User login
Business and Practice Management Knowledge Deficiencies in Graduating Orthopedic Residents
With the increasing complexity of health care policy, significant changes in reimbursement and payer sources, and constant push to improve the cost-efficiency of care delivery, there has been a growing focus on the importance of business knowledge and practice management (PM) skills among physicians. Family medicine was the first specialty to require PM training during residency; other specialities have begun implementing business training into their residency curriculum.1 In 1999, the Accreditation Council for Graduate Medical Education (ACGME) identified 6 core competencies that should be included in resident training. One of these core competencies involves training in health care systems and PM.2,3
Residency program directors have also recognized the need for business training among residents. One study that surveyed general surgery program directors found that more than 87% agreed that residents should be trained in business and PM.4 Although these directors recognized the need for training, they also acknowledged the current deficiency: more than 70% thought their current trainees were inadequately trained in business and PM. Similarly, residents and physicians in multiple specialties have reported significant deficiencies in their training and knowledge of PM and business principles.5-11 For example, in a recent survey of ophthalmologists who had been in practice less than 5 years, 70% reported being not very well or not at all trained in overall PM skills during residency.5 Yet, most respondents thought training in this area was the responsibility of the training program.
The call for more business and PM training during residency has been tempered by increasing demands on medical and surgical skills training and time limitations such as duty-hour restrictions. These limitations reinforce the need to find efficient and effective means of teaching necessary business knowledge and PM skills. Paramount to doing this is recognizing the difference between general knowledge and functional knowledge—essentially, what is specifically needed to function effectively in practice.
We conducted a study not only to determine the general level of knowledge that physicians have in different business and PM topics when they complete their residency, but also to evaluate the level of knowledge that graduating physicians need in different business and PM topics in order to function effectively in a medical practice. Toward this end, we developed a novel model that could help determine the level of the functional knowledge deficiency (FKD) of particular business topics. We thought this model would allow us to quantify how much knowledge physicians needed to acquire in a given topic in order to function effectively in practice. We hypothesized that graduating residents would report overall low levels of business knowledge and high FKDs.
Materials and Methods
To minimize variability in the specific type and amount of business training received, we focused this study on a single institution that had maintained a uniform business management curriculum over an extended period. The business training program provided to residents in the orthopedic surgery residency at this institution included 6 hours of didactic lectures on various business topics annually. This program has been in place for more than 15 years and has not undergone any significant changes during that time.
Using the program’s alumni directory, we emailed a cover letter and an 11-question survey to all 332 residents and fellows who had completed their residency or fellowship training at our institution between 1970 and 2008. Anyone who did not reply to the email was mailed a copy of the cover letter and the survey.
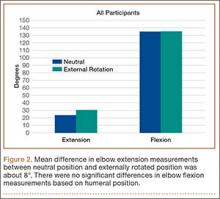
The first 4 survey questions involved the demographics of the surgeon and the surgeon’s practice. Subsequent questions focused on the surgeon’s understanding of 9 different general business and PM topics and their importance in the practice. The topics were marketing, business operations, human resources, contract negotiations, malpractice issues, coding/billing, medical records management, accounting, and economic analytical tools. The surgeon was asked to use a 10-point scale ranging from 1 (“knew nothing at all”) to 10 (“complete understanding”) to rate his or her understanding of each topic at the completion of residency. The surgeon was also asked to rate how important it was to understand that topic in the surgeon’s current practice. Again, a 10-point scale was used: 1 (“not important at all”) to 10 (“absolutely vital”) (Figure).
When the surveys were returned, their data were compiled and analyzed to determine the overall knowledge levels for each topic and the levels based on years in practice, type of practice, and level of involvement in PM. We also wanted to determine the amount of business knowledge that they needed in order to function effectively in practice (and that they lacked at time of graduation). We defined this as the FKD at graduation and calculated it as the difference between the surgeon’s reported importance of a topic in his or her current practice and his or her level of understanding of that topic at graduation. A larger FKD score represented greater deficiency, with a maximal possible FKD score of 9. A score of 0 would reflect an appropriate amount of knowledge to function effectively, and a negative score would reflect a knowledge surplus. Using the demographic information from the survey, we were then able to further analyze the levels of overall knowledge as well as the FKD for each topic with respect to length of time in practice, type of practice, and the surgeon’s involvement in PM.
We evaluated the reported levels of knowledge based on both type of practice (academic, hospital-employed, private practice) and who managed the practice (physician, nonphysician). Academic practices were defined as those associated with an academic medical center; hospital-employed practices were those in which the physician was an employee of a health system not associated with an academic medical center; and private practices were defined as physician-owned orthopedic practices not associated with an academic medical center. Regarding management, practices in which physicians were primarily responsible for the daily operations of the practice were considered physician-managed; conversely, practices in which operations were controlled by either employed or institutionally assigned administration were defined as nonphysician-managed.
Statistical analysis of the results for different practice types and levels of involvement in management was performed for both general knowledge and FKD. Means, medians, and standard deviations were calculated. One-way analysis of variance or t tests were then used to examine mean differences overall and within each business topic. When a difference was found, a post hoc Tukey multiple range test was performed to identify it. Differences at P < .05 were considered significant.
Results
One hundred eighty-two surgeons answered the survey, yielding a response rate of 55%. All had completed their training at our institution. Seven respondents were removed from the study because they had retired from practice (5) or had returned incomplete surveys (2).
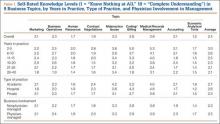
The overall self-rated level of business knowledge of all responding surgeons at the conclusion of their training was 2.4 on the 10-point scale (Table 1). Specifically, physicians reported the lowest levels of business understanding in economic analytical tools (1.5), human resources (1.7), and contract negotiations (1.9), suggesting minimal knowledge of these topics generally. They reported the highest levels of knowledge in medical records management (3.8) and malpractice issues (3.3). Even these topics, however, still reflected overall low levels of knowledge.
There was no statistically significant difference between private practice and academic physicians. In addition, surgeons in physician-managed practices reported significantly (P = .045) higher levels of understanding of economic analytical tools than surgeons in nonphysician-managed practices (Table 1). There were no other statistically significant differences among groups.
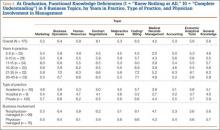
The overall calculated FKD for all surgeons was 5.6. FKDs were calculated for all 9 business topics. The worst FKDs were in business operations (6.4) and coding/billing (6.3). The topic with the least deficiency (lowest FKD) was in medical records management (4.2) (Table 2).
Surgeons’ FKDs based on practice type (academic, hospital-employed, private practice) were compared to identify potentially significant differences. Hospital-employed physicians had the lowest overall FKD (4.0), followed by physicians in academic practices (5.1) and private practices (5.9). Hospital-employed physicians reported statistically significantly better (lower) FKDs in comparison with physicians in private practice in multiple topics, including human resources, contract negotiations, malpractice issues, coding/billing, and accounting (Table 2). Similarly, physicians in academic practices also had statistically significantly better FKDs than physicians in private practice in the topics of business operations, contract negotiations, and billing/coding. Compared with hospital-employed physicians, physicians in academic practices had significantly more knowledge about marketing, business operations, and accounting. Physicians in private practice did not have significantly better FKDs in any topic in comparison with hospital-employed or academic physicians. There was no significant difference in FKDs for medical records management or economic analytical tools based on practice type.
Comparisons based on PM involvement showed that physicians in practices with nonphysician management had only a slightly better FKD (5.6) at graduation than those in practices with physician involvement (5.7). None of the 9 topics was statistically significant different based on physician involvement in PM.
Discussion
Building a successful medical practice has become more difficult for graduating orthopedic surgery residents because of an increasingly complex health care system, shrinking reimbursement rates, and looming regulatory changes. These challenges have reinforced the importance of teaching residents the necessary PM knowledge and skills to function effectively in a medical practice. Multiple studies from different specialties surveying or testing graduating residents and young practicing physicians on their business management knowledge or specific business topics have shown severe deficiencies.5-11 Unfortunately, graduating orthopedic surgery residents also appear inadequately prepared in PM. In a study of resident coding/billing knowledge, Gill and Schutt6 surveyed 2006 graduating orthopedic residents and found that only 13% felt confident in their coding ability. Our study results add to our understanding of multiple PM topics and demonstrate graduating orthopedic residents’ deficiencies throughout these topics.
Increased efforts to develop business management training programs and curricula have helped improve both overall PM and business knowledge in other specialties.12-15 ACGME now requires 100 hours of PM training among family medicine residency programs.16 A curriculum instituted in a general surgery residency focused on improving coding found that accuracy improved from 36% to 88% over 12 months.13 A family practice residency instituted a “simulated practice” model for its residents to improve practical PM learning and found statistically significant improvement over their prior didactic lectures.15 However, there continues to be significant variability in the topics and methods covered in business management curricula as programs struggle to determine how to most effectively use their limited time to prepare graduating residents.
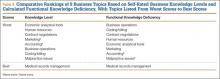
In this study, we introduced the concept of FKD. With limited time available for teaching business knowledge and PM skills in residency, it has become imperative that training be efficient and effective. The FKD model can improve training efficiency by directing training to the topics that will produce the highest yield in preparing physicians for practice. As our results demonstrate, topics with the lowest levels of knowledge among surgeons often are not the same as the topics that are most needed to function effectively in practice (Table 3). The FKD model identifies deficiencies in practical, applicable knowledge rather than focusing on a general knowledge level. We suspect that focusing on topics with a high FKD would provide a higher yield in preparing physicians for practice. As such, our results suggest that training in business operations and coding/billing would likely provide the highest practical value, despite the fact that these were not the areas of least general knowledge.
Another finding of this study was the FKD difference based on type of practice. Compared with private practice physicians, hospital-employed or academic physicians had substantially lower overall FKDs and significantly lower FKDs in several specific topics. However, these FKD differences exist despite minimal differences in overall levels of knowledge. This would suggest that less business knowledge was needed by physicians to enter these types of practices compared with traditional private practice. We speculate that this may be one factor influencing the recent trend by graduating orthopedic residents to take hospital-employed positions, as these positions may appear less demanding in terms of learning the management aspects of the new practice.
Our results also showed slightly higher reported average business knowledge and lower FKD reported by those who had recently completed training (within 2-5 years) versus those in practice much longer. This is particularly interesting, as our institution has maintained the same lecture-based program for many years without significant changes. Although these differences may not be statistically significant, they may reflect an increased interest in and attention to learning PM skills while in training. However, we acknowledge this is only one of many possible explanations for these findings.
This study had several limitations. First, all respondents were graduates of a single institution. We were trying to limit the variability in business training, but this also limits the scope of the results. Second, self-ratings on surveys provide subjective measures of business knowledge and functional knowledge. Scores may vary based on individuals’ understanding of given topics, or they may inaccurately represent their level of understanding. This is especially true of respondents who graduated from residency, for example, 20 years earlier—their survey responses may reflect erroneous recollection of business training at time of graduation compared with respondents who graduated more recently. Conversely, more recent graduates may not have a fully formed or accurate picture of how much business knowledge is required to function in practice. Nevertheless, we found no significant differences in measured parameters based on graduation date, so we chose not to exclude older respondents, which also may have weakened our data pool. Further, FKDs are relative values used to compare subjective deficiencies rather than absolute scores of specific general knowledge. As such, subjectivity, including recollection of business training, is inherent in the model used in this study.
Conclusion
Graduating orthopedic surgeons currently appear inadequately prepared to effectively manage business issues in their practices, as evidenced by their low overall knowledge levels and high FKDs. The novel FKD model described in this study helps define FKD levels and identify topics that may provide the highest yield in improving effectiveness in practice. Residency curricula focused on improving business and PM knowledge, particularly in the topics with the highest FKDs (eg, business operations, coding/billing), may improve training efficiency in these areas. Further studies with larger numbers of physicians across multiple institutions are needed to confirm these findings and to validate the FKD concept.
1. Rose EA, Neale AV, Rathur WA. Teaching practice management during residency. Fam Med. 1999;31(2):107-113.
2. Accreditation Council for Graduate Medical Education. ACGME common program requirements. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/CPRs2013.pdf. Updated June 9, 2013. Accessed August 25, 2015.
3. Itani K. A positive approach to core competencies and benchmarks for graduate medical education. Am J Surg. 2002;184(3):196-203.
4. Lusco VC, Martinez SA, Polk HC Jr. Program directors in surgery agree that residents should be formally trained in business and practice management. Am J Surg. 2005;189(1):11-13.
5. McDonnell PJ, Kirwan TJ, Brinton GS, et al. Perceptions of recent ophthalmology residency graduates regarding preparation for practice. Ophthalmology. 2007;114(2):387-391.
6. Gill JB, Schutt RC Jr. Practice management education in orthopaedic surgical residencies. J Bone Joint Surg Am. 2007;89(1):216-219.
7. Satiani B. Business knowledge in surgeons. Am J Surg. 2004;188(1):13-16.
8. Cantor JC, Baker LC, Hughes RG. Preparedness for practice. Young physicians’ views of their professional education. JAMA. 1993;270(9):1035-1040.
9. Fakhry SM, Robinson L, Hendershot K, Reines HD. Surgical residents’ knowledge of documentation and coding for professional services: an opportunity for a focused educational offering. Am J Surg. 2007;194(2):263-267.
10. Williford LE, Ling FW, Summitt RL Jr, Stovall TG. Practice management in obstetrics and gynecology residency curriculum. Obstet Gynecol. 1999;94(3):476-479.
11. Andreae MC, Dunham K, Freed GL. Inadequate training in billing and coding as perceived by recent pediatric graduates. Clin Pediatr. 2009;48(9):939-944.
12. Kolva DE, Barzee KA, Morley CP. Practice management residency curricula: a systematic literature review. Fam Med. 2009;41(6):411-419.
13. Jones K, Lebron RA, Mangram A, Dunn E. Practice management education during surgical residency. Am J Surg. 2008;196(6):878-881.
14. Kerfoot BP, Conlin PR, Travison T, McMahon GT. Web-based education in systems-based practice: a randomized trial. Arch Intern Med. 2007;167(4):361-366.
15. LoPresti L, Ginn P, Treat R. Using a simulated practice to improve practice management learning. Fam Med. 2009;41(9):640-645.
16. Accreditation Council for Graduate Medical Education. Family medicine program requirements. https://www.acgme.org/acgmeweb/tabid/132/ProgramandInstitutionalAccreditation/MedicalSpecialties/FamilyMedicine.aspx. Accessed September 23, 2015.
With the increasing complexity of health care policy, significant changes in reimbursement and payer sources, and constant push to improve the cost-efficiency of care delivery, there has been a growing focus on the importance of business knowledge and practice management (PM) skills among physicians. Family medicine was the first specialty to require PM training during residency; other specialities have begun implementing business training into their residency curriculum.1 In 1999, the Accreditation Council for Graduate Medical Education (ACGME) identified 6 core competencies that should be included in resident training. One of these core competencies involves training in health care systems and PM.2,3
Residency program directors have also recognized the need for business training among residents. One study that surveyed general surgery program directors found that more than 87% agreed that residents should be trained in business and PM.4 Although these directors recognized the need for training, they also acknowledged the current deficiency: more than 70% thought their current trainees were inadequately trained in business and PM. Similarly, residents and physicians in multiple specialties have reported significant deficiencies in their training and knowledge of PM and business principles.5-11 For example, in a recent survey of ophthalmologists who had been in practice less than 5 years, 70% reported being not very well or not at all trained in overall PM skills during residency.5 Yet, most respondents thought training in this area was the responsibility of the training program.
The call for more business and PM training during residency has been tempered by increasing demands on medical and surgical skills training and time limitations such as duty-hour restrictions. These limitations reinforce the need to find efficient and effective means of teaching necessary business knowledge and PM skills. Paramount to doing this is recognizing the difference between general knowledge and functional knowledge—essentially, what is specifically needed to function effectively in practice.
We conducted a study not only to determine the general level of knowledge that physicians have in different business and PM topics when they complete their residency, but also to evaluate the level of knowledge that graduating physicians need in different business and PM topics in order to function effectively in a medical practice. Toward this end, we developed a novel model that could help determine the level of the functional knowledge deficiency (FKD) of particular business topics. We thought this model would allow us to quantify how much knowledge physicians needed to acquire in a given topic in order to function effectively in practice. We hypothesized that graduating residents would report overall low levels of business knowledge and high FKDs.
