User login
The evolution of coronary artery bypass grafting (CABG) has been a key component in significantly reducing the morbidity and mortality associated with occlusive coronary artery disease (CAD). Cleveland Clinic surgeons, through their technical interventions and innovations, have led the evolution in coronary revascularization starting in the 1960s and continuing today. This article provides a brief overview of the evolution and describes the issues associated with current CABG approaches.
EARLY WORK IN RECONSTRUCTIVE CORONARY ARTERY SURGERY
Results from the first large series of venous grafting for CAD were reported in 1970 by Favaloro and colleagues at Cleveland Clinic.1 They showed the efficacy of grafting in treating CAD, with low associated morbidity and mortality, thus establishing this surgery as the treatment modality for CAD.
The technique of surgical myocardial revascularization was a culmination of developments that began years earlier with the Vineberg procedure, involving suturing of the mammary artery to the muscle rather than a vessel-to-vessel anastomosis. From this followed the coronary patch, end-to-end bypass, and then end-to-side bypass.
In the 1970s, the refinement of suturing the left internal mammary artery (LIMA) directly to the left anterior descending (LAD) artery using magnifying loops was pioneered and popularized at Cleveland Clinic. This later became the cornerstone of future coronary revascularizations.
As a direct result of the successful technical advances and excellent clinical outcomes, the volume of CABG procedures in the United States rose steadily during the 1980s and reached its peak in 1995. It then began a slow decline that continued until 2013, when the trend began to reverse. It was still rising through 2015.
WHY THE RENEWED INTEREST IN CABG?
A key component to continued use of CABG is that it appears to have a clinical edge over other treatments. This has been shown in several high-profile studies: SYNTAX,2,3 FREEDOM,4,5 BEST,6 and NOBLE.7 For example, in the SYNTAX trial, which compared CABG vs percutaneous coronary intervention (PCI), the conclusion from both the 1-year2 and the 5-year3 results was that CABG should remain the standard of care for patients with complex lesions—those with an intermediate or high burden of CAD.
The 5-year outcomes showed that the rate of major adverse cardiac and cerebrovascular events favored CABG over PCI (26.9% vs 37.3%, respectively; P < .0001).3 All-cause mortality, although not statistically significant, also was better for CABG (11.4% vs 13.9%). This indicates that as the complexity and burden of disease increase, the benefit of CABG over PCI becomes more prominent. In short, the worse the disease, the better the results with CABG.
Why is CABG better?
One rationale is that CABG not only bypasses the culprit-lesion vessel, it also protects against future lesions. An elegant study published in 2010 showed that in most cases of acute myocardial infarction (MI), the culprit coronary lesion is in the first 7 cm of the LAD.8 With CABG, most distal anastomoses are beyond 7 cm and, thus, are beyond the location of the vast majority of potential future culprit lesions.
An important factor is the modern-day safety record of CABG. According to the Society of Thoracic
Surgeons Adult Cardiac Surgery Database,9 in 2016 the expected operative mortality for CABG was just over 2%. At the Cleveland Clinic, CABG mortality has consistently been below 1% despite the complexity of the cases and the higher percentage of reoperations performed at the Clinic. In addition, the low incidence of major complications after CABG has contributed to its endurance as an important therapeutic option for CAD over the decades.
IMPROVING LONG-TERM CABG OUTCOMES
Improving vein graft patency
The Achilles heel of CABG is the decline of patency of saphenous vein grafts. The occlusion rate of these veins is 6% to 8% at hospital discharge and approximately 10% at 1 year after CABG. By 10 years, half of the vein grafts are diseased or occluded, with progression of atherosclerotic disease over time.
There has been controversy about whether open harvesting of the saphenous vein is better than endoscopic vein harvesting for patency-related outcomes. This arose after the publication of an ad hoc analysis that gave poor marks to endoscopic vein-graft harvesting.10 Its major finding was that endoscopic vein harvesting had higher rates of vein-graft failure at 12 to 18 months than open vein harvesting (46.7% vs 38.0%, respectively; P < .001). At 3 years, endoscopic harvesting was associated with higher rates of death, MI, or repeat revascularization (20.2% vs 17.4%, P = .04).
A US Food and Drug Administration-sanctioned Society of Thoracic Surgeons observational study, however, reviewed outcomes from 235,394 patients who underwent CABG from 2003 through 2008 and found no significant increase in 5-year mortality rates with use of endoscopic vein-graft harvesting vs open harvesting.11 This study showed that the less invasive endoscopic approach is still an option.
In 2015, Taggart and colleagues12 reported on a pioneering procedure that wraps the saphenous vein graft with a stent. Initial results showed external stenting had the potential to improve vein-graft lumen and reduce intimal hyperplasia at 1 year postoperatively. Surgeons can expect more data on this technology in the future.
COMPARING CONDUIT OPTIONS FOR CABG
Arterial vs venous grafts
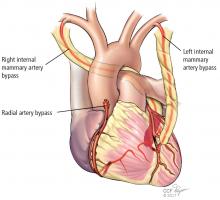
The 1986 report by Loop and colleagues from Cleveland Clinic showed that the patency of the mammary artery graft was superior to that of the saphenous vein and that patients receiving a mammary bypass had significantly better 10-year survival (82.6% vs 71.0%, respectively; P < .0001).13 The findings of this landmark study established the LIMA-to-LAD bypass as the technical standard for surgical coronary revascularization.
Single vs bilateral mammary artery grafts
In December 2016, results of the Arterial Revascularization Trial (ART) were published comparing single vs double mammary artery grafts.14 In this prospective randomized trial, the 5-year results showed no significant difference between these mammary grafts in terms of all-cause mortality, MI, or stroke. Bilateral mammary artery grafts, however, were associated with a higher risk of sternal wound complications (3.5% vs 1.9%, respectively; P = .005) and sternal reconstruction (1.9% vs 0.6%; P = .002).
