User login
In the early morning hours of June 10, 2009, a 77-year-old man who had been undergoing chemotherapy for multiple myeloma took sleep medication. He then fell down a flight of stairs in his split-level home.
The patient sustained a laceration to his scalp but returned to bed and waited until later that morning to call his internist for an appointment. Later that day, the physician placed 11 sutures for the scalp laceration and performed a neurologic examination; he did not note any abnormalities. The patient complained of back pain, so the physician ordered a back x-ray, which revealed a TI2 fracture that had occurred from the fall. No further treatment was provided for the scalp injury, except removal of the stitches about a week later.
Six days after the fall and doctor visit, the patient’s condition began to deteriorate rapidly, with noted slurred speech and loss of consciousness. He was transported to an emergency department, where CT revealed a massive subdural hematoma. An immediate craniotomy was performed. However, on June 27, 2009, the patient died as a result of the brain bleed.
His estate filed suit against the physician and his practice, alleging medical malpractice and violations in the standard of care. The estate alleged that the standard of care required the physician to obtain a CT scan and that, had one been performed, it would have revealed a small subdural hematoma in time for it to have been successfully treated (ie, before the massive second related bleed). The estate’s theory of the case did not rest on the presentation of clinical symptoms. A medical expert who testified for the estate stated that the subdural hematoma began at the time of the fall.
The defense denied any violations in the standard of care. The physician contended that the patient had presented with no symptoms other than a head laceration, and there were no criteria for ordering CT. Further, the defense asserted that the patient was symptom free for 6 days post-fall. According to the defense, the patient experienced a sudden arterial bleed that was not caused by the fall and would not have been revealed on CT ordered at the time of initial presentation, because it did not occur until 6 days later.
VERDICT
After a 10-day trial and 25 minutes’ deliberation, the jury returned a defense verdict.
COMMENTARY
The 25-minute deliberation suggests that terms such as “bridging veins” and “shearing injury” were unlikely bandied about in the jury room. The jury was likely dismissive of the plaintiff’s claim owing to his cancer diagnosis, and perhaps rightly so. But if we eliminate the multiple myeloma diagnosis, the jury might have decided differently.
Continue to: The defendant physician...
The defendant physician did a good job of documenting a negative neurologic exam, which helped him convince the jury that the patient did not have any signs or symptoms when first evaluated. But in this patient, was imaging to rule out intracranial bleeding indicated?
As an oversimplification, we tend to think of intracranial hemorrhage in 2 varieties: the insidious and the bold. Subdural hematomas are stealthy, they are sneaky, and they prey on the old. They step out of the shadows to cause symptoms. They are the ninjas of intracranial hemorrhage. Beware.
Epidural hematomas and subarachnoid hemorrhage (SAH) are the opposite. They classically present with a sudden and severe symptom complex: with epidural hematoma, the loss of consciousness, lucid interval, and final loss of consciousness; with SAH, the “worst in your life” thunder-clap headache, which may be heralded by a sentinel headache.1 When manifesting this way, they are brash, direct, and unsubtle to the point of being obnoxious—the Steven Stifler of intracranial bleeding.
This generalization is made to highlight the potentially sneaky nature of subdural hemorrhage. There are circumstances in which the clinical presentation of epidural hematoma and SAH will be more challenging. The question here is whether a negative initial neurologic exam can adequately screen for a potentially stealthy subdural hematoma.
Subdural hemorrhage is caused by rapidly changing velocity that may stretch and tear small bridging veins.2,3 Subdural hematoma is more common in the elderly, those who abuse alcohol, and those with a prior history of head trauma.4 As the brain shrinks with age or atrophy, the subdural space enlarges and traversing veins are stretched to cover a wider distance—rendering them vulnerable to rupture.5 These structures may also weaken as a result of low cerebrospinal fluid (intracranial hypotension); as pressure decreases (eg, from a leak), the brain’s buoyancy is reduced, causing traction on anchoring and supporting structures (eg, bridging veins).5 Injury to bridging veins can even occur as a result of a coup-contrecoup mechanism in the absence of direct physical impact.6,7 Bottom line: the injury itself may be subtle, requiring an index of suspicion to make the diagnosis.
Continue to: The case patient was...
The case patient was elderly. He had a chronic malignancy and sustained a fall down the stairs. He was taking sleeping pills, which may have slowed reflexive protective mechanisms after he started to fall (resulting in greater force imparted to his head). Multiple myeloma can predispose a patient to coagulopathy, and we don’t know in this case if this patient’s multiple myeloma made him more susceptible to bleeding—but it certainly didn’t help.8 The patient’s age, the mechanism of injury, and the history of malignancy made this a setup for hemorrhage.
Interestingly, we are not given details about how the patient looked during his suture removal. We are told the time between the initial fall and deterioration was 6 days. Scalp sutures were removed “about a week later,” which was after the deterioration—so this can’t be correct. Removing scalp sutures after 5 days seems premature, but that is the only possibility if 6 days elapsed between the fall and the deterioration.
