User login
Irritability. Tremors. Sweating and a rapid heart rate. Extreme confusion. Fever. Convulsions. These are all symptoms of acute alcohol withdrawal syndrome. A patient may develop acute alcohol withdrawal syndrome when chronic alcohol use is interrupted by hospital admission. Increasingly patients are being treated for alcohol withdrawal on general medical wards.
Acute withdrawal is most safely managed in an inpatient setting if the patient has been using high doses of sedatives, has a history of seizures or delirium tremens, or has co-morbid medical or psychiatric problems.1 The severity of the withdrawal syndrome is affected by concurrent medical illness. Up to 20% of patients develop delirium tremens if left untreated.2 Recognition and effective treatment of alcohol withdrawal are needed to prevent excess mortality or prolonged hospitalization due to complications. It is essential for hospitalists to recognize and effectively treat acute alcohol withdrawal to prevent adverse outcomes in hospitalized patients.
Development of Withdrawal
Hospitalized patients may not be forthcoming about their alcohol consumption for numerous reasons. They may not consider it a problem; they may not recognize that acute withdrawal is a serious and even fatal complication; or they may wish to conceal their alcoholism from family and physicians due to concerns about stigmatization.
Even when patients acknowledge their drinking, they often underestimate the amount, which may be because a patient is minimizing or because alcohol is an amnestic agent, causing drinkers to lose count of how much they have had to drink. It is simplest to ask—in a nonjudgmental manner—all patients admitted to the hospital about drinking and to be alert for signs of acute alcohol withdrawal in all patients.
Not all patients who drink alcohol will develop an acute withdrawal syndrome. Those who drink less frequently—only on weekends with no drinking at all on weekdays, for example—are at lower risk of acute withdrawal. Those who drink on most days of the week are more likely—due to tolerance—to develop withdrawal. Even a habit of two or three drinks each day is enough to set up a person for withdrawal. Not all daily drinkers are guaranteed to develop withdrawal, and it is difficult to predict who will and who will not. The best predictor of whether a patient will develop acute withdrawal while hospitalized is a past history of acute alcohol withdrawal.
The alcohol withdrawal syndrome has two phases: early withdrawal and late withdrawal. (See Table 1, below.) The signs and symptoms of early withdrawal usually occur within 48 hours of the last drink. The initial indication is an elevation of vital signs: heart rate, blood pressure, and temperature. Tremors develop next—first a fine tremor of the hands and fasciculation of the tongue, then gross tremors of the extremities. As the syndrome progresses, disorientation and mild hallucinations (often auditory but occasionally visual) develop, accompanied by diaphoresis. Seizures are an early sign of alcohol withdrawal and may even be the presenting symptom.
Late alcohol withdrawal is also known as delirium tremens—the DTs—and consists of the worsening autonomic dysregulation that is responsible for the morbidity and mortality attributed to alcohol withdrawal. It begins after early withdrawal—usually 72 hours or more after the last drink. Some patients do not progress from early to late withdrawal, and their symptoms simply subside after a few days, with or without treatment. But it is impossible to predict which patients will progress and which will not. The signs of late withdrawal consist of worsening diaphoresis, nausea, and vomiting (which may result in aspiration pneumonia), delirium with frank hallucinations, and rapid, severe fluctuation in vital signs. Sudden changes in blood pressure and heart rate may result in complications such as myocardial infarction or a cerebrovascular event. Untreated late withdrawal results in significant morbidity and even death.3 Adequate treatment of early withdrawal prevents progression to late withdrawal.
Assessment
When you or a colleague suspect that a hospitalized patient may develop alcohol withdrawal, regularly assess the patient for signs of early withdrawal. Use a validated assessment scale to quantify the severity of the withdrawal syndrome, and initiate treatment decisions such as the dose of medication. If no withdrawal signs manifest after 48 hours, then it is usually safe to discontinue monitoring for withdrawal. Monitor patients for whom alcohol withdrawal is not considered but who then develop withdrawal signs using an assessment scale.
The revised Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) is commonly used to assess severity of withdrawal.4 Competent nurses can give it in less than five minutes. A CIWA-Ar score less than 5 indicates minimal withdrawal with no need for pharmacotherapy, whereas a score that falls in the range of 6-19 indicates mild withdrawal that may benefit from medical treatment. A score greater than 30 indicates severe withdrawal that requires close monitoring due to the risk for complications such as seizures and autonomic instability.5
The CIWA-Ar is just as useful for evaluating and treating withdrawal in hospitalized patients on general medical wards as it is for use in chemical dependency units. It can also be used to determine an appropriate pharmacotherapy dose for patients in withdrawal who also have other medical illnesses.6
Monitor patients every few hours, with the frequency of evaluation varying by severity of withdrawal signs. Every four hours is sufficient for most patients, but those who have developed late withdrawal or those with CIWA-Ar scores greater than 30 should be monitored hourly to prevent complications. Continue regular assessment until the withdrawal syndrome has been under control (CIWA-Ar score less than 6) for at least 24 hours.
