User login
Rethinking Resident Supervision
Close supervision of residents potentially leads to fewer errors, lower patient mortality, and improved quality of care.19 An Institute of Medicine (IOM) report3 recommended improving supervision through more frequent consultations between residents and their supervisors. Although current Accreditation Council for Graduate Medical Education (ACGME) guidelines also recommend that attending physicians (attendings) supervise residents, detailed guidance about what constitutes adequate supervision and how it should be implemented is not well defined.10, 11 The ACGME stresses that supervision should promote resident autonomy in clinical care.10 However, when trainees act independently, it might lead to critical communication breakdowns and other patient safety concerns.5, 6, 1214 Although attendings can encourage (or discourage) residents from seeking advice,15, 16 residents also play important roles in asking for help (ie, initiating their own supervision).1719 Additional research is needed on how residents walk the fine line between exercising independence and seeking supervision.
Lack of resident supervision is especially problematic in high‐risk settings such as the medical intensive care unit (ICU), where medical errors are as frequent as 1.7 errors per patient per day,20, 21 and the adverse drug event rate is twice that of non‐ICU settings.22 Because medication errors are one of the most common errors residents make,23, 24 resident interactions with nursing and pharmacy staff may significantly influence medication safety in error‐prone ICUs.2529 Studies of traditional hierarchical supervision tend to overlook how interactions with other professionals influence resident training.12, 18, 30, 31
We define supervision as a process of providing trainees with monitoring, guidance, and feedback9(p828) as they care for patients.3 Whereas traditionally, supervisors are identified by their positions of formal authority in the medical chain of command; we conceptualize supervision as a process in which professionals engaged in supervisory activities need not have formal authority over their trainees.
To examine how residents seek supervision through both the traditional medical hierarchical chain of command (including attendings, fellows and senior residents) and interprofessional communication channels (including nursing and pharmacy staff), we conducted a qualitative study of residents working in ICUs in three tertiary care hospitals. Using semi‐structured interviews, we asked residents to describe how they experienced supervision as they provided medications to patients. Two broad research questions guided data analysis:
How do residents receive supervision from physicians in the traditional medical hierarchy?
How do residents receive supervision from other professionals (ie, nurses, staff pharmacists, and clinical pharmacists)?
METHODS
Study Design and Sample
We conducted a qualitative study using data from interviews with 17 residents working in the medical ICUs of three large tertiary care hospitals (henceforth referred to as South, West, and North hospitals). The interviews were conducted as part of a longitudinal research project that examined how hospitals learn from medication errors.32 The research project focused on hospitals where medication error prevention was salient because of a vulnerable patient population and/or extensive high‐hazard drug usage. For each ICU, the research design included interviews with 6 attendings, 6 fellows, and a purposeful random sample33 of 6 residents. The goal was to reduce bias from supervisors selecting study participants, and thus enhance the credibility of the small sample, rather than generalize from it.32 Surgical residents were excluded, because of the medication focus. The local Institutional Review Boards approved the research.
Drawing on preliminary analyses of research project data, we designed the current study to examine how residents experienced supervision.33 A qualitative research design was particularly appropriate, because this study is exploratory34 and examines the processes of how supervision is implemented.33 By gathering longitudinal data from 2001 to 2007 and from ICUs in different hospitals, we were able to search for persistent patterns (and systematic variations over time) in how residents experienced supervision that might not have been revealed by a cross‐sectional study in one hospital ICU.
Data Collection
The principal investigator ([PI] M.T.) interviewed residents to gather data about their experiences with medication safety and supervision when providing medication to ICU patients. A general interview guide33 addressed residents' personal experiences with ordering medications, receiving supervision, and their perceptions of institutional medication safety programs (see Supporting Table 1 in the online version of this article). The interviewer consistently prompted residents to provide examples of their supervision experiences. The PI conducted confidential interviews in a private location near the ICU. Using confidential open‐ended, in‐depth interviews33 enabled the participating residents to provide frank answers to potentially sensitive questions.
The current study focuses on interviews with 17 residents; 8 from South Hospital, 6 from West Hospital, and 3 from North Hospital ICUs. Residents were at different training stages (years 14), and none declined participation. Interviews were audio‐recorded, transcribed professionally, checked for accuracy of transcription, and de‐identified. On average, each interview lasted about an hour, resulted in a 30‐page transcript, and focused on how residents experienced supervision for over two‐thirds of the transcript. Interviewees frequently described specific examples in vivid detail, yielding rich information. These data are consistent with Patton's observation that the validity, meaningfulness, and insights generated from qualitative inquiry have more to do with the information richness of the cases selected than with sample size.33(p245) Field notes, document review, and observations of routine activities supplemented the interviews.
Data Analysis
We coded and analyzed interview transcripts by applying the constant comparative method, in which we systematically examined and refined variations in the concepts that emerged from the data.33 To focus on the residents' perceptions of their training experiences, we began the data analysis without preexisting codes. We refined and reconstructed the coding scheme in several iterative stages. Based on the initial review by two investigators (M.T., H.S.), the PI and the coding team (T.D.G., S.M.) developed a preliminary coding scheme by induction, considering the residents' description of their experiences in the context of organizational research.34 They applied the coding scheme to three interview transcripts, and reevaluated and revised it based on comments from other investigators (H.S., E.J.T.).
The PI and the coding team met regularly to review and refine the codes. The PI and the coding team finalized the coding scheme only after it was validated by two other investigators and reapplied to the first set of interview transcripts. Constructing a detailed coding guide, we defined specific codes and classified them under seven broad themes.
We engaged in an iterative coding process to ensure credibility33 and consistent data analysis.34 Both coding team members independently coded each interview and resolved differences through consensus. The PI reviewed each coded transcript and met with the team to resolve any remaining coding disagreements. We used ATLAS.ti 5.0 software (ATLAS.ti Scientific Software Development, Berlin, Germany) to manage data, assist in detecting patterns, and compile relevant quotations.
We observed patterns in the data; we inductively identified themes that emerged from the data as well as those related to organizational research. During the period that we conducted interviews, new rules limiting residents' working hours were implemented.10 We did not discern any pattern changes before and after the new rules. To enhance data analysis credibility,34 two investigators (H.S., E.J.T.), serving as peer debriefers,35 examined whether the themes accurately reflected the data and rigorously searched for counter‐examples that contradicted the proposed themes.
RESULTS
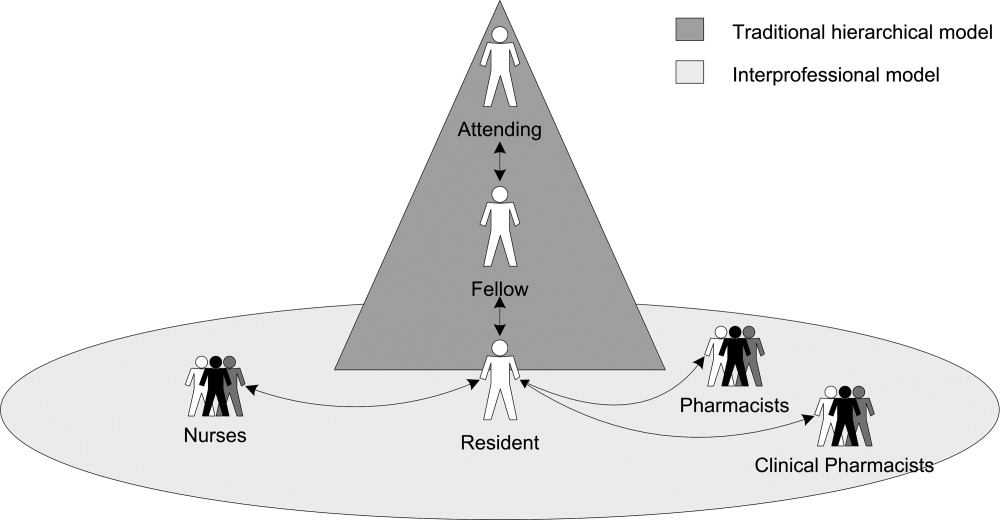
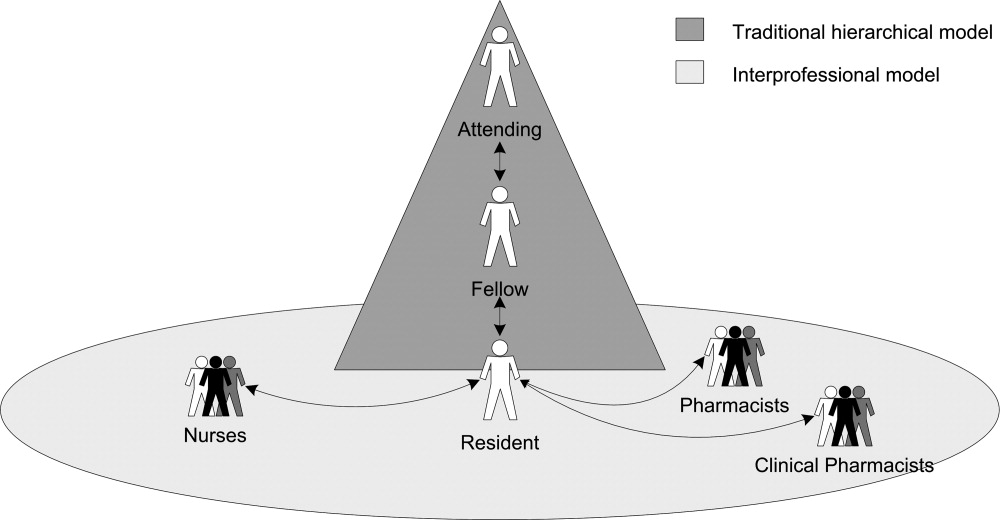
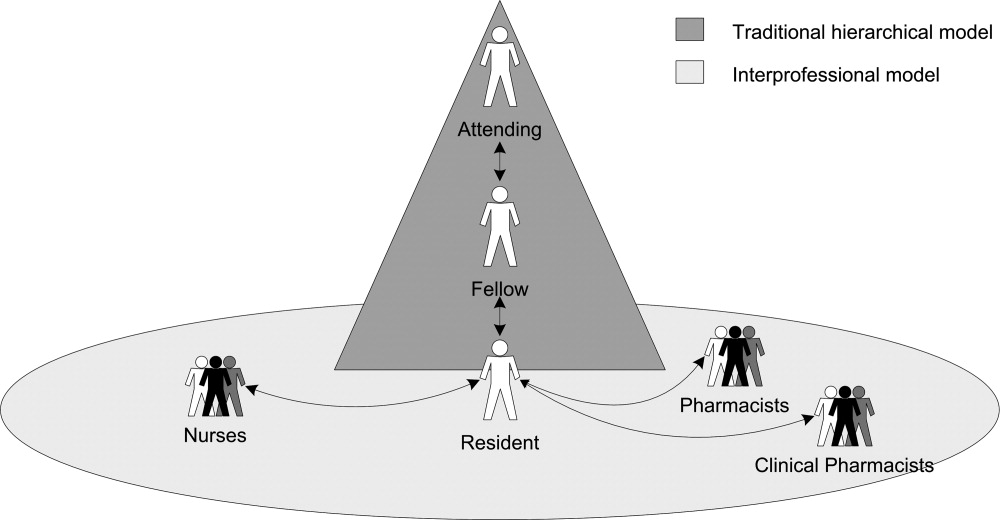
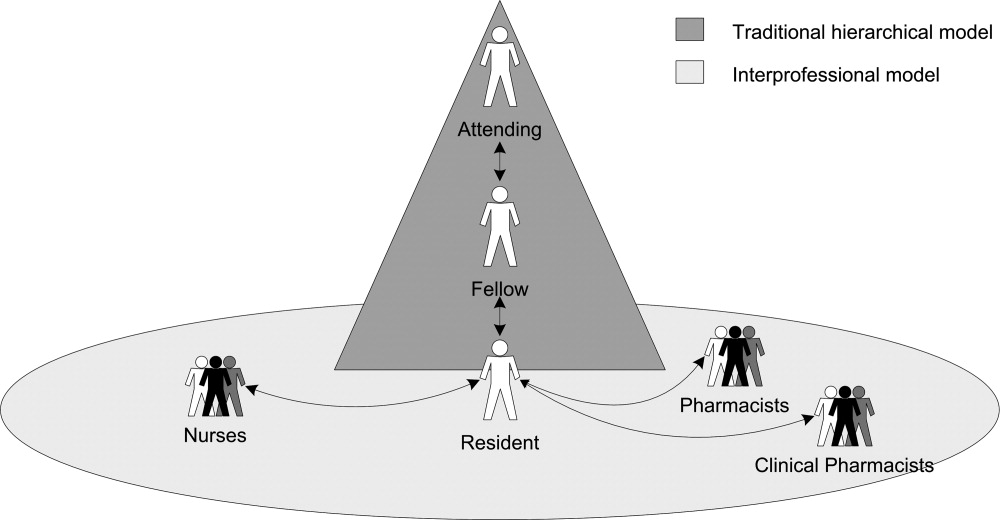
Residents described how they were supervised not only by other physicians within the traditional medical hierarchy, but also by other professionals, including nurses, staff pharmacists, and clinical pharmacists, ie, interprofessional supervision (Figure 1). After presenting these results, we examine how physicians and other professionals used communication strategies during interprofessional supervision. Here we use the term residents to include trainees at all levels, from interns to upper‐level residents, and male pronouns for de‐identification.