In short, these are difficult cases. If intracranial bleeding can be subtle and delayed, how can we be sure a patient is not experiencing a bleed? We can only apply the relevant standard of care using all the clinical information we have. The Canadian CT Head Rule and New Orleans Criteria are clinical tools designed to help providers determine when to image (see Table for details).9
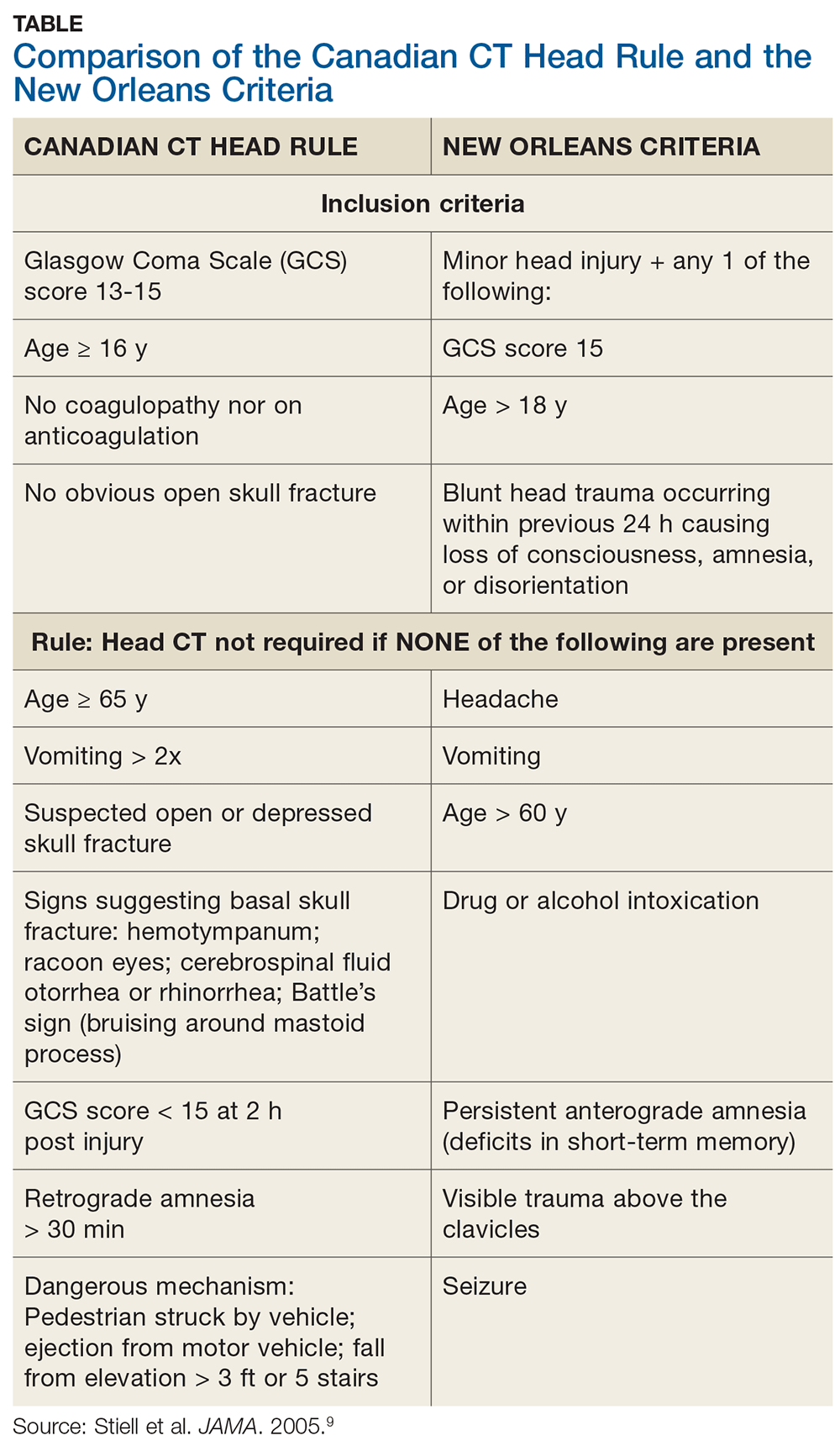
Applying the Canadian CT Head Rule to the facts of this case, we would image the patient because he fell down a “flight” of stairs (which is > 5 stairs) and he is 77 years old (older than 65). The New Orleans Criteria require head CT for minor injury with any positive findings.9 Because the patient is older than 60, he would be scanned according this rule.
