User login
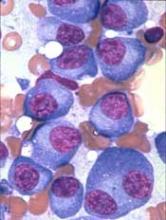
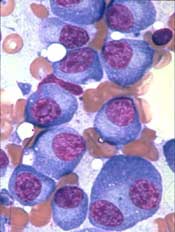
NEW YORK, NY—The B-cell maturation antigen (BCMA) is emerging as a promising target in multiple myeloma (MM), according to Adam D. Cohen, MD, of the University of Pennsylvania in Philadelphia.
BCMA is highly expressed on MM cells and, with its 2 ligands, is responsible for maintaining normal plasma cell homeostasis.
“And it’s really not expressed on any other normal tissues of the body,” Dr Cohen said.
“Importantly, BCMA is not just sitting on the cell surface as a target but actually promotes myeloma pathogenesis.”
Dr Cohen reviewed the progress being made using BCMA as a target in MM, paying particular attention to chimeric antigen receptor (CAR) T cells. He presented the update at Lymphoma & Myeloma 2017.
NCI BCMA-specific CARs
The first CAR to specifically target BCMA in MM was developed at the National Cancer Institute (NCI). It consisted of a murine single-chain variable fragment (scFv), CD3/CD28 signaling domains, and a gamma-retroviral vector.
Investigators conducted the first-in-human trial of this CAR T-cell therapy in 12 relapsed/refractory MM patients.
All patients received a lymphodepleting conditioning regimen of cyclophosphamide and fludarabine and a single infusion of 1 of 4 doses of the CAR T-cell therapy.
At higher dose levels, the BCMA-CAR produced objective responses “even in these highly refractory patients,” Dr Cohen said. “Some responses lasted 4 to 6 months.”
Patients who had the greatest degree of expansion of CAR T cells were the ones who had the best responses.
The BCMA-CAR is associated with the same toxicities as the CD19-directed CAR T-cell therapies now approved in acute lymphoblastic leukemia and non-Hodgkin lymphoma—cytokine release syndrome (CRS) and neurotoxicity.
The NCI study (NCT02215967) is ongoing.
Penn BCMA-specific CAR
A different BCMA CAR is being investigated at the University of Pennsylvania. It is a fully human CAR that consists of a human scFv, CD3/4-1BB costimulatory domains, and a lentiviral vector.
Investigators designed the first-in-human trial* (NCT02546167) with 3 different cohorts.
Patients in cohort 1 received 5 x 108 CAR T cells without any lymphodepleting chemotherapy.
The remaining patients received cyclophosphamide, followed by 5 x 107 CAR T cells in cohort 2 and 5 x 108 CAR T cells in cohort 3.
Dr Cohen reviewed current data from cohort 1, which included 9 patients. They were a median age of 57 (range, 44-70), and 67% were male. They were heavily pretreated with a median of 9 prior lines of therapy (range, 4-11).
All had high-risk cytogenetics, 67% had deletion 17p or TP53 mutation, and they had a median of 80% bone marrow plasma cells (range, 15%-95%).
“Despite this,” Dr Cohen said, “we were able to generate, successfully, CAR T cells from all patients, although 1 patient did require a second apheresis and manufacturing attempt.”
Four of the 9 patients achieved very good partial responses, and an additional 2 patients had minimal responses.
One patient had a stringent CR (sCR) for close to 2 years without having any intervening therapy.
“[The sCR] shows the potential for this [therapy] to create a durable remission in a patient without any other therapy,” Dr Cohen said. “And this patient still has circulating CAR cells detectable.”
Most of the other patients did not have as durable a response. Responses lasted a median of 3 to 5 months before the patients relapsed.
Dr Cohen noted that the Penn data confirm the NCI experience showing proof of principle.
“You can target BCMA with these cells and get objective responses that can lead to a durable one in a subset of patients,” he added.
Dr Cohen is scheduled to report the preliminary data on the cyclophosphamide cohorts (cohorts 2 and 3) at ASH 2017. Those cohorts, he said, are showing a bit more persistence and increased frequency of responses.
Other BCMA-specific CAR trials
Another BCMA CAR, bb2121, consists of a human anti-BCMA scFv, a lentiviral vector, and a CD3/4-1BB costimulatory domain.
In the first-in-human trial of bb2121* (NCT02658929), all 21 patients received cyclophosphamide and fludarabine conditioning first.
There were “very impressive response rates in this study,” Dr Cohen said.
Once patients were dosed at the higher levels of 150 million cells or greater, every patient responded.
“Many responses are still durable,” he pointed out, “some approaching a year.”
LCAR-B38M is structurally different from the other BCMA-specific CARs. It has 2 binding sites for BCMA.
Thirty-five patients enrolled on the trial of LCAR-B38M (NCT03090659), and 19 were evaluable for response.