Radial artery vs saphenous vein grafts
In the largest randomized study comparing these two graft options,16 the 1-year results showed no difference in graft patency; a follow-up analysis is in progress. In contrast, randomized studies from Canada17 and the United Kingdom18 suggest that there are potential benefits associated with use of radial artery grafts in terms of patency and clinical outcomes. In addition, observational data from centers experienced in radial artery grafting have demonstrated favorable outcomes. Radial arteries perform best when bypassing totally occluded or severely stenotic vessels in which there is no or little risk of competitive flow from the native circulation.
Right internal mammary vs radial artery grafts
A propensity-matched comparison study looking at multiple studies (N = 15,374 patients) concluded that use of the right internal mammary artery provides better outcomes.19 It was associated with a 25% risk reduction for late death and a 63% risk reduction for repeat vascularization, both statistically significant vs the radial artery rates. But there is a randomized study showing that the radial artery is as good as or better than the right internal mammary artery. At this point, it is not clear which artery is better as an adjunct for the LIMA-to-LAD bypass.
GUIDELINES FOR GRAFT SELECTION
In 2016, the Society of Thoracic Surgeons published guidelines that encouraged the use of arterial grafts, giving it a class IIa designation, meaning that the evidence indicates it is reasonable to consider.20
The guidelines note the following:
- The internal mammary artery should be used to bypass the LAD when bypass of the LAD is indicated.
- As an adjunct to the left internal mammary artery, a second arterial graft (the right internal mammary artery or radial artery) should be considered in appropriate patients.
- Use of bilateral internal mammary arteries should be considered in patients who are not at high risk for sternal complications.
COMPARING SURGICAL APPROACHES
Traditional CABG performed via median sternotomy and with the use of cardiopulmonary bypass remains the technical standard in surgical coronary revascularization. However, technologies have allowed surgeons to use different and sometimes less invasive approaches that may have good outcomes in select patients with suitable risk profiles and favorable coronary anatomies.
On-pump vs off-pump CABG
The popularity of CABG without cardiopulmonary bypass (“off-pump”) peaked in 2002, when it constituted approximately 23% of CABG procedures and then declined to 17% by 2012.21 The ROOBY (Veterans Affairs Randomized On/Off Bypass) trial of 2,203 VA patients showed that at 1 year, those in the off-pump group had worse composite outcomes, poorer graft patency, and greater incidence of incomplete revascularization than the on-pump group.22 However, the use of off-pump CABG was vindicated in two other trials—CORONARY and GOPCABE—in which experienced surgeons in high-volume centers with high-risk patients had no difference in outcomes at 1 and 5 years.23–25 The recommendation is to tailor the procedure to the patient rather than the patient to the procedure. The best option is always to do what is right for the patient. For example, patients with diseased ascending aortas or liver disease may benefit from an off-pump approach.
MINIMALLY INVASIVE CABG
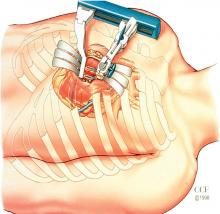
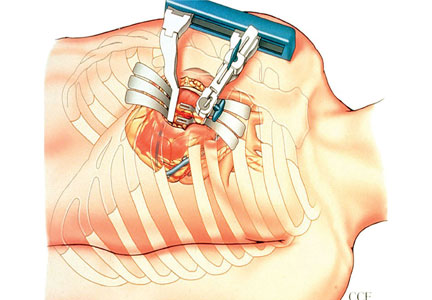
Robotic CABG
This procedure has advantages and disadvantages. The advantages are primarily related to the minimally invasive approach:
- There is no surgeon hand tremor
- It is less invasive
- It provides better cosmetic results
- It is expected to result in less pain, fewer transfusions, fewer complications, and shorter length of hospital stay, although those have not been proven.
Disadvantages include the following:
- Compromised completeness of revascularization—with some “difficult” vessels left unbypassed
- Longer operative times
- Higher cost
- Concern about graft patency with inexperienced surgeons
- Higher-than-expected mortality in some reports.
In 2013, a study of 500 patients treated with robotic totally endoscopic CABG showed that this procedure could be safe and effective, although the best outcomes were achieved in patients with less severe disease requiring fewer bypasses.26 In other words, it is more appropriate for LIMA-to-LAD suturing and less complex anatomy, and it is best performed with cardiopulmonary bypass with the heart arrested.
Hybrid revascularization
This procedure is a combination of minimally invasive CABG (MIDCAB or robotic CABG) to revascularize the LAD and PCI to treat the remaining vessels in multivessel CAD. The CABG and PCI can be concurrent or staged. The hybrid approach has the attraction of being less invasive and uses the technical standard LIMA-to-LAD approach, but it has the obvious limitation of not incorporating additional arterial grafting and the possibility of a compromised technical outcome in less experienced hands.
A collaborative task force from several cardiovascular medical societies developed evidence-based guidelines to address the hybrid coronary revascularization approach. They give it a class IIa recommendation, indicating that it is a reasonable approach to treating patients in whom there are limitations and challenges to traditional CABG. For other patients, they gave it a class IIb recommendation, indicating that it may be reasonable to use as an alternative to multivessel PCI or CABG.27
THE EVOLUTION CONTINUES: CABG VS PCI
As CABG and PCI continue to evolve, surgical approaches to CAD are becoming more sophisticated with the use of more arterial conduits, less invasive surgical approaches, and development of new types of stents for PCI; however, expect the debate to continue regarding which approach to CAD is best. This is not a battle between surgical and nonsurgical specialties. Rather, the goal should be an amicable, collaborative heart-care team. After all, the most important question is, as always, which therapy is best for the individual patient.
- Sheldon WC, Favaloro RG, Sones FM Jr, Effler DB. Reconstructive coronary artery surgery: venous autograft technique. JAMA 1970; 213:78–82.
- Serruys PW, Morice M-C, Kappetein AP, et al; for the SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009; 360:961–972.
- Mohr FW, Morice M-C, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 2013; 381:629–638.
- Farkouh ME, Domanski M, Sleeper LA, et al; for the FREEDOM Trial Investigators. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012; 367:2375–2384.
- Dangas GD, Farkouh ME, Sleeper LA, et al; for the FREEDOM Investigators. Long-term outcome of PCI versus CABG in insulin and non-insulin-treated diabetic patients: results from the FREEDOM trial. J Am Coll Cardiol 2014; 64:1189–1197.
