User login
Postdischarge Follow‐Up Visits for Medical/Pharmacy Students
The increasing burden of chronic illness has prompted concerns about the traditional education model that focuses on management of acute disease.13 Chronic illness has replaced acute disease as the major cause of disability and total national health care expenditures.46 Medical educators have called for improved chronic disease curricula,2, 3 and the Institute of Medicine has asserted that health professions, including medicine and pharmacy, must reexamine how students are educated to manage patients with complex illnesses.7, 8 Despite the rising prevalence of chronic illness, the positive attitudes of medical students toward providing care to such patients decline during training.2, 9 One theory is that the current model of core clerkship training excessively exposes students to highly complex, seriously ill hospitalized patients. Students may become disillusioned and overwhelmed by these encounters, particularly without the opportunity to see improvement or thriving in the outpatient setting.2
There are few curricula on how to transition chronically ill patients from an inpatient to an outpatient setting and the inherent safety risks of this transition. For these patients, the posthospital discharge period is particularly confusing because of the sudden change in health status and new medication regimens.1012 It is very likely that communication among providers and patients will be insufficient during the discharge process,11, 1315 yet physicians tend to overestimate patients' understanding of postdischarge treatment plans and thereby underanticipate problems.16 One intervention to address these concerns is a postdischarge visit. Home visits have been shown to improve students' understanding of continuity of care and of the impact of chronic illness on their patients' medical and psychosocial situations.1719
There is scant structured teaching of third‐year medical students about another critical aspect of transitional care: the role of different health care disciplines. Although research about the impact of undergraduate interdisciplinary education on patient outcomes is limited, training students in interdisciplinary collaboration may improve their ability to provide quality care.2022 Multiple disciplines are critical for a smooth transition of chronically ill patients from an inpatient to an outpatient setting. In particular, pharmacist involvement in a predischarge medication review, patient counseling, and telephone follow‐up has been associated with improved outcomes.11, 12, 23, 24 Early introduction of interdisciplinary team training can improve student attitudes about working within a team.25
To teach the importance of safe discharges and interdisciplinary collaboration in caring for chronically ill patients, we developed an inpatient medicine clerkship curriculum for medical and pharmacy students that included postdischarge visits to students' own team patients. The purpose of the study was to assess the impact of this didactic and experiential curriculum on students' attitudes and self‐assessed skills in the interdisciplinary care and transitional care of chronically ill patients. We hypothesized that the discharge curriculum would improve student attitudes and self‐assessed skills in these domains. Finally, we hypothesized that visiting a patient's home would highlight for students the potential challenges of care transitions for patients.
METHODS
Participants and Setting
Participants were third‐year medical students on an 8‐week internal medicine (IM) clerkship and fourth‐year pharmacy students on a 6‐week pharmacy practice clerkship at a tertiary‐care university‐based hospital between April 2005 and April 2006. The hospital is 1 of 3 IM clerkship sites for medical students and 1 of 9 for pharmacy students. This site was selected because it included both medical and pharmacy students on most inpatient teams.
Clerkship students were assigned to all 7 medical teams, each consisting of an attending physician, a senior IM resident (postgraduate year 2 or 3), 2 IM interns (postgraduate year 1), 1 or 2 medical students, and up to 1 pharmacy student. Hospitalists covered 52% of inpatient months, with the remainder staffed by faculty primary care physicians, specialists, or chief residents. Although only three‐quarters of the medical teams were randomly assigned a pharmacy student at any given point, each team had a pharmacy student for a portion of time that overlapped with the rotation of the medical students. Over the year, 810 medical students rotated on the service during each of 6 blocks, and 46 pharmacy students and 1 pharmacy practice resident rotated during each of 8 blocks. The pharmacy students rotated on a different schedule than the medical students, and thus the curriculum was scheduled around the medical students' clerkship.
The Institutional Review Board of the University of California at San Francisco approved the study.
Intervention (Curriculum Description)
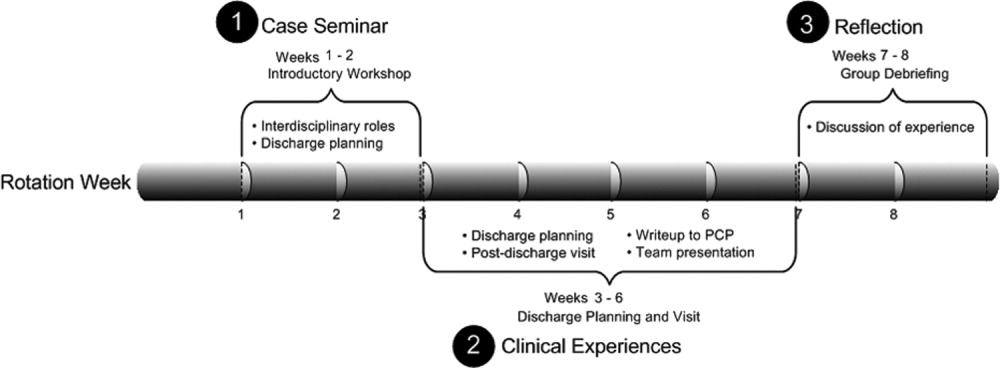
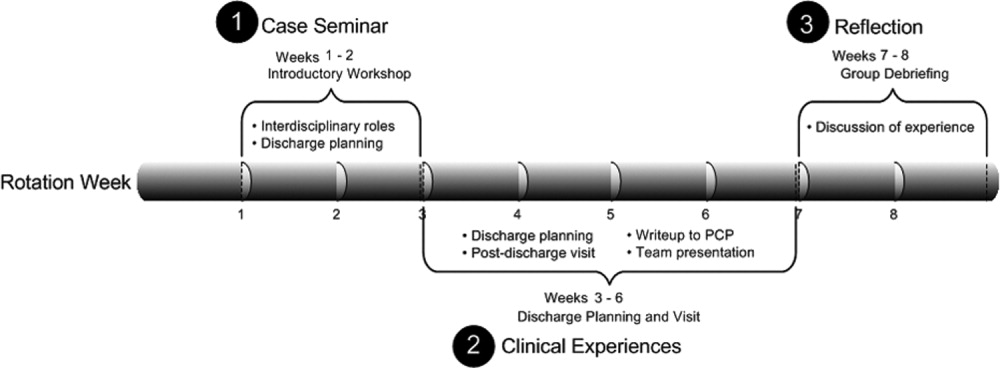
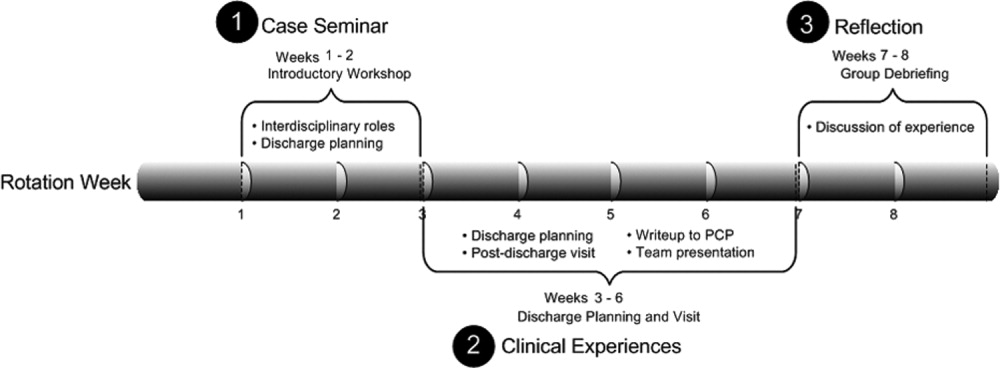
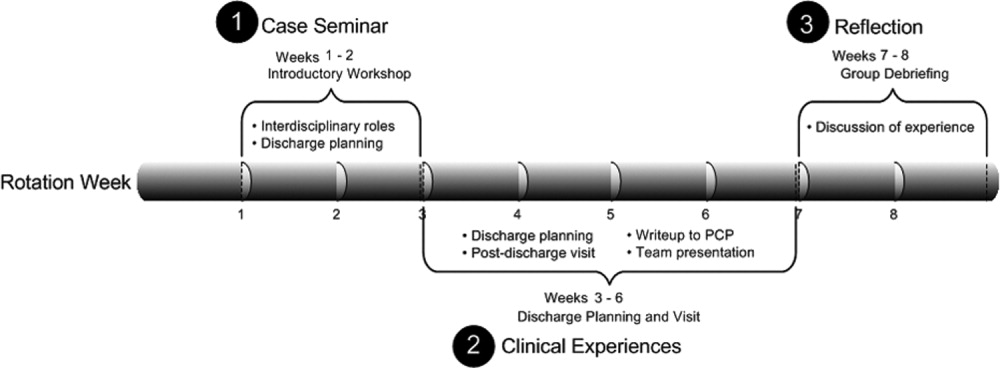
We developed a 3‐part pilot interdisciplinary curriculum (Fig. 1). During the first 2 weeks of the IM clerkship, interdisciplinary faculty, including 3 pharmacists, 2 hospitalists, and occasionally a social worker and geriatric clinical nurse specialist, led a 1‐hour interactive workshop on transitional care. The 3 workshop topics were: roles that various disciplines such as social work and pharmacy play in discharge care; the challenges a patient faces around the time of discharge, using a typical case; and discussion of elements of a postdischarge visit.
Medical and pharmacy students were partnered based on clerkship team assignments in teams of up to 3 student partners (1 or 2 medical students and 1 pharmacy student). Partners were advised to select a consenting patient known to them from the ward team for 1 postdischarge visit. Suggested selection criteria were at least 1 chronic illness, 1 prior hospitalization, and older than age 65 because patients fitting these criteria are most at risk for readmission or adverse outcomes following discharge.15, 26, 27 The student partners scheduled a postdischarge visit by the end of the rotation to the patient's home, nursing home, or subacute care facility. Each patient and the patient's primary care provider (PCP) gave informed consent.