Patients had a median of 3 or 4 lines of prior therapy. All received cyclophosphamide alone as conditioning.
All 19 evaluable patients responded, and 14 (74%) achieved an sCR.
Dr Cohen noted the differences among the 4 trials: costimulatory domains varied, the Penn study did not require a pre-existing level of BCMA on the MM cells, other studies excluded patients who didn’t meet a certain threshold level of BCMA expression, median lines of prior therapy differed, and conditioning regimens differed as well.
All trials, however, presented data on fewer than 20 patients.
“And so I think it’s a little too early to compare head-to-head between all of these, but they all are really demonstrating promising results so far,” he observed.
Toxicities
“Unfortunately, there’s no free lunch with CAR T cells,” Dr Cohen stated, “and these extraordinary responses do come at the cost of several somewhat unique toxicities that can be serious.”
Toxicities have included:
- Tumor lysis syndrome, which is expected and manageable
- B-cell aplasia, which is not as much of an issue with BCMA as with CD19-directed CAR Ts, since most B cells don’t express BCMA
- Hypogammaglobulinemia, which can be mitigated with IVIG
- CRS, which can be alleviated with tocilizumab
- Neurotoxicity and encephalopathy, which do not occur as frequently as CRS.
“These, I think, are things we still obviously need to learn more about and try to mitigate before this [BCMA-directed CAR therapy] is expanded and brought earlier to patients,” Dr Cohen said.
“The other issues with CAR T cells are logistical. Limited access (the procedure is available at only a few centers); manufacturing can take 2 to 4 weeks, during which time it is difficult to maintain disease control; and the cost is significant.”
“We are really in the early days of CAR cells for myeloma, but, certainly, this appears very bright in terms of its future.” ![]()
* Data from the presentation differ from the abstract.
NEW YORK, NY—The B-cell maturation antigen (BCMA) is emerging as a promising target in multiple myeloma (MM), according to Adam D. Cohen, MD, of the University of Pennsylvania in Philadelphia.
BCMA is highly expressed on MM cells and, with its 2 ligands, is responsible for maintaining normal plasma cell homeostasis.
“And it’s really not expressed on any other normal tissues of the body,” Dr Cohen said.
“Importantly, BCMA is not just sitting on the cell surface as a target but actually promotes myeloma pathogenesis.”
Dr Cohen reviewed the progress being made using BCMA as a target in MM, paying particular attention to chimeric antigen receptor (CAR) T cells. He presented the update at Lymphoma & Myeloma 2017.
NCI BCMA-specific CARs
The first CAR to specifically target BCMA in MM was developed at the National Cancer Institute (NCI). It consisted of a murine single-chain variable fragment (scFv), CD3/CD28 signaling domains, and a gamma-retroviral vector.
Investigators conducted the first-in-human trial of this CAR T-cell therapy in 12 relapsed/refractory MM patients.
All patients received a lymphodepleting conditioning regimen of cyclophosphamide and fludarabine and a single infusion of 1 of 4 doses of the CAR T-cell therapy.
At higher dose levels, the BCMA-CAR produced objective responses “even in these highly refractory patients,” Dr Cohen said. “Some responses lasted 4 to 6 months.”
Patients who had the greatest degree of expansion of CAR T cells were the ones who had the best responses.
The BCMA-CAR is associated with the same toxicities as the CD19-directed CAR T-cell therapies now approved in acute lymphoblastic leukemia and non-Hodgkin lymphoma—cytokine release syndrome (CRS) and neurotoxicity.
The NCI study (NCT02215967) is ongoing.
Penn BCMA-specific CAR
A different BCMA CAR is being investigated at the University of Pennsylvania. It is a fully human CAR that consists of a human scFv, CD3/4-1BB costimulatory domains, and a lentiviral vector.
Investigators designed the first-in-human trial* (NCT02546167) with 3 different cohorts.
Patients in cohort 1 received 5 x 108 CAR T cells without any lymphodepleting chemotherapy.
The remaining patients received cyclophosphamide, followed by 5 x 107 CAR T cells in cohort 2 and 5 x 108 CAR T cells in cohort 3.
Dr Cohen reviewed current data from cohort 1, which included 9 patients. They were a median age of 57 (range, 44-70), and 67% were male. They were heavily pretreated with a median of 9 prior lines of therapy (range, 4-11).
All had high-risk cytogenetics, 67% had deletion 17p or TP53 mutation, and they had a median of 80% bone marrow plasma cells (range, 15%-95%).
“Despite this,” Dr Cohen said, “we were able to generate, successfully, CAR T cells from all patients, although 1 patient did require a second apheresis and manufacturing attempt.”
Four of the 9 patients achieved very good partial responses, and an additional 2 patients had minimal responses.
