with the surgeon, 31 ± 5.2 (range, 9-35) for perceived physician empathy, and 40 ± 10 (range 15-56) for upper extremity disability. Most patients (n = 130, 87%) were seen in 2 of 5 offices, and 106 (71%) were seen by 2 out of 6 participating surgeons.
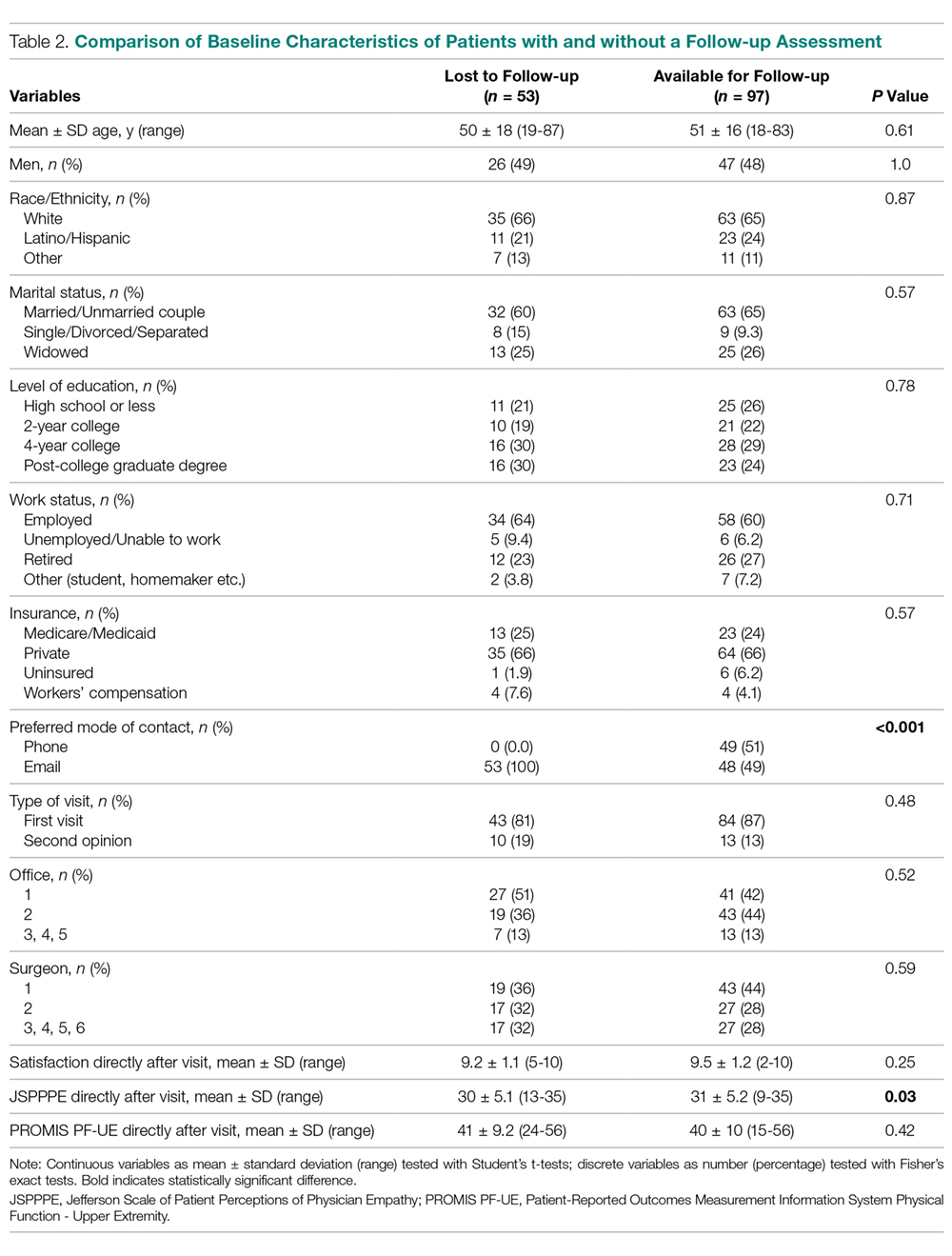
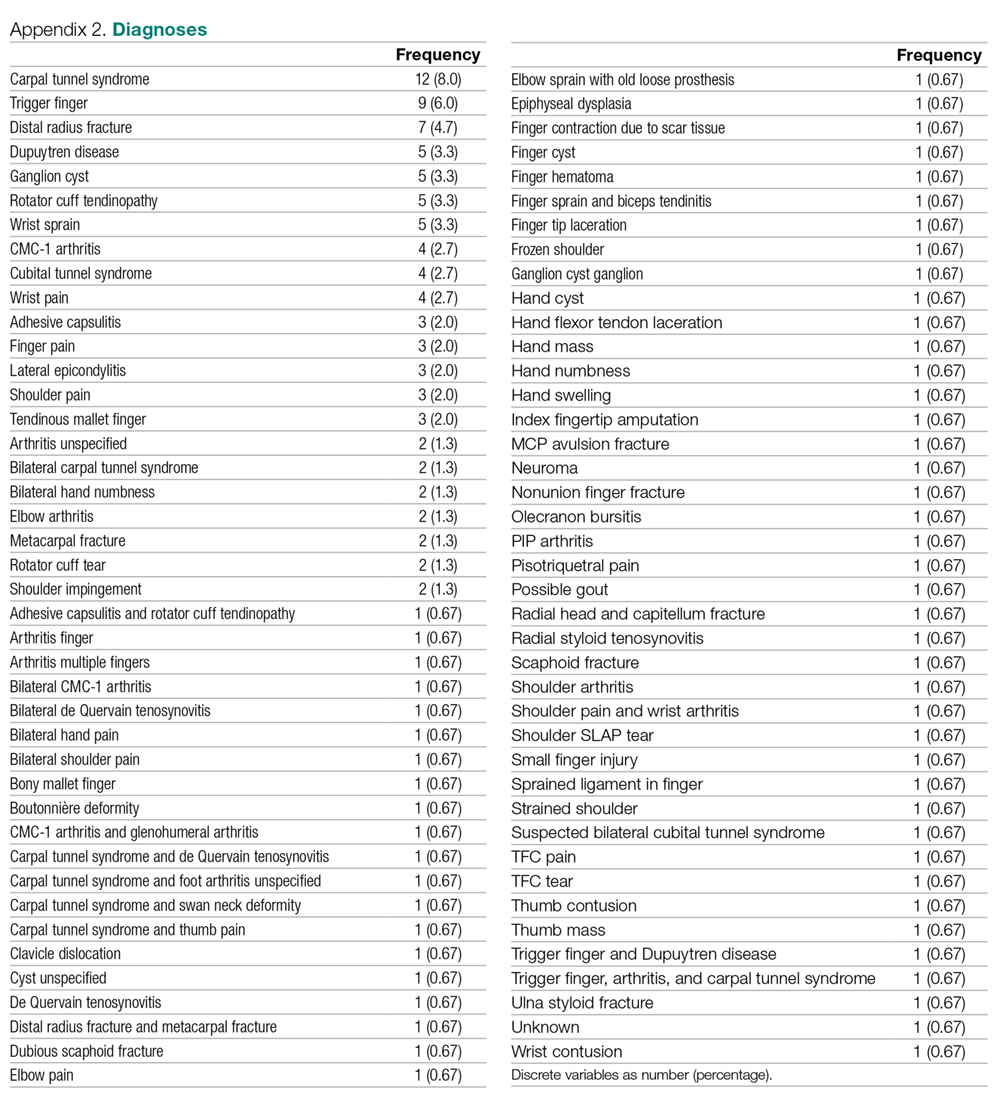
Ninety-seven (65%) patients completed their follow-up assessment 2 weeks after their initial visit, 49 (51%) by phone and 48 (49%) by email. This is a slightly better rate than the 36% rate reported in previous research.18 After 2 weeks, the mean score for satisfaction with the surgeon was 9.1 ± 1.5 (range, 0-10), the mean perceived empathy score was 31 ± 5.1 (range, 6-35), and the mean upper extremity disability score was 40 ± 8.7 (range, 23-56). Responders did not differ from nonresponders based on demographic data (Table 2). However, nonresponders had lower perceived empathy scores directly after their visit (P = 0.03) and none had initially chosen phone as their preferred mode of contact for follow-up (P < 0.001). A list of all diagnoses with frequencies the surgeons stated is listed in Appendix 2.