- Park S-J, Ahn J-M, Kim Y-H, et al; for the BEST Trial Investigators. Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med 2015; 372:1204–1212.
- Mäkikallio T, Holm NR, Lindsay M, et al; for the NOBLE study investigators. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet 2016; 388:2743–2752.
- Jeon C, Candia SC, Wang JC, et al. Relative spatial distributions of coronary artery bypass graft insertion and acute thrombosis: a model for protection from acute myocardial infarction. Am Heart J 2010; 160:195–201.
- The Society of Thoracic Surgeons and Duke Clinical Research Institute. Adult cardiac surgery database: executive summary (10 years—STS period ending March 31, 2016). https://www.sts.org/sites/default/files/documents/2016Harvest2_ExecutiveSummary_new.pdf. Accessed March 10, 2017.
- Lopes RD, Hafley GE, Allen KB, et al. Endoscopic versus open vein-graft harvesting in coronary-artery bypass surgery. N Engl J Med 2009; 361:235–244.
- Williams JB, Peterson ED, Brennan JM, et al. Association between endoscopic vs open vein-graft harvesting and mortality, wound complications, and cardiovascular events in patients undergoing CABG surgery. JAMA 2012; 308:475–484.
- Taggart DP, Ben Gal Y, Lees B, et al. A randomized trial of external stenting for saphenous vein grafts in coronary artery bypass grafting. Ann Thorac Surg 2015; 99:2039–2045.
- Loop FD, Lytle BW, Cosgrove DM, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med 1986; 314:1–6.
- Taggart DP, Gray AM, et al; for the ART Investigators. Randomized trial of bilateral versus single internal-thoracic-artery grafts. N Engl J Med 2016; 375:2540–2549.
- Lytle BW, Blackstone EH, Sabik JF, et al. The effect of bilateral internal thoracic artery grafting on survival during 20 postoperative years. Ann Thorac Surg 2004; 78:2005–2012; discussion 2012–2014.
- Goldman S, Sethi GK, Holman W, et al. Radial artery grafts vs saphenous vein grafts in coronary artery bypass surgery: a randomized trial. JAMA 2011; 305:167–174.
- Desai ND, Cohen EA, Naylor CD, Fremes SE; for the Radial Artery Patency Study Investigators. A randomized comparison of radial-artery and saphenous-vein coronary bypass grafts. N Engl J Med 2004; 351:2302–2309.
- Collins P, Webb CM, Chong CF, Moat NE; for the Radial Artery Versus Saphenous Vein Patency (RSVP) Trial Investigators. Radial artery versus saphenous vein patency randomized trial: five-year angiographic follow-up. Circulation 2008; 117:2859–2864.
- Benedetto U, Caputo M, Gaudino M, et al. Right internal thoracic artery or radial artery? A propensity-matched comparison on the second-best arterial conduit. J Thorac Cardiovasc Surg 2017; 153:79–88.
- Aldea GS, Bakaeen FG, Pal J, et al. The Society of Thoracic Surgeons clinical practice guidelines on arterial conduits for coronary artery bypass grafting. Ann Thorac Surg 2016; 101:801–809.
- Bakaeen FG, Shroyer AL, Gammie JS, et al. Trends in use of off-pump coronary artery bypass grafting: results from the Society of Thoracic Surgeons Adult Cardiac Surgery Database. J Thorac Cardiovasc Surg 2014; 148:856–864.
- Shroyer AL, Grover FL, Hattler B, et al; for the Veterans Affairs Randomized On/Off Bypass (ROOBY) Study Group. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 2009; 361:1827–1837.
- Diegeler A, Börgermann J, Kappert U, et al; for the GOPCABE Study Group. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med 2013; 368:1189–1198.
Lamy A, Devereaux PJ, Prabhakaran D, et al; for the CORONARY Investigators. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med 2013; 368:1179–1188. - Lamy A, Devereaux PJ, Prabhakaran D, et al; for the CORONARY Investigators. Five-year outcomes after off-pump or on-pump coronary-artery bypass grafting. N Engl J Med 2016; 375:2359–2368.
- Bonaros N, Schachner T, Lehr E, et al. Five hundred cases of robotic totally endoscopic coronary artery bypass grafting: predictors of success and safety. Ann Thorac Surg 2013; 95:803–812.
- Fihn SD, Gardin JM, Abrams J, et al; American College of Cardiology Foundation/American Heart Association Task Force. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2012; 126:e354–e471.
The evolution of coronary artery bypass grafting (CABG) has been a key component in significantly reducing the morbidity and mortality associated with occlusive coronary artery disease (CAD). Cleveland Clinic surgeons, through their technical interventions and innovations, have led the evolution in coronary revascularization starting in the 1960s and continuing today. This article provides a brief overview of the evolution and describes the issues associated with current CABG approaches.
EARLY WORK IN RECONSTRUCTIVE CORONARY ARTERY SURGERY
Results from the first large series of venous grafting for CAD were reported in 1970 by Favaloro and colleagues at Cleveland Clinic.1 They showed the efficacy of grafting in treating CAD, with low associated morbidity and mortality, thus establishing this surgery as the treatment modality for CAD.
The technique of surgical myocardial revascularization was a culmination of developments that began years earlier with the Vineberg procedure, involving suturing of the mammary artery to the muscle rather than a vessel-to-vessel anastomosis. From this followed the coronary patch, end-to-end bypass, and then end-to-side bypass.
In the 1970s, the refinement of suturing the left internal mammary artery (LIMA) directly to the left anterior descending (LAD) artery using magnifying loops was pioneered and popularized at Cleveland Clinic. This later became the cornerstone of future coronary revascularizations.
As a direct result of the successful technical advances and excellent clinical outcomes, the volume of CABG procedures in the United States rose steadily during the 1980s and reached its peak in 1995. It then began a slow decline that continued until 2013, when the trend began to reverse. It was still rising through 2015.
WHY THE RENEWED INTEREST IN CABG?