One patient had a stringent CR (sCR) for close to 2 years without having any intervening therapy.
“[The sCR] shows the potential for this [therapy] to create a durable remission in a patient without any other therapy,” Dr Cohen said. “And this patient still has circulating CAR cells detectable.”
Most of the other patients did not have as durable a response. Responses lasted a median of 3 to 5 months before the patients relapsed.
Dr Cohen noted that the Penn data confirm the NCI experience showing proof of principle.
“You can target BCMA with these cells and get objective responses that can lead to a durable one in a subset of patients,” he added.
Dr Cohen is scheduled to report the preliminary data on the cyclophosphamide cohorts (cohorts 2 and 3) at ASH 2017. Those cohorts, he said, are showing a bit more persistence and increased frequency of responses.
Other BCMA-specific CAR trials
Another BCMA CAR, bb2121, consists of a human anti-BCMA scFv, a lentiviral vector, and a CD3/4-1BB costimulatory domain.
In the first-in-human trial of bb2121* (NCT02658929), all 21 patients received cyclophosphamide and fludarabine conditioning first.
There were “very impressive response rates in this study,” Dr Cohen said.
Once patients were dosed at the higher levels of 150 million cells or greater, every patient responded.
“Many responses are still durable,” he pointed out, “some approaching a year.”
LCAR-B38M is structurally different from the other BCMA-specific CARs. It has 2 binding sites for BCMA.
Thirty-five patients enrolled on the trial of LCAR-B38M (NCT03090659), and 19 were evaluable for response.
Patients had a median of 3 or 4 lines of prior therapy. All received cyclophosphamide alone as conditioning.
All 19 evaluable patients responded, and 14 (74%) achieved an sCR.
Dr Cohen noted the differences among the 4 trials: costimulatory domains varied, the Penn study did not require a pre-existing level of BCMA on the MM cells, other studies excluded patients who didn’t meet a certain threshold level of BCMA expression, median lines of prior therapy differed, and conditioning regimens differed as well.
All trials, however, presented data on fewer than 20 patients.
“And so I think it’s a little too early to compare head-to-head between all of these, but they all are really demonstrating promising results so far,” he observed.
Toxicities
“Unfortunately, there’s no free lunch with CAR T cells,” Dr Cohen stated, “and these extraordinary responses do come at the cost of several somewhat unique toxicities that can be serious.”
Toxicities have included:
- Tumor lysis syndrome, which is expected and manageable
- B-cell aplasia, which is not as much of an issue with BCMA as with CD19-directed CAR Ts, since most B cells don’t express BCMA
- Hypogammaglobulinemia, which can be mitigated with IVIG
- CRS, which can be alleviated with tocilizumab
- Neurotoxicity and encephalopathy, which do not occur as frequently as CRS.
“These, I think, are things we still obviously need to learn more about and try to mitigate before this [BCMA-directed CAR therapy] is expanded and brought earlier to patients,” Dr Cohen said.
“The other issues with CAR T cells are logistical. Limited access (the procedure is available at only a few centers); manufacturing can take 2 to 4 weeks, during which time it is difficult to maintain disease control; and the cost is significant.”
“We are really in the early days of CAR cells for myeloma, but, certainly, this appears very bright in terms of its future.” ![]()
* Data from the presentation differ from the abstract.
NEW YORK, NY—The B-cell maturation antigen (BCMA) is emerging as a promising target in multiple myeloma (MM), according to Adam D. Cohen, MD, of the University of Pennsylvania in Philadelphia.
BCMA is highly expressed on MM cells and, with its 2 ligands, is responsible for maintaining normal plasma cell homeostasis.
“And it’s really not expressed on any other normal tissues of the body,” Dr Cohen said.
“Importantly, BCMA is not just sitting on the cell surface as a target but actually promotes myeloma pathogenesis.”
Dr Cohen reviewed the progress being made using BCMA as a target in MM, paying particular attention to chimeric antigen receptor (CAR) T cells. He presented the update at Lymphoma & Myeloma 2017.
NCI BCMA-specific CARs
The first CAR to specifically target BCMA in MM was developed at the National Cancer Institute (NCI). It consisted of a murine single-chain variable fragment (scFv), CD3/CD28 signaling domains, and a gamma-retroviral vector.
Investigators conducted the first-in-human trial of this CAR T-cell therapy in 12 relapsed/refractory MM patients.
All patients received a lymphodepleting conditioning regimen of cyclophosphamide and fludarabine and a single infusion of 1 of 4 doses of the CAR T-cell therapy.
At higher dose levels, the BCMA-CAR produced objective responses “even in these highly refractory patients,” Dr Cohen said. “Some responses lasted 4 to 6 months.”
Patients who had the greatest degree of expansion of CAR T cells were the ones who had the best responses.