Materials and Methods
To minimize variability in the specific type and amount of business training received, we focused this study on a single institution that had maintained a uniform business management curriculum over an extended period. The business training program provided to residents in the orthopedic surgery residency at this institution included 6 hours of didactic lectures on various business topics annually. This program has been in place for more than 15 years and has not undergone any significant changes during that time.
Using the program’s alumni directory, we emailed a cover letter and an 11-question survey to all 332 residents and fellows who had completed their residency or fellowship training at our institution between 1970 and 2008. Anyone who did not reply to the email was mailed a copy of the cover letter and the survey.
The first 4 survey questions involved the demographics of the surgeon and the surgeon’s practice. Subsequent questions focused on the surgeon’s understanding of 9 different general business and PM topics and their importance in the practice. The topics were marketing, business operations, human resources, contract negotiations, malpractice issues, coding/billing, medical records management, accounting, and economic analytical tools. The surgeon was asked to use a 10-point scale ranging from 1 (“knew nothing at all”) to 10 (“complete understanding”) to rate his or her understanding of each topic at the completion of residency. The surgeon was also asked to rate how important it was to understand that topic in the surgeon’s current practice. Again, a 10-point scale was used: 1 (“not important at all”) to 10 (“absolutely vital”) (Figure).
When the surveys were returned, their data were compiled and analyzed to determine the overall knowledge levels for each topic and the levels based on years in practice, type of practice, and level of involvement in PM. We also wanted to determine the amount of business knowledge that they needed in order to function effectively in practice (and that they lacked at time of graduation). We defined this as the FKD at graduation and calculated it as the difference between the surgeon’s reported importance of a topic in his or her current practice and his or her level of understanding of that topic at graduation. A larger FKD score represented greater deficiency, with a maximal possible FKD score of 9. A score of 0 would reflect an appropriate amount of knowledge to function effectively, and a negative score would reflect a knowledge surplus. Using the demographic information from the survey, we were then able to further analyze the levels of overall knowledge as well as the FKD for each topic with respect to length of time in practice, type of practice, and the surgeon’s involvement in PM.
We evaluated the reported levels of knowledge based on both type of practice (academic, hospital-employed, private practice) and who managed the practice (physician, nonphysician). Academic practices were defined as those associated with an academic medical center; hospital-employed practices were those in which the physician was an employee of a health system not associated with an academic medical center; and private practices were defined as physician-owned orthopedic practices not associated with an academic medical center. Regarding management, practices in which physicians were primarily responsible for the daily operations of the practice were considered physician-managed; conversely, practices in which operations were controlled by either employed or institutionally assigned administration were defined as nonphysician-managed.
Statistical analysis of the results for different practice types and levels of involvement in management was performed for both general knowledge and FKD. Means, medians, and standard deviations were calculated. One-way analysis of variance or t tests were then used to examine mean differences overall and within each business topic. When a difference was found, a post hoc Tukey multiple range test was performed to identify it. Differences at P < .05 were considered significant.
Results
One hundred eighty-two surgeons answered the survey, yielding a response rate of 55%. All had completed their training at our institution. Seven respondents were removed from the study because they had retired from practice (5) or had returned incomplete surveys (2).
The overall self-rated level of business knowledge of all responding surgeons at the conclusion of their training was 2.4 on the 10-point scale (Table 1). Specifically, physicians reported the lowest levels of business understanding in economic analytical tools (1.5), human resources (1.7), and contract negotiations (1.9), suggesting minimal knowledge of these topics generally. They reported the highest levels of knowledge in medical records management (3.8) and malpractice issues (3.3). Even these topics, however, still reflected overall low levels of knowledge.
There was no statistically significant difference between private practice and academic physicians. In addition, surgeons in physician-managed practices reported significantly (P = .045) higher levels of understanding of economic analytical tools than surgeons in nonphysician-managed practices (Table 1). There were no other statistically significant differences among groups.
The overall calculated FKD for all surgeons was 5.6. FKDs were calculated for all 9 business topics. The worst FKDs were in business operations (6.4) and coding/billing (6.3). The topic with the least deficiency (lowest FKD) was in medical records management (4.2) (Table 2).
Surgeons’ FKDs based on practice type (academic, hospital-employed, private practice) were compared to identify potentially significant differences. Hospital-employed physicians had the lowest overall FKD (4.0), followed by physicians in academic practices (5.1) and private practices (5.9). Hospital-employed physicians reported statistically significantly better (lower) FKDs in comparison with physicians in private practice in multiple topics, including human resources, contract negotiations, malpractice issues, coding/billing, and accounting (Table 2). Similarly, physicians in academic practices also had statistically significantly better FKDs than physicians in private practice in the topics of business operations, contract negotiations, and billing/coding. Compared with hospital-employed physicians, physicians in academic practices had significantly more knowledge about marketing, business operations, and accounting. Physicians in private practice did not have significantly better FKDs in any topic in comparison with hospital-employed or academic physicians. There was no significant difference in FKDs for medical records management or economic analytical tools based on practice type.
Comparisons based on PM involvement showed that physicians in practices with nonphysician management had only a slightly better FKD (5.6) at graduation than those in practices with physician involvement (5.7). None of the 9 topics was statistically significant different based on physician involvement in PM.
Discussion
Building a successful medical practice has become more difficult for graduating orthopedic surgery residents because of an increasingly complex health care system, shrinking reimbursement rates, and looming regulatory changes. These challenges have reinforced the importance of teaching residents the necessary PM knowledge and skills to function effectively in a medical practice. Multiple studies from different specialties surveying or testing graduating residents and young practicing physicians on their business management knowledge or specific business topics have shown severe deficiencies.5-11 Unfortunately, graduating orthopedic surgery residents also appear inadequately prepared in PM. In a study of resident coding/billing knowledge, Gill and Schutt6 surveyed 2006 graduating orthopedic residents and found that only 13% felt confident in their coding ability. Our study results add to our understanding of multiple PM topics and demonstrate graduating orthopedic residents’ deficiencies throughout these topics.
Increased efforts to develop business management training programs and curricula have helped improve both overall PM and business knowledge in other specialties.12-15 ACGME now requires 100 hours of PM training among family medicine residency programs.16 A curriculum instituted in a general surgery residency focused on improving coding found that accuracy improved from 36% to 88% over 12 months.13 A family practice residency instituted a “simulated practice” model for its residents to improve practical PM learning and found statistically significant improvement over their prior didactic lectures.15 However, there continues to be significant variability in the topics and methods covered in business management curricula as programs struggle to determine how to most effectively use their limited time to prepare graduating residents.
In this study, we introduced the concept of FKD. With limited time available for teaching business knowledge and PM skills in residency, it has become imperative that training be efficient and effective. The FKD model can improve training efficiency by directing training to the topics that will produce the highest yield in preparing physicians for practice. As our results demonstrate, topics with the lowest levels of knowledge among surgeons often are not the same as the topics that are most needed to function effectively in practice (Table 3). The FKD model identifies deficiencies in practical, applicable knowledge rather than focusing on a general knowledge level. We suspect that focusing on topics with a high FKD would provide a higher yield in preparing physicians for practice. As such, our results suggest that training in business operations and coding/billing would likely provide the highest practical value, despite the fact that these were not the areas of least general knowledge.
Another finding of this study was the FKD difference based on type of practice. Compared with private practice physicians, hospital-employed or academic physicians had substantially lower overall FKDs and significantly lower FKDs in several specific topics. However, these FKD differences exist despite minimal differences in overall levels of knowledge. This would suggest that less business knowledge was needed by physicians to enter these types of practices compared with traditional private practice. We speculate that this may be one factor influencing the recent trend by graduating orthopedic residents to take hospital-employed positions, as these positions may appear less demanding in terms of learning the management aspects of the new practice.
Our results also showed slightly higher reported average business knowledge and lower FKD reported by those who had recently completed training (within 2-5 years) versus those in practice much longer. This is particularly interesting, as our institution has maintained the same lecture-based program for many years without significant changes. Although these differences may not be statistically significant, they may reflect an increased interest in and attention to learning PM skills while in training. However, we acknowledge this is only one of many possible explanations for these findings.
This study had several limitations. First, all respondents were graduates of a single institution. We were trying to limit the variability in business training, but this also limits the scope of the results. Second, self-ratings on surveys provide subjective measures of business knowledge and functional knowledge. Scores may vary based on individuals’ understanding of given topics, or they may inaccurately represent their level of understanding. This is especially true of respondents who graduated from residency, for example, 20 years earlier—their survey responses may reflect erroneous recollection of business training at time of graduation compared with respondents who graduated more recently. Conversely, more recent graduates may not have a fully formed or accurate picture of how much business knowledge is required to function in practice. Nevertheless, we found no significant differences in measured parameters based on graduation date, so we chose not to exclude older respondents, which also may have weakened our data pool. Further, FKDs are relative values used to compare subjective deficiencies rather than absolute scores of specific general knowledge. As such, subjectivity, including recollection of business training, is inherent in the model used in this study.
Conclusion
Graduating orthopedic surgeons currently appear inadequately prepared to effectively manage business issues in their practices, as evidenced by their low overall knowledge levels and high FKDs. The novel FKD model described in this study helps define FKD levels and identify topics that may provide the highest yield in improving effectiveness in practice. Residency curricula focused on improving business and PM knowledge, particularly in the topics with the highest FKDs (eg, business operations, coding/billing), may improve training efficiency in these areas. Further studies with larger numbers of physicians across multiple institutions are needed to confirm these findings and to validate the FKD concept.
With the increasing complexity of health care policy, significant changes in reimbursement and payer sources, and constant push to improve the cost-efficiency of care delivery, there has been a growing focus on the importance of business knowledge and practice management (PM) skills among physicians. Family medicine was the first specialty to require PM training during residency; other specialities have begun implementing business training into their residency curriculum.1 In 1999, the Accreditation Council for Graduate Medical Education (ACGME) identified 6 core competencies that should be included in resident training. One of these core competencies involves training in health care systems and PM.2,3
Residency program directors have also recognized the need for business training among residents. One study that surveyed general surgery program directors found that more than 87% agreed that residents should be trained in business and PM.4 Although these directors recognized the need for training, they also acknowledged the current deficiency: more than 70% thought their current trainees were inadequately trained in business and PM. Similarly, residents and physicians in multiple specialties have reported significant deficiencies in their training and knowledge of PM and business principles.5-11 For example, in a recent survey of ophthalmologists who had been in practice less than 5 years, 70% reported being not very well or not at all trained in overall PM skills during residency.5 Yet, most respondents thought training in this area was the responsibility of the training program.
The call for more business and PM training during residency has been tempered by increasing demands on medical and surgical skills training and time limitations such as duty-hour restrictions. These limitations reinforce the need to find efficient and effective means of teaching necessary business knowledge and PM skills. Paramount to doing this is recognizing the difference between general knowledge and functional knowledge—essentially, what is specifically needed to function effectively in practice.
We conducted a study not only to determine the general level of knowledge that physicians have in different business and PM topics when they complete their residency, but also to evaluate the level of knowledge that graduating physicians need in different business and PM topics in order to function effectively in a medical practice. Toward this end, we developed a novel model that could help determine the level of the functional knowledge deficiency (FKD) of particular business topics. We thought this model would allow us to quantify how much knowledge physicians needed to acquire in a given topic in order to function effectively in practice. We hypothesized that graduating residents would report overall low levels of business knowledge and high FKDs.
Materials and Methods
To minimize variability in the specific type and amount of business training received, we focused this study on a single institution that had maintained a uniform business management curriculum over an extended period. The business training program provided to residents in the orthopedic surgery residency at this institution included 6 hours of didactic lectures on various business topics annually. This program has been in place for more than 15 years and has not undergone any significant changes during that time.
Using the program’s alumni directory, we emailed a cover letter and an 11-question survey to all 332 residents and fellows who had completed their residency or fellowship training at our institution between 1970 and 2008. Anyone who did not reply to the email was mailed a copy of the cover letter and the survey.
The first 4 survey questions involved the demographics of the surgeon and the surgeon’s practice. Subsequent questions focused on the surgeon’s understanding of 9 different general business and PM topics and their importance in the practice. The topics were marketing, business operations, human resources, contract negotiations, malpractice issues, coding/billing, medical records management, accounting, and economic analytical tools. The surgeon was asked to use a 10-point scale ranging from 1 (“knew nothing at all”) to 10 (“complete understanding”) to rate his or her understanding of each topic at the completion of residency. The surgeon was also asked to rate how important it was to understand that topic in the surgeon’s current practice. Again, a 10-point scale was used: 1 (“not important at all”) to 10 (“absolutely vital”) (Figure).
When the surveys were returned, their data were compiled and analyzed to determine the overall knowledge levels for each topic and the levels based on years in practice, type of practice, and level of involvement in PM. We also wanted to determine the amount of business knowledge that they needed in order to function effectively in practice (and that they lacked at time of graduation). We defined this as the FKD at graduation and calculated it as the difference between the surgeon’s reported importance of a topic in his or her current practice and his or her level of understanding of that topic at graduation. A larger FKD score represented greater deficiency, with a maximal possible FKD score of 9. A score of 0 would reflect an appropriate amount of knowledge to function effectively, and a negative score would reflect a knowledge surplus. Using the demographic information from the survey, we were then able to further analyze the levels of overall knowledge as well as the FKD for each topic with respect to length of time in practice, type of practice, and the surgeon’s involvement in PM.
We evaluated the reported levels of knowledge based on both type of practice (academic, hospital-employed, private practice) and who managed the practice (physician, nonphysician). Academic practices were defined as those associated with an academic medical center; hospital-employed practices were those in which the physician was an employee of a health system not associated with an academic medical center; and private practices were defined as physician-owned orthopedic practices not associated with an academic medical center. Regarding management, practices in which physicians were primarily responsible for the daily operations of the practice were considered physician-managed; conversely, practices in which operations were controlled by either employed or institutionally assigned administration were defined as nonphysician-managed.
Statistical analysis of the results for different practice types and levels of involvement in management was performed for both general knowledge and FKD. Means, medians, and standard deviations were calculated. One-way analysis of variance or t tests were then used to examine mean differences overall and within each business topic. When a difference was found, a post hoc Tukey multiple range test was performed to identify it. Differences at P < .05 were considered significant.
Results
One hundred eighty-two surgeons answered the survey, yielding a response rate of 55%. All had completed their training at our institution. Seven respondents were removed from the study because they had retired from practice (5) or had returned incomplete surveys (2).
The overall self-rated level of business knowledge of all responding surgeons at the conclusion of their training was 2.4 on the 10-point scale (Table 1). Specifically, physicians reported the lowest levels of business understanding in economic analytical tools (1.5), human resources (1.7), and contract negotiations (1.9), suggesting minimal knowledge of these topics generally. They reported the highest levels of knowledge in medical records management (3.8) and malpractice issues (3.3). Even these topics, however, still reflected overall low levels of knowledge.
There was no statistically significant difference between private practice and academic physicians. In addition, surgeons in physician-managed practices reported significantly (P = .045) higher levels of understanding of economic analytical tools than surgeons in nonphysician-managed practices (Table 1). There were no other statistically significant differences among groups.
The overall calculated FKD for all surgeons was 5.6. FKDs were calculated for all 9 business topics. The worst FKDs were in business operations (6.4) and coding/billing (6.3). The topic with the least deficiency (lowest FKD) was in medical records management (4.2) (Table 2).
Surgeons’ FKDs based on practice type (academic, hospital-employed, private practice) were compared to identify potentially significant differences. Hospital-employed physicians had the lowest overall FKD (4.0), followed by physicians in academic practices (5.1) and private practices (5.9). Hospital-employed physicians reported statistically significantly better (lower) FKDs in comparison with physicians in private practice in multiple topics, including human resources, contract negotiations, malpractice issues, coding/billing, and accounting (Table 2). Similarly, physicians in academic practices also had statistically significantly better FKDs than physicians in private practice in the topics of business operations, contract negotiations, and billing/coding. Compared with hospital-employed physicians, physicians in academic practices had significantly more knowledge about marketing, business operations, and accounting. Physicians in private practice did not have significantly better FKDs in any topic in comparison with hospital-employed or academic physicians. There was no significant difference in FKDs for medical records management or economic analytical tools based on practice type.