During the postdischarge visit, student partners assessed medication discrepancies, environmental safety, and clinical status using structured data collection protocols developed by the investigators after review of the literature.28, 29 After the visit, students reported back to the ward teams on the patient's status and wrote a visit summary letter to the patient's PCP. The letter described the patient's clinical status and home environment, any medication discrepancies, and follow‐up plans and included a reflection piece. Reflection questions included, How did the visit change your perspective of patient discharge? What were the most critical aspects of this or any discharge? How do you think this experience will affect your future practice? What was the best thing about this experience?
During the last 2 weeks of the rotation, all student participants met with faculty preceptors for an hour‐long group debriefing session on the postdischarge visits.
Survey Instrument and Procedure
Students were asked to complete a presurvey at the beginning of the first workshop and a postsurvey at the end of the second (debriefing) workshop. The surveys contained self‐assessment questions on attitudes and skills in 3 domains: interdisciplinary care, chronic illness management, and transitional care. Questions were developed and tested with IM faculty with experience in student education and with ineligible students on previous rotations, and questions were revised for clarity and comprehensiveness. Students had the option to write a 4‐digit identifier on the pre‐ and postsurveys to allow matched analysis.
The 10‐item presurvey contained 4 items on interdisciplinary care and 3 each on chronic care and follow‐up visits. We reviewed surveys in the literature regarding home care and chronic illness to inform the development of our survey.30, 31 Students rated each item on a 5‐point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). The 22‐item postsurvey included the same 10 items and additional Likert‐scaled questions on satisfaction with the curriculum. Two open‐ended questions solicited opinions about the value of the program and lessons learned for future patient encounters.
Statistical Analysis
We assessed the mean Likert score ( SD) for each presurvey and postsurvey question and compared means ( SD). We evaluated the differences between medical students and for pharmacy students in mean Likert score on the surveys using a dependent‐samples t test and set the level of significance at 0.05.
Change in scores between prepost survey variables were calculated overall and within student type (medicine vs. pharmacy). Because no intercorrelations and possible patterns indicating a structure were found, a factor analysis was not conducted.
Two investigators (C.L., H.N.) read all written responses to the open‐ended questions and independently generated a list of themes. The list was reconciled through discussion and was used to code all comments in order to determine the frequency of each theme. Discrepancies were discussed until consensus was reached.
RESULTS
Participants
Ninety‐seven percent of eligible students (37 of 39 medical students and 22 of 22 pharmacy students) completed the curriculum. Two medical students did not complete the home visit because their patients did not keep the appointment. The presurvey response was 100% for medical students and 91% for pharmacy students. The postsurvey response was 92% for medical students and 86% for pharmacy students; 58% of medical students and 59% of pharmacy students wrote in matching prepost survey identifiers for statistical analysis. Prepost survey responses showed an increase for both student groups in positive attitudes and self‐assessed skill in interdisciplinary collaboration, chronic illness management, and transitional care. Trends over time were highly significant for individual items on matched surveys (P < 0.05; Table 1a,b).
| Question | Medical students (matched respondents n = 23) | Pharmacy students (matched respondents n = 13) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Presurvey, mean (SD) | Postsurvey, mean (SD) | Mean difference | P value | Effect size | Presurvey, mean (SD) | Postsurvey, mean (SD) | Mean difference | P value | Effect size | |
| ||||||||||
| 1. I am able to state the various roles of the pharmacy students and/or pharmacists (or medical students and/or physicians) in taking care of hospitalized patients. | 2.83 (0.89) | 4.35 (0.57) | 1.52 | < .001* | 1.72 | 3.69 (0.63) | 4.15 (0.38) | 0.46 | .03* | 0.73 |
| 2. I am able to state the various roles of the case manager and/or social worker in taking care of hospitalized patients. | 2.83 (0.78) | 3.91 (0.42) | 1.09 | < .001* | 1.40 | 2.77 (0.83) | 3.54 (0.97) | 0.77 | .01* | 0.92 |
| 3. I am confident in my ability to work with a pharmacy student or pharmacist (or medical student and/or physician) in taking care of inpatients with chronic illness. | 3.22 (1.00) | 4.52 (0.51) | 1.30 | < .001* | 1.31 | 3.62 (0.87) | 4.23 (0.44) | 0.62 | .04* | 0.71 |
| 4. I am confident in my ability to work with a case manager and/or social worker in taking care of inpatients with chronic illness. | 2.96 (0.71) | 3.96 (0.56) | 1.00 | < .001* | 1.42 | 3.08 (0.95) | 3.38 (0.87) | 0.31 | .34 | 0.32 |
| 5. I am confident in my ability to involve patients in making a plan for their care. | 3.74 (0.62) | 4.26 (0.54) | 0.52 | < .001* | 0.84 | 3.23 (0.60) | 4.15 (0.55) | 0.92 | < .001* | 1.54 |
| 6. I am able to assist patients in solving problems they encounter in self‐management of their chronic illness. | 3.30 (0.70) | 3.91 (0.60) | 0.61 | < .001* | 0.87 | 3.75 (0.87) | 3.92 (0.49) | 0.17 | .50 | 0.20 |
| 7. I am confident in my ability to review patients' medications and side effects. | 3.00 (0.85) | 3.70 (0.76) | 0.70 | < .001* | 0.82 | 3.92 (0.76) | 4.46 (0.52) | 0.54 | .03* | 0.71 |
| 8. I am able to review the goals of a follow‐up visit with a patient. | 3.52 (0.95) | 4.43 (0.51) | 0.91 | < .001* | 0.96 | 3.08 (0.76) | 3.62 (0.77) | 0.54 | .05 | 0.71 |
| 9. I can identify factors that may facilitate or impede a patient's transition to an outpatient setting. | 3.48 (0.51) | 4.35 (0.49) | 0.87 | < .001* | 1.70 | 3.00 (0.82) | 3.85 (0.69) | 0.85 | .01* | 1.04 |
| 10. I can identify several topics for review at a follow‐up visit to confirm a safe transition to an outpatient setting. | 3.39 (0.94) | 4.52 (0.59) | 1.13 | < .001* | 1.20 | 3.23 (0.73) | 3.77 (0.73) | 0.54 | .11 | 0.74 |
Twenty‐two student partners of 1 or 2 medical students and 1 pharmacy student visited 22 patients (64% women; mean age 71 years). Most visits (91%) occurred at patients' homes.
Students were satisfied with the curriculum (Table 2). Both the medical and the pharmacy students perceived the 2 most valuable components to be the interdisciplinary collaboration on patient care and the postdischarge visit, followed by the debriefing session. The least useful were the initial workshop on interdisciplinary roles and the write‐up to the PCP. Ninety‐one percent of students agreed that they learned skills valuable for future patient care (medical students 4.4, SD 0.61; pharmacy students 4.1, SD 0.62; Table 3). Most students agreed that the program enhanced their learning about interdisciplinary care (4.3, SD 0.72), discharge planning (4.4, SD 0.70), and humanism (4.4, SD 0.63). Ninety‐three percent agreed that this curriculum was valuable to their education.
| Component | Mean score* (SD) | Rated very good or excellent (%) |
|---|---|---|
| ||
| Joint patient care with medical/pharmacy student | 4.5 (1.04) | 94% |
| Postdischarge visit | 4.3 (0.68) | 91% |
| Debriefing session | 3.9 (1.04) | 75% |
| Team presentation after patient visit | 3.7 (1.32) | 63% |
| Case‐based workshop | 3.6 (1.18) | 54% |
| Write‐up on experience | 3.4 (0.81) | 48% |
| Overall program | 4.1 (1.14) | 86% |
| Medical students (n = 35) | Pharmacy students (n = 18) | All students (n = 53) | ||||
|---|---|---|---|---|---|---|
| Mean score* (SD) | Agree/strongly agree (%) | Mean score (SD) | Agree/strongly agree (%) | Mean score (SD) | Agree/strongly agree (%) | |
| ||||||
| I have learned skills from this program that I plan to apply to future patient care experiences. | 4.4 (0.61) | 94% | 4.1 (0.62) | 84% | 4.3 (0.63) | 91% |
| This program added to my learning about an interdisciplinary approach to patient care beyond the other experiences of this clerkship. | 4.3 (0.74) | 91% | 4.2 (0.71) | 84% | 4.3 (0.72) | 89% |
| This program added to my learning about discharge planning and transitional care beyond the other experiences of this clerkship. | 4.4 (0.66) | 91% | 4.2 (0.79) | 89% | 4.4 (0.70) | 91% |
| This program added to my understanding of a patient as a whole person beyond the other experiences of this clerkship. | 4.3 (0.69) | 89% | 4.5 (0.51) | 100% | 4.4 (0.63) | 93% |
| This program was valuable to my medical education. | 4.3 (0.74) | 91% | 4.4 (0.60) | 95% | 4.4 (0.68) | 93% |
Open‐Ended Comments on Educational Value
Twenty‐nine medical students and 15 pharmacy students wrote responses to the open‐ended questions. Students identified the most valuable component of the curriculum as seeing patients at home in their social context (30 total comments). In the reflection write‐up, one student explained,
I was unaware of the types of living conditions many patients face, especially in the setting of chronic disease. In the future I will try to gain a more detailed understanding of my patients' social situations in order to help identify and anticipate problems in the management of their medical issues.
Thirteen students commented that working as an interdisciplinary team was a valuable experience. Eight students expressed appreciation at learning about transitional care and the components of discharge planning.
I was a little surprised during this home visit to find how much Ms. C had altered her medication regimen. She didn't like how she was feeling on the higher blood pressure medications, so she halved them. She doesn't really like taking pills, in general, so she stopped taking the aspirin, Senna, and Colace. I suppose something that might have made this discharge more successful would have been if we had really elicited her preferences regarding medications while she was in the hospital, such that we could have been more selective in what we prescribed and very clear with her with respect to what exactly we were hoping to accomplish with each.