Treatment
Medications: Pharmacotherapy is indicated for the management of moderate to severe withdrawal. Any cross-tolerant medication may be used; benzodiazepines or barbiturates are most commonly prescribed. It is inappropriate to use beverage alcohol to prevent or treat alcohol withdrawal. Use of intravenous alcohol infusion is reserved for poisoning with methanol, isopropanol, or ethylene glycol. It should not be given for treatment of acute alcohol withdrawal due to potential complications such as intoxication with delirium and development of gastritis.
Both benzodiazepines and barbiturates, which are different classes of sedative-hypnotic medications, are cross-tolerant with alcohol and effectively treat alcohol withdrawal.7 Acute alcohol withdrawal in the United States is most often managed with benzodiazepines.8 There are a variety of benzodiazepines available, from ultra-short-acting to long-acting, as well as parenteral and oral forms. Diazepam has been used extensively due to rapid onset of action when given intravenously and long duration of action when given orally.
For similar reasons, chlordiazepoxide is also used widely. Lorazepam, an intermediate-acting benzodiazepine that can be given orally or parenterally, has been used extensively for treatment of acute alcohol withdrawal, especially in hospitalized patients, because it has fewer active metabolites than other benzodiazepines. This makes it safer to use in treating patients with severe liver disease, which is important when treating chronic alcoholics. Benzodiazepines have a relatively high therapeutic index when used to treat patients with illnesses in addition to acute withdrawal. This makes benzodiazepines an excellent choice for the treatment of acute withdrawal in patients on general medical wards.
Barbiturates have been used successfully to treat acute alcohol withdrawal syndrome in general medical inpatients, with phenobarbital the most common choice.9,10 Phenobarbital may be preferable to other sedative-hypnotics; with its longer half-life, patients rarely achieve a “high” as they do with other sedatives, and it is available in multiple dosage forms.11
A number of alternative non-sedative-hypnotic medications exist to treat acute alcohol withdrawal. Beta-adrenergic blockers (atenolol, propranolol), clonidine, and anticonvulsant agents (carbamazepine, valproate) decrease alcohol withdrawal symptoms and have been used successfully in the treatment of mild withdrawal. They are not cross-tolerant with alcohol, however, and may result in progression of the withdrawal syndrome. These alternative medications are not appropriate to use as single agents in the treatment of withdrawal in a general medical setting.
Dosing regimens: There are no standard protocols for withdrawal management in widespread use.12 A fixed dosing schedule is commonly used for treatment of acute withdrawal, but either fixed-schedule or symptom-triggered dosing—medication given as needed for withdrawal signs—is efficacious in the treatment of withdrawal, even in patients with medical comorbidity.6
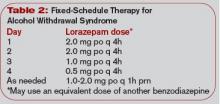
Fixed-schedule dosing is a one-size-fits-all approach for treating alcohol withdrawal. It uses the same dose of cross-tolerant medication on a fixed schedule for all patients for 24-48 hours; the dose is then tapered if the patient is stable. (See Table 2, left.) Reducing the dose by 10%-20% of the initial dose each day over five to 10 days provides a comfortable taper—especially in patients who initially required higher doses of medication to control the withdrawal. Fixed-schedule dosing offers less flexibility for individual patients, but it is a simple approach that can be applied in many settings.
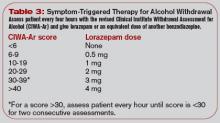
Symptom-triggered therapy occurs when cross-tolerant medication is given only for symptoms of withdrawal rather than on a schedule. (See Table 3, p. 25.) Patients are monitored closely and assessed regularly using a tool such as the CIWA-Ar. The dose of cross-tolerant medication prescribed is based on the severity of withdrawal symptoms as measured by the CIWA-Ar score. This approach is similar to the sliding scale of insulin dosing used to treat hyperglycemia. Symptom-triggered therapy provides individualized treatment for withdrawal without overmedicating or underdosing, but it is a complex system to carry out on a general medical unit.
Severe withdrawal: Treat severe DTs manifested by abnormal and fluctuating vital signs and/or delirium aggressively in an ICU environment with sufficiently large doses of medication to suppress the withdrawal.11 Use IV medications with a rapid onset of action for immediate effect. Lorazepam and diazepam have a rapid onset of action when given intravenously, although the duration of action is shorter than when given orally.