Difference in Satisfaction with the Surgeon
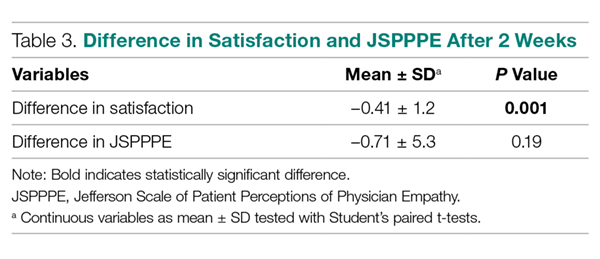
Satisfaction with the surgeon 2 weeks after the in-person visit was slightly, but significantly, lower on bivariate analysis compared to satisfaction with the surgeon immediately after the initial visit (–0.41 ± 1.2, P = 0.001; Table 3).
Difference in Perceived Physician Empathy
Perceived physician empathy 2 weeks after the in-person visit was not significantly lower on bivariate analysis compared to perceived physician empathy immediately after the initial visit (–0.71 ± 5.3, P = 0.19; Table 3).
Factors Associated with Change in Satisfaction with the Surgeon
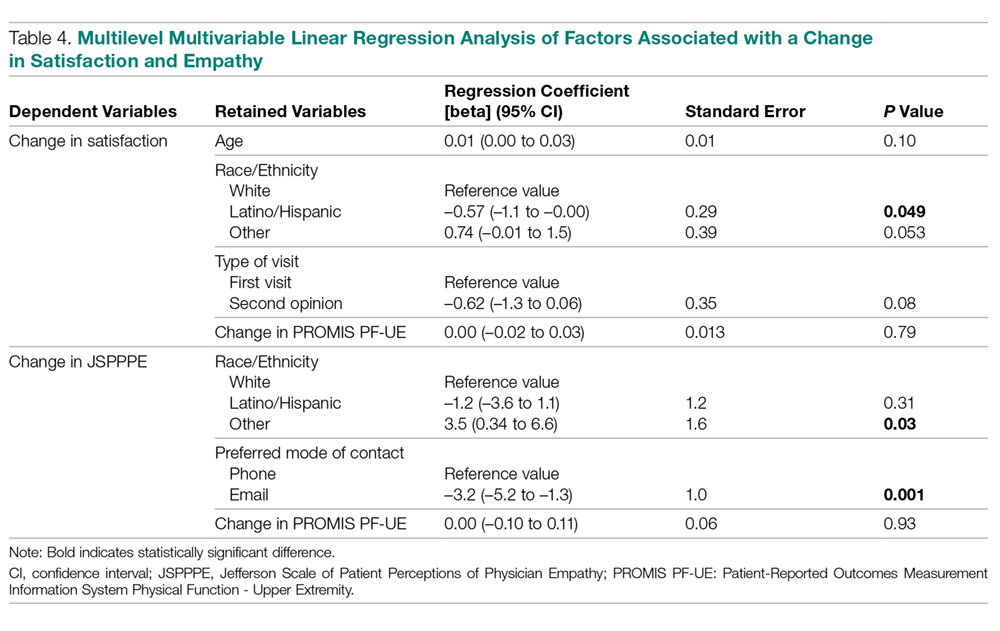
Accounting for potential interaction of variables using multilevel multivariable analysis, change in disability of the upper extremity was not associated with change in satisfaction with the surgeon (regression coefficient [beta], 0.00 [95% confidence interval {CI}, –0.02 to 0.03]; standard error [SE], 0.01; P = 0.79 [Table 4]). Being Latino was independently associated with less change in satisfaction with the surgeon (beta coefficient, –0.57 [95% CI, –1.1 to 0.00]; SE, 0.29; P = 0.049).
Factors Associated with Change in Perceived Physician Empathy
Accounting for potential interaction of variables using multilevel multivariable analysis, change in disability of the upper extremity was not associated with change in perceived physician empathy (beta coefficient = 0.00 [95% CI, –0.10 to 0.11]; SE, 0.06; P = 0.93 [Table 4]). Race/ethnicity other than white or Latino was independently associated with more change in perceived physician empathy (beta coefficient, 3.5 [95% CI, 0.34 to 6.6]; SE, 1.6; P = 0.030), and preferring email as mode of contact for follow-up was independently associated with less change in perceived physician empathy (beta coefficient, –3.2 [95% CI, –5.2 to –1.3]; SE, 1.0; P = 0.001).
Discussion
Patient satisfaction is considered a quality measure1-8 and is typically measured directly after an in-person visit. This study tested differences in patient satisfaction and perceived empathy immediately after the initial visit compared to 2 weeks later. In addition, we assessed whether change in disability was independently associated with change in satisfaction and empathy after the initial visit compared to 2 weeks later.
We acknowledge some study limitations. First, we only measured satisfaction based on 1 visit rather than multiple visits over time. It might be that satisfaction ratings differ when the physician-patient relationship is more established. However, we found overall high satisfaction ratings and a well-established relationship might not add to this finding. Second, surgeons were aware of the study and its purpose, which might have resulted in subconsciously altering the behavior to improve satisfaction. The effect of people acting differently as a result of being observed is called the Hawthorne effect.19 Third, we only used 1 simple ordinal measure to assess patient satisfaction with the surgeon. There is a wide variety of satisfaction measures,20 though the focus of this study was not to test the best possible satisfaction measure but to assess changes in satisfaction over time and its predictors. The simple 11-point ordinal satisfaction measure has proved reliable.6 Fourth, 35% of patients did not make a second rating. This is not unusual for phone or email studies. Our response rate was relatively high compared to other studies in our field,18 perhaps because the time to the second assessment was only 2 weeks and all people were available for follow-up by phone. Fifth, we analyzed 4 surgeons as 1 group and 3 offices as 1 group since we did not enroll enough patients per surgeon and office for individual analysis. However, multilevel linear analysis takes surgeon specific factors into account within that group.
The finding that satisfaction with the surgeon after 2 weeks was significantly lower on bivariate analysis compared to immediately after the initial visit is different from a study that found small increases in satisfaction after 2 weeks and 3 months,1 but comparable to another study in our field.21 Although significant, we believe the decrease in satisfaction is probably not clinically relevant. It might also be that satisfaction at follow-up is lower than measured, but that the least satisfied people did not respond on the follow-up survey.