Comparisons based on PM involvement showed that physicians in practices with nonphysician management had only a slightly better FKD (5.6) at graduation than those in practices with physician involvement (5.7). None of the 9 topics was statistically significant different based on physician involvement in PM.
Discussion
Building a successful medical practice has become more difficult for graduating orthopedic surgery residents because of an increasingly complex health care system, shrinking reimbursement rates, and looming regulatory changes. These challenges have reinforced the importance of teaching residents the necessary PM knowledge and skills to function effectively in a medical practice. Multiple studies from different specialties surveying or testing graduating residents and young practicing physicians on their business management knowledge or specific business topics have shown severe deficiencies.5-11 Unfortunately, graduating orthopedic surgery residents also appear inadequately prepared in PM. In a study of resident coding/billing knowledge, Gill and Schutt6 surveyed 2006 graduating orthopedic residents and found that only 13% felt confident in their coding ability. Our study results add to our understanding of multiple PM topics and demonstrate graduating orthopedic residents’ deficiencies throughout these topics.
Increased efforts to develop business management training programs and curricula have helped improve both overall PM and business knowledge in other specialties.12-15 ACGME now requires 100 hours of PM training among family medicine residency programs.16 A curriculum instituted in a general surgery residency focused on improving coding found that accuracy improved from 36% to 88% over 12 months.13 A family practice residency instituted a “simulated practice” model for its residents to improve practical PM learning and found statistically significant improvement over their prior didactic lectures.15 However, there continues to be significant variability in the topics and methods covered in business management curricula as programs struggle to determine how to most effectively use their limited time to prepare graduating residents.
In this study, we introduced the concept of FKD. With limited time available for teaching business knowledge and PM skills in residency, it has become imperative that training be efficient and effective. The FKD model can improve training efficiency by directing training to the topics that will produce the highest yield in preparing physicians for practice. As our results demonstrate, topics with the lowest levels of knowledge among surgeons often are not the same as the topics that are most needed to function effectively in practice (Table 3). The FKD model identifies deficiencies in practical, applicable knowledge rather than focusing on a general knowledge level. We suspect that focusing on topics with a high FKD would provide a higher yield in preparing physicians for practice. As such, our results suggest that training in business operations and coding/billing would likely provide the highest practical value, despite the fact that these were not the areas of least general knowledge.
Another finding of this study was the FKD difference based on type of practice. Compared with private practice physicians, hospital-employed or academic physicians had substantially lower overall FKDs and significantly lower FKDs in several specific topics. However, these FKD differences exist despite minimal differences in overall levels of knowledge. This would suggest that less business knowledge was needed by physicians to enter these types of practices compared with traditional private practice. We speculate that this may be one factor influencing the recent trend by graduating orthopedic residents to take hospital-employed positions, as these positions may appear less demanding in terms of learning the management aspects of the new practice.
Our results also showed slightly higher reported average business knowledge and lower FKD reported by those who had recently completed training (within 2-5 years) versus those in practice much longer. This is particularly interesting, as our institution has maintained the same lecture-based program for many years without significant changes. Although these differences may not be statistically significant, they may reflect an increased interest in and attention to learning PM skills while in training. However, we acknowledge this is only one of many possible explanations for these findings.
This study had several limitations. First, all respondents were graduates of a single institution. We were trying to limit the variability in business training, but this also limits the scope of the results. Second, self-ratings on surveys provide subjective measures of business knowledge and functional knowledge. Scores may vary based on individuals’ understanding of given topics, or they may inaccurately represent their level of understanding. This is especially true of respondents who graduated from residency, for example, 20 years earlier—their survey responses may reflect erroneous recollection of business training at time of graduation compared with respondents who graduated more recently. Conversely, more recent graduates may not have a fully formed or accurate picture of how much business knowledge is required to function in practice. Nevertheless, we found no significant differences in measured parameters based on graduation date, so we chose not to exclude older respondents, which also may have weakened our data pool. Further, FKDs are relative values used to compare subjective deficiencies rather than absolute scores of specific general knowledge. As such, subjectivity, including recollection of business training, is inherent in the model used in this study.
Conclusion
Graduating orthopedic surgeons currently appear inadequately prepared to effectively manage business issues in their practices, as evidenced by their low overall knowledge levels and high FKDs. The novel FKD model described in this study helps define FKD levels and identify topics that may provide the highest yield in improving effectiveness in practice. Residency curricula focused on improving business and PM knowledge, particularly in the topics with the highest FKDs (eg, business operations, coding/billing), may improve training efficiency in these areas. Further studies with larger numbers of physicians across multiple institutions are needed to confirm these findings and to validate the FKD concept.
1. Rose EA, Neale AV, Rathur WA. Teaching practice management during residency. Fam Med. 1999;31(2):107-113.
2. Accreditation Council for Graduate Medical Education. ACGME common program requirements. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/CPRs2013.pdf. Updated June 9, 2013. Accessed August 25, 2015.
3. Itani K. A positive approach to core competencies and benchmarks for graduate medical education. Am J Surg. 2002;184(3):196-203.
4. Lusco VC, Martinez SA, Polk HC Jr. Program directors in surgery agree that residents should be formally trained in business and practice management. Am J Surg. 2005;189(1):11-13.
5. McDonnell PJ, Kirwan TJ, Brinton GS, et al. Perceptions of recent ophthalmology residency graduates regarding preparation for practice. Ophthalmology. 2007;114(2):387-391.
6. Gill JB, Schutt RC Jr. Practice management education in orthopaedic surgical residencies. J Bone Joint Surg Am. 2007;89(1):216-219.
7. Satiani B. Business knowledge in surgeons. Am J Surg. 2004;188(1):13-16.
8. Cantor JC, Baker LC, Hughes RG. Preparedness for practice. Young physicians’ views of their professional education. JAMA. 1993;270(9):1035-1040.
9. Fakhry SM, Robinson L, Hendershot K, Reines HD. Surgical residents’ knowledge of documentation and coding for professional services: an opportunity for a focused educational offering. Am J Surg. 2007;194(2):263-267.
10. Williford LE, Ling FW, Summitt RL Jr, Stovall TG. Practice management in obstetrics and gynecology residency curriculum. Obstet Gynecol. 1999;94(3):476-479.
11. Andreae MC, Dunham K, Freed GL. Inadequate training in billing and coding as perceived by recent pediatric graduates. Clin Pediatr. 2009;48(9):939-944.
12. Kolva DE, Barzee KA, Morley CP. Practice management residency curricula: a systematic literature review. Fam Med. 2009;41(6):411-419.
13. Jones K, Lebron RA, Mangram A, Dunn E. Practice management education during surgical residency. Am J Surg. 2008;196(6):878-881.
14. Kerfoot BP, Conlin PR, Travison T, McMahon GT. Web-based education in systems-based practice: a randomized trial. Arch Intern Med. 2007;167(4):361-366.
15. LoPresti L, Ginn P, Treat R. Using a simulated practice to improve practice management learning. Fam Med. 2009;41(9):640-645.
16. Accreditation Council for Graduate Medical Education. Family medicine program requirements. https://www.acgme.org/acgmeweb/tabid/132/ProgramandInstitutionalAccreditation/MedicalSpecialties/FamilyMedicine.aspx. Accessed September 23, 2015.
1. Rose EA, Neale AV, Rathur WA. Teaching practice management during residency. Fam Med. 1999;31(2):107-113.
2. Accreditation Council for Graduate Medical Education. ACGME common program requirements. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/CPRs2013.pdf. Updated June 9, 2013. Accessed August 25, 2015.
3. Itani K. A positive approach to core competencies and benchmarks for graduate medical education. Am J Surg. 2002;184(3):196-203.
4. Lusco VC, Martinez SA, Polk HC Jr. Program directors in surgery agree that residents should be formally trained in business and practice management. Am J Surg. 2005;189(1):11-13.
5. McDonnell PJ, Kirwan TJ, Brinton GS, et al. Perceptions of recent ophthalmology residency graduates regarding preparation for practice. Ophthalmology. 2007;114(2):387-391.
6. Gill JB, Schutt RC Jr. Practice management education in orthopaedic surgical residencies. J Bone Joint Surg Am. 2007;89(1):216-219.
7. Satiani B. Business knowledge in surgeons. Am J Surg. 2004;188(1):13-16.
8. Cantor JC, Baker LC, Hughes RG. Preparedness for practice. Young physicians’ views of their professional education. JAMA. 1993;270(9):1035-1040.
9. Fakhry SM, Robinson L, Hendershot K, Reines HD. Surgical residents’ knowledge of documentation and coding for professional services: an opportunity for a focused educational offering. Am J Surg. 2007;194(2):263-267.
10. Williford LE, Ling FW, Summitt RL Jr, Stovall TG. Practice management in obstetrics and gynecology residency curriculum. Obstet Gynecol. 1999;94(3):476-479.
11. Andreae MC, Dunham K, Freed GL. Inadequate training in billing and coding as perceived by recent pediatric graduates. Clin Pediatr. 2009;48(9):939-944.
12. Kolva DE, Barzee KA, Morley CP. Practice management residency curricula: a systematic literature review. Fam Med. 2009;41(6):411-419.
13. Jones K, Lebron RA, Mangram A, Dunn E. Practice management education during surgical residency. Am J Surg. 2008;196(6):878-881.
14. Kerfoot BP, Conlin PR, Travison T, McMahon GT. Web-based education in systems-based practice: a randomized trial. Arch Intern Med. 2007;167(4):361-366.
15. LoPresti L, Ginn P, Treat R. Using a simulated practice to improve practice management learning. Fam Med. 2009;41(9):640-645.
16. Accreditation Council for Graduate Medical Education. Family medicine program requirements. https://www.acgme.org/acgmeweb/tabid/132/ProgramandInstitutionalAccreditation/MedicalSpecialties/FamilyMedicine.aspx. Accessed September 23, 2015.
Comparison of Outcomes and Costs of Tension-Band and Locking-Plate Osteosynthesis in Transverse Olecranon Fractures: A Matched-Cohort Study
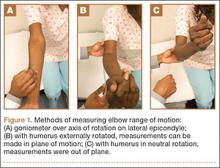
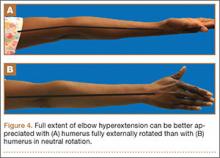
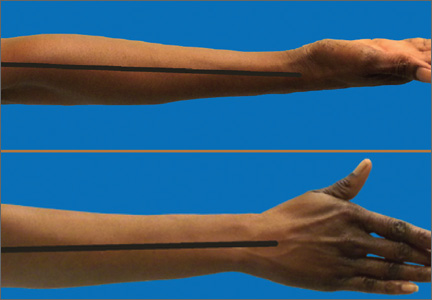
Olecranon fractures are a common injury, representing 10% of all upper extremity fractures.1 Displaced fractures require fixation to restore anatomical alignment and minimize posttraumatic arthrosis.2,3 Multiple surgical techniques have been developed to treat these fractures, with implant choice largely dictated by fracture pattern and associated injuries. Simple, noncomminuted, transverse, proximal fractures can be treated with a tension-band construct, and fractures that are comminuted, oblique, distal to the midpoint of the sigmoid notch, or associated with complex elbow injuries generally require locking-plate fixation.4,5 Although both tension bands and locking plates have been used successfully (Figures 1A, 1B), they remain some of the most frequently removed orthopedic implants, usually because of implant prominence.6
Both fixation devices have potential advantages and disadvantages. Tension-band fixation requires relatively “low-tech” instrumentation and implants and, as a result, has less cost and potentially less operative time for application. As it is smaller than a plate-and-screw construct, a tension band may be less prone to prominence, but this has not been substantiated in the literature.7-14 Implant migration has been a reported complication of tension-band fixation.7,11,13,15
Locking-plate fixation has been shown to be biomechanically stronger,16 and some reports have shown fewer repeat operations for implant prominence than with tension-band fixation.1,8,17-22 Because of more advanced product development and manufacturing, however, it comes at a higher cost. Plate fixation also requires more steps for application, which may require more operative time, and implant prominence has remained a problem, even with modern plates with lower profiles.19
Previous studies of olecranon fixation have included complex fractures and osteotomies or did not include current-generation precontoured locking plates. We found no other study that compared the outcomes, complications, and costs of tension-band and modern locking-plate fixation of isolated transverse olecranon fractures.
To determine if there are significant differences in outcomes and costs between tension-band and locking-plate fixation of transverse olecranon fractures in adults, we retrospectively compared functional outcomes, complications, and costs in 2 matched cohorts of displaced transverse olecranon fractures. We hypothesized that there would be no differences in functional outcomes, implant prominence, posttraumatic arthrosis, complications, or operative time, but that costs would be less with tension-band fixation.
Materials and Methods
After obtaining institutional review board approval, we retrospectively reviewed the medical records of patients who had undergone fixation of an isolated, transverse, noncomminuted olecranon fracture (Orthopaedic Trauma Association 21B1) at our institution between 2004 and 2011. Inclusion criteria included use of a tension-band construct or a precontoured locking plate, skeletal maturity at time of injury, and minimum 2-year follow-up. Exclusion criteria were open fractures, osteotomies, any other ipsilateral upper extremity fracture, and fractures with comminution, obliquity, or distal location.
Although, based on fracture pattern, tension-band fixation is appropriate for olecranon osteotomies used for distal humeral exposure, we did not include osteotomies because functional outcomes would likely be different from those of true olecranon fractures, in addition to the possibility that the soft-tissue injury from a distal humeral fracture and resultant exposure could result in a different level of implant prominence. To control for demographic variables, we used a cohort design in which patients were matched on age and length of follow-up.
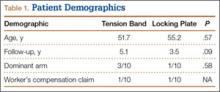
During the study period, we treated 287 olecranon fractures. Forty-nine patients met the inclusion criteria. The study population consisted of 20 patients, 10 in each cohort matched on age and length of follow-up. There were no statistically significant differences between groups in demographic variables, including dominant arm involved and number of worker’s compensation claims (Table 1). Mechanisms of injury were similar in the groups. In the tension-band group, 9 patients fell directly onto their elbow, and 1 fell onto her outstretched hand. In the locking-plate group, 8 patients fell directly onto the elbow, 1 fell onto her outstretched hand, and 1 was injured in a motorcycle accident.
All surgeons, regardless of implant selected, used a posterior incision that curved slightly laterally about the tip of the olecranon. Surgeon preference determined which fixation construct to use. Tension-band fixation was performed using 2 bicortical Kirschner wires and a stainless-steel wire through a distal drill hole to complete the tension band. Of the 10 locking-plate constructs used, 4 were PERI-LOC olecranon locking plates (Smith & Nephew), 3 were LCP olecranon plates (Synthes), and 3 were periarticular proximal ulna locking plates (Zimmer).
All returning patients were seen by either Dr. Amini or Mr. Wilson and underwent range of motion (ROM) measurement with a goniometer; assessment for subjective and objective implant prominence (graded none, mild, moderate, or severe/already had implant removed); and functional scoring using the Mayo Elbow Performance Score (MEPS) and the Quick Disability of the Arm, Shoulder, and Hand (QDASH). Results were classified excellent (MEPS, >90), good (75-89), fair (60-74), and poor (<60).23
Anteroposterior and lateral radiographs of the elbow were obtained at follow-up and were examined for maintenance/integrity of implants, radiographic union, and posttraumatic arthrosis. Arthrosis was graded using the Broberg and Morrey24 classification: grade 0 (normal elbow), grade 1 (slight joint-space narrowing with minimal osteophyte formation), grade 2 (moderate joint-space narrowing with moderate osteophyte formation), grade 3 (severe degenerative changes with gross destruction of joint).
Medical records were examined to determine surgery time. Billing information was examined to determine charges related to each operation, specifically the charge for the implants and the overall charge for the operation, which included anesthesia charges. Subsequent operations were included as applicable.
Student t test was used to compare differences in normative data, and Pearson χ2 test to compare differences in categorical data. Differences with P < .05 were considered significant.
Results
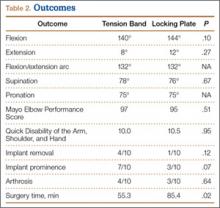
There were no clinically or statistically significant differences in ROM or functional outcomes (Table 2). According to MEPS, results were excellent in 8 and good in 2 patients in the tension-band group and excellent in 7 and good in 3 patients in the locking-plate group.
