User login
For all the differences highlighted in my April and May columns studying the 1995 and 1997 documentation guidelines set forth by the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA), decision making remains consistent in both.
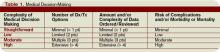
Physician documentation addresses the complexity of the patient’s condition in terms of the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality. The “diagnoses” and “data” categories follow a point system (see Table 1, below) determined by local Medicare contractors, whereas the “risk” category utilizes a universal table to define medical and/or procedural risks for the patient. The final result of complexity is classified as straightforward, low, moderate, or high.
A complete and accurate description of the patient’s condition should be conveyed through the plan of care. While acuity and severity may be inferred by a physician’s colleagues from particular pieces of information included in the record (e.g., critical lab values), the importance of this information may be lost on auditors and medical record reviewers. This article will assist in explaining the categories of medical decision making, as well as provide documentation tips to best represent patient complexity.
Diagnoses, Care Options
The plan of care outlines problems the physician personally manages and those that affect their management options, even if another physician directly oversees the problem. For example, the hospitalist may primarily manage a patient’s diabetes while the nephrologist manages renal insufficiency. Since the renal insufficiency may affect the hospitalist’s plan for diabetic management, the hospitalist receives credit for the documented renal insufficiency diagnosis and hospitalist-related care plan.
Physicians should address all problems in the documentation for each encounter regardless of any changes to the treatment plan. Credit is provided for each problem that has an associated plan, even if the plan states “continue same treatment.” Additional credit is provided when the treatment to be “continued” is referenced somewhere in the progress note (e.g., in the history).
The amount of credit varies depending upon the problem type. An established problem, defined as having a care plan established by the physician or someone from the same group practice during the current hospitalization, is considered less complex than an undiagnosed new problem for which a prognosis cannot be determined. Severity of the problem affects the weight of complexity. A stable, improving problem is not as complex as a progressing problem.
When documenting diagnoses/treatment options:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined; and
- Indicate the management/treatment option(s) for each problem.
When documentation indicates a continuation of current management options (e.g., “continue meds”), be sure the management options to be continued are noted somewhere in the progress note for that encounter (e.g., medication list).
Data Ordered/Reviewed
“Data” order/review comes in many forms: pathology/laboratory testing, radiology, and medicine-based diagnostics. Although an intuitive part of medical practice, the data section of the progress note is often underdocumented by physicians. Pertinent orders or results may be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note.
When documenting amount and/or complexity of data:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Test review may be documented by including a brief entry in the progress note (e.g., “decreased Hgb” or “CXR shows NAD”), or by dating and initialing the report;
- Physicians receive credit for reviewing old records or obtaining history from someone other than the patient, when necessary, as long as a summary of the review or discussion is documented in the medical record; and
- Indicate when images, tracings, or specimens are “personally reviewed” by the physician.
Discussion of unexpected or contradictory test results with the performing physician should be summarized in the medical record.
Risks of Complication
Risk is viewed in light of the patient’s presenting problem, diagnostic procedures ordered, and management options selected.
Risk is graded as minimal, low, moderate, and high with corresponding items that help to differentiate each level (see Table 2, right). The single highest item in any given risk category determines the risk level.
Chronic conditions and invasive procedures expose the patient to more risk than acute, uncomplicated illnesses or non-invasive procedures, respectively. As in the diagnoses/treatment options category, a stable or improving problem poses less risk than a progressing problem. Medication risk varies with the type and degree of potential adverse effects associated with each medication.
When documenting risk:
- Indicate status of all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), etc.;
- Document all diagnostic procedures being considered;
- Identify surgical risk factors involving co-morbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding. medication (e.g., “Continue coumadin, monitor PT/INR”). A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change.
Determine Complexity
To determine the final complexity of medical decision making, two of three categories must be met. For example, if a physician satisfies the requirements for “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician achieves moderate complexity decision-making.
Remember that decision-making is just one of three components of evaluation and management services, along with history and exam.