During group debriefing, students reinforced the themes in their written comments and shared additional reflections. Students observed a shift in dynamics between patient and student provider; the patients appeared more comfortable in familiar settings. Students were also surprised that many of their patients did not have a clear understanding of medication regimens at home. In addition, they discussed the importance of communicating with patients' PCPs about the hospital course and follow‐up.
Also during the debriefing, students expressed the value of the postdischarge visit and interdisciplinary collaboration. Medical students appreciated seeing how the pharmacy students reviewed medications and taught patients how to use their medications. However, the students thought that preparation of paperwork prior to the visit and the write‐up seemed less valuable.
DISCUSSION
A discharge curriculum that included a postdischarge visit to a recently hospitalized patient improved the attitudes and self‐assessed skills of third‐year medical students and fourth‐year pharmacy students about interdisciplinary collaboration and transitions in care. It also deepened their appreciation of the impact of chronic illness on individual patients. To our knowledge, this is the first study to report an interdisciplinary curriculum with postdischarge home visits for students on their inpatient medicine clerkship.
Our curriculum was unique because its activities were linked to patients the students had cared for in the inpatient setting, a relationship that was key to students accepting the curriculum, as was the autonomy they had in selecting one of their patients for a visit. Although home visits are often part of medical school training, they generally occur in the preclinical years5, 19 or during third‐year primary care rotations, during which students are assigned patients at home or in outpatient facilities.17, 32 Home visits have been qualitatively reported to be a valuable aspect of geriatric, primary care, and other ambulatory‐based rotations of medical students.17, 19, 32 Postdischarge visits in graduate medical education have been shown to improve residents' awareness of and skills with transitions in care.28, 33, 34
Another novel aspect of this curriculum was the interdisciplinary collaboration in discharge planning and postdischarge visits. Although educators have implemented conferences on interdisciplinary education in preclinical medical education,3537 patient‐centered curricula in real‐time allow realistic interdisciplinary collaboration between medical and pharmacy students in their core clerkships. In our study, quantitative and qualitative data showed that the student partners valued each other's expertise in the context of a clinically relevant activitydischarge planning and a follow‐up home visit. Students reported confidence in their collaborative abilities after completing the curriculum, and comments supported a broadened understanding of other professionals' roles in patient care. Given that pharmacist involvement in discharge planning has been shown to improve patient outcomes,11, 24 our study supports the idea that medical educators should develop structured curricula on interdisciplinary training in core clerkships.
By evaluating the impact of hospitalization and chronic illness on their patients after discharge, our students developed an appreciation for safe transitions and opportunities to improve patients' health and level of function. We observed that students also appreciated the positive effect of the home environment on patient health and well‐being. From their postdischarge visit, students also became aware of the need for communication with primary care providers, particularly for patients with comorbidities. This type of transitional care experience may help to counter the negative attitudes toward chronic illness that students typically develop during clerkships.2, 9, 38, 39
Of note, although pharmacy students reported improvement in their attitudes and skills with transitional care, the trend toward significance was less than that for medical students. This difference was consistent with the broader rotation goals of each group. At the end of the curriculum, the pharmacy students expressed more comfort with medication review than did medical students, although the latter were better able to conduct transitional care including postdischarge visits and identification of barriers or facilitators to a safe discharge. Another interesting note is that pharmacy students came into the curriculum with a better understanding of the roles of physicians, whereas the medical students had a less clear idea of the pharmacist's role. A possible explanation is that pharmacy students are better trained in their preclinical years to work as a team with medical personnel. The pharmacy school curriculum places an emphasis on independent learning and interdisciplinary collaboration, which may lead to the greater comfort felt by the pharmacy students.
This study had several limitations. The absolute number of visits was small overall; however, nearly all student partners completed their visits. Although the response rate to the postcurriculum survey was high, the response rate to matched prepost surveys was lower. In addition, the survey questions were not validated. Further, although there was significant improvement in students' attitudes and self‐assessed skills after completion of the curriculum, we cannot be certain whether this improvement was a result of the curriculum or of other rotation experiences. We attempted to clarify this effect by asking if the curriculum added to their learning beyond other clerkship experiences, and students perceived that our curriculum was responsible for the positive effect. Also, the curriculum was used at 1 academic site and may not be generalizable to other hospitals, student populations, or team structures. The patients were selected by students, and thus the results may not be reproducible for every population; in some situations, students had to ask several patients until a patient consented to a postdischarge visit.
In implementing this interdisciplinary curriculum, we were challenged by the discordant schedules of the medical and pharmacy students. Initially, it was also difficult to overcome students' concerns about adding an additional expectation to an already busy rotation. The medical students, in particular, voiced concerns about having to leave the hospital during their inpatient rotation. However, this has become much less of an issue with time as the value of the postdischarge visit has become clear to students and team members, with the latter now aware of and supportive of the program.
This discharge curriculum represents a clinically relevant experience that addresses national educational mandates regarding interdisciplinary care and chronic illness across care settings. We are now expanding the curriculum from the original site to our other clerkship sites and are evaluating its impact on patient safety and clinical outcomes. Future research should focus on whether these interdisciplinary postdischarge patient visits lead to improved attitudes and skills during residency training or practice and whether, ultimately, they lead to improved patient outcomes.
Acknowledgements
The authors gratefully acknowledge Deborah Airo for editorial review and Kathleen Kerr for statistical support.
- ,,,,,.Medical students' experiences with and perceptions of chronic illness prior to medical school.Med Educ.1993;27:355–359.
- ,,,,,.Do clerkship experiences affect medical students' attitudes toward chronically ill patients?Acad Med.2001;76:815–820.
- ,,,,.More training needed in chronic care: a survey of US physicians.Acad Med.2004;79:541–548.
- .Chronic disease—the need for a new clinical education.JAMA.2004;292:1057–1059.
- ,,.Medical students as health coaches.Acad Med.2002;77:1164–1166.
- ,,.Persons with chronic conditions. Their prevalence and costs.JAMA.1996;276:1473–1479.
- ,,.To Err Is Human.Washington, DC:National Academy Press;2000.
- Institute of Medicine.Health Professions Education: A Bridge to Quality.Washington DC:National Academy Press;2000.
- ,.The loss of student idealism in the 3rd‐year clinical clerkships.Eval Health Prof.2001:24:61–71.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20:317–323.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- ,,,,.Does the addition of a pharmacist transition coordinator improve evidence‐based medication management and health outcomes in older adults moving from the hospital to a long‐term care facility? Results of a randomized, controlled trial.Am J Geriatr Pharmacother.2004;2:257–264.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,,.Posthospital medication discrepancies: Prevalence and contributing factors.Arch Intern Med.2005;165:1842–1847.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,, et al.Patient‐physician communication at hospital discharge and patients' understanding of the postdischarge treatment plan.Arch Intern Med.1997;157:1026–1030.
- ,,,,,.Reflections of medical students on visiting chronically ill older patients in the home.J Am Geriatr Soc.2006;54:1778–1783.
- ,,.Home care.JAMA.2003;290:1203–1207.
- ,,,,,.Mi casa o su casa? Assessing function and values in the home.J Am Geriatr Soc.2005;53:336–342.
- ,.Interdisciplinary education, and teamwork: a long and winding road.Med Educ.2001;35:867–875.
- ,,.Interdisciplinary education: evaluation of a palliative care training intervention for pre‐professionals.Acad Med.2004;79:769–776.
- ,.Effective interdisciplinary training: Lessons from the University of North Carolina's Student Health Action Coalition.Acad Med.2006;81:749–759.
- ,,,.The impact of follow‐up telephone calls to patients after hospitalization.Am J Med.2001;111(9B):26S–30S.
- ,,,.Clinical pharmacists and inpatient medical care: A systematic review.Arch Intern Med.2006;166:955–964.
- ,,,.Developing an evidence base for interdisciplinary learning: a systematic review.J Adv Nurs.2001;35:228–237.
- ,,,,,.Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan.Am J Med.1999;107:13–17.
- ,,.Risk factors for early unplanned hospital readmission in the elderly.J Gen Intern Med.1991;6:223–228.
- ,,, et al.Hospital to home: Improving internal medicine residents' understanding of the needs of older persons after a hospital stay.Acad Med.2003;78:793–797.
- . Care transitions program. University of Colorado at Denver, Health Sciences Center. Available at: http://www.caretransitions.org/index.asp. Accessed April 9,2007.
- ,,,,,.Validation of an instrument designed to assess medical student attitudes toward home care.J Am Geriatr Soc.2001;49:470–473.
- Patient Assessment of Chronic Illness Care (PACIC) from Improving Chronic Illness Care, a national program of the Robert Wood Johnson Foundation. Available at: http://improvingchroniccare.org/tools/pacic.htm. Accessed April 9,2007.
- ,,,,.The determinants of attitudinal change among medical students participating in home care training: A multi‐center study.Acad Med.2002;77:336–343.
- ,,,,.There's no place like home: Evaluating family medicine residents' training in home care.Home Health Care Serv Q.2002;21:1–17.
- ,,.Geriatric follow‐up by home visits after discharge from hospital: a randomized controlled trial.Age Ageing.1992;21:445–450.
- ,,.Multiprofessional learning: the attitudes of medical nursing, and pharmacy students to shared learning.Med Educ.2001;35:876–883.
- ,,.Can participation in a health affairs interdisciplinary case conference improve medical students' knowledge and attitudes?Acad Med.2006;81:257–261.
- ,,, et al.Bringing interdisciplinary and multicultural team building to health care education: the Downstate Team‐Building Initiative.Acad Med.2005;80:74–83.
- , and.“It's always continuing”: First year medical students' perspectives on chronic illness and the care of chronically ill patients.Acad Med.2005;80:183–188.
- ,,,,,.Training U.S. medical students to care for the chronically ill.Acad Med.2004;79:32–40.