For example, give lorazepam in a dose of one to four mg every 10-30 minutes until the patient is calm but awake and the heart rate is below 120 beats per minute. A continuous intravenous infusion may be warranted to control withdrawal symptoms, and the rate can be titrated to the desired level of consciousness. After stabilization, the patient can be changed to an equivalent dose of a long-acting sedative-hypnotic and tapered as above.
Assessing and medicating acute withdrawal remain necessary first steps in the treatment of the disease of alcohol dependence. After acute detoxification has begun, long-term treatment of alcoholism is necessary to prevent readmission for continuing medical problems due to alcohol consumption. Refer patients who have been treated for alcohol withdrawal for long-term treatment of alcoholism. This may include Alcoholics Anonymous, outpatient counseling, and other treatment modalities.
Conclusion
Ask all patients admitted to the hospital about drinking alcohol and be alert for signs of acute alcohol withdrawal in any patient. The best predictor of whether a patient will develop acute withdrawal is a past history of withdrawal. Signs of withdrawal usually occur within 48 hours of the last drink. Untreated withdrawal may result in significant morbidity and mortality.
Patients in withdrawal should be monitored closely and given appropriate doses of benzodiazepines or barbiturates to treat withdrawal signs. Cross-tolerant medication may be given on a fixed schedule or as symptom-triggered therapy. Severe withdrawal may require a continuous intravenous infusion in an ICU. Recognition and effective treatment of alcohol withdrawal can prevent significant complications in hospitalized patients. TH
Dr. Weaver is associate professor of internal medicine and psychiatry at Virginia Commonwealth University, Richmond.
References
- Saitz R. Introduction to alcohol withdrawal. Alcohol Health Res World. 1998;22(1):5-12.
- Cross GM, Hennessey PT. Principles and practice of detoxification. Prim Care. 1993;20(1):81-93.
- Cutshall BJ. The Saunderssutton syndrome: an analysis of delirium tremens. Q J Stud Alcohol. 1965;26(3):423-448.
- Sullivan JT, Sykora K, Schneiderman J, et al. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict. 1989;84:1353-1357.
- Foy A, March S, Drinkwater V. Use of an objective clinical scale in the assessment and management of alcohol withdrawal in a large general hospital. Alcohol Clin Exp Res. 1988;12(3):360-364.
- Weaver MF, Hoffman HJ, Johnson RE. Alcohol withdrawal pharmacotherapy for inpatients with medical comorbidity. J Addict Dis. 2006;25(2):17-24.
- Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA. 1997;278(2):144-151.
- Saitz R, Mayo-Smith MF, Roberts MS, et al. Individualized treatment for alcohol withdrawal. A randomized double-blind controlled trial. JAMA. 1994;272(7):519-523.
- Yeh HS, Dhopesh V, Maany I. Seizures during detoxification. J Gen Intern Med. 1992;7(1):123.
- Young GP, Rores C, Murphy C, et al. Intravenous phenobarbital for alcohol withdrawal and convulsions. Ann Emerg Med. 1987;16(8):847-850.
- Weaver MF, Jarvis MA, Schnoll SH. Role of the primary care physician in problems of substance abuse. Arch Intern Med. 1999;159(9):913-924.
Irritability. Tremors. Sweating and a rapid heart rate. Extreme confusion. Fever. Convulsions. These are all symptoms of acute alcohol withdrawal syndrome. A patient may develop acute alcohol withdrawal syndrome when chronic alcohol use is interrupted by hospital admission. Increasingly patients are being treated for alcohol withdrawal on general medical wards.
Acute withdrawal is most safely managed in an inpatient setting if the patient has been using high doses of sedatives, has a history of seizures or delirium tremens, or has co-morbid medical or psychiatric problems.1 The severity of the withdrawal syndrome is affected by concurrent medical illness. Up to 20% of patients develop delirium tremens if left untreated.2 Recognition and effective treatment of alcohol withdrawal are needed to prevent excess mortality or prolonged hospitalization due to complications. It is essential for hospitalists to recognize and effectively treat acute alcohol withdrawal to prevent adverse outcomes in hospitalized patients.
Development of Withdrawal
Hospitalized patients may not be forthcoming about their alcohol consumption for numerous reasons. They may not consider it a problem; they may not recognize that acute withdrawal is a serious and even fatal complication; or they may wish to conceal their alcoholism from family and physicians due to concerns about stigmatization.
Even when patients acknowledge their drinking, they often underestimate the amount, which may be because a patient is minimizing or because alcohol is an amnestic agent, causing drinkers to lose count of how much they have had to drink. It is simplest to ask—in a nonjudgmental manner—all patients admitted to the hospital about drinking and to be alert for signs of acute alcohol withdrawal in all patients.
