User login
Case Report
A 42-year-old man presented to our dermatology clinic for evaluation of “dark spots” on both hands for 2 months (Figure 1). He had been treated 1 month earlier with various topical agents, including mid-potency steroids and lightening agents, and had not seen a change. Interestingly, he reported recent-onset of similar lesions on the feet (Figure 2). Initially, our differential diagnosis indicated some form of postinflammatory hyperpigmentation, but the recent onset of the lesions on the feet 1 week prior, the distribution of the lesions, and the absence of an inciting factor did not fit the clinical picture. Among various laboratory tests, rapid plasma reagin was positive, and the patient was appropriately diagnosed and treated for secondary syphilis with 2.4 million U of benzathine penicillin.
 |
 |
The Great Masquerader
Syphilis has been called “the great masquerader” or “the great imitator” because it is protean in appearance, manifests in different stages, and can affect different parts of the body.1 In fact, another case of secondary syphilis I saw prior to this patient appeared different. Secondary syphilis has variable clinical presentations and thus is difficult to recognize. It is estimated that approximately half of community physicians will not clinically suspect secondary syphilis.2
Resurgence of Syphilis
It is not every day that you may diagnose syphilis in an outpatient clinic or consultation service, but it recently has been making resurgence, particularly in inner-city settings. Although syphilis is one of the oldest sexually transmitted diseases and has established and effective treatment options, it is now reemerging as a major public health problem in urban communities. A 2001 study by Williams and Ekundayo3 evaluated the distribution of and factors affecting the syphilis epidemic among inner-city minorities in Baltimore, Maryland, and found that it was the city with the highest number of syphilis cases in the nation, surpassing the national average of 2.6 cases per 100,000 population. The factors that particularly favored syphilis infectivity were poverty, poor communication with health care providers, exchanging sex for drugs, lower educational background, and inadequate health education.3 Although syphilis should not be forgotten as part of a differential diagnosis, preventative health education should be undertaken.
Diagnostic Approach
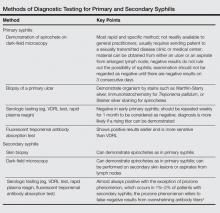
The best way to approach a possible case of syphilis is to have a high index of suspicion (Table). The skin findings of secondary syphilis may mimic other skin conditions (as described above), including pityriasis rosea, erythema multiforme, drug reactions, psoriasis, pityriasis lichenoides et varioliformis acuta, and dyshidrotic eczema, among others. Although the disease usually begins approximately 6 weeks after the onset of a primary chancre, approximately 25% of patients with secondary syphilis will not recall a chancre, and in other cases, the primary chancre will still be present.5 The case reported above did not have any other associated symptoms, but commonly reported symptoms in other cases have included headaches, fevers, pruritus, loss of appetite, and malaise.6
Clinical Features of Secondary Syphilis
Usually, the lesions of syphiloderms consist of variably scaly macules and papules that can be annular, pustular, or psoriasiform. They typically are widespread and symmetric, though in some cases they can remain localized. The appearance also may vary depending on immunocompromised status, which may cause a more aggressive and quicker appearance of the rash.
The Connection to Human Immunodeficiency Virus and AIDS
It is known that patients with syphilis have an increased incidence of other sexually transmitted infections such as venereal warts, gonorrhea, and human immunodeficiency virus (HIV) infection, thus patients should be tested for these conditions as part of their course of treatment. It has been shown that cutaneous sores/chancres facilitate transmission and acquisition of HIV infection. The risk for acquiring HIV increases 2- to 5-fold if exposure occurs when syphilis is present.7 Additionally, syphilis will increase viral loads in patients who are already infected with HIV. These data are concerning, particularly because many patients with syphilis also are infected with HIV.8
Final Thoughts
Although syphilis is known to present with highly variable clinical presentations, early diagnosis, appropriate treatment, and patient education are crucial to avoid further complications.9 Social factors have contributed to a resurgence of syphilis; although easily treatable, it can lead to great suffering and morbidity. In summary, syphilis is a treatable infectious disease and physicians should test for it when investigating a patient, particularly one with risk factors as well as a symmetric hyperpigmented rash on the acral surfaces. There are uncommon presentations of syphilis, thus it is important to consider it early on and treat appropriately to prevent life-threatening complications.