The increasing burden of chronic illness has prompted concerns about the traditional education model that focuses on management of acute disease.13 Chronic illness has replaced acute disease as the major cause of disability and total national health care expenditures.46 Medical educators have called for improved chronic disease curricula,2, 3 and the Institute of Medicine has asserted that health professions, including medicine and pharmacy, must reexamine how students are educated to manage patients with complex illnesses.7, 8 Despite the rising prevalence of chronic illness, the positive attitudes of medical students toward providing care to such patients decline during training.2, 9 One theory is that the current model of core clerkship training excessively exposes students to highly complex, seriously ill hospitalized patients. Students may become disillusioned and overwhelmed by these encounters, particularly without the opportunity to see improvement or thriving in the outpatient setting.2
There are few curricula on how to transition chronically ill patients from an inpatient to an outpatient setting and the inherent safety risks of this transition. For these patients, the posthospital discharge period is particularly confusing because of the sudden change in health status and new medication regimens.1012 It is very likely that communication among providers and patients will be insufficient during the discharge process,11, 1315 yet physicians tend to overestimate patients' understanding of postdischarge treatment plans and thereby underanticipate problems.16 One intervention to address these concerns is a postdischarge visit. Home visits have been shown to improve students' understanding of continuity of care and of the impact of chronic illness on their patients' medical and psychosocial situations.1719
There is scant structured teaching of third‐year medical students about another critical aspect of transitional care: the role of different health care disciplines. Although research about the impact of undergraduate interdisciplinary education on patient outcomes is limited, training students in interdisciplinary collaboration may improve their ability to provide quality care.2022 Multiple disciplines are critical for a smooth transition of chronically ill patients from an inpatient to an outpatient setting. In particular, pharmacist involvement in a predischarge medication review, patient counseling, and telephone follow‐up has been associated with improved outcomes.11, 12, 23, 24 Early introduction of interdisciplinary team training can improve student attitudes about working within a team.25
To teach the importance of safe discharges and interdisciplinary collaboration in caring for chronically ill patients, we developed an inpatient medicine clerkship curriculum for medical and pharmacy students that included postdischarge visits to students' own team patients. The purpose of the study was to assess the impact of this didactic and experiential curriculum on students' attitudes and self‐assessed skills in the interdisciplinary care and transitional care of chronically ill patients. We hypothesized that the discharge curriculum would improve student attitudes and self‐assessed skills in these domains. Finally, we hypothesized that visiting a patient's home would highlight for students the potential challenges of care transitions for patients.
METHODS
Participants and Setting
Participants were third‐year medical students on an 8‐week internal medicine (IM) clerkship and fourth‐year pharmacy students on a 6‐week pharmacy practice clerkship at a tertiary‐care university‐based hospital between April 2005 and April 2006. The hospital is 1 of 3 IM clerkship sites for medical students and 1 of 9 for pharmacy students. This site was selected because it included both medical and pharmacy students on most inpatient teams.
Clerkship students were assigned to all 7 medical teams, each consisting of an attending physician, a senior IM resident (postgraduate year 2 or 3), 2 IM interns (postgraduate year 1), 1 or 2 medical students, and up to 1 pharmacy student. Hospitalists covered 52% of inpatient months, with the remainder staffed by faculty primary care physicians, specialists, or chief residents. Although only three‐quarters of the medical teams were randomly assigned a pharmacy student at any given point, each team had a pharmacy student for a portion of time that overlapped with the rotation of the medical students. Over the year, 810 medical students rotated on the service during each of 6 blocks, and 46 pharmacy students and 1 pharmacy practice resident rotated during each of 8 blocks. The pharmacy students rotated on a different schedule than the medical students, and thus the curriculum was scheduled around the medical students' clerkship.
The Institutional Review Board of the University of California at San Francisco approved the study.
Intervention (Curriculum Description)
We developed a 3‐part pilot interdisciplinary curriculum (Fig. 1). During the first 2 weeks of the IM clerkship, interdisciplinary faculty, including 3 pharmacists, 2 hospitalists, and occasionally a social worker and geriatric clinical nurse specialist, led a 1‐hour interactive workshop on transitional care. The 3 workshop topics were: roles that various disciplines such as social work and pharmacy play in discharge care; the challenges a patient faces around the time of discharge, using a typical case; and discussion of elements of a postdischarge visit.
Medical and pharmacy students were partnered based on clerkship team assignments in teams of up to 3 student partners (1 or 2 medical students and 1 pharmacy student). Partners were advised to select a consenting patient known to them from the ward team for 1 postdischarge visit. Suggested selection criteria were at least 1 chronic illness, 1 prior hospitalization, and older than age 65 because patients fitting these criteria are most at risk for readmission or adverse outcomes following discharge.15, 26, 27 The student partners scheduled a postdischarge visit by the end of the rotation to the patient's home, nursing home, or subacute care facility. Each patient and the patient's primary care provider (PCP) gave informed consent.
During the postdischarge visit, student partners assessed medication discrepancies, environmental safety, and clinical status using structured data collection protocols developed by the investigators after review of the literature.28, 29 After the visit, students reported back to the ward teams on the patient's status and wrote a visit summary letter to the patient's PCP. The letter described the patient's clinical status and home environment, any medication discrepancies, and follow‐up plans and included a reflection piece. Reflection questions included, How did the visit change your perspective of patient discharge? What were the most critical aspects of this or any discharge? How do you think this experience will affect your future practice? What was the best thing about this experience?
During the last 2 weeks of the rotation, all student participants met with faculty preceptors for an hour‐long group debriefing session on the postdischarge visits.
Survey Instrument and Procedure
Students were asked to complete a presurvey at the beginning of the first workshop and a postsurvey at the end of the second (debriefing) workshop. The surveys contained self‐assessment questions on attitudes and skills in 3 domains: interdisciplinary care, chronic illness management, and transitional care. Questions were developed and tested with IM faculty with experience in student education and with ineligible students on previous rotations, and questions were revised for clarity and comprehensiveness. Students had the option to write a 4‐digit identifier on the pre‐ and postsurveys to allow matched analysis.
The 10‐item presurvey contained 4 items on interdisciplinary care and 3 each on chronic care and follow‐up visits. We reviewed surveys in the literature regarding home care and chronic illness to inform the development of our survey.30, 31 Students rated each item on a 5‐point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). The 22‐item postsurvey included the same 10 items and additional Likert‐scaled questions on satisfaction with the curriculum. Two open‐ended questions solicited opinions about the value of the program and lessons learned for future patient encounters.
Statistical Analysis
We assessed the mean Likert score ( SD) for each presurvey and postsurvey question and compared means ( SD). We evaluated the differences between medical students and for pharmacy students in mean Likert score on the surveys using a dependent‐samples t test and set the level of significance at 0.05.
Change in scores between prepost survey variables were calculated overall and within student type (medicine vs. pharmacy). Because no intercorrelations and possible patterns indicating a structure were found, a factor analysis was not conducted.
Two investigators (C.L., H.N.) read all written responses to the open‐ended questions and independently generated a list of themes. The list was reconciled through discussion and was used to code all comments in order to determine the frequency of each theme. Discrepancies were discussed until consensus was reached.
RESULTS
Participants
Ninety‐seven percent of eligible students (37 of 39 medical students and 22 of 22 pharmacy students) completed the curriculum. Two medical students did not complete the home visit because their patients did not keep the appointment. The presurvey response was 100% for medical students and 91% for pharmacy students. The postsurvey response was 92% for medical students and 86% for pharmacy students; 58% of medical students and 59% of pharmacy students wrote in matching prepost survey identifiers for statistical analysis. Prepost survey responses showed an increase for both student groups in positive attitudes and self‐assessed skill in interdisciplinary collaboration, chronic illness management, and transitional care. Trends over time were highly significant for individual items on matched surveys (P < 0.05; Table 1a,b).
| Question | Medical students (matched respondents n = 23) | Pharmacy students (matched respondents n = 13) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Presurvey, mean (SD) | Postsurvey, mean (SD) | Mean difference | P value | Effect size | Presurvey, mean (SD) | Postsurvey, mean (SD) | Mean difference | P value | Effect size | |
| ||||||||||
| 1. I am able to state the various roles of the pharmacy students and/or pharmacists (or medical students and/or physicians) in taking care of hospitalized patients. | 2.83 (0.89) | 4.35 (0.57) | 1.52 | < .001* | 1.72 | 3.69 (0.63) | 4.15 (0.38) | 0.46 | .03* | 0.73 |
| 2. I am able to state the various roles of the case manager and/or social worker in taking care of hospitalized patients. | 2.83 (0.78) | 3.91 (0.42) | 1.09 | < .001* | 1.40 | 2.77 (0.83) | 3.54 (0.97) | 0.77 | .01* | 0.92 |
| 3. I am confident in my ability to work with a pharmacy student or pharmacist (or medical student and/or physician) in taking care of inpatients with chronic illness. | 3.22 (1.00) | 4.52 (0.51) | 1.30 | < .001* | 1.31 | 3.62 (0.87) | 4.23 (0.44) | 0.62 | .04* | 0.71 |
| 4. I am confident in my ability to work with a case manager and/or social worker in taking care of inpatients with chronic illness. | 2.96 (0.71) | 3.96 (0.56) | 1.00 | < .001* | 1.42 | 3.08 (0.95) | 3.38 (0.87) | 0.31 | .34 | 0.32 |
| 5. I am confident in my ability to involve patients in making a plan for their care. | 3.74 (0.62) | 4.26 (0.54) | 0.52 | < .001* | 0.84 | 3.23 (0.60) | 4.15 (0.55) | 0.92 | < .001* | 1.54 |
| 6. I am able to assist patients in solving problems they encounter in self‐management of their chronic illness. | 3.30 (0.70) | 3.91 (0.60) | 0.61 | < .001* | 0.87 | 3.75 (0.87) | 3.92 (0.49) | 0.17 | .50 | 0.20 |
| 7. I am confident in my ability to review patients' medications and side effects. | 3.00 (0.85) | 3.70 (0.76) | 0.70 | < .001* | 0.82 | 3.92 (0.76) | 4.46 (0.52) | 0.54 | .03* | 0.71 |
| 8. I am able to review the goals of a follow‐up visit with a patient. | 3.52 (0.95) | 4.43 (0.51) | 0.91 | < .001* | 0.96 | 3.08 (0.76) | 3.62 (0.77) | 0.54 | .05 | 0.71 |
| 9. I can identify factors that may facilitate or impede a patient's transition to an outpatient setting. | 3.48 (0.51) | 4.35 (0.49) | 0.87 | < .001* | 1.70 | 3.00 (0.82) | 3.85 (0.69) | 0.85 | .01* | 1.04 |
| 10. I can identify several topics for review at a follow‐up visit to confirm a safe transition to an outpatient setting. | 3.39 (0.94) | 4.52 (0.59) | 1.13 | < .001* | 1.20 | 3.23 (0.73) | 3.77 (0.73) | 0.54 | .11 | 0.74 |
Twenty‐two student partners of 1 or 2 medical students and 1 pharmacy student visited 22 patients (64% women; mean age 71 years). Most visits (91%) occurred at patients' homes.