In this case, the tools indicate scanning would have been appropriate. The patient’s multiple myeloma might have further impelled a decision to image. However, the jury was persuaded that the defendant’s negative neurologic exam was reasonable under the circumstances. This was likely made possible by the physician’s good recordkeeping and demonstrated genuine concern for the patient’s well-being—as well as a differing viewpoint of the patient’s age and health status.
Continue to: Finally, a word about...
Finally, a word about falls and the elderly: We’ve all heard the 80s advertising catchphrase (which lives on as a present-day meme) “I’ve fallen, and I can’t get up!” The problem is, many don’t. It would be more clinically accurate to say, “I’ve fallen, and I’ll be hospitalized for an extended period of time, then transferred to a skilled nursing facility, but I won’t survive to discharge.” The reality is that falls kill, and the severity is underestimated.10 If it were a “brain-eating amoeba,” the media would be all over it. With falls, not so much. We tend to pay less attention.
Risk factors for a fall include postural hypotension; use of benzodiazepines or other sedative-hypnotic drugs; use of ≥ 4 medications; environmental hazards for tripping; impairment in balance and transfer skills; and gait impairment.11 Home setup also contributes—loose throw rugs, uneven carpet edges, cracked sidewalks, clutter and furniture, cables and wires and cords, oh my.
Do your older patients a favor by reinforcing fall risk. Instruct them to rise slowly from seated or recumbent positions; always consider central nervous system sedation and/or the coordination-hampering properties of medications, particularly in combination. Raise the issue of home safety. A brief 10-second comment from you may plant a seed in a family member’s head to do what you cannot: scan and make safe the patient’s living environment.
1. de Falco FA. Sentinel headache. Neurol Sci. 2004;25(suppl 3):S215-S217.
2. Miller JD, Nader R. Acute subdural hematoma from bridging vein rupture: a potential mechanism for growth. J Neurosurg. 2014;120(6):1378-1384.
3. Victor M, Ropper A. Craniocerebral trauma. In: Victor M, Ropper A, eds. Adams and Victor’s Principles of Neurology. 7th ed. New York, NY: McGraw-Hill; 2001:925.
4. McBridde W. Subdural hematoma in adults: etiology, clinical features, and diagnosis. UpToDate website. www.uptodate.com/contents/subdural-hematoma-in-adults-etiology-clinical-features-and-diagnosis? search=subdural%20hematoma. Published December 10, 2018. Accessed September 23, 2019.
5. US National Library of Medicine. Subdural hematoma. Medline Plus website. https://medlineplus.gov/ency/article/000713.htm. Accessed September 23, 2019.
6. Besenski N. Traumatic injuries: imaging of head injuries. Eur Radiol. 2002;12(6):1237-1252.
7. Mayer S, Rowland L. Head injury. In: Rowland L, ed. Merritt’s Neurology. Philadelphia, PA: Lippincott Williams & Wilkins; 2000:401.
8. Saif MW, Allegra CJ, Greenberg B. Bleeding diathesis in multiple myeloma. J Hematother Stem Cell Res. 2001;10(5):657-660.
9. Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005;294(12):1511-1518.
10. Abdelrahman H, Almadani A, El-Menyar A, et al. Home-related falls: an underestimated mechanism of injury. J Family Community Med. 2018; 25(1):48-51.
11. Fuller GF. Falls in the elderly. Am Fam Physician. 2000;61(7):2159-2168.
In the early morning hours of June 10, 2009, a 77-year-old man who had been undergoing chemotherapy for multiple myeloma took sleep medication. He then fell down a flight of stairs in his split-level home.
The patient sustained a laceration to his scalp but returned to bed and waited until later that morning to call his internist for an appointment. Later that day, the physician placed 11 sutures for the scalp laceration and performed a neurologic examination; he did not note any abnormalities. The patient complained of back pain, so the physician ordered a back x-ray, which revealed a TI2 fracture that had occurred from the fall. No further treatment was provided for the scalp injury, except removal of the stitches about a week later.
Six days after the fall and doctor visit, the patient’s condition began to deteriorate rapidly, with noted slurred speech and loss of consciousness. He was transported to an emergency department, where CT revealed a massive subdural hematoma. An immediate craniotomy was performed. However, on June 27, 2009, the patient died as a result of the brain bleed.
His estate filed suit against the physician and his practice, alleging medical malpractice and violations in the standard of care. The estate alleged that the standard of care required the physician to obtain a CT scan and that, had one been performed, it would have revealed a small subdural hematoma in time for it to have been successfully treated (ie, before the massive second related bleed). The estate’s theory of the case did not rest on the presentation of clinical symptoms. A medical expert who testified for the estate stated that the subdural hematoma began at the time of the fall.
The defense denied any violations in the standard of care. The physician contended that the patient had presented with no symptoms other than a head laceration, and there were no criteria for ordering CT. Further, the defense asserted that the patient was symptom free for 6 days post-fall. According to the defense, the patient experienced a sudden arterial bleed that was not caused by the fall and would not have been revealed on CT ordered at the time of initial presentation, because it did not occur until 6 days later.