We found no significant change in perceived empathy after 2 weeks. Since empathy is a strong driver of satisfaction,2,4-7 we did not expect to find differing results for empathy and for satisfaction over time. Both satisfaction and empathy seem to be relatively durable measures with current measurement tools.
The finding that change in disability was neither independently associated with change in satisfaction nor change in empathy is consistent with prior research.2,3,21 We cannot adequately study the impact of changes since we did not find an important change in either satisfaction or empathy over time. Jackson et al found higher satisfaction ratings over time in patients who had an increase in physical function and a decrease in symptoms.1 They also found that met expectations was associated with higher satisfaction immediately after the visit, after 2 weeks, and after 3 months.1 We feel that met expectations and fewer symptoms and limitations are likely highly co-linear with satisfaction. We therefore may not be able to learn much about one from the others.
The slight change we found in satisfaction with the surgeon among Latino patients was significantly less than the change among white patients. This suggests Latino patients might have a more stable opinion over time (a cultural phenomenon), or it might be spurious given the small number of Latino patients included in the study. The same can be said for the finding that race/ethnicity other than white or Latino was independently associated with greater change in empathy. Providing email as the preferred mode of contact was found to be independently associated with less change in perceived empathy compared to follow-up by phone. We had a 100% success rate for our follow-ups by phone. Our findings suggest that patients might more easily switch ratings on an 11-point ordinal scale than on a 5-item Likert scale. However, both measures are often rated at the ceiling of the scale.2,21
Conclusion
Satisfaction and perceived empathy are relatively stable constructs, are not clearly associated with other factors, and are strongly correlated with one another. This study supports the research practice of measuring satisfaction immediately after the visit, which is more convenient for both participant and researcher and avoids the loss of more than one third of the patients, and those with a worse experience in particular. To improve the utility and interpretation of patient-reported experience measures such as these, we might direct our efforts to developing scales with less ceiling effect.
Corresponding author: David Ring, MD, PhD, Dell Medical School, The University of Texas at Austin, Health Discovery Building HDB 6.706, 1701 Trinity St., Austin, TX 78705; david.ring@austin.utexas.edu.
Financial disclosures: Dr. Ring has or may receive payment or benefits from Skeletal Dynamics, Wright Medical for elbow implants, Deputy Editor for Clinical Orthopaedics and Related Research, Universities and Hospitals, Lawyers outside the submitted work.
Dr. Teunis has or may receive payment or benefits from VCC, PATIENT+, and AO Trauma TK network unrelated to this work and consultant fees from Synthes.
1. Jackson JL, Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52:609-620.
2. Menendez ME, Chen NC, Mudgal CS, et al. Physician empathy as a driver of hand surgery patient satisfaction. J Hand Surg Am. 2015;40(9):1860-1865.
3. Parrish RC 2nd, Menendez ME, Mudgal CS, et al. Patient Satisfaction and its relation to perceived visit duration with a hand surgeon. J Hand Surg Am. 2016;41(2):257-262.
4. Waters S, Edmondston SJ, Yates PJ, Gucciardi DF. Identification of factors influencing patient satisfaction with orthopaedic outpatient clinic consultation: A qualitative study. Man Ther. 2016;25:48-55.
5. Voutilainen A, Pitkaaho T, Kvist T, Vehvilainen-Julkunen K. How to ask about patient satisfaction? The visual analogue scale is less vulnerable to confounding factors and ceiling effect than a symmetric Likert scale. J Adv Nurs. 2016;72:946-957.
6. van Berckel MM, Bosma NH, Hageman MG, et al. The correlation between a numerical rating scale of patient satisfaction with current management of an upper extremity disorder and a general measure of satisfaction with the medical visit. Hand (N Y). 2017;12:202-206.
7. Garcia D, Bautista O, Venereo L, et al. Training in empathic skills improves the patient-physician relationship during the first consultation in a fertility clinic. Fertil Steril. 2013;99:1413-1418.
8. Fitzpatrick RM, Hopkins A. Patients’ satisfaction with communication in neurological outpatient clinics. J Psychosom Res. 1981;25:329-334.
9. Kincey J, Bradshaw P, Ley P. Patients’ satisfaction and reported acceptance of advice in general practice. J R Coll Gen Pract. 1975;25:558-566.
10. Ley P, Whitworth MA, Skilbeck CE, et al. Improving doctor-patient communication in general practice. J R Coll Gen Pract. 1976;26:720-724.
11. Meakin R, Weinman J. The ‘Medical Interview Satisfaction Scale’ (MISS-21) adapted for British general practice. Fam Pract. 2002;19:257-263.
12. Wolf MH, Putnam SM, James SA, Stiles WB. The Medical Interview Satisfaction Scale: development of a scale to measure patient perceptions of physician behavior. J Behav Med. 1978;1:391-401.
13. Kane GC, Gotto JL, Mangione S, et al. Jefferson Scale of Patient’s Perceptions of Physician Empathy: preliminary psychometric data. Croat Med J. 2007;48:81-86.
14. Beckmann JT , Hung M, Voss MW, et al. Evaluation of the patient-reported outcomes measurement information system upper extremity computer adaptive test. J Hand Surg Am. 2016;41:739-744.
15. PROMIS. PROMIS PF Scoring. Available at www.healthmeasures.net/administrator/components/com_instruments/uploads/PROMIS%20Physical%20Function%20Scoring%20Manual.pdf. Accessed March 1, 2019.
16. PROMIS. PROMIS Measures. Available at wwwnihpromisorg. Accessed March 1, 2019.
17. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-381.
18. Bot AG, Anderson JA, Neuhaus V, Ring D. Factors associated with survey response in hand surgery research. Clin Orthop Relat Res. 2013;471(10):3237-3242.
19. Sedgwick P, Greenwood N. Understanding the Hawthorne effect. BMJ. 2015;351:h4672.
20. Ross CK, Steward CA, Sinacore JM. A comparative study of seven measures of patient satisfaction. Med Care. 1995;33:392-406.
21. Teunis T, Thornton ER, Jayakumar P, Ring D. Time seeing a hand surgeon is not associated with patient satisfaction. Clin Orthop Relat Res. 2015;473:2362-2368.
From the Department of Surgery and Perioperative Care, Dell Medical School, The University of Texas at Austin, Austin, TX (Dr. Kortlever, Ms. Haidar, Dr. Reichel, Dr. Driscoll, Dr. Ring, and Dr. Vagner) and University Medical Center Utrecht, Utrecht, The Netherlands (Dr. Teunis).
Abstract
- Objective: Patient satisfaction is considered a quality measure. Satisfaction is typically measured directly after an in-person visit in research and 2 weeks later in practice surveys. We assessed if there was a difference in immediate and delayed measurement of satisfaction.
- Questions: (1) There is no difference in patient satisfaction (measured by Numerical Rating Scale [NRS]) and (2) perceived empathy (measured by the Jefferson Scale of Patient Perceptions of Physician Empathy [JSPPPE]) immediately after the initial visit compared to 2 weeks later. (3) Change in disability (measured by the Patient-Reported Outcome Measurement Information System Physical Function-Upper Extremity [PROMIS PF-UE]) is not independently associated with change in satisfaction and (4) empathy after the initial visit compared to 2 weeks later.
- Methods: 150 new patients completed a survey of demographics, satisfaction with the surgeon, rating of the surgeon’s empathy, and upper extremity specific limitations. The satisfaction, empathy, and limitation questionnaires were repeated 2 weeks later.
