User login
BOSTON – It’s a trade-off that few people would be likely to make, but having cancer – particularly a type treated by chemotherapy – is associated with a significantly decreased risk for developing Alzheimer’s disease, a retrospective study has shown.
An inverse relationship was found between the incidence of the majority of different types of cancer and Alzheimer’s disease (AD) risk, in a review of the records of nearly 3.5 million U.S. veterans.
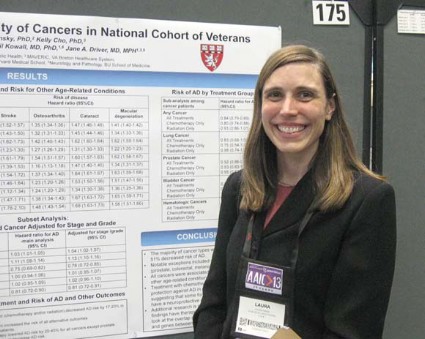
Liver cancer survivors had the lowest risk for AD (hazard ratio = 0.49), followed by survivors of pancreatic cancer (HR = 0.56), esophageal cancer (0.67), and multiple myeloma (0.74), reported Dr. Laura Frain of the geriatric research education and clinical center at Boston VA Medical Center.
However, survivors of prostate cancer had a small but significantly higher risk for AD (HR = 1.11), and other screening-detected cancers (colorectal cancer, melanoma) were not associated with a reduced risk, Dr. Frain and her associates found.
"There may be something different about prostate cancer survivors, but whether that’s biologic or related to the way that they’re screened is unclear," Dr. Frain said in an interview.
Many types of cancer were associated with an increased risk for non-AD dementias, with increased risks ranging from an HR of 1.11 for head and neck cancer to 2.64 for brain cancer.
The investigators attempted to control for the possibility that people with cancer may not survive long enough to develop frank dementia by looking at other age-related conditions, including stroke, osteoarthritis, cataracts, and macular degeneration. They found that all cancers were associated with an increased risk for other age-related conditions, suggesting that their findings of reduced AD risk were valid, Dr. Frain said at the Alzheimer’s Association International Conference 2013.
Findings corroborated
The findings parallel those of a recently published study of more than 1 million residents of Northern Italy (Neurology 2013 July 10 [doi:10.1212/WNL.0b013e31829c5ec1]). The investigators in that study found that "[t]he risk of cancer in patients with AD dementia was halved, and the risk of AD dementia in patients with cancer was 35% reduced. This relationship was observed in almost all subgroup analyses, suggesting that some anticipated potential confounding factors did not significantly influence the results."
Dr. Frain noted that three previous prospective cohort studies had found that older adults with cancer had a reduction in risk for incident AD, ranging from a 33% to a 60% decline. Those studies, however, were limited by small numbers of patients with cancer, limiting the ability to look for associations with specific cancer or treatment types.
The current study drew on data from the massive U.S. National Veterans Affairs Healthcare System to assemble a cohort of 3,499,378 veterans who received outpatient care within the system from 1997 to 2011. The investigators used regression analysis models adjusted for cancer treatment, multiple comorbidities, follow-up time, and number of visits per year before baseline. In addition, the researchers performed subanalyses of patients with diagnoses of prostate, lung, colorectal, and bladder cancers and lymphoma, with the models adjusted for cancer stage and grade.
The median age of the cohort was 71 years, 98% were males, and 66% were white. A total of 771,285 veterans (22%) had a cancer diagnosis. Of the 82,028 veterans who developed AD (2.3% of the entire cohort), 24% were cancer survivors, and the remainder had no cancer history.
The investigators also found that "treatment with chemotherapy conferred additional protection against AD in nearly all cancer types, suggesting that some forms of chemotherapy may have neuroprotective action."
Chemotherapy lowered the risk of AD associated with all cancers except prostate cancer by 20%-45%.
The investigators plan to look at individual categories of anticancer agents, and to see whether they may be common factors between cancer and AD in regard to proteins, genes, and biochemical pathways.
One intriguing target for exploration, Dr. Frain said, is peptidyl-prolyl cis-trans isomerase NIMA-interacting 1 (PIN1), an enzyme that when upregulated has been associated with the pathogenesis of some forms of cancer, and when downregulated may be associated with the development of AD.