In patients who had implants removed, average time to subsequent procedure was 6.2 months, and all patients who underwent implant removal did so before 1-year follow-up. Implant removal was required in 4 tension-band patients and 1 locking-plate patient (P = .12). Similarly, 7 tension-band patients (including those with implants removed) and 3 locking-plate patients had implant-related symptoms, with the difference trending (P = .07) toward significance (Table 2).
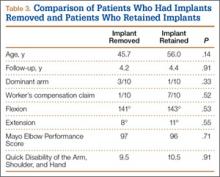
Patients who elected to have their implants removed tended to be younger than those who did not (45.7 vs 56.0 years); the difference (P = .14) was not significant. Worker’s compensation status did not affect the decision to undergo implant removal. At final follow-up, there were no differences in ROM or functional outcomes between patients who had implants removed and those who did not. No variable predicted which patients had implants removed or not (Table 3).
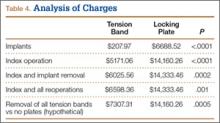
Implant charges were $207.97 for the tension-band cohort and $6688.52 for the locking-plate cohort (P < .0001). Operative charges for the index procedures were $5171.06 for tension-band fixation and $14,160.26 for locking-plate fixation (P < .0001). Overall operative charges, including charges for subsequent operations, were $6598.36 in the tension-band cohort and $14,333.46 in the locking-plate cohort (P = .001). In a comparison of combined charges for index procedure and implant removal (excluding other repeat operations), charges were $6025.56 for the tension-band cohort and $14,333.46 for the locking-plate cohort (P = .0002). Even if all patients with tension-band fixation and no patients with locking-plate fixation had implant removal, mean charges for all operative care would still be significantly (P = .0005) less in the tension-band cohort than in the locking-plate cohort ($7307.31 vs $14,160.26) (Table 4).
Surgery time was significantly (P = .025) less for tension-band fixation than for locking-plate fixation (55.3 vs 85.4 minutes) (Table 2).
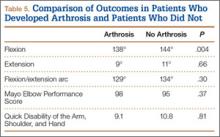
Four tension-band patients and 3 locking-plate patients had radiographic evidence of grade 1 posttraumatic arthrosis (P = .64). None required subsequent procedures. Patients with posttraumatic arthrosis had slightly less flexion, but there was no difference in overall flexion-extension arc or functional outcomes between patients with and without arthrosis (Table 5).
The locking-plate cohort had no other complications, and the tension-band cohort had 3. In 1 tension-band patient, the wire disengaged from the Kirschner wires. The fracture healed, but a subsequent procedure was required for symptomatic implant prominence (Figures 2A–2C). Another tension-band patient developed both posttraumatic arthrofibrosis and cubital tunnel syndrome, in addition to a prominent implant. She underwent capsular release, ulnar nerve transposition, and implant removal. At final follow-up, motion was improved, and ulnar nerve symptoms were resolved. There were no infections in either group. Overall, there were no statistically significant differences in complications between groups.
Discussion
We conducted this study to determine differences between tension-band and locking-plate fixation of isolated, closed, noncomminuted, transverse olecranon fractures. Few studies have directly compared tension-band and locking-plate fixation,8,10,19,25 particularly in reference to outcomes of functional scores, implant prominence, complications, operative time, and cost-effectiveness. We found no study that clinically compared these implants since the advent of precontoured locking plates, and no study that compared results in similar fracture patterns. In our study, we found no differences in functional or radiographic outcomes between groups, but significant differences in charges and overall cost of care.
Our findings suggest that patients return to high functional level an average of 4.3 years after fixation of an olecranon fracture with either a tension band or a locking plate. Both cohorts achieved QDASH scores equivalent to normative values for the general population,26 and all patients in both cohorts achieved either good or excellent results based on MEPS values.23 This is comparable to reported functional outcomes in the literature, with previous reports suggesting 86% to 92% of patients obtain good or excellent results.1,7,8,12,14,17,18,27 The rate of posttraumatic arthrosis in both cohorts was low, and, when present, arthrosis was radiographically mild (no patient had grade 2 or 3 arthrosis). Patients with and without radiographic evidence of arthrosis had similar ROM and functional outcomes.
Our findings also suggest a trend toward fewer implant-related symptoms and less need for implant removal in patients treated with locking plates. Although both implants have high rates of prominence requiring removal, most studies support our findings that tension bands are more prominent than locking plates. Fixation has been reported to cause prominence requiring removal in 42% to 82% of patients with tension bands7-14 and 0% to 47% of patients with locking plates.1,8,17,18,20-22,28 It is important to note that many earlier studies either were conducted before the advent of precontoured locking plates or were not comparative.1,7,9-14,17,18,20-22,28 In one recent study, however, Edwards and colleagues19 surveyed 138 patients and found very similar implant removal rates: 63.6% for tension bands and 62.5% for locking plates. Nevertheless, implant removal rates for fixation of olecranon fractures remain high, regardless of implant used.
Our data did not reveal any difference in ROM or functional outcomes between patients who had and did not have implants removed. This suggests, first, that QDASH and MEPS may not be sensitive in identifying patients with implant prominence, as neither questionnaire incorporates implant prominence into its scoring, and, second, that implant removal does not significantly impair ROM. As a result, surgeons should consider asking patients specifically about symptoms of prominent implants once there is convincing evidence of union and counseling them about implant removal if appropriate.
To our knowledge, the differences in cost and operative time between tension-band and locking-plate fixation have not been previously reported. Our data suggest that the financial differences resulted mainly from implant charges; overall, tension-band fixation was roughly half the cost of locking-plate fixation. In addition, in patients who eventually had implants removed, the cost of implant removal was relatively small compared with the cost of the initial fixation in both cohorts. As a result, even if all patients in the tension-band cohort and no patients in the locking-plate cohort had implants removed, tension-band fixation and subsequent implant removal would still cost half as much as locking-plate fixation without implant removal. Moreover, fixation with a tension band took roughly 30 minutes less than fixation with a plate. Less time in the operating room likely contributed to the additional cost savings realized with tension-band fixation beyond those directly resulting from implant cost.
The strength of this study lies in the homogeneity of cohorts. Each cohort was matched primarily on age and secondarily on length of follow-up. All patients had closed, proximal, transverse fractures without comminution, and we excluded olecranon osteotomies as these represent an entity different from true fractures. Fractures with comminution or distal extension may represent more severe injuries, and functional scores, complications, hardware prominence, and operative time might have been affected by inclusion of these fractures. Further, there were no infections in either group to skew the rate of implant prominence or removal.
The weaknesses of the study lie in its limited sample sizes, retrospective design, and lack of long-term follow-up. Group size was limited by our attempts to create homogenous cohorts. As a result, some patients were not included as participants because of strict exclusion criteria. Most notably, we excluded any fracture not appropriate for tension-band fixation, as well as open fractures and osteotomies. Despite the retrospective nature of the study, all patients were examined by the investigators at final follow-up (minimum, 2 years) for the purpose of this study. It is possible that these functional results may not be sustained over the long term, as the risk for posttraumatic arthrosis in articular injuries builds with time. Although some patients may want to have implants removed later, all our study patients who had implants removed had them removed within 1 year, and all 20 patients were reached at minimum 2-year follow-up. Thus, it is unlikely but possible that some of the other study patients will elect to have implants removed.
1. Buijze G, Kloen P. Clinical evaluation of locking compression plate fixation for comminuted olecranon fractures. J Bone Joint Surg Am. 2009;91(10):
2416-2420.
2. Newman SD, Mauffrey C, Krikler S. Olecranon fractures. Injury. 2009;40(6):575-581.
3. Veillette CJ, Steinmann SP. Olecranon fractures. Orthop Clin North Am. 2008;39(2):229-236.
4. Baecher N, Edwards S. Olecranon fractures. J Hand Surg Am. 2013;38(3):593-604.
5. Hak DJ, Golladay GJ. Olecranon fractures: treatment options. J Am Acad Orthop Surg. 2000;8(4):266-275.
6. Busam ML, Esther RJ, Obremskey WT. Hardware removal: indications and expectations. J Am Acad Orthop Surg. 2006;14(2):113-120.
7. Chalidis BE, Sachinis NC, Samoladas EP, Dimitriou CG, Pournaras JD. Is tension band wiring technique the “gold standard” for the treatment of olecranon fractures? A long term functional outcome study. J Orthop Surg Res. 2008;3:9.
8. Hume MC, Wiss DA. Olecranon fractures: a clinical and radiographic comparison of tension-band wiring and plate fixation. Clin Orthop Relat Res. 1992;(285):229-235.
9. Karlsson MK, Hasserius R, Besjakov J, Karlsson C, Josefsson PO. Comparison of tension-band and figure-of-eight wiring techniques for treatment of olecranon fractures. J Shoulder Elbow Surg. 2002;11(4):377-382.
10. Lindenhovius AL, Brouwer KM, Doornberg JN, Ring DC, Kloen P. Long-term outcome of operatively treated fracture-dislocations of the olecranon. J Orthop Trauma. 2008;22(5):325-331.
11. Macko D, Szabo RM. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg Am. 1985;67(9):1396-1401.
12. Romero JM, Miran A, Jensen CH. Complications and re-operation rate after tension-band wiring of olecranon fractures. J Orthop Sci. 2000;5(4):318-320.
13. Rommens PM, Schneider RU, Reuter M. Functional results after operative treatment of olecranon fractures. Acta Chir Belg. 2004;104(2):191-197.
14. Villanueva P, Osorio F, Commessatti M, Sanchez-Sotelo J. Tension-band wiring for olecranon fractures: analysis of risk factors for failure. J Shoulder Elbow Surg. 2006;15(3):351-356.
15. Sahajpal D, Wright TW. Proximal ulna fractures. J Hand Surg Am. 2009;34(2):357-362.
16. Rouleau DM, Sandman E, van Riet R, Galatz LM. Management of fractures of the proximal ulna. J Am Acad Orthop Surg. 2013;21(3):149-160.
17. Anderson ML, Larson AN, Merten SM, Steinmann SP. Congruent elbow plate fixation of olecranon fractures. J Orthop Trauma. 2007;21(6):386-393.
18. Bailey CS, MacDermid J, Patterson SD, King GJ. Outcome of plate fixation of olecranon fractures. J Orthop Trauma. 2001;15(8):542-548.
19. Edwards SG, Cohen MS, Lattanza LL, et al. Surgeon perceptions and patient outcomes regarding proximal ulna fixation: a multicenter experience. J Shoulder Elbow Surg. 2012;21(12):1637-1643.
20. Munoz-Mahamud E, Fernandez-Valencia JA, Riba J. Plate osteosynthesis for severe olecranon fractures. J Orthop Surg. 2010;18(1):80-84.
21. Simpson NS, Goodman LA, Jupiter JB. Contoured LCDC plating of the proximal ulna. Injury. 1996;27(6):411-417.
22. Tejwani NC, Garnham IR, Wolinsky PR, Kummer FJ, Koval KJ. Posterior olecranon plating: biomechanical and clinical evaluation of a new operative technique. Bull Hosp Jt Dis. 2002-2003;61(1-2):27-31.
23. Morrey BF, An KN. Functional evaluation of the elbow. In: Morrey BF, Sanchez-Sotelo J, eds. The Elbow and Its Disorders. 4th ed. Philadelphia, PA: Elsevier; 2008:87-88.
24. Broberg MA, Morrey BF. The results of delayed excision of the radial head for fracture. J Bone Joint Surg Am. 1986;68(5):669-674.
25. Horne JG, Tanzer TL. Olecranon fractures: a review of 100 cases. J Trauma. 1981;21(6):469-472.
26. Hunsaker FG, Cioffi DA, Amadio PC, Wright JG, Caughlin B. The American Academy of Orthopaedic Surgeons outcomes instruments: normative values from the general population. J Bone Joint Surg Am. 2002;84(2):208-215.
27. Ikeda M, Fukushima Y, Kobayashi Y, Oka Y. Comminuted fractures of the olecranon. Management by bone graft from the iliac crest and multiple tension-band wiring. J Bone Joint Surg Br. 2001;83(6):805-808.
28. Erturer RE, Sever C, Sonmez MM, Ozcelik IB, Akman S, Ozturk I. Results of open reduction and plate osteosynthesis in comminuted fracture of the olecranon. J Shoulder Elbow Surg. 2011;20(3):449-454.
Olecranon fractures are a common injury, representing 10% of all upper extremity fractures.1 Displaced fractures require fixation to restore anatomical alignment and minimize posttraumatic arthrosis.2,3 Multiple surgical techniques have been developed to treat these fractures, with implant choice largely dictated by fracture pattern and associated injuries. Simple, noncomminuted, transverse, proximal fractures can be treated with a tension-band construct, and fractures that are comminuted, oblique, distal to the midpoint of the sigmoid notch, or associated with complex elbow injuries generally require locking-plate fixation.4,5 Although both tension bands and locking plates have been used successfully (Figures 1A, 1B), they remain some of the most frequently removed orthopedic implants, usually because of implant prominence.6
Both fixation devices have potential advantages and disadvantages. Tension-band fixation requires relatively “low-tech” instrumentation and implants and, as a result, has less cost and potentially less operative time for application. As it is smaller than a plate-and-screw construct, a tension band may be less prone to prominence, but this has not been substantiated in the literature.7-14 Implant migration has been a reported complication of tension-band fixation.7,11,13,15
Locking-plate fixation has been shown to be biomechanically stronger,16 and some reports have shown fewer repeat operations for implant prominence than with tension-band fixation.1,8,17-22 Because of more advanced product development and manufacturing, however, it comes at a higher cost. Plate fixation also requires more steps for application, which may require more operative time, and implant prominence has remained a problem, even with modern plates with lower profiles.19
Previous studies of olecranon fixation have included complex fractures and osteotomies or did not include current-generation precontoured locking plates. We found no other study that compared the outcomes, complications, and costs of tension-band and modern locking-plate fixation of isolated transverse olecranon fractures.
To determine if there are significant differences in outcomes and costs between tension-band and locking-plate fixation of transverse olecranon fractures in adults, we retrospectively compared functional outcomes, complications, and costs in 2 matched cohorts of displaced transverse olecranon fractures. We hypothesized that there would be no differences in functional outcomes, implant prominence, posttraumatic arthrosis, complications, or operative time, but that costs would be less with tension-band fixation.
Materials and Methods
After obtaining institutional review board approval, we retrospectively reviewed the medical records of patients who had undergone fixation of an isolated, transverse, noncomminuted olecranon fracture (Orthopaedic Trauma Association 21B1) at our institution between 2004 and 2011. Inclusion criteria included use of a tension-band construct or a precontoured locking plate, skeletal maturity at time of injury, and minimum 2-year follow-up. Exclusion criteria were open fractures, osteotomies, any other ipsilateral upper extremity fracture, and fractures with comminution, obliquity, or distal location.
Although, based on fracture pattern, tension-band fixation is appropriate for olecranon osteotomies used for distal humeral exposure, we did not include osteotomies because functional outcomes would likely be different from those of true olecranon fractures, in addition to the possibility that the soft-tissue injury from a distal humeral fracture and resultant exposure could result in a different level of implant prominence. To control for demographic variables, we used a cohort design in which patients were matched on age and length of follow-up.
During the study period, we treated 287 olecranon fractures. Forty-nine patients met the inclusion criteria. The study population consisted of 20 patients, 10 in each cohort matched on age and length of follow-up. There were no statistically significant differences between groups in demographic variables, including dominant arm involved and number of worker’s compensation claims (Table 1). Mechanisms of injury were similar in the groups. In the tension-band group, 9 patients fell directly onto their elbow, and 1 fell onto her outstretched hand. In the locking-plate group, 8 patients fell directly onto the elbow, 1 fell onto her outstretched hand, and 1 was injured in a motorcycle accident.
All surgeons, regardless of implant selected, used a posterior incision that curved slightly laterally about the tip of the olecranon. Surgeon preference determined which fixation construct to use. Tension-band fixation was performed using 2 bicortical Kirschner wires and a stainless-steel wire through a distal drill hole to complete the tension band. Of the 10 locking-plate constructs used, 4 were PERI-LOC olecranon locking plates (Smith & Nephew), 3 were LCP olecranon plates (Synthes), and 3 were periarticular proximal ulna locking plates (Zimmer).