1. Tampa M, Sarbu I, Matei C, et al. Brief history of syphilis. J Med Life. 2014;7:4-10.
2. Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2007. Atlanta, GA: US Department of Health and Human Services; 2008.
3. Williams PB, Ekundayo O. Study of distribution and factors affecting syphilis epidemic among inner-city minorities of Baltimore. Public Health. 2001;115:387-393.
4. Ruchi S, Mangala HC, Murugesh SB, et al. Prozone phenomenon in secondary syphilis. Indian J Sex Trans Dis. 2011;32:47-49.
5. Lee V, Kinghorn G. Syphilis: an update. Clin Med. 2008;8:330-333.
6. Chapel TA. The signs and symptoms of secondary syphilis. Sex Transm Dis. 1980;7:161-164.
7. Bolan G. Syphilis and HIV: a dangerous duo affecting gay and bisexual men. https://blog.aids.gov/2012/12/ syphilis-and-hiv-a-dangerous-duo-affecting-gay-and -bisexual-men.html. Published December 13, 2012. Accessed August 19, 2015.
8. Zetola NM, Klausner JD. Syphilis and HIV infection: an update. Clin Infect Dis. 2007;44:1222-1228.
9. Green CB, Fitzpatrick J. Syphilis. In: Fitzpatrick J, Morelli J, eds. Dermatology Secrets Plus. Philadelphia, PA: Elsevier Mosby; 2011:195-200.
Case Report
A 42-year-old man presented to our dermatology clinic for evaluation of “dark spots” on both hands for 2 months (Figure 1). He had been treated 1 month earlier with various topical agents, including mid-potency steroids and lightening agents, and had not seen a change. Interestingly, he reported recent-onset of similar lesions on the feet (Figure 2). Initially, our differential diagnosis indicated some form of postinflammatory hyperpigmentation, but the recent onset of the lesions on the feet 1 week prior, the distribution of the lesions, and the absence of an inciting factor did not fit the clinical picture. Among various laboratory tests, rapid plasma reagin was positive, and the patient was appropriately diagnosed and treated for secondary syphilis with 2.4 million U of benzathine penicillin.
 |
 |
The Great Masquerader
Syphilis has been called “the great masquerader” or “the great imitator” because it is protean in appearance, manifests in different stages, and can affect different parts of the body.1 In fact, another case of secondary syphilis I saw prior to this patient appeared different. Secondary syphilis has variable clinical presentations and thus is difficult to recognize. It is estimated that approximately half of community physicians will not clinically suspect secondary syphilis.2
Resurgence of Syphilis
It is not every day that you may diagnose syphilis in an outpatient clinic or consultation service, but it recently has been making resurgence, particularly in inner-city settings. Although syphilis is one of the oldest sexually transmitted diseases and has established and effective treatment options, it is now reemerging as a major public health problem in urban communities. A 2001 study by Williams and Ekundayo3 evaluated the distribution of and factors affecting the syphilis epidemic among inner-city minorities in Baltimore, Maryland, and found that it was the city with the highest number of syphilis cases in the nation, surpassing the national average of 2.6 cases per 100,000 population. The factors that particularly favored syphilis infectivity were poverty, poor communication with health care providers, exchanging sex for drugs, lower educational background, and inadequate health education.3 Although syphilis should not be forgotten as part of a differential diagnosis, preventative health education should be undertaken.
Diagnostic Approach
The best way to approach a possible case of syphilis is to have a high index of suspicion (Table). The skin findings of secondary syphilis may mimic other skin conditions (as described above), including pityriasis rosea, erythema multiforme, drug reactions, psoriasis, pityriasis lichenoides et varioliformis acuta, and dyshidrotic eczema, among others. Although the disease usually begins approximately 6 weeks after the onset of a primary chancre, approximately 25% of patients with secondary syphilis will not recall a chancre, and in other cases, the primary chancre will still be present.5 The case reported above did not have any other associated symptoms, but commonly reported symptoms in other cases have included headaches, fevers, pruritus, loss of appetite, and malaise.6
Clinical Features of Secondary Syphilis
Usually, the lesions of syphiloderms consist of variably scaly macules and papules that can be annular, pustular, or psoriasiform. They typically are widespread and symmetric, though in some cases they can remain localized. The appearance also may vary depending on immunocompromised status, which may cause a more aggressive and quicker appearance of the rash.