A key component to continued use of CABG is that it appears to have a clinical edge over other treatments. This has been shown in several high-profile studies: SYNTAX,2,3 FREEDOM,4,5 BEST,6 and NOBLE.7 For example, in the SYNTAX trial, which compared CABG vs percutaneous coronary intervention (PCI), the conclusion from both the 1-year2 and the 5-year3 results was that CABG should remain the standard of care for patients with complex lesions—those with an intermediate or high burden of CAD.
The 5-year outcomes showed that the rate of major adverse cardiac and cerebrovascular events favored CABG over PCI (26.9% vs 37.3%, respectively; P < .0001).3 All-cause mortality, although not statistically significant, also was better for CABG (11.4% vs 13.9%). This indicates that as the complexity and burden of disease increase, the benefit of CABG over PCI becomes more prominent. In short, the worse the disease, the better the results with CABG.
Why is CABG better?
One rationale is that CABG not only bypasses the culprit-lesion vessel, it also protects against future lesions. An elegant study published in 2010 showed that in most cases of acute myocardial infarction (MI), the culprit coronary lesion is in the first 7 cm of the LAD.8 With CABG, most distal anastomoses are beyond 7 cm and, thus, are beyond the location of the vast majority of potential future culprit lesions.
An important factor is the modern-day safety record of CABG. According to the Society of Thoracic
Surgeons Adult Cardiac Surgery Database,9 in 2016 the expected operative mortality for CABG was just over 2%. At the Cleveland Clinic, CABG mortality has consistently been below 1% despite the complexity of the cases and the higher percentage of reoperations performed at the Clinic. In addition, the low incidence of major complications after CABG has contributed to its endurance as an important therapeutic option for CAD over the decades.
IMPROVING LONG-TERM CABG OUTCOMES
Improving vein graft patency
The Achilles heel of CABG is the decline of patency of saphenous vein grafts. The occlusion rate of these veins is 6% to 8% at hospital discharge and approximately 10% at 1 year after CABG. By 10 years, half of the vein grafts are diseased or occluded, with progression of atherosclerotic disease over time.
There has been controversy about whether open harvesting of the saphenous vein is better than endoscopic vein harvesting for patency-related outcomes. This arose after the publication of an ad hoc analysis that gave poor marks to endoscopic vein-graft harvesting.10 Its major finding was that endoscopic vein harvesting had higher rates of vein-graft failure at 12 to 18 months than open vein harvesting (46.7% vs 38.0%, respectively; P < .001). At 3 years, endoscopic harvesting was associated with higher rates of death, MI, or repeat revascularization (20.2% vs 17.4%, P = .04).
A US Food and Drug Administration-sanctioned Society of Thoracic Surgeons observational study, however, reviewed outcomes from 235,394 patients who underwent CABG from 2003 through 2008 and found no significant increase in 5-year mortality rates with use of endoscopic vein-graft harvesting vs open harvesting.11 This study showed that the less invasive endoscopic approach is still an option.
In 2015, Taggart and colleagues12 reported on a pioneering procedure that wraps the saphenous vein graft with a stent. Initial results showed external stenting had the potential to improve vein-graft lumen and reduce intimal hyperplasia at 1 year postoperatively. Surgeons can expect more data on this technology in the future.
COMPARING CONDUIT OPTIONS FOR CABG
Arterial vs venous grafts
The 1986 report by Loop and colleagues from Cleveland Clinic showed that the patency of the mammary artery graft was superior to that of the saphenous vein and that patients receiving a mammary bypass had significantly better 10-year survival (82.6% vs 71.0%, respectively; P < .0001).13 The findings of this landmark study established the LIMA-to-LAD bypass as the technical standard for surgical coronary revascularization.
Single vs bilateral mammary artery grafts
In December 2016, results of the Arterial Revascularization Trial (ART) were published comparing single vs double mammary artery grafts.14 In this prospective randomized trial, the 5-year results showed no significant difference between these mammary grafts in terms of all-cause mortality, MI, or stroke. Bilateral mammary artery grafts, however, were associated with a higher risk of sternal wound complications (3.5% vs 1.9%, respectively; P = .005) and sternal reconstruction (1.9% vs 0.6%; P = .002).
Radial artery vs saphenous vein grafts
In the largest randomized study comparing these two graft options,16 the 1-year results showed no difference in graft patency; a follow-up analysis is in progress. In contrast, randomized studies from Canada17 and the United Kingdom18 suggest that there are potential benefits associated with use of radial artery grafts in terms of patency and clinical outcomes. In addition, observational data from centers experienced in radial artery grafting have demonstrated favorable outcomes. Radial arteries perform best when bypassing totally occluded or severely stenotic vessels in which there is no or little risk of competitive flow from the native circulation.
Right internal mammary vs radial artery grafts
A propensity-matched comparison study looking at multiple studies (N = 15,374 patients) concluded that use of the right internal mammary artery provides better outcomes.19 It was associated with a 25% risk reduction for late death and a 63% risk reduction for repeat vascularization, both statistically significant vs the radial artery rates. But there is a randomized study showing that the radial artery is as good as or better than the right internal mammary artery. At this point, it is not clear which artery is better as an adjunct for the LIMA-to-LAD bypass.
GUIDELINES FOR GRAFT SELECTION
In 2016, the Society of Thoracic Surgeons published guidelines that encouraged the use of arterial grafts, giving it a class IIa designation, meaning that the evidence indicates it is reasonable to consider.20
The guidelines note the following:
- The internal mammary artery should be used to bypass the LAD when bypass of the LAD is indicated.
- As an adjunct to the left internal mammary artery, a second arterial graft (the right internal mammary artery or radial artery) should be considered in appropriate patients.
- Use of bilateral internal mammary arteries should be considered in patients who are not at high risk for sternal complications.
COMPARING SURGICAL APPROACHES
Traditional CABG performed via median sternotomy and with the use of cardiopulmonary bypass remains the technical standard in surgical coronary revascularization. However, technologies have allowed surgeons to use different and sometimes less invasive approaches that may have good outcomes in select patients with suitable risk profiles and favorable coronary anatomies.