VERDICT
After a 10-day trial and 25 minutes’ deliberation, the jury returned a defense verdict.
COMMENTARY
The 25-minute deliberation suggests that terms such as “bridging veins” and “shearing injury” were unlikely bandied about in the jury room. The jury was likely dismissive of the plaintiff’s claim owing to his cancer diagnosis, and perhaps rightly so. But if we eliminate the multiple myeloma diagnosis, the jury might have decided differently.
Continue to: The defendant physician...
The defendant physician did a good job of documenting a negative neurologic exam, which helped him convince the jury that the patient did not have any signs or symptoms when first evaluated. But in this patient, was imaging to rule out intracranial bleeding indicated?
As an oversimplification, we tend to think of intracranial hemorrhage in 2 varieties: the insidious and the bold. Subdural hematomas are stealthy, they are sneaky, and they prey on the old. They step out of the shadows to cause symptoms. They are the ninjas of intracranial hemorrhage. Beware.
Epidural hematomas and subarachnoid hemorrhage (SAH) are the opposite. They classically present with a sudden and severe symptom complex: with epidural hematoma, the loss of consciousness, lucid interval, and final loss of consciousness; with SAH, the “worst in your life” thunder-clap headache, which may be heralded by a sentinel headache.1 When manifesting this way, they are brash, direct, and unsubtle to the point of being obnoxious—the Steven Stifler of intracranial bleeding.
This generalization is made to highlight the potentially sneaky nature of subdural hemorrhage. There are circumstances in which the clinical presentation of epidural hematoma and SAH will be more challenging. The question here is whether a negative initial neurologic exam can adequately screen for a potentially stealthy subdural hematoma.
Subdural hemorrhage is caused by rapidly changing velocity that may stretch and tear small bridging veins.2,3 Subdural hematoma is more common in the elderly, those who abuse alcohol, and those with a prior history of head trauma.4 As the brain shrinks with age or atrophy, the subdural space enlarges and traversing veins are stretched to cover a wider distance—rendering them vulnerable to rupture.5 These structures may also weaken as a result of low cerebrospinal fluid (intracranial hypotension); as pressure decreases (eg, from a leak), the brain’s buoyancy is reduced, causing traction on anchoring and supporting structures (eg, bridging veins).5 Injury to bridging veins can even occur as a result of a coup-contrecoup mechanism in the absence of direct physical impact.6,7 Bottom line: the injury itself may be subtle, requiring an index of suspicion to make the diagnosis.
Continue to: The case patient was...
The case patient was elderly. He had a chronic malignancy and sustained a fall down the stairs. He was taking sleeping pills, which may have slowed reflexive protective mechanisms after he started to fall (resulting in greater force imparted to his head). Multiple myeloma can predispose a patient to coagulopathy, and we don’t know in this case if this patient’s multiple myeloma made him more susceptible to bleeding—but it certainly didn’t help.8 The patient’s age, the mechanism of injury, and the history of malignancy made this a setup for hemorrhage.