Initiating Supervision in the Traditional Medical Hierarchy
Residents described teaching rounds as the formal setting where the attending and other team members guided and gave feedback on their medication‐related decisions. After rounds, residents referred to the formal chain of command (from senior resident to fellow or attending) for their questions. However, residents also described enacting their own supervision by deciding when and how to ask for advice.
Residents developed different strategies for initiating supervision (Table 1). Some described a rule of thumb or personal decision‐making routine for determining when to approach a supervising physician with a question (eg, if the patient is in serious condition) (Table 1, columns 1 and 2). Others described how they decided when and how to ask an attending about their mistakes (Table 1, columns 3 and 4). As might be expected, residents' strategies usually reflected a desire for professional autonomy tempered with varying assessments of their own limitations (Table 1, columns 1 and 2, see Autonomy).
| Strategies for Asking Questions | Strategies for Seeking Feedback on Mistakes | ||
|---|---|---|---|
| When to Ask | When Not to Ask | When to Disclose a Mistake | How to Disclose a Mistake |
| Potential for adverse patient outcome: | Autonomy: | Potential for adverse patient outcome: | Direct: |
If you expect this is really bad, you try to cover yourselfand try to get the experience of somebody else, how to fix it .[And if it's less serious?] Yeah, then you can handle it. If I know it's a busy night, I let two or three admissions come in and then I call the fellow. But if the patient is really, really sick I call the fellow. | There's always a fellow to help us if we have questions. Being like almost a third year though, a lot of the things we kind of can handle on our own. Replacing the electrolytes and blood pressure medicines; we don't need hardly any oversight. | Well, I don't want to call a fellow. I think this medication, if it is wrong, is not going to kill a patient, is not going to adversely affect the outcome. | And I went straight up to the attending and I'll be like: Listen, this is what happened. Now I know. I know what happened, but how can I prevent this from happening again or what should I have done differently? |
| Medication choice: | Nights: | Medication choice and potential for adverse patient outcome: | Indirect: |
| If it's what type of medicine we give, then I usually contact my fellow. But most of the time I just make a decision on my own. | I never call Dr. [Attending] at night because you can get in touch with the fellow. The intern should talk to the attending, but the intern couldn't reach the attending. Sometimes it's like 2:00 or 3:00 in the morning. Then you can wait. If it's not an emergency, not in bad shape, you can wait. In the morning, when the attending physician is there, we'll talk about it. We can then ask. | If I know I have made a small mistake and I think it is inconsequential, I am not going to bother anybody. But if it is a different antibiotic that needed to be started, or what other medications might I have forgotten I would say [to the attending], I forgot to do this yesterday and I am sorry. | Instead of going up and saying, I made this mistake, you know, This is what I did and this is what happened, was it wrong? And I will let them tell me that this was a mistake, or not a mistake, and why. [If it's] really bad, you kind of talk with a fellow and say, This is what I've done. Is it okay? |
| Divergence from plan: | |||
If it's not something in the plan and we have to call someone, like an attending in a neurology service. Things that are discussed in advance, that may be potentially serious, I won't discuss, but basically anything that wasn't discussed in advance that I judge to be serious, then I will ask. | |||
We also identified patterns in how residents and their supervising physicians communicated when residents initiated supervision (Table 2, column 1). In general, residents considered attendings and fellows to be receptive to their questions. One resident explained: There is no one here who is unapproachableeven an attending. Nonetheless, residents reported using deferential language when initiating supervision (Table 2, column 1, row 2). Residents noted that attendings and fellows varied in their responses to questions and mistakes, as reflected in how they communicated with residents (Table 2, column 1, rows 1 and 3).
| Communication Strategies | Hierarchical Supervision: Resident Initiated Supervision | Interprofessional Supervision: Other Professional Initiated Supervision |
|---|---|---|
| ||
| Nonjudgmental language* | Fellow to resident: | Resident to nurse: |
| There's no dumb question. Ask. You can call me any time. | I'll say, It's not such a good idea for this reason. I feel they've [nurses] questioned you on it, so you deserve an appropriate answer. It's not okay to just be like, No, we're not gonna do that. | |
| Attending to resident: | ||
| Listen, [the mistake] could have happened to anybody . Now you know. Next time [you] do this, but [the patient is] gonna be okay. | ||
| Deferential language | Resident to difficult attending: | Pharmacist questions resident: |
| And when you call, you're polite and respectful: I'm sorry sir, I hate to bother you but I have a dumb question | The pharmacy called me up and said, Now listen, are you sure you want to give that dosage? | |
| Resident to fellow: | Nurse questions resident: | |
| Listen, in humbleness say, I don't know this, or am I doing this right? Can you help me out here? | [Nurses] might say like, Oh, you really? You sure you want to do this? | |
| Nurse guides resident: | ||
| Hey I know it's your decision, but this is what Dr. [Attending] would do. | ||
| Judgmental language | Attending response to a gross error: | Nurses questions resident: |
| What the hell were you thinking? We'll try to fix it, but God, what were you thinking? | At first [the nurses] were making fun of the resident who wrote [an unfamiliar medication order] . They just assume you're stupid until you prove them wrong, which is fine. But it gets annoying, too, because we did go to school for a long timewe actually know what the hell we're doing. | |
| Fellow response to resident question: | ||
| The cardiology fellow on call at 2 AM, when you call with a question will be like, Why would you even ask me that question? How could you not know that? | ||
Despite recognizing the importance of asking questions, several residents expressed conflicting beliefs; they raised concerns about the personal consequences of seeking assistance. For instance, one resident advocated: My point of view is I think it's wonderful when you ask questions. Cause that means you're conscientious enough to care about the patientsenough to do the right thing. However, we observed that when he interrupted the research interview to consult with a fellow, he prefaced his query with: Hey, I think this is a dumb question. Some residents expressed contradictory beliefs when they described their embarrassment over appearing stupid and fears of looking weak in front of supervising physicians, even those they perceived as being approachable. Indeed, for one resident, the attending's accessibility increased his anxiety: I don't want to lose respect by asking a stupid question.
Interprofessional Supervision
Residents described how other professionals used various methods of supervising their decision‐making (Table 3). Nurses and pharmacists intercepted medication orders and asked for clarifications, whereas clinical pharmacists also advised residents on ordering alternative medications (Table 3, row 1). Other professionals regularly double‐checked order implementation (Table 3, row 2). Nurses, in particular, routinely guided the future actions of residents by giving them cues and suggesting the next therapeutic tasks they should perform (Table 3, row 3). When assessing residents' clinical decisions, these professionals applied different guidelines (Table 4). Nurses compared residents' clinical decisions to their expectations for usual experience‐based practices (Table 4, column 1); pharmacists consulted and noticed deviations from national and hospital pharmacy standards (Table 4, column 2); and clinical pharmacists supplemented pharmacy standards with their professional judgment (Table 4, column 3).
| Provider Type | Example |
|---|---|
| Intercepting medication orders | |
| Nurses and pharmacists | Clarifying and correcting orders: |
The [pharmacist] said, How much do you really want to give? I was like, Okay. Let me take a look at it. And when I looked at it, I knew it wasn't calculated right. The nurse will call me and say, or the pharmacist will call me and say, Can you please change this? This is not the right dose. | |
| Clinical pharmacists | Suggesting alternative medications: |
| You know, this might be a better medication to use because the half life is | |
| Double‐checking order implementation | |
| Nurses | The nurses in [the unit] are wonderful about doing their own calculations, so if it's a rate, like if it's a drip, I've seen almost all the nurses go back over my drip and do the doses. |
| Clinical pharmacists | Cause even after rounds, he'll go back through and look at all, everything. And if he sees something that doesn't make sense or we could do different, he lets us know. |
| Guiding future actions | |
| Nurses | [The nurses] talk to you about everything. They see the labs before you. They see the labs in the morning and are like, His potassium is high, can you fix this? His blood pressure has been running up, do you want to give him something? They guide you towards making the right decision. |
| Clinical pharmacists | I wouldn't give these two [medications] together. There may be an interaction. |
| Nurses | Staff Pharmacists | Clinical Pharmacists |
|---|---|---|
| Experience on unit and with patients: | Standardized pharmacy guidelines for normal dosage ranges: | Standardized pharmacy guidelines for normal dosage ranges: |
| They're with the patients 12 hours a day. Some of them, they've been doing this for 30 years. | No, [the pharmacists] wouldn't have known on that one [error] because it was a normal it's within a normal range of dosing and it's not that it would cause any harm to the patient, but it was just that it needed to go to a higher dose. [I] did a very high dose, compared with the current dose. Then [the pharmacist] called me back and said, I think this is not the right dose. | [The clinical pharmacist is] the one who says, Oh, by the way, do you really want it IV or PO? Or It should be q 6 versus q 8. |
| Expectations for practice norms: | Patient‐specific dosage guidelines: | Clinical judgment based on specialized pharmacology expertise: |
| [The nurses] can pick up mistakes just as easily as anyone else because they are used to this environment and they are used to seeing all the orders that are written generally. | The [unit‐based] pharmacist came to me and said, This patient's almost in renal failure. Did you want to give them a smaller dose because of the renal failure? And I said, Oh, yeah. I didn't even think about that. | That's all [clinical pharmacists] know is medicine and research and studies, and so you know, there may be a paper that came out last week that none of us have even had a chance to read. But they would be up to date on it. So as far as all the drug trials and everything. |
| The usual practices in the unit: | ||
| An experienced nurse came to me and told me that in the unit, doctor, we used to do it 1 gram, not 0.5 gram. | ||
| The attending's preferences: | ||
| I know sometimes you'll want to start a certain pressor and the nurse will be like Well, Dr. [Attending] likes to use this pressor instead. | ||
| Formal standards: | ||
| A nurse would say, especially in the medications I wrote out to be canceled because of the antibiotic policy here . Doctor, the patient doesn't have any more doses of [antibiotic], what do you want me to start, or do you need to call the [antibiotic policy] team? |
Initiating Interprofessional Supervision
Residents, in turn, sought advice from other professionals. They actively engaged pharmacists in their supervision by asking questions ranging from basic clarifications to complex technical queries. You can just take [the clinical pharmacist] to the side and say, Hey listen. I forgot this medication. What am I supposed to give? It starts with an L, explained a resident. Other residents consulted clinical pharmacists for specialized expertise: The [clinical pharmacists] usually have a protocol that they like to follow that a lot of the residents and probably even a lot of the attendings aren't aware of. In one hospital, residents depended on the clinical pharmacists: They're always available and they really help out the team. In another hospital, unit‐based (on‐site) pharmacists served as an informal but extremely useful resource. Residents also relied on central pharmacy‐based staff, who provided essential backup, especially after‐hours: [The pharmacy is] always available, like if you have a questionthere's a medicine you've never given, but it's the middle of the night, nobody else around, you want to call the pharmacist. Residents uniformly noted that nurses monitored their decisions (Table 2, column 2; Table 4, column 1), and one specifically mentioned soliciting advice from nurses on organizing intravenous lines.