All returning patients were seen by either Dr. Amini or Mr. Wilson and underwent range of motion (ROM) measurement with a goniometer; assessment for subjective and objective implant prominence (graded none, mild, moderate, or severe/already had implant removed); and functional scoring using the Mayo Elbow Performance Score (MEPS) and the Quick Disability of the Arm, Shoulder, and Hand (QDASH). Results were classified excellent (MEPS, >90), good (75-89), fair (60-74), and poor (<60).23
Anteroposterior and lateral radiographs of the elbow were obtained at follow-up and were examined for maintenance/integrity of implants, radiographic union, and posttraumatic arthrosis. Arthrosis was graded using the Broberg and Morrey24 classification: grade 0 (normal elbow), grade 1 (slight joint-space narrowing with minimal osteophyte formation), grade 2 (moderate joint-space narrowing with moderate osteophyte formation), grade 3 (severe degenerative changes with gross destruction of joint).
Medical records were examined to determine surgery time. Billing information was examined to determine charges related to each operation, specifically the charge for the implants and the overall charge for the operation, which included anesthesia charges. Subsequent operations were included as applicable.
Student t test was used to compare differences in normative data, and Pearson χ2 test to compare differences in categorical data. Differences with P < .05 were considered significant.
Results
There were no clinically or statistically significant differences in ROM or functional outcomes (Table 2). According to MEPS, results were excellent in 8 and good in 2 patients in the tension-band group and excellent in 7 and good in 3 patients in the locking-plate group.
In patients who had implants removed, average time to subsequent procedure was 6.2 months, and all patients who underwent implant removal did so before 1-year follow-up. Implant removal was required in 4 tension-band patients and 1 locking-plate patient (P = .12). Similarly, 7 tension-band patients (including those with implants removed) and 3 locking-plate patients had implant-related symptoms, with the difference trending (P = .07) toward significance (Table 2).
Patients who elected to have their implants removed tended to be younger than those who did not (45.7 vs 56.0 years); the difference (P = .14) was not significant. Worker’s compensation status did not affect the decision to undergo implant removal. At final follow-up, there were no differences in ROM or functional outcomes between patients who had implants removed and those who did not. No variable predicted which patients had implants removed or not (Table 3).
Implant charges were $207.97 for the tension-band cohort and $6688.52 for the locking-plate cohort (P < .0001). Operative charges for the index procedures were $5171.06 for tension-band fixation and $14,160.26 for locking-plate fixation (P < .0001). Overall operative charges, including charges for subsequent operations, were $6598.36 in the tension-band cohort and $14,333.46 in the locking-plate cohort (P = .001). In a comparison of combined charges for index procedure and implant removal (excluding other repeat operations), charges were $6025.56 for the tension-band cohort and $14,333.46 for the locking-plate cohort (P = .0002). Even if all patients with tension-band fixation and no patients with locking-plate fixation had implant removal, mean charges for all operative care would still be significantly (P = .0005) less in the tension-band cohort than in the locking-plate cohort ($7307.31 vs $14,160.26) (Table 4).
Surgery time was significantly (P = .025) less for tension-band fixation than for locking-plate fixation (55.3 vs 85.4 minutes) (Table 2).
Four tension-band patients and 3 locking-plate patients had radiographic evidence of grade 1 posttraumatic arthrosis (P = .64). None required subsequent procedures. Patients with posttraumatic arthrosis had slightly less flexion, but there was no difference in overall flexion-extension arc or functional outcomes between patients with and without arthrosis (Table 5).
The locking-plate cohort had no other complications, and the tension-band cohort had 3. In 1 tension-band patient, the wire disengaged from the Kirschner wires. The fracture healed, but a subsequent procedure was required for symptomatic implant prominence (Figures 2A–2C). Another tension-band patient developed both posttraumatic arthrofibrosis and cubital tunnel syndrome, in addition to a prominent implant. She underwent capsular release, ulnar nerve transposition, and implant removal. At final follow-up, motion was improved, and ulnar nerve symptoms were resolved. There were no infections in either group. Overall, there were no statistically significant differences in complications between groups.
Discussion
We conducted this study to determine differences between tension-band and locking-plate fixation of isolated, closed, noncomminuted, transverse olecranon fractures. Few studies have directly compared tension-band and locking-plate fixation,8,10,19,25 particularly in reference to outcomes of functional scores, implant prominence, complications, operative time, and cost-effectiveness. We found no study that clinically compared these implants since the advent of precontoured locking plates, and no study that compared results in similar fracture patterns. In our study, we found no differences in functional or radiographic outcomes between groups, but significant differences in charges and overall cost of care.
Our findings suggest that patients return to high functional level an average of 4.3 years after fixation of an olecranon fracture with either a tension band or a locking plate. Both cohorts achieved QDASH scores equivalent to normative values for the general population,26 and all patients in both cohorts achieved either good or excellent results based on MEPS values.23 This is comparable to reported functional outcomes in the literature, with previous reports suggesting 86% to 92% of patients obtain good or excellent results.1,7,8,12,14,17,18,27 The rate of posttraumatic arthrosis in both cohorts was low, and, when present, arthrosis was radiographically mild (no patient had grade 2 or 3 arthrosis). Patients with and without radiographic evidence of arthrosis had similar ROM and functional outcomes.
Our findings also suggest a trend toward fewer implant-related symptoms and less need for implant removal in patients treated with locking plates. Although both implants have high rates of prominence requiring removal, most studies support our findings that tension bands are more prominent than locking plates. Fixation has been reported to cause prominence requiring removal in 42% to 82% of patients with tension bands7-14 and 0% to 47% of patients with locking plates.1,8,17,18,20-22,28 It is important to note that many earlier studies either were conducted before the advent of precontoured locking plates or were not comparative.1,7,9-14,17,18,20-22,28 In one recent study, however, Edwards and colleagues19 surveyed 138 patients and found very similar implant removal rates: 63.6% for tension bands and 62.5% for locking plates. Nevertheless, implant removal rates for fixation of olecranon fractures remain high, regardless of implant used.
Our data did not reveal any difference in ROM or functional outcomes between patients who had and did not have implants removed. This suggests, first, that QDASH and MEPS may not be sensitive in identifying patients with implant prominence, as neither questionnaire incorporates implant prominence into its scoring, and, second, that implant removal does not significantly impair ROM. As a result, surgeons should consider asking patients specifically about symptoms of prominent implants once there is convincing evidence of union and counseling them about implant removal if appropriate.
To our knowledge, the differences in cost and operative time between tension-band and locking-plate fixation have not been previously reported. Our data suggest that the financial differences resulted mainly from implant charges; overall, tension-band fixation was roughly half the cost of locking-plate fixation. In addition, in patients who eventually had implants removed, the cost of implant removal was relatively small compared with the cost of the initial fixation in both cohorts. As a result, even if all patients in the tension-band cohort and no patients in the locking-plate cohort had implants removed, tension-band fixation and subsequent implant removal would still cost half as much as locking-plate fixation without implant removal. Moreover, fixation with a tension band took roughly 30 minutes less than fixation with a plate. Less time in the operating room likely contributed to the additional cost savings realized with tension-band fixation beyond those directly resulting from implant cost.
The strength of this study lies in the homogeneity of cohorts. Each cohort was matched primarily on age and secondarily on length of follow-up. All patients had closed, proximal, transverse fractures without comminution, and we excluded olecranon osteotomies as these represent an entity different from true fractures. Fractures with comminution or distal extension may represent more severe injuries, and functional scores, complications, hardware prominence, and operative time might have been affected by inclusion of these fractures. Further, there were no infections in either group to skew the rate of implant prominence or removal.
The weaknesses of the study lie in its limited sample sizes, retrospective design, and lack of long-term follow-up. Group size was limited by our attempts to create homogenous cohorts. As a result, some patients were not included as participants because of strict exclusion criteria. Most notably, we excluded any fracture not appropriate for tension-band fixation, as well as open fractures and osteotomies. Despite the retrospective nature of the study, all patients were examined by the investigators at final follow-up (minimum, 2 years) for the purpose of this study. It is possible that these functional results may not be sustained over the long term, as the risk for posttraumatic arthrosis in articular injuries builds with time. Although some patients may want to have implants removed later, all our study patients who had implants removed had them removed within 1 year, and all 20 patients were reached at minimum 2-year follow-up. Thus, it is unlikely but possible that some of the other study patients will elect to have implants removed.
Olecranon fractures are a common injury, representing 10% of all upper extremity fractures.1 Displaced fractures require fixation to restore anatomical alignment and minimize posttraumatic arthrosis.2,3 Multiple surgical techniques have been developed to treat these fractures, with implant choice largely dictated by fracture pattern and associated injuries. Simple, noncomminuted, transverse, proximal fractures can be treated with a tension-band construct, and fractures that are comminuted, oblique, distal to the midpoint of the sigmoid notch, or associated with complex elbow injuries generally require locking-plate fixation.4,5 Although both tension bands and locking plates have been used successfully (Figures 1A, 1B), they remain some of the most frequently removed orthopedic implants, usually because of implant prominence.6
Both fixation devices have potential advantages and disadvantages. Tension-band fixation requires relatively “low-tech” instrumentation and implants and, as a result, has less cost and potentially less operative time for application. As it is smaller than a plate-and-screw construct, a tension band may be less prone to prominence, but this has not been substantiated in the literature.7-14 Implant migration has been a reported complication of tension-band fixation.7,11,13,15
Locking-plate fixation has been shown to be biomechanically stronger,16 and some reports have shown fewer repeat operations for implant prominence than with tension-band fixation.1,8,17-22 Because of more advanced product development and manufacturing, however, it comes at a higher cost. Plate fixation also requires more steps for application, which may require more operative time, and implant prominence has remained a problem, even with modern plates with lower profiles.19
Previous studies of olecranon fixation have included complex fractures and osteotomies or did not include current-generation precontoured locking plates. We found no other study that compared the outcomes, complications, and costs of tension-band and modern locking-plate fixation of isolated transverse olecranon fractures.
To determine if there are significant differences in outcomes and costs between tension-band and locking-plate fixation of transverse olecranon fractures in adults, we retrospectively compared functional outcomes, complications, and costs in 2 matched cohorts of displaced transverse olecranon fractures. We hypothesized that there would be no differences in functional outcomes, implant prominence, posttraumatic arthrosis, complications, or operative time, but that costs would be less with tension-band fixation.
Materials and Methods
After obtaining institutional review board approval, we retrospectively reviewed the medical records of patients who had undergone fixation of an isolated, transverse, noncomminuted olecranon fracture (Orthopaedic Trauma Association 21B1) at our institution between 2004 and 2011. Inclusion criteria included use of a tension-band construct or a precontoured locking plate, skeletal maturity at time of injury, and minimum 2-year follow-up. Exclusion criteria were open fractures, osteotomies, any other ipsilateral upper extremity fracture, and fractures with comminution, obliquity, or distal location.
Although, based on fracture pattern, tension-band fixation is appropriate for olecranon osteotomies used for distal humeral exposure, we did not include osteotomies because functional outcomes would likely be different from those of true olecranon fractures, in addition to the possibility that the soft-tissue injury from a distal humeral fracture and resultant exposure could result in a different level of implant prominence. To control for demographic variables, we used a cohort design in which patients were matched on age and length of follow-up.
During the study period, we treated 287 olecranon fractures. Forty-nine patients met the inclusion criteria. The study population consisted of 20 patients, 10 in each cohort matched on age and length of follow-up. There were no statistically significant differences between groups in demographic variables, including dominant arm involved and number of worker’s compensation claims (Table 1). Mechanisms of injury were similar in the groups. In the tension-band group, 9 patients fell directly onto their elbow, and 1 fell onto her outstretched hand. In the locking-plate group, 8 patients fell directly onto the elbow, 1 fell onto her outstretched hand, and 1 was injured in a motorcycle accident.
All surgeons, regardless of implant selected, used a posterior incision that curved slightly laterally about the tip of the olecranon. Surgeon preference determined which fixation construct to use. Tension-band fixation was performed using 2 bicortical Kirschner wires and a stainless-steel wire through a distal drill hole to complete the tension band. Of the 10 locking-plate constructs used, 4 were PERI-LOC olecranon locking plates (Smith & Nephew), 3 were LCP olecranon plates (Synthes), and 3 were periarticular proximal ulna locking plates (Zimmer).
All returning patients were seen by either Dr. Amini or Mr. Wilson and underwent range of motion (ROM) measurement with a goniometer; assessment for subjective and objective implant prominence (graded none, mild, moderate, or severe/already had implant removed); and functional scoring using the Mayo Elbow Performance Score (MEPS) and the Quick Disability of the Arm, Shoulder, and Hand (QDASH). Results were classified excellent (MEPS, >90), good (75-89), fair (60-74), and poor (<60).23
Anteroposterior and lateral radiographs of the elbow were obtained at follow-up and were examined for maintenance/integrity of implants, radiographic union, and posttraumatic arthrosis. Arthrosis was graded using the Broberg and Morrey24 classification: grade 0 (normal elbow), grade 1 (slight joint-space narrowing with minimal osteophyte formation), grade 2 (moderate joint-space narrowing with moderate osteophyte formation), grade 3 (severe degenerative changes with gross destruction of joint).
Medical records were examined to determine surgery time. Billing information was examined to determine charges related to each operation, specifically the charge for the implants and the overall charge for the operation, which included anesthesia charges. Subsequent operations were included as applicable.
Student t test was used to compare differences in normative data, and Pearson χ2 test to compare differences in categorical data. Differences with P < .05 were considered significant.
Results
There were no clinically or statistically significant differences in ROM or functional outcomes (Table 2). According to MEPS, results were excellent in 8 and good in 2 patients in the tension-band group and excellent in 7 and good in 3 patients in the locking-plate group.
In patients who had implants removed, average time to subsequent procedure was 6.2 months, and all patients who underwent implant removal did so before 1-year follow-up. Implant removal was required in 4 tension-band patients and 1 locking-plate patient (P = .12). Similarly, 7 tension-band patients (including those with implants removed) and 3 locking-plate patients had implant-related symptoms, with the difference trending (P = .07) toward significance (Table 2).
Patients who elected to have their implants removed tended to be younger than those who did not (45.7 vs 56.0 years); the difference (P = .14) was not significant. Worker’s compensation status did not affect the decision to undergo implant removal. At final follow-up, there were no differences in ROM or functional outcomes between patients who had implants removed and those who did not. No variable predicted which patients had implants removed or not (Table 3).
Implant charges were $207.97 for the tension-band cohort and $6688.52 for the locking-plate cohort (P < .0001). Operative charges for the index procedures were $5171.06 for tension-band fixation and $14,160.26 for locking-plate fixation (P < .0001). Overall operative charges, including charges for subsequent operations, were $6598.36 in the tension-band cohort and $14,333.46 in the locking-plate cohort (P = .001). In a comparison of combined charges for index procedure and implant removal (excluding other repeat operations), charges were $6025.56 for the tension-band cohort and $14,333.46 for the locking-plate cohort (P = .0002). Even if all patients with tension-band fixation and no patients with locking-plate fixation had implant removal, mean charges for all operative care would still be significantly (P = .0005) less in the tension-band cohort than in the locking-plate cohort ($7307.31 vs $14,160.26) (Table 4).
Surgery time was significantly (P = .025) less for tension-band fixation than for locking-plate fixation (55.3 vs 85.4 minutes) (Table 2).
Four tension-band patients and 3 locking-plate patients had radiographic evidence of grade 1 posttraumatic arthrosis (P = .64). None required subsequent procedures. Patients with posttraumatic arthrosis had slightly less flexion, but there was no difference in overall flexion-extension arc or functional outcomes between patients with and without arthrosis (Table 5).
The locking-plate cohort had no other complications, and the tension-band cohort had 3. In 1 tension-band patient, the wire disengaged from the Kirschner wires. The fracture healed, but a subsequent procedure was required for symptomatic implant prominence (Figures 2A–2C). Another tension-band patient developed both posttraumatic arthrofibrosis and cubital tunnel syndrome, in addition to a prominent implant. She underwent capsular release, ulnar nerve transposition, and implant removal. At final follow-up, motion was improved, and ulnar nerve symptoms were resolved. There were no infections in either group. Overall, there were no statistically significant differences in complications between groups.