On-pump vs off-pump CABG
The popularity of CABG without cardiopulmonary bypass (“off-pump”) peaked in 2002, when it constituted approximately 23% of CABG procedures and then declined to 17% by 2012.21 The ROOBY (Veterans Affairs Randomized On/Off Bypass) trial of 2,203 VA patients showed that at 1 year, those in the off-pump group had worse composite outcomes, poorer graft patency, and greater incidence of incomplete revascularization than the on-pump group.22 However, the use of off-pump CABG was vindicated in two other trials—CORONARY and GOPCABE—in which experienced surgeons in high-volume centers with high-risk patients had no difference in outcomes at 1 and 5 years.23–25 The recommendation is to tailor the procedure to the patient rather than the patient to the procedure. The best option is always to do what is right for the patient. For example, patients with diseased ascending aortas or liver disease may benefit from an off-pump approach.
MINIMALLY INVASIVE CABG
Robotic CABG
This procedure has advantages and disadvantages. The advantages are primarily related to the minimally invasive approach:
- There is no surgeon hand tremor
- It is less invasive
- It provides better cosmetic results
- It is expected to result in less pain, fewer transfusions, fewer complications, and shorter length of hospital stay, although those have not been proven.
Disadvantages include the following:
- Compromised completeness of revascularization—with some “difficult” vessels left unbypassed
- Longer operative times
- Higher cost
- Concern about graft patency with inexperienced surgeons
- Higher-than-expected mortality in some reports.
In 2013, a study of 500 patients treated with robotic totally endoscopic CABG showed that this procedure could be safe and effective, although the best outcomes were achieved in patients with less severe disease requiring fewer bypasses.26 In other words, it is more appropriate for LIMA-to-LAD suturing and less complex anatomy, and it is best performed with cardiopulmonary bypass with the heart arrested.
Hybrid revascularization
This procedure is a combination of minimally invasive CABG (MIDCAB or robotic CABG) to revascularize the LAD and PCI to treat the remaining vessels in multivessel CAD. The CABG and PCI can be concurrent or staged. The hybrid approach has the attraction of being less invasive and uses the technical standard LIMA-to-LAD approach, but it has the obvious limitation of not incorporating additional arterial grafting and the possibility of a compromised technical outcome in less experienced hands.
A collaborative task force from several cardiovascular medical societies developed evidence-based guidelines to address the hybrid coronary revascularization approach. They give it a class IIa recommendation, indicating that it is a reasonable approach to treating patients in whom there are limitations and challenges to traditional CABG. For other patients, they gave it a class IIb recommendation, indicating that it may be reasonable to use as an alternative to multivessel PCI or CABG.27
THE EVOLUTION CONTINUES: CABG VS PCI
As CABG and PCI continue to evolve, surgical approaches to CAD are becoming more sophisticated with the use of more arterial conduits, less invasive surgical approaches, and development of new types of stents for PCI; however, expect the debate to continue regarding which approach to CAD is best. This is not a battle between surgical and nonsurgical specialties. Rather, the goal should be an amicable, collaborative heart-care team. After all, the most important question is, as always, which therapy is best for the individual patient.
The evolution of coronary artery bypass grafting (CABG) has been a key component in significantly reducing the morbidity and mortality associated with occlusive coronary artery disease (CAD). Cleveland Clinic surgeons, through their technical interventions and innovations, have led the evolution in coronary revascularization starting in the 1960s and continuing today. This article provides a brief overview of the evolution and describes the issues associated with current CABG approaches.
EARLY WORK IN RECONSTRUCTIVE CORONARY ARTERY SURGERY
Results from the first large series of venous grafting for CAD were reported in 1970 by Favaloro and colleagues at Cleveland Clinic.1 They showed the efficacy of grafting in treating CAD, with low associated morbidity and mortality, thus establishing this surgery as the treatment modality for CAD.
The technique of surgical myocardial revascularization was a culmination of developments that began years earlier with the Vineberg procedure, involving suturing of the mammary artery to the muscle rather than a vessel-to-vessel anastomosis. From this followed the coronary patch, end-to-end bypass, and then end-to-side bypass.
In the 1970s, the refinement of suturing the left internal mammary artery (LIMA) directly to the left anterior descending (LAD) artery using magnifying loops was pioneered and popularized at Cleveland Clinic. This later became the cornerstone of future coronary revascularizations.
As a direct result of the successful technical advances and excellent clinical outcomes, the volume of CABG procedures in the United States rose steadily during the 1980s and reached its peak in 1995. It then began a slow decline that continued until 2013, when the trend began to reverse. It was still rising through 2015.
WHY THE RENEWED INTEREST IN CABG?
A key component to continued use of CABG is that it appears to have a clinical edge over other treatments. This has been shown in several high-profile studies: SYNTAX,2,3 FREEDOM,4,5 BEST,6 and NOBLE.7 For example, in the SYNTAX trial, which compared CABG vs percutaneous coronary intervention (PCI), the conclusion from both the 1-year2 and the 5-year3 results was that CABG should remain the standard of care for patients with complex lesions—those with an intermediate or high burden of CAD.
The 5-year outcomes showed that the rate of major adverse cardiac and cerebrovascular events favored CABG over PCI (26.9% vs 37.3%, respectively; P < .0001).3 All-cause mortality, although not statistically significant, also was better for CABG (11.4% vs 13.9%). This indicates that as the complexity and burden of disease increase, the benefit of CABG over PCI becomes more prominent. In short, the worse the disease, the better the results with CABG.
Why is CABG better?
One rationale is that CABG not only bypasses the culprit-lesion vessel, it also protects against future lesions. An elegant study published in 2010 showed that in most cases of acute myocardial infarction (MI), the culprit coronary lesion is in the first 7 cm of the LAD.8 With CABG, most distal anastomoses are beyond 7 cm and, thus, are beyond the location of the vast majority of potential future culprit lesions.
An important factor is the modern-day safety record of CABG. According to the Society of Thoracic
Surgeons Adult Cardiac Surgery Database,9 in 2016 the expected operative mortality for CABG was just over 2%. At the Cleveland Clinic, CABG mortality has consistently been below 1% despite the complexity of the cases and the higher percentage of reoperations performed at the Clinic. In addition, the low incidence of major complications after CABG has contributed to its endurance as an important therapeutic option for CAD over the decades.
