User login
ANSWER
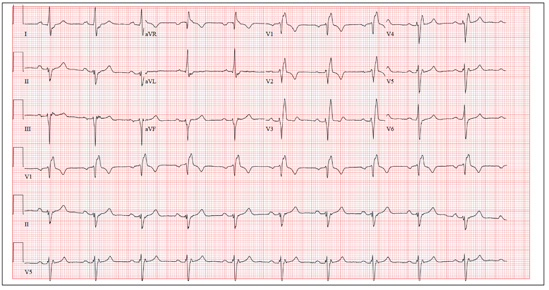
The correct interpretation includes normal sinus rhythm, right bundle branch block, and left anterior fascicular block. Normal sinus rhythm is evidenced by a rate between 60 and 100 beats/min, with a corresponding P for every QRS and a QRS for every P.
Right bundle branch block is evidenced by a QRS duration > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. Left anterior fascicular block is evident from the finding that the S waves are greater than the R waves in leads II, III, and aVF.
The presence of a right ventricular block and left anterior fascicular block (bifascicular block) is consistent with a history of a VSD and/or surgical repair. The right and left bundles proceed from the atrioventricular node and bundle of His down the ventricular septum to the Purkinje fibers in the distal ventricular myocardium. Therefore, congenital anomalies of the ventricular septum, and/or surgical intervention within it, often affect conduction of the right and/or left bundle.
This patient’s symptoms were a result of his dilated aorta, and he underwent successful repair, with resolution of his symptoms.
ANSWER
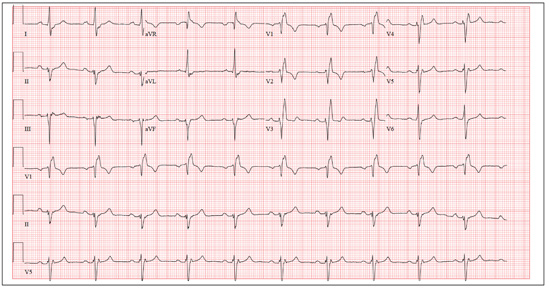
The correct interpretation includes normal sinus rhythm, right bundle branch block, and left anterior fascicular block. Normal sinus rhythm is evidenced by a rate between 60 and 100 beats/min, with a corresponding P for every QRS and a QRS for every P.
Right bundle branch block is evidenced by a QRS duration > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. Left anterior fascicular block is evident from the finding that the S waves are greater than the R waves in leads II, III, and aVF.
The presence of a right ventricular block and left anterior fascicular block (bifascicular block) is consistent with a history of a VSD and/or surgical repair. The right and left bundles proceed from the atrioventricular node and bundle of His down the ventricular septum to the Purkinje fibers in the distal ventricular myocardium. Therefore, congenital anomalies of the ventricular septum, and/or surgical intervention within it, often affect conduction of the right and/or left bundle.
This patient’s symptoms were a result of his dilated aorta, and he underwent successful repair, with resolution of his symptoms.
ANSWER
The correct interpretation includes normal sinus rhythm, right bundle branch block, and left anterior fascicular block. Normal sinus rhythm is evidenced by a rate between 60 and 100 beats/min, with a corresponding P for every QRS and a QRS for every P.
Right bundle branch block is evidenced by a QRS duration > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. Left anterior fascicular block is evident from the finding that the S waves are greater than the R waves in leads II, III, and aVF.
The presence of a right ventricular block and left anterior fascicular block (bifascicular block) is consistent with a history of a VSD and/or surgical repair. The right and left bundles proceed from the atrioventricular node and bundle of His down the ventricular septum to the Purkinje fibers in the distal ventricular myocardium. Therefore, congenital anomalies of the ventricular septum, and/or surgical intervention within it, often affect conduction of the right and/or left bundle.
This patient’s symptoms were a result of his dilated aorta, and he underwent successful repair, with resolution of his symptoms.
A man, 50, has a history of tetralogy of Fallot (ventricular septal defect [VSD], pulmonary stenosis, right ventricular hypertrophy, and overriding aorta). He underwent surgical correction at age 4, with placement of a Blalock-Taussig shunt and closure of his VSD, and was asymptomatic until one year ago. In the past year, he has developed progressive shortness of breath and dyspnea on exertion. In the past three months, he has developed chest pain that he describes as sharp, nonradiating, and occurring most often with dyspnea on exertion. He denies syncope, near-syncope, palpitations, or tachycardia. He cannot walk more than one-and-a-half blocks before stopping to rest, and he avoids hills and stairs if at all possible. A review of his most recent cardiac work-up (performed six months ago) reveals no significant coronary artery disease or evidence of aortic stenosis; it shows moderate aortic regurgitation, normal systolic aortic pressures, and normal left ventricular end diastolic pressures. The right ventricular pressures were elevated due to pulmonic stenosis; however, the estimated pulmonary artery pressures were normal. A cardiac MRI performed one month ago shows a significantly dilated aortic root with aneurysmal dilatation extending to the aortic arch, with effacement at the sinotubular junction and moderate aortic regurgitation. Additional findings include a markedly dilated right ventricular outflow tract with no pulmonic stenosis, evi-dence of a previous right Blalock-Taussig shunt, and moderate right atrial enlargement. Medical history is remarkable for hypertension. Family history is remarkable for hypertension, diabetes, and coronary artery disease, but not congenital heart disease. The patient does not smoke and drinks socially on the weekends. His medications include amlodipine, aspirin, and lisinopril. He is allergic to penicillin and amox-icillin. A review of systems reveals that he has had flulike symptoms for the past four days, with a dry, nonproductive cough. Physical exam reveals a well-developed, obese male in no distress. His height is 67”and his weight, 208 lb. Blood pressure is 102/70 mm Hg; pulse, 70 beats/min; respiratory rate, 16 breaths/min-1; and temperature, 98.4°F. His oxygen saturation is 98% on room air. Pertinent physical findings include a grade II/VI holosystolic murmur and a grade III/VI diastolic murmur, with a prominent S2 best heard at the left lower sternal border. There is no jugular venous distention, no peripheral edema, and no abnormal pulmonary finding. An ECG previously ordered for today’s visit reveals the following: a ventricular rate of 63 beats/min; PR interval, 196 ms; QRS duration, 174 ms; QT/QTc inter-val, 460/470 ms; P axis, 34°; R axis, –67°; and T axis, 56°. What is your interpretation of this ECG? How does the patient’s history predict the findings?