User login
In June the Centers for Medicare and Medicaid Services (CMS) issued a notice proposing changes to the Medicare Physician Fee Schedule (MPFS) that, if enacted, would significantly increase Medicare payments to hospitalists for many services routinely performed. Because many private health plans use the Medicare-approved RVUs for their own fee schedules, it is anticipated that hospitalists will likely see payment increases for their non-Medicare services as well.
The changes, which will take effect in January 2007 if enacted, reflect the recommendations of the Relative Value Update Committee (RUC) of the American Medical Association, along with input from SHM. At this point, however, they are only proposed changes that CMS could modify based on input from affected groups and Congress. SHM will continue to urge CMS to implement the proposed changes and we encourage all hospitalists and other interested individuals to send a letter to CMS indicating support for the proposed changes. (See “How to Show Your Support,” p. 15.) CMS is accepting comments on the rule until August 21, with the final ruling expected in November.
The suggested revisions—the largest ever proposed for services related to patient evaluation and management—are designed to improve the accuracy of payments to physicians for the services they furnish to Medicare beneficiaries. The proposed notice includes substantial increases for “evaluation and management” services (that is, time and effort that physicians spend with patients in evaluating their condition and advising and assisting them in managing their health).
The proposed notice addresses two components of physician payments under the MPFS:
- A comprehensive review of physician work RVUs; and
- A proposed change in the methodology for calculating practice expenses.
“Medicare law requires CMS to assess the accuracy of the work relative values it assigns to physician-services every five years,” says SHM CEO Larry Wellikson, MD. “SHM, on behalf of our members, participated in a coalition of internal medicine groups, led by the American College of Physicians, which provided survey data and other evidence to the RUC to show that many services were undervalued compared to other physician services and that it was essential that their work RVUs be increased.”
Consistent with the RUC’s recommendations, CMS is proposing the largest increase in the work RVUs assigned to office and hospital visits and consultations since Medicare implemented its physician fee schedule in 1992. Many of these reflect double-digit increases for codes commonly billed by hospitalists:
- The work RVU for initial hospital care (CPT code 99221) would increase by 47%;
- The work RVU for subsequent hospital care (CPT code 99232) would increase by 31%; and
- The work RVU for subsequent hospital care (CPT code 99233) would increase by 32%.
“It’s time to increase Medicare’s payment rates for physicians to spend time with their patients,” says CMS Administrator Mark McClellan, MD, PhD. “We expect that improved payments for evaluation and management services will result in better outcomes because physicians will get financial support for giving patients the help they need to manage illnesses more effectively.”
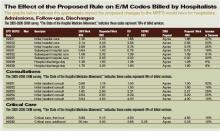
While Medicare payments to each hospitalist won’t increase by the same percentages listed in the above examples, 2007 Medicare payments for many evaluation and management services would increase significantly, assuming continuation of the current 2006 dollar conversion factor. (See “The Effect of the Proposed Rule on E/M Codes Billed by Hospitalists,” above.)
Changes in physician work RVUs affect approximately 55% of the total RVUs (the rest are determined by changes in practice expense and medical liability RVUs), so the increase in work RVUs will determine more than half of the total payments per service.
Further, by law CMS must offset the total increases in work RVUs from the five-year review with a separate budget neutrality adjustment so that 2007 expenditures are roughly equal to their 2006 level. The agency is estimating that the proposed changes to the work RVUs would cost Medicare approximately $4 billion. To achieve budget neutrality, CMS is proposing to reduce the work RVU for each service by 10%.
Overall, the proposed notice revises work RVUs for more than 400 services to better reflect the work and time required of a physician in furnishing the service, which can include not just procedures performed but also the services involved in evaluating a patient’s condition, and determining a course of treatment (known as “evaluation and management” services).
Work RVUs account for approximately $35 billion in MPFS payments, representing more than 50% of overall Medicare payments under the fee schedule. TH
SHM encourages hospitalists and others to send a letter to CMS indicating support for the proposed changes.