- Results: We found a slight but significant decrease in satisfaction 2 weeks after the in-person visit (–0.41, P = 0.001). There was no significant change in perceived empathy (–0.71, P = 0.19). Change in limitations did not account for a change in satisfaction (P = 0.79) or perceived empathy (P = 0.93).
- Conclusion: Satisfaction and perceived empathy are relatively stable constructs that can be measured immediately after the visit.
Keywords: satisfaction, empathy, change, upper extremity, disability.
Patient satisfaction is increasingly being used as a performance measure to evaluate quality of care.1-8 Patient satisfaction correlates with adherence with recommended treatment.1,6,8-10 Satisfaction measured on an 11-point ordinal scale immediately after the visit correlates strongly with the perception of clinician empathy.2,3 Indeed, some satisfaction questionnaires such as the Medical Interview Satisfaction Scale (MISS)11,12 have questions very similar to empathy questionnaires. It may be that satisfaction is a construct similar to feeling that your doctor listened and cared about you as an individual (perceived physician empathy).
Higher ratings of satisfaction also seem to be related to a physician’s communication style.1,4,7-10 One study of 13 fertility doctors found that training in effective communication strategies led to improved patient satisfaction.7 A qualitative study of 36 patients, health professionals, and clinical support staff in an orthopaedic outpatient setting held interviews and focus group sessions to identify themes influencing patient satisfaction.4 Communication and expectation were among the 7 themes identified. We have noticed a high ceiling effect (maximum scores) with measures of patient satisfaction and perceived empathy.2,3 Another study also noted a high ceiling effect when using an ordinal scale.5 It may be that people with a positive feeling shortly after a health care encounter give top ratings out of politeness or gratefulness. It is also possible they will feel differently a few weeks after they leave the office. Furthermore, ratings of satisfaction gathered by a practice or health care system for practice assessment/improvement are often obtained several days to weeks after the visit, while research often obtains satisfaction ratings immediately after the visit for practical reasons. There may be differences between immediate and delayed measurement of satisfaction beyond the mentioned social norms.
Therefore, this study tested the primary null hypothesis that there is no difference in patient satisfaction (measured by Numerical Rating Scale [NRS]) immediately after the initial visit compared to 2 weeks later. Additionally, we assessed the difference in perceived empathy immediately after the initial visit compared to 2 weeks later, and whether change in disability was independently associated with change in satisfaction and empathy after the initial visit compared to 2 weeks later.
Methods
Study Design
After Institutional Review Board approval of this prospective, longitudinal, observational cohort study, we prospectively enrolled 150 adult patients between November 29, 2017 and January 10, 2018. Patients were seen at 5 orthopaedic clinics in a large urban area. We included all new English-speaking patients aged 18 to 89 years who were visiting 1 of 6 participating orthopaedic surgeons for any upper extremity problem and who were able to provide informed consent. We excluded follow-up visits and patients who were unable to speak and understand English. Four research assistants who were not involved with patient treatment described the study to patients before or after the visit with the surgeon. We were granted a waiver of written informed consent; patients indicated their consent by completing the surveys.
Patients could choose either phone or email as their preferred mode of contact for follow-up in this study. For patients who selected email as the preferred mode of contact, the follow-up survey was sent automatically 2 weeks after completion date, and a maximum of 3 reminder emails with 2-day time intervals between them were sent to those who did not respond to the initial invitation. For patients who selected phone as the preferred mode of contact, the follow-up survey was done by an English-speaking research assistant who was not involved with patient treatment. When a response was not obtained on the initial phone call, 3 additional phone calls were made (1 later that same day and 2 the next day). One patient declined participation because he was not interested in the study and had no time after his visit.
Measurements
Patients were asked to complete a set of questionnaires at the end of their visit:
1. A demographic questionnaire consisting of preferred mode of contact for follow-up (phone or email), age, sex, race/ethnicity, marital status, education status, work status, insurance status, and type of visit (first visit or second opinion);
2. An 11-point ordinal measure of satisfaction with the surgeon, with scores ranging from 0 (Worst Surgeon Possible) to 10 (Best Surgeon Possible);
3. The patient’s rating of the surgeon’s empathy, measured by the Jefferson Scale of Patient Perceptions of Physician Empathy (JSPPPE).13 The JSPPPE is a 5-item questionnaire, measured on a 7-point Likert scale, with scores ranging from 1 (Strongly Disagree) to 7 (Strongly Agree), that assesses agreement with statements about the physician. The total score is the sum of all item scores (5-35), with higher scores representing a higher degree of perceived physician empathy.
4. Upper extremity disability, measured by the Patient-Reported Outcomes Measurement Information System Physical Function-Upper Extremity (PROMIS PF-UE) Computer Adaptive Test (CAT).14-16 This is a measure of physical limitations in the upper extremity. It can be completed with as few as 4 questions while still achieving high precision in scoring and thereby decreasing survey burden. PROMIS presents a continuous T-score with a mean of 50 and standard deviation (SD) of 10, with higher scores reflecting better physical function compared to the average of the US general population.15
After completing the initial questionnaire, the research assistant filled out the office and surgeon name and asked the surgeon to complete the diagnosis. All questionnaires were administered on an encrypted tablet via the secure, HIPAA-compliant electronic platform REDCap (Research Electronic Data Capture), a web-based application for building and managing online surveys and databases.17 The follow-up survey was sent automatically or was done by phone call as previously described. The follow-up survey consisted of (1) the 11-point ordinal measure of satisfaction with the surgeon, (2) the JSPPPE for perceived empathy, and (3) the PROMIS PF-UE for physical limitations in the upper extremity.
Analysis
Continuous variables are presented as mean ± SD and discrete data as proportions. We used Student’s t-tests to assess baseline differences between continuous variables and Fisher’s exact tests for discrete variables. To assess differences in satisfaction and perceived empathy after 2 weeks, we used Student’s paired t-tests. We created 2 multilevel multivariable linear regression models to assess factors associated with (1) change in satisfaction with the surgeon and (2) change in perceived physician empathy. These models account for correlation of patients treated by the same surgeon. We selected variables to be included in the final models by running multilevel models with only 1 independent variable of interest (Appendix 1). Variables with P < 0.10 were included in our final models. We also included change in PROMIS PF-UE in both models because this was our variable of interest. We considered P < 0.05 significant.
We performed a power analysis for the difference in patient satisfaction immediately after the first visit compared to 2 weeks later. Based on our pilot data where we found an initial mean satisfaction score of 9.4 and mean satisfaction score after 2 weeks of 9.1 (SD of difference 1.0), a priori power analysis showed that we needed a minimum sample size of 90 patients to detect a difference with power set at 0.80 and alpha set at 0.05. In order to account for loss to follow-up as previously noted,18 we enrolled 67% more patients (total of 150).
Results
Respondent Characteristics
None of the 150 patients were excluded from the analysis. The study patients’ mean age was 51 ± 16 years (range, 18-87 years), and 73 (49%) were men (Table 1). Mean scores directly after the visit were 9.4 ± 1.2 (range, 2-10) for satisfaction with the surgeon, 31 ± 5.2 (range, 9-35) for perceived physician empathy, and 40 ± 10 (range 15-56) for upper extremity disability. Most patients (n = 130, 87%) were seen in 2 of 5 offices, and 106 (71%) were seen by 2 out of 6 participating surgeons.