Students were satisfied with the curriculum (Table 2). Both the medical and the pharmacy students perceived the 2 most valuable components to be the interdisciplinary collaboration on patient care and the postdischarge visit, followed by the debriefing session. The least useful were the initial workshop on interdisciplinary roles and the write‐up to the PCP. Ninety‐one percent of students agreed that they learned skills valuable for future patient care (medical students 4.4, SD 0.61; pharmacy students 4.1, SD 0.62; Table 3). Most students agreed that the program enhanced their learning about interdisciplinary care (4.3, SD 0.72), discharge planning (4.4, SD 0.70), and humanism (4.4, SD 0.63). Ninety‐three percent agreed that this curriculum was valuable to their education.
| Component | Mean score* (SD) | Rated very good or excellent (%) |
|---|---|---|
| ||
| Joint patient care with medical/pharmacy student | 4.5 (1.04) | 94% |
| Postdischarge visit | 4.3 (0.68) | 91% |
| Debriefing session | 3.9 (1.04) | 75% |
| Team presentation after patient visit | 3.7 (1.32) | 63% |
| Case‐based workshop | 3.6 (1.18) | 54% |
| Write‐up on experience | 3.4 (0.81) | 48% |
| Overall program | 4.1 (1.14) | 86% |
| Medical students (n = 35) | Pharmacy students (n = 18) | All students (n = 53) | ||||
|---|---|---|---|---|---|---|
| Mean score* (SD) | Agree/strongly agree (%) | Mean score (SD) | Agree/strongly agree (%) | Mean score (SD) | Agree/strongly agree (%) | |
| ||||||
| I have learned skills from this program that I plan to apply to future patient care experiences. | 4.4 (0.61) | 94% | 4.1 (0.62) | 84% | 4.3 (0.63) | 91% |
| This program added to my learning about an interdisciplinary approach to patient care beyond the other experiences of this clerkship. | 4.3 (0.74) | 91% | 4.2 (0.71) | 84% | 4.3 (0.72) | 89% |
| This program added to my learning about discharge planning and transitional care beyond the other experiences of this clerkship. | 4.4 (0.66) | 91% | 4.2 (0.79) | 89% | 4.4 (0.70) | 91% |
| This program added to my understanding of a patient as a whole person beyond the other experiences of this clerkship. | 4.3 (0.69) | 89% | 4.5 (0.51) | 100% | 4.4 (0.63) | 93% |
| This program was valuable to my medical education. | 4.3 (0.74) | 91% | 4.4 (0.60) | 95% | 4.4 (0.68) | 93% |
Open‐Ended Comments on Educational Value
Twenty‐nine medical students and 15 pharmacy students wrote responses to the open‐ended questions. Students identified the most valuable component of the curriculum as seeing patients at home in their social context (30 total comments). In the reflection write‐up, one student explained,
I was unaware of the types of living conditions many patients face, especially in the setting of chronic disease. In the future I will try to gain a more detailed understanding of my patients' social situations in order to help identify and anticipate problems in the management of their medical issues.
Thirteen students commented that working as an interdisciplinary team was a valuable experience. Eight students expressed appreciation at learning about transitional care and the components of discharge planning.
I was a little surprised during this home visit to find how much Ms. C had altered her medication regimen. She didn't like how she was feeling on the higher blood pressure medications, so she halved them. She doesn't really like taking pills, in general, so she stopped taking the aspirin, Senna, and Colace. I suppose something that might have made this discharge more successful would have been if we had really elicited her preferences regarding medications while she was in the hospital, such that we could have been more selective in what we prescribed and very clear with her with respect to what exactly we were hoping to accomplish with each.
During group debriefing, students reinforced the themes in their written comments and shared additional reflections. Students observed a shift in dynamics between patient and student provider; the patients appeared more comfortable in familiar settings. Students were also surprised that many of their patients did not have a clear understanding of medication regimens at home. In addition, they discussed the importance of communicating with patients' PCPs about the hospital course and follow‐up.
Also during the debriefing, students expressed the value of the postdischarge visit and interdisciplinary collaboration. Medical students appreciated seeing how the pharmacy students reviewed medications and taught patients how to use their medications. However, the students thought that preparation of paperwork prior to the visit and the write‐up seemed less valuable.
DISCUSSION
A discharge curriculum that included a postdischarge visit to a recently hospitalized patient improved the attitudes and self‐assessed skills of third‐year medical students and fourth‐year pharmacy students about interdisciplinary collaboration and transitions in care. It also deepened their appreciation of the impact of chronic illness on individual patients. To our knowledge, this is the first study to report an interdisciplinary curriculum with postdischarge home visits for students on their inpatient medicine clerkship.
Our curriculum was unique because its activities were linked to patients the students had cared for in the inpatient setting, a relationship that was key to students accepting the curriculum, as was the autonomy they had in selecting one of their patients for a visit. Although home visits are often part of medical school training, they generally occur in the preclinical years5, 19 or during third‐year primary care rotations, during which students are assigned patients at home or in outpatient facilities.17, 32 Home visits have been qualitatively reported to be a valuable aspect of geriatric, primary care, and other ambulatory‐based rotations of medical students.17, 19, 32 Postdischarge visits in graduate medical education have been shown to improve residents' awareness of and skills with transitions in care.28, 33, 34
Another novel aspect of this curriculum was the interdisciplinary collaboration in discharge planning and postdischarge visits. Although educators have implemented conferences on interdisciplinary education in preclinical medical education,3537 patient‐centered curricula in real‐time allow realistic interdisciplinary collaboration between medical and pharmacy students in their core clerkships. In our study, quantitative and qualitative data showed that the student partners valued each other's expertise in the context of a clinically relevant activitydischarge planning and a follow‐up home visit. Students reported confidence in their collaborative abilities after completing the curriculum, and comments supported a broadened understanding of other professionals' roles in patient care. Given that pharmacist involvement in discharge planning has been shown to improve patient outcomes,11, 24 our study supports the idea that medical educators should develop structured curricula on interdisciplinary training in core clerkships.
By evaluating the impact of hospitalization and chronic illness on their patients after discharge, our students developed an appreciation for safe transitions and opportunities to improve patients' health and level of function. We observed that students also appreciated the positive effect of the home environment on patient health and well‐being. From their postdischarge visit, students also became aware of the need for communication with primary care providers, particularly for patients with comorbidities. This type of transitional care experience may help to counter the negative attitudes toward chronic illness that students typically develop during clerkships.2, 9, 38, 39
Of note, although pharmacy students reported improvement in their attitudes and skills with transitional care, the trend toward significance was less than that for medical students. This difference was consistent with the broader rotation goals of each group. At the end of the curriculum, the pharmacy students expressed more comfort with medication review than did medical students, although the latter were better able to conduct transitional care including postdischarge visits and identification of barriers or facilitators to a safe discharge. Another interesting note is that pharmacy students came into the curriculum with a better understanding of the roles of physicians, whereas the medical students had a less clear idea of the pharmacist's role. A possible explanation is that pharmacy students are better trained in their preclinical years to work as a team with medical personnel. The pharmacy school curriculum places an emphasis on independent learning and interdisciplinary collaboration, which may lead to the greater comfort felt by the pharmacy students.
This study had several limitations. The absolute number of visits was small overall; however, nearly all student partners completed their visits. Although the response rate to the postcurriculum survey was high, the response rate to matched prepost surveys was lower. In addition, the survey questions were not validated. Further, although there was significant improvement in students' attitudes and self‐assessed skills after completion of the curriculum, we cannot be certain whether this improvement was a result of the curriculum or of other rotation experiences. We attempted to clarify this effect by asking if the curriculum added to their learning beyond other clerkship experiences, and students perceived that our curriculum was responsible for the positive effect. Also, the curriculum was used at 1 academic site and may not be generalizable to other hospitals, student populations, or team structures. The patients were selected by students, and thus the results may not be reproducible for every population; in some situations, students had to ask several patients until a patient consented to a postdischarge visit.
In implementing this interdisciplinary curriculum, we were challenged by the discordant schedules of the medical and pharmacy students. Initially, it was also difficult to overcome students' concerns about adding an additional expectation to an already busy rotation. The medical students, in particular, voiced concerns about having to leave the hospital during their inpatient rotation. However, this has become much less of an issue with time as the value of the postdischarge visit has become clear to students and team members, with the latter now aware of and supportive of the program.
This discharge curriculum represents a clinically relevant experience that addresses national educational mandates regarding interdisciplinary care and chronic illness across care settings. We are now expanding the curriculum from the original site to our other clerkship sites and are evaluating its impact on patient safety and clinical outcomes. Future research should focus on whether these interdisciplinary postdischarge patient visits lead to improved attitudes and skills during residency training or practice and whether, ultimately, they lead to improved patient outcomes.