Interestingly, we are not given details about how the patient looked during his suture removal. We are told the time between the initial fall and deterioration was 6 days. Scalp sutures were removed “about a week later,” which was after the deterioration—so this can’t be correct. Removing scalp sutures after 5 days seems premature, but that is the only possibility if 6 days elapsed between the fall and the deterioration.
In short, these are difficult cases. If intracranial bleeding can be subtle and delayed, how can we be sure a patient is not experiencing a bleed? We can only apply the relevant standard of care using all the clinical information we have. The Canadian CT Head Rule and New Orleans Criteria are clinical tools designed to help providers determine when to image (see Table for details).9
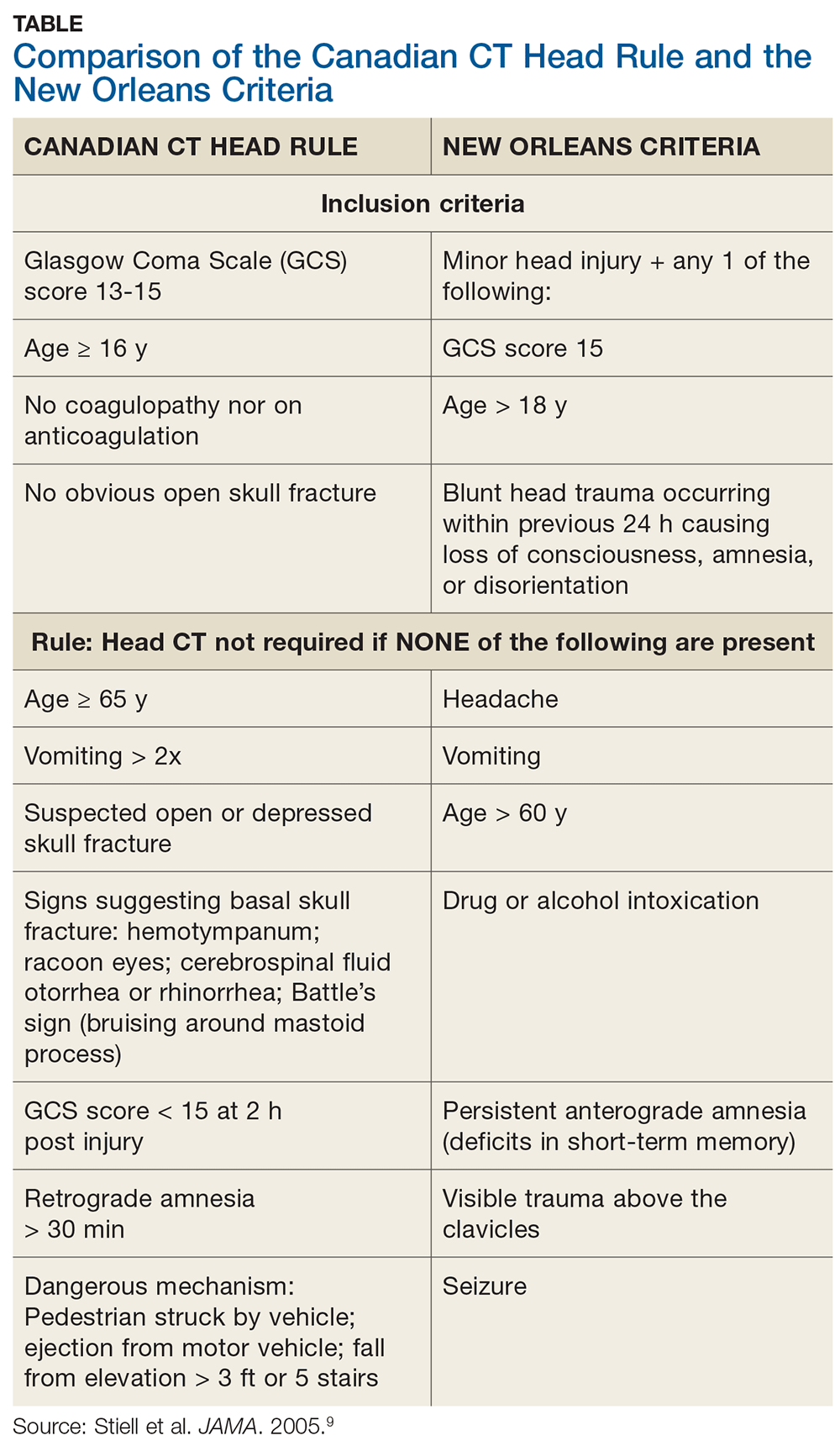
Applying the Canadian CT Head Rule to the facts of this case, we would image the patient because he fell down a “flight” of stairs (which is > 5 stairs) and he is 77 years old (older than 65). The New Orleans Criteria require head CT for minor injury with any positive findings.9 Because the patient is older than 60, he would be scanned according this rule.
In this case, the tools indicate scanning would have been appropriate. The patient’s multiple myeloma might have further impelled a decision to image. However, the jury was persuaded that the defendant’s negative neurologic exam was reasonable under the circumstances. This was likely made possible by the physician’s good recordkeeping and demonstrated genuine concern for the patient’s well-being—as well as a differing viewpoint of the patient’s age and health status.
Continue to: Finally, a word about...
Finally, a word about falls and the elderly: We’ve all heard the 80s advertising catchphrase (which lives on as a present-day meme) “I’ve fallen, and I can’t get up!” The problem is, many don’t. It would be more clinically accurate to say, “I’ve fallen, and I’ll be hospitalized for an extended period of time, then transferred to a skilled nursing facility, but I won’t survive to discharge.” The reality is that falls kill, and the severity is underestimated.10 If it were a “brain-eating amoeba,” the media would be all over it. With falls, not so much. We tend to pay less attention.
Risk factors for a fall include postural hypotension; use of benzodiazepines or other sedative-hypnotic drugs; use of ≥ 4 medications; environmental hazards for tripping; impairment in balance and transfer skills; and gait impairment.11 Home setup also contributes—loose throw rugs, uneven carpet edges, cracked sidewalks, clutter and furniture, cables and wires and cords, oh my.
Do your older patients a favor by reinforcing fall risk. Instruct them to rise slowly from seated or recumbent positions; always consider central nervous system sedation and/or the coordination-hampering properties of medications, particularly in combination. Raise the issue of home safety. A brief 10-second comment from you may plant a seed in a family member’s head to do what you cannot: scan and make safe the patient’s living environment.
In the early morning hours of June 10, 2009, a 77-year-old man who had been undergoing chemotherapy for multiple myeloma took sleep medication. He then fell down a flight of stairs in his split-level home.