IMPROVING LONG-TERM CABG OUTCOMES
Improving vein graft patency
The Achilles heel of CABG is the decline of patency of saphenous vein grafts. The occlusion rate of these veins is 6% to 8% at hospital discharge and approximately 10% at 1 year after CABG. By 10 years, half of the vein grafts are diseased or occluded, with progression of atherosclerotic disease over time.
There has been controversy about whether open harvesting of the saphenous vein is better than endoscopic vein harvesting for patency-related outcomes. This arose after the publication of an ad hoc analysis that gave poor marks to endoscopic vein-graft harvesting.10 Its major finding was that endoscopic vein harvesting had higher rates of vein-graft failure at 12 to 18 months than open vein harvesting (46.7% vs 38.0%, respectively; P < .001). At 3 years, endoscopic harvesting was associated with higher rates of death, MI, or repeat revascularization (20.2% vs 17.4%, P = .04).
A US Food and Drug Administration-sanctioned Society of Thoracic Surgeons observational study, however, reviewed outcomes from 235,394 patients who underwent CABG from 2003 through 2008 and found no significant increase in 5-year mortality rates with use of endoscopic vein-graft harvesting vs open harvesting.11 This study showed that the less invasive endoscopic approach is still an option.
In 2015, Taggart and colleagues12 reported on a pioneering procedure that wraps the saphenous vein graft with a stent. Initial results showed external stenting had the potential to improve vein-graft lumen and reduce intimal hyperplasia at 1 year postoperatively. Surgeons can expect more data on this technology in the future.
COMPARING CONDUIT OPTIONS FOR CABG
Arterial vs venous grafts
The 1986 report by Loop and colleagues from Cleveland Clinic showed that the patency of the mammary artery graft was superior to that of the saphenous vein and that patients receiving a mammary bypass had significantly better 10-year survival (82.6% vs 71.0%, respectively; P < .0001).13 The findings of this landmark study established the LIMA-to-LAD bypass as the technical standard for surgical coronary revascularization.
Single vs bilateral mammary artery grafts
In December 2016, results of the Arterial Revascularization Trial (ART) were published comparing single vs double mammary artery grafts.14 In this prospective randomized trial, the 5-year results showed no significant difference between these mammary grafts in terms of all-cause mortality, MI, or stroke. Bilateral mammary artery grafts, however, were associated with a higher risk of sternal wound complications (3.5% vs 1.9%, respectively; P = .005) and sternal reconstruction (1.9% vs 0.6%; P = .002).
Radial artery vs saphenous vein grafts
In the largest randomized study comparing these two graft options,16 the 1-year results showed no difference in graft patency; a follow-up analysis is in progress. In contrast, randomized studies from Canada17 and the United Kingdom18 suggest that there are potential benefits associated with use of radial artery grafts in terms of patency and clinical outcomes. In addition, observational data from centers experienced in radial artery grafting have demonstrated favorable outcomes. Radial arteries perform best when bypassing totally occluded or severely stenotic vessels in which there is no or little risk of competitive flow from the native circulation.
Right internal mammary vs radial artery grafts
A propensity-matched comparison study looking at multiple studies (N = 15,374 patients) concluded that use of the right internal mammary artery provides better outcomes.19 It was associated with a 25% risk reduction for late death and a 63% risk reduction for repeat vascularization, both statistically significant vs the radial artery rates. But there is a randomized study showing that the radial artery is as good as or better than the right internal mammary artery. At this point, it is not clear which artery is better as an adjunct for the LIMA-to-LAD bypass.
GUIDELINES FOR GRAFT SELECTION
In 2016, the Society of Thoracic Surgeons published guidelines that encouraged the use of arterial grafts, giving it a class IIa designation, meaning that the evidence indicates it is reasonable to consider.20
The guidelines note the following:
- The internal mammary artery should be used to bypass the LAD when bypass of the LAD is indicated.
- As an adjunct to the left internal mammary artery, a second arterial graft (the right internal mammary artery or radial artery) should be considered in appropriate patients.
- Use of bilateral internal mammary arteries should be considered in patients who are not at high risk for sternal complications.
COMPARING SURGICAL APPROACHES
Traditional CABG performed via median sternotomy and with the use of cardiopulmonary bypass remains the technical standard in surgical coronary revascularization. However, technologies have allowed surgeons to use different and sometimes less invasive approaches that may have good outcomes in select patients with suitable risk profiles and favorable coronary anatomies.
On-pump vs off-pump CABG
The popularity of CABG without cardiopulmonary bypass (“off-pump”) peaked in 2002, when it constituted approximately 23% of CABG procedures and then declined to 17% by 2012.21 The ROOBY (Veterans Affairs Randomized On/Off Bypass) trial of 2,203 VA patients showed that at 1 year, those in the off-pump group had worse composite outcomes, poorer graft patency, and greater incidence of incomplete revascularization than the on-pump group.22 However, the use of off-pump CABG was vindicated in two other trials—CORONARY and GOPCABE—in which experienced surgeons in high-volume centers with high-risk patients had no difference in outcomes at 1 and 5 years.23–25 The recommendation is to tailor the procedure to the patient rather than the patient to the procedure. The best option is always to do what is right for the patient. For example, patients with diseased ascending aortas or liver disease may benefit from an off-pump approach.
MINIMALLY INVASIVE CABG
Robotic CABG
This procedure has advantages and disadvantages. The advantages are primarily related to the minimally invasive approach:
- There is no surgeon hand tremor
- It is less invasive
- It provides better cosmetic results
- It is expected to result in less pain, fewer transfusions, fewer complications, and shorter length of hospital stay, although those have not been proven.
Disadvantages include the following:
- Compromised completeness of revascularization—with some “difficult” vessels left unbypassed
- Longer operative times
- Higher cost
- Concern about graft patency with inexperienced surgeons
- Higher-than-expected mortality in some reports.
In 2013, a study of 500 patients treated with robotic totally endoscopic CABG showed that this procedure could be safe and effective, although the best outcomes were achieved in patients with less severe disease requiring fewer bypasses.26 In other words, it is more appropriate for LIMA-to-LAD suturing and less complex anatomy, and it is best performed with cardiopulmonary bypass with the heart arrested.