Acknowledgements
The authors gratefully acknowledge Deborah Airo for editorial review and Kathleen Kerr for statistical support.
The increasing burden of chronic illness has prompted concerns about the traditional education model that focuses on management of acute disease.13 Chronic illness has replaced acute disease as the major cause of disability and total national health care expenditures.46 Medical educators have called for improved chronic disease curricula,2, 3 and the Institute of Medicine has asserted that health professions, including medicine and pharmacy, must reexamine how students are educated to manage patients with complex illnesses.7, 8 Despite the rising prevalence of chronic illness, the positive attitudes of medical students toward providing care to such patients decline during training.2, 9 One theory is that the current model of core clerkship training excessively exposes students to highly complex, seriously ill hospitalized patients. Students may become disillusioned and overwhelmed by these encounters, particularly without the opportunity to see improvement or thriving in the outpatient setting.2
There are few curricula on how to transition chronically ill patients from an inpatient to an outpatient setting and the inherent safety risks of this transition. For these patients, the posthospital discharge period is particularly confusing because of the sudden change in health status and new medication regimens.1012 It is very likely that communication among providers and patients will be insufficient during the discharge process,11, 1315 yet physicians tend to overestimate patients' understanding of postdischarge treatment plans and thereby underanticipate problems.16 One intervention to address these concerns is a postdischarge visit. Home visits have been shown to improve students' understanding of continuity of care and of the impact of chronic illness on their patients' medical and psychosocial situations.1719
There is scant structured teaching of third‐year medical students about another critical aspect of transitional care: the role of different health care disciplines. Although research about the impact of undergraduate interdisciplinary education on patient outcomes is limited, training students in interdisciplinary collaboration may improve their ability to provide quality care.2022 Multiple disciplines are critical for a smooth transition of chronically ill patients from an inpatient to an outpatient setting. In particular, pharmacist involvement in a predischarge medication review, patient counseling, and telephone follow‐up has been associated with improved outcomes.11, 12, 23, 24 Early introduction of interdisciplinary team training can improve student attitudes about working within a team.25
To teach the importance of safe discharges and interdisciplinary collaboration in caring for chronically ill patients, we developed an inpatient medicine clerkship curriculum for medical and pharmacy students that included postdischarge visits to students' own team patients. The purpose of the study was to assess the impact of this didactic and experiential curriculum on students' attitudes and self‐assessed skills in the interdisciplinary care and transitional care of chronically ill patients. We hypothesized that the discharge curriculum would improve student attitudes and self‐assessed skills in these domains. Finally, we hypothesized that visiting a patient's home would highlight for students the potential challenges of care transitions for patients.
METHODS
Participants and Setting
Participants were third‐year medical students on an 8‐week internal medicine (IM) clerkship and fourth‐year pharmacy students on a 6‐week pharmacy practice clerkship at a tertiary‐care university‐based hospital between April 2005 and April 2006. The hospital is 1 of 3 IM clerkship sites for medical students and 1 of 9 for pharmacy students. This site was selected because it included both medical and pharmacy students on most inpatient teams.
Clerkship students were assigned to all 7 medical teams, each consisting of an attending physician, a senior IM resident (postgraduate year 2 or 3), 2 IM interns (postgraduate year 1), 1 or 2 medical students, and up to 1 pharmacy student. Hospitalists covered 52% of inpatient months, with the remainder staffed by faculty primary care physicians, specialists, or chief residents. Although only three‐quarters of the medical teams were randomly assigned a pharmacy student at any given point, each team had a pharmacy student for a portion of time that overlapped with the rotation of the medical students. Over the year, 810 medical students rotated on the service during each of 6 blocks, and 46 pharmacy students and 1 pharmacy practice resident rotated during each of 8 blocks. The pharmacy students rotated on a different schedule than the medical students, and thus the curriculum was scheduled around the medical students' clerkship.
The Institutional Review Board of the University of California at San Francisco approved the study.
Intervention (Curriculum Description)
We developed a 3‐part pilot interdisciplinary curriculum (Fig. 1). During the first 2 weeks of the IM clerkship, interdisciplinary faculty, including 3 pharmacists, 2 hospitalists, and occasionally a social worker and geriatric clinical nurse specialist, led a 1‐hour interactive workshop on transitional care. The 3 workshop topics were: roles that various disciplines such as social work and pharmacy play in discharge care; the challenges a patient faces around the time of discharge, using a typical case; and discussion of elements of a postdischarge visit.
Medical and pharmacy students were partnered based on clerkship team assignments in teams of up to 3 student partners (1 or 2 medical students and 1 pharmacy student). Partners were advised to select a consenting patient known to them from the ward team for 1 postdischarge visit. Suggested selection criteria were at least 1 chronic illness, 1 prior hospitalization, and older than age 65 because patients fitting these criteria are most at risk for readmission or adverse outcomes following discharge.15, 26, 27 The student partners scheduled a postdischarge visit by the end of the rotation to the patient's home, nursing home, or subacute care facility. Each patient and the patient's primary care provider (PCP) gave informed consent.
During the postdischarge visit, student partners assessed medication discrepancies, environmental safety, and clinical status using structured data collection protocols developed by the investigators after review of the literature.28, 29 After the visit, students reported back to the ward teams on the patient's status and wrote a visit summary letter to the patient's PCP. The letter described the patient's clinical status and home environment, any medication discrepancies, and follow‐up plans and included a reflection piece. Reflection questions included, How did the visit change your perspective of patient discharge? What were the most critical aspects of this or any discharge? How do you think this experience will affect your future practice? What was the best thing about this experience?
During the last 2 weeks of the rotation, all student participants met with faculty preceptors for an hour‐long group debriefing session on the postdischarge visits.
Survey Instrument and Procedure
Students were asked to complete a presurvey at the beginning of the first workshop and a postsurvey at the end of the second (debriefing) workshop. The surveys contained self‐assessment questions on attitudes and skills in 3 domains: interdisciplinary care, chronic illness management, and transitional care. Questions were developed and tested with IM faculty with experience in student education and with ineligible students on previous rotations, and questions were revised for clarity and comprehensiveness. Students had the option to write a 4‐digit identifier on the pre‐ and postsurveys to allow matched analysis.
The 10‐item presurvey contained 4 items on interdisciplinary care and 3 each on chronic care and follow‐up visits. We reviewed surveys in the literature regarding home care and chronic illness to inform the development of our survey.30, 31 Students rated each item on a 5‐point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree). The 22‐item postsurvey included the same 10 items and additional Likert‐scaled questions on satisfaction with the curriculum. Two open‐ended questions solicited opinions about the value of the program and lessons learned for future patient encounters.
Statistical Analysis
We assessed the mean Likert score ( SD) for each presurvey and postsurvey question and compared means ( SD). We evaluated the differences between medical students and for pharmacy students in mean Likert score on the surveys using a dependent‐samples t test and set the level of significance at 0.05.
Change in scores between prepost survey variables were calculated overall and within student type (medicine vs. pharmacy). Because no intercorrelations and possible patterns indicating a structure were found, a factor analysis was not conducted.
Two investigators (C.L., H.N.) read all written responses to the open‐ended questions and independently generated a list of themes. The list was reconciled through discussion and was used to code all comments in order to determine the frequency of each theme. Discrepancies were discussed until consensus was reached.
RESULTS
Participants
Ninety‐seven percent of eligible students (37 of 39 medical students and 22 of 22 pharmacy students) completed the curriculum. Two medical students did not complete the home visit because their patients did not keep the appointment. The presurvey response was 100% for medical students and 91% for pharmacy students. The postsurvey response was 92% for medical students and 86% for pharmacy students; 58% of medical students and 59% of pharmacy students wrote in matching prepost survey identifiers for statistical analysis. Prepost survey responses showed an increase for both student groups in positive attitudes and self‐assessed skill in interdisciplinary collaboration, chronic illness management, and transitional care. Trends over time were highly significant for individual items on matched surveys (P < 0.05; Table 1a,b).
| Question | Medical students (matched respondents n = 23) | Pharmacy students (matched respondents n = 13) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Presurvey, mean (SD) | Postsurvey, mean (SD) | Mean difference | P value | Effect size | Presurvey, mean (SD) | Postsurvey, mean (SD) | Mean difference | P value | Effect size | |
| ||||||||||
| 1. I am able to state the various roles of the pharmacy students and/or pharmacists (or medical students and/or physicians) in taking care of hospitalized patients. | 2.83 (0.89) | 4.35 (0.57) | 1.52 | < .001* | 1.72 | 3.69 (0.63) | 4.15 (0.38) | 0.46 | .03* | 0.73 |
| 2. I am able to state the various roles of the case manager and/or social worker in taking care of hospitalized patients. | 2.83 (0.78) | 3.91 (0.42) | 1.09 | < .001* | 1.40 | 2.77 (0.83) | 3.54 (0.97) | 0.77 | .01* | 0.92 |
| 3. I am confident in my ability to work with a pharmacy student or pharmacist (or medical student and/or physician) in taking care of inpatients with chronic illness. | 3.22 (1.00) | 4.52 (0.51) | 1.30 | < .001* | 1.31 | 3.62 (0.87) | 4.23 (0.44) | 0.62 | .04* | 0.71 |
| 4. I am confident in my ability to work with a case manager and/or social worker in taking care of inpatients with chronic illness. | 2.96 (0.71) | 3.96 (0.56) | 1.00 | < .001* | 1.42 | 3.08 (0.95) | 3.38 (0.87) | 0.31 | .34 | 0.32 |
| 5. I am confident in my ability to involve patients in making a plan for their care. | 3.74 (0.62) | 4.26 (0.54) | 0.52 | < .001* | 0.84 | 3.23 (0.60) | 4.15 (0.55) | 0.92 | < .001* | 1.54 |
| 6. I am able to assist patients in solving problems they encounter in self‐management of their chronic illness. | 3.30 (0.70) | 3.91 (0.60) | 0.61 | < .001* | 0.87 | 3.75 (0.87) | 3.92 (0.49) | 0.17 | .50 | 0.20 |
| 7. I am confident in my ability to review patients' medications and side effects. | 3.00 (0.85) | 3.70 (0.76) | 0.70 | < .001* | 0.82 | 3.92 (0.76) | 4.46 (0.52) | 0.54 | .03* | 0.71 |
| 8. I am able to review the goals of a follow‐up visit with a patient. | 3.52 (0.95) | 4.43 (0.51) | 0.91 | < .001* | 0.96 | 3.08 (0.76) | 3.62 (0.77) | 0.54 | .05 | 0.71 |
| 9. I can identify factors that may facilitate or impede a patient's transition to an outpatient setting. | 3.48 (0.51) | 4.35 (0.49) | 0.87 | < .001* | 1.70 | 3.00 (0.82) | 3.85 (0.69) | 0.85 | .01* | 1.04 |
| 10. I can identify several topics for review at a follow‐up visit to confirm a safe transition to an outpatient setting. | 3.39 (0.94) | 4.52 (0.59) | 1.13 | < .001* | 1.20 | 3.23 (0.73) | 3.77 (0.73) | 0.54 | .11 | 0.74 |
Twenty‐two student partners of 1 or 2 medical students and 1 pharmacy student visited 22 patients (64% women; mean age 71 years). Most visits (91%) occurred at patients' homes.