In June the Centers for Medicare and Medicaid Services (CMS) issued a notice proposing changes to the Medicare Physician Fee Schedule (MPFS) that, if enacted, would significantly increase Medicare payments to hospitalists for many services routinely performed. Because many private health plans use the Medicare-approved RVUs for their own fee schedules, it is anticipated that hospitalists will likely see payment increases for their non-Medicare services as well.
The changes, which will take effect in January 2007 if enacted, reflect the recommendations of the Relative Value Update Committee (RUC) of the American Medical Association, along with input from SHM. At this point, however, they are only proposed changes that CMS could modify based on input from affected groups and Congress. SHM will continue to urge CMS to implement the proposed changes and we encourage all hospitalists and other interested individuals to send a letter to CMS indicating support for the proposed changes. (See “How to Show Your Support,” p. 15.) CMS is accepting comments on the rule until August 21, with the final ruling expected in November.
The suggested revisions—the largest ever proposed for services related to patient evaluation and management—are designed to improve the accuracy of payments to physicians for the services they furnish to Medicare beneficiaries. The proposed notice includes substantial increases for “evaluation and management” services (that is, time and effort that physicians spend with patients in evaluating their condition and advising and assisting them in managing their health).
The proposed notice addresses two components of physician payments under the MPFS:
- A comprehensive review of physician work RVUs; and
- A proposed change in the methodology for calculating practice expenses.
“Medicare law requires CMS to assess the accuracy of the work relative values it assigns to physician-services every five years,” says SHM CEO Larry Wellikson, MD. “SHM, on behalf of our members, participated in a coalition of internal medicine groups, led by the American College of Physicians, which provided survey data and other evidence to the RUC to show that many services were undervalued compared to other physician services and that it was essential that their work RVUs be increased.”
Consistent with the RUC’s recommendations, CMS is proposing the largest increase in the work RVUs assigned to office and hospital visits and consultations since Medicare implemented its physician fee schedule in 1992. Many of these reflect double-digit increases for codes commonly billed by hospitalists:
- The work RVU for initial hospital care (CPT code 99221) would increase by 47%;
- The work RVU for subsequent hospital care (CPT code 99232) would increase by 31%; and
- The work RVU for subsequent hospital care (CPT code 99233) would increase by 32%.
“It’s time to increase Medicare’s payment rates for physicians to spend time with their patients,” says CMS Administrator Mark McClellan, MD, PhD. “We expect that improved payments for evaluation and management services will result in better outcomes because physicians will get financial support for giving patients the help they need to manage illnesses more effectively.”
While Medicare payments to each hospitalist won’t increase by the same percentages listed in the above examples, 2007 Medicare payments for many evaluation and management services would increase significantly, assuming continuation of the current 2006 dollar conversion factor. (See “The Effect of the Proposed Rule on E/M Codes Billed by Hospitalists,” above.)
Changes in physician work RVUs affect approximately 55% of the total RVUs (the rest are determined by changes in practice expense and medical liability RVUs), so the increase in work RVUs will determine more than half of the total payments per service.
Further, by law CMS must offset the total increases in work RVUs from the five-year review with a separate budget neutrality adjustment so that 2007 expenditures are roughly equal to their 2006 level. The agency is estimating that the proposed changes to the work RVUs would cost Medicare approximately $4 billion. To achieve budget neutrality, CMS is proposing to reduce the work RVU for each service by 10%.
Overall, the proposed notice revises work RVUs for more than 400 services to better reflect the work and time required of a physician in furnishing the service, which can include not just procedures performed but also the services involved in evaluating a patient’s condition, and determining a course of treatment (known as “evaluation and management” services).
Work RVUs account for approximately $35 billion in MPFS payments, representing more than 50% of overall Medicare payments under the fee schedule. TH
SHM encourages hospitalists and others to send a letter to CMS indicating support for the proposed changes.