Communication Strategies for Managing Differences in Status and Expertise
Unlike the medical hierarchy that clearly differentiates among residents, fellows, and attendings, interdisciplinary differences were less clearly delineated. Residents were perceived as having higher status than other professionals, due in part to their medical education and responsibility for signing orders. Nurses and pharmacists, however, often had extensive experience and/or specialized training, and thus more expertise than residents. For instance, residents noticed their ambiguous status compared to nurses:
I don't know if some people might psychologically think it was better or worse, worse because it was coming from a nurse and maybe somebody would think that they wouldn't know as much or something like that. But other people would think of it as, they're a team member and they have the perfect right to know more. And maybe it's better because that way like maybe the fellow or attending wouldn't find out that you made a mistake [emphasis added].
To manage the ambiguous differences in their status, experience, and expertise, residents and other professionals used various communication strategies (Table 2, column 2). Residents consistently recounted that pharmacists and nurses used deferential language, for example, by asking questions, rather than directly stating their concerns (Table 2, column 2, row 2). One resident appreciated the unit‐nurses' indirect language: Over here they're really cool about it. They'll say, Is this right, are you sure about this? However, some residents also recalled that nurses used more direct language, such as I am not comfortable, especially when giving residents feedback on IV drug administration. In contrast, when asking pharmacists questions, residents consistently reported using nonjudgmental language, but not deferential language. However, some residents used judgmental language when they disagreed with a pharmacist's intervention.
Individual residents bitterly recalled their encounters with other professionals during previous rotations. One described nurses who were resident‐unfriendly and used judgmental language to mock a resident's choice of medications (Table 2, column 2, row 3). Another worked with clinical pharmacists who feel like they are teaching the residents and they are above the residents. These interactions illustrate how communication choices can create interprofessional tensions, especially when differences in status and expertise conflict or are unclear.
DISCUSSION
We analyzed interviews of residents working in medical ICUs to understand their supervision experiences related to medication safety. Although residents espoused beliefs in seeking assistance from supervising physicians and articulated strategies for doing so, many experienced difficulties in initiating supervision through the traditional medical hierarchy. Some residents were embarrassed by their mistaken decisions; others were concerned that their questions would reflect poorly on them.
Residents also received interprofessional supervision from nurses and pharmacists, who proactively monitored, intervened in, and guided residents' decisions. Other professionals evaluated residents' decisions by comparing them to distinctive professional guidelines and routinely used deferential language when conveying their concerns. Residents, in turn, asked other professionals for assistance.
We posit that interprofessional supervision clearly meets an accepted definition of supervision.3, 9 Residents received monitoring, guidance and feedback9(p828) from other professionals, who engaged in routine monitoring and in situation‐specific double‐checks of residents' clinical decisions, similar to those performed by supervising physicians.30 Moreover, other professionals demonstrated the ability to anticipate a doctor's strengths and weaknesses in particular clinical situations in order to maximize patient safety.9(p829)
Our study results have implications for graduate medical education (GME) reform. First, trainees experienced supervision as a two‐way interaction.36 Residents balanced the countervailing pressures to act independently or to seek a supervising physician's advice, in part, by developing strategies for deciding when to ask questions. Kennedy et al. identified similar rhetorical strategies.18 By asking questions about their clinical decisions, residents requested that supervising physicians guide their work; thus, they proactively initiated and thereby enacted their own supervision. Fostering the conditions for initiating supervision is essential, especially given the association between lack of effective supervision and adverse outcomes.5, 6, 1214
Second, residents expressed contradictory expectations about seeking advice from supervising physicians. Some residents were wary of approaching attending physicians for fear of appearing incompetent or being ridiculed.12, 16, 18, 31 However, we found that other residents remained reluctant to seek advice despite simultaneously appreciating that attendings encouraged them to ask for assistance. Whereas the perceived approachability of supervising physicians was important,18, 19 our exploratory findings suggest that it may be a necessary, but not a sufficient, condition for creating a learning environment. Creating a supportive learning environmentin which residents feel comfortable in revealing their perceived shortcomings to supervising physicians3begins with cultural changes, such as building medical teams,6 but such changes can be slow to develop.
Third, interprofessional supervision offers a strategy for improving supervision. The ubiquitous involvement of nursing and pharmacy staff in monitoring and intervening in residents' medication‐related decisions could result in overlooking their unique contributions to resident supervision. Mindful that supervising physicians evaluate them, residents selectively sought nonjudgmental advice from professionals outside the medical hierarchy. Therefore, improving supervision could entail offering residents ready access to other professionals who can advise them, especially during late night hours when supervising physicians might not be present.17, 27
The importance of interprofessional supervision has not been adequately recognized and emphasized in GME. Our study findings, if supported by future research, highlight how interpersonal communication techniques could influence both interprofessional supervision and hierarchical supervision among physicians. Medical team training programs3739 emphasize developing skills, such as mutual performance monitoring,40(p13) by training providers to raise and respond to potentially sensitive questions. Improving supervision by enhancing interpersonal communication skills may be important, not only when relative status differences are clear (ie, physician hierarchy), but also when status differences are ambiguous (ie, residents and other professionals). GME programs could consider incorporating these techniques into their formal curricula, as could programs for nursing and pharmacy staff.
Our study has several limitations. Because of the larger research project objectives, we focused on medication safety in medical ICU settings, where nurses and pharmacists may be especially vigilant and proactive in monitoring residents. Thus, our findings may be specific to medication issues and less relevant outside ICUs. We had a relatively small sample size and do not claim to generalize from it, although we believe it offers meaningful insights. We also did not continue enlarging our sample until reaching redundancy.35(p202) Nevertheless, the purposeful random sample of residents produced rich information. Indeed, some study results are consistent with previous resident education research,18 adding validity to our findings. Although the interview protocol was not designed specifically to investigate supervision, the resulting interviews yielded abundant data containing residents' detailed descriptions of how they experienced supervision. Whereas we were careful to note whether particular perceptions were unique to one resident, or shared by others, we recognize that the value of residents' observations is assessed by the quality of the insights they provide, not necessarily by the number of residents who described the same experience.
In conclusion, we found that residents experienced difficulties in initiating traditional hierarchical supervision related to medication safety in the ICU. However, they reported ubiquitous interprofessional supervision, albeit limited in scope, which they relied upon for nonjudgmental guidance in their therapeutic decision‐making, especially after‐hours. In our study, interprofessional supervision proved crucial to improving medication safety in the ICU.
- ,,.Resident supervision in the operating room: Does this impact on outcome?J Trauma.1993;35:556–560.
- ,.Supervision in the outpatient clinic: Effects on teaching and patient care.J Gen Intern Med.1993;8:378–380.
- Institute of Medicine (IOM).Resident Duty Hours: Enhancing Sleep, Supervision, and Safety.Washington, DC:National Academic Press;2008.
- Joint Committee of the Group on Resident Affairs and Organization of Resident Representatives. Patient Safety and Graduate Medical Education. Washington, DC: Association of American Medical Colleges; 2003. Available at: https://services.aamc.org/publications/showfile.cfm?file=version13.pdf145:592–598.
- ,,,.Medical errors involving trainees: A study of closed malpractice claims from 5 insurers.Arch Intern Med.2007;167:2030–2036.
- .Resident duty hour reform and mortality in hospitalized patients.JAMA.2007;298:2865–2866.
- ,,,.Progressive independence in clinical training: A tradition worth defending?Acad Med.2005;80:S106–S111.
- ,.Effective supervision in clinical practice settings: A literature review.Med Educ.2000;34:827–840.
- Accreditation Council for Graduate Medical Education. ACGME Residency Review Committee Program Requirements in Critical Care Medicine. 2007. Available at: http://www.acgme.org/acWebsite/downloads/RRC_progReq/142pr707_ims.pdf Accessed August 14, 2009.
- ,.Resident supervision.Accreditation Council for Graduate Medical Education Bulletin.2005; September:15–17. Available at: http://www.acgme.org/acWebsite/bulletin/bulletin09_05. pdf. Accessed March 14,year="2009"2009.
- ,,,,.Resident uncertainty in clinical decision making and impact on patient care: A qualitative study.Qual Saf Health Care.2008;17:122–126.
- ,,, et al.Patterns of communication breakdowns resulting in injury to surgical patients.J Am Coll Surg.2007;204:533–540.
- ,,.Communication failures: An insidious contributor to medical mishaps.Acad Med.2004;79:186–194.
- ,,, et al.Attending doctors' perspectives on how residents learn.Med Educ.2007;41:1050–1058.
- ,,.Teaching but not learning: How medical residency programs handle errors.J Organiz Behav.2006;27:869–896.
- ,,,,.On‐call supervision and resident autonomy: From micromanager to absentee attending.Am J Med.2009;122:784–788.
- ,,,.Preserving professional credibility: Grounded theory study of medical trainees' requests for clinical support.BMJ.2009;338:b128.
- ,,,,,.Who wants feedback? An investigation of the variables influencing residents' feedback‐seeking behavior in relation to night shifts.Acad Med.2009;84:910–917.
- ,,, et al.A look into the nature and causes of human errors in the intensive care unit.Crit Care Med.1995;23:294–300.
- ,,, et al.The Critical Care Safety Study: The incidence and nature of adverse events and serious medical errors in intensive care.Crit Care Med.2005;33:1694–1700.
- ,,,,,.Preventable adverse drug events in hospitalized patients: A comparative study of intensive care and general care units.Crit Care Med.1997;25:1289–1297.
- ,,,,,.Residents report on adverse events and their causes.Arch Intern Med.2005;165:2607–2613.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351:1838–1848.
- ,,,,.Unit‐based clinical pharmacists' prevention of serious medication errors in pediatric inpatients.Am J Health Syst Pharm.2008;65:1254–1260.
- ,,,,.Improving medication safety in the ICU: The pharmacist's role.Hospital Pharmacy.2007;42:337–344.
- ,,,,,.Collaboration between pharmacists, physicians and nurse practitioners: A qualitative investigation of working relationships in the inpatient medical setting.J Interprof Care.2009;23:169–184.
- ,,,.Role of registered nurses in error prevention, discovery and correction.Qual Saf Health Care.2008;17:117–121.
- ,,, et al.Recovery from medical errors: The critical care nursing safety net.Jt Comm J Qual Patient Saf.2006;32:63–72.
- ,,,,.Clinical oversight: Conceptualizing the relationship between supervision and safety.J Gen Intern Med.2007;22:1080–1085.
- .To call or not to call: A judgment of risk by pre‐registration house officers.Med Educ.2008;42:938–944.
- ,.Classifying and interpreting threats to patient safety in hospitals: Insights from aviation.J Organiz Behav.2006;27:919–940.
- .Qualitative Research and Evaluation Methods.3rd ed.Thousand Oaks, CA:Sage Publications;2002.
- ,.Qualitative Data Analysis.2nd. ed.Thousand Oaks, CA:Sage Publications;2006.
- ,.Naturalistic Inquiry.Beverly Hills, CA:Sage Publications;1985.
- ,,.Supervision: A 2‐way street.Arch Intern Med.2008;168:1117.
- ,,, et al.Effects of teamwork training on adverse outcomes and process of care in labor and delivery: A randomized controlled trial.Obstet Gynecol.2007;109:48–55.