Discussion
We conducted this study to determine differences between tension-band and locking-plate fixation of isolated, closed, noncomminuted, transverse olecranon fractures. Few studies have directly compared tension-band and locking-plate fixation,8,10,19,25 particularly in reference to outcomes of functional scores, implant prominence, complications, operative time, and cost-effectiveness. We found no study that clinically compared these implants since the advent of precontoured locking plates, and no study that compared results in similar fracture patterns. In our study, we found no differences in functional or radiographic outcomes between groups, but significant differences in charges and overall cost of care.
Our findings suggest that patients return to high functional level an average of 4.3 years after fixation of an olecranon fracture with either a tension band or a locking plate. Both cohorts achieved QDASH scores equivalent to normative values for the general population,26 and all patients in both cohorts achieved either good or excellent results based on MEPS values.23 This is comparable to reported functional outcomes in the literature, with previous reports suggesting 86% to 92% of patients obtain good or excellent results.1,7,8,12,14,17,18,27 The rate of posttraumatic arthrosis in both cohorts was low, and, when present, arthrosis was radiographically mild (no patient had grade 2 or 3 arthrosis). Patients with and without radiographic evidence of arthrosis had similar ROM and functional outcomes.
Our findings also suggest a trend toward fewer implant-related symptoms and less need for implant removal in patients treated with locking plates. Although both implants have high rates of prominence requiring removal, most studies support our findings that tension bands are more prominent than locking plates. Fixation has been reported to cause prominence requiring removal in 42% to 82% of patients with tension bands7-14 and 0% to 47% of patients with locking plates.1,8,17,18,20-22,28 It is important to note that many earlier studies either were conducted before the advent of precontoured locking plates or were not comparative.1,7,9-14,17,18,20-22,28 In one recent study, however, Edwards and colleagues19 surveyed 138 patients and found very similar implant removal rates: 63.6% for tension bands and 62.5% for locking plates. Nevertheless, implant removal rates for fixation of olecranon fractures remain high, regardless of implant used.
Our data did not reveal any difference in ROM or functional outcomes between patients who had and did not have implants removed. This suggests, first, that QDASH and MEPS may not be sensitive in identifying patients with implant prominence, as neither questionnaire incorporates implant prominence into its scoring, and, second, that implant removal does not significantly impair ROM. As a result, surgeons should consider asking patients specifically about symptoms of prominent implants once there is convincing evidence of union and counseling them about implant removal if appropriate.
To our knowledge, the differences in cost and operative time between tension-band and locking-plate fixation have not been previously reported. Our data suggest that the financial differences resulted mainly from implant charges; overall, tension-band fixation was roughly half the cost of locking-plate fixation. In addition, in patients who eventually had implants removed, the cost of implant removal was relatively small compared with the cost of the initial fixation in both cohorts. As a result, even if all patients in the tension-band cohort and no patients in the locking-plate cohort had implants removed, tension-band fixation and subsequent implant removal would still cost half as much as locking-plate fixation without implant removal. Moreover, fixation with a tension band took roughly 30 minutes less than fixation with a plate. Less time in the operating room likely contributed to the additional cost savings realized with tension-band fixation beyond those directly resulting from implant cost.
The strength of this study lies in the homogeneity of cohorts. Each cohort was matched primarily on age and secondarily on length of follow-up. All patients had closed, proximal, transverse fractures without comminution, and we excluded olecranon osteotomies as these represent an entity different from true fractures. Fractures with comminution or distal extension may represent more severe injuries, and functional scores, complications, hardware prominence, and operative time might have been affected by inclusion of these fractures. Further, there were no infections in either group to skew the rate of implant prominence or removal.
The weaknesses of the study lie in its limited sample sizes, retrospective design, and lack of long-term follow-up. Group size was limited by our attempts to create homogenous cohorts. As a result, some patients were not included as participants because of strict exclusion criteria. Most notably, we excluded any fracture not appropriate for tension-band fixation, as well as open fractures and osteotomies. Despite the retrospective nature of the study, all patients were examined by the investigators at final follow-up (minimum, 2 years) for the purpose of this study. It is possible that these functional results may not be sustained over the long term, as the risk for posttraumatic arthrosis in articular injuries builds with time. Although some patients may want to have implants removed later, all our study patients who had implants removed had them removed within 1 year, and all 20 patients were reached at minimum 2-year follow-up. Thus, it is unlikely but possible that some of the other study patients will elect to have implants removed.
1. Buijze G, Kloen P. Clinical evaluation of locking compression plate fixation for comminuted olecranon fractures. J Bone Joint Surg Am. 2009;91(10):
2416-2420.
2. Newman SD, Mauffrey C, Krikler S. Olecranon fractures. Injury. 2009;40(6):575-581.
3. Veillette CJ, Steinmann SP. Olecranon fractures. Orthop Clin North Am. 2008;39(2):229-236.
4. Baecher N, Edwards S. Olecranon fractures. J Hand Surg Am. 2013;38(3):593-604.
5. Hak DJ, Golladay GJ. Olecranon fractures: treatment options. J Am Acad Orthop Surg. 2000;8(4):266-275.
6. Busam ML, Esther RJ, Obremskey WT. Hardware removal: indications and expectations. J Am Acad Orthop Surg. 2006;14(2):113-120.
7. Chalidis BE, Sachinis NC, Samoladas EP, Dimitriou CG, Pournaras JD. Is tension band wiring technique the “gold standard” for the treatment of olecranon fractures? A long term functional outcome study. J Orthop Surg Res. 2008;3:9.
8. Hume MC, Wiss DA. Olecranon fractures: a clinical and radiographic comparison of tension-band wiring and plate fixation. Clin Orthop Relat Res. 1992;(285):229-235.
9. Karlsson MK, Hasserius R, Besjakov J, Karlsson C, Josefsson PO. Comparison of tension-band and figure-of-eight wiring techniques for treatment of olecranon fractures. J Shoulder Elbow Surg. 2002;11(4):377-382.
10. Lindenhovius AL, Brouwer KM, Doornberg JN, Ring DC, Kloen P. Long-term outcome of operatively treated fracture-dislocations of the olecranon. J Orthop Trauma. 2008;22(5):325-331.
11. Macko D, Szabo RM. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg Am. 1985;67(9):1396-1401.
12. Romero JM, Miran A, Jensen CH. Complications and re-operation rate after tension-band wiring of olecranon fractures. J Orthop Sci. 2000;5(4):318-320.
13. Rommens PM, Schneider RU, Reuter M. Functional results after operative treatment of olecranon fractures. Acta Chir Belg. 2004;104(2):191-197.
14. Villanueva P, Osorio F, Commessatti M, Sanchez-Sotelo J. Tension-band wiring for olecranon fractures: analysis of risk factors for failure. J Shoulder Elbow Surg. 2006;15(3):351-356.
15. Sahajpal D, Wright TW. Proximal ulna fractures. J Hand Surg Am. 2009;34(2):357-362.
16. Rouleau DM, Sandman E, van Riet R, Galatz LM. Management of fractures of the proximal ulna. J Am Acad Orthop Surg. 2013;21(3):149-160.
17. Anderson ML, Larson AN, Merten SM, Steinmann SP. Congruent elbow plate fixation of olecranon fractures. J Orthop Trauma. 2007;21(6):386-393.
18. Bailey CS, MacDermid J, Patterson SD, King GJ. Outcome of plate fixation of olecranon fractures. J Orthop Trauma. 2001;15(8):542-548.
19. Edwards SG, Cohen MS, Lattanza LL, et al. Surgeon perceptions and patient outcomes regarding proximal ulna fixation: a multicenter experience. J Shoulder Elbow Surg. 2012;21(12):1637-1643.
20. Munoz-Mahamud E, Fernandez-Valencia JA, Riba J. Plate osteosynthesis for severe olecranon fractures. J Orthop Surg. 2010;18(1):80-84.
21. Simpson NS, Goodman LA, Jupiter JB. Contoured LCDC plating of the proximal ulna. Injury. 1996;27(6):411-417.
22. Tejwani NC, Garnham IR, Wolinsky PR, Kummer FJ, Koval KJ. Posterior olecranon plating: biomechanical and clinical evaluation of a new operative technique. Bull Hosp Jt Dis. 2002-2003;61(1-2):27-31.
23. Morrey BF, An KN. Functional evaluation of the elbow. In: Morrey BF, Sanchez-Sotelo J, eds. The Elbow and Its Disorders. 4th ed. Philadelphia, PA: Elsevier; 2008:87-88.
24. Broberg MA, Morrey BF. The results of delayed excision of the radial head for fracture. J Bone Joint Surg Am. 1986;68(5):669-674.
25. Horne JG, Tanzer TL. Olecranon fractures: a review of 100 cases. J Trauma. 1981;21(6):469-472.
26. Hunsaker FG, Cioffi DA, Amadio PC, Wright JG, Caughlin B. The American Academy of Orthopaedic Surgeons outcomes instruments: normative values from the general population. J Bone Joint Surg Am. 2002;84(2):208-215.
27. Ikeda M, Fukushima Y, Kobayashi Y, Oka Y. Comminuted fractures of the olecranon. Management by bone graft from the iliac crest and multiple tension-band wiring. J Bone Joint Surg Br. 2001;83(6):805-808.
28. Erturer RE, Sever C, Sonmez MM, Ozcelik IB, Akman S, Ozturk I. Results of open reduction and plate osteosynthesis in comminuted fracture of the olecranon. J Shoulder Elbow Surg. 2011;20(3):449-454.
1. Buijze G, Kloen P. Clinical evaluation of locking compression plate fixation for comminuted olecranon fractures. J Bone Joint Surg Am. 2009;91(10):
2416-2420.
2. Newman SD, Mauffrey C, Krikler S. Olecranon fractures. Injury. 2009;40(6):575-581.
3. Veillette CJ, Steinmann SP. Olecranon fractures. Orthop Clin North Am. 2008;39(2):229-236.
4. Baecher N, Edwards S. Olecranon fractures. J Hand Surg Am. 2013;38(3):593-604.
5. Hak DJ, Golladay GJ. Olecranon fractures: treatment options. J Am Acad Orthop Surg. 2000;8(4):266-275.
6. Busam ML, Esther RJ, Obremskey WT. Hardware removal: indications and expectations. J Am Acad Orthop Surg. 2006;14(2):113-120.
7. Chalidis BE, Sachinis NC, Samoladas EP, Dimitriou CG, Pournaras JD. Is tension band wiring technique the “gold standard” for the treatment of olecranon fractures? A long term functional outcome study. J Orthop Surg Res. 2008;3:9.
8. Hume MC, Wiss DA. Olecranon fractures: a clinical and radiographic comparison of tension-band wiring and plate fixation. Clin Orthop Relat Res. 1992;(285):229-235.
9. Karlsson MK, Hasserius R, Besjakov J, Karlsson C, Josefsson PO. Comparison of tension-band and figure-of-eight wiring techniques for treatment of olecranon fractures. J Shoulder Elbow Surg. 2002;11(4):377-382.
10. Lindenhovius AL, Brouwer KM, Doornberg JN, Ring DC, Kloen P. Long-term outcome of operatively treated fracture-dislocations of the olecranon. J Orthop Trauma. 2008;22(5):325-331.
11. Macko D, Szabo RM. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg Am. 1985;67(9):1396-1401.
12. Romero JM, Miran A, Jensen CH. Complications and re-operation rate after tension-band wiring of olecranon fractures. J Orthop Sci. 2000;5(4):318-320.
13. Rommens PM, Schneider RU, Reuter M. Functional results after operative treatment of olecranon fractures. Acta Chir Belg. 2004;104(2):191-197.
14. Villanueva P, Osorio F, Commessatti M, Sanchez-Sotelo J. Tension-band wiring for olecranon fractures: analysis of risk factors for failure. J Shoulder Elbow Surg. 2006;15(3):351-356.
15. Sahajpal D, Wright TW. Proximal ulna fractures. J Hand Surg Am. 2009;34(2):357-362.
16. Rouleau DM, Sandman E, van Riet R, Galatz LM. Management of fractures of the proximal ulna. J Am Acad Orthop Surg. 2013;21(3):149-160.
17. Anderson ML, Larson AN, Merten SM, Steinmann SP. Congruent elbow plate fixation of olecranon fractures. J Orthop Trauma. 2007;21(6):386-393.
18. Bailey CS, MacDermid J, Patterson SD, King GJ. Outcome of plate fixation of olecranon fractures. J Orthop Trauma. 2001;15(8):542-548.
19. Edwards SG, Cohen MS, Lattanza LL, et al. Surgeon perceptions and patient outcomes regarding proximal ulna fixation: a multicenter experience. J Shoulder Elbow Surg. 2012;21(12):1637-1643.
20. Munoz-Mahamud E, Fernandez-Valencia JA, Riba J. Plate osteosynthesis for severe olecranon fractures. J Orthop Surg. 2010;18(1):80-84.
21. Simpson NS, Goodman LA, Jupiter JB. Contoured LCDC plating of the proximal ulna. Injury. 1996;27(6):411-417.
22. Tejwani NC, Garnham IR, Wolinsky PR, Kummer FJ, Koval KJ. Posterior olecranon plating: biomechanical and clinical evaluation of a new operative technique. Bull Hosp Jt Dis. 2002-2003;61(1-2):27-31.
23. Morrey BF, An KN. Functional evaluation of the elbow. In: Morrey BF, Sanchez-Sotelo J, eds. The Elbow and Its Disorders. 4th ed. Philadelphia, PA: Elsevier; 2008:87-88.
24. Broberg MA, Morrey BF. The results of delayed excision of the radial head for fracture. J Bone Joint Surg Am. 1986;68(5):669-674.
25. Horne JG, Tanzer TL. Olecranon fractures: a review of 100 cases. J Trauma. 1981;21(6):469-472.
26. Hunsaker FG, Cioffi DA, Amadio PC, Wright JG, Caughlin B. The American Academy of Orthopaedic Surgeons outcomes instruments: normative values from the general population. J Bone Joint Surg Am. 2002;84(2):208-215.
27. Ikeda M, Fukushima Y, Kobayashi Y, Oka Y. Comminuted fractures of the olecranon. Management by bone graft from the iliac crest and multiple tension-band wiring. J Bone Joint Surg Br. 2001;83(6):805-808.
28. Erturer RE, Sever C, Sonmez MM, Ozcelik IB, Akman S, Ozturk I. Results of open reduction and plate osteosynthesis in comminuted fracture of the olecranon. J Shoulder Elbow Surg. 2011;20(3):449-454.
The Effect of Humeral Rotation on Elbow Range-of-Motion Measurements
Elbow motion is crucial for activities of daily living and full function of the upper extremity.1 Measuring the elbow flexion arc accurately and consistently is an important part of the physical examination of patients with elbow pathology. Orthopedic surgeons rely on these measurements to follow patients over time, and they often base their treatment decisions on the range and progression/regression of motion arc.
In the clinical setting, elbow range of motion (ROM) is commonly measured with a handheld goniometer.2,3 The literature also suggests that goniometric measurements are highly reliable in the clinical setting and that intrarater reliability of elbow ROM measurements is high.2-4 Despite the routine use and clinical importance of flexion arc assessment, there is no universal recommendation regarding optimal measurement position. Textbooks and journal articles commonly do not specify arm position at time of elbow ROM measurements,5-8 and a literature review found no studies directly addressing this issue.
From a biomechanical standpoint, humeral rotation is often affected by forearm pronosupination position. Although forearm pronosupination is a product of the motion at the radioulnar joints, forearm position during elbow flexion arc measurement can influence the relationship of the distal humeral intercondylar axis to the plane of measurement. Full forearm supination rotates the distal humeral intercondylar axis externally to a position parallel to the floor and in line with the plane of measurement. Humeral rotation with the forearm in neutral pronosupination places the humeral condyles internally rotated relative to the floor. Therefore, for the purposes of this study, we defined full humeral external rotation and true plane of ulnohumeral motion as full forearm supination, and relative humeral and ulnohumeral joint internal rotation as neutral pronosupination.
Because of the potential for elbow ROM measurement changes caused by differences in the motion plane in which measurements are taken, some have advocated taking flexion arc measurements with the arm in full supination to allow measurements to be taken in the true plane of motion. We hypothesized that elbow flexion arc measurements taken with the forearm in neutral rotation would underestimate the extent of elbow flexion contractures compared with measurements taken in full supination.