In June the Centers for Medicare and Medicaid Services (CMS) issued a notice proposing changes to the Medicare Physician Fee Schedule (MPFS) that, if enacted, would significantly increase Medicare payments to hospitalists for many services routinely performed. Because many private health plans use the Medicare-approved RVUs for their own fee schedules, it is anticipated that hospitalists will likely see payment increases for their non-Medicare services as well.
The changes, which will take effect in January 2007 if enacted, reflect the recommendations of the Relative Value Update Committee (RUC) of the American Medical Association, along with input from SHM. At this point, however, they are only proposed changes that CMS could modify based on input from affected groups and Congress. SHM will continue to urge CMS to implement the proposed changes and we encourage all hospitalists and other interested individuals to send a letter to CMS indicating support for the proposed changes. (See “How to Show Your Support,” p. 15.) CMS is accepting comments on the rule until August 21, with the final ruling expected in November.
The suggested revisions—the largest ever proposed for services related to patient evaluation and management—are designed to improve the accuracy of payments to physicians for the services they furnish to Medicare beneficiaries. The proposed notice includes substantial increases for “evaluation and management” services (that is, time and effort that physicians spend with patients in evaluating their condition and advising and assisting them in managing their health).
The proposed notice addresses two components of physician payments under the MPFS:
- A comprehensive review of physician work RVUs; and
- A proposed change in the methodology for calculating practice expenses.
“Medicare law requires CMS to assess the accuracy of the work relative values it assigns to physician-services every five years,” says SHM CEO Larry Wellikson, MD. “SHM, on behalf of our members, participated in a coalition of internal medicine groups, led by the American College of Physicians, which provided survey data and other evidence to the RUC to show that many services were undervalued compared to other physician services and that it was essential that their work RVUs be increased.”
Consistent with the RUC’s recommendations, CMS is proposing the largest increase in the work RVUs assigned to office and hospital visits and consultations since Medicare implemented its physician fee schedule in 1992. Many of these reflect double-digit increases for codes commonly billed by hospitalists:
- The work RVU for initial hospital care (CPT code 99221) would increase by 47%;
- The work RVU for subsequent hospital care (CPT code 99232) would increase by 31%; and
- The work RVU for subsequent hospital care (CPT code 99233) would increase by 32%.
“It’s time to increase Medicare’s payment rates for physicians to spend time with their patients,” says CMS Administrator Mark McClellan, MD, PhD. “We expect that improved payments for evaluation and management services will result in better outcomes because physicians will get financial support for giving patients the help they need to manage illnesses more effectively.”
While Medicare payments to each hospitalist won’t increase by the same percentages listed in the above examples, 2007 Medicare payments for many evaluation and management services would increase significantly, assuming continuation of the current 2006 dollar conversion factor. (See “The Effect of the Proposed Rule on E/M Codes Billed by Hospitalists,” above.)
Changes in physician work RVUs affect approximately 55% of the total RVUs (the rest are determined by changes in practice expense and medical liability RVUs), so the increase in work RVUs will determine more than half of the total payments per service.
Further, by law CMS must offset the total increases in work RVUs from the five-year review with a separate budget neutrality adjustment so that 2007 expenditures are roughly equal to their 2006 level. The agency is estimating that the proposed changes to the work RVUs would cost Medicare approximately $4 billion. To achieve budget neutrality, CMS is proposing to reduce the work RVU for each service by 10%.
Overall, the proposed notice revises work RVUs for more than 400 services to better reflect the work and time required of a physician in furnishing the service, which can include not just procedures performed but also the services involved in evaluating a patient’s condition, and determining a course of treatment (known as “evaluation and management” services).
Work RVUs account for approximately $35 billion in MPFS payments, representing more than 50% of overall Medicare payments under the fee schedule. TH
SHM encourages hospitalists and others to send a letter to CMS indicating support for the proposed changes.