The BCMA-CAR is associated with the same toxicities as the CD19-directed CAR T-cell therapies now approved in acute lymphoblastic leukemia and non-Hodgkin lymphoma—cytokine release syndrome (CRS) and neurotoxicity.
The NCI study (NCT02215967) is ongoing.
Penn BCMA-specific CAR
A different BCMA CAR is being investigated at the University of Pennsylvania. It is a fully human CAR that consists of a human scFv, CD3/4-1BB costimulatory domains, and a lentiviral vector.
Investigators designed the first-in-human trial* (NCT02546167) with 3 different cohorts.
Patients in cohort 1 received 5 x 108 CAR T cells without any lymphodepleting chemotherapy.
The remaining patients received cyclophosphamide, followed by 5 x 107 CAR T cells in cohort 2 and 5 x 108 CAR T cells in cohort 3.
Dr Cohen reviewed current data from cohort 1, which included 9 patients. They were a median age of 57 (range, 44-70), and 67% were male. They were heavily pretreated with a median of 9 prior lines of therapy (range, 4-11).
All had high-risk cytogenetics, 67% had deletion 17p or TP53 mutation, and they had a median of 80% bone marrow plasma cells (range, 15%-95%).
“Despite this,” Dr Cohen said, “we were able to generate, successfully, CAR T cells from all patients, although 1 patient did require a second apheresis and manufacturing attempt.”
Four of the 9 patients achieved very good partial responses, and an additional 2 patients had minimal responses.
One patient had a stringent CR (sCR) for close to 2 years without having any intervening therapy.
“[The sCR] shows the potential for this [therapy] to create a durable remission in a patient without any other therapy,” Dr Cohen said. “And this patient still has circulating CAR cells detectable.”
Most of the other patients did not have as durable a response. Responses lasted a median of 3 to 5 months before the patients relapsed.
Dr Cohen noted that the Penn data confirm the NCI experience showing proof of principle.
“You can target BCMA with these cells and get objective responses that can lead to a durable one in a subset of patients,” he added.
Dr Cohen is scheduled to report the preliminary data on the cyclophosphamide cohorts (cohorts 2 and 3) at ASH 2017. Those cohorts, he said, are showing a bit more persistence and increased frequency of responses.
Other BCMA-specific CAR trials
Another BCMA CAR, bb2121, consists of a human anti-BCMA scFv, a lentiviral vector, and a CD3/4-1BB costimulatory domain.
In the first-in-human trial of bb2121* (NCT02658929), all 21 patients received cyclophosphamide and fludarabine conditioning first.
There were “very impressive response rates in this study,” Dr Cohen said.
Once patients were dosed at the higher levels of 150 million cells or greater, every patient responded.
“Many responses are still durable,” he pointed out, “some approaching a year.”
LCAR-B38M is structurally different from the other BCMA-specific CARs. It has 2 binding sites for BCMA.
Thirty-five patients enrolled on the trial of LCAR-B38M (NCT03090659), and 19 were evaluable for response.
Patients had a median of 3 or 4 lines of prior therapy. All received cyclophosphamide alone as conditioning.
All 19 evaluable patients responded, and 14 (74%) achieved an sCR.
Dr Cohen noted the differences among the 4 trials: costimulatory domains varied, the Penn study did not require a pre-existing level of BCMA on the MM cells, other studies excluded patients who didn’t meet a certain threshold level of BCMA expression, median lines of prior therapy differed, and conditioning regimens differed as well.
All trials, however, presented data on fewer than 20 patients.
“And so I think it’s a little too early to compare head-to-head between all of these, but they all are really demonstrating promising results so far,” he observed.
Toxicities
“Unfortunately, there’s no free lunch with CAR T cells,” Dr Cohen stated, “and these extraordinary responses do come at the cost of several somewhat unique toxicities that can be serious.”
Toxicities have included:
- Tumor lysis syndrome, which is expected and manageable
- B-cell aplasia, which is not as much of an issue with BCMA as with CD19-directed CAR Ts, since most B cells don’t express BCMA
- Hypogammaglobulinemia, which can be mitigated with IVIG
- CRS, which can be alleviated with tocilizumab
- Neurotoxicity and encephalopathy, which do not occur as frequently as CRS.
“These, I think, are things we still obviously need to learn more about and try to mitigate before this [BCMA-directed CAR therapy] is expanded and brought earlier to patients,” Dr Cohen said.
“The other issues with CAR T cells are logistical. Limited access (the procedure is available at only a few centers); manufacturing can take 2 to 4 weeks, during which time it is difficult to maintain disease control; and the cost is significant.”
“We are really in the early days of CAR cells for myeloma, but, certainly, this appears very bright in terms of its future.” ![]()
* Data from the presentation differ from the abstract.