Hybrid revascularization
This procedure is a combination of minimally invasive CABG (MIDCAB or robotic CABG) to revascularize the LAD and PCI to treat the remaining vessels in multivessel CAD. The CABG and PCI can be concurrent or staged. The hybrid approach has the attraction of being less invasive and uses the technical standard LIMA-to-LAD approach, but it has the obvious limitation of not incorporating additional arterial grafting and the possibility of a compromised technical outcome in less experienced hands.
A collaborative task force from several cardiovascular medical societies developed evidence-based guidelines to address the hybrid coronary revascularization approach. They give it a class IIa recommendation, indicating that it is a reasonable approach to treating patients in whom there are limitations and challenges to traditional CABG. For other patients, they gave it a class IIb recommendation, indicating that it may be reasonable to use as an alternative to multivessel PCI or CABG.27
THE EVOLUTION CONTINUES: CABG VS PCI
As CABG and PCI continue to evolve, surgical approaches to CAD are becoming more sophisticated with the use of more arterial conduits, less invasive surgical approaches, and development of new types of stents for PCI; however, expect the debate to continue regarding which approach to CAD is best. This is not a battle between surgical and nonsurgical specialties. Rather, the goal should be an amicable, collaborative heart-care team. After all, the most important question is, as always, which therapy is best for the individual patient.
- Sheldon WC, Favaloro RG, Sones FM Jr, Effler DB. Reconstructive coronary artery surgery: venous autograft technique. JAMA 1970; 213:78–82.
- Serruys PW, Morice M-C, Kappetein AP, et al; for the SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009; 360:961–972.
- Mohr FW, Morice M-C, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 2013; 381:629–638.
- Farkouh ME, Domanski M, Sleeper LA, et al; for the FREEDOM Trial Investigators. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012; 367:2375–2384.
- Dangas GD, Farkouh ME, Sleeper LA, et al; for the FREEDOM Investigators. Long-term outcome of PCI versus CABG in insulin and non-insulin-treated diabetic patients: results from the FREEDOM trial. J Am Coll Cardiol 2014; 64:1189–1197.
- Park S-J, Ahn J-M, Kim Y-H, et al; for the BEST Trial Investigators. Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med 2015; 372:1204–1212.
- Mäkikallio T, Holm NR, Lindsay M, et al; for the NOBLE study investigators. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet 2016; 388:2743–2752.
- Jeon C, Candia SC, Wang JC, et al. Relative spatial distributions of coronary artery bypass graft insertion and acute thrombosis: a model for protection from acute myocardial infarction. Am Heart J 2010; 160:195–201.
- The Society of Thoracic Surgeons and Duke Clinical Research Institute. Adult cardiac surgery database: executive summary (10 years—STS period ending March 31, 2016). https://www.sts.org/sites/default/files/documents/2016Harvest2_ExecutiveSummary_new.pdf. Accessed March 10, 2017.
- Lopes RD, Hafley GE, Allen KB, et al. Endoscopic versus open vein-graft harvesting in coronary-artery bypass surgery. N Engl J Med 2009; 361:235–244.
- Williams JB, Peterson ED, Brennan JM, et al. Association between endoscopic vs open vein-graft harvesting and mortality, wound complications, and cardiovascular events in patients undergoing CABG surgery. JAMA 2012; 308:475–484.
- Taggart DP, Ben Gal Y, Lees B, et al. A randomized trial of external stenting for saphenous vein grafts in coronary artery bypass grafting. Ann Thorac Surg 2015; 99:2039–2045.
- Loop FD, Lytle BW, Cosgrove DM, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med 1986; 314:1–6.
- Taggart DP, Gray AM, et al; for the ART Investigators. Randomized trial of bilateral versus single internal-thoracic-artery grafts. N Engl J Med 2016; 375:2540–2549.
- Lytle BW, Blackstone EH, Sabik JF, et al. The effect of bilateral internal thoracic artery grafting on survival during 20 postoperative years. Ann Thorac Surg 2004; 78:2005–2012; discussion 2012–2014.
- Goldman S, Sethi GK, Holman W, et al. Radial artery grafts vs saphenous vein grafts in coronary artery bypass surgery: a randomized trial. JAMA 2011; 305:167–174.
- Desai ND, Cohen EA, Naylor CD, Fremes SE; for the Radial Artery Patency Study Investigators. A randomized comparison of radial-artery and saphenous-vein coronary bypass grafts. N Engl J Med 2004; 351:2302–2309.
- Collins P, Webb CM, Chong CF, Moat NE; for the Radial Artery Versus Saphenous Vein Patency (RSVP) Trial Investigators. Radial artery versus saphenous vein patency randomized trial: five-year angiographic follow-up. Circulation 2008; 117:2859–2864.
- Benedetto U, Caputo M, Gaudino M, et al. Right internal thoracic artery or radial artery? A propensity-matched comparison on the second-best arterial conduit. J Thorac Cardiovasc Surg 2017; 153:79–88.
- Aldea GS, Bakaeen FG, Pal J, et al. The Society of Thoracic Surgeons clinical practice guidelines on arterial conduits for coronary artery bypass grafting. Ann Thorac Surg 2016; 101:801–809.
- Bakaeen FG, Shroyer AL, Gammie JS, et al. Trends in use of off-pump coronary artery bypass grafting: results from the Society of Thoracic Surgeons Adult Cardiac Surgery Database. J Thorac Cardiovasc Surg 2014; 148:856–864.
- Shroyer AL, Grover FL, Hattler B, et al; for the Veterans Affairs Randomized On/Off Bypass (ROOBY) Study Group. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 2009; 361:1827–1837.
- Diegeler A, Börgermann J, Kappert U, et al; for the GOPCABE Study Group. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med 2013; 368:1189–1198.
Lamy A, Devereaux PJ, Prabhakaran D, et al; for the CORONARY Investigators. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med 2013; 368:1179–1188. - Lamy A, Devereaux PJ, Prabhakaran D, et al; for the CORONARY Investigators. Five-year outcomes after off-pump or on-pump coronary-artery bypass grafting. N Engl J Med 2016; 375:2359–2368.