The Connection to Human Immunodeficiency Virus and AIDS
It is known that patients with syphilis have an increased incidence of other sexually transmitted infections such as venereal warts, gonorrhea, and human immunodeficiency virus (HIV) infection, thus patients should be tested for these conditions as part of their course of treatment. It has been shown that cutaneous sores/chancres facilitate transmission and acquisition of HIV infection. The risk for acquiring HIV increases 2- to 5-fold if exposure occurs when syphilis is present.7 Additionally, syphilis will increase viral loads in patients who are already infected with HIV. These data are concerning, particularly because many patients with syphilis also are infected with HIV.8
Final Thoughts
Although syphilis is known to present with highly variable clinical presentations, early diagnosis, appropriate treatment, and patient education are crucial to avoid further complications.9 Social factors have contributed to a resurgence of syphilis; although easily treatable, it can lead to great suffering and morbidity. In summary, syphilis is a treatable infectious disease and physicians should test for it when investigating a patient, particularly one with risk factors as well as a symmetric hyperpigmented rash on the acral surfaces. There are uncommon presentations of syphilis, thus it is important to consider it early on and treat appropriately to prevent life-threatening complications.
Case Report
A 42-year-old man presented to our dermatology clinic for evaluation of “dark spots” on both hands for 2 months (Figure 1). He had been treated 1 month earlier with various topical agents, including mid-potency steroids and lightening agents, and had not seen a change. Interestingly, he reported recent-onset of similar lesions on the feet (Figure 2). Initially, our differential diagnosis indicated some form of postinflammatory hyperpigmentation, but the recent onset of the lesions on the feet 1 week prior, the distribution of the lesions, and the absence of an inciting factor did not fit the clinical picture. Among various laboratory tests, rapid plasma reagin was positive, and the patient was appropriately diagnosed and treated for secondary syphilis with 2.4 million U of benzathine penicillin.
 |
 |
The Great Masquerader
Syphilis has been called “the great masquerader” or “the great imitator” because it is protean in appearance, manifests in different stages, and can affect different parts of the body.1 In fact, another case of secondary syphilis I saw prior to this patient appeared different. Secondary syphilis has variable clinical presentations and thus is difficult to recognize. It is estimated that approximately half of community physicians will not clinically suspect secondary syphilis.2
Resurgence of Syphilis
It is not every day that you may diagnose syphilis in an outpatient clinic or consultation service, but it recently has been making resurgence, particularly in inner-city settings. Although syphilis is one of the oldest sexually transmitted diseases and has established and effective treatment options, it is now reemerging as a major public health problem in urban communities. A 2001 study by Williams and Ekundayo3 evaluated the distribution of and factors affecting the syphilis epidemic among inner-city minorities in Baltimore, Maryland, and found that it was the city with the highest number of syphilis cases in the nation, surpassing the national average of 2.6 cases per 100,000 population. The factors that particularly favored syphilis infectivity were poverty, poor communication with health care providers, exchanging sex for drugs, lower educational background, and inadequate health education.3 Although syphilis should not be forgotten as part of a differential diagnosis, preventative health education should be undertaken.
Diagnostic Approach
The best way to approach a possible case of syphilis is to have a high index of suspicion (Table). The skin findings of secondary syphilis may mimic other skin conditions (as described above), including pityriasis rosea, erythema multiforme, drug reactions, psoriasis, pityriasis lichenoides et varioliformis acuta, and dyshidrotic eczema, among others. Although the disease usually begins approximately 6 weeks after the onset of a primary chancre, approximately 25% of patients with secondary syphilis will not recall a chancre, and in other cases, the primary chancre will still be present.5 The case reported above did not have any other associated symptoms, but commonly reported symptoms in other cases have included headaches, fevers, pruritus, loss of appetite, and malaise.6
Clinical Features of Secondary Syphilis
Usually, the lesions of syphiloderms consist of variably scaly macules and papules that can be annular, pustular, or psoriasiform. They typically are widespread and symmetric, though in some cases they can remain localized. The appearance also may vary depending on immunocompromised status, which may cause a more aggressive and quicker appearance of the rash.