- ,,,.Does crew resource management training work? An update, an extension, and some critical needs.Hum Factors.2006;48:392–412.
- ,,,,,.Team training in the neonatal resuscitation program for interns: Teamwork and quality of resuscitations.Pediatrics.2010;125:539–546.
- ,,,,.Medical Teamwork and Patient Safety: The Evidence‐Based Relation.Rockville, MD:Agency for Healthcare Research and Quality 2005. Publication No. 05–0053. Available at: http://www.ahrq.gov/qual/medteam. Accessed October 15,2010.
Close supervision of residents potentially leads to fewer errors, lower patient mortality, and improved quality of care.19 An Institute of Medicine (IOM) report3 recommended improving supervision through more frequent consultations between residents and their supervisors. Although current Accreditation Council for Graduate Medical Education (ACGME) guidelines also recommend that attending physicians (attendings) supervise residents, detailed guidance about what constitutes adequate supervision and how it should be implemented is not well defined.10, 11 The ACGME stresses that supervision should promote resident autonomy in clinical care.10 However, when trainees act independently, it might lead to critical communication breakdowns and other patient safety concerns.5, 6, 1214 Although attendings can encourage (or discourage) residents from seeking advice,15, 16 residents also play important roles in asking for help (ie, initiating their own supervision).1719 Additional research is needed on how residents walk the fine line between exercising independence and seeking supervision.
Lack of resident supervision is especially problematic in high‐risk settings such as the medical intensive care unit (ICU), where medical errors are as frequent as 1.7 errors per patient per day,20, 21 and the adverse drug event rate is twice that of non‐ICU settings.22 Because medication errors are one of the most common errors residents make,23, 24 resident interactions with nursing and pharmacy staff may significantly influence medication safety in error‐prone ICUs.2529 Studies of traditional hierarchical supervision tend to overlook how interactions with other professionals influence resident training.12, 18, 30, 31
We define supervision as a process of providing trainees with monitoring, guidance, and feedback9(p828) as they care for patients.3 Whereas traditionally, supervisors are identified by their positions of formal authority in the medical chain of command; we conceptualize supervision as a process in which professionals engaged in supervisory activities need not have formal authority over their trainees.
To examine how residents seek supervision through both the traditional medical hierarchical chain of command (including attendings, fellows and senior residents) and interprofessional communication channels (including nursing and pharmacy staff), we conducted a qualitative study of residents working in ICUs in three tertiary care hospitals. Using semi‐structured interviews, we asked residents to describe how they experienced supervision as they provided medications to patients. Two broad research questions guided data analysis:
How do residents receive supervision from physicians in the traditional medical hierarchy?
How do residents receive supervision from other professionals (ie, nurses, staff pharmacists, and clinical pharmacists)?
METHODS
Study Design and Sample
We conducted a qualitative study using data from interviews with 17 residents working in the medical ICUs of three large tertiary care hospitals (henceforth referred to as South, West, and North hospitals). The interviews were conducted as part of a longitudinal research project that examined how hospitals learn from medication errors.32 The research project focused on hospitals where medication error prevention was salient because of a vulnerable patient population and/or extensive high‐hazard drug usage. For each ICU, the research design included interviews with 6 attendings, 6 fellows, and a purposeful random sample33 of 6 residents. The goal was to reduce bias from supervisors selecting study participants, and thus enhance the credibility of the small sample, rather than generalize from it.32 Surgical residents were excluded, because of the medication focus. The local Institutional Review Boards approved the research.
Drawing on preliminary analyses of research project data, we designed the current study to examine how residents experienced supervision.33 A qualitative research design was particularly appropriate, because this study is exploratory34 and examines the processes of how supervision is implemented.33 By gathering longitudinal data from 2001 to 2007 and from ICUs in different hospitals, we were able to search for persistent patterns (and systematic variations over time) in how residents experienced supervision that might not have been revealed by a cross‐sectional study in one hospital ICU.
Data Collection
The principal investigator ([PI] M.T.) interviewed residents to gather data about their experiences with medication safety and supervision when providing medication to ICU patients. A general interview guide33 addressed residents' personal experiences with ordering medications, receiving supervision, and their perceptions of institutional medication safety programs (see Supporting Table 1 in the online version of this article). The interviewer consistently prompted residents to provide examples of their supervision experiences. The PI conducted confidential interviews in a private location near the ICU. Using confidential open‐ended, in‐depth interviews33 enabled the participating residents to provide frank answers to potentially sensitive questions.
The current study focuses on interviews with 17 residents; 8 from South Hospital, 6 from West Hospital, and 3 from North Hospital ICUs. Residents were at different training stages (years 14), and none declined participation. Interviews were audio‐recorded, transcribed professionally, checked for accuracy of transcription, and de‐identified. On average, each interview lasted about an hour, resulted in a 30‐page transcript, and focused on how residents experienced supervision for over two‐thirds of the transcript. Interviewees frequently described specific examples in vivid detail, yielding rich information. These data are consistent with Patton's observation that the validity, meaningfulness, and insights generated from qualitative inquiry have more to do with the information richness of the cases selected than with sample size.33(p245) Field notes, document review, and observations of routine activities supplemented the interviews.
Data Analysis
We coded and analyzed interview transcripts by applying the constant comparative method, in which we systematically examined and refined variations in the concepts that emerged from the data.33 To focus on the residents' perceptions of their training experiences, we began the data analysis without preexisting codes. We refined and reconstructed the coding scheme in several iterative stages. Based on the initial review by two investigators (M.T., H.S.), the PI and the coding team (T.D.G., S.M.) developed a preliminary coding scheme by induction, considering the residents' description of their experiences in the context of organizational research.34 They applied the coding scheme to three interview transcripts, and reevaluated and revised it based on comments from other investigators (H.S., E.J.T.).
The PI and the coding team met regularly to review and refine the codes. The PI and the coding team finalized the coding scheme only after it was validated by two other investigators and reapplied to the first set of interview transcripts. Constructing a detailed coding guide, we defined specific codes and classified them under seven broad themes.
We engaged in an iterative coding process to ensure credibility33 and consistent data analysis.34 Both coding team members independently coded each interview and resolved differences through consensus. The PI reviewed each coded transcript and met with the team to resolve any remaining coding disagreements. We used ATLAS.ti 5.0 software (ATLAS.ti Scientific Software Development, Berlin, Germany) to manage data, assist in detecting patterns, and compile relevant quotations.
We observed patterns in the data; we inductively identified themes that emerged from the data as well as those related to organizational research. During the period that we conducted interviews, new rules limiting residents' working hours were implemented.10 We did not discern any pattern changes before and after the new rules. To enhance data analysis credibility,34 two investigators (H.S., E.J.T.), serving as peer debriefers,35 examined whether the themes accurately reflected the data and rigorously searched for counter‐examples that contradicted the proposed themes.
RESULTS
Residents described how they were supervised not only by other physicians within the traditional medical hierarchy, but also by other professionals, including nurses, staff pharmacists, and clinical pharmacists, ie, interprofessional supervision (Figure 1). After presenting these results, we examine how physicians and other professionals used communication strategies during interprofessional supervision. Here we use the term residents to include trainees at all levels, from interns to upper‐level residents, and male pronouns for de‐identification.
Initiating Supervision in the Traditional Medical Hierarchy
Residents described teaching rounds as the formal setting where the attending and other team members guided and gave feedback on their medication‐related decisions. After rounds, residents referred to the formal chain of command (from senior resident to fellow or attending) for their questions. However, residents also described enacting their own supervision by deciding when and how to ask for advice.
Residents developed different strategies for initiating supervision (Table 1). Some described a rule of thumb or personal decision‐making routine for determining when to approach a supervising physician with a question (eg, if the patient is in serious condition) (Table 1, columns 1 and 2). Others described how they decided when and how to ask an attending about their mistakes (Table 1, columns 3 and 4). As might be expected, residents' strategies usually reflected a desire for professional autonomy tempered with varying assessments of their own limitations (Table 1, columns 1 and 2, see Autonomy).
| Strategies for Asking Questions | Strategies for Seeking Feedback on Mistakes | ||
|---|---|---|---|
| When to Ask | When Not to Ask | When to Disclose a Mistake | How to Disclose a Mistake |
| Potential for adverse patient outcome: | Autonomy: | Potential for adverse patient outcome: | Direct: |
If you expect this is really bad, you try to cover yourselfand try to get the experience of somebody else, how to fix it .[And if it's less serious?] Yeah, then you can handle it. If I know it's a busy night, I let two or three admissions come in and then I call the fellow. But if the patient is really, really sick I call the fellow. | There's always a fellow to help us if we have questions. Being like almost a third year though, a lot of the things we kind of can handle on our own. Replacing the electrolytes and blood pressure medicines; we don't need hardly any oversight. | Well, I don't want to call a fellow. I think this medication, if it is wrong, is not going to kill a patient, is not going to adversely affect the outcome. | And I went straight up to the attending and I'll be like: Listen, this is what happened. Now I know. I know what happened, but how can I prevent this from happening again or what should I have done differently? |
| Medication choice: | Nights: | Medication choice and potential for adverse patient outcome: | Indirect: |
| If it's what type of medicine we give, then I usually contact my fellow. But most of the time I just make a decision on my own. | I never call Dr. [Attending] at night because you can get in touch with the fellow. The intern should talk to the attending, but the intern couldn't reach the attending. Sometimes it's like 2:00 or 3:00 in the morning. Then you can wait. If it's not an emergency, not in bad shape, you can wait. In the morning, when the attending physician is there, we'll talk about it. We can then ask. | If I know I have made a small mistake and I think it is inconsequential, I am not going to bother anybody. But if it is a different antibiotic that needed to be started, or what other medications might I have forgotten I would say [to the attending], I forgot to do this yesterday and I am sorry. | Instead of going up and saying, I made this mistake, you know, This is what I did and this is what happened, was it wrong? And I will let them tell me that this was a mistake, or not a mistake, and why. [If it's] really bad, you kind of talk with a fellow and say, This is what I've done. Is it okay? |
| Divergence from plan: | |||
If it's not something in the plan and we have to call someone, like an attending in a neurology service. Things that are discussed in advance, that may be potentially serious, I won't discuss, but basically anything that wasn't discussed in advance that I judge to be serious, then I will ask. | |||
We also identified patterns in how residents and their supervising physicians communicated when residents initiated supervision (Table 2, column 1). In general, residents considered attendings and fellows to be receptive to their questions. One resident explained: There is no one here who is unapproachableeven an attending. Nonetheless, residents reported using deferential language when initiating supervision (Table 2, column 1, row 2). Residents noted that attendings and fellows varied in their responses to questions and mistakes, as reflected in how they communicated with residents (Table 2, column 1, rows 1 and 3).
| Communication Strategies | Hierarchical Supervision: Resident Initiated Supervision | Interprofessional Supervision: Other Professional Initiated Supervision |
|---|---|---|
| ||
| Nonjudgmental language* | Fellow to resident: | Resident to nurse: |
| There's no dumb question. Ask. You can call me any time. | I'll say, It's not such a good idea for this reason. I feel they've [nurses] questioned you on it, so you deserve an appropriate answer. It's not okay to just be like, No, we're not gonna do that. | |
| Attending to resident: | ||
| Listen, [the mistake] could have happened to anybody . Now you know. Next time [you] do this, but [the patient is] gonna be okay. | ||
| Deferential language | Resident to difficult attending: | Pharmacist questions resident: |
| And when you call, you're polite and respectful: I'm sorry sir, I hate to bother you but I have a dumb question | The pharmacy called me up and said, Now listen, are you sure you want to give that dosage? | |
| Resident to fellow: | Nurse questions resident: | |
| Listen, in humbleness say, I don't know this, or am I doing this right? Can you help me out here? | [Nurses] might say like, Oh, you really? You sure you want to do this? | |
| Nurse guides resident: | ||
| Hey I know it's your decision, but this is what Dr. [Attending] would do. | ||
| Judgmental language | Attending response to a gross error: | Nurses questions resident: |
| What the hell were you thinking? We'll try to fix it, but God, what were you thinking? | At first [the nurses] were making fun of the resident who wrote [an unfamiliar medication order] . They just assume you're stupid until you prove them wrong, which is fine. But it gets annoying, too, because we did go to school for a long timewe actually know what the hell we're doing. | |
| Fellow response to resident question: | ||
| The cardiology fellow on call at 2 AM, when you call with a question will be like, Why would you even ask me that question? How could you not know that? | ||
Despite recognizing the importance of asking questions, several residents expressed conflicting beliefs; they raised concerns about the personal consequences of seeking assistance. For instance, one resident advocated: My point of view is I think it's wonderful when you ask questions. Cause that means you're conscientious enough to care about the patientsenough to do the right thing. However, we observed that when he interrupted the research interview to consult with a fellow, he prefaced his query with: Hey, I think this is a dumb question. Some residents expressed contradictory beliefs when they described their embarrassment over appearing stupid and fears of looking weak in front of supervising physicians, even those they perceived as being approachable. Indeed, for one resident, the attending's accessibility increased his anxiety: I don't want to lose respect by asking a stupid question.