Students were satisfied with the curriculum (Table 2). Both the medical and the pharmacy students perceived the 2 most valuable components to be the interdisciplinary collaboration on patient care and the postdischarge visit, followed by the debriefing session. The least useful were the initial workshop on interdisciplinary roles and the write‐up to the PCP. Ninety‐one percent of students agreed that they learned skills valuable for future patient care (medical students 4.4, SD 0.61; pharmacy students 4.1, SD 0.62; Table 3). Most students agreed that the program enhanced their learning about interdisciplinary care (4.3, SD 0.72), discharge planning (4.4, SD 0.70), and humanism (4.4, SD 0.63). Ninety‐three percent agreed that this curriculum was valuable to their education.
| Component | Mean score* (SD) | Rated very good or excellent (%) |
|---|---|---|
| ||
| Joint patient care with medical/pharmacy student | 4.5 (1.04) | 94% |
| Postdischarge visit | 4.3 (0.68) | 91% |
| Debriefing session | 3.9 (1.04) | 75% |
| Team presentation after patient visit | 3.7 (1.32) | 63% |
| Case‐based workshop | 3.6 (1.18) | 54% |
| Write‐up on experience | 3.4 (0.81) | 48% |
| Overall program | 4.1 (1.14) | 86% |
| Medical students (n = 35) | Pharmacy students (n = 18) | All students (n = 53) | ||||
|---|---|---|---|---|---|---|
| Mean score* (SD) | Agree/strongly agree (%) | Mean score (SD) | Agree/strongly agree (%) | Mean score (SD) | Agree/strongly agree (%) | |
| ||||||
| I have learned skills from this program that I plan to apply to future patient care experiences. | 4.4 (0.61) | 94% | 4.1 (0.62) | 84% | 4.3 (0.63) | 91% |
| This program added to my learning about an interdisciplinary approach to patient care beyond the other experiences of this clerkship. | 4.3 (0.74) | 91% | 4.2 (0.71) | 84% | 4.3 (0.72) | 89% |
| This program added to my learning about discharge planning and transitional care beyond the other experiences of this clerkship. | 4.4 (0.66) | 91% | 4.2 (0.79) | 89% | 4.4 (0.70) | 91% |
| This program added to my understanding of a patient as a whole person beyond the other experiences of this clerkship. | 4.3 (0.69) | 89% | 4.5 (0.51) | 100% | 4.4 (0.63) | 93% |
| This program was valuable to my medical education. | 4.3 (0.74) | 91% | 4.4 (0.60) | 95% | 4.4 (0.68) | 93% |
Open‐Ended Comments on Educational Value
Twenty‐nine medical students and 15 pharmacy students wrote responses to the open‐ended questions. Students identified the most valuable component of the curriculum as seeing patients at home in their social context (30 total comments). In the reflection write‐up, one student explained,
I was unaware of the types of living conditions many patients face, especially in the setting of chronic disease. In the future I will try to gain a more detailed understanding of my patients' social situations in order to help identify and anticipate problems in the management of their medical issues.
Thirteen students commented that working as an interdisciplinary team was a valuable experience. Eight students expressed appreciation at learning about transitional care and the components of discharge planning.
I was a little surprised during this home visit to find how much Ms. C had altered her medication regimen. She didn't like how she was feeling on the higher blood pressure medications, so she halved them. She doesn't really like taking pills, in general, so she stopped taking the aspirin, Senna, and Colace. I suppose something that might have made this discharge more successful would have been if we had really elicited her preferences regarding medications while she was in the hospital, such that we could have been more selective in what we prescribed and very clear with her with respect to what exactly we were hoping to accomplish with each.
During group debriefing, students reinforced the themes in their written comments and shared additional reflections. Students observed a shift in dynamics between patient and student provider; the patients appeared more comfortable in familiar settings. Students were also surprised that many of their patients did not have a clear understanding of medication regimens at home. In addition, they discussed the importance of communicating with patients' PCPs about the hospital course and follow‐up.
Also during the debriefing, students expressed the value of the postdischarge visit and interdisciplinary collaboration. Medical students appreciated seeing how the pharmacy students reviewed medications and taught patients how to use their medications. However, the students thought that preparation of paperwork prior to the visit and the write‐up seemed less valuable.
DISCUSSION
A discharge curriculum that included a postdischarge visit to a recently hospitalized patient improved the attitudes and self‐assessed skills of third‐year medical students and fourth‐year pharmacy students about interdisciplinary collaboration and transitions in care. It also deepened their appreciation of the impact of chronic illness on individual patients. To our knowledge, this is the first study to report an interdisciplinary curriculum with postdischarge home visits for students on their inpatient medicine clerkship.
Our curriculum was unique because its activities were linked to patients the students had cared for in the inpatient setting, a relationship that was key to students accepting the curriculum, as was the autonomy they had in selecting one of their patients for a visit. Although home visits are often part of medical school training, they generally occur in the preclinical years5, 19 or during third‐year primary care rotations, during which students are assigned patients at home or in outpatient facilities.17, 32 Home visits have been qualitatively reported to be a valuable aspect of geriatric, primary care, and other ambulatory‐based rotations of medical students.17, 19, 32 Postdischarge visits in graduate medical education have been shown to improve residents' awareness of and skills with transitions in care.28, 33, 34
Another novel aspect of this curriculum was the interdisciplinary collaboration in discharge planning and postdischarge visits. Although educators have implemented conferences on interdisciplinary education in preclinical medical education,3537 patient‐centered curricula in real‐time allow realistic interdisciplinary collaboration between medical and pharmacy students in their core clerkships. In our study, quantitative and qualitative data showed that the student partners valued each other's expertise in the context of a clinically relevant activitydischarge planning and a follow‐up home visit. Students reported confidence in their collaborative abilities after completing the curriculum, and comments supported a broadened understanding of other professionals' roles in patient care. Given that pharmacist involvement in discharge planning has been shown to improve patient outcomes,11, 24 our study supports the idea that medical educators should develop structured curricula on interdisciplinary training in core clerkships.
By evaluating the impact of hospitalization and chronic illness on their patients after discharge, our students developed an appreciation for safe transitions and opportunities to improve patients' health and level of function. We observed that students also appreciated the positive effect of the home environment on patient health and well‐being. From their postdischarge visit, students also became aware of the need for communication with primary care providers, particularly for patients with comorbidities. This type of transitional care experience may help to counter the negative attitudes toward chronic illness that students typically develop during clerkships.2, 9, 38, 39
Of note, although pharmacy students reported improvement in their attitudes and skills with transitional care, the trend toward significance was less than that for medical students. This difference was consistent with the broader rotation goals of each group. At the end of the curriculum, the pharmacy students expressed more comfort with medication review than did medical students, although the latter were better able to conduct transitional care including postdischarge visits and identification of barriers or facilitators to a safe discharge. Another interesting note is that pharmacy students came into the curriculum with a better understanding of the roles of physicians, whereas the medical students had a less clear idea of the pharmacist's role. A possible explanation is that pharmacy students are better trained in their preclinical years to work as a team with medical personnel. The pharmacy school curriculum places an emphasis on independent learning and interdisciplinary collaboration, which may lead to the greater comfort felt by the pharmacy students.
This study had several limitations. The absolute number of visits was small overall; however, nearly all student partners completed their visits. Although the response rate to the postcurriculum survey was high, the response rate to matched prepost surveys was lower. In addition, the survey questions were not validated. Further, although there was significant improvement in students' attitudes and self‐assessed skills after completion of the curriculum, we cannot be certain whether this improvement was a result of the curriculum or of other rotation experiences. We attempted to clarify this effect by asking if the curriculum added to their learning beyond other clerkship experiences, and students perceived that our curriculum was responsible for the positive effect. Also, the curriculum was used at 1 academic site and may not be generalizable to other hospitals, student populations, or team structures. The patients were selected by students, and thus the results may not be reproducible for every population; in some situations, students had to ask several patients until a patient consented to a postdischarge visit.
In implementing this interdisciplinary curriculum, we were challenged by the discordant schedules of the medical and pharmacy students. Initially, it was also difficult to overcome students' concerns about adding an additional expectation to an already busy rotation. The medical students, in particular, voiced concerns about having to leave the hospital during their inpatient rotation. However, this has become much less of an issue with time as the value of the postdischarge visit has become clear to students and team members, with the latter now aware of and supportive of the program.
