User login
In the years since the introduction of robotically assisted mitral valve surgery, surgeons have looked for ways to improve techniques and procedures. A study from Cleveland Clinic presented at the American Association for Thoracic Surgery in 2016 assessed efficacy and safety outcomes associated with 1,000 consecutive robotically assisted mitral valve surgeries at Cleveland Clinic.1 The purpose of the study was to assess the clinical outcomes from these cases and analyze whether the outcomes changed over time as surgeons became more competent with robotic techniques. This analysis was also designed to identify procedural processes that improved outcomes during the trial.
STUDY METHODS
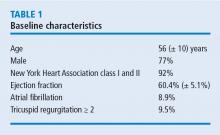
Nearly all cases (96%) were classified as degenerative mitral valve disease (N = 960). Of those, most had posterior leaflet prolapse (68%), about one-third (29%) had bileaflet prolapse, and only 3% had anterior leaflet involvement.
All surgeries were performed through right port incisions and used femoral cannulation for peripheral bypass. The aorta was occluded with either a Chitwood transthoracic clamp or a balloon.
STUDY RESULTS
It is important to remember that with femoral artery perfusion, the blood flow is opposite to the normal direction; thus, it goes up the aorta into the head vessels, which presents its own risks and challenges. Also, during retrograde perfusion, there is a risk of dislodging atherosclerotic plaque leading to brain embolus and stroke.
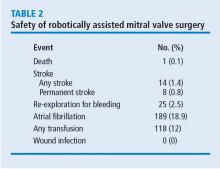
In these 1,000 cases, 997 were planned mitral valve repairs, 2 were mitral valve replacements, and 1 was resection of a mitral valve fibroelastoma. Results for the mitral valve repairs were excellent, with postoperative mitral regurgitation occurring in less than 1% of patients.
PROCEDURAL IMPROVEMENTS
A primary point of interest was to identify procedural improvements that occurred during the course of the study. The areas evaluated in robotically assisted mitral valve surgery were the efficacy of the procedure in time, transfusion rates, stroke risk, how many mitral valve replacements occurred, and how many required conversion to sternotomy. These were assessed to determine whether surgical experience resulted in improvement.
Results showed that those efficiencies improved during the study. Cardiopulmonary bypass time decreased from about 140 minutes to 130 minutes. Cross-clamp time improved more dramatically from about 110 minutes to 90 minutes. And the percentage of cases requiring postoperative or intraoperative blood transfusion improved from about 24% to 10%.
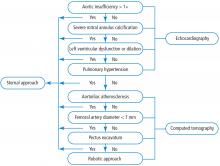
PATIENT SELECTION CRITERIA: ALGORITHM
ALGORITHM IMPACT
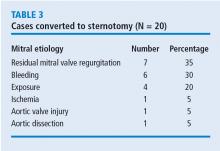
What was the effect of this algorithm? In the 500 cases after its implementation, the stroke rate decreased by more than half—from 10 incidents before to 4 incidents after—and mitral replacements dropped from 4 to 0. The rate of conversion from robotic repair to conventional sternotomy in this patient series also improved, although this likely reflects surgical experience more than the algorithm. The conversion rate initially increased as surgeons gained experience with the robotic techniques. It rose to 4% during the first 300 to 400 cases, then dropped to 2% at the 500-case mark. It leveled off for the next 300 cases before dropping to 0 toward the end of the series.
Other metrics improved as well, which were attributed to a combination of surgical experience with robotic assistance and use of the patient-selection algorithm. The stroke risk declined to 0.8%, ischemic and cardiopulmonary bypass times declined, and the transfusion rate declined. No mitral replacements were done in the last 500 cases, and the conversion to conventional sternotomy rate declined to 1%.
In conclusion, this Cleveland Clinic study showed that a combination of a focused preoperative assessment using the patient-selection algorithm and increased surgical experience with robotic techniques enhanced clinical outcomes and improved procedural efficiency associated with robotically assisted mitral valve surgery.