Determining the final visit level (e.g., 9922x) depends upon each of these three key components for initial hospital care and consultations, and two key components for subsequent hospital care. However, medical decision making always should drive visit level selection as it is the best representation of medical necessity for the service involved.
Contributory Factors
In addition to the three categories of medical decision making, a payer (e.g., TrailblazerHealth) may consider contributory factors when determining patient complexity and selecting visit levels.
For example, the nature of the presenting problem may play a role when reviewing claims for subsequent hospital care codes (99231-99233). Found in the code descriptors of the CPT manual, problems are identified as:
- 99231: Stable, recovering or improving;
- 99232: Responding inadequately to therapy or developed a minor complication; and
- 99233: Unstable or has developed a significant complication or a significant new problem.
Although this is not a general requirement, it represents a locally established standard for reviewing claims for medical necessity. It should not be used exclusively to determine the visit level.
Be sure to query your payer’s policy via written communication or Web site posting (e.g., www.trailblazerhealth.com/Publications/Job%20Aid/medical%20necessity.pdf) for guidance on how payers review documentation. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
For all the differences highlighted in my April and May columns studying the 1995 and 1997 documentation guidelines set forth by the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA), decision making remains consistent in both.
Physician documentation addresses the complexity of the patient’s condition in terms of the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality. The “diagnoses” and “data” categories follow a point system (see Table 1, below) determined by local Medicare contractors, whereas the “risk” category utilizes a universal table to define medical and/or procedural risks for the patient. The final result of complexity is classified as straightforward, low, moderate, or high.
A complete and accurate description of the patient’s condition should be conveyed through the plan of care. While acuity and severity may be inferred by a physician’s colleagues from particular pieces of information included in the record (e.g., critical lab values), the importance of this information may be lost on auditors and medical record reviewers. This article will assist in explaining the categories of medical decision making, as well as provide documentation tips to best represent patient complexity.
Diagnoses, Care Options
The plan of care outlines problems the physician personally manages and those that affect their management options, even if another physician directly oversees the problem. For example, the hospitalist may primarily manage a patient’s diabetes while the nephrologist manages renal insufficiency. Since the renal insufficiency may affect the hospitalist’s plan for diabetic management, the hospitalist receives credit for the documented renal insufficiency diagnosis and hospitalist-related care plan.
Physicians should address all problems in the documentation for each encounter regardless of any changes to the treatment plan. Credit is provided for each problem that has an associated plan, even if the plan states “continue same treatment.” Additional credit is provided when the treatment to be “continued” is referenced somewhere in the progress note (e.g., in the history).
The amount of credit varies depending upon the problem type. An established problem, defined as having a care plan established by the physician or someone from the same group practice during the current hospitalization, is considered less complex than an undiagnosed new problem for which a prognosis cannot be determined. Severity of the problem affects the weight of complexity. A stable, improving problem is not as complex as a progressing problem.
When documenting diagnoses/treatment options:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined; and
- Indicate the management/treatment option(s) for each problem.
When documentation indicates a continuation of current management options (e.g., “continue meds”), be sure the management options to be continued are noted somewhere in the progress note for that encounter (e.g., medication list).
Data Ordered/Reviewed
“Data” order/review comes in many forms: pathology/laboratory testing, radiology, and medicine-based diagnostics. Although an intuitive part of medical practice, the data section of the progress note is often underdocumented by physicians. Pertinent orders or results may be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note.
When documenting amount and/or complexity of data:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Test review may be documented by including a brief entry in the progress note (e.g., “decreased Hgb” or “CXR shows NAD”), or by dating and initialing the report;
- Physicians receive credit for reviewing old records or obtaining history from someone other than the patient, when necessary, as long as a summary of the review or discussion is documented in the medical record; and
- Indicate when images, tracings, or specimens are “personally reviewed” by the physician.
Discussion of unexpected or contradictory test results with the performing physician should be summarized in the medical record.
Risks of Complication
Risk is viewed in light of the patient’s presenting problem, diagnostic procedures ordered, and management options selected.