Interprofessional Supervision
Residents described how other professionals used various methods of supervising their decision‐making (Table 3). Nurses and pharmacists intercepted medication orders and asked for clarifications, whereas clinical pharmacists also advised residents on ordering alternative medications (Table 3, row 1). Other professionals regularly double‐checked order implementation (Table 3, row 2). Nurses, in particular, routinely guided the future actions of residents by giving them cues and suggesting the next therapeutic tasks they should perform (Table 3, row 3). When assessing residents' clinical decisions, these professionals applied different guidelines (Table 4). Nurses compared residents' clinical decisions to their expectations for usual experience‐based practices (Table 4, column 1); pharmacists consulted and noticed deviations from national and hospital pharmacy standards (Table 4, column 2); and clinical pharmacists supplemented pharmacy standards with their professional judgment (Table 4, column 3).
| Provider Type | Example |
|---|---|
| Intercepting medication orders | |
| Nurses and pharmacists | Clarifying and correcting orders: |
The [pharmacist] said, How much do you really want to give? I was like, Okay. Let me take a look at it. And when I looked at it, I knew it wasn't calculated right. The nurse will call me and say, or the pharmacist will call me and say, Can you please change this? This is not the right dose. | |
| Clinical pharmacists | Suggesting alternative medications: |
| You know, this might be a better medication to use because the half life is | |
| Double‐checking order implementation | |
| Nurses | The nurses in [the unit] are wonderful about doing their own calculations, so if it's a rate, like if it's a drip, I've seen almost all the nurses go back over my drip and do the doses. |
| Clinical pharmacists | Cause even after rounds, he'll go back through and look at all, everything. And if he sees something that doesn't make sense or we could do different, he lets us know. |
| Guiding future actions | |
| Nurses | [The nurses] talk to you about everything. They see the labs before you. They see the labs in the morning and are like, His potassium is high, can you fix this? His blood pressure has been running up, do you want to give him something? They guide you towards making the right decision. |
| Clinical pharmacists | I wouldn't give these two [medications] together. There may be an interaction. |
| Nurses | Staff Pharmacists | Clinical Pharmacists |
|---|---|---|
| Experience on unit and with patients: | Standardized pharmacy guidelines for normal dosage ranges: | Standardized pharmacy guidelines for normal dosage ranges: |
| They're with the patients 12 hours a day. Some of them, they've been doing this for 30 years. | No, [the pharmacists] wouldn't have known on that one [error] because it was a normal it's within a normal range of dosing and it's not that it would cause any harm to the patient, but it was just that it needed to go to a higher dose. [I] did a very high dose, compared with the current dose. Then [the pharmacist] called me back and said, I think this is not the right dose. | [The clinical pharmacist is] the one who says, Oh, by the way, do you really want it IV or PO? Or It should be q 6 versus q 8. |
| Expectations for practice norms: | Patient‐specific dosage guidelines: | Clinical judgment based on specialized pharmacology expertise: |
| [The nurses] can pick up mistakes just as easily as anyone else because they are used to this environment and they are used to seeing all the orders that are written generally. | The [unit‐based] pharmacist came to me and said, This patient's almost in renal failure. Did you want to give them a smaller dose because of the renal failure? And I said, Oh, yeah. I didn't even think about that. | That's all [clinical pharmacists] know is medicine and research and studies, and so you know, there may be a paper that came out last week that none of us have even had a chance to read. But they would be up to date on it. So as far as all the drug trials and everything. |
| The usual practices in the unit: | ||
| An experienced nurse came to me and told me that in the unit, doctor, we used to do it 1 gram, not 0.5 gram. | ||
| The attending's preferences: | ||
| I know sometimes you'll want to start a certain pressor and the nurse will be like Well, Dr. [Attending] likes to use this pressor instead. | ||
| Formal standards: | ||
| A nurse would say, especially in the medications I wrote out to be canceled because of the antibiotic policy here . Doctor, the patient doesn't have any more doses of [antibiotic], what do you want me to start, or do you need to call the [antibiotic policy] team? |
Initiating Interprofessional Supervision
Residents, in turn, sought advice from other professionals. They actively engaged pharmacists in their supervision by asking questions ranging from basic clarifications to complex technical queries. You can just take [the clinical pharmacist] to the side and say, Hey listen. I forgot this medication. What am I supposed to give? It starts with an L, explained a resident. Other residents consulted clinical pharmacists for specialized expertise: The [clinical pharmacists] usually have a protocol that they like to follow that a lot of the residents and probably even a lot of the attendings aren't aware of. In one hospital, residents depended on the clinical pharmacists: They're always available and they really help out the team. In another hospital, unit‐based (on‐site) pharmacists served as an informal but extremely useful resource. Residents also relied on central pharmacy‐based staff, who provided essential backup, especially after‐hours: [The pharmacy is] always available, like if you have a questionthere's a medicine you've never given, but it's the middle of the night, nobody else around, you want to call the pharmacist. Residents uniformly noted that nurses monitored their decisions (Table 2, column 2; Table 4, column 1), and one specifically mentioned soliciting advice from nurses on organizing intravenous lines.
Communication Strategies for Managing Differences in Status and Expertise
Unlike the medical hierarchy that clearly differentiates among residents, fellows, and attendings, interdisciplinary differences were less clearly delineated. Residents were perceived as having higher status than other professionals, due in part to their medical education and responsibility for signing orders. Nurses and pharmacists, however, often had extensive experience and/or specialized training, and thus more expertise than residents. For instance, residents noticed their ambiguous status compared to nurses:
I don't know if some people might psychologically think it was better or worse, worse because it was coming from a nurse and maybe somebody would think that they wouldn't know as much or something like that. But other people would think of it as, they're a team member and they have the perfect right to know more. And maybe it's better because that way like maybe the fellow or attending wouldn't find out that you made a mistake [emphasis added].
To manage the ambiguous differences in their status, experience, and expertise, residents and other professionals used various communication strategies (Table 2, column 2). Residents consistently recounted that pharmacists and nurses used deferential language, for example, by asking questions, rather than directly stating their concerns (Table 2, column 2, row 2). One resident appreciated the unit‐nurses' indirect language: Over here they're really cool about it. They'll say, Is this right, are you sure about this? However, some residents also recalled that nurses used more direct language, such as I am not comfortable, especially when giving residents feedback on IV drug administration. In contrast, when asking pharmacists questions, residents consistently reported using nonjudgmental language, but not deferential language. However, some residents used judgmental language when they disagreed with a pharmacist's intervention.
Individual residents bitterly recalled their encounters with other professionals during previous rotations. One described nurses who were resident‐unfriendly and used judgmental language to mock a resident's choice of medications (Table 2, column 2, row 3). Another worked with clinical pharmacists who feel like they are teaching the residents and they are above the residents. These interactions illustrate how communication choices can create interprofessional tensions, especially when differences in status and expertise conflict or are unclear.
DISCUSSION
We analyzed interviews of residents working in medical ICUs to understand their supervision experiences related to medication safety. Although residents espoused beliefs in seeking assistance from supervising physicians and articulated strategies for doing so, many experienced difficulties in initiating supervision through the traditional medical hierarchy. Some residents were embarrassed by their mistaken decisions; others were concerned that their questions would reflect poorly on them.
Residents also received interprofessional supervision from nurses and pharmacists, who proactively monitored, intervened in, and guided residents' decisions. Other professionals evaluated residents' decisions by comparing them to distinctive professional guidelines and routinely used deferential language when conveying their concerns. Residents, in turn, asked other professionals for assistance.
We posit that interprofessional supervision clearly meets an accepted definition of supervision.3, 9 Residents received monitoring, guidance and feedback9(p828) from other professionals, who engaged in routine monitoring and in situation‐specific double‐checks of residents' clinical decisions, similar to those performed by supervising physicians.30 Moreover, other professionals demonstrated the ability to anticipate a doctor's strengths and weaknesses in particular clinical situations in order to maximize patient safety.9(p829)
Our study results have implications for graduate medical education (GME) reform. First, trainees experienced supervision as a two‐way interaction.36 Residents balanced the countervailing pressures to act independently or to seek a supervising physician's advice, in part, by developing strategies for deciding when to ask questions. Kennedy et al. identified similar rhetorical strategies.18 By asking questions about their clinical decisions, residents requested that supervising physicians guide their work; thus, they proactively initiated and thereby enacted their own supervision. Fostering the conditions for initiating supervision is essential, especially given the association between lack of effective supervision and adverse outcomes.5, 6, 1214
Second, residents expressed contradictory expectations about seeking advice from supervising physicians. Some residents were wary of approaching attending physicians for fear of appearing incompetent or being ridiculed.12, 16, 18, 31 However, we found that other residents remained reluctant to seek advice despite simultaneously appreciating that attendings encouraged them to ask for assistance. Whereas the perceived approachability of supervising physicians was important,18, 19 our exploratory findings suggest that it may be a necessary, but not a sufficient, condition for creating a learning environment. Creating a supportive learning environmentin which residents feel comfortable in revealing their perceived shortcomings to supervising physicians3begins with cultural changes, such as building medical teams,6 but such changes can be slow to develop.
Third, interprofessional supervision offers a strategy for improving supervision. The ubiquitous involvement of nursing and pharmacy staff in monitoring and intervening in residents' medication‐related decisions could result in overlooking their unique contributions to resident supervision. Mindful that supervising physicians evaluate them, residents selectively sought nonjudgmental advice from professionals outside the medical hierarchy. Therefore, improving supervision could entail offering residents ready access to other professionals who can advise them, especially during late night hours when supervising physicians might not be present.17, 27
The importance of interprofessional supervision has not been adequately recognized and emphasized in GME. Our study findings, if supported by future research, highlight how interpersonal communication techniques could influence both interprofessional supervision and hierarchical supervision among physicians. Medical team training programs3739 emphasize developing skills, such as mutual performance monitoring,40(p13) by training providers to raise and respond to potentially sensitive questions. Improving supervision by enhancing interpersonal communication skills may be important, not only when relative status differences are clear (ie, physician hierarchy), but also when status differences are ambiguous (ie, residents and other professionals). GME programs could consider incorporating these techniques into their formal curricula, as could programs for nursing and pharmacy staff.
Our study has several limitations. Because of the larger research project objectives, we focused on medication safety in medical ICU settings, where nurses and pharmacists may be especially vigilant and proactive in monitoring residents. Thus, our findings may be specific to medication issues and less relevant outside ICUs. We had a relatively small sample size and do not claim to generalize from it, although we believe it offers meaningful insights. We also did not continue enlarging our sample until reaching redundancy.35(p202) Nevertheless, the purposeful random sample of residents produced rich information. Indeed, some study results are consistent with previous resident education research,18 adding validity to our findings. Although the interview protocol was not designed specifically to investigate supervision, the resulting interviews yielded abundant data containing residents' detailed descriptions of how they experienced supervision. Whereas we were careful to note whether particular perceptions were unique to one resident, or shared by others, we recognize that the value of residents' observations is assessed by the quality of the insights they provide, not necessarily by the number of residents who described the same experience.