Not all patients who drink alcohol will develop an acute withdrawal syndrome. Those who drink less frequently—only on weekends with no drinking at all on weekdays, for example—are at lower risk of acute withdrawal. Those who drink on most days of the week are more likely—due to tolerance—to develop withdrawal. Even a habit of two or three drinks each day is enough to set up a person for withdrawal. Not all daily drinkers are guaranteed to develop withdrawal, and it is difficult to predict who will and who will not. The best predictor of whether a patient will develop acute withdrawal while hospitalized is a past history of acute alcohol withdrawal.
The alcohol withdrawal syndrome has two phases: early withdrawal and late withdrawal. (See Table 1, below.) The signs and symptoms of early withdrawal usually occur within 48 hours of the last drink. The initial indication is an elevation of vital signs: heart rate, blood pressure, and temperature. Tremors develop next—first a fine tremor of the hands and fasciculation of the tongue, then gross tremors of the extremities. As the syndrome progresses, disorientation and mild hallucinations (often auditory but occasionally visual) develop, accompanied by diaphoresis. Seizures are an early sign of alcohol withdrawal and may even be the presenting symptom.
Late alcohol withdrawal is also known as delirium tremens—the DTs—and consists of the worsening autonomic dysregulation that is responsible for the morbidity and mortality attributed to alcohol withdrawal. It begins after early withdrawal—usually 72 hours or more after the last drink. Some patients do not progress from early to late withdrawal, and their symptoms simply subside after a few days, with or without treatment. But it is impossible to predict which patients will progress and which will not. The signs of late withdrawal consist of worsening diaphoresis, nausea, and vomiting (which may result in aspiration pneumonia), delirium with frank hallucinations, and rapid, severe fluctuation in vital signs. Sudden changes in blood pressure and heart rate may result in complications such as myocardial infarction or a cerebrovascular event. Untreated late withdrawal results in significant morbidity and even death.3 Adequate treatment of early withdrawal prevents progression to late withdrawal.
Assessment
When you or a colleague suspect that a hospitalized patient may develop alcohol withdrawal, regularly assess the patient for signs of early withdrawal. Use a validated assessment scale to quantify the severity of the withdrawal syndrome, and initiate treatment decisions such as the dose of medication. If no withdrawal signs manifest after 48 hours, then it is usually safe to discontinue monitoring for withdrawal. Monitor patients for whom alcohol withdrawal is not considered but who then develop withdrawal signs using an assessment scale.
The revised Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) is commonly used to assess severity of withdrawal.4 Competent nurses can give it in less than five minutes. A CIWA-Ar score less than 5 indicates minimal withdrawal with no need for pharmacotherapy, whereas a score that falls in the range of 6-19 indicates mild withdrawal that may benefit from medical treatment. A score greater than 30 indicates severe withdrawal that requires close monitoring due to the risk for complications such as seizures and autonomic instability.5
The CIWA-Ar is just as useful for evaluating and treating withdrawal in hospitalized patients on general medical wards as it is for use in chemical dependency units. It can also be used to determine an appropriate pharmacotherapy dose for patients in withdrawal who also have other medical illnesses.6
Monitor patients every few hours, with the frequency of evaluation varying by severity of withdrawal signs. Every four hours is sufficient for most patients, but those who have developed late withdrawal or those with CIWA-Ar scores greater than 30 should be monitored hourly to prevent complications. Continue regular assessment until the withdrawal syndrome has been under control (CIWA-Ar score less than 6) for at least 24 hours.
Treatment
Medications: Pharmacotherapy is indicated for the management of moderate to severe withdrawal. Any cross-tolerant medication may be used; benzodiazepines or barbiturates are most commonly prescribed. It is inappropriate to use beverage alcohol to prevent or treat alcohol withdrawal. Use of intravenous alcohol infusion is reserved for poisoning with methanol, isopropanol, or ethylene glycol. It should not be given for treatment of acute alcohol withdrawal due to potential complications such as intoxication with delirium and development of gastritis.
Both benzodiazepines and barbiturates, which are different classes of sedative-hypnotic medications, are cross-tolerant with alcohol and effectively treat alcohol withdrawal.7 Acute alcohol withdrawal in the United States is most often managed with benzodiazepines.8 There are a variety of benzodiazepines available, from ultra-short-acting to long-acting, as well as parenteral and oral forms. Diazepam has been used extensively due to rapid onset of action when given intravenously and long duration of action when given orally.