Ninety-seven (65%) patients completed their follow-up assessment 2 weeks after their initial visit, 49 (51%) by phone and 48 (49%) by email. This is a slightly better rate than the 36% rate reported in previous research.18 After 2 weeks, the mean score for satisfaction with the surgeon was 9.1 ± 1.5 (range, 0-10), the mean perceived empathy score was 31 ± 5.1 (range, 6-35), and the mean upper extremity disability score was 40 ± 8.7 (range, 23-56). Responders did not differ from nonresponders based on demographic data (Table 2). However, nonresponders had lower perceived empathy scores directly after their visit (P = 0.03) and none had initially chosen phone as their preferred mode of contact for follow-up (P < 0.001). A list of all diagnoses with frequencies the surgeons stated is listed in Appendix 2.
Difference in Satisfaction with the Surgeon
Satisfaction with the surgeon 2 weeks after the in-person visit was slightly, but significantly, lower on bivariate analysis compared to satisfaction with the surgeon immediately after the initial visit (–0.41 ± 1.2, P = 0.001; Table 3).
Difference in Perceived Physician Empathy
Perceived physician empathy 2 weeks after the in-person visit was not significantly lower on bivariate analysis compared to perceived physician empathy immediately after the initial visit (–0.71 ± 5.3, P = 0.19; Table 3).
Factors Associated with Change in Satisfaction with the Surgeon
Accounting for potential interaction of variables using multilevel multivariable analysis, change in disability of the upper extremity was not associated with change in satisfaction with the surgeon (regression coefficient [beta], 0.00 [95% confidence interval {CI}, –0.02 to 0.03]; standard error [SE], 0.01; P = 0.79 [Table 4]). Being Latino was independently associated with less change in satisfaction with the surgeon (beta coefficient, –0.57 [95% CI, –1.1 to 0.00]; SE, 0.29; P = 0.049).
Factors Associated with Change in Perceived Physician Empathy
Accounting for potential interaction of variables using multilevel multivariable analysis, change in disability of the upper extremity was not associated with change in perceived physician empathy (beta coefficient = 0.00 [95% CI, –0.10 to 0.11]; SE, 0.06; P = 0.93 [Table 4]). Race/ethnicity other than white or Latino was independently associated with more change in perceived physician empathy (beta coefficient, 3.5 [95% CI, 0.34 to 6.6]; SE, 1.6; P = 0.030), and preferring email as mode of contact for follow-up was independently associated with less change in perceived physician empathy (beta coefficient, –3.2 [95% CI, –5.2 to –1.3]; SE, 1.0; P = 0.001).
Discussion
Patient satisfaction is considered a quality measure1-8 and is typically measured directly after an in-person visit. This study tested differences in patient satisfaction and perceived empathy immediately after the initial visit compared to 2 weeks later. In addition, we assessed whether change in disability was independently associated with change in satisfaction and empathy after the initial visit compared to 2 weeks later.
We acknowledge some study limitations. First, we only measured satisfaction based on 1 visit rather than multiple visits over time. It might be that satisfaction ratings differ when the physician-patient relationship is more established. However, we found overall high satisfaction ratings and a well-established relationship might not add to this finding. Second, surgeons were aware of the study and its purpose, which might have resulted in subconsciously altering the behavior to improve satisfaction. The effect of people acting differently as a result of being observed is called the Hawthorne effect.19 Third, we only used 1 simple ordinal measure to assess patient satisfaction with the surgeon. There is a wide variety of satisfaction measures,20 though the focus of this study was not to test the best possible satisfaction measure but to assess changes in satisfaction over time and its predictors. The simple 11-point ordinal satisfaction measure has proved reliable.6 Fourth, 35% of patients did not make a second rating. This is not unusual for phone or email studies. Our response rate was relatively high compared to other studies in our field,18 perhaps because the time to the second assessment was only 2 weeks and all people were available for follow-up by phone. Fifth, we analyzed 4 surgeons as 1 group and 3 offices as 1 group since we did not enroll enough patients per surgeon and office for individual analysis. However, multilevel linear analysis takes surgeon specific factors into account within that group.
The finding that satisfaction with the surgeon after 2 weeks was significantly lower on bivariate analysis compared to immediately after the initial visit is different from a study that found small increases in satisfaction after 2 weeks and 3 months,1 but comparable to another study in our field.21 Although significant, we believe the decrease in satisfaction is probably not clinically relevant. It might also be that satisfaction at follow-up is lower than measured, but that the least satisfied people did not respond on the follow-up survey.
We found no significant change in perceived empathy after 2 weeks. Since empathy is a strong driver of satisfaction,2,4-7 we did not expect to find differing results for empathy and for satisfaction over time. Both satisfaction and empathy seem to be relatively durable measures with current measurement tools.
The finding that change in disability was neither independently associated with change in satisfaction nor change in empathy is consistent with prior research.2,3,21 We cannot adequately study the impact of changes since we did not find an important change in either satisfaction or empathy over time. Jackson et al found higher satisfaction ratings over time in patients who had an increase in physical function and a decrease in symptoms.1 They also found that met expectations was associated with higher satisfaction immediately after the visit, after 2 weeks, and after 3 months.1 We feel that met expectations and fewer symptoms and limitations are likely highly co-linear with satisfaction. We therefore may not be able to learn much about one from the others.
The slight change we found in satisfaction with the surgeon among Latino patients was significantly less than the change among white patients. This suggests Latino patients might have a more stable opinion over time (a cultural phenomenon), or it might be spurious given the small number of Latino patients included in the study. The same can be said for the finding that race/ethnicity other than white or Latino was independently associated with greater change in empathy. Providing email as the preferred mode of contact was found to be independently associated with less change in perceived empathy compared to follow-up by phone. We had a 100% success rate for our follow-ups by phone. Our findings suggest that patients might more easily switch ratings on an 11-point ordinal scale than on a 5-item Likert scale. However, both measures are often rated at the ceiling of the scale.2,21
Conclusion
Satisfaction and perceived empathy are relatively stable constructs, are not clearly associated with other factors, and are strongly correlated with one another. This study supports the research practice of measuring satisfaction immediately after the visit, which is more convenient for both participant and researcher and avoids the loss of more than one third of the patients, and those with a worse experience in particular. To improve the utility and interpretation of patient-reported experience measures such as these, we might direct our efforts to developing scales with less ceiling effect.
Corresponding author: David Ring, MD, PhD, Dell Medical School, The University of Texas at Austin, Health Discovery Building HDB 6.706, 1701 Trinity St., Austin, TX 78705; david.ring@austin.utexas.edu.
Financial disclosures: Dr. Ring has or may receive payment or benefits from Skeletal Dynamics, Wright Medical for elbow implants, Deputy Editor for Clinical Orthopaedics and Related Research, Universities and Hospitals, Lawyers outside the submitted work.
Dr. Teunis has or may receive payment or benefits from VCC, PATIENT+, and AO Trauma TK network unrelated to this work and consultant fees from Synthes.
From the Department of Surgery and Perioperative Care, Dell Medical School, The University of Texas at Austin, Austin, TX (Dr. Kortlever, Ms. Haidar, Dr. Reichel, Dr. Driscoll, Dr. Ring, and Dr. Vagner) and University Medical Center Utrecht, Utrecht, The Netherlands (Dr. Teunis).
Abstract
- Objective: Patient satisfaction is considered a quality measure. Satisfaction is typically measured directly after an in-person visit in research and 2 weeks later in practice surveys. We assessed if there was a difference in immediate and delayed measurement of satisfaction.