- Bonaros N, Schachner T, Lehr E, et al. Five hundred cases of robotic totally endoscopic coronary artery bypass grafting: predictors of success and safety. Ann Thorac Surg 2013; 95:803–812.
- Fihn SD, Gardin JM, Abrams J, et al; American College of Cardiology Foundation/American Heart Association Task Force. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2012; 126:e354–e471.
- Sheldon WC, Favaloro RG, Sones FM Jr, Effler DB. Reconstructive coronary artery surgery: venous autograft technique. JAMA 1970; 213:78–82.
- Serruys PW, Morice M-C, Kappetein AP, et al; for the SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med 2009; 360:961–972.
- Mohr FW, Morice M-C, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 2013; 381:629–638.
- Farkouh ME, Domanski M, Sleeper LA, et al; for the FREEDOM Trial Investigators. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012; 367:2375–2384.
- Dangas GD, Farkouh ME, Sleeper LA, et al; for the FREEDOM Investigators. Long-term outcome of PCI versus CABG in insulin and non-insulin-treated diabetic patients: results from the FREEDOM trial. J Am Coll Cardiol 2014; 64:1189–1197.
- Park S-J, Ahn J-M, Kim Y-H, et al; for the BEST Trial Investigators. Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med 2015; 372:1204–1212.
- Mäkikallio T, Holm NR, Lindsay M, et al; for the NOBLE study investigators. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet 2016; 388:2743–2752.
- Jeon C, Candia SC, Wang JC, et al. Relative spatial distributions of coronary artery bypass graft insertion and acute thrombosis: a model for protection from acute myocardial infarction. Am Heart J 2010; 160:195–201.
- The Society of Thoracic Surgeons and Duke Clinical Research Institute. Adult cardiac surgery database: executive summary (10 years—STS period ending March 31, 2016). https://www.sts.org/sites/default/files/documents/2016Harvest2_ExecutiveSummary_new.pdf. Accessed March 10, 2017.
- Lopes RD, Hafley GE, Allen KB, et al. Endoscopic versus open vein-graft harvesting in coronary-artery bypass surgery. N Engl J Med 2009; 361:235–244.
- Williams JB, Peterson ED, Brennan JM, et al. Association between endoscopic vs open vein-graft harvesting and mortality, wound complications, and cardiovascular events in patients undergoing CABG surgery. JAMA 2012; 308:475–484.
- Taggart DP, Ben Gal Y, Lees B, et al. A randomized trial of external stenting for saphenous vein grafts in coronary artery bypass grafting. Ann Thorac Surg 2015; 99:2039–2045.
- Loop FD, Lytle BW, Cosgrove DM, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med 1986; 314:1–6.
- Taggart DP, Gray AM, et al; for the ART Investigators. Randomized trial of bilateral versus single internal-thoracic-artery grafts. N Engl J Med 2016; 375:2540–2549.
- Lytle BW, Blackstone EH, Sabik JF, et al. The effect of bilateral internal thoracic artery grafting on survival during 20 postoperative years. Ann Thorac Surg 2004; 78:2005–2012; discussion 2012–2014.
- Goldman S, Sethi GK, Holman W, et al. Radial artery grafts vs saphenous vein grafts in coronary artery bypass surgery: a randomized trial. JAMA 2011; 305:167–174.
- Desai ND, Cohen EA, Naylor CD, Fremes SE; for the Radial Artery Patency Study Investigators. A randomized comparison of radial-artery and saphenous-vein coronary bypass grafts. N Engl J Med 2004; 351:2302–2309.
- Collins P, Webb CM, Chong CF, Moat NE; for the Radial Artery Versus Saphenous Vein Patency (RSVP) Trial Investigators. Radial artery versus saphenous vein patency randomized trial: five-year angiographic follow-up. Circulation 2008; 117:2859–2864.
- Benedetto U, Caputo M, Gaudino M, et al. Right internal thoracic artery or radial artery? A propensity-matched comparison on the second-best arterial conduit. J Thorac Cardiovasc Surg 2017; 153:79–88.
- Aldea GS, Bakaeen FG, Pal J, et al. The Society of Thoracic Surgeons clinical practice guidelines on arterial conduits for coronary artery bypass grafting. Ann Thorac Surg 2016; 101:801–809.
- Bakaeen FG, Shroyer AL, Gammie JS, et al. Trends in use of off-pump coronary artery bypass grafting: results from the Society of Thoracic Surgeons Adult Cardiac Surgery Database. J Thorac Cardiovasc Surg 2014; 148:856–864.
- Shroyer AL, Grover FL, Hattler B, et al; for the Veterans Affairs Randomized On/Off Bypass (ROOBY) Study Group. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 2009; 361:1827–1837.
- Diegeler A, Börgermann J, Kappert U, et al; for the GOPCABE Study Group. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med 2013; 368:1189–1198.
Lamy A, Devereaux PJ, Prabhakaran D, et al; for the CORONARY Investigators. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med 2013; 368:1179–1188. - Lamy A, Devereaux PJ, Prabhakaran D, et al; for the CORONARY Investigators. Five-year outcomes after off-pump or on-pump coronary-artery bypass grafting. N Engl J Med 2016; 375:2359–2368.
- Bonaros N, Schachner T, Lehr E, et al. Five hundred cases of robotic totally endoscopic coronary artery bypass grafting: predictors of success and safety. Ann Thorac Surg 2013; 95:803–812.
- Fihn SD, Gardin JM, Abrams J, et al; American College of Cardiology Foundation/American Heart Association Task Force. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2012; 126:e354–e471.
KEY POINTS
- CABG is considered the standard of care for patients with intermediate or high coronary artery disease burden.
- Traditional CABG performed via median sternotomy with the use of cardiopulmonary bypass is the technical standard for surgical coronary revascularization.
- Suturing the left internal mammary artery directly to the left anterior descending artery is the most effective technique for coronary revascularization.
- Minimally invasive approaches to CABG are safe and effective alternatives in select patient populations.