Materials and Methods
This study received institutional review board approval. Eighty-four patients who presented with elbow dysfunction to a single shoulder and elbow orthopedic surgeon enrolled in the study. Skeletally immature patients and patients with a fracture or other disorder that prohibited elbow ROM were excluded. A standard goniometer was used to measure elbow flexion and extension with the humerus in 2 positions: full external rotation and neutral rotation.
All goniometer measurements were made by the same surgeon (to eliminate interobserver reliability error) using a standardized technique with the patient sitting upright. The goniometer was positioned laterally with its center of rotation over the lateral epicondyle, aligned proximally with the humeral head and distally with the center of the wrist. Measurements were obtained sequentially with the hand in both positions. For external rotation measurements, the patient’s arm was fully supinated to bring the humeral condyles parallel to the floor. For neutral positioning, the patient’s arm was placed in the “thumb-up” position with the hand perpendicular to the horizontal axis of the floor (Figures 1A–1C).
Data collected included demographics, diagnosis, hand dominance, affected side, and elbow ROM measurements with the hand in the 2 positions. These data were compiled and analyzed for all patients and then stratified into 3 groups by extent of elbow flexion contracture in the supinated position (group 1, hyperextension; group 2, 0°-29° elbow extension; group 3, ≥30° flexion contracture).
Statistically, paired t tests were used to identify differences between the 2 elbow ROM measurement methods. P < .05 was considered significant.
Results
Eighty-four (44 male, 40 female) consecutive patients (85 elbows) met the inclusion and exclusion criteria. Mean age was 51 years (range, 19-84 years). Seventy-six patients were right-handed, 7 were left-handed, and dominance was unknown in 1 patient. The right elbow was affected in 45 patients, the left in 38, and both in 1 patient. There were 25 different diagnoses, the most common of which was lateral epicondylitis; 7 patients had multiple disorders (Table).
The first set of data, elbow ROM measurements, was taken with all 84 patients analyzed as a single group. In neutral humeral rotation, mean elbow extension was 14° (range, 10°-72°), and mean elbow flexion was 134° (range, 72°-145°). In external rotation, mean elbow extension was 20° (range, 12°-87°), and mean elbow flexion was 134° (range, 72°-145°). For the group, mean absolute difference in elbow extension was 8° (range, 0°-30°; P < .0001); there was no difference between external rotation and neutral rotation in flexion (Figure 2).
The data were reanalyzed after being stratified into 3 groups based on extent of elbow flexion contracture measured in supination.
The 9 elbows in group 1 (hyperextension) had mean extension of –2° (range, 10°-2°) and mean flexion of 141° (range, 130°-145°) in the neutral position. In external rotation, mean extension was –9° (range, –12° to –1°), and mean flexion was 141° (range, 130°-145°). When the 2 measurement positions were compared, group 1 had mean elbow ROM differences of –6° (range, –14° to 0°; P = .0033) for elbow extension and 0° for elbow flexion (Figure 3A).
The 50 elbows in group 2 (0°-29° flexion contracture) had mean extension of 7° (range, 0°-20°) and mean flexion of 138° (range, 100°-145°) in the neutral position. In external rotation, mean extension was 13° (range, 0°-26°), and mean flexion was 138° (range, 100°-145°). Mean difference between neutral and external rotation measurements was 6° (range, 0°-20°; P < .0001) in extension and 0° in flexion (Figure 3B).
The 26 elbows in group 3 (≥30° flexion contracture) had mean extension of 33° (range, 0°-72°) and mean flexion of 124° (range, 72°-145°) in the neutral position. In external rotation, mean extension was 45° (range, 30°-87°), and mean flexion was 124° (range, 72°-145°). Mean difference between neutral and external rotation measurements was 12° (range, 0°-30°; P < .0001) in extension and 0° in flexion (Figure 3C).
Discussion
Elbow flexion arc measurements are crucial for patient outcomes and activities of daily living. Commonly cited as functional ROM, the 30°-to-130° flexion arc often is used to guide clinical decisions in patients with elbow disorders.1 However, our data indicate that humeral position can alter elbow ROM measurements. Specifically, because of neutral forearm pronosupination, measurements made with the humerus in neutral rotation underestimate both the extent of elbow hyperextension and the degree of flexion contracture (Figures 4A, 4B). The more severe the flexion contracture, the more values are altered by measurements taken in this position. The same does not apply for elbow flexion measurements, as varying humeral rotation did not significantly affect those values.
Our results indicate that patients evaluated with the arm in neutral humeral rotation had flexion contractures underestimated by a mean of 8°, while there was a negligible difference in flexion measurements. Stratifying our data into 3 groups, we found that neutral humeral rotation kept elbow extension measurements closer to 0° for patients with both hyperextension and contractures. With increasing severity of flexion contractures in groups 2 and 3, the measurement errors were magnified. The differences in extension measurement values between these 2 groups based on humeral rotation increased more than 4°—an indication that, as flexion contracture severity increases, so does the degree of measurement error when elbow extension is measured with the humerus in neutral rotation rather than external rotation.
Our literature review found no studies on ROM value differences based on position of humeral rotation. Most texts, in their descriptions of elbow ROM and biomechanics, make no reference to position of pronosupination at time of flexion arc measurement.5-8 Although many elbow authorities recommend taking elbow ROM measurements in full external rotation, we found no corroborating evidence.
Other investigators have evaluated the reliability of goniometer measurements.2,3 Rothstein and colleagues3 concluded that elbow and knee goniometric measurements are highly reliable in the clinical setting when taken by the same person. In particular, intratester reliability for elbow extension measurements was high. Armstrong and colleagues2 specifically examined intratester, intertester, and interdevice reliability and found that intratester reliability was much higher than intertester reliability for universal goniometry. In our study, all patients were measured with the same technique by the same orthopedic surgeon to eliminate any intertester reliability error. Armstrong and colleagues2 also found that intratester changes vis-a-vis extension measurements are meaningful when goniometric differences are more than 7°. In our study, the difference in extension measurements between the 2 humeral positions averaged 8° overall and 12° in group 3. This suggests that the data reported here reflect a true difference dependent on humeral rotation and are not a result of goniometer intratester variability.
Other studies have examined measurement devices other than the standard universal goniometer. Cleffken and colleagues4 found that the electronic digital inclinometer was reliable for elbow ROM measurements. Blonna and colleagues9 used digital photography–based goniometry to measure patient outcomes without doctor–patient contact at tertiary-care centers and found it to be more accurate and reliable than clinical goniometry in measuring elbow flexion and extension. Chapleau and colleagues10 compared the validity of goniometric elbow measurements in radiographic methods and concluded that the maximal error of goniometric measurements in extension was 10.3°. However, they also found high intraclass correlation coefficients for goniometric measurements. With the accepted clinical reliability of universal goniometry,2-4,10 we believe it to be the best clinical tool for this study because of its availability, minimal cost, and ease of use.
In the clinical setting, elbow flexion arc measurements are a major factor in treatment decisions and often dictate whether to proceed with operative interventions such as capsular release. In addition, ROM measurements are crucial in determining the success of treatments and the progression of disease. Erroneous elbow extension measurements can have significant consequences if they falsely indicate functional ROM when taken in neutral position. This is particularly true for patients with elbow flexion contractures of more than 30°, in whom differences in humeral rotation resulted in about 12° of variance between measured values. For instance, a patient with a true 40° flexion contracture in the externally rotated position could be determined to have functional ROM based on measurements made in the neutral position.
Limitations of this study include those involving goniometer reliability and intraobserver variability (already described) and the validity of goniometer measurements compared with radiographic measurements.
Conclusion
Because elbow goniometer extension measurements taken in neutral humeral rotation underestimate both the degree of elbow hyperextension and the degree of elbow flexion contracture, we recommend taking elbow flexion arc measurements in the true plane of motion, with the humerus externally rotated by fully supinating the forearm, such that the distal humeral condyles are parallel to the floor.
1. Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63(6):872-877.
2. Armstrong AD, MacDermid JC, Chinchalkar S, Stevens RS, King GJ. Reliability of range-of-motion measurement in the elbow and forearm. J Shoulder Elbow Surg. 1998;7(6):573-580.
3. Rothstein JM, Miller PJ, Roettger RF. Goniometric reliability in a clinical setting. Elbow and knee measurements. Phys Ther. 1983;63(10):1611-1615.
4. Cleffken B, van Breukelen G, van Mameren H, Brink P, Olde Damink S. Test–retest reproducibility of elbow goniometric measurements in a rigid double-blinded protocol: intervals for distinguishing between measurement error and clinical change. J Shoulder Elbow Surg. 2007;16(6):788-794.
5. Hoppenfeld S. Physical Examination of the Spine and Extremities. Englewood Cliffs, NJ: Prentice-Hall; 1976.
6. Miller RM 3rd, Azar FM, Throckmorton TW. Shoulder and elbow injuries. In: Canale S, Beaty J, eds. Campbell’s Operative Orthopaedics. 12th ed. Philadelphia, PA: Mosby Elsevier; 2013:2241-2253.
7. Ring D. Elbow fractures and dislocations. In: Bucholz R, Heckman J, Court-Brown C, eds. Rockwood and Green’s Fractures in Adults. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:901-991.
8. Katolik LI, Cohen MS. Lateral columnar release for extracapsular elbow contracture. In: Wiesel S, ed. Operative Techniques in Orthopaedic Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2011:3406-3407.
9. Blonna D, Zarkadas PC, Fitzsimmons JS, O’Driscoll SW. Validation of a photography-based goniometry method for measuring joint range of motion. J Shoulder Elbow Surg. 2012;21(1):29-35.
10. Chapleau J, Canet F, Petit Y, Laflamme G, Rouleau D. Validity of elbow goniometer measurements. Comparative study with a radiographic method. Clin Orthop. 2001;(469):3134-3140.
Elbow motion is crucial for activities of daily living and full function of the upper extremity.1 Measuring the elbow flexion arc accurately and consistently is an important part of the physical examination of patients with elbow pathology. Orthopedic surgeons rely on these measurements to follow patients over time, and they often base their treatment decisions on the range and progression/regression of motion arc.
In the clinical setting, elbow range of motion (ROM) is commonly measured with a handheld goniometer.2,3 The literature also suggests that goniometric measurements are highly reliable in the clinical setting and that intrarater reliability of elbow ROM measurements is high.2-4 Despite the routine use and clinical importance of flexion arc assessment, there is no universal recommendation regarding optimal measurement position. Textbooks and journal articles commonly do not specify arm position at time of elbow ROM measurements,5-8 and a literature review found no studies directly addressing this issue.
From a biomechanical standpoint, humeral rotation is often affected by forearm pronosupination position. Although forearm pronosupination is a product of the motion at the radioulnar joints, forearm position during elbow flexion arc measurement can influence the relationship of the distal humeral intercondylar axis to the plane of measurement. Full forearm supination rotates the distal humeral intercondylar axis externally to a position parallel to the floor and in line with the plane of measurement. Humeral rotation with the forearm in neutral pronosupination places the humeral condyles internally rotated relative to the floor. Therefore, for the purposes of this study, we defined full humeral external rotation and true plane of ulnohumeral motion as full forearm supination, and relative humeral and ulnohumeral joint internal rotation as neutral pronosupination.
Because of the potential for elbow ROM measurement changes caused by differences in the motion plane in which measurements are taken, some have advocated taking flexion arc measurements with the arm in full supination to allow measurements to be taken in the true plane of motion. We hypothesized that elbow flexion arc measurements taken with the forearm in neutral rotation would underestimate the extent of elbow flexion contractures compared with measurements taken in full supination.
Materials and Methods
This study received institutional review board approval. Eighty-four patients who presented with elbow dysfunction to a single shoulder and elbow orthopedic surgeon enrolled in the study. Skeletally immature patients and patients with a fracture or other disorder that prohibited elbow ROM were excluded. A standard goniometer was used to measure elbow flexion and extension with the humerus in 2 positions: full external rotation and neutral rotation.
All goniometer measurements were made by the same surgeon (to eliminate interobserver reliability error) using a standardized technique with the patient sitting upright. The goniometer was positioned laterally with its center of rotation over the lateral epicondyle, aligned proximally with the humeral head and distally with the center of the wrist. Measurements were obtained sequentially with the hand in both positions. For external rotation measurements, the patient’s arm was fully supinated to bring the humeral condyles parallel to the floor. For neutral positioning, the patient’s arm was placed in the “thumb-up” position with the hand perpendicular to the horizontal axis of the floor (Figures 1A–1C).
Data collected included demographics, diagnosis, hand dominance, affected side, and elbow ROM measurements with the hand in the 2 positions. These data were compiled and analyzed for all patients and then stratified into 3 groups by extent of elbow flexion contracture in the supinated position (group 1, hyperextension; group 2, 0°-29° elbow extension; group 3, ≥30° flexion contracture).
Statistically, paired t tests were used to identify differences between the 2 elbow ROM measurement methods. P < .05 was considered significant.
Results
Eighty-four (44 male, 40 female) consecutive patients (85 elbows) met the inclusion and exclusion criteria. Mean age was 51 years (range, 19-84 years). Seventy-six patients were right-handed, 7 were left-handed, and dominance was unknown in 1 patient. The right elbow was affected in 45 patients, the left in 38, and both in 1 patient. There were 25 different diagnoses, the most common of which was lateral epicondylitis; 7 patients had multiple disorders (Table).
The first set of data, elbow ROM measurements, was taken with all 84 patients analyzed as a single group. In neutral humeral rotation, mean elbow extension was 14° (range, 10°-72°), and mean elbow flexion was 134° (range, 72°-145°). In external rotation, mean elbow extension was 20° (range, 12°-87°), and mean elbow flexion was 134° (range, 72°-145°). For the group, mean absolute difference in elbow extension was 8° (range, 0°-30°; P < .0001); there was no difference between external rotation and neutral rotation in flexion (Figure 2).
The data were reanalyzed after being stratified into 3 groups based on extent of elbow flexion contracture measured in supination.
The 9 elbows in group 1 (hyperextension) had mean extension of –2° (range, 10°-2°) and mean flexion of 141° (range, 130°-145°) in the neutral position. In external rotation, mean extension was –9° (range, –12° to –1°), and mean flexion was 141° (range, 130°-145°). When the 2 measurement positions were compared, group 1 had mean elbow ROM differences of –6° (range, –14° to 0°; P = .0033) for elbow extension and 0° for elbow flexion (Figure 3A).
The 50 elbows in group 2 (0°-29° flexion contracture) had mean extension of 7° (range, 0°-20°) and mean flexion of 138° (range, 100°-145°) in the neutral position. In external rotation, mean extension was 13° (range, 0°-26°), and mean flexion was 138° (range, 100°-145°). Mean difference between neutral and external rotation measurements was 6° (range, 0°-20°; P < .0001) in extension and 0° in flexion (Figure 3B).
The 26 elbows in group 3 (≥30° flexion contracture) had mean extension of 33° (range, 0°-72°) and mean flexion of 124° (range, 72°-145°) in the neutral position. In external rotation, mean extension was 45° (range, 30°-87°), and mean flexion was 124° (range, 72°-145°). Mean difference between neutral and external rotation measurements was 12° (range, 0°-30°; P < .0001) in extension and 0° in flexion (Figure 3C).
Discussion
Elbow flexion arc measurements are crucial for patient outcomes and activities of daily living. Commonly cited as functional ROM, the 30°-to-130° flexion arc often is used to guide clinical decisions in patients with elbow disorders.1 However, our data indicate that humeral position can alter elbow ROM measurements. Specifically, because of neutral forearm pronosupination, measurements made with the humerus in neutral rotation underestimate both the extent of elbow hyperextension and the degree of flexion contracture (Figures 4A, 4B). The more severe the flexion contracture, the more values are altered by measurements taken in this position. The same does not apply for elbow flexion measurements, as varying humeral rotation did not significantly affect those values.
Our results indicate that patients evaluated with the arm in neutral humeral rotation had flexion contractures underestimated by a mean of 8°, while there was a negligible difference in flexion measurements. Stratifying our data into 3 groups, we found that neutral humeral rotation kept elbow extension measurements closer to 0° for patients with both hyperextension and contractures. With increasing severity of flexion contractures in groups 2 and 3, the measurement errors were magnified. The differences in extension measurement values between these 2 groups based on humeral rotation increased more than 4°—an indication that, as flexion contracture severity increases, so does the degree of measurement error when elbow extension is measured with the humerus in neutral rotation rather than external rotation.