The patient sustained a laceration to his scalp but returned to bed and waited until later that morning to call his internist for an appointment. Later that day, the physician placed 11 sutures for the scalp laceration and performed a neurologic examination; he did not note any abnormalities. The patient complained of back pain, so the physician ordered a back x-ray, which revealed a TI2 fracture that had occurred from the fall. No further treatment was provided for the scalp injury, except removal of the stitches about a week later.
Six days after the fall and doctor visit, the patient’s condition began to deteriorate rapidly, with noted slurred speech and loss of consciousness. He was transported to an emergency department, where CT revealed a massive subdural hematoma. An immediate craniotomy was performed. However, on June 27, 2009, the patient died as a result of the brain bleed.
His estate filed suit against the physician and his practice, alleging medical malpractice and violations in the standard of care. The estate alleged that the standard of care required the physician to obtain a CT scan and that, had one been performed, it would have revealed a small subdural hematoma in time for it to have been successfully treated (ie, before the massive second related bleed). The estate’s theory of the case did not rest on the presentation of clinical symptoms. A medical expert who testified for the estate stated that the subdural hematoma began at the time of the fall.
The defense denied any violations in the standard of care. The physician contended that the patient had presented with no symptoms other than a head laceration, and there were no criteria for ordering CT. Further, the defense asserted that the patient was symptom free for 6 days post-fall. According to the defense, the patient experienced a sudden arterial bleed that was not caused by the fall and would not have been revealed on CT ordered at the time of initial presentation, because it did not occur until 6 days later.
VERDICT
After a 10-day trial and 25 minutes’ deliberation, the jury returned a defense verdict.
COMMENTARY
The 25-minute deliberation suggests that terms such as “bridging veins” and “shearing injury” were unlikely bandied about in the jury room. The jury was likely dismissive of the plaintiff’s claim owing to his cancer diagnosis, and perhaps rightly so. But if we eliminate the multiple myeloma diagnosis, the jury might have decided differently.
Continue to: The defendant physician...
The defendant physician did a good job of documenting a negative neurologic exam, which helped him convince the jury that the patient did not have any signs or symptoms when first evaluated. But in this patient, was imaging to rule out intracranial bleeding indicated?
As an oversimplification, we tend to think of intracranial hemorrhage in 2 varieties: the insidious and the bold. Subdural hematomas are stealthy, they are sneaky, and they prey on the old. They step out of the shadows to cause symptoms. They are the ninjas of intracranial hemorrhage. Beware.
Epidural hematomas and subarachnoid hemorrhage (SAH) are the opposite. They classically present with a sudden and severe symptom complex: with epidural hematoma, the loss of consciousness, lucid interval, and final loss of consciousness; with SAH, the “worst in your life” thunder-clap headache, which may be heralded by a sentinel headache.1 When manifesting this way, they are brash, direct, and unsubtle to the point of being obnoxious—the Steven Stifler of intracranial bleeding.
This generalization is made to highlight the potentially sneaky nature of subdural hemorrhage. There are circumstances in which the clinical presentation of epidural hematoma and SAH will be more challenging. The question here is whether a negative initial neurologic exam can adequately screen for a potentially stealthy subdural hematoma.
Subdural hemorrhage is caused by rapidly changing velocity that may stretch and tear small bridging veins.2,3 Subdural hematoma is more common in the elderly, those who abuse alcohol, and those with a prior history of head trauma.4 As the brain shrinks with age or atrophy, the subdural space enlarges and traversing veins are stretched to cover a wider distance—rendering them vulnerable to rupture.5 These structures may also weaken as a result of low cerebrospinal fluid (intracranial hypotension); as pressure decreases (eg, from a leak), the brain’s buoyancy is reduced, causing traction on anchoring and supporting structures (eg, bridging veins).5 Injury to bridging veins can even occur as a result of a coup-contrecoup mechanism in the absence of direct physical impact.6,7 Bottom line: the injury itself may be subtle, requiring an index of suspicion to make the diagnosis.
Continue to: The case patient was...
The case patient was elderly. He had a chronic malignancy and sustained a fall down the stairs. He was taking sleeping pills, which may have slowed reflexive protective mechanisms after he started to fall (resulting in greater force imparted to his head). Multiple myeloma can predispose a patient to coagulopathy, and we don’t know in this case if this patient’s multiple myeloma made him more susceptible to bleeding—but it certainly didn’t help.8 The patient’s age, the mechanism of injury, and the history of malignancy made this a setup for hemorrhage.
Interestingly, we are not given details about how the patient looked during his suture removal. We are told the time between the initial fall and deterioration was 6 days. Scalp sutures were removed “about a week later,” which was after the deterioration—so this can’t be correct. Removing scalp sutures after 5 days seems premature, but that is the only possibility if 6 days elapsed between the fall and the deterioration.