This discharge curriculum represents a clinically relevant experience that addresses national educational mandates regarding interdisciplinary care and chronic illness across care settings. We are now expanding the curriculum from the original site to our other clerkship sites and are evaluating its impact on patient safety and clinical outcomes. Future research should focus on whether these interdisciplinary postdischarge patient visits lead to improved attitudes and skills during residency training or practice and whether, ultimately, they lead to improved patient outcomes.
Acknowledgements
The authors gratefully acknowledge Deborah Airo for editorial review and Kathleen Kerr for statistical support.
- ,,,,,.Medical students' experiences with and perceptions of chronic illness prior to medical school.Med Educ.1993;27:355–359.
- ,,,,,.Do clerkship experiences affect medical students' attitudes toward chronically ill patients?Acad Med.2001;76:815–820.
- ,,,,.More training needed in chronic care: a survey of US physicians.Acad Med.2004;79:541–548.
- .Chronic disease—the need for a new clinical education.JAMA.2004;292:1057–1059.
- ,,.Medical students as health coaches.Acad Med.2002;77:1164–1166.
- ,,.Persons with chronic conditions. Their prevalence and costs.JAMA.1996;276:1473–1479.
- ,,.To Err Is Human.Washington, DC:National Academy Press;2000.
- Institute of Medicine.Health Professions Education: A Bridge to Quality.Washington DC:National Academy Press;2000.
- ,.The loss of student idealism in the 3rd‐year clinical clerkships.Eval Health Prof.2001:24:61–71.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20:317–323.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- ,,,,.Does the addition of a pharmacist transition coordinator improve evidence‐based medication management and health outcomes in older adults moving from the hospital to a long‐term care facility? Results of a randomized, controlled trial.Am J Geriatr Pharmacother.2004;2:257–264.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,,.Posthospital medication discrepancies: Prevalence and contributing factors.Arch Intern Med.2005;165:1842–1847.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,, et al.Patient‐physician communication at hospital discharge and patients' understanding of the postdischarge treatment plan.Arch Intern Med.1997;157:1026–1030.
- ,,,,,.Reflections of medical students on visiting chronically ill older patients in the home.J Am Geriatr Soc.2006;54:1778–1783.
- ,,.Home care.JAMA.2003;290:1203–1207.
- ,,,,,.Mi casa o su casa? Assessing function and values in the home.J Am Geriatr Soc.2005;53:336–342.
- ,.Interdisciplinary education, and teamwork: a long and winding road.Med Educ.2001;35:867–875.
- ,,.Interdisciplinary education: evaluation of a palliative care training intervention for pre‐professionals.Acad Med.2004;79:769–776.
- ,.Effective interdisciplinary training: Lessons from the University of North Carolina's Student Health Action Coalition.Acad Med.2006;81:749–759.
- ,,,.The impact of follow‐up telephone calls to patients after hospitalization.Am J Med.2001;111(9B):26S–30S.
- ,,,.Clinical pharmacists and inpatient medical care: A systematic review.Arch Intern Med.2006;166:955–964.
- ,,,.Developing an evidence base for interdisciplinary learning: a systematic review.J Adv Nurs.2001;35:228–237.
- ,,,,,.Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan.Am J Med.1999;107:13–17.
- ,,.Risk factors for early unplanned hospital readmission in the elderly.J Gen Intern Med.1991;6:223–228.
- ,,, et al.Hospital to home: Improving internal medicine residents' understanding of the needs of older persons after a hospital stay.Acad Med.2003;78:793–797.
- . Care transitions program. University of Colorado at Denver, Health Sciences Center. Available at: http://www.caretransitions.org/index.asp. Accessed April 9,2007.
- ,,,,,.Validation of an instrument designed to assess medical student attitudes toward home care.J Am Geriatr Soc.2001;49:470–473.
- Patient Assessment of Chronic Illness Care (PACIC) from Improving Chronic Illness Care, a national program of the Robert Wood Johnson Foundation. Available at: http://improvingchroniccare.org/tools/pacic.htm. Accessed April 9,2007.
- ,,,,.The determinants of attitudinal change among medical students participating in home care training: A multi‐center study.Acad Med.2002;77:336–343.
- ,,,,.There's no place like home: Evaluating family medicine residents' training in home care.Home Health Care Serv Q.2002;21:1–17.
- ,,.Geriatric follow‐up by home visits after discharge from hospital: a randomized controlled trial.Age Ageing.1992;21:445–450.
- ,,.Multiprofessional learning: the attitudes of medical nursing, and pharmacy students to shared learning.Med Educ.2001;35:876–883.
- ,,.Can participation in a health affairs interdisciplinary case conference improve medical students' knowledge and attitudes?Acad Med.2006;81:257–261.
- ,,, et al.Bringing interdisciplinary and multicultural team building to health care education: the Downstate Team‐Building Initiative.Acad Med.2005;80:74–83.
- , and.“It's always continuing”: First year medical students' perspectives on chronic illness and the care of chronically ill patients.Acad Med.2005;80:183–188.
- ,,,,,.Training U.S. medical students to care for the chronically ill.Acad Med.2004;79:32–40.
- ,,,,,.Medical students' experiences with and perceptions of chronic illness prior to medical school.Med Educ.1993;27:355–359.
- ,,,,,.Do clerkship experiences affect medical students' attitudes toward chronically ill patients?Acad Med.2001;76:815–820.
- ,,,,.More training needed in chronic care: a survey of US physicians.Acad Med.2004;79:541–548.
- .Chronic disease—the need for a new clinical education.JAMA.2004;292:1057–1059.
- ,,.Medical students as health coaches.Acad Med.2002;77:1164–1166.
- ,,.Persons with chronic conditions. Their prevalence and costs.JAMA.1996;276:1473–1479.
- ,,.To Err Is Human.Washington, DC:National Academy Press;2000.
- Institute of Medicine.Health Professions Education: A Bridge to Quality.Washington DC:National Academy Press;2000.
- ,.The loss of student idealism in the 3rd‐year clinical clerkships.Eval Health Prof.2001:24:61–71.
- ,,,,.Adverse drug events occurring following hospital discharge.J Gen Intern Med.2005;20:317–323.
- ,,, et al.Role of pharmacist counseling in preventing adverse drug events after hospitalization.Arch Intern Med.2006;166:565–571.
- ,,,,.Does the addition of a pharmacist transition coordinator improve evidence‐based medication management and health outcomes in older adults moving from the hospital to a long‐term care facility? Results of a randomized, controlled trial.Am J Geriatr Pharmacother.2004;2:257–264.
- ,,,,.The incidence and severity of adverse events affecting patients after discharge from the hospital.Ann Intern Med.2003;138:161–167.
- ,,,.Posthospital medication discrepancies: Prevalence and contributing factors.Arch Intern Med.2005;165:1842–1847.
- ,,, et al.Adverse events among medical patients after discharge from hospital.CMAJ.2004;170:345–349.
- ,,, et al.Patient‐physician communication at hospital discharge and patients' understanding of the postdischarge treatment plan.Arch Intern Med.1997;157:1026–1030.
- ,,,,,.Reflections of medical students on visiting chronically ill older patients in the home.J Am Geriatr Soc.2006;54:1778–1783.
- ,,.Home care.JAMA.2003;290:1203–1207.
- ,,,,,.Mi casa o su casa? Assessing function and values in the home.J Am Geriatr Soc.2005;53:336–342.
- ,.Interdisciplinary education, and teamwork: a long and winding road.Med Educ.2001;35:867–875.
- ,,.Interdisciplinary education: evaluation of a palliative care training intervention for pre‐professionals.Acad Med.2004;79:769–776.
- ,.Effective interdisciplinary training: Lessons from the University of North Carolina's Student Health Action Coalition.Acad Med.2006;81:749–759.
- ,,,.The impact of follow‐up telephone calls to patients after hospitalization.Am J Med.2001;111(9B):26S–30S.
- ,,,.Clinical pharmacists and inpatient medical care: A systematic review.Arch Intern Med.2006;166:955–964.
- ,,,.Developing an evidence base for interdisciplinary learning: a systematic review.J Adv Nurs.2001;35:228–237.
- ,,,,,.Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan.Am J Med.1999;107:13–17.
- ,,.Risk factors for early unplanned hospital readmission in the elderly.J Gen Intern Med.1991;6:223–228.
- ,,, et al.Hospital to home: Improving internal medicine residents' understanding of the needs of older persons after a hospital stay.Acad Med.2003;78:793–797.
- . Care transitions program. University of Colorado at Denver, Health Sciences Center. Available at: http://www.caretransitions.org/index.asp. Accessed April 9,2007.
- ,,,,,.Validation of an instrument designed to assess medical student attitudes toward home care.J Am Geriatr Soc.2001;49:470–473.
- Patient Assessment of Chronic Illness Care (PACIC) from Improving Chronic Illness Care, a national program of the Robert Wood Johnson Foundation. Available at: http://improvingchroniccare.org/tools/pacic.htm. Accessed April 9,2007.
- ,,,,.The determinants of attitudinal change among medical students participating in home care training: A multi‐center study.Acad Med.2002;77:336–343.
- ,,,,.There's no place like home: Evaluating family medicine residents' training in home care.Home Health Care Serv Q.2002;21:1–17.
- ,,.Geriatric follow‐up by home visits after discharge from hospital: a randomized controlled trial.Age Ageing.1992;21:445–450.
- ,,.Multiprofessional learning: the attitudes of medical nursing, and pharmacy students to shared learning.Med Educ.2001;35:876–883.
- ,,.Can participation in a health affairs interdisciplinary case conference improve medical students' knowledge and attitudes?Acad Med.2006;81:257–261.
- ,,, et al.Bringing interdisciplinary and multicultural team building to health care education: the Downstate Team‐Building Initiative.Acad Med.2005;80:74–83.
- , and.“It's always continuing”: First year medical students' perspectives on chronic illness and the care of chronically ill patients.Acad Med.2005;80:183–188.
- ,,,,,.Training U.S. medical students to care for the chronically ill.Acad Med.2004;79:32–40.
Copyright © 2008 Society of Hospital Medicine