The study was supported by grants from the Department of Veterans Affairs. Dr. Frain is supported by a VA Special Fellowship in geriatrics.
BOSTON – It’s a trade-off that few people would be likely to make, but having cancer – particularly a type treated by chemotherapy – is associated with a significantly decreased risk for developing Alzheimer’s disease, a retrospective study has shown.
An inverse relationship was found between the incidence of the majority of different types of cancer and Alzheimer’s disease (AD) risk, in a review of the records of nearly 3.5 million U.S. veterans.
Liver cancer survivors had the lowest risk for AD (hazard ratio = 0.49), followed by survivors of pancreatic cancer (HR = 0.56), esophageal cancer (0.67), and multiple myeloma (0.74), reported Dr. Laura Frain of the geriatric research education and clinical center at Boston VA Medical Center.
However, survivors of prostate cancer had a small but significantly higher risk for AD (HR = 1.11), and other screening-detected cancers (colorectal cancer, melanoma) were not associated with a reduced risk, Dr. Frain and her associates found.
"There may be something different about prostate cancer survivors, but whether that’s biologic or related to the way that they’re screened is unclear," Dr. Frain said in an interview.
Many types of cancer were associated with an increased risk for non-AD dementias, with increased risks ranging from an HR of 1.11 for head and neck cancer to 2.64 for brain cancer.
The investigators attempted to control for the possibility that people with cancer may not survive long enough to develop frank dementia by looking at other age-related conditions, including stroke, osteoarthritis, cataracts, and macular degeneration. They found that all cancers were associated with an increased risk for other age-related conditions, suggesting that their findings of reduced AD risk were valid, Dr. Frain said at the Alzheimer’s Association International Conference 2013.
Findings corroborated
The findings parallel those of a recently published study of more than 1 million residents of Northern Italy (Neurology 2013 July 10 [doi:10.1212/WNL.0b013e31829c5ec1]). The investigators in that study found that "[t]he risk of cancer in patients with AD dementia was halved, and the risk of AD dementia in patients with cancer was 35% reduced. This relationship was observed in almost all subgroup analyses, suggesting that some anticipated potential confounding factors did not significantly influence the results."
Dr. Frain noted that three previous prospective cohort studies had found that older adults with cancer had a reduction in risk for incident AD, ranging from a 33% to a 60% decline. Those studies, however, were limited by small numbers of patients with cancer, limiting the ability to look for associations with specific cancer or treatment types.
The current study drew on data from the massive U.S. National Veterans Affairs Healthcare System to assemble a cohort of 3,499,378 veterans who received outpatient care within the system from 1997 to 2011. The investigators used regression analysis models adjusted for cancer treatment, multiple comorbidities, follow-up time, and number of visits per year before baseline. In addition, the researchers performed subanalyses of patients with diagnoses of prostate, lung, colorectal, and bladder cancers and lymphoma, with the models adjusted for cancer stage and grade.
The median age of the cohort was 71 years, 98% were males, and 66% were white. A total of 771,285 veterans (22%) had a cancer diagnosis. Of the 82,028 veterans who developed AD (2.3% of the entire cohort), 24% were cancer survivors, and the remainder had no cancer history.
The investigators also found that "treatment with chemotherapy conferred additional protection against AD in nearly all cancer types, suggesting that some forms of chemotherapy may have neuroprotective action."
Chemotherapy lowered the risk of AD associated with all cancers except prostate cancer by 20%-45%.
The investigators plan to look at individual categories of anticancer agents, and to see whether they may be common factors between cancer and AD in regard to proteins, genes, and biochemical pathways.
One intriguing target for exploration, Dr. Frain said, is peptidyl-prolyl cis-trans isomerase NIMA-interacting 1 (PIN1), an enzyme that when upregulated has been associated with the pathogenesis of some forms of cancer, and when downregulated may be associated with the development of AD.
The study was supported by grants from the Department of Veterans Affairs. Dr. Frain is supported by a VA Special Fellowship in geriatrics.
BOSTON – It’s a trade-off that few people would be likely to make, but having cancer – particularly a type treated by chemotherapy – is associated with a significantly decreased risk for developing Alzheimer’s disease, a retrospective study has shown.