Risk is graded as minimal, low, moderate, and high with corresponding items that help to differentiate each level (see Table 2, right). The single highest item in any given risk category determines the risk level.
Chronic conditions and invasive procedures expose the patient to more risk than acute, uncomplicated illnesses or non-invasive procedures, respectively. As in the diagnoses/treatment options category, a stable or improving problem poses less risk than a progressing problem. Medication risk varies with the type and degree of potential adverse effects associated with each medication.
When documenting risk:
- Indicate status of all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), etc.;
- Document all diagnostic procedures being considered;
- Identify surgical risk factors involving co-morbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding. medication (e.g., “Continue coumadin, monitor PT/INR”). A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change.
Determine Complexity
To determine the final complexity of medical decision making, two of three categories must be met. For example, if a physician satisfies the requirements for “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician achieves moderate complexity decision-making.
Remember that decision-making is just one of three components of evaluation and management services, along with history and exam.
Determining the final visit level (e.g., 9922x) depends upon each of these three key components for initial hospital care and consultations, and two key components for subsequent hospital care. However, medical decision making always should drive visit level selection as it is the best representation of medical necessity for the service involved.
Contributory Factors
In addition to the three categories of medical decision making, a payer (e.g., TrailblazerHealth) may consider contributory factors when determining patient complexity and selecting visit levels.
For example, the nature of the presenting problem may play a role when reviewing claims for subsequent hospital care codes (99231-99233). Found in the code descriptors of the CPT manual, problems are identified as:
- 99231: Stable, recovering or improving;
- 99232: Responding inadequately to therapy or developed a minor complication; and
- 99233: Unstable or has developed a significant complication or a significant new problem.
Although this is not a general requirement, it represents a locally established standard for reviewing claims for medical necessity. It should not be used exclusively to determine the visit level.
Be sure to query your payer’s policy via written communication or Web site posting (e.g., www.trailblazerhealth.com/Publications/Job%20Aid/medical%20necessity.pdf) for guidance on how payers review documentation. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.
For all the differences highlighted in my April and May columns studying the 1995 and 1997 documentation guidelines set forth by the Centers for Medicare and Medicaid Services (CMS) and the American Medical Association (AMA), decision making remains consistent in both.
Physician documentation addresses the complexity of the patient’s condition in terms of the number of diagnoses and/or treatment options, the amount and/or complexity of data ordered/reviewed, and the risk of complications/morbidity/mortality. The “diagnoses” and “data” categories follow a point system (see Table 1, below) determined by local Medicare contractors, whereas the “risk” category utilizes a universal table to define medical and/or procedural risks for the patient. The final result of complexity is classified as straightforward, low, moderate, or high.
A complete and accurate description of the patient’s condition should be conveyed through the plan of care. While acuity and severity may be inferred by a physician’s colleagues from particular pieces of information included in the record (e.g., critical lab values), the importance of this information may be lost on auditors and medical record reviewers. This article will assist in explaining the categories of medical decision making, as well as provide documentation tips to best represent patient complexity.
Diagnoses, Care Options
The plan of care outlines problems the physician personally manages and those that affect their management options, even if another physician directly oversees the problem. For example, the hospitalist may primarily manage a patient’s diabetes while the nephrologist manages renal insufficiency. Since the renal insufficiency may affect the hospitalist’s plan for diabetic management, the hospitalist receives credit for the documented renal insufficiency diagnosis and hospitalist-related care plan.
Physicians should address all problems in the documentation for each encounter regardless of any changes to the treatment plan. Credit is provided for each problem that has an associated plan, even if the plan states “continue same treatment.” Additional credit is provided when the treatment to be “continued” is referenced somewhere in the progress note (e.g., in the history).
The amount of credit varies depending upon the problem type. An established problem, defined as having a care plan established by the physician or someone from the same group practice during the current hospitalization, is considered less complex than an undiagnosed new problem for which a prognosis cannot be determined. Severity of the problem affects the weight of complexity. A stable, improving problem is not as complex as a progressing problem.