- Questions: (1) There is no difference in patient satisfaction (measured by Numerical Rating Scale [NRS]) and (2) perceived empathy (measured by the Jefferson Scale of Patient Perceptions of Physician Empathy [JSPPPE]) immediately after the initial visit compared to 2 weeks later. (3) Change in disability (measured by the Patient-Reported Outcome Measurement Information System Physical Function-Upper Extremity [PROMIS PF-UE]) is not independently associated with change in satisfaction and (4) empathy after the initial visit compared to 2 weeks later.
- Methods: 150 new patients completed a survey of demographics, satisfaction with the surgeon, rating of the surgeon’s empathy, and upper extremity specific limitations. The satisfaction, empathy, and limitation questionnaires were repeated 2 weeks later.
- Results: We found a slight but significant decrease in satisfaction 2 weeks after the in-person visit (–0.41, P = 0.001). There was no significant change in perceived empathy (–0.71, P = 0.19). Change in limitations did not account for a change in satisfaction (P = 0.79) or perceived empathy (P = 0.93).
- Conclusion: Satisfaction and perceived empathy are relatively stable constructs that can be measured immediately after the visit.
Keywords: satisfaction, empathy, change, upper extremity, disability.
Patient satisfaction is increasingly being used as a performance measure to evaluate quality of care.1-8 Patient satisfaction correlates with adherence with recommended treatment.1,6,8-10 Satisfaction measured on an 11-point ordinal scale immediately after the visit correlates strongly with the perception of clinician empathy.2,3 Indeed, some satisfaction questionnaires such as the Medical Interview Satisfaction Scale (MISS)11,12 have questions very similar to empathy questionnaires. It may be that satisfaction is a construct similar to feeling that your doctor listened and cared about you as an individual (perceived physician empathy).
Higher ratings of satisfaction also seem to be related to a physician’s communication style.1,4,7-10 One study of 13 fertility doctors found that training in effective communication strategies led to improved patient satisfaction.7 A qualitative study of 36 patients, health professionals, and clinical support staff in an orthopaedic outpatient setting held interviews and focus group sessions to identify themes influencing patient satisfaction.4 Communication and expectation were among the 7 themes identified. We have noticed a high ceiling effect (maximum scores) with measures of patient satisfaction and perceived empathy.2,3 Another study also noted a high ceiling effect when using an ordinal scale.5 It may be that people with a positive feeling shortly after a health care encounter give top ratings out of politeness or gratefulness. It is also possible they will feel differently a few weeks after they leave the office. Furthermore, ratings of satisfaction gathered by a practice or health care system for practice assessment/improvement are often obtained several days to weeks after the visit, while research often obtains satisfaction ratings immediately after the visit for practical reasons. There may be differences between immediate and delayed measurement of satisfaction beyond the mentioned social norms.
Therefore, this study tested the primary null hypothesis that there is no difference in patient satisfaction (measured by Numerical Rating Scale [NRS]) immediately after the initial visit compared to 2 weeks later. Additionally, we assessed the difference in perceived empathy immediately after the initial visit compared to 2 weeks later, and whether change in disability was independently associated with change in satisfaction and empathy after the initial visit compared to 2 weeks later.
Methods
Study Design
After Institutional Review Board approval of this prospective, longitudinal, observational cohort study, we prospectively enrolled 150 adult patients between November 29, 2017 and January 10, 2018. Patients were seen at 5 orthopaedic clinics in a large urban area. We included all new English-speaking patients aged 18 to 89 years who were visiting 1 of 6 participating orthopaedic surgeons for any upper extremity problem and who were able to provide informed consent. We excluded follow-up visits and patients who were unable to speak and understand English. Four research assistants who were not involved with patient treatment described the study to patients before or after the visit with the surgeon. We were granted a waiver of written informed consent; patients indicated their consent by completing the surveys.
Patients could choose either phone or email as their preferred mode of contact for follow-up in this study. For patients who selected email as the preferred mode of contact, the follow-up survey was sent automatically 2 weeks after completion date, and a maximum of 3 reminder emails with 2-day time intervals between them were sent to those who did not respond to the initial invitation. For patients who selected phone as the preferred mode of contact, the follow-up survey was done by an English-speaking research assistant who was not involved with patient treatment. When a response was not obtained on the initial phone call, 3 additional phone calls were made (1 later that same day and 2 the next day). One patient declined participation because he was not interested in the study and had no time after his visit.
Measurements
Patients were asked to complete a set of questionnaires at the end of their visit:
1. A demographic questionnaire consisting of preferred mode of contact for follow-up (phone or email), age, sex, race/ethnicity, marital status, education status, work status, insurance status, and type of visit (first visit or second opinion);
2. An 11-point ordinal measure of satisfaction with the surgeon, with scores ranging from 0 (Worst Surgeon Possible) to 10 (Best Surgeon Possible);
3. The patient’s rating of the surgeon’s empathy, measured by the Jefferson Scale of Patient Perceptions of Physician Empathy (JSPPPE).13 The JSPPPE is a 5-item questionnaire, measured on a 7-point Likert scale, with scores ranging from 1 (Strongly Disagree) to 7 (Strongly Agree), that assesses agreement with statements about the physician. The total score is the sum of all item scores (5-35), with higher scores representing a higher degree of perceived physician empathy.
4. Upper extremity disability, measured by the Patient-Reported Outcomes Measurement Information System Physical Function-Upper Extremity (PROMIS PF-UE) Computer Adaptive Test (CAT).14-16 This is a measure of physical limitations in the upper extremity. It can be completed with as few as 4 questions while still achieving high precision in scoring and thereby decreasing survey burden. PROMIS presents a continuous T-score with a mean of 50 and standard deviation (SD) of 10, with higher scores reflecting better physical function compared to the average of the US general population.15
After completing the initial questionnaire, the research assistant filled out the office and surgeon name and asked the surgeon to complete the diagnosis. All questionnaires were administered on an encrypted tablet via the secure, HIPAA-compliant electronic platform REDCap (Research Electronic Data Capture), a web-based application for building and managing online surveys and databases.17 The follow-up survey was sent automatically or was done by phone call as previously described. The follow-up survey consisted of (1) the 11-point ordinal measure of satisfaction with the surgeon, (2) the JSPPPE for perceived empathy, and (3) the PROMIS PF-UE for physical limitations in the upper extremity.
Analysis
Continuous variables are presented as mean ± SD and discrete data as proportions. We used Student’s t-tests to assess baseline differences between continuous variables and Fisher’s exact tests for discrete variables. To assess differences in satisfaction and perceived empathy after 2 weeks, we used Student’s paired t-tests. We created 2 multilevel multivariable linear regression models to assess factors associated with (1) change in satisfaction with the surgeon and (2) change in perceived physician empathy. These models account for correlation of patients treated by the same surgeon. We selected variables to be included in the final models by running multilevel models with only 1 independent variable of interest (Appendix 1). Variables with P < 0.10 were included in our final models. We also included change in PROMIS PF-UE in both models because this was our variable of interest. We considered P < 0.05 significant.
We performed a power analysis for the difference in patient satisfaction immediately after the first visit compared to 2 weeks later. Based on our pilot data where we found an initial mean satisfaction score of 9.4 and mean satisfaction score after 2 weeks of 9.1 (SD of difference 1.0), a priori power analysis showed that we needed a minimum sample size of 90 patients to detect a difference with power set at 0.80 and alpha set at 0.05. In order to account for loss to follow-up as previously noted,18 we enrolled 67% more patients (total of 150).