For similar reasons, chlordiazepoxide is also used widely. Lorazepam, an intermediate-acting benzodiazepine that can be given orally or parenterally, has been used extensively for treatment of acute alcohol withdrawal, especially in hospitalized patients, because it has fewer active metabolites than other benzodiazepines. This makes it safer to use in treating patients with severe liver disease, which is important when treating chronic alcoholics. Benzodiazepines have a relatively high therapeutic index when used to treat patients with illnesses in addition to acute withdrawal. This makes benzodiazepines an excellent choice for the treatment of acute withdrawal in patients on general medical wards.
Barbiturates have been used successfully to treat acute alcohol withdrawal syndrome in general medical inpatients, with phenobarbital the most common choice.9,10 Phenobarbital may be preferable to other sedative-hypnotics; with its longer half-life, patients rarely achieve a “high” as they do with other sedatives, and it is available in multiple dosage forms.11
A number of alternative non-sedative-hypnotic medications exist to treat acute alcohol withdrawal. Beta-adrenergic blockers (atenolol, propranolol), clonidine, and anticonvulsant agents (carbamazepine, valproate) decrease alcohol withdrawal symptoms and have been used successfully in the treatment of mild withdrawal. They are not cross-tolerant with alcohol, however, and may result in progression of the withdrawal syndrome. These alternative medications are not appropriate to use as single agents in the treatment of withdrawal in a general medical setting.
Dosing regimens: There are no standard protocols for withdrawal management in widespread use.12 A fixed dosing schedule is commonly used for treatment of acute withdrawal, but either fixed-schedule or symptom-triggered dosing—medication given as needed for withdrawal signs—is efficacious in the treatment of withdrawal, even in patients with medical comorbidity.6
Fixed-schedule dosing is a one-size-fits-all approach for treating alcohol withdrawal. It uses the same dose of cross-tolerant medication on a fixed schedule for all patients for 24-48 hours; the dose is then tapered if the patient is stable. (See Table 2, left.) Reducing the dose by 10%-20% of the initial dose each day over five to 10 days provides a comfortable taper—especially in patients who initially required higher doses of medication to control the withdrawal. Fixed-schedule dosing offers less flexibility for individual patients, but it is a simple approach that can be applied in many settings.
Symptom-triggered therapy occurs when cross-tolerant medication is given only for symptoms of withdrawal rather than on a schedule. (See Table 3, p. 25.) Patients are monitored closely and assessed regularly using a tool such as the CIWA-Ar. The dose of cross-tolerant medication prescribed is based on the severity of withdrawal symptoms as measured by the CIWA-Ar score. This approach is similar to the sliding scale of insulin dosing used to treat hyperglycemia. Symptom-triggered therapy provides individualized treatment for withdrawal without overmedicating or underdosing, but it is a complex system to carry out on a general medical unit.
Severe withdrawal: Treat severe DTs manifested by abnormal and fluctuating vital signs and/or delirium aggressively in an ICU environment with sufficiently large doses of medication to suppress the withdrawal.11 Use IV medications with a rapid onset of action for immediate effect. Lorazepam and diazepam have a rapid onset of action when given intravenously, although the duration of action is shorter than when given orally.
For example, give lorazepam in a dose of one to four mg every 10-30 minutes until the patient is calm but awake and the heart rate is below 120 beats per minute. A continuous intravenous infusion may be warranted to control withdrawal symptoms, and the rate can be titrated to the desired level of consciousness. After stabilization, the patient can be changed to an equivalent dose of a long-acting sedative-hypnotic and tapered as above.
Assessing and medicating acute withdrawal remain necessary first steps in the treatment of the disease of alcohol dependence. After acute detoxification has begun, long-term treatment of alcoholism is necessary to prevent readmission for continuing medical problems due to alcohol consumption. Refer patients who have been treated for alcohol withdrawal for long-term treatment of alcoholism. This may include Alcoholics Anonymous, outpatient counseling, and other treatment modalities.
Conclusion
Ask all patients admitted to the hospital about drinking alcohol and be alert for signs of acute alcohol withdrawal in any patient. The best predictor of whether a patient will develop acute withdrawal is a past history of withdrawal. Signs of withdrawal usually occur within 48 hours of the last drink. Untreated withdrawal may result in significant morbidity and mortality.
Patients in withdrawal should be monitored closely and given appropriate doses of benzodiazepines or barbiturates to treat withdrawal signs. Cross-tolerant medication may be given on a fixed schedule or as symptom-triggered therapy. Severe withdrawal may require a continuous intravenous infusion in an ICU. Recognition and effective treatment of alcohol withdrawal can prevent significant complications in hospitalized patients. TH
Dr. Weaver is associate professor of internal medicine and psychiatry at Virginia Commonwealth University, Richmond.