In short, these are difficult cases. If intracranial bleeding can be subtle and delayed, how can we be sure a patient is not experiencing a bleed? We can only apply the relevant standard of care using all the clinical information we have. The Canadian CT Head Rule and New Orleans Criteria are clinical tools designed to help providers determine when to image (see Table for details).9
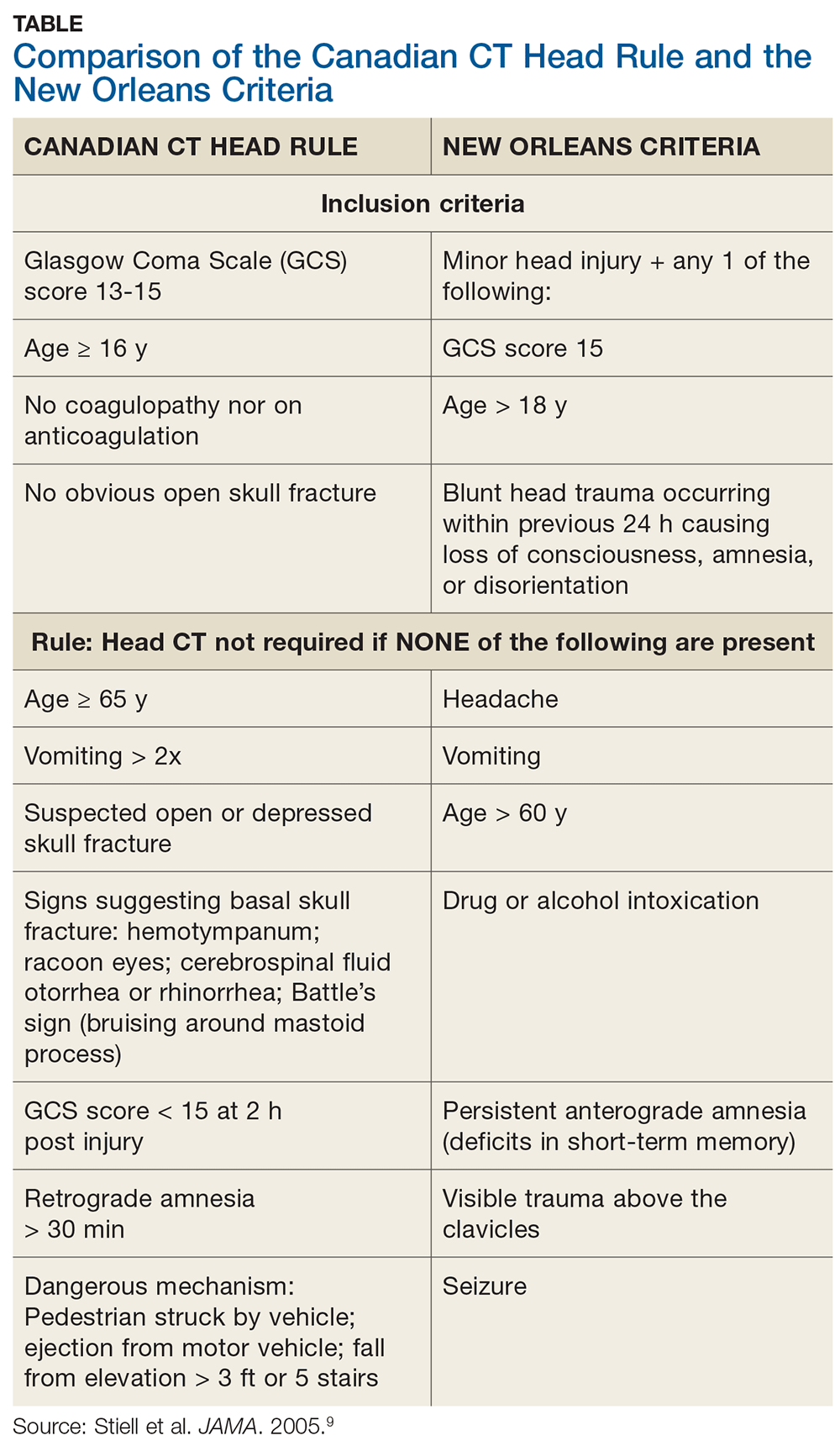
Applying the Canadian CT Head Rule to the facts of this case, we would image the patient because he fell down a “flight” of stairs (which is > 5 stairs) and he is 77 years old (older than 65). The New Orleans Criteria require head CT for minor injury with any positive findings.9 Because the patient is older than 60, he would be scanned according this rule.
In this case, the tools indicate scanning would have been appropriate. The patient’s multiple myeloma might have further impelled a decision to image. However, the jury was persuaded that the defendant’s negative neurologic exam was reasonable under the circumstances. This was likely made possible by the physician’s good recordkeeping and demonstrated genuine concern for the patient’s well-being—as well as a differing viewpoint of the patient’s age and health status.