When documenting diagnoses/treatment options:
- Identify all problems managed or addressed during each encounter;
- Identify problems as stable or progressing, when appropriate;
- Indicate differential diagnoses when the problem remains undefined; and
- Indicate the management/treatment option(s) for each problem.
When documentation indicates a continuation of current management options (e.g., “continue meds”), be sure the management options to be continued are noted somewhere in the progress note for that encounter (e.g., medication list).
Data Ordered/Reviewed
“Data” order/review comes in many forms: pathology/laboratory testing, radiology, and medicine-based diagnostics. Although an intuitive part of medical practice, the data section of the progress note is often underdocumented by physicians. Pertinent orders or results may be noted in the visit record, but most of the background interactions and communications involving testing are undetected when reviewing the progress note.
When documenting amount and/or complexity of data:
- Specify tests ordered and rationale in the physician’s progress note or make an entry that refers to another auditor-accessible location for ordered tests and studies;
- Test review may be documented by including a brief entry in the progress note (e.g., “decreased Hgb” or “CXR shows NAD”), or by dating and initialing the report;
- Physicians receive credit for reviewing old records or obtaining history from someone other than the patient, when necessary, as long as a summary of the review or discussion is documented in the medical record; and
- Indicate when images, tracings, or specimens are “personally reviewed” by the physician.
Discussion of unexpected or contradictory test results with the performing physician should be summarized in the medical record.
Risks of Complication
Risk is viewed in light of the patient’s presenting problem, diagnostic procedures ordered, and management options selected.
Risk is graded as minimal, low, moderate, and high with corresponding items that help to differentiate each level (see Table 2, right). The single highest item in any given risk category determines the risk level.
Chronic conditions and invasive procedures expose the patient to more risk than acute, uncomplicated illnesses or non-invasive procedures, respectively. As in the diagnoses/treatment options category, a stable or improving problem poses less risk than a progressing problem. Medication risk varies with the type and degree of potential adverse effects associated with each medication.
When documenting risk:
- Indicate status of all problems in the plan of care; identify them as stable, worsening, exacerbating (mild or severe), etc.;
- Document all diagnostic procedures being considered;
- Identify surgical risk factors involving co-morbid conditions, when appropriate; and
- Associate the labs ordered to monitor for toxicity with the corresponding. medication (e.g., “Continue coumadin, monitor PT/INR”). A patient maintains the same level of risk for a given medication whether the dosage is increased, decreased, or continued without change.
Determine Complexity
To determine the final complexity of medical decision making, two of three categories must be met. For example, if a physician satisfies the requirements for “multiple” diagnoses/treatment options, “minimal” data, and “high” risk, the physician achieves moderate complexity decision-making.
Remember that decision-making is just one of three components of evaluation and management services, along with history and exam.
Determining the final visit level (e.g., 9922x) depends upon each of these three key components for initial hospital care and consultations, and two key components for subsequent hospital care. However, medical decision making always should drive visit level selection as it is the best representation of medical necessity for the service involved.
Contributory Factors
In addition to the three categories of medical decision making, a payer (e.g., TrailblazerHealth) may consider contributory factors when determining patient complexity and selecting visit levels.
For example, the nature of the presenting problem may play a role when reviewing claims for subsequent hospital care codes (99231-99233). Found in the code descriptors of the CPT manual, problems are identified as:
- 99231: Stable, recovering or improving;
- 99232: Responding inadequately to therapy or developed a minor complication; and
- 99233: Unstable or has developed a significant complication or a significant new problem.
Although this is not a general requirement, it represents a locally established standard for reviewing claims for medical necessity. It should not be used exclusively to determine the visit level.
Be sure to query your payer’s policy via written communication or Web site posting (e.g., www.trailblazerhealth.com/Publications/Job%20Aid/medical%20necessity.pdf) for guidance on how payers review documentation. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She also is on the faculty of SHM’s inpatient coding course.