References
- Saitz R. Introduction to alcohol withdrawal. Alcohol Health Res World. 1998;22(1):5-12.
- Cross GM, Hennessey PT. Principles and practice of detoxification. Prim Care. 1993;20(1):81-93.
- Cutshall BJ. The Saunderssutton syndrome: an analysis of delirium tremens. Q J Stud Alcohol. 1965;26(3):423-448.
- Sullivan JT, Sykora K, Schneiderman J, et al. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict. 1989;84:1353-1357.
- Foy A, March S, Drinkwater V. Use of an objective clinical scale in the assessment and management of alcohol withdrawal in a large general hospital. Alcohol Clin Exp Res. 1988;12(3):360-364.
- Weaver MF, Hoffman HJ, Johnson RE. Alcohol withdrawal pharmacotherapy for inpatients with medical comorbidity. J Addict Dis. 2006;25(2):17-24.
- Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA. 1997;278(2):144-151.
- Saitz R, Mayo-Smith MF, Roberts MS, et al. Individualized treatment for alcohol withdrawal. A randomized double-blind controlled trial. JAMA. 1994;272(7):519-523.
- Yeh HS, Dhopesh V, Maany I. Seizures during detoxification. J Gen Intern Med. 1992;7(1):123.
- Young GP, Rores C, Murphy C, et al. Intravenous phenobarbital for alcohol withdrawal and convulsions. Ann Emerg Med. 1987;16(8):847-850.
- Weaver MF, Jarvis MA, Schnoll SH. Role of the primary care physician in problems of substance abuse. Arch Intern Med. 1999;159(9):913-924.
Irritability. Tremors. Sweating and a rapid heart rate. Extreme confusion. Fever. Convulsions. These are all symptoms of acute alcohol withdrawal syndrome. A patient may develop acute alcohol withdrawal syndrome when chronic alcohol use is interrupted by hospital admission. Increasingly patients are being treated for alcohol withdrawal on general medical wards.
Acute withdrawal is most safely managed in an inpatient setting if the patient has been using high doses of sedatives, has a history of seizures or delirium tremens, or has co-morbid medical or psychiatric problems.1 The severity of the withdrawal syndrome is affected by concurrent medical illness. Up to 20% of patients develop delirium tremens if left untreated.2 Recognition and effective treatment of alcohol withdrawal are needed to prevent excess mortality or prolonged hospitalization due to complications. It is essential for hospitalists to recognize and effectively treat acute alcohol withdrawal to prevent adverse outcomes in hospitalized patients.
Development of Withdrawal
Hospitalized patients may not be forthcoming about their alcohol consumption for numerous reasons. They may not consider it a problem; they may not recognize that acute withdrawal is a serious and even fatal complication; or they may wish to conceal their alcoholism from family and physicians due to concerns about stigmatization.
Even when patients acknowledge their drinking, they often underestimate the amount, which may be because a patient is minimizing or because alcohol is an amnestic agent, causing drinkers to lose count of how much they have had to drink. It is simplest to ask—in a nonjudgmental manner—all patients admitted to the hospital about drinking and to be alert for signs of acute alcohol withdrawal in all patients.
Not all patients who drink alcohol will develop an acute withdrawal syndrome. Those who drink less frequently—only on weekends with no drinking at all on weekdays, for example—are at lower risk of acute withdrawal. Those who drink on most days of the week are more likely—due to tolerance—to develop withdrawal. Even a habit of two or three drinks each day is enough to set up a person for withdrawal. Not all daily drinkers are guaranteed to develop withdrawal, and it is difficult to predict who will and who will not. The best predictor of whether a patient will develop acute withdrawal while hospitalized is a past history of acute alcohol withdrawal.
The alcohol withdrawal syndrome has two phases: early withdrawal and late withdrawal. (See Table 1, below.) The signs and symptoms of early withdrawal usually occur within 48 hours of the last drink. The initial indication is an elevation of vital signs: heart rate, blood pressure, and temperature. Tremors develop next—first a fine tremor of the hands and fasciculation of the tongue, then gross tremors of the extremities. As the syndrome progresses, disorientation and mild hallucinations (often auditory but occasionally visual) develop, accompanied by diaphoresis. Seizures are an early sign of alcohol withdrawal and may even be the presenting symptom.