In conclusion, we found that residents experienced difficulties in initiating traditional hierarchical supervision related to medication safety in the ICU. However, they reported ubiquitous interprofessional supervision, albeit limited in scope, which they relied upon for nonjudgmental guidance in their therapeutic decision‐making, especially after‐hours. In our study, interprofessional supervision proved crucial to improving medication safety in the ICU.
Close supervision of residents potentially leads to fewer errors, lower patient mortality, and improved quality of care.19 An Institute of Medicine (IOM) report3 recommended improving supervision through more frequent consultations between residents and their supervisors. Although current Accreditation Council for Graduate Medical Education (ACGME) guidelines also recommend that attending physicians (attendings) supervise residents, detailed guidance about what constitutes adequate supervision and how it should be implemented is not well defined.10, 11 The ACGME stresses that supervision should promote resident autonomy in clinical care.10 However, when trainees act independently, it might lead to critical communication breakdowns and other patient safety concerns.5, 6, 1214 Although attendings can encourage (or discourage) residents from seeking advice,15, 16 residents also play important roles in asking for help (ie, initiating their own supervision).1719 Additional research is needed on how residents walk the fine line between exercising independence and seeking supervision.
Lack of resident supervision is especially problematic in high‐risk settings such as the medical intensive care unit (ICU), where medical errors are as frequent as 1.7 errors per patient per day,20, 21 and the adverse drug event rate is twice that of non‐ICU settings.22 Because medication errors are one of the most common errors residents make,23, 24 resident interactions with nursing and pharmacy staff may significantly influence medication safety in error‐prone ICUs.2529 Studies of traditional hierarchical supervision tend to overlook how interactions with other professionals influence resident training.12, 18, 30, 31
We define supervision as a process of providing trainees with monitoring, guidance, and feedback9(p828) as they care for patients.3 Whereas traditionally, supervisors are identified by their positions of formal authority in the medical chain of command; we conceptualize supervision as a process in which professionals engaged in supervisory activities need not have formal authority over their trainees.
To examine how residents seek supervision through both the traditional medical hierarchical chain of command (including attendings, fellows and senior residents) and interprofessional communication channels (including nursing and pharmacy staff), we conducted a qualitative study of residents working in ICUs in three tertiary care hospitals. Using semi‐structured interviews, we asked residents to describe how they experienced supervision as they provided medications to patients. Two broad research questions guided data analysis:
How do residents receive supervision from physicians in the traditional medical hierarchy?
How do residents receive supervision from other professionals (ie, nurses, staff pharmacists, and clinical pharmacists)?
METHODS
Study Design and Sample
We conducted a qualitative study using data from interviews with 17 residents working in the medical ICUs of three large tertiary care hospitals (henceforth referred to as South, West, and North hospitals). The interviews were conducted as part of a longitudinal research project that examined how hospitals learn from medication errors.32 The research project focused on hospitals where medication error prevention was salient because of a vulnerable patient population and/or extensive high‐hazard drug usage. For each ICU, the research design included interviews with 6 attendings, 6 fellows, and a purposeful random sample33 of 6 residents. The goal was to reduce bias from supervisors selecting study participants, and thus enhance the credibility of the small sample, rather than generalize from it.32 Surgical residents were excluded, because of the medication focus. The local Institutional Review Boards approved the research.
Drawing on preliminary analyses of research project data, we designed the current study to examine how residents experienced supervision.33 A qualitative research design was particularly appropriate, because this study is exploratory34 and examines the processes of how supervision is implemented.33 By gathering longitudinal data from 2001 to 2007 and from ICUs in different hospitals, we were able to search for persistent patterns (and systematic variations over time) in how residents experienced supervision that might not have been revealed by a cross‐sectional study in one hospital ICU.
Data Collection
The principal investigator ([PI] M.T.) interviewed residents to gather data about their experiences with medication safety and supervision when providing medication to ICU patients. A general interview guide33 addressed residents' personal experiences with ordering medications, receiving supervision, and their perceptions of institutional medication safety programs (see Supporting Table 1 in the online version of this article). The interviewer consistently prompted residents to provide examples of their supervision experiences. The PI conducted confidential interviews in a private location near the ICU. Using confidential open‐ended, in‐depth interviews33 enabled the participating residents to provide frank answers to potentially sensitive questions.
The current study focuses on interviews with 17 residents; 8 from South Hospital, 6 from West Hospital, and 3 from North Hospital ICUs. Residents were at different training stages (years 14), and none declined participation. Interviews were audio‐recorded, transcribed professionally, checked for accuracy of transcription, and de‐identified. On average, each interview lasted about an hour, resulted in a 30‐page transcript, and focused on how residents experienced supervision for over two‐thirds of the transcript. Interviewees frequently described specific examples in vivid detail, yielding rich information. These data are consistent with Patton's observation that the validity, meaningfulness, and insights generated from qualitative inquiry have more to do with the information richness of the cases selected than with sample size.33(p245) Field notes, document review, and observations of routine activities supplemented the interviews.
Data Analysis
We coded and analyzed interview transcripts by applying the constant comparative method, in which we systematically examined and refined variations in the concepts that emerged from the data.33 To focus on the residents' perceptions of their training experiences, we began the data analysis without preexisting codes. We refined and reconstructed the coding scheme in several iterative stages. Based on the initial review by two investigators (M.T., H.S.), the PI and the coding team (T.D.G., S.M.) developed a preliminary coding scheme by induction, considering the residents' description of their experiences in the context of organizational research.34 They applied the coding scheme to three interview transcripts, and reevaluated and revised it based on comments from other investigators (H.S., E.J.T.).
The PI and the coding team met regularly to review and refine the codes. The PI and the coding team finalized the coding scheme only after it was validated by two other investigators and reapplied to the first set of interview transcripts. Constructing a detailed coding guide, we defined specific codes and classified them under seven broad themes.
We engaged in an iterative coding process to ensure credibility33 and consistent data analysis.34 Both coding team members independently coded each interview and resolved differences through consensus. The PI reviewed each coded transcript and met with the team to resolve any remaining coding disagreements. We used ATLAS.ti 5.0 software (ATLAS.ti Scientific Software Development, Berlin, Germany) to manage data, assist in detecting patterns, and compile relevant quotations.
We observed patterns in the data; we inductively identified themes that emerged from the data as well as those related to organizational research. During the period that we conducted interviews, new rules limiting residents' working hours were implemented.10 We did not discern any pattern changes before and after the new rules. To enhance data analysis credibility,34 two investigators (H.S., E.J.T.), serving as peer debriefers,35 examined whether the themes accurately reflected the data and rigorously searched for counter‐examples that contradicted the proposed themes.
RESULTS
Residents described how they were supervised not only by other physicians within the traditional medical hierarchy, but also by other professionals, including nurses, staff pharmacists, and clinical pharmacists, ie, interprofessional supervision (Figure 1). After presenting these results, we examine how physicians and other professionals used communication strategies during interprofessional supervision. Here we use the term residents to include trainees at all levels, from interns to upper‐level residents, and male pronouns for de‐identification.
Initiating Supervision in the Traditional Medical Hierarchy
Residents described teaching rounds as the formal setting where the attending and other team members guided and gave feedback on their medication‐related decisions. After rounds, residents referred to the formal chain of command (from senior resident to fellow or attending) for their questions. However, residents also described enacting their own supervision by deciding when and how to ask for advice.
Residents developed different strategies for initiating supervision (Table 1). Some described a rule of thumb or personal decision‐making routine for determining when to approach a supervising physician with a question (eg, if the patient is in serious condition) (Table 1, columns 1 and 2). Others described how they decided when and how to ask an attending about their mistakes (Table 1, columns 3 and 4). As might be expected, residents' strategies usually reflected a desire for professional autonomy tempered with varying assessments of their own limitations (Table 1, columns 1 and 2, see Autonomy).
| Strategies for Asking Questions | Strategies for Seeking Feedback on Mistakes | ||
|---|---|---|---|
| When to Ask | When Not to Ask | When to Disclose a Mistake | How to Disclose a Mistake |
| Potential for adverse patient outcome: | Autonomy: | Potential for adverse patient outcome: | Direct: |
If you expect this is really bad, you try to cover yourselfand try to get the experience of somebody else, how to fix it .[And if it's less serious?] Yeah, then you can handle it. If I know it's a busy night, I let two or three admissions come in and then I call the fellow. But if the patient is really, really sick I call the fellow. | There's always a fellow to help us if we have questions. Being like almost a third year though, a lot of the things we kind of can handle on our own. Replacing the electrolytes and blood pressure medicines; we don't need hardly any oversight. | Well, I don't want to call a fellow. I think this medication, if it is wrong, is not going to kill a patient, is not going to adversely affect the outcome. | And I went straight up to the attending and I'll be like: Listen, this is what happened. Now I know. I know what happened, but how can I prevent this from happening again or what should I have done differently? |
| Medication choice: | Nights: | Medication choice and potential for adverse patient outcome: | Indirect: |
| If it's what type of medicine we give, then I usually contact my fellow. But most of the time I just make a decision on my own. | I never call Dr. [Attending] at night because you can get in touch with the fellow. The intern should talk to the attending, but the intern couldn't reach the attending. Sometimes it's like 2:00 or 3:00 in the morning. Then you can wait. If it's not an emergency, not in bad shape, you can wait. In the morning, when the attending physician is there, we'll talk about it. We can then ask. | If I know I have made a small mistake and I think it is inconsequential, I am not going to bother anybody. But if it is a different antibiotic that needed to be started, or what other medications might I have forgotten I would say [to the attending], I forgot to do this yesterday and I am sorry. | Instead of going up and saying, I made this mistake, you know, This is what I did and this is what happened, was it wrong? And I will let them tell me that this was a mistake, or not a mistake, and why. [If it's] really bad, you kind of talk with a fellow and say, This is what I've done. Is it okay? |
| Divergence from plan: | |||
If it's not something in the plan and we have to call someone, like an attending in a neurology service. Things that are discussed in advance, that may be potentially serious, I won't discuss, but basically anything that wasn't discussed in advance that I judge to be serious, then I will ask. | |||
We also identified patterns in how residents and their supervising physicians communicated when residents initiated supervision (Table 2, column 1). In general, residents considered attendings and fellows to be receptive to their questions. One resident explained: There is no one here who is unapproachableeven an attending. Nonetheless, residents reported using deferential language when initiating supervision (Table 2, column 1, row 2). Residents noted that attendings and fellows varied in their responses to questions and mistakes, as reflected in how they communicated with residents (Table 2, column 1, rows 1 and 3).
| Communication Strategies | Hierarchical Supervision: Resident Initiated Supervision | Interprofessional Supervision: Other Professional Initiated Supervision |
|---|---|---|
| ||
| Nonjudgmental language* | Fellow to resident: | Resident to nurse: |
| There's no dumb question. Ask. You can call me any time. | I'll say, It's not such a good idea for this reason. I feel they've [nurses] questioned you on it, so you deserve an appropriate answer. It's not okay to just be like, No, we're not gonna do that. | |
| Attending to resident: | ||
| Listen, [the mistake] could have happened to anybody . Now you know. Next time [you] do this, but [the patient is] gonna be okay. | ||
| Deferential language | Resident to difficult attending: | Pharmacist questions resident: |
| And when you call, you're polite and respectful: I'm sorry sir, I hate to bother you but I have a dumb question | The pharmacy called me up and said, Now listen, are you sure you want to give that dosage? | |
| Resident to fellow: | Nurse questions resident: | |
| Listen, in humbleness say, I don't know this, or am I doing this right? Can you help me out here? | [Nurses] might say like, Oh, you really? You sure you want to do this? | |
| Nurse guides resident: | ||
| Hey I know it's your decision, but this is what Dr. [Attending] would do. | ||
| Judgmental language | Attending response to a gross error: | Nurses questions resident: |
| What the hell were you thinking? We'll try to fix it, but God, what were you thinking? | At first [the nurses] were making fun of the resident who wrote [an unfamiliar medication order] . They just assume you're stupid until you prove them wrong, which is fine. But it gets annoying, too, because we did go to school for a long timewe actually know what the hell we're doing. | |
| Fellow response to resident question: | ||
| The cardiology fellow on call at 2 AM, when you call with a question will be like, Why would you even ask me that question? How could you not know that? | ||
Despite recognizing the importance of asking questions, several residents expressed conflicting beliefs; they raised concerns about the personal consequences of seeking assistance. For instance, one resident advocated: My point of view is I think it's wonderful when you ask questions. Cause that means you're conscientious enough to care about the patientsenough to do the right thing. However, we observed that when he interrupted the research interview to consult with a fellow, he prefaced his query with: Hey, I think this is a dumb question. Some residents expressed contradictory beliefs when they described their embarrassment over appearing stupid and fears of looking weak in front of supervising physicians, even those they perceived as being approachable. Indeed, for one resident, the attending's accessibility increased his anxiety: I don't want to lose respect by asking a stupid question.