An inverse relationship was found between the incidence of the majority of different types of cancer and Alzheimer’s disease (AD) risk, in a review of the records of nearly 3.5 million U.S. veterans.
Liver cancer survivors had the lowest risk for AD (hazard ratio = 0.49), followed by survivors of pancreatic cancer (HR = 0.56), esophageal cancer (0.67), and multiple myeloma (0.74), reported Dr. Laura Frain of the geriatric research education and clinical center at Boston VA Medical Center.
However, survivors of prostate cancer had a small but significantly higher risk for AD (HR = 1.11), and other screening-detected cancers (colorectal cancer, melanoma) were not associated with a reduced risk, Dr. Frain and her associates found.
"There may be something different about prostate cancer survivors, but whether that’s biologic or related to the way that they’re screened is unclear," Dr. Frain said in an interview.
Many types of cancer were associated with an increased risk for non-AD dementias, with increased risks ranging from an HR of 1.11 for head and neck cancer to 2.64 for brain cancer.
The investigators attempted to control for the possibility that people with cancer may not survive long enough to develop frank dementia by looking at other age-related conditions, including stroke, osteoarthritis, cataracts, and macular degeneration. They found that all cancers were associated with an increased risk for other age-related conditions, suggesting that their findings of reduced AD risk were valid, Dr. Frain said at the Alzheimer’s Association International Conference 2013.
Findings corroborated
The findings parallel those of a recently published study of more than 1 million residents of Northern Italy (Neurology 2013 July 10 [doi:10.1212/WNL.0b013e31829c5ec1]). The investigators in that study found that "[t]he risk of cancer in patients with AD dementia was halved, and the risk of AD dementia in patients with cancer was 35% reduced. This relationship was observed in almost all subgroup analyses, suggesting that some anticipated potential confounding factors did not significantly influence the results."
Dr. Frain noted that three previous prospective cohort studies had found that older adults with cancer had a reduction in risk for incident AD, ranging from a 33% to a 60% decline. Those studies, however, were limited by small numbers of patients with cancer, limiting the ability to look for associations with specific cancer or treatment types.
The current study drew on data from the massive U.S. National Veterans Affairs Healthcare System to assemble a cohort of 3,499,378 veterans who received outpatient care within the system from 1997 to 2011. The investigators used regression analysis models adjusted for cancer treatment, multiple comorbidities, follow-up time, and number of visits per year before baseline. In addition, the researchers performed subanalyses of patients with diagnoses of prostate, lung, colorectal, and bladder cancers and lymphoma, with the models adjusted for cancer stage and grade.
The median age of the cohort was 71 years, 98% were males, and 66% were white. A total of 771,285 veterans (22%) had a cancer diagnosis. Of the 82,028 veterans who developed AD (2.3% of the entire cohort), 24% were cancer survivors, and the remainder had no cancer history.
The investigators also found that "treatment with chemotherapy conferred additional protection against AD in nearly all cancer types, suggesting that some forms of chemotherapy may have neuroprotective action."
Chemotherapy lowered the risk of AD associated with all cancers except prostate cancer by 20%-45%.
The investigators plan to look at individual categories of anticancer agents, and to see whether they may be common factors between cancer and AD in regard to proteins, genes, and biochemical pathways.
One intriguing target for exploration, Dr. Frain said, is peptidyl-prolyl cis-trans isomerase NIMA-interacting 1 (PIN1), an enzyme that when upregulated has been associated with the pathogenesis of some forms of cancer, and when downregulated may be associated with the development of AD.
The study was supported by grants from the Department of Veterans Affairs. Dr. Frain is supported by a VA Special Fellowship in geriatrics.
AT AAIC 2013
Major finding: The risk for incident Alzheimer’s disease was reduced by 51% in liver cancer survivors, 44% in survivors of pancreatic cancer, and 23% in survivors of esophageal cancer.
Data source: A retrospective cohort study of 3,499,378 U.S. veterans.
Disclosures: The study was supported by grants from the Department of Veterans Affairs. Dr. Frain is supported by a VA Special Fellowship in geriatrics.