Late alcohol withdrawal is also known as delirium tremens—the DTs—and consists of the worsening autonomic dysregulation that is responsible for the morbidity and mortality attributed to alcohol withdrawal. It begins after early withdrawal—usually 72 hours or more after the last drink. Some patients do not progress from early to late withdrawal, and their symptoms simply subside after a few days, with or without treatment. But it is impossible to predict which patients will progress and which will not. The signs of late withdrawal consist of worsening diaphoresis, nausea, and vomiting (which may result in aspiration pneumonia), delirium with frank hallucinations, and rapid, severe fluctuation in vital signs. Sudden changes in blood pressure and heart rate may result in complications such as myocardial infarction or a cerebrovascular event. Untreated late withdrawal results in significant morbidity and even death.3 Adequate treatment of early withdrawal prevents progression to late withdrawal.
Assessment
When you or a colleague suspect that a hospitalized patient may develop alcohol withdrawal, regularly assess the patient for signs of early withdrawal. Use a validated assessment scale to quantify the severity of the withdrawal syndrome, and initiate treatment decisions such as the dose of medication. If no withdrawal signs manifest after 48 hours, then it is usually safe to discontinue monitoring for withdrawal. Monitor patients for whom alcohol withdrawal is not considered but who then develop withdrawal signs using an assessment scale.
The revised Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) is commonly used to assess severity of withdrawal.4 Competent nurses can give it in less than five minutes. A CIWA-Ar score less than 5 indicates minimal withdrawal with no need for pharmacotherapy, whereas a score that falls in the range of 6-19 indicates mild withdrawal that may benefit from medical treatment. A score greater than 30 indicates severe withdrawal that requires close monitoring due to the risk for complications such as seizures and autonomic instability.5
The CIWA-Ar is just as useful for evaluating and treating withdrawal in hospitalized patients on general medical wards as it is for use in chemical dependency units. It can also be used to determine an appropriate pharmacotherapy dose for patients in withdrawal who also have other medical illnesses.6
Monitor patients every few hours, with the frequency of evaluation varying by severity of withdrawal signs. Every four hours is sufficient for most patients, but those who have developed late withdrawal or those with CIWA-Ar scores greater than 30 should be monitored hourly to prevent complications. Continue regular assessment until the withdrawal syndrome has been under control (CIWA-Ar score less than 6) for at least 24 hours.
Treatment
Medications: Pharmacotherapy is indicated for the management of moderate to severe withdrawal. Any cross-tolerant medication may be used; benzodiazepines or barbiturates are most commonly prescribed. It is inappropriate to use beverage alcohol to prevent or treat alcohol withdrawal. Use of intravenous alcohol infusion is reserved for poisoning with methanol, isopropanol, or ethylene glycol. It should not be given for treatment of acute alcohol withdrawal due to potential complications such as intoxication with delirium and development of gastritis.
Both benzodiazepines and barbiturates, which are different classes of sedative-hypnotic medications, are cross-tolerant with alcohol and effectively treat alcohol withdrawal.7 Acute alcohol withdrawal in the United States is most often managed with benzodiazepines.8 There are a variety of benzodiazepines available, from ultra-short-acting to long-acting, as well as parenteral and oral forms. Diazepam has been used extensively due to rapid onset of action when given intravenously and long duration of action when given orally.
For similar reasons, chlordiazepoxide is also used widely. Lorazepam, an intermediate-acting benzodiazepine that can be given orally or parenterally, has been used extensively for treatment of acute alcohol withdrawal, especially in hospitalized patients, because it has fewer active metabolites than other benzodiazepines. This makes it safer to use in treating patients with severe liver disease, which is important when treating chronic alcoholics. Benzodiazepines have a relatively high therapeutic index when used to treat patients with illnesses in addition to acute withdrawal. This makes benzodiazepines an excellent choice for the treatment of acute withdrawal in patients on general medical wards.
Barbiturates have been used successfully to treat acute alcohol withdrawal syndrome in general medical inpatients, with phenobarbital the most common choice.9,10 Phenobarbital may be preferable to other sedative-hypnotics; with its longer half-life, patients rarely achieve a “high” as they do with other sedatives, and it is available in multiple dosage forms.11
A number of alternative non-sedative-hypnotic medications exist to treat acute alcohol withdrawal. Beta-adrenergic blockers (atenolol, propranolol), clonidine, and anticonvulsant agents (carbamazepine, valproate) decrease alcohol withdrawal symptoms and have been used successfully in the treatment of mild withdrawal. They are not cross-tolerant with alcohol, however, and may result in progression of the withdrawal syndrome. These alternative medications are not appropriate to use as single agents in the treatment of withdrawal in a general medical setting.