Interprofessional Supervision
Residents described how other professionals used various methods of supervising their decision‐making (Table 3). Nurses and pharmacists intercepted medication orders and asked for clarifications, whereas clinical pharmacists also advised residents on ordering alternative medications (Table 3, row 1). Other professionals regularly double‐checked order implementation (Table 3, row 2). Nurses, in particular, routinely guided the future actions of residents by giving them cues and suggesting the next therapeutic tasks they should perform (Table 3, row 3). When assessing residents' clinical decisions, these professionals applied different guidelines (Table 4). Nurses compared residents' clinical decisions to their expectations for usual experience‐based practices (Table 4, column 1); pharmacists consulted and noticed deviations from national and hospital pharmacy standards (Table 4, column 2); and clinical pharmacists supplemented pharmacy standards with their professional judgment (Table 4, column 3).
| Provider Type | Example |
|---|---|
| Intercepting medication orders | |
| Nurses and pharmacists | Clarifying and correcting orders: |
The [pharmacist] said, How much do you really want to give? I was like, Okay. Let me take a look at it. And when I looked at it, I knew it wasn't calculated right. The nurse will call me and say, or the pharmacist will call me and say, Can you please change this? This is not the right dose. | |
| Clinical pharmacists | Suggesting alternative medications: |
| You know, this might be a better medication to use because the half life is | |
| Double‐checking order implementation | |
| Nurses | The nurses in [the unit] are wonderful about doing their own calculations, so if it's a rate, like if it's a drip, I've seen almost all the nurses go back over my drip and do the doses. |
| Clinical pharmacists | Cause even after rounds, he'll go back through and look at all, everything. And if he sees something that doesn't make sense or we could do different, he lets us know. |
| Guiding future actions | |
| Nurses | [The nurses] talk to you about everything. They see the labs before you. They see the labs in the morning and are like, His potassium is high, can you fix this? His blood pressure has been running up, do you want to give him something? They guide you towards making the right decision. |
| Clinical pharmacists | I wouldn't give these two [medications] together. There may be an interaction. |
| Nurses | Staff Pharmacists | Clinical Pharmacists |
|---|---|---|
| Experience on unit and with patients: | Standardized pharmacy guidelines for normal dosage ranges: | Standardized pharmacy guidelines for normal dosage ranges: |
| They're with the patients 12 hours a day. Some of them, they've been doing this for 30 years. | No, [the pharmacists] wouldn't have known on that one [error] because it was a normal it's within a normal range of dosing and it's not that it would cause any harm to the patient, but it was just that it needed to go to a higher dose. [I] did a very high dose, compared with the current dose. Then [the pharmacist] called me back and said, I think this is not the right dose. | [The clinical pharmacist is] the one who says, Oh, by the way, do you really want it IV or PO? Or It should be q 6 versus q 8. |
| Expectations for practice norms: | Patient‐specific dosage guidelines: | Clinical judgment based on specialized pharmacology expertise: |
| [The nurses] can pick up mistakes just as easily as anyone else because they are used to this environment and they are used to seeing all the orders that are written generally. | The [unit‐based] pharmacist came to me and said, This patient's almost in renal failure. Did you want to give them a smaller dose because of the renal failure? And I said, Oh, yeah. I didn't even think about that. | That's all [clinical pharmacists] know is medicine and research and studies, and so you know, there may be a paper that came out last week that none of us have even had a chance to read. But they would be up to date on it. So as far as all the drug trials and everything. |
| The usual practices in the unit: | ||
| An experienced nurse came to me and told me that in the unit, doctor, we used to do it 1 gram, not 0.5 gram. | ||
| The attending's preferences: | ||
| I know sometimes you'll want to start a certain pressor and the nurse will be like Well, Dr. [Attending] likes to use this pressor instead. | ||
| Formal standards: | ||
| A nurse would say, especially in the medications I wrote out to be canceled because of the antibiotic policy here . Doctor, the patient doesn't have any more doses of [antibiotic], what do you want me to start, or do you need to call the [antibiotic policy] team? |
Initiating Interprofessional Supervision
Residents, in turn, sought advice from other professionals. They actively engaged pharmacists in their supervision by asking questions ranging from basic clarifications to complex technical queries. You can just take [the clinical pharmacist] to the side and say, Hey listen. I forgot this medication. What am I supposed to give? It starts with an L, explained a resident. Other residents consulted clinical pharmacists for specialized expertise: The [clinical pharmacists] usually have a protocol that they like to follow that a lot of the residents and probably even a lot of the attendings aren't aware of. In one hospital, residents depended on the clinical pharmacists: They're always available and they really help out the team. In another hospital, unit‐based (on‐site) pharmacists served as an informal but extremely useful resource. Residents also relied on central pharmacy‐based staff, who provided essential backup, especially after‐hours: [The pharmacy is] always available, like if you have a questionthere's a medicine you've never given, but it's the middle of the night, nobody else around, you want to call the pharmacist. Residents uniformly noted that nurses monitored their decisions (Table 2, column 2; Table 4, column 1), and one specifically mentioned soliciting advice from nurses on organizing intravenous lines.
Communication Strategies for Managing Differences in Status and Expertise
Unlike the medical hierarchy that clearly differentiates among residents, fellows, and attendings, interdisciplinary differences were less clearly delineated. Residents were perceived as having higher status than other professionals, due in part to their medical education and responsibility for signing orders. Nurses and pharmacists, however, often had extensive experience and/or specialized training, and thus more expertise than residents. For instance, residents noticed their ambiguous status compared to nurses:
I don't know if some people might psychologically think it was better or worse, worse because it was coming from a nurse and maybe somebody would think that they wouldn't know as much or something like that. But other people would think of it as, they're a team member and they have the perfect right to know more. And maybe it's better because that way like maybe the fellow or attending wouldn't find out that you made a mistake [emphasis added].
To manage the ambiguous differences in their status, experience, and expertise, residents and other professionals used various communication strategies (Table 2, column 2). Residents consistently recounted that pharmacists and nurses used deferential language, for example, by asking questions, rather than directly stating their concerns (Table 2, column 2, row 2). One resident appreciated the unit‐nurses' indirect language: Over here they're really cool about it. They'll say, Is this right, are you sure about this? However, some residents also recalled that nurses used more direct language, such as I am not comfortable, especially when giving residents feedback on IV drug administration. In contrast, when asking pharmacists questions, residents consistently reported using nonjudgmental language, but not deferential language. However, some residents used judgmental language when they disagreed with a pharmacist's intervention.
Individual residents bitterly recalled their encounters with other professionals during previous rotations. One described nurses who were resident‐unfriendly and used judgmental language to mock a resident's choice of medications (Table 2, column 2, row 3). Another worked with clinical pharmacists who feel like they are teaching the residents and they are above the residents. These interactions illustrate how communication choices can create interprofessional tensions, especially when differences in status and expertise conflict or are unclear.
DISCUSSION
We analyzed interviews of residents working in medical ICUs to understand their supervision experiences related to medication safety. Although residents espoused beliefs in seeking assistance from supervising physicians and articulated strategies for doing so, many experienced difficulties in initiating supervision through the traditional medical hierarchy. Some residents were embarrassed by their mistaken decisions; others were concerned that their questions would reflect poorly on them.
Residents also received interprofessional supervision from nurses and pharmacists, who proactively monitored, intervened in, and guided residents' decisions. Other professionals evaluated residents' decisions by comparing them to distinctive professional guidelines and routinely used deferential language when conveying their concerns. Residents, in turn, asked other professionals for assistance.
We posit that interprofessional supervision clearly meets an accepted definition of supervision.3, 9 Residents received monitoring, guidance and feedback9(p828) from other professionals, who engaged in routine monitoring and in situation‐specific double‐checks of residents' clinical decisions, similar to those performed by supervising physicians.30 Moreover, other professionals demonstrated the ability to anticipate a doctor's strengths and weaknesses in particular clinical situations in order to maximize patient safety.9(p829)
Our study results have implications for graduate medical education (GME) reform. First, trainees experienced supervision as a two‐way interaction.36 Residents balanced the countervailing pressures to act independently or to seek a supervising physician's advice, in part, by developing strategies for deciding when to ask questions. Kennedy et al. identified similar rhetorical strategies.18 By asking questions about their clinical decisions, residents requested that supervising physicians guide their work; thus, they proactively initiated and thereby enacted their own supervision. Fostering the conditions for initiating supervision is essential, especially given the association between lack of effective supervision and adverse outcomes.5, 6, 1214
Second, residents expressed contradictory expectations about seeking advice from supervising physicians. Some residents were wary of approaching attending physicians for fear of appearing incompetent or being ridiculed.12, 16, 18, 31 However, we found that other residents remained reluctant to seek advice despite simultaneously appreciating that attendings encouraged them to ask for assistance. Whereas the perceived approachability of supervising physicians was important,18, 19 our exploratory findings suggest that it may be a necessary, but not a sufficient, condition for creating a learning environment. Creating a supportive learning environmentin which residents feel comfortable in revealing their perceived shortcomings to supervising physicians3begins with cultural changes, such as building medical teams,6 but such changes can be slow to develop.
Third, interprofessional supervision offers a strategy for improving supervision. The ubiquitous involvement of nursing and pharmacy staff in monitoring and intervening in residents' medication‐related decisions could result in overlooking their unique contributions to resident supervision. Mindful that supervising physicians evaluate them, residents selectively sought nonjudgmental advice from professionals outside the medical hierarchy. Therefore, improving supervision could entail offering residents ready access to other professionals who can advise them, especially during late night hours when supervising physicians might not be present.17, 27
The importance of interprofessional supervision has not been adequately recognized and emphasized in GME. Our study findings, if supported by future research, highlight how interpersonal communication techniques could influence both interprofessional supervision and hierarchical supervision among physicians. Medical team training programs3739 emphasize developing skills, such as mutual performance monitoring,40(p13) by training providers to raise and respond to potentially sensitive questions. Improving supervision by enhancing interpersonal communication skills may be important, not only when relative status differences are clear (ie, physician hierarchy), but also when status differences are ambiguous (ie, residents and other professionals). GME programs could consider incorporating these techniques into their formal curricula, as could programs for nursing and pharmacy staff.