Our literature review found no studies on ROM value differences based on position of humeral rotation. Most texts, in their descriptions of elbow ROM and biomechanics, make no reference to position of pronosupination at time of flexion arc measurement.5-8 Although many elbow authorities recommend taking elbow ROM measurements in full external rotation, we found no corroborating evidence.
Other investigators have evaluated the reliability of goniometer measurements.2,3 Rothstein and colleagues3 concluded that elbow and knee goniometric measurements are highly reliable in the clinical setting when taken by the same person. In particular, intratester reliability for elbow extension measurements was high. Armstrong and colleagues2 specifically examined intratester, intertester, and interdevice reliability and found that intratester reliability was much higher than intertester reliability for universal goniometry. In our study, all patients were measured with the same technique by the same orthopedic surgeon to eliminate any intertester reliability error. Armstrong and colleagues2 also found that intratester changes vis-a-vis extension measurements are meaningful when goniometric differences are more than 7°. In our study, the difference in extension measurements between the 2 humeral positions averaged 8° overall and 12° in group 3. This suggests that the data reported here reflect a true difference dependent on humeral rotation and are not a result of goniometer intratester variability.
Other studies have examined measurement devices other than the standard universal goniometer. Cleffken and colleagues4 found that the electronic digital inclinometer was reliable for elbow ROM measurements. Blonna and colleagues9 used digital photography–based goniometry to measure patient outcomes without doctor–patient contact at tertiary-care centers and found it to be more accurate and reliable than clinical goniometry in measuring elbow flexion and extension. Chapleau and colleagues10 compared the validity of goniometric elbow measurements in radiographic methods and concluded that the maximal error of goniometric measurements in extension was 10.3°. However, they also found high intraclass correlation coefficients for goniometric measurements. With the accepted clinical reliability of universal goniometry,2-4,10 we believe it to be the best clinical tool for this study because of its availability, minimal cost, and ease of use.
In the clinical setting, elbow flexion arc measurements are a major factor in treatment decisions and often dictate whether to proceed with operative interventions such as capsular release. In addition, ROM measurements are crucial in determining the success of treatments and the progression of disease. Erroneous elbow extension measurements can have significant consequences if they falsely indicate functional ROM when taken in neutral position. This is particularly true for patients with elbow flexion contractures of more than 30°, in whom differences in humeral rotation resulted in about 12° of variance between measured values. For instance, a patient with a true 40° flexion contracture in the externally rotated position could be determined to have functional ROM based on measurements made in the neutral position.
Limitations of this study include those involving goniometer reliability and intraobserver variability (already described) and the validity of goniometer measurements compared with radiographic measurements.
Conclusion
Because elbow goniometer extension measurements taken in neutral humeral rotation underestimate both the degree of elbow hyperextension and the degree of elbow flexion contracture, we recommend taking elbow flexion arc measurements in the true plane of motion, with the humerus externally rotated by fully supinating the forearm, such that the distal humeral condyles are parallel to the floor.
Elbow motion is crucial for activities of daily living and full function of the upper extremity.1 Measuring the elbow flexion arc accurately and consistently is an important part of the physical examination of patients with elbow pathology. Orthopedic surgeons rely on these measurements to follow patients over time, and they often base their treatment decisions on the range and progression/regression of motion arc.
In the clinical setting, elbow range of motion (ROM) is commonly measured with a handheld goniometer.2,3 The literature also suggests that goniometric measurements are highly reliable in the clinical setting and that intrarater reliability of elbow ROM measurements is high.2-4 Despite the routine use and clinical importance of flexion arc assessment, there is no universal recommendation regarding optimal measurement position. Textbooks and journal articles commonly do not specify arm position at time of elbow ROM measurements,5-8 and a literature review found no studies directly addressing this issue.
From a biomechanical standpoint, humeral rotation is often affected by forearm pronosupination position. Although forearm pronosupination is a product of the motion at the radioulnar joints, forearm position during elbow flexion arc measurement can influence the relationship of the distal humeral intercondylar axis to the plane of measurement. Full forearm supination rotates the distal humeral intercondylar axis externally to a position parallel to the floor and in line with the plane of measurement. Humeral rotation with the forearm in neutral pronosupination places the humeral condyles internally rotated relative to the floor. Therefore, for the purposes of this study, we defined full humeral external rotation and true plane of ulnohumeral motion as full forearm supination, and relative humeral and ulnohumeral joint internal rotation as neutral pronosupination.
Because of the potential for elbow ROM measurement changes caused by differences in the motion plane in which measurements are taken, some have advocated taking flexion arc measurements with the arm in full supination to allow measurements to be taken in the true plane of motion. We hypothesized that elbow flexion arc measurements taken with the forearm in neutral rotation would underestimate the extent of elbow flexion contractures compared with measurements taken in full supination.
Materials and Methods
This study received institutional review board approval. Eighty-four patients who presented with elbow dysfunction to a single shoulder and elbow orthopedic surgeon enrolled in the study. Skeletally immature patients and patients with a fracture or other disorder that prohibited elbow ROM were excluded. A standard goniometer was used to measure elbow flexion and extension with the humerus in 2 positions: full external rotation and neutral rotation.
All goniometer measurements were made by the same surgeon (to eliminate interobserver reliability error) using a standardized technique with the patient sitting upright. The goniometer was positioned laterally with its center of rotation over the lateral epicondyle, aligned proximally with the humeral head and distally with the center of the wrist. Measurements were obtained sequentially with the hand in both positions. For external rotation measurements, the patient’s arm was fully supinated to bring the humeral condyles parallel to the floor. For neutral positioning, the patient’s arm was placed in the “thumb-up” position with the hand perpendicular to the horizontal axis of the floor (Figures 1A–1C).
Data collected included demographics, diagnosis, hand dominance, affected side, and elbow ROM measurements with the hand in the 2 positions. These data were compiled and analyzed for all patients and then stratified into 3 groups by extent of elbow flexion contracture in the supinated position (group 1, hyperextension; group 2, 0°-29° elbow extension; group 3, ≥30° flexion contracture).
Statistically, paired t tests were used to identify differences between the 2 elbow ROM measurement methods. P < .05 was considered significant.
Results
Eighty-four (44 male, 40 female) consecutive patients (85 elbows) met the inclusion and exclusion criteria. Mean age was 51 years (range, 19-84 years). Seventy-six patients were right-handed, 7 were left-handed, and dominance was unknown in 1 patient. The right elbow was affected in 45 patients, the left in 38, and both in 1 patient. There were 25 different diagnoses, the most common of which was lateral epicondylitis; 7 patients had multiple disorders (Table).
The first set of data, elbow ROM measurements, was taken with all 84 patients analyzed as a single group. In neutral humeral rotation, mean elbow extension was 14° (range, 10°-72°), and mean elbow flexion was 134° (range, 72°-145°). In external rotation, mean elbow extension was 20° (range, 12°-87°), and mean elbow flexion was 134° (range, 72°-145°). For the group, mean absolute difference in elbow extension was 8° (range, 0°-30°; P < .0001); there was no difference between external rotation and neutral rotation in flexion (Figure 2).
The data were reanalyzed after being stratified into 3 groups based on extent of elbow flexion contracture measured in supination.
The 9 elbows in group 1 (hyperextension) had mean extension of –2° (range, 10°-2°) and mean flexion of 141° (range, 130°-145°) in the neutral position. In external rotation, mean extension was –9° (range, –12° to –1°), and mean flexion was 141° (range, 130°-145°). When the 2 measurement positions were compared, group 1 had mean elbow ROM differences of –6° (range, –14° to 0°; P = .0033) for elbow extension and 0° for elbow flexion (Figure 3A).
The 50 elbows in group 2 (0°-29° flexion contracture) had mean extension of 7° (range, 0°-20°) and mean flexion of 138° (range, 100°-145°) in the neutral position. In external rotation, mean extension was 13° (range, 0°-26°), and mean flexion was 138° (range, 100°-145°). Mean difference between neutral and external rotation measurements was 6° (range, 0°-20°; P < .0001) in extension and 0° in flexion (Figure 3B).
The 26 elbows in group 3 (≥30° flexion contracture) had mean extension of 33° (range, 0°-72°) and mean flexion of 124° (range, 72°-145°) in the neutral position. In external rotation, mean extension was 45° (range, 30°-87°), and mean flexion was 124° (range, 72°-145°). Mean difference between neutral and external rotation measurements was 12° (range, 0°-30°; P < .0001) in extension and 0° in flexion (Figure 3C).
Discussion
Elbow flexion arc measurements are crucial for patient outcomes and activities of daily living. Commonly cited as functional ROM, the 30°-to-130° flexion arc often is used to guide clinical decisions in patients with elbow disorders.1 However, our data indicate that humeral position can alter elbow ROM measurements. Specifically, because of neutral forearm pronosupination, measurements made with the humerus in neutral rotation underestimate both the extent of elbow hyperextension and the degree of flexion contracture (Figures 4A, 4B). The more severe the flexion contracture, the more values are altered by measurements taken in this position. The same does not apply for elbow flexion measurements, as varying humeral rotation did not significantly affect those values.
Our results indicate that patients evaluated with the arm in neutral humeral rotation had flexion contractures underestimated by a mean of 8°, while there was a negligible difference in flexion measurements. Stratifying our data into 3 groups, we found that neutral humeral rotation kept elbow extension measurements closer to 0° for patients with both hyperextension and contractures. With increasing severity of flexion contractures in groups 2 and 3, the measurement errors were magnified. The differences in extension measurement values between these 2 groups based on humeral rotation increased more than 4°—an indication that, as flexion contracture severity increases, so does the degree of measurement error when elbow extension is measured with the humerus in neutral rotation rather than external rotation.
Our literature review found no studies on ROM value differences based on position of humeral rotation. Most texts, in their descriptions of elbow ROM and biomechanics, make no reference to position of pronosupination at time of flexion arc measurement.5-8 Although many elbow authorities recommend taking elbow ROM measurements in full external rotation, we found no corroborating evidence.
Other investigators have evaluated the reliability of goniometer measurements.2,3 Rothstein and colleagues3 concluded that elbow and knee goniometric measurements are highly reliable in the clinical setting when taken by the same person. In particular, intratester reliability for elbow extension measurements was high. Armstrong and colleagues2 specifically examined intratester, intertester, and interdevice reliability and found that intratester reliability was much higher than intertester reliability for universal goniometry. In our study, all patients were measured with the same technique by the same orthopedic surgeon to eliminate any intertester reliability error. Armstrong and colleagues2 also found that intratester changes vis-a-vis extension measurements are meaningful when goniometric differences are more than 7°. In our study, the difference in extension measurements between the 2 humeral positions averaged 8° overall and 12° in group 3. This suggests that the data reported here reflect a true difference dependent on humeral rotation and are not a result of goniometer intratester variability.
Other studies have examined measurement devices other than the standard universal goniometer. Cleffken and colleagues4 found that the electronic digital inclinometer was reliable for elbow ROM measurements. Blonna and colleagues9 used digital photography–based goniometry to measure patient outcomes without doctor–patient contact at tertiary-care centers and found it to be more accurate and reliable than clinical goniometry in measuring elbow flexion and extension. Chapleau and colleagues10 compared the validity of goniometric elbow measurements in radiographic methods and concluded that the maximal error of goniometric measurements in extension was 10.3°. However, they also found high intraclass correlation coefficients for goniometric measurements. With the accepted clinical reliability of universal goniometry,2-4,10 we believe it to be the best clinical tool for this study because of its availability, minimal cost, and ease of use.
In the clinical setting, elbow flexion arc measurements are a major factor in treatment decisions and often dictate whether to proceed with operative interventions such as capsular release. In addition, ROM measurements are crucial in determining the success of treatments and the progression of disease. Erroneous elbow extension measurements can have significant consequences if they falsely indicate functional ROM when taken in neutral position. This is particularly true for patients with elbow flexion contractures of more than 30°, in whom differences in humeral rotation resulted in about 12° of variance between measured values. For instance, a patient with a true 40° flexion contracture in the externally rotated position could be determined to have functional ROM based on measurements made in the neutral position.
Limitations of this study include those involving goniometer reliability and intraobserver variability (already described) and the validity of goniometer measurements compared with radiographic measurements.
Conclusion
Because elbow goniometer extension measurements taken in neutral humeral rotation underestimate both the degree of elbow hyperextension and the degree of elbow flexion contracture, we recommend taking elbow flexion arc measurements in the true plane of motion, with the humerus externally rotated by fully supinating the forearm, such that the distal humeral condyles are parallel to the floor.
1. Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63(6):872-877.
2. Armstrong AD, MacDermid JC, Chinchalkar S, Stevens RS, King GJ. Reliability of range-of-motion measurement in the elbow and forearm. J Shoulder Elbow Surg. 1998;7(6):573-580.
3. Rothstein JM, Miller PJ, Roettger RF. Goniometric reliability in a clinical setting. Elbow and knee measurements. Phys Ther. 1983;63(10):1611-1615.
4. Cleffken B, van Breukelen G, van Mameren H, Brink P, Olde Damink S. Test–retest reproducibility of elbow goniometric measurements in a rigid double-blinded protocol: intervals for distinguishing between measurement error and clinical change. J Shoulder Elbow Surg. 2007;16(6):788-794.
5. Hoppenfeld S. Physical Examination of the Spine and Extremities. Englewood Cliffs, NJ: Prentice-Hall; 1976.
6. Miller RM 3rd, Azar FM, Throckmorton TW. Shoulder and elbow injuries. In: Canale S, Beaty J, eds. Campbell’s Operative Orthopaedics. 12th ed. Philadelphia, PA: Mosby Elsevier; 2013:2241-2253.
7. Ring D. Elbow fractures and dislocations. In: Bucholz R, Heckman J, Court-Brown C, eds. Rockwood and Green’s Fractures in Adults. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:901-991.
8. Katolik LI, Cohen MS. Lateral columnar release for extracapsular elbow contracture. In: Wiesel S, ed. Operative Techniques in Orthopaedic Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2011:3406-3407.
9. Blonna D, Zarkadas PC, Fitzsimmons JS, O’Driscoll SW. Validation of a photography-based goniometry method for measuring joint range of motion. J Shoulder Elbow Surg. 2012;21(1):29-35.
10. Chapleau J, Canet F, Petit Y, Laflamme G, Rouleau D. Validity of elbow goniometer measurements. Comparative study with a radiographic method. Clin Orthop. 2001;(469):3134-3140.
1. Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63(6):872-877.
2. Armstrong AD, MacDermid JC, Chinchalkar S, Stevens RS, King GJ. Reliability of range-of-motion measurement in the elbow and forearm. J Shoulder Elbow Surg. 1998;7(6):573-580.
3. Rothstein JM, Miller PJ, Roettger RF. Goniometric reliability in a clinical setting. Elbow and knee measurements. Phys Ther. 1983;63(10):1611-1615.
4. Cleffken B, van Breukelen G, van Mameren H, Brink P, Olde Damink S. Test–retest reproducibility of elbow goniometric measurements in a rigid double-blinded protocol: intervals for distinguishing between measurement error and clinical change. J Shoulder Elbow Surg. 2007;16(6):788-794.
5. Hoppenfeld S. Physical Examination of the Spine and Extremities. Englewood Cliffs, NJ: Prentice-Hall; 1976.
6. Miller RM 3rd, Azar FM, Throckmorton TW. Shoulder and elbow injuries. In: Canale S, Beaty J, eds. Campbell’s Operative Orthopaedics. 12th ed. Philadelphia, PA: Mosby Elsevier; 2013:2241-2253.
7. Ring D. Elbow fractures and dislocations. In: Bucholz R, Heckman J, Court-Brown C, eds. Rockwood and Green’s Fractures in Adults. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:901-991.
8. Katolik LI, Cohen MS. Lateral columnar release for extracapsular elbow contracture. In: Wiesel S, ed. Operative Techniques in Orthopaedic Surgery. Philadelphia, PA: Lippincott Williams & Wilkins; 2011:3406-3407.
9. Blonna D, Zarkadas PC, Fitzsimmons JS, O’Driscoll SW. Validation of a photography-based goniometry method for measuring joint range of motion. J Shoulder Elbow Surg. 2012;21(1):29-35.
10. Chapleau J, Canet F, Petit Y, Laflamme G, Rouleau D. Validity of elbow goniometer measurements. Comparative study with a radiographic method. Clin Orthop. 2001;(469):3134-3140.