Results
Respondent Characteristics
None of the 150 patients were excluded from the analysis. The study patients’ mean age was 51 ± 16 years (range, 18-87 years), and 73 (49%) were men (Table 1). Mean scores directly after the visit were 9.4 ± 1.2 (range, 2-10) for satisfaction with the surgeon, 31 ± 5.2 (range, 9-35) for perceived physician empathy, and 40 ± 10 (range 15-56) for upper extremity disability. Most patients (n = 130, 87%) were seen in 2 of 5 offices, and 106 (71%) were seen by 2 out of 6 participating surgeons.
Ninety-seven (65%) patients completed their follow-up assessment 2 weeks after their initial visit, 49 (51%) by phone and 48 (49%) by email. This is a slightly better rate than the 36% rate reported in previous research.18 After 2 weeks, the mean score for satisfaction with the surgeon was 9.1 ± 1.5 (range, 0-10), the mean perceived empathy score was 31 ± 5.1 (range, 6-35), and the mean upper extremity disability score was 40 ± 8.7 (range, 23-56). Responders did not differ from nonresponders based on demographic data (Table 2). However, nonresponders had lower perceived empathy scores directly after their visit (P = 0.03) and none had initially chosen phone as their preferred mode of contact for follow-up (P < 0.001). A list of all diagnoses with frequencies the surgeons stated is listed in Appendix 2.
Difference in Satisfaction with the Surgeon
Satisfaction with the surgeon 2 weeks after the in-person visit was slightly, but significantly, lower on bivariate analysis compared to satisfaction with the surgeon immediately after the initial visit (–0.41 ± 1.2, P = 0.001; Table 3).
Difference in Perceived Physician Empathy
Perceived physician empathy 2 weeks after the in-person visit was not significantly lower on bivariate analysis compared to perceived physician empathy immediately after the initial visit (–0.71 ± 5.3, P = 0.19; Table 3).
Factors Associated with Change in Satisfaction with the Surgeon
Accounting for potential interaction of variables using multilevel multivariable analysis, change in disability of the upper extremity was not associated with change in satisfaction with the surgeon (regression coefficient [beta], 0.00 [95% confidence interval {CI}, –0.02 to 0.03]; standard error [SE], 0.01; P = 0.79 [Table 4]). Being Latino was independently associated with less change in satisfaction with the surgeon (beta coefficient, –0.57 [95% CI, –1.1 to 0.00]; SE, 0.29; P = 0.049).
Factors Associated with Change in Perceived Physician Empathy
Accounting for potential interaction of variables using multilevel multivariable analysis, change in disability of the upper extremity was not associated with change in perceived physician empathy (beta coefficient = 0.00 [95% CI, –0.10 to 0.11]; SE, 0.06; P = 0.93 [Table 4]). Race/ethnicity other than white or Latino was independently associated with more change in perceived physician empathy (beta coefficient, 3.5 [95% CI, 0.34 to 6.6]; SE, 1.6; P = 0.030), and preferring email as mode of contact for follow-up was independently associated with less change in perceived physician empathy (beta coefficient, –3.2 [95% CI, –5.2 to –1.3]; SE, 1.0; P = 0.001).
Discussion
Patient satisfaction is considered a quality measure1-8 and is typically measured directly after an in-person visit. This study tested differences in patient satisfaction and perceived empathy immediately after the initial visit compared to 2 weeks later. In addition, we assessed whether change in disability was independently associated with change in satisfaction and empathy after the initial visit compared to 2 weeks later.
We acknowledge some study limitations. First, we only measured satisfaction based on 1 visit rather than multiple visits over time. It might be that satisfaction ratings differ when the physician-patient relationship is more established. However, we found overall high satisfaction ratings and a well-established relationship might not add to this finding. Second, surgeons were aware of the study and its purpose, which might have resulted in subconsciously altering the behavior to improve satisfaction. The effect of people acting differently as a result of being observed is called the Hawthorne effect.19 Third, we only used 1 simple ordinal measure to assess patient satisfaction with the surgeon. There is a wide variety of satisfaction measures,20 though the focus of this study was not to test the best possible satisfaction measure but to assess changes in satisfaction over time and its predictors. The simple 11-point ordinal satisfaction measure has proved reliable.6 Fourth, 35% of patients did not make a second rating. This is not unusual for phone or email studies. Our response rate was relatively high compared to other studies in our field,18 perhaps because the time to the second assessment was only 2 weeks and all people were available for follow-up by phone. Fifth, we analyzed 4 surgeons as 1 group and 3 offices as 1 group since we did not enroll enough patients per surgeon and office for individual analysis. However, multilevel linear analysis takes surgeon specific factors into account within that group.
The finding that satisfaction with the surgeon after 2 weeks was significantly lower on bivariate analysis compared to immediately after the initial visit is different from a study that found small increases in satisfaction after 2 weeks and 3 months,1 but comparable to another study in our field.21 Although significant, we believe the decrease in satisfaction is probably not clinically relevant. It might also be that satisfaction at follow-up is lower than measured, but that the least satisfied people did not respond on the follow-up survey.
We found no significant change in perceived empathy after 2 weeks. Since empathy is a strong driver of satisfaction,2,4-7 we did not expect to find differing results for empathy and for satisfaction over time. Both satisfaction and empathy seem to be relatively durable measures with current measurement tools.
The finding that change in disability was neither independently associated with change in satisfaction nor change in empathy is consistent with prior research.2,3,21 We cannot adequately study the impact of changes since we did not find an important change in either satisfaction or empathy over time. Jackson et al found higher satisfaction ratings over time in patients who had an increase in physical function and a decrease in symptoms.1 They also found that met expectations was associated with higher satisfaction immediately after the visit, after 2 weeks, and after 3 months.1 We feel that met expectations and fewer symptoms and limitations are likely highly co-linear with satisfaction. We therefore may not be able to learn much about one from the others.
The slight change we found in satisfaction with the surgeon among Latino patients was significantly less than the change among white patients. This suggests Latino patients might have a more stable opinion over time (a cultural phenomenon), or it might be spurious given the small number of Latino patients included in the study. The same can be said for the finding that race/ethnicity other than white or Latino was independently associated with greater change in empathy. Providing email as the preferred mode of contact was found to be independently associated with less change in perceived empathy compared to follow-up by phone. We had a 100% success rate for our follow-ups by phone. Our findings suggest that patients might more easily switch ratings on an 11-point ordinal scale than on a 5-item Likert scale. However, both measures are often rated at the ceiling of the scale.2,21
Conclusion
Satisfaction and perceived empathy are relatively stable constructs, are not clearly associated with other factors, and are strongly correlated with one another. This study supports the research practice of measuring satisfaction immediately after the visit, which is more convenient for both participant and researcher and avoids the loss of more than one third of the patients, and those with a worse experience in particular. To improve the utility and interpretation of patient-reported experience measures such as these, we might direct our efforts to developing scales with less ceiling effect.
Corresponding author: David Ring, MD, PhD, Dell Medical School, The University of Texas at Austin, Health Discovery Building HDB 6.706, 1701 Trinity St., Austin, TX 78705; david.ring@austin.utexas.edu.
Financial disclosures: Dr. Ring has or may receive payment or benefits from Skeletal Dynamics, Wright Medical for elbow implants, Deputy Editor for Clinical Orthopaedics and Related Research, Universities and Hospitals, Lawyers outside the submitted work.