Continue to: Finally, a word about...
Finally, a word about falls and the elderly: We’ve all heard the 80s advertising catchphrase (which lives on as a present-day meme) “I’ve fallen, and I can’t get up!” The problem is, many don’t. It would be more clinically accurate to say, “I’ve fallen, and I’ll be hospitalized for an extended period of time, then transferred to a skilled nursing facility, but I won’t survive to discharge.” The reality is that falls kill, and the severity is underestimated.10 If it were a “brain-eating amoeba,” the media would be all over it. With falls, not so much. We tend to pay less attention.
Risk factors for a fall include postural hypotension; use of benzodiazepines or other sedative-hypnotic drugs; use of ≥ 4 medications; environmental hazards for tripping; impairment in balance and transfer skills; and gait impairment.11 Home setup also contributes—loose throw rugs, uneven carpet edges, cracked sidewalks, clutter and furniture, cables and wires and cords, oh my.
Do your older patients a favor by reinforcing fall risk. Instruct them to rise slowly from seated or recumbent positions; always consider central nervous system sedation and/or the coordination-hampering properties of medications, particularly in combination. Raise the issue of home safety. A brief 10-second comment from you may plant a seed in a family member’s head to do what you cannot: scan and make safe the patient’s living environment.
1. de Falco FA. Sentinel headache. Neurol Sci. 2004;25(suppl 3):S215-S217.
2. Miller JD, Nader R. Acute subdural hematoma from bridging vein rupture: a potential mechanism for growth. J Neurosurg. 2014;120(6):1378-1384.
3. Victor M, Ropper A. Craniocerebral trauma. In: Victor M, Ropper A, eds. Adams and Victor’s Principles of Neurology. 7th ed. New York, NY: McGraw-Hill; 2001:925.
4. McBridde W. Subdural hematoma in adults: etiology, clinical features, and diagnosis. UpToDate website. www.uptodate.com/contents/subdural-hematoma-in-adults-etiology-clinical-features-and-diagnosis? search=subdural%20hematoma. Published December 10, 2018. Accessed September 23, 2019.
5. US National Library of Medicine. Subdural hematoma. Medline Plus website. https://medlineplus.gov/ency/article/000713.htm. Accessed September 23, 2019.
6. Besenski N. Traumatic injuries: imaging of head injuries. Eur Radiol. 2002;12(6):1237-1252.
7. Mayer S, Rowland L. Head injury. In: Rowland L, ed. Merritt’s Neurology. Philadelphia, PA: Lippincott Williams & Wilkins; 2000:401.
8. Saif MW, Allegra CJ, Greenberg B. Bleeding diathesis in multiple myeloma. J Hematother Stem Cell Res. 2001;10(5):657-660.
9. Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005;294(12):1511-1518.
10. Abdelrahman H, Almadani A, El-Menyar A, et al. Home-related falls: an underestimated mechanism of injury. J Family Community Med. 2018; 25(1):48-51.
11. Fuller GF. Falls in the elderly. Am Fam Physician. 2000;61(7):2159-2168.
1. de Falco FA. Sentinel headache. Neurol Sci. 2004;25(suppl 3):S215-S217.
2. Miller JD, Nader R. Acute subdural hematoma from bridging vein rupture: a potential mechanism for growth. J Neurosurg. 2014;120(6):1378-1384.
3. Victor M, Ropper A. Craniocerebral trauma. In: Victor M, Ropper A, eds. Adams and Victor’s Principles of Neurology. 7th ed. New York, NY: McGraw-Hill; 2001:925.
4. McBridde W. Subdural hematoma in adults: etiology, clinical features, and diagnosis. UpToDate website. www.uptodate.com/contents/subdural-hematoma-in-adults-etiology-clinical-features-and-diagnosis? search=subdural%20hematoma. Published December 10, 2018. Accessed September 23, 2019.
5. US National Library of Medicine. Subdural hematoma. Medline Plus website. https://medlineplus.gov/ency/article/000713.htm. Accessed September 23, 2019.
6. Besenski N. Traumatic injuries: imaging of head injuries. Eur Radiol. 2002;12(6):1237-1252.
7. Mayer S, Rowland L. Head injury. In: Rowland L, ed. Merritt’s Neurology. Philadelphia, PA: Lippincott Williams & Wilkins; 2000:401.
8. Saif MW, Allegra CJ, Greenberg B. Bleeding diathesis in multiple myeloma. J Hematother Stem Cell Res. 2001;10(5):657-660.
9. Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005;294(12):1511-1518.
10. Abdelrahman H, Almadani A, El-Menyar A, et al. Home-related falls: an underestimated mechanism of injury. J Family Community Med. 2018; 25(1):48-51.
11. Fuller GF. Falls in the elderly. Am Fam Physician. 2000;61(7):2159-2168.