The Connection to Human Immunodeficiency Virus and AIDS
It is known that patients with syphilis have an increased incidence of other sexually transmitted infections such as venereal warts, gonorrhea, and human immunodeficiency virus (HIV) infection, thus patients should be tested for these conditions as part of their course of treatment. It has been shown that cutaneous sores/chancres facilitate transmission and acquisition of HIV infection. The risk for acquiring HIV increases 2- to 5-fold if exposure occurs when syphilis is present.7 Additionally, syphilis will increase viral loads in patients who are already infected with HIV. These data are concerning, particularly because many patients with syphilis also are infected with HIV.8
Final Thoughts
Although syphilis is known to present with highly variable clinical presentations, early diagnosis, appropriate treatment, and patient education are crucial to avoid further complications.9 Social factors have contributed to a resurgence of syphilis; although easily treatable, it can lead to great suffering and morbidity. In summary, syphilis is a treatable infectious disease and physicians should test for it when investigating a patient, particularly one with risk factors as well as a symmetric hyperpigmented rash on the acral surfaces. There are uncommon presentations of syphilis, thus it is important to consider it early on and treat appropriately to prevent life-threatening complications.
1. Tampa M, Sarbu I, Matei C, et al. Brief history of syphilis. J Med Life. 2014;7:4-10.
2. Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2007. Atlanta, GA: US Department of Health and Human Services; 2008.
3. Williams PB, Ekundayo O. Study of distribution and factors affecting syphilis epidemic among inner-city minorities of Baltimore. Public Health. 2001;115:387-393.
4. Ruchi S, Mangala HC, Murugesh SB, et al. Prozone phenomenon in secondary syphilis. Indian J Sex Trans Dis. 2011;32:47-49.
5. Lee V, Kinghorn G. Syphilis: an update. Clin Med. 2008;8:330-333.
6. Chapel TA. The signs and symptoms of secondary syphilis. Sex Transm Dis. 1980;7:161-164.
7. Bolan G. Syphilis and HIV: a dangerous duo affecting gay and bisexual men. https://blog.aids.gov/2012/12/ syphilis-and-hiv-a-dangerous-duo-affecting-gay-and -bisexual-men.html. Published December 13, 2012. Accessed August 19, 2015.
8. Zetola NM, Klausner JD. Syphilis and HIV infection: an update. Clin Infect Dis. 2007;44:1222-1228.
9. Green CB, Fitzpatrick J. Syphilis. In: Fitzpatrick J, Morelli J, eds. Dermatology Secrets Plus. Philadelphia, PA: Elsevier Mosby; 2011:195-200.
1. Tampa M, Sarbu I, Matei C, et al. Brief history of syphilis. J Med Life. 2014;7:4-10.
2. Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2007. Atlanta, GA: US Department of Health and Human Services; 2008.
3. Williams PB, Ekundayo O. Study of distribution and factors affecting syphilis epidemic among inner-city minorities of Baltimore. Public Health. 2001;115:387-393.
4. Ruchi S, Mangala HC, Murugesh SB, et al. Prozone phenomenon in secondary syphilis. Indian J Sex Trans Dis. 2011;32:47-49.
5. Lee V, Kinghorn G. Syphilis: an update. Clin Med. 2008;8:330-333.
6. Chapel TA. The signs and symptoms of secondary syphilis. Sex Transm Dis. 1980;7:161-164.
7. Bolan G. Syphilis and HIV: a dangerous duo affecting gay and bisexual men. https://blog.aids.gov/2012/12/ syphilis-and-hiv-a-dangerous-duo-affecting-gay-and -bisexual-men.html. Published December 13, 2012. Accessed August 19, 2015.
8. Zetola NM, Klausner JD. Syphilis and HIV infection: an update. Clin Infect Dis. 2007;44:1222-1228.
9. Green CB, Fitzpatrick J. Syphilis. In: Fitzpatrick J, Morelli J, eds. Dermatology Secrets Plus. Philadelphia, PA: Elsevier Mosby; 2011:195-200.