- Gillinov AM, Mihaljevic T, Javadikasgari H, Suri R, Mick S, Navia J, et al. Safety and effectiveness of robotically-assisted mitral valve surgery: analysis of 1,000 consecutive cases. Presented at the 96th Annual Meeting of the American Association for Thoracic Surgery; May 14-18, 2016; Baltimore, MD.
In the years since the introduction of robotically assisted mitral valve surgery, surgeons have looked for ways to improve techniques and procedures. A study from Cleveland Clinic presented at the American Association for Thoracic Surgery in 2016 assessed efficacy and safety outcomes associated with 1,000 consecutive robotically assisted mitral valve surgeries at Cleveland Clinic.1 The purpose of the study was to assess the clinical outcomes from these cases and analyze whether the outcomes changed over time as surgeons became more competent with robotic techniques. This analysis was also designed to identify procedural processes that improved outcomes during the trial.
STUDY METHODS
Nearly all cases (96%) were classified as degenerative mitral valve disease (N = 960). Of those, most had posterior leaflet prolapse (68%), about one-third (29%) had bileaflet prolapse, and only 3% had anterior leaflet involvement.
All surgeries were performed through right port incisions and used femoral cannulation for peripheral bypass. The aorta was occluded with either a Chitwood transthoracic clamp or a balloon.
STUDY RESULTS
It is important to remember that with femoral artery perfusion, the blood flow is opposite to the normal direction; thus, it goes up the aorta into the head vessels, which presents its own risks and challenges. Also, during retrograde perfusion, there is a risk of dislodging atherosclerotic plaque leading to brain embolus and stroke.
In these 1,000 cases, 997 were planned mitral valve repairs, 2 were mitral valve replacements, and 1 was resection of a mitral valve fibroelastoma. Results for the mitral valve repairs were excellent, with postoperative mitral regurgitation occurring in less than 1% of patients.
PROCEDURAL IMPROVEMENTS
A primary point of interest was to identify procedural improvements that occurred during the course of the study. The areas evaluated in robotically assisted mitral valve surgery were the efficacy of the procedure in time, transfusion rates, stroke risk, how many mitral valve replacements occurred, and how many required conversion to sternotomy. These were assessed to determine whether surgical experience resulted in improvement.
Results showed that those efficiencies improved during the study. Cardiopulmonary bypass time decreased from about 140 minutes to 130 minutes. Cross-clamp time improved more dramatically from about 110 minutes to 90 minutes. And the percentage of cases requiring postoperative or intraoperative blood transfusion improved from about 24% to 10%.
PATIENT SELECTION CRITERIA: ALGORITHM
ALGORITHM IMPACT
What was the effect of this algorithm? In the 500 cases after its implementation, the stroke rate decreased by more than half—from 10 incidents before to 4 incidents after—and mitral replacements dropped from 4 to 0. The rate of conversion from robotic repair to conventional sternotomy in this patient series also improved, although this likely reflects surgical experience more than the algorithm. The conversion rate initially increased as surgeons gained experience with the robotic techniques. It rose to 4% during the first 300 to 400 cases, then dropped to 2% at the 500-case mark. It leveled off for the next 300 cases before dropping to 0 toward the end of the series.
Other metrics improved as well, which were attributed to a combination of surgical experience with robotic assistance and use of the patient-selection algorithm. The stroke risk declined to 0.8%, ischemic and cardiopulmonary bypass times declined, and the transfusion rate declined. No mitral replacements were done in the last 500 cases, and the conversion to conventional sternotomy rate declined to 1%.
In conclusion, this Cleveland Clinic study showed that a combination of a focused preoperative assessment using the patient-selection algorithm and increased surgical experience with robotic techniques enhanced clinical outcomes and improved procedural efficiency associated with robotically assisted mitral valve surgery.
In the years since the introduction of robotically assisted mitral valve surgery, surgeons have looked for ways to improve techniques and procedures. A study from Cleveland Clinic presented at the American Association for Thoracic Surgery in 2016 assessed efficacy and safety outcomes associated with 1,000 consecutive robotically assisted mitral valve surgeries at Cleveland Clinic.1 The purpose of the study was to assess the clinical outcomes from these cases and analyze whether the outcomes changed over time as surgeons became more competent with robotic techniques. This analysis was also designed to identify procedural processes that improved outcomes during the trial.