Dr. Teunis has or may receive payment or benefits from VCC, PATIENT+, and AO Trauma TK network unrelated to this work and consultant fees from Synthes.
1. Jackson JL, Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52:609-620.
2. Menendez ME, Chen NC, Mudgal CS, et al. Physician empathy as a driver of hand surgery patient satisfaction. J Hand Surg Am. 2015;40(9):1860-1865.
3. Parrish RC 2nd, Menendez ME, Mudgal CS, et al. Patient Satisfaction and its relation to perceived visit duration with a hand surgeon. J Hand Surg Am. 2016;41(2):257-262.
4. Waters S, Edmondston SJ, Yates PJ, Gucciardi DF. Identification of factors influencing patient satisfaction with orthopaedic outpatient clinic consultation: A qualitative study. Man Ther. 2016;25:48-55.
5. Voutilainen A, Pitkaaho T, Kvist T, Vehvilainen-Julkunen K. How to ask about patient satisfaction? The visual analogue scale is less vulnerable to confounding factors and ceiling effect than a symmetric Likert scale. J Adv Nurs. 2016;72:946-957.
6. van Berckel MM, Bosma NH, Hageman MG, et al. The correlation between a numerical rating scale of patient satisfaction with current management of an upper extremity disorder and a general measure of satisfaction with the medical visit. Hand (N Y). 2017;12:202-206.
7. Garcia D, Bautista O, Venereo L, et al. Training in empathic skills improves the patient-physician relationship during the first consultation in a fertility clinic. Fertil Steril. 2013;99:1413-1418.
8. Fitzpatrick RM, Hopkins A. Patients’ satisfaction with communication in neurological outpatient clinics. J Psychosom Res. 1981;25:329-334.
9. Kincey J, Bradshaw P, Ley P. Patients’ satisfaction and reported acceptance of advice in general practice. J R Coll Gen Pract. 1975;25:558-566.
10. Ley P, Whitworth MA, Skilbeck CE, et al. Improving doctor-patient communication in general practice. J R Coll Gen Pract. 1976;26:720-724.
11. Meakin R, Weinman J. The ‘Medical Interview Satisfaction Scale’ (MISS-21) adapted for British general practice. Fam Pract. 2002;19:257-263.
12. Wolf MH, Putnam SM, James SA, Stiles WB. The Medical Interview Satisfaction Scale: development of a scale to measure patient perceptions of physician behavior. J Behav Med. 1978;1:391-401.
13. Kane GC, Gotto JL, Mangione S, et al. Jefferson Scale of Patient’s Perceptions of Physician Empathy: preliminary psychometric data. Croat Med J. 2007;48:81-86.
14. Beckmann JT , Hung M, Voss MW, et al. Evaluation of the patient-reported outcomes measurement information system upper extremity computer adaptive test. J Hand Surg Am. 2016;41:739-744.
15. PROMIS. PROMIS PF Scoring. Available at www.healthmeasures.net/administrator/components/com_instruments/uploads/PROMIS%20Physical%20Function%20Scoring%20Manual.pdf. Accessed March 1, 2019.
16. PROMIS. PROMIS Measures. Available at wwwnihpromisorg. Accessed March 1, 2019.
17. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-381.
18. Bot AG, Anderson JA, Neuhaus V, Ring D. Factors associated with survey response in hand surgery research. Clin Orthop Relat Res. 2013;471(10):3237-3242.
19. Sedgwick P, Greenwood N. Understanding the Hawthorne effect. BMJ. 2015;351:h4672.
20. Ross CK, Steward CA, Sinacore JM. A comparative study of seven measures of patient satisfaction. Med Care. 1995;33:392-406.
21. Teunis T, Thornton ER, Jayakumar P, Ring D. Time seeing a hand surgeon is not associated with patient satisfaction. Clin Orthop Relat Res. 2015;473:2362-2368.
1. Jackson JL, Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52:609-620.
2. Menendez ME, Chen NC, Mudgal CS, et al. Physician empathy as a driver of hand surgery patient satisfaction. J Hand Surg Am. 2015;40(9):1860-1865.
3. Parrish RC 2nd, Menendez ME, Mudgal CS, et al. Patient Satisfaction and its relation to perceived visit duration with a hand surgeon. J Hand Surg Am. 2016;41(2):257-262.
4. Waters S, Edmondston SJ, Yates PJ, Gucciardi DF. Identification of factors influencing patient satisfaction with orthopaedic outpatient clinic consultation: A qualitative study. Man Ther. 2016;25:48-55.
5. Voutilainen A, Pitkaaho T, Kvist T, Vehvilainen-Julkunen K. How to ask about patient satisfaction? The visual analogue scale is less vulnerable to confounding factors and ceiling effect than a symmetric Likert scale. J Adv Nurs. 2016;72:946-957.
6. van Berckel MM, Bosma NH, Hageman MG, et al. The correlation between a numerical rating scale of patient satisfaction with current management of an upper extremity disorder and a general measure of satisfaction with the medical visit. Hand (N Y). 2017;12:202-206.
7. Garcia D, Bautista O, Venereo L, et al. Training in empathic skills improves the patient-physician relationship during the first consultation in a fertility clinic. Fertil Steril. 2013;99:1413-1418.
8. Fitzpatrick RM, Hopkins A. Patients’ satisfaction with communication in neurological outpatient clinics. J Psychosom Res. 1981;25:329-334.
9. Kincey J, Bradshaw P, Ley P. Patients’ satisfaction and reported acceptance of advice in general practice. J R Coll Gen Pract. 1975;25:558-566.
10. Ley P, Whitworth MA, Skilbeck CE, et al. Improving doctor-patient communication in general practice. J R Coll Gen Pract. 1976;26:720-724.
11. Meakin R, Weinman J. The ‘Medical Interview Satisfaction Scale’ (MISS-21) adapted for British general practice. Fam Pract. 2002;19:257-263.
12. Wolf MH, Putnam SM, James SA, Stiles WB. The Medical Interview Satisfaction Scale: development of a scale to measure patient perceptions of physician behavior. J Behav Med. 1978;1:391-401.
13. Kane GC, Gotto JL, Mangione S, et al. Jefferson Scale of Patient’s Perceptions of Physician Empathy: preliminary psychometric data. Croat Med J. 2007;48:81-86.
14. Beckmann JT , Hung M, Voss MW, et al. Evaluation of the patient-reported outcomes measurement information system upper extremity computer adaptive test. J Hand Surg Am. 2016;41:739-744.
15. PROMIS. PROMIS PF Scoring. Available at www.healthmeasures.net/administrator/components/com_instruments/uploads/PROMIS%20Physical%20Function%20Scoring%20Manual.pdf. Accessed March 1, 2019.
16. PROMIS. PROMIS Measures. Available at wwwnihpromisorg. Accessed March 1, 2019.
17. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-381.
18. Bot AG, Anderson JA, Neuhaus V, Ring D. Factors associated with survey response in hand surgery research. Clin Orthop Relat Res. 2013;471(10):3237-3242.
19. Sedgwick P, Greenwood N. Understanding the Hawthorne effect. BMJ. 2015;351:h4672.
20. Ross CK, Steward CA, Sinacore JM. A comparative study of seven measures of patient satisfaction. Med Care. 1995;33:392-406.
21. Teunis T, Thornton ER, Jayakumar P, Ring D. Time seeing a hand surgeon is not associated with patient satisfaction. Clin Orthop Relat Res. 2015;473:2362-2368.