Dosing regimens: There are no standard protocols for withdrawal management in widespread use.12 A fixed dosing schedule is commonly used for treatment of acute withdrawal, but either fixed-schedule or symptom-triggered dosing—medication given as needed for withdrawal signs—is efficacious in the treatment of withdrawal, even in patients with medical comorbidity.6
Fixed-schedule dosing is a one-size-fits-all approach for treating alcohol withdrawal. It uses the same dose of cross-tolerant medication on a fixed schedule for all patients for 24-48 hours; the dose is then tapered if the patient is stable. (See Table 2, left.) Reducing the dose by 10%-20% of the initial dose each day over five to 10 days provides a comfortable taper—especially in patients who initially required higher doses of medication to control the withdrawal. Fixed-schedule dosing offers less flexibility for individual patients, but it is a simple approach that can be applied in many settings.
Symptom-triggered therapy occurs when cross-tolerant medication is given only for symptoms of withdrawal rather than on a schedule. (See Table 3, p. 25.) Patients are monitored closely and assessed regularly using a tool such as the CIWA-Ar. The dose of cross-tolerant medication prescribed is based on the severity of withdrawal symptoms as measured by the CIWA-Ar score. This approach is similar to the sliding scale of insulin dosing used to treat hyperglycemia. Symptom-triggered therapy provides individualized treatment for withdrawal without overmedicating or underdosing, but it is a complex system to carry out on a general medical unit.
Severe withdrawal: Treat severe DTs manifested by abnormal and fluctuating vital signs and/or delirium aggressively in an ICU environment with sufficiently large doses of medication to suppress the withdrawal.11 Use IV medications with a rapid onset of action for immediate effect. Lorazepam and diazepam have a rapid onset of action when given intravenously, although the duration of action is shorter than when given orally.
For example, give lorazepam in a dose of one to four mg every 10-30 minutes until the patient is calm but awake and the heart rate is below 120 beats per minute. A continuous intravenous infusion may be warranted to control withdrawal symptoms, and the rate can be titrated to the desired level of consciousness. After stabilization, the patient can be changed to an equivalent dose of a long-acting sedative-hypnotic and tapered as above.
Assessing and medicating acute withdrawal remain necessary first steps in the treatment of the disease of alcohol dependence. After acute detoxification has begun, long-term treatment of alcoholism is necessary to prevent readmission for continuing medical problems due to alcohol consumption. Refer patients who have been treated for alcohol withdrawal for long-term treatment of alcoholism. This may include Alcoholics Anonymous, outpatient counseling, and other treatment modalities.
Conclusion
Ask all patients admitted to the hospital about drinking alcohol and be alert for signs of acute alcohol withdrawal in any patient. The best predictor of whether a patient will develop acute withdrawal is a past history of withdrawal. Signs of withdrawal usually occur within 48 hours of the last drink. Untreated withdrawal may result in significant morbidity and mortality.
Patients in withdrawal should be monitored closely and given appropriate doses of benzodiazepines or barbiturates to treat withdrawal signs. Cross-tolerant medication may be given on a fixed schedule or as symptom-triggered therapy. Severe withdrawal may require a continuous intravenous infusion in an ICU. Recognition and effective treatment of alcohol withdrawal can prevent significant complications in hospitalized patients. TH
Dr. Weaver is associate professor of internal medicine and psychiatry at Virginia Commonwealth University, Richmond.
References
- Saitz R. Introduction to alcohol withdrawal. Alcohol Health Res World. 1998;22(1):5-12.
- Cross GM, Hennessey PT. Principles and practice of detoxification. Prim Care. 1993;20(1):81-93.
- Cutshall BJ. The Saunderssutton syndrome: an analysis of delirium tremens. Q J Stud Alcohol. 1965;26(3):423-448.
- Sullivan JT, Sykora K, Schneiderman J, et al. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict. 1989;84:1353-1357.
- Foy A, March S, Drinkwater V. Use of an objective clinical scale in the assessment and management of alcohol withdrawal in a large general hospital. Alcohol Clin Exp Res. 1988;12(3):360-364.
- Weaver MF, Hoffman HJ, Johnson RE. Alcohol withdrawal pharmacotherapy for inpatients with medical comorbidity. J Addict Dis. 2006;25(2):17-24.
- Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA. 1997;278(2):144-151.
- Saitz R, Mayo-Smith MF, Roberts MS, et al. Individualized treatment for alcohol withdrawal. A randomized double-blind controlled trial. JAMA. 1994;272(7):519-523.
- Yeh HS, Dhopesh V, Maany I. Seizures during detoxification. J Gen Intern Med. 1992;7(1):123.
- Young GP, Rores C, Murphy C, et al. Intravenous phenobarbital for alcohol withdrawal and convulsions. Ann Emerg Med. 1987;16(8):847-850.
- Weaver MF, Jarvis MA, Schnoll SH. Role of the primary care physician in problems of substance abuse. Arch Intern Med. 1999;159(9):913-924.