STUDY METHODS
Nearly all cases (96%) were classified as degenerative mitral valve disease (N = 960). Of those, most had posterior leaflet prolapse (68%), about one-third (29%) had bileaflet prolapse, and only 3% had anterior leaflet involvement.
All surgeries were performed through right port incisions and used femoral cannulation for peripheral bypass. The aorta was occluded with either a Chitwood transthoracic clamp or a balloon.
STUDY RESULTS
It is important to remember that with femoral artery perfusion, the blood flow is opposite to the normal direction; thus, it goes up the aorta into the head vessels, which presents its own risks and challenges. Also, during retrograde perfusion, there is a risk of dislodging atherosclerotic plaque leading to brain embolus and stroke.
In these 1,000 cases, 997 were planned mitral valve repairs, 2 were mitral valve replacements, and 1 was resection of a mitral valve fibroelastoma. Results for the mitral valve repairs were excellent, with postoperative mitral regurgitation occurring in less than 1% of patients.
PROCEDURAL IMPROVEMENTS
A primary point of interest was to identify procedural improvements that occurred during the course of the study. The areas evaluated in robotically assisted mitral valve surgery were the efficacy of the procedure in time, transfusion rates, stroke risk, how many mitral valve replacements occurred, and how many required conversion to sternotomy. These were assessed to determine whether surgical experience resulted in improvement.
Results showed that those efficiencies improved during the study. Cardiopulmonary bypass time decreased from about 140 minutes to 130 minutes. Cross-clamp time improved more dramatically from about 110 minutes to 90 minutes. And the percentage of cases requiring postoperative or intraoperative blood transfusion improved from about 24% to 10%.
PATIENT SELECTION CRITERIA: ALGORITHM
ALGORITHM IMPACT
What was the effect of this algorithm? In the 500 cases after its implementation, the stroke rate decreased by more than half—from 10 incidents before to 4 incidents after—and mitral replacements dropped from 4 to 0. The rate of conversion from robotic repair to conventional sternotomy in this patient series also improved, although this likely reflects surgical experience more than the algorithm. The conversion rate initially increased as surgeons gained experience with the robotic techniques. It rose to 4% during the first 300 to 400 cases, then dropped to 2% at the 500-case mark. It leveled off for the next 300 cases before dropping to 0 toward the end of the series.
Other metrics improved as well, which were attributed to a combination of surgical experience with robotic assistance and use of the patient-selection algorithm. The stroke risk declined to 0.8%, ischemic and cardiopulmonary bypass times declined, and the transfusion rate declined. No mitral replacements were done in the last 500 cases, and the conversion to conventional sternotomy rate declined to 1%.
In conclusion, this Cleveland Clinic study showed that a combination of a focused preoperative assessment using the patient-selection algorithm and increased surgical experience with robotic techniques enhanced clinical outcomes and improved procedural efficiency associated with robotically assisted mitral valve surgery.
- Gillinov AM, Mihaljevic T, Javadikasgari H, Suri R, Mick S, Navia J, et al. Safety and effectiveness of robotically-assisted mitral valve surgery: analysis of 1,000 consecutive cases. Presented at the 96th Annual Meeting of the American Association for Thoracic Surgery; May 14-18, 2016; Baltimore, MD.
- Gillinov AM, Mihaljevic T, Javadikasgari H, Suri R, Mick S, Navia J, et al. Safety and effectiveness of robotically-assisted mitral valve surgery: analysis of 1,000 consecutive cases. Presented at the 96th Annual Meeting of the American Association for Thoracic Surgery; May 14-18, 2016; Baltimore, MD.
KEY POINTS
- Surgeon competence with robotic techniques, which can be improved through experience, is a key to improving outcomes.
- This patient-selection algorithm provides an evidence-based approach to identifying patients who are the best candidates for the robotic approach.
- This study showed that increased surgical competence and improved patient selection improved patient outcomes for the primary end points.