Our study has several limitations. Because of the larger research project objectives, we focused on medication safety in medical ICU settings, where nurses and pharmacists may be especially vigilant and proactive in monitoring residents. Thus, our findings may be specific to medication issues and less relevant outside ICUs. We had a relatively small sample size and do not claim to generalize from it, although we believe it offers meaningful insights. We also did not continue enlarging our sample until reaching redundancy.35(p202) Nevertheless, the purposeful random sample of residents produced rich information. Indeed, some study results are consistent with previous resident education research,18 adding validity to our findings. Although the interview protocol was not designed specifically to investigate supervision, the resulting interviews yielded abundant data containing residents' detailed descriptions of how they experienced supervision. Whereas we were careful to note whether particular perceptions were unique to one resident, or shared by others, we recognize that the value of residents' observations is assessed by the quality of the insights they provide, not necessarily by the number of residents who described the same experience.
In conclusion, we found that residents experienced difficulties in initiating traditional hierarchical supervision related to medication safety in the ICU. However, they reported ubiquitous interprofessional supervision, albeit limited in scope, which they relied upon for nonjudgmental guidance in their therapeutic decision‐making, especially after‐hours. In our study, interprofessional supervision proved crucial to improving medication safety in the ICU.
- ,,.Resident supervision in the operating room: Does this impact on outcome?J Trauma.1993;35:556–560.
- ,.Supervision in the outpatient clinic: Effects on teaching and patient care.J Gen Intern Med.1993;8:378–380.
- Institute of Medicine (IOM).Resident Duty Hours: Enhancing Sleep, Supervision, and Safety.Washington, DC:National Academic Press;2008.
- Joint Committee of the Group on Resident Affairs and Organization of Resident Representatives. Patient Safety and Graduate Medical Education. Washington, DC: Association of American Medical Colleges; 2003. Available at: https://services.aamc.org/publications/showfile.cfm?file=version13.pdf145:592–598.
- ,,,.Medical errors involving trainees: A study of closed malpractice claims from 5 insurers.Arch Intern Med.2007;167:2030–2036.
- .Resident duty hour reform and mortality in hospitalized patients.JAMA.2007;298:2865–2866.
- ,,,.Progressive independence in clinical training: A tradition worth defending?Acad Med.2005;80:S106–S111.
- ,.Effective supervision in clinical practice settings: A literature review.Med Educ.2000;34:827–840.
- Accreditation Council for Graduate Medical Education. ACGME Residency Review Committee Program Requirements in Critical Care Medicine. 2007. Available at: http://www.acgme.org/acWebsite/downloads/RRC_progReq/142pr707_ims.pdf Accessed August 14, 2009.
- ,.Resident supervision.Accreditation Council for Graduate Medical Education Bulletin.2005; September:15–17. Available at: http://www.acgme.org/acWebsite/bulletin/bulletin09_05. pdf. Accessed March 14,year="2009"2009.
- ,,,,.Resident uncertainty in clinical decision making and impact on patient care: A qualitative study.Qual Saf Health Care.2008;17:122–126.
- ,,, et al.Patterns of communication breakdowns resulting in injury to surgical patients.J Am Coll Surg.2007;204:533–540.
- ,,.Communication failures: An insidious contributor to medical mishaps.Acad Med.2004;79:186–194.
- ,,, et al.Attending doctors' perspectives on how residents learn.Med Educ.2007;41:1050–1058.
- ,,.Teaching but not learning: How medical residency programs handle errors.J Organiz Behav.2006;27:869–896.
- ,,,,.On‐call supervision and resident autonomy: From micromanager to absentee attending.Am J Med.2009;122:784–788.
- ,,,.Preserving professional credibility: Grounded theory study of medical trainees' requests for clinical support.BMJ.2009;338:b128.
- ,,,,,.Who wants feedback? An investigation of the variables influencing residents' feedback‐seeking behavior in relation to night shifts.Acad Med.2009;84:910–917.
- ,,, et al.A look into the nature and causes of human errors in the intensive care unit.Crit Care Med.1995;23:294–300.
- ,,, et al.The Critical Care Safety Study: The incidence and nature of adverse events and serious medical errors in intensive care.Crit Care Med.2005;33:1694–1700.
- ,,,,,.Preventable adverse drug events in hospitalized patients: A comparative study of intensive care and general care units.Crit Care Med.1997;25:1289–1297.
- ,,,,,.Residents report on adverse events and their causes.Arch Intern Med.2005;165:2607–2613.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351:1838–1848.
- ,,,,.Unit‐based clinical pharmacists' prevention of serious medication errors in pediatric inpatients.Am J Health Syst Pharm.2008;65:1254–1260.
- ,,,,.Improving medication safety in the ICU: The pharmacist's role.Hospital Pharmacy.2007;42:337–344.
- ,,,,,.Collaboration between pharmacists, physicians and nurse practitioners: A qualitative investigation of working relationships in the inpatient medical setting.J Interprof Care.2009;23:169–184.
- ,,,.Role of registered nurses in error prevention, discovery and correction.Qual Saf Health Care.2008;17:117–121.
- ,,, et al.Recovery from medical errors: The critical care nursing safety net.Jt Comm J Qual Patient Saf.2006;32:63–72.
- ,,,,.Clinical oversight: Conceptualizing the relationship between supervision and safety.J Gen Intern Med.2007;22:1080–1085.
- .To call or not to call: A judgment of risk by pre‐registration house officers.Med Educ.2008;42:938–944.
- ,.Classifying and interpreting threats to patient safety in hospitals: Insights from aviation.J Organiz Behav.2006;27:919–940.
- .Qualitative Research and Evaluation Methods.3rd ed.Thousand Oaks, CA:Sage Publications;2002.
- ,.Qualitative Data Analysis.2nd. ed.Thousand Oaks, CA:Sage Publications;2006.
- ,.Naturalistic Inquiry.Beverly Hills, CA:Sage Publications;1985.
- ,,.Supervision: A 2‐way street.Arch Intern Med.2008;168:1117.
- ,,, et al.Effects of teamwork training on adverse outcomes and process of care in labor and delivery: A randomized controlled trial.Obstet Gynecol.2007;109:48–55.
- ,,,.Does crew resource management training work? An update, an extension, and some critical needs.Hum Factors.2006;48:392–412.
- ,,,,,.Team training in the neonatal resuscitation program for interns: Teamwork and quality of resuscitations.Pediatrics.2010;125:539–546.
- ,,,,.Medical Teamwork and Patient Safety: The Evidence‐Based Relation.Rockville, MD:Agency for Healthcare Research and Quality 2005. Publication No. 05–0053. Available at: http://www.ahrq.gov/qual/medteam. Accessed October 15,2010.
- ,,.Resident supervision in the operating room: Does this impact on outcome?J Trauma.1993;35:556–560.
- ,.Supervision in the outpatient clinic: Effects on teaching and patient care.J Gen Intern Med.1993;8:378–380.
- Institute of Medicine (IOM).Resident Duty Hours: Enhancing Sleep, Supervision, and Safety.Washington, DC:National Academic Press;2008.
- Joint Committee of the Group on Resident Affairs and Organization of Resident Representatives. Patient Safety and Graduate Medical Education. Washington, DC: Association of American Medical Colleges; 2003. Available at: https://services.aamc.org/publications/showfile.cfm?file=version13.pdf145:592–598.
- ,,,.Medical errors involving trainees: A study of closed malpractice claims from 5 insurers.Arch Intern Med.2007;167:2030–2036.
- .Resident duty hour reform and mortality in hospitalized patients.JAMA.2007;298:2865–2866.
- ,,,.Progressive independence in clinical training: A tradition worth defending?Acad Med.2005;80:S106–S111.
- ,.Effective supervision in clinical practice settings: A literature review.Med Educ.2000;34:827–840.
- Accreditation Council for Graduate Medical Education. ACGME Residency Review Committee Program Requirements in Critical Care Medicine. 2007. Available at: http://www.acgme.org/acWebsite/downloads/RRC_progReq/142pr707_ims.pdf Accessed August 14, 2009.
- ,.Resident supervision.Accreditation Council for Graduate Medical Education Bulletin.2005; September:15–17. Available at: http://www.acgme.org/acWebsite/bulletin/bulletin09_05. pdf. Accessed March 14,year="2009"2009.
- ,,,,.Resident uncertainty in clinical decision making and impact on patient care: A qualitative study.Qual Saf Health Care.2008;17:122–126.
- ,,, et al.Patterns of communication breakdowns resulting in injury to surgical patients.J Am Coll Surg.2007;204:533–540.
- ,,.Communication failures: An insidious contributor to medical mishaps.Acad Med.2004;79:186–194.
- ,,, et al.Attending doctors' perspectives on how residents learn.Med Educ.2007;41:1050–1058.
- ,,.Teaching but not learning: How medical residency programs handle errors.J Organiz Behav.2006;27:869–896.
- ,,,,.On‐call supervision and resident autonomy: From micromanager to absentee attending.Am J Med.2009;122:784–788.
- ,,,.Preserving professional credibility: Grounded theory study of medical trainees' requests for clinical support.BMJ.2009;338:b128.
- ,,,,,.Who wants feedback? An investigation of the variables influencing residents' feedback‐seeking behavior in relation to night shifts.Acad Med.2009;84:910–917.
- ,,, et al.A look into the nature and causes of human errors in the intensive care unit.Crit Care Med.1995;23:294–300.
- ,,, et al.The Critical Care Safety Study: The incidence and nature of adverse events and serious medical errors in intensive care.Crit Care Med.2005;33:1694–1700.
- ,,,,,.Preventable adverse drug events in hospitalized patients: A comparative study of intensive care and general care units.Crit Care Med.1997;25:1289–1297.
- ,,,,,.Residents report on adverse events and their causes.Arch Intern Med.2005;165:2607–2613.
- ,,, et al.Effect of reducing interns' work hours on serious medical errors in intensive care units.N Engl J Med.2004;351:1838–1848.
- ,,,,.Unit‐based clinical pharmacists' prevention of serious medication errors in pediatric inpatients.Am J Health Syst Pharm.2008;65:1254–1260.
- ,,,,.Improving medication safety in the ICU: The pharmacist's role.Hospital Pharmacy.2007;42:337–344.
- ,,,,,.Collaboration between pharmacists, physicians and nurse practitioners: A qualitative investigation of working relationships in the inpatient medical setting.J Interprof Care.2009;23:169–184.
- ,,,.Role of registered nurses in error prevention, discovery and correction.Qual Saf Health Care.2008;17:117–121.
- ,,, et al.Recovery from medical errors: The critical care nursing safety net.Jt Comm J Qual Patient Saf.2006;32:63–72.
- ,,,,.Clinical oversight: Conceptualizing the relationship between supervision and safety.J Gen Intern Med.2007;22:1080–1085.
- .To call or not to call: A judgment of risk by pre‐registration house officers.Med Educ.2008;42:938–944.
- ,.Classifying and interpreting threats to patient safety in hospitals: Insights from aviation.J Organiz Behav.2006;27:919–940.
- .Qualitative Research and Evaluation Methods.3rd ed.Thousand Oaks, CA:Sage Publications;2002.
- ,.Qualitative Data Analysis.2nd. ed.Thousand Oaks, CA:Sage Publications;2006.
- ,.Naturalistic Inquiry.Beverly Hills, CA:Sage Publications;1985.
- ,,.Supervision: A 2‐way street.Arch Intern Med.2008;168:1117.
- ,,, et al.Effects of teamwork training on adverse outcomes and process of care in labor and delivery: A randomized controlled trial.Obstet Gynecol.2007;109:48–55.
- ,,,.Does crew resource management training work? An update, an extension, and some critical needs.Hum Factors.2006;48:392–412.
- ,,,,,.Team training in the neonatal resuscitation program for interns: Teamwork and quality of resuscitations.Pediatrics.2010;125:539–546.
- ,,,,.Medical Teamwork and Patient Safety: The Evidence‐Based Relation.Rockville, MD:Agency for Healthcare Research and Quality 2005. Publication No. 05–0053. Available at: http://www.ahrq.gov/qual/medteam. Accessed October 15,2010.
Copyright © 2011 Society of Hospital Medicine